DR MUHAMMAD ANEES CHARIMAN HOD NEPHROLOGY DEPTT KEMUMAYO






- Slides: 69
DR MUHAMMAD ANEES CHARIMAN. HOD NEPHROLOGY DEPTT KEMU/MAYO HOSPITAL, LAHORE
CLINICAL SCENERIO A 60 years old man, known case of CKD stage 4 secondary to hypertension, presented to nephrology clinic with fatigue. A full blood count shows a normocytic anemia with Hb of 9. 7 g/dl. WBC and platelets are normal. What is the most likely cause of anemia in this patient a)folate deficiency b)vit. B 12 deficiency c)endogenous erythropoeitin deficiency d)haemoglobinopathies Ans: C
you are considering commencing treatment for this patient’s anemia. What is most appropriate investigation to help guide treatment ? a)peripheral blood film b)serum erythropoeitin c)serum ferritin d)serum LDH Ans: C
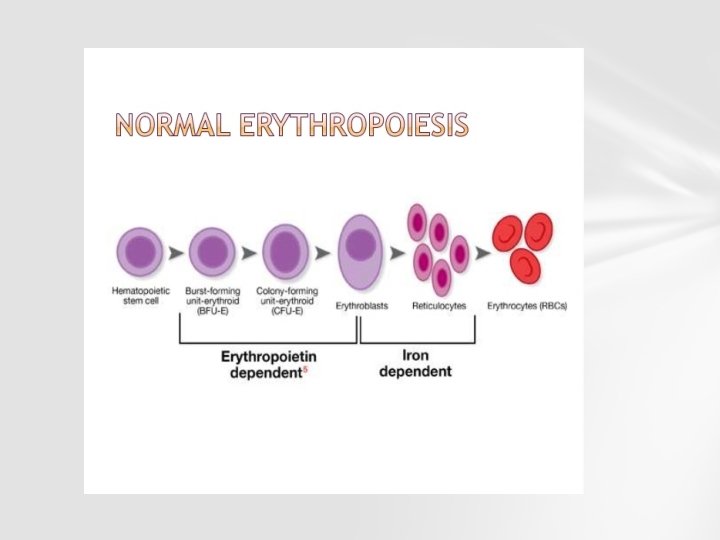
ERYTHROPOEISIS

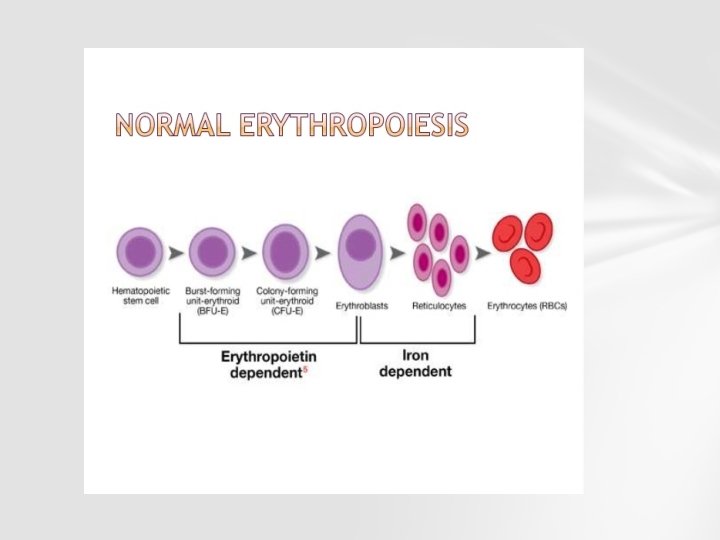
Mature erythrocytes are derived from committed erythroid proginator cells through a series of mitotic divisions and maturation phases.
ROLE OF KIDNEY IN ERYTHROPOEISIS Erythropoietin (from Greek word erythros 'red' , poiein 'make') also known as EPO, hematopoietin, or hemopoietin, is a glycoproteine hormone that controls erythropoiesis, or red blood cell production. It is a cytokine (protein signaling molecule) for erythrocyte precursors in the bone marrow.
SITE OF RELEASE Erythropoietin is produced by interstitial fibroblasts in the kidney in close association with peritubular capillary bed of renal cortex. It is also produced in perisinosidal cells in the liver While liver production predominates in the fetal and perinatal period, renal production is predominant during adulthood.
MECHANISM OF ACTION EPO is highly glycosylated with half-life in blood around five hours. EPO binds to the erythropoietin receptor on the red cell progenitor surface and activates a JAK 2 signaling cascade. High level erythropoietin receptor expression is localized to erythroid progenitor cells
EPO is the primary erythropoietic factor that cooperates with various other growth factors (e. g. , IL-3, IL 6, glucocorticoids, SCF)in the development of erythroid lineage from multipotent progenitors. The BFU-E cells start erythropoietin receptor expression and are sensitive to erythropoietin. Subsequent CFU-E, expresses maximal erythropoietin receptor density and is completely dependent on erythropoietin for further differentiation.
