1 APPROACH TO PROTENURIA Mehryar Mehrkash Pediatric Nephrologist
































- Slides: 68

1 APPROACH TO PROTENURIA Mehryar Mehrkash Pediatric Nephrologist
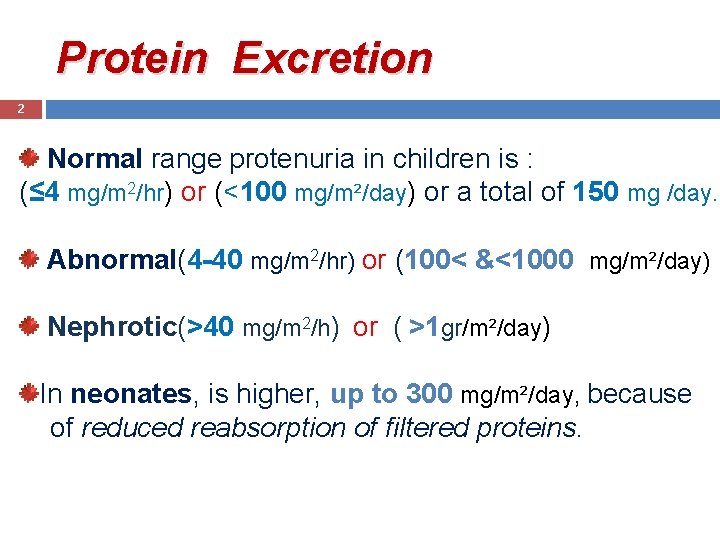
Protein Excretion 2 Normal range protenuria in children is : (≤ 4 mg/m 2/hr) or (<100 mg/m²/day) or a total of 150 mg /day. Abnormal(4 -40 mg/m 2/hr) or (100< &<1000 mg/m²/day) Nephrotic(>40 mg/m 2/h) or ( >1 gr/m²/day) In neonates, is higher, up to 300 mg/m²/day, because of reduced reabsorption of filtered proteins.
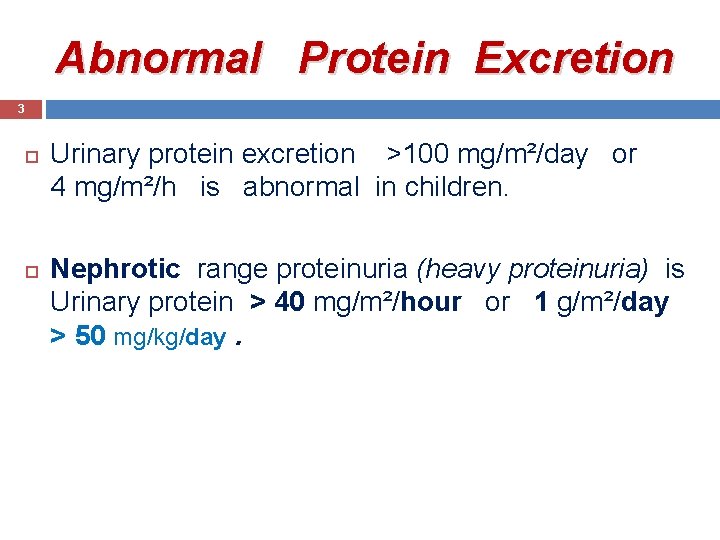
Abnormal Protein Excretion 3 Urinary protein excretion >100 mg/m²/day or 4 mg/m²/h is abnormal in children. Nephrotic range proteinuria (heavy proteinuria) is Urinary protein > 40 mg/m²/hour or 1 g/m²/day > 50 mg/kg/day.
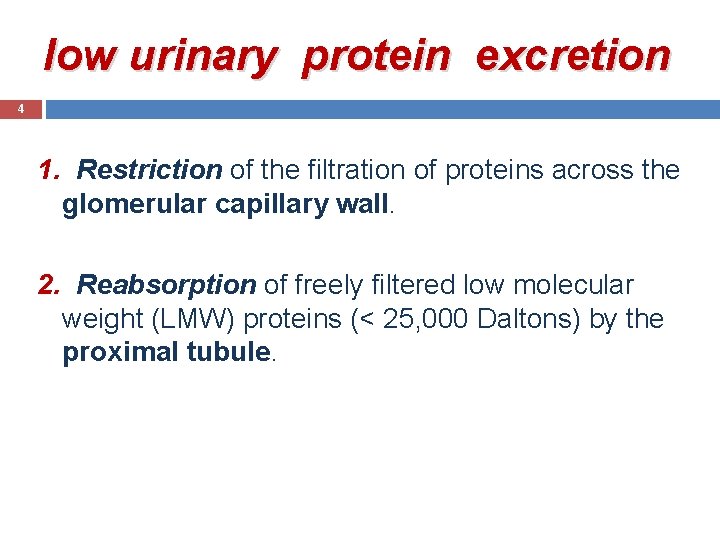
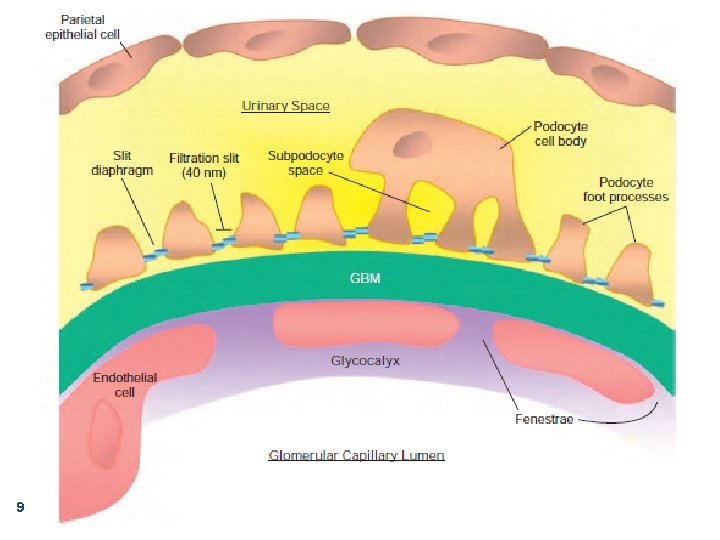
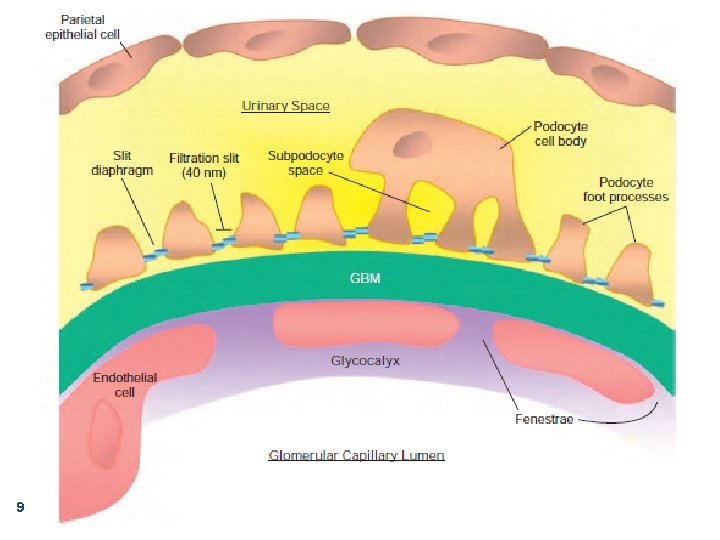
low urinary protein excretion 4 1. Restriction of the filtration of proteins across the glomerular capillary wall. 2. Reabsorption of freely filtered low molecular weight (LMW) proteins (< 25, 000 Daltons) by the proximal tubule.
5 Mechanisms of protein excretion 1. 2. 3. Glomerular Tubular Overflow proteinuria


