Osteomyelitis and Septic arthritis 8 2551 Complication n

- Slides: 43
Osteomyelitis and Septic arthritis ��. �� ��������� 8������� 2551
Complication n Sepsis, Toxic shock n disability and deformity
Classification n Age group q q q n Neonate Childhood Adolescent Duration of symptom q q q Acute Sub-acute Chronic
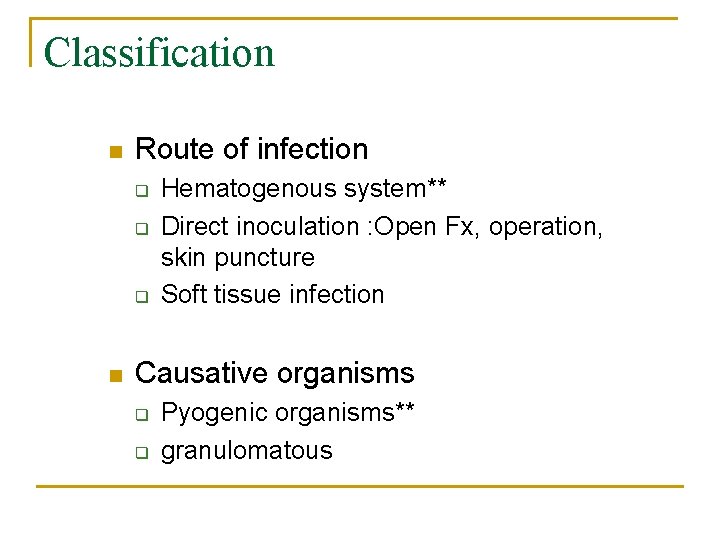
Classification n Route of infection q q q n Hematogenous system** Direct inoculation : Open Fx, operation, skin puncture Soft tissue infection Causative organisms q q Pyogenic organisms** granulomatous
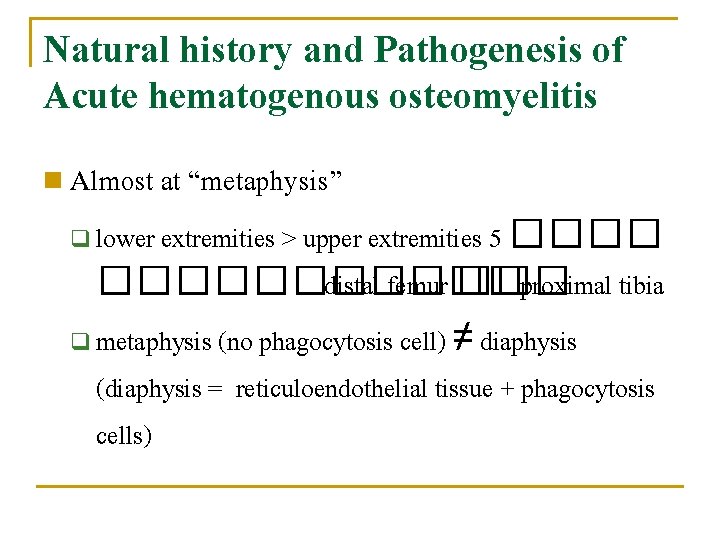
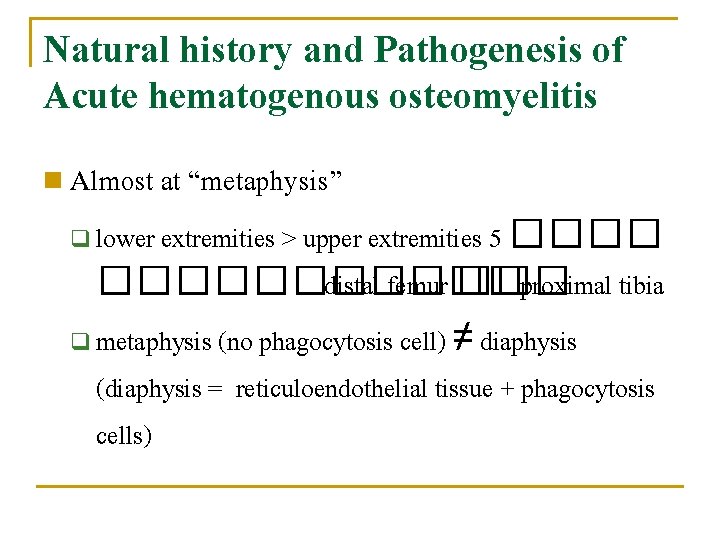
Natural history and Pathogenesis of Acute hematogenous osteomyelitis n Almost at “metaphysis” lower extremities > upper extremities 5 ����������� distal femur ��� proximal tibia q metaphysis (no phagocytosis cell) ≠ diaphysis (diaphysis = reticuloendothelial tissue + phagocytosis cells) q
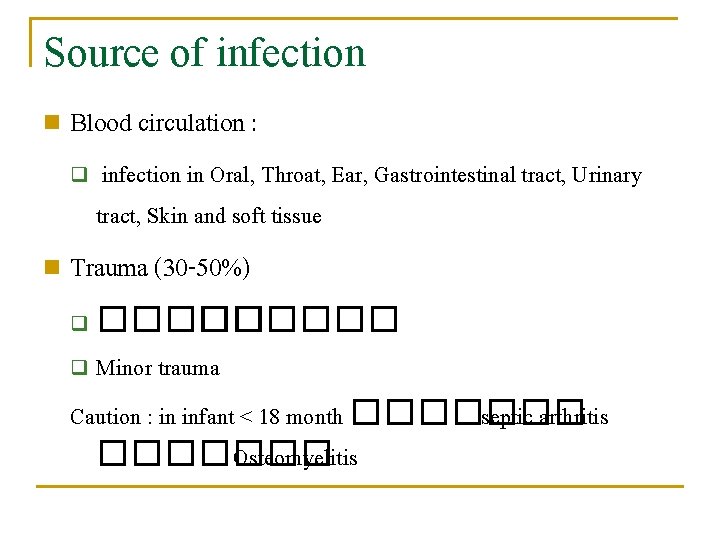
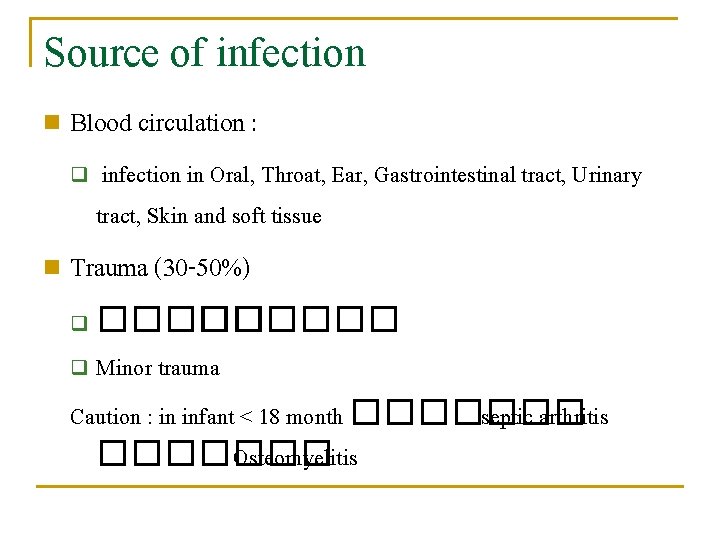
Source of infection n Blood circulation : q n infection in Oral, Throat, Ear, Gastrointestinal tract, Urinary tract, Skin and soft tissue Trauma (30 -50%) ������ q Minor trauma Caution : in infant < 18 month ������� septic arthritis ������� Osteomyelitis q
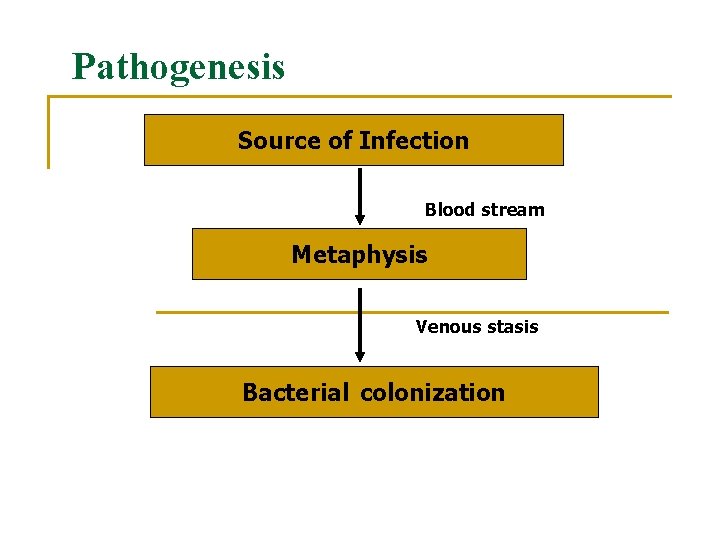
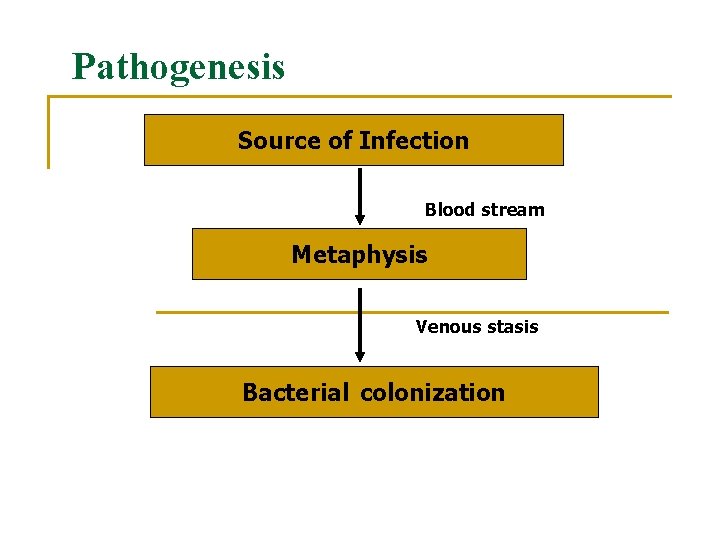
Pathogenesis Source of Infection Blood stream Metaphysis Venous stasis Bacterial colonization
