Management of Septic Shock Dr Rajath A Septic

- Slides: 29
Management of Septic Shock Dr Rajath A.
Septic Shock • Septic shock- once a uniformly fatal condition with 100% mortality. • Present recovery rates are upto 50%. • Significance: Frequent occurrence and high mortality.
Septic Shock I. Introduction. II. Pathophysiology III. Clinical Manifestations IV. Management
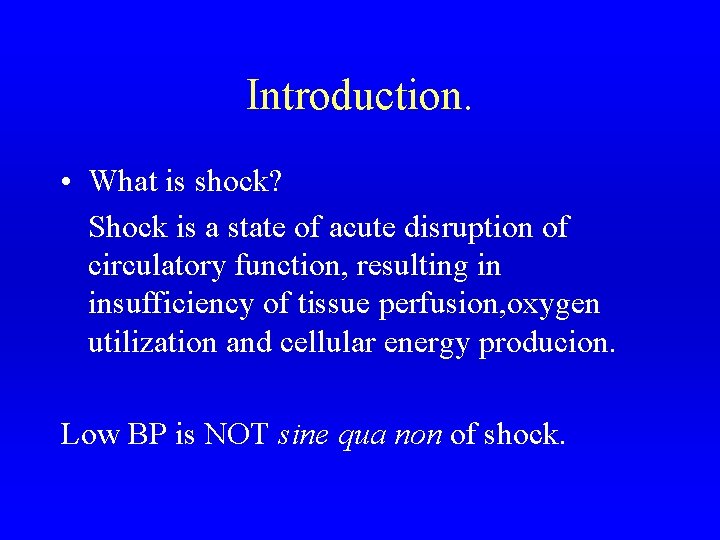
Introduction. • What is shock? Shock is a state of acute disruption of circulatory function, resulting in insufficiency of tissue perfusion, oxygen utilization and cellular energy producion. Low BP is NOT sine qua non of shock.
Septic Shock I. Introduction. II. Pathophysiology III. Clinical Manifestations IV. Management
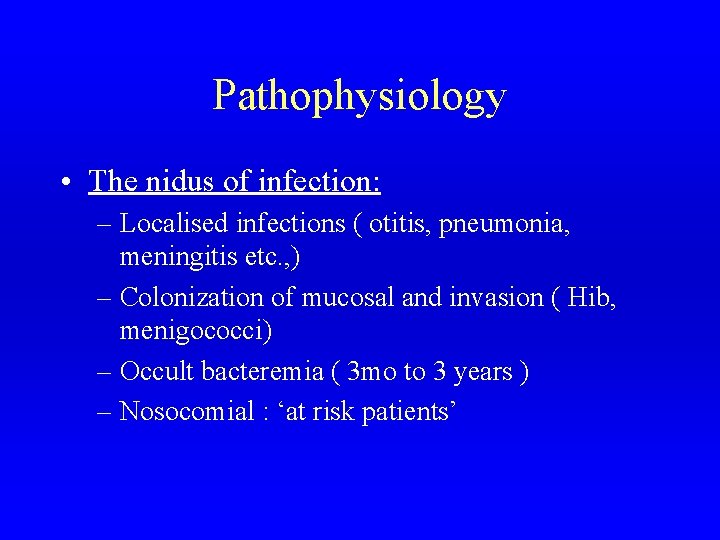
Pathophysiology • The nidus of infection: – Localised infections ( otitis, pneumonia, meningitis etc. , ) – Colonization of mucosal and invasion ( Hib, menigococci) – Occult bacteremia ( 3 mo to 3 years ) – Nosocomial : ‘at risk patients’
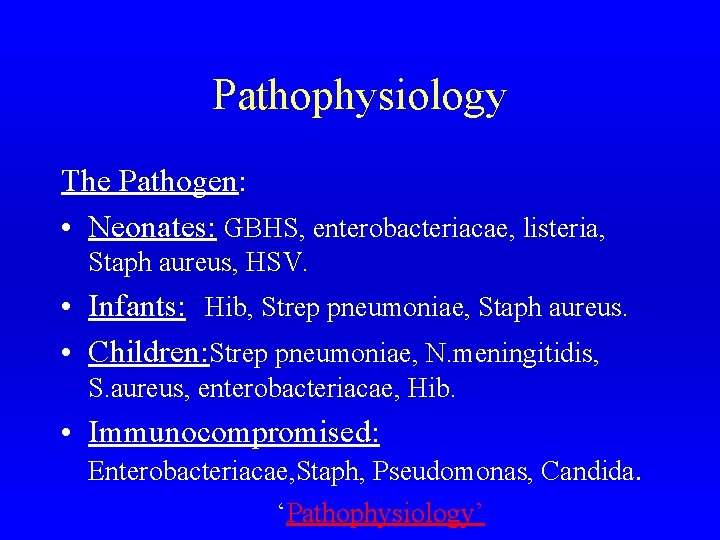
Pathophysiology The Pathogen: • Neonates: GBHS, enterobacteriacae, listeria, Staph aureus, HSV. • Infants: Hib, Strep pneumoniae, Staph aureus. • Children: Strep pneumoniae, N. meningitidis, S. aureus, enterobacteriacae, Hib. • Immunocompromised: Enterobacteriacae, Staph, Pseudomonas, Candida. ‘Pathophysiology’
Pathophysiology • The agent - host interaction leads to ‘CHAOS’
