Schizophrenia A severe mental condition in which there
- Slides: 90
Schizophrenia
A severe mental condition in which there is disorganization of the personality, deterioration in social functioning, and loss of contact with, or distortion of, reality. There may be evidence of hallucinations and delusional thinking. Psychosis can occur with or without the presence of organic impairment.
Schizophrenia Spectrum and Other Psychotic Disorders Schizotypal personality disorder Delusional Disorder Brief Psychotic disorder Schizophreinform Disorder Schizophrenia Schizoaffective disorder Substance / medication – induced psychotic disorder Psychotic disorder due to another medical condition Catatonia
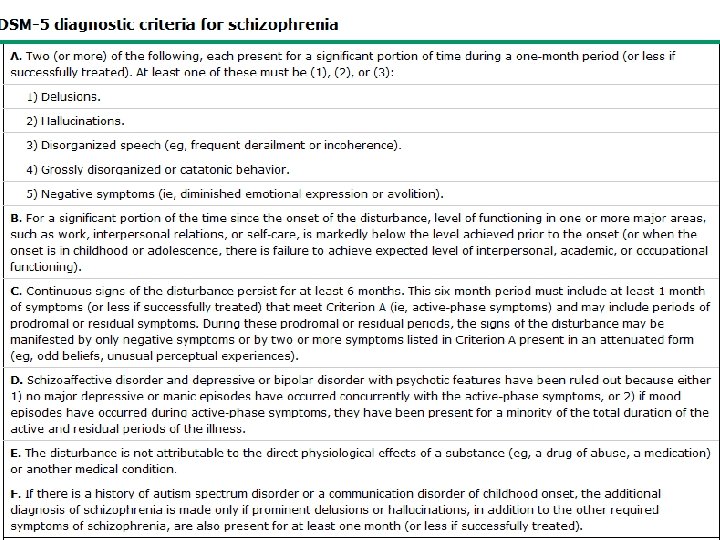
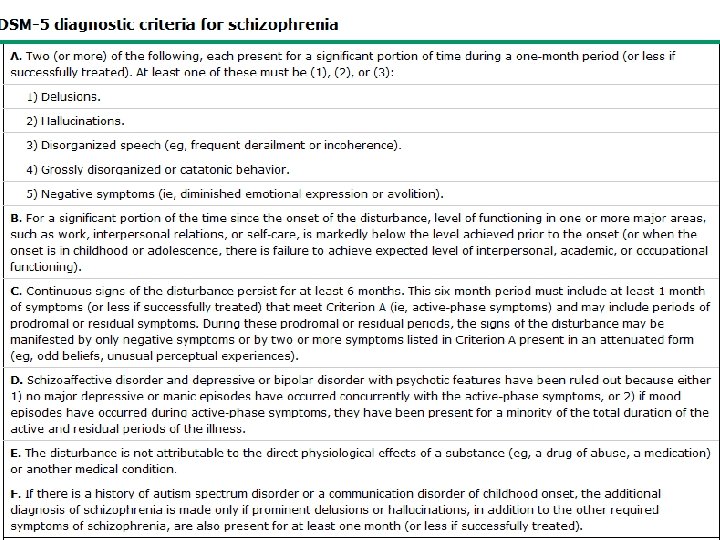
Diagnostic Criteria A. Two or more of the following almost all day most days of the month: at least one of these must be 1, 2, or 3 1. Delusions – Bizarre delusions such as: – Example » A person’s belief that a stranger has removed his or her internal organs and has replaced it with someone else’s organs without leaving any wounds or scars • • • Thought broadcasting Thought insertion Delusion of being controlled Thought withdrawal Paranoid delusions
Delusion Types • Persecutory delusion: the person believes he or she is being tormented, followed, tricked, spied on, or ridiculed. • Referential delusions: the person believes certain gesture, comments, passage from a book, newspapers, songs or other environmental cues are specially directed towards him or her • Thought broadcasting • The person believes that his thoughts are being broadcasted by TV, Radio, or being read by other people
Delusion Types • Thought withdrawal: a person’s belief that his or her thought have been taken away by some outside force (or stolen) • Thought insertion: alien thoughts have been put into his or her mind (thoughts are implanted in their minds from outside source) • Delusion of being controlled: the person’s body or actions are being acted upon or manipulated by some outside force
Delusion Types • Erotomanic: With this type of delusion, the individual believes that someone, usually of a higher status, is in love with him or her. • Grandiose: Individuals with grandiose delusions have irrational ideas regarding their own worth, talent, knowledge, or power. • Somatic: Individuals with somatic delusions believe they have some physical defect, disorder, or disease.
Delusion Types • Jealousy: The content of jealous delusions centers on the idea that the person’s sexual partner is unfaithful. • Nihilistic: The individual has a false idea that the self, a part of the self, others, or the world is nonexistent (e. g. , “The world no longer exists, ” “I have no heart. ”). • Mixed
Diagnostic Criteria 2. Hallucinations: are perception like experiences that occur without an external stimuli. • They are vivid and clear • With full force and impact of normal perceptions, and not under voluntary control • Mostly auditory – Two talking about the patient as a third person, – Voices conversing together – One voice running commentaries on the patient’s thoughts or behaviors
Diagnostic Criteria • Note: Those hallucination that occur while falling asleep (hypnagogic) or waking up (hypnopompic) are considered within normal. Hallucination may be a normal part of religious experience in certain cultural contexts. • Types of Hallucination 1. Auditory: are false perceptions of sound or voices 2. Visual: These are false visual perceptions. 3. Gustatory: are false perceptions of the sense of touch, often of something on or under the skin. 4. Tactile: This type of hallucination is a false perception of taste. 5. Olfactory: are false perceptions of the sense of smell.
