IN THE NAME OF GOD F SAMADIAN NEPHROLOGIST







- Slides: 108
IN THE NAME OF GOD F. SAMADIAN NEPHROLOGIST
n Peritonitis and Exit Site Infection

n the introduction of Y-set and double-bag disconnect systems has reduced this to approximately one episode per patient every 24 months

Potential routes of infection: ¨ Intraluminal ¨ Periluminal ¨ Transmural ¨ Hematogenous ¨ Transvaginal
Intraluminal: This allows bacteria to gain access to the peritoneal cavity via the catheter lumen n
Periluminal: Bacteria present on the skin surface can enter the peritoneal cavity via the peritoneal catheter tract n
Transmural: Bacteria of intestinal origin can enter the peritoneal cavity by migrating through the bowel wall This is the usual mechanism of peritonitis associated with diarrheal states and/or states instrumentation of the colon and may be colon seen also with strangulated hernia n
Hematogenous: Less commonly, peritonitis is due to bacteria that have seeded the peritoneum from a distant site by way of the bloodstream n
Transvaginal: it may explain some instances of Candida peritonitis n

n The responsible pathogen is almost always a bacterium, usually of the Grampositive variety
n The occurrence of fungal peritonitis (e. g. , Candida) is uncommon
n Infections with Mycobacterium tuberculosis or other type of mycobacteria have been reported but are unusual
Diagnostic criteria for peritonitis: At least two of the following three conditions should be present: n symptoms and signs of peritoneal inflammation n cloudy peritoneal fluid with an elevated peritoneal fluid cell count (more than 100/mc. L) due predominantly (more than 50%) to neutrophils n demonstration of bacteria in the peritoneal effluent by Gram stain or culture
Symptoms and signs: n n The most common symptom of peritonitis is abdominal pain However, peritonitis should be suspected whenever a patient suffers from generalized malaise, particularly if nausea, vomiting, or diarrhea is also present
n Not all abdominal pain in a patient receiving PD is peritonitis
n Strangulated hernia is a common mimic for peritonitis
Cloudiness of the fluid: The peritoneal fluid generally becomes cloudy when the cell count exceeds 50100/mc. L n
n In most patients, sudden onset of cloudy fluid with appropriate abdominal symptoms is sufficient evidence of peritonitis to warrant initiation of antimicrobial therapy
n However, peritoneal fluid cloudiness may be due to other factors (e. g. , fibrin, blood, or, rarely, malignancy or chyle)
n On the other hand, a relatively translucent peritoneal fluid does not completely exclude the possibility that peritonitis is present (early in the course of peritonitis)
n The absolute peritoneal fluid cell count in CAPD patients is usually <50 cells/mc. L and is often <10 cells/mc. L
n Normally, the peritoneal fluid contains predominantly mononuclear cells (macrophages, monocytes, and, to a lesser extent, lymphocytes)
n The percentage of neutrophils does not normally exceed 15% of the total nonerythrocyte cell count and a value >50% strongly suggests peritonitis, whereas one >35% should raise suspicion
n Vancomycin or a first-generation cephalosporin such as cefazolin or cephalothin is used in combination with an antibiotic to cover Gram-negative organisms such as ceftazidime
n It is now recommended that aminoglycosides be avoided if possible in patients with residual renal function because of their nephrotoxicity
n n n CAPD Loading dose: Infuse 2 L of 1. 5% dextrose dialysis solution containing: 1 g ceftazidime 1 g cefazolin 1, 000 units/L heparin Allow to dwell for 3 -4 hours. Continue regular CAPD schedule. Add 125 mg per L ceftazidime, 125 mg/L cefazolin, and 1, 000 units/L heparin to each dialysis solution bag
n If a patient appears toxic recommend a single loading dose IV
Duration of therapy: n If patient improvement is prompt, antimicrobial therapy should be continued for a total of 14 days n If a cephalosporin is being used, then some physicians will switch to PO therapy after the first 5 days
n Severe S. aureus infections require antimicrobials for 3 weeks, and treatment with one IP antistaphylococcal drug plus PO rifampin is recommended
n Patients in whom S. aureus peritonitis develops not uncommonly are found to carry this organism in the nose
n This can be accomplished with intranasal mupirocin (b. i. d. for 5 days every 4 weeks) or oral rifampin (300 mg b. i. d. for 5 days every 3 months
Exit site infection Approximately one fifth of peritonitis episodes are temporally associated with exit site and tunnel infections n
Etiology and pathogenesis: n Exit site infections are predominantly due to S. aureus or Gram-negative organisms, particularly Pseudomona n In contrast to peritonitis, S. epidermidis is the causative organism in <20% of patients eradication of the carrier state is very helpful to effective management
Treatment is dependent on whethere is erythema alone or erythema in conjunction with purulent drainage n In the former case, topical treatment with hypertonic saline compresses, hydrogen peroxide, or mupirocin 2% ointment is usually sufficient n
Treatment is more problematic and more prone to failure when there is purulent drainage n some exit site infections extend into the subcutaneous tunnel n
n The major risk factor for exit site infection is staphylococcal nasal carriage
n Persistently positive nasal cultures are nasal associated with a 3 -4 fold increase in risk fold of staphylococcal exit site infection
Protocols used include -rifampin (600 mg PO for 5 days), -mupirocin (2% ointment twice daily for 5 days every 4 weeks) -trimethoprim-sulfamethoxazole (singlestrength tablet three times weekly) n
n Mechanical Complications of Peritoneal Dialysis

