DISEASES OF THE DIGESTIVE SYSTEM Eman MS Muhammad












- Slides: 64
DISEASES OF THE DIGESTIVE SYSTEM Eman MS Muhammad
DISEASES OF THE INTESTINE
TYPHOID FEVER n n n Definition: Infectious disease caused by Salmonella typhi affecting mainly the lymphoid tissue of the intestine. Mode of Infection: Ingestion of food or drink contaminated by typhoid bacilli from a patient or a carrier. The contamination may be direct or by the way of flies.
n n n Pathogenesis: The bacteria are carried by macrophages from the intestinal lumen to the intestinal lymphoid tissue (Peyer's patches). No local damage or inflammation occurs. The organisms invade the lymphatics to the mesenteric lymph nodes and finally reach the blood stream via the thoracic duct i. e. bacteremia results. Next the bacteria are removed from the blood by the cells of the reticulo-endothelial system (in the liver, spleen, bone marrow. . . etc. ).
n n n The bacteria multiply in the RE cells. By the end of the incubation period (10 -14 days) the RE cells carrying the bacilli undergo necrosis and large number of bacteria enter the blood stream i. e. septicemia. This is accompanied by the development of the pathological lesions. Tissue Reaction: Consists of macrophages (monocytes and histiocytes). The reaction appears to be a delayed hypersensitivity reaction.
Pathological Lesions: I. Intestinal Lesions: n The lesions develop in the lymphoid tissue of the Peyer's patches and solitary follicles. n They are most marked just above the ileo -cecal valve. n The following changes occur: (1) The mucosa and lymphoid tissue become hyperemic. n A large number of macrophages appear among the lymphoid tissue which become swollen and project on the surface. n These changes occur during the first week of the disease. n
(2) Focal necrosis of the covering mucosa occurs. n The foci of necrosis become confluent and end in slough formation. n These changes occur during the second week of the disease. (3) Separation of the slough during the third week of the disease results in ulcer formation. n The ulcer is irregularly oval, raised and its longitudinal axis is parallel to that of the intestine. n The edges are soft and undermined and the floor is smooth and necrotic.
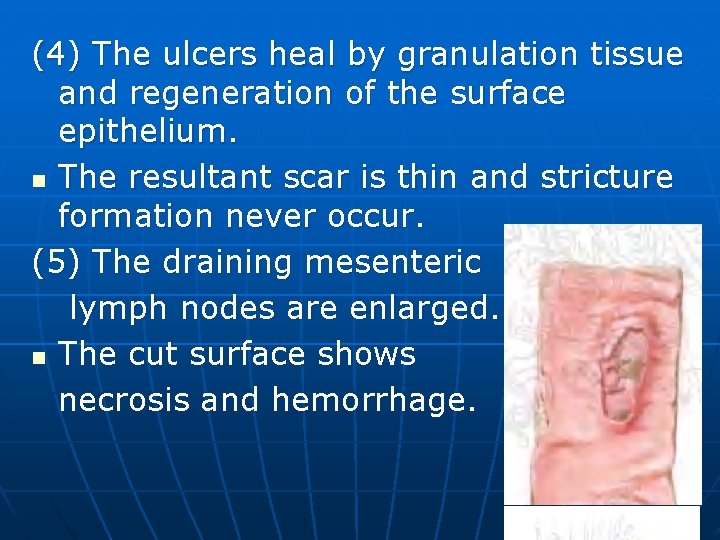
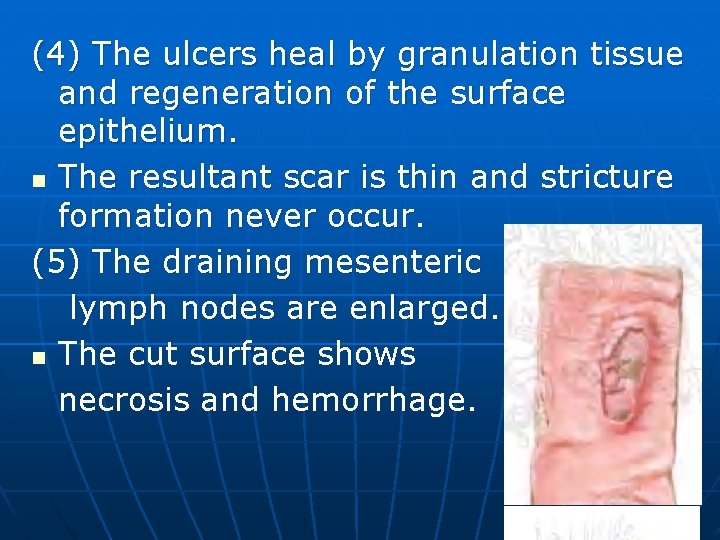
(4) The ulcers heal by granulation tissue and regeneration of the surface epithelium. n The resultant scar is thin and stricture formation never occur. (5) The draining mesenteric lymph nodes are enlarged. n The cut surface shows necrosis and hemorrhage.
II. Extra-intestinal Lesions: (1) Spleen: n Shows the picture of acute splenic swelling. n The organ is moderately enlarged. n The pulp is soft, dark red and shows greyish areas of necrosis. n Microscopically the red pulp is congested and crowded by macrophages. n The lymph follicles are compressed.
(2) Bone marrow: n A tissue reaction composed of macrophages crowds the bone marrow and reduces the formation of the white blood series. n Leucopenia with relative or absolute monocytosis results. (3) Gallbladder: n The typhoid bacilli multiply in the gall bladder and reach the intestine in the bile to be discharged in the stool, so a carrier state may result after recovery. n The bacilli may form a nucleus for gall stone formation (mixed type), and may induce acute or chronic cholecystitis.
(4) Degenerative changes: n Caused by toxemia. n Liver: Cloudy swelling, fatty change and focal necrosis. n Heart: Cloudy swelling, fatty change and dilatation of its cavities. n Muscles: Zenker's degeneration may occur in the rectus abdominus, diaphragm or intercostal muscles. n Vessels: Thrombosis in the leg veins and cerebral sinuses due to toxic endophlebitis. n Skin: Maculopapular rose rashes.
