Septic Arthritis Saran Promwangkhwa M D Orthopedics Pua








- Slides: 47
Septic Arthritis Saran Promwangkhwa, M. D. Orthopedics Pua Hospital, Nan
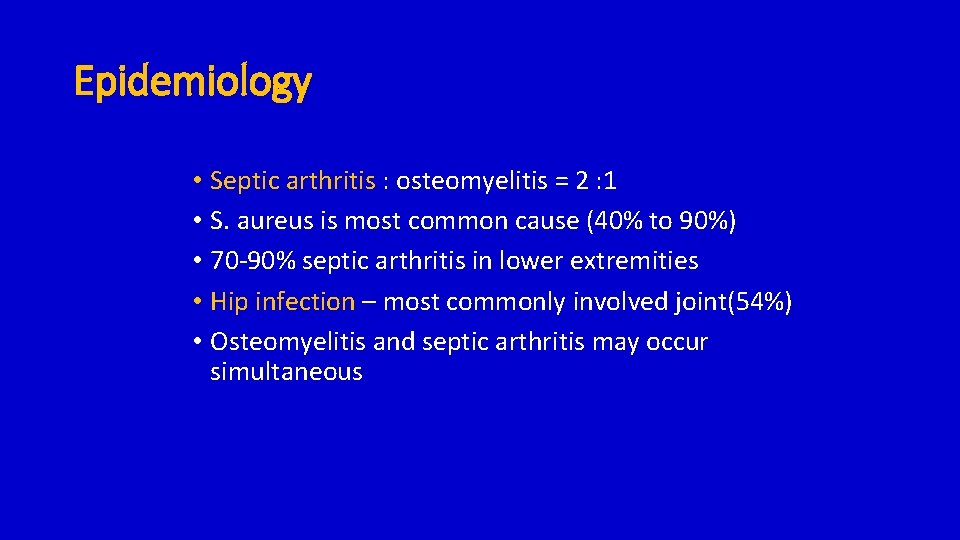
Epidemiology • Septic arthritis : osteomyelitis = 2 : 1 • S. aureus is most common cause (40% to 90%) • 70 -90% septic arthritis in lower extremities • Hip infection – most commonly involved joint(54%) • Osteomyelitis and septic arthritis may occur simultaneous
Common organism • Neonate • Group B strep, gonococci, S. aureus, coliform bacteria (gram negative) • Unimmunized infants younger than 2 yrs • H. influenzae, group A strep, K kingae, S. aureus • Immunized infants and older children • S. aureus , pneumococcus, group A strep
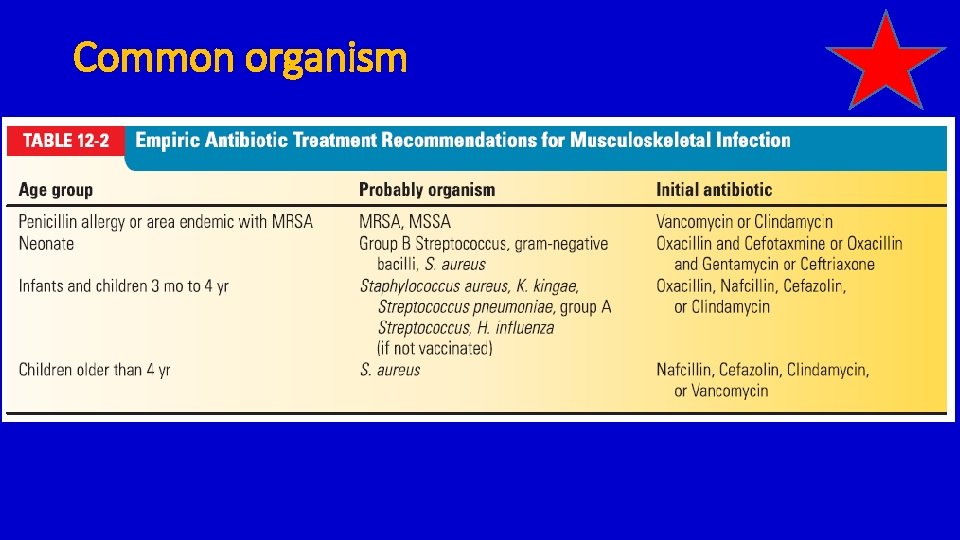
Common organism

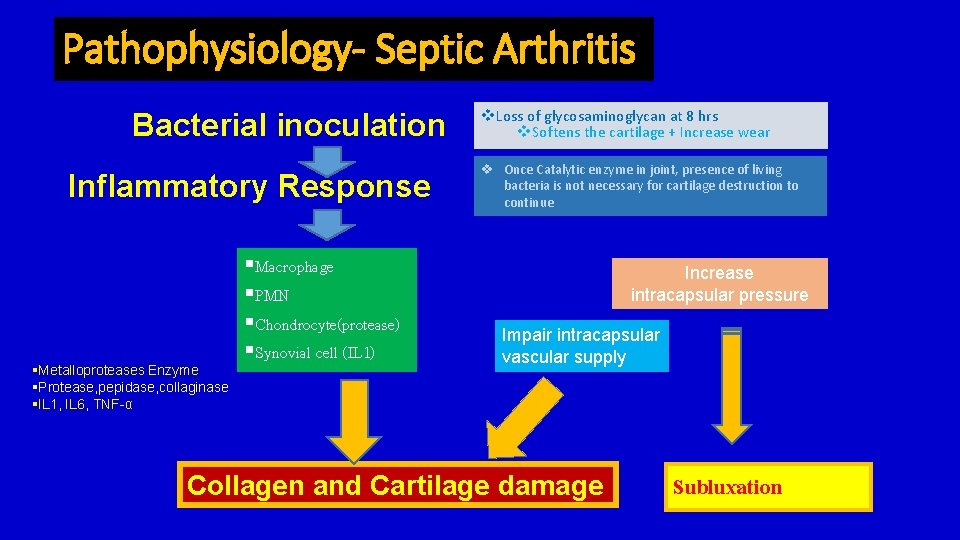
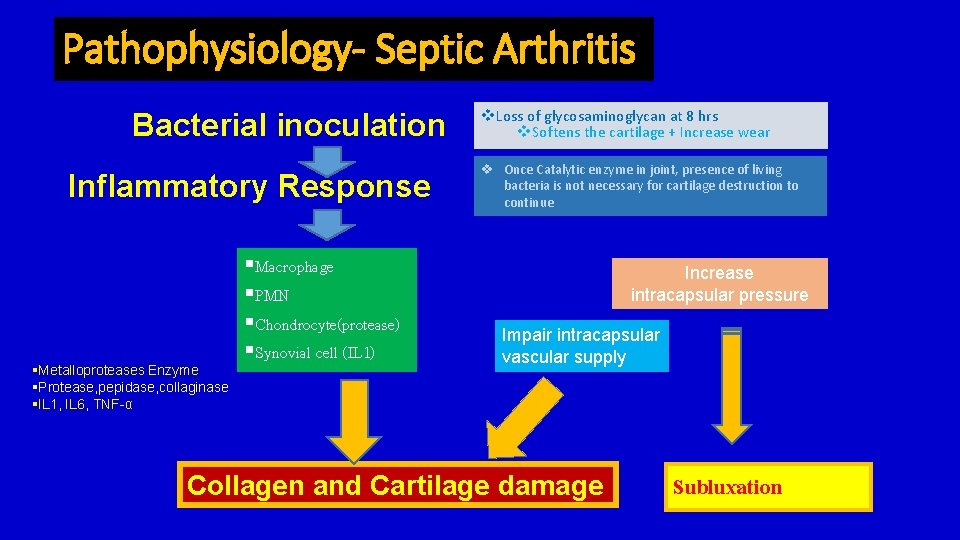
Pathophysiology- Septic Arthritis Bacterial inoculation Inflammatory Response §Metalloproteases Enzyme §Protease, pepidase, collaginase §IL 1, IL 6, TNF-α §Macrophage §PMN §Chondrocyte(protease) §Synovial cell (IL 1) v. Loss of glycosaminoglycan at 8 hrs v. Softens the cartilage + Increase wear v Once Catalytic enzyme in joint, presence of living bacteria is not necessary for cartilage destruction to continue Increase intracapsular pressure Impair intracapsular vascular supply Collagen and Cartilage damage Subluxation
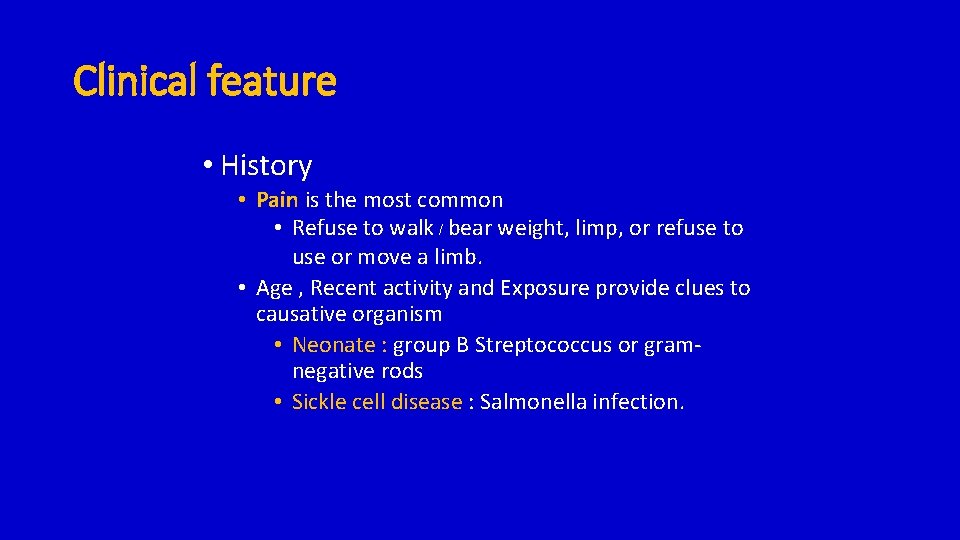
Clinical feature • History • Pain is the most common • Refuse to walk / bear weight, limp, or refuse to use or move a limb. • Age , Recent activity and Exposure provide clues to causative organism • Neonate : group B Streptococcus or gramnegative rods • Sickle cell disease : Salmonella infection.
