Osteomyelitis Epidemiology Osteomyelitis and suppurative arthritis are most


- Slides: 45
Osteomyelitis
Epidemiology. • Osteomyelitis and suppurative arthritis are most common in young children – 1/3 cases < 2 y/o – 1/2 cases < 5 y/o • boys : girls, usually 2: 1 • 1/3 cases have minor, closed trauma
Etiology. • A microbial etiology is confirmed in about 3/4 of cases of osteomyelitis • Staphylococcus aureus – the most common infecting organism in all age groups • Group B streptococcus and gram-negative enteric bacilli – prominent pathogens in neonates • group A streptococcus – less than 10% of all cases • After 6 yr of age, most are S. aureus
Etiology. • Exclusive. – puncture wounds of the foot: Pseudomonas aeruginosa – sickle cell anemia: Salmonella and S. aureus • other consideration: – penetrating injuries: atypical mycobacteria – Fungal infections usually occur as part of multisystem disseminated disease – Candida osteomyelitis sometimes occursin neonates with indwelling vascular catheters • Primary viral infections of bones--> rare; – but complain of arthralgia or arthritis may be due to immune responce
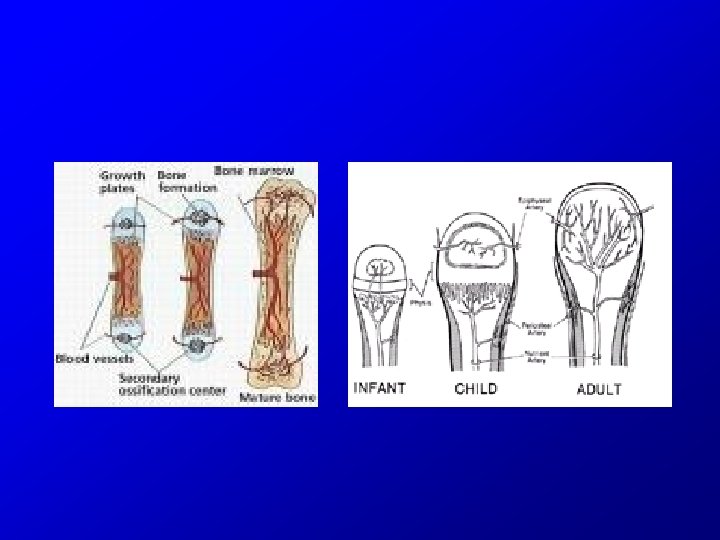
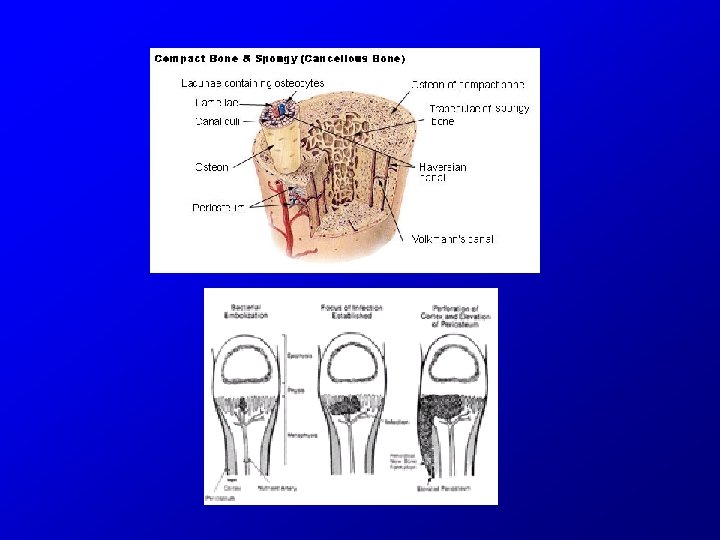
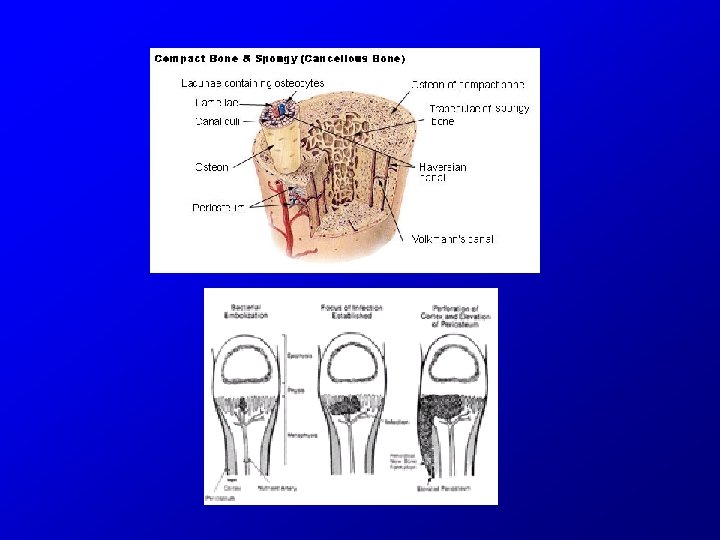
Pathogenesis • In newborns and young infants: – transphyseal blood vessels connect the metaphysis and epiphysis – common for pus from the metaphysis joint space • latter part of the first year of life, the physis forms – obliterating the transphyseal blood vessels • later childhood the periosteum becomes more adherent, – favoring pus to decompress through the periosteum • growth plate closes in late adolescence – begins in the diaphysis, and can spread to the entire intramedullary canal