Inflammation: acute osteomyelitis n First 24 hours Vascular congestion n Polymorphonuclear leukocyte infiltration n Exudation n
Inflammation: acute osteomyelitis n 2 -3 day No treat with antibiotic n Intraosseus pressure intense pain intravascular thrombosis ischemia ��������
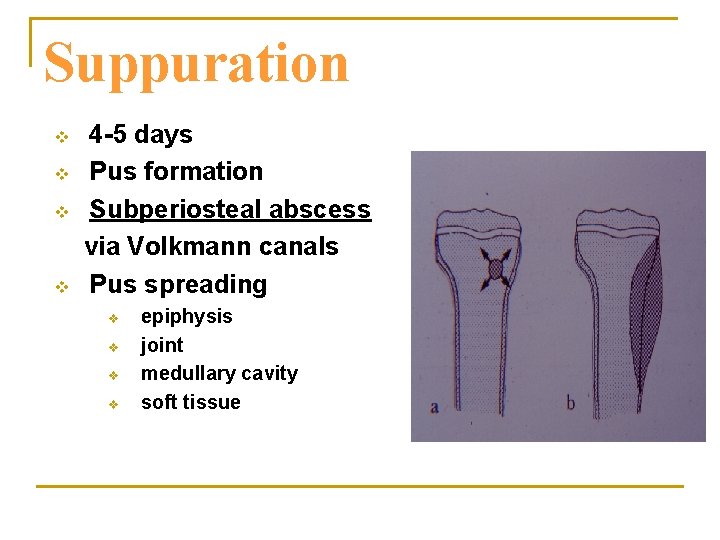
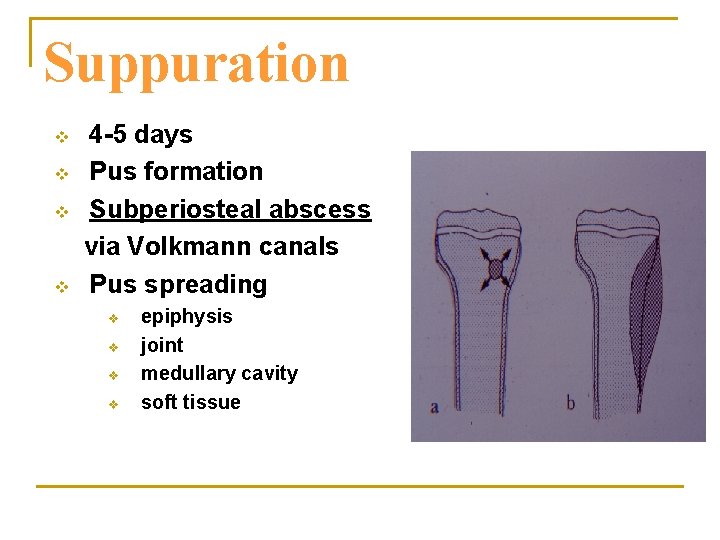
Suppuration v v 4 -5 days Pus formation Subperiosteal abscess via Volkmann canals Pus spreading v v epiphysis joint medullary cavity soft tissue
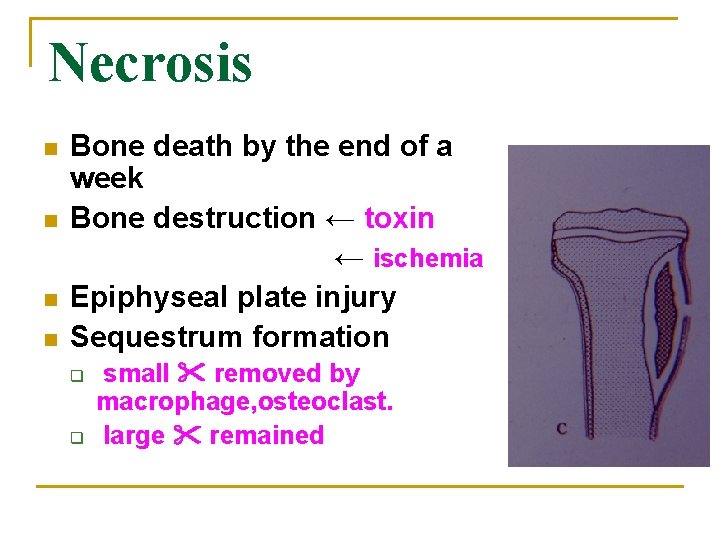
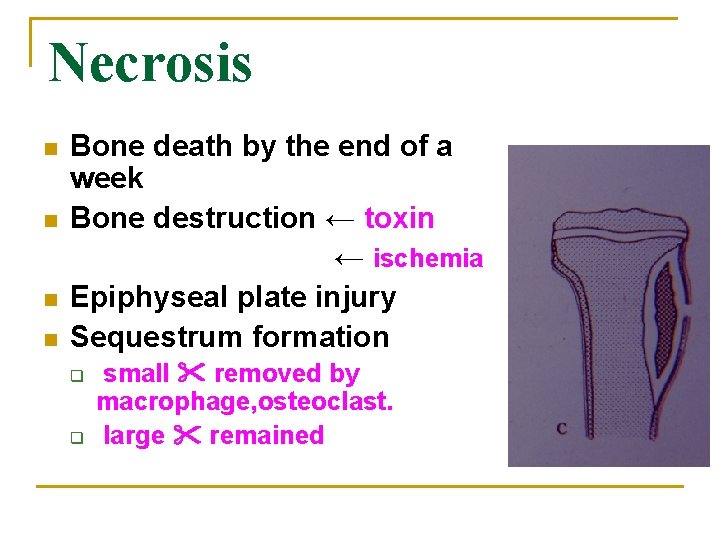
Necrosis n n Bone death by the end of a week Bone destruction ← toxin ← ischemia Epiphyseal plate injury Sequestrum formation q q small removed by macrophage, osteoclast. large remained
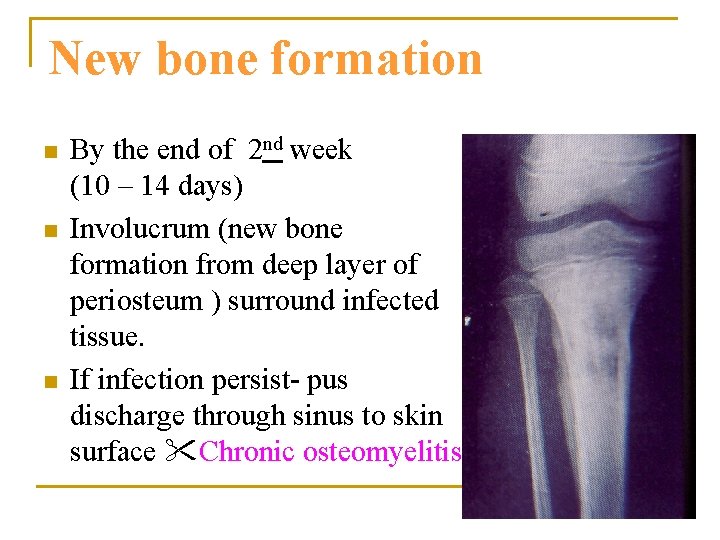
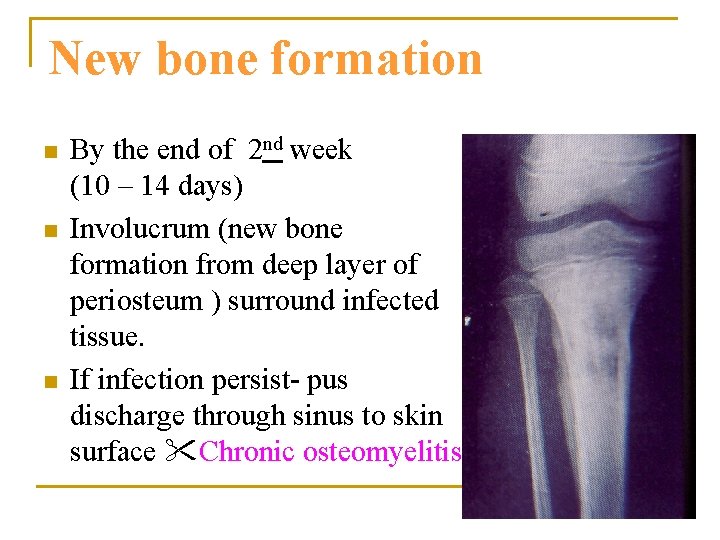
New bone formation n By the end of 2 nd week (10 – 14 days) Involucrum (new bone formation from deep layer of periosteum ) surround infected tissue. If infection persist- pus discharge through sinus to skin surface Chronic osteomyelitis
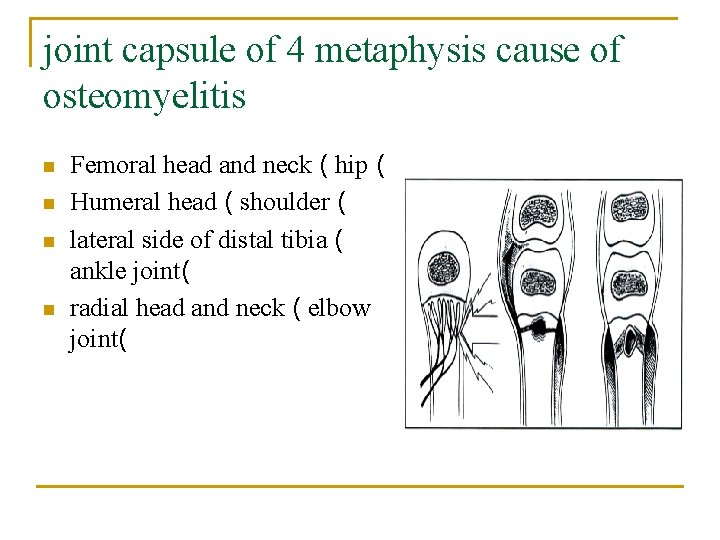
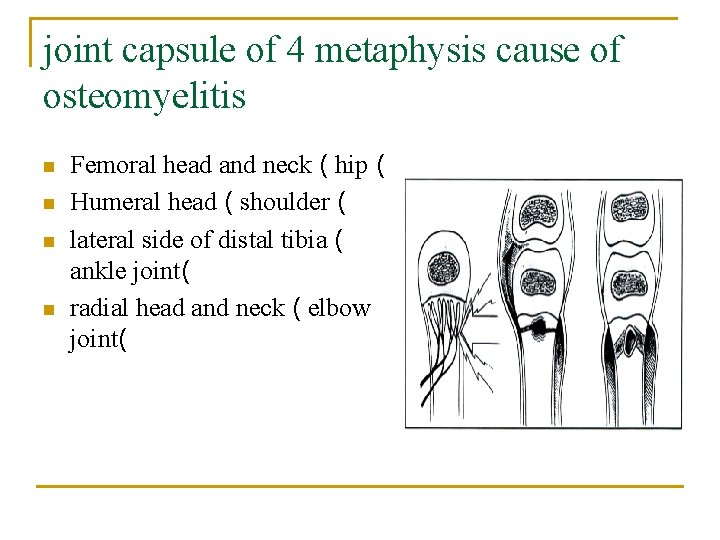
joint capsule of 4 metaphysis cause of osteomyelitis n n Femoral head and neck ( hip ( Humeral head ( shoulder ( lateral side of distal tibia ( ankle joint( radial head and neck ( elbow joint(
Signs and Symptoms in infant Drowsy Ø Irritable Ø Fails to thrive Ø history of birth difficulties Ø History of umbilical artery catheterization Ø Metaphyseal tenderness and resistance to joint movement Ø