n The instillation of dialysis fluid into the peritoneal cavity is accompanied by an increase in intra-abdominal pressure (IAP)
n The two principal determinants of the magnitude of the increased IAP are dialysate volume and the position of the volume position patient during the dwell
n The supine position is associated with the supine lowest IAP for a given dialysate volume; sitting entails the highest sitting
Hernia formation as many as 10%-20% of patients may develop a hernia at some time on peritoneal dialysis n
Potential risk factors for hernia formation -Large dialysis solution volume -Sitting position -Isometric exercise -Valsalva maneuver (e. g. , coughing) -Recent abdominal surgery -Pericatheter leak or hematoma -Obesity -Multiparity -Congenital anatomical defects n
n Many different types of hernias have been described in the peritoneal dialysis patient
n Types of hernias reported in peritoneal dialysis patients. Ventral Epigastric Pericatheter Umbilical Inguinal (direct and indirect) Femoral Spigelian Richter Foramen of Morgagni Cystocele Enterocele
n Pericatheter hernias need to be differentiated from masses caused by a hematoma, seroma, or abscess
Ultrasonography n CTscan n MRI n
Small hernias pose the greatest risk of incarceration or strangulation of bowel
n Abdominal wall and pericatheter leak
n Abdominal wall leak may be difficult to diagnose clinically
n It may be mistaken for ultrafiltration failure when dialysate returns are less than the instilled volume
The diagnosis should be considered with: -decreased effluent volumes -weight gain -protuberant abdomen -absence of generalized edema n
n The patient should stand during the examination as this may reveal asymmetry of the abdomen
n Diagnosis can be proven using contrast CT scanning
n Pericatheter leak usually occurs as a postoperative complication of catheter implantation
In most cases, the leak seals spontaneously n If it persists, the catheter should be removed and reinserted at another site n
n In contrast to pericatheter leaks, abdominal wall leaks can occur early or late
n Sometimes surgical repair is feasible
Vaginal leaks can also occur Some may result from tracking of dialysate through the fallopian tubes and may resolve with tubal ligation n
Genital edema: Dialysate can reach the genitalia by two routes n
n One is by traveling through a patent processus vaginalis to the tunica vaginalis, resulting in hydrocele
n The second route is through a defect in the abdominal wall, often associated with the catheter
n This complication is often painful and distressing to the patient who is quick to bring it to medical attention
n CT peritoneography should be performed to distinguish which route has led to the genital swelling (i. e. , anterior abdominal wall or processus vaginalis)
Peritoneal dialysis should be temporarily stopped n Bed rest and scrotal elevation are helpful n
n A leak via a patent processus vaginalis can be repaired surgically
n If the leak is through the anterior abdominal wall, replacement of the catheter can be helpful
Respiratory complications: Hydrothorax Under the influence of raised IAP, dialysate can travel from the peritoneal to the pleural cavity, leading to a pleural effusion composed of dialysis effluent n
n These defects may be congenital, in congenital, which case hydrothorax can occur with the first dialysis exchange, or acquired, acquired whereby hydrothorax can be a late complication
n They occur almost exclusively on the right side, probably because the left side hemidiaphragm is mostly covered by heart and pericardium
n Symptoms of hydrothorax range from asymptomatic pleural effusion to severe asymptomatic shortness of breath
n Such symptoms may worsen with administration of hypertonic dialysate, dialysate which raises IAP
n Thoracentesis can be done for diagnosis or to relieve symptoms
n The most diagnostic feature of the pleural fluid is the very high glucose level, level although this is not always a consistent finding
transudative n It is typically transudate, with variable transudate numbers of leukocytes
n Radionuclide scanning with technetium is also helpful
Back pain: The presence of dialysate in the peritoneal cavity both raises IAP and swings the center of gravity forward, producing lordotic stress on the lumbar vertebrae and paraspinal muscles n

