Chronic Tonsillitis and Tonsillectomy Definition Chronic inflammation of

- Slides: 21
Chronic Tonsillitis and Tonsillectomy
Definition �Chronic inflammation of the palatine tonsils secondary to repeated attacks of acute tonsillitis or inadequately treated acute tonsillitis
Aetiology �Complication of acute tonsillitis �Subclinical infection �Mostly seen in children and young adults �Commonest causative organism: beta hemolytic streptococcus �Predisposing factors: Chronic dental infection and sinusitis
Types �Chronic follicular tonsillitis Crypts with cheesy material Seen as yellow spots on the surface Common in adults �Chronic parenchymatous tonsillitis Hyperplasia of lymphoid tissue due to recurrent attacks with gross tonsillar enlargement �Chronic fibrotic tonsillitis Small, infected tonsils
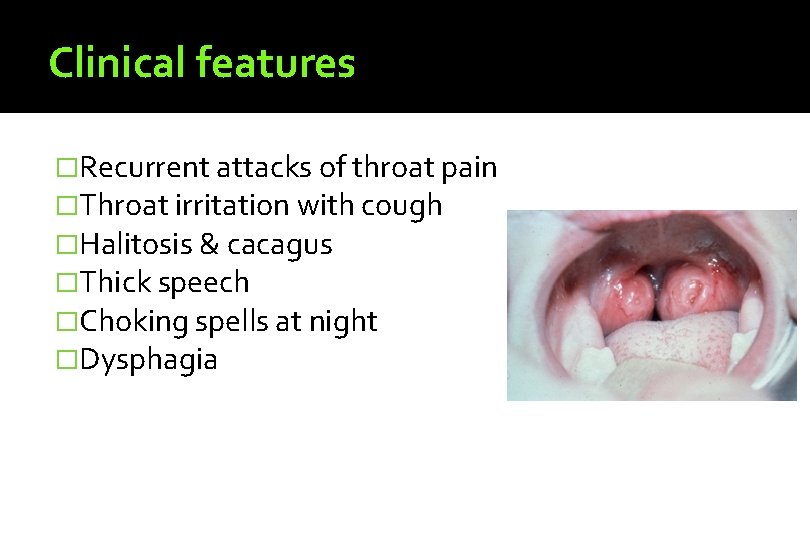
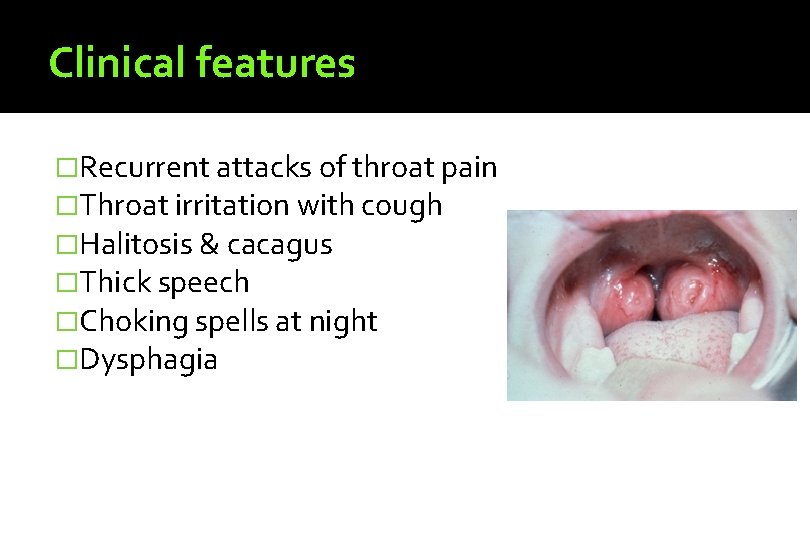
Clinical features �Recurrent attacks of throat pain �Throat irritation with cough �Halitosis & cacagus �Thick speech �Choking spells at night �Dysphagia
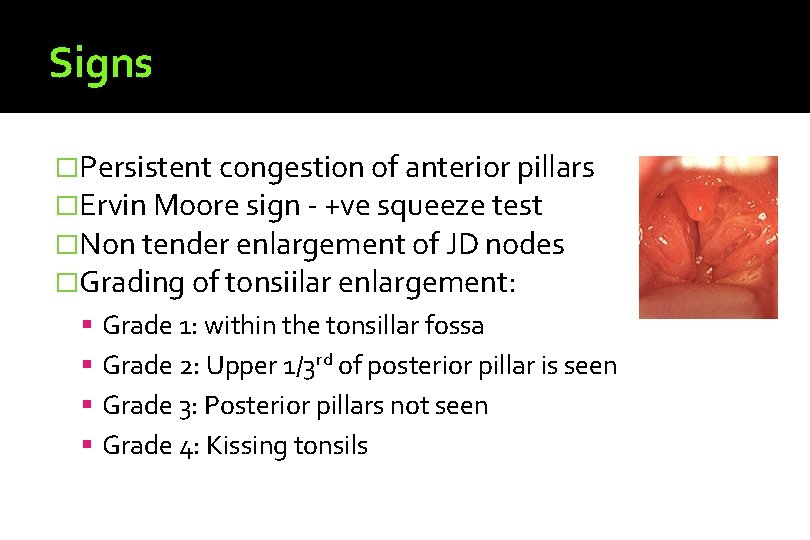
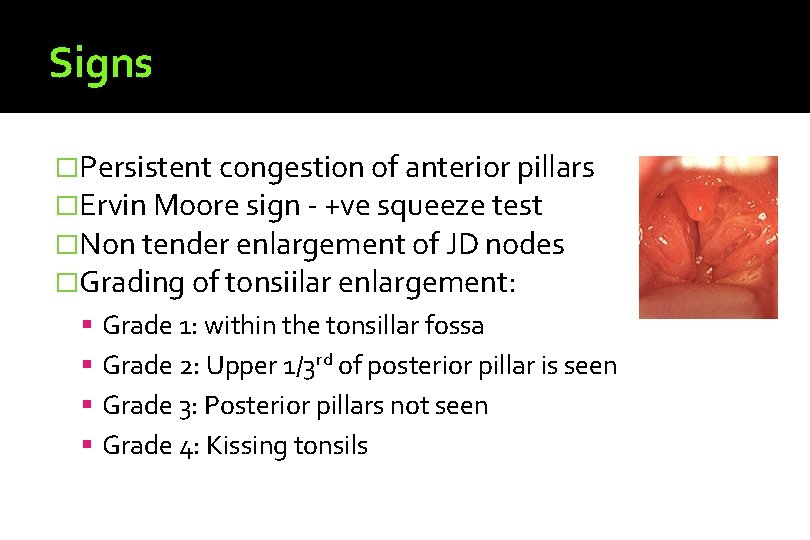
Signs �Persistent congestion of anterior pillars �Ervin Moore sign - +ve squeeze test �Non tender enlargement of JD nodes �Grading of tonsiilar enlargement: Grade 1: within the tonsillar fossa Grade 2: Upper 1/3 rd of posterior pillar is seen Grade 3: Posterior pillars not seen Grade 4: Kissing tonsils

Complications �Peritonsillar abscess �Parapharyngeal Abscess �Intratonsillar abscess �Tonsillolith & tonsillar cysts �Focus of infection in rheumatic fever, eye and skin disorders and acute glomerulonephritis
Investigations �CBC, ESR, platelet count �Bleeding parameters: BT, CT, PT, APTT �Blood grouping & typing �Urine routine
