Thyroid Disorders in Pregnancy Prevalence of hypothyroidism recent






![Miscarriage Pregnancy induced hypertension [PIH] Thyroid storm Maternal complications of Hyperthyroidism in pregnancy Preterm Miscarriage Pregnancy induced hypertension [PIH] Thyroid storm Maternal complications of Hyperthyroidism in pregnancy Preterm](https://slidetodoc.com/presentation_image_h/a2994a93ddf6785479cecc161061eeab/image-31.jpg)

- Slides: 44
Thyroid Disorders in Pregnancy
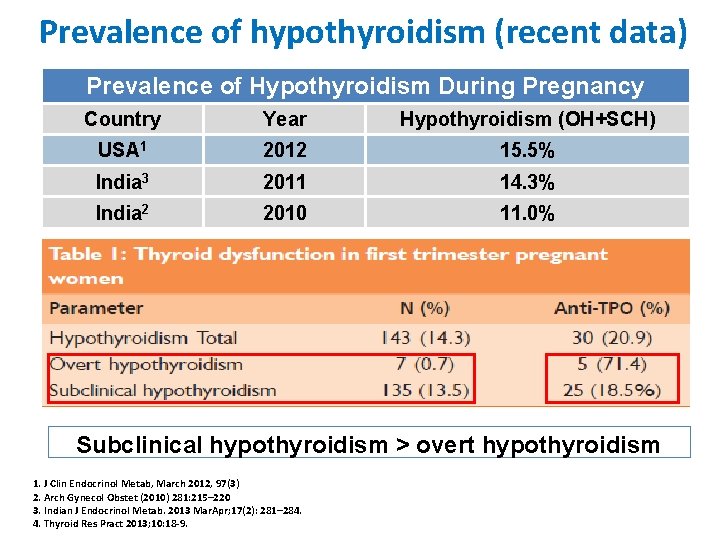
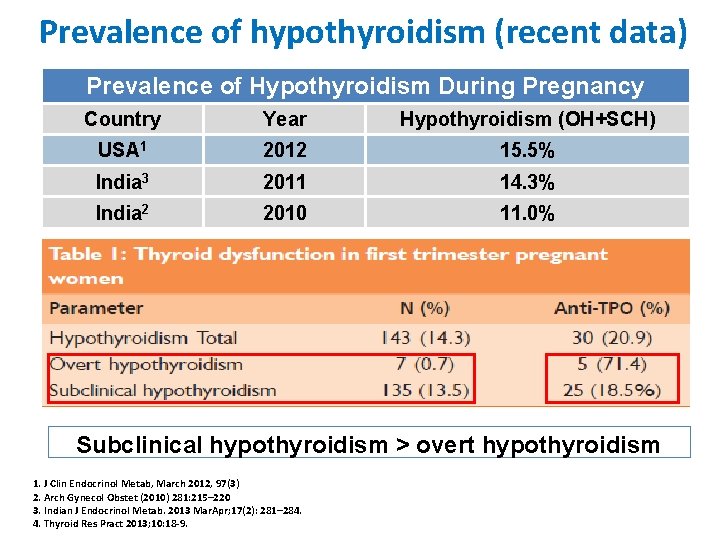
Prevalence of hypothyroidism (recent data) Prevalence of Hypothyroidism During Pregnancy Country Year Hypothyroidism (OH+SCH) USA 1 2012 15. 5% India 3 2011 14. 3% India 2 2010 11. 0% Subclinical hypothyroidism > overt hypothyroidism 1. J Clin Endocrinol Metab, March 2012, 97(3) 2. Arch Gynecol Obstet (2010) 281: 215– 220 3. Indian J Endocrinol Metab. 2013 Mar. Apr; 17(2): 281– 284. 4. Thyroid Res Pract 2013; 10: 18 -9.
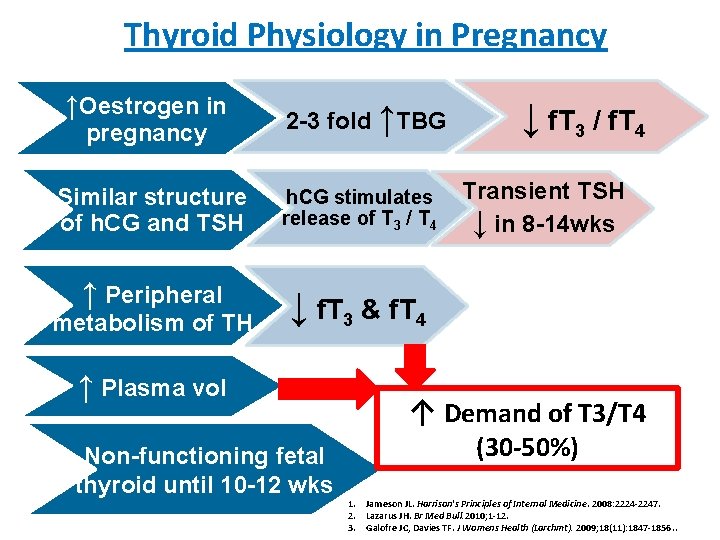
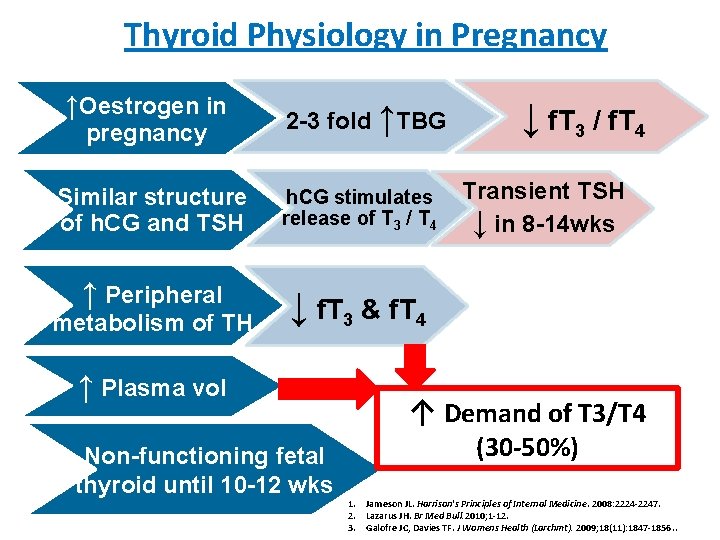
Thyroid Physiology in Pregnancy ↑Oestrogen in pregnancy 2 -3 fold ↑TBG Similar structure of h. CG and TSH h. CG stimulates release of T 3 / T 4 ↑ Peripheral ↓ f. T 3 & f. T 4 metabolism of TH ↑ Plasma vol Non-functioning fetal thyroid until 10 -12 wks ↓ f. T 3 / f. T 4 Transient TSH ↓ in 8 -14 wks ↑ Demand of T 3/T 4 (30 -50%) 1. Jameson JL. Harrison's Principles of Internal Medicine. 2008: 2224 -2247. 2. Lazarus JH. Br Med Bull. 2010; 1 -12. 3. Galofre JC, Davies TF. J Womens Health (Larchmt). 2009; 18(11): 1847 -1856. .
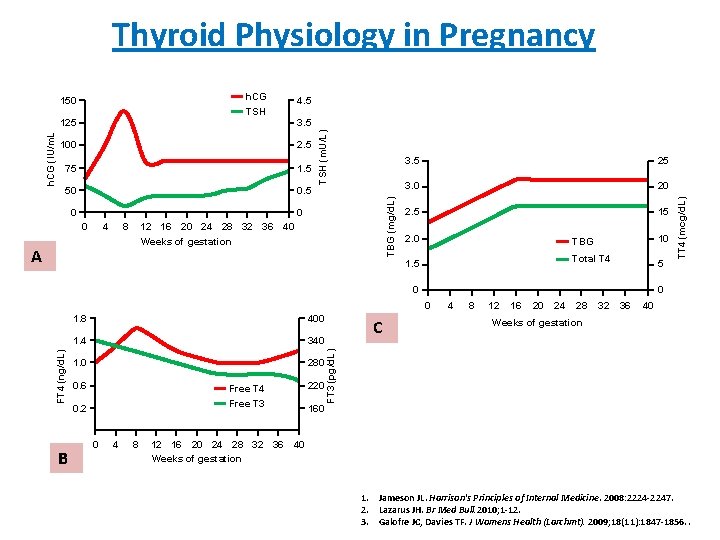
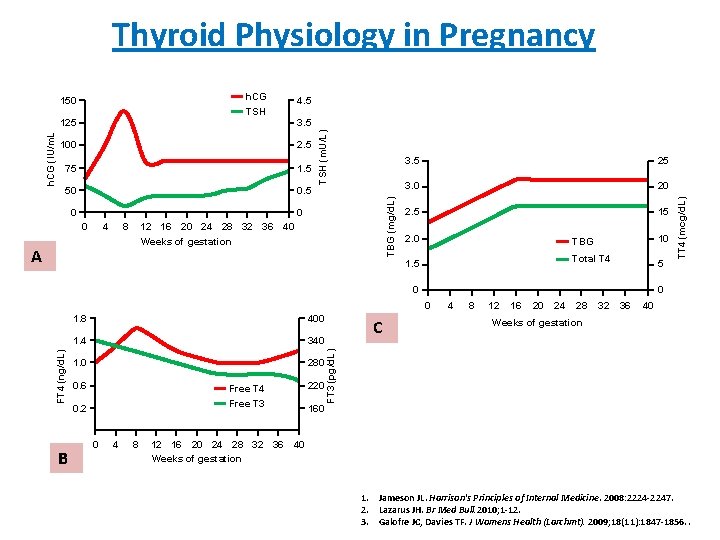
Thyroid Physiology in Pregnancy h. CG 3. 5 100 2. 5 75 1. 5 50 0. 5 0 TBG (mg/d. L) 125 0 0 4 8 12 16 20 24 28 32 36 Weeks of gestation A 40 3. 5 25 3. 0 20 2. 5 15 2. 0 10 TBG Total T 4 1. 5 5 0 0 B 400 1. 4 340 1. 0 280 0. 6 Free T 4 220 0. 2 Free T 3 160 0 4 8 C 4 8 12 16 20 24 28 32 36 40 Weeks of gestation FT 3 (pg/d. L) FT 4 (ng/d. L) 0 1. 8 TT 4 (mcg/d. L) 4. 5 TSH (m. U/L) h. CG (IU/m. L 150 12 16 20 24 28 32 36 40 Weeks of gestation 1. Jameson JL. Harrison's Principles of Internal Medicine. 2008: 2224 -2247. 2. Lazarus JH. Br Med Bull. 2010; 1 -12. 3. Galofre JC, Davies TF. J Womens Health (Larchmt). 2009; 18(11): 1847 -1856. .
