Pathophysiology of reflex syncope Mechanisms of Vasovagal Syncope
- Slides: 39
Pathophysiology of reflex syncope
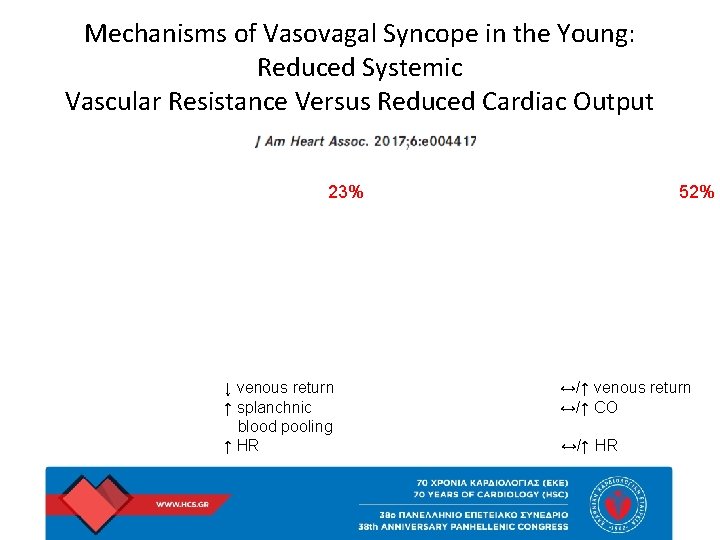
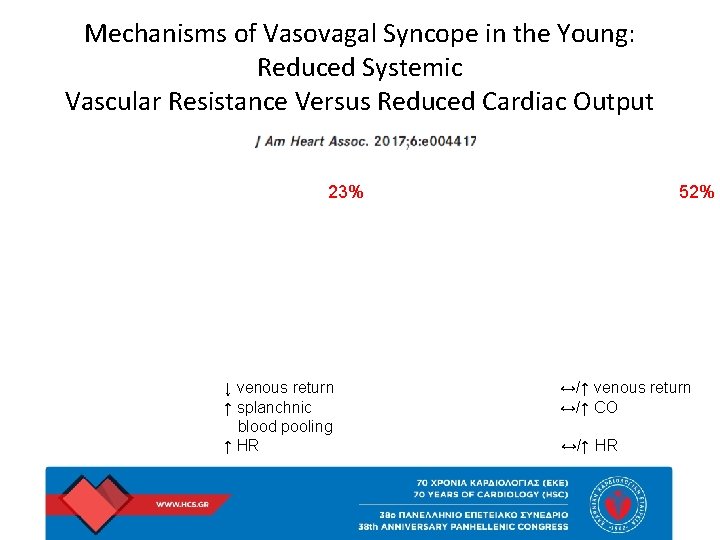
Mechanisms of Vasovagal Syncope in the Young: Reduced Systemic Vascular Resistance Versus Reduced Cardiac Output 23% ↓ venous return ↑ splanchnic blood pooling ↑ HR 52% ↔/↑ venous return ↔/↑ CO ↔/↑ HR
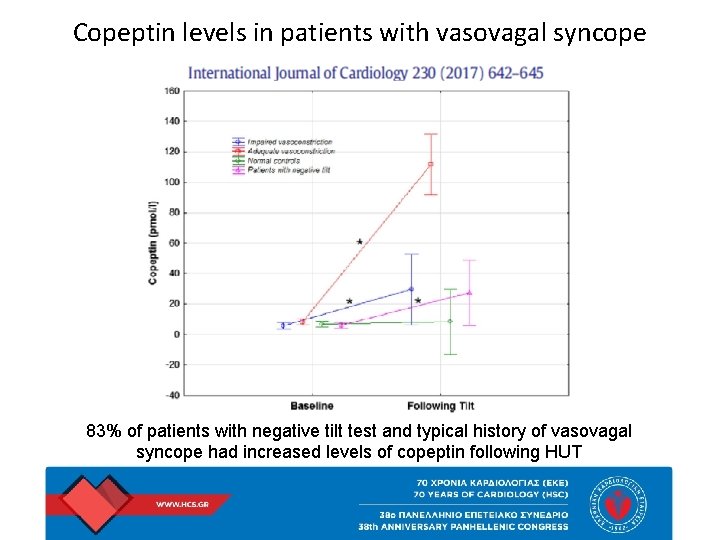
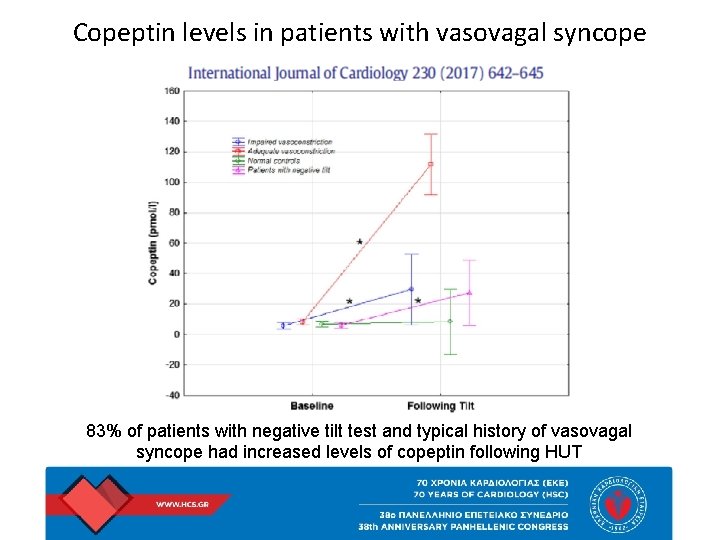
Copeptin levels in patients with vasovagal syncope 83% of patients with negative tilt test and typical history of vasovagal syncope had increased levels of copeptin following HUT
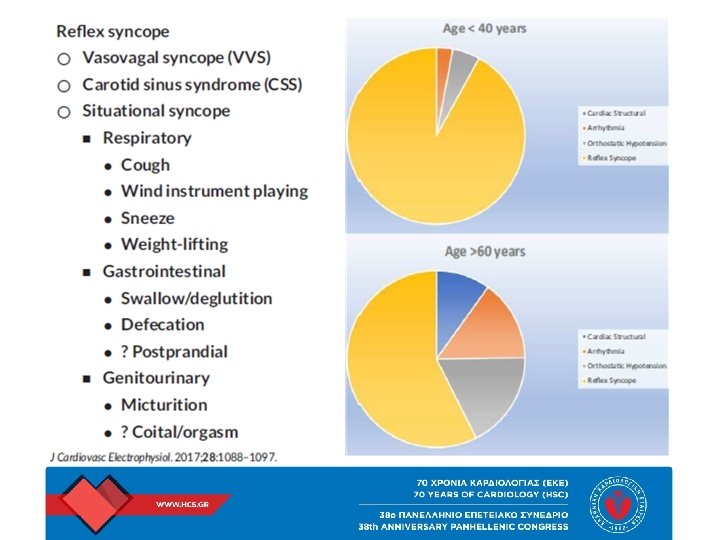
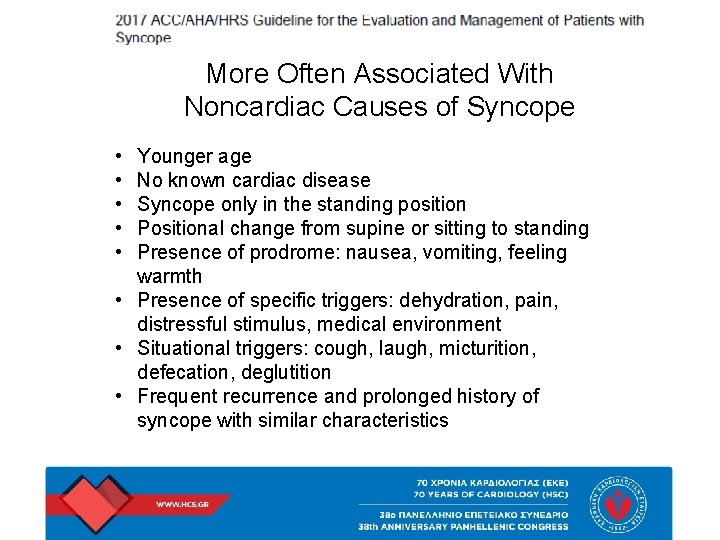
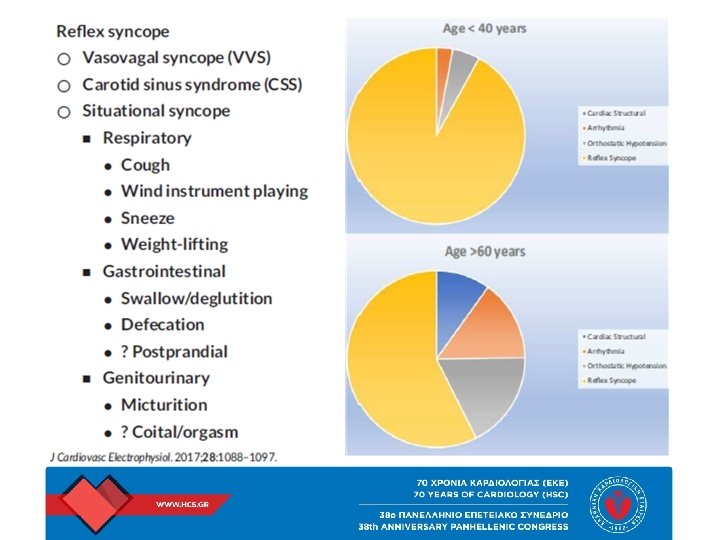