7

8
9

Glomerular basal membrane 10

Glomerular barrier tubule • Normally, the larger proteins are excluded at the glomerular barrier. • Smaller proteins can pass, but are mostly reabsorbed. 11
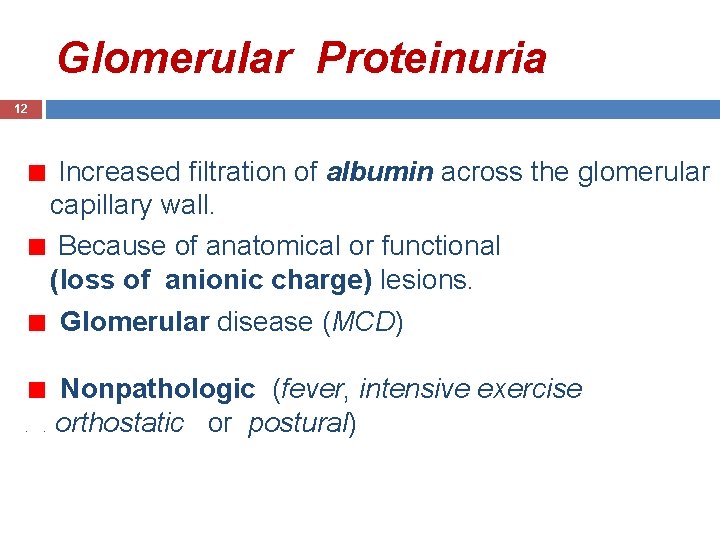
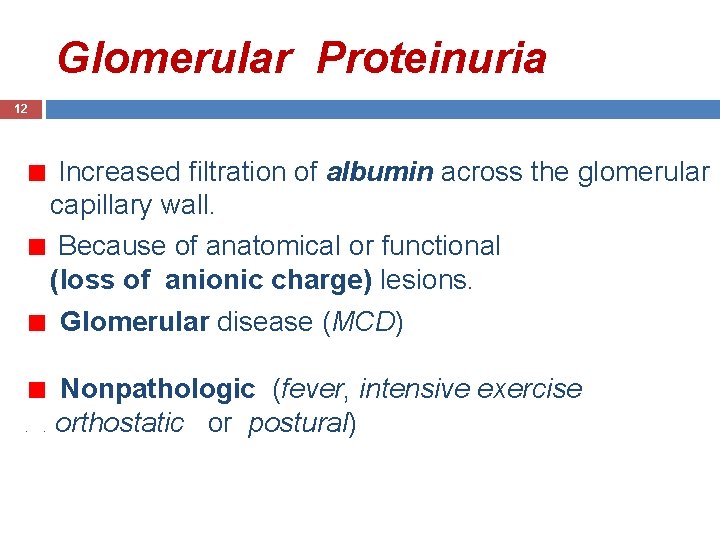
Glomerular Proteinuria 12 Increased filtration of albumin across the glomerular capillary wall. Because of anatomical or functional (loss of anionic charge) lesions. Glomerular disease (MCD) . Nonpathologic (fever, intensive exercise orthostatic or postural) .
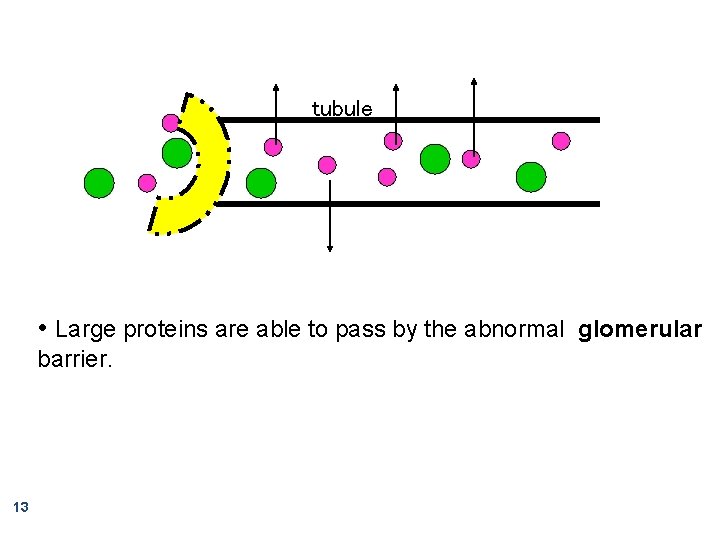
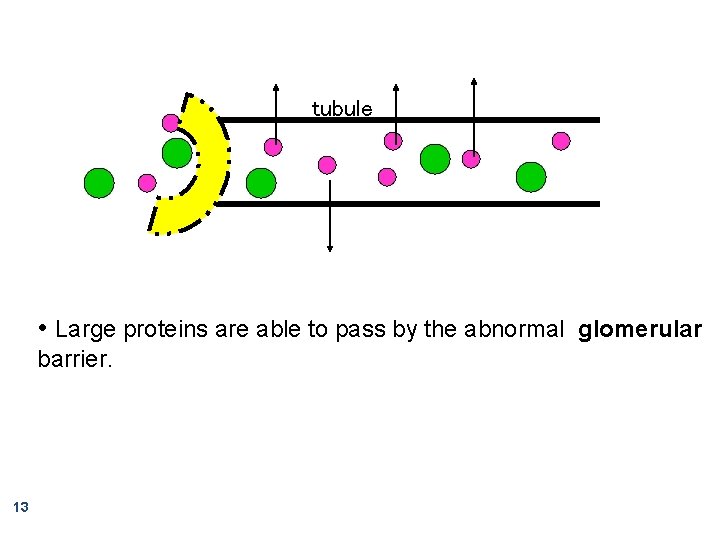
tubule • Large proteins are able to pass by the abnormal glomerular barrier. 13
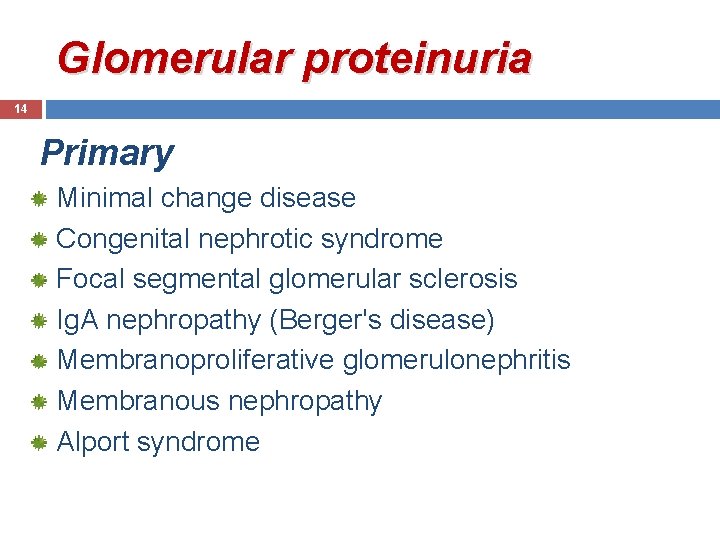
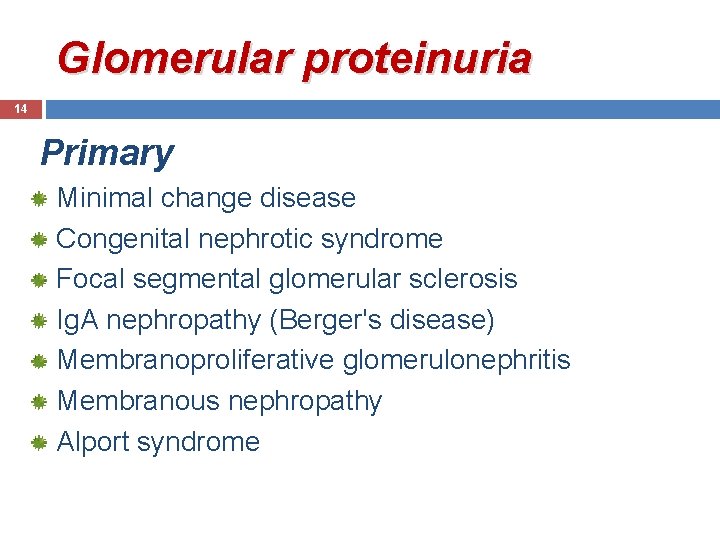
Glomerular proteinuria 14 Primary Minimal change disease Congenital nephrotic syndrome Focal segmental glomerular sclerosis Ig. A nephropathy (Berger's disease) Membranoproliferative glomerulonephritis Membranous nephropathy Alport syndrome