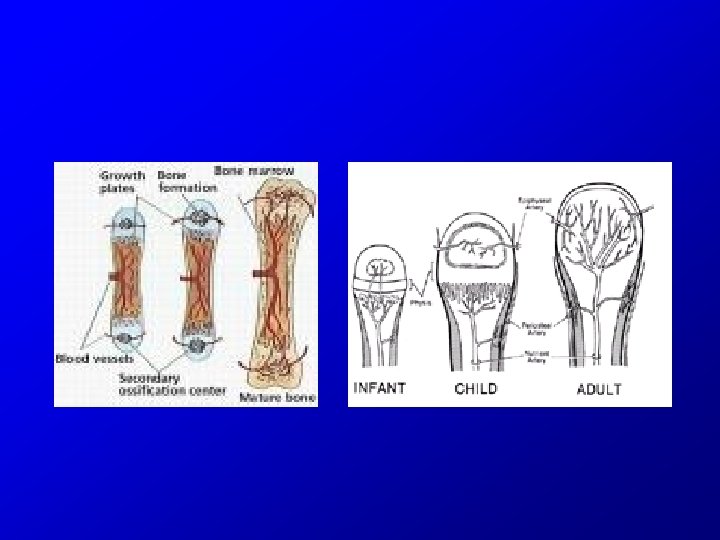
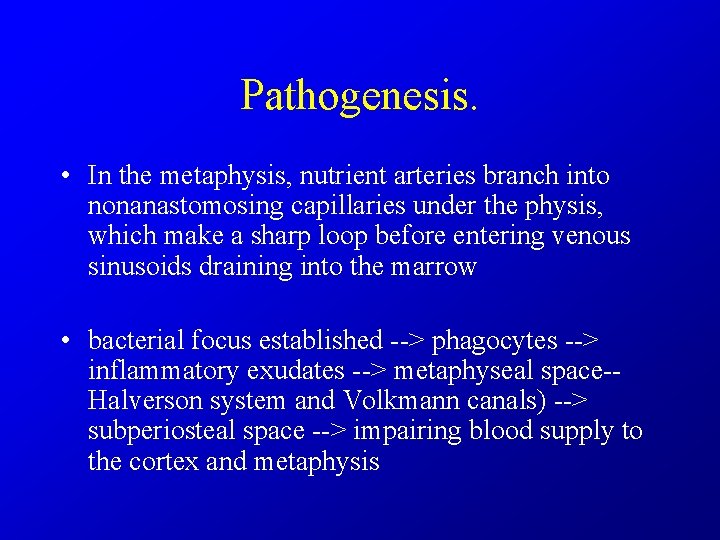
Pathogenesis. • In the metaphysis, nutrient arteries branch into nonanastomosing capillaries under the physis, which make a sharp loop before entering venous sinusoids draining into the marrow • bacterial focus established --> phagocytes --> inflammatory exudates --> metaphyseal space-Halverson system and Volkmann canals) --> subperiosteal space --> impairing blood supply to the cortex and metaphysis
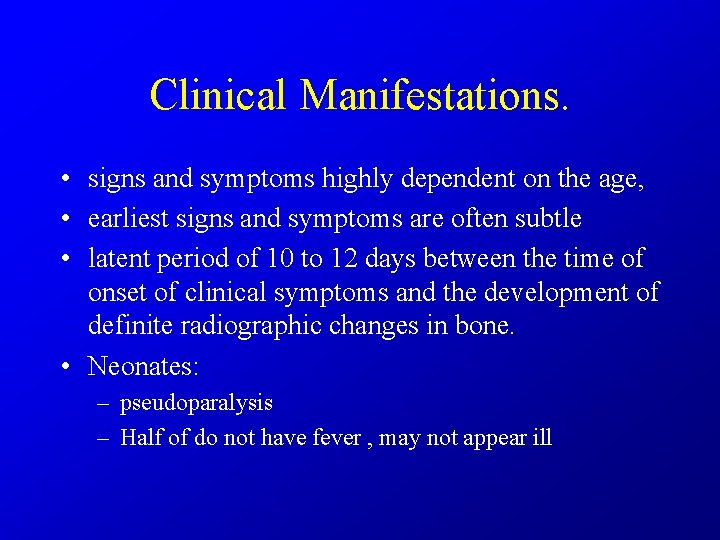
Clinical Manifestations. • signs and symptoms highly dependent on the age, • earliest signs and symptoms are often subtle • latent period of 10 to 12 days between the time of onset of clinical symptoms and the development of definite radiographic changes in bone. • Neonates: – pseudoparalysis – Half of do not have fever , may not appear ill
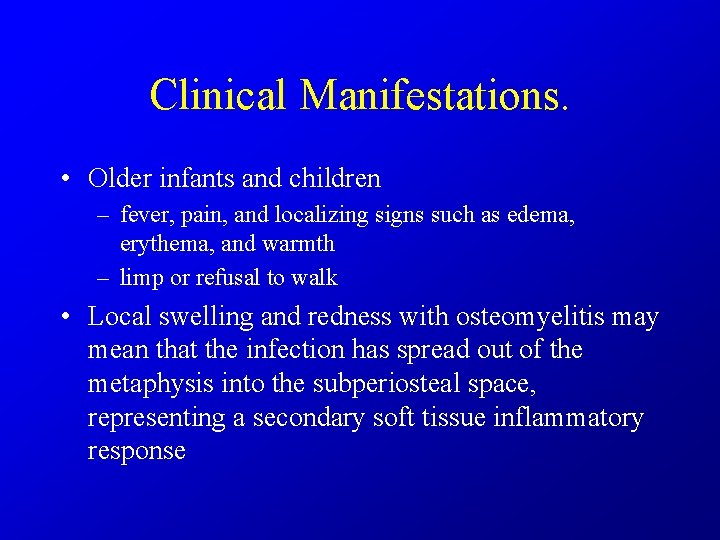
Clinical Manifestations. • Older infants and children – fever, pain, and localizing signs such as edema, erythema, and warmth – limp or refusal to walk • Local swelling and redness with osteomyelitis may mean that the infection has spread out of the metaphysis into the subperiosteal space, representing a secondary soft tissue inflammatory response
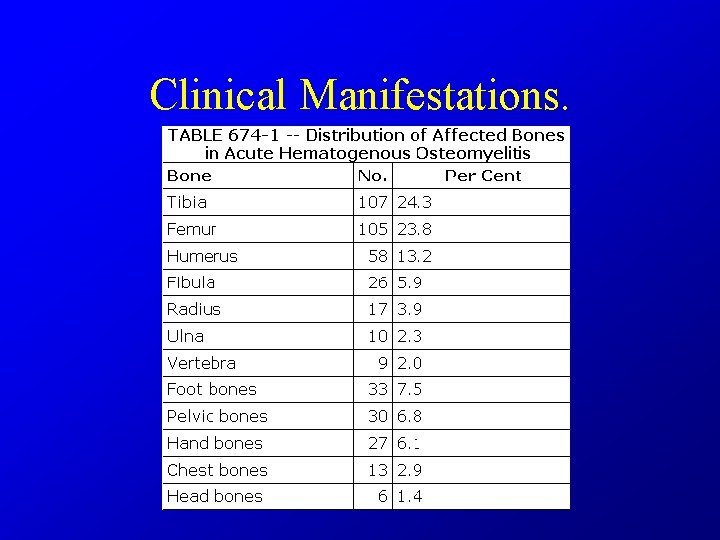
Clinical Manifestations.
