Asthma COPD Finals Teaching 2013 Alison Portes FY












- Slides: 33

+ Asthma & COPD Finals Teaching 2013 Alison Portes FY 1
+ Objectives n Main features of asthma and COPD n Focus on clinicals – history, examination, investigations, management n 10 minutes on each n Quiz and summary of key points n A few added extras…

+ Asthma

+ Asthma n Definition n Pathophysiology n History n Examination n Investigations n Management n n Acute Chronic n Medications n Paediatric Asthma
+ Definition n Obstructive airways disease n Chronic n Inflammatory n Variable n Reversible n Hyperresponsiveness
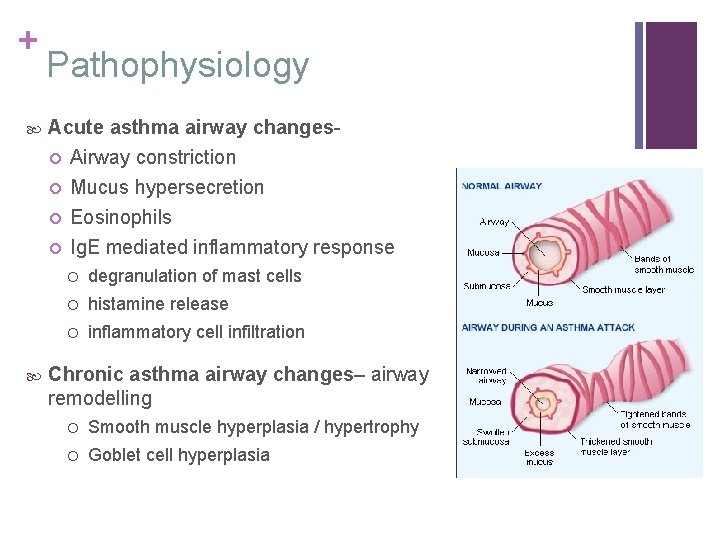
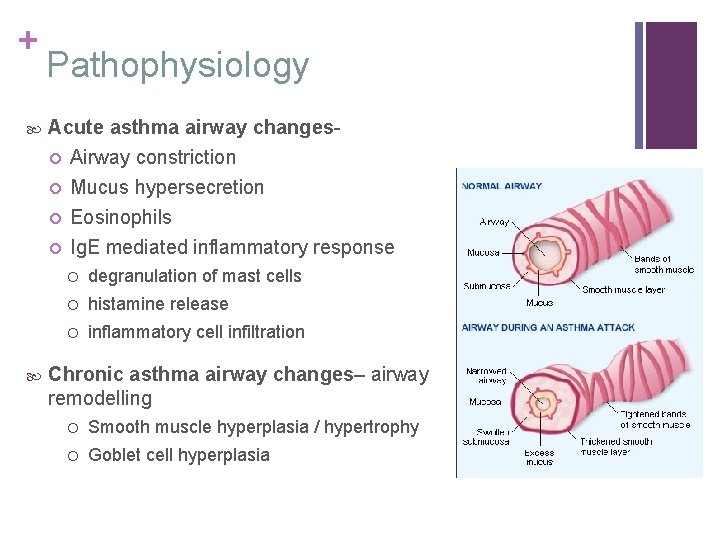
+ Pathophysiology Acute asthma airway changes Airway constriction Mucus hypersecretion Eosinophils Ig. E mediated inflammatory response degranulation of mast cells histamine release inflammatory cell infiltration Chronic asthma airway changes– airway remodelling Smooth muscle hyperplasia / hypertrophy Goblet cell hyperplasia
+ History n Full respiratory history plus… n Triggers (exercise, illness, cold, pets…) n Diurnal variation n Disturbed sleep n Atopy/family history of atopy n Occupation n Compliance with meds n GP/A&E/ITU attendances
+ Examination n Standard respiratory exam n ? Start at the back n Tachypnoea n Widespread polyphonic wheeze n Hyperresonant percussion note n Diminished breath sounds n Hyperinflated chest
+ Investigations n Bedside n n Bloods n n Blood gas – when and why? Imaging n n PEF CXR – when and why? Special tests n PEF monitoring n Spirometry - Bronchodilator challenge

+ Management - chronic asthma n BTS guidelines n Step 1: SABA only n Step 2: SABA & ICS 200 -800 mcg/day n Step 3: add LABA (combined) n Step 4: ↑ ICS dose (stop LABA if no benefit), monteleukast n Step 5: help! Oral steroids…

Asthma Medications Beclomethasone Salbutamol Salmeterol plus flixotide Salmeterol Mechanism?