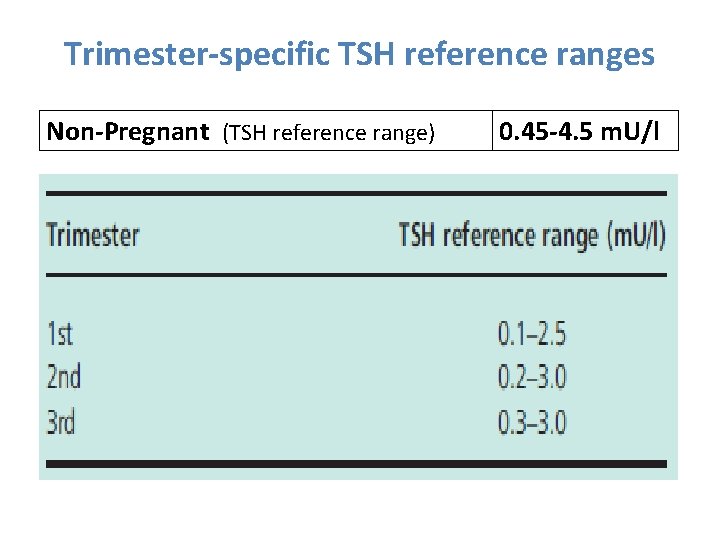
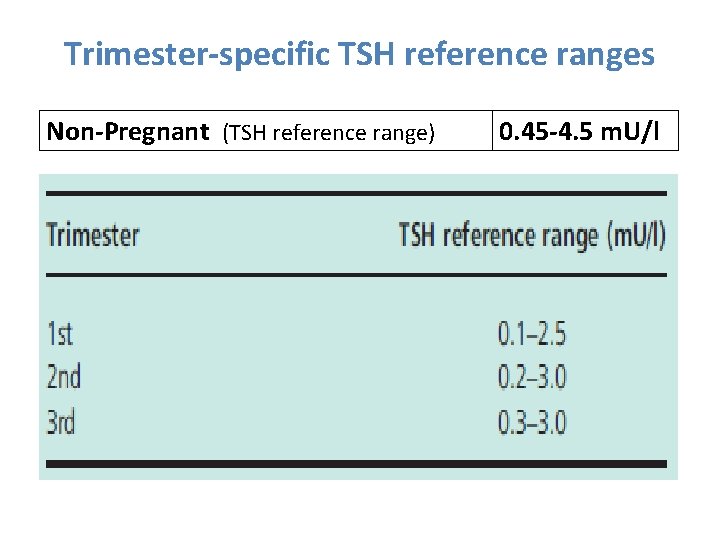
Trimester-specific TSH reference ranges Non-Pregnant (TSH reference range) 0. 45 -4. 5 m. U/l
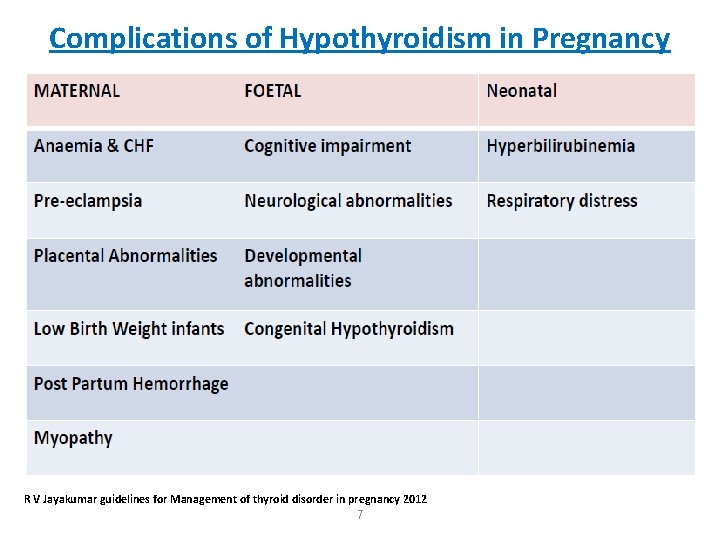
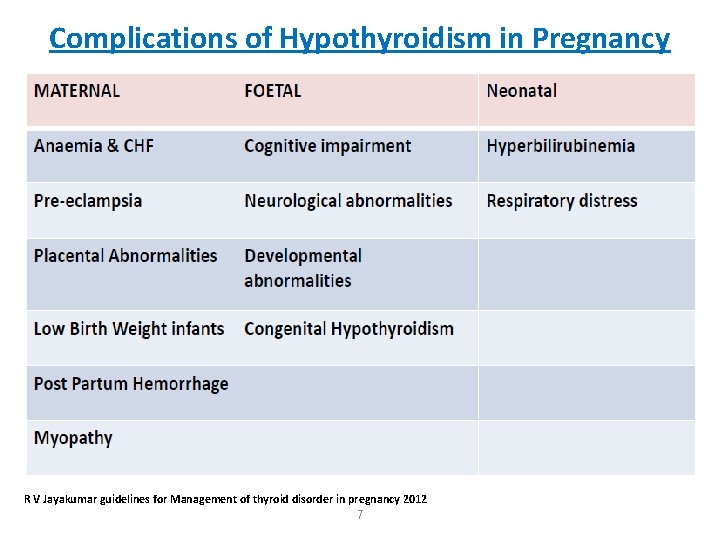
Complications of Hypothyroidism in Pregnancy R V Jayakumar guidelines for Management of thyroid disorder in pregnancy 2012 7
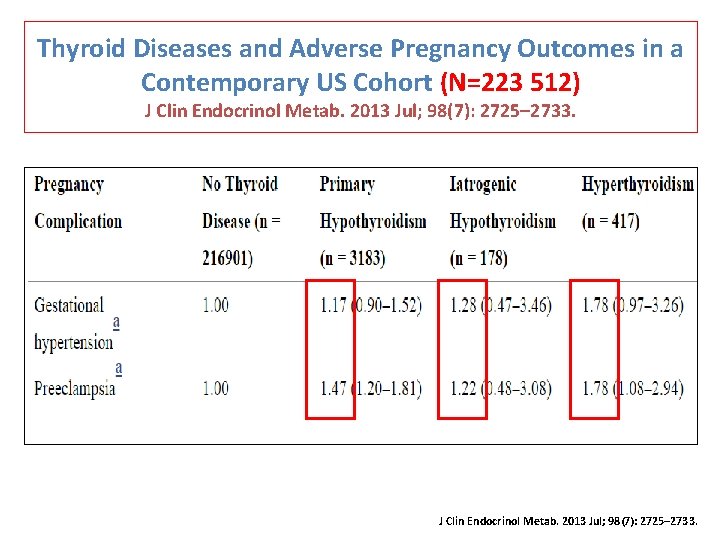
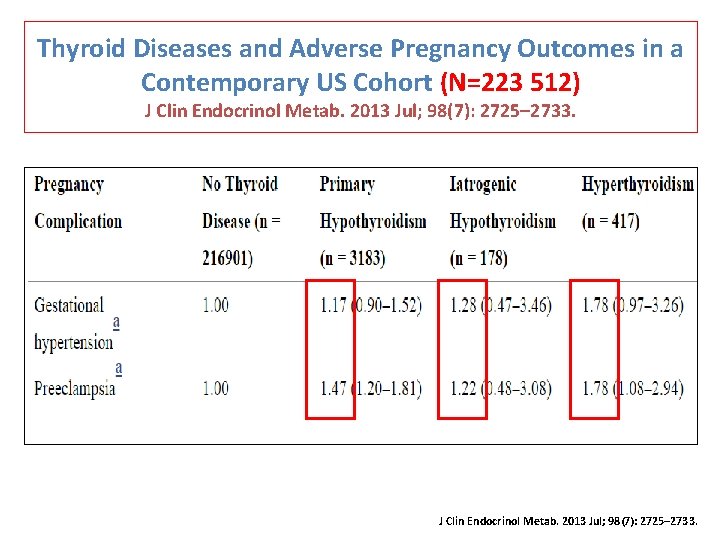
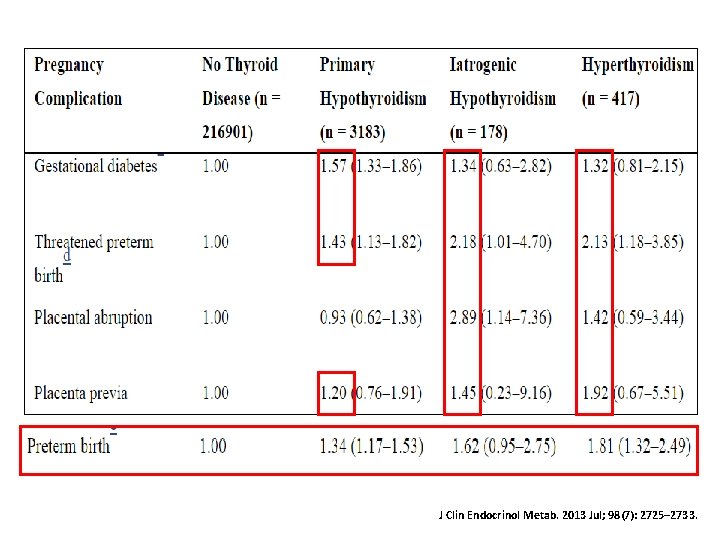
Thyroid Diseases and Adverse Pregnancy Outcomes in a Contemporary US Cohort (N=223 512) J Clin Endocrinol Metab. 2013 Jul; 98(7): 2725– 2733.
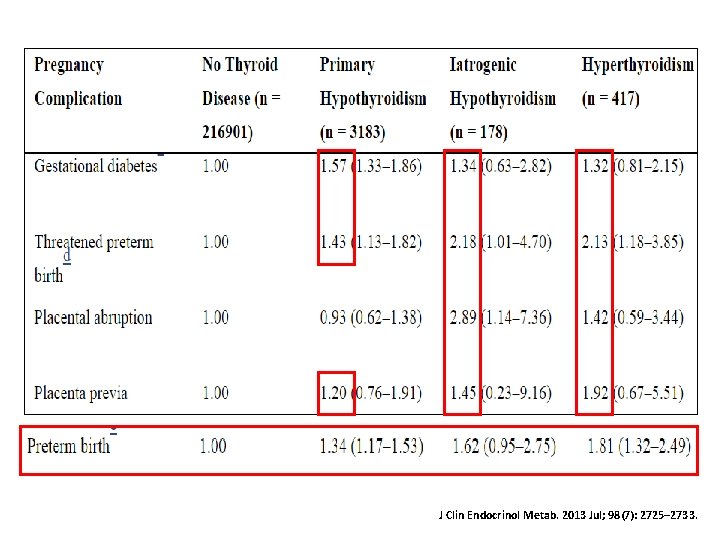
J Clin Endocrinol Metab. 2013 Jul; 98(7): 2725– 2733.
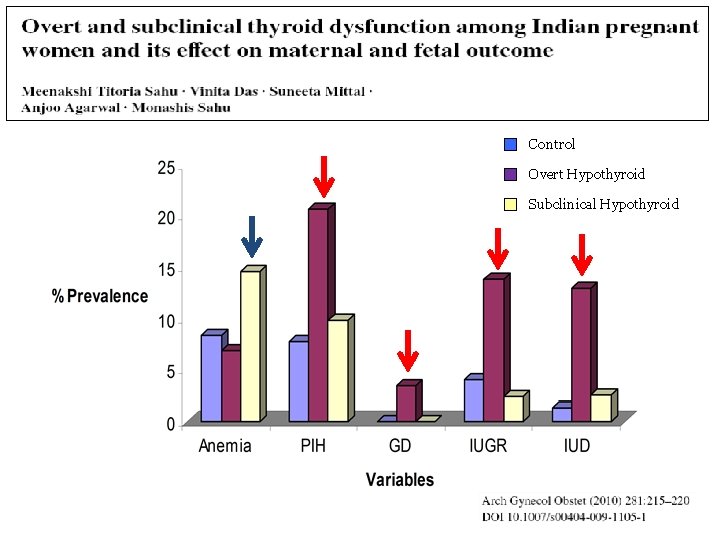
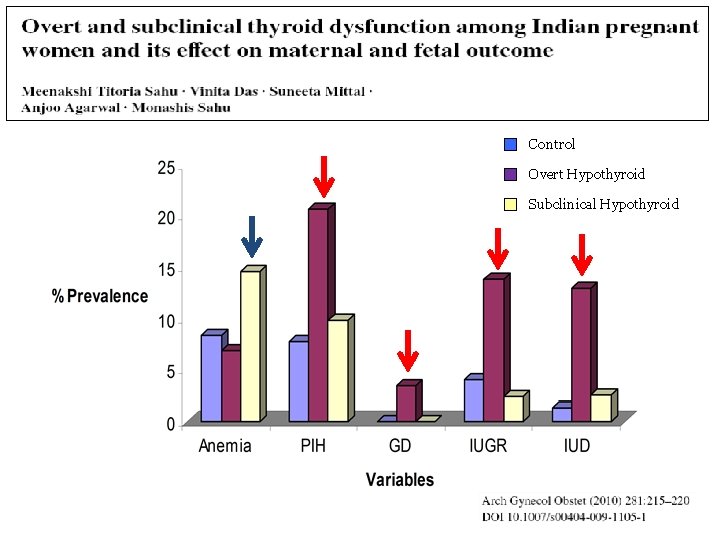
Maternal Medical & Obstetric Variables Assessed in Antenatal Period Control Overt Hypothyroid Subclinical Hypothyroid
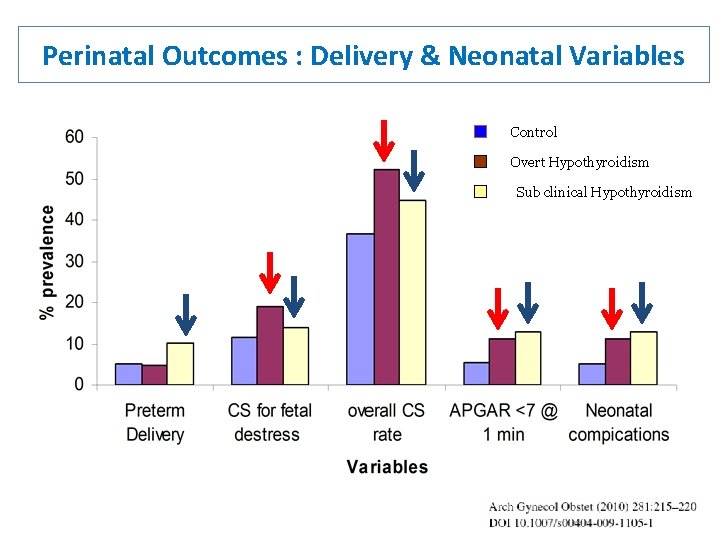
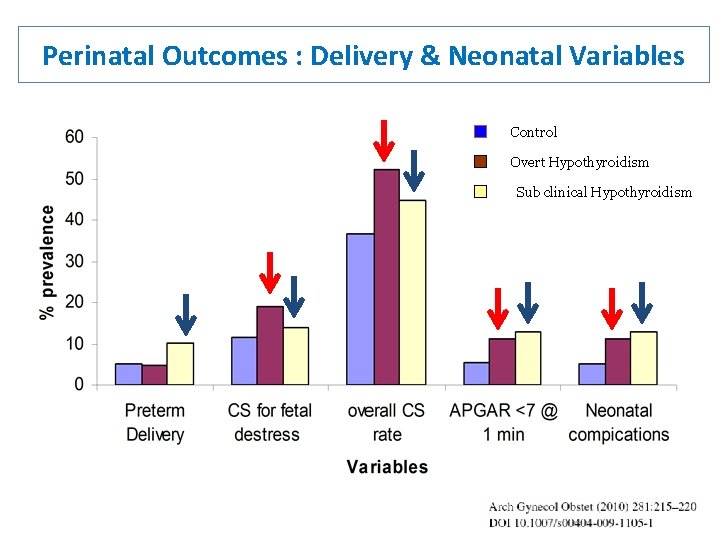
Perinatal Outcomes : Delivery & Neonatal Variables Control Overt Hypothyroidism Sub clinical Hypothyroidism
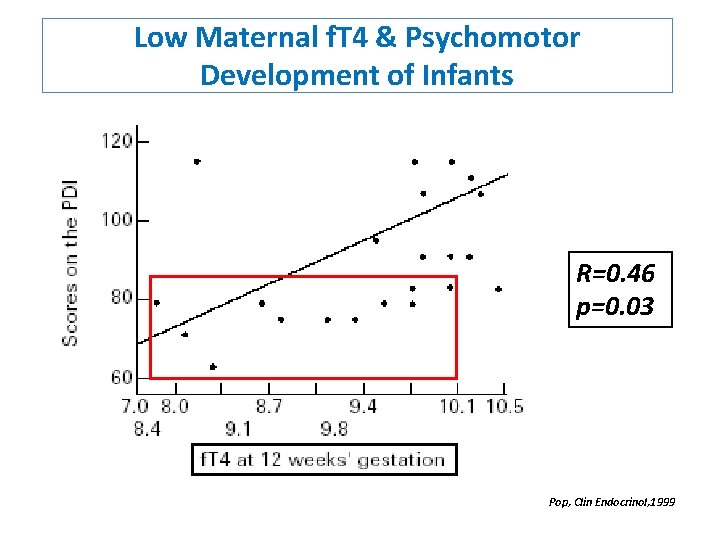
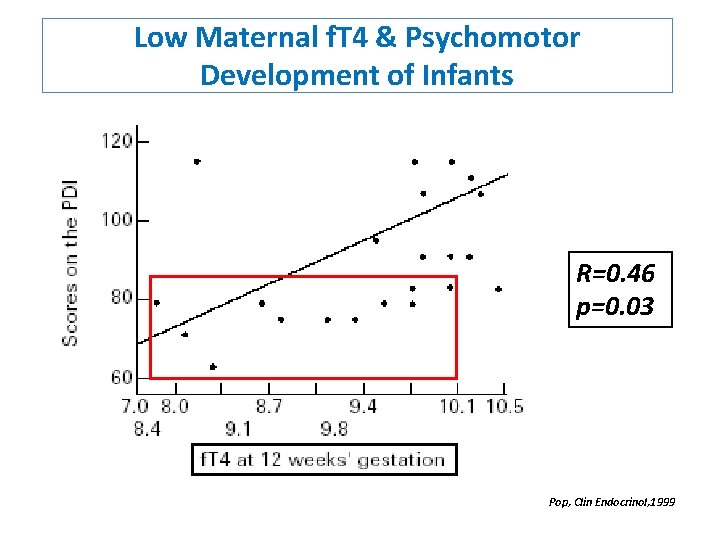
Low Maternal f. T 4 & Psychomotor Development of Infants R=0. 46 p=0. 03 Pop, Clin Endocrinol, 1999
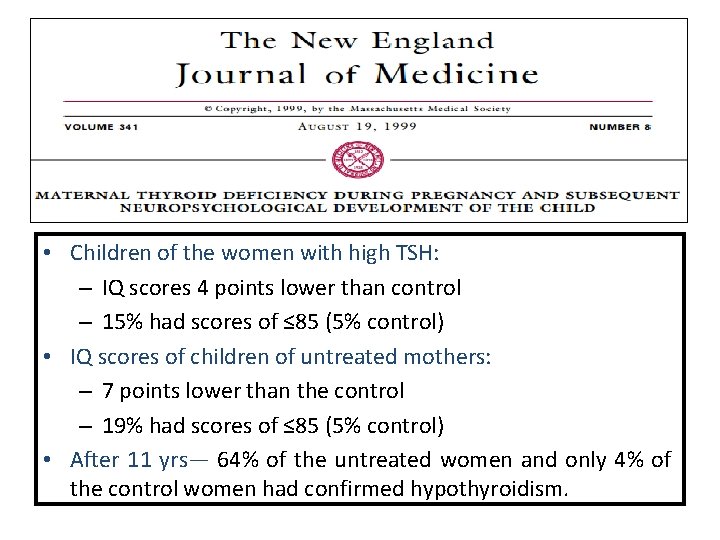
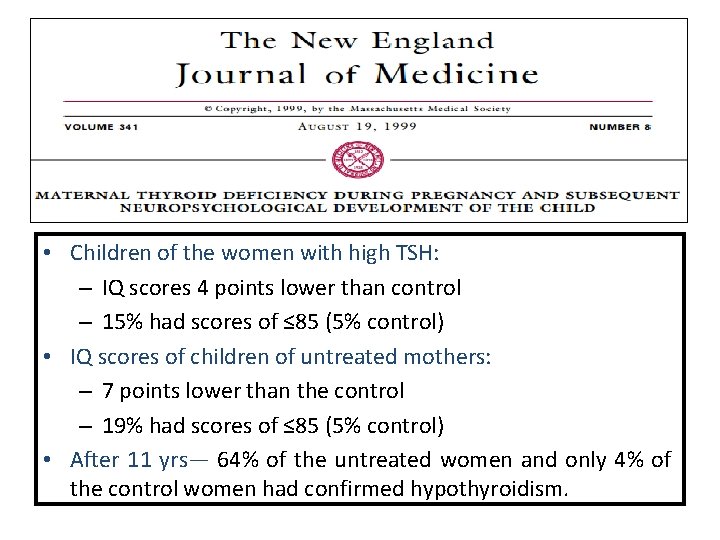
• Children of the women with high TSH: – IQ scores 4 points lower than control – 15% had scores of ≤ 85 (5% control) • IQ scores of children of untreated mothers: – 7 points lower than the control – 19% had scores of ≤ 85 (5% control) • After 11 yrs— 64% of the untreated women and only 4% of the control women had confirmed hypothyroidism.

Recurrent pregnancy loss in patients with Autoimmune thyroid dysfunction (AITD) • AITD present in around 4% of young females • TPO ab: present in 10% of women at 14 weeks§ ↑ Miscarriage § ↑ Gestational thyroid dysfunction § ↑ Postpartum thyroiditis • AITD does not interfere with normal embryo implantation • Risk of early miscarriage is substantially raised • Up to 15% are at risk with AITD Clin Obstet Gynecol. 2011; 54: 499– 505. Hormones (Athens) 2008; 7: 294– 302.

Meta analysis of thyroid antibodies and miscarriage risk (19 cohort studies) 4. 3 [2. 1 -8. 9] 9 studies 3. 1 [2. 2 -4. 4] 7 studies 4. 2 [0. 97 -18. 4] 3 studies Thangaratinam BMJ 2011 342: d 2616