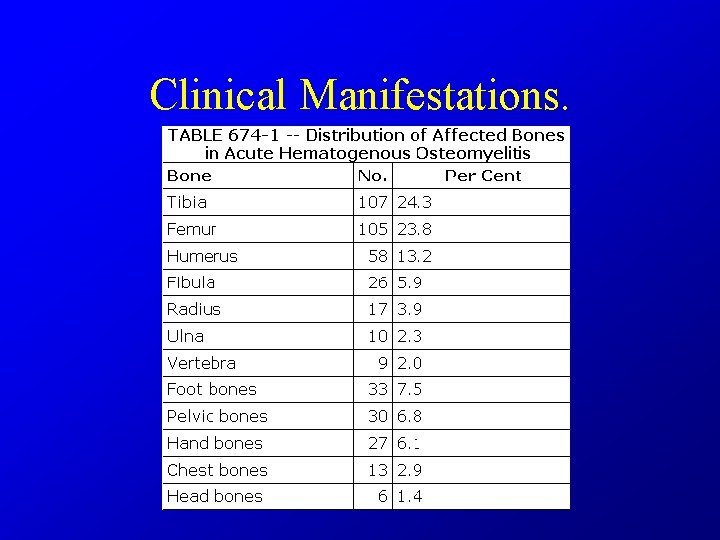
Clinical Manifestations. • upper extremities account for one fourth of all cases. Flat bones are less commonly • Several bones or joints are infected in fewer than 10% of cases – exceptions are gonococcal infections and osteomyelitis in neonates • two or more bones are involved in almost half of the cases
Diagnosis. • Take samples: – Aspiration of the infected site for Gram stain and culture • steel needle is needed to penetrate the cortex into the metaphysis. • If pus is encountered in the subperiosteal space, there is no need to go farther. – If gonococcus is suspected, • cervical, and throat cultures should also be obtained – blood culture should be performed
Diagnosis. • Other Lab. Exam – no specific laboratory tests for osteomyelitis – CBC/DC, ESR, CRP--> very sensitive but not specific – normal test results cannot r/o osteomyelitis – can monitor dz progress
Diagnosis. • RADIOGRAPHIC EVALUATION. • Plain Radiographs. – Within 72 hours of onset of symptoms of osteomyelitis – soft tissue technique, displacement or obliteration of the normal fat planes adjacent to deep muscle – compared to the opposite extremity, – can show displacement of the deep muscle
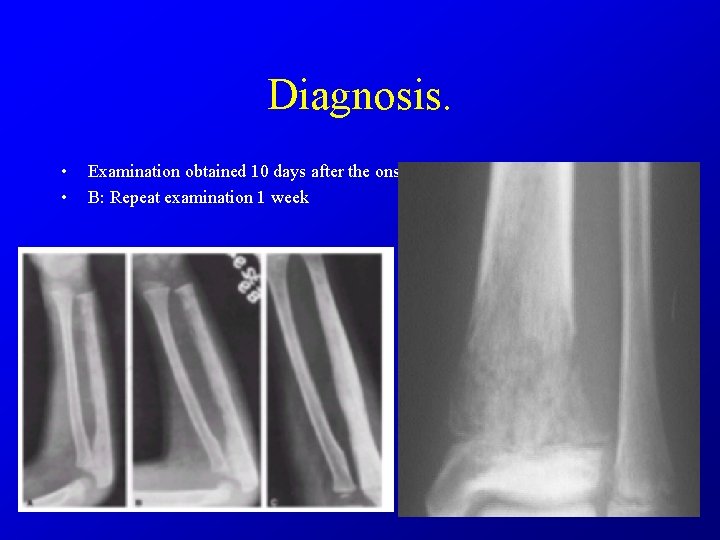
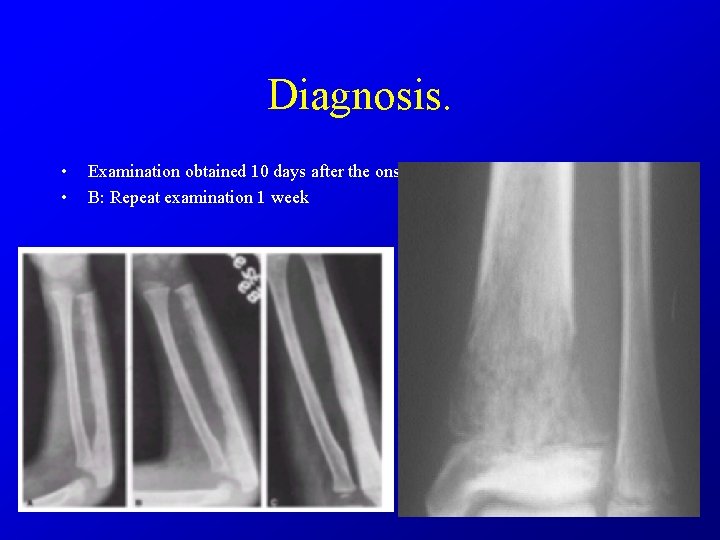
Diagnosis. • • Examination obtained 10 days after the onset B: Repeat examination 1 week
Diagnosis. • Plain Radiographs. – minimal amount of periosteal new-bone formation laid down parallel to the outer margin of the cortex – The actual disease process is usually much more extensive than showed by radiograph
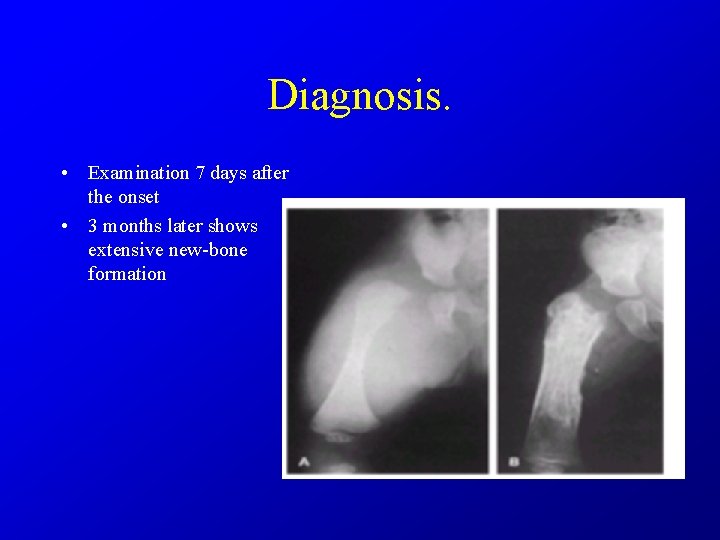
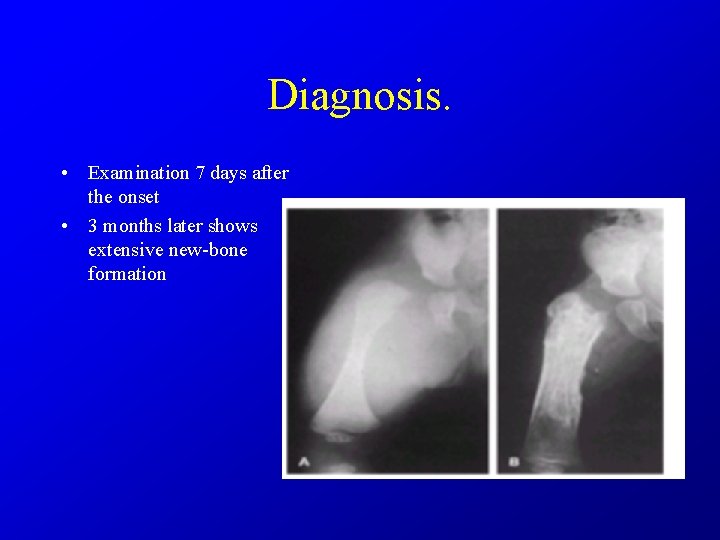
Diagnosis. • Examination 7 days after the onset • 3 months later shows extensive new-bone formation