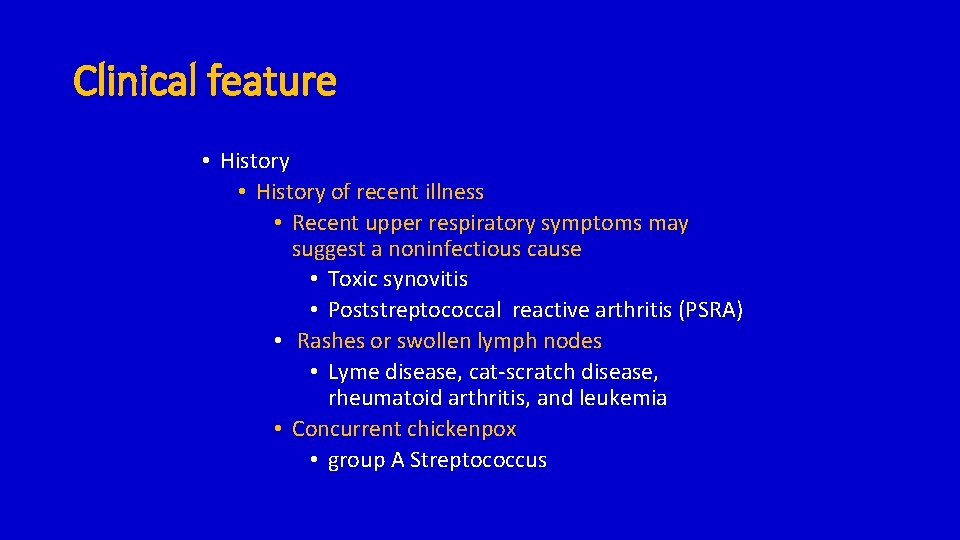
Clinical feature • History of recent illness • Recent upper respiratory symptoms may suggest a noninfectious cause • Toxic synovitis • Poststreptococcal reactive arthritis (PSRA) • Rashes or swollen lymph nodes • Lyme disease, cat-scratch disease, rheumatoid arthritis, and leukemia • Concurrent chickenpox • group A Streptococcus
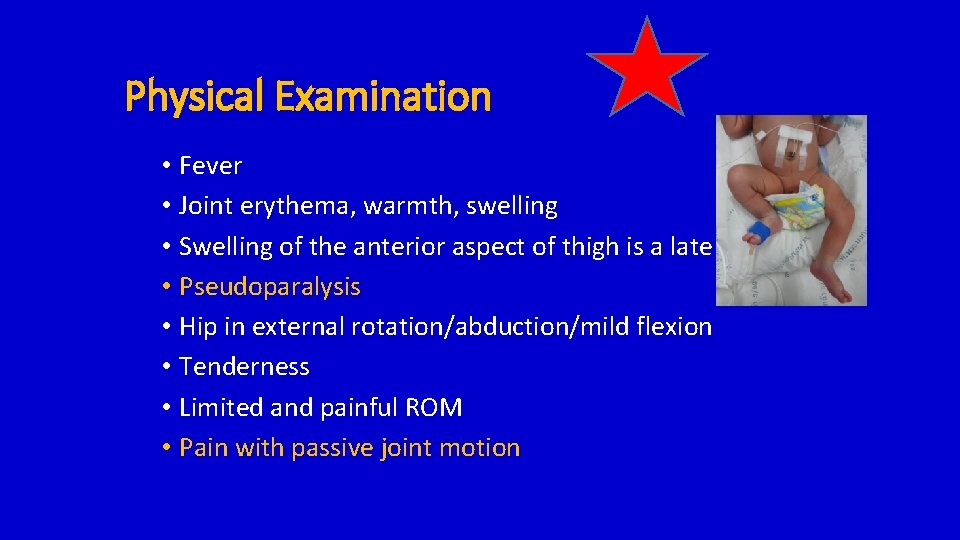
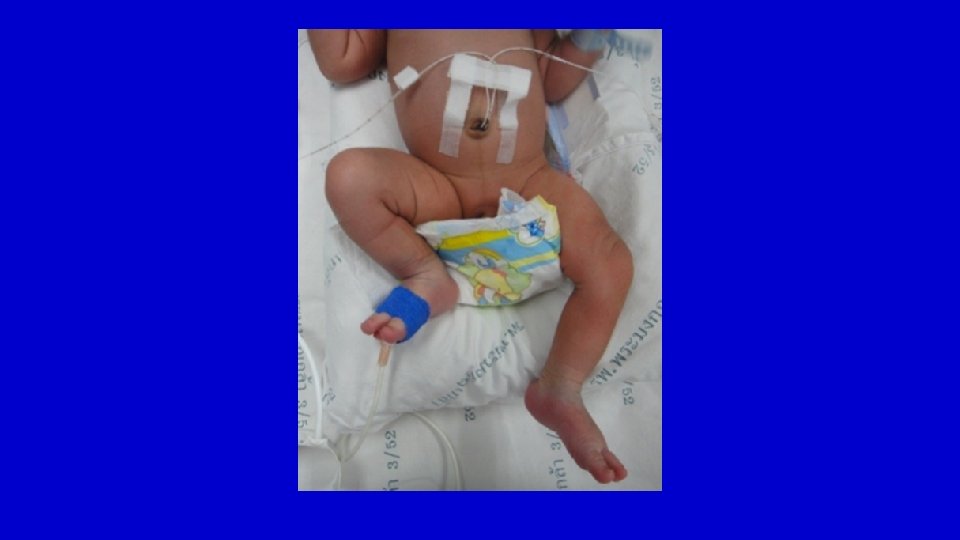
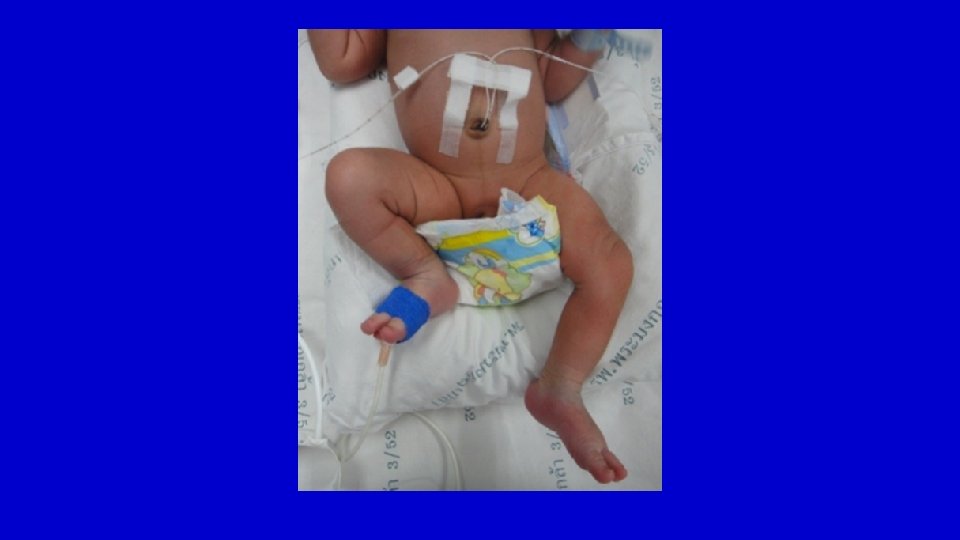
Physical Examination • Fever • Joint erythema, warmth, swelling • Swelling of the anterior aspect of thigh is a late sign • Pseudoparalysis • Hip in external rotation/abduction/mild flexion • Tenderness • Limited and painful ROM • Pain with passive joint motion

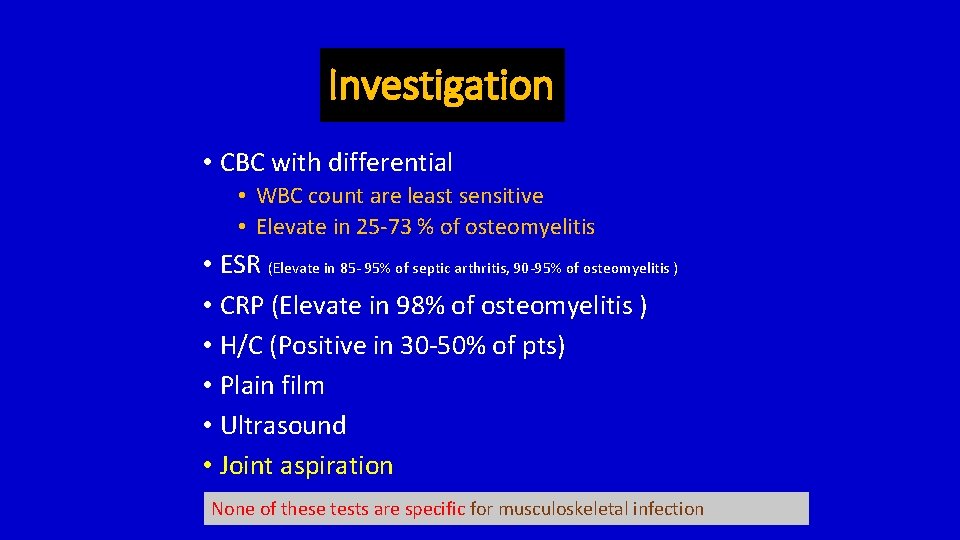
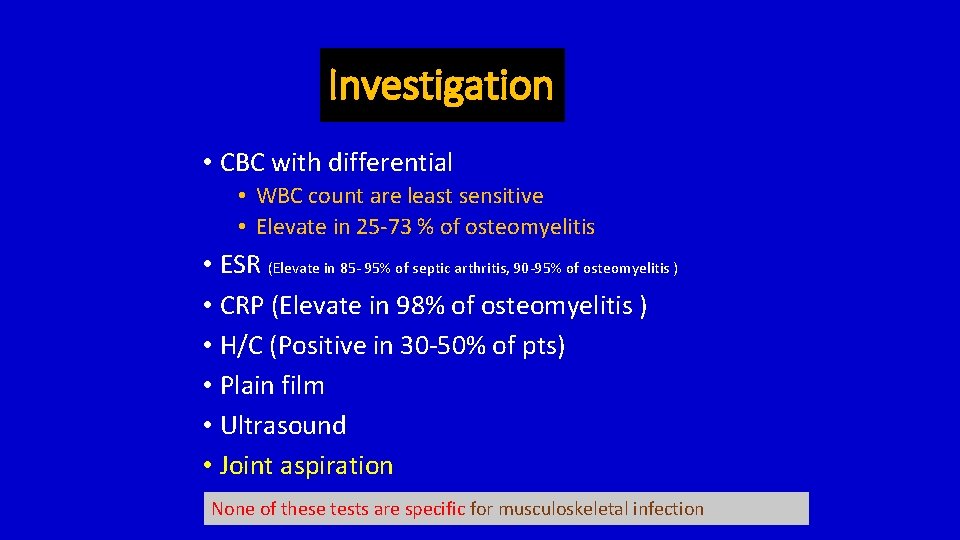
Investigation • CBC with differential • WBC count are least sensitive • Elevate in 25 -73 % of osteomyelitis • ESR (Elevate in 85 - 95% of septic arthritis, 90 -95% of osteomyelitis ) • CRP (Elevate in 98% of osteomyelitis ) • H/C (Positive in 30 -50% of pts) • Plain film • Ultrasound • Joint aspiration None of these tests are specific for musculoskeletal infection
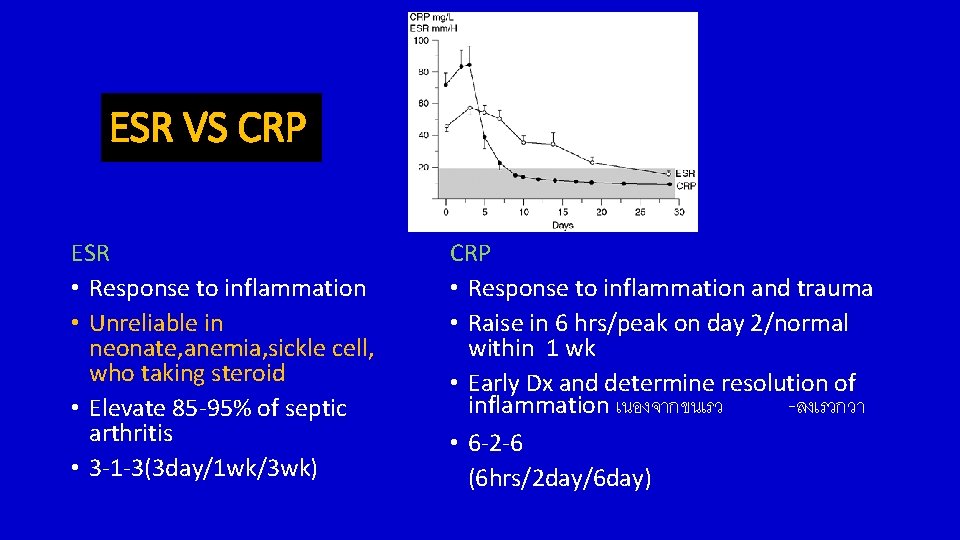
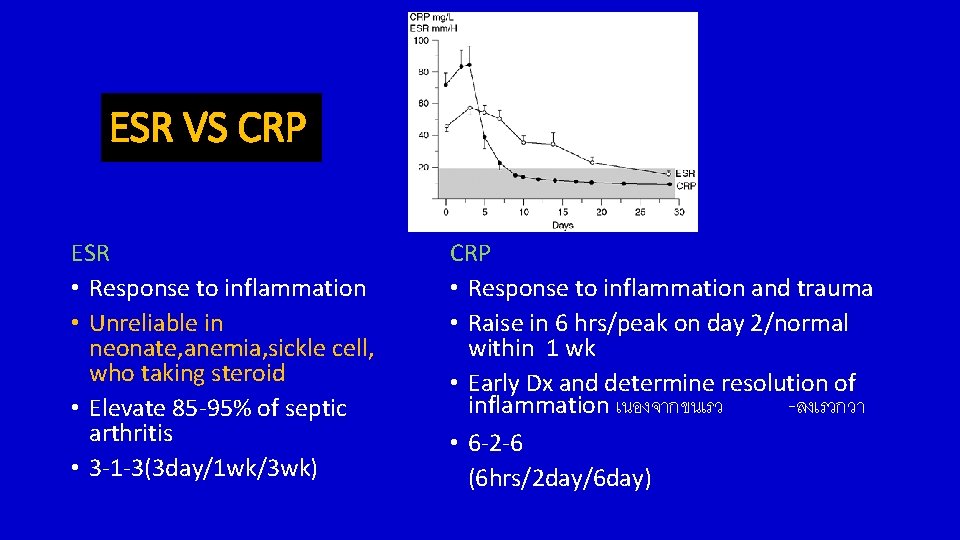