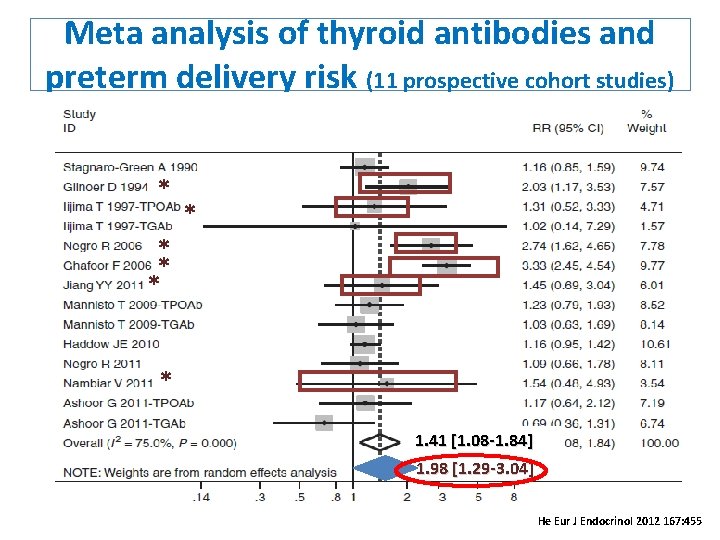
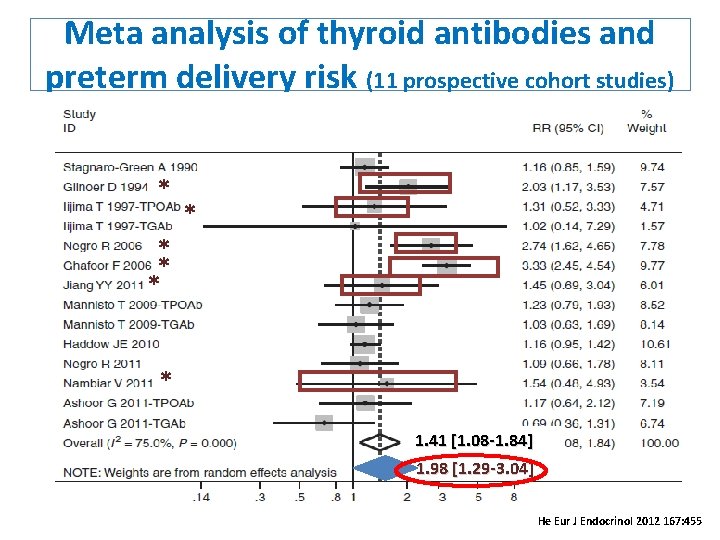
Meta analysis of thyroid antibodies and preterm delivery risk (11 prospective cohort studies) * * * 1. 41 [1. 08 -1. 84] 1. 98 [1. 29 -3. 04] He Eur J Endocrinol 2012 167: 455
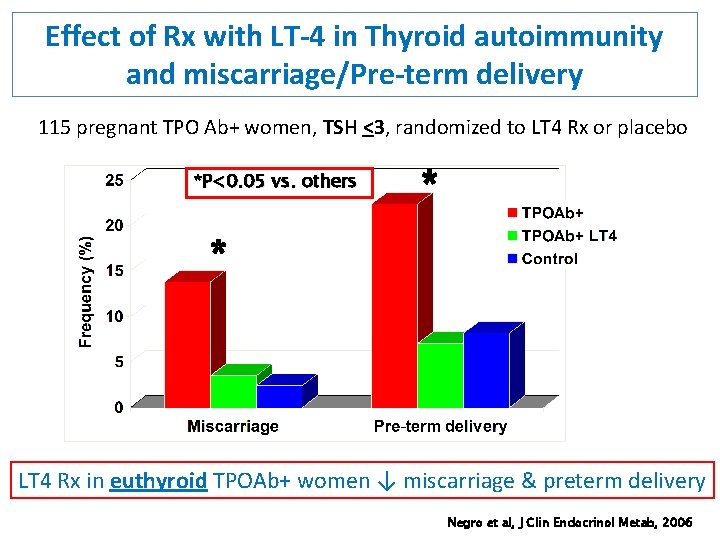
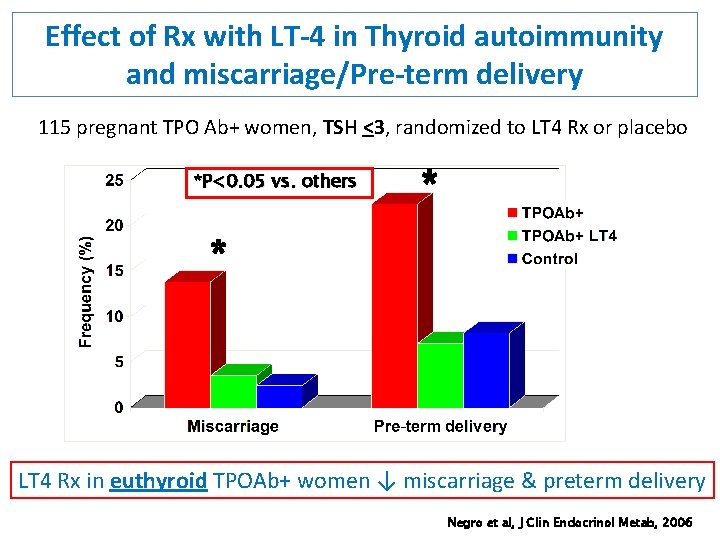
Effect of Rx with LT-4 in Thyroid autoimmunity and miscarriage/Pre-term delivery 115 pregnant TPO Ab+ women, TSH <3, randomized to LT 4 Rx or placebo *P<0. 05 vs. others * * LT 4 Rx in euthyroid TPOAb+ women ↓ miscarriage & preterm delivery Negro et al, J Clin Endocrinol Metab, 2006

Maternal Screening AACE Thyroid Guidelines (2002)- • Routine TSH before pregnancy or during 1 st trimester Endocrine Society Clinical practice guidelines (2007)- screen if: • H/O thyroid abnormalities • Family H/O thyroid abnormalities • Goiter • Thyroid auto-antibodies • Symptoms, signs suggestive of thyroid disease • Type-1 DM • Other autoimmune disorders • Infertility • Previous head or neck irradiation • H/O miscarriage or preterm delivery
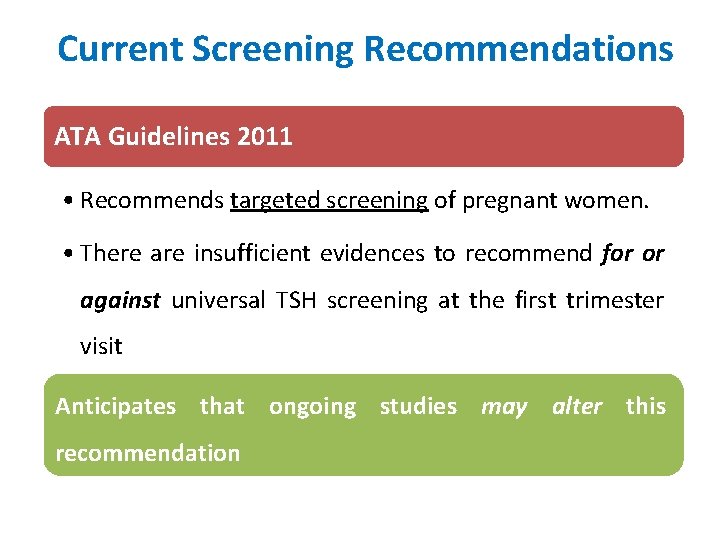
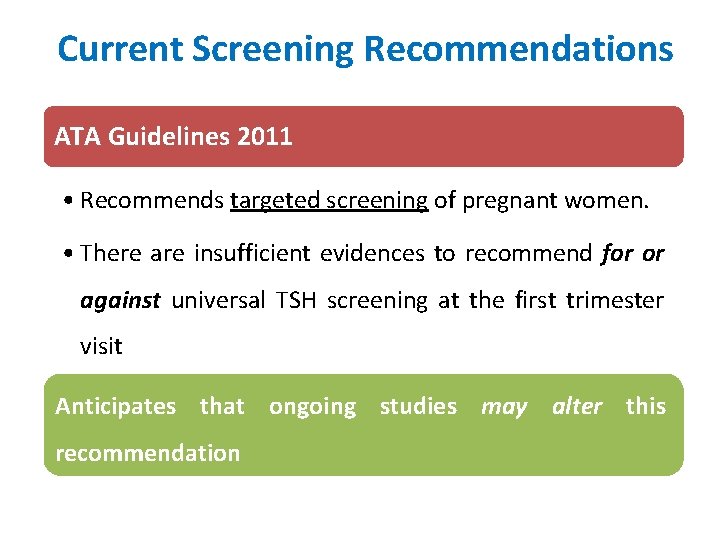
Current Screening Recommendations ATA Guidelines 2011 • Recommends targeted screening of pregnant women. • There are insufficient evidences to recommend for or against universal TSH screening at the first trimester visit Anticipates that ongoing studies may alter this recommendation

Consensus Indian Guideline on the Management of Maternal Thyroid disorders Indian Thyroid Society National task force Endocrinologists & Gynecologists Evaluated recommendations and evidence using the methodology of the United States Preventive Service Task Force (USPSTF), on the basis of the strength of evidence and magnitude of net benefit Review and endorsement by Indian Thyroid Society, Endocrine Society and FOGSI 21
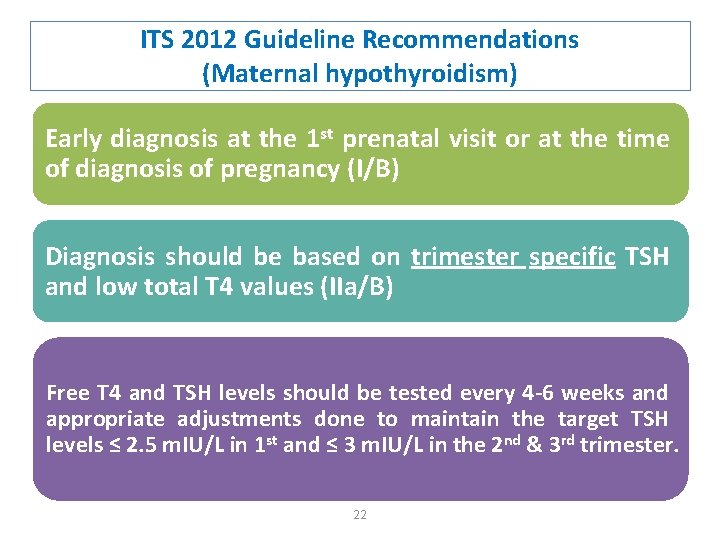
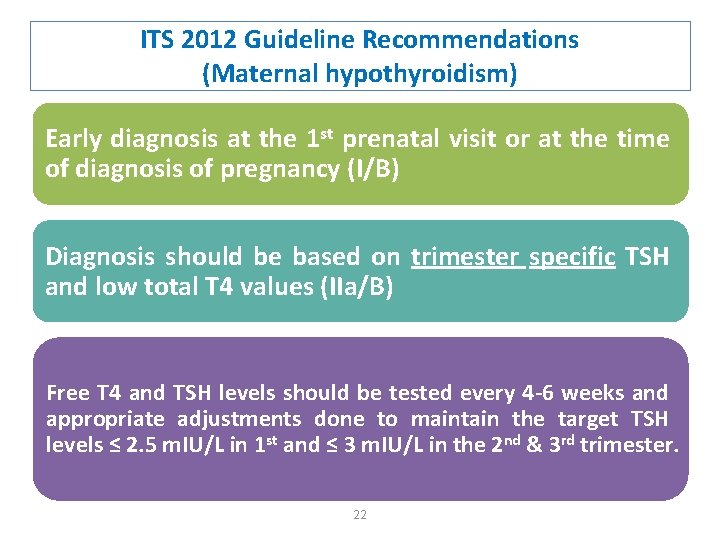
ITS 2012 Guideline Recommendations (Maternal hypothyroidism) Early diagnosis at the 1 st prenatal visit or at the time of diagnosis of pregnancy (I/B) Diagnosis should be based on trimester specific TSH and low total T 4 values (IIa/B) Free T 4 and TSH levels should be tested every 4 -6 weeks and appropriate adjustments done to maintain the target TSH levels ≤ 2. 5 m. IU/L in 1 st and ≤ 3 m. IU/L in the 2 nd & 3 rd trimester. 22

