WHO WHAT WHY HOW Jen Adam Consultant Nephrologist


- Slides: 20
WHO? WHAT? WHY? HOW? Jen Adam, Consultant Nephrologist North Cumbria Integrated Care Trust
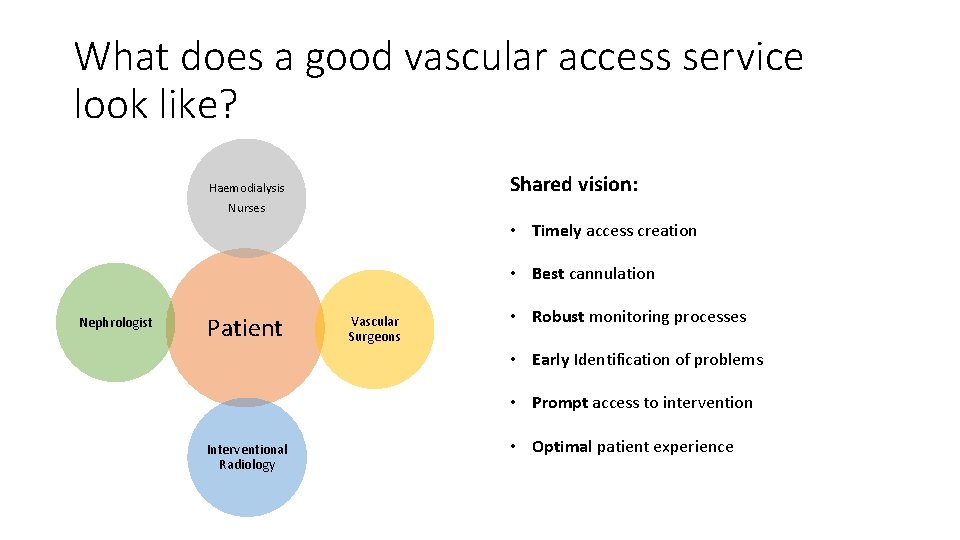
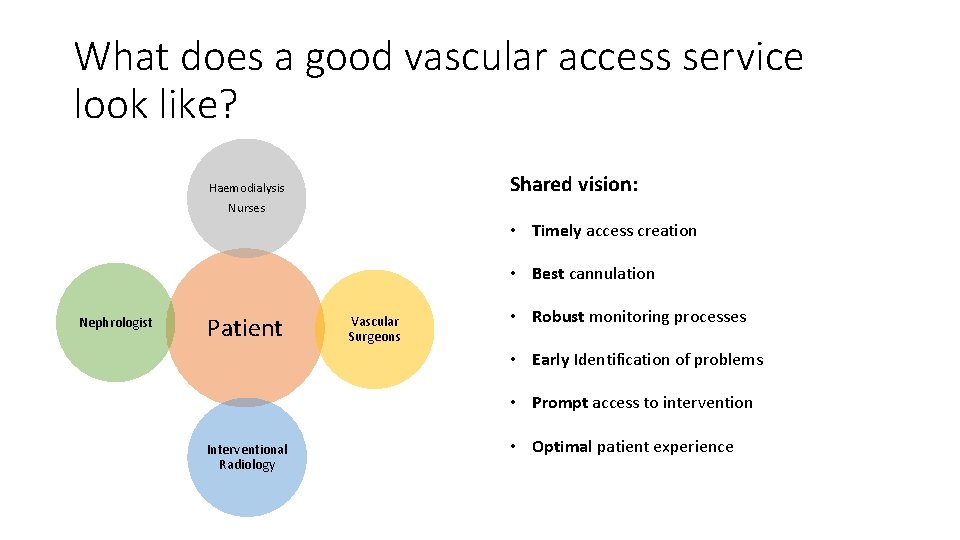
What does a good vascular access service look like? Shared vision: Haemodialysis Nurses • Timely access creation • Best cannulation Nephrologist Patient Vascular Surgeons • Robust