Signs and Symptoms in child Ø Severe pain Ø Malaise Ø Fever Ø Toxemia Ø History of recent infection Ø Local inflammation Ø Lymphadenopathy pus escape from bone
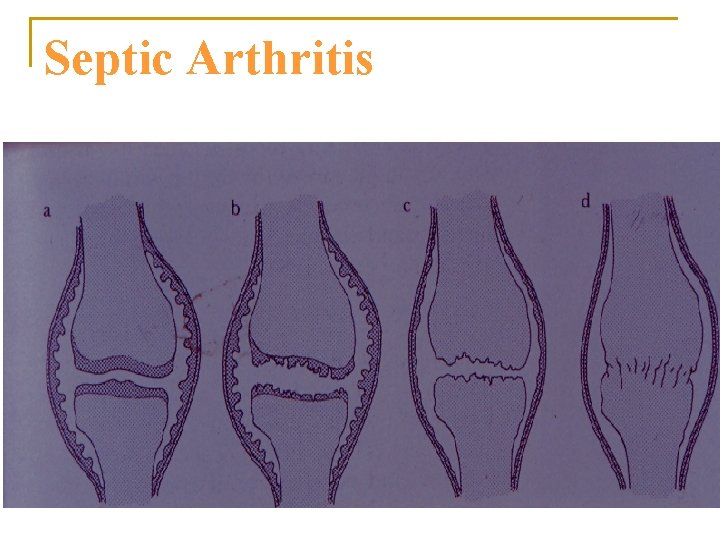
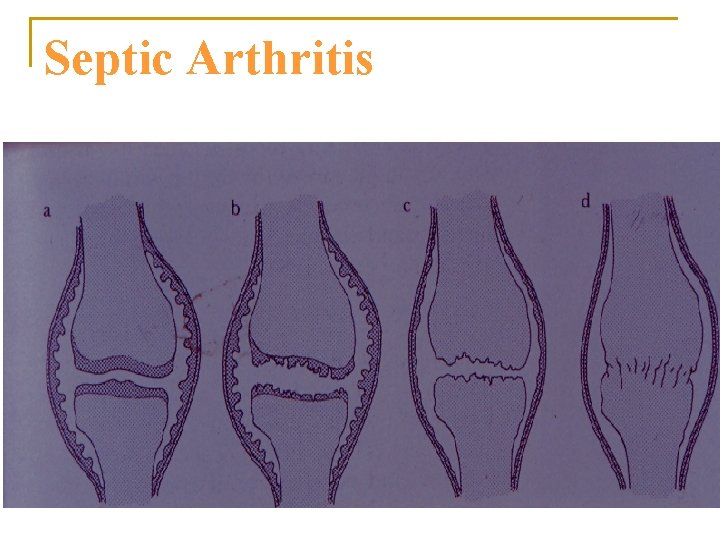
Septic Arthritis
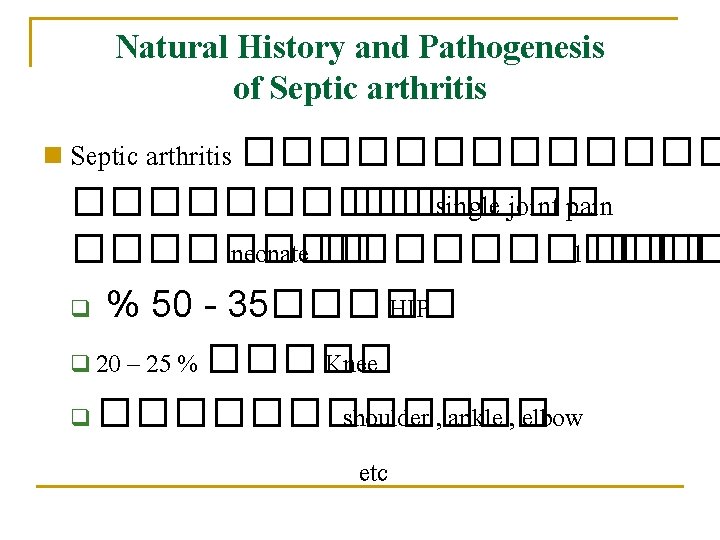
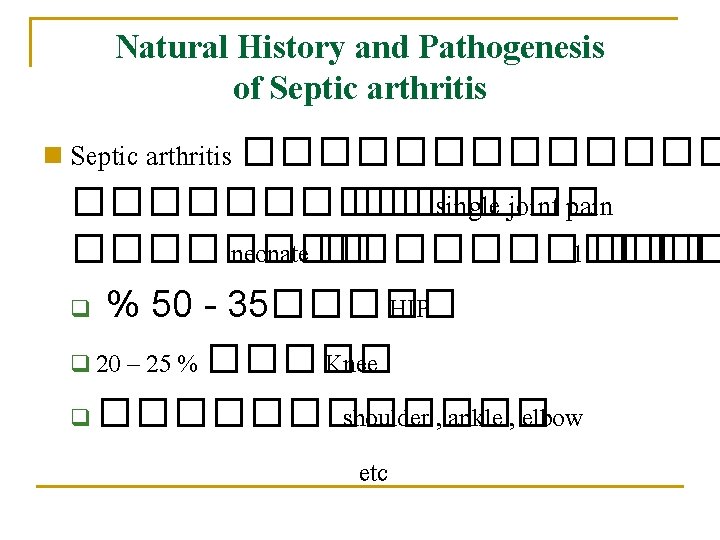
Natural History and Pathogenesis of Septic arthritis n Septic arthritis �������������� single joint pain ���� neonate ������ 1 ��� q % 50 - 35����� HIP q 20 – 25 % ����� Knee q ������ shoulder , ankle , elbow etc
Source of infection n Same as hematogenous osteomyelitis : Blood circulation q Post operation q Skin and tissue infection etc. q
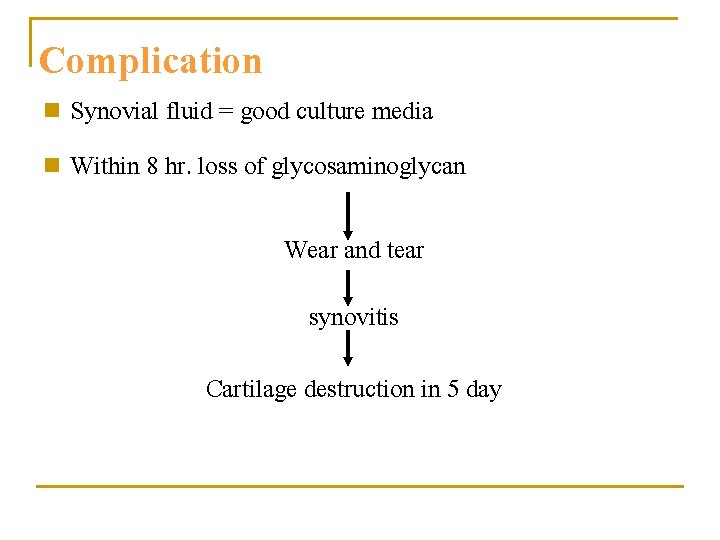
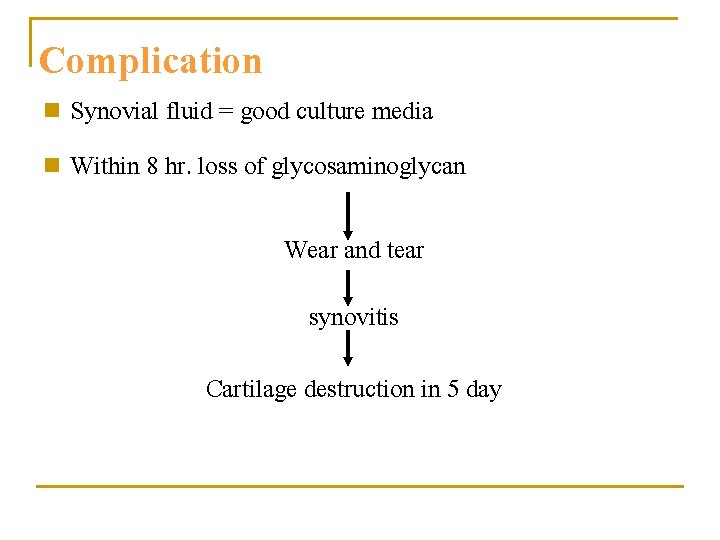
Complication n Synovial fluid = good culture media n Within 8 hr. loss of glycosaminoglycan Wear and tear synovitis Cartilage destruction in 5 day
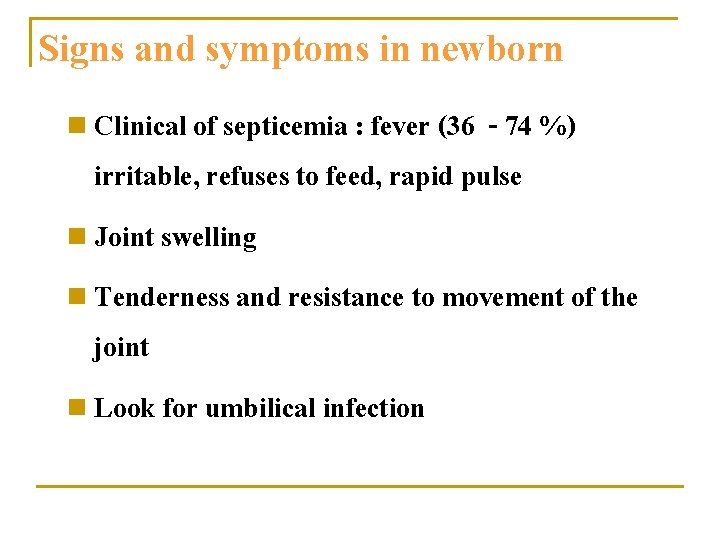
Signs and symptoms in newborn n Clinical of septicemia : fever (36 - 74 %) irritable, refuses to feed, rapid pulse n Joint swelling n Tenderness and resistance to movement of the joint n Look for umbilical infection
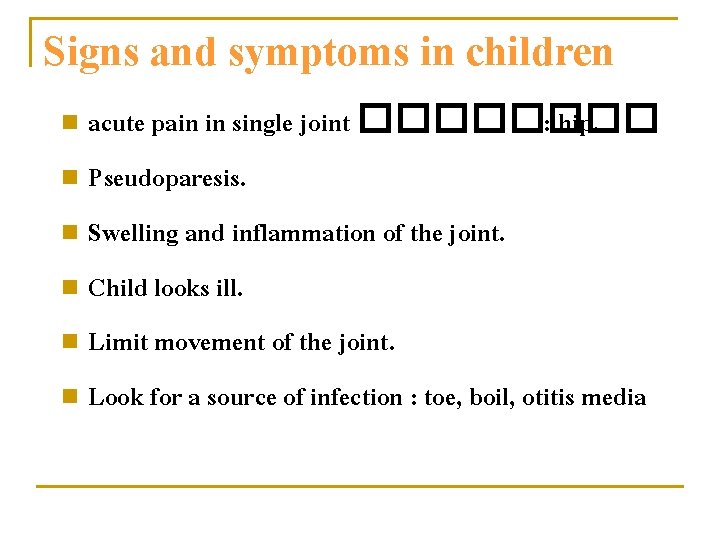
Signs and symptoms in children acute pain in single joint ���� : hip. n Pseudoparesis. n Swelling and inflammation of the joint. n Child looks ill. n Limit movement of the joint. n Look for a source of infection : toe, boil, otitis media n