Complications: (1) Intestinal hemorrhage from slough separation in 5 -10%. (2) Septic peritonitis results from perforation of a deep ulcer. (3) Acute heart failure due to toxemia. (4) Bronchopneumonia caused by typhoid bacilli or a mixture of pathogenic bacteria. (5) Cholecystitis, gall stones and Zenker's degeneration. (6) Degenerative changes due to toxemia. (7) Typhoid osteomyelitis, localized periostitis which develops after months or years. (8) Meningitis, encephalitis, neuritis, pyelonephritis and endocarditis. n
DYSENTERY Definition: n Inflammation of the colon characterized by diarrhea, tenesmus and passage of blood and mucous in stool. n Types: n The common types are: (1) Amoebic dysentery (2) Bacillary dysentery (3) Bilharzial dysentery n
(1) AMOEBIC DYSENTERY n n n Etiology: Cause: Intestinal infection by Entamoeba histolytica. Pathogenesis: Infection is by the encysted amoebae transmitted by fresh vegetables, contaminated water or by the house flies. The cyst wall disintegrates in the small intestine due to its alkalinity with the liberation of a four nucleated amoeba which divides into 8 vegetative forms.
n The amoebae pass to the large intestine where fecal stagnation allows them to invade the intestinal mucosa by the aid of their proteolytic and hyaluronidase enzymes.
n n n Gross Picture: The amoebae destroy the mucosa and muscularis mucosa to reach the submucosa mainly in the cecum and rectum where they multiply. In the submucosa they cause marked necrosis by their enzymes. Separation of the necrotic material results in small flask shaped ulcers. They have undermined edges, yellowish necrotic floor and the base is formed of the muscle layer. The mucosa in between the ulcers appears normal.
n n n In the majority of cases healing of the above lesions occurs due to the high body resistance. However the organism may remain in the intestinal tissue and a carrier state results. In 10% of cases the lesions progress and result in round or oval ulcers measuring up to few cm's. The ulcers have undermined edges and variable depths. Healing of these ulcers leaves smooth depressed surface and fibrous stricture may result.

n n n n Microscopic picture: The edges and floor of the ulcers consist of necrotic tissue. The inflammatory cells are few in number and consist of neutrophils and macrophages. The amoebae are present in the tissues and inside the blood vessels. They are rounded or oval, 20 -25 micron, the nucleus is eccentric and measures 2 -5 micron and the cytoplasm contains digestive vacuoles. The amoebae are surrounded by clear rings due to digestion of the surrounding tissues by the proteolytic enzymes. Degenerated and dead amoebae stain red with eosin.

Entamoeba histolytica in colon. High-power view of the organisms.

n Complications of Intestinal Amoebiasis: (1) Ulceration causes intestinal hemorrhage. (2) Perforation of a deep ulcer causes pericolic abscess or diffuse suppurative peritonitis. (3) Abnormal peristalsis may result in intussusception. (4) Continual straining at stool may result in rectal prolapse. (5) Intestinal stricture and chronic intestinal obstruction.
(6) Amoeboma is a granuloma seen in the cecum and rectum as a result of amoebic infection and secondary bacterial infection. (7) Amoebic infection may spread directly to the perianal skin and vagina, and by blood to the liver causing amoebic hepatitis or amoebic abscess. (8) Amoebic lung and brain abscess rarely occur.
AMOEBIC LIVER ABSCESS n n n Etiology: Large number of amoebae reaching the liver from the intestine by the portal blood. Pathological features: Extensive foci of necrosis occur. The necrotic areas undergo softening and liquefaction and coalesce together forming one or more large abscess mostly in the right lobe.
n n n The lining of the abscesses are soft and shreddy, composed of necrotic liver cells amongst which amoebae are present, but cellular infiltration (neutrophils and macrophages) is poor or absent. The abscesses contain thick chocolate colored odorless pus. The pus is composed of necrotic liver cells, fat globules, cholesterol crystals, macrophages, and few neutrophils.
The abscess may show: (1) Secondary bacterial infection which changes it to a septic one. (2) Rupture in the subphrenic space, pleura, lung, pericardium or peritoneum. (3) Obstruct the common bile duct, pylorus or duodenum. (4) Show fibrosis of the wall and calcification of the contents. n
(2) BACILIARY DYSENTERY n Definition: n Pseudo-membranous inflammation of the colon caused by Shigella organisms. n Mode of Infection: n Ingestion of the bacilli in contaminated food or drink. n Contamination is transmitted mainly by flies.
n n n Gross Picture: Early the mucosa of the colon is congested and edematous. Next greyish white patches of necrosis appear. A pseudo-membrane forms on the surface. The membrane may be stained green by bile or dark brown by blood. Separation of parts of the membrane results in small irregular superficial ulcers which may coalesce.
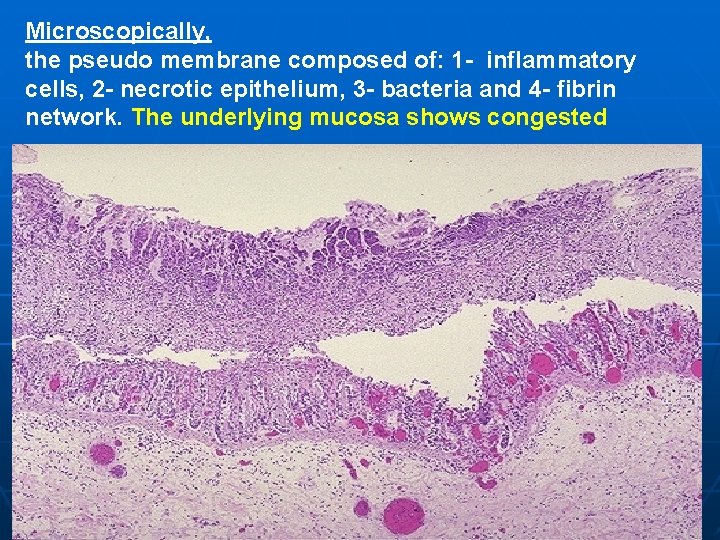
n n n The intestinal lumen contains dark greyish fluid, blood and mucous. The draining lymph nodes are enlarged, soft and hyperemic. Microscopic picture: The surface is covered by a pseudomembrane composed of the bacteria, necrotic mucosa, and acute inflammatory cells held together by fibrin network. The submucosa shows congestion, edema, fibrin network and acute inflammatory cells.