monitoring processes • Early Identification of problems • Prompt access to intervention Interventional Radiology • Optimal patient experience
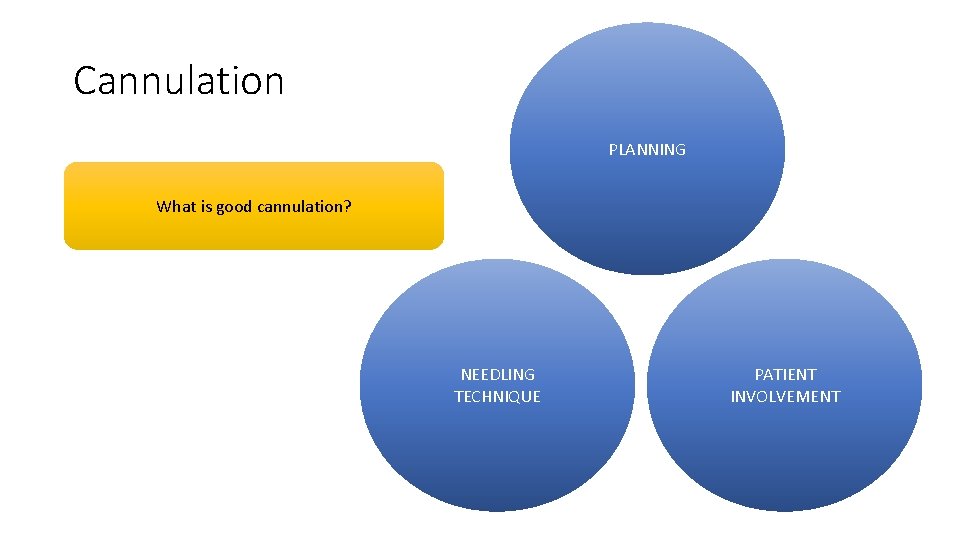
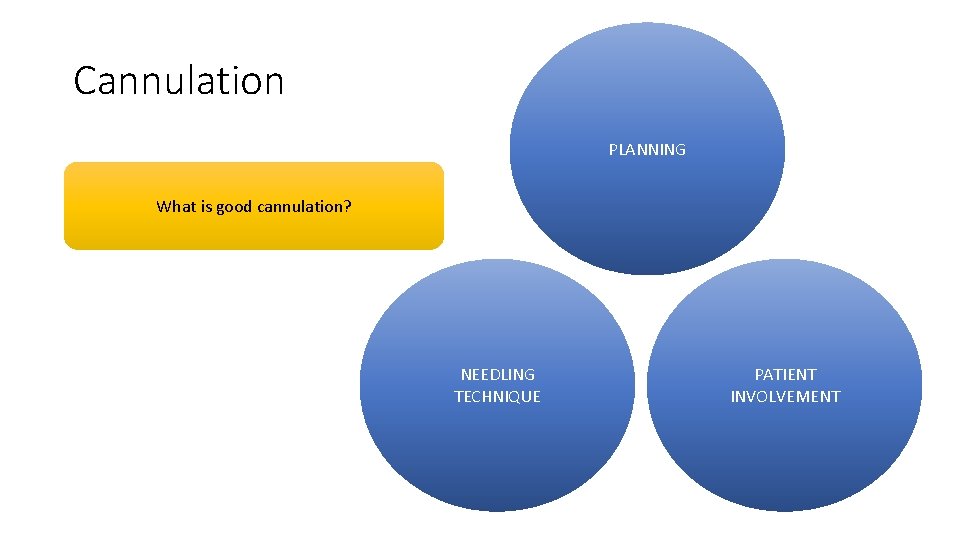
Cannulation PLANNING What is good cannulation? NEEDLING TECHNIQUE PATIENT INVOLVEMENT
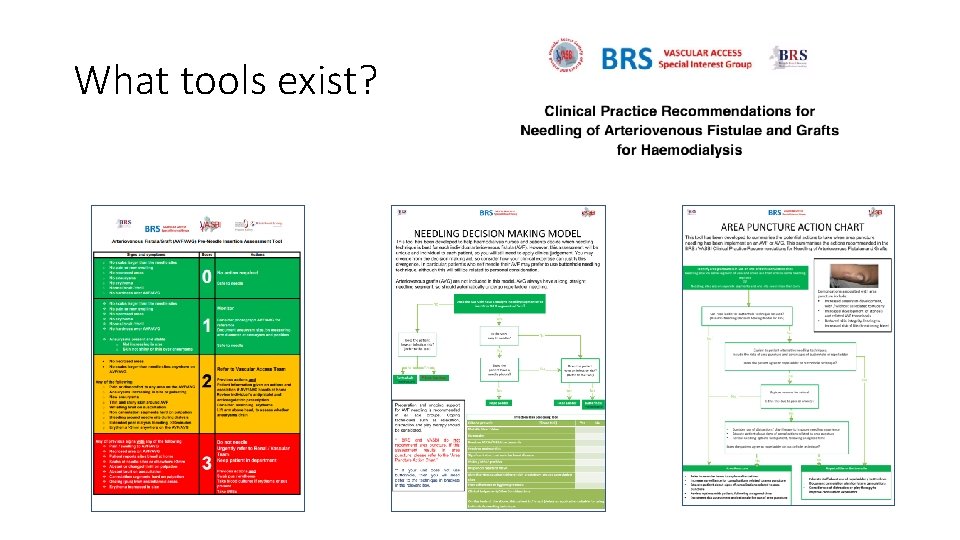
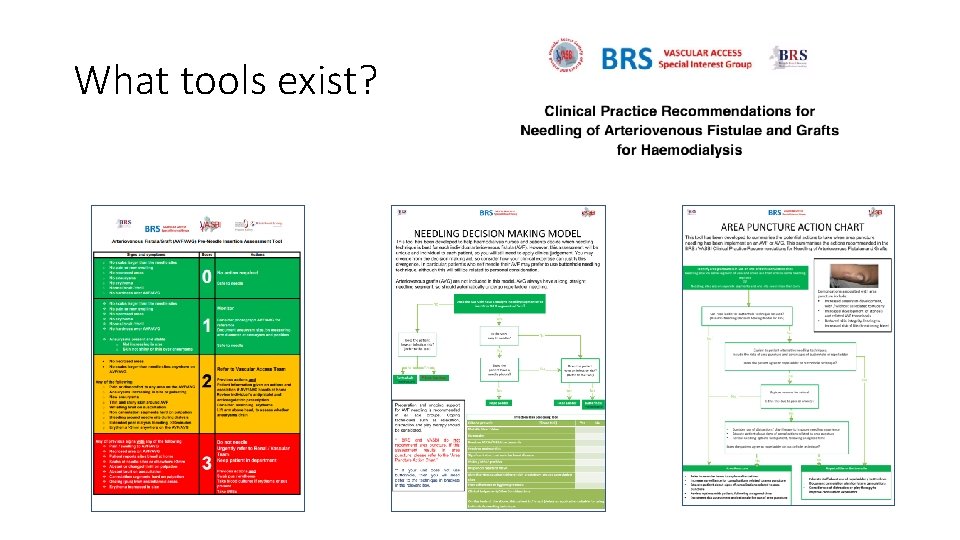
What tools exist?