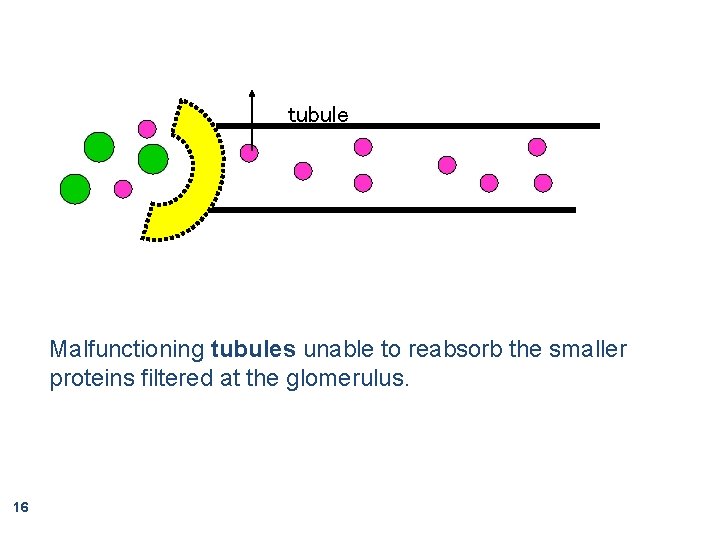
Tubular Proteinuria 15 low molecular weight proteins such as β 2 microglobulin, α 1 -microglobulin, and retinol-binding protein. These molecules filtered across the glomerulus and reabsorbed in the proximal tubule. . Associated with other defects in proximal tubular function( glycosuria, RTA 2 , and phosphaturia).
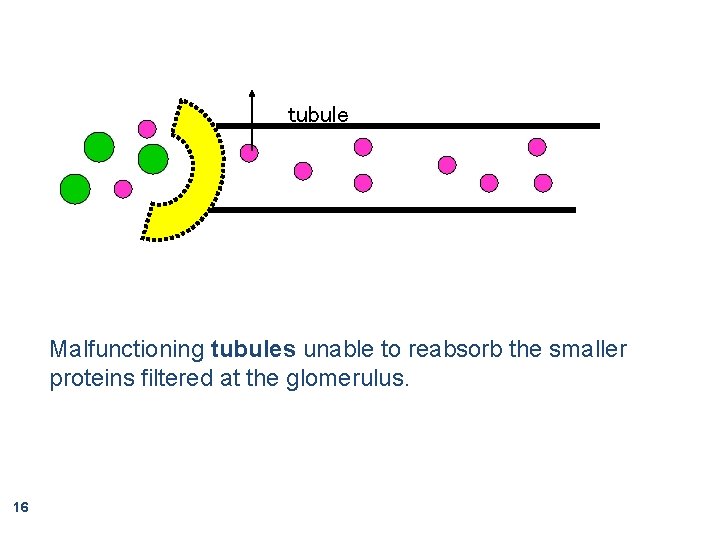
tubule Malfunctioning tubules unable to reabsorb the smaller proteins filtered at the glomerulus. 16