The proerythroblasts and basophilic erythroblasts also express erythropoietin receptor and are affected by it. Erythropoietin has its primary effect on red blood cell progenitors and precursors (which are found in the bone marrow in humans) by promoting their survival through protecting these cells from apoptosis.
SYNTHESIS AND REGULATION Erythropoietin levels in blood are low in the absence of anemia, at around 10 m. U/ml. In hypoxic stress, EPO production may increase up to 1000 -fold, reaching 10, 000 m. U/ml of blood. Regulation is believed to rely on a feedback mechanism measuring blood oxygenation and iron availability. Transcription factors for EPO, known as hypoxiainducible factors, are hydroxylated and proteosomally digested in the presence of oxygen and iron.
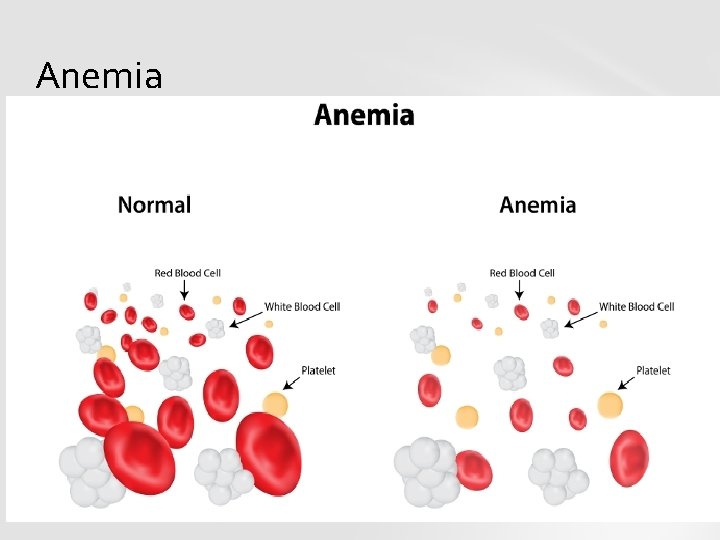
ANEMIA Anaemia is a condition in which the number of red blood cells or their oxygen-carrying capacity is insufficient to meet physiologic needs, which vary by age, sex, altitude, smoking, and pregnancy status. Normal values of Hb: 13 -14 g/dl in male 12 -13 g/dl in female
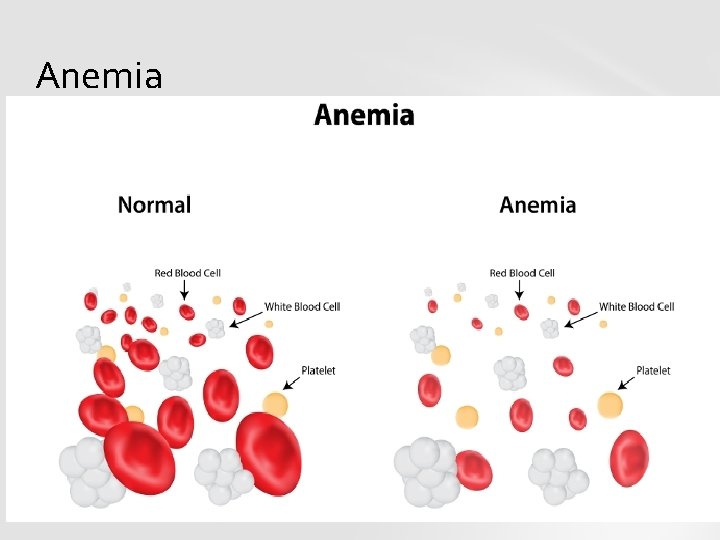
Anemia
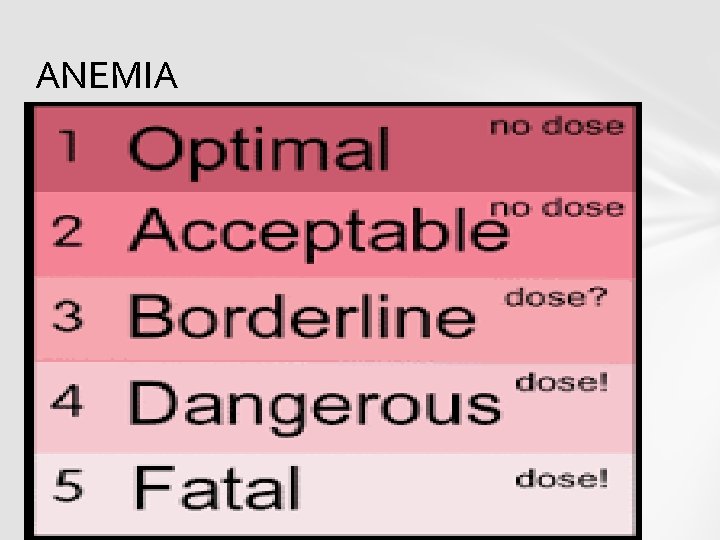
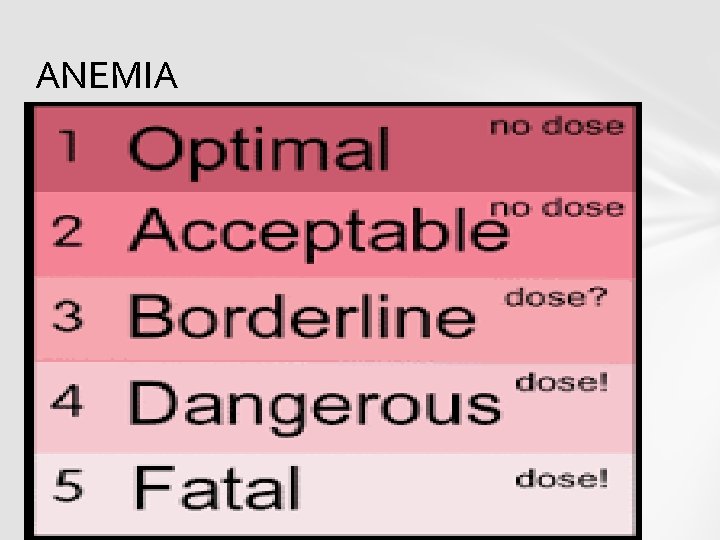
ANEMIA
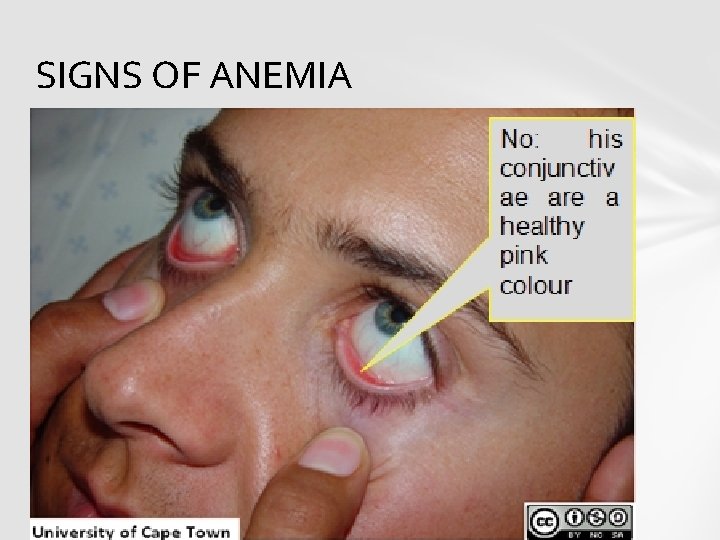
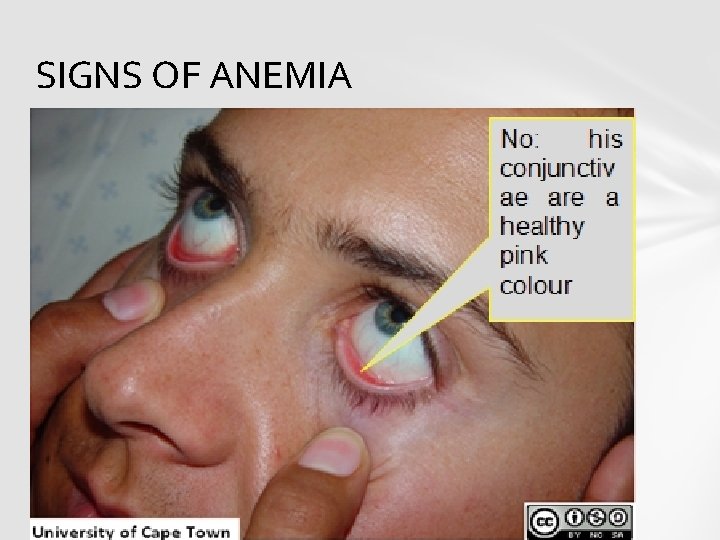
SIGNS OF ANEMIA
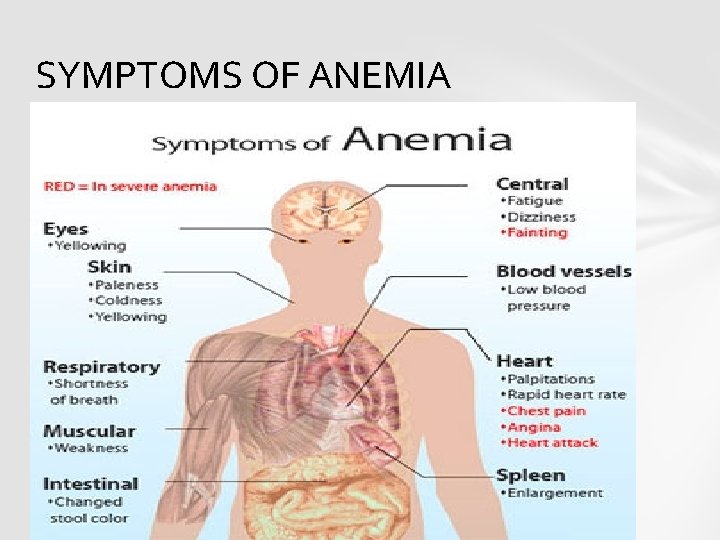
SYMPTOMS • If you are often tired even though you have slept well • If you have a headache and feel dizzy all the time
SYMPTOMS AND SIGNS § pale skin § shortness of breath § a tingling or crawling feeling in legs § tongue swelling or soreness § cold hands and feet
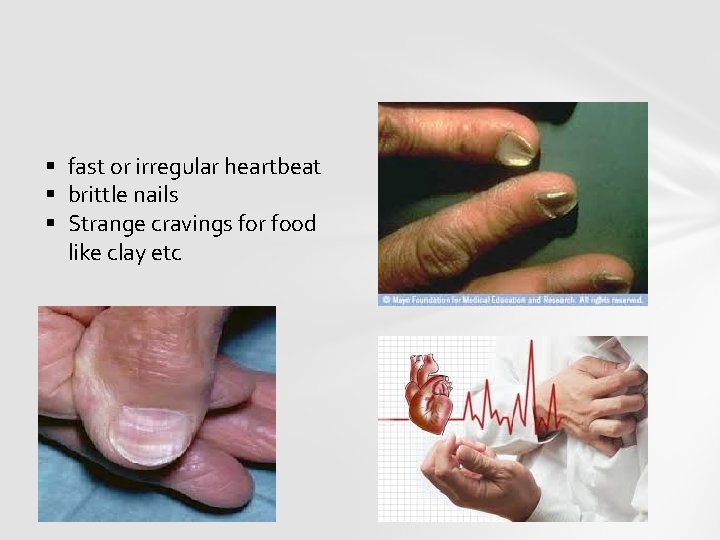
§ fast or irregular heartbeat § brittle nails § Strange cravings for food like clay etc
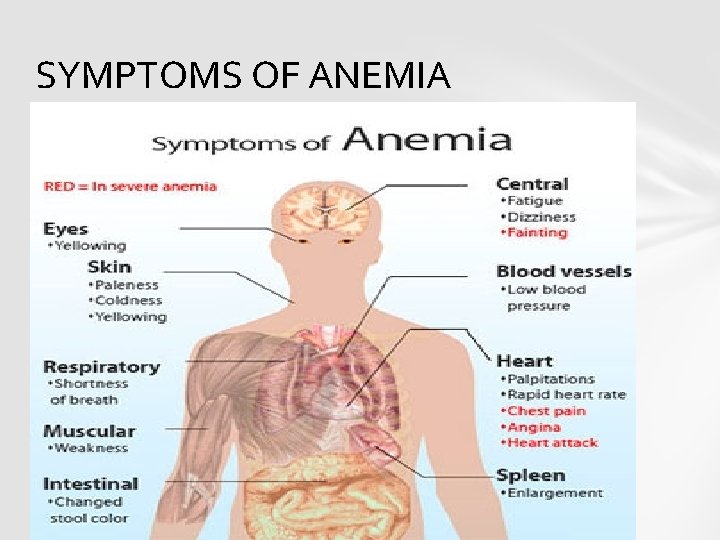
SYMPTOMS OF ANEMIA
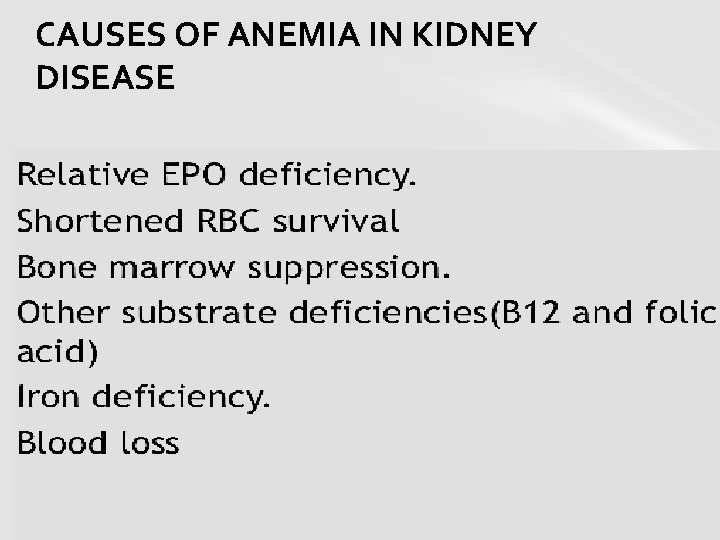
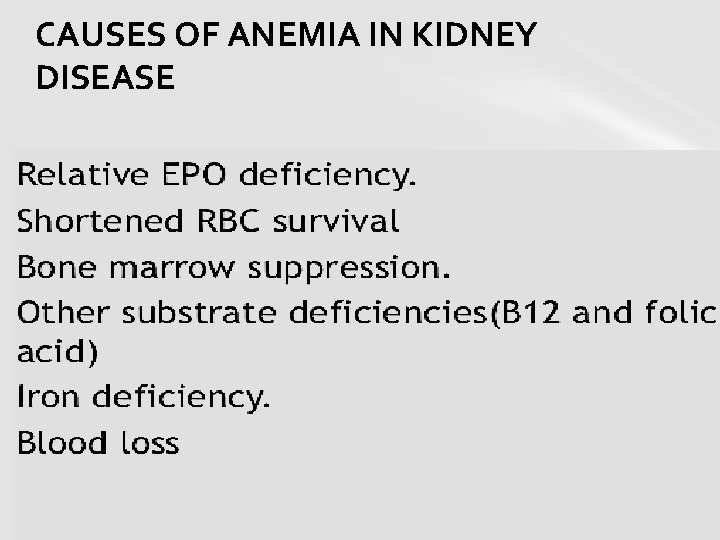
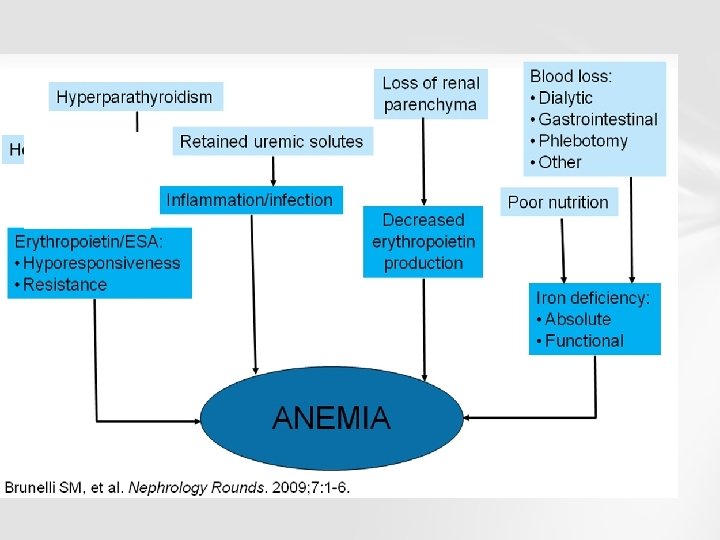
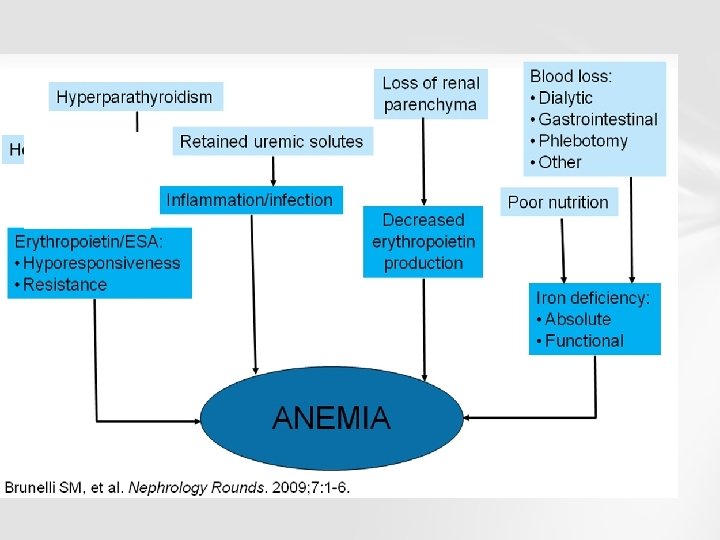
CAUSES OF ANEMIA IN KIDNEY DISEASE
TREATMENT OPTIONS § ADEQUATE IRON REPLACEMENT § ADAQUATE FOLIC ACID AND VITAMIN B 12 REPLACEMENT § ADEQUATE DOES OF EPO § ADEQUATE DOSE OF DIALYSIS § ADEQUATE FOLLOW UP FOR THE RESPONSE OF ABOVE……. . TREMENT OPTIONS
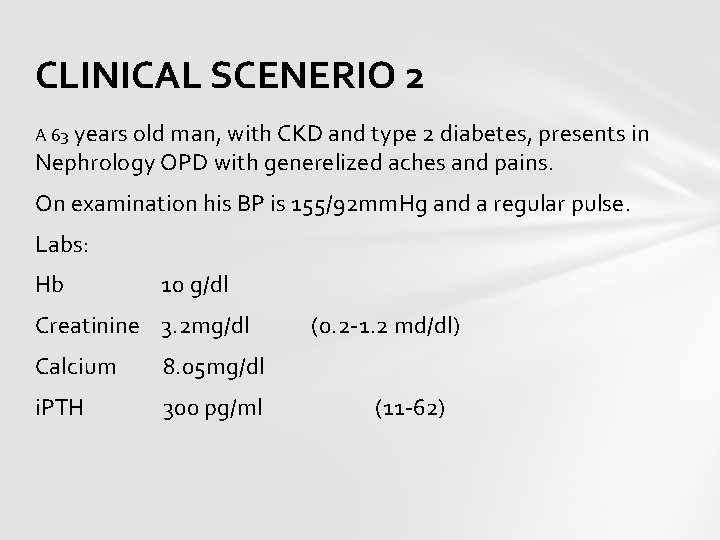