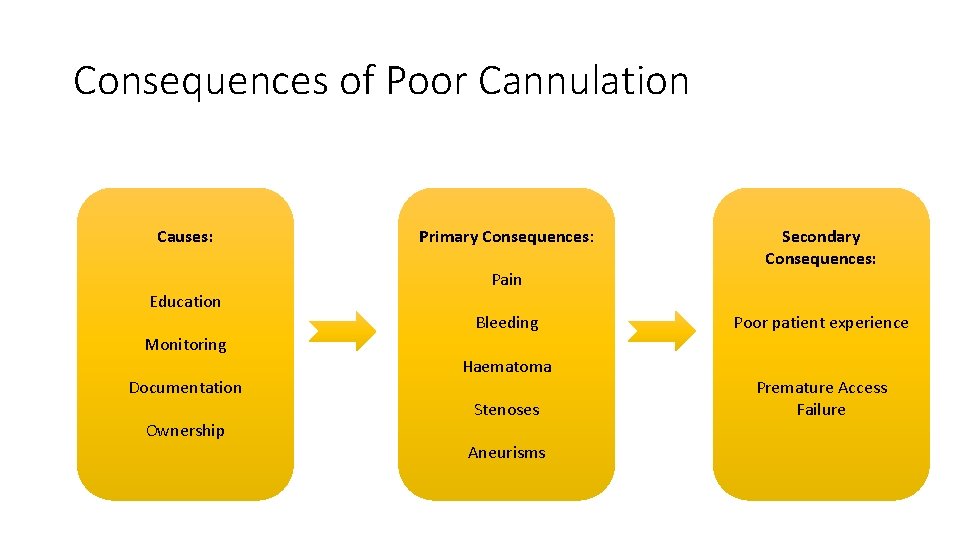
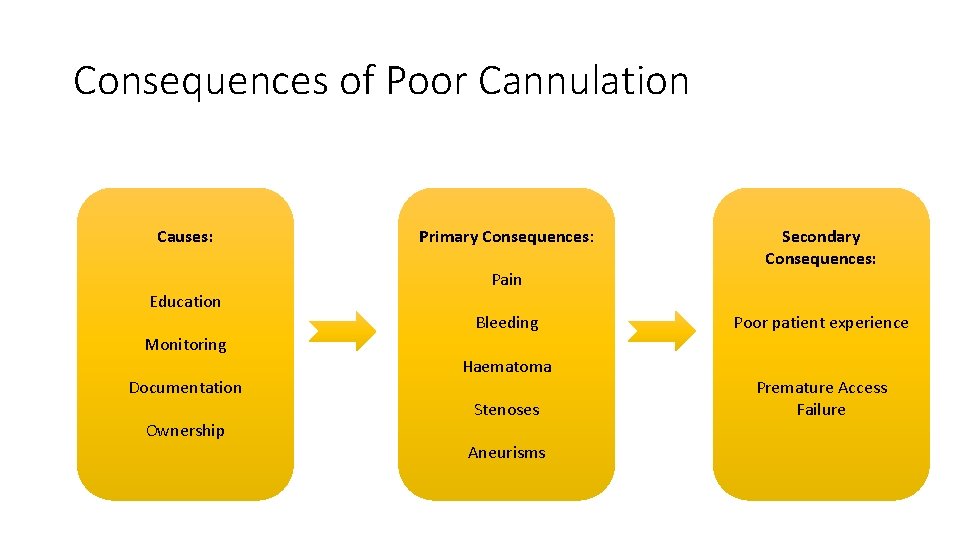
Consequences of Poor Cannulation Causes: Education Monitoring Documentation Ownership Primary Consequences: Pain Bleeding Haematoma Stenoses Aneurisms Secondary Consequences: Poor patient experience Premature Access Failure
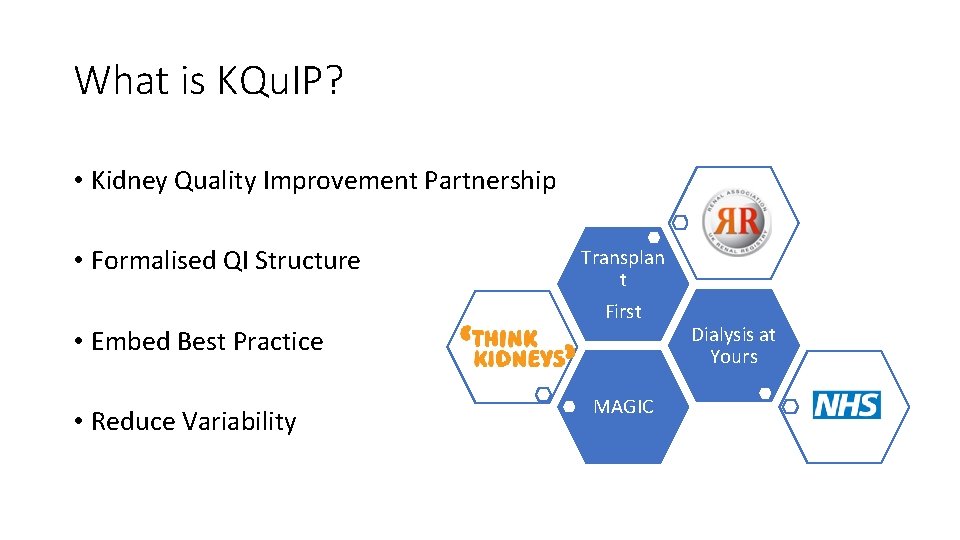
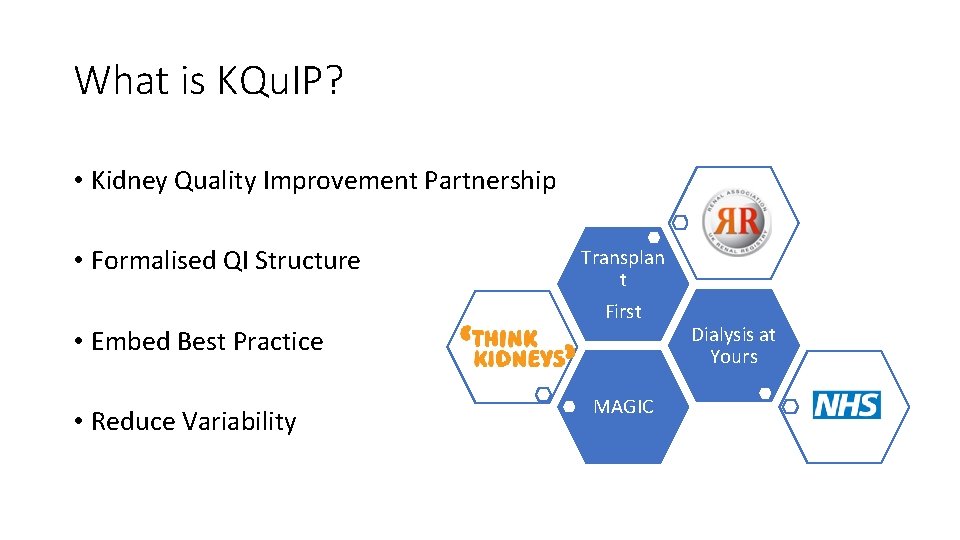
What is KQu. IP? • Kidney Quality Improvement Partnership • Formalised QI Structure • Embed Best Practice • Reduce Variability Transplan t First MAGIC Dialysis at Yours
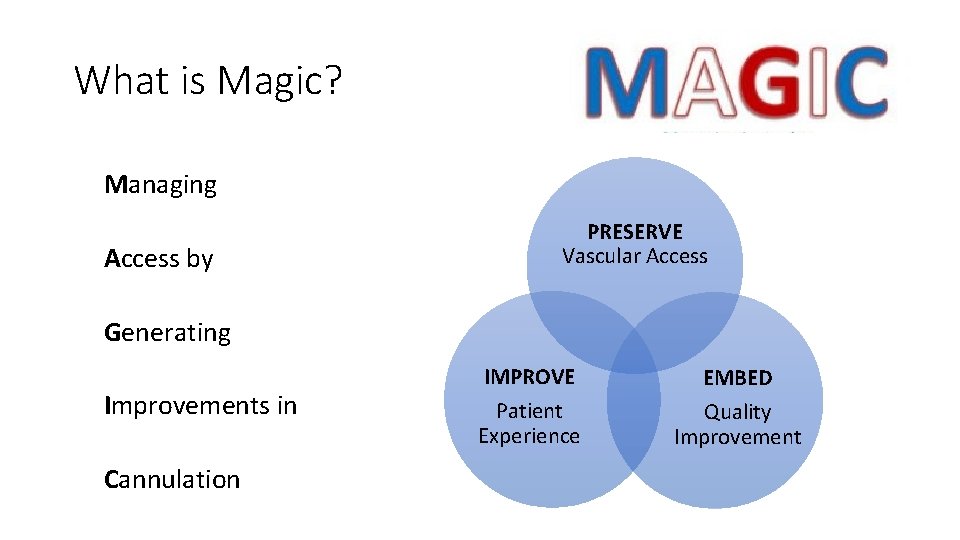
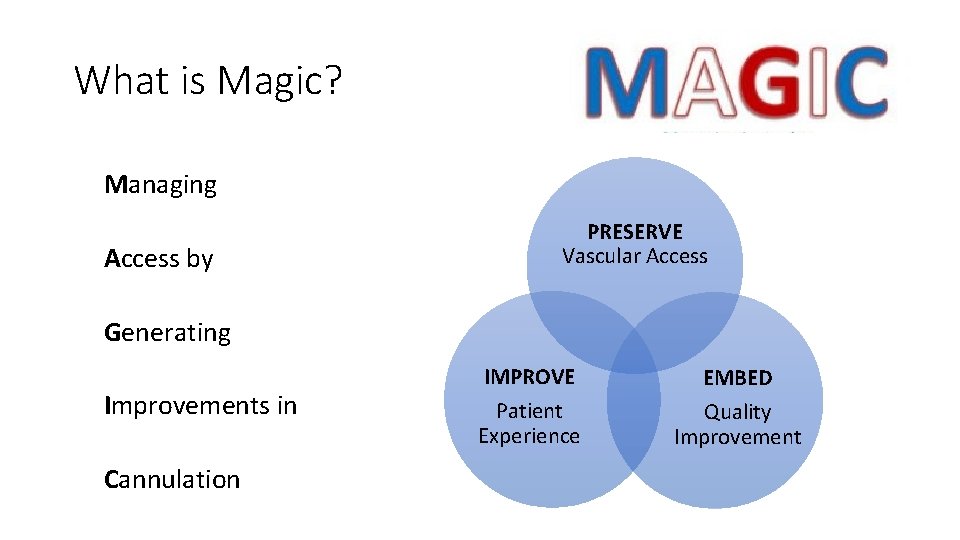
What is Magic? Managing Access by PRESERVE Vascular Access Generating Improvements in Cannulation IMPROVE Patient Experience EMBED Quality Improvement