+ Acute severe asthma n PEFR 50 -33% n RR ≥ 25 n HR ≥ 110 n Unable to complete sentences n But Sp. O 2 >92% n Worse = life-threatening (silent chest, cyanosis, low Sp. O 2) 3392 -CHEST n Better = moderate asthma
+ Management - Acute severe asthma n How would you like to manage this patient? n Immediate n A to E n Salbutamol 5 mg via oxygen driven nebuliser n Repeat obs (Sp. O 2, HR, RR) and PEF to assess for progression of severity and risk to life n If clinically stable and PEF >75%, can repeat Salbutamol nebs and consider oral prednisolone 40 -50 mg n Otherwise, add ipratropium nebs, IV hydrocortisone, consider magnesium sulphate IV and call for help!
+ Respiratory Failure n p. O 2 < 8 k. Pa n Type I n Normal/low p. CO 2 n V/Q mismatch/diffusion limitation n Atelectasis, pulmonary oedema, pneumonia, pneumothorax n Type II n ↑ p. CO 2 n ↓p. H if acute n Ventilatory failure n COPD, neuromuscular disorders (GBS, MND), CNS depression (drugs, brainstem injuries) n Needs controlled O 2 ± ventilation
+ Paediatric Asthma n Signs of chronic asthma/growth n Inhaler technique/spacers n Asthma vs. Viral induced wheeze n Differences in the BTS management guidelines n What age can a child do a peak flow? n Don’t let them leave without…
+ Communication Please explain to Mr X how to correctly use his inhaler Check understanding If you haven’t used it for a while, spray in the air to check it works Shake it As you breathe in, simultaneously press down on the inhaler Continue to breathe deeply Hold your breath for 10 seconds or as long as you comfortably can, before breathing out slowly. If you need to take another puff, wait for 30 seconds, shake your inhaler again then repeat Advise on using a spacer
+ COPD
+ COPD n Definition n Pathophysiology n History n Examination n Investigations n Management n Chronic n Acute Exacerbation
+ Definition n Umbrella term – chronic bronchitis and /or emphysema n Airflow obstruction (FEV 1/FVC < 0. 7) n Usually progressive n Not fully reversible n Doesn’t change markedly over few months n Predominantly caused by cigarette smoking n Differentiation from asthma

+ n n Pathophysiology Chronic bronchitis n Clinical diagnosis - chronic cough and sputum production on most days for at least 3 months per year for 2 years n Airway narrowing due to bronchiole inflammation, mucosal oedema and mucus hypersecretion Emphysema n Pathological diagnosis - permanent destructive enlargement of distal air spaces n Destruction and enlargement of alveoli that reduces elastic recoil and results in bullae

+ History n Full respiratory history plus… n Smoking, smoking!! n Consider your differentials – ILD, bronchiectasis, malignancy, heart failure – and rule them out n Red flag symptoms
+ Examination n Look and comment! n Tar stains n Accessory muscles n Barrel chest n Crepitations n Wheeze