More Often Associated With Noncardiac Causes of Syncope • • • Younger age No known cardiac disease Syncope only in the standing position Positional change from supine or sitting to standing Presence of prodrome: nausea, vomiting, feeling warmth • Presence of specific triggers: dehydration, pain, distressful stimulus, medical environment • Situational triggers: cough, laugh, micturition, defecation, deglutition • Frequent recurrence and prolonged history of syncope with similar characteristics
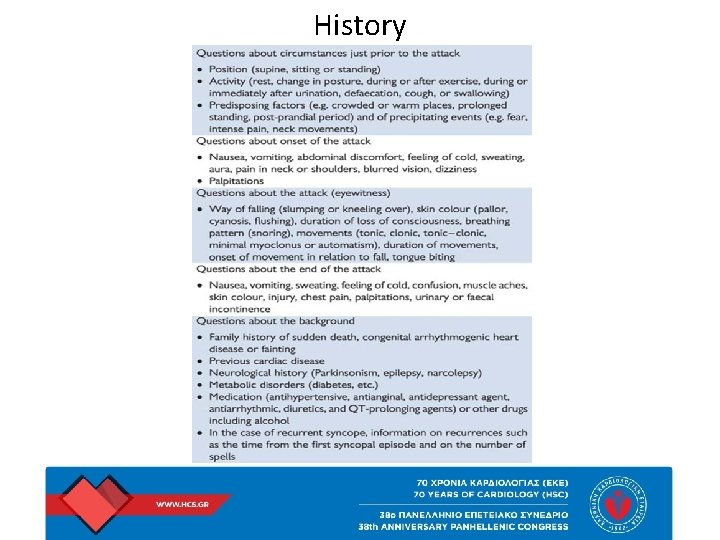
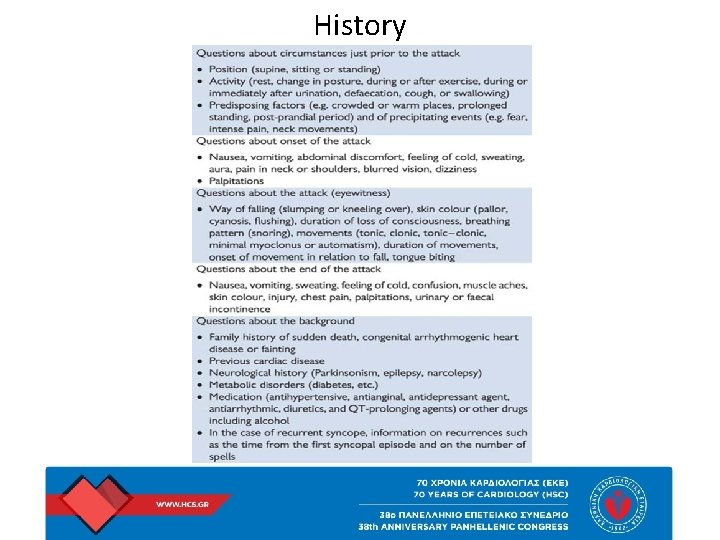
History
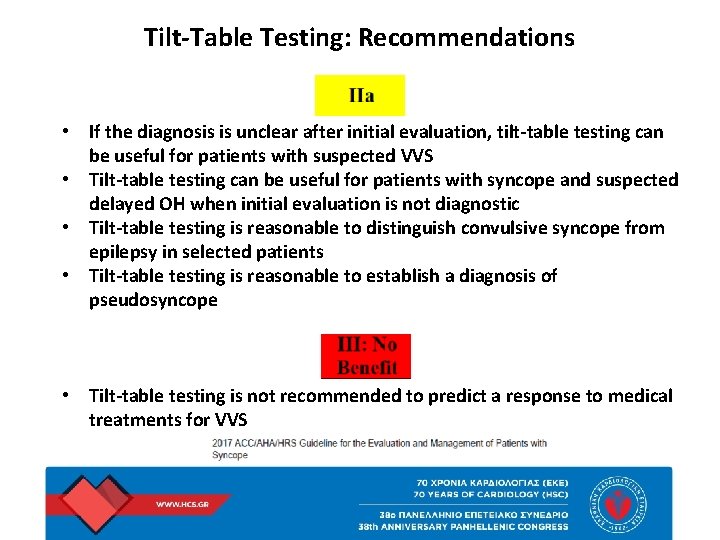
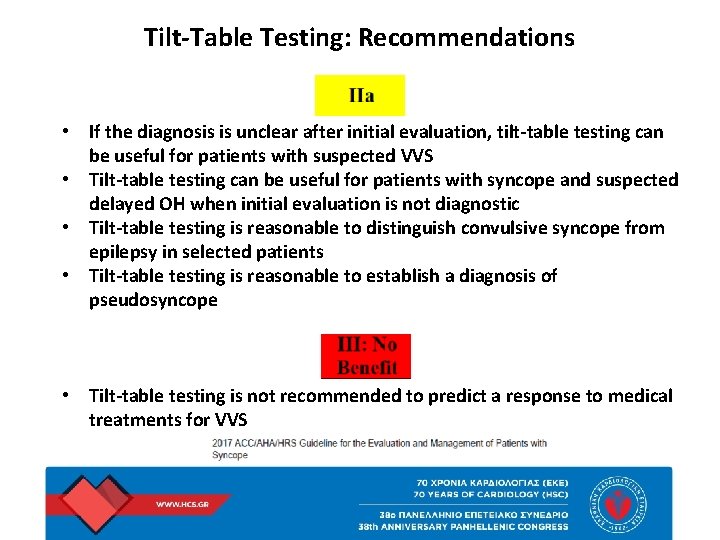
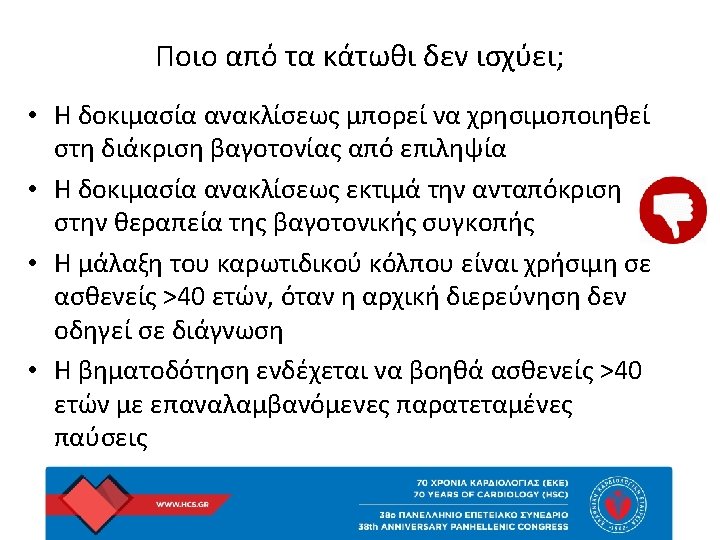
Tilt-Table Testing: Recommendations • If the diagnosis is unclear after initial evaluation, tilt-table testing can be useful for patients with suspected VVS • Tilt-table testing can be useful for patients with syncope and suspected delayed OH when initial evaluation is not diagnostic • Tilt-table testing is reasonable to distinguish convulsive syncope from epilepsy in selected patients • Tilt-table testing is reasonable to establish a diagnosis of pseudosyncope • Tilt-table testing is not recommended to predict a response to medical treatments for VVS
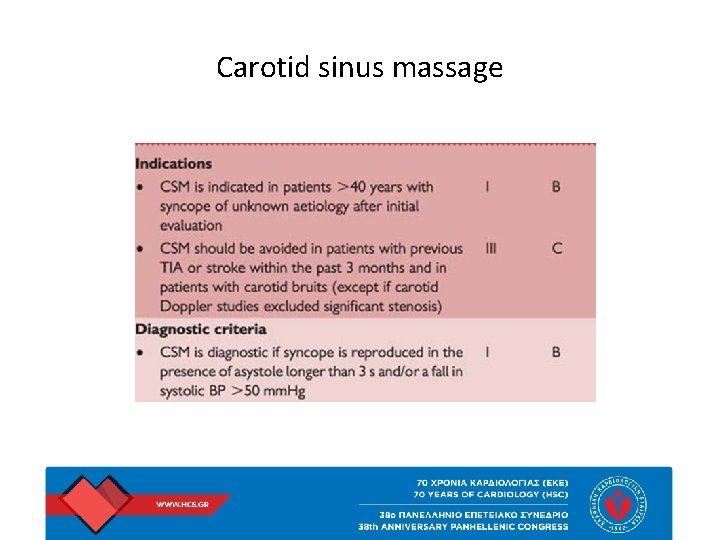
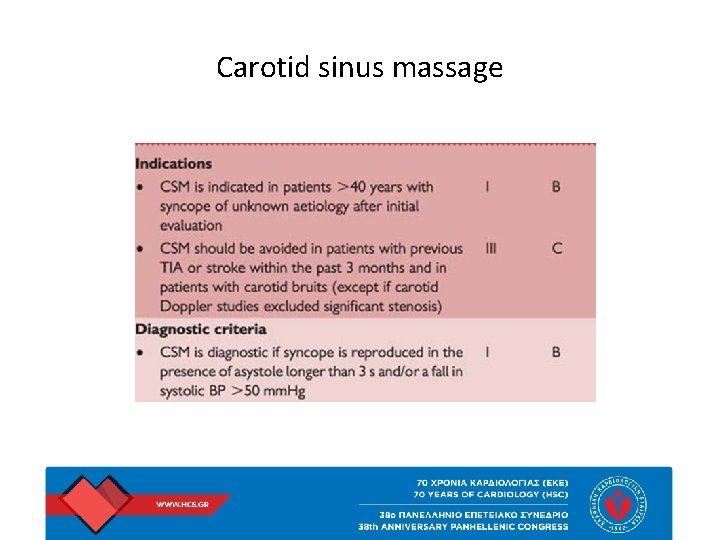
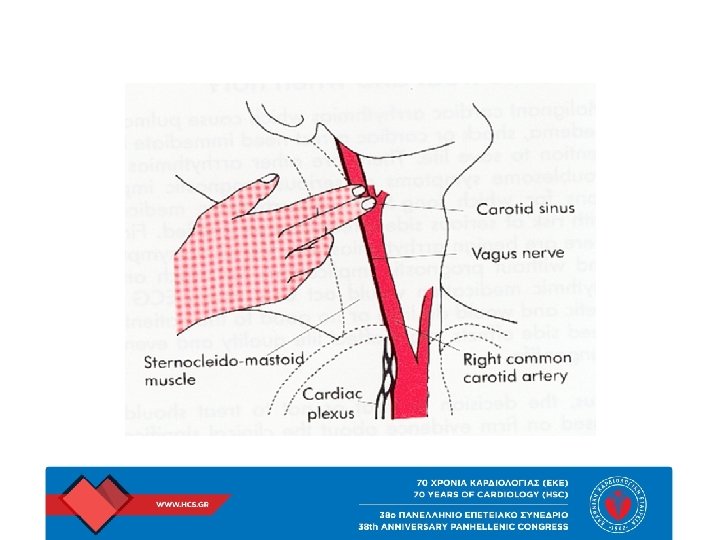
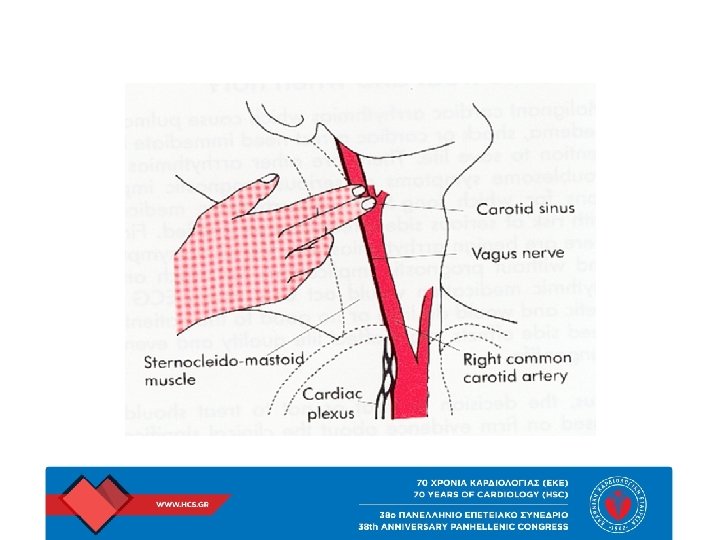
Carotid sinus massage
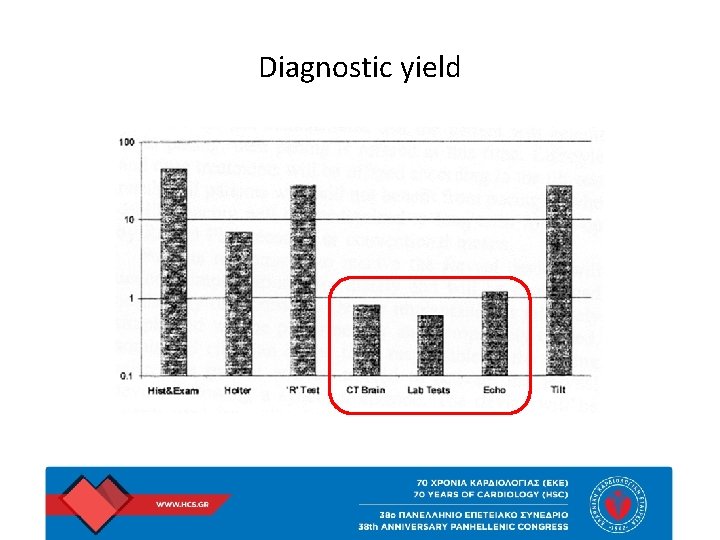
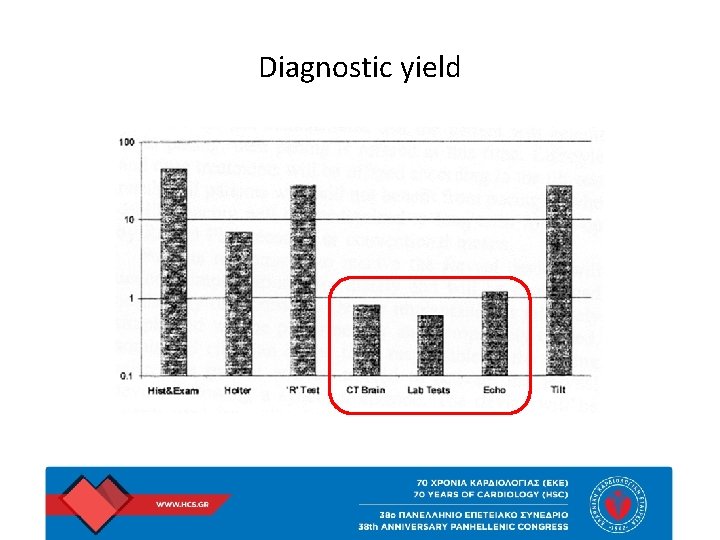
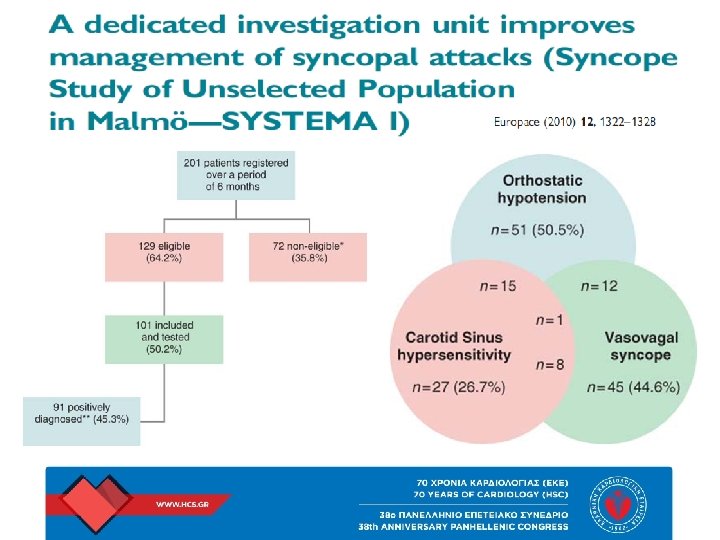
Diagnostic yield
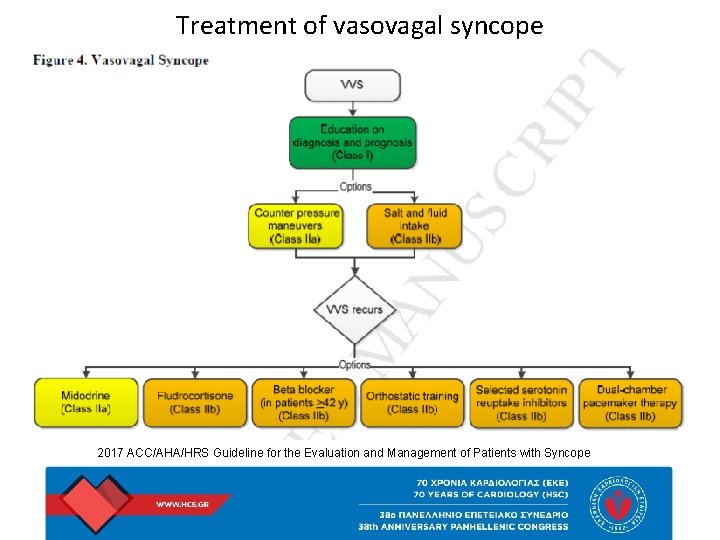
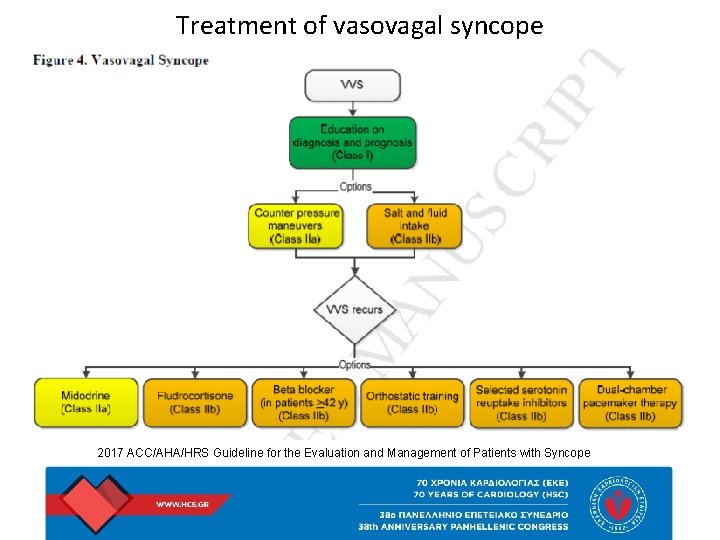
Treatment of vasovagal syncope 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope
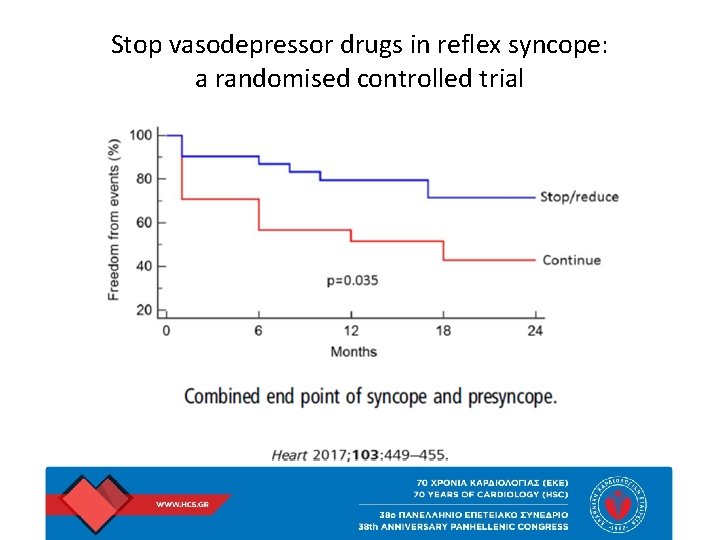
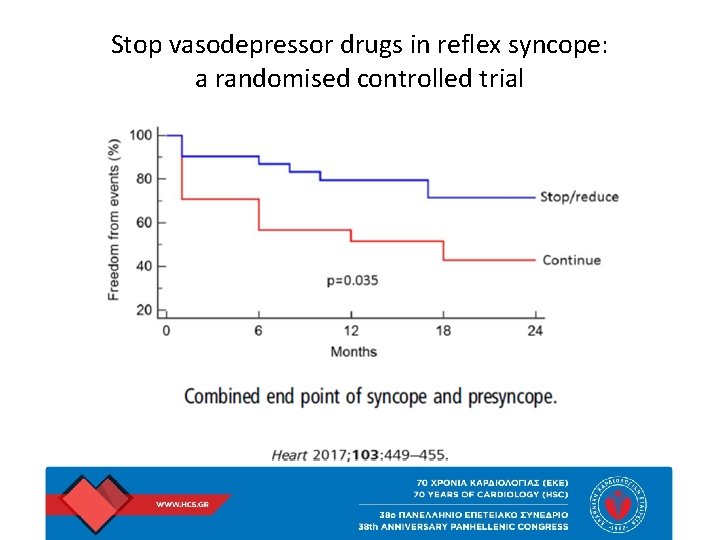
Stop vasodepressor drugs in reflex syncope: a randomised controlled trial