Pathophysiology • What ‘type of shock’ is septic shock? Septic shock has features of : – Hypovolemic shock – Cardiac shock – Distributive shock.
Septic Shock I. Introduction. II. Pathophysiology III. Clinical Manifestations IV. Management
Clinical Manifestations. The Continuum of infection to MODS and Death (Clinical Definitions)
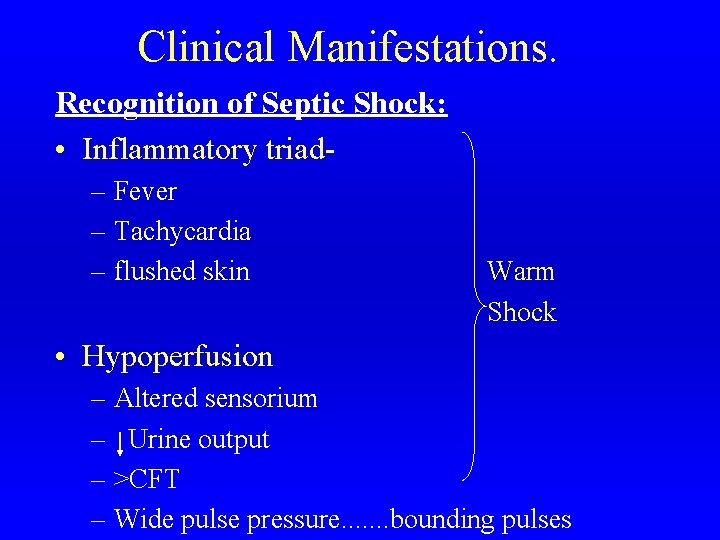
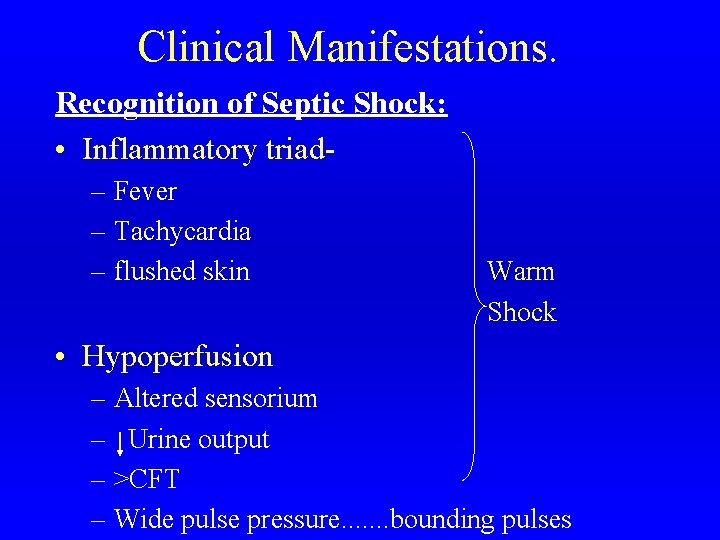
Clinical Manifestations. Recognition of Septic Shock: • Inflammatory triad– Fever – Tachycardia – flushed skin Warm Shock • Hypoperfusion – Altered sensorium – Urine output – >CFT – Wide pulse pressure. . . . bounding pulses
Clinical Manifestations. • Hypotension – Cold and clammy skin – Mottling – Tachycardia – Cyanosis – Narrow pulse pressure – Hypoxemia – Acidosis. Cold shock
Clinical Manifestations. Staging of Septic Shock: I. Compensated / Preshock / Hyperdynamic II. Decompensated / Organ hypoperfusion III. End organ failure / Irreversible
Septic Shock I. Introduction. II. Pathophysiology III. Clinical Manifestations IV. Management
Management Prevention: 1. Immunisation 2. Prompt treatment of local infections 3. Hospitalized patient: look out for nidus of infection- IV lines, catheters, E. tubes
Management Recognise septic shock early: • Remember- Inflammatory triad Signs of hypoperfusion • Do not wait for the BP to fall ! • Lower limit for systolic BP = 70 +( age x 2)