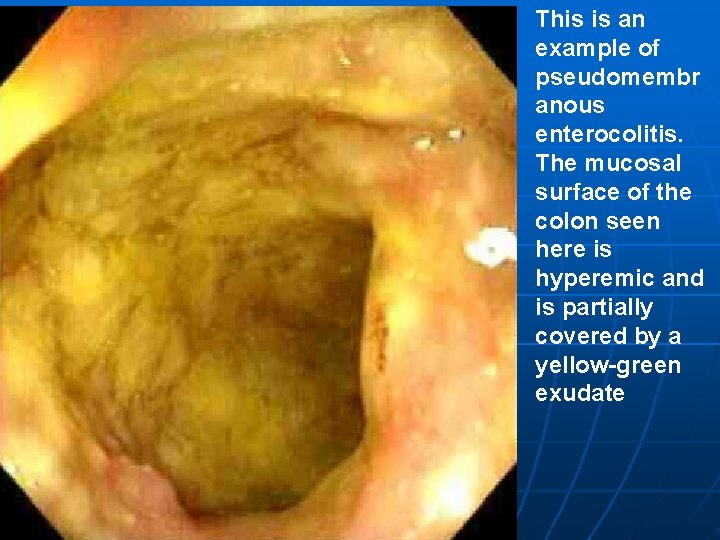
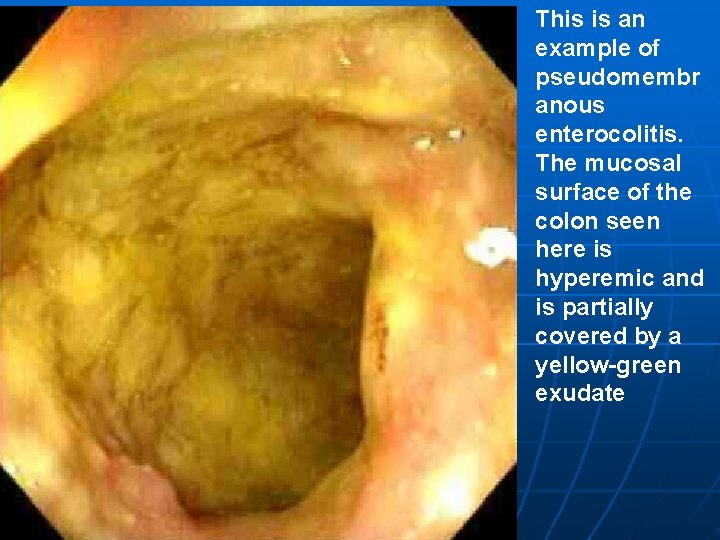
This is an example of pseudomembr anous enterocolitis. The mucosal surface of the colon seen here is hyperemic and is partially covered by a yellow-green exudate
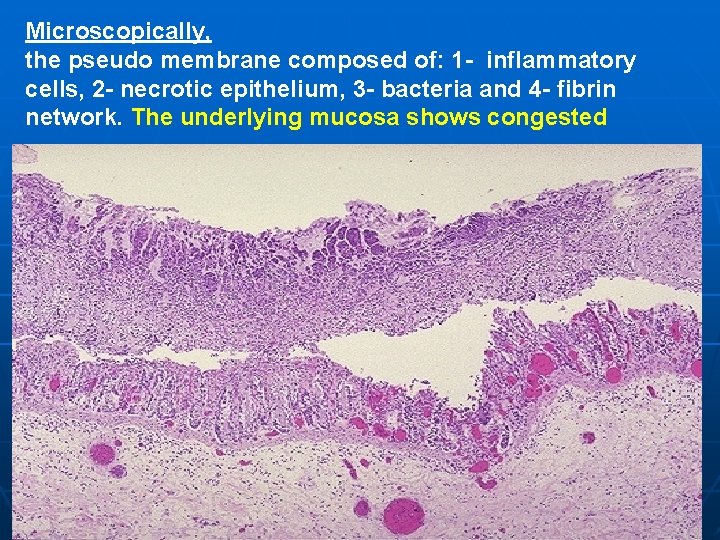
Microscopically, the pseudo membrane composed of: 1 - inflammatory cells, 2 - necrotic epithelium, 3 - bacteria and 4 - fibrin network. The underlying mucosa shows congested
Complications: (1) Intestinal hemorrhage. (2) Perforation and septic peritonitis is rare. (3) Chronicity with secondary bacterial infection. (4) Stenosis of the intestinal lumen due to fibrosis. (5) Toxemia causing acute iritis, acute arthritis, peripheral neuritis, toxic myocarditis and Zenker's degeneration. (6) Prolapse of the rectum due to continuous straining. n
DISEASES OF THE APPENDIX ACUTE APPENDICITIS n Organisms: n Streptococcus pyogenes, staphylococcus aureus and E. coli. n Pathogenesis: (1) Infection usually from the lumen but may be blood borne. (2) Obstruction is present in a large number of cases. n

Obstruction is caused by: (a) The lumen is obstructed by a foreign body as vegetable or fruit seeds or by a foecolith. This is the commonest cause. (b) Hyperplasia and swelling of the submucosal lymphoid tissue. (c) Post-inflammatory fibrosis of the wall. (d) Peritoneal adhesions. (e) Spasm of the muscle coat at the base of the appendix. n
n n n Obstruction causes mucous accumulation in the lumen. The pressure is raised and causes compression and occlusion of the arteries supplying the mucosa. The resulting ischemia causes devitalization of the mucosa and easy invasion by bacteria.

