Syncope initial approach diagnosis and management of neurocardiogenic














- Slides: 88
Syncope- initial approach, diagnosis and management of neurocardiogenic syncope Dr Sajeer K T Senior Resident Dept. of Cardiology MCH, Kozhikode 1

Definition: Syncope is a transient loss of consciousness due to transient global cerebral hypo perfusion characterized by rapid onset, short duration, and spontaneous complete recovery - ESC 2009 Mechanism: Transient global cerebral hypoperfusion. Brignole et al. Europace. 6: 467 -537; 2004 2
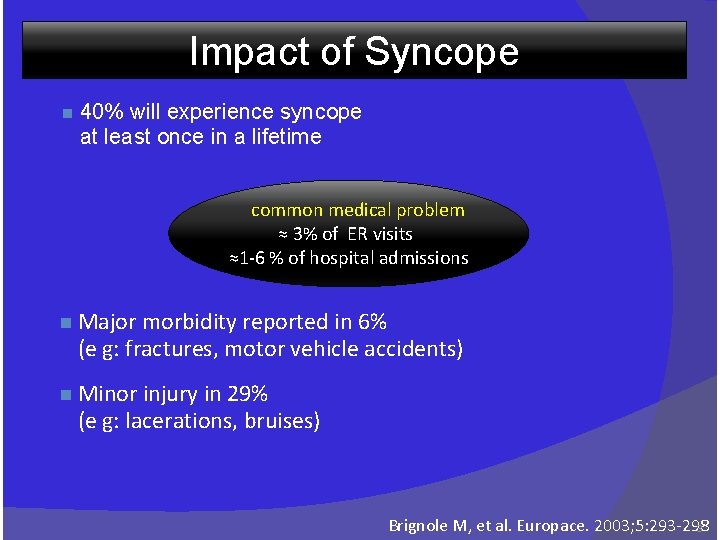
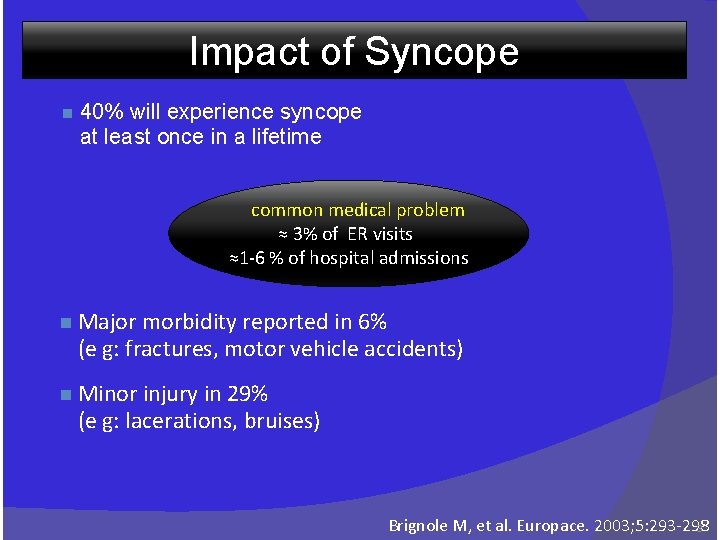
Impact of Syncope n 40% will experience syncope at least once in a lifetime common medical problem ≈ 3% of ER visits ≈1 -6 % of hospital admissions n Major morbidity reported in 6% (e g: fractures, motor vehicle accidents) n Minor injury in 29% (e g: lacerations, bruises) Brignole M, et al. Europace. 2003; 5: 293 -298 3
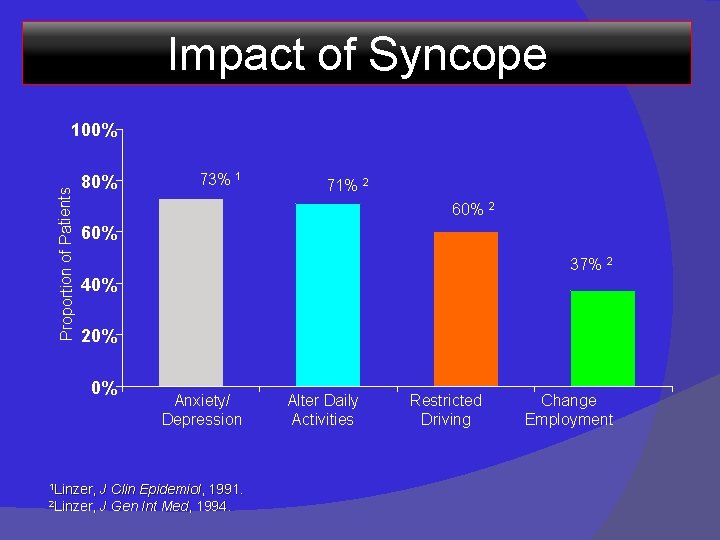
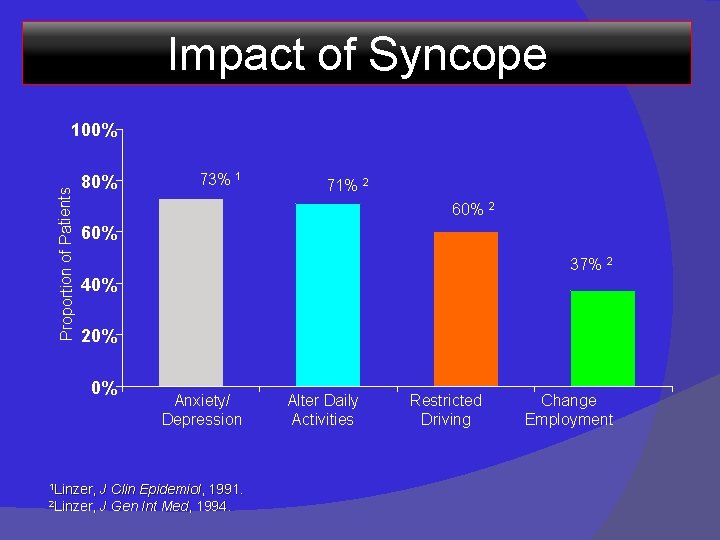
Impact of Syncope Proportion of Patients 100% 80% 73% 1 71% 2 60% 37% 2 40% 20% 0% 1 Linzer, 2 Linzer, Anxiety/ Depression J Clin Epidemiol, 1991. J Gen Int Med, 1994. Alter Daily Activities Restricted Driving Change Employment

Syncope – A Symptom, Not a Diagnosis Self-limited loss of consciousness and postural tone § Relatively rapid onset § Variable warning symptoms § Spontaneous, complete, and usually prompt recovery without medical or surgical intervention § Complete loss of consciousness in vasovagal syncope is usually no longer than 20 s in duration Brignole M, et al. Europace, 2004; 6: 467 -537. 5
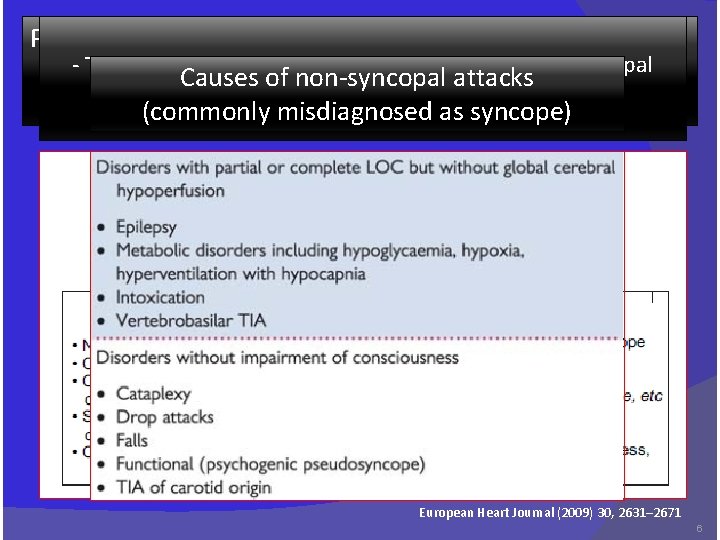
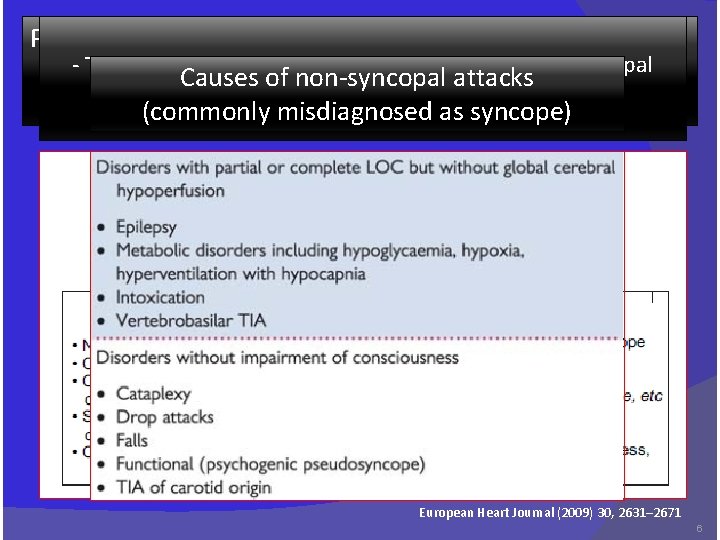
Pre-syncope or near-syncope - True indicate Syncope symptoms should be differentiated fromoccur Nonsyncopal and signs that before Causes of non-syncopal attacks events a/w real or apparent transient LOC unconsciousness in syncopeas syncope) (commonly misdiagnosed - Patients feels syncope is imminent - Symptoms associated with pre-syncope may be non-specific (e. g. dizziness) - tend to overlap the premonitory phase of true syncope ( light-headedness, nausea, sweating, weakness, and visual disturbances) European Heart Journal (2009) 30, 2631– 2671 6
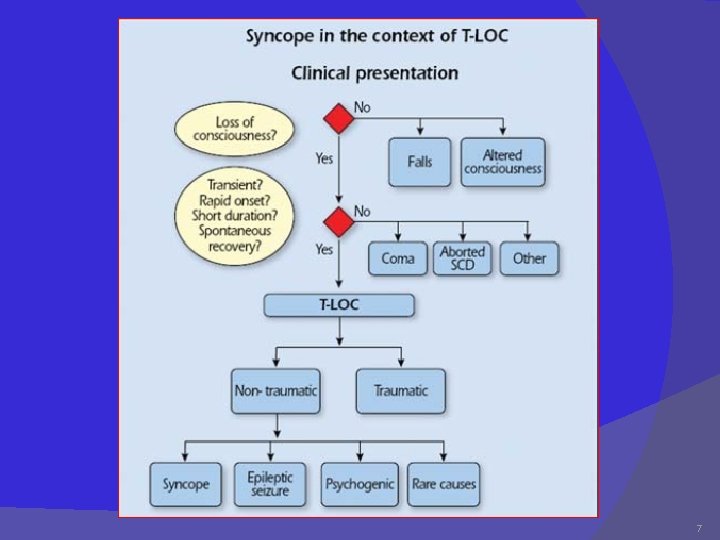
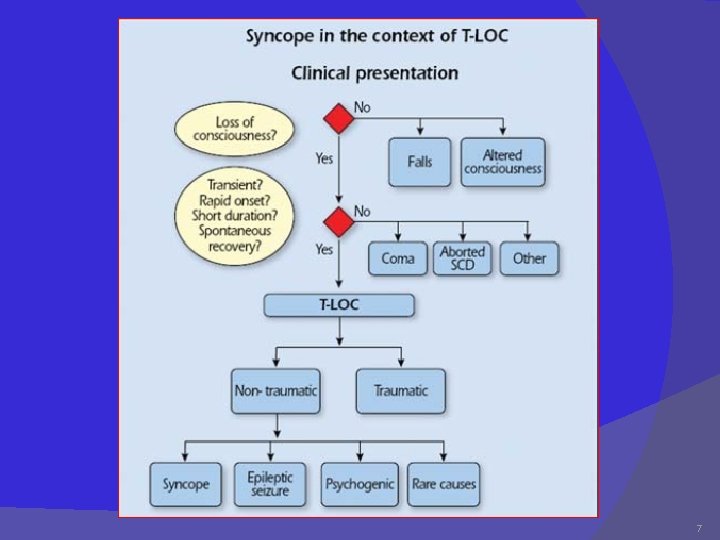
7
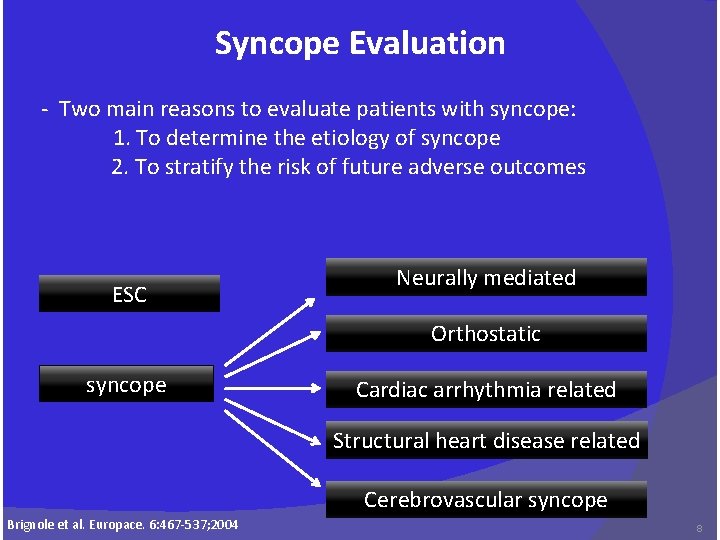
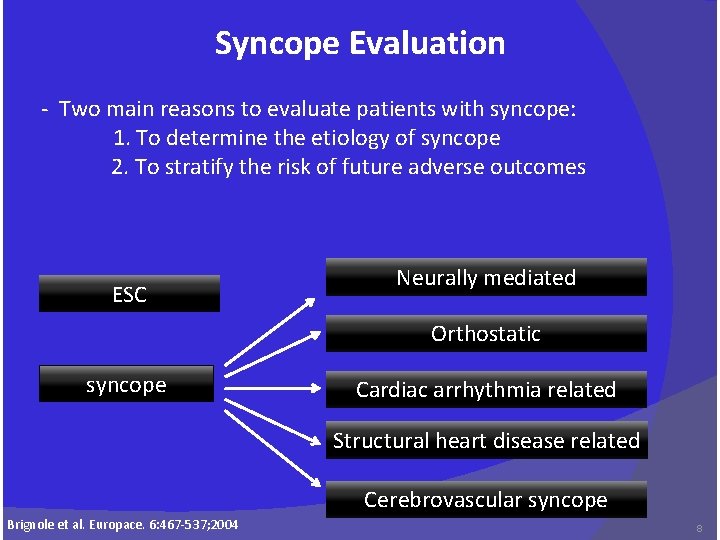
Syncope Evaluation - Two main reasons to evaluate patients with syncope: 1. To determine the etiology of syncope 2. To stratify the risk of future adverse outcomes ESC Neurally mediated Orthostatic syncope Cardiac arrhythmia related Structural heart disease related Cerebrovascular syncope Brignole et al. Europace. 6: 467 -537; 2004 8