Diagnosis. • Ultrasonography. – detecting joint effusion and fluid collection in the soft tissue and subperiosteal regions – may guide localization for aspiration or drainage.
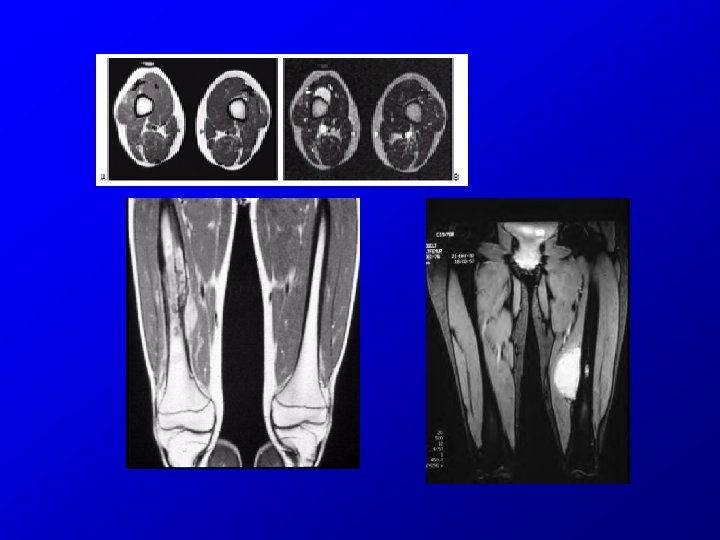
Diagnosis. • Computed Tomography and Magnetic Resonance Imaging. – CT is ideal for detecting gas in soft tissues – Increased attenuation occurs within the bone marrow early in the disease due to edema and pus
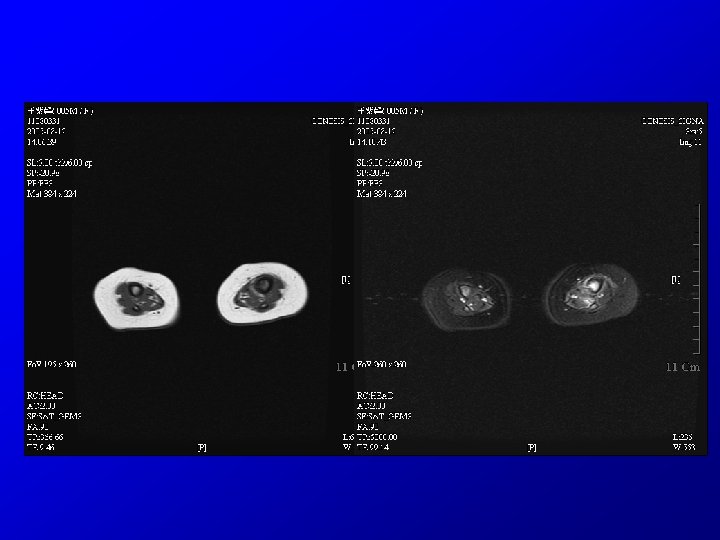
Diagnosis. • MRI is the best radiologic imaging technique for the identification of abscesses and for differentiation between bone and soft tissue infection – acute osteomyelitis, purulent debris and edema appear dark with decreased signal intensity on T 1 weighted images opposite is seen in T 2 weighted images – for possible surgical intervention – MRI is particularly useful in the evaluation of vertebral osteomyelitis and diskitis clear delineation
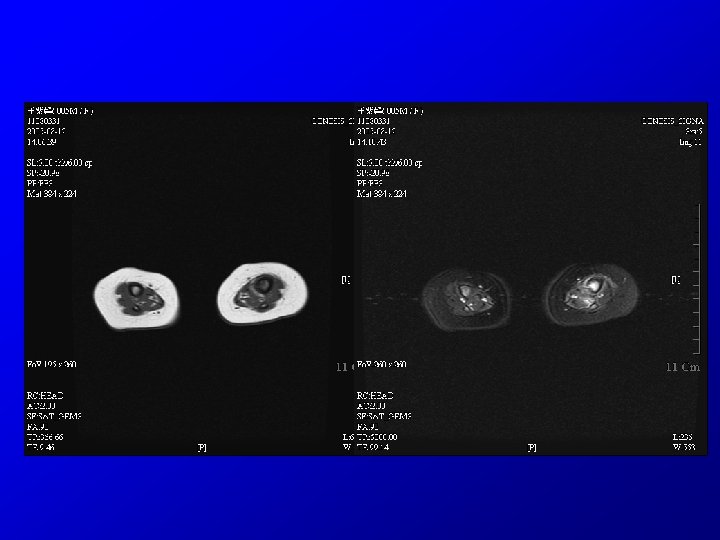
Diagnosis. • MRI – MRI does not reliably distinguish osteomyelitis from noninfectious bone marrow edema – not sensitive to changes within the cortex
Diagnosis. • Radionuclide Studies. – be valuable especially if multiple foci are suspected – Technetium-99 methylene diphosphonate (99 m Tc), which accumulates in areas of increased bone turnover – 99 m. Tc 3 phase perfusion, blood pool, and delayed images – Any areas of increased blood flow or inflammation cause increased uptake of 99 m Tc in the • first phase (5– 10? min) and • second phase (2– 4? hr), • but osteomyelitis causes increased uptake of 99 m Tc in the third phase (24? hr)