Tubular proteinuria 17 Fanconi syndrome Heavy metal poisoning Acute tubular necrosis Tubulointerstitial nephritis Secondary to obstructive uropathy
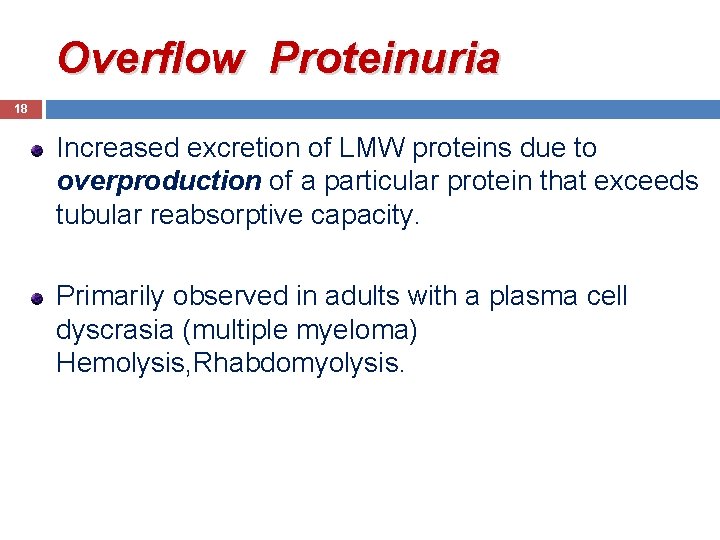
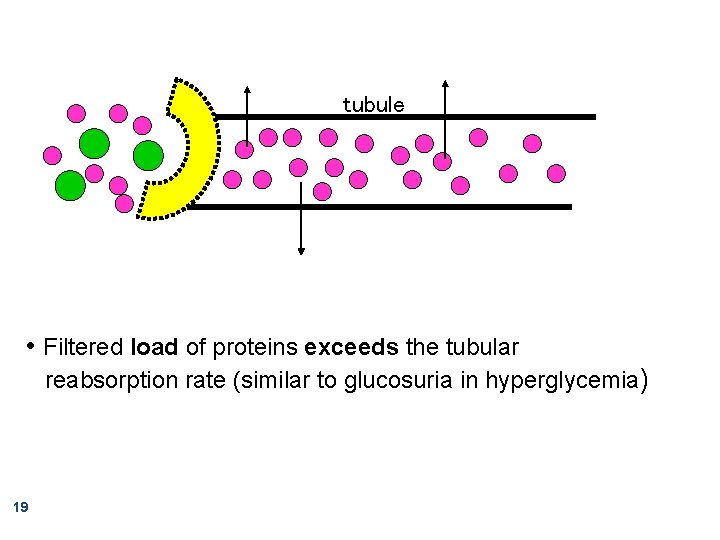
Overflow Proteinuria 18 Increased excretion of LMW proteins due to overproduction of a particular protein that exceeds tubular reabsorptive capacity. Primarily observed in adults with a plasma cell dyscrasia (multiple myeloma) Hemolysis, Rhabdomyolysis.
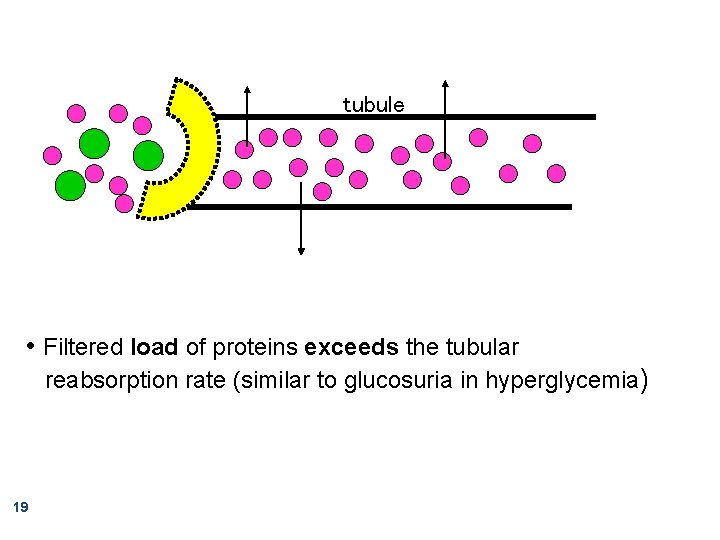
tubule • Filtered load of proteins exceeds the tubular reabsorption rate (similar to glucosuria in hyperglycemia) 19