Diagnostic Criteria 3. Disorganized Speech: (impaired communication) • loose association or derailment: slips from the track from one topic to another • Answers to questions obliquely related or completely unrelated (Tangentiality, circumstantiality) • Incoherent or ward salad, neologisms
Diagnostic Criteria 4. Odd behaviors (disorganized behavior) – Child like silliness to unpredictable agitation – May be noted in any form of goal-directed behaviors, leading to difficulties in performing ADL, such as maintaining hygiene, the person may dress in an unusual manner (wearing multiple overcoats, scarves, and gloves in a hot day) – Inappropriate sexual behavior (masturbation in public) – Unpredictable and un-triggered agitation (shouting and swearing) – Strange grimaces, sniffing, blowing out cheeks, wrinkling the forehead, or ritualistic activities– – Mannerism or catatonic--stupor, negativism, rigidity, excitement, waxy flexibility, or posturing – – Immobility, adopting odd postures for long periods of time.
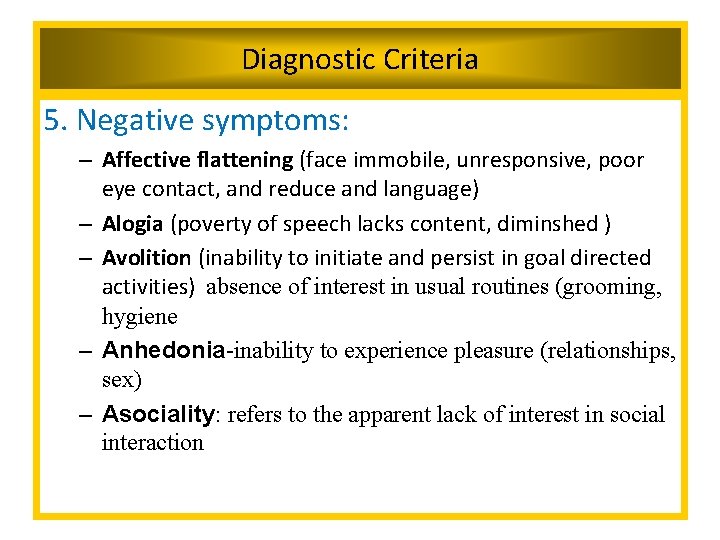
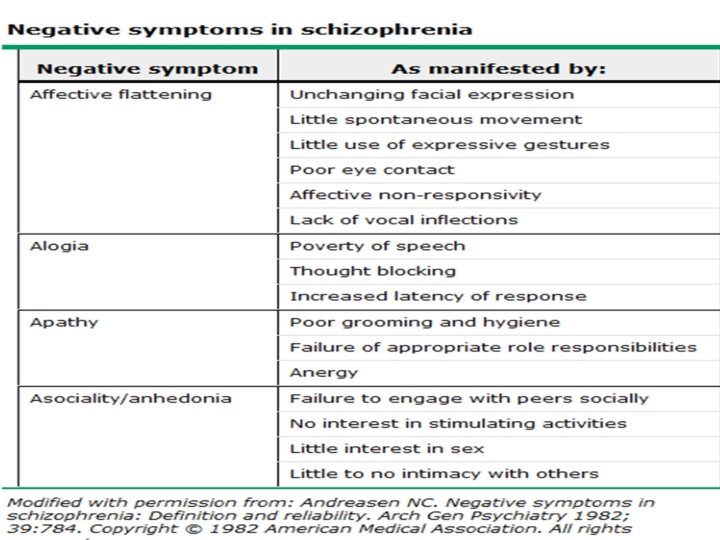
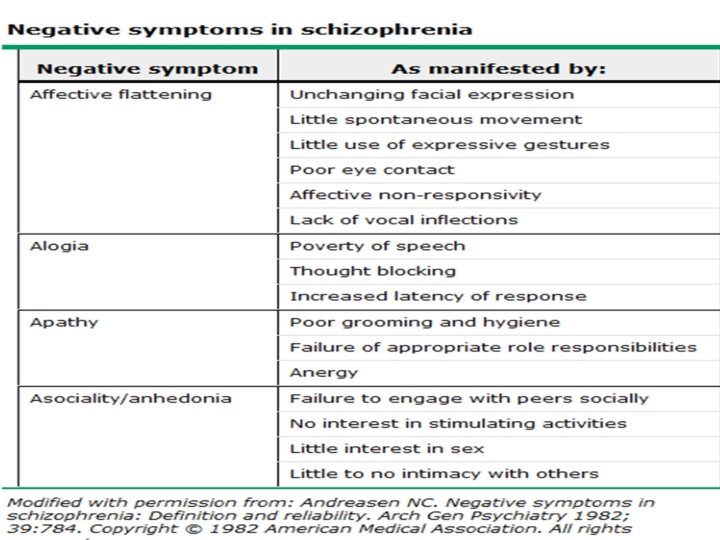
Diagnostic Criteria 5. Negative symptoms: – Affective flattening (face immobile, unresponsive, poor eye contact, and reduce and language) – Alogia (poverty of speech lacks content, diminshed ) – Avolition (inability to initiate and persist in goal directed activities) absence of interest in usual routines (grooming, hygiene – Anhedonia-inability to experience pleasure (relationships, sex) – Asociality: refers to the apparent lack of interest in social interaction
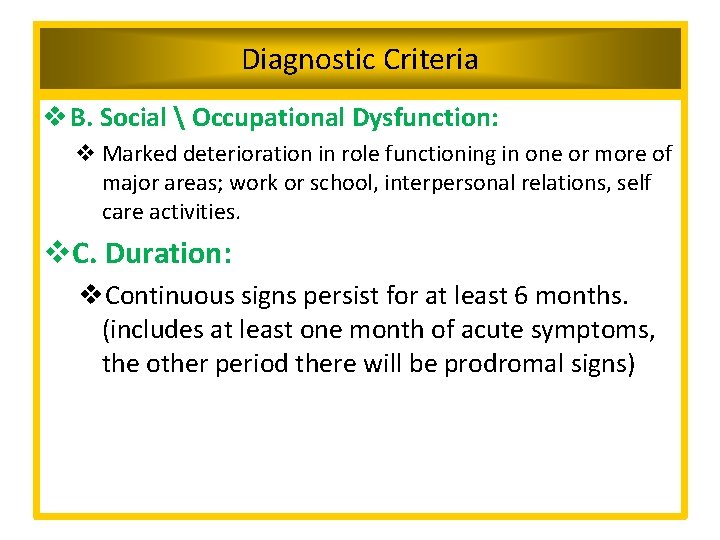
Diagnostic Criteria v B. Social Occupational Dysfunction: v Marked deterioration in role functioning in one or more of major areas; work or school, interpersonal relations, self care activities. v. C. Duration: v. Continuous signs persist for at least 6 months. (includes at least one month of acute symptoms, the other period there will be prodromal signs)
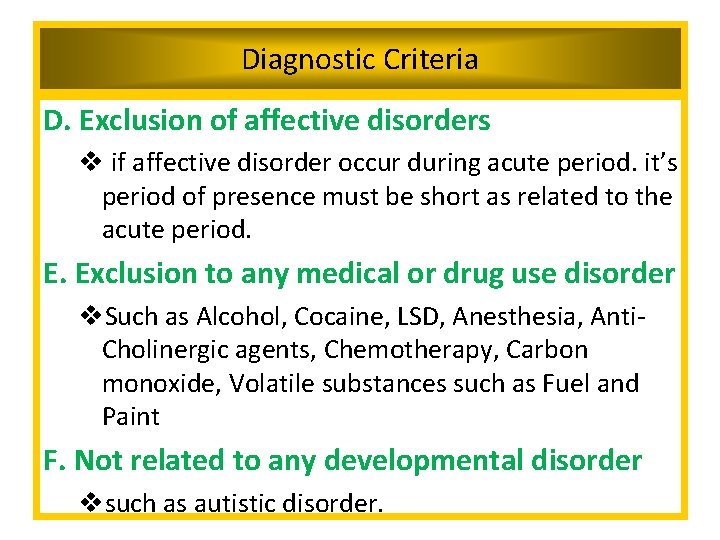
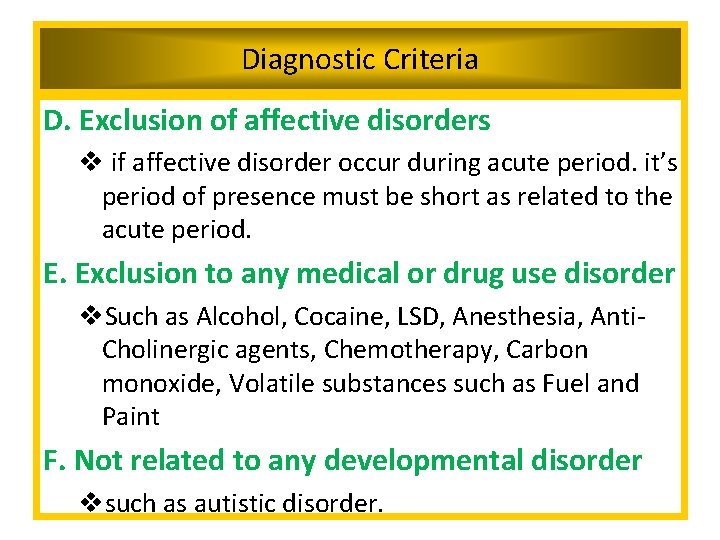
Diagnostic Criteria D. Exclusion of affective disorders v if affective disorder occur during acute period. it’s period of presence must be short as related to the acute period. E. Exclusion to any medical or drug use disorder v. Such as Alcohol, Cocaine, LSD, Anesthesia, Anti. Cholinergic agents, Chemotherapy, Carbon monoxide, Volatile substances such as Fuel and Paint F. Not related to any developmental disorder vsuch as autistic disorder.
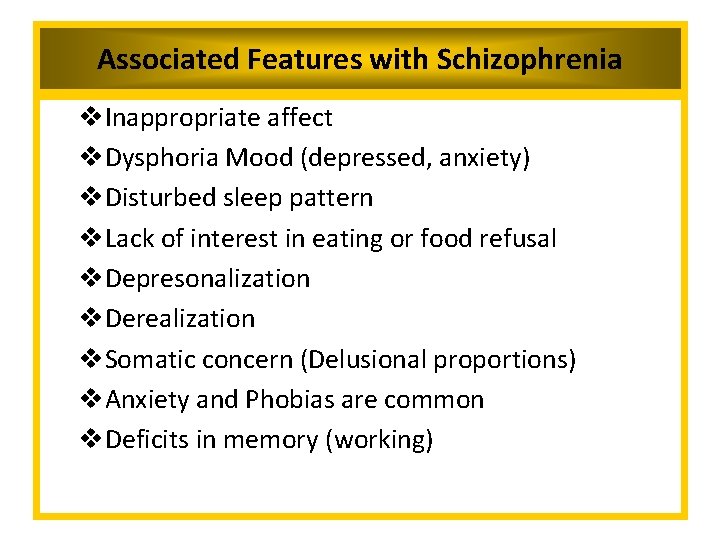
Associated Features with Schizophrenia v. Inappropriate affect v. Dysphoria Mood (depressed, anxiety) v. Disturbed sleep pattern v. Lack of interest in eating or food refusal v. Depresonalization v. Derealization v. Somatic concern (Delusional proportions) v. Anxiety and Phobias are common v. Deficits in memory (working)
Associated Features with Schizophrenia v. Deficits in language functions v. Abnormalities in sensory processing and inhibitory capacity v. Reduction in attention v. Social cognition deficits (inability to infer the intentions of other people) v. Lack of insight v. Hostility and aggression
Functional Consequences of Schizophrenia v. Schizophrenia is associated with significant social or occupational dysfunction. v. Individuals with schizophrenia have impaired educational progress and are unable to maintain employment (due Avolition or other symptoms) v. Most individuals are employed at a lower level than their parents. v. Most of them don’t marry or have limited contacts outside of their family.