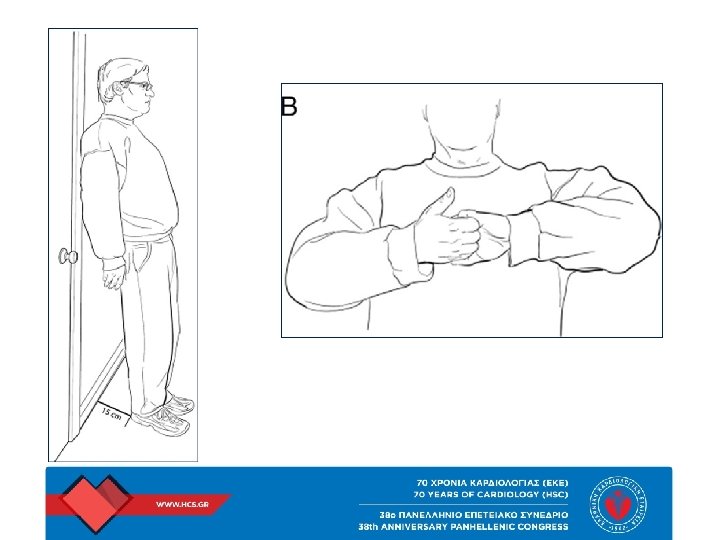
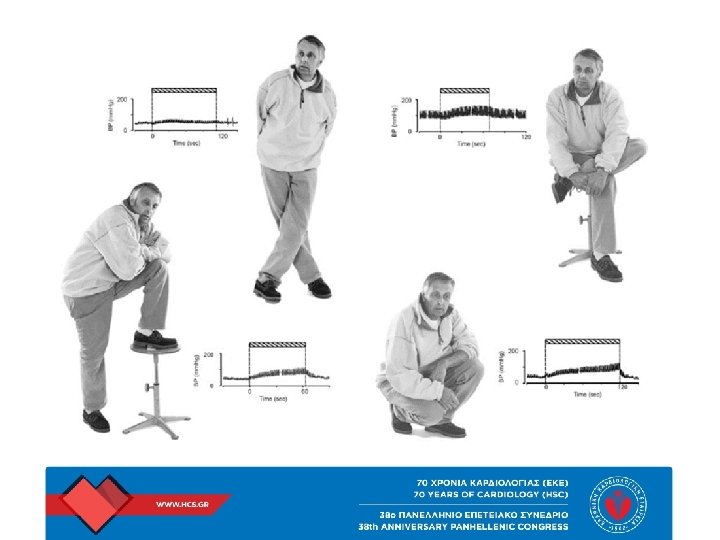
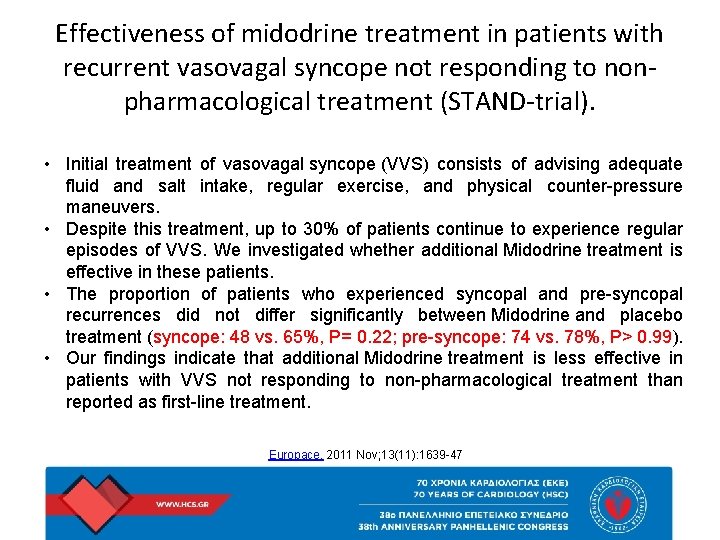
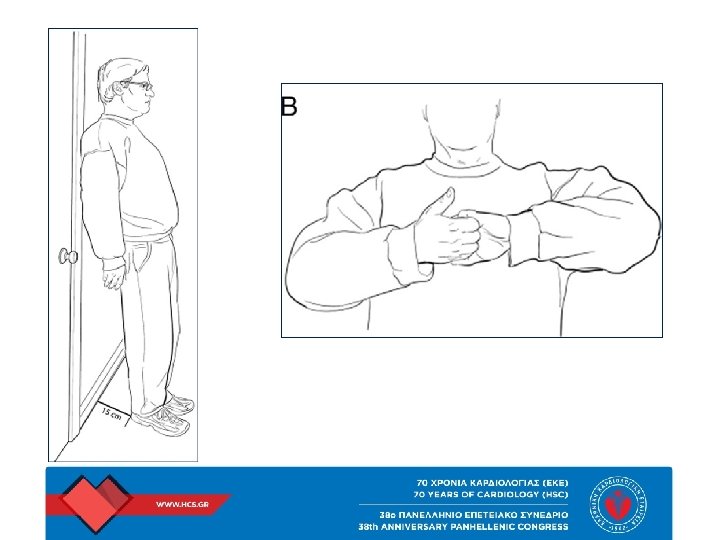
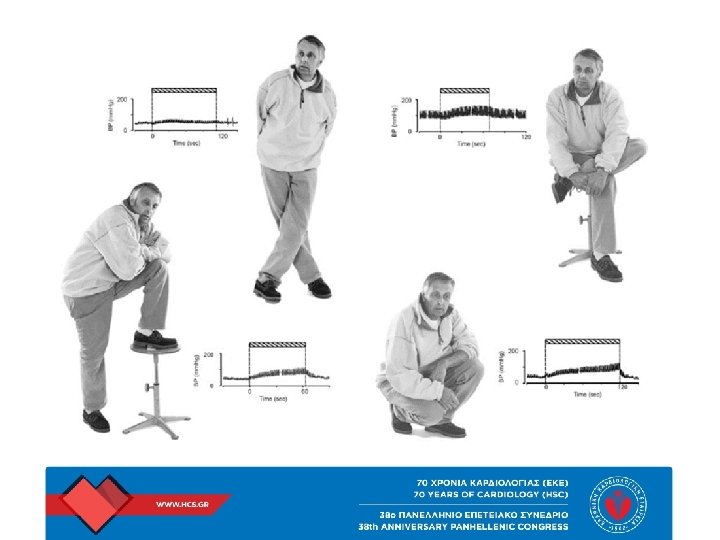
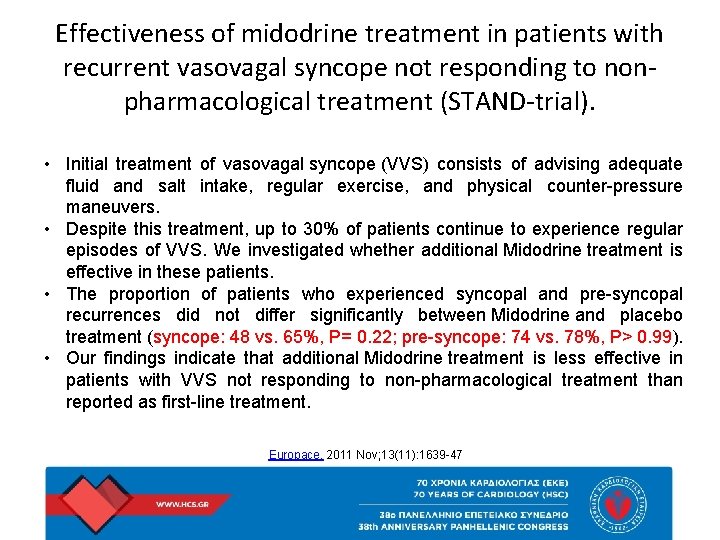
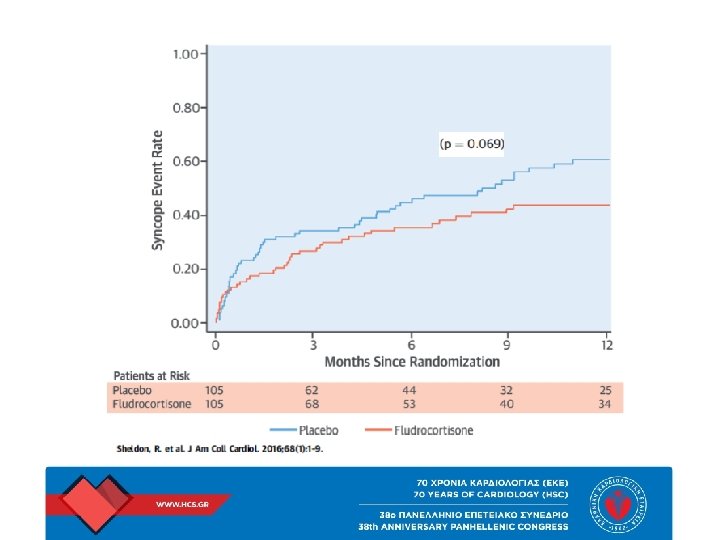
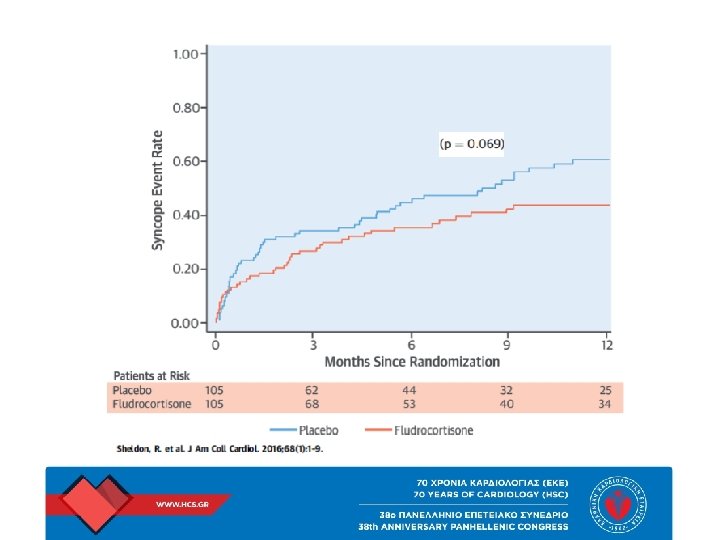
Effectiveness of midodrine treatment in patients with recurrent vasovagal syncope not responding to nonpharmacological treatment (STAND-trial). • Initial treatment of vasovagal syncope (VVS) consists of advising adequate fluid and salt intake, regular exercise, and physical counter-pressure maneuvers. • Despite this treatment, up to 30% of patients continue to experience regular episodes of VVS. We investigated whether additional Midodrine treatment is effective in these patients. • The proportion of patients who