Diagnosis. • Radionuclide Studies. – sensitivity (84– 100%) and specificity (70– 96%) – can detect osteomyelitis within 24– 48? hr after onset of symptoms – Gallium-67 uptake, Indium-111 leukocytes is more specific for infection – sensitivity in neonates is much lower owing to poor bone mineralization
Treatment. • Optimal treatment of skeletal infections requires collaborative efforts of pediatricians, orthopedic surgeons, radiologists, and physiatrists • one should not wait for the development of radiographic evidence of disease before treatment • empirical antibiotic – antistaphylococcal penicillin, such as nafcillin or oxacillin, and a broad-spectrum cephalosporin, such as cefotaxime – aminoglycoside may be take place of cephalosporin • but reduced antibacterial activity in sites with decreased oxygen tension and low p. H
Treatment • In infants and children younger than 5 yr of age – Cefuroxime • After 5 yr of age and in the absence of special circumstances – nafcillin or cefazolin • With sickle cell disease , gram-negative enteric bacteria are common – broad-spectrum cephalosporin such as cefotaxime or ceftriaxone
Treatment • When the pathogen is identified, appropriate adjustments in antibiotics are made • If a pathogen is not identified and a patient's condition is not improving – re-aspiration or biopsy – Recheck diagnosis
Treatment • Duration of antibiotic (1) the patient shows prompt resolution of signs and symptoms (within 5– 7 days) and (2) the ESR has normalized; a total of 4– 6 wk of therapy may be required – S. aureus or gram-negative bacillary infections, the minimum duration of antibiotics is 21 days – group A streptococcus, S. pneumoniae, or H. influenzae type b, antibiotics minimum of 10– 14 days – Pseudomonas postoperative need total of 7 d treatment – Immunocompromised, mycobacterial or fungal infection patients generally require prolonged courses