ESR VS CRP ESR • Response to inflammation • Unreliable in neonate, anemia, sickle cell, who taking steroid • Elevate 85 -95% of septic arthritis • 3 -1 -3(3 day/1 wk/3 wk) CRP • Response to inflammation and trauma • Raise in 6 hrs/peak on day 2/normal within 1 wk • Early Dx and determine resolution of inflammation เนองจากขนเรว -ลงเรวกวา • 6 -2 -6 (6 hrs/2 day/6 day)
Imaging • Plain radiograph • Bone scan • Ultrasonography • CT Scan • MRI
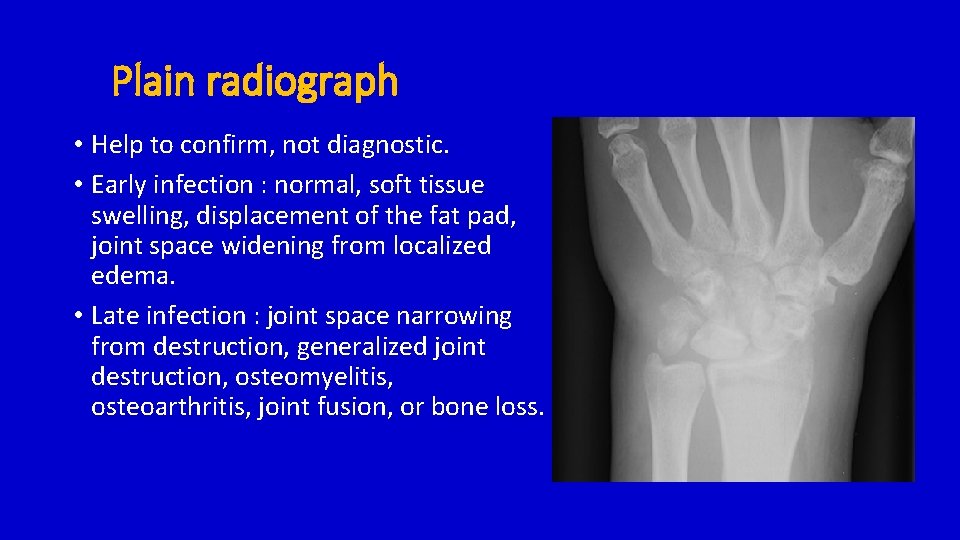
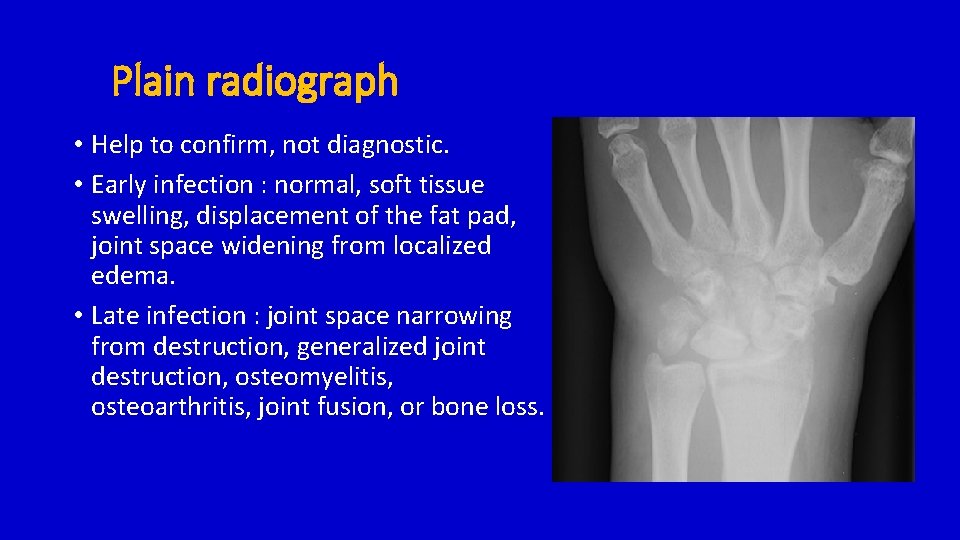
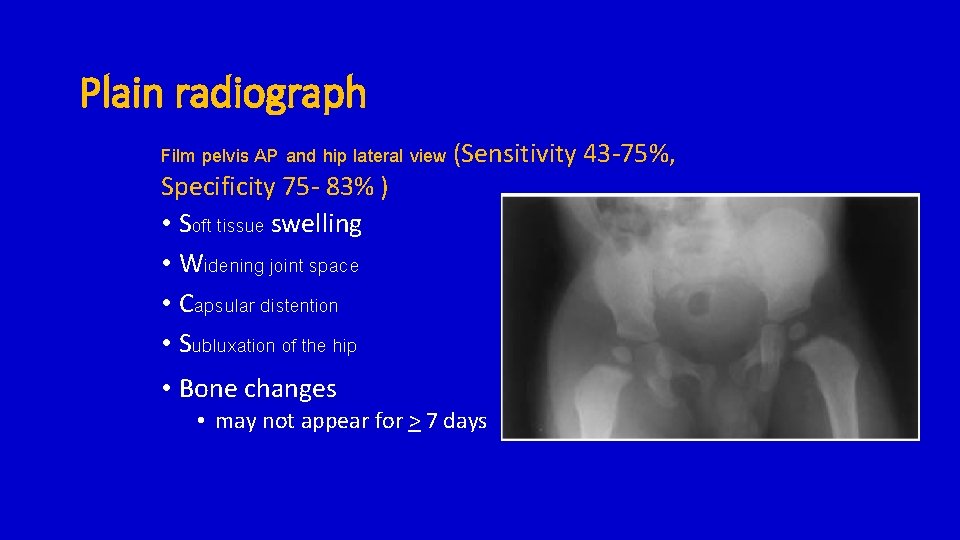
Plain radiograph • Help to confirm, not diagnostic. • Early infection : normal, soft tissue swelling, displacement of the fat pad, joint space widening from localized edema. • Late infection : joint space narrowing from destruction, generalized joint destruction, osteomyelitis, osteoarthritis, joint fusion, or bone loss.
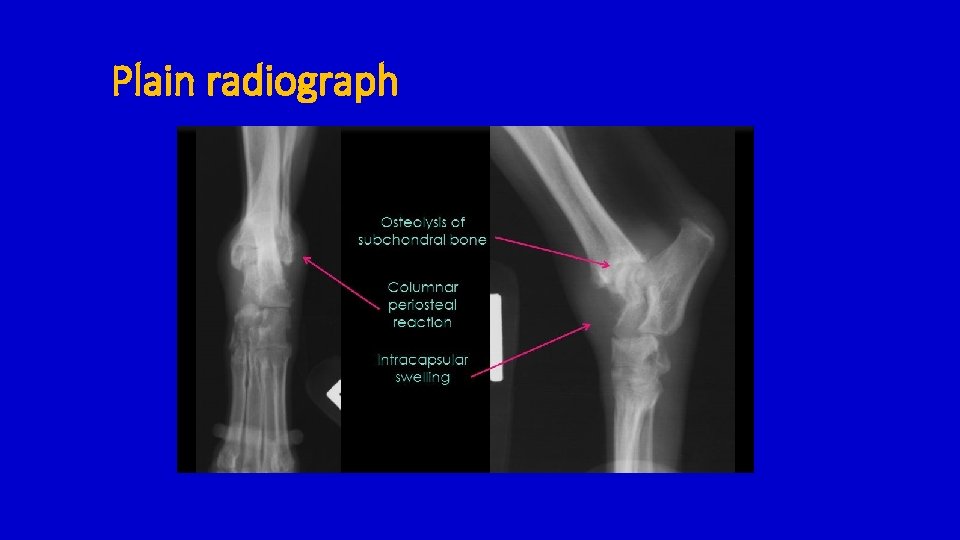
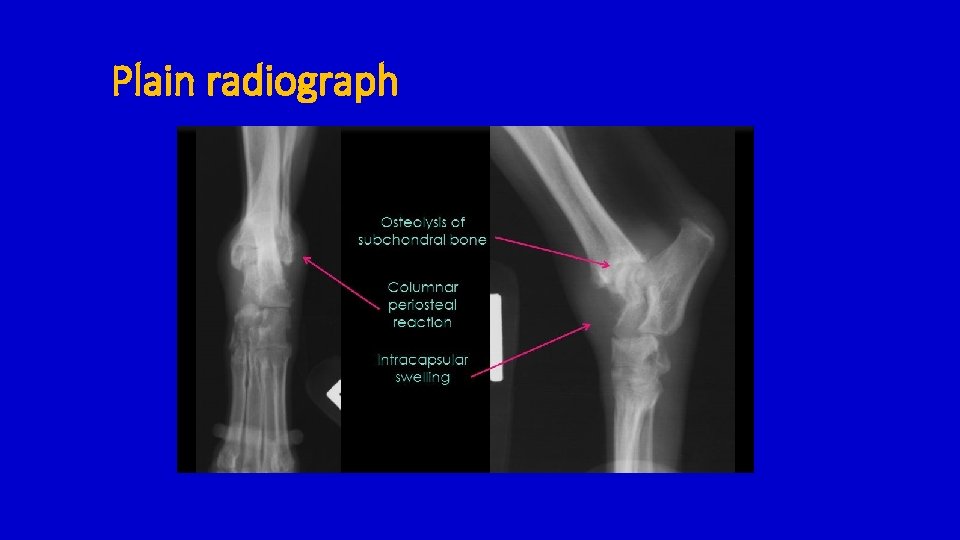
Plain radiograph
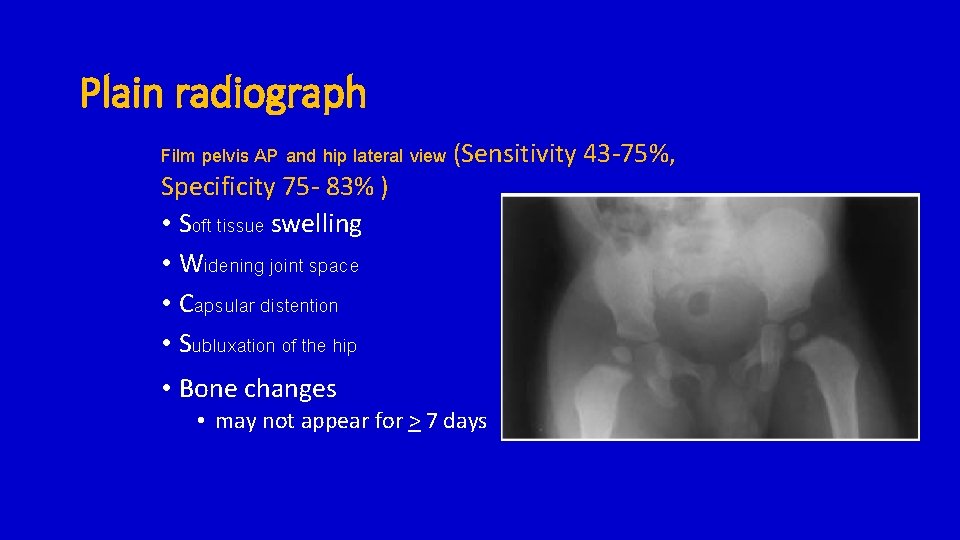
Plain radiograph Film pelvis AP and hip lateral view (Sensitivity 43 -75%, Specificity 75 - 83% ) • Soft tissue swelling • Widening joint space • Capsular distention • Subluxation of the hip • Bone changes • may not appear for > 7 days
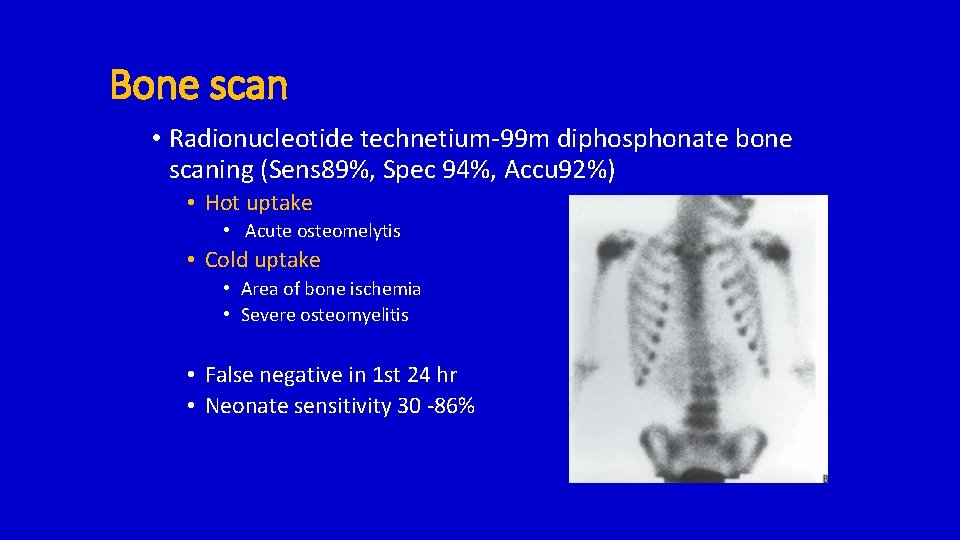