CLINICAL SCENERIO 2 A 63 years old man, with CKD and type 2 diabetes, presents in Nephrology OPD with generelized aches and pains. On examination his BP is 155/92 mm. Hg and a regular pulse. Labs: Hb 10 g/dl Creatinine 3. 2 mg/dl (0. 2 -1. 2 md/dl) Calcium 8. 05 mg/dl i. PTH 300 pg/ml (11 -62)
What is the underlying diagnosis a) Primary hyperpatathyroid b) Secondary hyperparathyroid c) Hypoparathyroid d) Vit D intoxication Ans: B
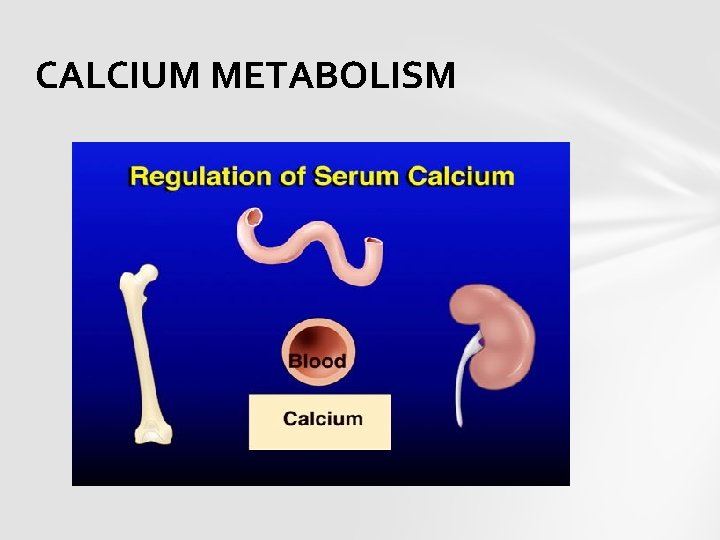
CALCIUM METABOLISM
ROLE OF KIDNEY The kidney filters 250 mmol of calcium ions a day in prourine (or glomerular filtrate), and resorbs 245 mmol, leading to a net average loss in the urine of about 5 mmol/d. The quantity of calcium ions excreted in the urine per day is partially under the influence of the plasma parathyroid hormone (PTH) level. Kidney processes vitamin D 3 into calcitriol, the active form, most effective in promoting the intestinal absorption of calcium.
Calcium is the most abundant mineral in human body. The average adult body contains approximately 1 kg, 99% in the skeleton in the form of calcium phosphate. The extracellular fluid (ECF) contains approximately 22 mmol, of which about 9 mmol is in plasma. Approximately 10 mmol of calcium is exchanged between bone and ECF over 24 hr. The concentration of calcium ions inside the cells is more than 7, 000 times lower than in the blood plasma.
FUNCTIONS • Controls internal regulation of functions of all cells • Regulates cell membrane permeability, nerve excitibility, muscle contraction and gland secretion • Regulates synthetic and secretory functions of PTH and thyroid C cells (for calcitonin) • Controls adhesiveness between cells • Maintains hardness and rigidity of bones and teeth through hydroxyapetite.
NORMAL RANGES The plasma total calcium concentration is in the range of 2. 2 -2. 6 mmol/L (9 -10. 5 mg/d. L), and the normal ionized calcium is 1. 3 -1. 5 mmol/L (4. 5 -5. 6 mg/d. L). The amount of total calcium in the blood varies with the level of plasma albumin, the most abundant protein in plasma, and therefore the main carrier of protein-bound calcium in the blood. The biologic effect of calcium is determined by the amount of ionized calcium.
BONE Although calcium flow to and from the bone is neutral, about 5– 10 mmol is turned over a day. Bone serves as an important storage point for calcium, as it contains 99% of the total body calcium. Calcium release from bone is regulated by PTH in conjunction with calcitriol.