Diff. diagnosis Toxic synovitis ������� direction �������� Rolling test ��������� flex ����� , extend ���� rotate ���������� n Toxic synovitis ( transient synovitis ) ���������� Rolling test ����������� internal ratation n Juvenile rheumatoid arthritis ������ ������������������� look sick n
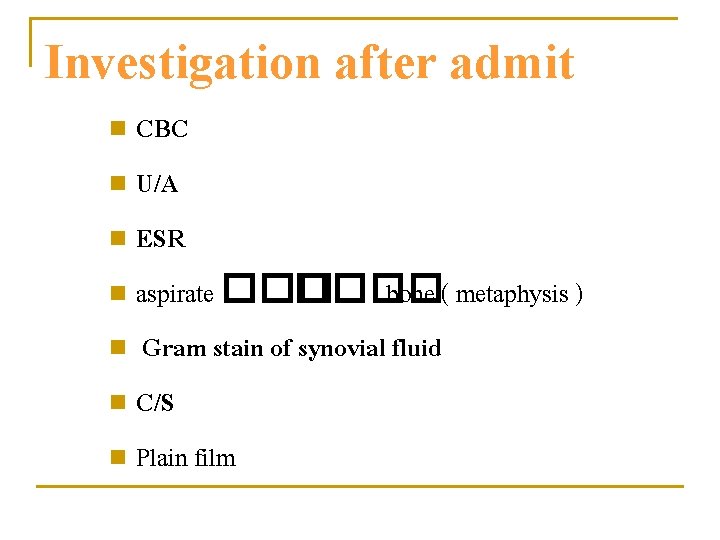
Investigation after admit CBC n U/A n ESR n aspirate ���� bone ( metaphysis ) n Gram stain of synovial fluid n C/S n Plain film n
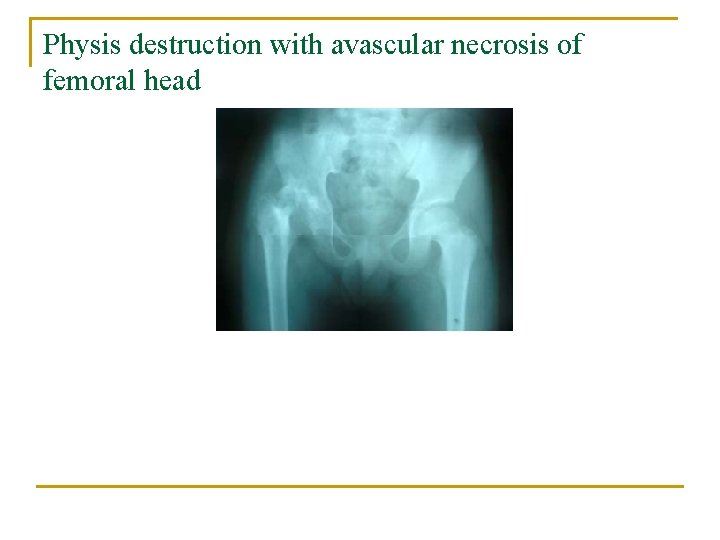
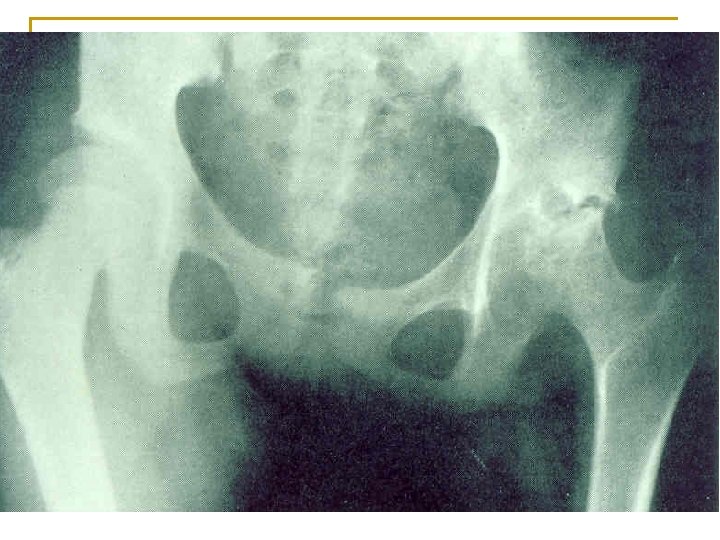
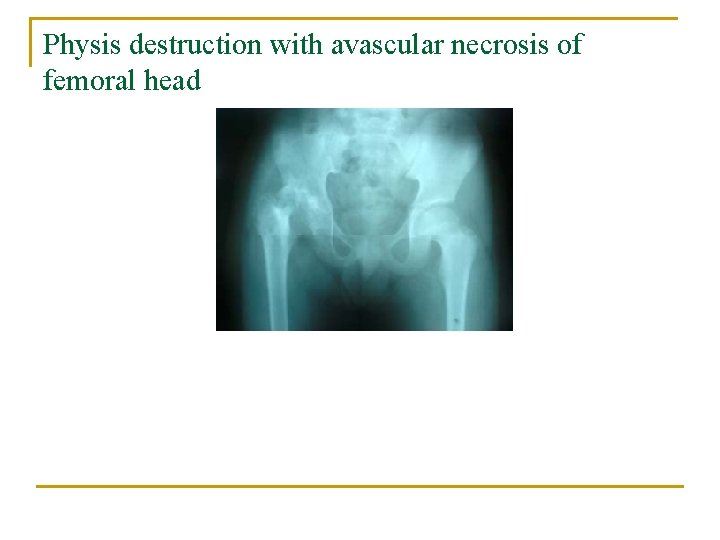
Physis destruction with avascular necrosis of femoral head
Investigation : Plain film ��������� 10 ��� Ø ���� periosteal new bone formation rarefaction, area of lytic and sclerotic lesion, sequestrum and involucrum. Ø ����������������� ��� X-ray Ø

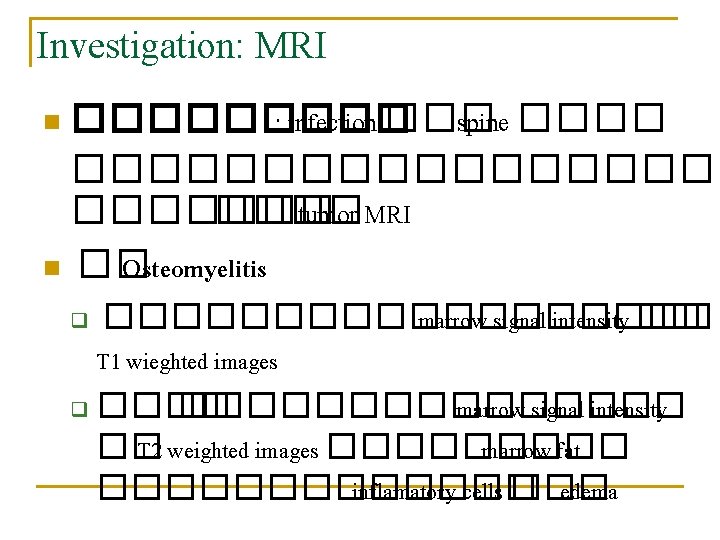
Investigation: MRI ����� : infection ��� spine ����������� tumor MRI n �� Osteomyelitis n ��������� marrow signal intensity �� T 1 wieghted images q ���������� marrow signal intensity �� T 2 weighted images ����� marrow fat ������� inflamatory cells ��� edema q
Investigation: CT scan n ���� extent ��� bone destruction �������� exposure ���� Osteomyelitis ��� spine ���� pelvis
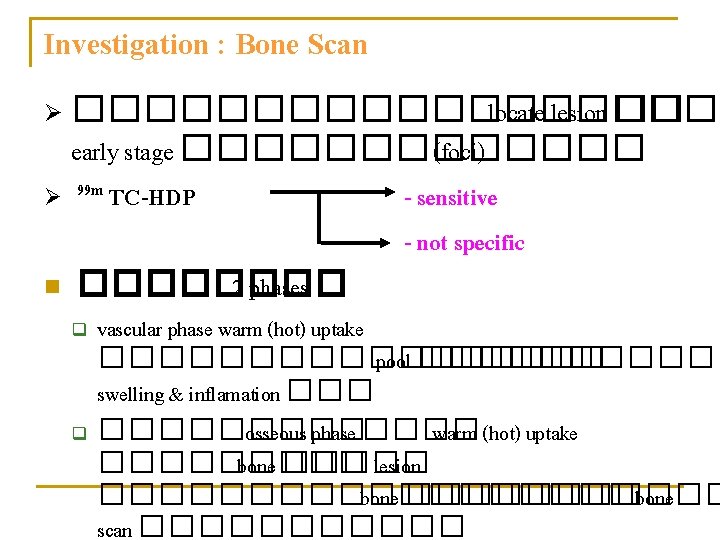
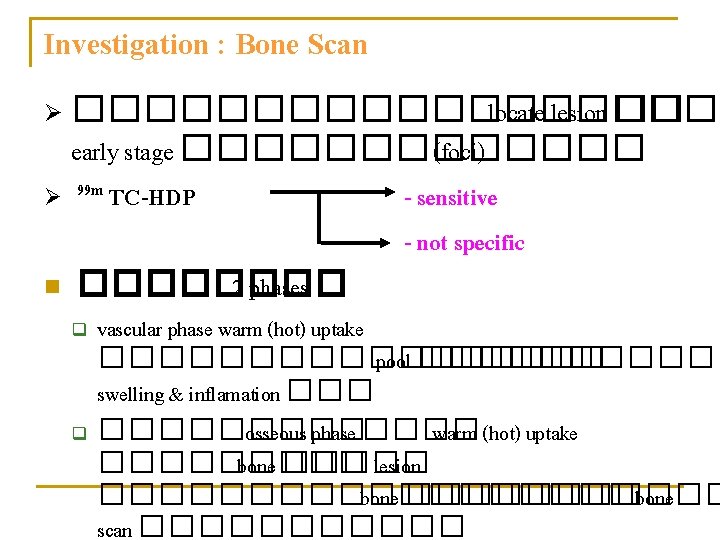