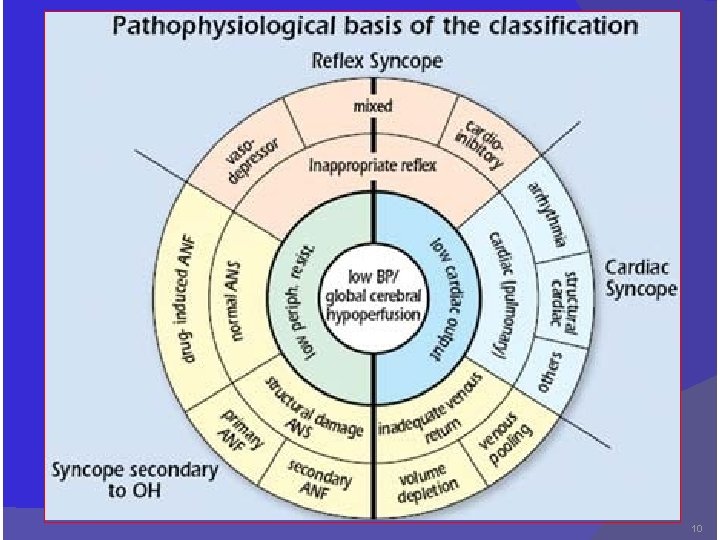
Classification and Etiology of Syncope Neurally. Mediated (24%) 1 • VVS • CSS • Situational ØCough ØPost. Micturition Orthostatic (11%) 2 • Drug-Induced • Vol. Depletion • ANS Failure ØPrimary ØSecondary Cardiac Arrhythmia (14%) Structural Cardio. Pulmonary (4% 4 3 • Brady ØSN Dysfunction ØAV Block • Tachy ØVT ØSVT • L QT S • Brugada • Acute Myocardial Ischemia • Aortic Stenosis • HCM • Pulmonary Hypertension • Aortic Dissection Unexplained Causes = Approximately 1/3 Cerebro. Vascular (12%) 5 • Vascular steal synd. • VBA disease • Carotid. A disease (34%) Brignole et al. Europace. 6: 467 -537; 2004 9
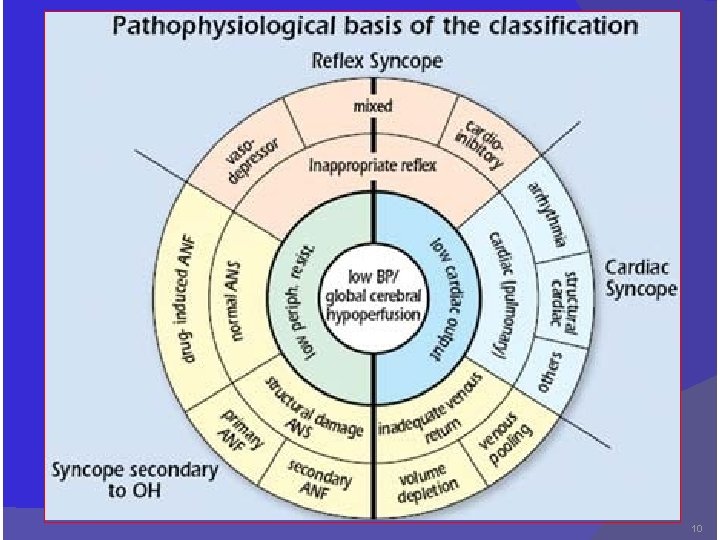
10
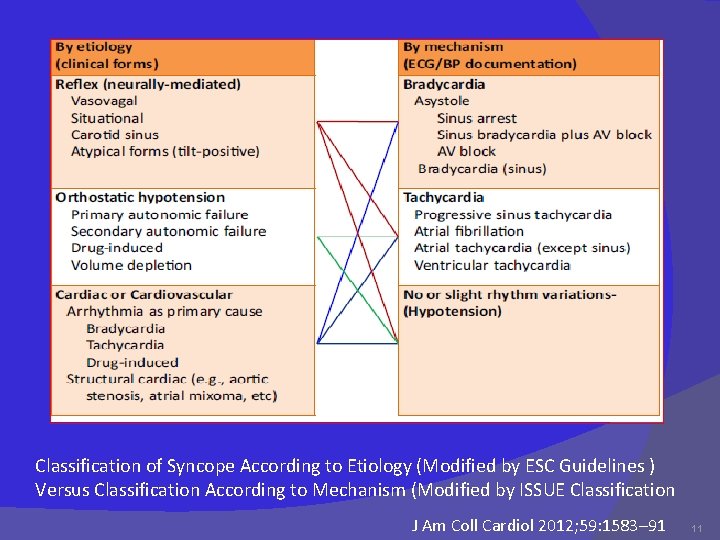
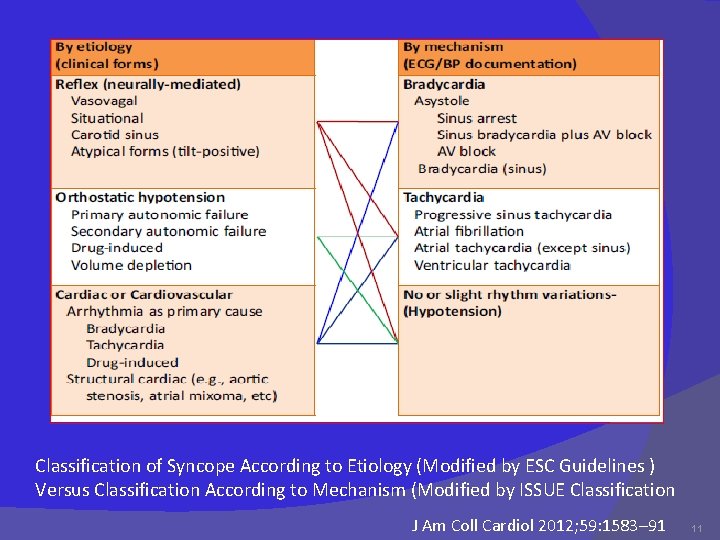
Classification of Syncope According to Etiology (Modified by ESC Guidelines ) Versus Classification According to Mechanism (Modified by ISSUE Classification J Am Coll Cardiol 2012; 59: 1583– 91 11
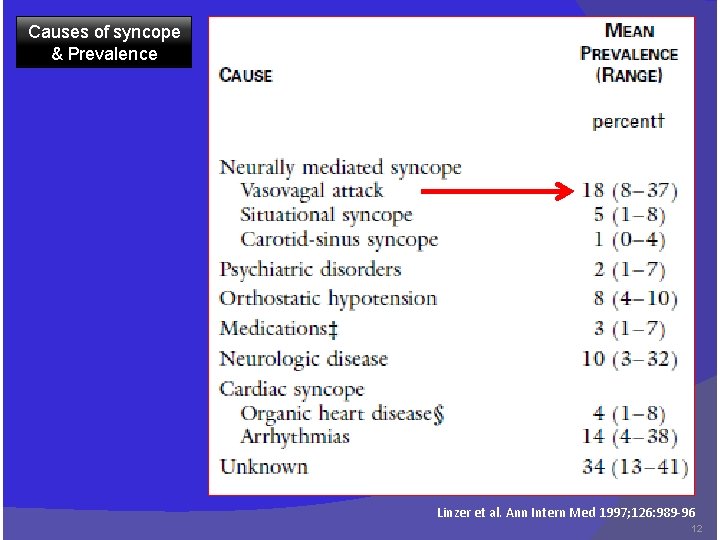
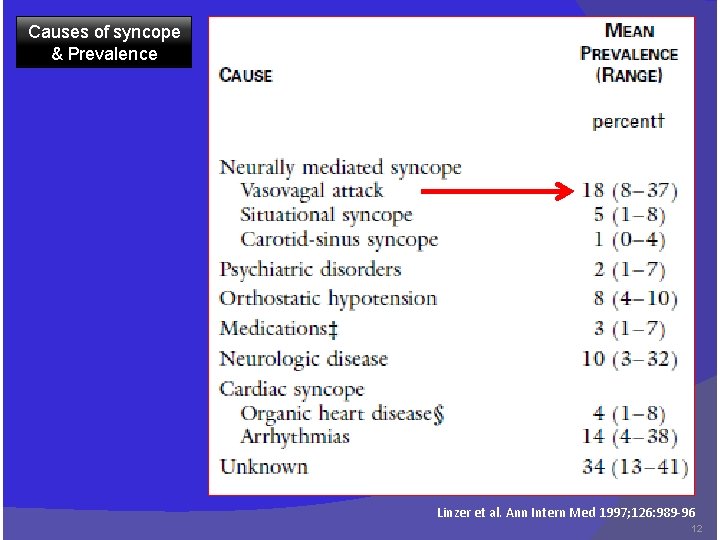
Causes of syncope & Prevalence Linzer et al. Ann Intern Med 1997; 126: 989 -96 12
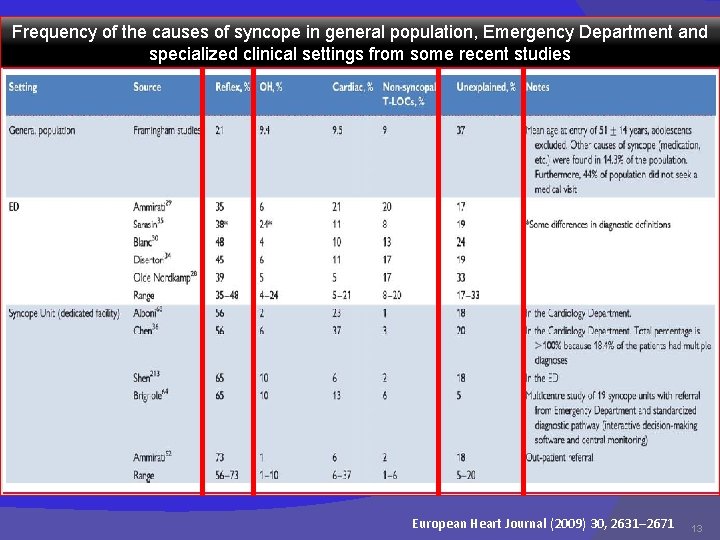
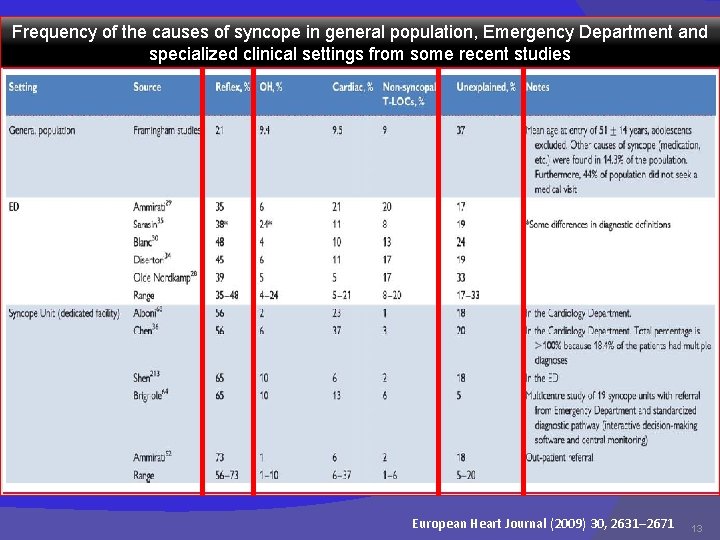
Frequency of the causes of syncope in general population, Emergency Department and specialized clinical settings from some recent studies European Heart Journal (2009) 30, 2631– 2671 13
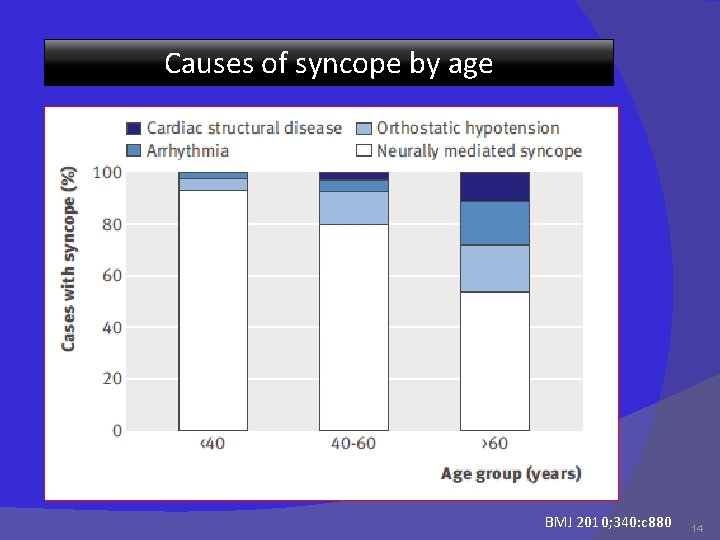
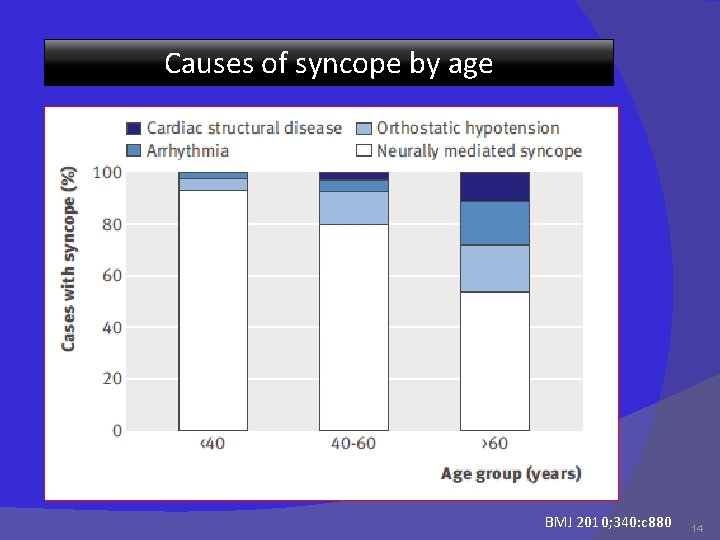
Causes of syncope by age BMJ 2010; 340: c 880 14
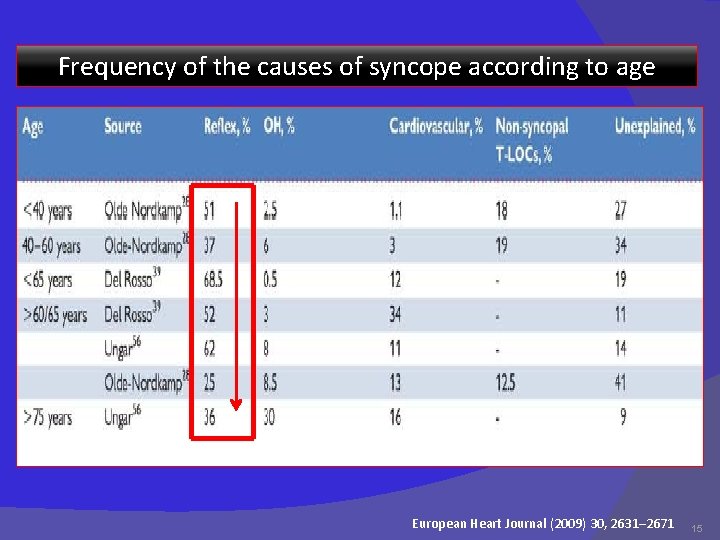
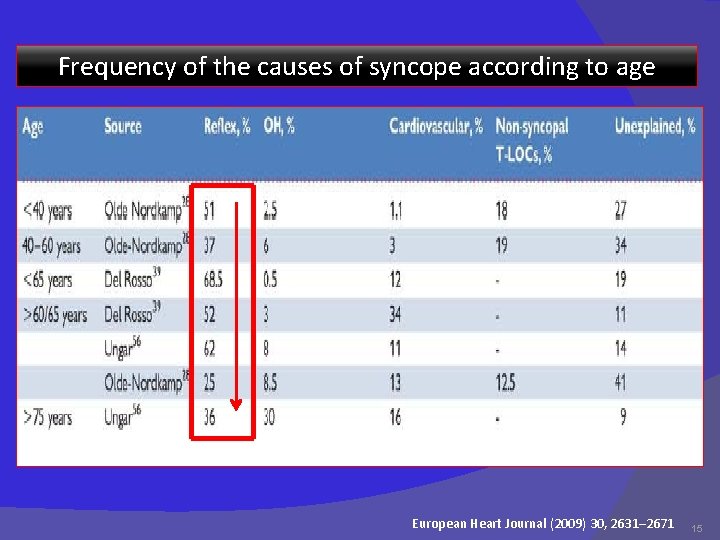
Frequency of the causes of syncope according to age European Heart Journal (2009) 30, 2631– 2671 15
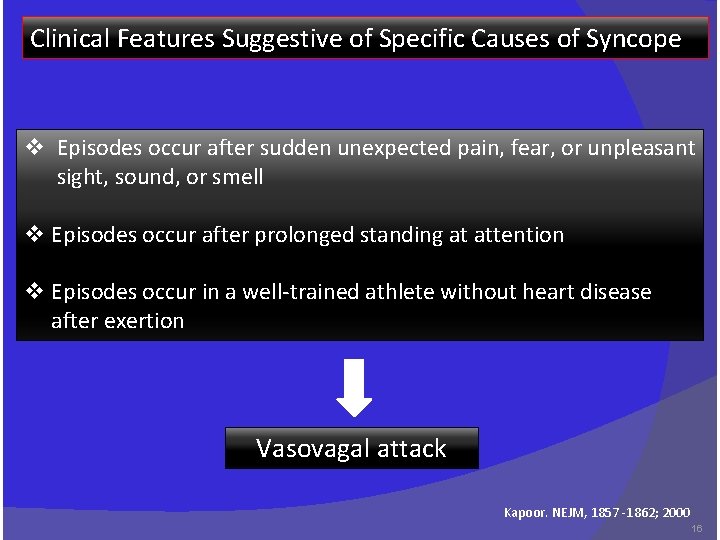
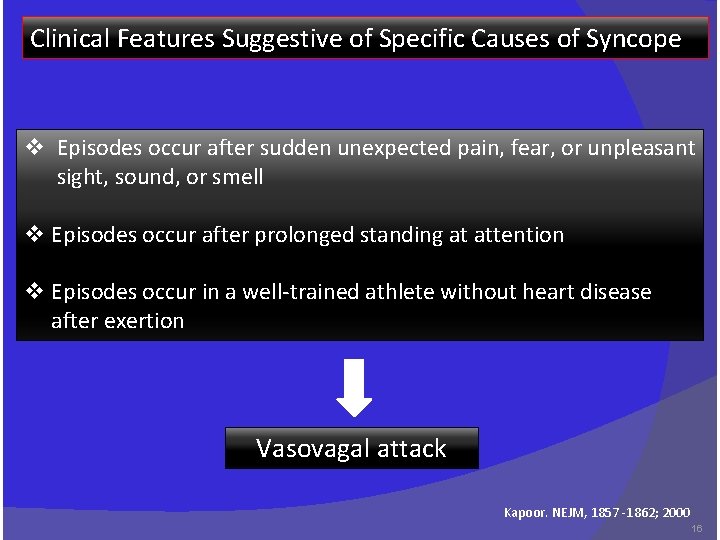
Clinical Features Suggestive of Specific Causes of Syncope v Episodes occur after sudden unexpected pain, fear, or unpleasant sight, sound, or smell v Episodes occur after prolonged standing at attention v Episodes occur in a well-trained athlete without heart disease after exertion Vasovagal attack Kapoor. NEJM, 1857 -1862; 2000 16

Episodes occur during or immediately after micturition, cough, swallowing, or defecation - Situational syncope Episodes occur with head rotation or pressure on carotid sinus (due to tumors, shaving, or tight collars) - Carotid-sinus syncope Episodes occur immediately on standing - Orthostatic hypotension Patient takes medications that may lead to a long QT interval or orthostasis and bradycardia - Drug-induced syncope Patient has a brief loss of consciousness with no prodrome and has heart disease - Arrhythmias Syncope occurs with exertion - AS, Pul. HTN, MS, HCM CAD Patient has frequent syncope with somatic symptoms but no heart disease - Psychiatric illness Patient is confused after episode, or loss of consciousness lasts >5 minutes - Seizure Kapoor. NEJM, 1857 -1862; 200017
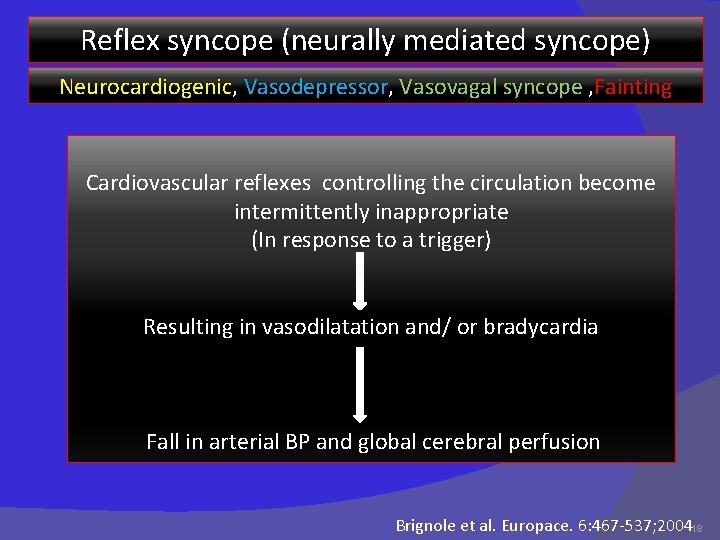
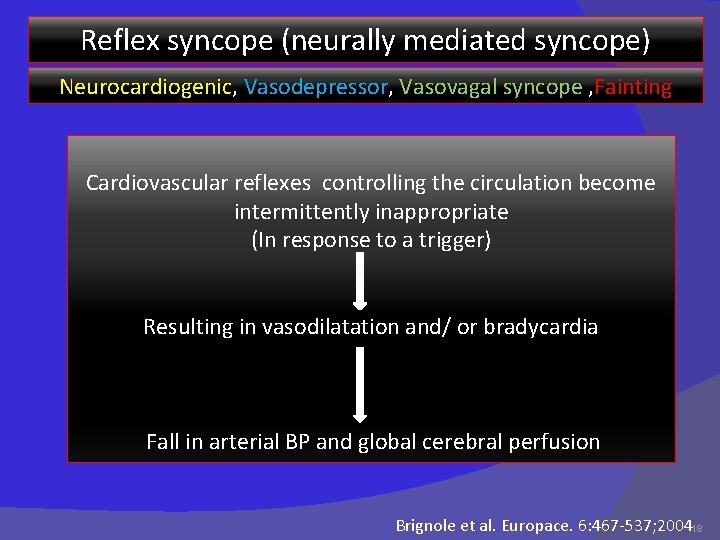
Reflex syncope (neurally mediated syncope) Neurocardiogenic, Vasodepressor, Vasovagal syncope , Fainting Cardiovascular reflexes controlling the circulation become intermittently inappropriate (In response to a trigger) Resulting in vasodilatation and/ or bradycardia Fall in arterial BP and global cerebral perfusion Brignole et al. Europace. 6: 467 -537; 200418