ITS 2012 Guideline Recommendations (Maternal hypothyroidism) For the following high risk groups screening should also include anti-TPO antibodies: • Personal H/O thyroid or autoimmune disorders • Family H/O thyroid disease • Women with goiter • H/O miscarriage or preterm delivery Subclinical hypothyroidism has been shown to be associated with an adverse outcome for both the mother and offspring and hence should be treated with LT 4 (I/B)
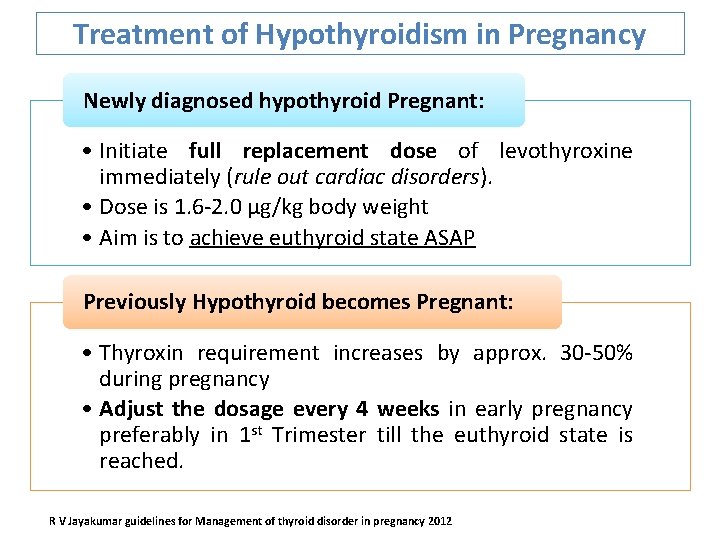
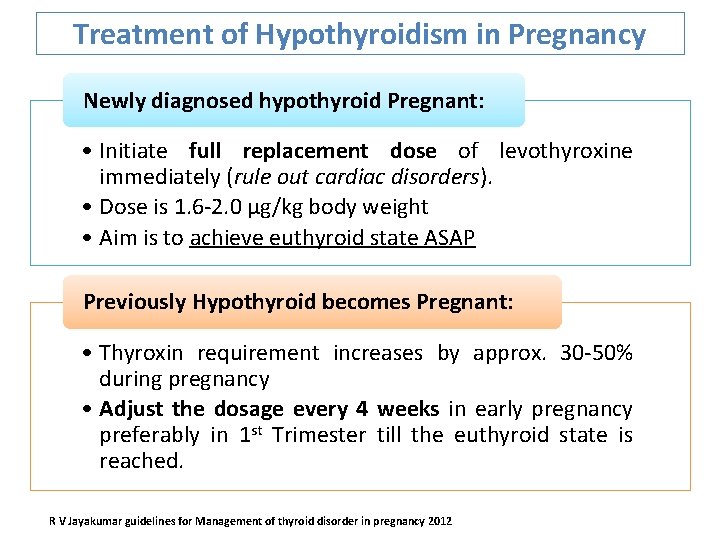
Treatment of Hypothyroidism in Pregnancy Newly diagnosed hypothyroid Pregnant: • Initiate full replacement dose of levothyroxine immediately (rule out cardiac disorders). • Dose is 1. 6 -2. 0 μg/kg body weight • Aim is to achieve euthyroid state ASAP Previously Hypothyroid becomes Pregnant: • Thyroxin requirement increases by approx. 30 -50% during pregnancy • Adjust the dosage every 4 weeks in early pregnancy preferably in 1 st Trimester till the euthyroid state is reached. R V Jayakumar guidelines for Management of thyroid disorder in pregnancy 2012
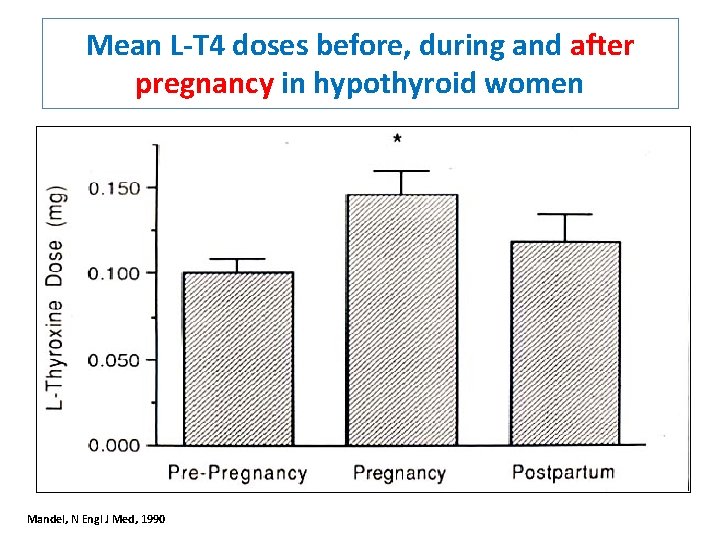
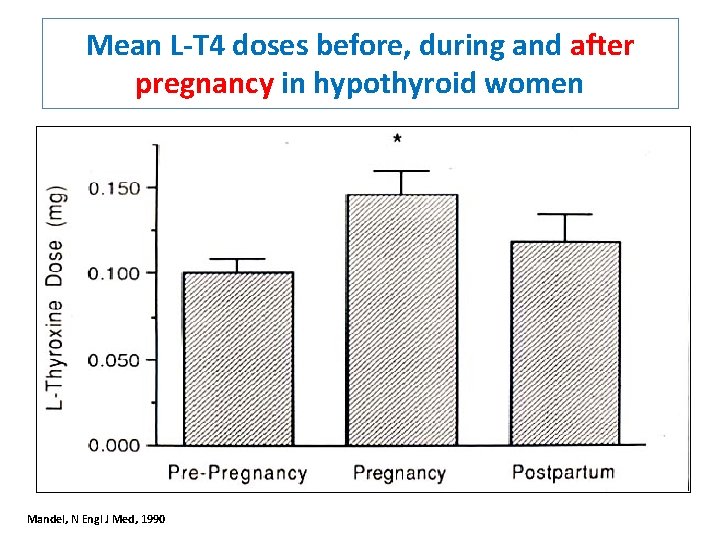
Mean L-T 4 doses before, during and after pregnancy in hypothyroid women Mandel, N Engl J Med, 1990

Hyperthyroidism in Pregnancy
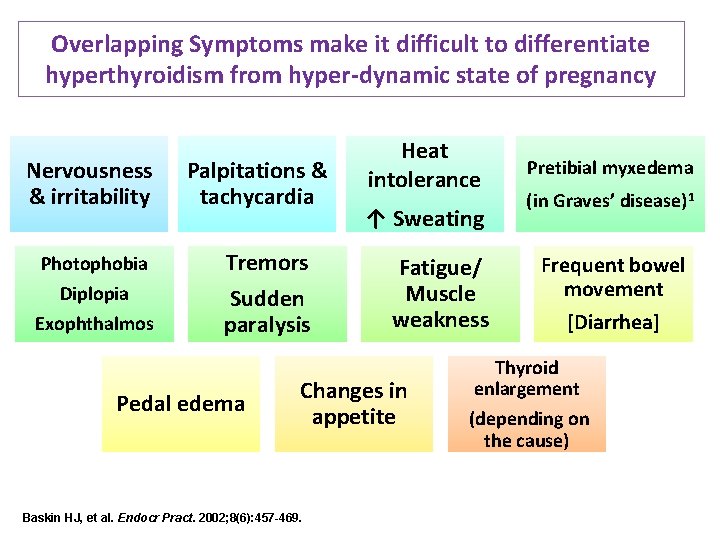
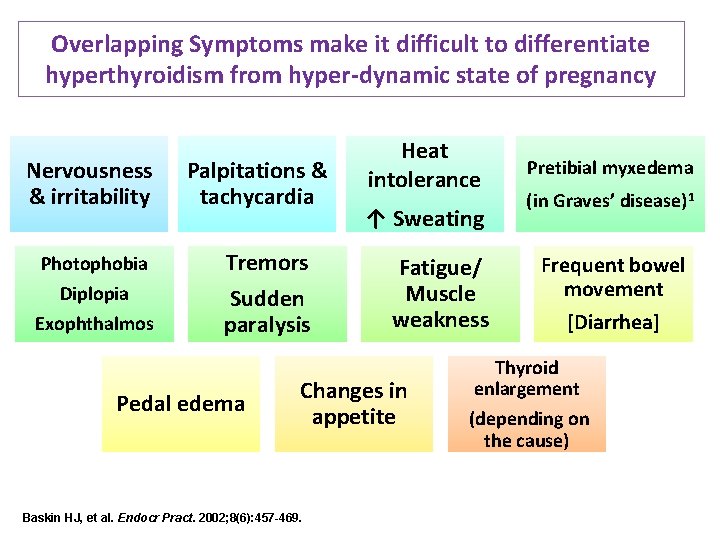
Overlapping Symptoms make it difficult to differentiate hyperthyroidism from hyper-dynamic state of pregnancy Nervousness & irritability Photophobia Diplopia Exophthalmos Palpitations & tachycardia Tremors Sudden paralysis Pedal edema Heat intolerance ↑ Sweating Fatigue/ Muscle weakness Changes in appetite Baskin HJ, et al. Endocr Pract. 2002; 8(6): 457 -469. Pretibial myxedema (in Graves’ disease)1 Frequent bowel movement [Diarrhea] Thyroid enlargement (depending on the cause)
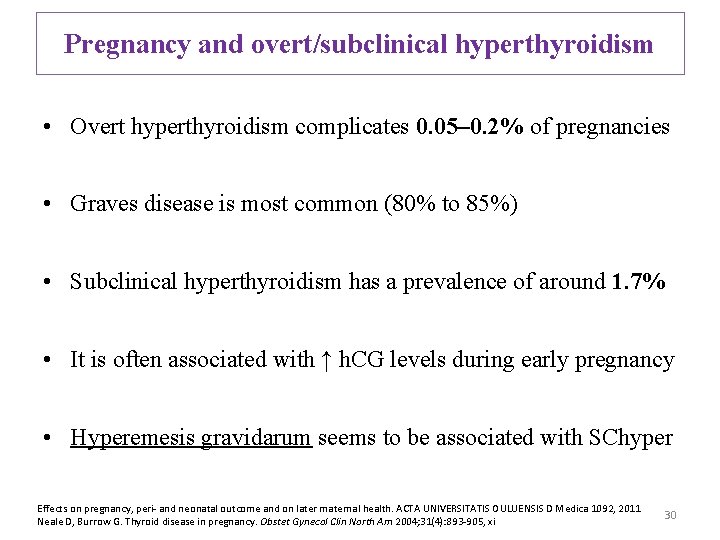
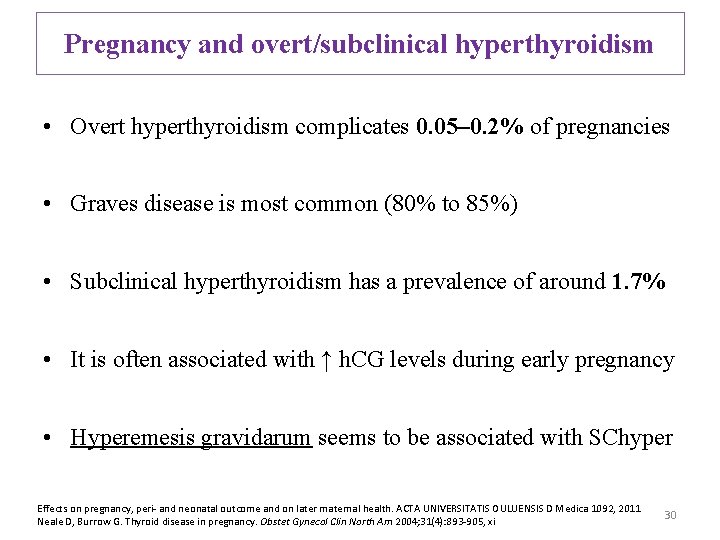
Pregnancy and overt/subclinical hyperthyroidism • Overt hyperthyroidism complicates 0. 05– 0. 2% of pregnancies • Graves disease is most common (80% to 85%) • Subclinical hyperthyroidism has a prevalence of around 1. 7% • It is often associated with ↑ h. CG levels during early pregnancy • Hyperemesis gravidarum seems to be associated with SChyper Effects on pregnancy, peri- and neonatal outcome and on later maternal health. ACTA UNIVERSITATIS OULUENSIS D Medica 1092, 2011 Neale D, Burrow G. Thyroid disease in pregnancy. Obstet Gynecol Clin North Am 2004; 31(4): 893 -905, xi 30
