THE PUERPERIUM PUERPERAL INFECTIONS Seluk ZDEN MD Prof

- Slides: 59
THE PUERPERIUM & PUERPERAL INFECTIONS Selçuk ÖZDEN MD, Prof
DEFINITION § Puerperium defines the time following delivery during which pregnancy-induced maternal anatomical and physiological changes return to the nonpregnant state. § It’s duration is understandably inexact, but is considered to be between 4 and 6 weeks.
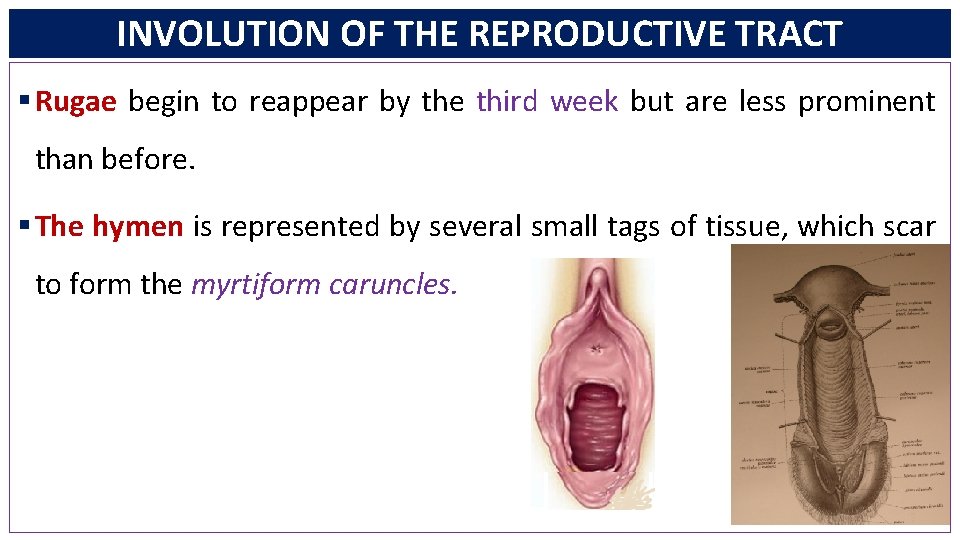
INVOLUTION OF THE REPRODUCTIVE TRACT § Rugae begin to reappear by the third week but are less prominent than before. § The hymen is represented by several small tags of tissue, which scar to form the myrtiform caruncles.
INVOLUTION OF THE REPRODUCTIVE TRACT § Vaginal epithelium begins to proliferate by 4 to 6 weeks, usually coincidental with resumed ovarian estrogen production. § Puerperal uterus: larger blood vessels become obliterated by hyaline changes, are gradually resorbed, and are replaced by smaller ones.
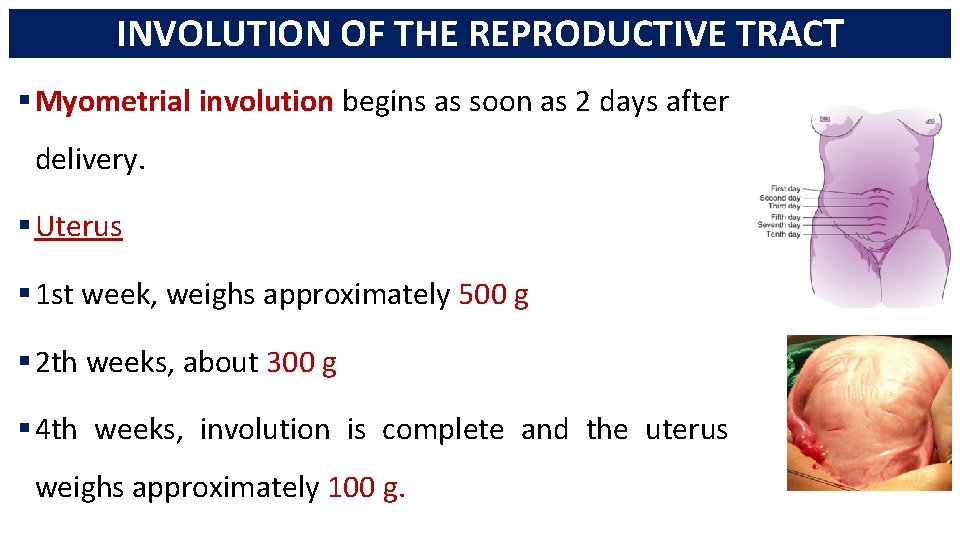
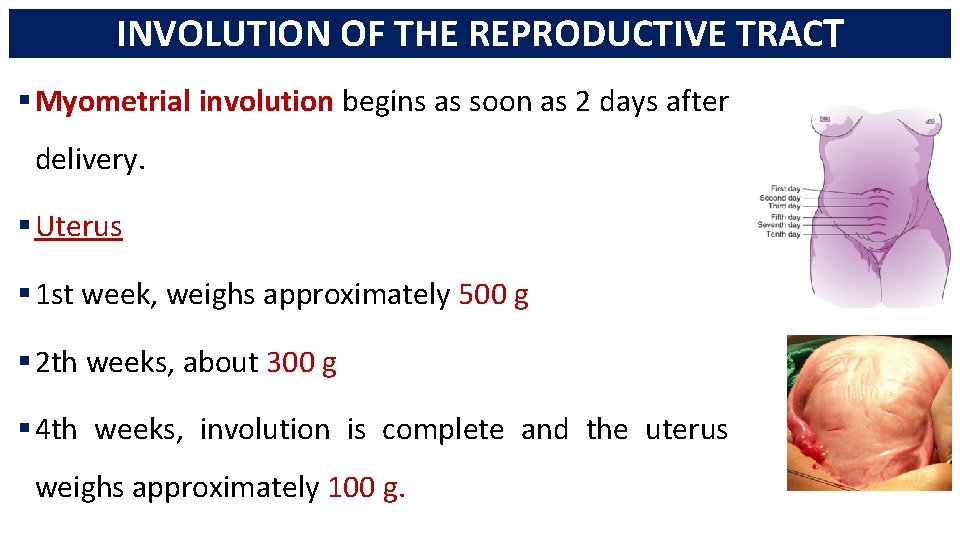
INVOLUTION OF THE REPRODUCTIVE TRACT § Myometrial involution begins as soon as 2 days after delivery. § Uterus § 1 st week, weighs approximately 500 g § 2 th weeks, about 300 g § 4 th weeks, involution is complete and the uterus weighs approximately 100 g.