experienced syncopal and pre-syncopal recurrences did not differ significantly between Midodrine and placebo treatment (syncope: 48 vs. 65%, P= 0. 22; pre-syncope: 74 vs. 78%, P> 0. 99). • Our findings indicate that additional Midodrine treatment is less effective in patients with VVS not responding to non-pharmacological treatment than reported as first-line treatment. Europace. 2011 Nov; 13(11): 1639 -47
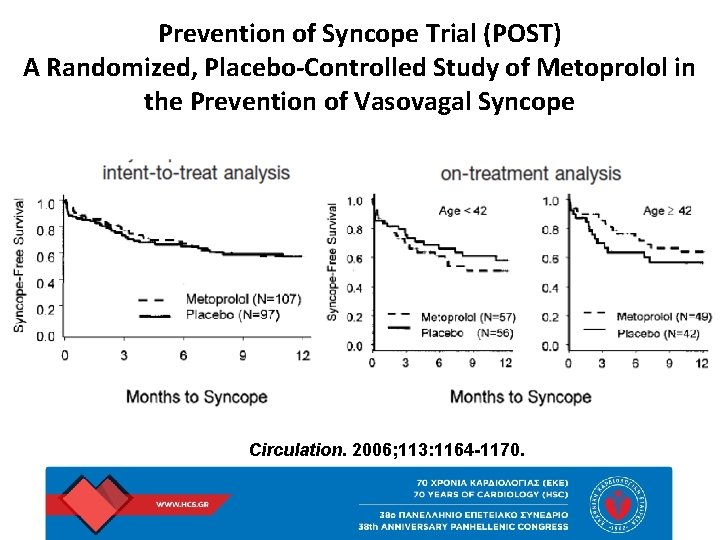
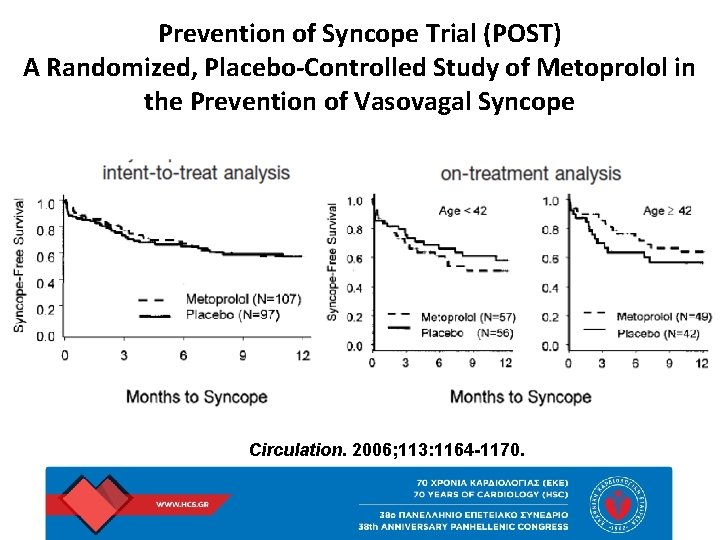
Prevention of Syncope Trial (POST) A Randomized, Placebo-Controlled Study of Metoprolol in the Prevention of Vasovagal Syncope Circulation. 2006; 113: 1164 -1170.
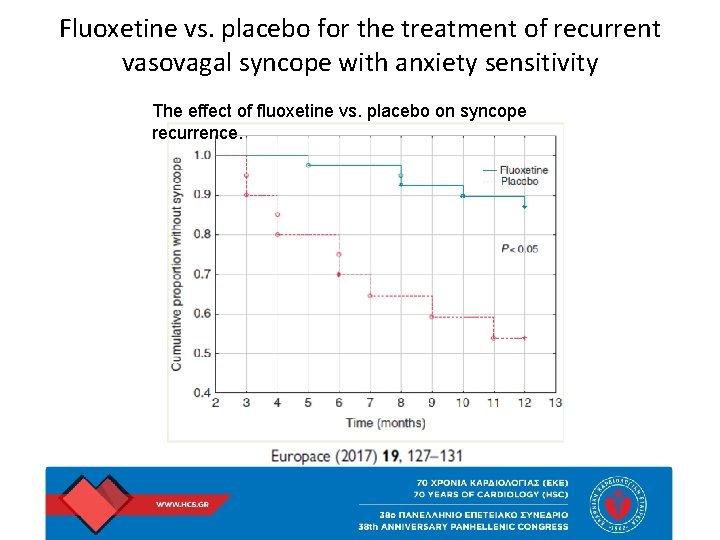
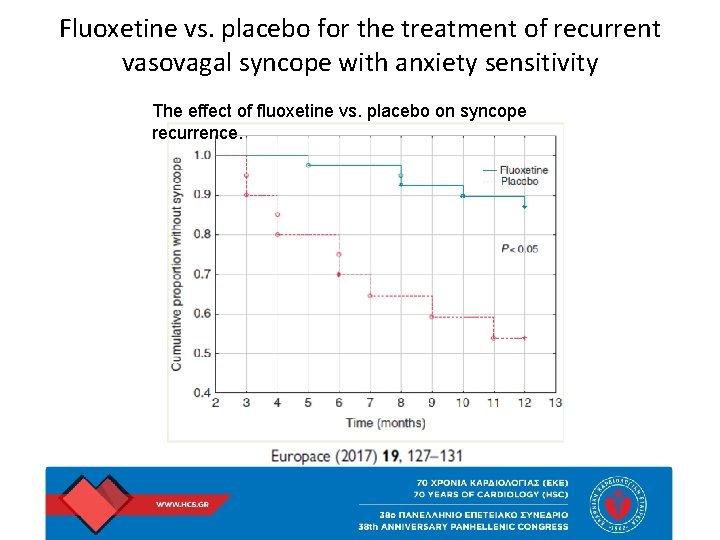
Fluoxetine vs. placebo for the treatment of recurrent vasovagal syncope with anxiety sensitivity The effect of fluoxetine vs. placebo on syncope recurrence.