n Some patients benefit from the performance of more frequent exchanges with smaller dialysate volumes

n Metabolic Complications of Peritoneal Dialysis
Glucose absorption Glucose has the advantage of being cheap, stable, and relatively nontoxic to the peritoneum n
n up to 100 g per day of glucose may be absorbed, which represents 500 -800 kcal per day
n This constitutes a significant portion of the recommended total energy intake of about 2, 500 kcal per day (35 kcal/kg per day) in a 70 -kg patient
n In some patients, this provides a welcome source of calories since achieving the nutritional recommendation for PD is often difficult
n In patients who start PD obese, the obese glucose loading from PD may contribute to further weight gain
n glucose absorption results in increased insulin secretion, which together with secretion insulin resistance (a common feature of chronic renal failure) results in plasma insulin levels that are persistently high
n Hyperinsulinemia may be an independent risk factor for the development of atherosclerosis
n Patients who were previously well controlled on oral hypoglycemics often require increased doses of these medications, and they may even require a change to insulin therapy after therapy initiation of PD
n To minimize glucose absorption, patients should be advised on appropriate salt and water management, which will management diminish the need for hypertonic solutions to maintain fluid balance
Lipid abnormalities patients on PD have a variety of lipid abnormalities n
n Typically, they have high total and LDL cholesterol, high triglycerides, low HDL cholesterol, high apo. B, low apo. A-I, and high lipoprotein(a) levels
n Compared with hemodialysis patients, the most striking differences are the high apo. B protein and LDL cholesterol levels, which are usually normal in hemodialysis patients
Protein loss: PD is associated with significant loss of protein across the peritoneum n
n This loss is about 0. 5 g/L of dialysate drainage, but may be higher and account for as much as 10 -20 g per day
n The major component of the protein losses is albumin
n Acute peritoneal inflammation is associated with substantially greater protein losses, and a rapid reduction in serum albumin is common during episodes of peritonitis
n The protein loss itself may become an indication to terminate peritoneal dialysis temporarily or, on occasion, permanently
Hypokalemia/hyperkalemiakm: n PD solution contains no potassium n Usually only patients who are noncompliant in performing their dialysis exchanges or who have excessive potassium intake have ongoing problems with hyperkalemia
n However, hypokalemia has been reported in 10%-30% of CAPD patients
n These cases are usually associated with poor nutritional intake, and most can be managed by liberalizing the diet
Dialysis solution calcium level PD solutions are available with 2. 5 m. Eq/L or 3. 5 m. Eq/L calcium concentrations n
n The 3. 5 m. Eq/L dialysis solution keeps the patient in positive calcium balance
n The standard solution is now considered to be the 1. 25 m. M (2. 5 m. Eq/L) calcium solution
n Hypocalcemia is not common in patients on PD because of the widespread use of calcium-based phosphate binders and vitamin D