20
tubule • Filtered load of proteins exceeds the tubular reabsorption rate (similar to glucosuria in hyperglycemia) 21
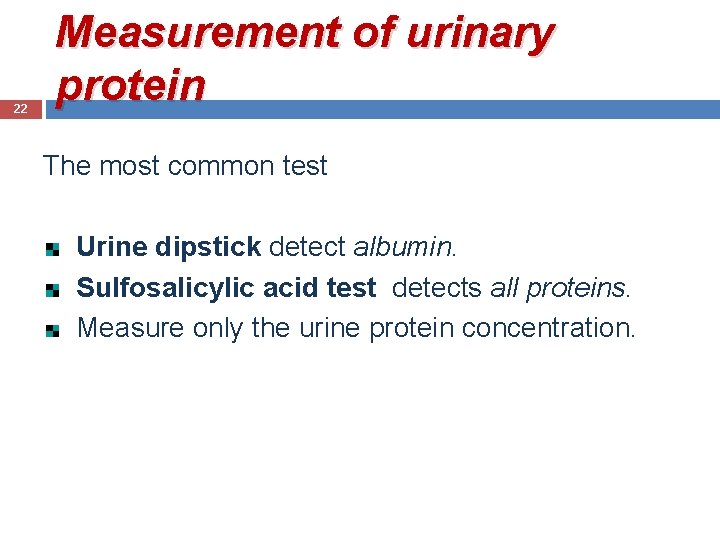
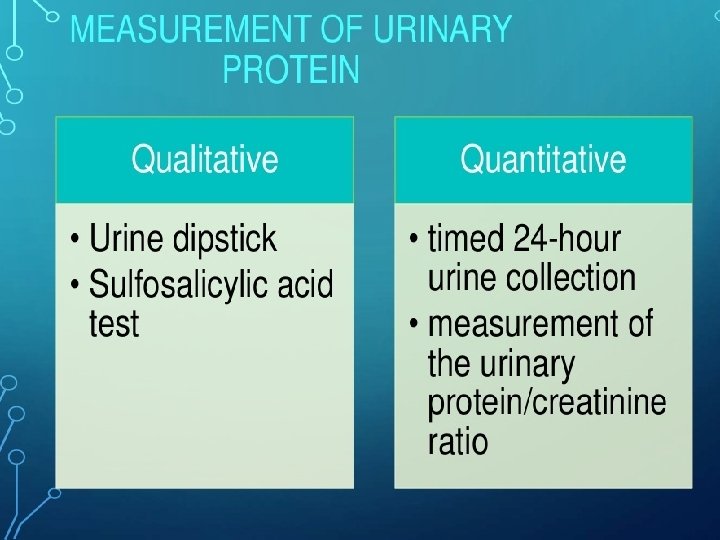
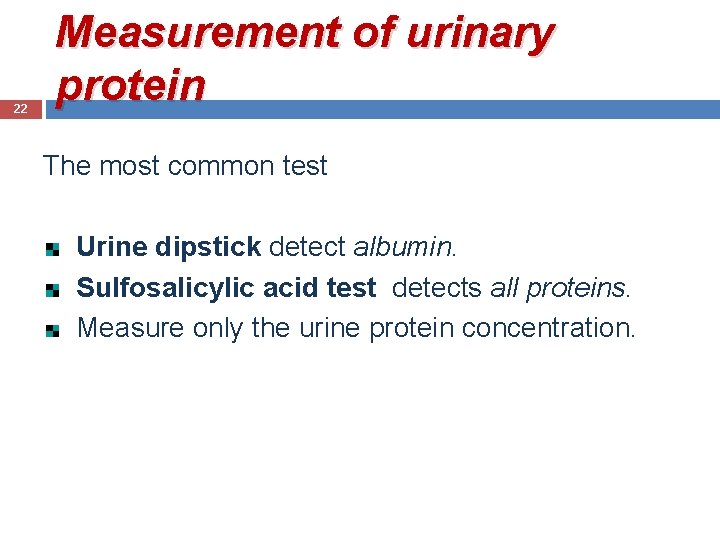
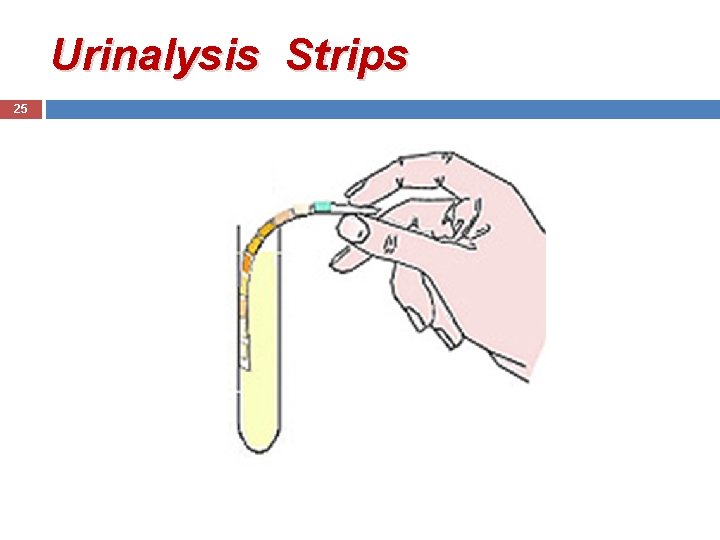
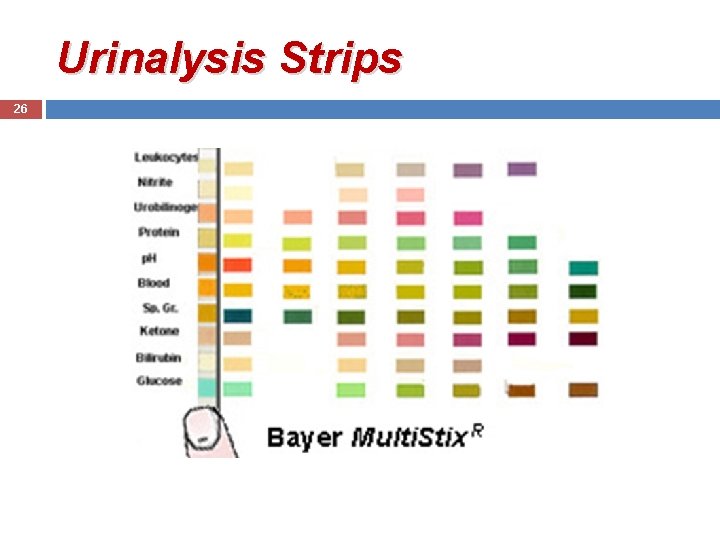
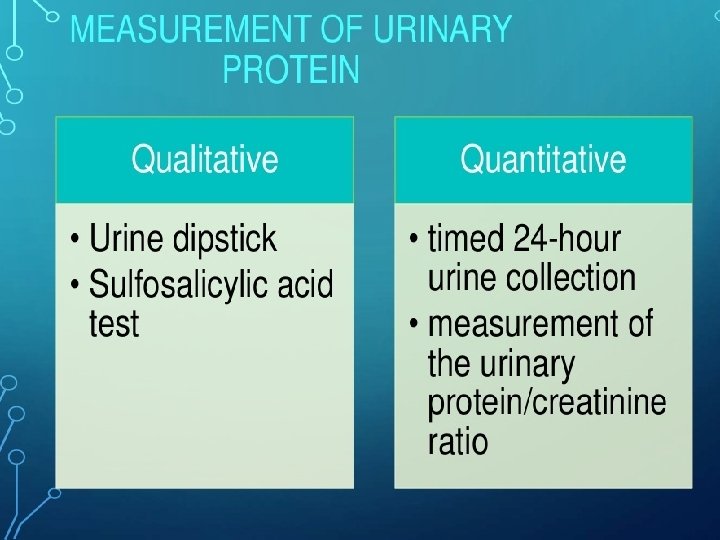
22 Measurement of urinary protein The most common test Urine dipstick detect albumin. Sulfosalicylic acid test detects all proteins. Measure only the urine protein concentration.
Urine Dipstick 23 Measures albumin via a colorimetric reaction between albumin and tetrabromophenol blue producing different shades of green. Dipstick testing will not detect LMW proteins.
Urinalysis Strips 24
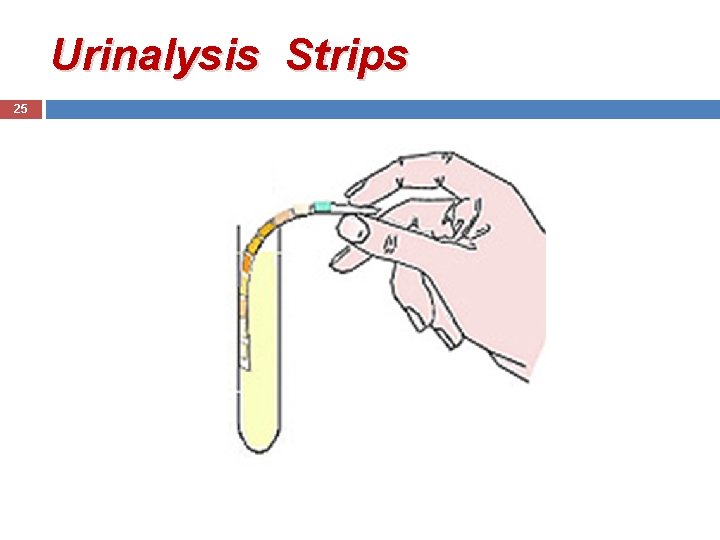
Urinalysis Strips 25
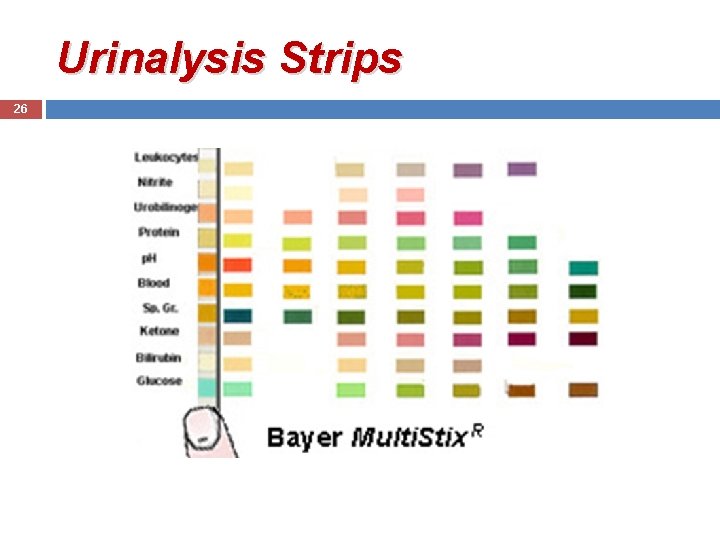
Urinalysis Strips 26
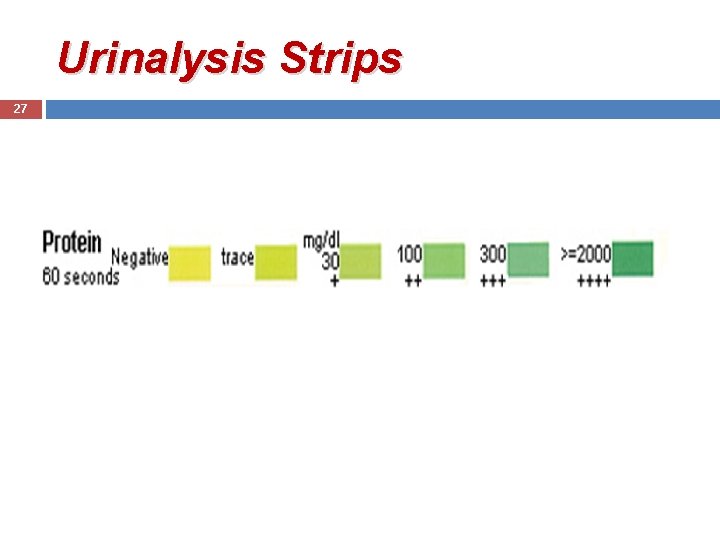
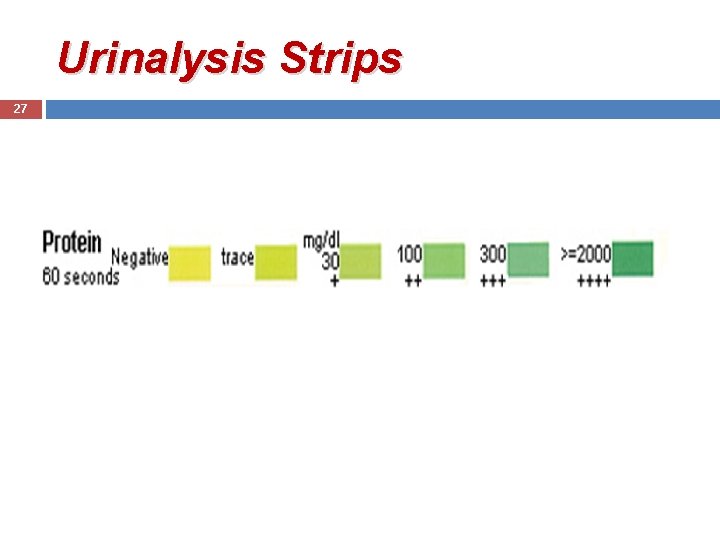
Urinalysis Strips 27
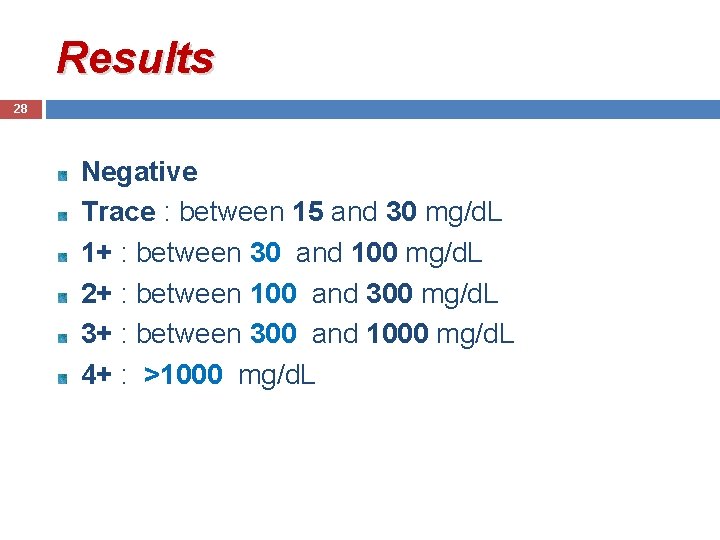
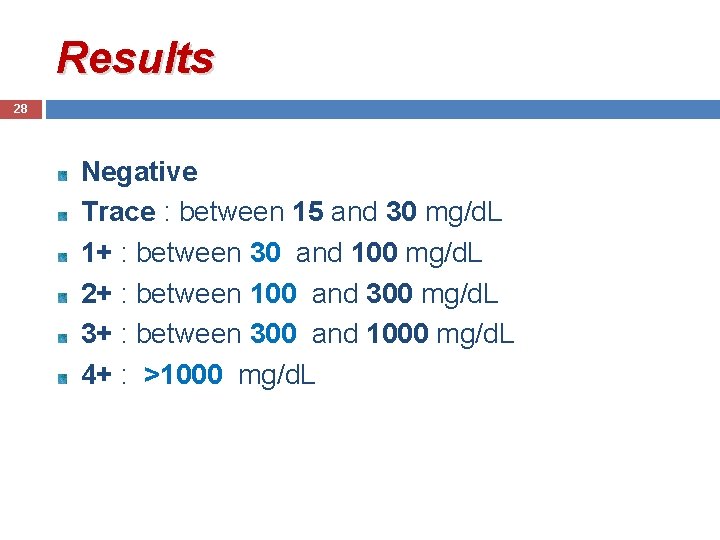
Results 28 Negative Trace : between 15 and 30 mg/d. L 1+ : between 30 and 100 mg/d. L 2+ : between 100 and 300 mg/d. L 3+ : between 300 and 1000 mg/d. L 4+ : >1000 mg/d. L

