ANTIHYPERLIPIDEMIA Definition Definition Hyperlipidemia hyperlipoproteinemia or dyslipidemia is
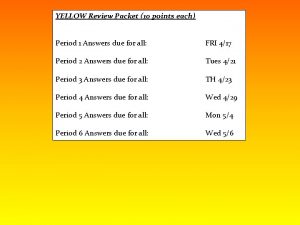
- Slides: 25
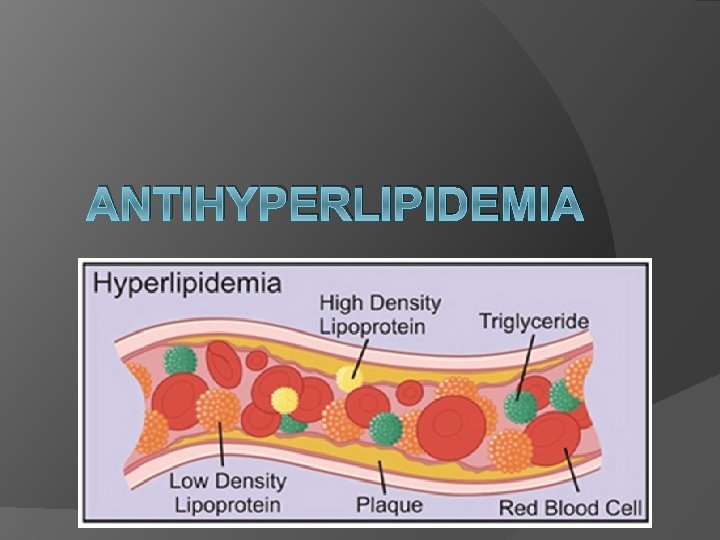
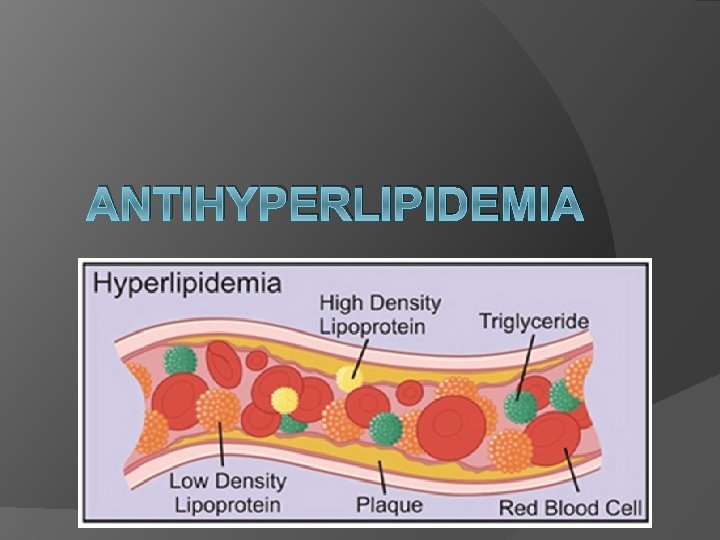
ANTIHYPERLIPIDEMIA
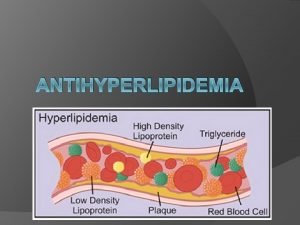
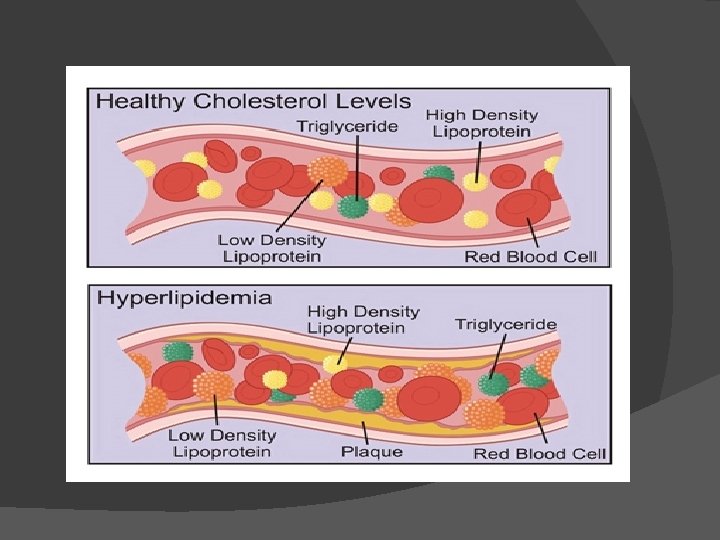
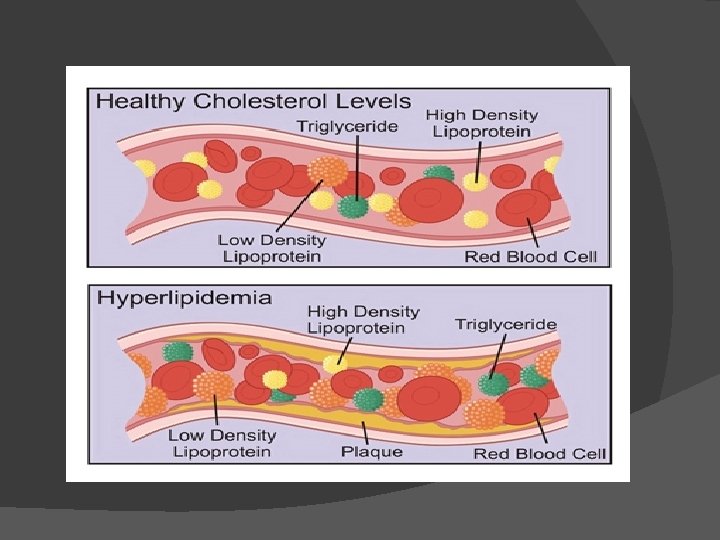
Definition : � Definition Hyperlipidemia, hyperlipoproteinemia or dyslipidemia is the presence of raised or abnormal levels of lipids and/or lipoproteins in the blood � Lipids are insoluble in aqueous solution. � Lipids (fatty molecules) are transported in a protein capsule, and the density of the lipids and type of protein determines the fate of the particle and its influence on metabolism. � Lipid and lipoprotein abnormalities are extremely common in the general population, and are regarded as a highly modifiable risk factor for cardiovascular disease due to the influence of cholesterol, one of the most clinically relevant lipid substances, on atherosclerosis.
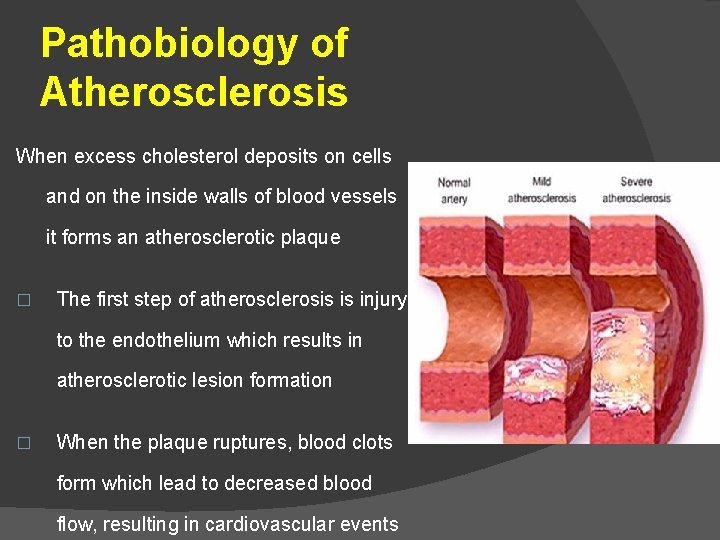
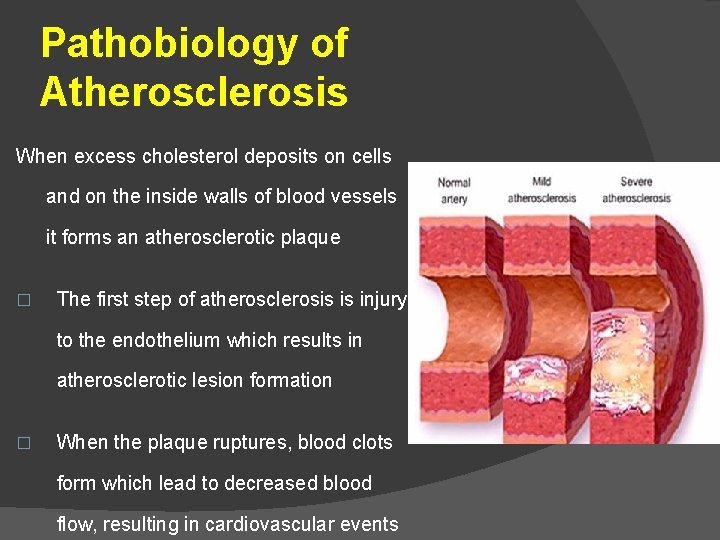