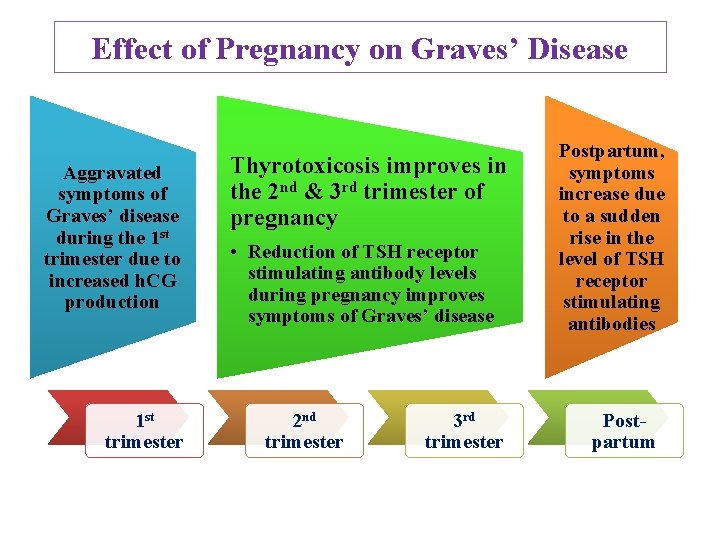
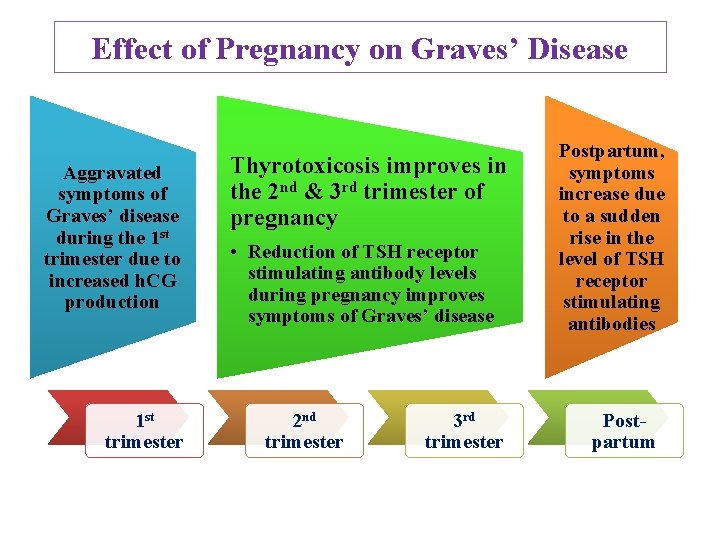
Effect of Pregnancy on Graves’ Disease Aggravated symptoms of Graves’ disease during the 1 st trimester due to increased h. CG production 1 st trimester Thyrotoxicosis improves in the 2 nd & 3 rd trimester of pregnancy • Reduction of TSH receptor stimulating antibody levels during pregnancy improves symptoms of Graves’ disease 2 nd trimester 3 rd trimester Postpartum, symptoms increase due to a sudden rise in the level of TSH receptor stimulating antibodies Postpartum
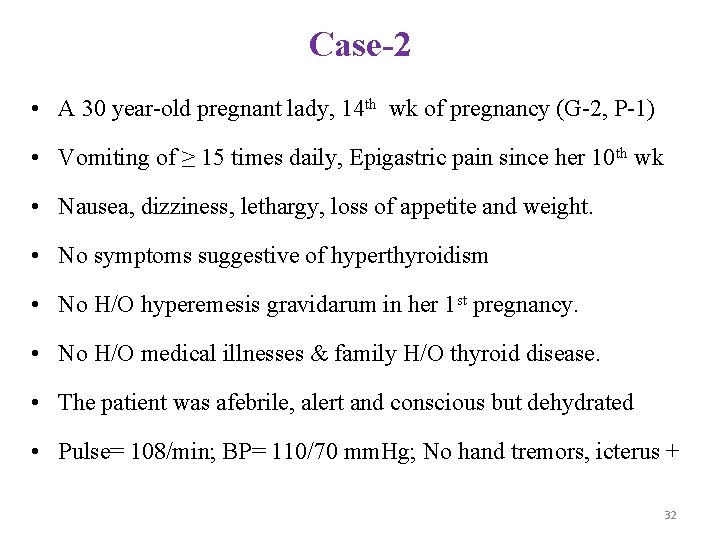
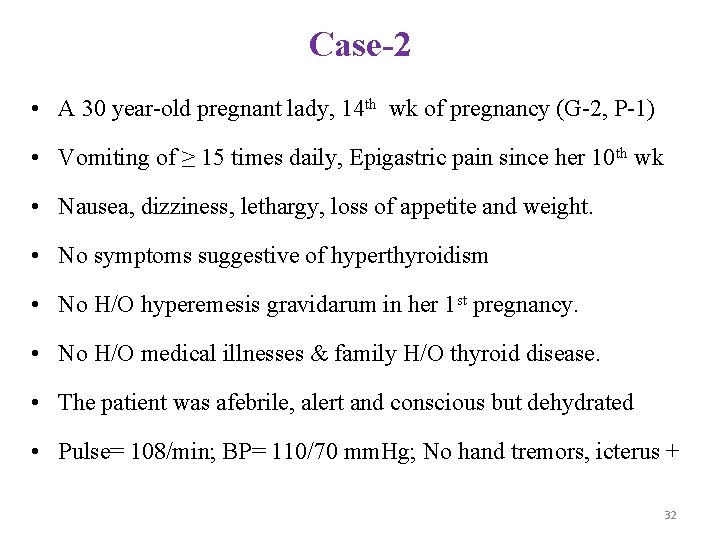
Case-2 • A 30 year-old pregnant lady, 14 th wk of pregnancy (G-2, P-1) • Vomiting of ≥ 15 times daily, Epigastric pain since her 10 th wk • Nausea, dizziness, lethargy, loss of appetite and weight. • No symptoms suggestive of hyperthyroidism • No H/O hyperemesis gravidarum in her 1 st pregnancy. • No H/O medical illnesses & family H/O thyroid disease. • The patient was afebrile, alert and conscious but dehydrated • Pulse= 108/min; BP= 110/70 mm. Hg; No hand tremors, icterus + 32
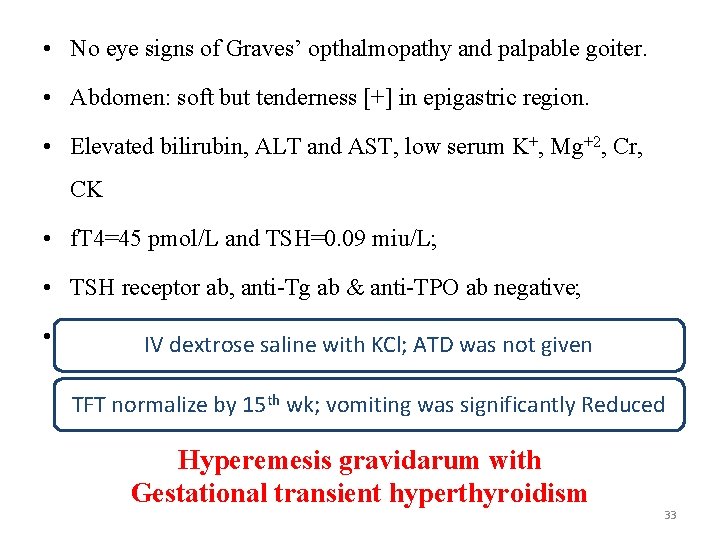
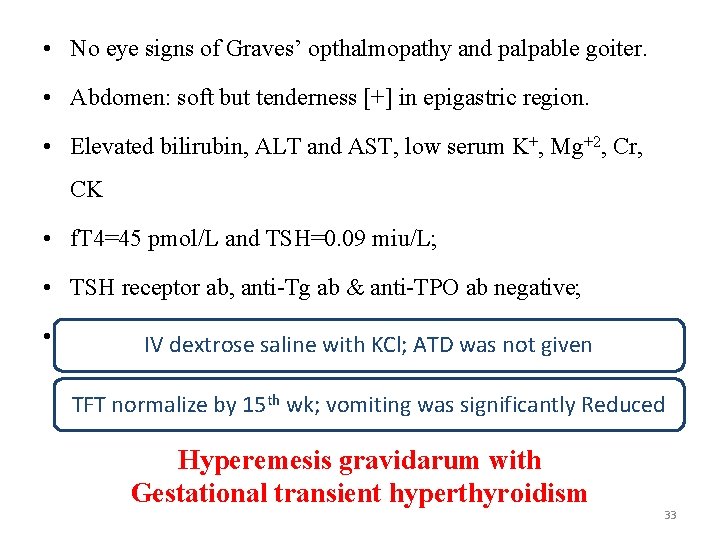
• No eye signs of Graves’ opthalmopathy and palpable goiter. • Abdomen: soft but tenderness [+] in epigastric region. • Elevated bilirubin, ALT and AST, low serum K+, Mg+2, Cr, CK • f. T 4=45 pmol/L and TSH=0. 09 miu/L; • TSH receptor ab, anti-Tg ab & anti-TPO ab negative; • Hepatitis B, C non-reactive. IVA, dextrose saline with KCl; ATD was not given TFT normalize by 15 th wk; vomiting was significantly Reduced Hyperemesis gravidarum with Gestational transient hyperthyroidism 33
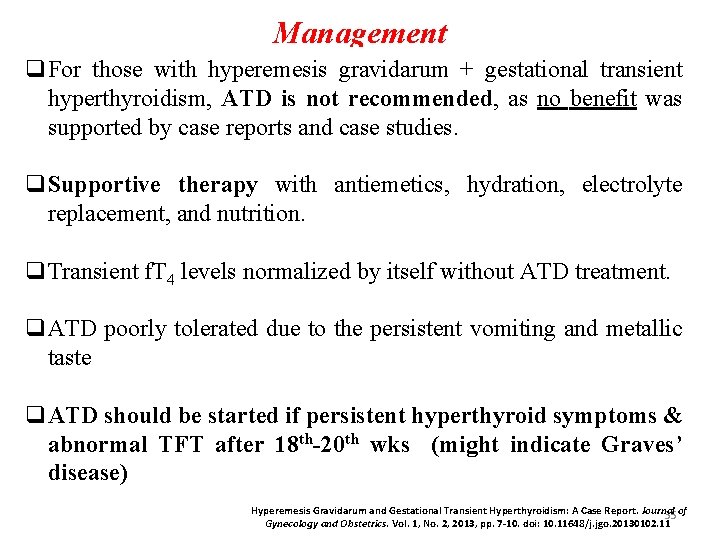
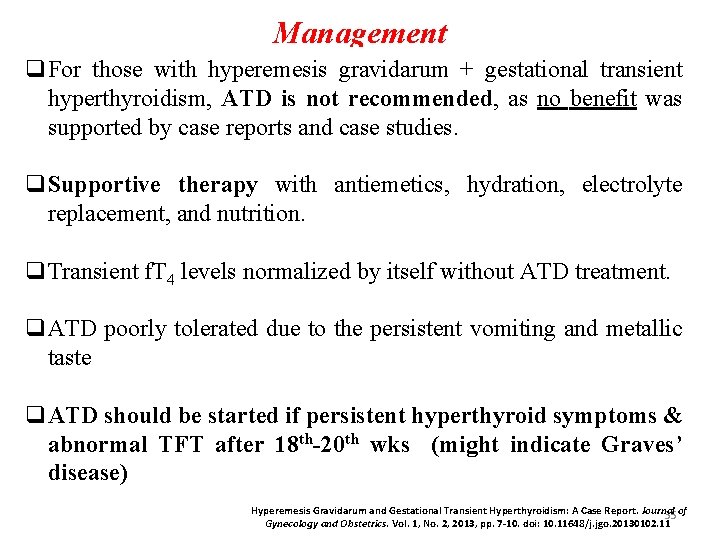
Management q. For those with hyperemesis gravidarum + gestational transient hyperthyroidism, ATD is not recommended, as no benefit was supported by case reports and case studies. q. Supportive therapy with antiemetics, hydration, electrolyte replacement, and nutrition. q. Transient f. T 4 levels normalized by itself without ATD treatment. q. ATD poorly tolerated due to the persistent vomiting and metallic taste q. ATD should be started if persistent hyperthyroid symptoms & abnormal TFT after 18 th-20 th wks (might indicate Graves’ disease) Hyperemesis Gravidarum and Gestational Transient Hyperthyroidism: A Case Report. Journal 35 of Gynecology and Obstetrics. Vol. 1, No. 2, 2013, pp. 7 -10. doi: 10. 11648/j. jgo. 20130102. 11