Management. • Two means of death: 1. Shock. 2. Multi organ failure. • Aims of treatment: 1. Assure perfusion of critical vascular beds. ( cerebral, coronary, renal) 2. Rx underlying cause.
Management STEPS 1. Prevent / correct hypoxemia: Supplement oxygen 95 -100%. 2. IV access: peripheral vein. 3. If IV access fails: Intraosseous line. 4. Fluid resuscitation: 20 m. L/Kg NS or RL as bolus, repeat upto 60 m. L/Kg. End point : Improved perfusion.
Management STEPS Improved perfusion => a. CFT b. Warmth c. Strong pulses d. mental status e. Tachycardia f. BP (ideal = 90 + age x 2; Min = 70+ age x 2) g. Urine output.

Management STEPS 5. Establish a 2 nd IV line for Dopamine infusion (Draw blood for culture) 6. Administer IV antibiotics <2 mo: Ampicillin + gentamicin or Ampicillin+ceftriaxone/cefataxime >2 mo: Ceftriaxone or Cefotaxime alone or Ampicillin + Chloramphenicol
Management STEPS 7. Correct metabolic derangement: – Metabolic acidosis. – Hyper or hypoglycemia : always correct hypoglycemia.
Management STEPS 8. DIC: • Restoration of normovolemia reverses abnormal activation. • ‘Component replacement’ (Goal - Normal PT, PTT, fibrinogen, PC = 40, 000 to 1 Lakh/cumm. ) a. FFP - most beneficial in early stages. b. Cryo- consider 1 unit/3 units of FFP transfused. c. Platelet concentrate
Management STEPS 9. Recognize and manage organ failure: a. Cardiovascular support: Rate & rythm- correct 02, acidosis, Ca, Mg, K variations Stroke volume - fluid correction & replace losses Ionotrope support.