Treatment • Oral route – Changing antibiotics from the intravenous route to oral administration when a patient's condition has stabilized, generally after 1 wk – serum bactericidal titers, or Schlichter titers, 45– 60? min after a dose of suspension or 60– 90? min after a capsule or tablet. • A serum bactericidal titer of 1: 8 or more is considered desirable – ß-lactam drugs for staphylococcal or streptococcal infection, a dosage 2~3 times that used for other infections is prescribed

Treatment • SURGICAL THERAPY. – When frank pus is obtained from subperiosteal or metaphyseal aspiration a surgical drainage procedure is usually indicated. – penetrating injury and when a retained foreign body – Infection of the hip is considered a surgical emergency – chronic osteomyelitis consists of surgical removal of sinus tracts and sequestrum Antibiotic therapy is continued for several months until clinical and radiographic
Prognosis. • Failure to improve or worsening by 72? hr requires review of the appropriateness of the antibiotic therapy • CRP typically normalizes within 7 days after start of treatment; ESR typically rises for 5– 7 days, then falls slowly; dropping sharply after 10– 14 d • Recurrence of disease and development of chronic infection after treatment < 10% of patients • initiation of medical and surgical therapy < 1 wk of onset of symptoms better prognosis
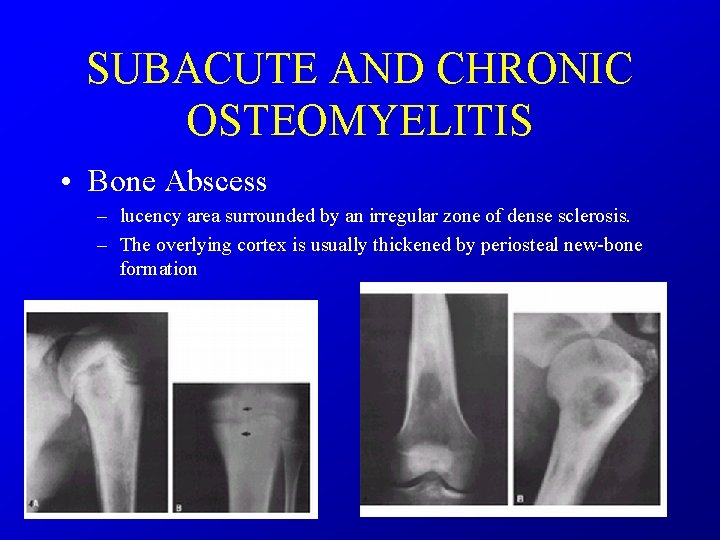
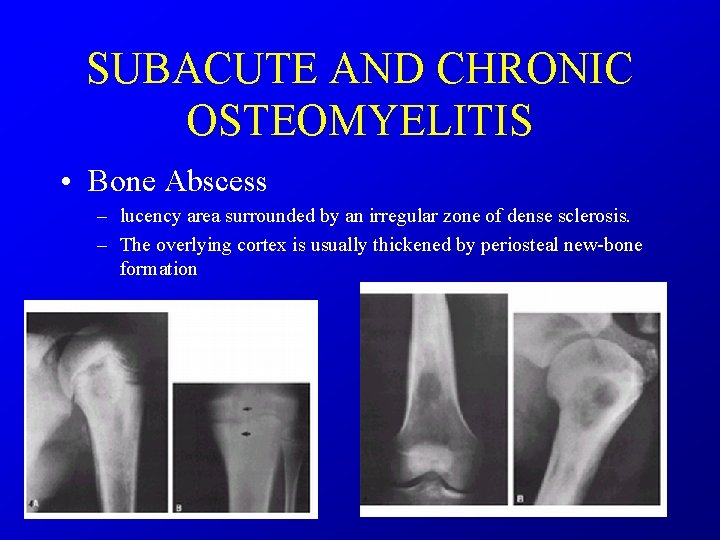
SUBACUTE AND CHRONIC OSTEOMYELITIS • Bone Abscess – lucency area surrounded by an irregular zone of dense sclerosis. – The overlying cortex is usually thickened by periosteal new-bone formation
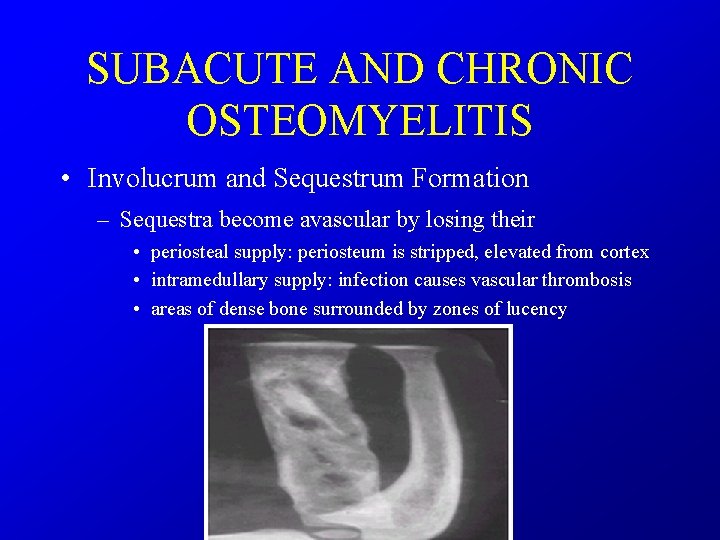