Treatment �Conservative: General health Diet Treatment of co-existing disorders of teeth, nose and sinuses �Surgical: Tonsillectomy
Historical Perspective � Tonsillectomy Latin word tonsilla ▪ “stake to which boats are tied” Greek word ektome ▪ “excision” � Aulus Cornelius Celsus – 50 AD Gives the earliest account of tonsillectomy…using a finger!
Techniques �Dissection and snare – most commonly used �Cryosurgery �Elecrocautery assisted �Laser assisted – KTP & CO 2 Lasers �Coblation - Radiofrequency �Harmonic scalpel – uses ultrasound �Microdebrider assisted – preserves the capsule �Guillotine - outdated
Dissection and snare technique �Most commonly used �Fairly easy and safe �Better performed under GA �Minimal bleeding
Absolute Indications Recurrent attacks - 6 -7 in one year, 4 -5/year for 2 years, 3/ year for 3 years or > loss of 2 weeks of school or work 2 nd attack of quinsy Sleep apnea syndrome
Relative Indications � Carriers of diphtheria and streptococci � Tonsillar cyst, tonsillolith & impacted FB � Tonsillitis with febrile convulsions � Suspicion of lymphoma of the tonsil � Benign tumours of the tonsil � Tonsils acting as a septic focus for kidney, cardiovascular, skin, eye and joint disorders � Halitosis & cacagus after ruling out other causes � Primary tuberculosis of tonsil � Unexplained cervical lymphadenopathy � Failure to gain weight in the absence of other causes � Surgical approach to styloid process, glossopharyngeal nerve, UVPP
Contraindications �Acute infection �Anaemia �Age below 3 years �Bleeding disorders �Epidemic of Polio �Pregnancy & menstruation �Uncontrolled systemic disorders �Cervical spine abnormalities
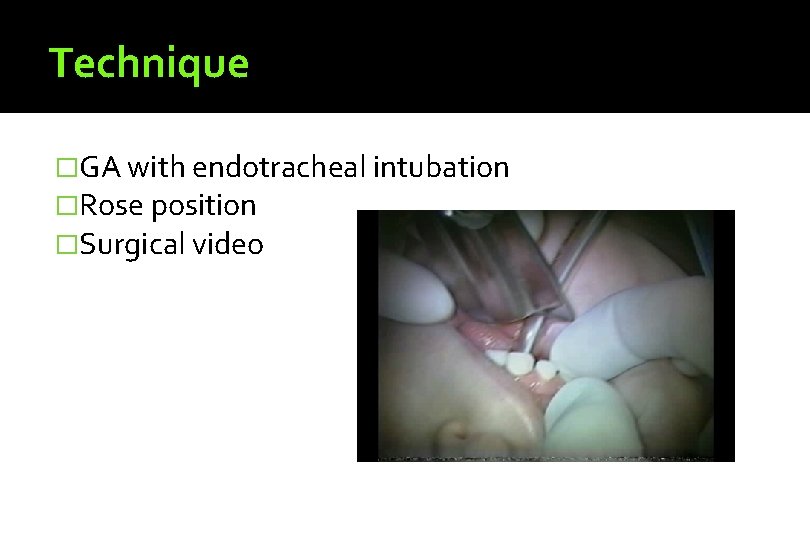
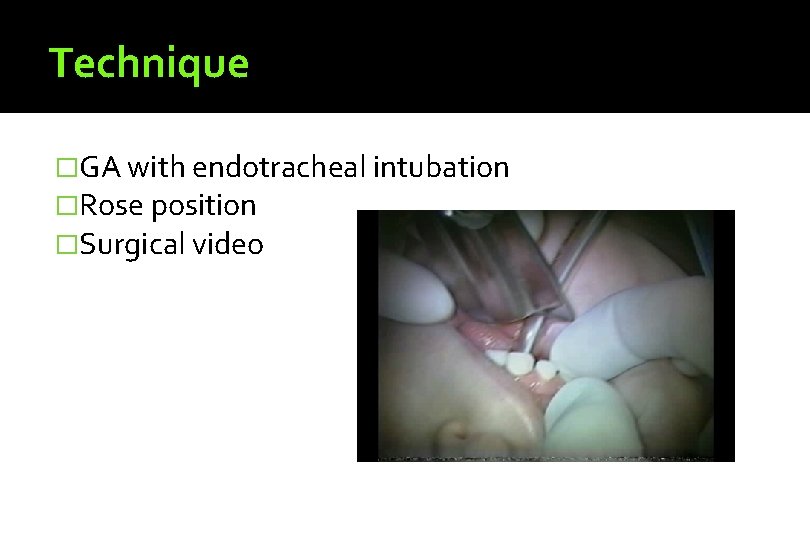
Technique �GA with endotracheal intubation �Rose position �Surgical video