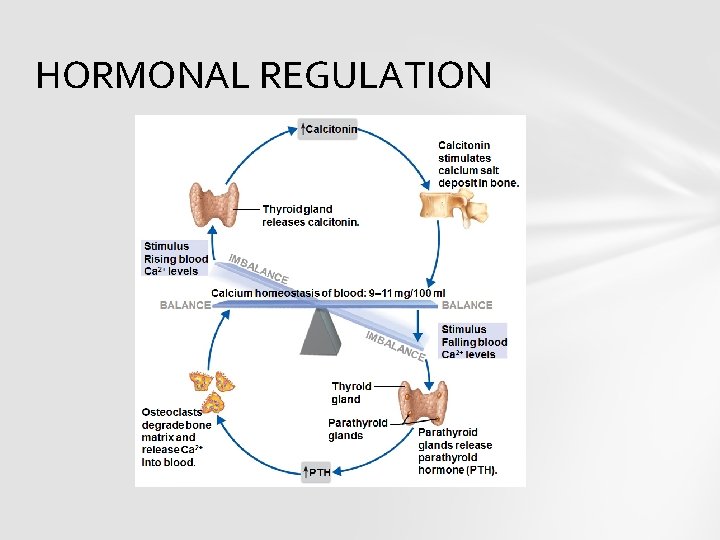
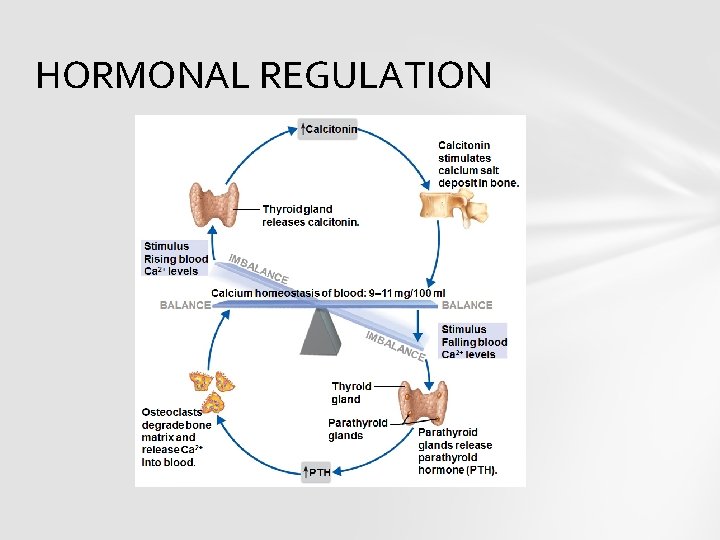
HORMONAL REGULATION
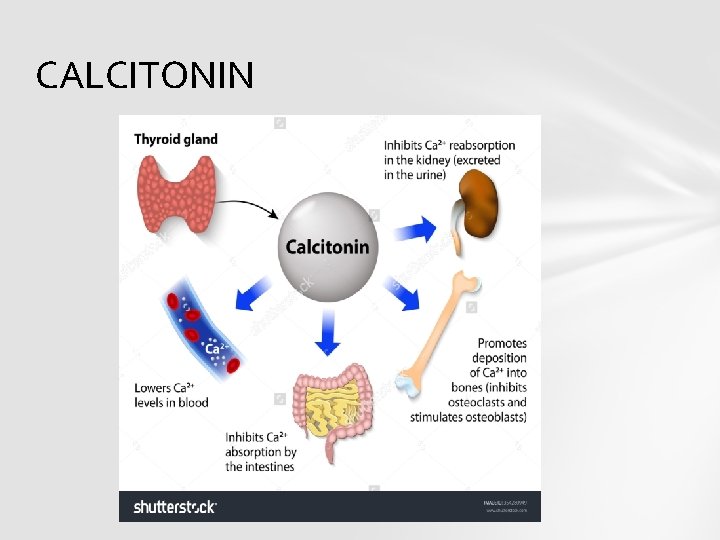
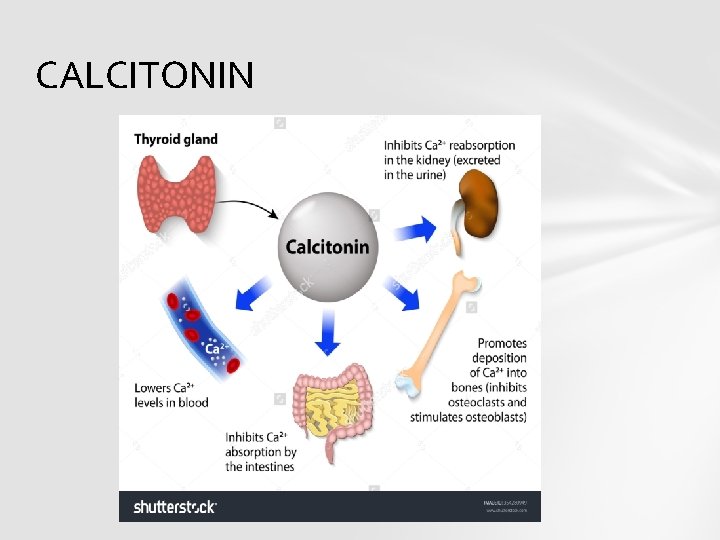
CALCITONIN
Both parafollicular cells of thyroid and the parathyroid glands constantly sense the concentration of calcium ions in blood. When Ca concentration rises, the parafollicular cells of thyroid increase secretion of calcitonin in blood. At the same time the parathyroid glands reduce PTH secretion.
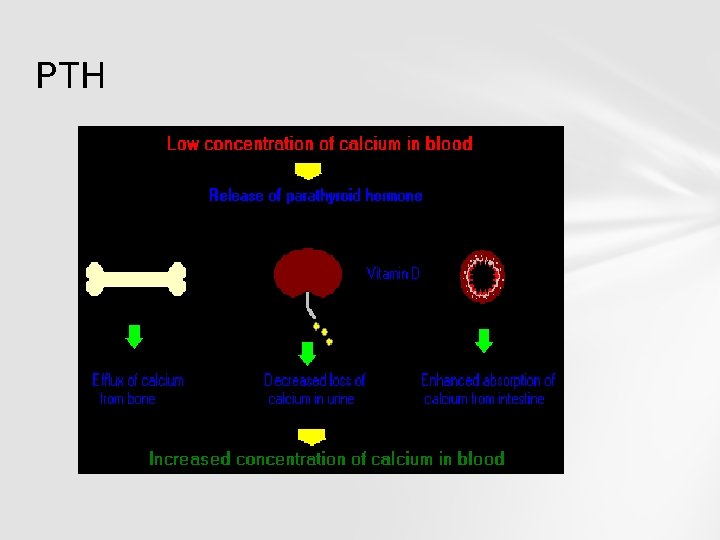
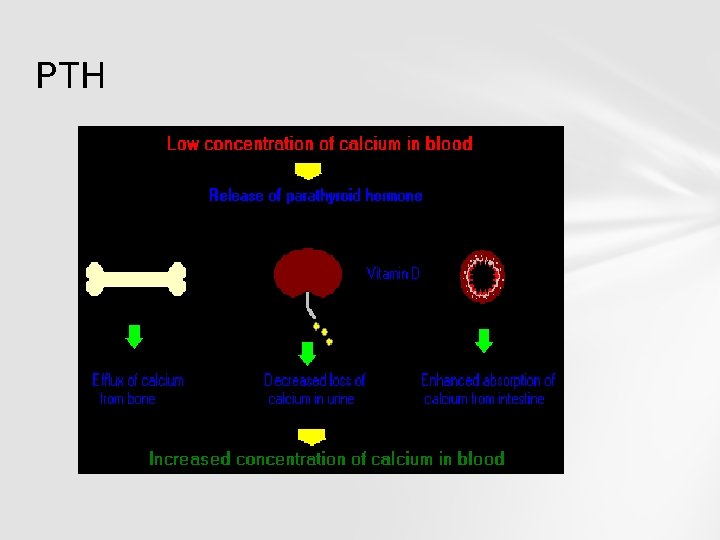
PTH
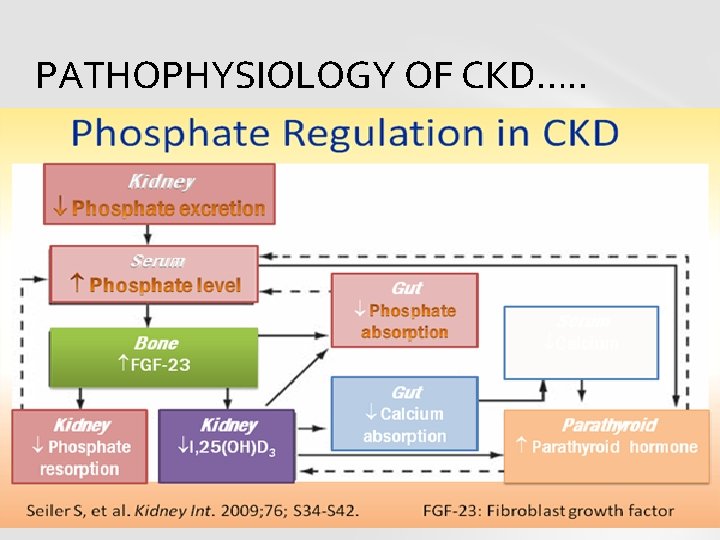
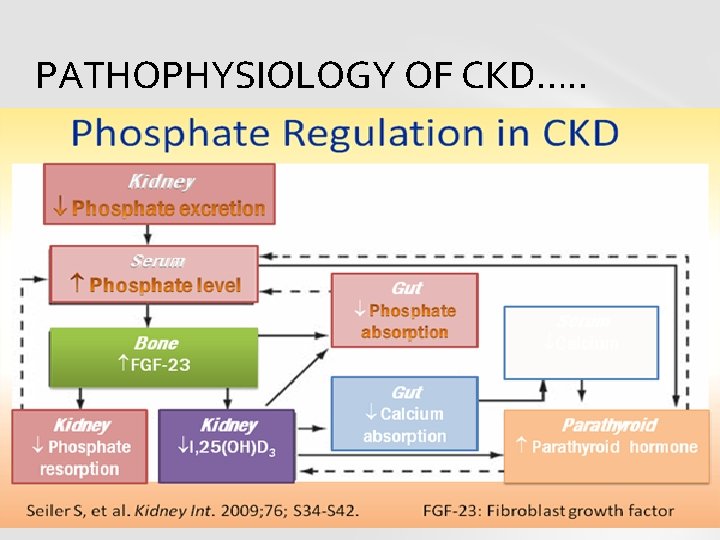
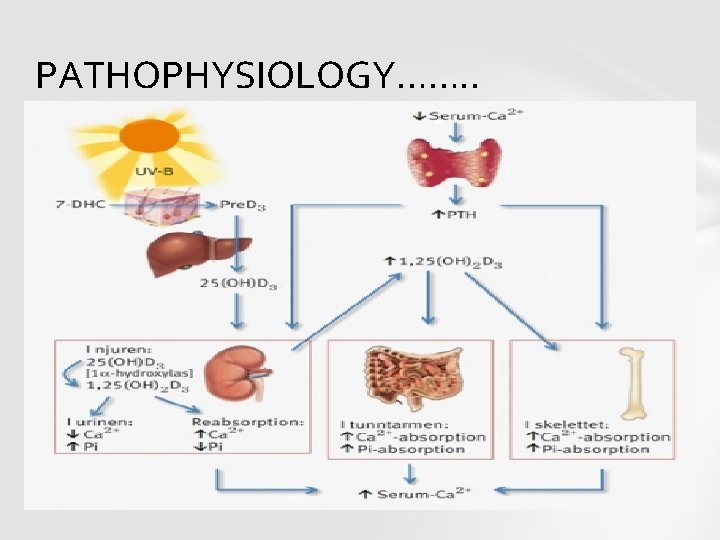
PATHOPHYSIOLOGY OF CKD…. .