CATATONIA • The clinical picture is dominated by three or more of the following symptoms: • One or two of the following symptoms are present for at least two weeks: – Stupor: (marked decrease in reactivity to the environment the person might seem as in coma but still aware about the environment). – Excitement (purposeless motor activity, not influenced by external environment). – Posturing (voluntary assumption and maintenance of inappropriate or bizarre positions) 21
CATATONIA – Negativism: (motiveless resistance to any attempt to move the patient) – Mannerism: (odd movement, goal directed ) – Stereotypy: (repetitive, abnormal frequent- not goal directed) – Agitation: not influenced by external stimuli – Echolalia: mimicking another speech – Echopraxia: mimicking another movement • Tends to be severe and quite rare 22
CATATONIA – Posturing: (spontaneous and active maintenance of a posture against gravity) – Rigidity: (maintenance of rigid posture against efforts to be moved) – Waxy flexibility: Slight resistance to positioning by examiner – Catalepsy: (Passive induction of a posture held against gravity – Mutism: (No or very little verbal response exclude aphasia. 23
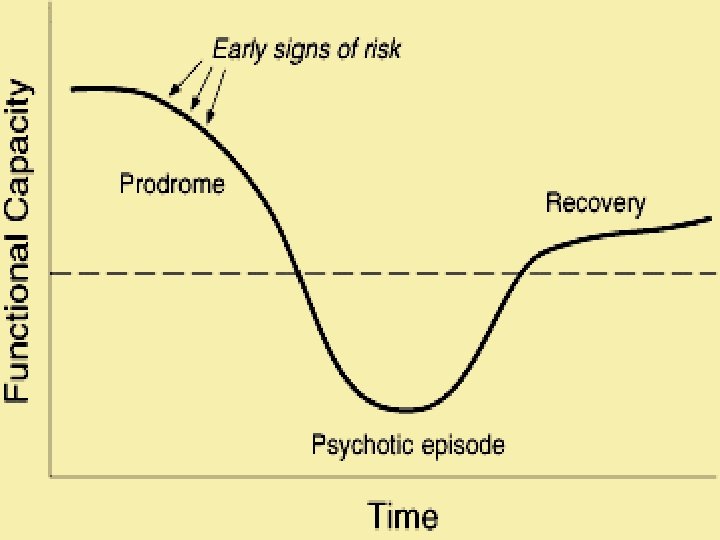
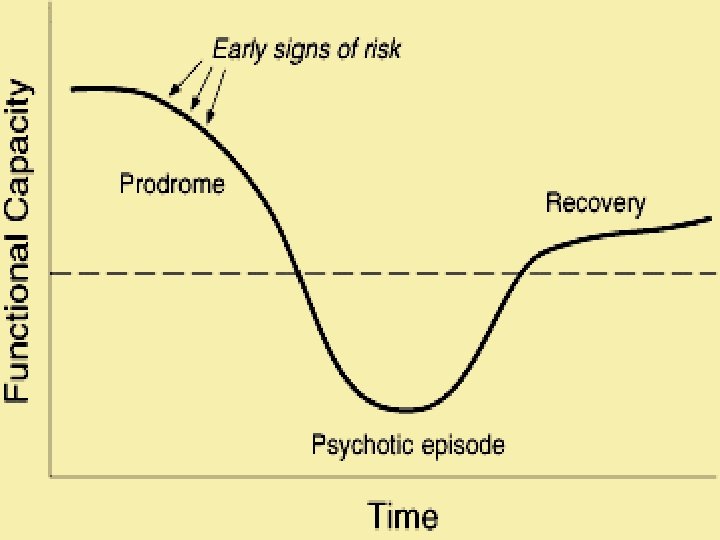
Schizophrenia: Phases • Phase I: Schizoid personality – Emotional coldness (limited range of emotional expression), Do not enjoy relationships, prefers solitary activities – Not all client who develop schizophrenia has schizoid personality • Phase II: The prodromal phase – Social withdrawal, neglect of hygiene & grooming, blunted or inappropriate affect, bizarre ideas, lack of initiatives, interest or energy. – May last for many years (gradual onset)
Schizophrenia: Phases • Phase III: Schizophrenia – Acute episode of signs & symptoms • Phase IV: Residual phase – Periods of remission & exacerbation – Similar to prodromal phase
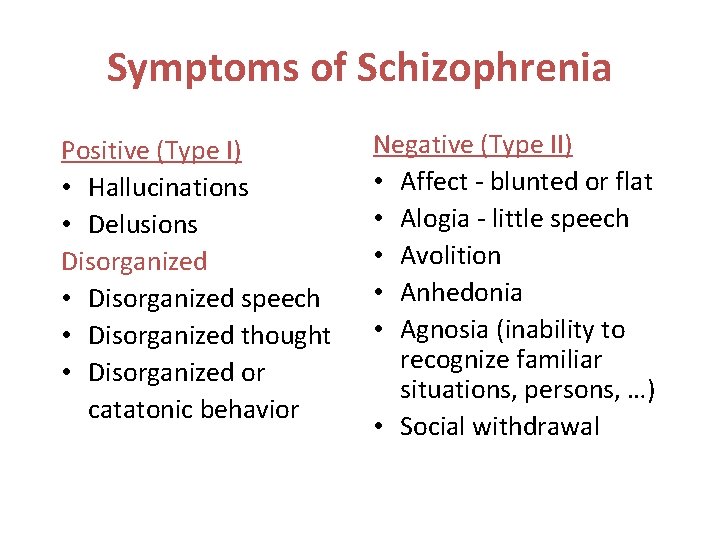
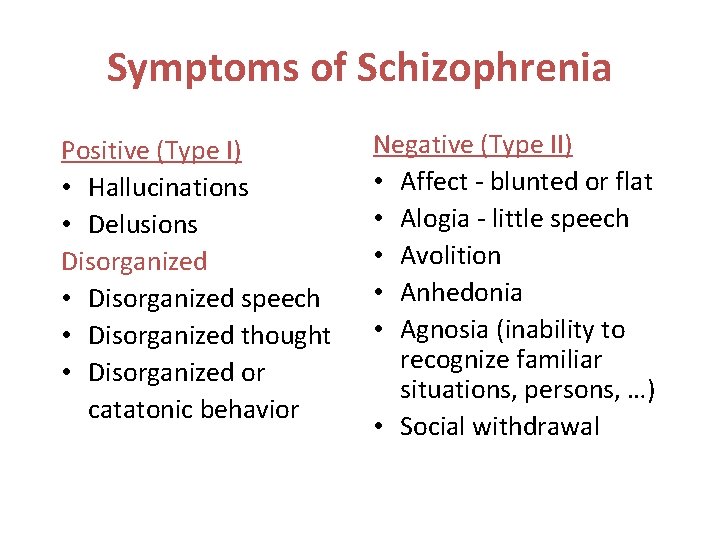
Symptoms of Schizophrenia Positive (Type I) • Hallucinations • Delusions Disorganized • Disorganized speech • Disorganized thought • Disorganized or catatonic behavior Negative (Type II) • Affect - blunted or flat • Alogia - little speech • Avolition • Anhedonia • Agnosia (inability to recognize familiar situations, persons, …) • Social withdrawal
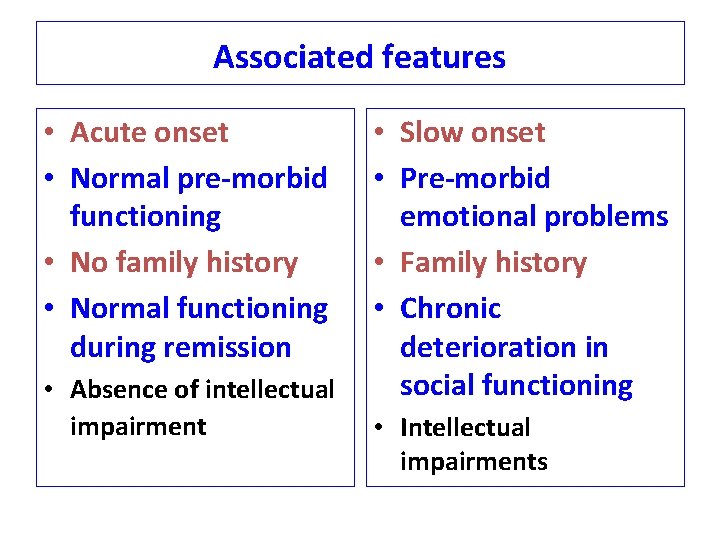
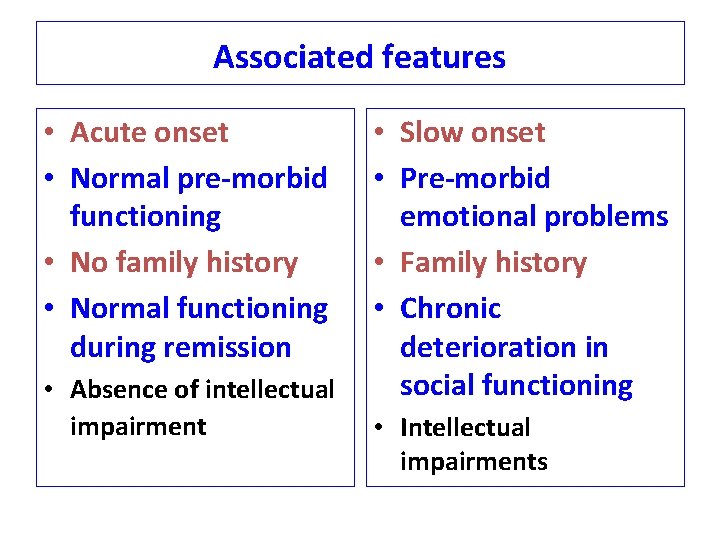
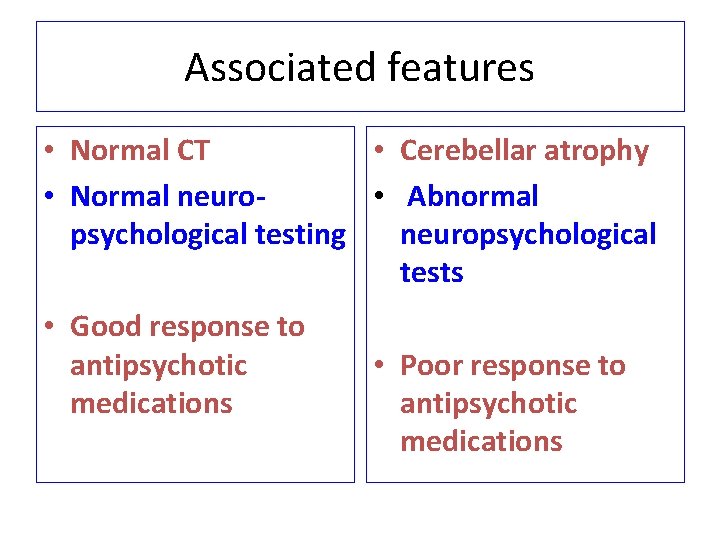
Associated features • Acute onset • Normal pre-morbid functioning • No family history • Normal functioning during remission • Absence of intellectual impairment • Slow onset • Pre-morbid emotional problems • Family history • Chronic deterioration in social functioning • Intellectual impairments
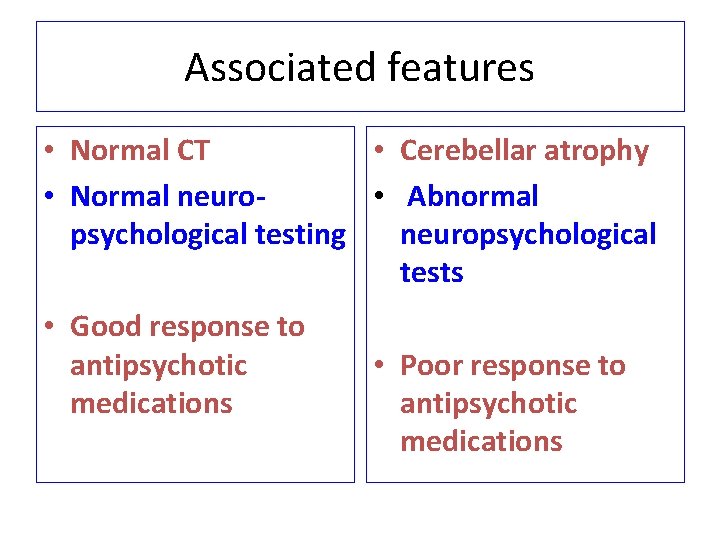
Associated features • Normal CT • Cerebellar atrophy • Normal neuro • Abnormal psychological testing neuropsychological tests • Good response to antipsychotic medications • Poor response to antipsychotic medications