Investigation : Bone Scan Ø ���������� locate lesion �� early stage ������� (foci) Ø 99 m TC-HDP n ���� 2 phases q q - sensitive - not specific vascular phase warm (hot) uptake ��������� pool ������ swelling & inflamation ��������� osseous phase ���� warm (hot) uptake ����� bone ����� lesion ��������� bone scan ������
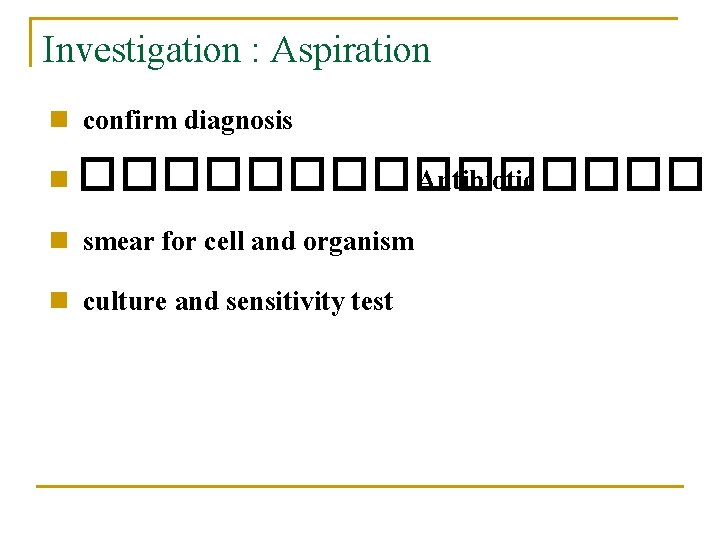
Investigation : Aspiration confirm diagnosis n �������� Antibiotic n smear for cell and organism n culture and sensitivity test n
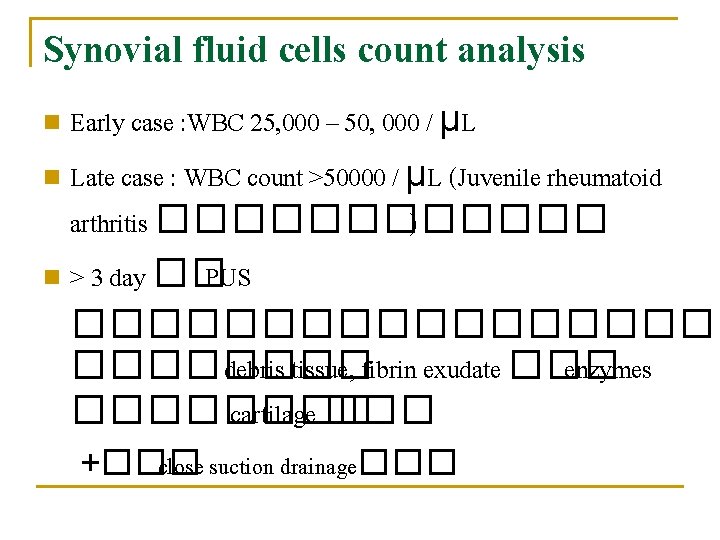
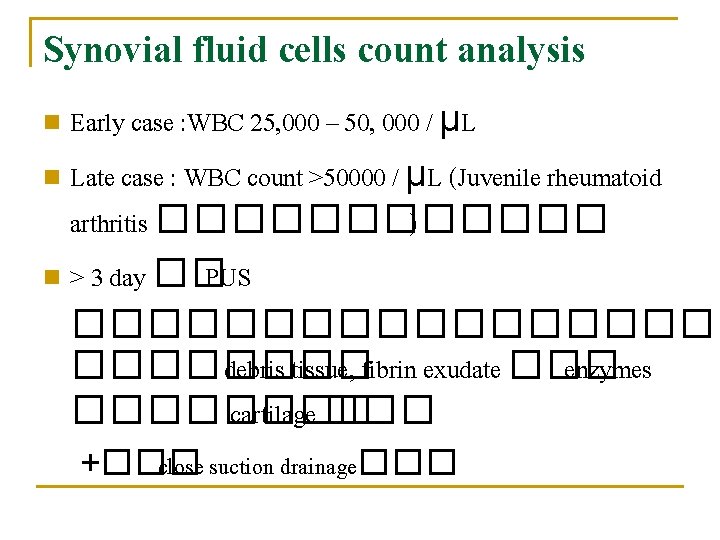
Synovial fluid cells count analysis Early case : WBC 25, 000 – 50, 000 / μL n Late case : WBC count >50000 / μL (Juvenile rheumatoid arthritis ������ ) n > 3 day �� PUS ��������� debris tissue, fibrin exudate ��� enzymes ���� cartilage ��� n +��� close suction drainage���
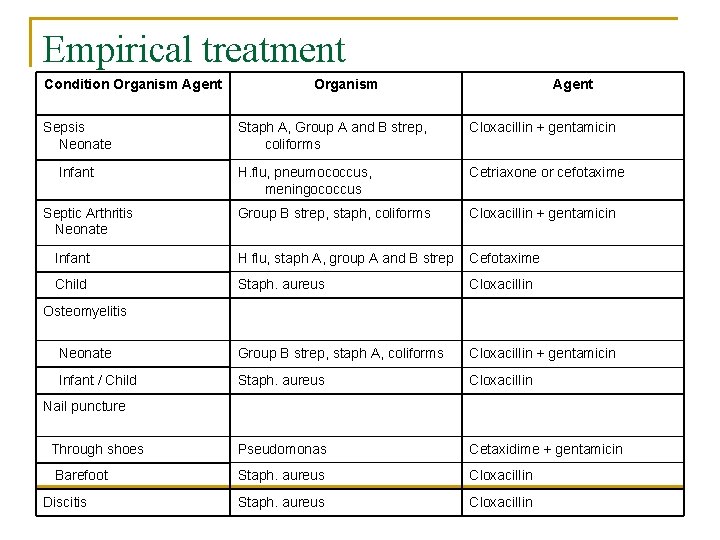
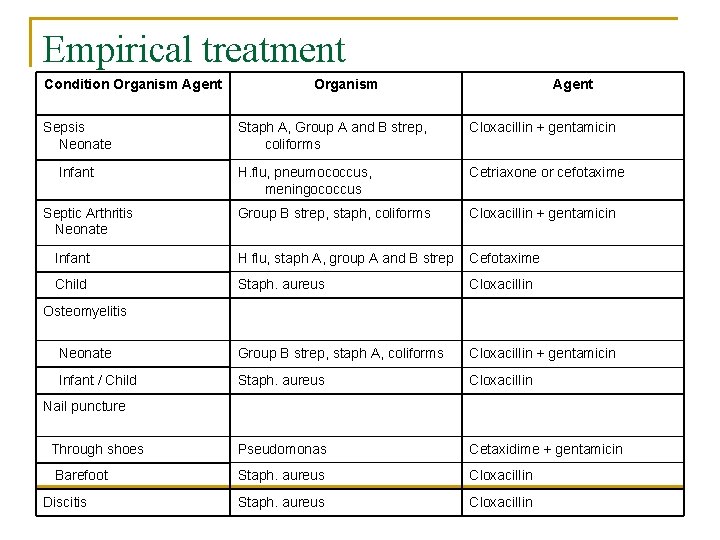
Empirical treatment Condition Organism Agent Sepsis Neonate Organism Agent Staph A, Group A and B strep, coliforms Cloxacillin + gentamicin H. flu, pneumococcus, meningococcus Cetriaxone or cefotaxime Group B strep, staph, coliforms Cloxacillin + gentamicin Infant H flu, staph A, group A and B strep Cefotaxime Child Staph. aureus Cloxacillin Neonate Group B strep, staph A, coliforms Cloxacillin + gentamicin Infant / Child Staph. aureus Cloxacillin Through shoes Pseudomonas Cetaxidime + gentamicin Barefoot Staph. aureus Cloxacillin Infant Septic Arthritis Neonate Osteomyelitis Nail puncture Discitis
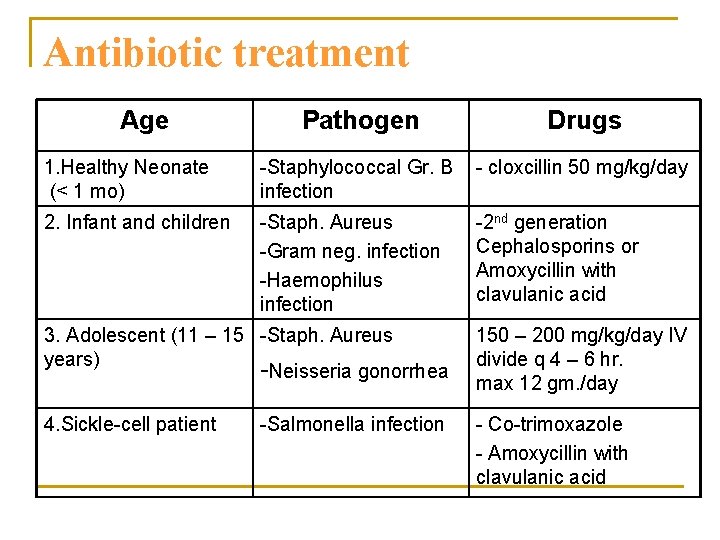
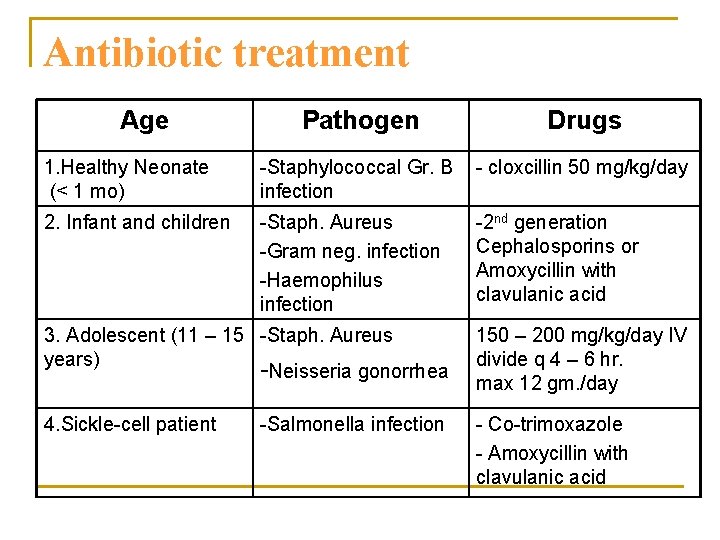