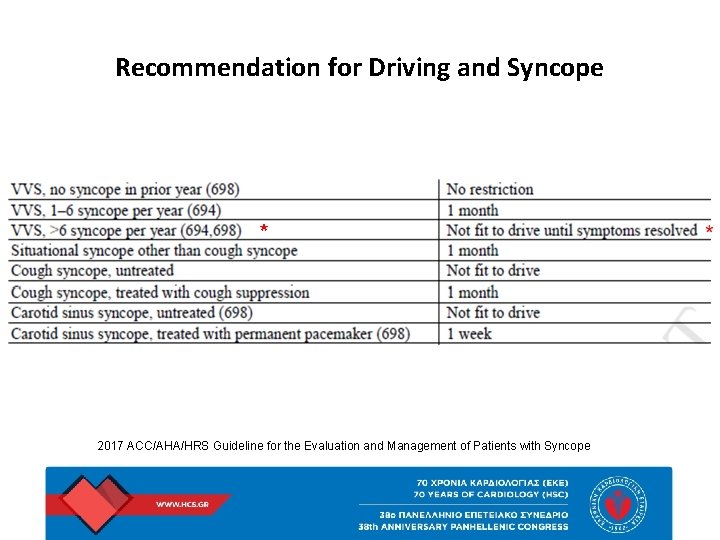
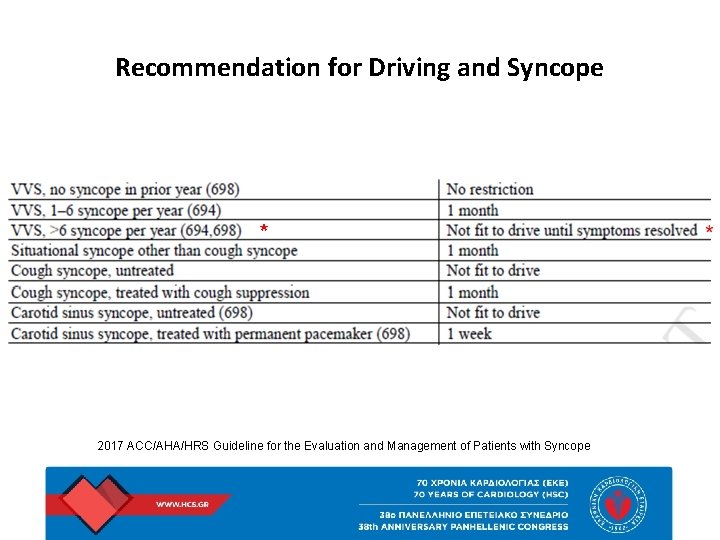
Recommendation for Driving and Syncope * 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope
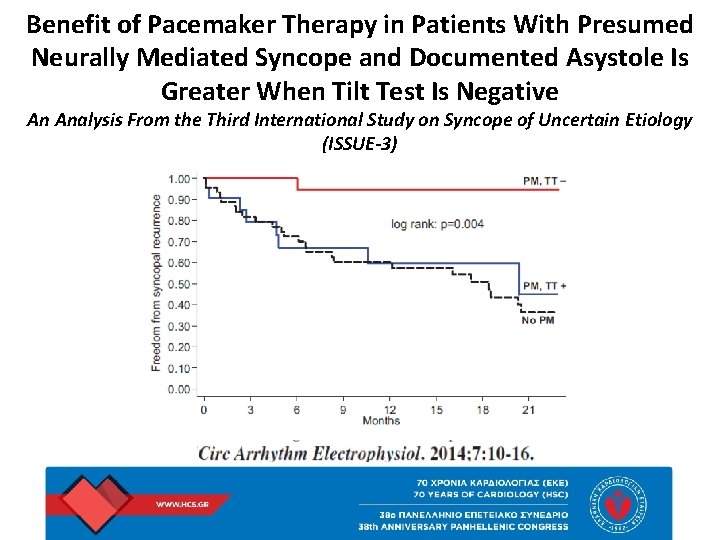
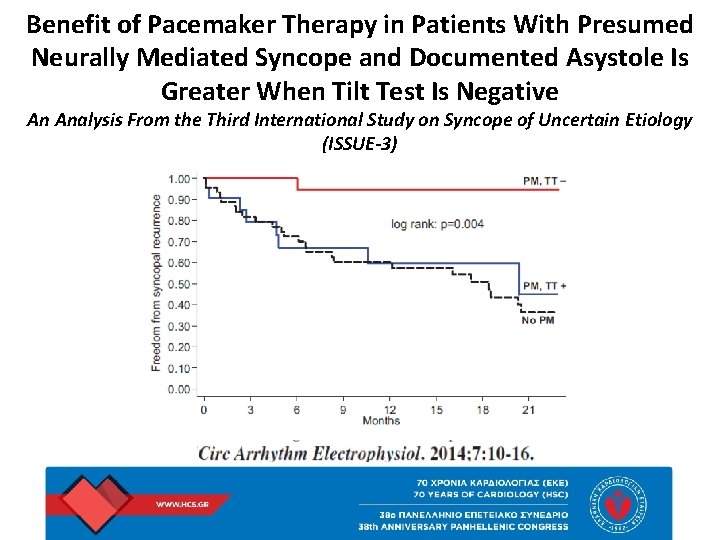
Benefit of Pacemaker Therapy in Patients With Presumed Neurally Mediated Syncope and Documented Asystole Is Greater When Tilt Test Is Negative An Analysis From the Third International Study on Syncope of Uncertain Etiology (ISSUE-3)
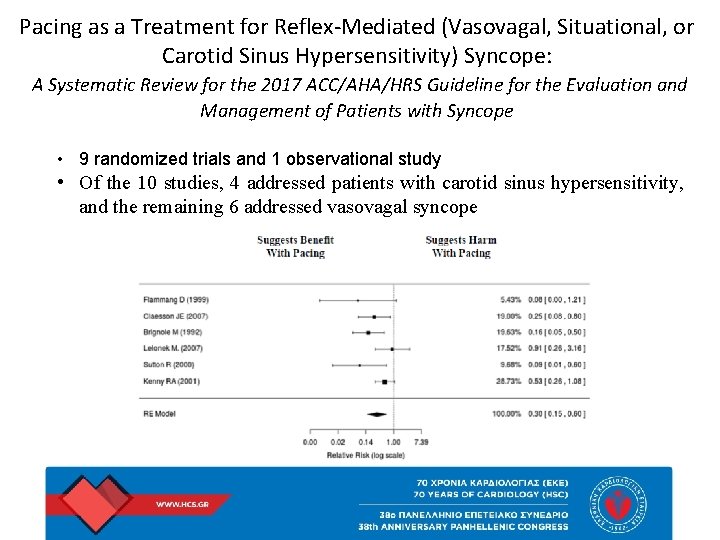
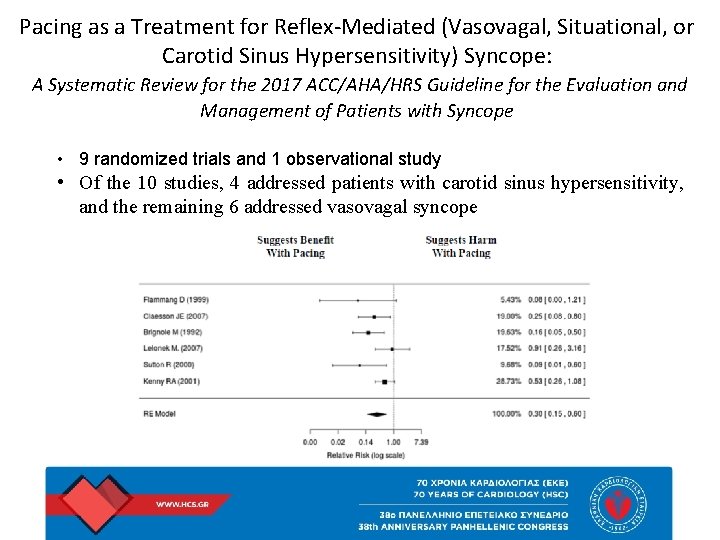
Pacing as a Treatment for Reflex-Mediated (Vasovagal, Situational, or Carotid Sinus Hypersensitivity) Syncope: A Systematic Review for the 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope • 9 randomized trials and 1 observational study • Of the 10 studies, 4 addressed patients with carotid sinus hypersensitivity, and the remaining 6 addressed vasovagal syncope
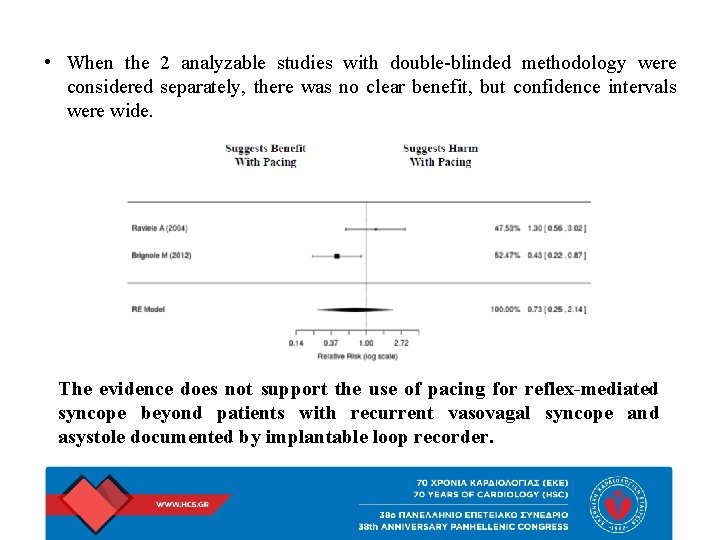
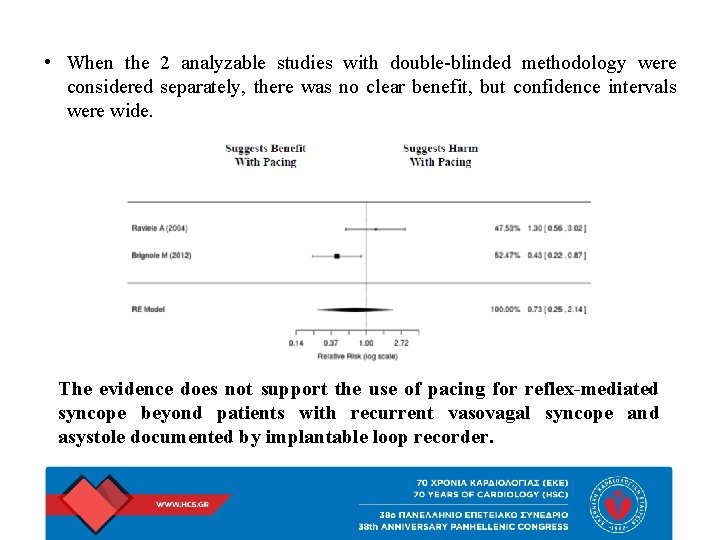
• When the 2 analyzable studies with double-blinded methodology were considered separately, there was no clear benefit, but confidence intervals were wide. The evidence does not support the use of pacing for reflex-mediated syncope beyond patients with recurrent vasovagal syncope and asystole documented by implantable loop recorder.
Vasovagal Syncope To Pace or Not to Pace • It is possible that some ISSUE-3 patients who had severe bradycardia actually had sick sinus syndrome instead of VVS. • Increasing the heart rate early after abrupt heart rate decline (“rate drop response”) has been proposed, but even with the rate-drop response algorithm, therapeutic benefit from pacing may be too late and can be overwhelmed by placebo effects. • The tilt-table test may or may not predict clinical cardioinhibitory responses during VVS. • Monitoring heart rhythm is problematic because asystole may occur after the hemodynamic collapse is already underway.
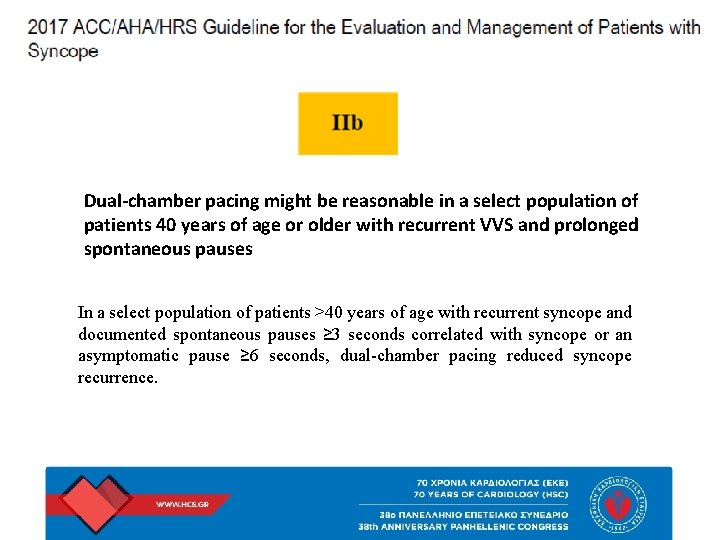
Dual-chamber pacing might be reasonable in a select population of patients 40 years of age or older with recurrent VVS and prolonged spontaneous pauses In a select population of patients >40 years of age with recurrent syncope and documented spontaneous pauses ≥ 3 seconds correlated with syncope or an asymptomatic pause ≥ 6 seconds, dual-chamber pacing reduced syncope recurrence.