Pathobiology of Atherosclerosis When excess cholesterol deposits on cells and on the inside walls of blood vessels it forms an atherosclerotic plaque � The first step of atherosclerosis is injury to the endothelium which results in atherosclerotic lesion formation � When the plaque ruptures, blood clots form which lead to decreased blood flow, resulting in cardiovascular events
Complications of Hyperlipidemia � Macrovascular complications: �Unstable Angina (chest pain) �Myocardial Infarction (heart attack) �Ischemic Cerebrovascular Disease (stroke) �Coronary Artery Disease (heart disease) � Microvascular complications: �Retinopathy (vision loss) �Nephropathy (kidney disease) �Neuropathy (loss of sensation in the feet and legs)
Risk Factors for Hyperlipidemia � Obesity � Type 2 diabetes mellitus � Advanced age Hypothyroidism � Obstructive liver disease � Genetics � Drug induced: (e. g. glucocorticoids, thiazide diuretics, beta blockers, protease inhibitors, sirolimus, cyclosporine, progestins and alcohol)
Treatment Goals : �Reduce total cholesterol and LDL (bad) cholesterol �Prevent the formation of atherosclerotic plaques and stop the progression of established plaques �Prevent heart disease �Prevent morbidity and mortality
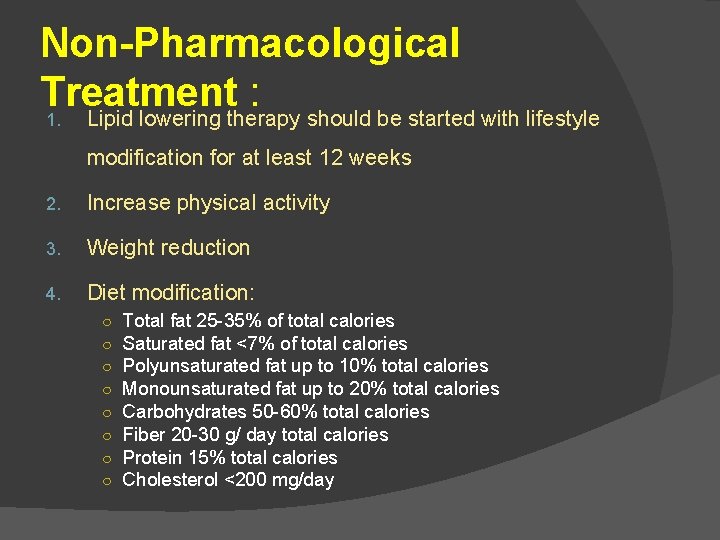