Reflex syncope (neurally mediated syncope) Neurocardiogenic, Vasodepressor, Vasovagal syncope , Fainting - Common abnormality of blood pressure regulation characterized by the abrupt onset of hypotension with or without bradycardia - Triggers: - orthostatic stress ( prolonged standing ) - hot shower - emotional stress ( sight of blood) - Neurally mediated syncope results from a paradoxical reflex - initiated when ventricular preload is reduced by venous pooling 19
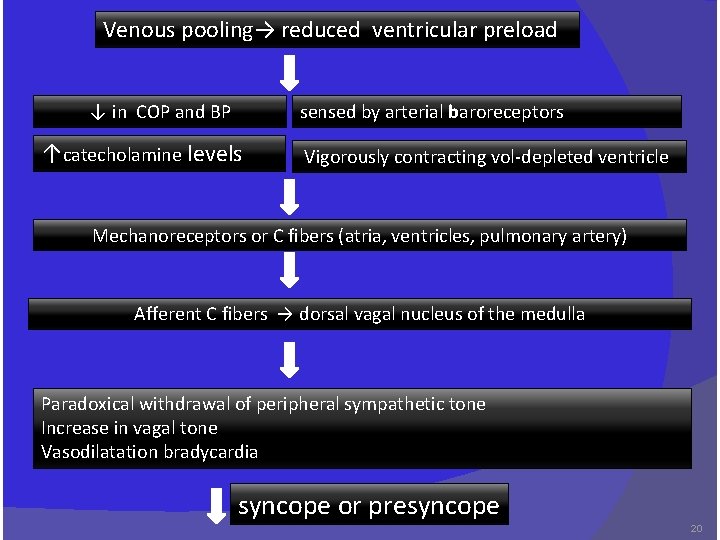
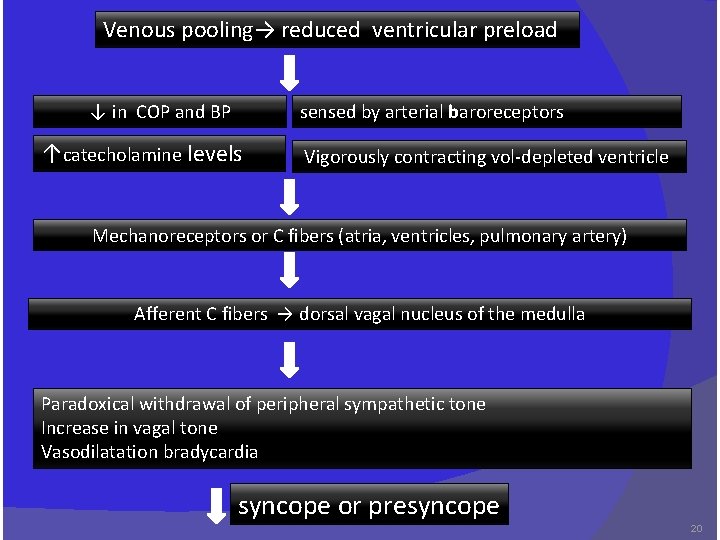
Venous pooling→ reduced ventricular preload ↓ in COP and BP sensed by arterial baroreceptors ↑catecholamine levels Vigorously contracting vol-depleted ventricle Mechanoreceptors or C fibers (atria, ventricles, pulmonary artery) Afferent C fibers → dorsal vagal nucleus of the medulla Paradoxical withdrawal of peripheral sympathetic tone Increase in vagal tone Vasodilatation bradycardia syncope or presyncope 20
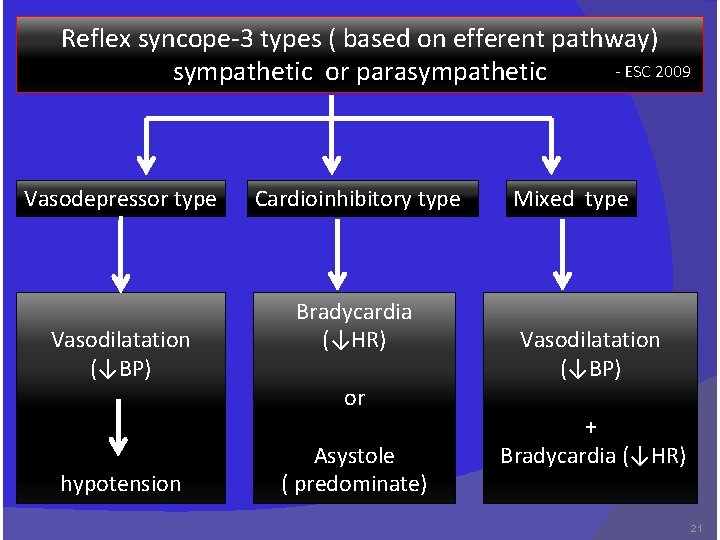
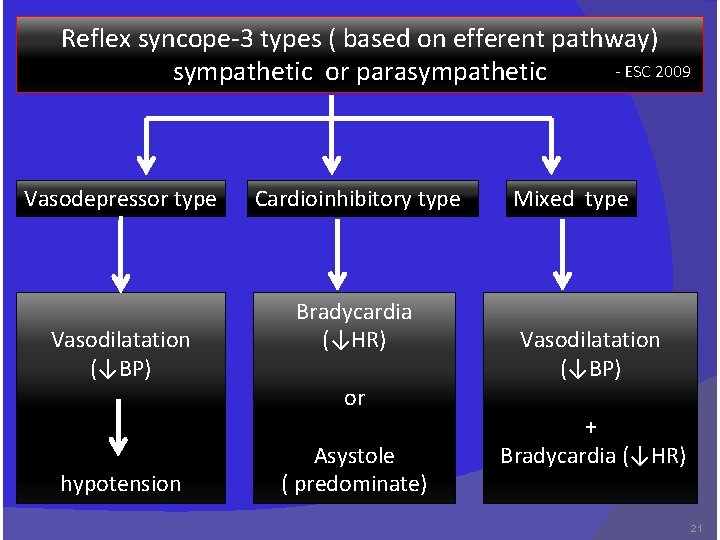
Reflex syncope-3 types ( based on efferent pathway) - ESC 2009 sympathetic or parasympathetic Vasodepressor type Vasodilatation (↓BP) hypotension Cardioinhibitory type Bradycardia (↓HR) or Asystole ( predominate) Mixed type Vasodilatation (↓BP) + Bradycardia (↓HR) 21
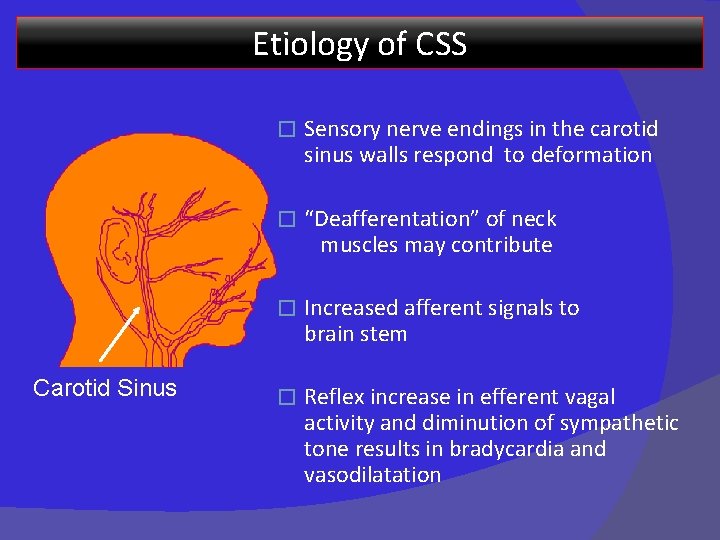
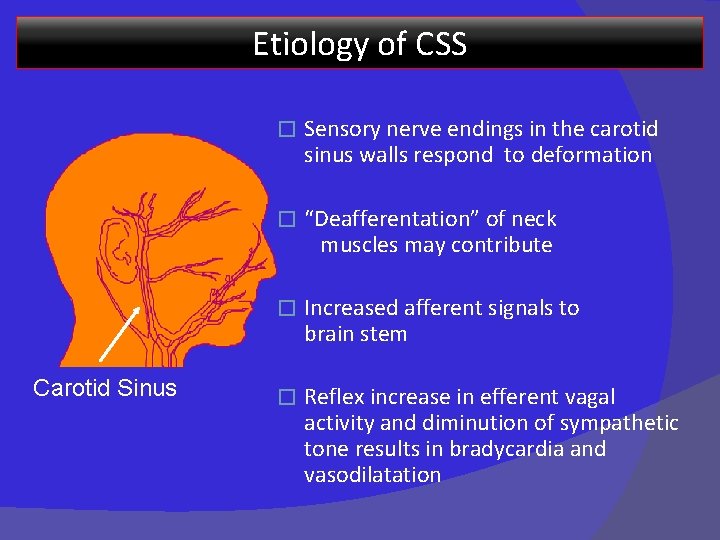
Etiology of CSS Carotid Sinus � Sensory nerve endings in the carotid sinus walls respond to deformation � “Deafferentation” of neck muscles may contribute � Increased afferent signals to brain stem � Reflex increase in efferent vagal activity and diminution of sympathetic tone results in bradycardia and vasodilatation
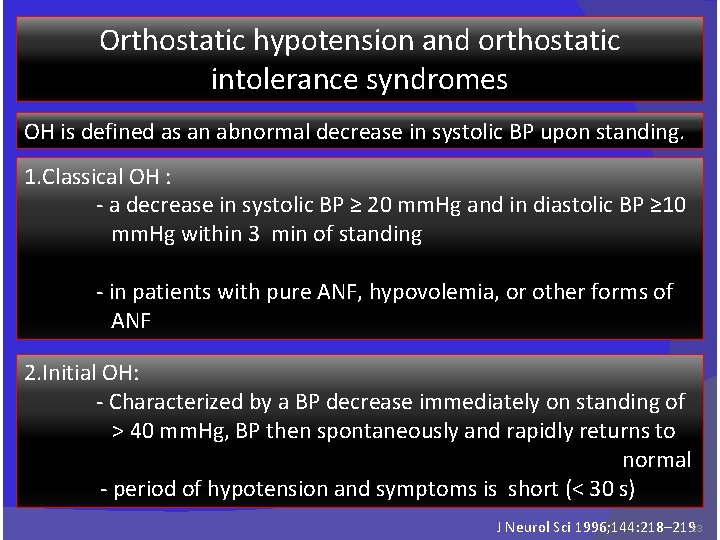
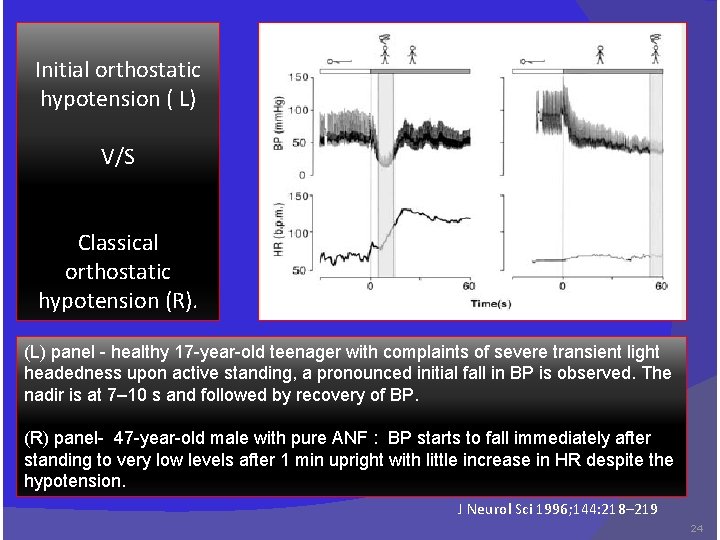
Orthostatic hypotension and orthostatic intolerance syndromes OH is defined as an abnormal decrease in systolic BP upon standing. 1. Classical OH : - a decrease in systolic BP ≥ 20 mm. Hg and in diastolic BP ≥ 10 mm. Hg within 3 min of standing - in patients with pure ANF, hypovolemia, or other forms of ANF 2. Initial OH: - Characterized by a BP decrease immediately on standing of > 40 mm. Hg, BP then spontaneously and rapidly returns to normal - period of hypotension and symptoms is short (< 30 s) J Neurol Sci 1996; 144: 218– 21923
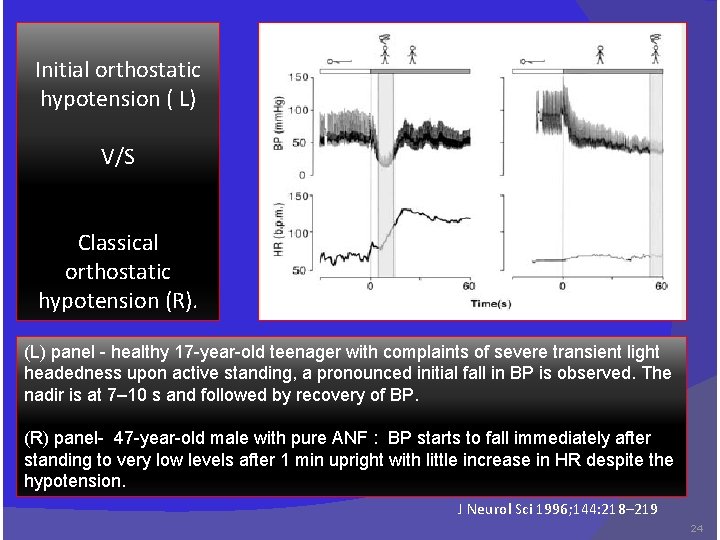
Initial orthostatic hypotension ( L) V/S Classical orthostatic hypotension (R). (L) panel - healthy 17 -year-old teenager with complaints of severe transient light headedness upon active standing, a pronounced initial fall in BP is observed. The nadir is at 7– 10 s and followed by recovery of BP. (R) panel- 47 -year-old male with pure ANF : BP starts to fall immediately after standing to very low levels after 1 min upright with little increase in HR despite the hypotension. J Neurol Sci 1996; 144: 218– 219 24
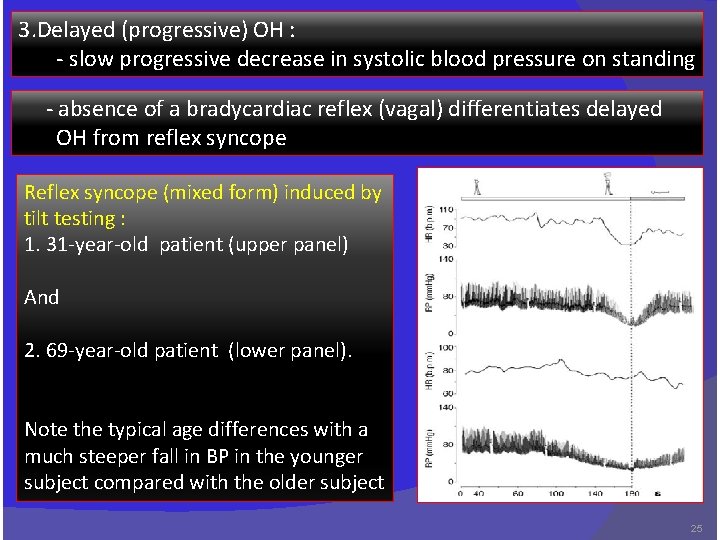
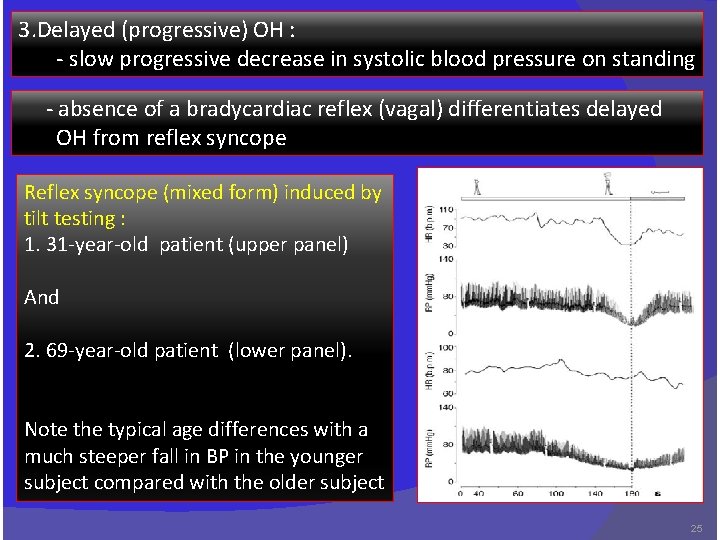
3. Delayed (progressive) OH : - slow progressive decrease in systolic blood pressure on standing - absence of a bradycardiac reflex (vagal) differentiates delayed OH from reflex syncope Reflex syncope (mixed form) induced by tilt testing : 1. 31 -year-old patient (upper panel) And 2. 69 -year-old patient (lower panel). Note the typical age differences with a much steeper fall in BP in the younger subject compared with the older subject 25