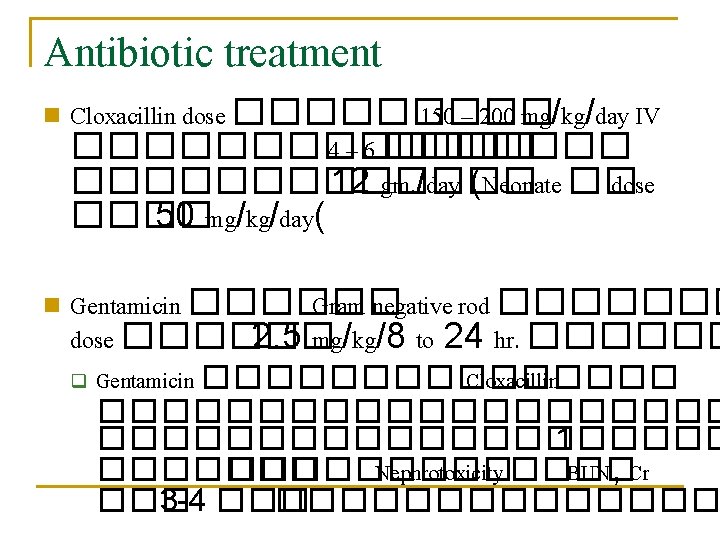
Antibiotic treatment Age Pathogen Drugs 1. Healthy Neonate (< 1 mo) -Staphylococcal Gr. B infection - cloxcillin 50 mg/kg/day 2. Infant and children -Staph. Aureus -Gram neg. infection -Haemophilus infection -2 nd generation Cephalosporins or Amoxycillin with clavulanic acid 3. Adolescent (11 – 15 -Staph. Aureus years) -Neisseria gonorrhea 150 – 200 mg/kg/day IV divide q 4 – 6 hr. max 12 gm. /day 4. Sickle-cell patient - Co-trimoxazole - Amoxycillin with clavulanic acid -Salmonella infection
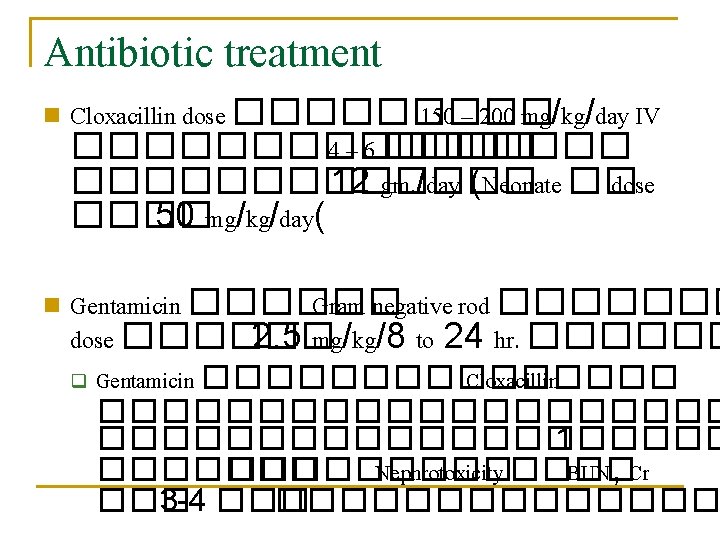
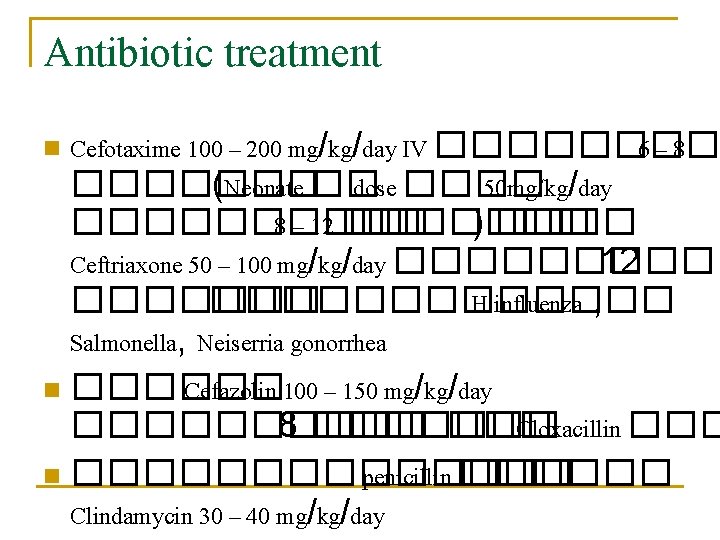
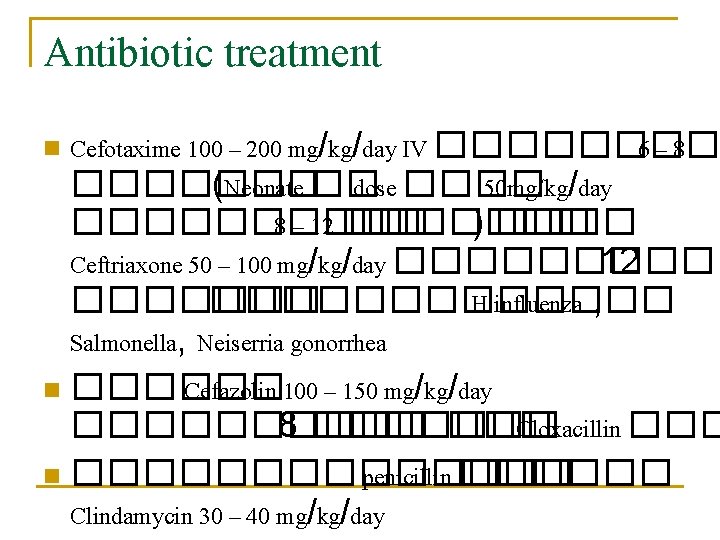
Antibiotic treatment Cefotaxime 100 – 200 mg/kg/day IV ���� 6– 8 ������� (Neonate �� dose ���� 50 mg/kg/day ����� 8 – 12 ������� ) ���� Ceftriaxone 50 – 100 mg/kg/day ����� 12 ������������� H. influenza , Salmonella, Neiserria gonorrhea n ������ Cefazolin 100 – 150 mg/kg/day ����� 8 ������� Cloxacillin ������� penicillin ������ Clindamycin 30 – 40 mg/kg/day n
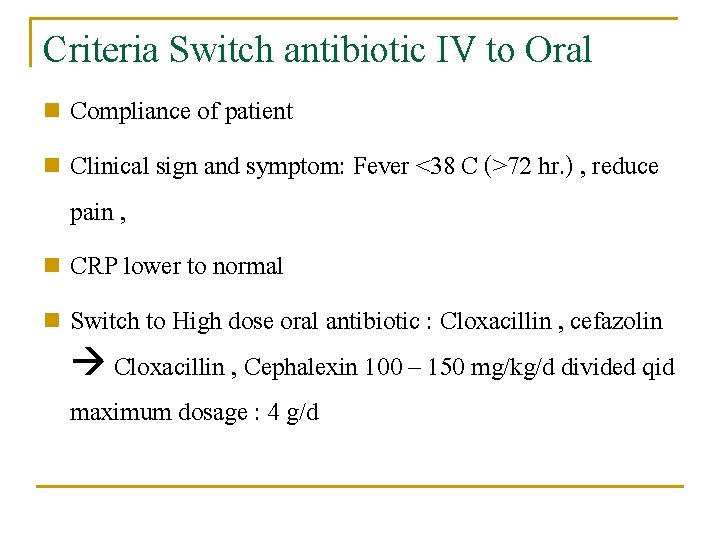
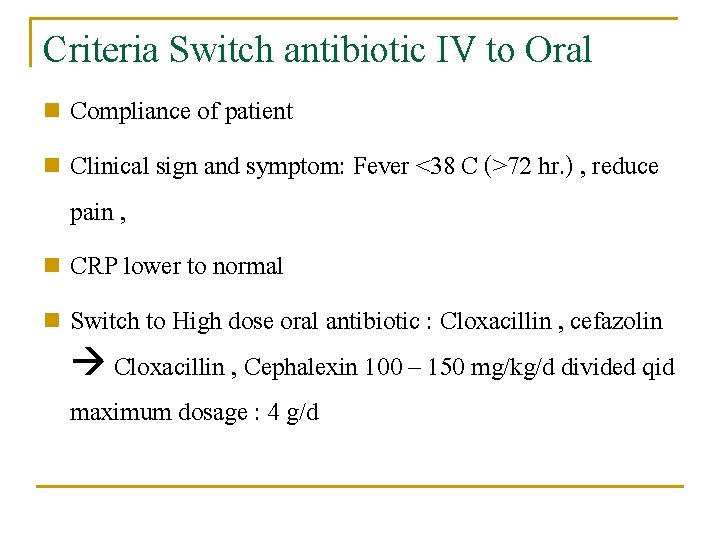
Criteria Switch antibiotic IV to Oral Compliance of patient n Clinical sign and symptom: Fever <38 C (>72 hr. ) , reduce pain , n CRP lower to normal n Switch to High dose oral antibiotic : Cloxacillin , cefazolin Cloxacillin , Cephalexin 100 – 150 mg/kg/d divided qid maximum dosage : 4 g/d n
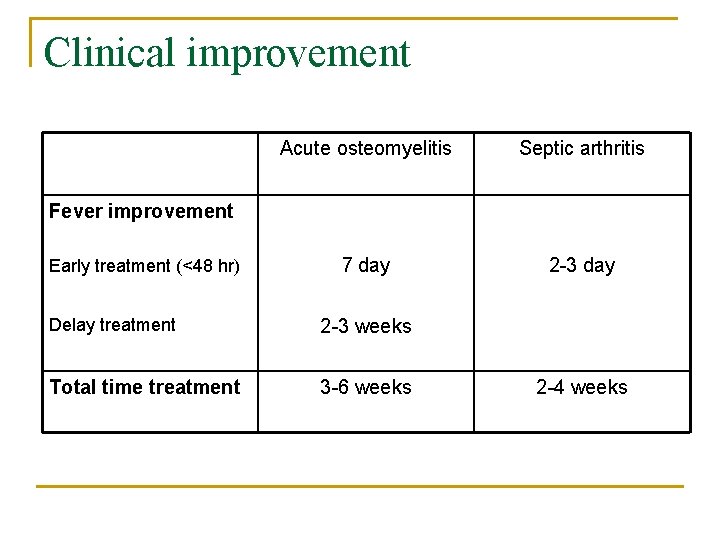
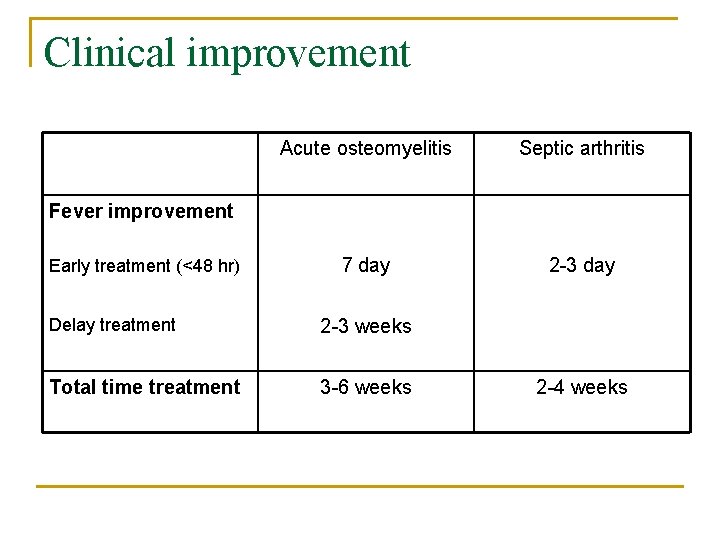