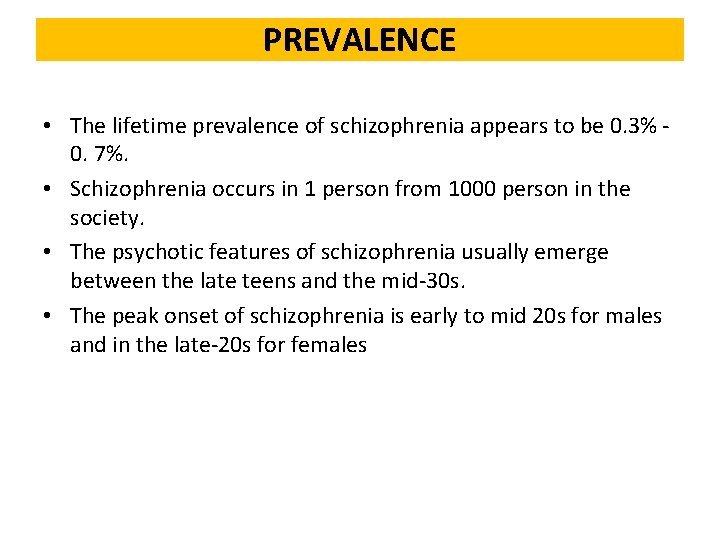
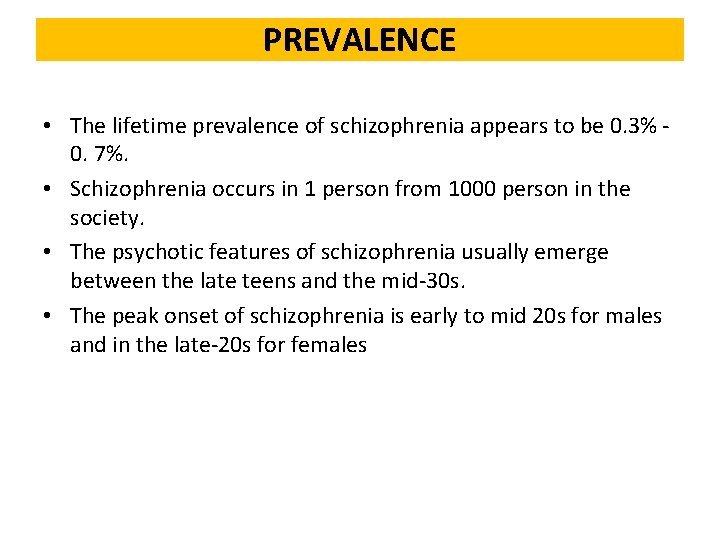
PREVALENCE • The lifetime prevalence of schizophrenia appears to be 0. 3% 0. 7%. • Schizophrenia occurs in 1 person from 1000 person in the society. • The psychotic features of schizophrenia usually emerge between the late teens and the mid-30 s. • The peak onset of schizophrenia is early to mid 20 s for males and in the late-20 s for females
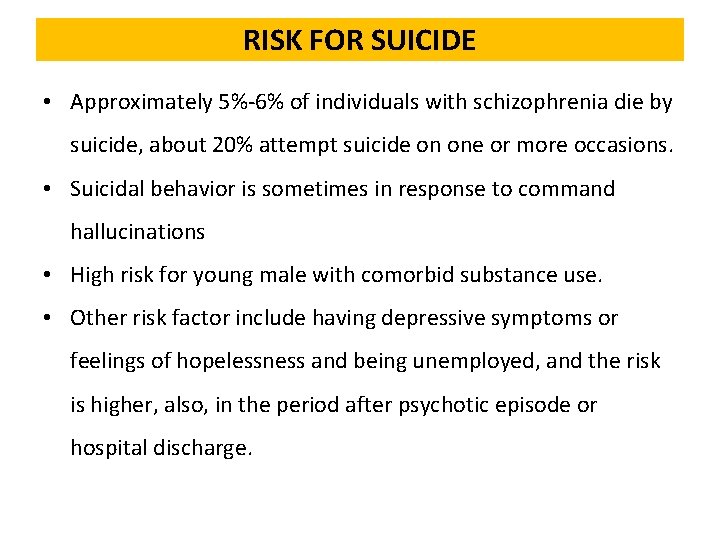
RISK FOR SUICIDE • Approximately 5%-6% of individuals with schizophrenia die by suicide, about 20% attempt suicide on one or more occasions. • Suicidal behavior is sometimes in response to command hallucinations • High risk for young male with comorbid substance use. • Other risk factor include having depressive symptoms or feelings of hopelessness and being unemployed, and the risk is higher, also, in the period after psychotic episode or hospital discharge.
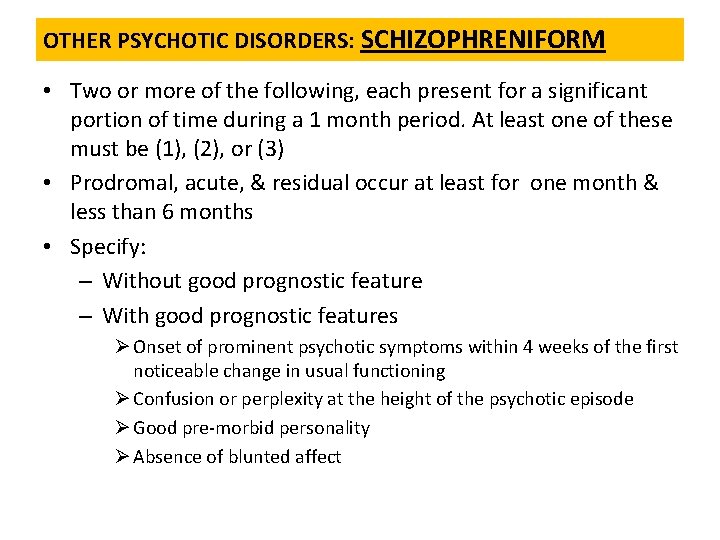
OTHER PSYCHOTIC DISORDERS: SCHIZOPHRENIFORM • Two or more of the following, each present for a significant portion of time during a 1 month period. At least one of these must be (1), (2), or (3) • Prodromal, acute, & residual occur at least for one month & less than 6 months • Specify: – Without good prognostic feature – With good prognostic features Ø Onset of prominent psychotic symptoms within 4 weeks of the first noticeable change in usual functioning Ø Confusion or perplexity at the height of the psychotic episode Ø Good pre-morbid personality Ø Absence of blunted affect
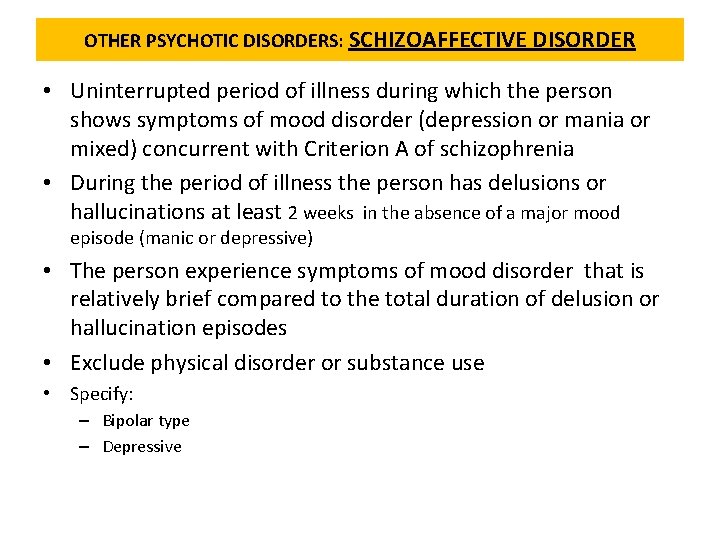
OTHER PSYCHOTIC DISORDERS: SCHIZOAFFECTIVE DISORDER • Uninterrupted period of illness during which the person shows symptoms of mood disorder (depression or mania or mixed) concurrent with Criterion A of schizophrenia • During the period of illness the person has delusions or hallucinations at least 2 weeks in the absence of a major mood episode (manic or depressive) • The person experience symptoms of mood disorder that is relatively brief compared to the total duration of delusion or hallucination episodes • Exclude physical disorder or substance use • Specify: – Bipolar type – Depressive
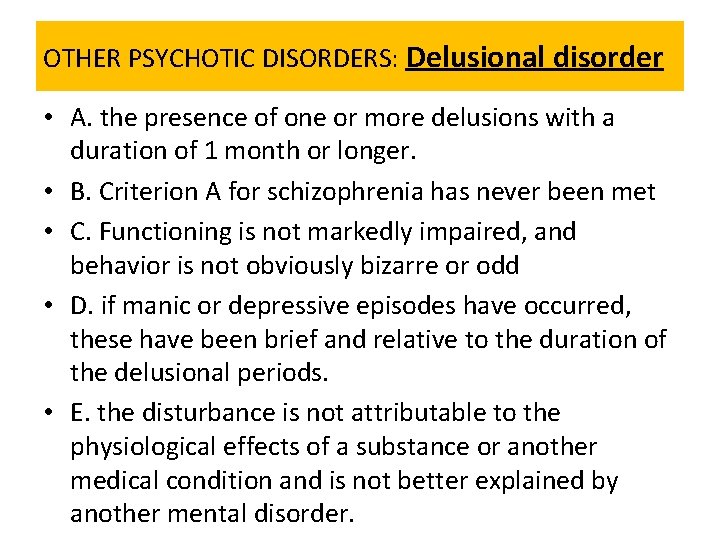
OTHER PSYCHOTIC DISORDERS: Delusional disorder • A. the presence of one or more delusions with a duration of 1 month or longer. • B. Criterion A for schizophrenia has never been met • C. Functioning is not markedly impaired, and behavior is not obviously bizarre or odd • D. if manic or depressive episodes have occurred, these have been brief and relative to the duration of the delusional periods. • E. the disturbance is not attributable to the physiological effects of a substance or another medical condition and is not better explained by another mental disorder.