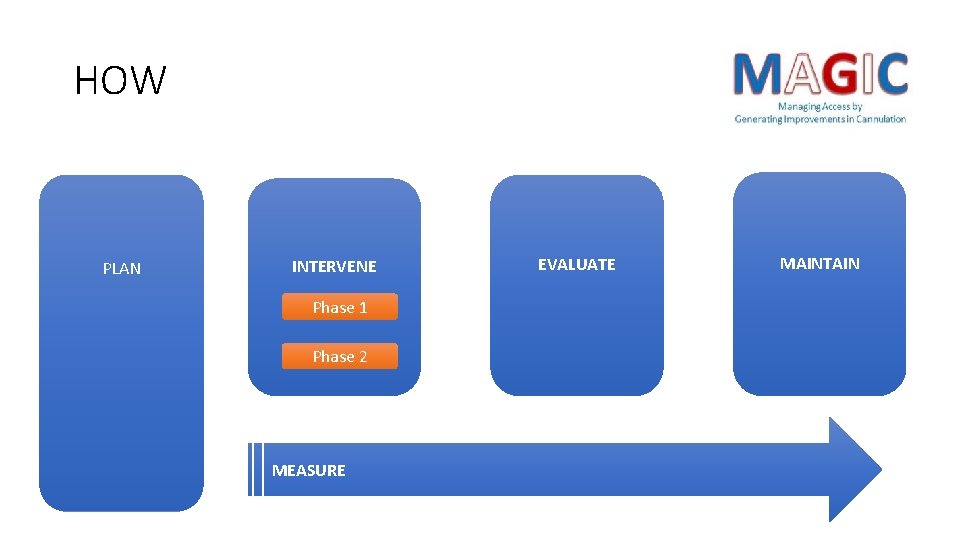
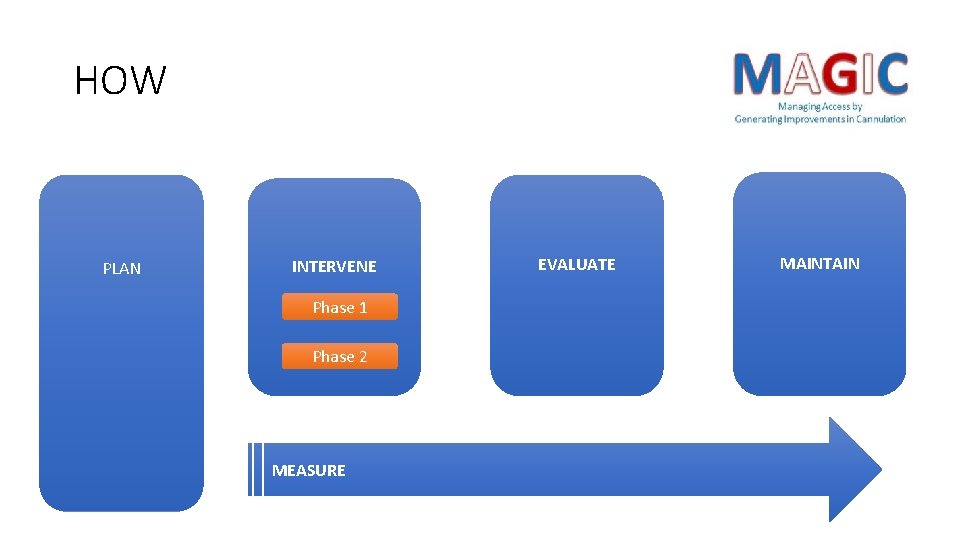
HOW PLAN INTERVENE Phase 1 Phase 2 MEASURE EVALUATE MAINTAIN
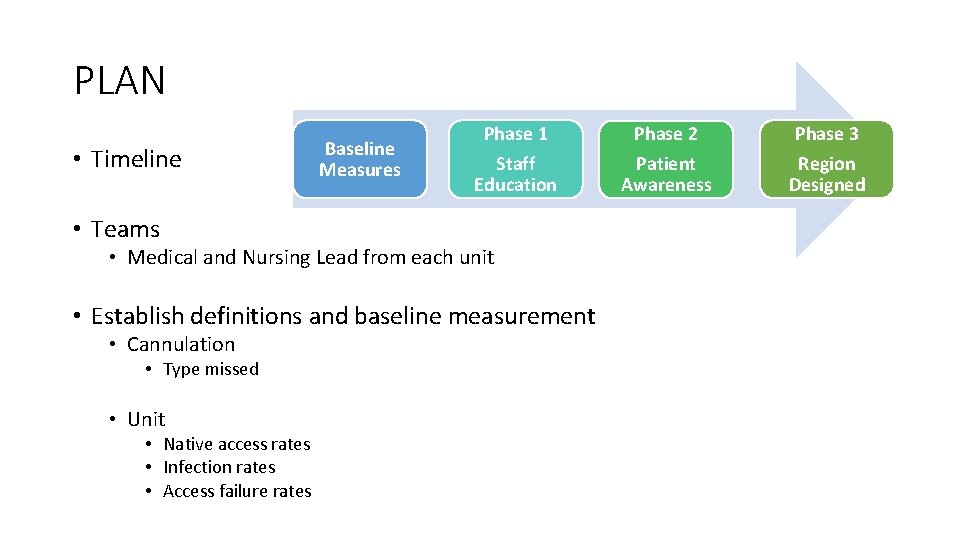
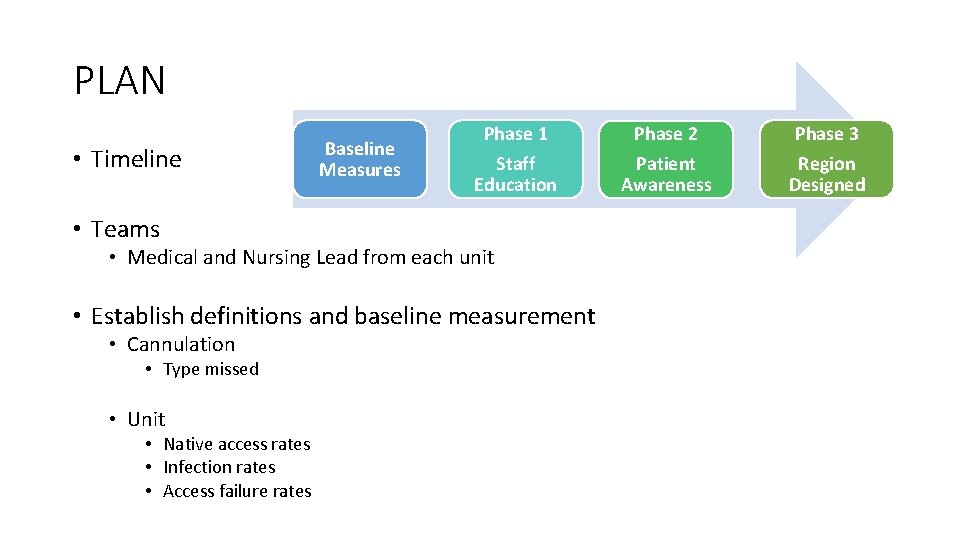
PLAN • Timeline Baseline Measures Phase 1 Phase 2 Phase 3 Staff Education Patient Awareness Region Designed • Teams • Medical and Nursing Lead from each unit • Establish definitions and baseline measurement • Cannulation • Type missed • Unit • Native access rates • Infection rates • Access failure rates
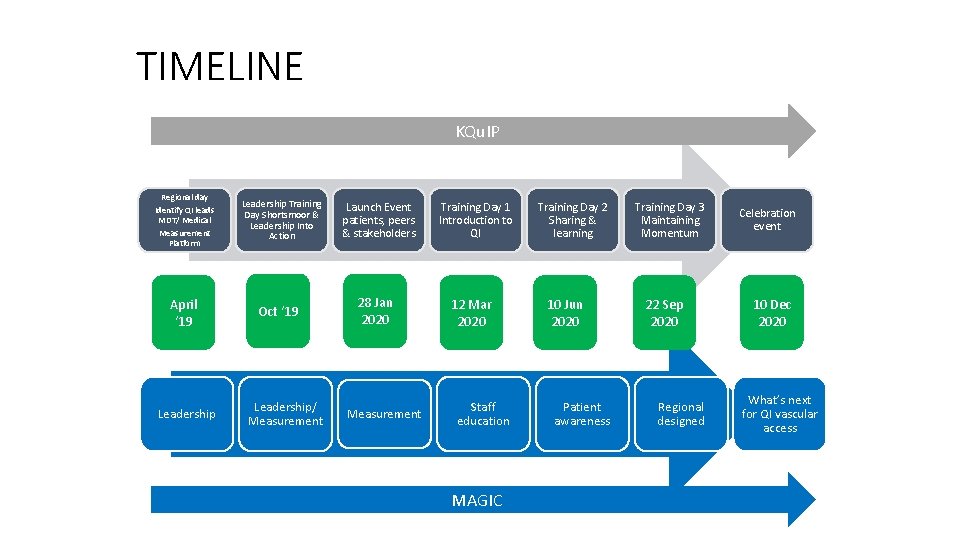
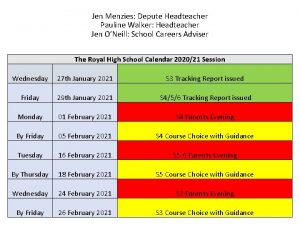
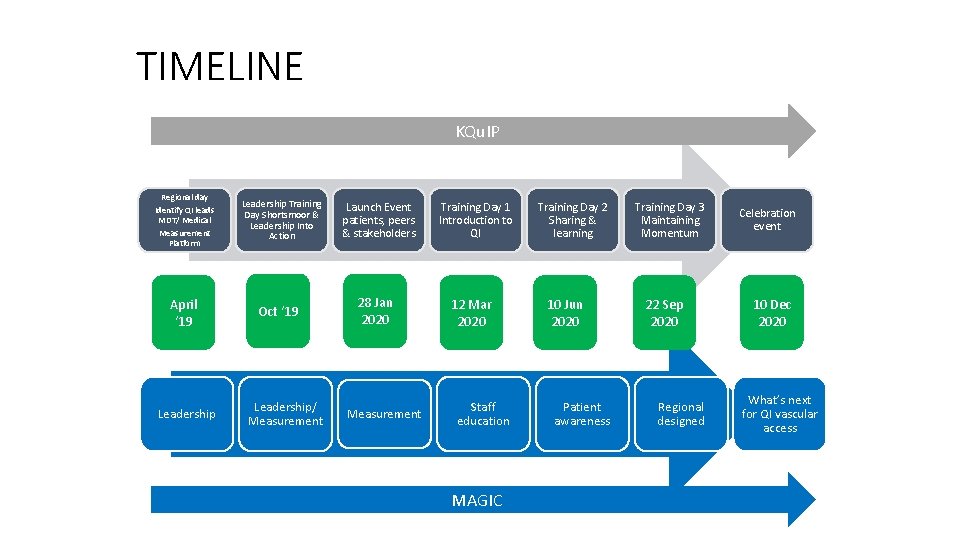