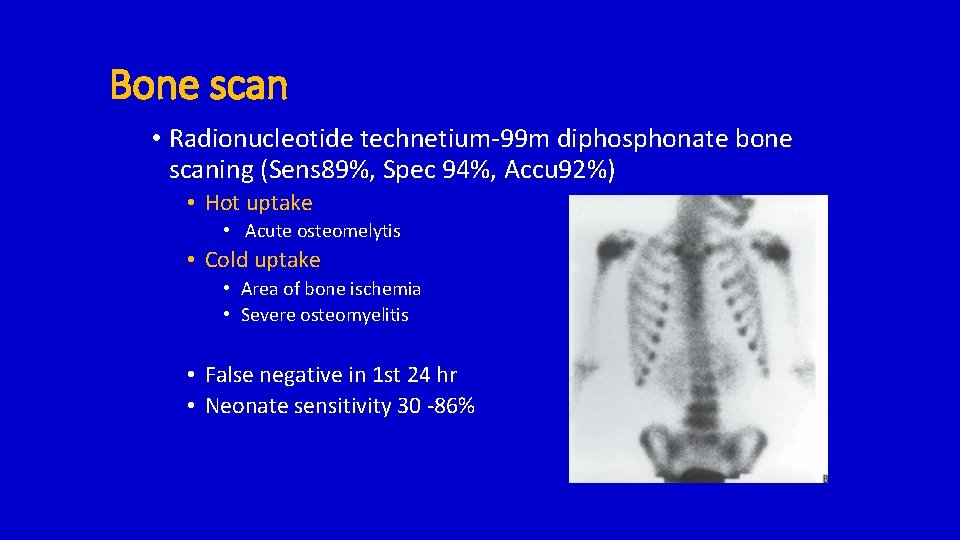
Bone scan • Radionucleotide technetium-99 m diphosphonate bone scaning (Sens 89%, Spec 94%, Accu 92%) • Hot uptake • Acute osteomelytis • Cold uptake • Area of bone ischemia • Severe osteomyelitis • False negative in 1 st 24 hr • Neonate sensitivity 30 -86%
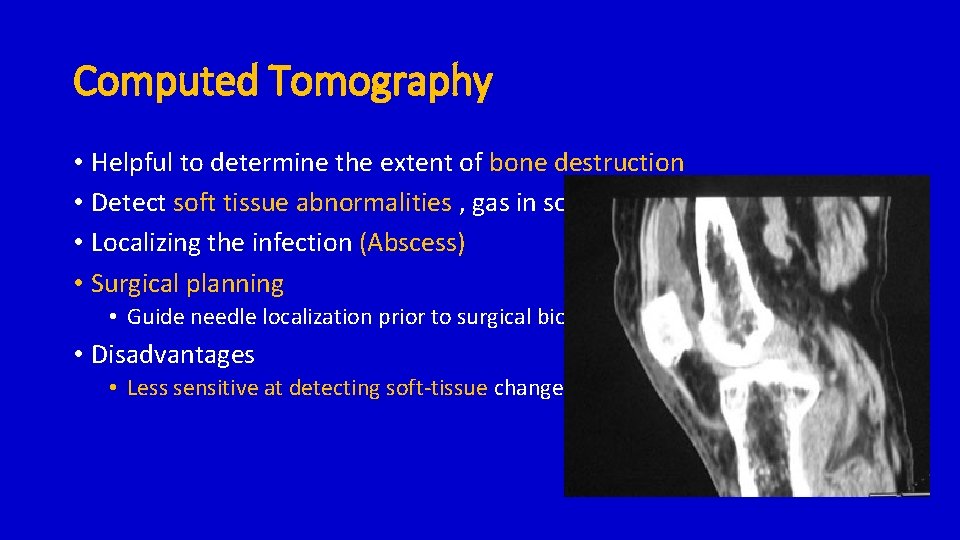
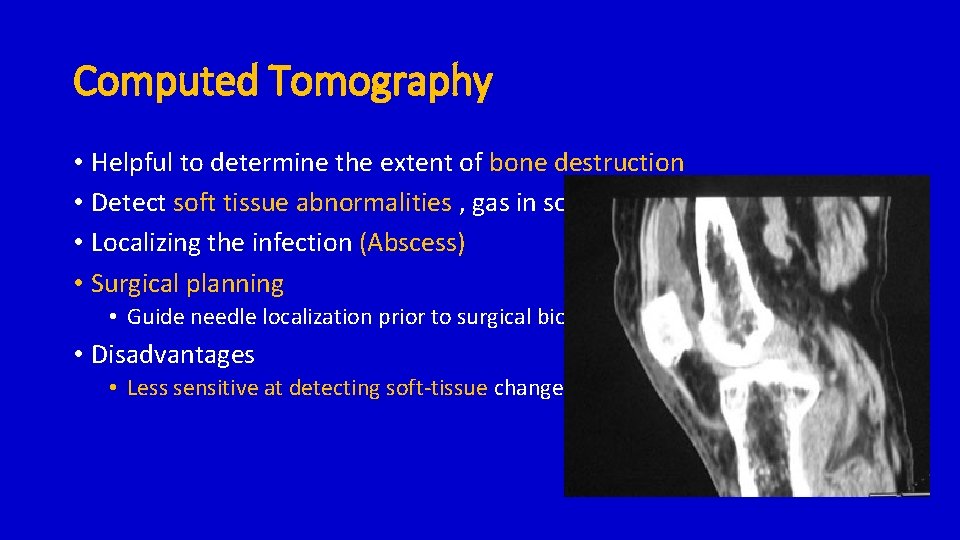
Computed Tomography • Helpful to determine the extent of bone destruction • Detect soft tissue abnormalities , gas in soft tissues • Localizing the infection (Abscess) • Surgical planning • Guide needle localization prior to surgical biopsy or debridement • Disadvantages • Less sensitive at detecting soft-tissue changes.
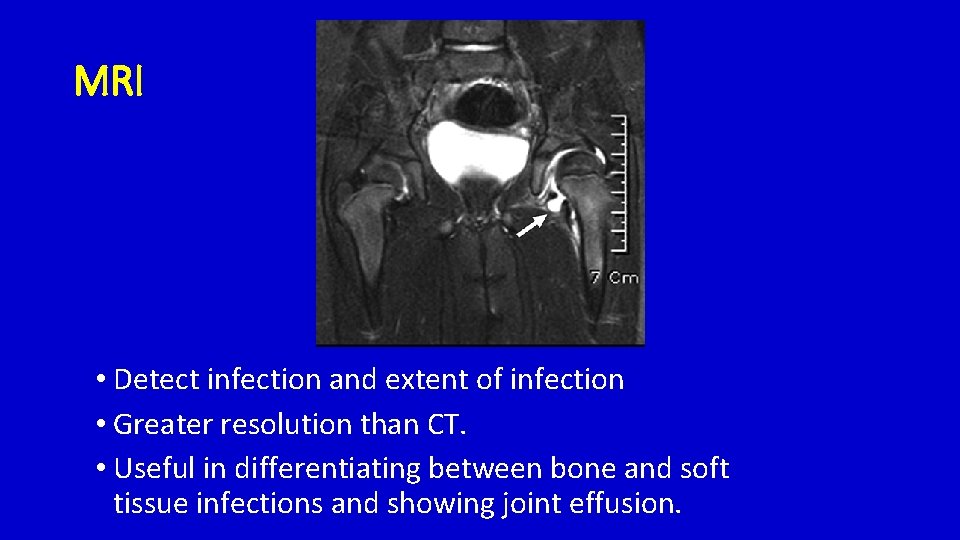
Magnetic Resonance Imaging ( MRI ) • Sensitivity 88% - 100%, specificity 75% - 100%, PPV 85% • Helpful when differentiating between osteomyelitis and primary bone malignancy Marrow involvement • MRI findings of osteomyelitis – Low T 1, High T 2 • Gadolinium – R/O neoplasm, fracture, or bone infarct • Disadvantages • Cost • Necessity for sedation
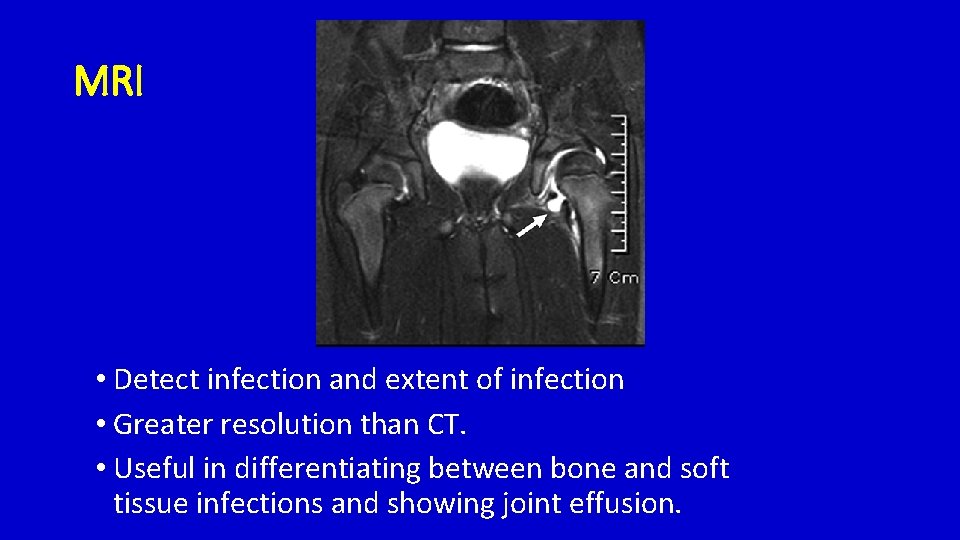
MRI • Detect infection and extent of infection • Greater resolution than CT. • Useful in differentiating between bone and soft tissue infections and showing joint effusion.