Syndromes of orthostatic intolerance which may cause syncope 26
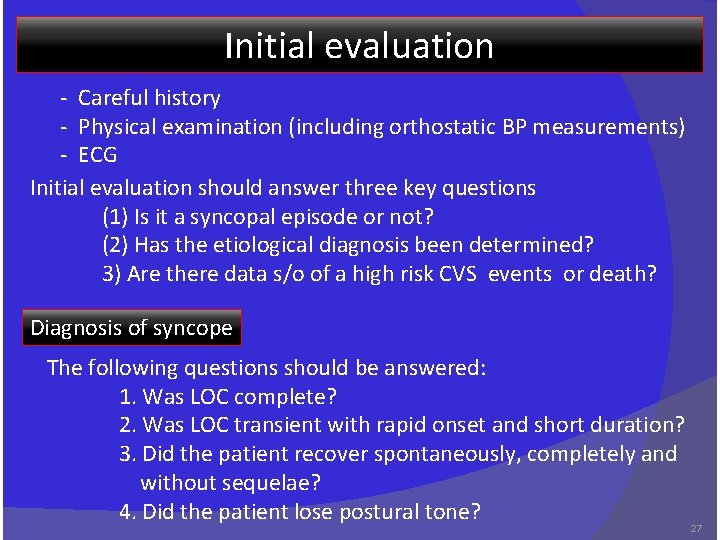
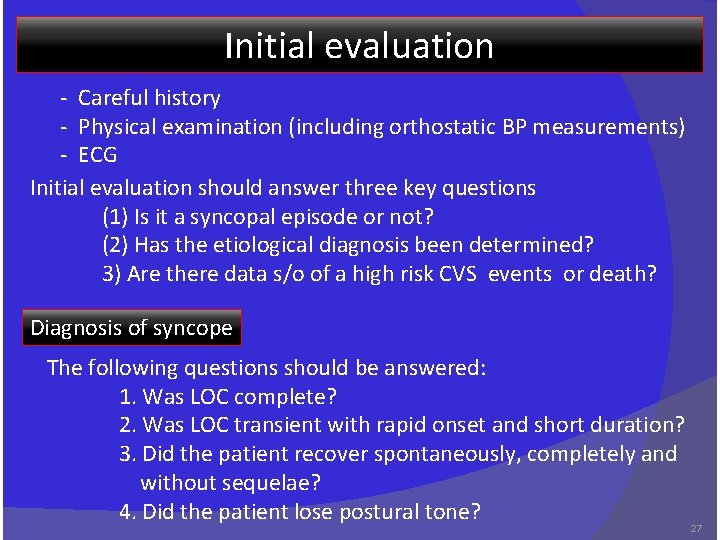
Initial evaluation - Careful history - Physical examination (including orthostatic BP measurements) - ECG Initial evaluation should answer three key questions (1) Is it a syncopal episode or not? (2) Has the etiological diagnosis been determined? 3) Are there data s/o of a high risk CVS events or death? Diagnosis of syncope The following questions should be answered: 1. Was LOC complete? 2. Was LOC transient with rapid onset and short duration? 3. Did the patient recover spontaneously, completely and without sequelae? 4. Did the patient lose postural tone? 27
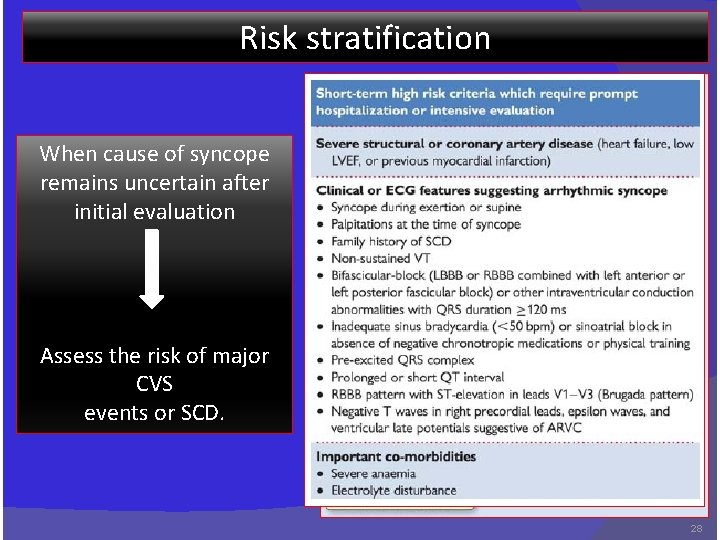
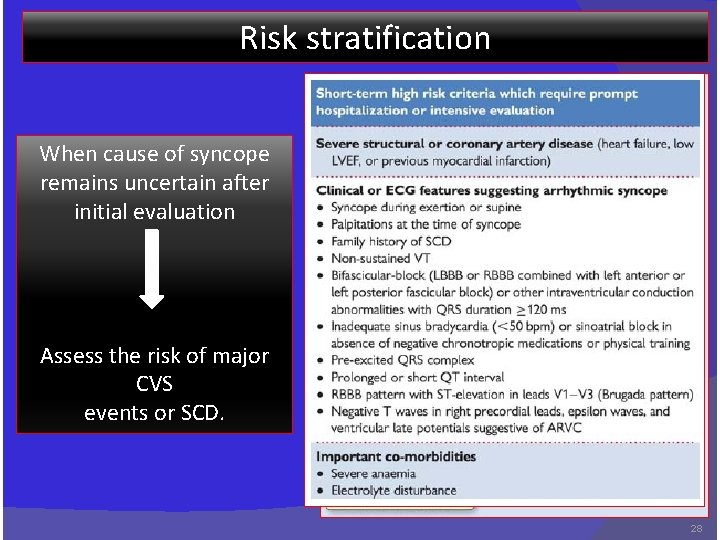
Risk stratification When cause of syncope remains uncertain after initial evaluation Assess the risk of major CVS events or SCD. 28
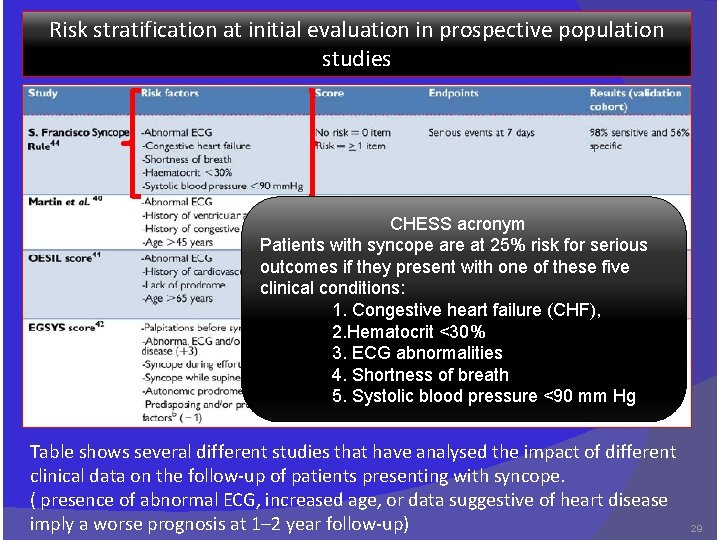
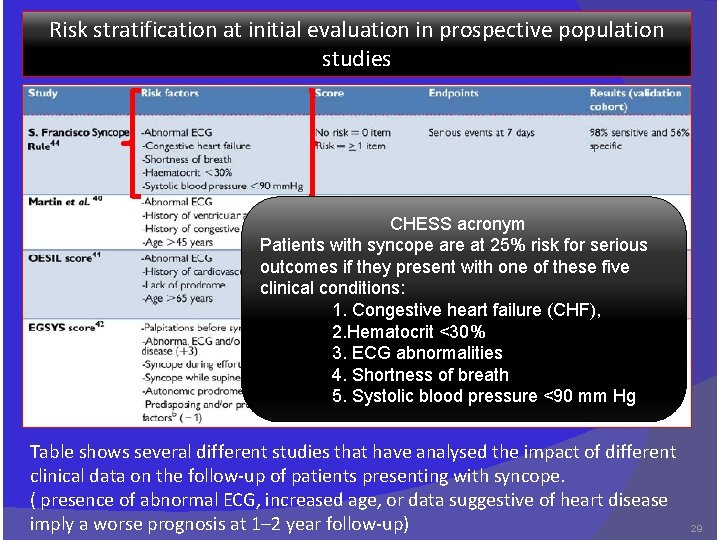
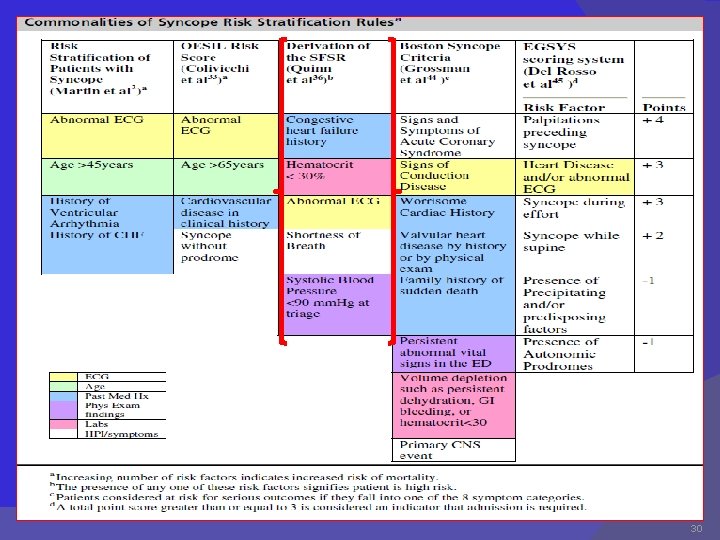
Risk stratification at initial evaluation in prospective population studies CHESS acronym Patients with syncope are at 25% risk for serious outcomes if they present with one of these five clinical conditions: 1. Congestive heart failure (CHF), 2. Hematocrit <30% 3. ECG abnormalities 4. Shortness of breath 5. Systolic blood pressure <90 mm Hg Table shows several different studies that have analysed the impact of different clinical data on the follow-up of patients presenting with syncope. ( presence of abnormal ECG, increased age, or data suggestive of heart disease imply a worse prognosis at 1– 2 year follow-up) 29
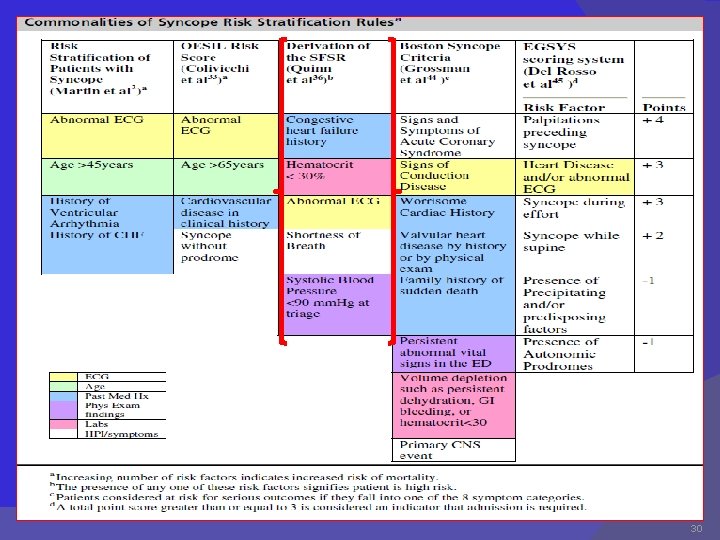
30
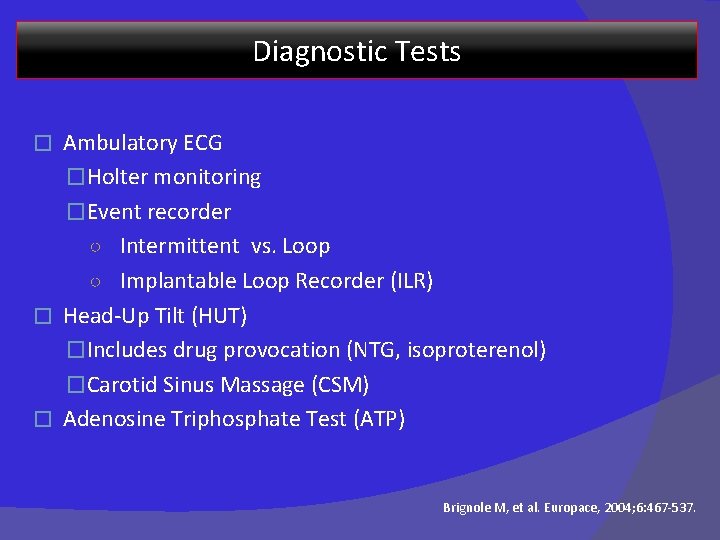
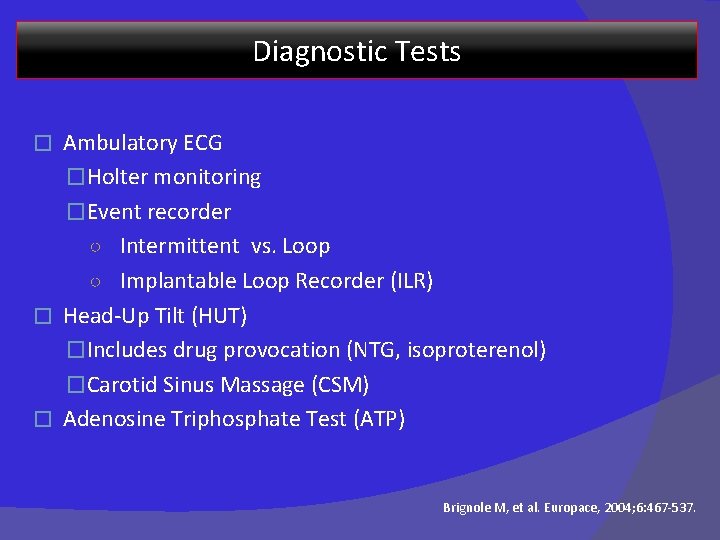
Diagnostic Tests Ambulatory ECG �Holter monitoring �Event recorder ○ Intermittent vs. Loop ○ Implantable Loop Recorder (ILR) � Head-Up Tilt (HUT) �Includes drug provocation (NTG, isoproterenol) �Carotid Sinus Massage (CSM) � Adenosine Triphosphate Test (ATP) � Brignole M, et al. Europace, 2004; 6: 467 -537.
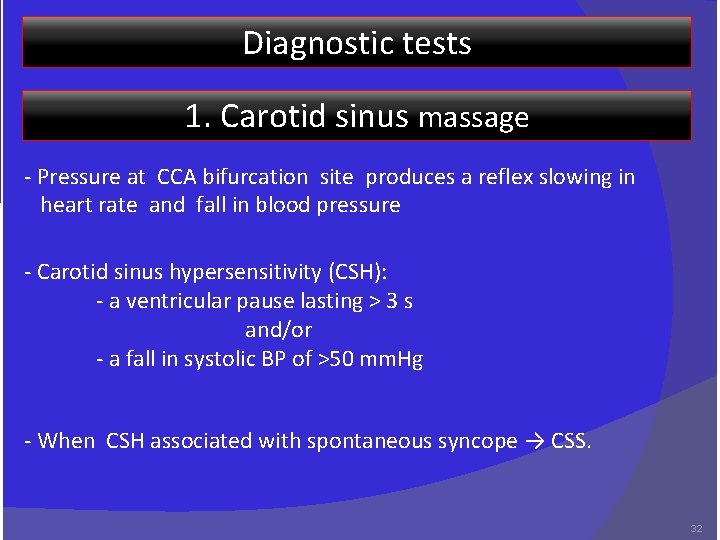
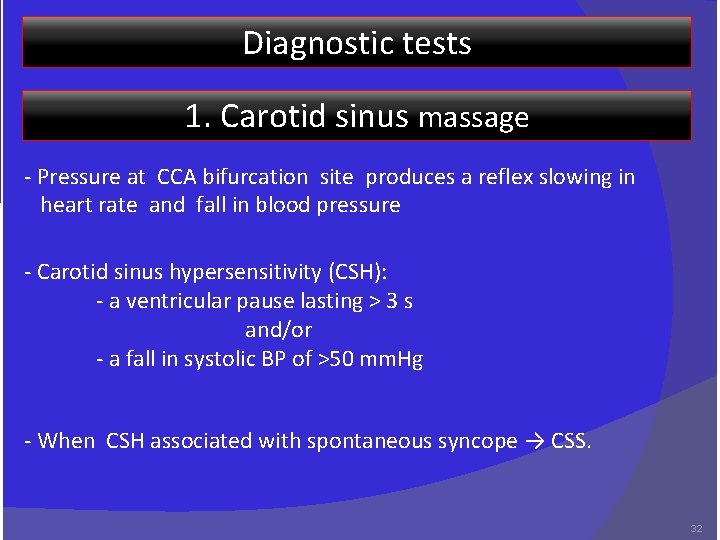
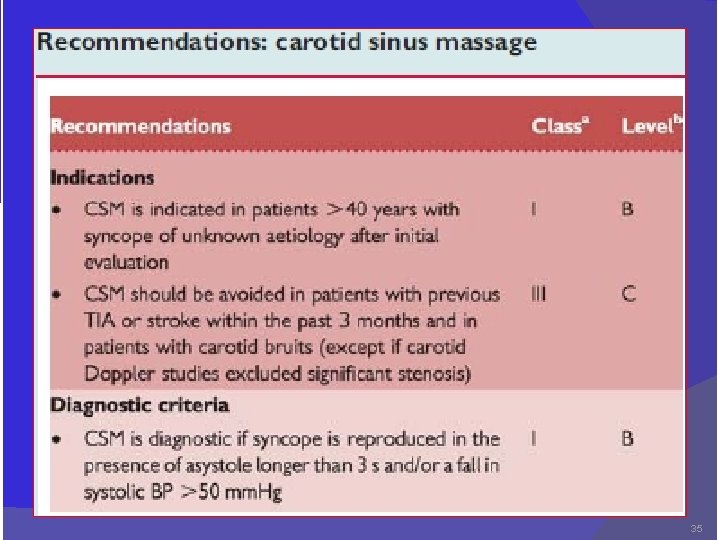
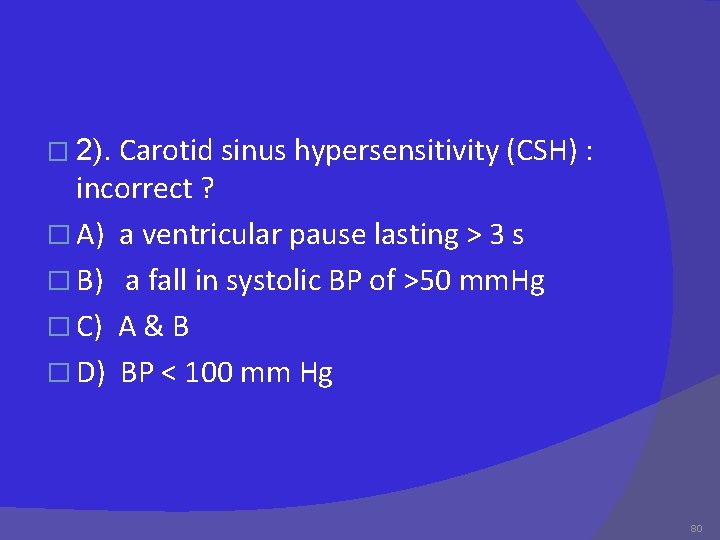
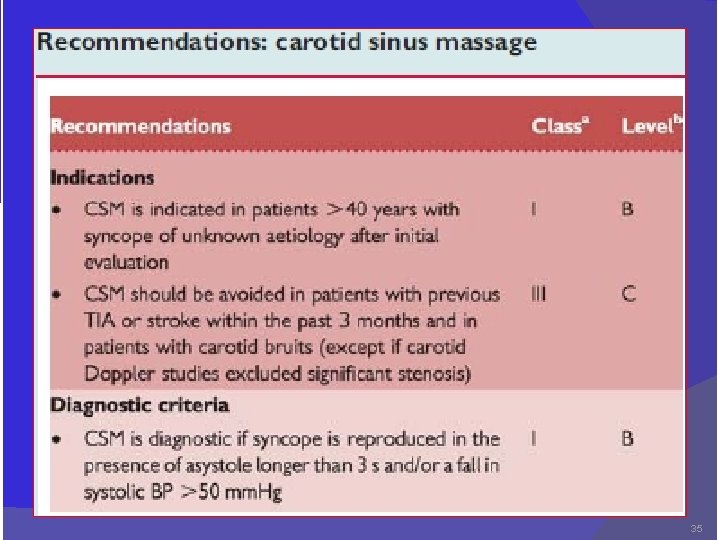
Diagnostic tests 1. Carotid sinus massage - Pressure at CCA bifurcation site produces a reflex slowing in heart rate and fall in blood pressure - Carotid sinus hypersensitivity (CSH): - a ventricular pause lasting > 3 s and/or - a fall in systolic BP of >50 mm. Hg - When CSH associated with spontaneous syncope → CSS. 32

Carotid sinus reflex arc Afferent limb arising from the mechanoreceptors of the carotid. A Midbrain centres ( vagal nucleus and the vasomotor centre) Efferent limb is via the vagal nerve and the parasympathetic ganglia to the sinus and atrioventricular nodes via the sympathetic nervous system to the heart and the blood vessels 33
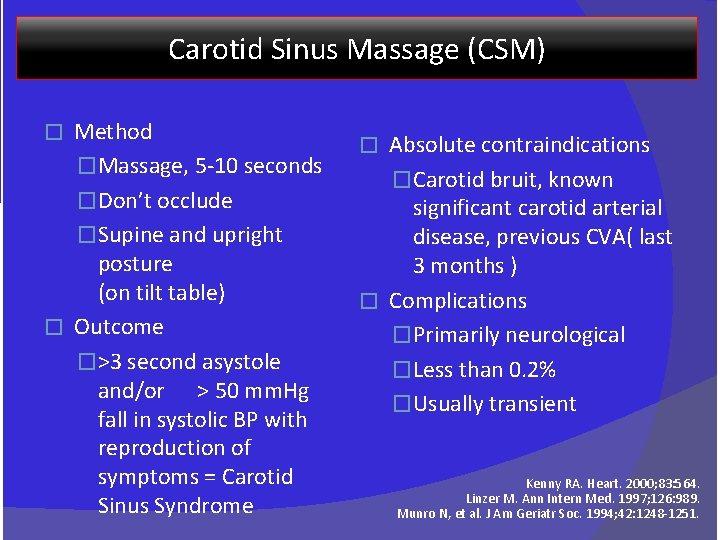
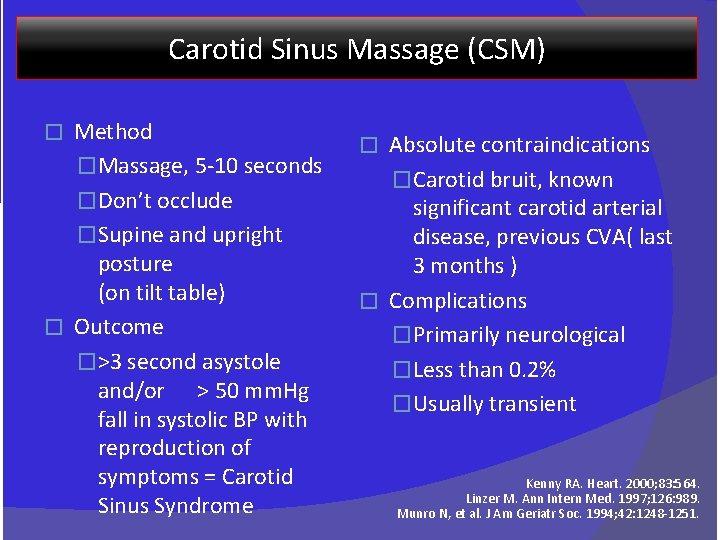
Carotid Sinus Massage (CSM) Method �Massage, 5 -10 seconds �Don’t occlude �Supine and upright posture (on tilt table) � Outcome �>3 second asystole and/or > 50 mm. Hg fall in systolic BP with reproduction of symptoms = Carotid Sinus Syndrome � Absolute contraindications �Carotid bruit, known significant carotid arterial disease, previous CVA( last 3 months ) � Complications �Primarily neurological �Less than 0. 2% �Usually transient � Kenny RA. Heart. 2000; 83: 564. Linzer M. Ann Intern Med. 1997; 126: 989. Munro N, et al. J Am Geriatr Soc. 1994; 42: 1248 -1251.
35