False-Negative 29 Dilute urine (specific gravity <1005) Urinary protein is not albumin

False-Positive 30 Highly concentrated urine ( SG >1025) Gross hematuria Urinary p. H >7. 0 Contaminated by antiseptic agents (chlorhexidine, benzalkonium chloride, hydrogen peroxide ) Phenazopyridine Iodinated radiocontrast
Quantitative Assessment 31 Children with persistent dipstick-positive proteinuria must undergo a quantitative measurement of protein excretion (timed 24 -hour urine collection).

Quantitative Assessment 32 Protein/cr ratio on a spot urine sample, in the first morning specimen. The normal value is <0. 2 in children greater than two years of age and <0. 5 in infants and toddlers from 6 to 24 months.

33 Proteinuria in children presents in three ways 1. Transient or intermittent 2. Orthostatic 3. Persistent
Transient proteinuria 34 Most common cause Fever, Exercise, Stress, Seizures, and Hypovolemia, or Exposure to extreme cold, act by altering renal hemodynamics.

Transient proteinuria Follow-up routinely Patient should have a repeat urinalysis on a first morning void in one year
Orthostatic Proteinuria 36 Increased protein excretion in the upright position (to 10 -fold) which returns to normal in the supine position. Common cause of proteinuria, in adolescent boys. Generally <1 g/day.

Orthostatic Proteinuria 37 The disorder is uncommon over the age of 30 years. The diagnosis by a negative dipstick on the first morning voided specimen.
Orthostatic Proteinuria 38 A short period (15 to 20 minutes) of maximal exercise increased Pr/Cr ratios. It is wise to delay measurement, for a period of 24 hours after exercise.

Orthostatic Proteinuria 39 A normal Pr/Cr ratio on the first morning void and dipstick-positive proteinuria on the second upright specimen indicate orthostatic proteinuria. In transient or orthostatic proteinuria, repeat urinalysis on a first morning void in one year.

Orthostatic Proteinuria Pathogenesis � Exaggeration normal response of transient increase protein in upright posture. � Subtle glomerular abnormalities. � Renal vein compression by aorta or superior mesenteric artery.
Prognosis 41 Benign condition, normal renal function after as long as 50 y of follow-up. The proteinuria resolves spontaneously, being present 50 percent at 10 years and only 17 percent at 20 years.

Persistent Proteinuria 42 Underlying renal disease v A positive dipstick for protein on a random U/A is common in children aged 8 -15 y (5 to 10%). . v Only 0. 1% of children have persistent proteinuria.
Persistent Proteinuria 43 In Glomerular and/or Parenchymal disease hematuria , red cell casts , pyuria , and/or lipiduria. RBC casts are pathognomonic for the GN.