Normal appendix

Acute suppurative appendicitis:
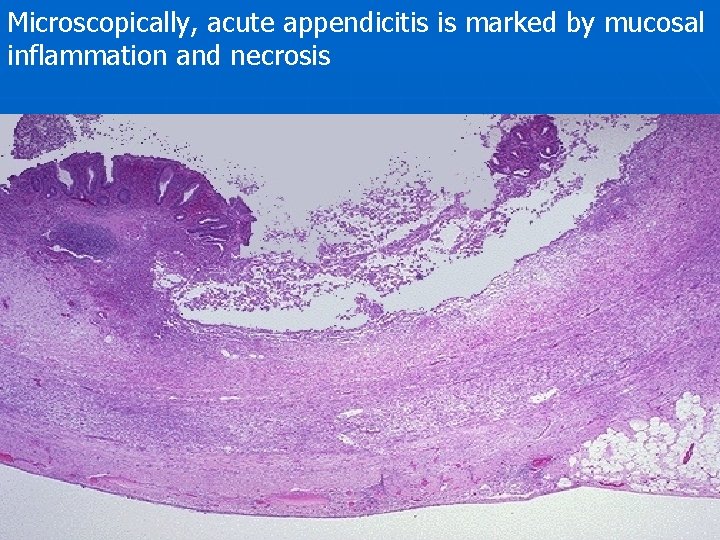
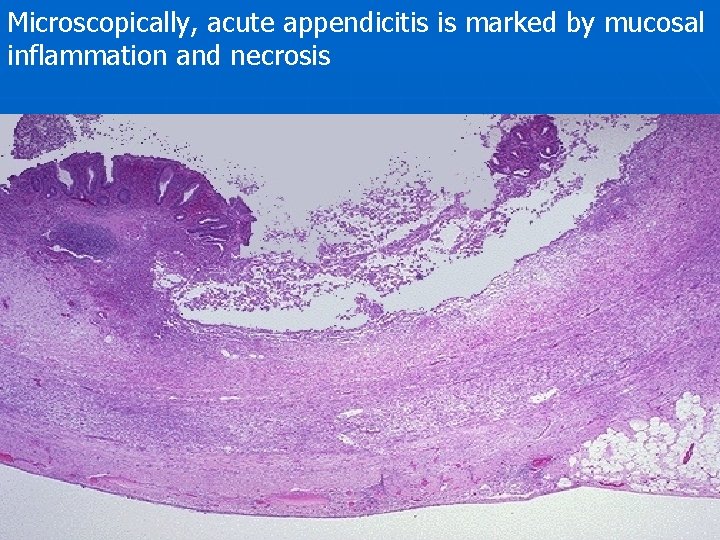
Microscopically, acute appendicitis is marked by mucosal inflammation and necrosis
Pathology: (1) Acute catarrhal appendicitis: n Is the early and mild stage of the disease. n The appendix is slightly swollen and congested. n Microscopically the mucosa and submucosa show hyperemia, edema, infiltration with neutrophils and increased mucous secretion. n At this stage the lesion may regress resulting in minimal fibrosis or pass to the suppurative stage. n
(2) Acute suppurative appendicitis: n Is the common and classic picture of acute appendicitis. n The appendix is elongated, swollen and congested. n The lumen is narrowed and filled with purulent exudate. n The mucosa is hyperemic, edematous and ulcerated. n The outer serosal surface shows dilated congested vessels and yellow patches of purulent exudate.

n n n Microscopically the mucosa shows partial shedding. All coats show hyperemia, inflammatory edema and infiltration by large number of polymorphonuclear leucocytes and pus cell. The omentum and loops of intestine may stuck by fibrinous exudate to the surface of the appendix resulting in a localized inflammatory mass "Appendicular mass. "
n n n The mass may resolve or suppuration occurs with the formation of appendicular abscess. The abscess may resolve or rupture on the abdominal wall, in a loop of intestine or in the peritoneal cavity causing diffuse septic peritonitis. Septic thrombophlebitis occurs in the appendicular vein and may cause portal pyemia.
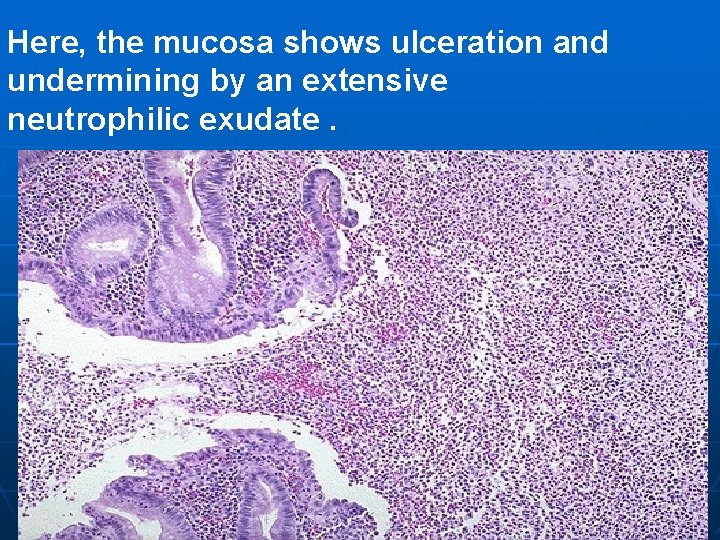
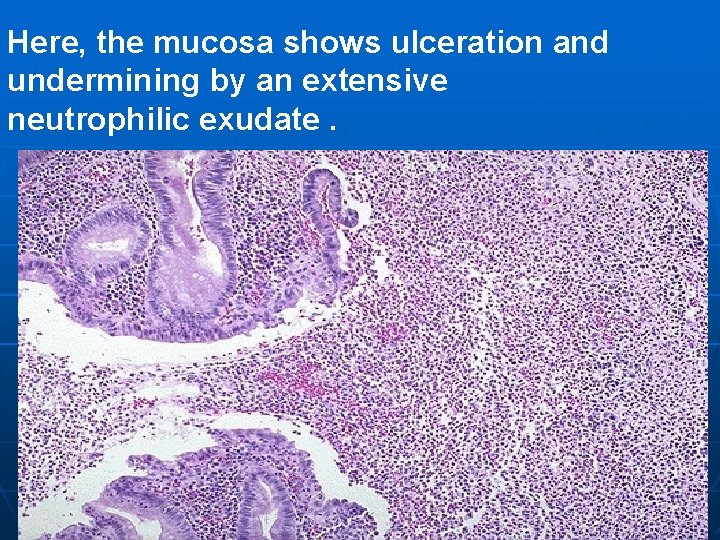
Here, the mucosa shows ulceration and undermining by an extensive neutrophilic exudate.
(3) Acute gangrenous appendicitis: n Occurs in severe cases accompanied by complete obstruction. n The suppuration proceeds to necrosis usually at the tip followed by putrefaction. n The appendix is dark brown to black, friable and usually perforate.
Complications: (1) Appendicular mass and appendicular abscess. (2) Septic peritonitis mostly localized. (3) Septic thrombophlebitis of the appendicular vein causes portal pyemia. (4) Persistence of the inflammatory reaction with fibrosis causes chronic appendicitis. (5) Fibrotic obstruction and distension of the lumen by mucus causes mucocele of the appendix. (6) Fistula formation. (7) Peritoneal adhesions. n
n n CHRONIC APPENDICITIS Chronic appendicitis is a fibrosed appendix resulting from healing of mild attacks of acute appendicitis. The fibrosis may be diffuse in the wall with a patent lumen (chronic nonobliterative appendicitis), or focal causing stenosis of the lumen. Marked fibrosis obliterates the lumen (chronic obliterative appendicitis).
n n n MUCOCELE OF THE APPENDIX Distension of the appendix by mucous as a result of obstruction of the lumen usually after the subsidence of acute appendicitis. Rupture of the mucocele causes implants of the appendicular mucosa on the peritoneal surface. The implants produce excess mucin in the peritoneal cavity "pseudomyxoma peritonii". Secondary infection in the mucocele changes the lesion to empyema of the appendix.