TIMELINE KQu. IP Regional day Identify QI leads MDT/ Medical Measurement Platform April ‘ 19 Leadership Training Day Shortsmoor & Leadership Into Action Oct ‘ 19 Leadership/ Measurement Launch Event patients, peers & stakeholders 28 Jan 2020 Measurement Training Day 1 Introduction to QI 12 Mar 2020 Staff education MAGIC Training Day 2 Sharing & learning 10 Jun 2020 Patient awareness Training Day 3 Maintaining Momentum 22 Sep 2020 Regional designed Celebration event 10 Dec 2020 What’s next for QI vascular access
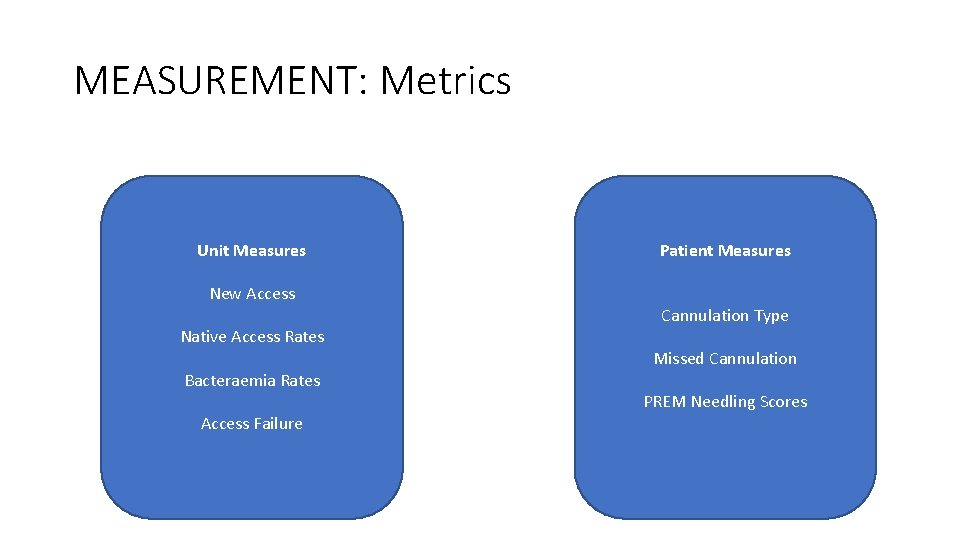
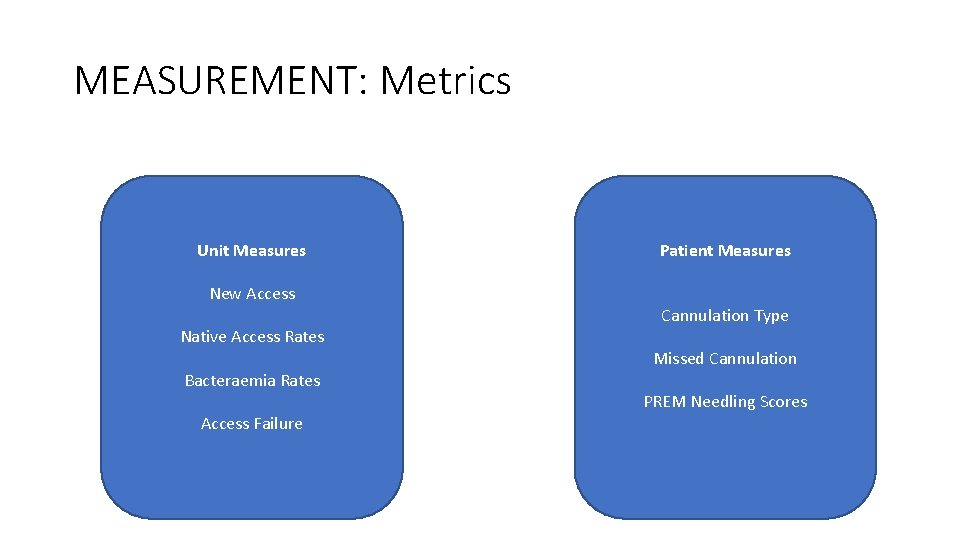
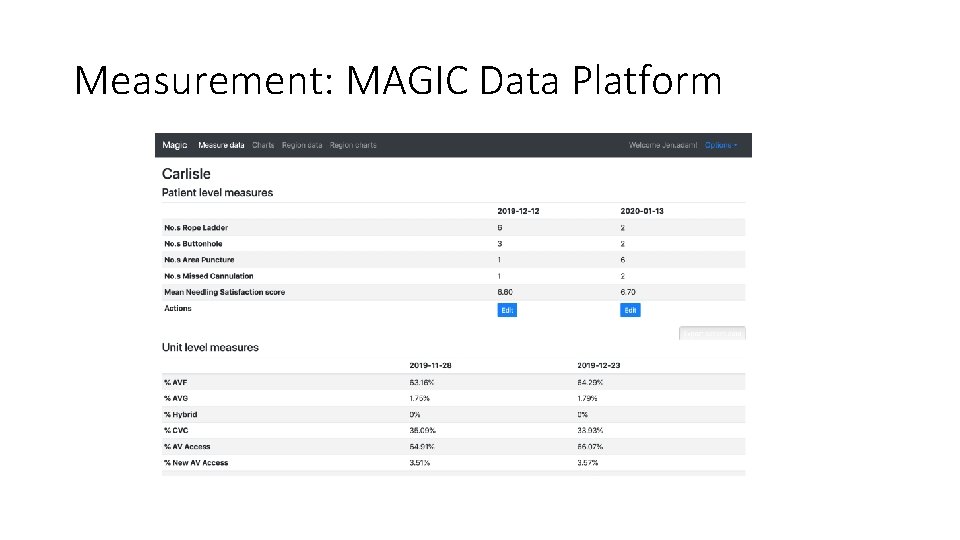
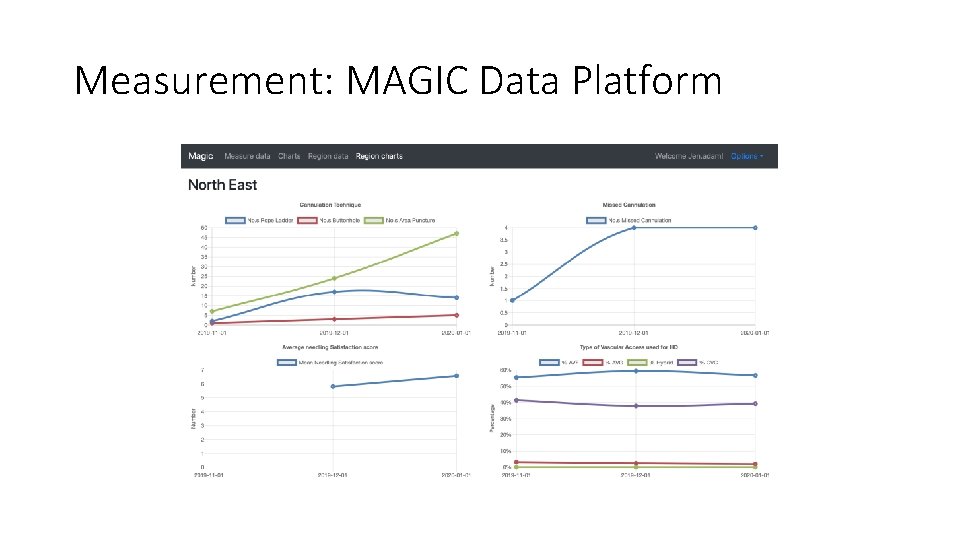