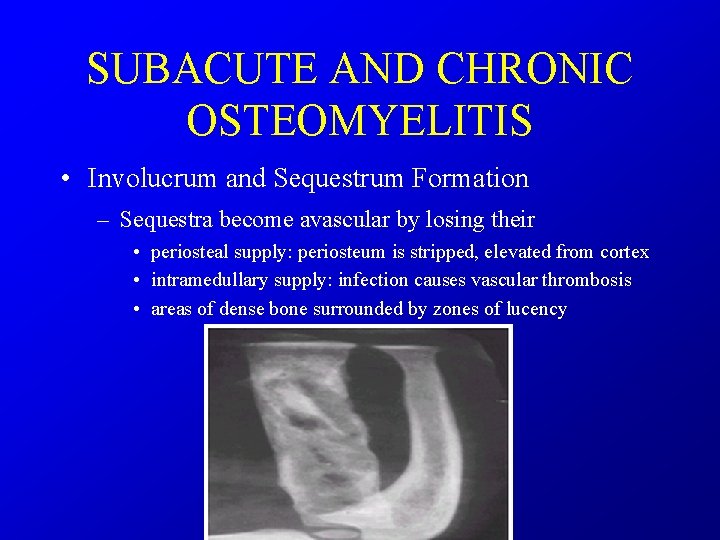
SUBACUTE AND CHRONIC OSTEOMYELITIS • Involucrum and Sequestrum Formation – Sequestra become avascular by losing their • periosteal supply: periosteum is stripped, elevated from cortex • intramedullary supply: infection causes vascular thrombosis • areas of dense bone surrounded by zones of lucency
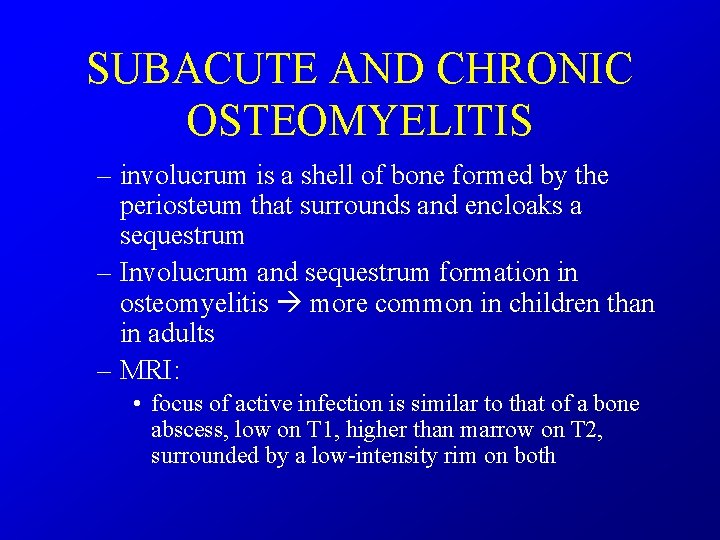
SUBACUTE AND CHRONIC OSTEOMYELITIS – involucrum is a shell of bone formed by the periosteum that surrounds and encloaks a sequestrum – Involucrum and sequestrum formation in osteomyelitis more common in children than in adults – MRI: • focus of active infection is similar to that of a bone abscess, low on T 1, higher than marrow on T 2, surrounded by a low-intensity rim on both
DIFFERENTIAL DIAGNOSIS. • • • trauma Neuroblastoma Primary bone tumors Cellulitis DVT
• Cellulitis – skin infection, soft-tissue swelling is superficial and does not involve the deeper tissues adjacent to the bone.
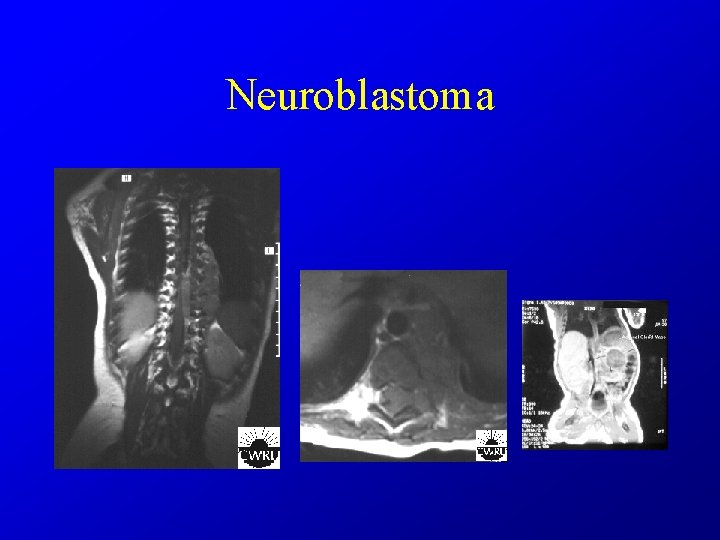
Neuroblastoma – arises from sympathetic nervous tissue, often within the adrenal gland. – A palpable mass in the abdomen may be the first evidence – metastatic neuroblastoma is the most common malignant-appearing tumor before the age of 1 year in bone tumor – Calcification often is visible within the primary tumor
Neuroblastoma • X-ray – cranial sutures are spread – In the skull: Thin, whisker-like calcifications frequently extend out and inward – long tubular bones: • moth-eaten, and the cortex often eroded • Periosteal new-bone formation may parallel the cortex or form thin spiculations at right angles to the cortex – Ewing's tumor, neuroblastoma, and leukemia, may have a similar radiographic appearance, particularly in the long bones.