INVOLUTION OF THE REPRODUCTIVE TRACT
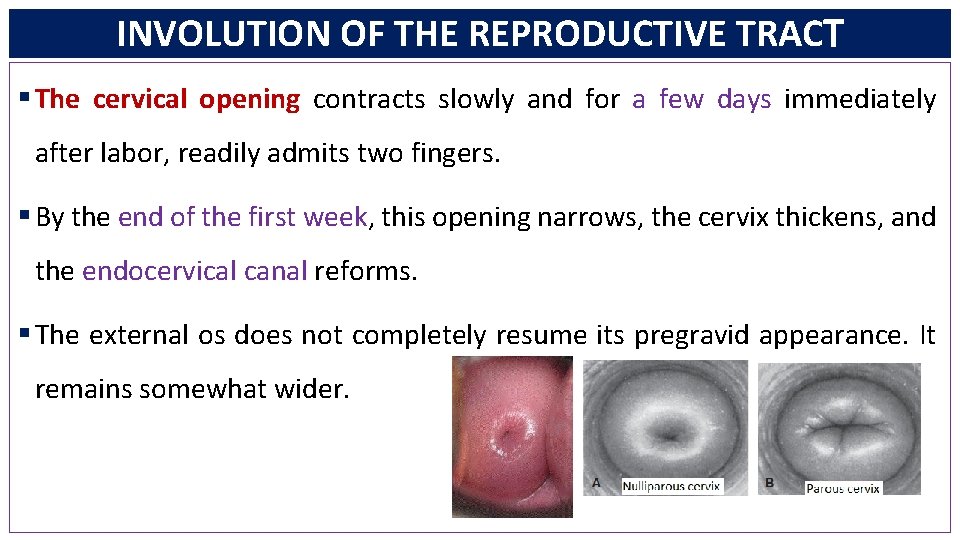
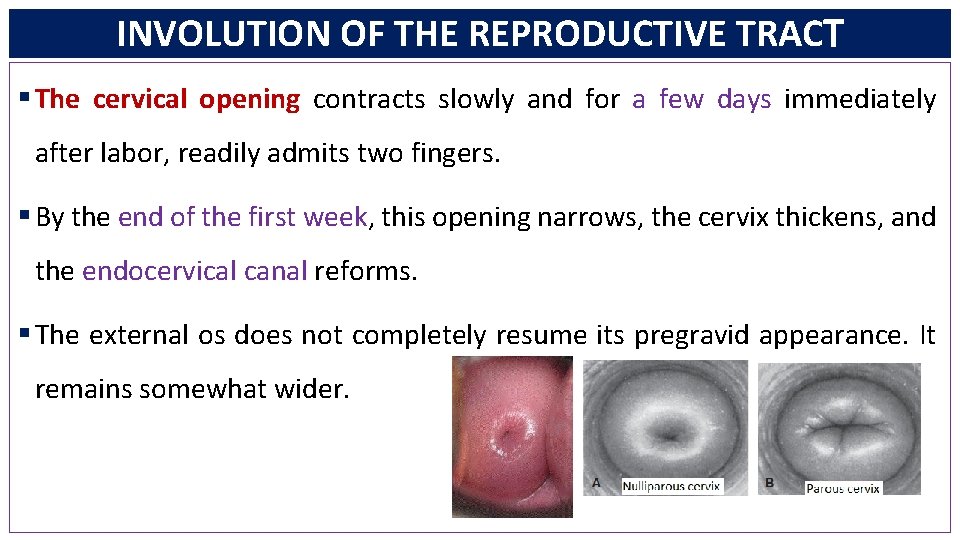
INVOLUTION OF THE REPRODUCTIVE TRACT § The cervical opening contracts slowly and for a few days immediately after labor, readily admits two fingers. § By the end of the first week, this opening narrows, the cervix thickens, and the endocervical canal reforms. § The external os does not completely resume its pregravid appearance. It remains somewhat wider.
INVOLUTION OF THE REPRODUCTIVE TRACT § Within 2 or 3 days after delivery, the remaining decidua becomes differentiated into two layers. § The superficial layer becomes necrotic and is sloughed in the lochia. § The basal layer remains intact and is the source of new endometrium. § Endometrial regeneration is rapid, except at the placental site.
AFTERPAINS § In primiparous women, the uterus tends to remain tonically contracted following delivery. § In multiparas, however, it often contracts vigorously at intervals and gives rise to afterpains, which are similar to but milder than labor contractions.
LOCHIA § Early in the puerperium, sloughing of decidual tissue results in a vaginal discharge of variable quantity. § The discharge is termed lochia and contains erythrocytes, shredded decidua, epithelial cells, and bacteria.
LOCHIA § Lochia rubra: first few days after delivery, there is blood sufficient to color it red. § Lochia serosa: After 3 or 4 days, lochia becomes progressively pale in color. § Lochia alba: After approximately the 10 th day, because of an admixture of leukocytes and reduced fluid content
SUBINVOLUTION § In some cases, uterine involution is hindered because of infection, retained placental fragments, or other causes. § Such subinvolution is accompanied by varied intervals of prolonged lochia as well as irregular or excessive uterine bleeding. § Ergonovine (Ergotrate) or methylergonovine (Methergine), 0. 2 mg orally every 3 to 4 hours for 24 to 48 hours, is recommended for treatment.
LATE POSTPARTUM HEMORRHAGE § Defines bleeding 24 hours to 12 weeks after delivery. § 1% of the women § Management § If sonographic examination shows an empty cavity, then uterotonics (oxytocin, methylergonovine, or a prostaglandin analogue) is given. § Antimicrobials are added if uterine infection is suspected. § Curettage is carried out only if appreciable bleeding persists or recurs after medical management.