+ Investigations n Bedside n n Bloods n n FBC, U&E, CRP, blood cultures, ABG Imaging n n n Sputum, ECG CXR Echo Special tests n n Spirometry α 1 -antitrypsin levels
+ Management of Chronic COPD Long term Conservative – smoking cessation, pulmonary rehabilitation, flu vaccination Medical – LTOT (only if not smoking), bronchodilators, antimuscarinics, home nebulisers, steroids (can consider if more than 2 infective exacerbations/year), prophylactic antibiotics Surgical – Transplant, lobectomy, bullectomy LTOT criteria Pa. O 2 <7. 3 k. Pa on air during period of clinical stability Pa. O 2 7. 3 -8. 0 k. Pa and signs of secondary polycythaemia, nocturnal hypoxaemia, peripheral oedema or pulmonary hypertension At least 15 hours a day
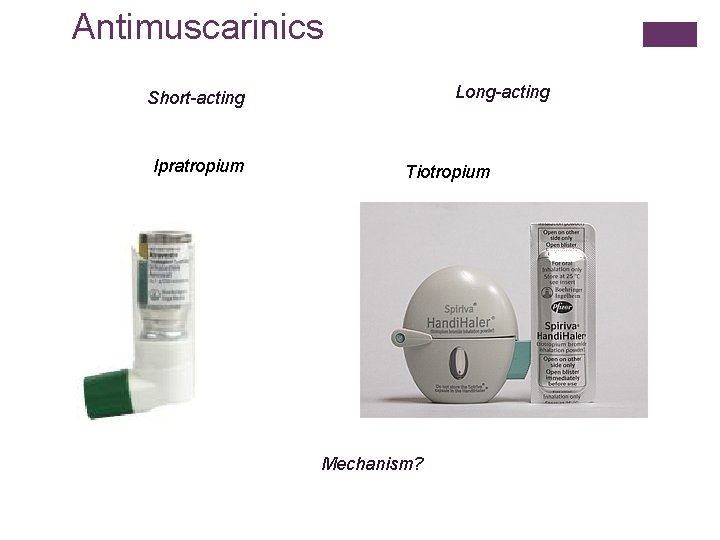
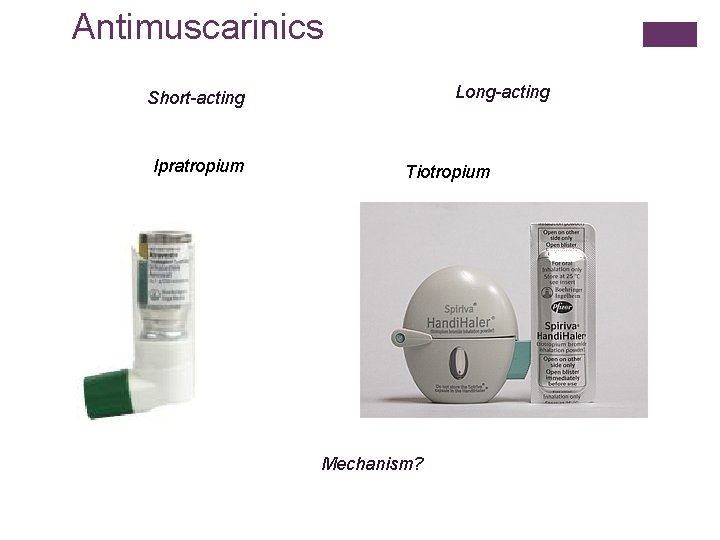
Antimuscarinics Long-acting Short-acting Ipratropium Tiotropium Mechanism?
+ Acute Exacerbation of COPD n Sustained worsening of symptoms from usual state n Beyond daily day-day variation n Acute in onset n Often associated with n n ↑ SOB, ↑ cough, ↑ sputum volume, ↑ sputum purulence Not pneumonia!