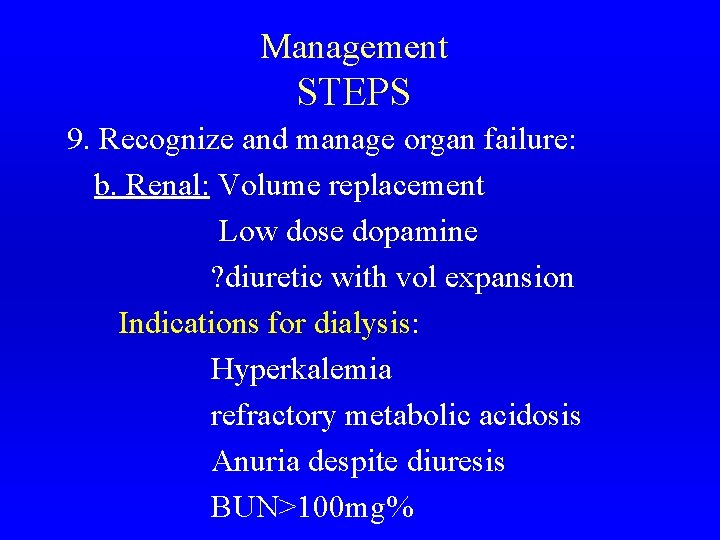
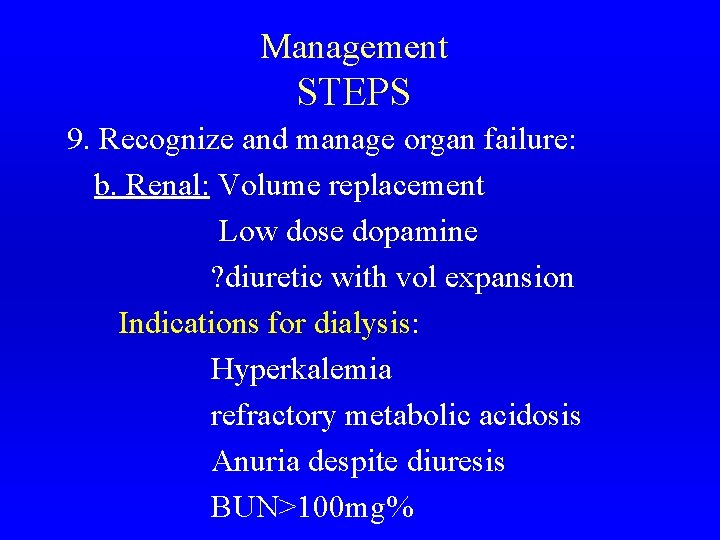
Management STEPS 9. Recognize and manage organ failure: b. Renal: Volume replacement Low dose dopamine ? diuretic with vol expansion Indications for dialysis: Hyperkalemia refractory metabolic acidosis Anuria despite diuresis BUN>100 mg%
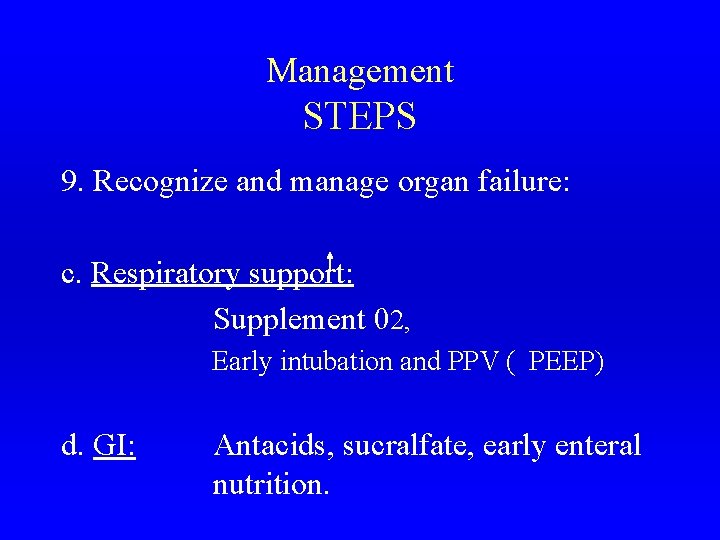
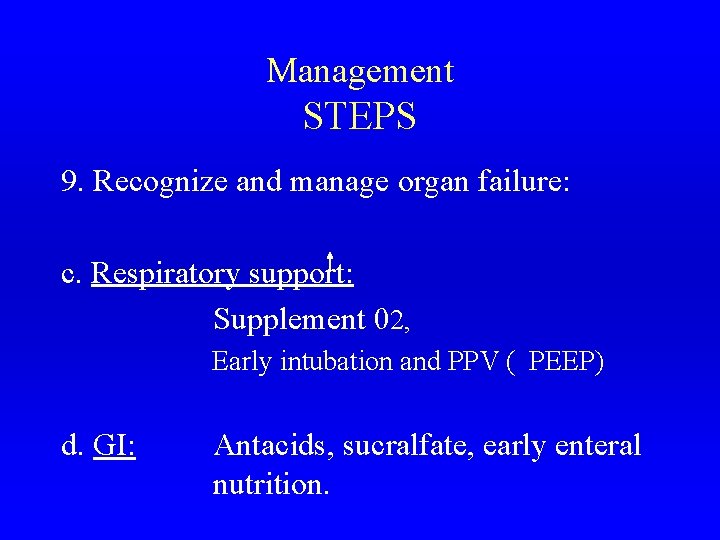
Management STEPS 9. Recognize and manage organ failure: c. Respiratory support: Supplement 02, Early intubation and PPV ( PEEP) d. GI: Antacids, sucralfate, early enteral nutrition.