Non-Pharmacological Treatment : 1. Lipid lowering therapy should be started with lifestyle modification for at least 12 weeks 2. Increase physical activity 3. Weight reduction 4. Diet modification: ○ ○ ○ ○ Total fat 25 -35% of total calories Saturated fat <7% of total calories Polyunsaturated fat up to 10% total calories Monounsaturated fat up to 20% total calories Carbohydrates 50 -60% total calories Fiber 20 -30 g/ day total calories Protein 15% total calories Cholesterol <200 mg/day
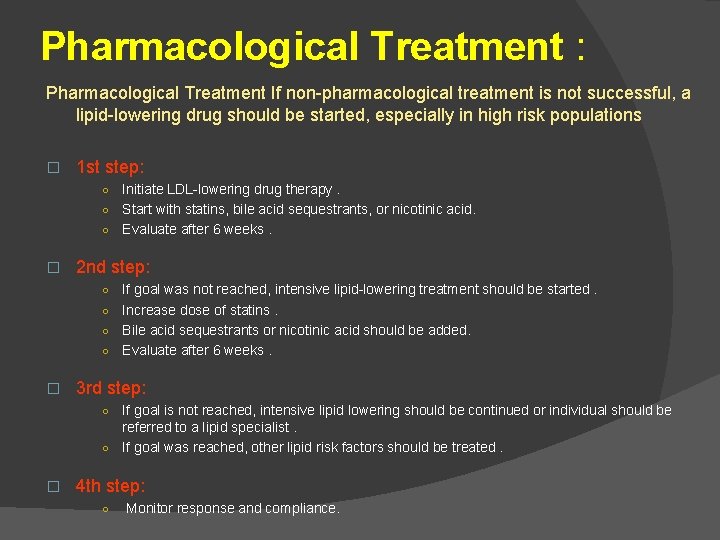
Pharmacological Treatment : Pharmacological Treatment If non-pharmacological treatment is not successful, a lipid-lowering drug should be started, especially in high risk populations � 1 st step: Initiate LDL-lowering drug therapy. ○ Start with statins, bile acid sequestrants, or nicotinic acid. ○ Evaluate after 6 weeks. ○ � 2 nd step: If goal was not reached, intensive lipid-lowering treatment should be started. ○ Increase dose of statins. ○ Bile acid sequestrants or nicotinic acid should be added. ○ Evaluate after 6 weeks. ○ � 3 rd step: If goal is not reached, intensive lipid lowering should be continued or individual should be referred to a lipid specialist. ○ If goal was reached, other lipid risk factors should be treated. ○ � 4 th step: ○ Monitor response and compliance.