Clinical improvement Acute osteomyelitis Septic arthritis 7 day 2 -3 day Fever improvement Early treatment (<48 hr) Delay treatment 2 -3 weeks Total time treatment 3 -6 weeks 2 -4 weeks
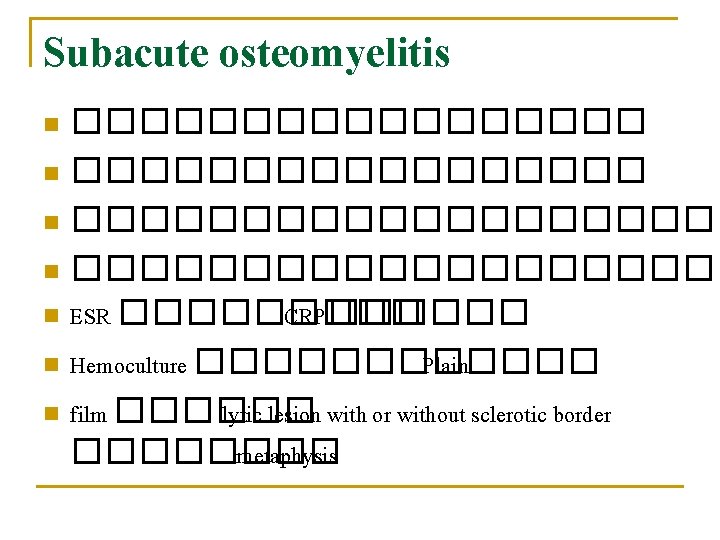
Subacute osteomyelitis ����������������� n �������������������� n ESR ����� CRP������ n Hemoculture ������ Plain n film ������ lytic lesion with or without sclerotic border ���� metaphysis n
Chronic osteomyelitis n n ����� delay diagnosis and treatment ��� Acute osteomyelitis ������� sequestrum, involucrum ��� chronic sinus drainage ����� sequestrum ������� plain film ������ debridement, sequestrectomy, saucerization n ����������� IV pre OP ��� post OP ������ 7 ��������� high dose ���� 6 ������� ESR < 25 ������� remove sequestrum ���� dead bone ����� blood supply ����� phagocytic cells ����������� n
Thank you for your attention
 Hypoandrogenism
Hypoandrogenism Septic arthritis complications
Septic arthritis complications Septic arthritis antibiotics
Septic arthritis antibiotics Septic arthritis antibiotics
Septic arthritis antibiotics Septic arthritis complications
Septic arthritis complications Bakgil
Bakgil Haemophilus influenzae septic arthritis
Haemophilus influenzae septic arthritis Haemophilus influenzae
Haemophilus influenzae Streptococcus gram negative
Streptococcus gram negative Septic workup
Septic workup Jean luc meynard
Jean luc meynard Sickle cell osteomyelitis
Sickle cell osteomyelitis Necrotikus
Necrotikus Osteomyelitits
Osteomyelitits Involucrum osteomyelitis