Underlying disorder 44 Primarily renal (glomerular and interstitial diseases) Secondary to a systemic process (infections, rheumatologic , immunologic).
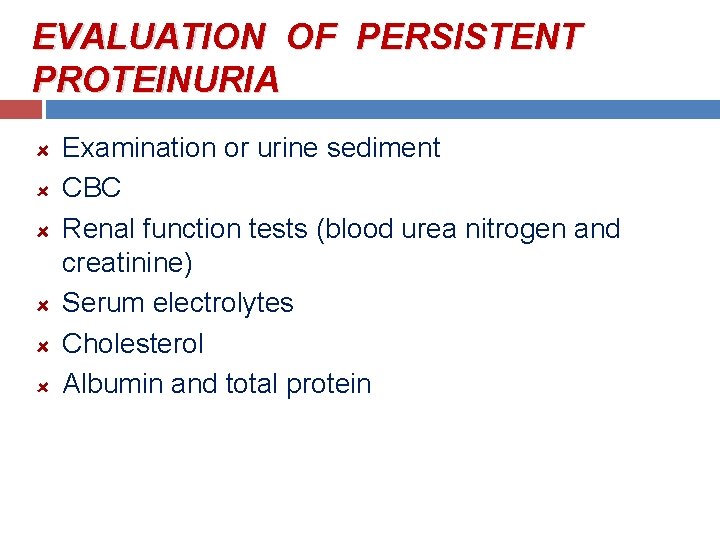
EVALUATION OF PERSISTENT PROTEINURIA Examination or urine sediment CBC Renal function tests (blood urea nitrogen and creatinine) Serum electrolytes Cholesterol Albumin and total protein
46 History , physical examination History of febrile illness, intensive physical exercise or a seizure Change in urine volume or color Edema Increased BP Recent streptococcal infection Family history renal disease. hearing loss (underlying disease)

Approach 47 If this initial evaluation is normal, the urine dipstick repeated on at least two additional specimens. If these tests are negative, the diagnosis is transient proteinuria.
Approach 48 The simplest approach is to measure the Pr/Cr on a first morning void obtained at home. A normal Pr/Cr on the first morning void indicate Orthostatic proteinuria. Elevated Pr/Cr on both specimens indicate persistent proteinuria.

LABORATORY EVALUATION Single urine positive for protein Obtain: 1) first morning void Pr/Cr 2) UA in office Pr/Cr and UA normal Pr/Cr normal, UA positive Both specimens abnormal Transient Proteinuria Orthostatic Proteinuria Persistent Proteinuria
UTI 50 Pyuria, bacteriuria, nitrites or leukocyte esterase with mild proteinuria. Proteinuria in UTI resolves with treatment of the infection. If the proteinuria persists after eradication of the infection, further work-up is indicated.
Asymptomatic Proteinuria Levels of protein excretion above the upper limits of normal for age No clinical manifestations such as edema, hematuria, oliguria, and hypertension

Asymptomatic Patients 52 With low-grade proteinuria (Pr/Cr 0. 2 -1. 0) Periodic re-evaluation (every 4 -6 m) Physical Exam BP U/A Cr Pr/Cr first morning urine
Management Avoid excessive restrictions in child’s lifestyle Dietary protein supplementation is of no benefit Salt restriction unnecessary (potentially dangerous) No indication for limitation of activity Regular follow-up
Symptomatic Child 54 General and nonspecific (fever, malaise, weight loss) Specific (edema, HTN, renal insufficiency).

Laboratory Evaluation 55 Renal function tests Serum electrolytes Cholesterol Albumin, total protein C 3 , C 4, ANA, streptozyme testing, hepatitis B and C , HIV Renal ultrasound

Indications for renal biopsy 56 Close monitoring if urinary protein < 500 mg/m²/day before biopsy. Assessment of BP, protein excretion, and renal function. If any of these parameters shows evidence of progressive disease, a renal biopsy performed.

57

Nephrotic syndrome 58
Nephrotic syndrome 59 Heavy proteinuria (spot urine Pr/Cr ratio > 2 or than 50 mg/kg/d) Serum albumin < 3 g/d. L Edema Hypercholesterolemia > 250 mg

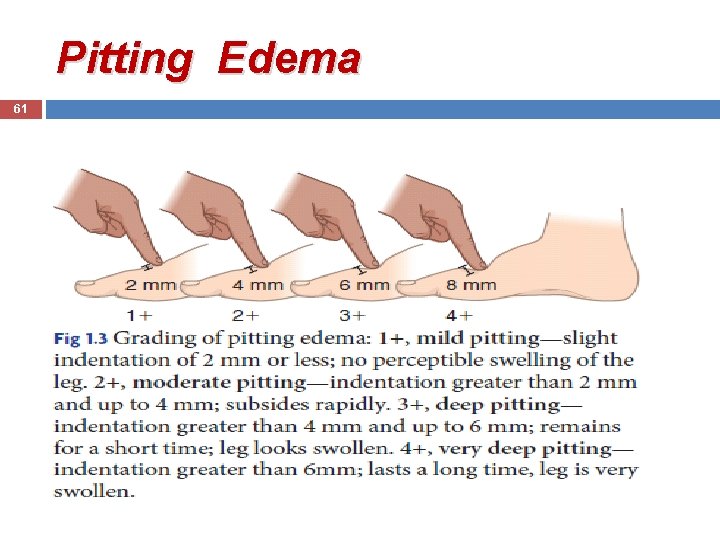
Pitting Edema 60
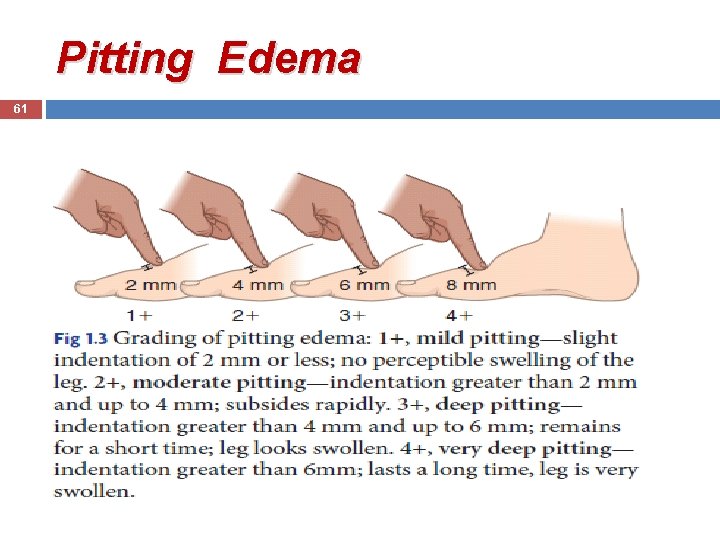
Pitting Edema 61

Pitting Edema 62
63 Mechanisms of glomerular injury Circulating nonimmune factors ( minimal change disease , primary FSGS). Circulating immune factors (MPGN, PSGN, lupus nephritis). Mutations in podocyte or slit diaphragm proteins (podocin , nephrin) in inherited forms of congenital, infantile, or glucocorticoid resistant nephrotic syndrome.