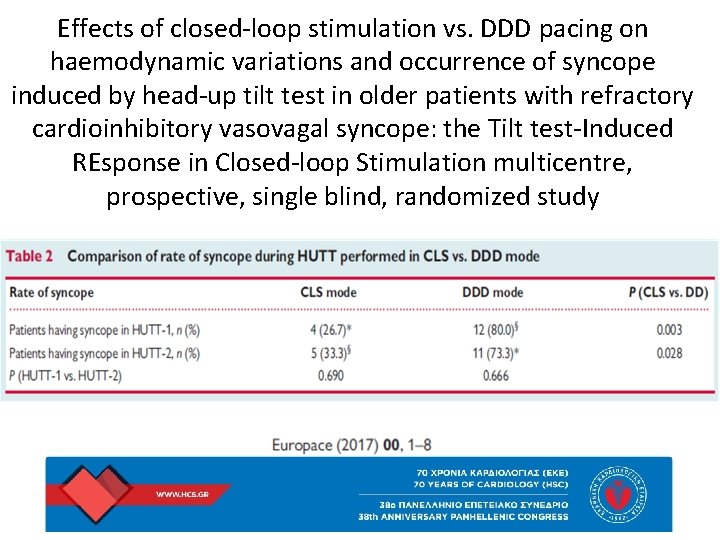
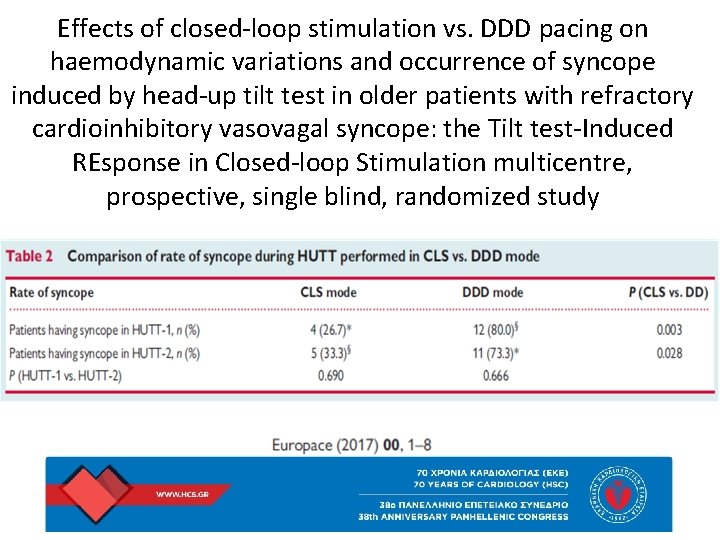
Effects of closed-loop stimulation vs. DDD pacing on haemodynamic variations and occurrence of syncope induced by head-up tilt test in older patients with refractory cardioinhibitory vasovagal syncope: the Tilt test-Induced REsponse in Closed-loop Stimulation multicentre, prospective, single blind, randomized study
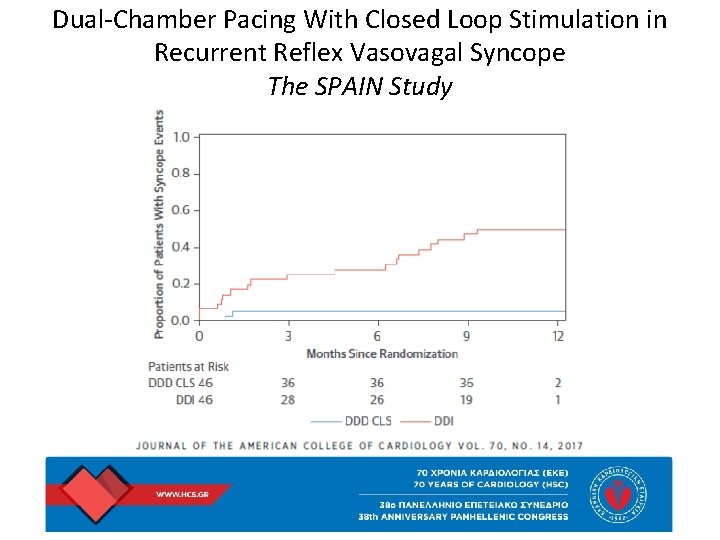
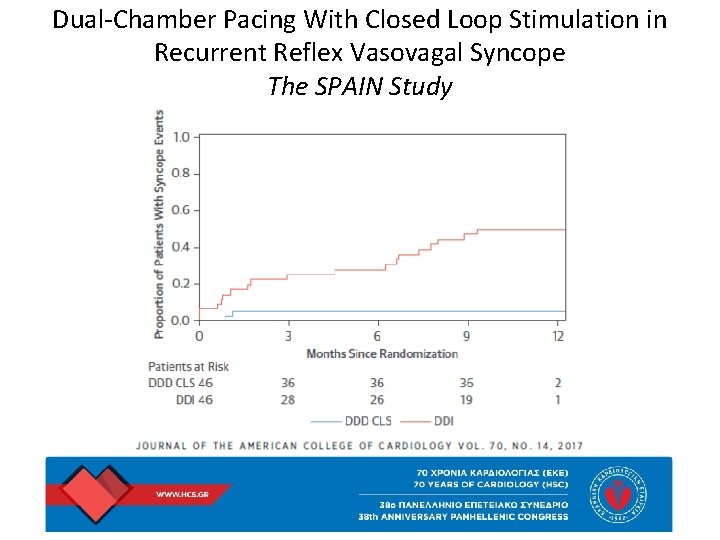
Dual-Chamber Pacing With Closed Loop Stimulation in Recurrent Reflex Vasovagal Syncope The SPAIN Study
Recommendations for Carotid Sinus Syndrome • Permanent cardiac pacing is reasonable in patients with carotid sinus syndrome that is cardioinhibitory or mixed (IIa) • It may be reasonable to implant a dual-chamber pacemaker in patients with carotid sinus syndrome who require permanent pacing (IIb) 2017 ACC/AHA/HRS Guideline for the Evaluation and Management of Patients with Syncope
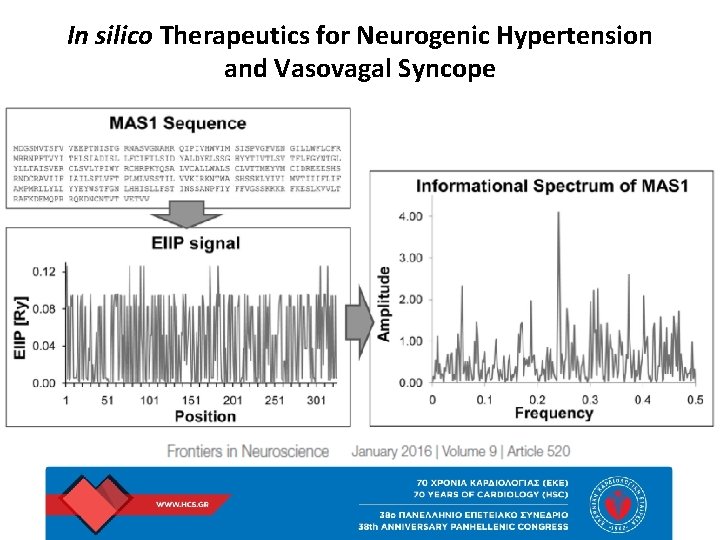
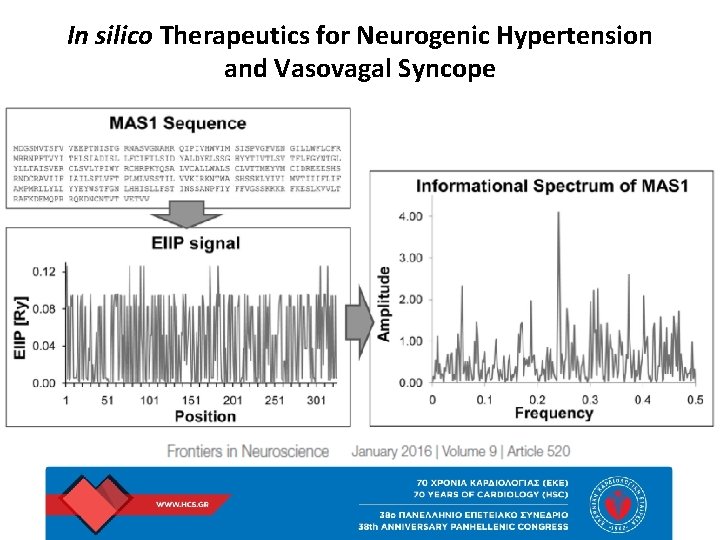
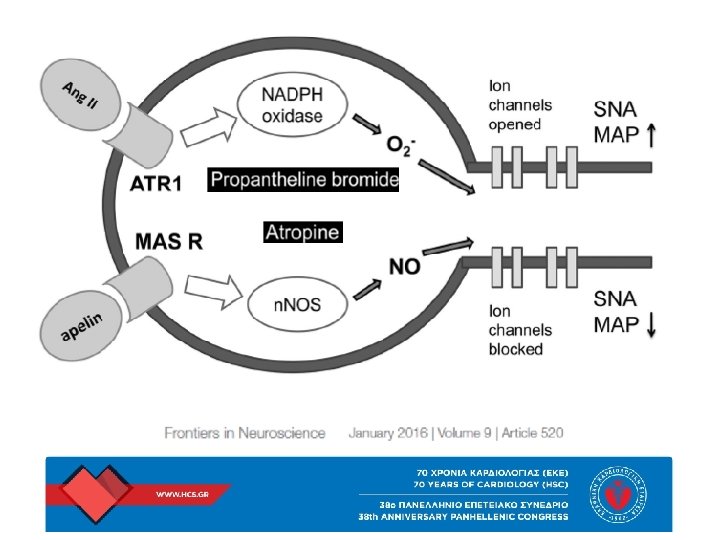
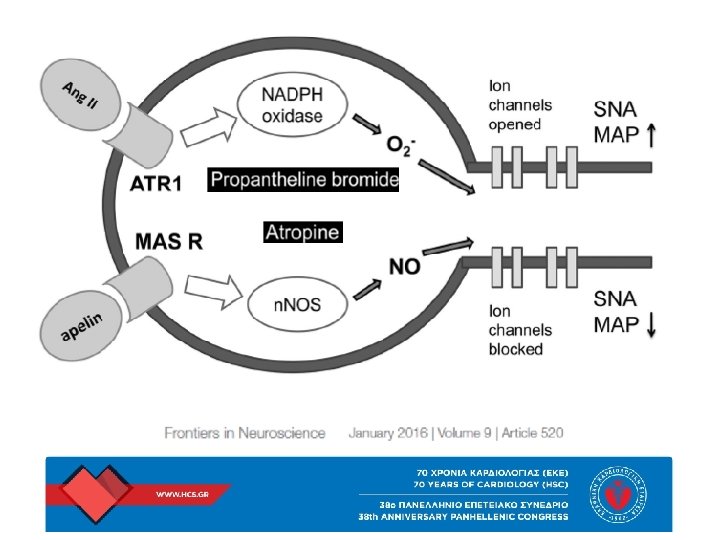
In silico Therapeutics for Neurogenic Hypertension and Vasovagal Syncope
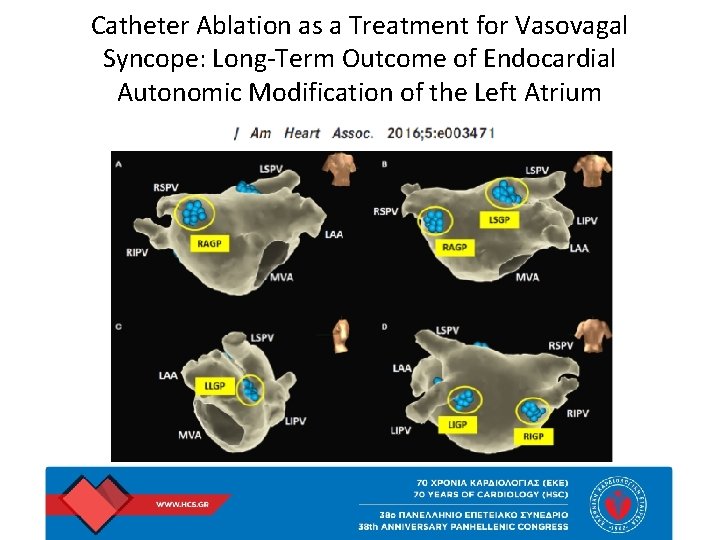
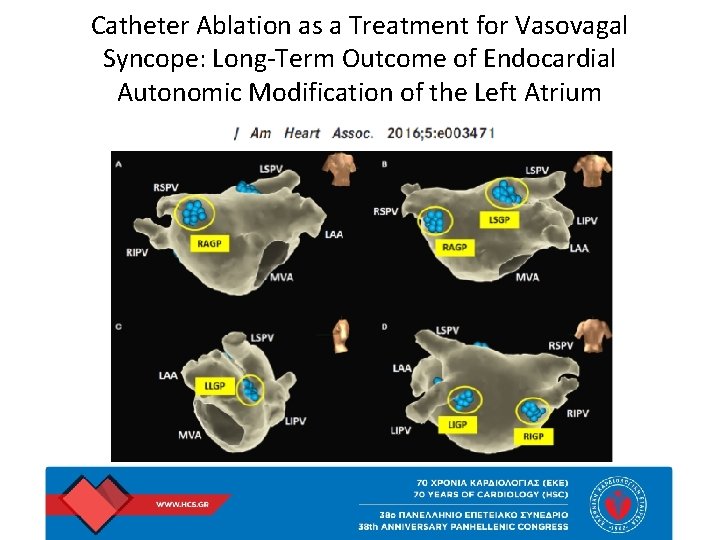
Catheter Ablation as a Treatment for Vasovagal Syncope: Long-Term Outcome of Endocardial Autonomic Modification of the Left Atrium
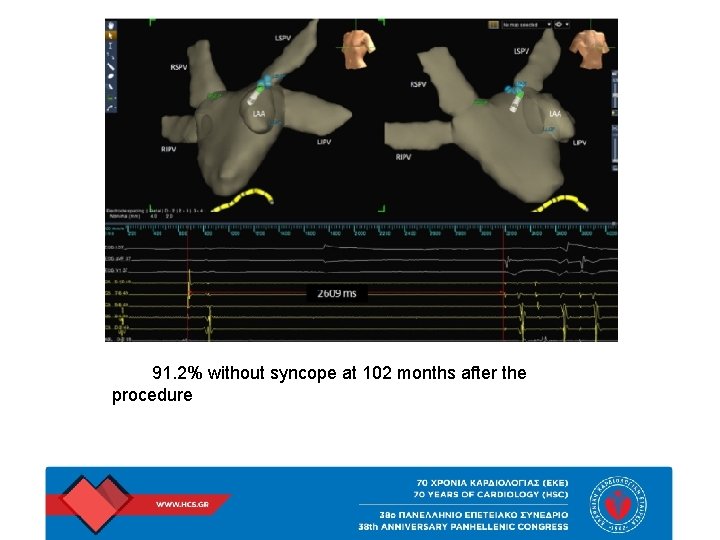
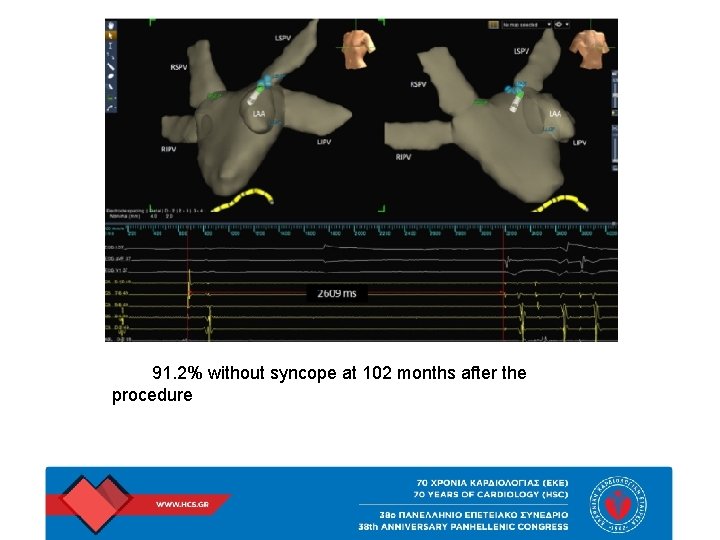
91. 2% without syncope at 102 months after the procedure
Vasovagal Syncope: Hypothesis Focusing on Its Being a Clinical Feature Unique to Humans Although seemingly a disadvantageous evolutionary adaptation, the faint causes the body to take on a gravitationally neutral position, and thereby provides a chance of restoring brain blood supply and preserving brain function.
 Complications of local anesthesia in dentistry
Complications of local anesthesia in dentistry Síncope vasovagal