![Miscarriage Pregnancy induced hypertension PIH Thyroid storm Maternal complications of Hyperthyroidism in pregnancy Preterm Miscarriage Pregnancy induced hypertension [PIH] Thyroid storm Maternal complications of Hyperthyroidism in pregnancy Preterm](https://slidetodoc.com/presentation_image_h/a2994a93ddf6785479cecc161061eeab/image-31.jpg)
Miscarriage Pregnancy induced hypertension [PIH] Thyroid storm Maternal complications of Hyperthyroidism in pregnancy Preterm labour Heart failure Placental abruption 36
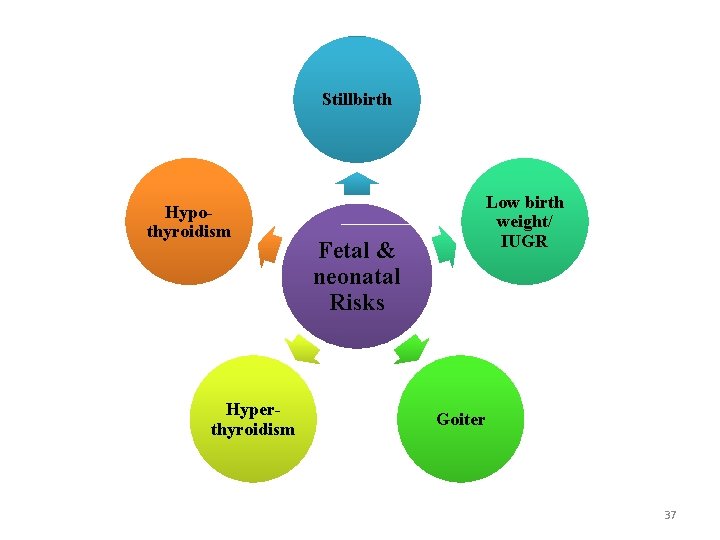
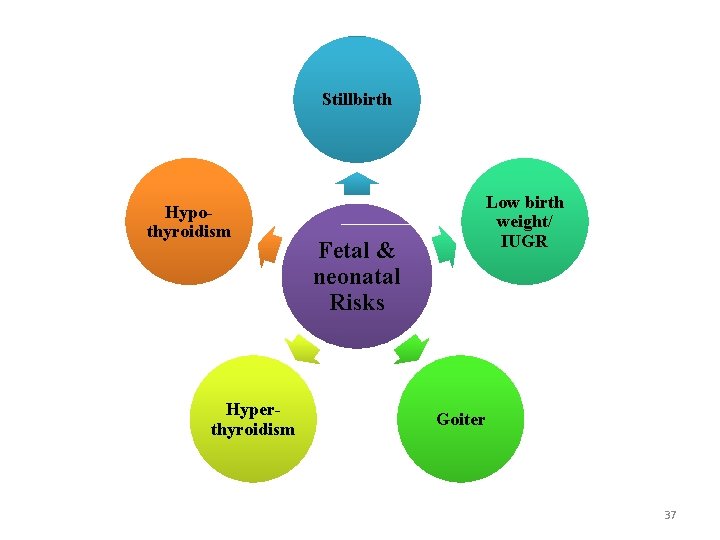
Stillbirth Hypothyroidism Hyperthyroidism Low birth weight/ IUGR Fetal & neonatal Risks Goiter 37
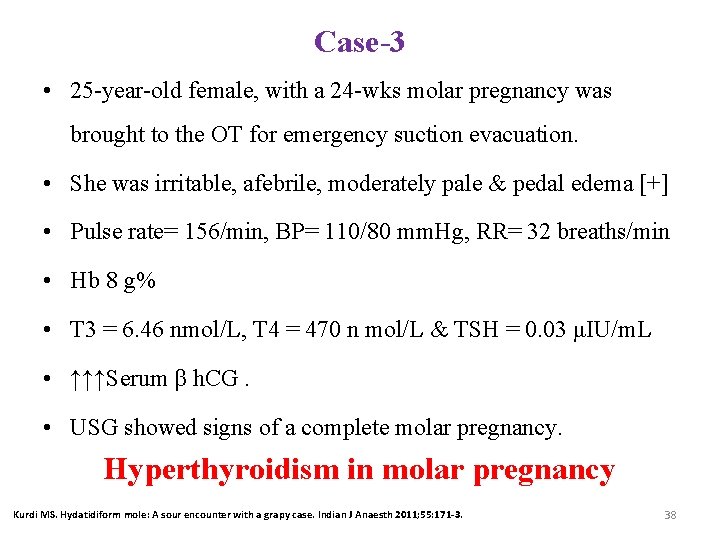
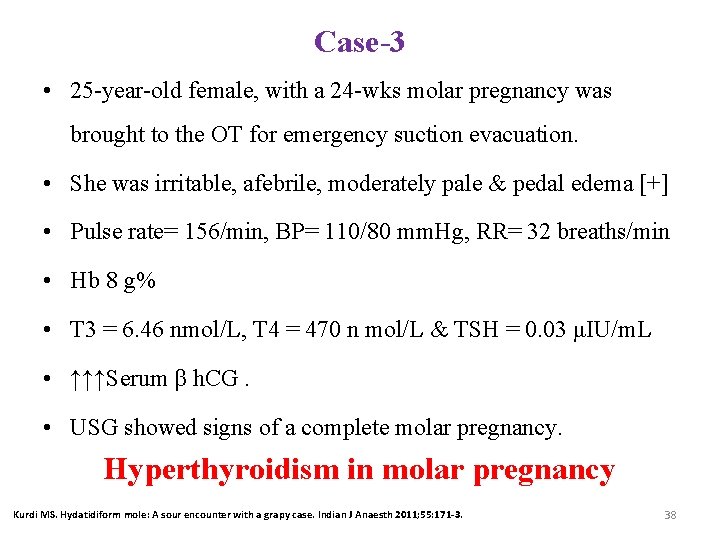
Case-3 • 25 -year-old female, with a 24 -wks molar pregnancy was brought to the OT for emergency suction evacuation. • She was irritable, afebrile, moderately pale & pedal edema [+] • Pulse rate= 156/min, BP= 110/80 mm. Hg, RR= 32 breaths/min • Hb 8 g% • T 3 = 6. 46 nmol/L, T 4 = 470 n mol/L & TSH = 0. 03 μIU/m. L • ↑↑↑Serum β h. CG. • USG showed signs of a complete molar pregnancy. Hyperthyroidism in molar pregnancy Kurdi MS. Hydatidiform mole: A sour encounter with a grapy case. Indian J Anaesth 2011; 55: 171 -3. 38
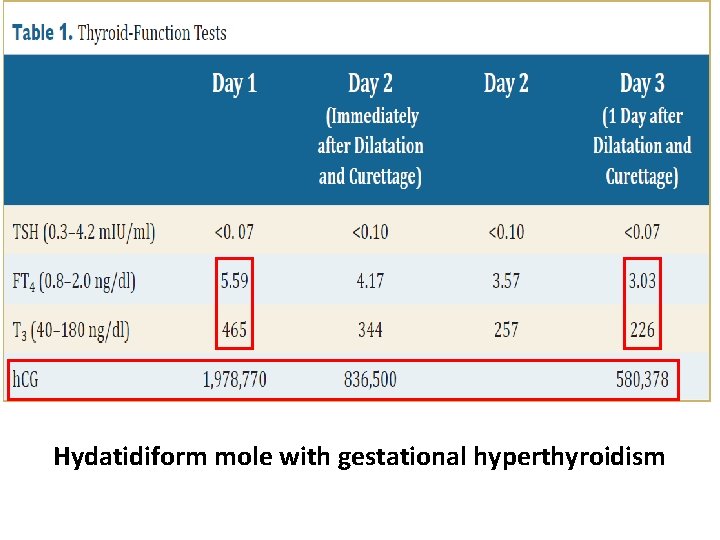
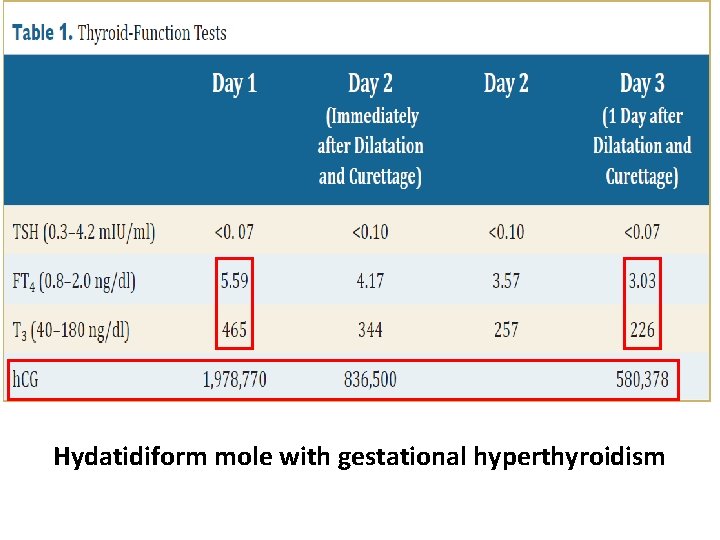
Hydatidiform mole with gestational hyperthyroidism
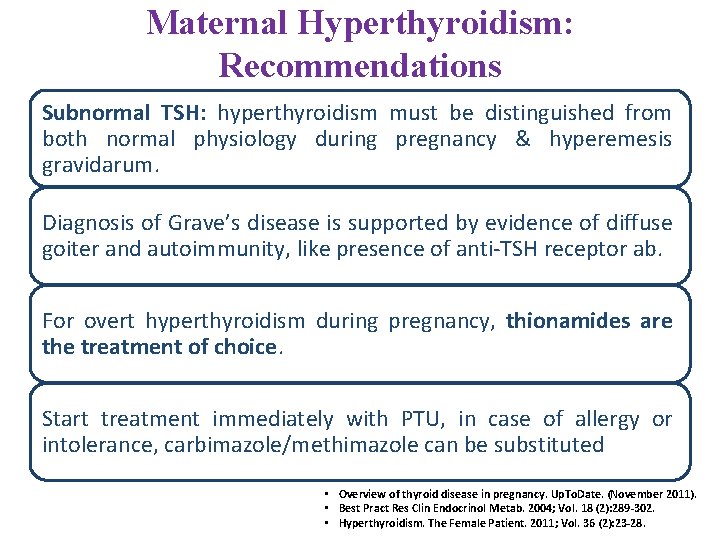
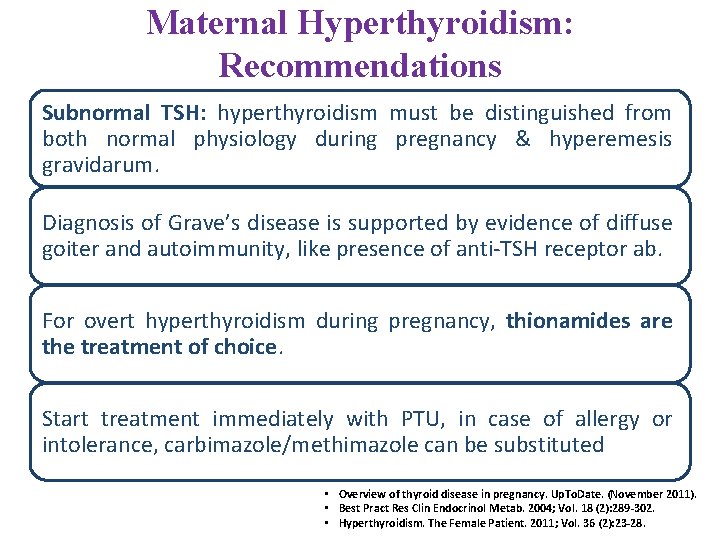
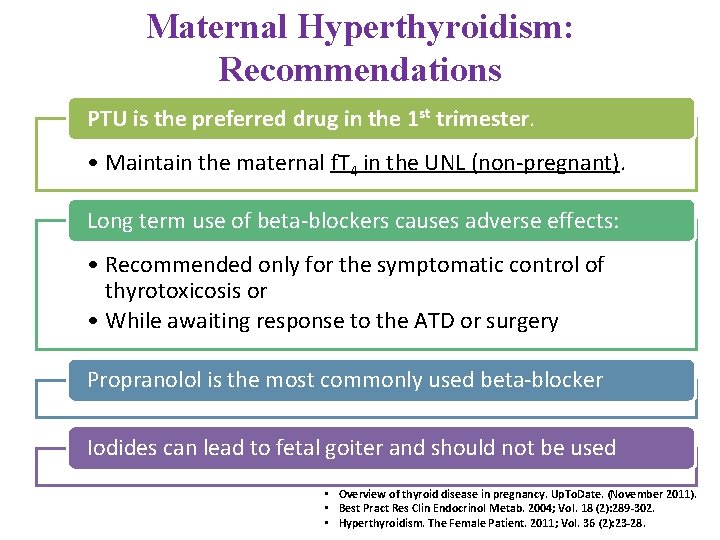
Maternal Hyperthyroidism: Recommendations Subnormal TSH: hyperthyroidism must be distinguished from both normal physiology during pregnancy & hyperemesis gravidarum. Diagnosis of Grave’s disease is supported by evidence of diffuse goiter and autoimmunity, like presence of anti-TSH receptor ab. For overt hyperthyroidism during pregnancy, thionamides are the treatment of choice. Start treatment immediately with PTU, in case of allergy or intolerance, carbimazole/methimazole can be substituted • Overview of thyroid disease in pregnancy. Up. To. Date. (November 2011). • Best Pract Res Clin Endocrinol Metab. 2004; Vol. 18 (2): 289 -302. • Hyperthyroidism. The Female Patient. 2011; Vol. 36 (2): 23 -28.