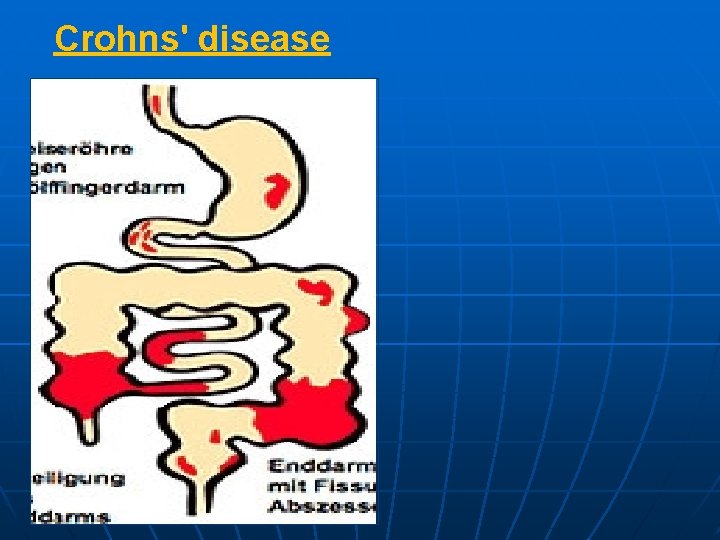
REGIONAL ENTERITIS (CROHN'S DISEASE) Definition: n Chronic non-specific granulomatous inflammation of the lower ileum. Any parts of the GIT could be affected from the mouth cavity to the anus. n Etiology: n The cause is unknown, but the disease may be related to: (1) Hypersensitivity to a particular microorganism, virus or bacteria. (2) An auto-immune or psychosomatic disease. n
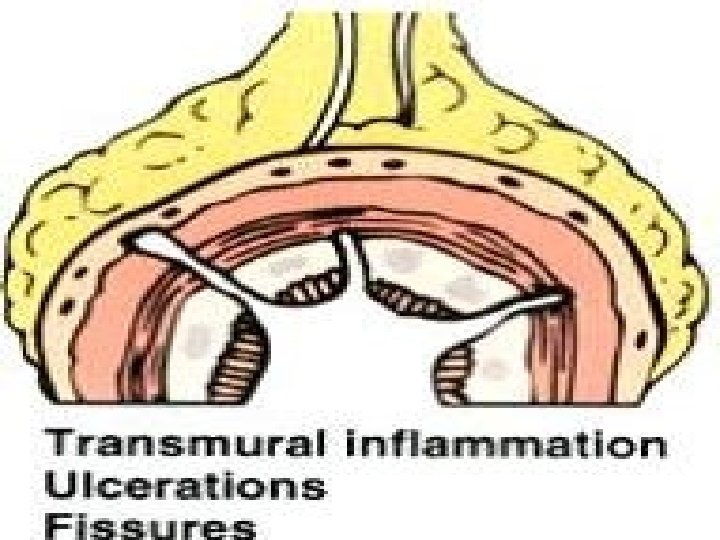
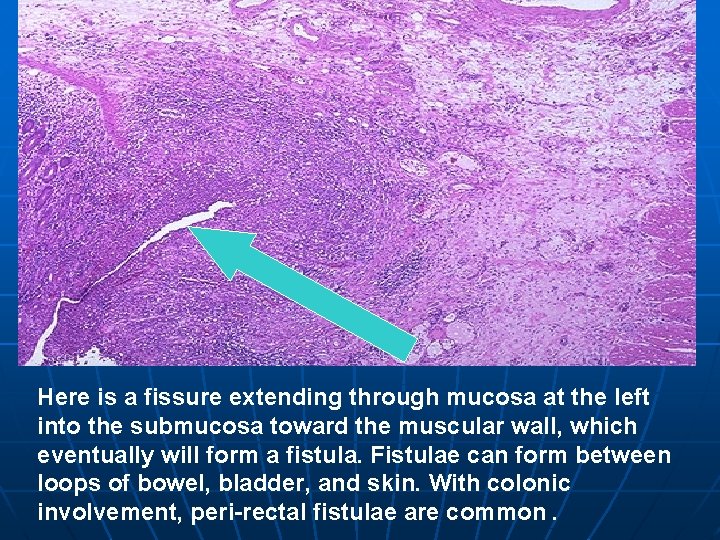
n n n Gross picture: Single or multiple segments are affected. The affected segment and its mesentery is congested, thickened due to edema and sharply demarcated. The mucosa shows linear ulcers and narrow fissures. Healing by fibrosis causes thickening of the wall, narrowing of the lumen and peritoneal adhesions. Mesenteric lymph nodes are enlarged and firm.
