Making Cataract Surgery Refractive Surgery Eric E Schmidt
- Slides: 51
Making Cataract Surgery Refractive Surgery Eric E. Schmidt, O. D. Bladen Eye Center Elizabethtown, NC
Cataract Surgery • It is considered to be the most successful surgery in the world! SO…. . • Why do we want to mess with success? • What’s all the fuss about? • What do we really want to achieve?
Goals Of Surgery • Visual improvement – maximum achievable visual acuity • 20/20 w/out eyeglasses! • No anisometropia • Remember though; 20/20 may not always be possible • Plano may not always be the best desired end point
Uncorrected 20/20 begins with you • • Choosing the right surgeon Counseling your patient Keep abreast of “new stuff” Guide your surgeon to become proficient at “new stuff” • Keep your staff up-to-date on the “new stuff” • Identify patients who would benefit from “new stuff” • You need to understand that cataract surgery should be considered refractive surgery
Why Bother With Co-Management? • • • Enhance px success Continuity of care Logistic concerns They are your patients Builds practice image • It is certainly not a monetary issue!!!
Pre-operative procedures • Set realistic goals for each individual patient • Perform detailed binocular refraction • Determine desired endpoint for the patient’s visual system • Choose the best procedure to achieve this • Perform all the necessary pre-op tests – – – A-Scan PAM BAT DFE Retinal imaging Wavefront testing
Pre-operative management • Px counseling – Describe the procedure, anesthesia – Describe the post-op course • • • Choose the surgeon Schedule the appt Pre-op regimen Prescribe the pre-op meds Discuss case w/ surgeon
A-Scan • Biometry- this is the key to choosing the correct IOL power. • IOL chosen based on desired endpoint refraction, axial length and keratometry • A-Scan ultrasound – very easy to perform • CPT code – 76516 76519 • Should this be done by the referring OD?
IOL MASTER • Zeiss • Not ultrasonography • High resolution partial coherence interferometry • Easy to perform (<1 minute, non-contact) • Yields extremely precise axial length (0. 02 mm), white-to-white, AC depth (+/0. 1 mm) and keratometry • Costs more, same reimbursement, but allows us to pinpoint endpoint refractive
IOL MASTER • Traditional SRK and Holladay Formulas, but. . • Haigis formula – – Surgeon specific – IOL specific – Allows a new level of mathematical flexibility in calculating IOL power • Greatly increases accuracy and precision as compared to A-scan
IOL Master • This renders a 5 -fold increase in accuracy • Solves some A-scan issues – Posterior staphyloma – Long eyes (>24. 5 mm) – Short eyes (<22 mm) – Silicone oil – Asteroid hyalosis
Cataract Surgery- We’ve Come A Long Way Baby! • • ICCE ECCE Phacoemulsification No-stitch, no patch
Surgical Incisions • Is one type really better than another? • Scleral tunnel • Clear cornea • Micro-incision (1 mm)
Phacoemulsification • • • No new advances in this ; until now! 2 new instruments Less energy, less heat No need for irrigation Sleeveless allows for micro-incisions • Capsulorhexis technique is very important
Current Phaco Energy Sources • Ultrasound – Efficiently emulsifies cataracts of any hardness – Rapid motion of phaco tip creates friction/heat • Laser – Efficiently emulsifies only +1 or +2 cataracts – Rests between laser bursts allow cooling • Sonic – Efficiently emulsifies only +1 or +2 cataracts – Less tip motion and friction/heat than ultrasound
Micro-incisions need micro IOL!!! • Super thin IOL • Injectable IOL • “Liquid” IOL – Lens refilling procedure
Post-operative regimen • Not much new to talk about EXCEPT… – The incidence rate of endophthalmitis is tripling • 0. 66% in clear cornea • 0. 25% in scleral tunnel – Can we prevent this? – Why is this happening?
Post-operative regimen • Antibiotic – 4 th generation fluoroquinolone QID • Steroid – prednisolone acetate 1% QID (or more) • NSAID • Intraocular steroid – Dex DSS • Post-op visits – 1 day – 1 week – 3 -4 weeks (DFE)
Clear Corneal Incisions Don’t Leak… They Suck !!!!
Endophthalmitis • Increase due to natural endogenous flora from lids • 75 -90% gram positives – Staph. Epidermidis (42%) – Staph. Aureus, Enterococcus • Pay close attention to the lids pre- and post-operatively
To reduce endophthalmitis incidence • Fluoroquinolone QID 4 days prior to surgery • Lid scrubs if needed • Artificial tears • Betadine prep peri-operatively • May need to leave px on topical antibiotics longer post-operatively • Orals ? ?
Post-op concerns • • • Glare and haloes Internal reflections Anisometropia 2 nd eye management Post. Capsule opacification
What About Astigmatism? • Toric IOL • Astigmatic Keratotomy • Who are candidates? • Are there refractive limitations? • What can the patient (and us ) realistically expect?