URINARY TRACT § Normal pregnancy-induced glomerular hyperfiltration persists on the first postpartum day but returns to prepregnancy baseline by 2 weeks. § Bladder trauma is associated most closely with labor length and thus to some degree is a normal accompaniment of vaginal delivery.
BREASTS and LACTATION § Endocrinology of Lactation § The precise humoral and neural mechanisms involved in lactation are complex. § Progesterone, estrogen, and placental lactogen, as well as prolactin, cortisol, and insulin, appear to act in concert to stimulate the growth and development of the milk-secreting apparatus.
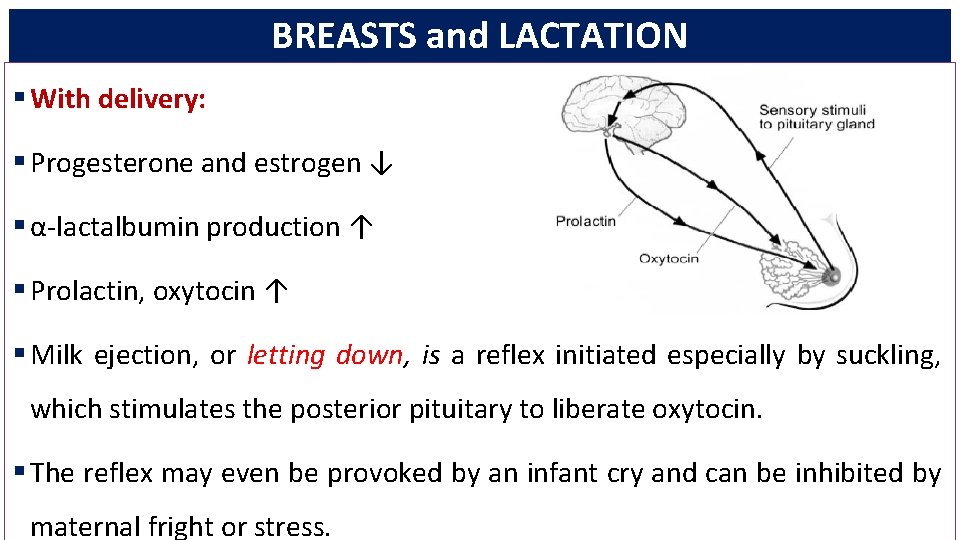
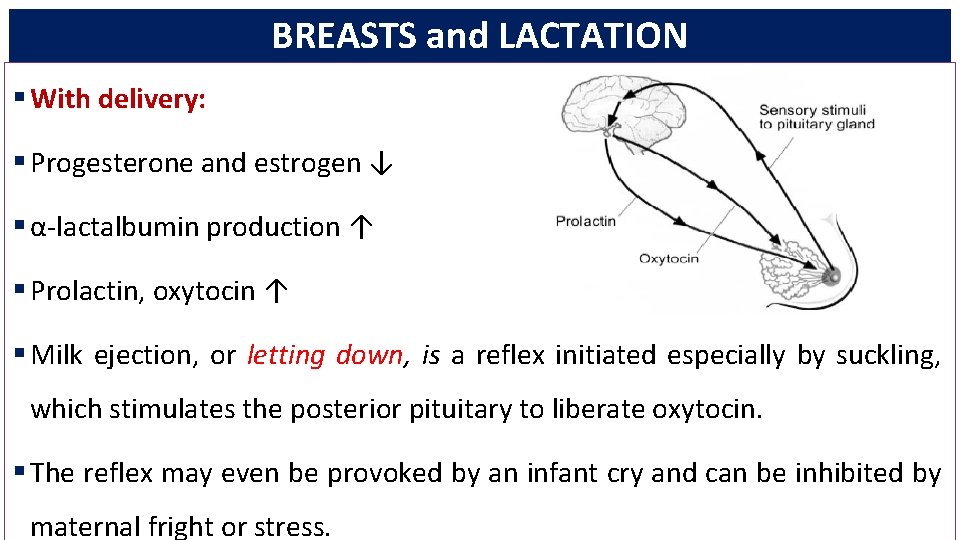
BREASTS and LACTATION § With delivery: § Progesterone and estrogen ↓ § α-lactalbumin production ↑ § Prolactin, oxytocin ↑ § Milk ejection, or letting down, is a reflex initiated especially by suckling, which stimulates the posterior pituitary to liberate oxytocin. § The reflex may even be provoked by an infant cry and can be inhibited by maternal fright or stress.