Postoperative care �Coma position �Monitoring the vital signs �Watch for frequent swallow reflex and bleeding �Ice creams, cold milk and soft diet �Dilute hydrogen peroxide gargles �Analgesics and antibiotics
Complications �Haemorrhage: Primary, reactionary & secondary �Injury to pillars, lips, soft palate, uvula, tongue & teeth �Anaesthetic complications including death �Aspiration of blood �Pulmonary complications: pneumonitis, atelactasis, abscess �Post operative airway obstruction due to oedema �Scarring – pillars, palate & post pharyngeal wall �Tonsillar remnants �Subluxation of Atlanto-occipital joint �Hypertrophy of lingual tonsil
Primary haemorrhage �At the time of operation �Due to presence of infection, bleeding disorders, injury to paratonsillar vein or other vessels, improper technique, patients on NSAIDs etc �Controlled by packing & pressure �Ligation or electocautery
Reactionary haemorrhage � Occurs within 24 hours, usually 5 -6 hours � Due to Loose ligature Failure to ligate all bleeding points Post operative increase in BP Increase in BP during recovery from GA Presence of clot in the fossa Excessive coughing or vomiting � Management Remove the clot, H 2 O 2 gargles, vasoconstictor swabs, Chemical cautery, Styptics etc Shift to OT, ligate or cauterise the bleeder Pillar to pillar suture ECA Ligation in the neck
Secondary Haemorrhage �Occurs between 7 th-10 th post operative day. �Due to sepsis and premature separation of the membrane over the fossa �Presents as bllod stained secretions or frank bleeding �Requires admission and assessment of blood loss, replacement if required, parenteral antibiotics, removal of clot, Dilute H 2 O 2 gargles, Pillar to pillar suturing if required �Ligation or cauterisation should not be attempted.