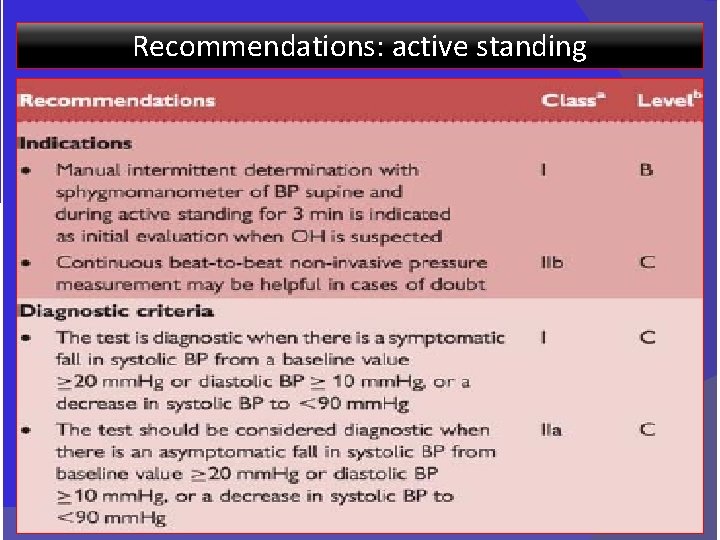
Tests for orthostatic challenge Changing from supine to upright position →displacement of blood from the thorax to the lower limbs → ↓ in venous return and CO In the absence of compensatory mechanisms→ a fall in BP may lead to syncope 2 methods: 1. Active standing: to erect) 2. Tilt table test : (in which patients arise actively from supine Brignole et al. Europace. 6: 467 -537; 200436
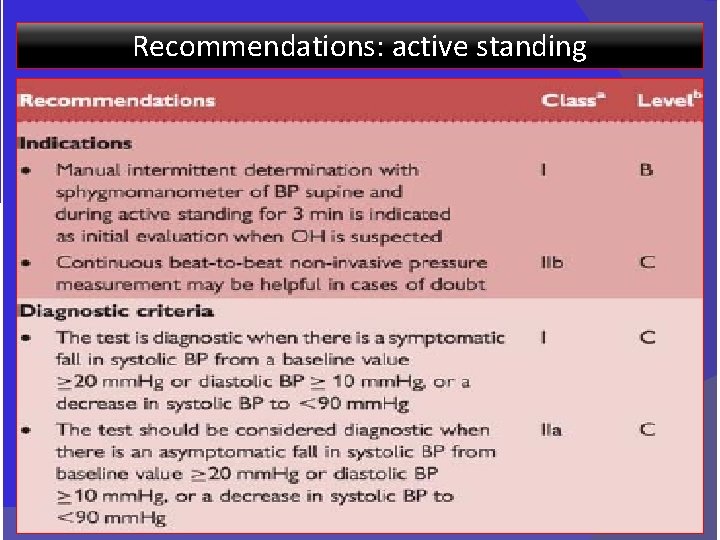
Recommendations: active standing 37
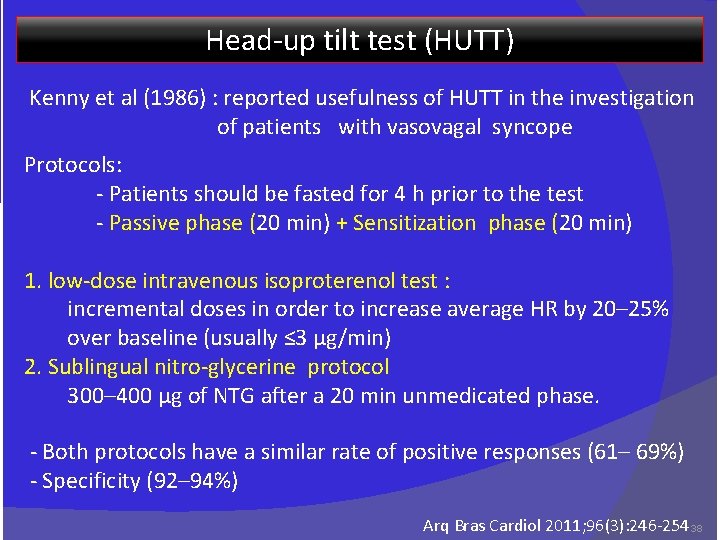
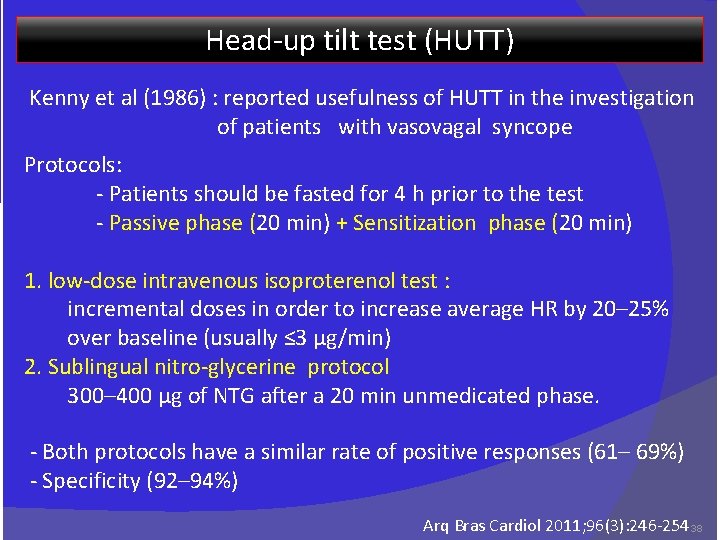
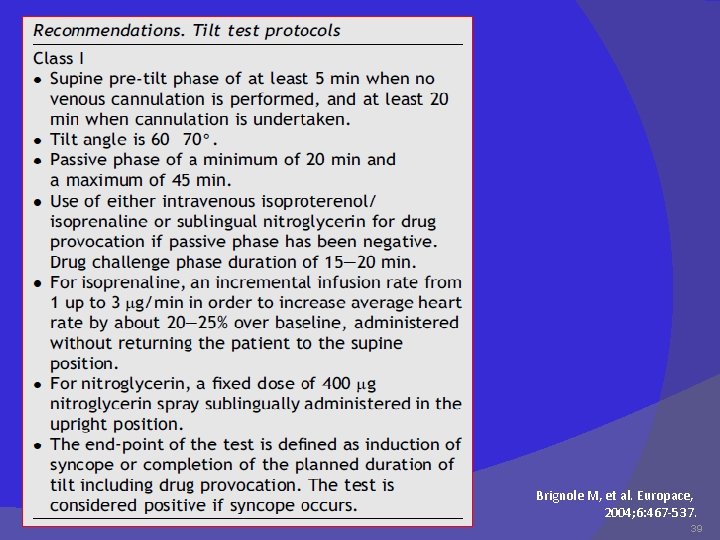
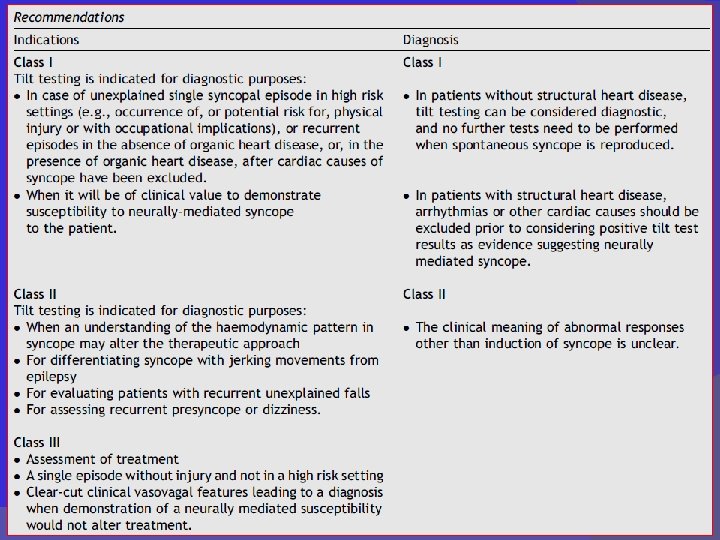
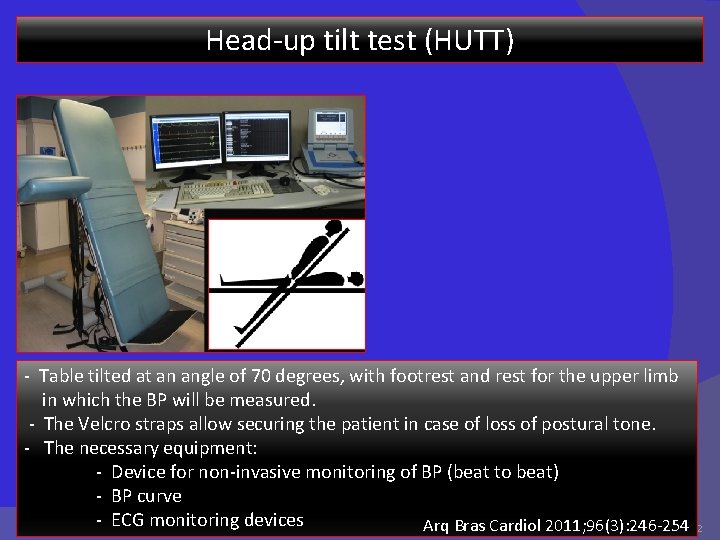
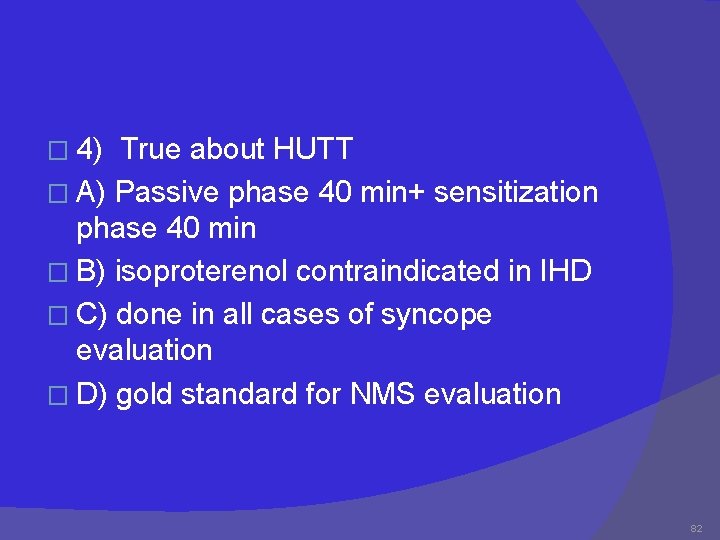
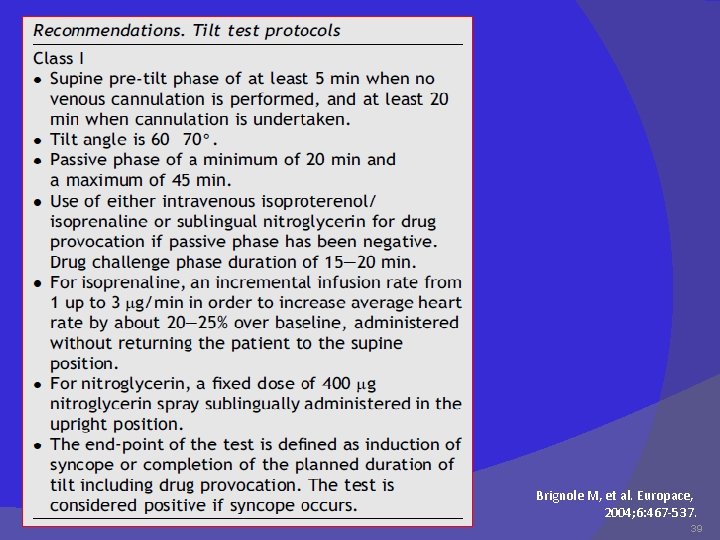
Head-up tilt test (HUTT) Kenny et al (1986) : reported usefulness of HUTT in the investigation of patients with vasovagal syncope Protocols: - Patients should be fasted for 4 h prior to the test - Passive phase (20 min) + Sensitization phase (20 min) 1. low-dose intravenous isoproterenol test : incremental doses in order to increase average HR by 20– 25% over baseline (usually ≤ 3 µg/min) 2. Sublingual nitro-glycerine protocol 300– 400 µg of NTG after a 20 min unmedicated phase. - Both protocols have a similar rate of positive responses (61– 69%) - Specificity (92– 94%) Arq Bras Cardiol 2011; 96(3): 246 -254 38
Brignole M, et al. Europace, 2004; 6: 467 -537. 39
40
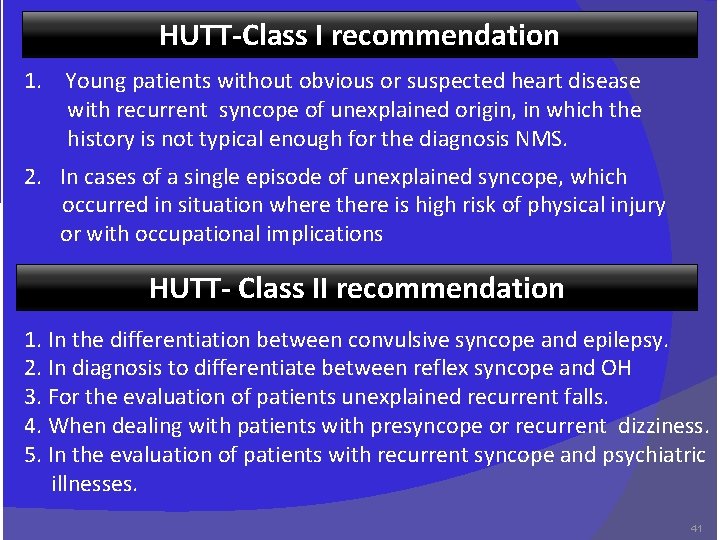
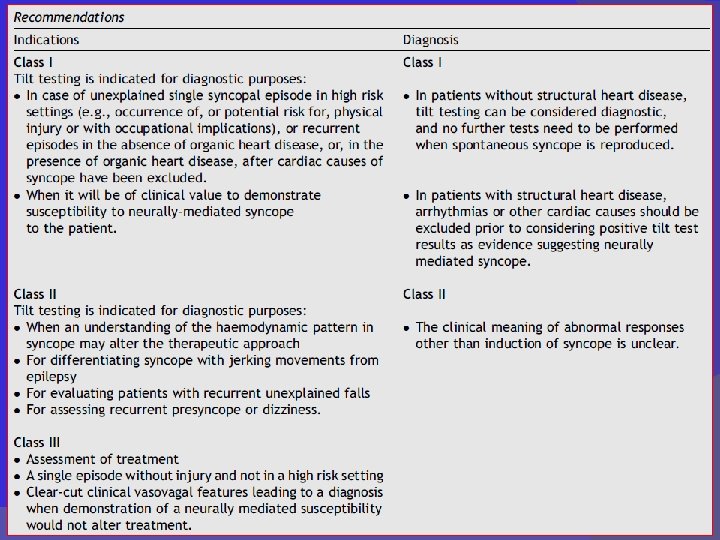
HUTT-Class I recommendation 1. Young patients without obvious or suspected heart disease with recurrent syncope of unexplained origin, in which the history is not typical enough for the diagnosis NMS. 2. In cases of a single episode of unexplained syncope, which occurred in situation where there is high risk of physical injury or with occupational implications HUTT- Class II recommendation 1. In the differentiation between convulsive syncope and epilepsy. 2. In diagnosis to differentiate between reflex syncope and OH 3. For the evaluation of patients unexplained recurrent falls. 4. When dealing with patients with presyncope or recurrent dizziness. 5. In the evaluation of patients with recurrent syncope and psychiatric illnesses. 41
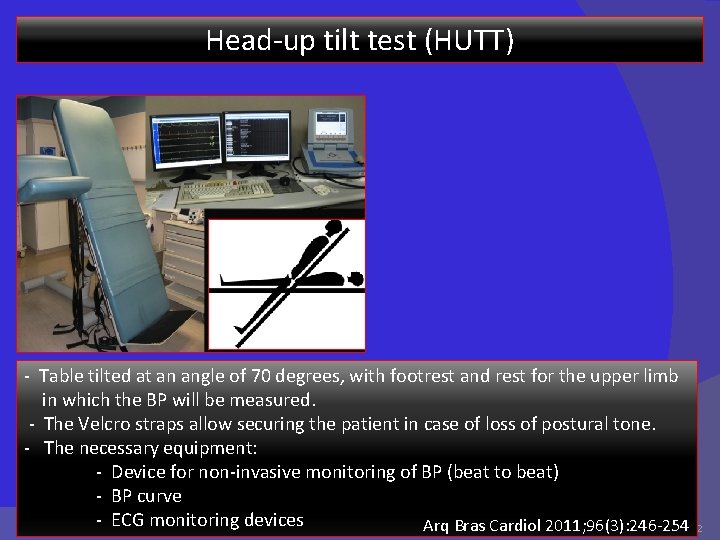
Head-up tilt test (HUTT) - Table tilted at an angle of 70 degrees, with footrest and rest for the upper limb in which the BP will be measured. - The Velcro straps allow securing the patient in case of loss of postural tone. - The necessary equipment: - Device for non-invasive monitoring of BP (beat to beat) - BP curve - ECG monitoring devices Arq Bras Cardiol 2011; 96(3): 246 -254 42
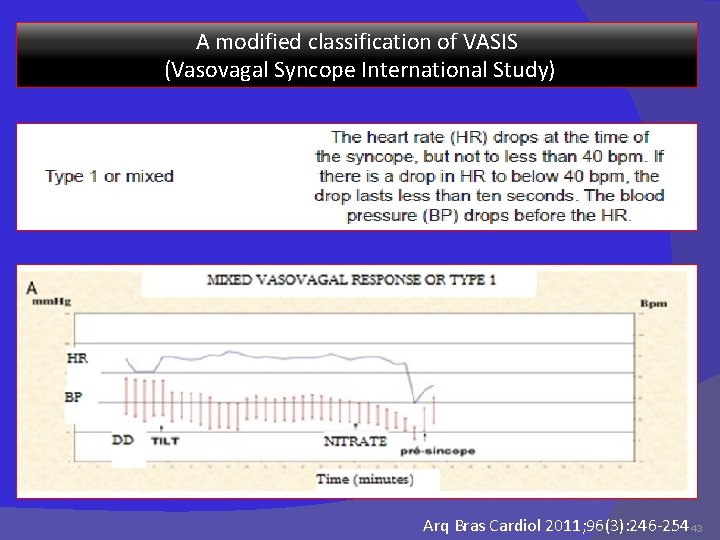