Toric IOL • STAAR Surgical silicone plate lens • Corrects 1. 4 – 2. 3 D of cyl at the spectacle plane • Corrects the astigmatism at the nodal point • Lessens distortion • Better qualitative visual acuity • Improved contrast sensitivity • There are some axis considerations
Toric IOL Success • Depends upon: – Surgical skill – the surgery must be astigmatically neutral – Proper IOL positioning – IOL maintaining a stable position in the bag – Aggressive post-operative monitoring
Toric IOL • Post-op considerations – Must be able to detect IOL rotation – If this occurs it must be corrected by 3 weeks – IOL may have to be rotated by surgeon – Patient must be dilated at 2 weeks to detect this
Astigmatic keratotomy • • Relaxing incision made nasally Shallow (<150 microns) Useful for pre-operative WTR cylinder -1. 00 to -2. 50 cylinder • How effective is it?
Astigmatic Keratotomy • When should you recommend it? – Plano in other eye – Px does not like to wear specs – CL wearer – Those “picky” patients – WTR cylinder (170 – 010) – High cylinder pxs • Post-op considerations
Astigmatic keratotomy • What are the drawbacks? – Poor predictability – Limited range of correction – Post-operative FB sensation
So an optometrists walks into an exam room to see a post-op px O. D. - How’re those eyes doing Mr. Jones? Px – Not so great. O. D. – Whaddaya mean , not so great? You’re seeing 20/20 in each eye without glasses! Px – Yeah, but I can’t see my newspaper!
What to do about presbyopia? • Monovision IOL • Presbyopic Lens Exchange (PRELEX) • Multifocal IOL • Accommodating IOL
Multifocal IOL options • Monovision • Refractive • Diffractive • Accommodative
The Ideal Multifocal IOL Patient • Baby Boomer – 50’s to the mid 60’s – Cataract starting to compromise quality of vision – Active lifestyle – Concerned about their appearance & ‘quality of life’ • Do not want to ‘get old’ • Spending billions on lifestyle enhancing procedures – Realistic Expectations – Motivated – Asks lots of questions
Who’s A Candidate? / Clinical • • Hyperopic Loss of accommodation Cataract Unilateral traumatic cataract Congenital cataract Astigmatism (can be corrected) High myopes (surgeon preference)
Who’s A Candidate? / Motivation • Wants to be less dependent on glasses • Understands the limitations of the Array® visual system • Willing to accept several months to adapt to their new visual system
Who’s Not A Candidate? • • Significant dry eyes Corneal scarring Mild to moderate myopia Pupil size < 2. 5 mm Monofocal implant in first eye Uncorrected post-op astigmatism > 0. 5 D Unstable capsular support Someone who demands perfect vision
Re. Zoom Multifocal IOL (AMO) • Refractive lens • 2 nd generation acrylic IOL • Delivers good near, distance and intermediate vision
Is The Re. Zoom Perfect? • The most common concerns – Distance blur – Monocular diplopia – Object glow – Ghosting – Halos at night • These are the biggest post-op challenges
Acrysof Re. Stor IOL (Alcon) • Diffractive technology • Silicone material • Uses “apodization” to soften blur and sharpen vision • Provides excellent VA at near, distance and intermediate ranges