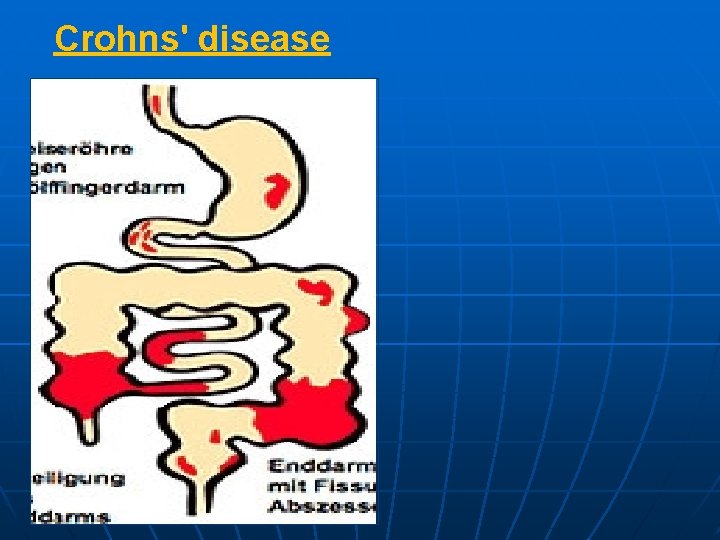
Crohns' disease
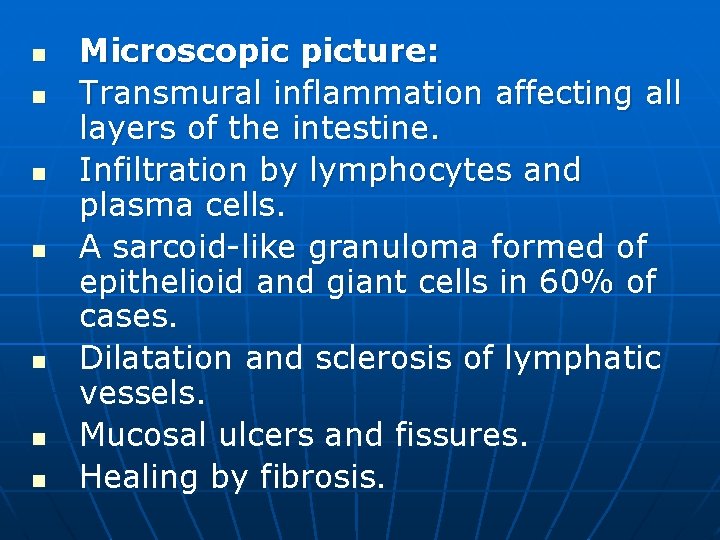
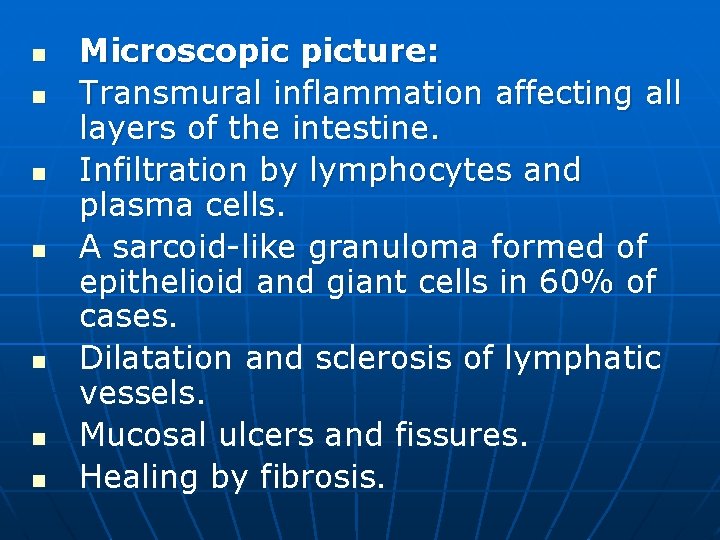
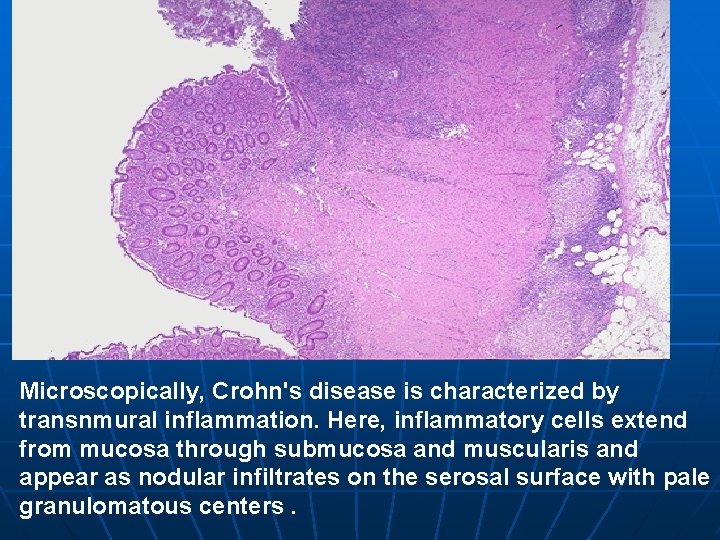
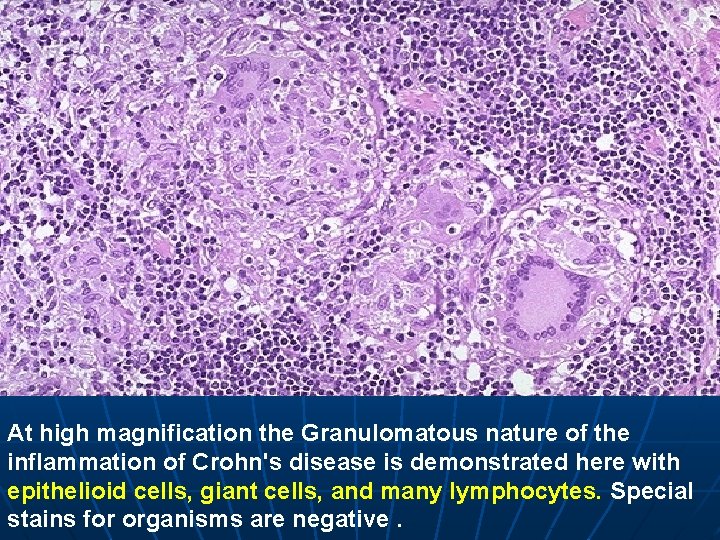
n n n n Microscopic picture: Transmural inflammation affecting all layers of the intestine. Infiltration by lymphocytes and plasma cells. A sarcoid-like granuloma formed of epithelioid and giant cells in 60% of cases. Dilatation and sclerosis of lymphatic vessels. Mucosal ulcers and fissures. Healing by fibrosis.