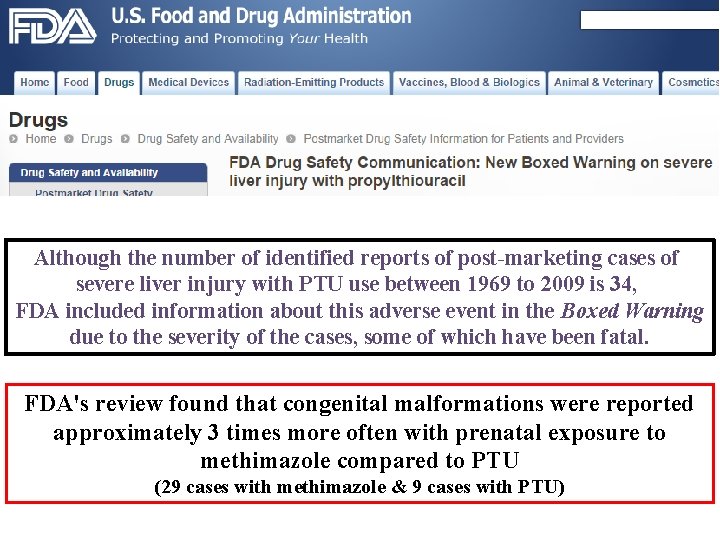
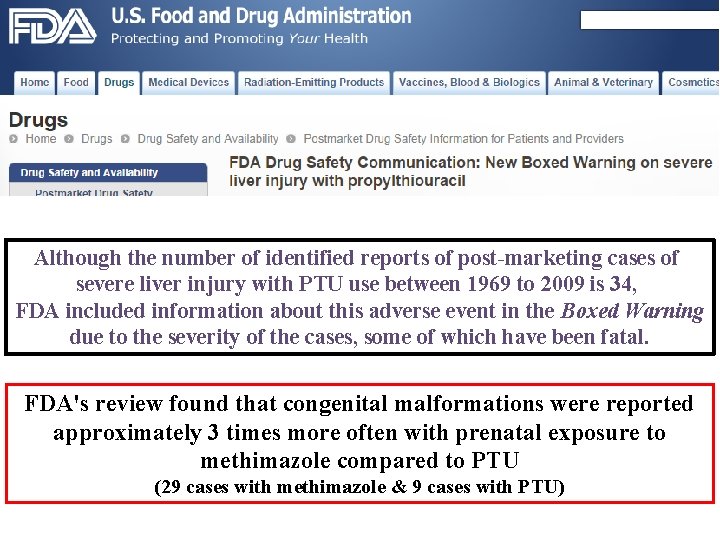
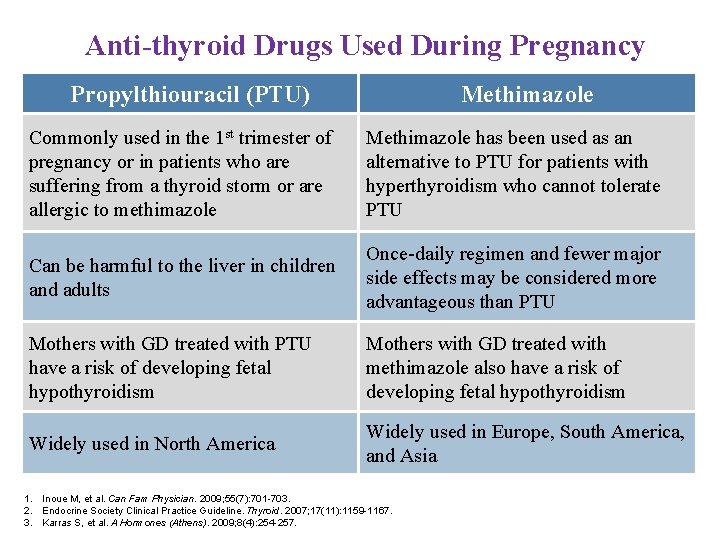
Although the number of identified reports of post-marketing cases of severe liver injury with PTU use between 1969 to 2009 is 34, FDA included information about this adverse event in the Boxed Warning due to the severity of the cases, some of which have been fatal. FDA's review found that congenital malformations were reported approximately 3 times more often with prenatal exposure to methimazole compared to PTU (29 cases with methimazole & 9 cases with PTU)
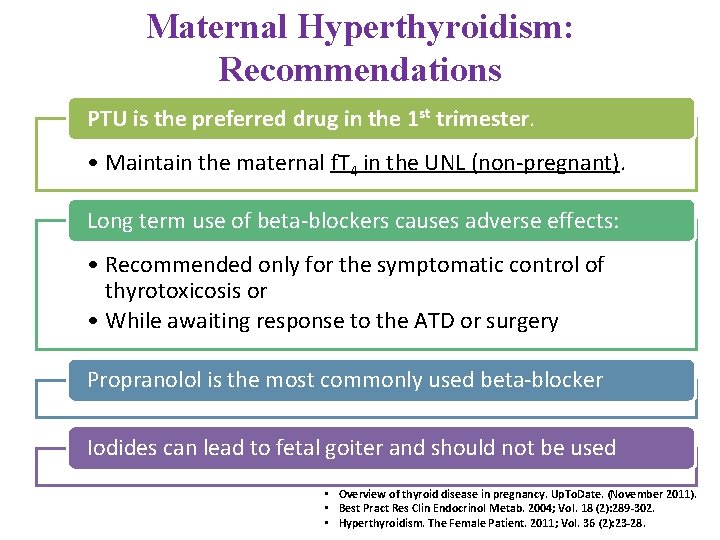
Maternal Hyperthyroidism: Recommendations PTU is the preferred drug in the 1 st trimester. • Maintain the maternal f. T 4 in the UNL (non-pregnant). Long term use of beta-blockers causes adverse effects: • Recommended only for the symptomatic control of thyrotoxicosis or • While awaiting response to the ATD or surgery Propranolol is the most commonly used beta-blocker Iodides can lead to fetal goiter and should not be used • Overview of thyroid disease in pregnancy. Up. To. Date. (November 2011). • Best Pract Res Clin Endocrinol Metab. 2004; Vol. 18 (2): 289 -302. • Hyperthyroidism. The Female Patient. 2011; Vol. 36 (2): 23 -28.
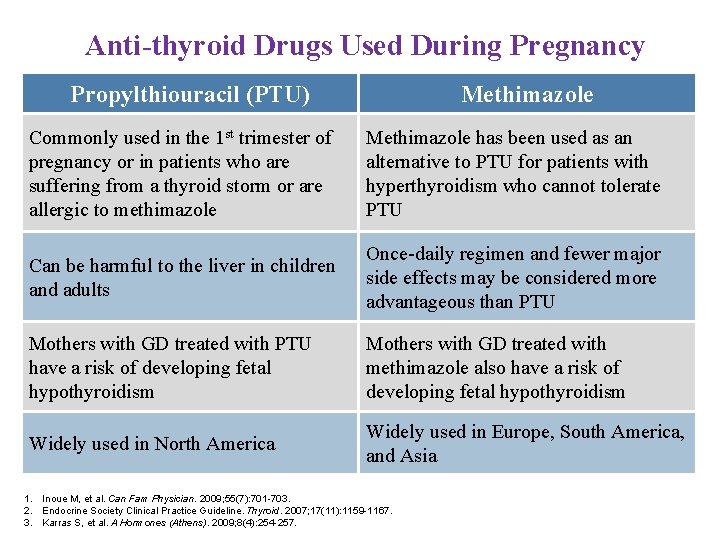
Anti-thyroid Drugs Used During Pregnancy Propylthiouracil (PTU) Methimazole Commonly used in the 1 st trimester of pregnancy or in patients who are suffering from a thyroid storm or are allergic to methimazole Methimazole has been used as an alternative to PTU for patients with hyperthyroidism who cannot tolerate PTU Can be harmful to the liver in children and adults Once-daily regimen and fewer major side effects may be considered more advantageous than PTU Mothers with GD treated with PTU have a risk of developing fetal hypothyroidism Mothers with GD treated with methimazole also have a risk of developing fetal hypothyroidism Widely used in North America Widely used in Europe, South America, and Asia 1. Inoue M, et al. Can Fam Physician. 2009; 55(7): 701 -703. 2. Endocrine Society Clinical Practice Guideline. Thyroid. 2007; 17(11): 1159 -1167. 3. Karras S, et al. A Hormones (Athens). 2009; 8(4): 254 -257.