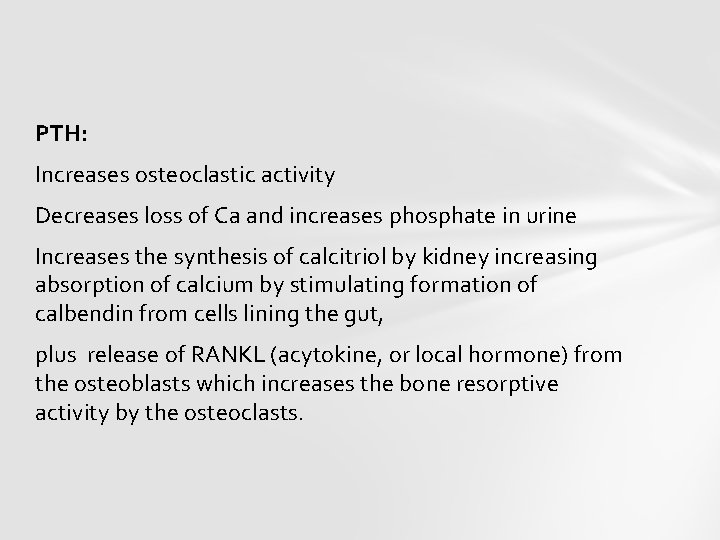
PTH: Increases osteoclastic activity Decreases loss of Ca and increases phosphate in urine Increases the synthesis of calcitriol by kidney increasing absorption of calcium by stimulating formation of calbendin from cells lining the gut, plus release of RANKL (acytokine, or local hormone) from the osteoblasts which increases the bone resorptive activity by the osteoclasts.

PATHOPHYSIOLOGY OF CKD…. . Reduced levels of PTH inhibit removal of calcium from bone , increase the loss of calcium in the urine, inhibit the loss of phosphate, inhibit the formation of calcitriol (1, 25 dihydroxyvitamin D 3) from cholecalciferol (vitamin D 3) by the kidneys. Phosphate in blood form insoluble salts with calcium ions, thereby removing them from the ionized calcium pool.
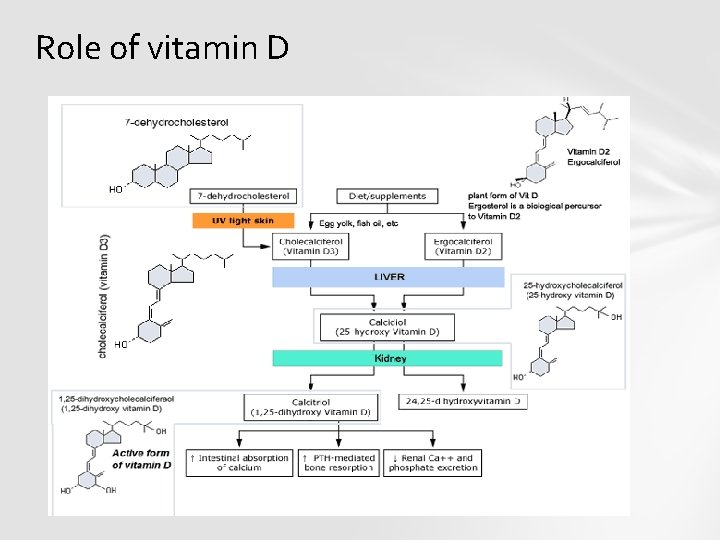
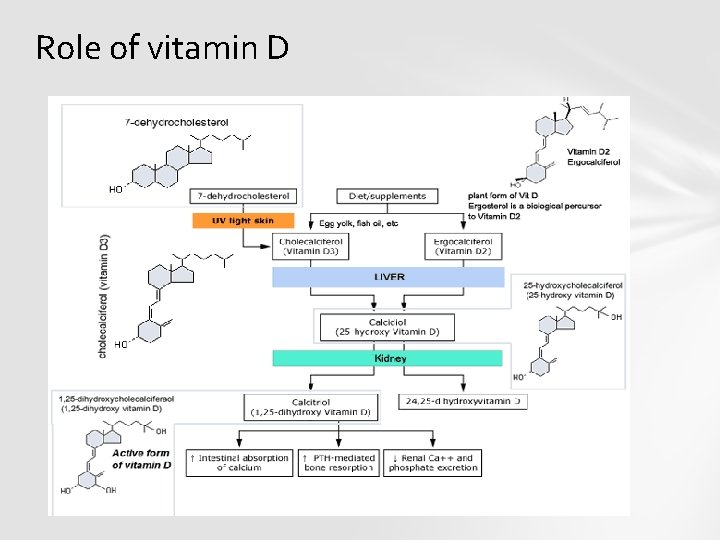
Role of vitamin D
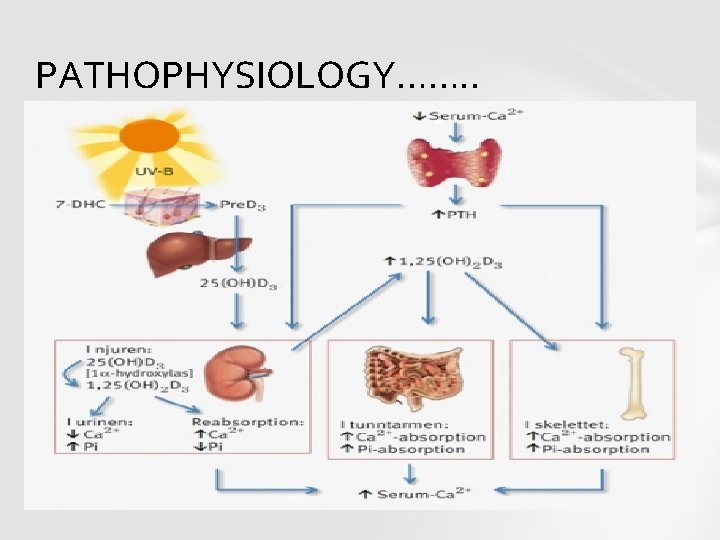
PATHOPHYSIOLOGY……. .
CLINICAL SCENERIO 3 A thirty years old lady presented with hypertension 160/110 mm. Hg and history of photosensitivity, oral ulcers arthralgias and a butterfly rash on face. What is the most immediate step in management a)anti hypertensive management b)corticosteriod c)plasma exchange ANS: A
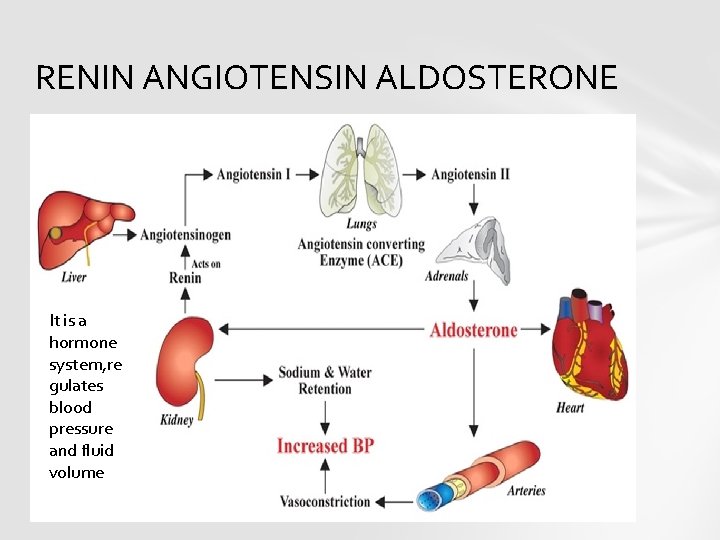
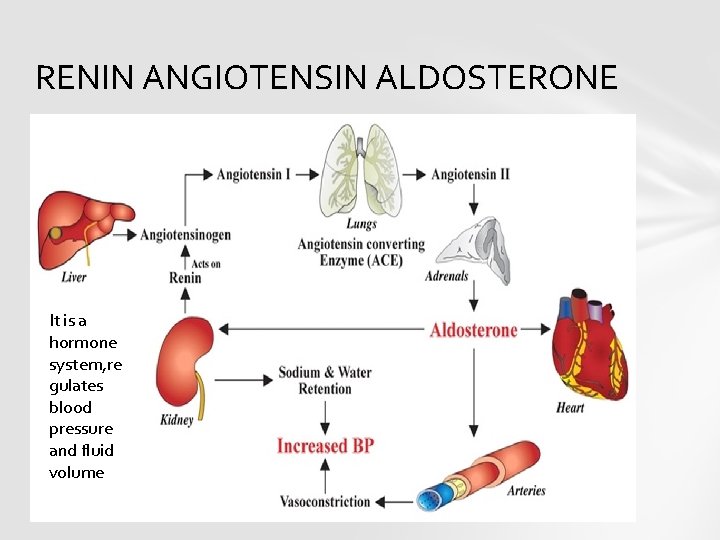
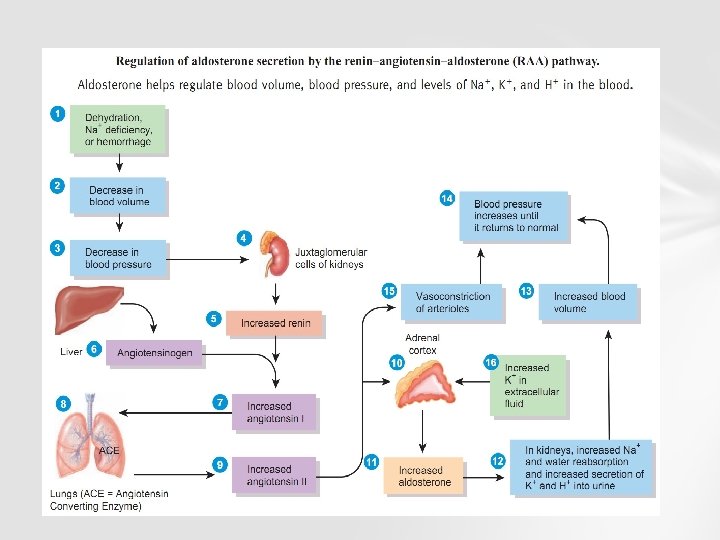
RENIN ANGIOTENSIN ALDOSTERONE It is a hormone system, re gulates blood pressure and fluid volume
TRIGERS FOR ACTIVATION and functions of RAAS loss of blood volume or a drop in blood pressure (such as in hemorrhage or dehydration), interpreted by baroreceptors in the carotid sinus.