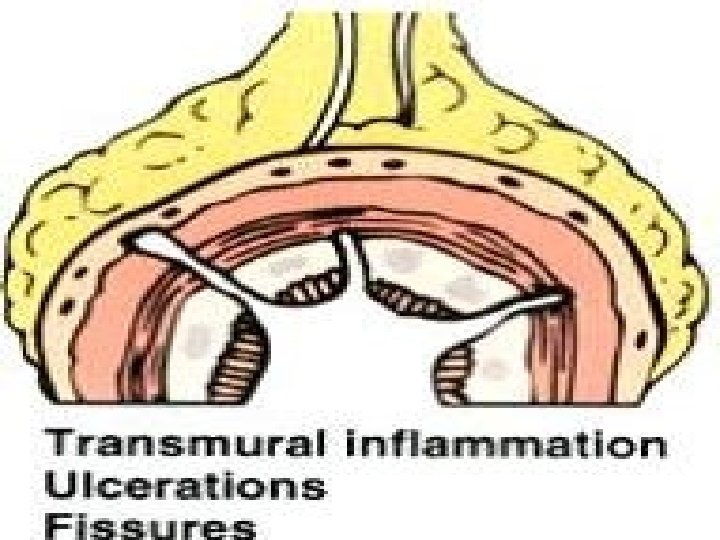
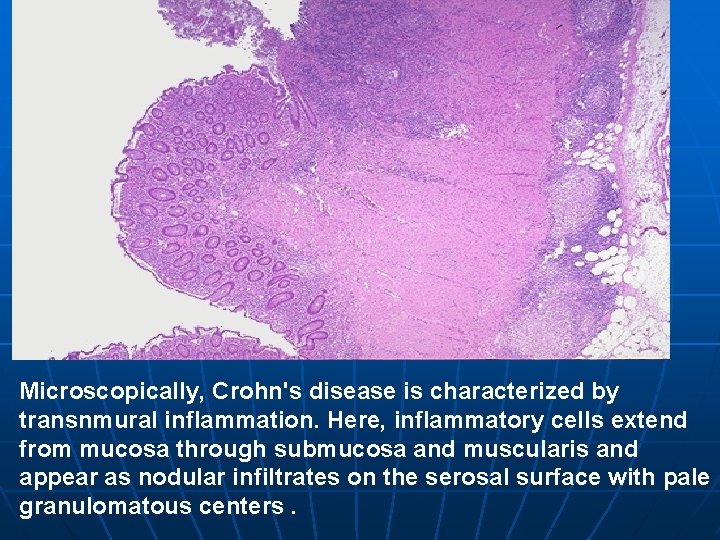
Microscopically, Crohn's disease is characterized by transnmural inflammation. Here, inflammatory cells extend from mucosa through submucosa and muscularis and appear as nodular infiltrates on the serosal surface with pale granulomatous centers.
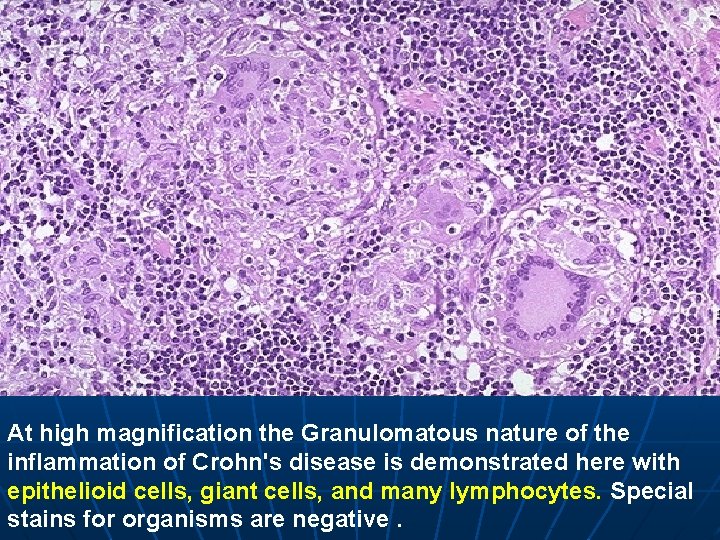
At high magnification the Granulomatous nature of the inflammation of Crohn's disease is demonstrated here with epithelioid cells, giant cells, and many lymphocytes. Special stains for organisms are negative.
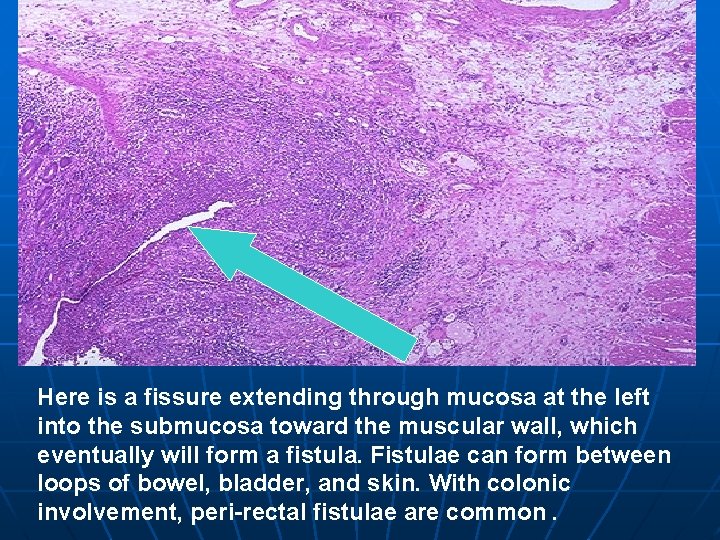
Here is a fissure extending through mucosa at the left into the submucosa toward the muscular wall, which eventually will form a fistula. Fistulae can form between loops of bowel, bladder, and skin. With colonic involvement, peri-rectal fistulae are common.
Complications: (1) Perforation and fistulae formation. (2) Fibrosis causes intestinal stenosis. (3) Secondary malabsorption syndrome. (4) Carcinoma of small and large intestine. n

ULCERATIVE COLITIS n n Definition: Chronic non-specific inflammation of the colon of unknown etiology. Etiology: The disease has a familial tendency and may be an allergic, auto-immune or psychosomatic disorder.
n n n Gross picture: Ulcerative colitis begins in the rectum and gradually extends along the colon in a retrograde fashion. The mucosa shows congestion, edema, focal hemorrhages and small ulcerations. The ulcers coalesce to form larger, irregular superficial ulcers. The mucosa in between the ulcers form hyperplastic pseudo-polypoid projections. Healing by fibrosis causes thickening of the wall and narrowing of the lumen.