MEASUREMENT: Metrics Unit Measures New Access Native Access Rates Bacteraemia Rates Access Failure Patient Measures Cannulation Type Missed Cannulation PREM Needling Scores
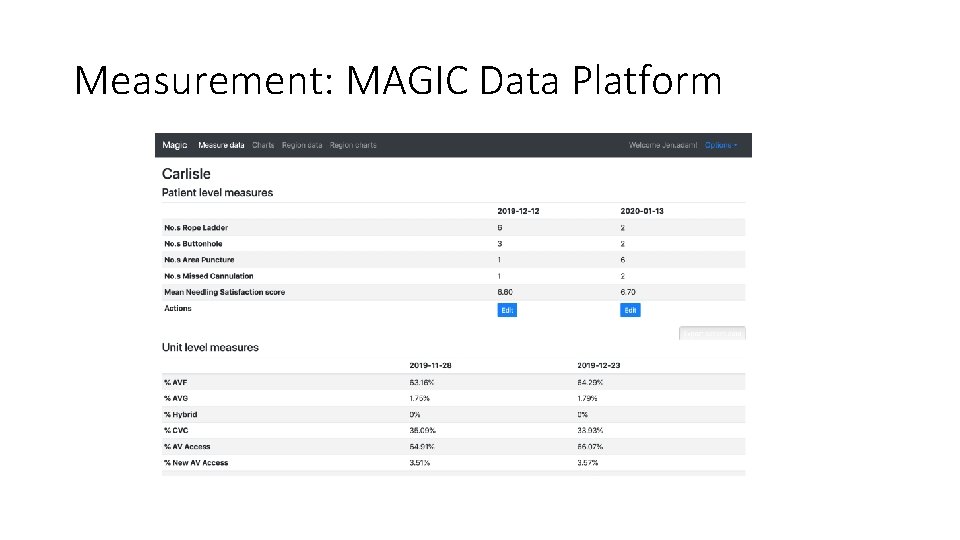
Measurement: MAGIC Data Platform
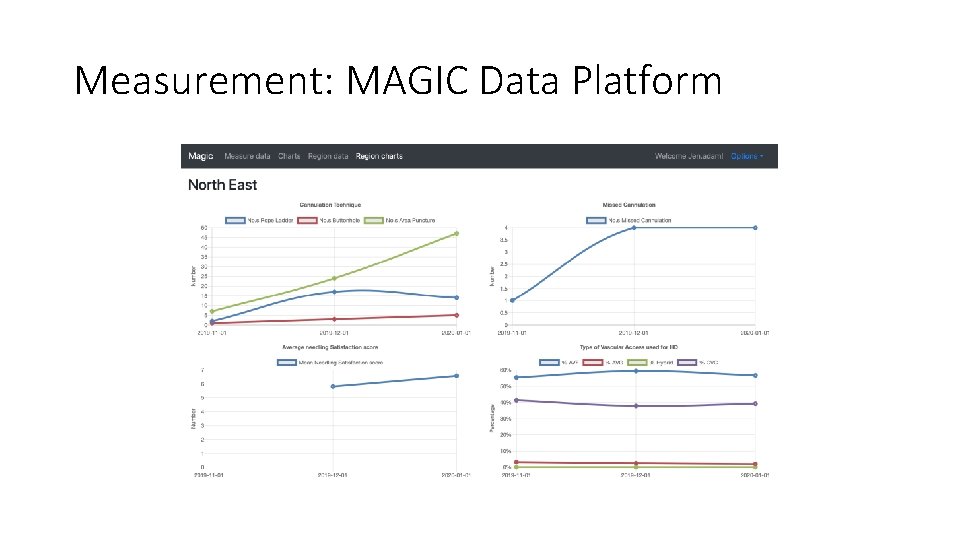
Measurement: MAGIC Data Platform
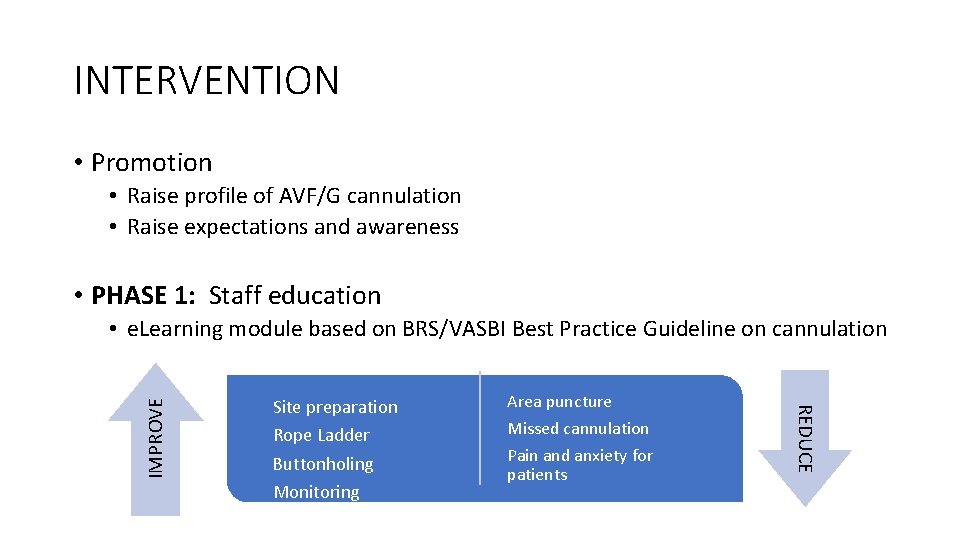
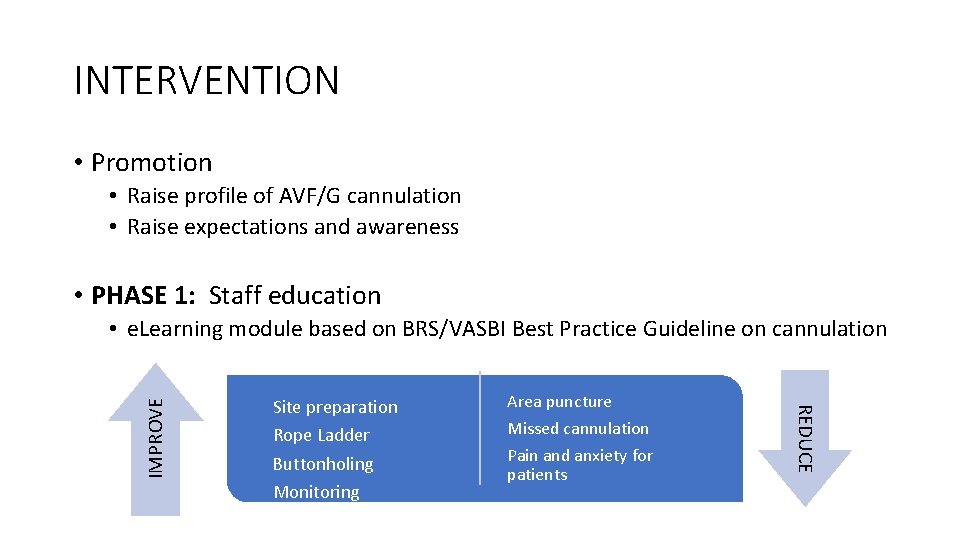
INTERVENTION • Promotion • Raise profile of AVF/G cannulation • Raise expectations and awareness • PHASE 1: Staff education Site preparation Rope Ladder Buttonholing Monitoring Area puncture Missed cannulation Pain and anxiety for patients REDUCE IMPROVE • e. Learning module based on BRS/VASBI Best Practice Guideline on cannulation