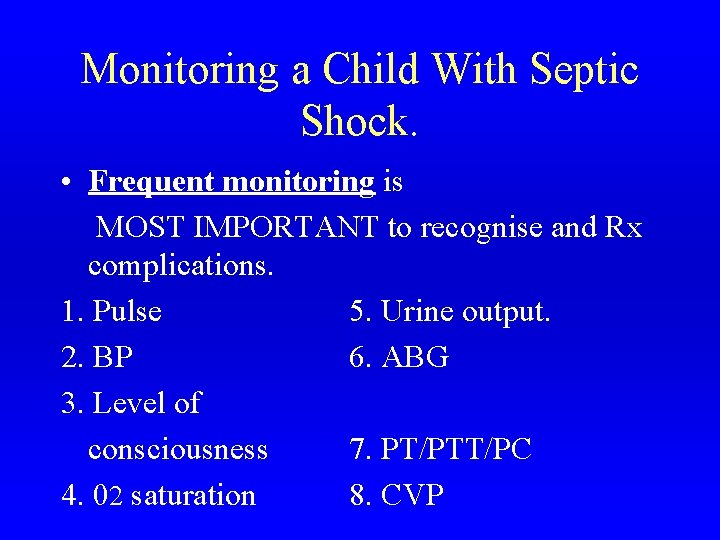
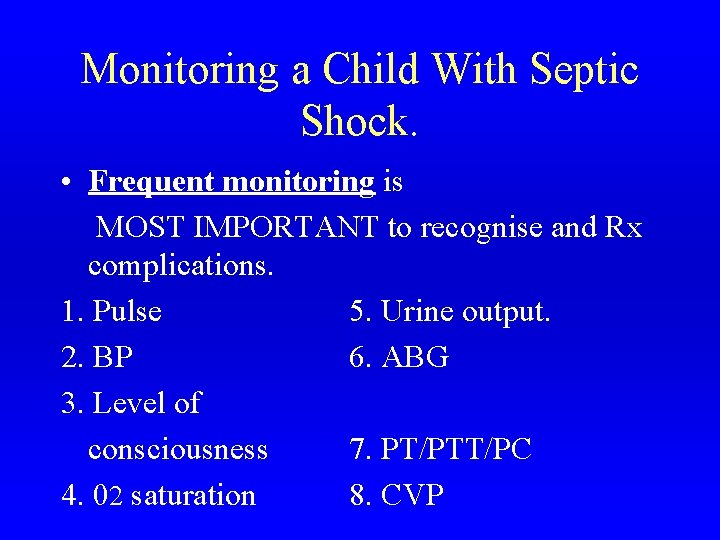
Monitoring a Child With Septic Shock. • Frequent monitoring is MOST IMPORTANT to recognise and Rx complications. 1. Pulse 5. Urine output. 2. BP 6. ABG 3. Level of consciousness 7. PT/PTT/PC 4. 02 saturation 8. CVP
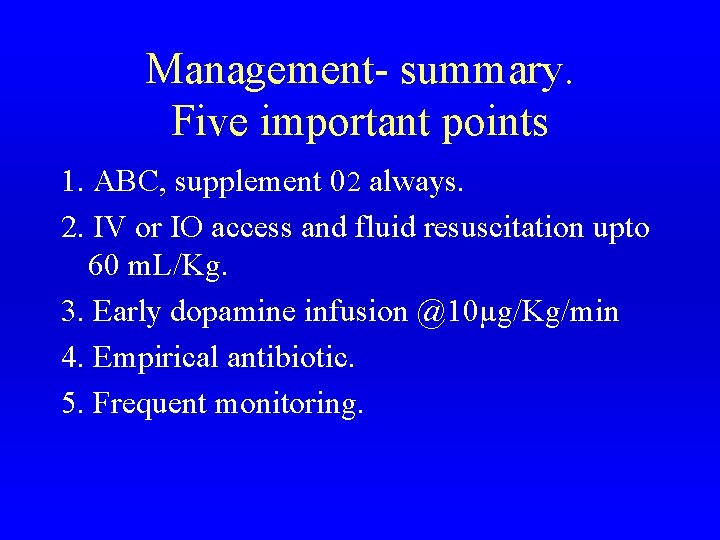
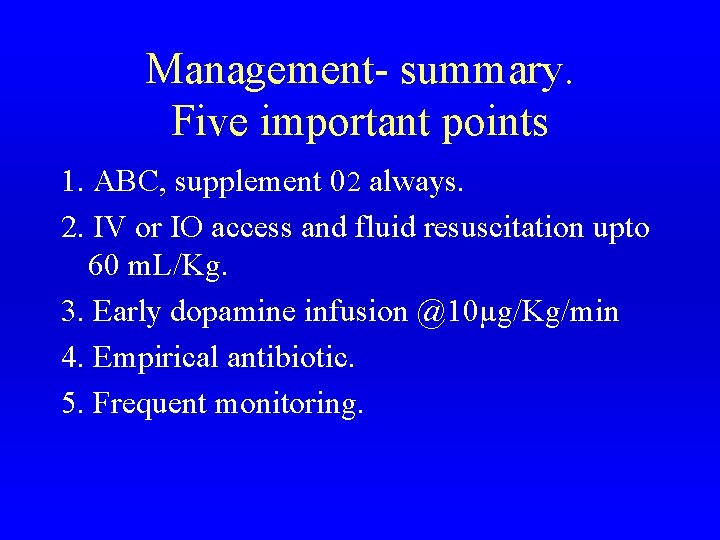
Management- summary. Five important points 1. ABC, supplement 02 always. 2. IV or IO access and fluid resuscitation upto 60 m. L/Kg. 3. Early dopamine infusion @10µg/Kg/min 4. Empirical antibiotic. 5. Frequent monitoring.
References 1. Nelson TB of Pediatrics. 16 th edn. 2. Medical Emergencies in Children. Meharban singh 3. PALS: 1997, AAP & AHA. 4. PCNA: Intensive Care. 1987. 5. TB of Pediatric Critical Care- P. R. Holbrook 6. Handbook of PIC- Rogers & Hefaler 7. Various Speakers: Critical Care CME, May 2002
 Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Shok neurogenico
Shok neurogenico Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Spinal shock symptoms
Spinal shock symptoms Spinal shock vs neurogenic shock
Spinal shock vs neurogenic shock Distributive shock
Distributive shock Jea septic tank phase out
Jea septic tank phase out Septic tank contamination groundwater
Septic tank contamination groundwater Gonorrhea symptoms
Gonorrhea symptoms Indianapolis septic tank elimination program
Indianapolis septic tank elimination program Ervin moore sign
Ervin moore sign Advantex septic system reviews
Advantex septic system reviews Barnstable county septic loan
Barnstable county septic loan Pickwickian syndrome in dogs
Pickwickian syndrome in dogs Septic arthritis complications
Septic arthritis complications Panhandle health septic
Panhandle health septic Septic arthritis antibiotics
Septic arthritis antibiotics Septic arthritis antibiotics
Septic arthritis antibiotics Qqq10
Qqq10 Multi flo aerator replacement
Multi flo aerator replacement Puraflo peat
Puraflo peat Septic arthritis complications
Septic arthritis complications Doc's septic tank cleaning
Doc's septic tank cleaning Septic arthritis
Septic arthritis Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Satellitism in haemophilus influenzae
Satellitism in haemophilus influenzae Example of gram negative cocci
Example of gram negative cocci Septic zone
Septic zone Septic spleen
Septic spleen Septic arthritis workup
Septic arthritis workup