BREASTS and LACTATION § Human milk contains several protective immunological substances, including secretory Ig. A and growth factors. § The antibodies in human milk are specifically directed against maternal environmental antigens such as against Escherichia coli.

ADVANTAGES of BREAST FEEDING ACOG-2012
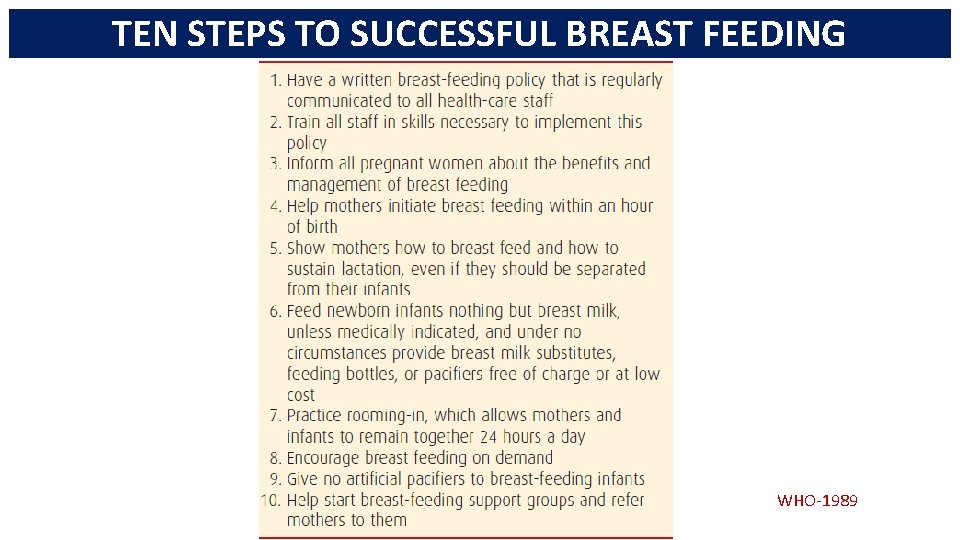
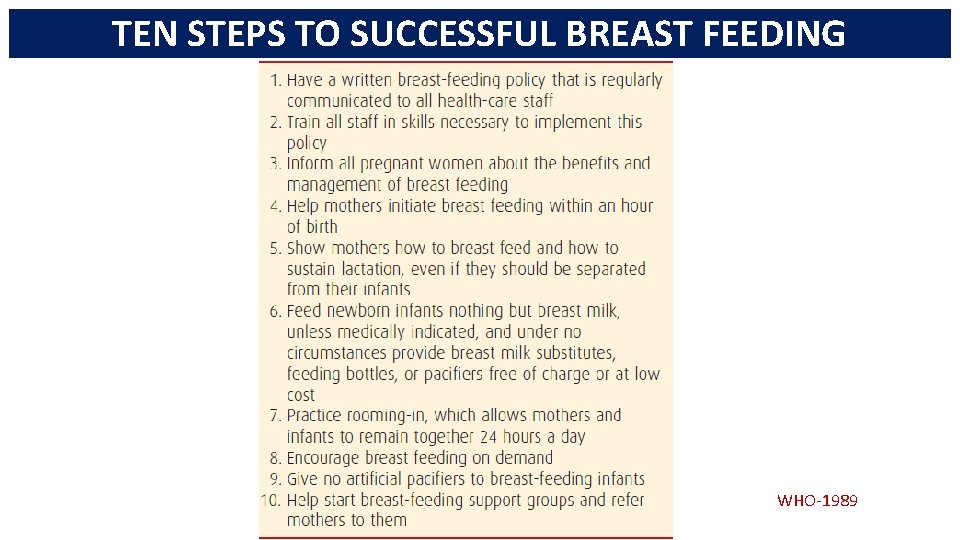
TEN STEPS TO SUCCESSFUL BREAST FEEDING WHO-1989
CONTRAINDICATIONS TO BREAST FEEDING § Nursing is contraindicated in women who § take street drugs or do not control their alcohol use; § have an infant with galactosemia; § have human immunodeficiency virus (HIV) infection; § have active, untreated tuberculosis § take certain medications; § or are undergoing breast cancer treatment.