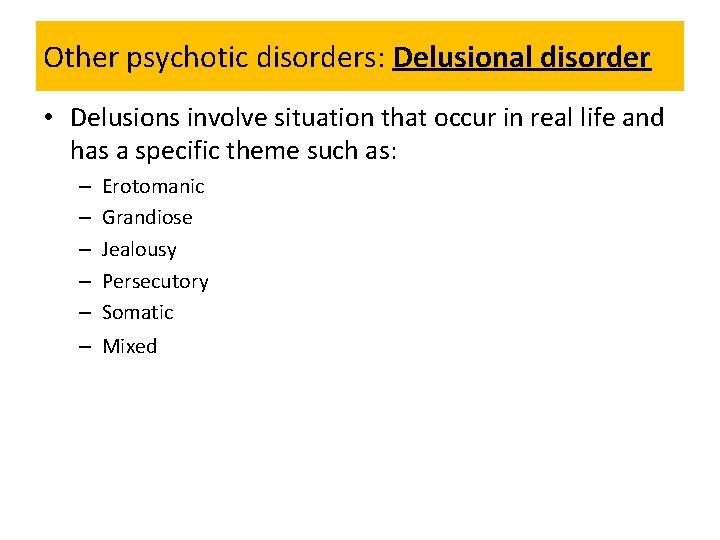
Other psychotic disorders: Delusional disorder • Delusions involve situation that occur in real life and has a specific theme such as: – – – Erotomanic Grandiose Jealousy Persecutory Somatic – Mixed
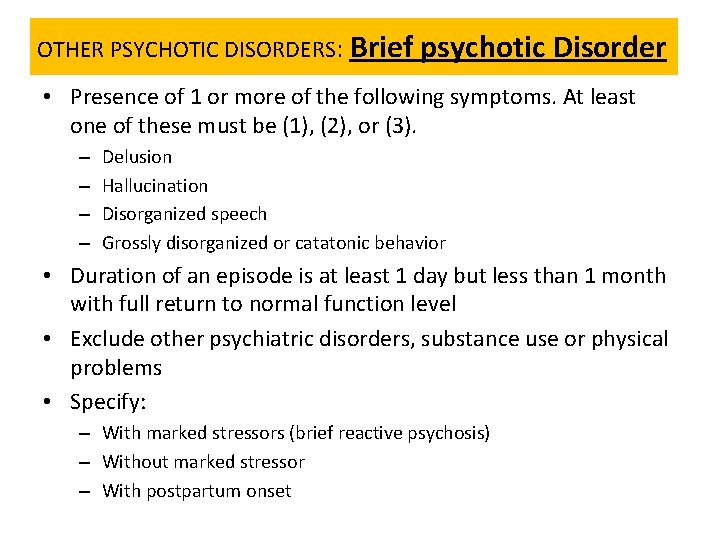
OTHER PSYCHOTIC DISORDERS: Brief psychotic Disorder • Presence of 1 or more of the following symptoms. At least one of these must be (1), (2), or (3). – – Delusion Hallucination Disorganized speech Grossly disorganized or catatonic behavior • Duration of an episode is at least 1 day but less than 1 month with full return to normal function level • Exclude other psychiatric disorders, substance use or physical problems • Specify: – With marked stressors (brief reactive psychosis) – Without marked stressor – With postpartum onset
Schizophrenia Co-morbid Conditions • • Depression Anxiety Aggression Substance use disorder 37
Treatment
Treatment Modalities • Cornerstones of treatment are: – Medication management—Antipsychotics – Psychosocial treatments
Antipsychotics • Divided into 2 classes: – Traditional or Typical – Novel or Atypical
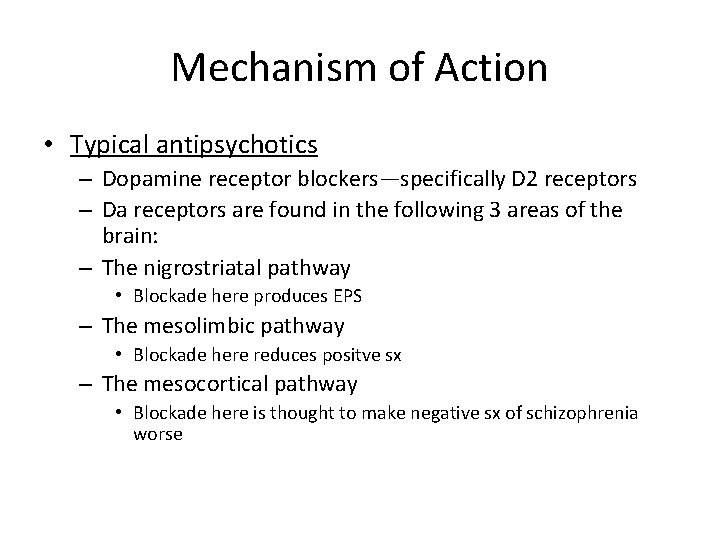
Mechanism of Action • Typical antipsychotics – Dopamine receptor blockers—specifically D 2 receptors – Da receptors are found in the following 3 areas of the brain: – The nigrostriatal pathway • Blockade here produces EPS – The mesolimbic pathway • Blockade here reduces positve sx – The mesocortical pathway • Blockade here is thought to make negative sx of schizophrenia worse
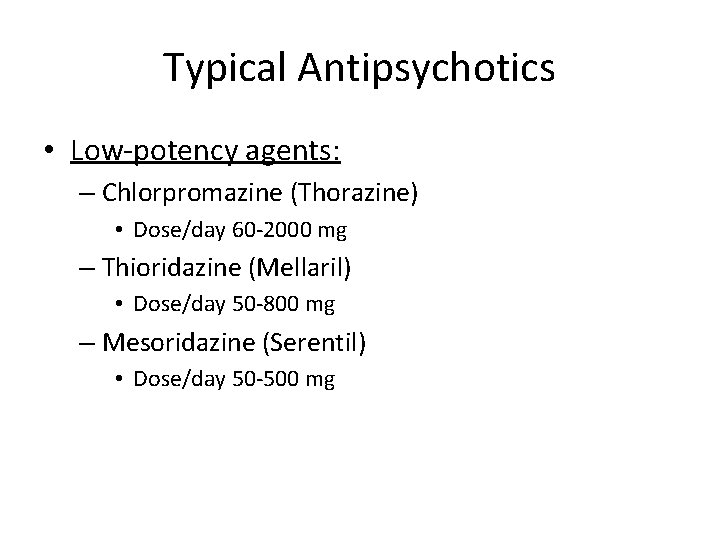
Typical Antipsychotics • Low-potency agents: – Chlorpromazine (Thorazine) • Dose/day 60 -2000 mg – Thioridazine (Mellaril) • Dose/day 50 -800 mg – Mesoridazine (Serentil) • Dose/day 50 -500 mg
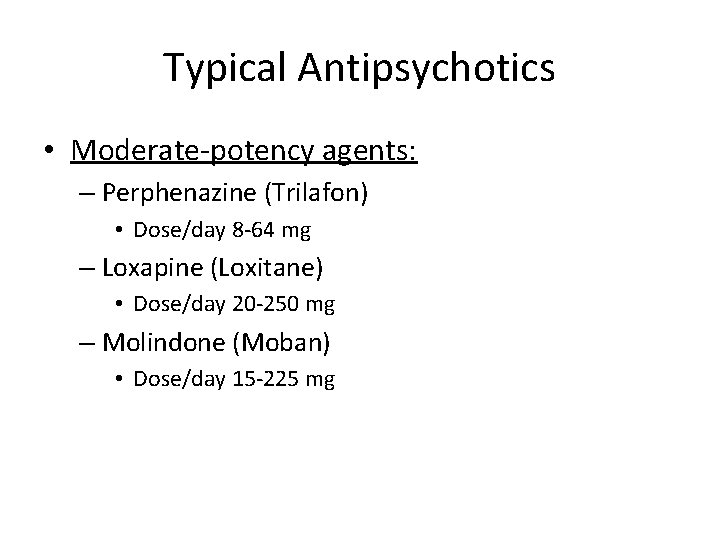
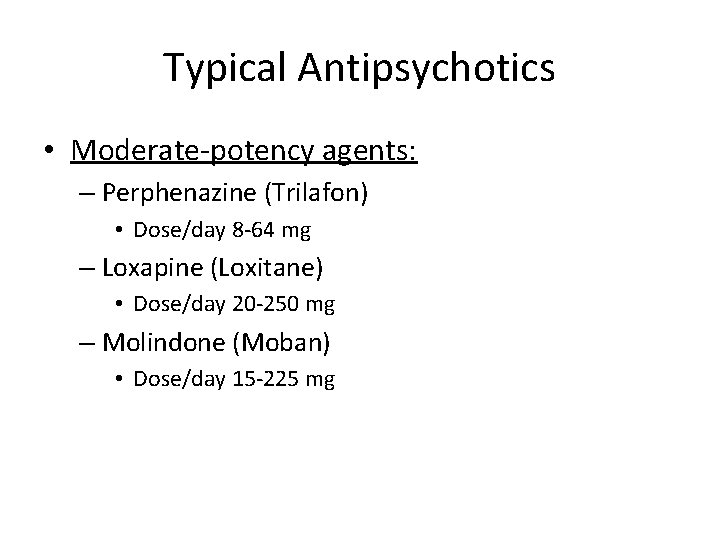
Typical Antipsychotics • Moderate-potency agents: – Perphenazine (Trilafon) • Dose/day 8 -64 mg – Loxapine (Loxitane) • Dose/day 20 -250 mg – Molindone (Moban) • Dose/day 15 -225 mg
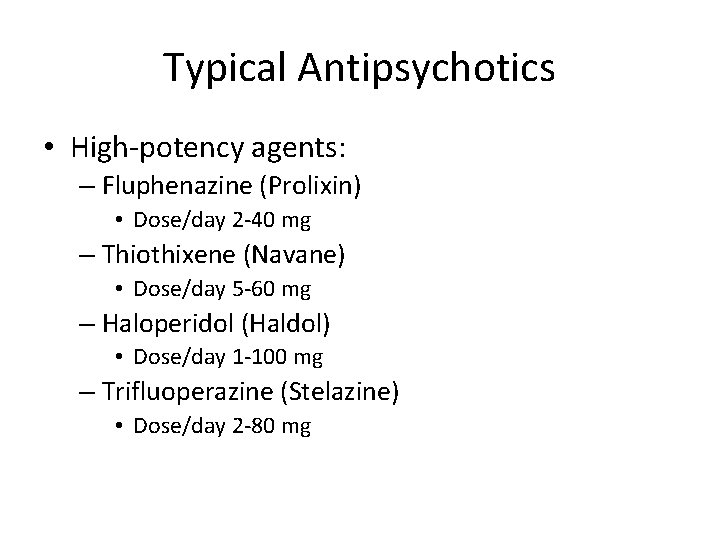
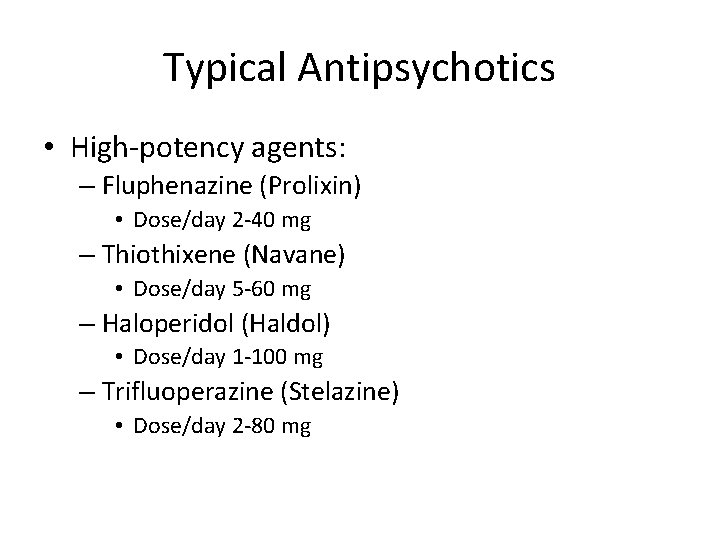
Typical Antipsychotics • High-potency agents: – Fluphenazine (Prolixin) • Dose/day 2 -40 mg – Thiothixene (Navane) • Dose/day 5 -60 mg – Haloperidol (Haldol) • Dose/day 1 -100 mg – Trifluoperazine (Stelazine) • Dose/day 2 -80 mg
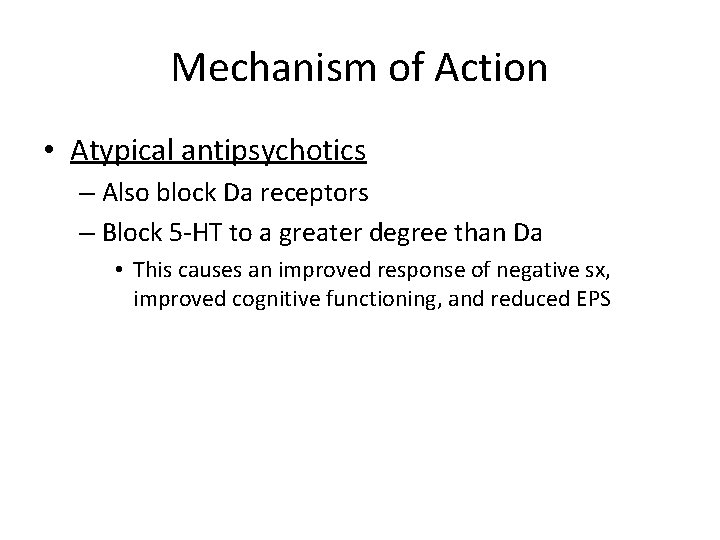
Mechanism of Action • Atypical antipsychotics – Also block Da receptors – Block 5 -HT to a greater degree than Da • This causes an improved response of negative sx, improved cognitive functioning, and reduced EPS
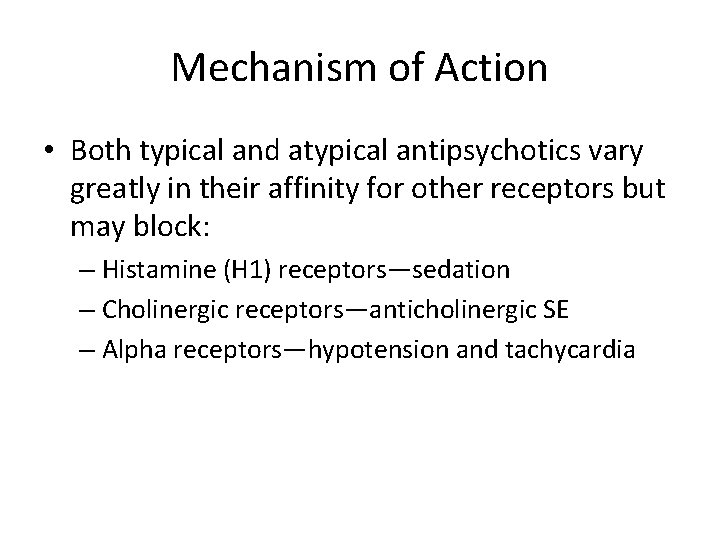
Mechanism of Action • Both typical and atypical antipsychotics vary greatly in their affinity for other receptors but may block: – Histamine (H 1) receptors—sedation – Cholinergic receptors—anticholinergic SE – Alpha receptors—hypotension and tachycardia
Side Effect Profile • Low-potency drugs cause more sedation and hypotension • High-potency drugs cause more EPS • Drugs vary greatly in the amount of anticholinergic effects they cause – Drugs that are more likely to cause EPS have < anticholinergic effects
Acute Dystonia • Muscular spasm that may occur in up to 10% of clients • May effect different muscle groups – Blepharospasm—eye closing – Torticollis—neck muscle contraction; pulling head to one side – Oculogyric crisis—severe upward deviation of the eyeballs