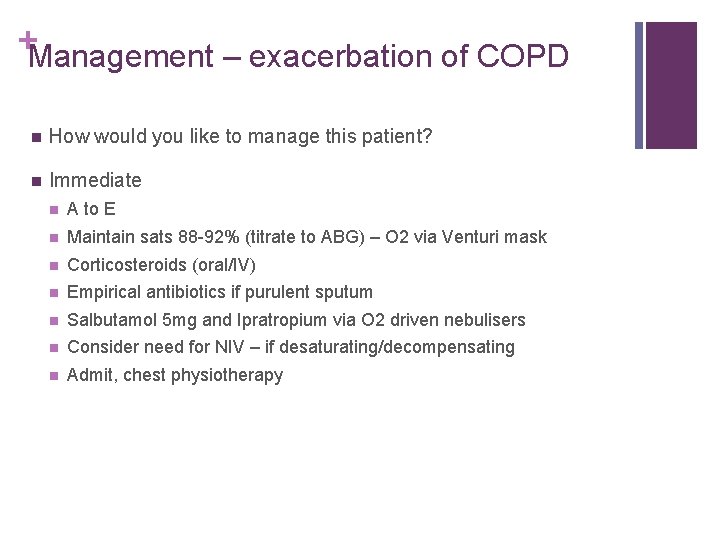
+Management – exacerbation of COPD n How would you like to manage this patient? n Immediate n A to E n Maintain sats 88 -92% (titrate to ABG) – O 2 via Venturi mask n Corticosteroids (oral/IV) n Empirical antibiotics if purulent sputum n Salbutamol 5 mg and Ipratropium via O 2 driven nebulisers n Consider need for NIV – if desaturating/decompensating n Admit, chest physiotherapy
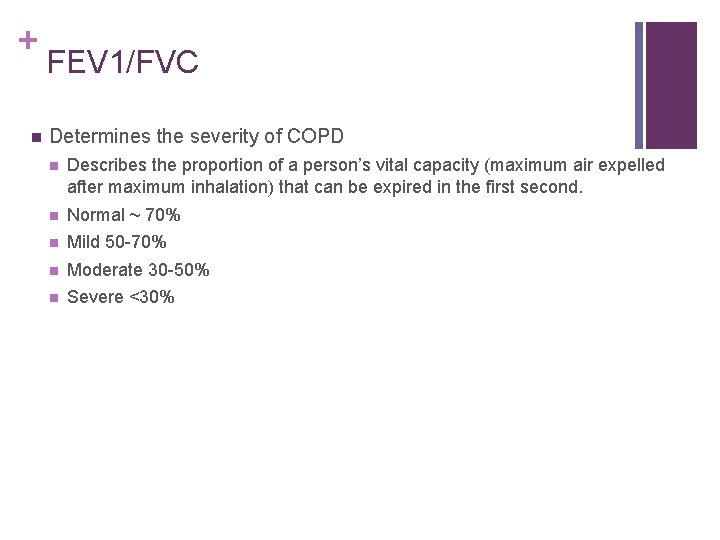
+ n FEV 1/FVC Determines the severity of COPD n Describes the proportion of a person’s vital capacity (maximum air expelled after maximum inhalation) that can be expired in the first second. n Normal ~ 70% n Mild 50 -70% n Moderate 30 -50% n Severe <30%
+ Quiz What is in a brown inhaler? What are the features of life-threatening asthma? List 4 classes of drug used to treat Asthma/COPD? What are the criteria for LTOT? What is the 2 nd step in the BTS asthma ladder? And the 4 th? What level Sp. O 2 should you aim for in COPD patients? What is Spiriva?