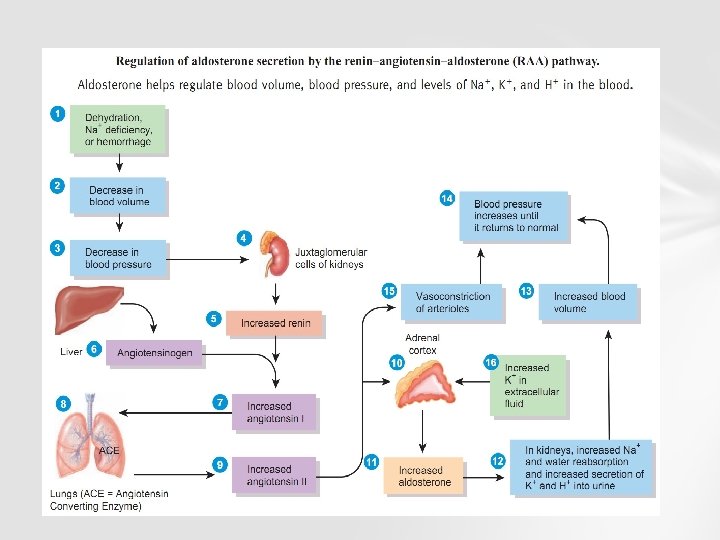
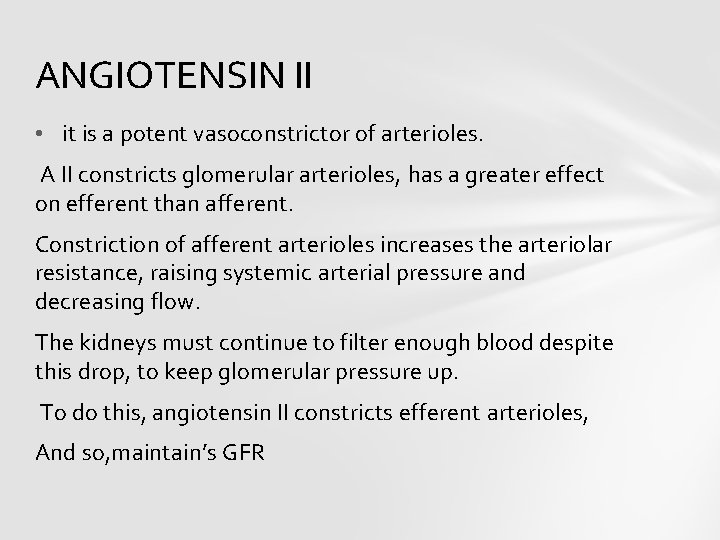
ANGIOTENSIN II • it is a potent vasoconstrictor of arterioles. A II constricts glomerular arterioles, has a greater effect on efferent than afferent. Constriction of afferent arterioles increases the arteriolar resistance, raising systemic arterial pressure and decreasing flow. The kidneys must continue to filter enough blood despite this drop, to keep glomerular pressure up. To do this, angiotensin II constricts efferent arterioles, And so, maintain’s GFR
Angiotensin II stimulates Na+/H+ exchangers on the apical membranes (faces the tubular lumen) of cells in the proximal tubule and thick ascending limb of the loop of Henle in addition to Na+ channels in collecting ducts. This, ultimately, leads to increased sodium reabsorption.
ALDOSTERONE Released from adrenal cortex, in response to angiotensin II. Aldosterone acts on the tubules (e. g. , the DCT and cortical collecting ducts) in the kidneys, causing them to reabsorb more sodium and water from the urine. This increases blood volume and, therefore, increases blood pressure. In exchange for the reabsorbing of sodium to blood, potassium is secreted into the tubules, becomes part of urine and is excreted.
CLINICAL SIGNIFICANCE • Inhibitors of ACE can be used to control blood pressure • ARBs can be used to prevent angiotensin II from acting on angiotensin receptors. • Direct renin inhibitors can also be used for hypertension. • The drugs that inhibit renin are aliskiren.