Acute Dystonia (cont) • Anticholinergic drugs are rapidly effective in treating these sx • Severe presentations should be treated with IM injection • Examples of meds include: – – Benzotrpine (Cogentin) Trihexyphenidyl (Artane) Diphenhydramine (Benadryl) Amantadine (Symmetrel)
Neuroleptic Induced Pseudoparkinsonism • Results from imbalance between Da and Ach in the nigrostriatal pathway • Sx include: – – – – Tremors Bradykinesia/akinesia (slowness of movement) Cogwheel rigidity Shuffling gait Masked facies Hypersalivation and drooling Treat sx with anticholinergic drugs
Akathisia • Presents with both objective and subjective components – Objective sx include: • • Motor restlessness Pacing Rocking Foot tapping – Subjective c/o include: • Inner restlessness—tension, irritability, inability to sit or lie down
Akathisia (cont) • Beta-blockers and benzos are the most common adjunctive Rxs – Propanolol (Inderal) – Lorazepam (Ativan)
Tardive Dyskinesia • Generally associated with long-term antipsychotic use • Irreversible • Characterized by choreoathetoid movements—rapid, jerky, and slow, writhing – Clients generally experience involuntary movements of the mouth, tongue, and face – Arm, finger, leg, feet, and truncal movements are also noted
Neuroleptic Malingnant Syndrome (NMS) • Potentially fatal reaction to antipsychotics • Characterized by: – – Muscular rigidity Hyperthermia Altered consciousness Autonomic dysfunction • Lab findings include: – Leucocytosis – Increased creatine phosphokinase – Increased myoglobinuria
Neuroleptic Malingnant Syndrome (NMS) • Can occur at any time during Rx but is more frequent shortly after initiation of antipsychotics or dose increases • Underling pathophysiology is unclear—has to do with depletion of Da in basal ganglia
Neuroleptic Malingnant Syndrome (NMS) • ***First D/C antipsychotic • Hydration and cooling are of major importance – May also give muscle relaxant IV – Dantrolene or bromocriptine (Da agonists) can also be prescribed to relieve rigidity
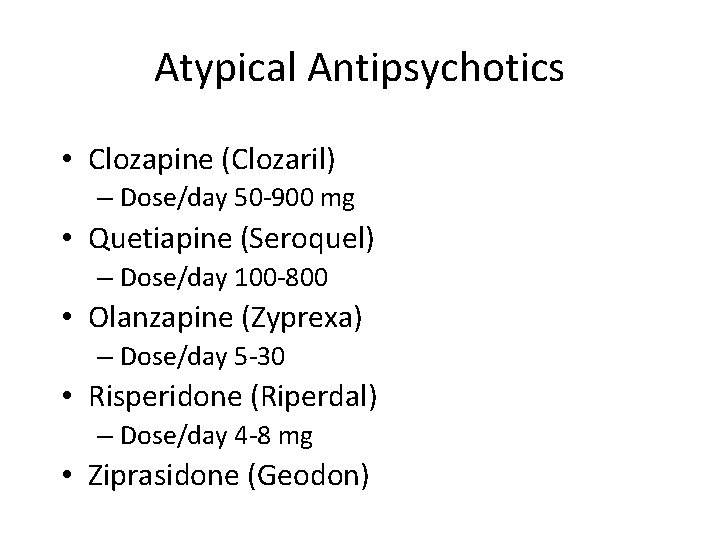
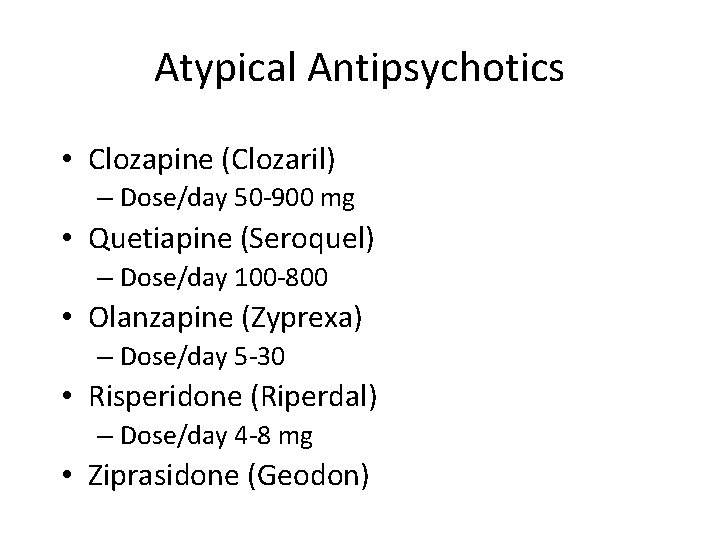
Atypical Antipsychotics • Clozapine (Clozaril) – Dose/day 50 -900 mg • Quetiapine (Seroquel) – Dose/day 100 -800 • Olanzapine (Zyprexa) – Dose/day 5 -30 • Risperidone (Riperdal) – Dose/day 4 -8 mg • Ziprasidone (Geodon)
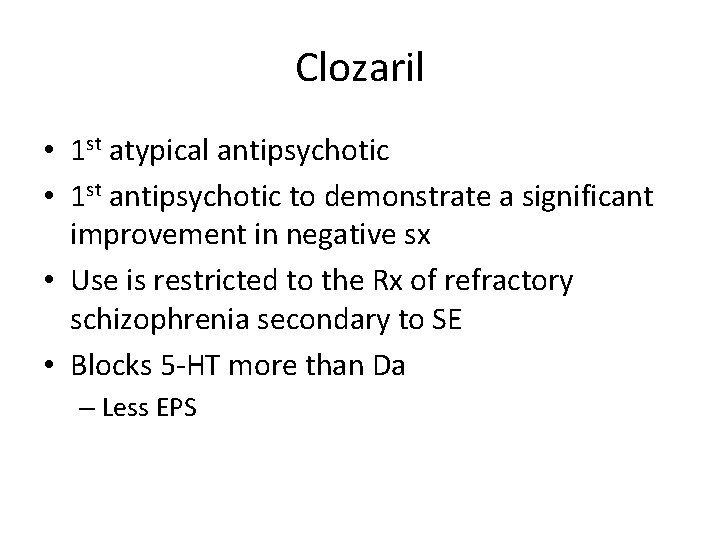
Clozaril • 1 st atypical antipsychotic • 1 st antipsychotic to demonstrate a significant improvement in negative sx • Use is restricted to the Rx of refractory schizophrenia secondary to SE • Blocks 5 -HT more than Da – Less EPS
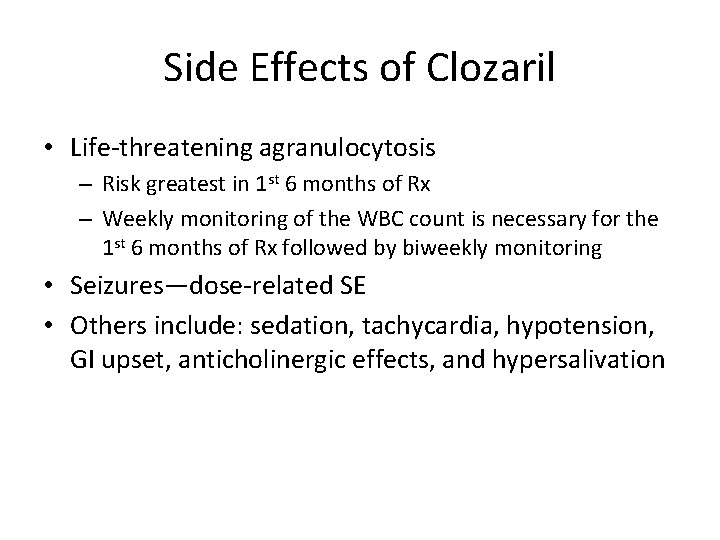
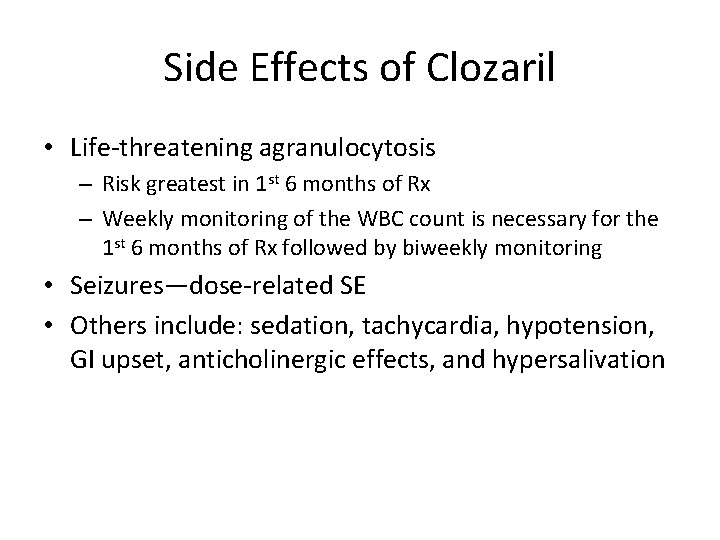
Side Effects of Clozaril • Life-threatening agranulocytosis – Risk greatest in 1 st 6 months of Rx – Weekly monitoring of the WBC count is necessary for the 1 st 6 months of Rx followed by biweekly monitoring • Seizures—dose-related SE • Others include: sedation, tachycardia, hypotension, GI upset, anticholinergic effects, and hypersalivation
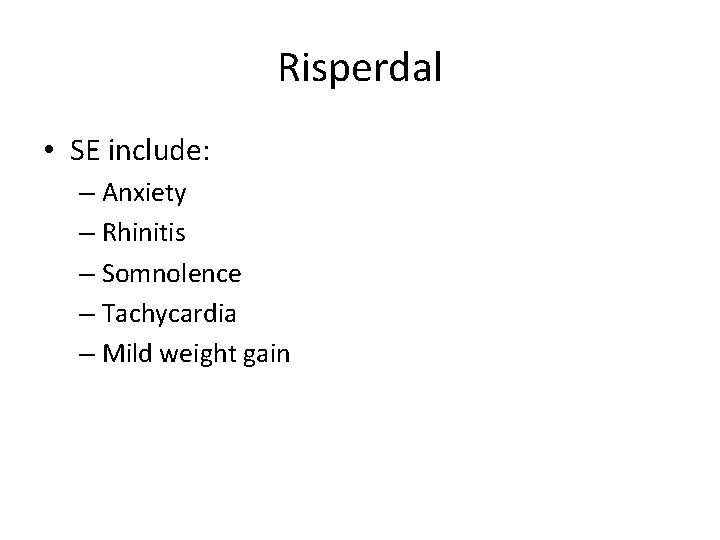
Risperdal • SE include: – Anxiety – Rhinitis – Somnolence – Tachycardia – Mild weight gain
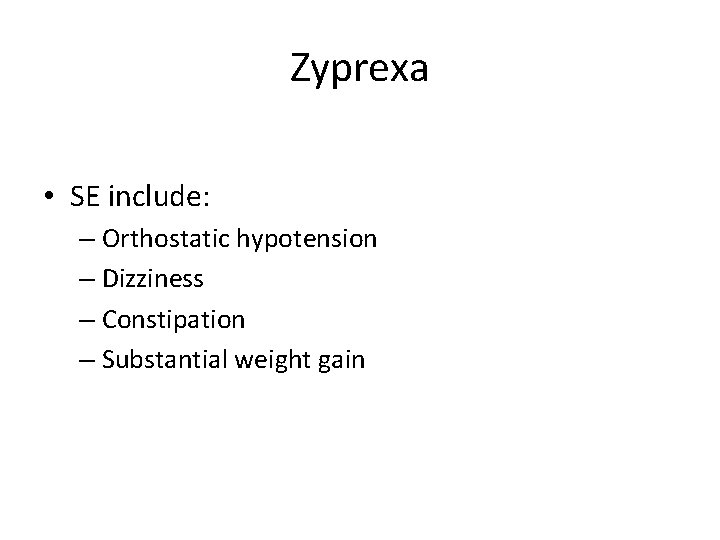
Zyprexa • SE include: – Orthostatic hypotension – Dizziness – Constipation – Substantial weight gain
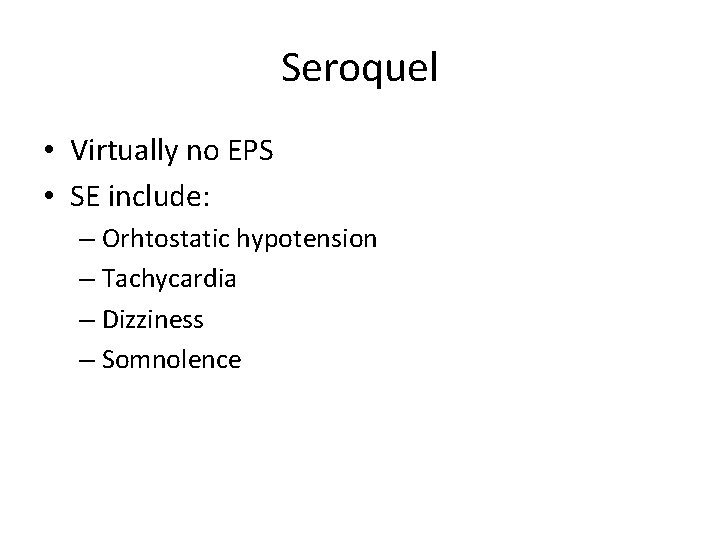
Seroquel • Virtually no EPS • SE include: – Orhtostatic hypotension – Tachycardia – Dizziness – Somnolence
Geodon • • • **Prolongs QTc interval Somnolence Hypotension Nausea Constipation