BREAST ENGORGEMENT § This is common in women who do not breast feed and is typified by milk leakage and breast pain. These peak 3 to 5 days after delivery. § Up to half of affected women require analgesia for breast-pain. § Breasts can be supported with a well-fitting brassiere, breast binder, or “sports bra. ” § Cool packs and oral analgesics for 12 to 24 hours aid discomfort. § Pharmacological or hormonal agents are not recommended to suppress lactation.
BREAST ENGORGEMENT § Fever caused by breast engorgement was common before the renaissance of breast feeding. § Mastitis is infection of the mammary parenchyma. It is relatively common in lactating women.
MEDICAL CARE DURING PUERPERIUM § Hospital Care § For 2 hours after delivery, blood pressure and pulse should be taken every 15 minutes, or more frequently if indicated. § Temperature is assessed every 4 hours for the first 8 hours and then at least every 8 hours subsequently. § The amount of vaginal bleeding is monitored, and the fundus palpated to ensure that it is well contracted.
MEDICAL CARE DURING PUERPERIUM § Early Ambulation: § Advantages of early ambulation include fewer bladder complications, less frequent constipation, and reduced rates of puerperal venous thromboembolism. § Almost half of thromboembolic events associated with pregnancy develop in the puerperium. § Pulmonary embolism is most common in the first 6 weeks postpartum.
MEDICAL CARE DURING PUERPERIUM § Immunizations § The D-negative woman who is not isoimmunized and whose infant is D-positive is given 300 μg of anti-D immune globulin shortly after delivery. § Women who are not already immune to rubella or rubeola measles are excellent candidates for combined measles-mumps-rubella vaccination (MMR) before discharge.