INTERVENTION • PHASE 2: Patient Education and empowerment • Encourage dialogue between patient and cannulating staff • Improve knowledge and understanding through visual cues
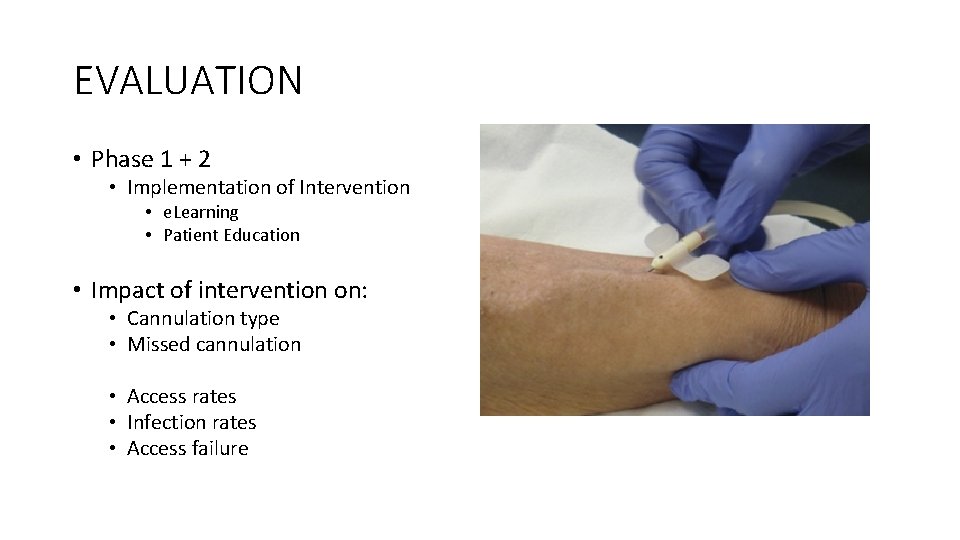
EVALUATION • Phase 1 + 2 • Implementation of Intervention • e. Learning • Patient Education • Impact of intervention on: • Cannulation type • Missed cannulation • Access rates • Infection rates • Access failure
MAINTENANCE…… TBC! • Embed good practice • Maintain awareness, knowledge, technique • Educate and assess new staff • Ongoing engagement of patients with cannulation • Future planning….

Making Best Practice Usual Practice
QUESTIONS?
 Dr vali nephrologist
Dr vali nephrologist Anemia eyes vs normal
Anemia eyes vs normal Hey hey bye bye
Hey hey bye bye Adam adam facebook
Adam adam facebook Zvony zvoní jen chvíli
Zvony zvoní jen chvíli Správně vidíme jen srdcem
Správně vidíme jen srdcem Jen andre
Jen andre Background of jean piaget
Background of jean piaget Cax protocol
Cax protocol Jen gorgas
Jen gorgas Catholic university
Catholic university Jen smyers orr
Jen smyers orr Confucianism jen
Confucianism jen Jen southern
Jen southern Jean val jen
Jean val jen Jonathan farthing
Jonathan farthing Jen mc
Jen mc Don't ask why why why
Don't ask why why why Modern data architecture consulting
Modern data architecture consulting Consultant mediu
Consultant mediu Claudia norman a marketing consultant
Claudia norman a marketing consultant