De-escalation Techniques • Manage the environment • Show confidence and leadership • Encourage verbalization • Personalize yourself and show concern • Use breakaways • Using and removing seclusion and restraints • Documenting event • Debriefing session with staff
Communication Techniques with the Psychotic Patient • Establish trust • Personal space • Soft tone of voice, open posture, not too much eye contact • Don’t argue with delusions • Present reality • Use diversions rather than confrontation • Allow patient to make own decisions when possible • Try to alleviate their fears due to misperceptions
Psychotherapeutic management • • Provide supportive care Strengthen patient’s self-esteem Treat patients as adults Prevent failure/ embarrassment Respect individuality - unique Reinforce reality Handle hostility calmly & matter-of-factly
Issues related to Schizophrenia • Family ⇔ the patient communication, overprotection, blaming • Non-compliance with medical regimen • Caregiver’s needs - cope with strange and frightening behaviors ie. apathy, poor personal hygiene, violence
Issues related to Schizophrenia (II) • Depression - part of the symptoms, be masked during acute stage • Relapse - stressors, noncompliance • Stress & coping • Substance abuse -30% have dual Dx. , cause (-) effect on the treatment & poor outcomes • Work - no work, inability, no motivation
Depression and Suicide in Schizo • Depression is a natural part of schizo • Depression can be masked especially during the acute phase • Depression is a reaction to schizo
Care of Hallucinations & Delusions • Hallucinations – Content of hallucination – commanding H -> suicidal or homicidal – N’s attitude – nonjudgmental, nonthreatening – Eye contact, louder voice, call the person by name • Delusion – Be empathic - Clarify the reality of the pt’s intent – Clarify misinterpretations of the environment – No argument
Delusion & Nursing Intervention • presenting reality, orient pts to time, person & place • avoid argument, touch, competitive activities, • reinforce positive behaviors • encourage verbalization
Disruptive Behavior Set limit decrease environmental stimuli intervention before acting out close observation safety environment - minimize potential weapons • making contract with the client • using restraints • • •
Withdrawn Patients • arrange nonthreatening activities • encourage participation - seating • provide remotivation and resocialization group experience • reinforce appropriate grooming and hygiene • provide psychosocial rehabilitation - social skill training, . . .
Suspicious Patients • • • Be matter-of-fact; (ie DST for depression) avoid close physical contact - no touch be consistent in activities offer special food avoid whisper Maintain eye contact
Hyperactivity Patients • Allow pt to stand for a few min in group • Provide a safe environment • Provide activities that do not require fine motor skills
Immobility Patients • Minimize circulatory problem • Provide adequate diet, exercise, and rest • Prevent victimization
Nursing interventions • • Medication compliance- 40 -60% noncompliance Avoid reinforcing hallucinations & delusion Maintain orientation Use touch minimally and judiciously Avoid easily misinterpreted behavior Reinforce positive behaviors Avoid competitive activities, Allow & encourage expression of feelings
Nursing interventions. Milieu management • • clear & realistic limits; consistency; Supportive environment – structured, predictable reduced stimulation early intervention for escalating behavior safety for the pt and others opportunity for nonthreatening social interaction remotivating and resocializing group Communication skills