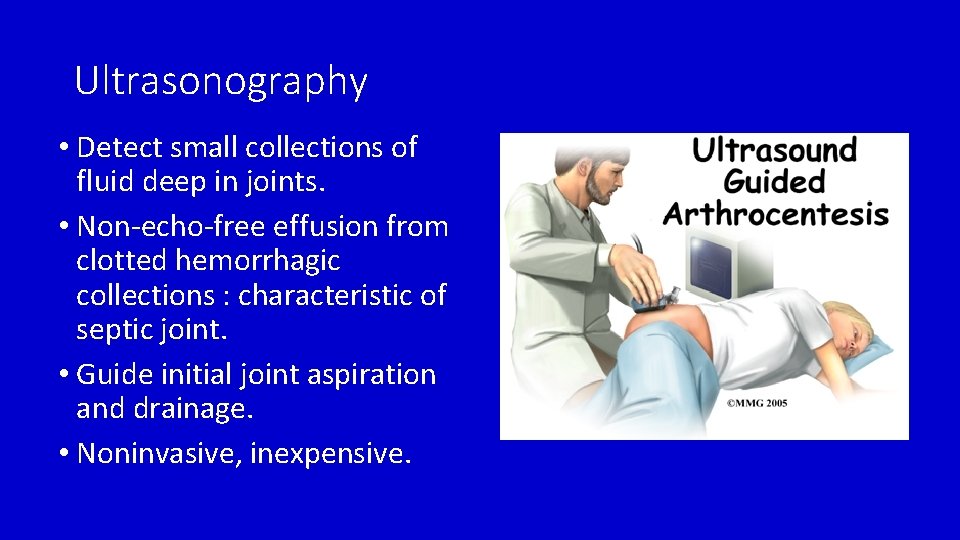
Ultrasonography • low cost , noninvasive, nonradiation, lack of need for sedation • PPV 87. 9% of septic arthritis • Septic arthritis : • Presence of intraarticular effusion • Capsule to bone distance > 2 mm • High sensitivity and low specificity
Ultrasonography
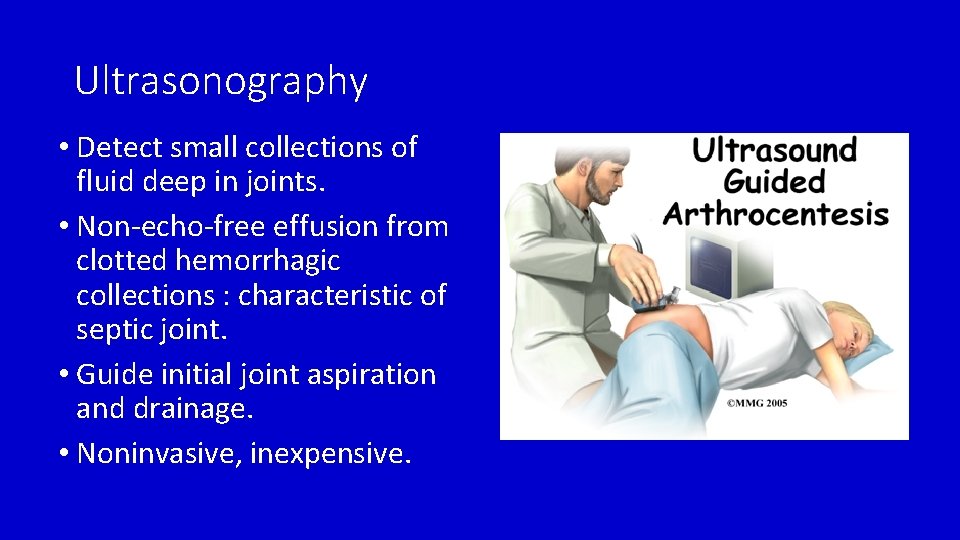
Ultrasonography • Detect small collections of fluid deep in joints. • Non-echo-free effusion from clotted hemorrhagic collections : characteristic of septic joint. • Guide initial joint aspiration and drainage. • Noninvasive, inexpensive.
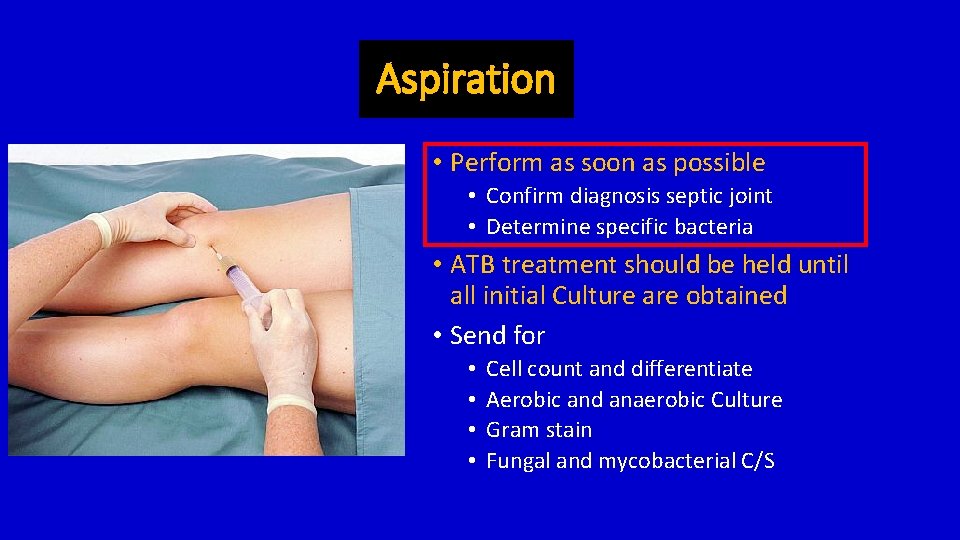
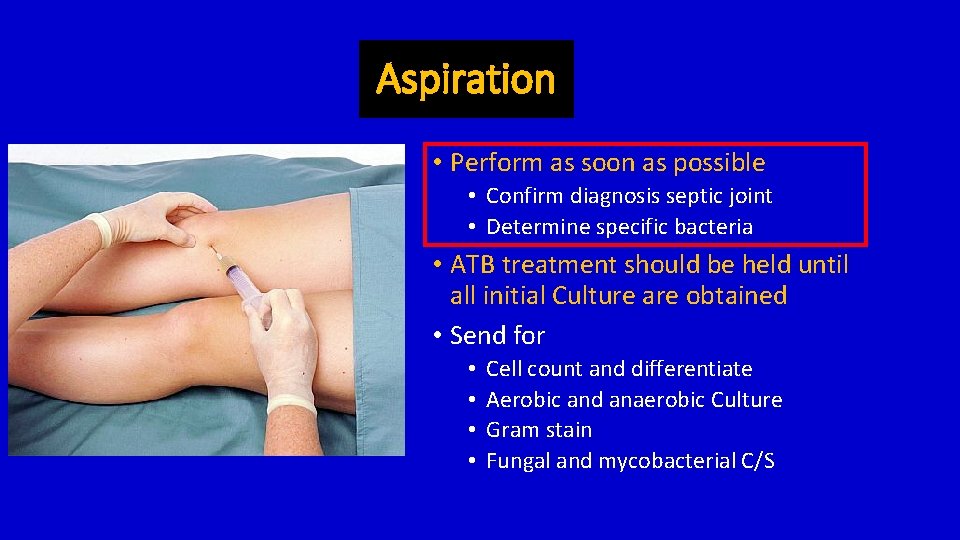
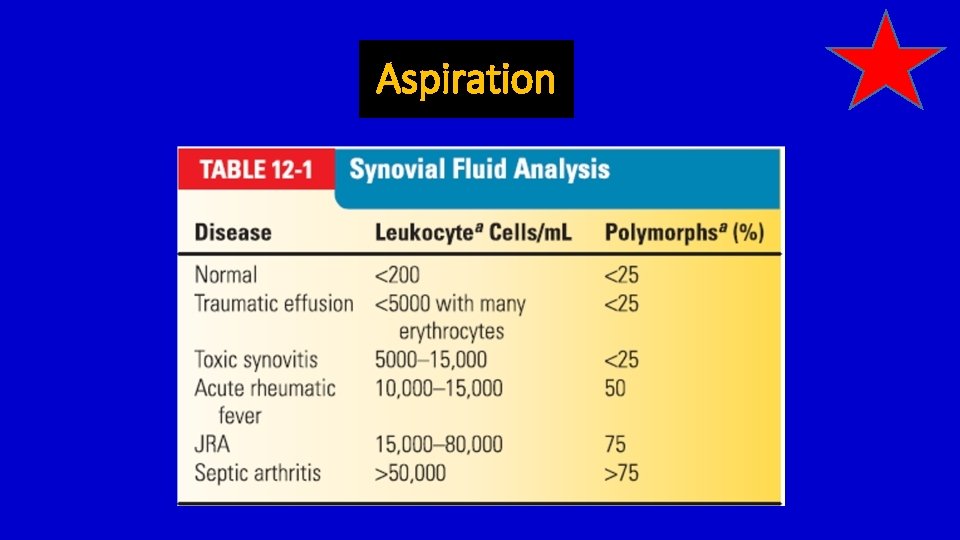
Aspiration • Perform as soon as possible • Confirm diagnosis septic joint • Determine specific bacteria • ATB treatment should be held until all initial Culture are obtained • Send for • • Cell count and differentiate Aerobic and anaerobic Culture Gram stain Fungal and mycobacterial C/S
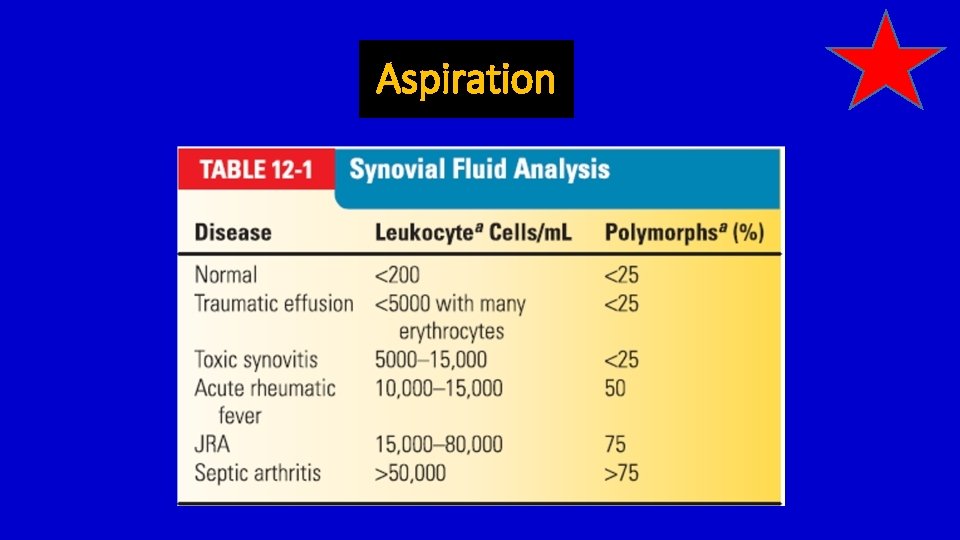
Aspiration
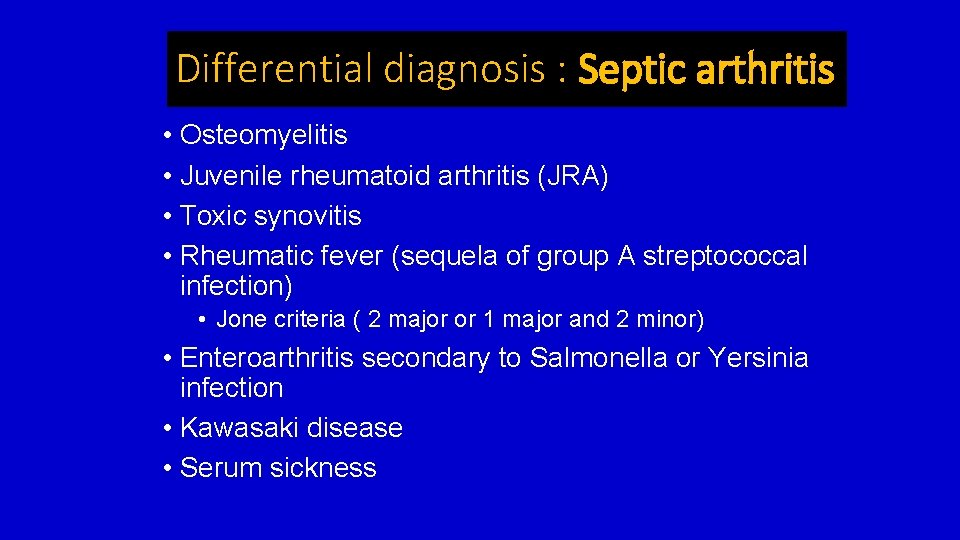