Strengths of the Acry. Sof® Re. STOR® IOL • High quality uncorrected near and distance vision with 20/40 or better intermediate vision without movement of the IOL • 80% Overall Spectacle Freedom • Nearly 94% of patients would have the lens again
Aspheric Multifocal IOL Technology
Do We currently have any aspheric multifocal IOLs? • Tecnis multifocal (AMO) • Sofport AO (Bausch & Lomb)
Explain the WOW! Factor (or lack thereof) • Haloes and glaare at night are commonthese diminish with time • Longer adaptation period – may take weeks or months for pxs to accept their “new” visual system • Near vision may be fuzzy to myopes • May need reading specs for prolonged nearpoint work
Accomodative IOL • Crystalens- eyeonics • Silicone IOL with hinged optics • IOL moves forward or back depending on ciliary muscle tone • Implanted using phaco technique • Capsulorhexis is critical • Pre-op biometry crucial
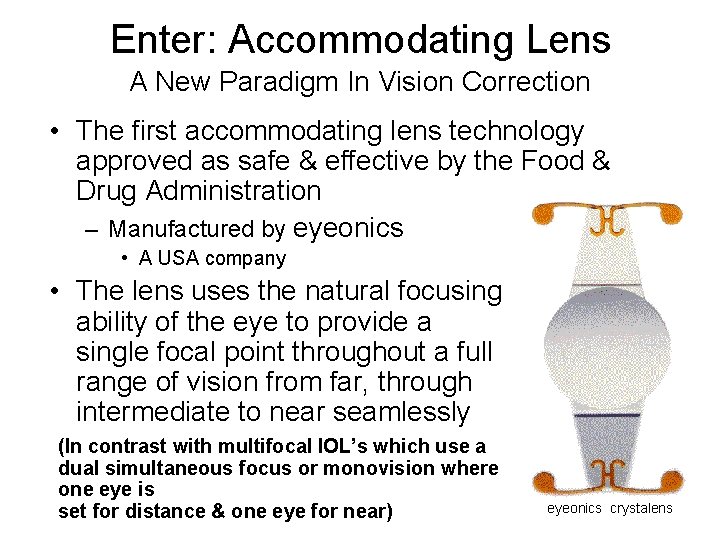
Enter: Accommodating Lens A New Paradigm In Vision Correction • The first accommodating lens technology approved as safe & effective by the Food & Drug Administration – Manufactured by eyeonics • A USA company • The lens uses the natural focusing ability of the eye to provide a single focal point throughout a full range of vision from far, through intermediate to near seamlessly (In contrast with multifocal IOL’s which use a dual simultaneous focus or monovision where one eye is set for distance & one eye for near) eyeonics crystalens
The Ideal Crystalens Patient • Baby Boomer – 50’s to the mid 60’s – Cataract starting to compromise quality of vision – Active lifestyle – Concerned about their appearance & ‘quality of life’ • Do not want to ‘get old’ • Spending billions on lifestyle enhancing procedures – Realistic Expectations – Motivated – Asks lots of questions
Crystalens Post-Op Considerations • • • 1% Atropine day of surgery & 1 day PO Otherwise standard post-op regimen Distance vision stable 1 week Near vision begins to return @ 2 weeks No significant glare or halos after 10 days Must follow more often
Crystalens Post-op: 10 -14 days post-op • • Keratometry Uncorrected distance and near visual acuity Controlled maximum plus refraction Distance and near visual acuity through distance correction • Gradual Plus Build-up to J 1 to determine add. • Verify refractive findings with cycloplegic refraction
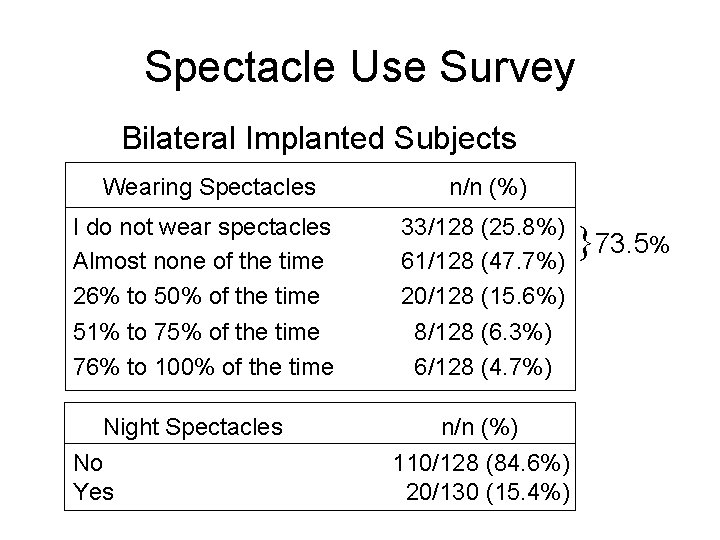
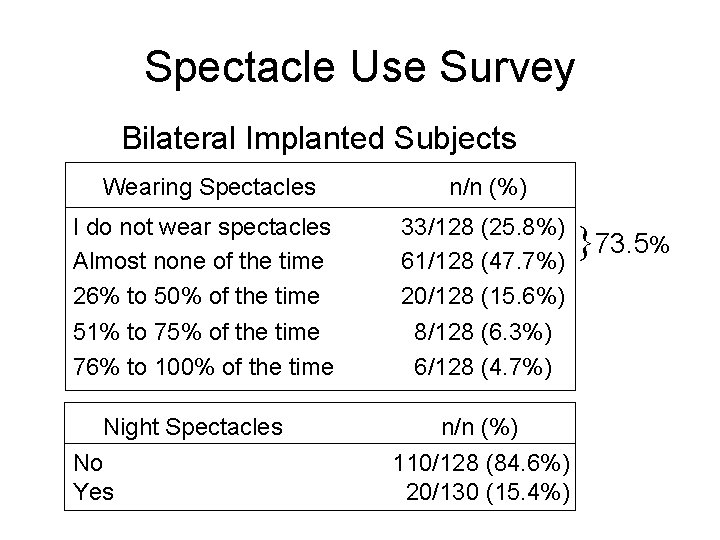
Spectacle Use Survey Bilateral Implanted Subjects Wearing Spectacles n/n (%) I do not wear spectacles Almost none of the time 26% to 50% of the time 33/128 (25. 8%) 61/128 (47. 7%) 20/128 (15. 6%) 51% to 75% of the time 76% to 100% of the time 8/128 (6. 3%) 6/128 (4. 7%) Night Spectacles No Yes n/n (%) 110/128 (84. 6%) 20/130 (15. 4%) }73. 5%
Is There A WOW Factor?
Cataract Surgery. What’s on the horizon? • Adjustable IOL– Material is fixed w/ laser to -0. 75 – Take to phoropter, refract to plano – “Fix” that w/ longer laser light • • ICL Clear Lens Extraction Impeller extraction technique Lens filling system