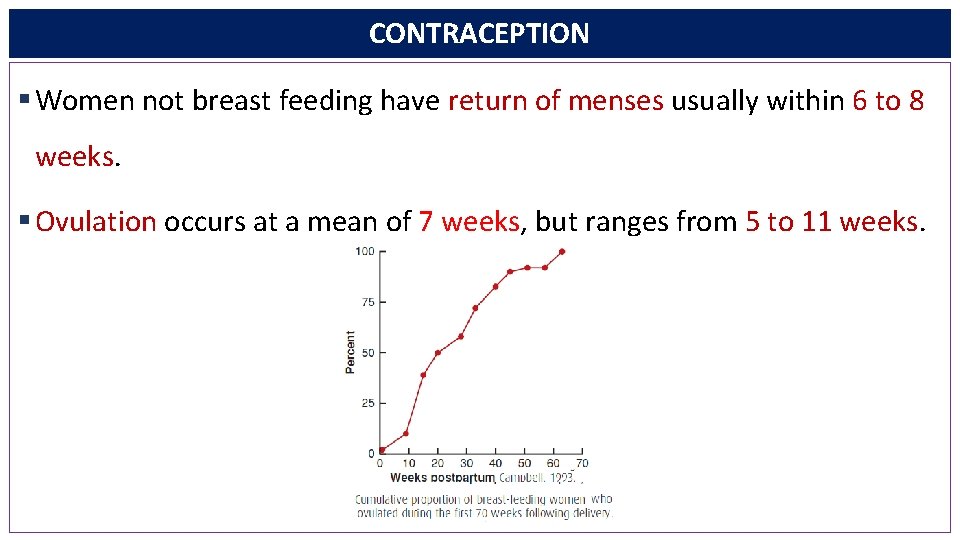
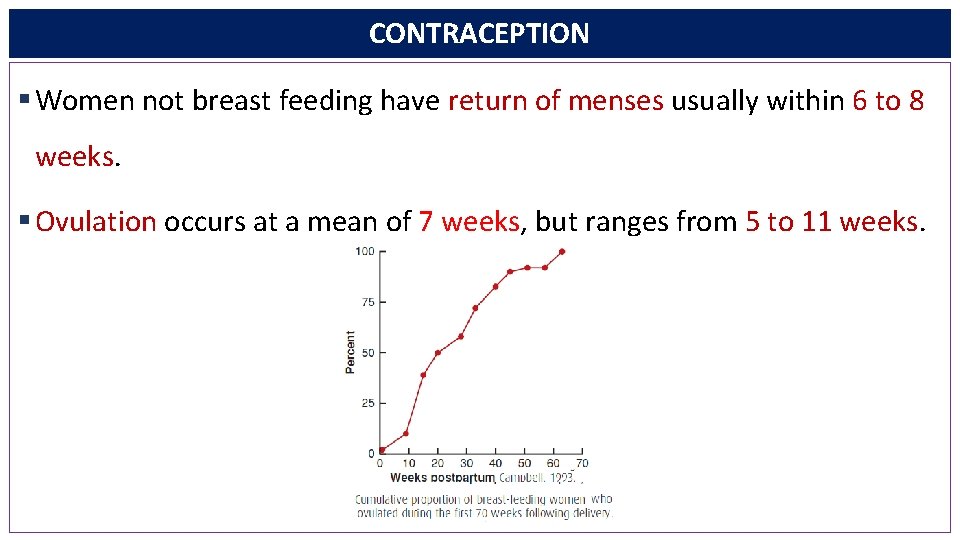
CONTRACEPTION § Women not breast feeding have return of menses usually within 6 to 8 weeks. § Ovulation occurs at a mean of 7 weeks, but ranges from 5 to 11 weeks.
CONTRACEPTION • Do not forget !!! 1. Resumption of ovulation was frequently marked by return of normal menstrual bleeding. 2. Breast-feeding episodes lasting 15 minutes seven times daily delayed ovulation resumption. 3. Ovulation can occur without bleeding. 4. Bleeding can be anovulatory. 5. The risk of pregnancy in breast-feeding women was approximately 4% per year
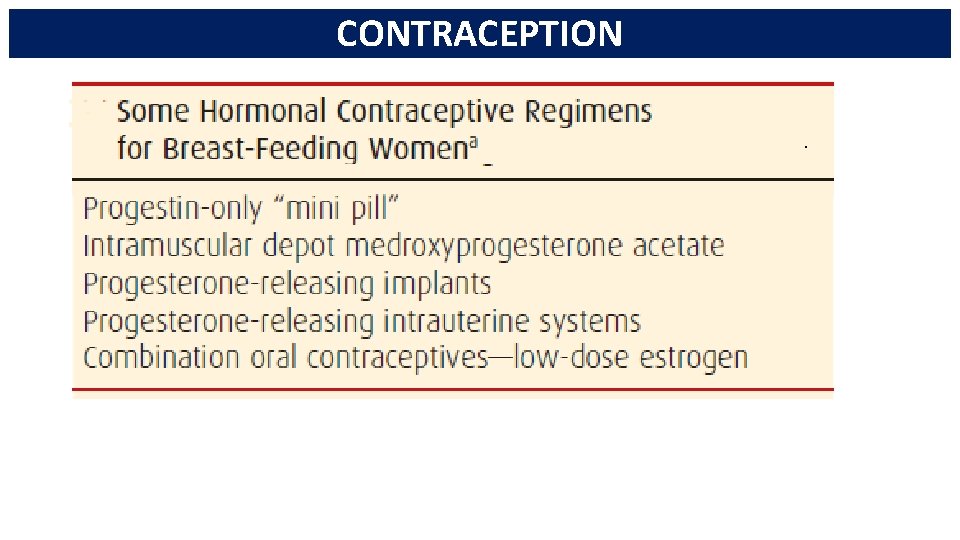
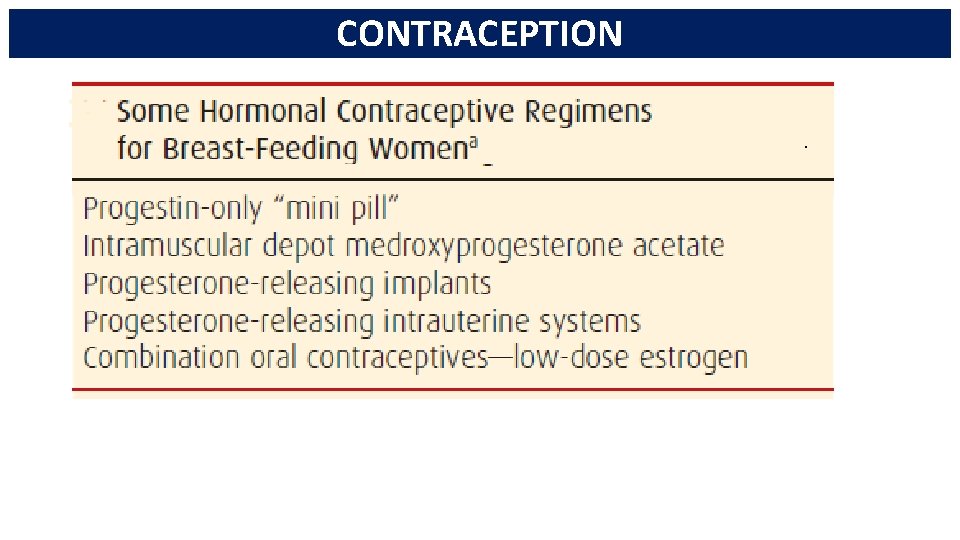
CONTRACEPTION
PUERPERAL INFECTIONS § Puerperal Infection describes any bacterial infection of the genital tract after delivery. § These infections as well as preeclampsia and obstetrical hemorrhage form the lethal triad of maternal death causes before and during the 20 th century. § Infection caused 10. 7% of pregnancy-related deaths and was the fifth leading cause.
PUERPERAL FEVER § A number of factors can cause fever—a temperature of 38. 0°C or higher—in the puerperium. § Most persistent fevers after childbirth are caused by genital tract infection.
PUERPERAL FEVER § 20% of women febrile within the first 24 hours after giving birth vaginally were subsequently diagnosed with pelvic infection. § Spiking fevers of 39°C or higher that develop within the first 24 hours postpartum may be associated with virulent pelvic infection caused by group A streptococcus.
PUERPERAL FEVER § Other causes of puerperal fever: § Breast engorgement § Urinary infections § Episiotomy and abdominal incisions § Perineal lacerations § Respiratory complications after cesarean delivery § Approximately 15% of women who do not breast feed develop postpartum fever from breast engorgement.