Differential diagnosis : Septic arthritis • Osteomyelitis • Juvenile rheumatoid arthritis (JRA) • Toxic synovitis • Rheumatic fever (sequela of group A streptococcal infection) • Jone criteria ( 2 major or 1 major and 2 minor) • Enteroarthritis secondary to Salmonella or Yersinia infection • Kawasaki disease • Serum sickness

Treatment septic arthritis
Principle of treatment • Adequate surgical drainage • Empiric intravenous antimicrobial therapy • Joint must be rested
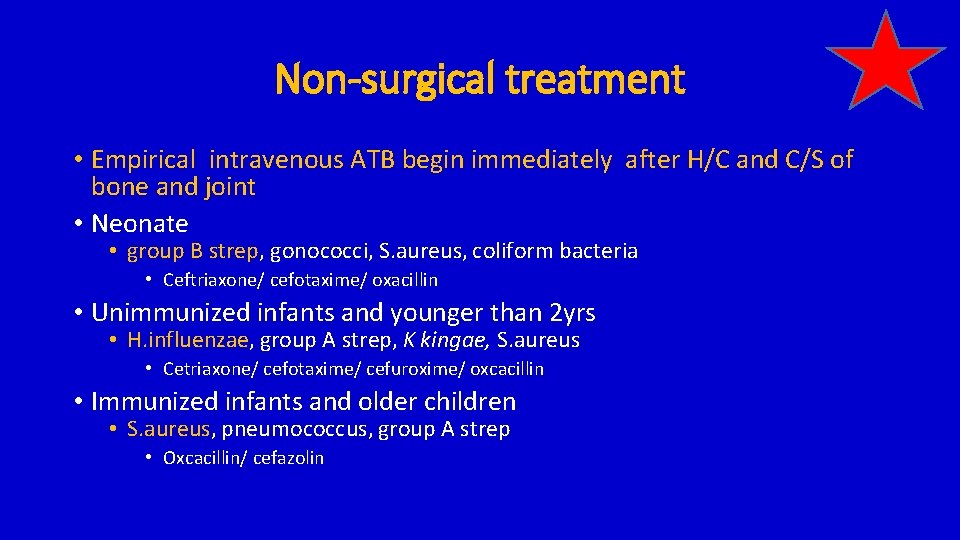
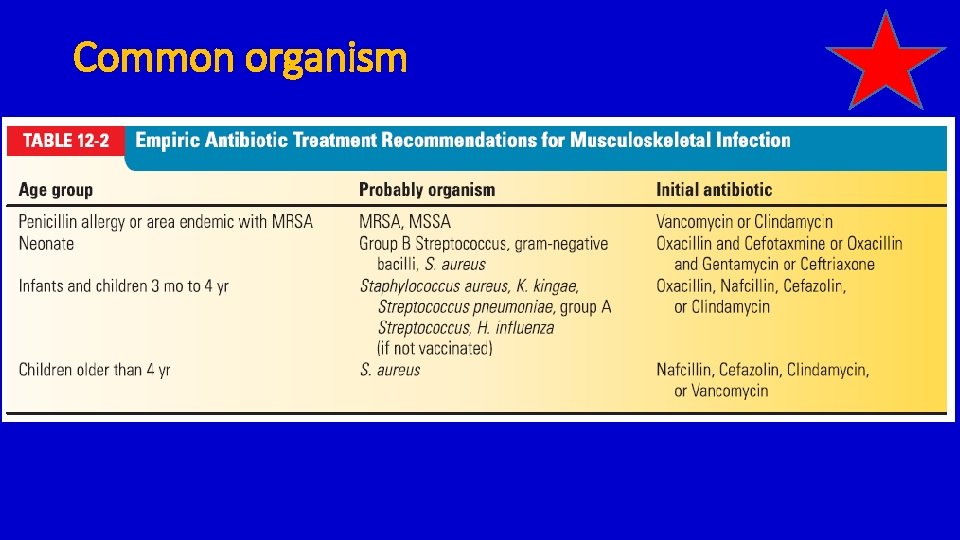
Non-surgical treatment • Empirical intravenous ATB begin immediately after H/C and C/S of bone and joint • Neonate • group B strep, gonococci, S. aureus, coliform bacteria • Ceftriaxone/ cefotaxime/ oxacillin • Unimmunized infants and younger than 2 yrs • H. influenzae, group A strep, K kingae, S. aureus • Cetriaxone/ cefotaxime/ cefuroxime/ oxcacillin • Immunized infants and older children • S. aureus, pneumococcus, group A strep • Oxcacillin/ cefazolin

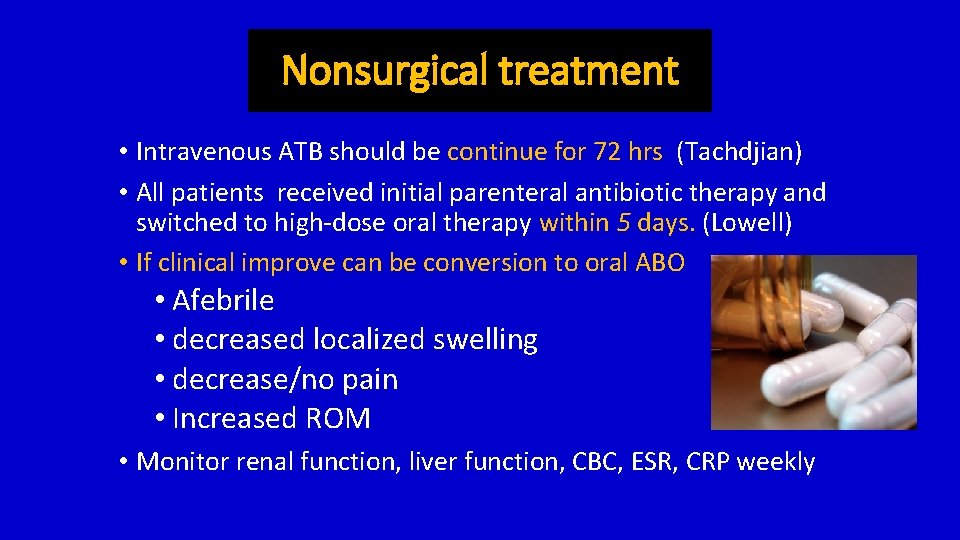
Nonsurgical treatment • Intravenous ATB should be continue for 72 hrs (Tachdjian) • All patients received initial parenteral antibiotic therapy and switched to high-dose oral therapy within 5 days. (Lowell) • If clinical improve can be conversion to oral ABO • Afebrile • decreased localized swelling • decrease/no pain • Increased ROM • Monitor renal function, liver function, CBC, ESR, CRP weekly