 Dr vali nephrologist
Dr vali nephrologist Pdf
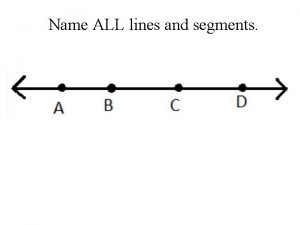
Pdf Name three lines
Name three lines Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên
Thế nào là giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Số nguyên tố là
Số nguyên tố là Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Our god is an awesome god vine
Our god is an awesome god vine Our god is an awesome god
Our god is an awesome god Our god is an awesome god medley
Our god is an awesome god medley God is good god is great speed
God is good god is great speed O god you are my god earnestly i seek you
O god you are my god earnestly i seek you God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. Justice and virtue
Justice and virtue My god's bigger than your god
My god's bigger than your god Using god's name in vain meaning
Using god's name in vain meaning God's covenant
God's covenant O lord how excellent
O lord how excellent In the name of god amen mayflower compact
In the name of god amen mayflower compact In the name of god most gracious prayer
In the name of god most gracious prayer 馮定華神父
馮定華神父 Mercury roman name
Mercury roman name In the name of god the beneficent the merciful
In the name of god the beneficent the merciful In the name of god the beneficent the merciful
In the name of god the beneficent the merciful In the name of god most gracious most merciful
In the name of god most gracious most merciful God of secrets name
God of secrets name Colossians 1:17-19
Colossians 1:17-19 God name
God name God saves name
God saves name In the name of god the most gracious the most merciful
In the name of god the most gracious the most merciful In the name of god the merciful
In the name of god the merciful His name is the word of god
His name is the word of god What was apollos realm
What was apollos realm Authors last name first name initial
Authors last name first name initial Name above every other name
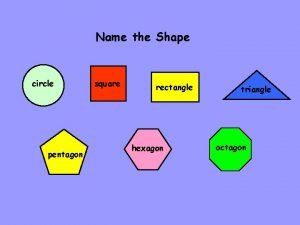
Name above every other name Shape that has 6 sides
Shape that has 6 sides![Private string[] Private string[]](data:image/svg+xml,%3Csvg%20xmlns=%22http://www.w3.org/2000/svg%22%20viewBox=%220%200%20200%20200%22%3E%3C/svg%3E) Private string[]
Private string[] What is name
What is name Name of presentation company name
Name of presentation company name Name of presentation company name
Name of presentation company name Name class date
Name class date Her name is betty
Her name is betty What is your name and how old are you
What is your name and how old are you Name class teacher date
Name class teacher date Student id name department name
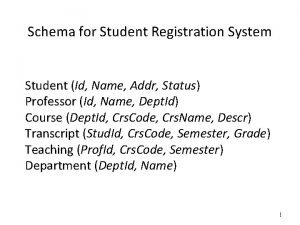
Student id name department name Git config global user name
Git config global user name Lecturer's name
Lecturer's name Agile project inception
Agile project inception Name date class
Name date class First name last name tpu
First name last name tpu Stibous
Stibous Work is a blessing from god
Work is a blessing from god Malachi divorce
Malachi divorce God hides us
God hides us Gods favourite number
Gods favourite number What is your commitment level
What is your commitment level Thy hand o god has guided
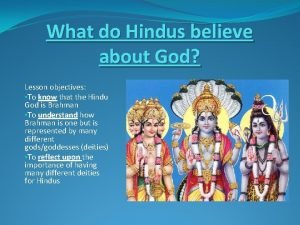
Thy hand o god has guided Brahman
Brahman Nu wij uiteengaan vragen wij god
Nu wij uiteengaan vragen wij god May the love of god enfold you bible verse
May the love of god enfold you bible verse God.oxomarket.net
God.oxomarket.net Zeus temper affected
Zeus temper affected Walking in divine favor
Walking in divine favor O heer my god lied 464
O heer my god lied 464 Estimation of glucose principle
Estimation of glucose principle Reward from god
Reward from god Amut egyptian god
Amut egyptian god Stealing god's glory
Stealing god's glory Is allah a personal god
Is allah a personal god Proverbs 6 16-19
Proverbs 6 16-19 If god closes a door he opens a window
If god closes a door he opens a window














































![Private string[] Private string[]](https://slidetodoc.com/wp-content/uploads/2020/12/3088144_f6d6e306d8f29e1538b2c0f548f94d87-300x225.jpg)