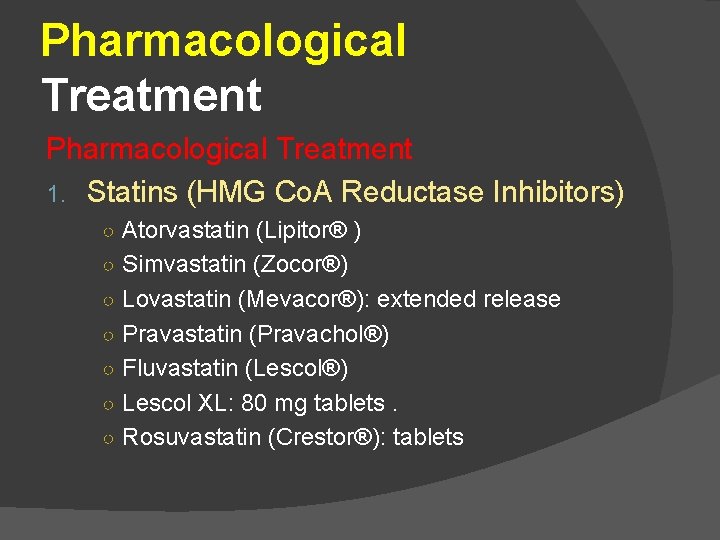
Pharmacological Treatment 1. Statins (HMG Co. A Reductase Inhibitors) ○ Atorvastatin (Lipitor® ) ○ Simvastatin (Zocor®) ○ Lovastatin (Mevacor®): extended release ○ Pravastatin (Pravachol®) ○ Fluvastatin (Lescol®) ○ Lescol XL: 80 mg tablets. ○ Rosuvastatin (Crestor®): tablets
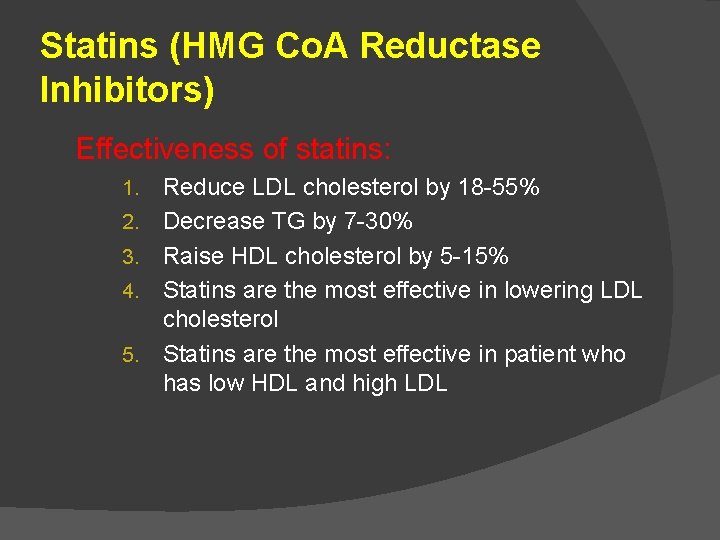
Statins (HMG Co. A Reductase Inhibitors) Effectiveness of statins: 1. 2. 3. 4. 5. Reduce LDL cholesterol by 18 -55% Decrease TG by 7 -30% Raise HDL cholesterol by 5 -15% Statins are the most effective in lowering LDL cholesterol Statins are the most effective in patient who has low HDL and high LDL
Statins (HMG Co. A Reductase Inhibitors) Mechanism of action: Statins inhibit HMG-Co. A reductase (enzyme involved in cholesterol synthesis) thus decreasing mevalonic acid production and stimulating LDL breakdown.
Statins (HMG Co. A Reductase Inhibitors) Side effects: �Muscle break down (rhabdomyolysis) �Increased liver enzymes �leading to renal failure �Fatigue, mild stomach disturbances, headache, or rash
Statins (HMG Co. A Reductase Inhibitors) Avoid use in: � Active or chronic liver disease and pregnancy Use with caution with: � Concomitant use of cyclosporine, macrolide antibiotics, antifungal agents. For example: Itraconazole, ketoconazole, erythromycin, clarithromycin, cyclosporine, nefazodone, HIV antiretrovirals � When statins are used with fibric acids and niacin, appropriate caution should be taken because of increasing incidence of muscle breakdown
Statins (HMG Co. A Reductase Inhibitors) Drug- food interaction: � Grapefruit juice increases concentration of statins � Pravastatin, rosuvastatin & fluvastatin concentrations are not affected by grapefruit juice. Monitoring: � Muscle soreness, tenderness, or pain. � Liver function tests : baseline, 4 -6 weeks after starting therapy, and then annually. � Muscle enzyme levels when individual has muscle pain
Pharmacological Treatment: 2. Bile Acid Sequestrants Mechanism of action: Bile acid sequestrants bind to bile acids in the intestine, thus inhibits uptake of intestinal bile salts into the blood and increases the fecal loss of bile salt-bound LDL
Bile Acid Sequestrants: 1) Cholestyramine (Questran®): Usual dose: 4 g by mouth 1 -2 times a day with meal to a maximum of 24 g per day. 2) Colesevelam (Welchol®): Usual dose: 3 tablets by mouth twice daily with meals or 6 tablets once daily with a meal. 3) Colestipol (Colestid®) Usual dose: ○ Granules: 5 -30 g by mouth daily given once or 2 -4 times a day with meal ○ Tablets: 2 -16 g by mouth daily.