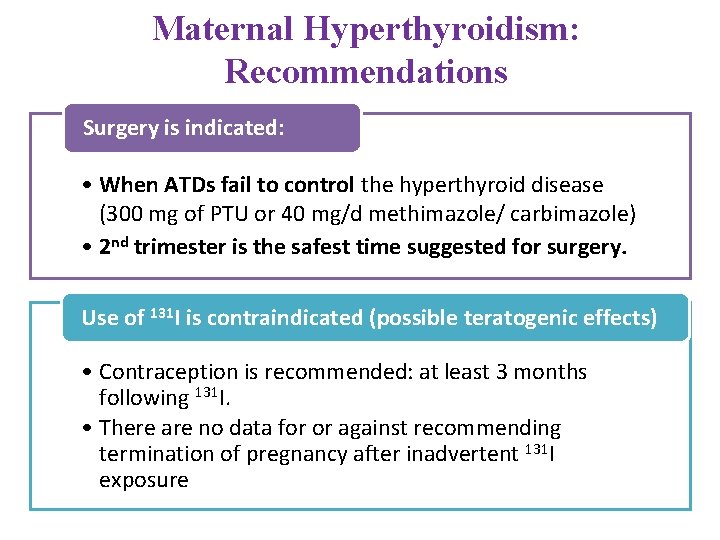
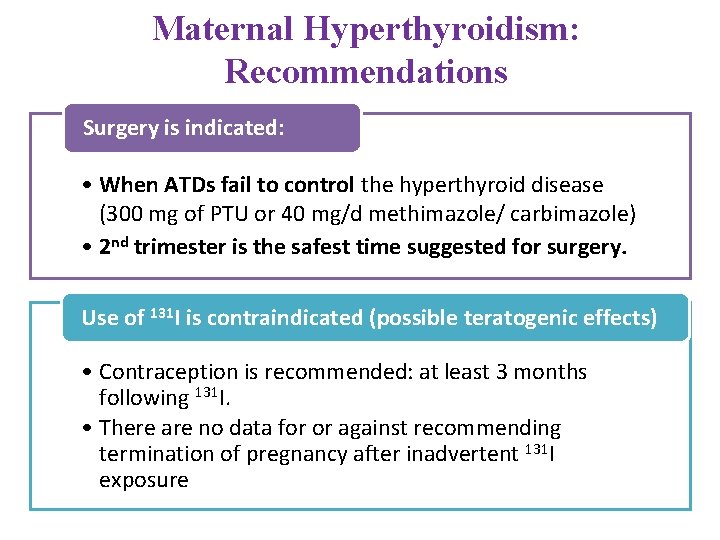
Maternal Hyperthyroidism: Recommendations Surgery is indicated: • When ATDs fail to control the hyperthyroid disease (300 mg of PTU or 40 mg/d methimazole/ carbimazole) • 2 nd trimester is the safest time suggested for surgery. Use of 131 I is contraindicated (possible teratogenic effects) • Contraception is recommended: at least 3 months following 131 I. • There are no data for or against recommending termination of pregnancy after inadvertent 131 I exposure
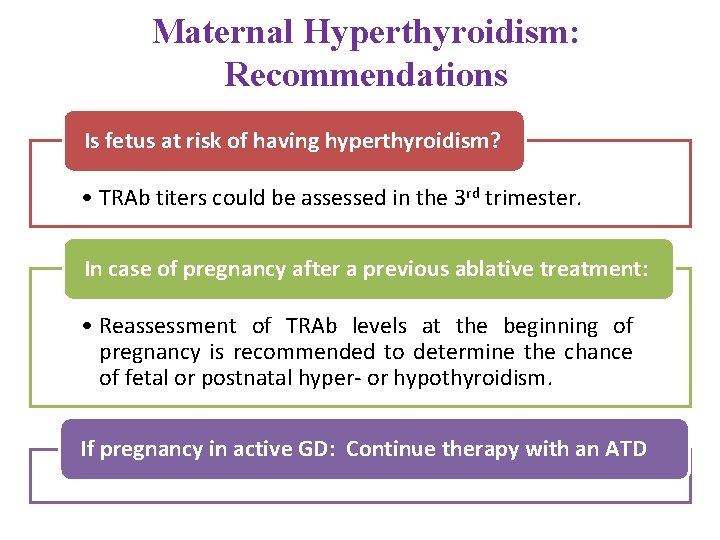
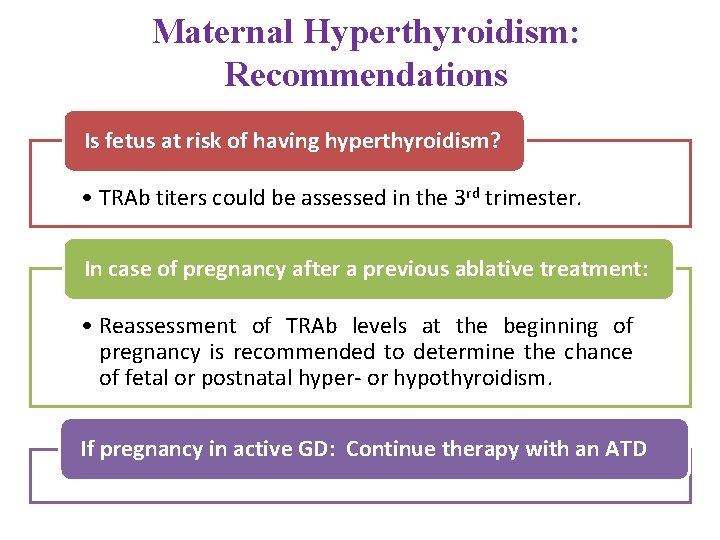
Maternal Hyperthyroidism: Recommendations Is fetus at risk of having hyperthyroidism? • TRAb titers could be assessed in the 3 rd trimester. In case of pregnancy after a previous ablative treatment: • Reassessment of TRAb levels at the beginning of pregnancy is recommended to determine the chance of fetal or postnatal hyper- or hypothyroidism. If pregnancy in active GD: Continue therapy with an ATD
Maternal Hyperthyroidism: Recommendations If mother is euthyroid but positive for TRAb: • There is a possibility of fetal thyrotoxicosis [assessed by FHR >160 bpm] If all other causes of fetal tachycardia ruled out: • Start mother on methimazole/carbimazole to control fetal thyrotoxicosis and LT 4 to maintain maternal euthyroidism Subclinical hyperthyroidism • Does not warrant any treatment.
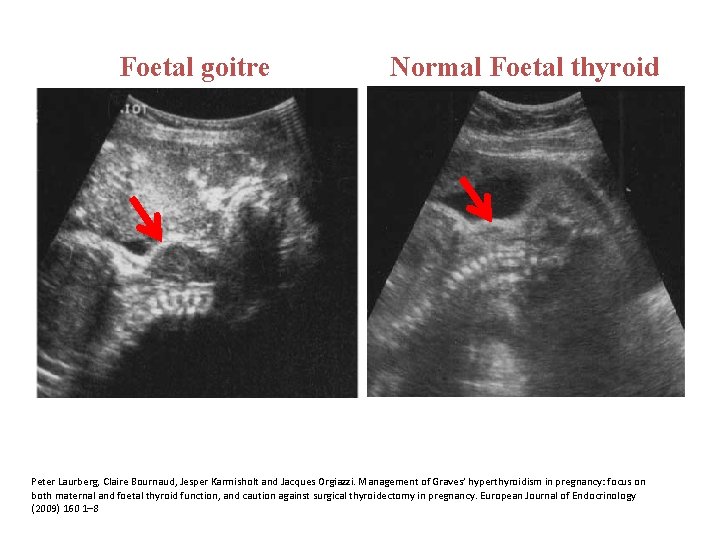
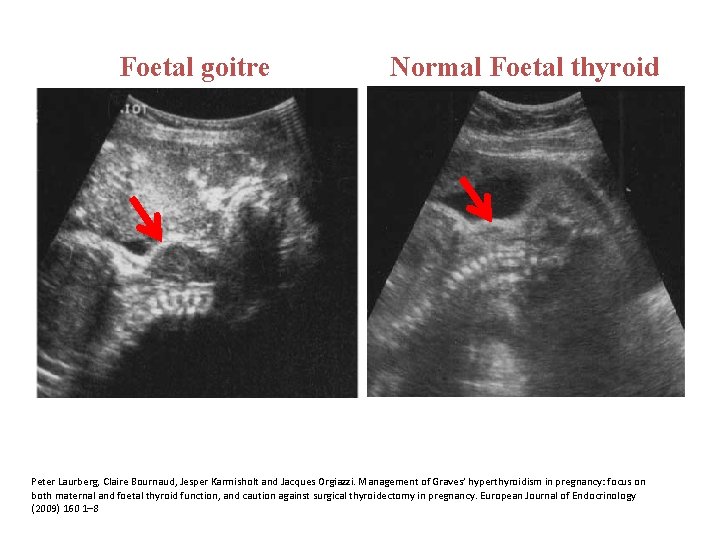
Foetal goitre Normal Foetal thyroid Peter Laurberg, Claire Bournaud, Jesper Karmisholt and Jacques Orgiazzi. Management of Graves’ hyperthyroidism in pregnancy: focus on both maternal and foetal thyroid function, and caution against surgical thyroidectomy in pregnancy. European Journal of Endocrinology (2009) 160 1– 8
Maternal Hyperthyroidism: Recommendations Pregnant women with TRAb or on ATD should have a fetal USG • To detect fetal thyroid dysfunction, this may include growth restriction, hydrops, presence of goiter, and cardiac failure. Once fetal hyperthyroidism is diagnosed • ATD therapy should be administered to the mother. The fetus should be re-evaluated: • Heart rate, goiter resolution by ultrasound in 2 weeks • Appropriate dose adjustment

 Period prevalence vs point prevalence
Period prevalence vs point prevalence Period prevalence vs point prevalence
Period prevalence vs point prevalence Defination of epidemiology
Defination of epidemiology Period prevalence vs point prevalence
Period prevalence vs point prevalence Target tsh in hypothyroidism in pregnancy
Target tsh in hypothyroidism in pregnancy Treatment for hyperthyroidism in pregnancy
Treatment for hyperthyroidism in pregnancy Hypothyroidism pregnancy
Hypothyroidism pregnancy American thyroid association guidelines pregnancy 2017
American thyroid association guidelines pregnancy 2017 Acog thyroid pregnancy
Acog thyroid pregnancy Molar pregnancy
Molar pregnancy Hypothyroidism complications
Hypothyroidism complications Causes of primary hypothyroidism
Causes of primary hypothyroidism Hashimoto's thyroiditis histology
Hashimoto's thyroiditis histology Secondary hypothyroidism
Secondary hypothyroidism Carbimazole dose
Carbimazole dose Hypothyroidism classification
Hypothyroidism classification Nursing diagnosis for hypothyroidism
Nursing diagnosis for hypothyroidism Hormone type 4
Hormone type 4 Pemberton sign
Pemberton sign Hypothyroidism ronaldo
Hypothyroidism ronaldo Hypothyroidism in children
Hypothyroidism in children What is a toxic multinodular goiter
What is a toxic multinodular goiter Hypothyrodism
Hypothyrodism Hypothyroidism
Hypothyroidism Thyroid issues in women
Thyroid issues in women Euthyroid syndrome
Euthyroid syndrome Hypothyroidism dwarfism
Hypothyroidism dwarfism Underactive thyroid symptoms
Underactive thyroid symptoms Graves disease mnemonic
Graves disease mnemonic Prevalence
Prevalence Prevalence ratio
Prevalence ratio Mortality formula
Mortality formula Prevalence vs incidence
Prevalence vs incidence Point prevalence rate adalah
Point prevalence rate adalah Uuuu_limited
Uuuu_limited Prevalence of schizophrenia
Prevalence of schizophrenia Prevalence of obesity
Prevalence of obesity Sinus vein thrombosis prevalence
Sinus vein thrombosis prevalence Who global estimates on prevalence of hearing loss 2020
Who global estimates on prevalence of hearing loss 2020 Ego-dystonic
Ego-dystonic Obesity prevalence europe
Obesity prevalence europe Ukuran asosiasi epidemiologi
Ukuran asosiasi epidemiologi Prevalence ratio
Prevalence ratio Ocd prevalence
Ocd prevalence Calculate prevalence rate
Calculate prevalence rate