Ulcerative colitis

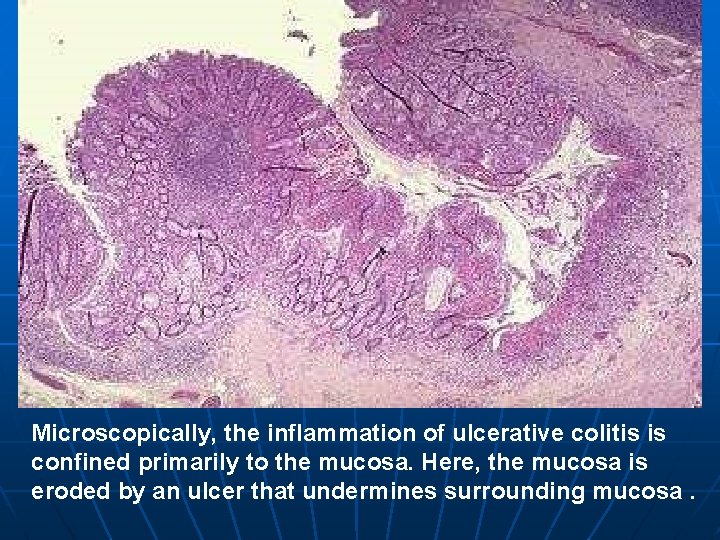
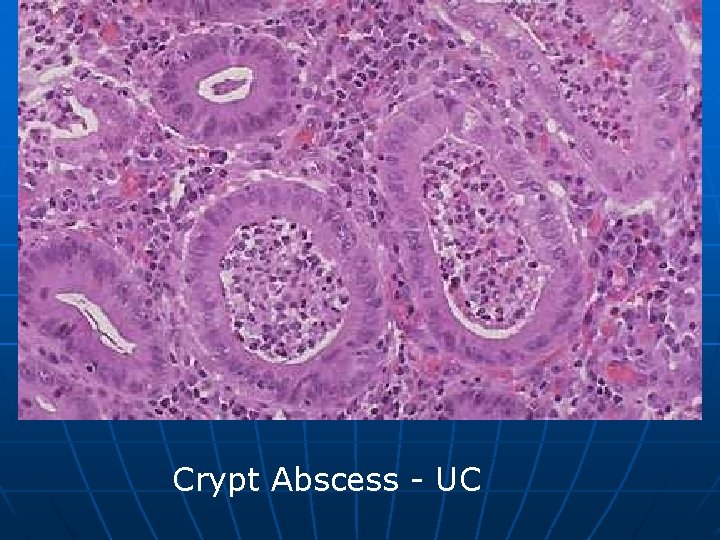
n n n Microscopic picture: Inflammation mainly affects the mucosa. The mucosa shows congestion, edema, ulceration and infiltration by lymphocytes, plasma cells, macrophages and eosinophils. Polymorpho-nuclear leucocytes (PML) and pus cells occasionally collect at the depth of the mucosal crypts forming small crypt abscesses. The pseudo-polyps consists of hyperplastic mucosa and granulation tissue. With healing epithelial regeneration occurs, but may show gastric metaplasia.
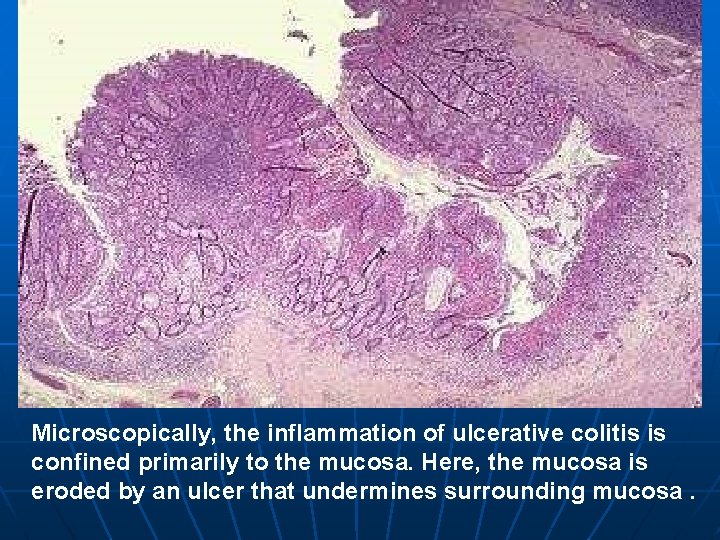
Microscopically, the inflammation of ulcerative colitis is confined primarily to the mucosa. Here, the mucosa is eroded by an ulcer that undermines surrounding mucosa.
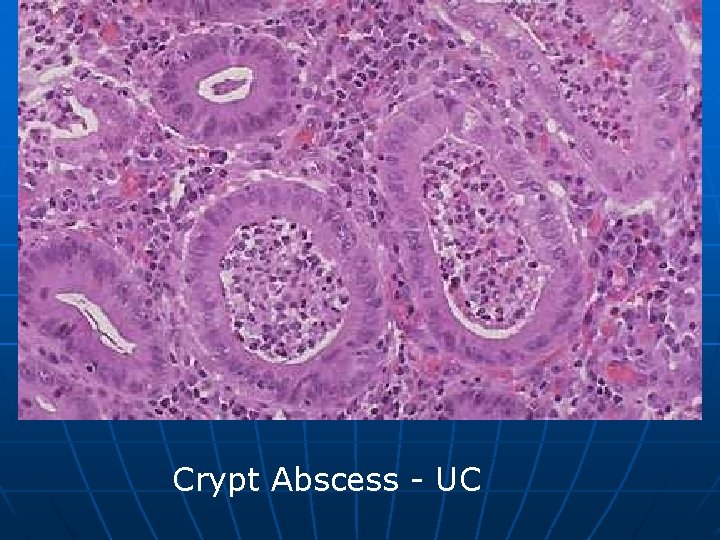
Crypt Abscess - UC

n (1) (2) (3) (4) (5) (6) Complications: Intestinal hemorrhage. Perforation causing peritonitis. Colonic stricture. Peri-anal fistula. Malignancy. Secondary amyloidosis.


Thank you
 Eman nayyab
Eman nayyab Eman güvenlik
Eman güvenlik اا
اا Attahiyyatu
Attahiyyatu Respiratory digestive and circulatory system
Respiratory digestive and circulatory system Chapter 6 musculoskeletal system
Chapter 6 musculoskeletal system Chapter 17 reproductive system diseases and disorders
Chapter 17 reproductive system diseases and disorders Chapter 15 nervous system diseases and disorders
Chapter 15 nervous system diseases and disorders 10 diseases of lymphatic system
10 diseases of lymphatic system Chapter 8 cardiovascular system
Chapter 8 cardiovascular system Glott medical term
Glott medical term Diseases of the musculoskeletal system
Diseases of the musculoskeletal system Female reproductive system diseases
Female reproductive system diseases Nervous system and digestive system
Nervous system and digestive system Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot So nguyen to
So nguyen to Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
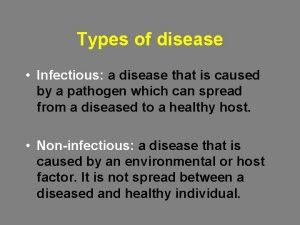
Thế nào là mạng điện lắp đặt kiểu nổi Types of diseases
Types of diseases Quality definition by quality gurus
Quality definition by quality gurus Protein deficiency diseases
Protein deficiency diseases Spectrum of diseases
Spectrum of diseases Lifestyle modern
Lifestyle modern Major nutritional deficiency diseases in emergencies
Major nutritional deficiency diseases in emergencies Abcsses
Abcsses Iceberg phenomenon of disease examples
Iceberg phenomenon of disease examples Human diseases a systemic approach
Human diseases a systemic approach