Bile Acid Sequestrants: � Effectiveness: ○ Reduces LDL cholesterol by 15 -30% ○ Increases HDL cholesterol by 3 -5% ○ Increases TG. � Drug interaction: ○ Decreased absorption of fat soluble Vitamins: A, D, E, K, C and folic acid ○ Decreased absorption of other drugs: tetracycline, thiazide diuretics, aspirin, phenobarbital, pravastatin, digoxin
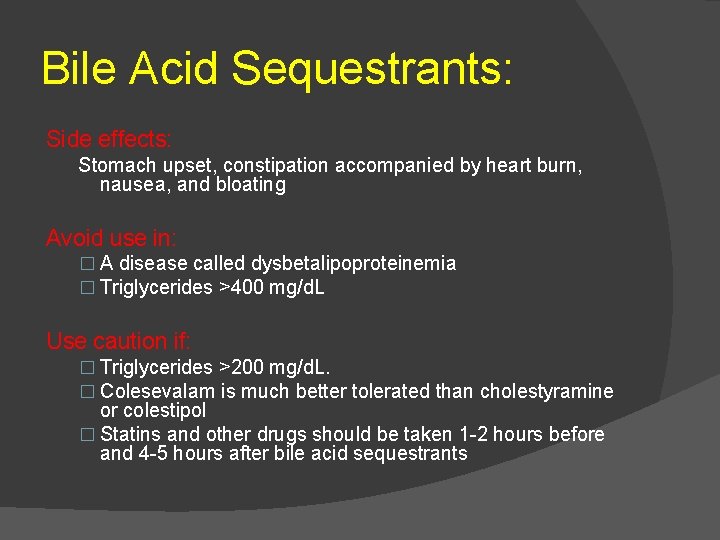
Bile Acid Sequestrants: Side effects: Stomach upset, constipation accompanied by heart burn, nausea, and bloating Avoid use in: � A disease called dysbetalipoproteinemia � Triglycerides >400 mg/d. L Use caution if: � Triglycerides >200 mg/d. L. � Colesevalam is much better tolerated than cholestyramine or colestipol � Statins and other drugs should be taken 1 -2 hours before and 4 -5 hours after bile acid sequestrants
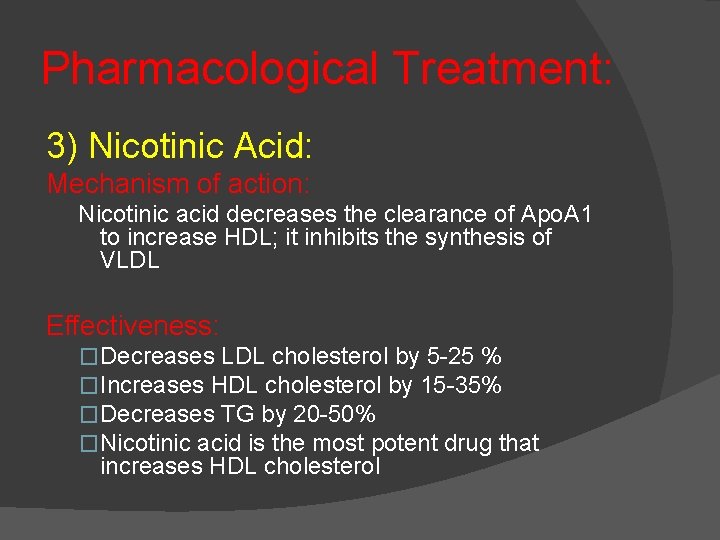
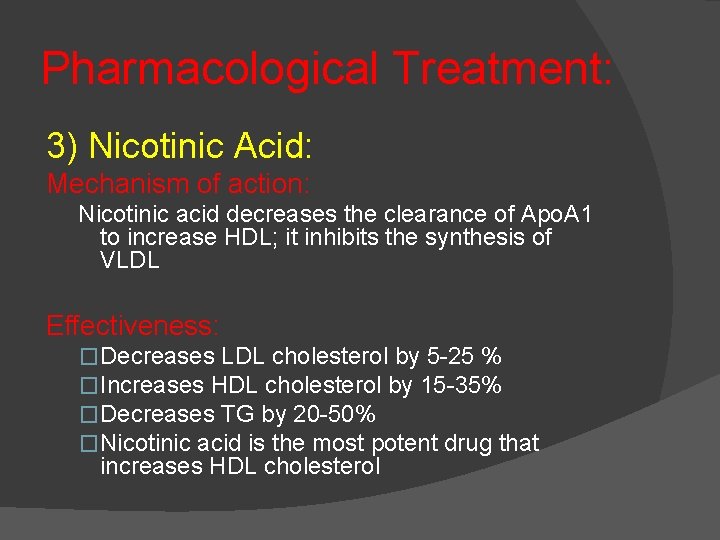
Pharmacological Treatment: 3) Nicotinic Acid: Mechanism of action: Nicotinic acid decreases the clearance of Apo. A 1 to increase HDL; it inhibits the synthesis of VLDL Effectiveness: �Decreases LDL cholesterol by 5 -25 % �Increases HDL cholesterol by 15 -35% �Decreases TG by 20 -50% �Nicotinic acid is the most potent drug that increases HDL cholesterol