Involucrum osteomyelitis Involucrum osteomyelitis
Involucrum osteomyelitis Tuberculous osteomyelitis
Tuberculous osteomyelitis Albuminous osteomyelitis
Albuminous osteomyelitis Jea septic tank phase out
Jea septic tank phase out Septic tank contamination groundwater
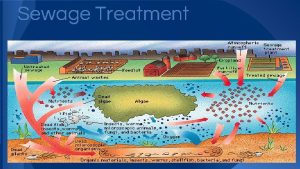
Septic tank contamination groundwater Indianapolis septic tank elimination program
Indianapolis septic tank elimination program Septic squeeze test tonsillitis
Septic squeeze test tonsillitis Advantex ax20 price
Advantex ax20 price Barnstable county septic loan
Barnstable county septic loan Septic implantation syndrome
Septic implantation syndrome Panhandle health septic
Panhandle health septic Bat septic
Bat septic Multiflow septic system
Multiflow septic system Puraflo peat septic system
Puraflo peat septic system Doc's septic tank cleaning
Doc's septic tank cleaning Chemical oxygen demand principle
Chemical oxygen demand principle Septic spleen
Septic spleen Septic
Septic Summit county septic permit
Summit county septic permit Admixtures
Admixtures Nitrex
Nitrex Zveren
Zveren Allergies and arthritis
Allergies and arthritis Osteoarthritis vs rheumatoid arthritis
Osteoarthritis vs rheumatoid arthritis Arthritis and food allergies
Arthritis and food allergies Complication of hydrocephalus
Complication of hydrocephalus Plot of the necklace
Plot of the necklace Complication of gestational diabetes
Complication of gestational diabetes Scqa
Scqa