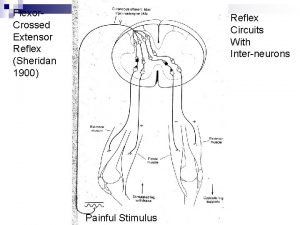
Síncope vasovagal Asymmetrical tonic neck reflex
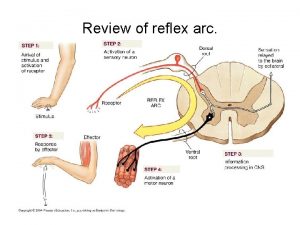
Asymmetrical tonic neck reflex Somatic reflex vs visceral reflex
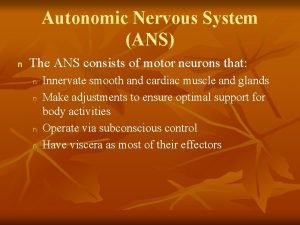
Somatic reflex vs visceral reflex Ans
Ans Migraine vs epilepsy
Migraine vs epilepsy Syncope
Syncope Vertebrobasilaire tia
Vertebrobasilaire tia Syncope
Syncope Syncope in the older patient is
Syncope in the older patient is Vasalvagal syncope
Vasalvagal syncope Syncope
Syncope Keppra loading dose
Keppra loading dose Nursing diagnosis pulmonary embolism
Nursing diagnosis pulmonary embolism Pain pathophysiology
Pain pathophysiology Asthma pathophysiology
Asthma pathophysiology Reactive arthritis pathophysiology
Reactive arthritis pathophysiology Ckd stage คือ
Ckd stage คือ 3392chest
3392chest Uterine bleeding
Uterine bleeding Nursing management of acute pancreatitis
Nursing management of acute pancreatitis Perinephric abscess symptoms
Perinephric abscess symptoms Pathophysiology of asthm
Pathophysiology of asthm Stage of shock
Stage of shock Pathophysiology of aortic aneurysm ppt
Pathophysiology of aortic aneurysm ppt Pathophysiology of valvular heart disease
Pathophysiology of valvular heart disease Chronic calculous cholecystitis
Chronic calculous cholecystitis Pathophysiology of migraine
Pathophysiology of migraine Electrocauterization
Electrocauterization 4l fio2
4l fio2 Joffroy sign pathophysiology
Joffroy sign pathophysiology Pathophysiology emphysema
Pathophysiology emphysema Case mysteries in pathophysiology (doc or html) file
Case mysteries in pathophysiology (doc or html) file Who is this
Who is this Cholecystitis pathophysiology
Cholecystitis pathophysiology Schizophrenia
Schizophrenia Multinodular goiter pathophysiology
Multinodular goiter pathophysiology Hellp syndrome pathophysiology
Hellp syndrome pathophysiology Scarred gallbladder
Scarred gallbladder Tanda ruptur bulbi
Tanda ruptur bulbi