Neuroblastoma
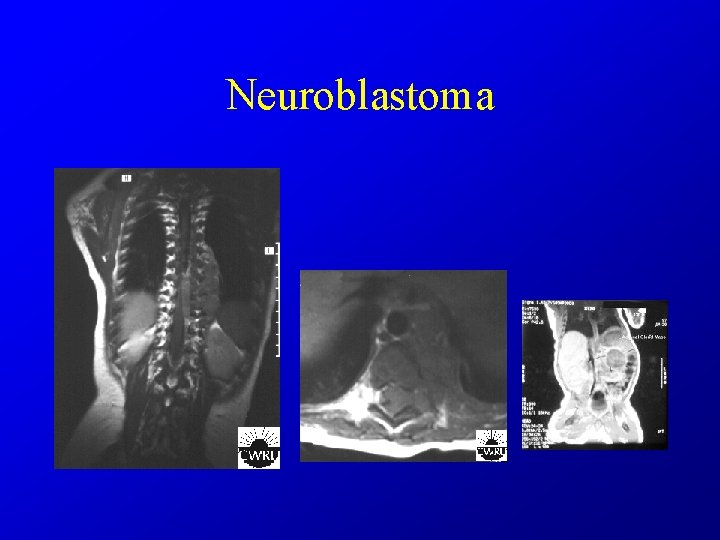
Neuroblastoma
Ewing's tumor • malignant tumor arising in the red bone marrow and closely related histologically to reticulum cell sarcoma • Mostly: 5 ~ 25 y/o ; rarely after 30 y/o; male> female • long bones, extremities, femur, metaphysis – Exception: > 20 y/o, flat bones > long bones • Metastasize easy, multiple lesions may be present • symptoms : pain, swelling; often fever and leukocytosis, like osteomyelitis
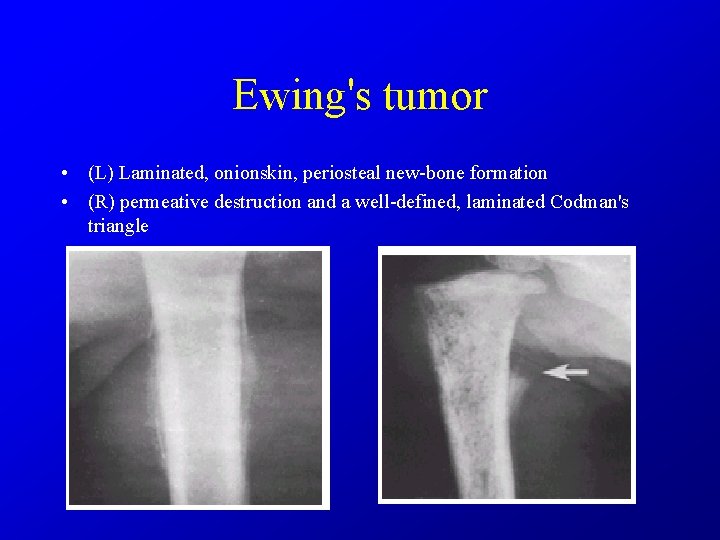
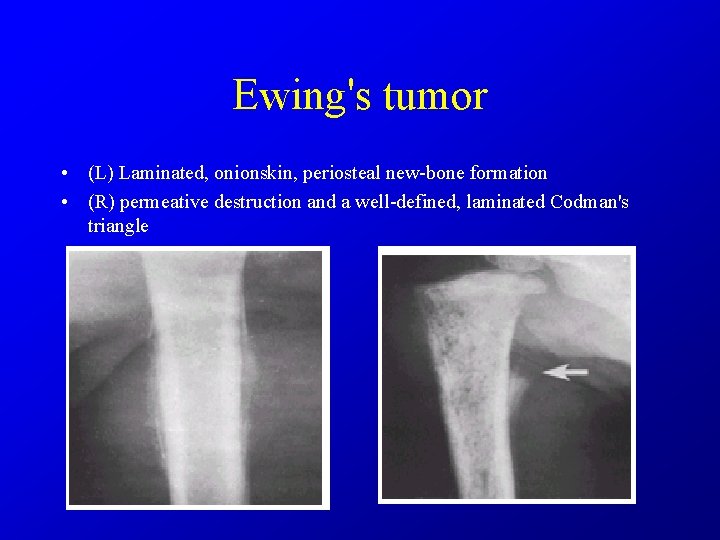
Ewing's tumor • (L) Laminated, onionskin, periosteal new-bone formation • (R) permeative destruction and a well-defined, laminated Codman's triangle
Ewing's tumor • X-ray – permeative, poorly marginated, destructive lesion that perforates the cortex – overlaid by a laminated, , onionskin periosteal reaction – Others may find: Codman's triangles, Fine spicules, – In the long bones, differentiation of Ewing's tumor and osteomyelitis may be difficult
 Insidan region jh
Insidan region jh Tubotympanic
Tubotympanic Foecolith
Foecolith Morphological pattern of acute inflammation
Morphological pattern of acute inflammation Acute suppurative appendicitis
Acute suppurative appendicitis Sickle cell osteomyelitis
Sickle cell osteomyelitis Osteomyelitis rtg
Osteomyelitis rtg Osteomyelitis anatomy
Osteomyelitis anatomy Usurace kosti
Usurace kosti Involucrum osteomyelitis
Involucrum osteomyelitis Tuberculous osteomyelitis
Tuberculous osteomyelitis Albuminous osteomyelitis
Albuminous osteomyelitis Difference between descriptive and analytical epidemiology
Difference between descriptive and analytical epidemiology Define nutritional epidemiology
Define nutritional epidemiology Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Incidence and prevalence meaning
Incidence and prevalence meaning Cbic recertification
Cbic recertification Person place and time model in epidemiology
Person place and time model in epidemiology Osler
Osler Allergies and arthritis
Allergies and arthritis Pictures of rheumatoid arthritis vs osteoarthritis
Pictures of rheumatoid arthritis vs osteoarthritis Arthritis and food allergies
Arthritis and food allergies Ukuran asosiasi dalam epidemiologi
Ukuran asosiasi dalam epidemiologi Logistic regression epidemiology
Logistic regression epidemiology Prevalence calculation example
Prevalence calculation example Cross sectional study advantages and disadvantages
Cross sectional study advantages and disadvantages Attack rate epidemiology formula
Attack rate epidemiology formula Bibliography of epidemiology
Bibliography of epidemiology Association and causation
Association and causation Formula for attack rate
Formula for attack rate Gate frame epidemiology
Gate frame epidemiology Web of causation vs wheel of causation
Web of causation vs wheel of causation Percentage defination
Percentage defination Defination of epidemiology
Defination of epidemiology Endemic definition in community health nursing
Endemic definition in community health nursing What is descriptive study in epidemiology
What is descriptive study in epidemiology Spurious association
Spurious association Field epidemiology ppt
Field epidemiology ppt Level of prevention
Level of prevention Gordon nichols
Gordon nichols Epidemiology kept simple
Epidemiology kept simple Diabetic ketoacidosis epidemiology
Diabetic ketoacidosis epidemiology Distribution in epidemiology
Distribution in epidemiology Effect modification vs confounding
Effect modification vs confounding Distribution in epidemiology
Distribution in epidemiology Ramboman
Ramboman