Surgical treatment • Surgery is indicated for • Culture and biopsy • Evacuation and elimination of bone or joint abscess • Stopping tissue destruction. • Neisseria gonorrhoeae And Tubercolous may not required Surgical drainage
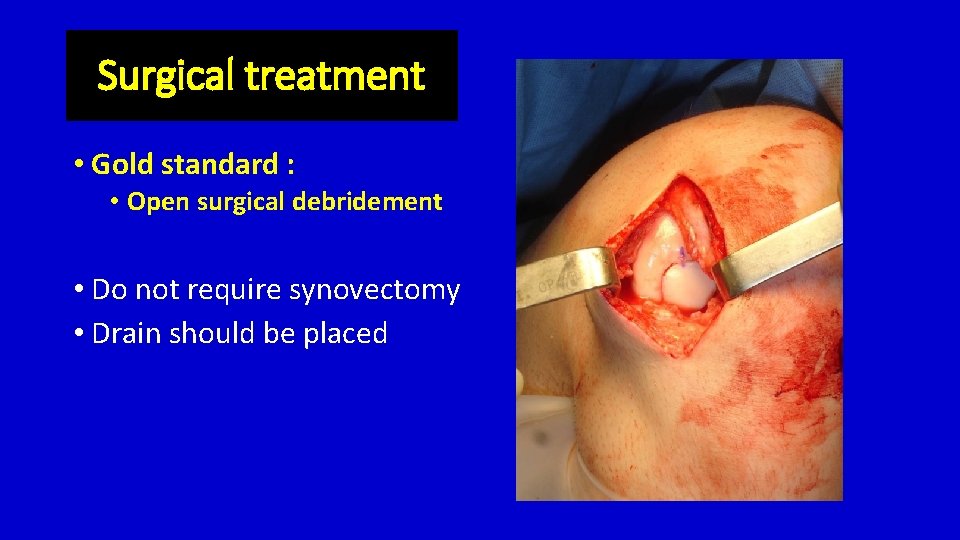
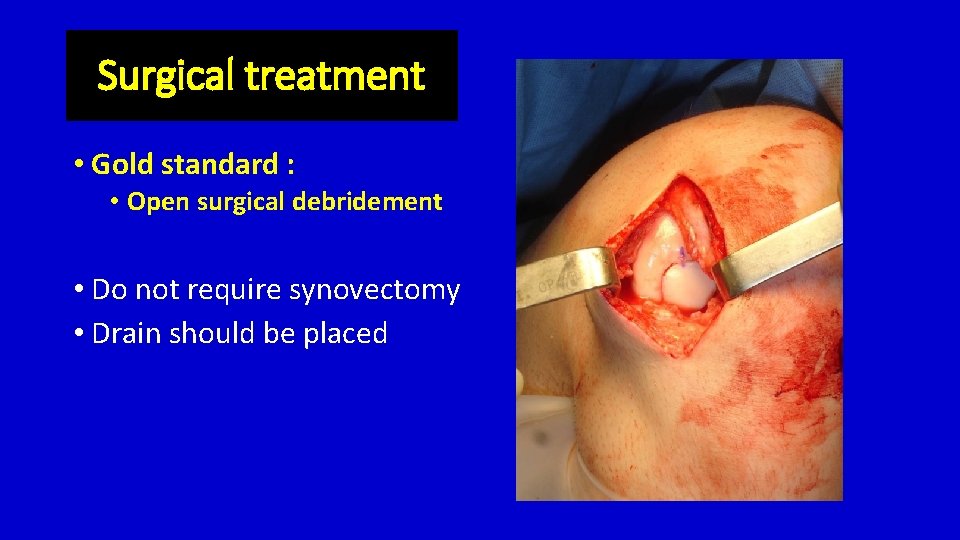
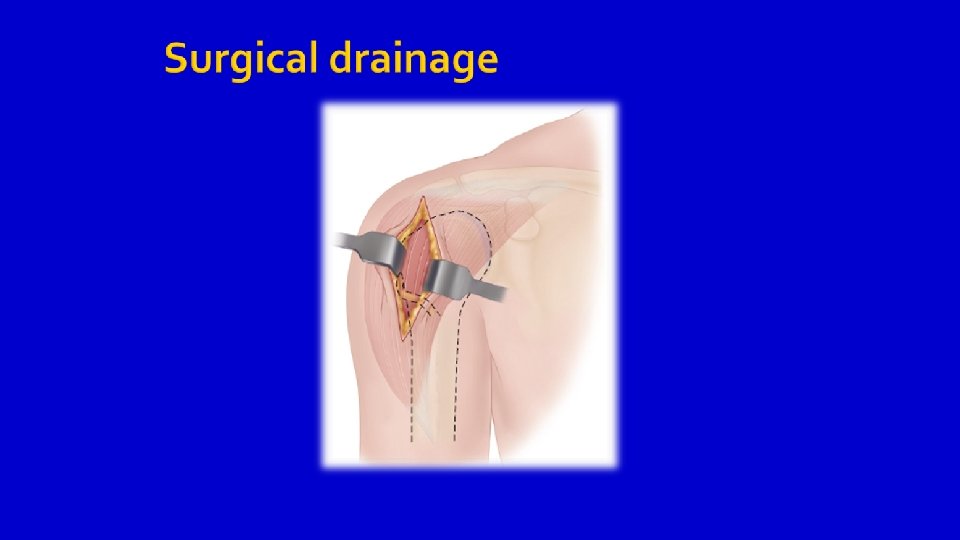
Surgical treatment • Gold standard : • Open surgical debridement • Do not require synovectomy • Drain should be placed

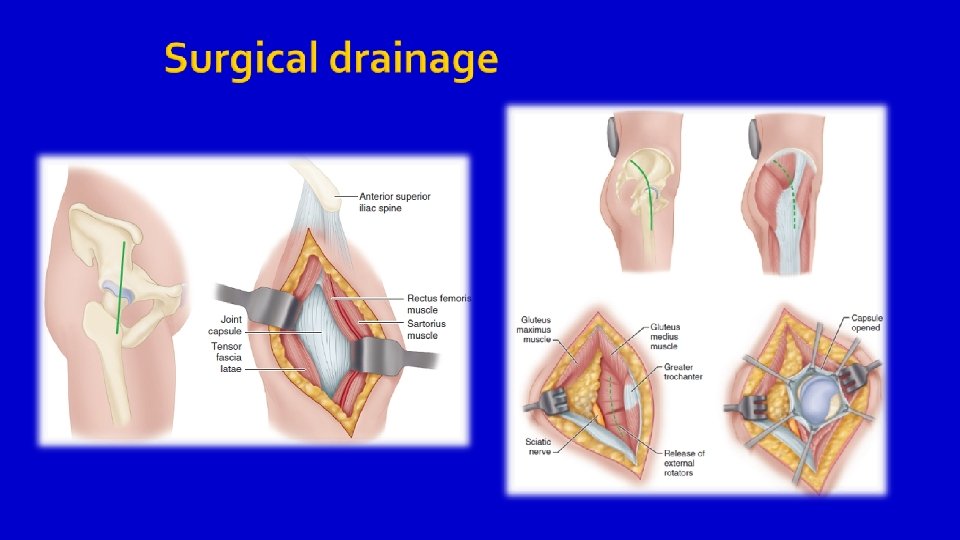
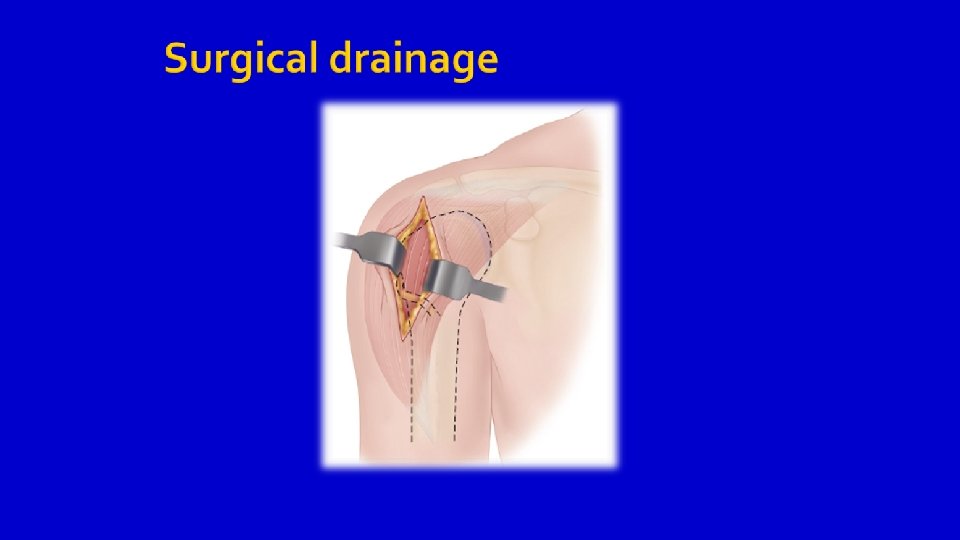

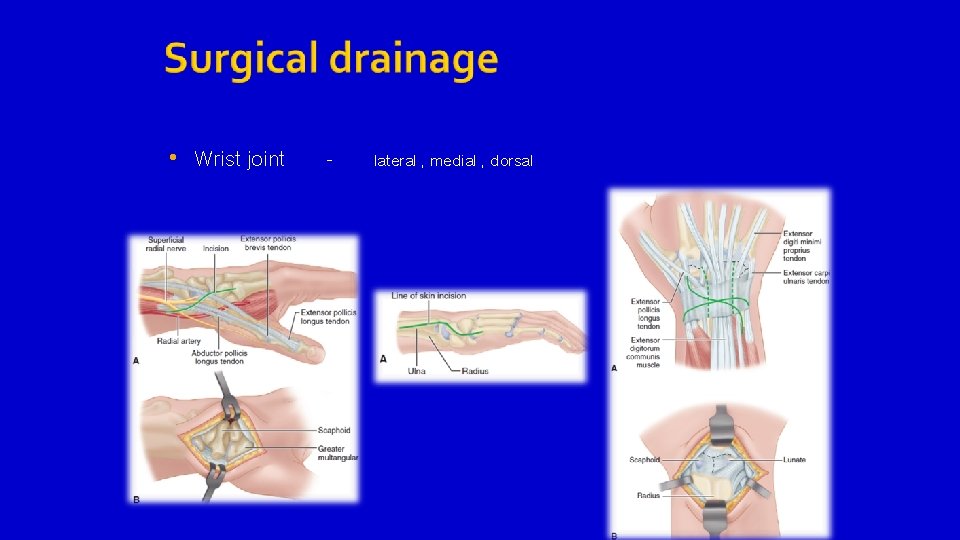
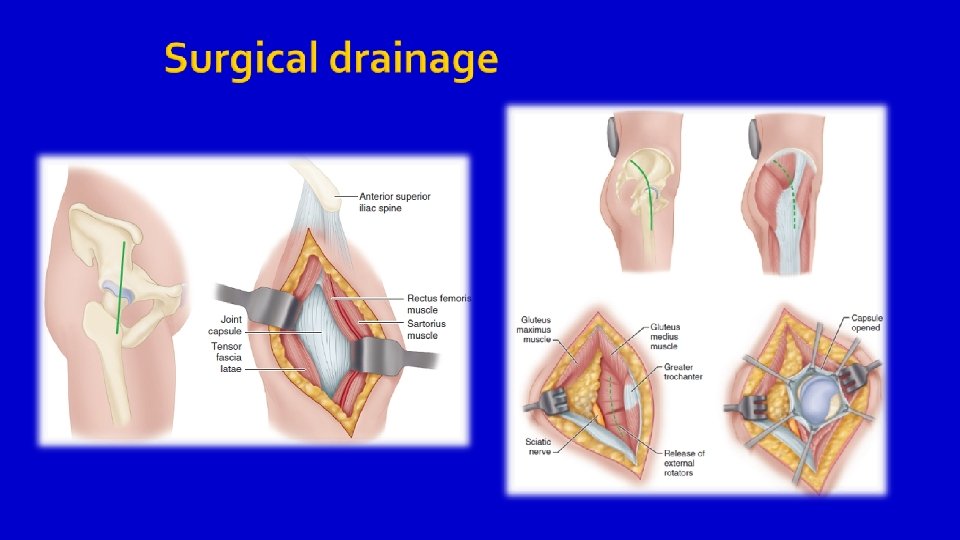
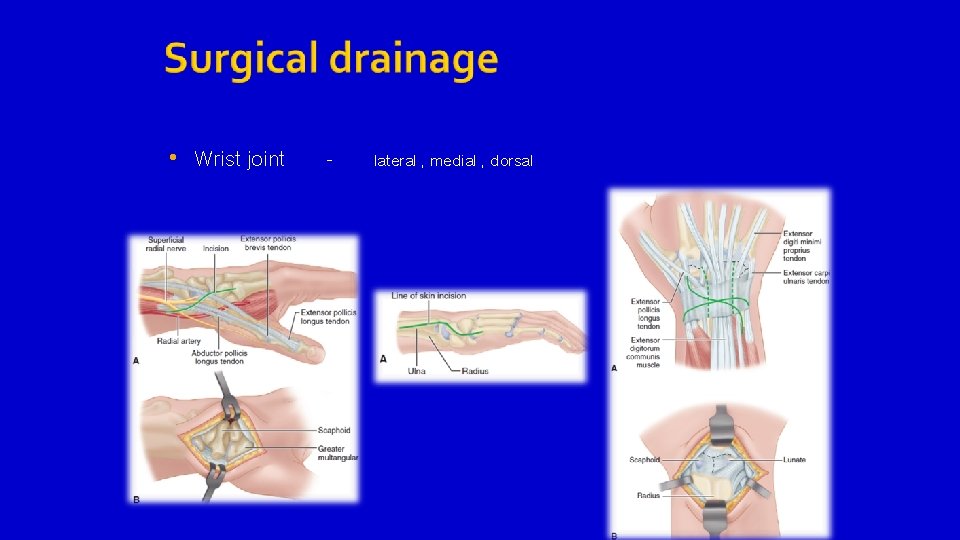
• Wrist joint - lateral , medial , dorsal
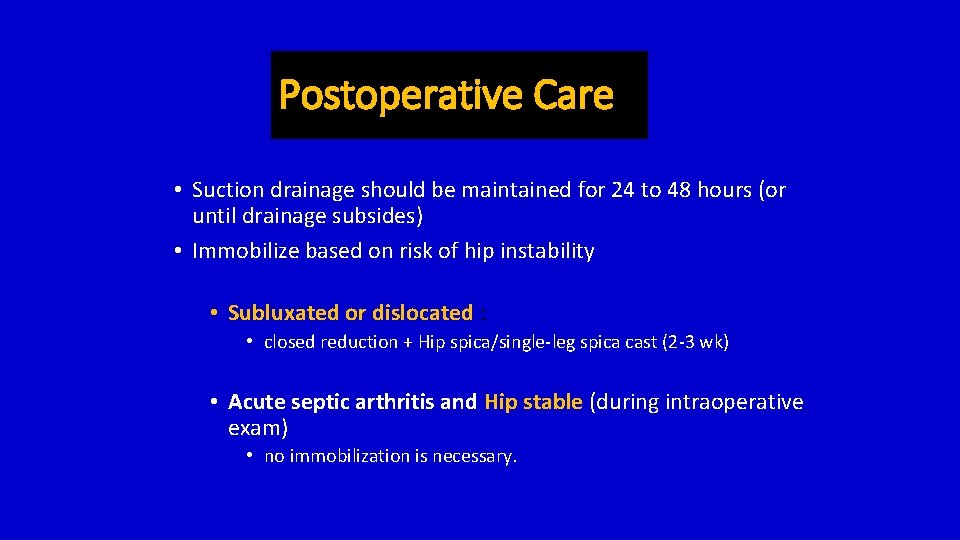
Postoperative Care • Suction drainage should be maintained for 24 to 48 hours (or until drainage subsides) • Immobilize based on risk of hip instability • Subluxated or dislocated : • closed reduction + Hip spica/single-leg spica cast (2 -3 wk) • Acute septic arthritis and Hip stable (during intraoperative exam) • no immobilization is necessary.