+ Key Points n History and Examination – concentrate on doing the basics well n Investigations – what differential will it rule out? n Learn the essentials now and keep repeating them… n Acute severe/life-threatening asthma criteria n BTS asthma guidelines – the ladder n T 1 vs T 2 respiratory failure n LTOT criteria n Practice communication task – PEF, inhalers n Questions?

+ Extras
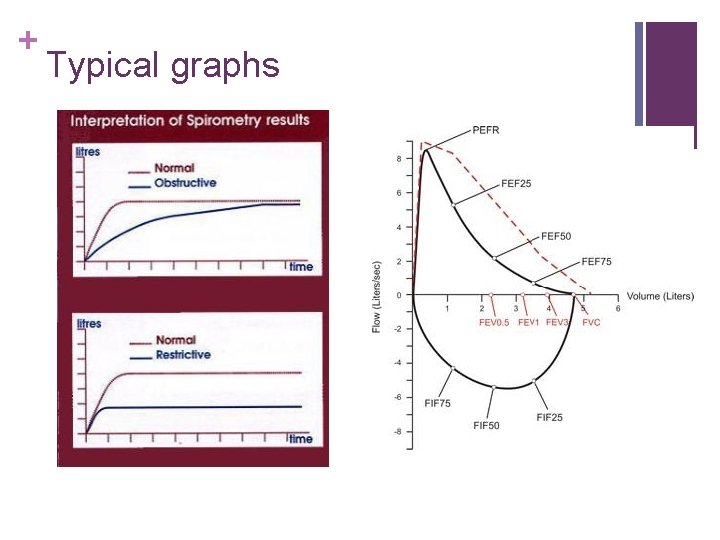
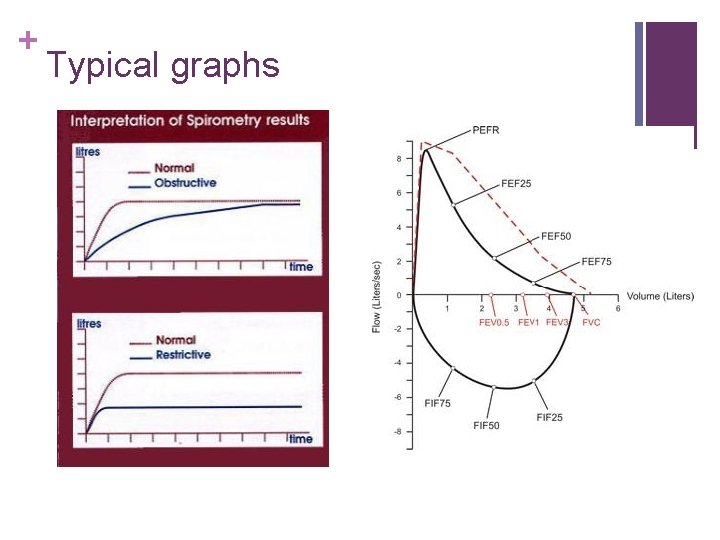
+ Typical graphs

Reading Chest X-Rays RIP. . . ABCDE Adequacy: -Rotation (symmetry of clavicles) -Inspiration (ribs) -Penetration (vertebral bodies) -Mention central lines, NG tubes, pacemakers etc -Airway: is the trachea central? -Boundaries and Both lungs: lung borders, consolidation, hazy etc -Cardiac: Heart size -Diaphragm -Everything else: soft tissue mass, fractures
 Asthma vs copd spirometry
Asthma vs copd spirometry Asthma vs copd spirometry
Asthma vs copd spirometry Pathophysiology definition
Pathophysiology definition Rvba
Rvba Sbu final exam schedule
Sbu final exam schedule Prelim, midterm finals grading system
Prelim, midterm finals grading system Fernando portes
Fernando portes Portes ouvertes staps nantes
Portes ouvertes staps nantes Lycée jean moulin albertville
Lycée jean moulin albertville Portes obertes pere calders
Portes obertes pere calders Fernando portes
Fernando portes Maximato que es
Maximato que es Portes ouvertes janson
Portes ouvertes janson Les portes du soleil juvignac
Les portes du soleil juvignac Discutez-en
Discutez-en Que es allo que tothom pren i ningu no les emporta
Que es allo que tothom pren i ningu no les emporta Dimensionet e portes se futbollit
Dimensionet e portes se futbollit Copd abcd assessment
Copd abcd assessment Copd stádiumai
Copd stádiumai Copd step up
Copd step up Ipassthebaton
Ipassthebaton Intercostaalspieren
Intercostaalspieren Copd exacerbation nursing management
Copd exacerbation nursing management Copd national action plan
Copd national action plan Blue and white inhaler
Blue and white inhaler Alveoli
Alveoli Pathogenesis of copd
Pathogenesis of copd Zorgleefplan 4 domeinen
Zorgleefplan 4 domeinen Conditietraining amsterdam oost
Conditietraining amsterdam oost Copd végstádium
Copd végstádium Copd pink puffer
Copd pink puffer Copd exacerbation nursing management
Copd exacerbation nursing management Bitemporal wasting in copd
Bitemporal wasting in copd Phân loại copd
Phân loại copd