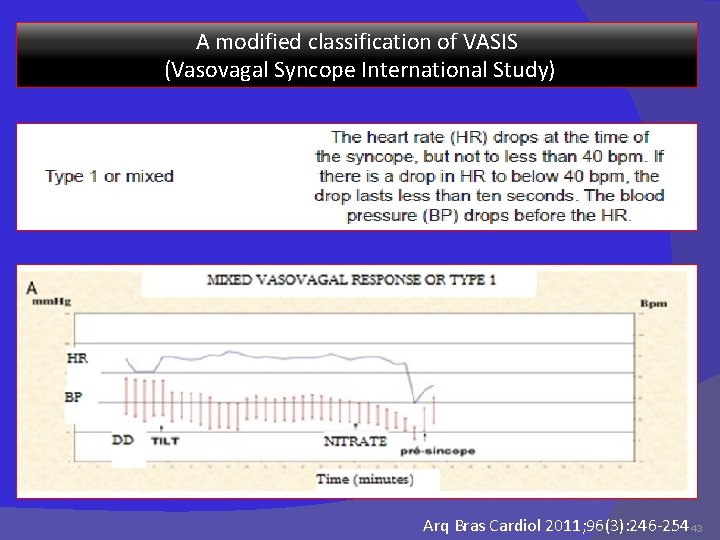
A modified classification of VASIS (Vasovagal Syncope International Study) Arq Bras Cardiol 2011; 96(3): 246 -254 43
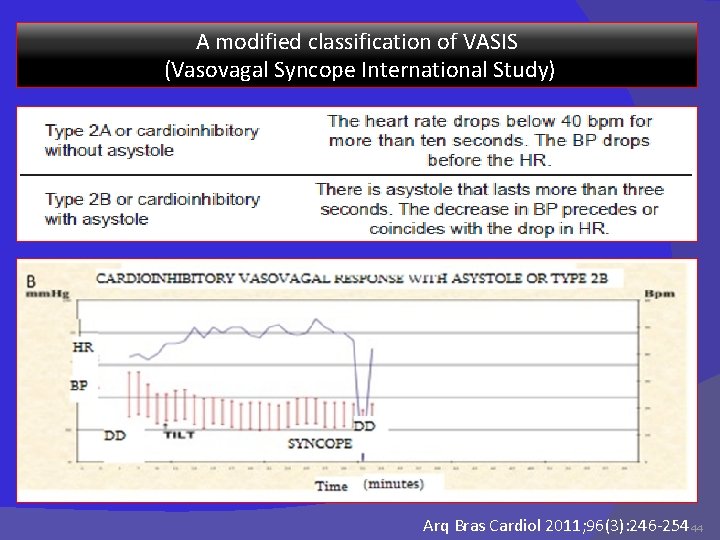
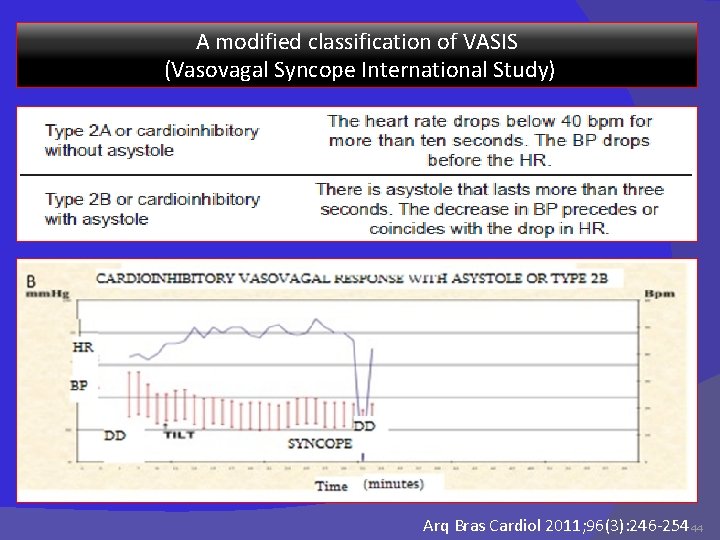
A modified classification of VASIS (Vasovagal Syncope International Study) Arq Bras Cardiol 2011; 96(3): 246 -254 44
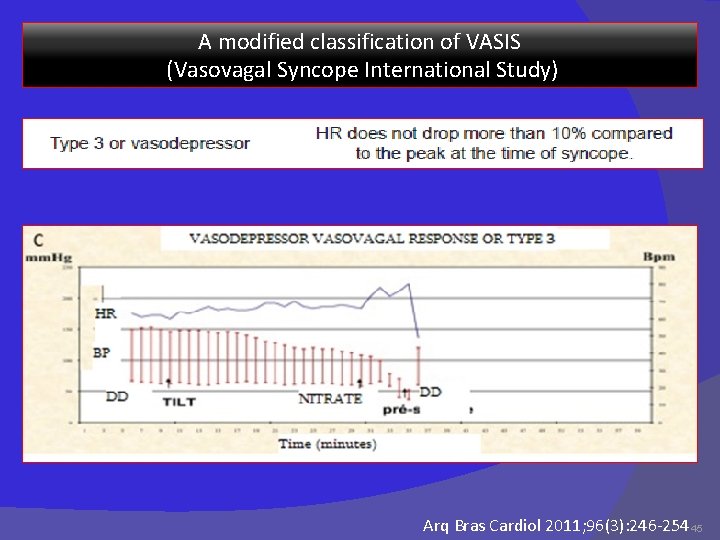
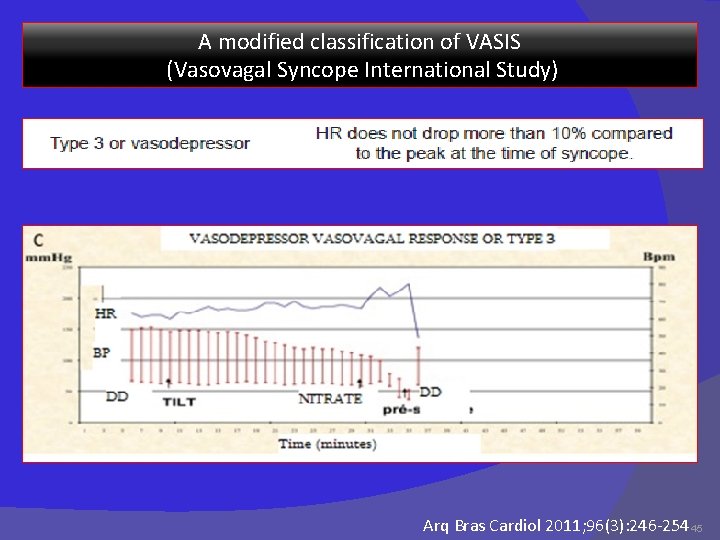
A modified classification of VASIS (Vasovagal Syncope International Study) Arq Bras Cardiol 2011; 96(3): 246 -254 45
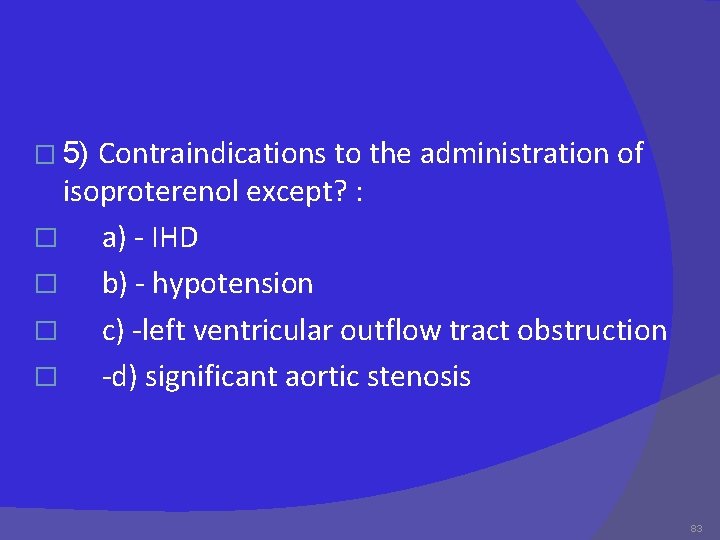
Complications and contraindications - Tilt testing is safe - life-threatening ventricular arrhythmias with isoproterenol in the presence of IHD or sick sinus syndrome -No complications have been published with the use of NTG - Minor side effects are common- Palpitations with isoproterenol - Headache with nitro glycerine Contraindications to the administration of isoproterenol : - IHD - uncontrolled HTN -left ventricular outflow tract obstruction - significant aortic stenosis 46
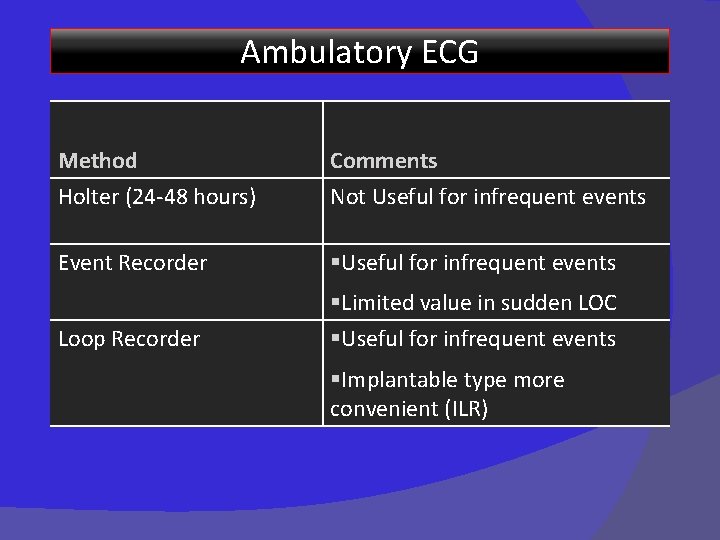
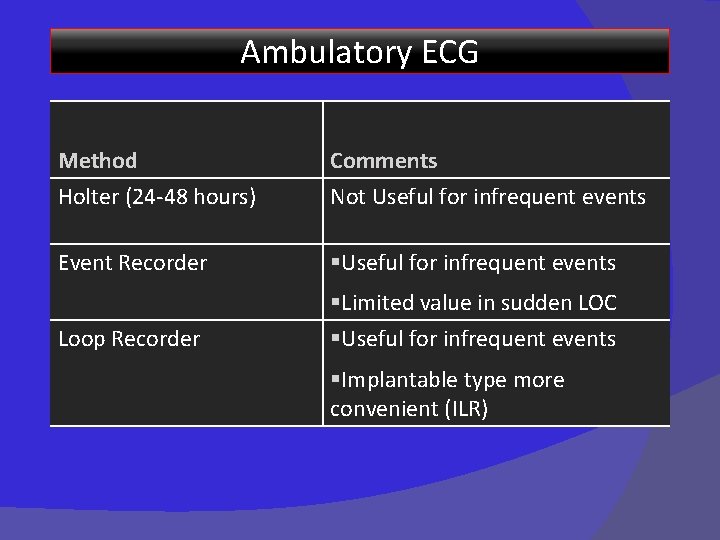
Ambulatory ECG Method Holter (24 -48 hours) Comments Not Useful for infrequent events Event Recorder §Useful for infrequent events Loop Recorder §Limited value in sudden LOC §Useful for infrequent events §Implantable type more convenient (ILR)
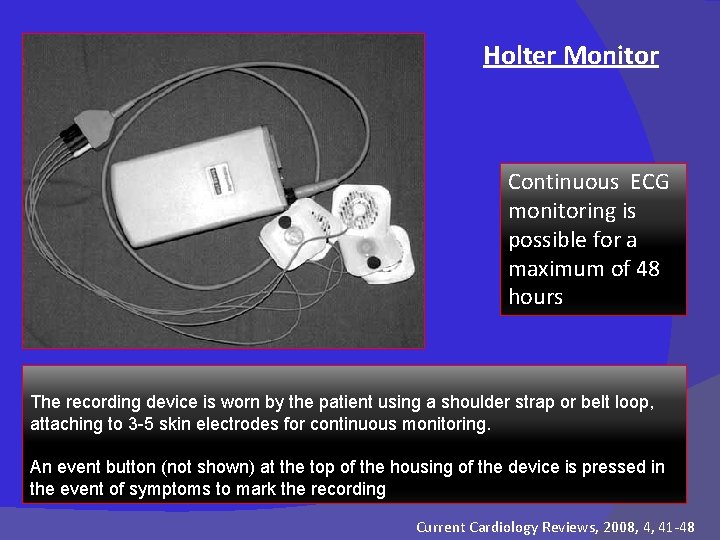
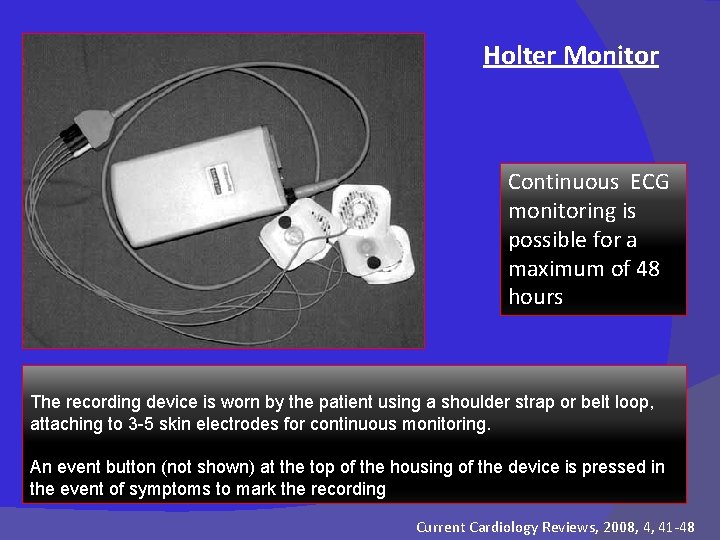
Holter Monitor Continuous ECG monitoring is possible for a maximum of 48 hours The recording device is worn by the patient using a shoulder strap or belt loop, attaching to 3 -5 skin electrodes for continuous monitoring. An event button (not shown) at the top of the housing of the device is pressed in the event of symptoms to mark the recording Current Cardiology Reviews, 2008, 4, 41 -48
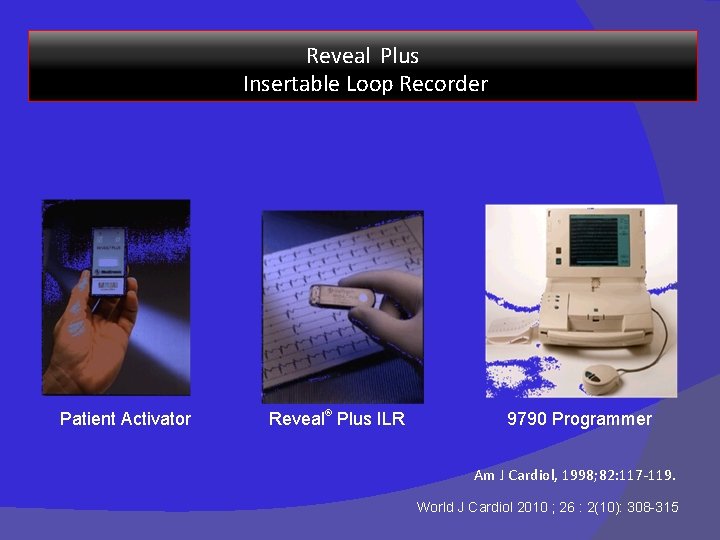
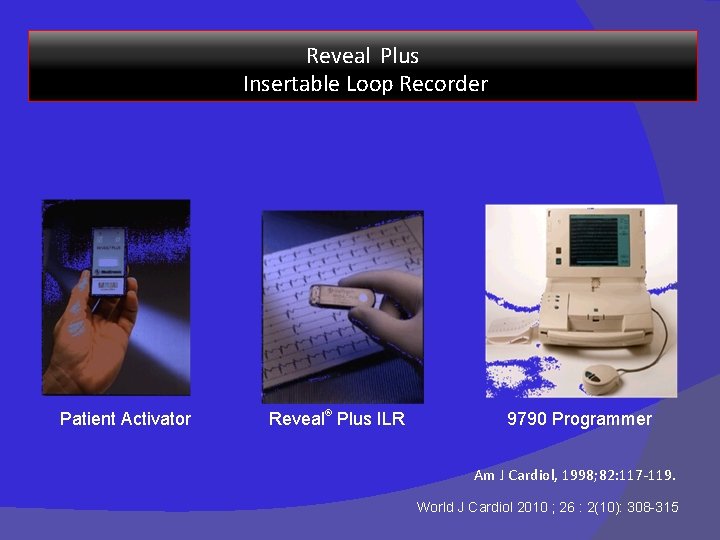
Reveal Plus Insertable Loop Recorder Patient Activator Reveal® Plus ILR 9790 Programmer Am J Cardiol, 1998; 82: 117 -119. World J Cardiol 2010 ; 26 : 2(10): 308 -315
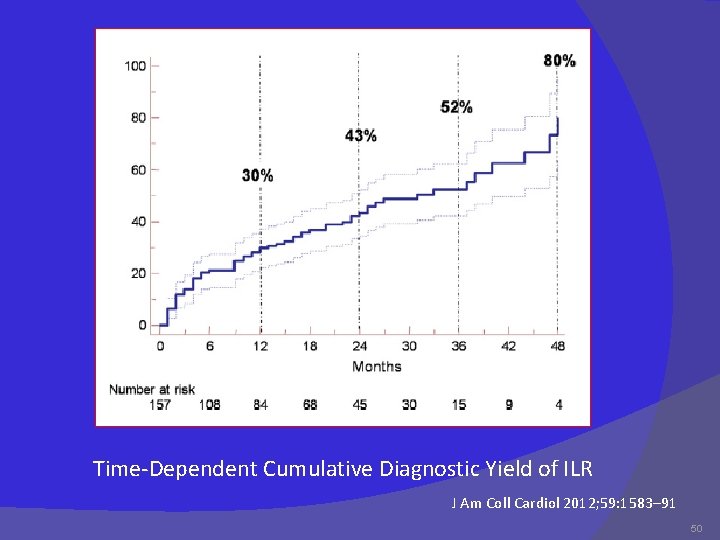
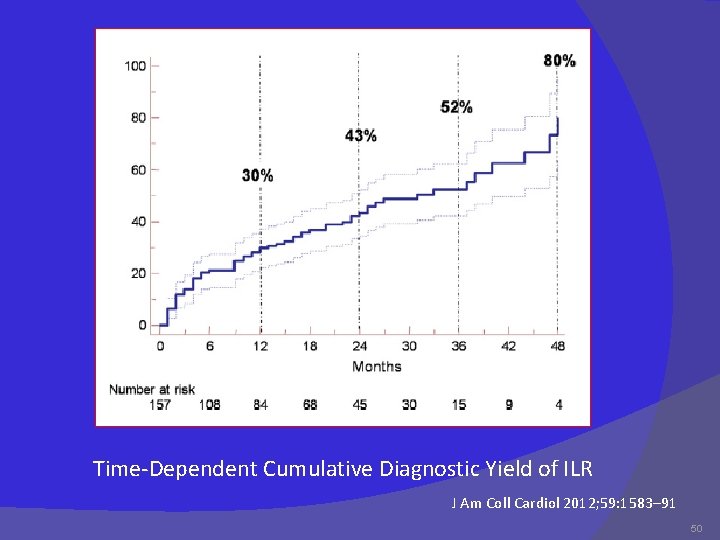
Time-Dependent Cumulative Diagnostic Yield of ILR J Am Coll Cardiol 2012; 59: 1583– 91 50
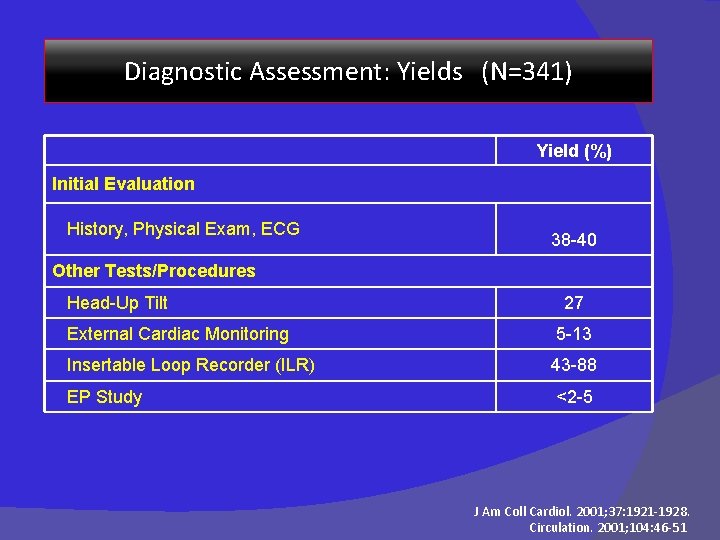
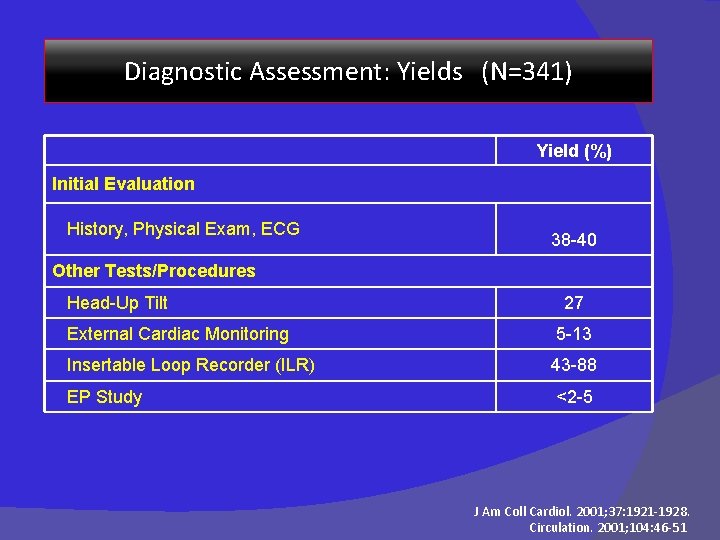
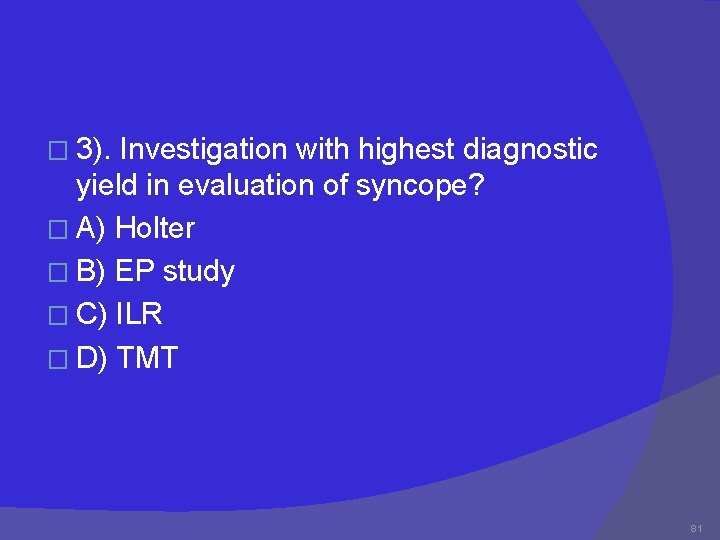
Diagnostic Assessment: Yields (N=341) Yield (%) Initial Evaluation History, Physical Exam, ECG 38 -40 Other Tests/Procedures Head-Up Tilt 27 External Cardiac Monitoring 5 -13 Insertable Loop Recorder (ILR) 43 -88 EP Study <2 -5 J Am Coll Cardiol. 2001; 37: 1921 -1928. Circulation. 2001; 104: 46 -51
Treatment of Neurocardiogenic syncope 52