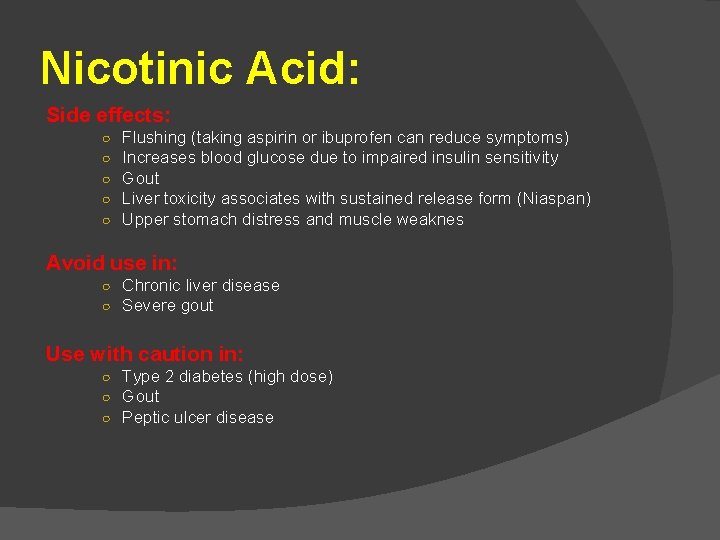
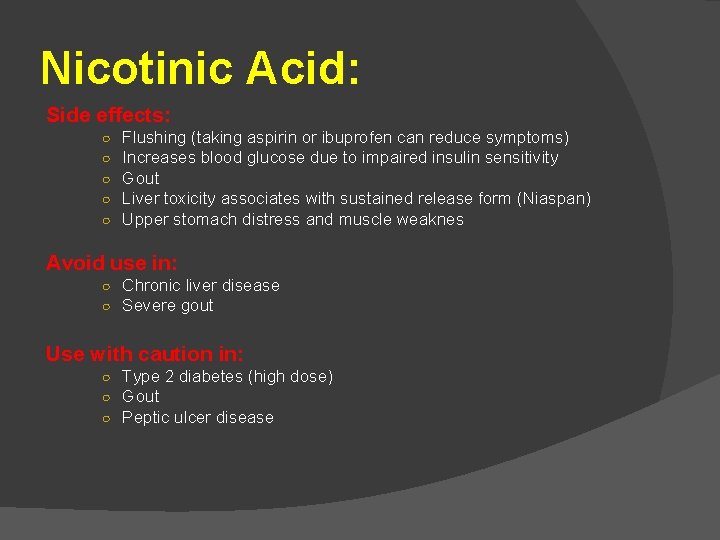
Nicotinic Acid: Side effects: ○ ○ ○ Flushing (taking aspirin or ibuprofen can reduce symptoms) Increases blood glucose due to impaired insulin sensitivity Gout Liver toxicity associates with sustained release form (Niaspan) Upper stomach distress and muscle weaknes Avoid use in: ○ Chronic liver disease ○ Severe gout Use with caution in: ○ Type 2 diabetes (high dose) ○ Gout ○ Peptic ulcer disease
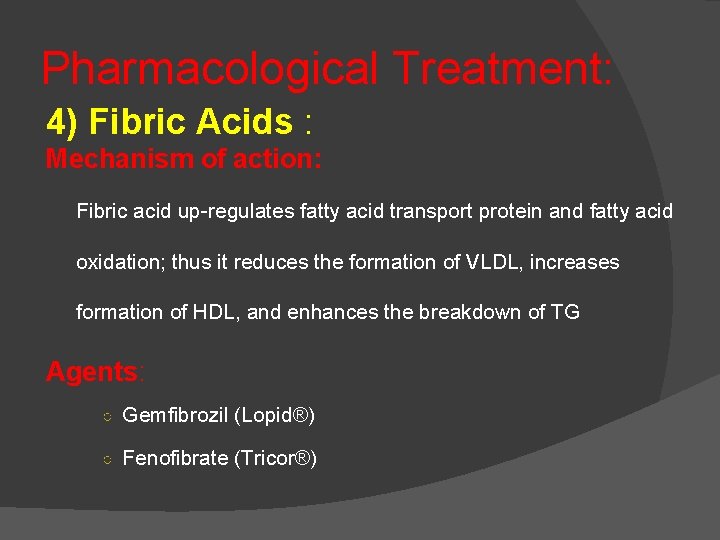
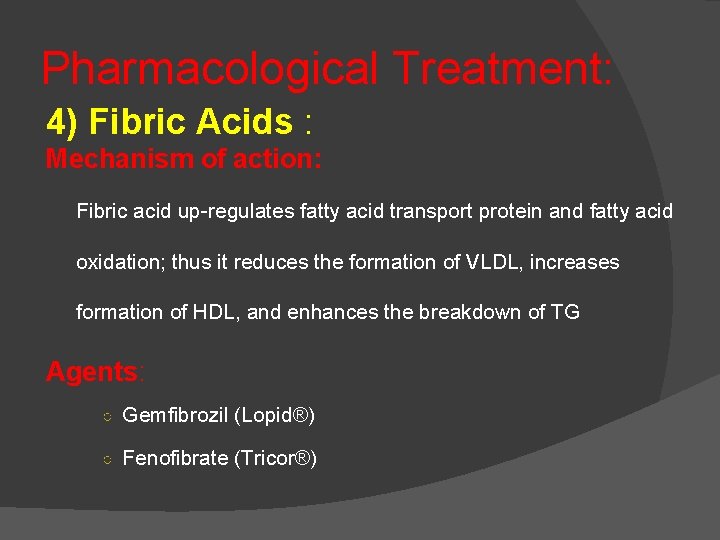
Pharmacological Treatment: 4) Fibric Acids : Mechanism of action: Fibric acid up-regulates fatty acid transport protein and fatty acid oxidation; thus it reduces the formation of VLDL, increases formation of HDL, and enhances the breakdown of TG Agents: ○ Gemfibrozil (Lopid®) ○ Fenofibrate (Tricor®)
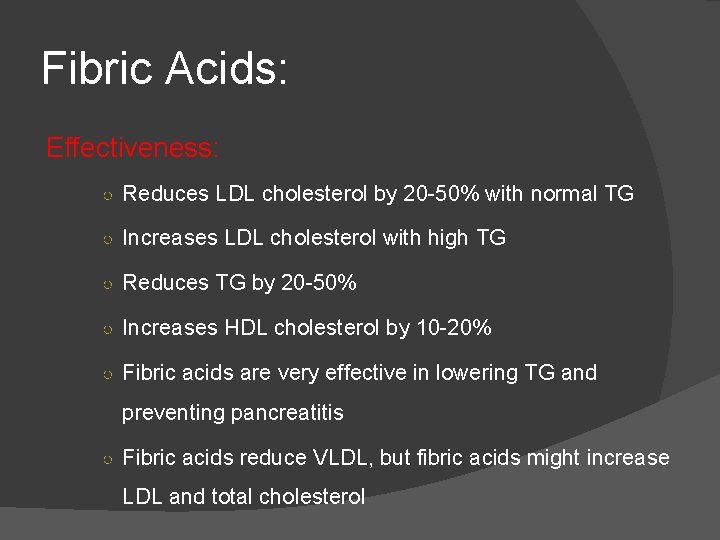
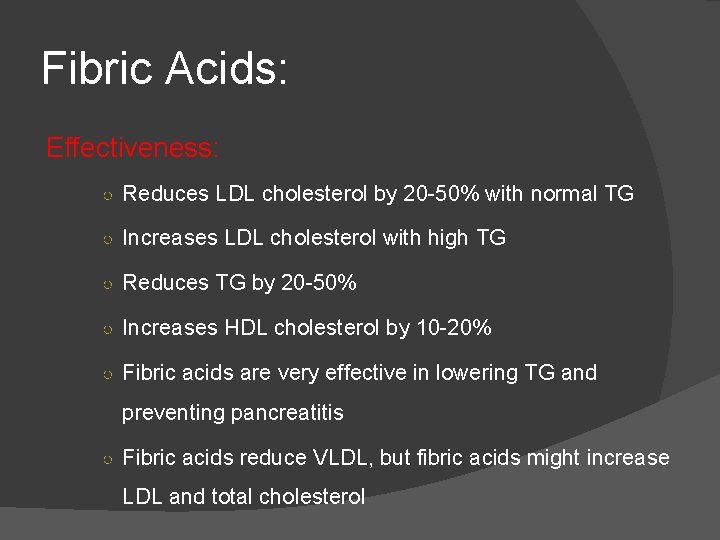
Fibric Acids: Effectiveness: ○ Reduces LDL cholesterol by 20 -50% with normal TG ○ Increases LDL cholesterol with high TG ○ Reduces TG by 20 -50% ○ Increases HDL cholesterol by 10 -20% ○ Fibric acids are very effective in lowering TG and preventing pancreatitis ○ Fibric acids reduce VLDL, but fibric acids might increase LDL and total cholesterol