CLINICAL SCENERIO 4 A 35 years old women attends renal clinic with weight gain and shortness of breath. LABs show a decreased albumin, rasied cholestrol and a 3+ proteinurea on dipstick What is the minimum value of 24 hrs urinary proteins for nephrotic syndrome a)3 g/24 hrs b)3. 5 g/24 hrs c)1 g/24 hrs Answer: B

YOUR PUFFY FACE…………

PUFFY FACE…. CAUSE…NS
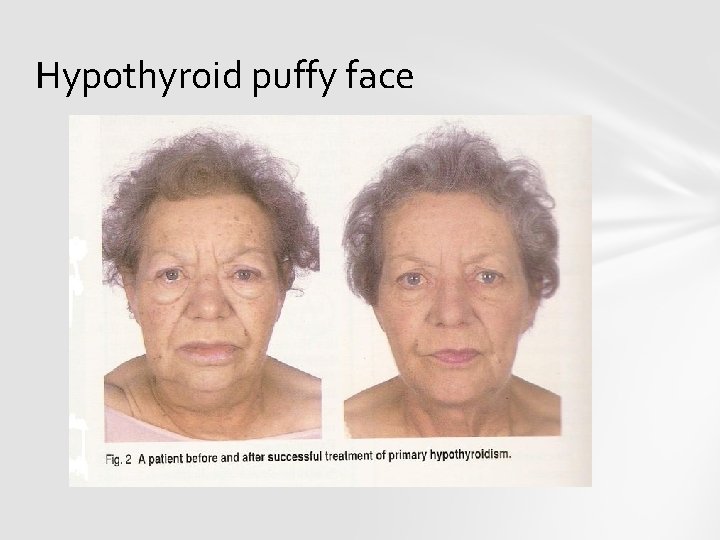
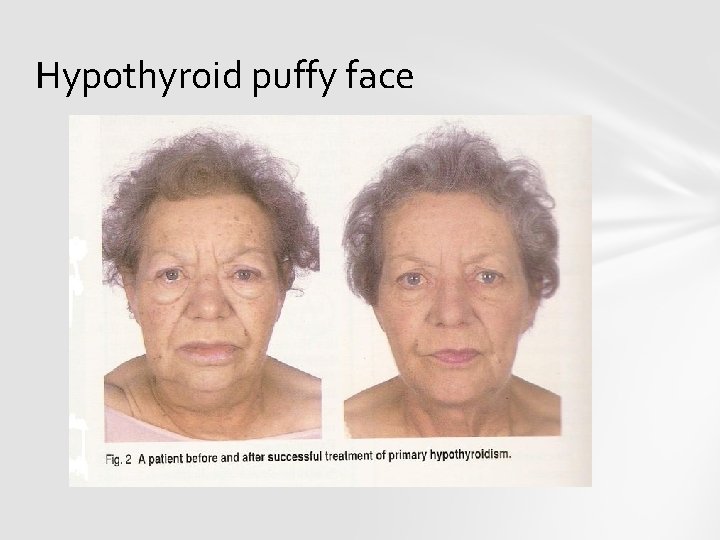
Hypothyroid puffy face
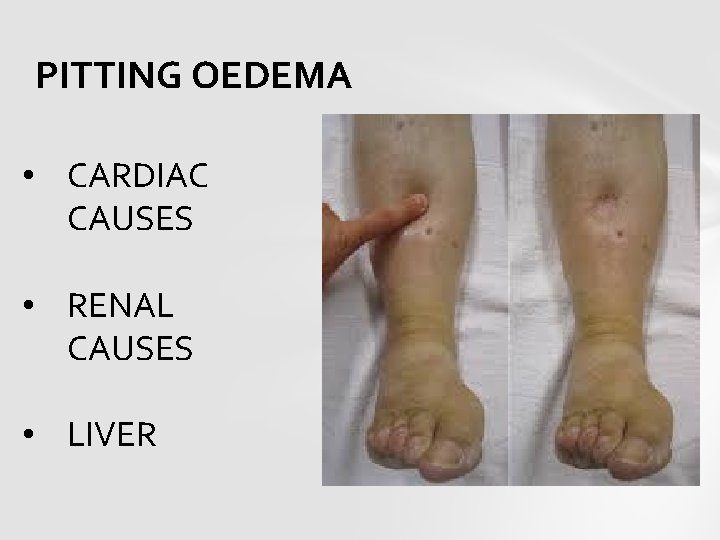
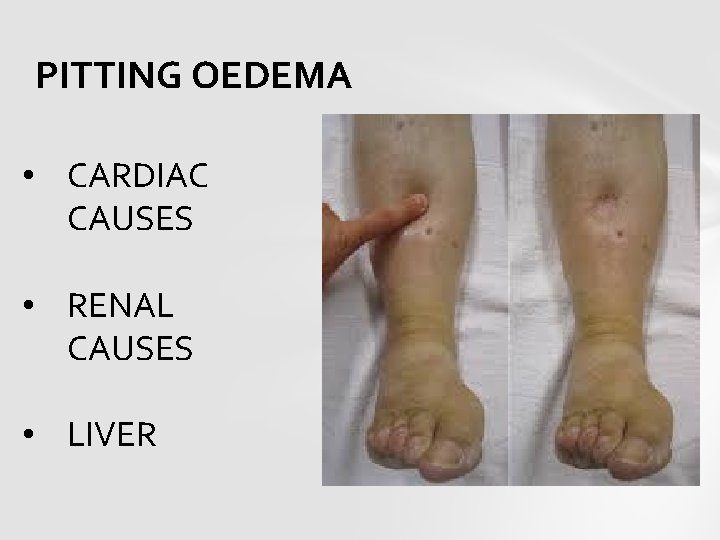
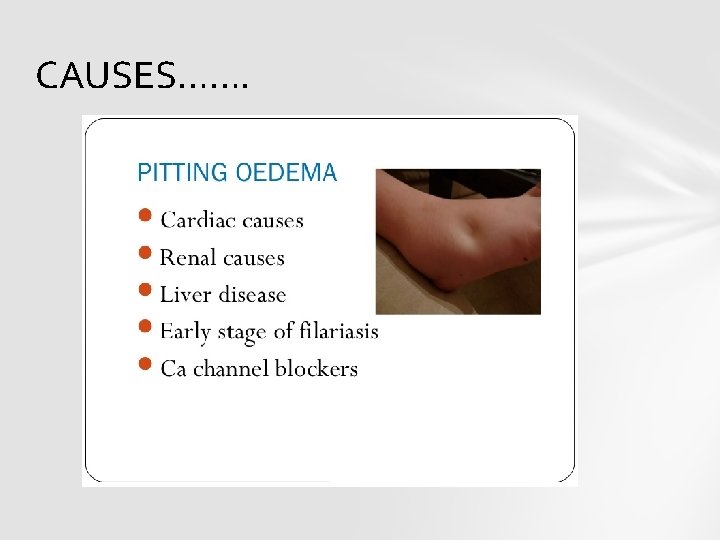
PITTING OEDEMA • CARDIAC CAUSES • RENAL CAUSES • LIVER
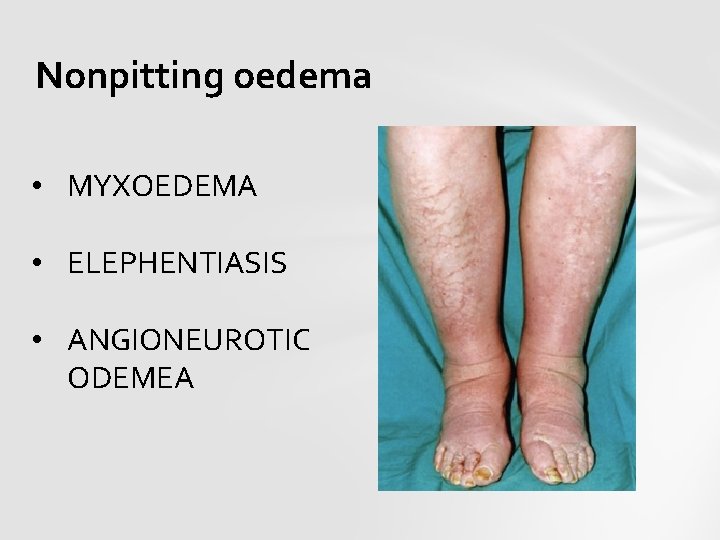
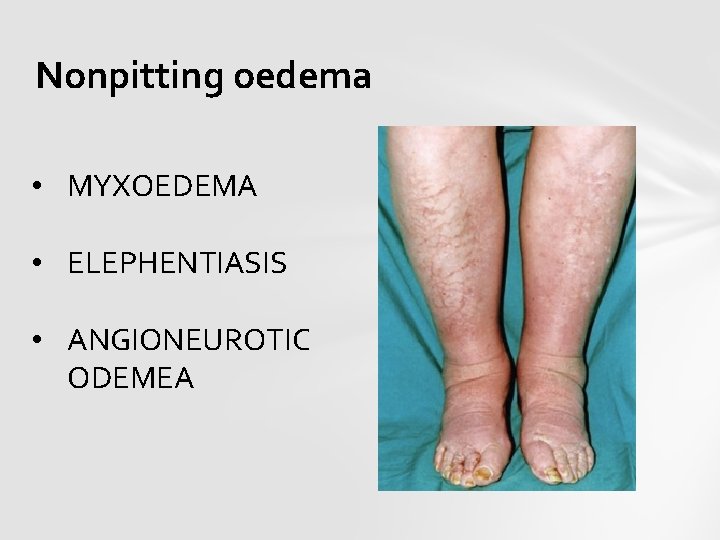
Nonpitting oedema • MYXOEDEMA • ELEPHENTIASIS • ANGIONEUROTIC ODEMEA
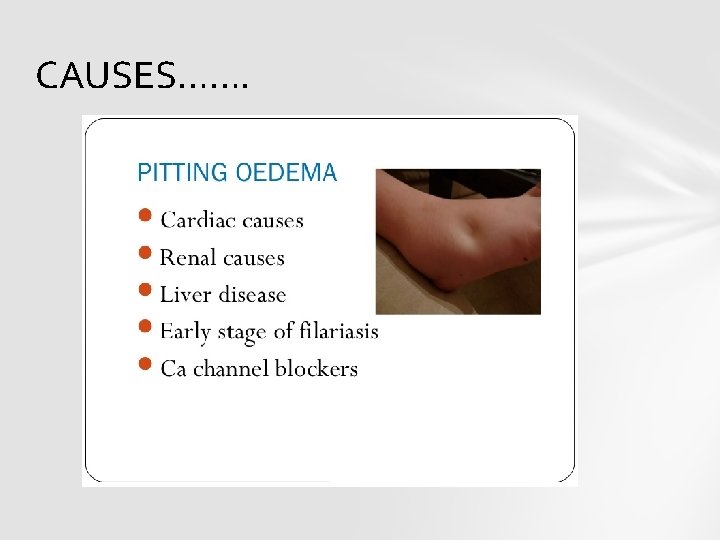
CAUSES…….

Puffy eyes of renal disease
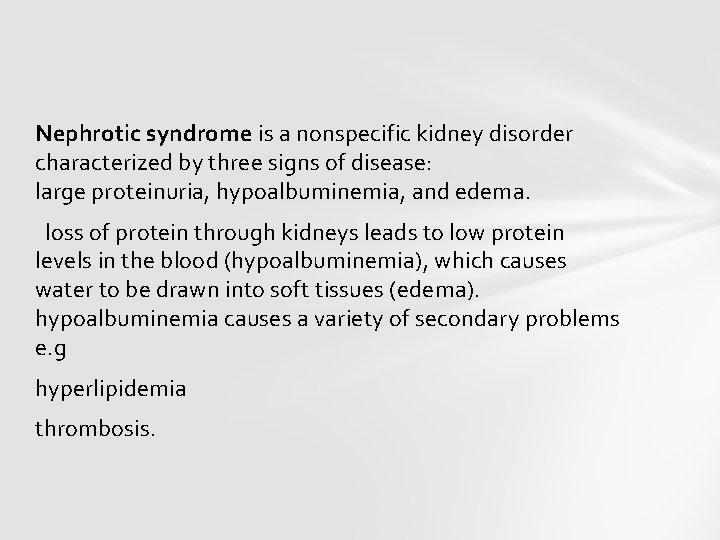
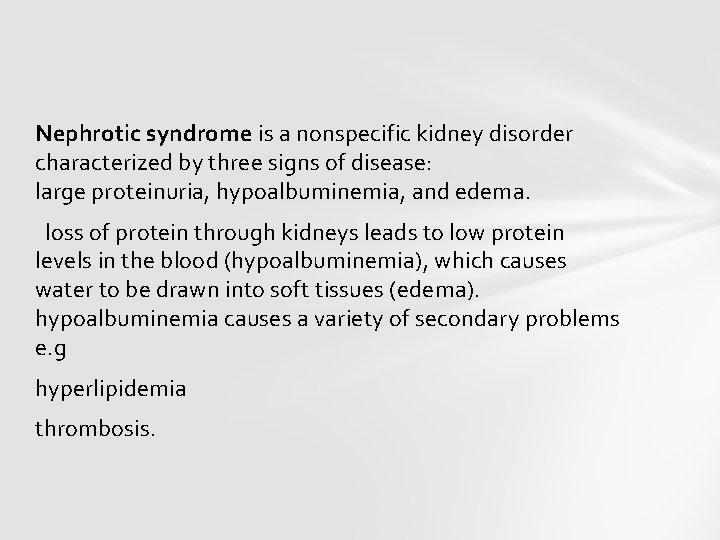
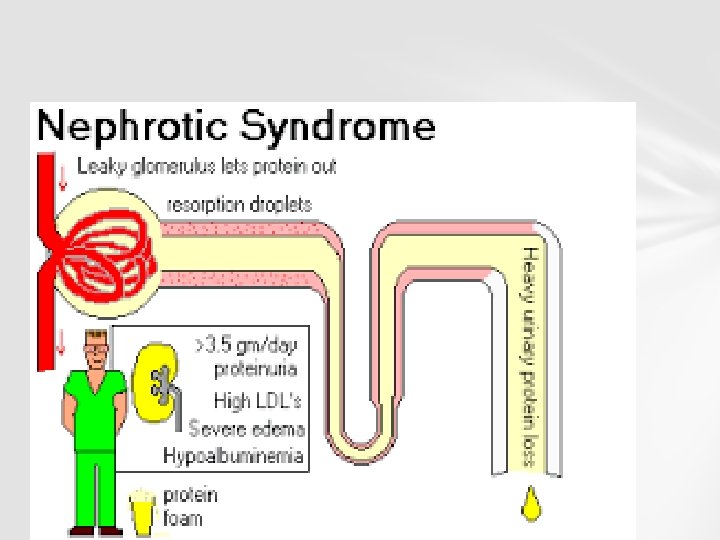
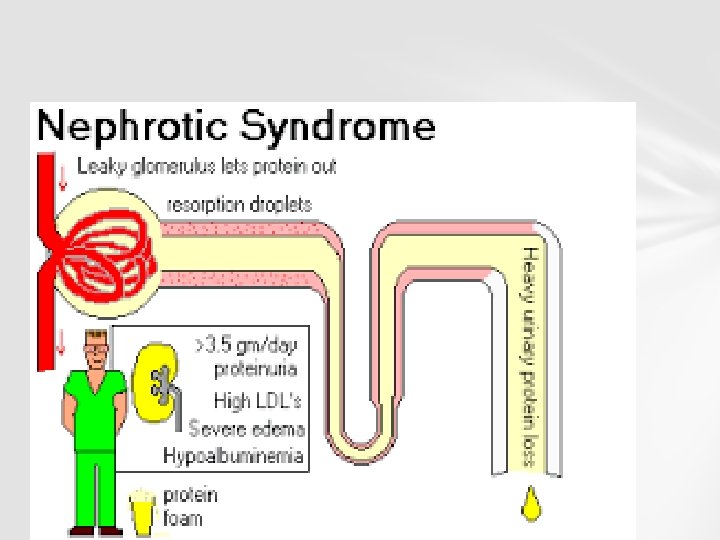
Nephrotic syndrome is a nonspecific kidney disorder characterized by three signs of disease: large proteinuria, hypoalbuminemia, and edema. loss of protein through kidneys leads to low protein levels in the blood (hypoalbuminemia), which causes water to be drawn into soft tissues (edema). hypoalbuminemia causes a variety of secondary problems e. g hyperlipidemia thrombosis.