Postoperative Care • Infection resolves : physical therapy. • Muscle strengthening, active ROM exercises. • Residual stage (deformity or limitation of motion) : correction, restoration of the joint.
Author preference treatment • Acute septic arthritis: • open surgical debridement • IV ATB • conversion to oral antibiotics after treatment response • Total treatment duration about 3 weeks (depending on clinical and laboratory response to treatment. )
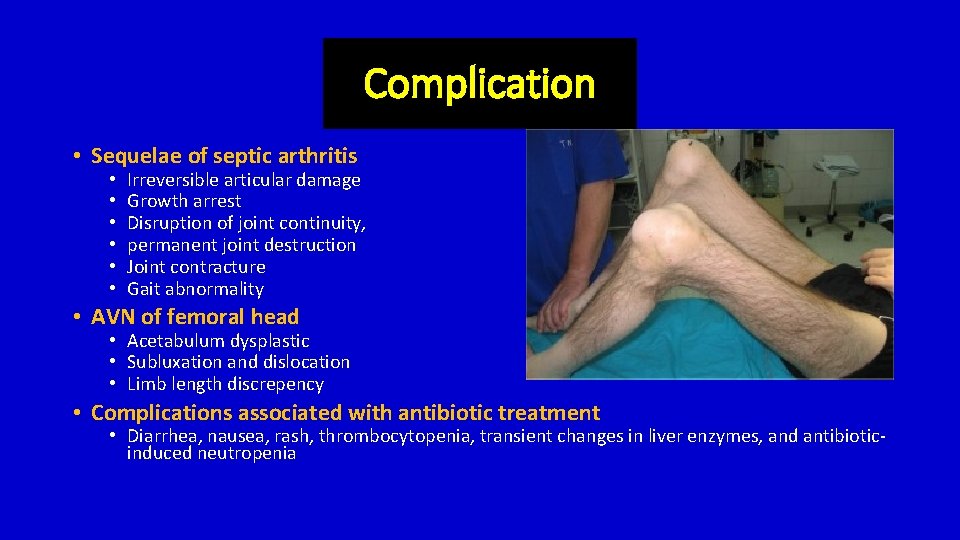
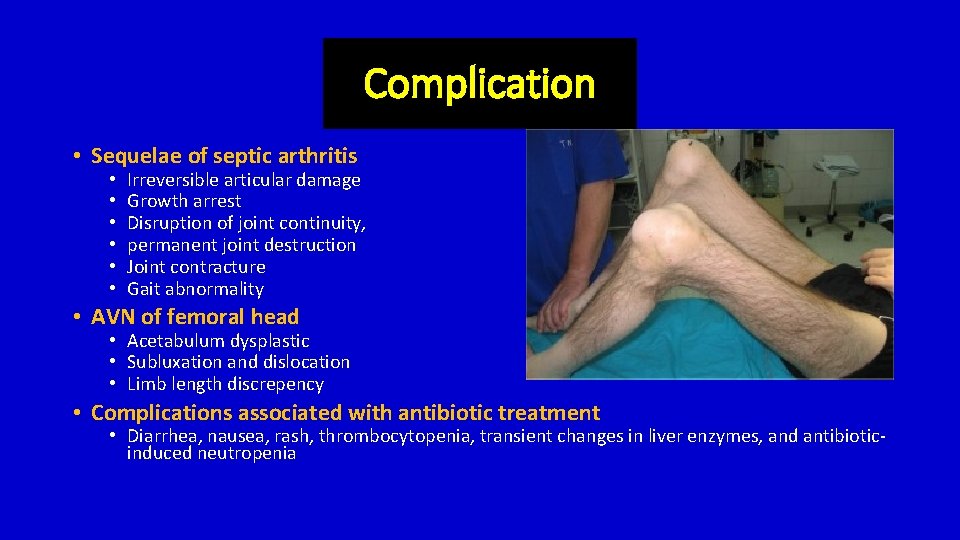
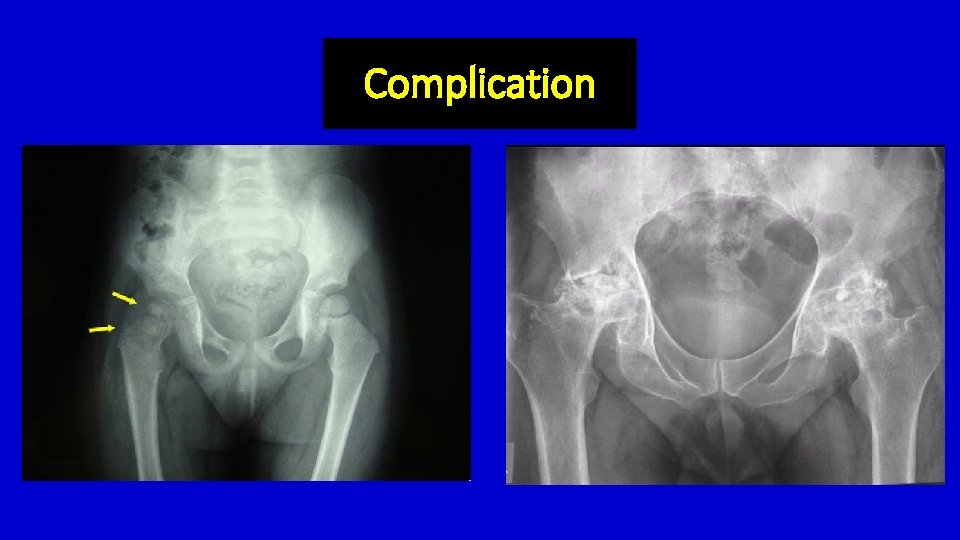
Complication • Sequelae of septic arthritis • • • Irreversible articular damage Growth arrest Disruption of joint continuity, permanent joint destruction Joint contracture Gait abnormality • AVN of femoral head • Acetabulum dysplastic • Subluxation and dislocation • Limb length discrepency • Complications associated with antibiotic treatment • Diarrhea, nausea, rash, thrombocytopenia, transient changes in liver enzymes, and antibioticinduced neutropenia

Complication
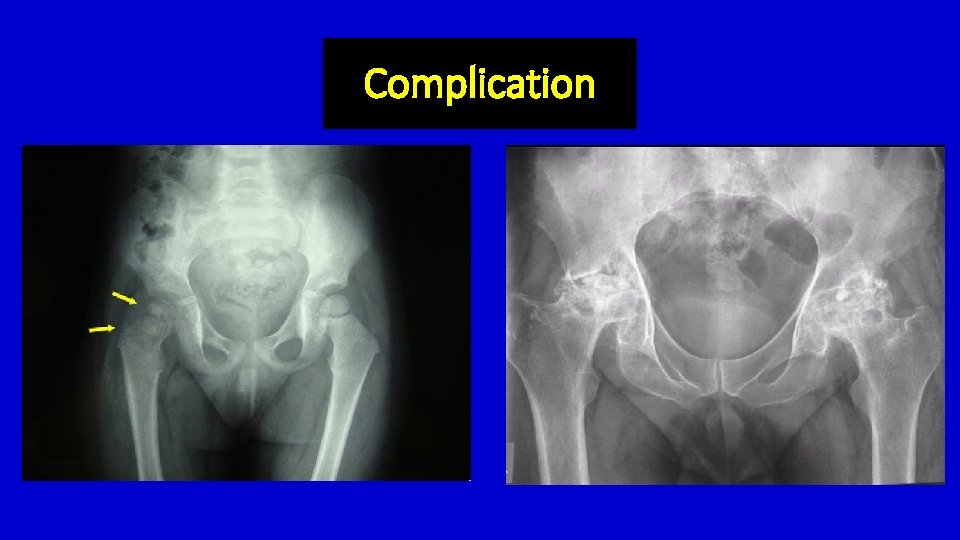
Complication
Summary - Investigation - ESR, CRP - Aspiration - Perform as soon as possible, Confirm diagnosis - Leukocyte > 50, 000, PMN > 75 % - Treatment • • Adequate surgical drainage Empiric intravenous antimicrobial therapy: If clinical improve can be conversion to oral ABO Joint must be rested
References
 Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Gonorrhea symptoms
Gonorrhea symptoms Septic arthritis complications
Septic arthritis complications Example of gram negative cocci
Example of gram negative cocci Septic arthritis complications
Septic arthritis complications Septic arthritis
Septic arthritis Septic workup
Septic workup Septic arthritis antibiotics
Septic arthritis antibiotics Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Reactive arthritis urethritis
Reactive arthritis urethritis Septic arthritis antibiotics
Septic arthritis antibiotics Android.pua.debugkey
Android.pua.debugkey Paul sheesley
Paul sheesley Early total care
Early total care Principles of applying plaster of paris
Principles of applying plaster of paris Reverse sugar tong splint
Reverse sugar tong splint Spica cast
Spica cast Meditouch clinic
Meditouch clinic Puraflo peat
Puraflo peat Thymoma location
Thymoma location Ervin moore sign
Ervin moore sign Carmody septic
Carmody septic Panhandle health septic
Panhandle health septic Jea septic tank phase out
Jea septic tank phase out Doc's septic tank cleaning
Doc's septic tank cleaning Septic
Septic Advantex ax20 price
Advantex ax20 price Qqq10
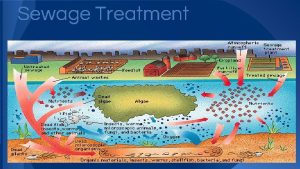
Qqq10 Septic tank contamination groundwater
Septic tank contamination groundwater Summit county septic permit
Summit county septic permit Barnstable county septic loan
Barnstable county septic loan Multiflow septic system
Multiflow septic system Chemical oxygen demand
Chemical oxygen demand Citizens energy group
Citizens energy group Rock solid precast
Rock solid precast Septic implantation syndrome
Septic implantation syndrome Two neutral conducting pop cans are touching each other
Two neutral conducting pop cans are touching each other Columna renalis
Columna renalis Saran dan harapan
Saran dan harapan Awal menulis laporan hasil observasi adalah
Awal menulis laporan hasil observasi adalah Prashant saran
Prashant saran Slidetodoc.com
Slidetodoc.com Teks editorial kritik penilaian prediksi harapan saran
Teks editorial kritik penilaian prediksi harapan saran Usul dan saran
Usul dan saran Huzur saran iit delhi
Huzur saran iit delhi Prinsip sumbang saran
Prinsip sumbang saran Düz kaslar iskeletimizi saran kaslardır
Düz kaslar iskeletimizi saran kaslardır Saran wrap structure
Saran wrap structure