Management Strategies for VVS � Optimal management strategies for VVS are a source of debate � Patient education, reassurance, instruction � Fluids, salts � Tilt Training � Drug therapies � Pacing � Class IIb indication for VVS patients with positive HUT and cardioinhibitory or mixed reflex
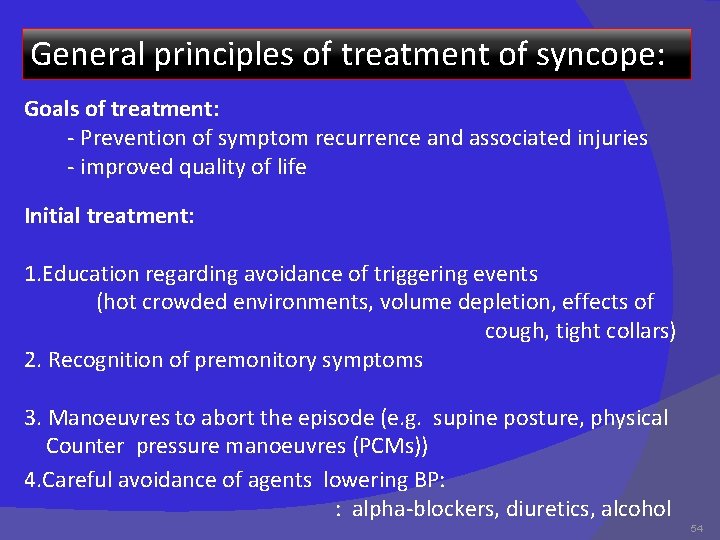
General principles of treatment of syncope: Goals of treatment: - Prevention of symptom recurrence and associated injuries - improved quality of life Initial treatment: 1. Education regarding avoidance of triggering events (hot crowded environments, volume depletion, effects of cough, tight collars) 2. Recognition of premonitory symptoms 3. Manoeuvres to abort the episode (e. g. supine posture, physical Counter pressure manoeuvres (PCMs)) 4. Careful avoidance of agents lowering BP: : alpha-blockers, diuretics, alcohol 54
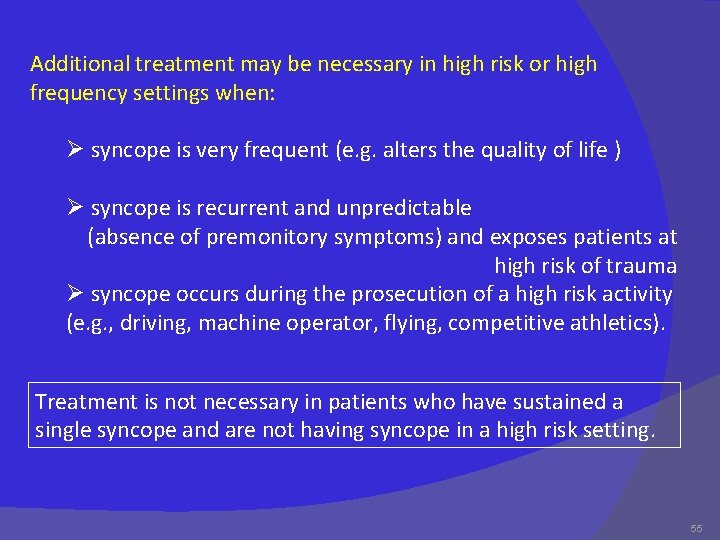
Additional treatment may be necessary in high risk or high frequency settings when: Ø syncope is very frequent (e. g. alters the quality of life ) Ø syncope is recurrent and unpredictable (absence of premonitory symptoms) and exposes patients at high risk of trauma Ø syncope occurs during the prosecution of a high risk activity (e. g. , driving, machine operator, flying, competitive athletics). Treatment is not necessary in patients who have sustained a single syncope and are not having syncope in a high risk setting. 55
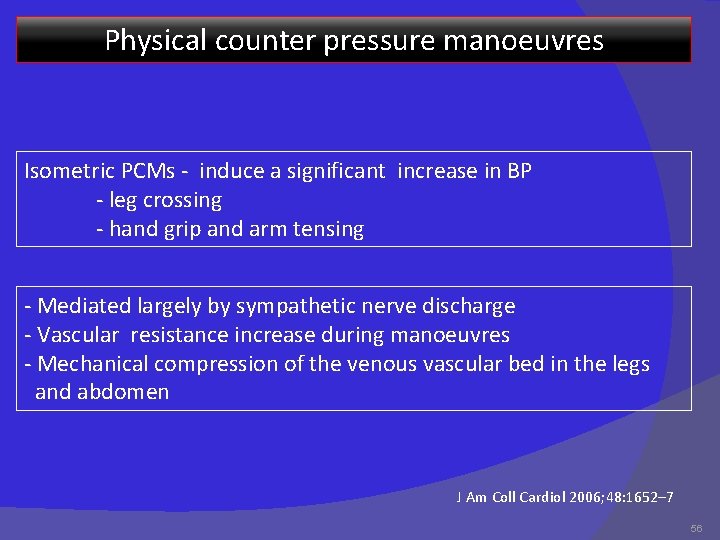
Physical counter pressure manoeuvres Isometric PCMs - induce a significant increase in BP - leg crossing - hand grip and arm tensing - Mediated largely by sympathetic nerve discharge - Vascular resistance increase during manoeuvres - Mechanical compression of the venous vascular bed in the legs and abdomen J Am Coll Cardiol 2006; 48: 1652– 7 56
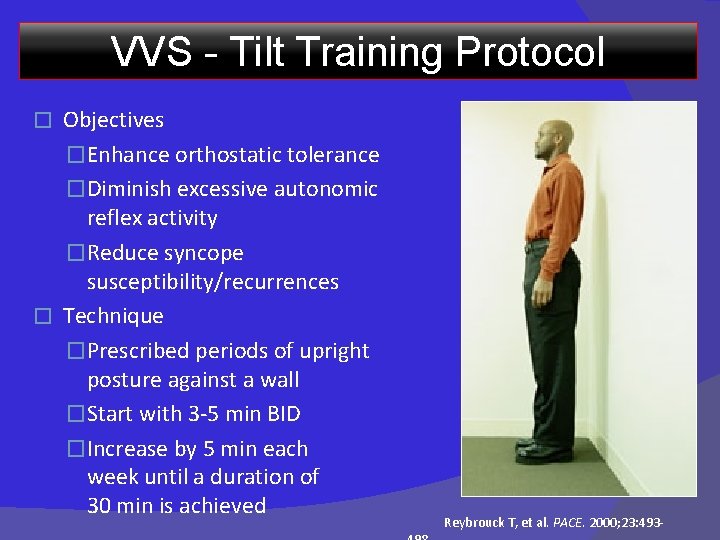
VVS - Tilt Training Protocol Objectives �Enhance orthostatic tolerance �Diminish excessive autonomic reflex activity �Reduce syncope susceptibility/recurrences � Technique �Prescribed periods of upright posture against a wall �Start with 3 -5 min BID �Increase by 5 min each week until a duration of 30 min is achieved � Reybrouck T, et al. PACE. 2000; 23: 493 -
VVS: Pharmacologic treatment Salt /Volume � Salt tablets � fludrocortisone � Beta-adrenergic blockers � � Disopyramide SSRIs Paroxetine � Vasoconstrictors Midodrine Etilephrine �
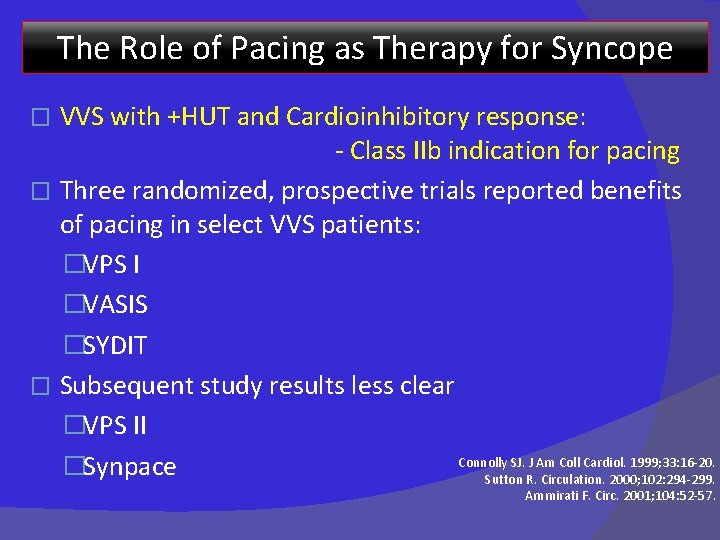
The Role of Pacing as Therapy for Syncope VVS with +HUT and Cardioinhibitory response: - Class IIb indication for pacing � Three randomized, prospective trials reported benefits of pacing in select VVS patients: �VPS I �VASIS �SYDIT � Subsequent study results less clear �VPS II Connolly SJ. J Am Coll Cardiol. 1999; 33: 16 -20. �Synpace Sutton R. Circulation. 2000; 102: 294 -299. � Ammirati F. Circ. 2001; 104: 52 -57.
VPS I (North American Vasovagal Pacemaker Study) � � � Objective: �To evaluate pacemaker therapy for severe recurrent vasovagal syncope Randomized, prospective, single center N=54 patients � 27: DDD pacemaker with rate drop response � 27: No pacemaker Inclusion: ≥ 6 lifetime episodes of syncope & +ve HUT Primary outcome: First recurrence of syncope Connolly SJ. J Am Coll Cardiol. 1999; 33: 16 -20.
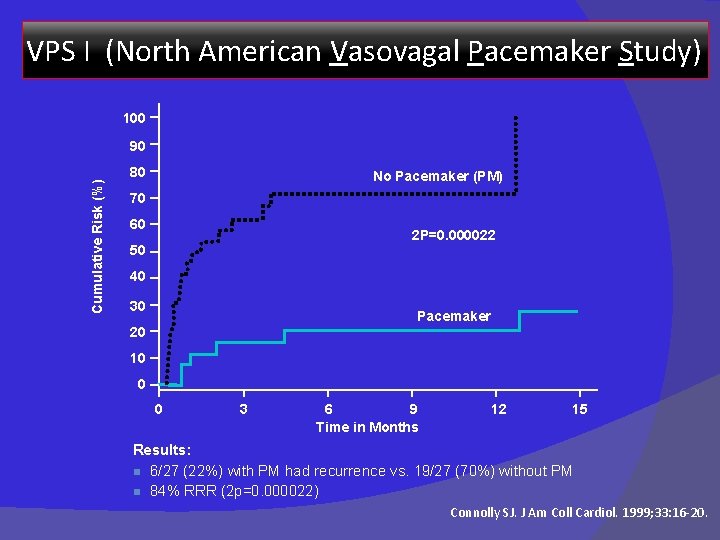
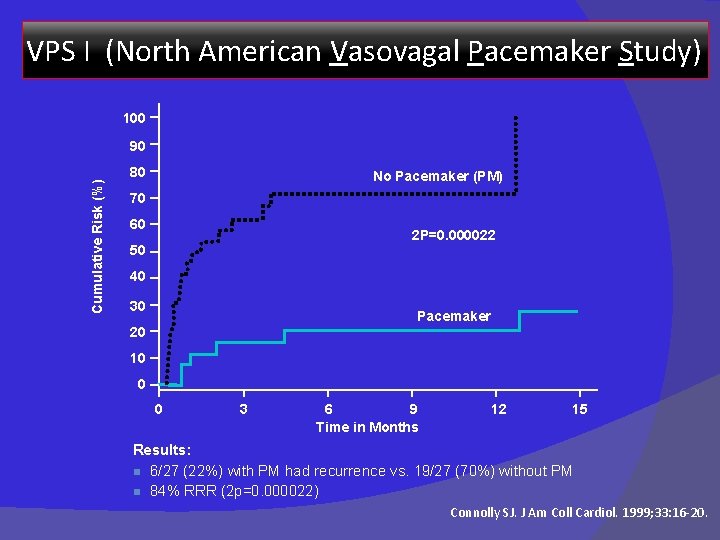
VPS I (North American Vasovagal Pacemaker Study) 100 Cumulative Risk (%) 90 80 No Pacemaker (PM) 70 60 2 P=0. 000022 50 40 30 Pacemaker 20 10 0 0 3 6 9 Time in Months 12 15 Results: n 6/27 (22%) with PM had recurrence vs. 19/27 (70%) without PM n 84% RRR (2 p=0. 000022) Connolly SJ. J Am Coll Cardiol. 1999; 33: 16 -20.
VASIS (VAsovagal Syncope International Study) � � � Objective: �To evaluate pacemaker therapy for severe cardioinhibitory tilt -positive neurally mediated syncope Randomized, prospective, multi-center N=42 patients � 19: Dual chamber pacemaker with rate hysteresis � 23: No pacemaker Inclusion: Positive cardioinhibitory response Primary outcome: First recurrence of syncope Sutton R. Circulation. 2000; 102: 294 -299.
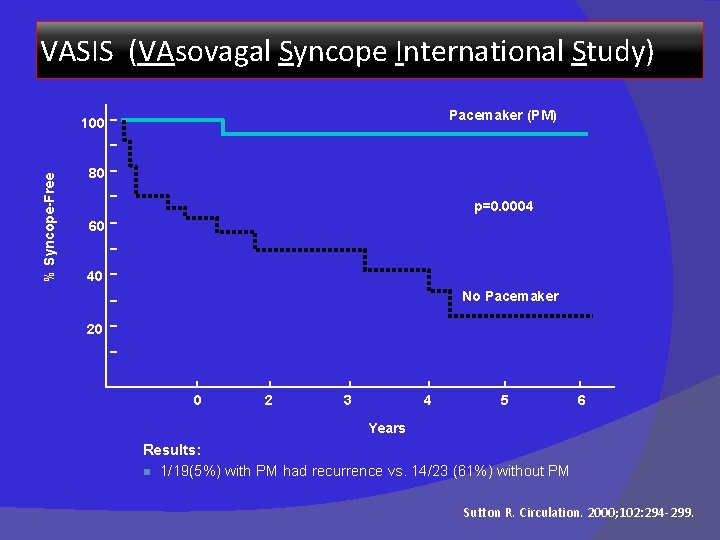
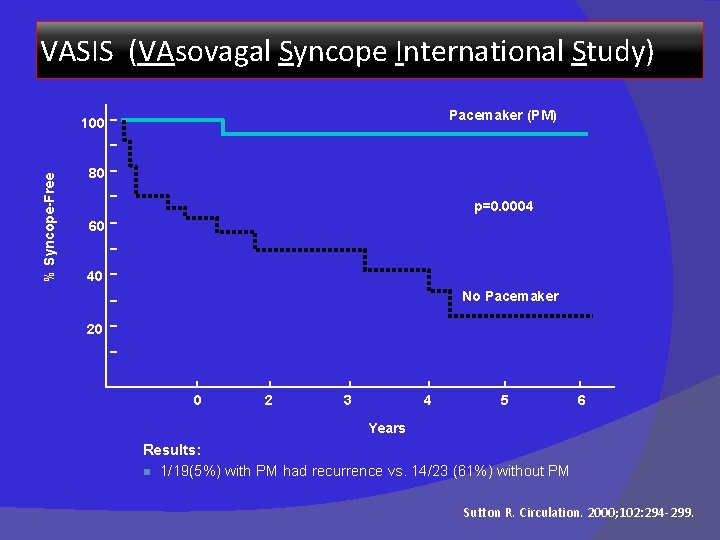
VASIS (VAsovagal Syncope International Study) Pacemaker (PM) % Syncope-Free 100 80 p=0. 0004 60 40 No Pacemaker 20 0 2 3 4 5 6 Years Results: n 1/19(5%) with PM had recurrence vs. 14/23 (61%) without PM Sutton R. Circulation. 2000; 102: 294 -299.
SYDIT (SYncope Diagnosis and Treatment) � � � Objective: �To compare the effects of cardiac pacing with pharmacological therapy in patients with recurrent vasovagal syncope Randomized, prospective, multi-center N=93 patients � 46: DDD pacemaker with rate drop response � 47: Atenolol 100 mg/d Inclusion: Positive HUT with relative bradycardia Primary outcome: First recurrence of syncope Ammirati F. Circulation. 2001; 104: 52 -57.
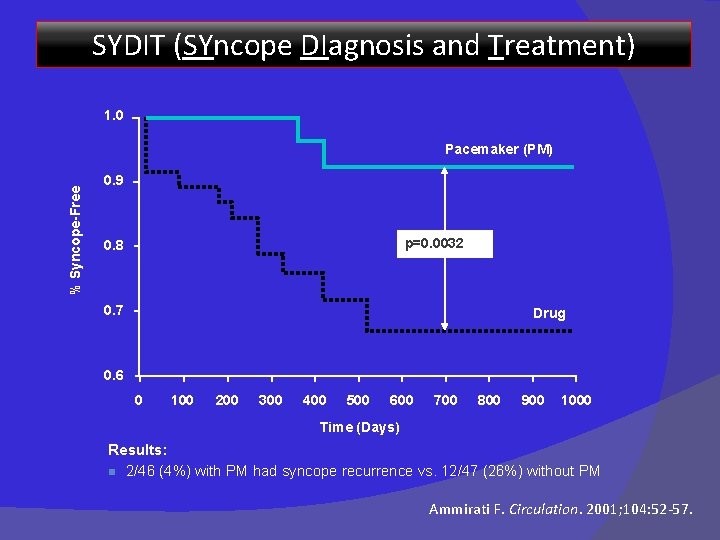
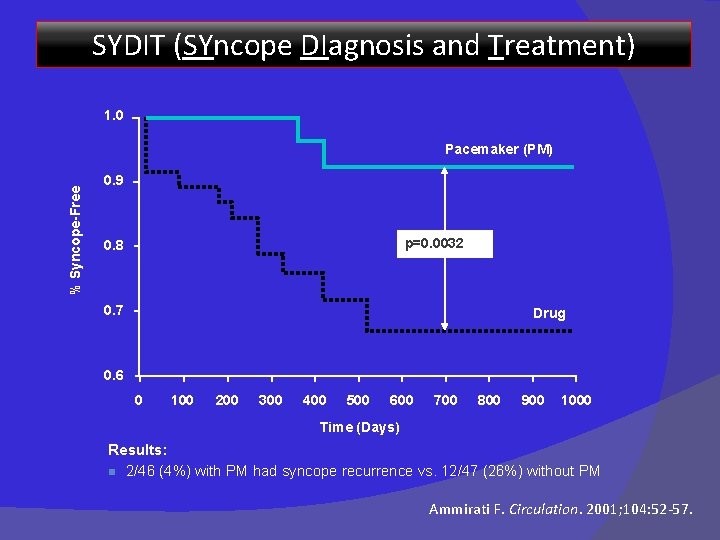
SYDIT (SYncope DIagnosis and Treatment) 1. 0 % Syncope-Free Pacemaker (PM) 0. 9 p=0. 0032 0. 8 0. 7 Drug 0. 6 0 100 200 300 400 500 600 700 800 900 1000 Time (Days) Results: n 2/46 (4%) with PM had syncope recurrence vs. 12/47 (26%) without PM Ammirati F. Circulation. 2001; 104: 52 -57.
VPS II (Vasovagal Pacemaker Study II) � � � Objective: �To determine if pacing therapy reduces the risk of syncope in patients with vasovagal syncope Randomized, double-blind, prospective, multi-center N=100 patients � 52: Only sensing without pacing � 48: DDD pacemaker with rate drop response Inclusion: Positive HUT with (HR x BP) < 6000/min x mm Hg Primary outcome: First recurrence of syncope Connolly S. JAMA. 2003; 289: 2224 -2229.
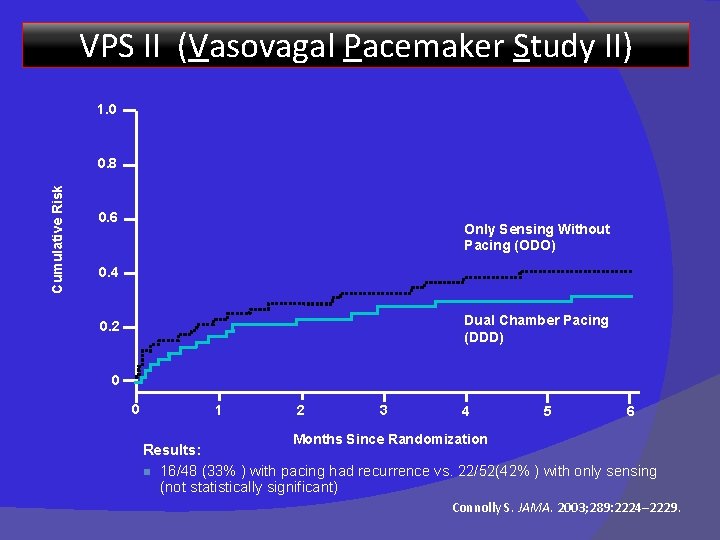
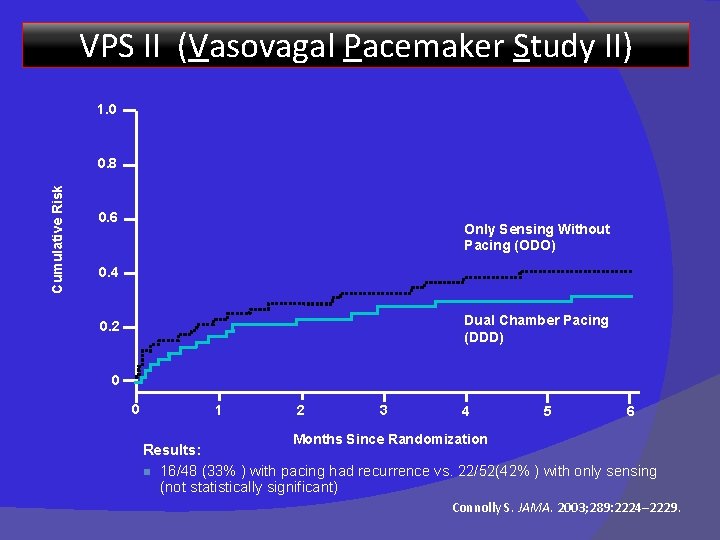
VPS II (Vasovagal Pacemaker Study II) 1. 0 Cumulative Risk 0. 8 0. 6 Only Sensing Without Pacing (ODO) 0. 4 Dual Chamber Pacing (DDD) 0. 2 0 0 1 2 3 4 5 6 Months Since Randomization Results: n 16/48 (33% ) with pacing had recurrence vs. 22/52(42% ) with only sensing (not statistically significant) Connolly S. JAMA. 2003; 289: 2224– 2229.
SYNPACE (Vasovagal SYNcope and PACing) � � � Objective: To determine if pacing therapy will reduce syncope relapses in patients with recurrent vasovagal syncope, compared to those with a pacemaker programmed to OFF Randomized, double-blind, prospective, multi-center, placebo-controlled N=29 patients � 16: DDD PM with rate drop response programmed ON � 13: PM programmed OFF (OOO mode) Inclusion: Recurrent VVS and +HUT with asystolic or mixed response Primary outcome: First recurrence of syncope Raviele A, et al. Eur Heart J. 2004; 25: 1741 -1748.
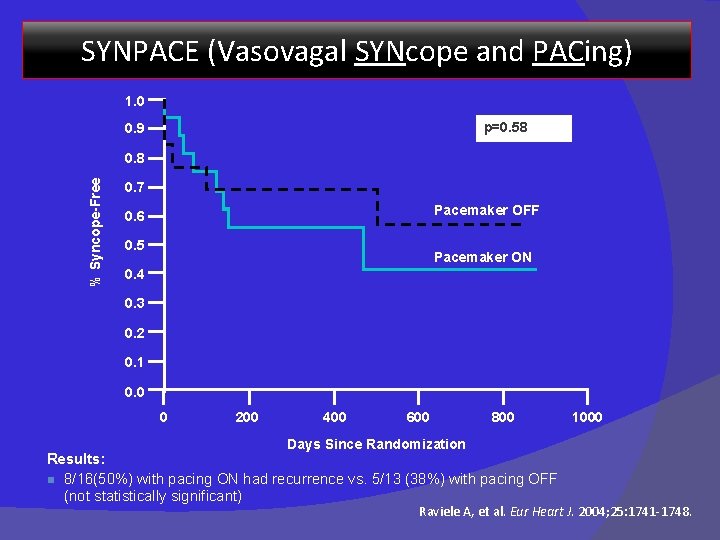
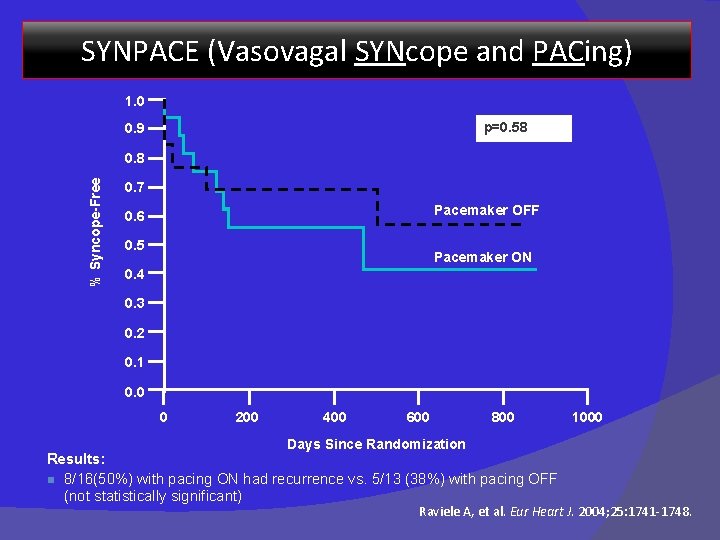
SYNPACE (Vasovagal SYNcope and PACing) 1. 0 p=0. 58 0. 9 % Syncope-Free 0. 8 0. 7 Pacemaker OFF 0. 6 0. 5 Pacemaker ON 0. 4 0. 3 0. 2 0. 1 0. 0 0 200 400 600 800 1000 Days Since Randomization Results: n 8/16(50%) with pacing ON had recurrence vs. 5/13 (38%) with pacing OFF (not statistically significant) Raviele A, et al. Eur Heart J. 2004; 25: 1741 -1748.
Role of Pacing as Therapy for Syncope: Summary Pacemaker implantation may modulate reflex syncope and autonomic responses � Study results may differ based on pre-implant selection criteria and tilt-testing techniques � Pacing therapy is effective in some but not all (cardioinhibition vs. vasodepression) � In five pacing studies, syncope recurred in 33/156 (21%) of paced patients, 72/162 (44%) in non-paced patients (p<0. 000) � Kapoor W. JAMA. 2003; 289: 2272 -2275.
CSS : Role of Pacing – Syncope Recurrence Rate � Class I indication for pacing (AHA and HRS) � Limit pacing to CSS that is: �Cardioinhibitory �Mixed � DDD/DDI superior to VVI If the diagnosis of CSH is based on a >3 -second pause with carotid sinus massage without clear, provocative events, pacemaker implantation is less strongly recommended (Class IIa).
VVS Pacing Trials Conclusions DDD pacing reduces the risk of syncope in patients with recurrent, refractory, highly-symptomatic, cardioinhibitory vasovagal syncope.