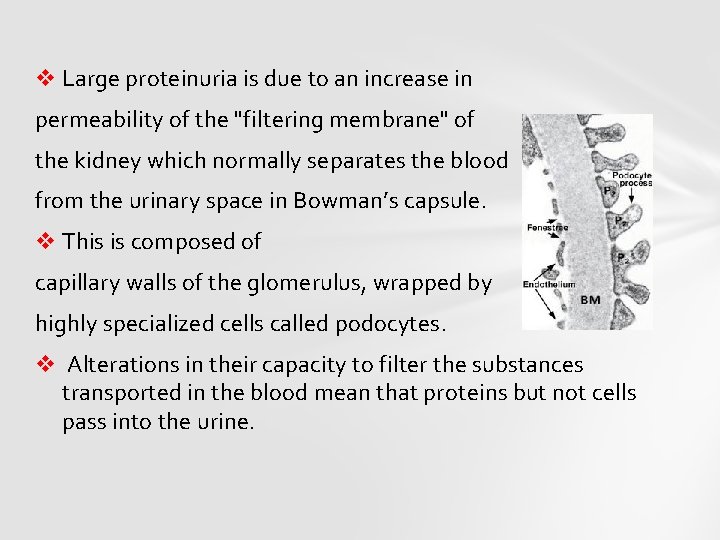
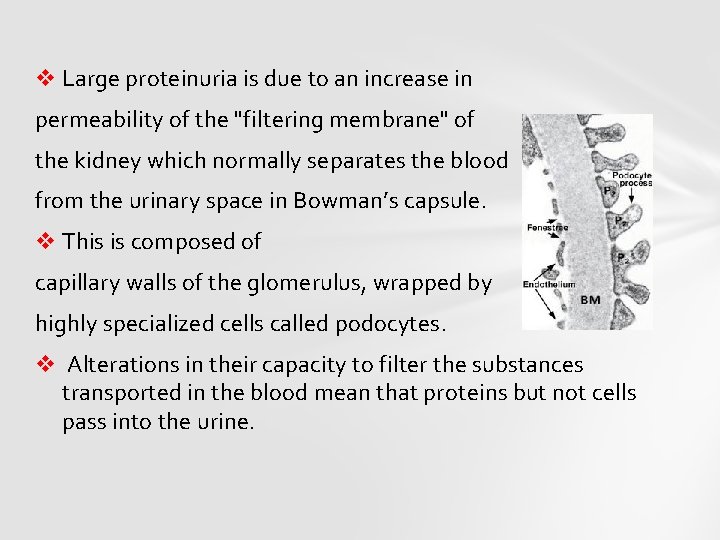
v Large proteinuria is due to an increase in permeability of the "filtering membrane" of the kidney which normally separates the blood from the urinary space in Bowman’s capsule. v This is composed of capillary walls of the glomerulus, wrapped by highly specialized cells called podocytes. v Alterations in their capacity to filter the substances transported in the blood mean that proteins but not cells pass into the urine.
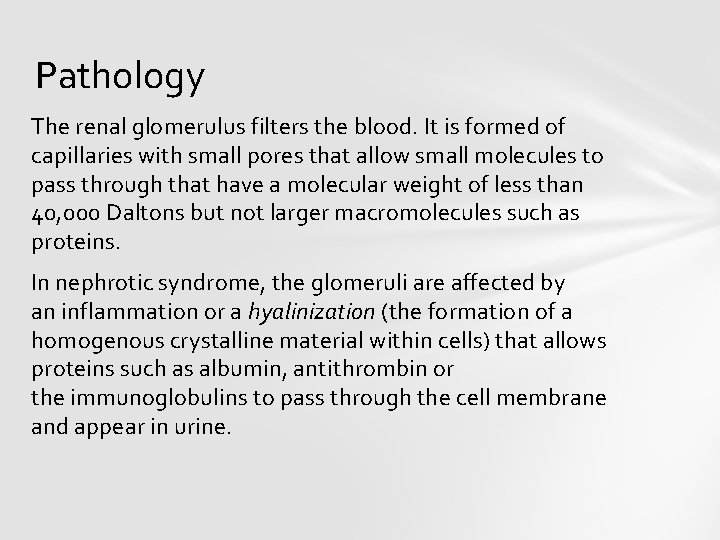
Pathology The renal glomerulus filters the blood. It is formed of capillaries with small pores that allow small molecules to pass through that have a molecular weight of less than 40, 000 Daltons but not larger macromolecules such as proteins. In nephrotic syndrome, the glomeruli are affected by an inflammation or a hyalinization (the formation of a homogenous crystalline material within cells) that allows proteins such as albumin, antithrombin or the immunoglobulins to pass through the cell membrane and appear in urine.
Albumin maintains oncotic pressure, which prevents the leakage of fluid into the extracellular medium and the subsequent formation of edemas. In response to hypoproteinemia the liver commences a compensatory mechanism involving the synthesis of proteins, such as alpha-2 macroglobulin and lipoproteins.
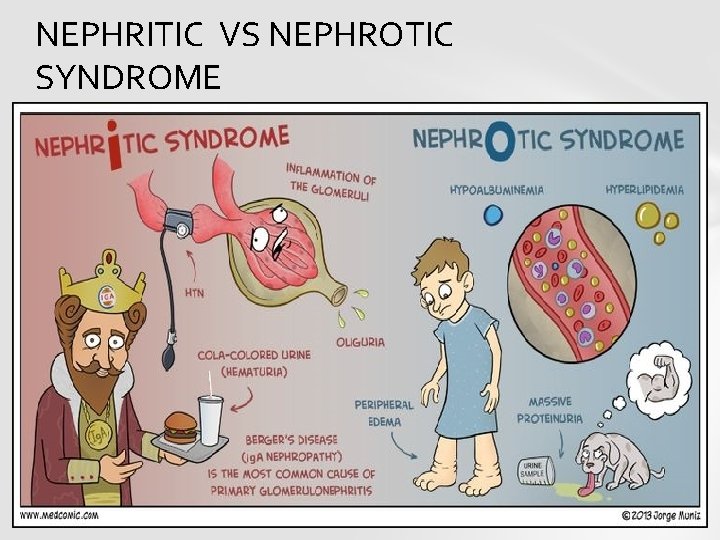
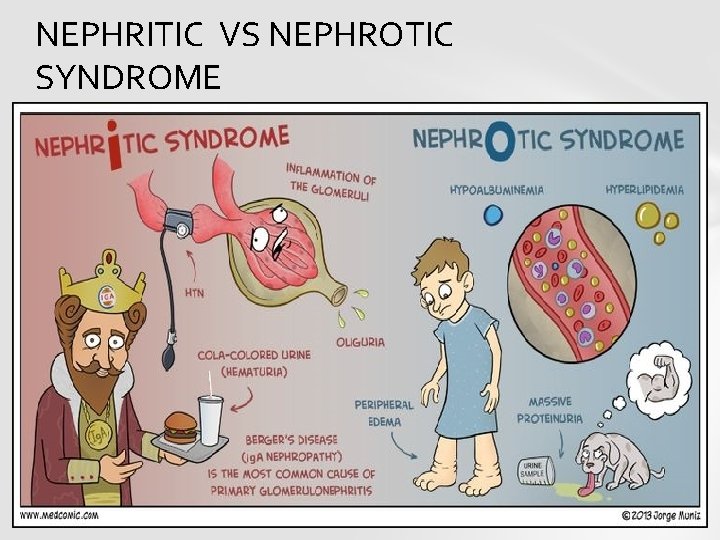
NEPHRITIC VS NEPHROTIC SYNDROME
Signs • The most common sign is excess fluid in the body due to the serum hypoalbuminemia. • Lower serum oncotic pressure causes fluid to accumulate in the interstitial tissues. • Sodium and water retention aggravates the edema. This may present as: • Puffiness around the eyes, characteristically in the morning. • Pitting edema over the legs.
• Pleural effusion, pulmonary edema. • Ascites. • Anasarca • Foamy or frothy urine • Anemia d/t loss of transferrin • Examination should also exclude other causes of gross edema—e. g cardiovascular and hepatic system.
Edema Caused either by hypoalbuminemia which lowers the oncotic pressure within vessels resulting in hypovolemia Activation of RAS Albumin causes a direct effect on the epithelial sodium channel (ENa. C) on the principal cell that leads to the reabsorption of sodium and water.
Hyperlipidemia is caused by increase in the synthesis of low and very low-density lipoproteins in the liver that are responsible for the transport of cholesterol and triglycerides. Overproduction of lipoproteins Decreased lipid catabolism of lipids d/t decreased lipoprotein lipase
CAUSES Primary: There is no obvious cause of the disease.
NEPHROTIC SYNDROME Secondary causes Diabetic nephropathy, SLE, Sarcoidosis Syphilis, Hepatitis B, Sjögren's syndrome HIV, Amyloidosis Multiple myeloma, Vasculitis Cancer Genetic disorders Drugs

THANK YOU VERY MUCH