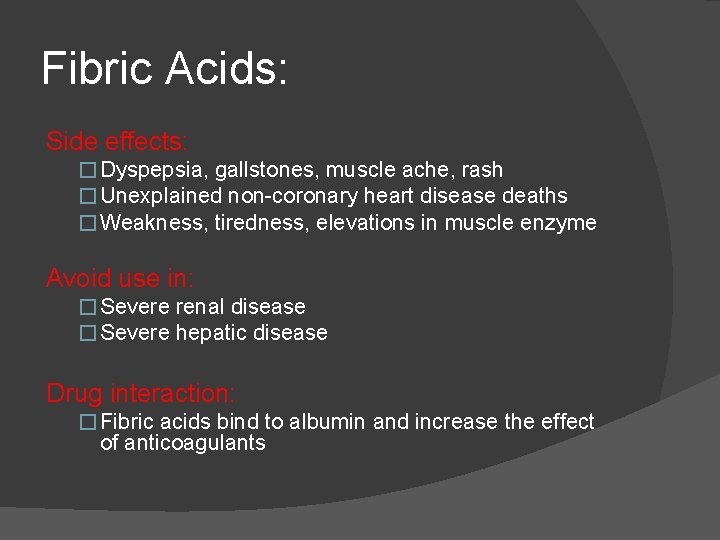
Fibric Acids: Side effects: � Dyspepsia, gallstones, muscle ache, rash � Unexplained non-coronary heart disease deaths � Weakness, tiredness, elevations in muscle enzyme Avoid use in: � Severe renal disease � Severe hepatic disease Drug interaction: � Fibric acids bind to albumin and increase the effect of anticoagulants
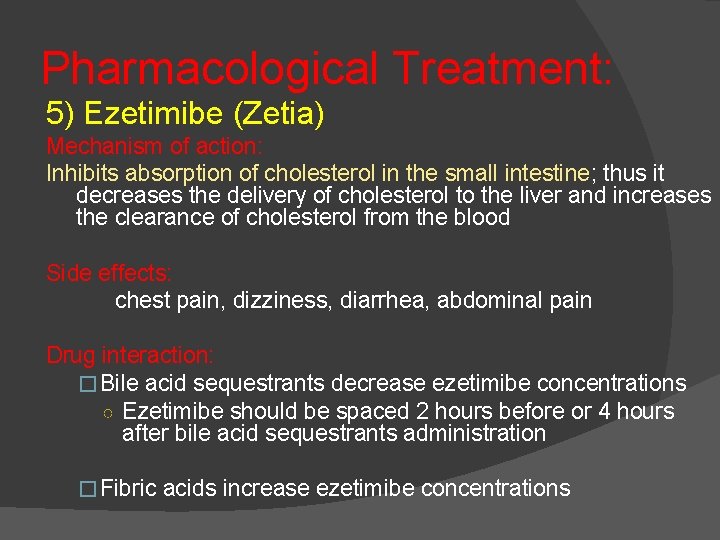
Pharmacological Treatment: 5) Ezetimibe (Zetia) Mechanism of action: Inhibits absorption of cholesterol in the small intestine; thus it decreases the delivery of cholesterol to the liver and increases the clearance of cholesterol from the blood Side effects: chest pain, dizziness, diarrhea, abdominal pain Drug interaction: �Bile acid sequestrants decrease ezetimibe concentrations ○ Ezetimibe should be spaced 2 hours before or 4 hours after bile acid sequestrants administration �Fibric acids increase ezetimibe concentrations
 Hyperlipidemia types
Hyperlipidemia types Hyperlipidemia complications
Hyperlipidemia complications Dyslipidemia cpg
Dyslipidemia cpg Dyslipidemia
Dyslipidemia Why there is hyperlipidemia in nephrotic syndrome
Why there is hyperlipidemia in nephrotic syndrome Hypertensive emergency
Hypertensive emergency Definition essay sample
Definition essay sample What is definition of terms in research example
What is definition of terms in research example Soziale wirklichkeit definition
Soziale wirklichkeit definition Thermogenese definition
Thermogenese definition Zakat meaning
Zakat meaning Career portfolio definition
Career portfolio definition Bildungsroman definition
Bildungsroman definition Tanzimat reforms definition
Tanzimat reforms definition Coconut shy definition
Coconut shy definition Internal conflict define
Internal conflict define Jonathan edwards apush definition
Jonathan edwards apush definition Apushreview.com
Apushreview.com Mini saga on time
Mini saga on time Narrative essay mean
Narrative essay mean Leq rubric whap
Leq rubric whap Expository paragraphs
Expository paragraphs Sensory detail definition
Sensory detail definition Objective summary verbs
Objective summary verbs Which is an objective summary of this part of the story
Which is an objective summary of this part of the story Definition of summary writing
Definition of summary writing