64 Classification Nephrotic Syndrome Primary : N. S in the absence of systemic disease. Secondary : N. S in the presence of systemic disease. Congenital and infantile : N. S < 1 y , primary or secondary (infection).

Clinical manifestation 65 Periorbital edema The edema is gravity dependent Over the day, periorbital edema decreases while edema of the lower extremities increases.

Severe periorbital edema 66

67 Marked Scrotal or Vulvar Edema
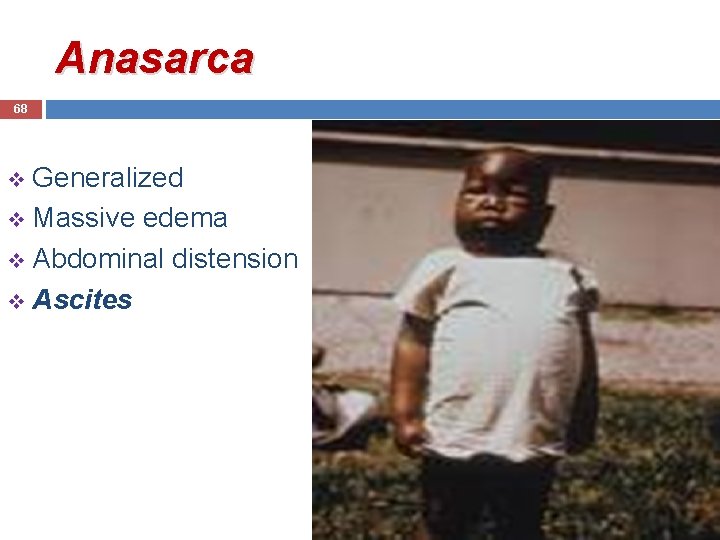
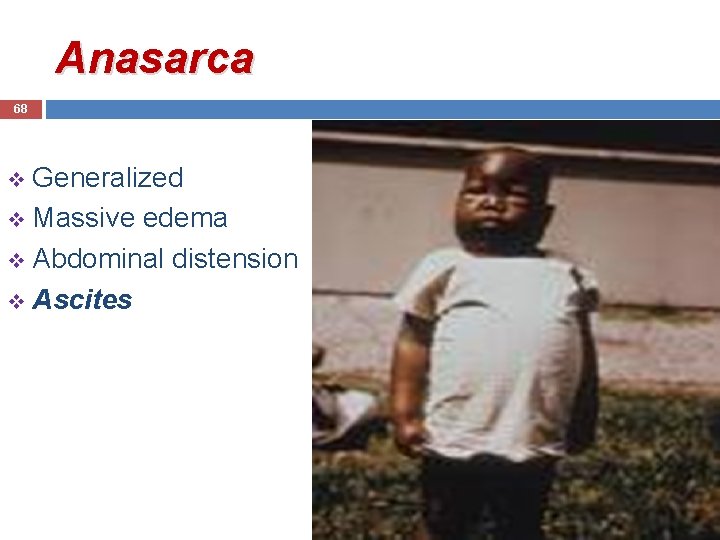
Anasarca 68 Generalized v Massive edema v Abdominal distension v Ascites v
 Site:slidetodoc.com
Site:slidetodoc.com Anemia eyes vs normal
Anemia eyes vs normal Dr vali nephrologist
Dr vali nephrologist Multiple approach-avoidance conflict
Multiple approach-avoidance conflict Tony wagner's seven survival skills
Tony wagner's seven survival skills Difference between virtual circuit and datagram networks
Difference between virtual circuit and datagram networks Bandura's reciprocal determinism
Bandura's reciprocal determinism Theoretical models of counseling
Theoretical models of counseling Research approach means
Research approach means Waterfall strategy marketing
Waterfall strategy marketing Traditional approach in system analysis and design
Traditional approach in system analysis and design Pediatric assessment triangle
Pediatric assessment triangle Isthmus area of class 2 cavity
Isthmus area of class 2 cavity Pediatric diabetes consortium
Pediatric diabetes consortium Pediatric trials network
Pediatric trials network Father of pediatric dentistry in india
Father of pediatric dentistry in india Miralax pediatric dosage chart
Miralax pediatric dosage chart Amoxicillin peds dosing chart
Amoxicillin peds dosing chart Pediatric cuff size
Pediatric cuff size Pediatric epinephrine dose chart
Pediatric epinephrine dose chart Physical environment for a sick child in paediatric ward
Physical environment for a sick child in paediatric ward Dextromethorphan dose pediatric
Dextromethorphan dose pediatric Definition of pediatric dentistry
Definition of pediatric dentistry Invocation in tagalog
Invocation in tagalog Impact of nf1pn
Impact of nf1pn Inguinal hernia in baby boys-pictures
Inguinal hernia in baby boys-pictures Jump start triage
Jump start triage Pyelonephritis child treatment
Pyelonephritis child treatment 421 rule
421 rule Pediatric bone injection gun
Pediatric bone injection gun Pediatric vision screening devices
Pediatric vision screening devices 21 audubon pediatric clinic
21 audubon pediatric clinic Co amoxiclav pediatric dose calculator
Co amoxiclav pediatric dose calculator Pediatric dysphagia resource guide
Pediatric dysphagia resource guide Chapter 57 pediatric dentistry recall
Chapter 57 pediatric dentistry recall Pediatric triangle
Pediatric triangle Rany gilpatrick
Rany gilpatrick Pediatric coma scale
Pediatric coma scale Pediatric triangle assessment
Pediatric triangle assessment Pediatric equipment list
Pediatric equipment list Deep tendon reflex
Deep tendon reflex Mt washington pediatric hospital feeding clinic
Mt washington pediatric hospital feeding clinic Pediatric trach ties
Pediatric trach ties New trends in pediatric nursing
New trends in pediatric nursing Pediatric nursing definition
Pediatric nursing definition Pediatric occupational therapy frames of reference
Pediatric occupational therapy frames of reference Pediatric seizures
Pediatric seizures Atraumatic care
Atraumatic care Pat pediatric assessment triangle
Pat pediatric assessment triangle Pediatrics shelf percentiles
Pediatrics shelf percentiles Diffusible and indiffusible suspension
Diffusible and indiffusible suspension Headache red flags
Headache red flags Bone injection gun
Bone injection gun Modern concept of health
Modern concept of health Pediatric behavior rating scale
Pediatric behavior rating scale Pico question pediatric oncology
Pico question pediatric oncology Pediatric rn
Pediatric rn Triage disaster
Triage disaster Pediatric first aid for caregivers
Pediatric first aid for caregivers Atraumatic care techniques
Atraumatic care techniques Tailwinds pediatric dentistry
Tailwinds pediatric dentistry Loading dose calculation example
Loading dose calculation example Pediatric urologist in atlanta ga
Pediatric urologist in atlanta ga Module cap
Module cap Pancrealipase
Pancrealipase Jennifer kean
Jennifer kean Epilepsy center nyu
Epilepsy center nyu Mock code checklist
Mock code checklist Father of pediatric dentistry in india
Father of pediatric dentistry in india