Nursing interventions – Family therapy • Involve the family – use appropriate community resources • Educate the family – chr. dis, S/S of relapse, med compliance, • Provide an outlet for the family – discuss feelings, explore alternative effective coping skills.
Psychotherapy • Individual Th – supportive therapy • Group Th – interpersonal skills, family problems, community support • Family Th – expand social network, problemsolving capacity, lower the emotional overinvolvement of families
Case Management • Limited hospital stay, 3 rd party payment • Discharge planning – transitional care • Partial hospitalization, halfway houses, day treatment programs • Community resources – NAMI, Schizophrenics Anonymous, …
Nurse’s feelings & self-assessment • Pt’s anxiety, loneliness, dependence, distrust > N’s uncomfort • Feelings of helplessness -> anxiety -> defensive behaviors ie denial, withdrawal, avoidance -> burnout • Peer group supervision can be helpful • Periodic reassessment of Tx goals,
Family/care taker education • Teaching about the disease –S/S • Medication teaching and side-effect management • Cognitive & social skills enhancement • Identifying signs of relapse • Attention to deficit in self-care, social and work functioning • Exploration of community resources
Signs of Potential Relapse • • • Feeling of tension Difficulty concentrating Trouble sleeping Increased withdrawal Increased bizarre/ magic thinking
Care of Hallucinations & Delusions • Hallucinations – Content of hallucination – commanding H -> suicidal or homicidal – N’s attitude – nonjudgmental, nonthreatening – Eye contact, louder voice, call the person by name • Delusion – Be empathic - Clarify the reality of the pt’s intent – Clarify misinterpretations of the environment – No argument
Treatment • Psychoeducation – Teach that stressors can exacerbate sx – Inform pt on illness and meds • Supportive Psychotherapy – Goal is to support ego function—help them to get through this—gentle guidance and advice • Milieu – Calm environment; safety • Symptom management – Focus on prodromal sx—make pt aware that they need to recognize these sx for exacerbations
Family Therapy • May be necessary to begin with individual family therapy in which each family member has a therapist • Need to target Expressed Emotion (EE) – Emphasize strengths not deficits – Share power—who is in control of the patient in the family – Contain outbursts – Problem solving skills • High levels of EE— 56% rehospitalization in 6 months • Low levels of EE— 21% rehospitalization in 6 months
Rehabilitation=Goal • Social skills training – Teach issues re: hygiene, personal space, eye contact, body language – Expressing interests in others – Teach empathy – Initiating contact with others • Vocational Rehab – Vocational counseling and education • Supportive employment – Get job in the community and have job coach come in to help you keep the job
Outcomes • 1/3 recover; 1/3 severe chronic; 1/3 exacerbations and remissions • In general, Schizophrenia is a relapsing and remitting course • Timing is relevant -early intervention ++ • Stabilize 1 st year • 1 st 6 months increased risk for suicide • Combined approaches best—meds alone aren’t enough
INTERNETRESOURCES http: //www. mentalhealth. com http: //www. mhsource. com/ http: //schizophrenia. mentalhelp. net/ http: //www. nami. org http: //www. healthcenter. com/mentalhealth/schizophrenia • http: //www. mss. mb. ca • http: //www. vaxxine. com/schizophrenia • http: //www. SAnonymous. org • • •