SAFE PACE Syncope And Falls in the Elderly – Pacing And Carotid Sinus Evaluation Objective �Determine whether cardiac pacing reduces falls in older adults with carotid sinus hypersensitivity � Randomized controlled trial (N=175) �Adults > 50 years, non-accidental fall, positive CSM �Pacing (n=87) vs. No Pacing (n=88) � � Results �More than 1/3 of adults over 50 years presented to the ER because of a fall �With pacing, falls 70% �Syncopal events 53% �Injurious events 70% Kenny RA. J Am Coll Cardiol. 2001; 38: 1491 -1496.
SAFE PACE � Conclusions �Strong association between non-accidental falls and cardioinhibitory CSH �Cardiac pacing significantly reduced subsequent falls �CSH should be considered in all older adults who have non-accidental falls Kenny RA, J Am Coll Cardiol. 2001; 38: 1491 -1496.
Conclusion Syncope is a common symptom with many causes � Deserves thorough investigation and appropriate treatment � A disciplined approach is essential � ESC guidelines offer current best practices �

REFERENCES 1. Guidelines for the diagnosis and management of syncope (version 2009)- The Task Force for the Diagnosis and Management of Syncope of the European Society of Cardiology (ESC)-European Heart Journal (2009) 30, 2631– 2671 2. Guidelines on Management (Diagnosis and Treatment) of Syncope Update 2004 Europace (2004) 6, 467 e 537 3. Kapoor- Syncope Review article New Eng J Med 2000, 12; 1856 -1867 4. Steve W Parry, Maw Pin Tan- clinical review- An approach to the evaluation and management of syncope in adults BMJ 2010; 340: c 880 5. Paula Gonçalves Macedo Tilt Test - from the Necessary to the Indispensable. Arq Bras Cardiol 2011; 96(3): 246 -254 6. Rajesh Subbiah Syncope: Review of Monitoring Modalities Current Cardiology Reviews 2008, 4, 41 -48 7. Michele Brignole, New Concepts in the Assessment of Syncope J Am Coll Cardiol 2012; 59: 1583– 91 8. Kapoor- Current evaluation of syncope Circulation. 2002; 106: 1606 -1609 9. Paolo Alboni Diagnostic Value of History in Patients With Syncope With or Without Heart Disease J Am Coll Cardiol 2001; 37: 1921– 8 10. Nynke van Dijk. Effectiveness of Physical Counterpressure Maneuvers in Preventing Vasovagal Syncope The Physical Counterpressure Manoeuvres Trial (PC-Trial) J Am Coll Cardiol 2006; 48: 1652– 7 11. Nevin T Wijesekera, Arvinder S Kurbaan Pacing for Vasovagal Syncope. Indian Pacing and Electr. Journal 2002 2(4): 114 -119 12. Blair P. Grubb, M. D Neurocardiogenic Syncope N Engl J Med 2005; 352: 1004 -10. 76

13. Joanne L. Evaluation and Management of Syncope Clinical Scholars Review, Vol. 2, No. 2, 2009 14. Attilio Del Rosso Relation of Clinical Presentation of Syncope to the Age of Patients Am J Cardiol 2005; 96: 1431– 1435 15. Chad Kessler The Emergency Department Approach to Syncope: Evidence-based Guidelines and Prediction Emerg Med Clin N Am 28 (2010) 487– 50 16. STUART J. The North American Vasovagal Pacemaker Study (VPS) A Randomized Trial of Permanent Cardiac Pacing for the Prevention of Vasovagal Syncope J Am Coll Cardiol 1999; 33: 16– 20 17. Richard Sutton et al. Dual-Chamber Pacing in the Treatment of Neurally Mediated Tilt-Positive Cardioinhibitory Syncope Pacemaker Versus No Therapy: A Multicenter Randomized Study Circulation. 2000; 102: 294 -299 18. Fabrizio Ammirati et al. Permanent Cardiac Pacing Versus Medical Treatment for the Prevention of Recurrent Vasovagal Circulation. 2001; 104: 52 -57 19. Rose Anne M. Kenny Carotid Sinus Syndrome: A Modifiable Risk Factor for Non accidental Falls in Older Adults (SAFE PACE) J Am Coll Cardiol 2001; 38: 1491– 6 20. Ward. Midodrine: a role in the management of neurocardiogenic syncope. Heart 1998; 79: 45– 49 21. Peter et al. Fludrocortisone in neurally mediated hypotension chronic fatigue syndrome JAMA 2001; 285: 52 -59. 22. Antonio Raviele et al. Effect of Etilefrine in Preventing Syncopal Recurrence in Patients With Vasovagal Syncope -A Double-Blind, Randomized, Placebo-Controlled Trial Circulation. 1999; 99: 1452 -1457. 23. Enrico Di Girolamo et al. Effects of Paroxetine Hydrochloride : A Selective Serotonin Reuptake Inhibitor, on Refractory Vasovagal Syncope: A Randomized, Double-blind, Placebo-controlled Study J Am Coll Cardiol 1999; 33: 1227– 30. 77

THANK YOU 78
MCQs � 1. Drugs proven to be useful in VVS except � A) Midodrine � B) Etilefrine � C) Fludrocortisone � D) Paroxetine � E) Atenolol 79
� 2). Carotid sinus hypersensitivity (CSH) : incorrect ? � A) a ventricular pause lasting > 3 s � B) a fall in systolic BP of >50 mm. Hg � C) A & B � D) BP < 100 mm Hg 80
� 3). Investigation with highest diagnostic yield in evaluation of syncope? � A) Holter � B) EP study � C) ILR � D) TMT 81
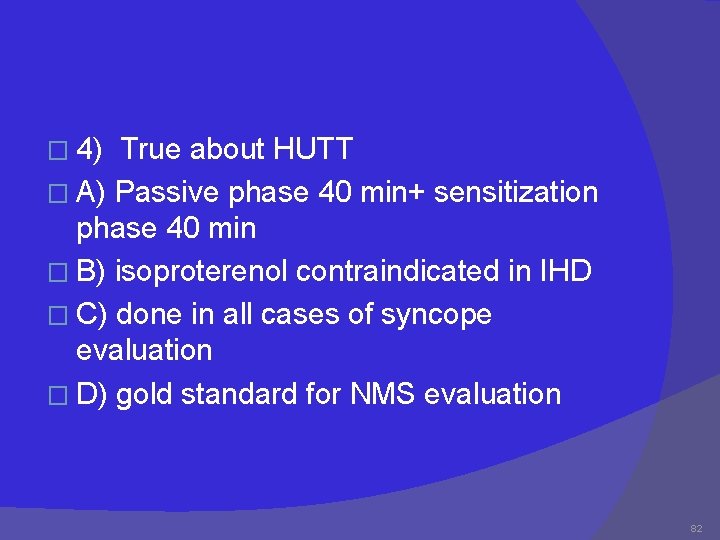
� 4) True about HUTT � A) Passive phase 40 min+ sensitization phase 40 min � B) isoproterenol contraindicated in IHD � C) done in all cases of syncope evaluation � D) gold standard for NMS evaluation 82
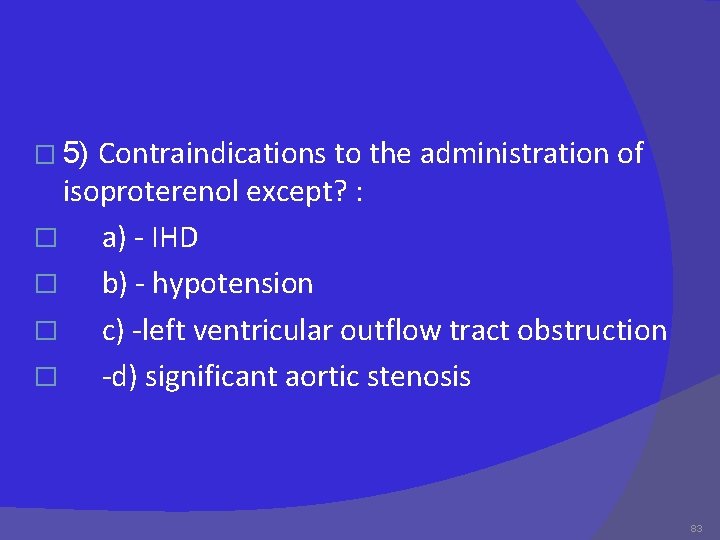
Contraindications to the administration of isoproterenol except? : � a) - IHD � b) - hypotension � c) -left ventricular outflow tract obstruction � -d) significant aortic stenosis � 5) 83
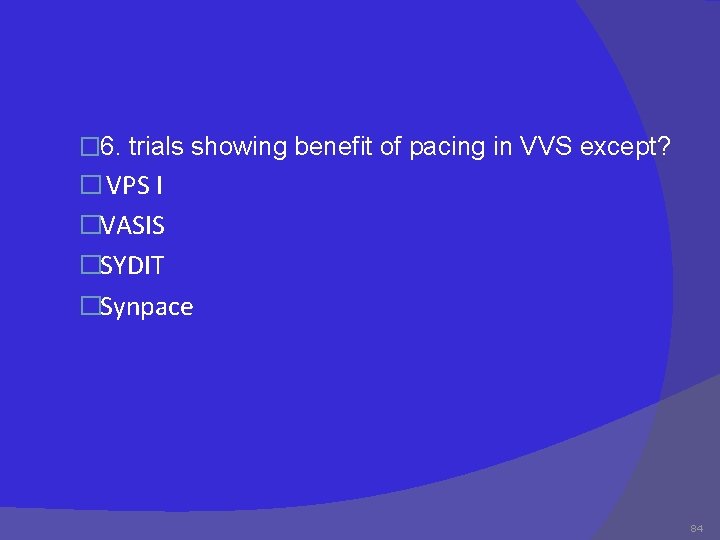
� 6. trials showing benefit of pacing in VVS except? � VPS I �VASIS �SYDIT �Synpace 84
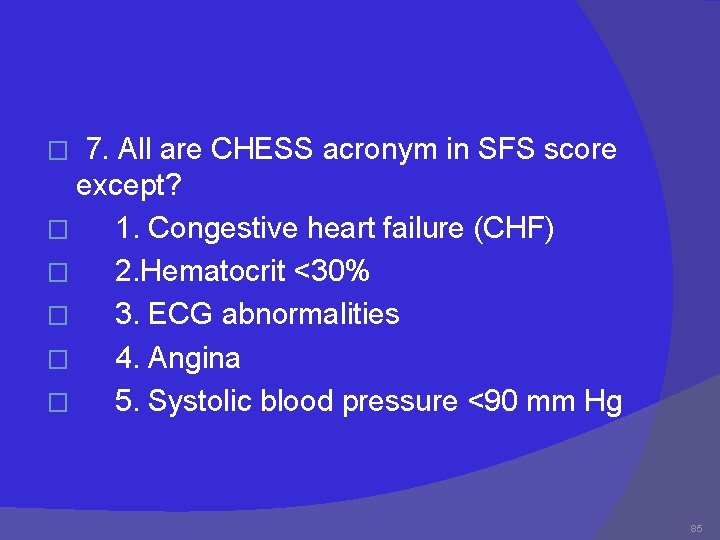
7. All are CHESS acronym in SFS score except? � 1. Congestive heart failure (CHF) � 2. Hematocrit <30% � 3. ECG abnormalities � 4. Angina � 5. Systolic blood pressure <90 mm Hg � 85

� 8) True about CSS except? a) Sensory nerve endings in the carotid sinus walls respond to deformation � B) “Deafferentation” of neck muscles may contribute � C) Increased afferent signals to brain stem � Reflex decrease in efferent vagal activity and diminution of sympathetic tone results in bradycardia and vasodilatation 86
� 9. True about pacing in NMS except? � A) class I recommendation in CSS � B) Calss II b recommendation In VVS � C) DDD with rate drop response is preferred � D) none 87
� 10. All are trials in VVS except? � A) VPS 1 � B) Issue 3 � C) VASIS � D) SAFE pace trial 88
 Definition of nursing diagnosis
Definition of nursing diagnosis Medical diagnosis and nursing diagnosis difference
Medical diagnosis and nursing diagnosis difference Types of nursing diagnosis
Types of nursing diagnosis Nursing process and critical thinking
Nursing process and critical thinking Syncope in the older patient is
Syncope in the older patient is Provoked seizure
Provoked seizure Syncope vs seizure
Syncope vs seizure Vertebrobasilaire tia
Vertebrobasilaire tia Chess score syncope
Chess score syncope Snycope
Snycope Nursing care plan for syncope
Nursing care plan for syncope Syncope
Syncope Syncope
Syncope Syncope
Syncope Perbedaan diagnosis gizi dan diagnosis medis
Perbedaan diagnosis gizi dan diagnosis medis Initial approach fix
Initial approach fix Difference between datagram and virtual circuit
Difference between datagram and virtual circuit Tony wagner's seven survival skills
Tony wagner's seven survival skills Type 1 diabetes in adults diagnosis and management
Type 1 diabetes in adults diagnosis and management Theoretical models of counseling
Theoretical models of counseling Waterfall strategy
Waterfall strategy Multiple approach-avoidance
Multiple approach-avoidance Bandura's reciprocal determinism
Bandura's reciprocal determinism Approach research meaning
Approach research meaning Traditional approach to systems implementation
Traditional approach to systems implementation System planning and initial investigation
System planning and initial investigation Ust grading system
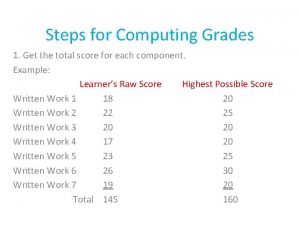
Ust grading system Initial velocity and final velocity formula
Initial velocity and final velocity formula Deceleration on velocity time graph
Deceleration on velocity time graph Primary resistance form definition
Primary resistance form definition Initial ray and terminal ray
Initial ray and terminal ray Project screening methods
Project screening methods Initial value theorem
Initial value theorem Derivation of laplace transform
Derivation of laplace transform Trusteeship management
Trusteeship management Scientific management
Scientific management Management pyramid
Management pyramid Top level management
Top level management Cecpd
Cecpd Impulse and momentum in basketball
Impulse and momentum in basketball Which graph best represents the greatest amount of work
Which graph best represents the greatest amount of work How to find initial pressure in boyle's law
How to find initial pressure in boyle's law The watch poem by frances cornford
The watch poem by frances cornford Repetition of the same beginning sound
Repetition of the same beginning sound Test resurse naturale
Test resurse naturale Dialogue initial mariage r71
Dialogue initial mariage r71 Repetition of initial consonant sounds
Repetition of initial consonant sounds Is the repetition of initial consonant sounds
Is the repetition of initial consonant sounds Repetition of beginning sounds of words.
Repetition of beginning sounds of words. S box in des
S box in des Initial value theorem
Initial value theorem Laplace transform
Laplace transform Is v final velocity
Is v final velocity Investigate a factor affecting the initial rate of reaction
Investigate a factor affecting the initial rate of reaction Cme market profile handbook pdf
Cme market profile handbook pdf Initial value problem
Initial value problem Labored breathing
Labored breathing From to chart
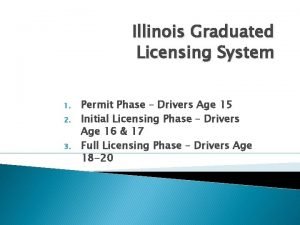
From to chart During the initial licensing phase
During the initial licensing phase Gcu annuities
Gcu annuities Mathematical expression of boyle's law
Mathematical expression of boyle's law Fact finding questions examples
Fact finding questions examples Scenario ideas
Scenario ideas The initial operational capability milestone occurs
The initial operational capability milestone occurs Initial value theorem
Initial value theorem Initial outlay
Initial outlay Initial outlay formula
Initial outlay formula Capital budgeting process
Capital budgeting process Authors by initials
Authors by initials The repetition of initial consonant sounds
The repetition of initial consonant sounds Examples of consonance
Examples of consonance Miss maudie atkinson quotes chapters 4-6
Miss maudie atkinson quotes chapters 4-6 Bernoulli equation conservation of energy
Bernoulli equation conservation of energy Initial observation definition
Initial observation definition Sa 510 initial audit engagement
Sa 510 initial audit engagement Rapid health assessment adalah
Rapid health assessment adalah Repeating consonants at the beginning of words
Repeating consonants at the beginning of words Method of initial rates
Method of initial rates Selection
Selection Security briefing example
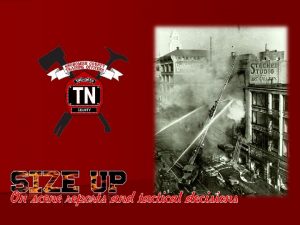
Security briefing example Blue card initial radio report
Blue card initial radio report Initial layout
Initial layout Factor-isolating
Factor-isolating Secondary resistance and retention form features
Secondary resistance and retention form features Initial ideas example
Initial ideas example Constraints when building a bridge
Constraints when building a bridge Initial eval
Initial eval Graduated drivers license alabama
Graduated drivers license alabama Please initial box
Please initial box