PUERPERAL FEVER § Other causes of puerperal fever: § “Breast fever” rarely exceeds 39°C in the first few postpartum days and usually lasts < 24 hours. § Urinary infections are uncommon § Atelectasis following abdominal delivery is caused by hypoventilation and is best prevented by coughing and deep breathing on a fixed schedule following surgery.
UTERINE INFECTION § Postpartum uterine infection or puerperal sepsis has been called variously endometritis, endomyometritis, and endoparametritis. § Because infection involves not only the decidua but also the myometrium and parametrial tissues, we prefer the inclusive term metritis with pelvic cellulitis.
UTERINE INFECTION § The route of delivery is the single most significant risk factor for the development of uterine infection. § A nearly 25 -fold increased infection-related mortality rate with cesarean versus vaginal delivery.
UTERINE INFECTION § Vaginal Delivery § 1 to 2% incidence of metritis. § Women at high risk for infection because of membrane rupture, prolonged labor, and multiple cervical examinations have a 5 to 6% frequency of metritis after vaginal delivery. § Manual removal of the placenta increased the puerperal metritis rate threefold.
UTERINE INFECTION § Cesarean Delivery § Single-dose perioperative antimicrobial prophylaxis is recommended for all women undergoing cesarean delivery. § Important risk factors § Prolonged labor, § Membrane rupture, § Multiple cervical examinations, § Internal fetal monitoring.
UTERINE INFECTION § Other Risk Factors § Bacterial colonization of the lower genital tract with certain microorganisms—for example, group B streptococcus, Chlamydia trachomatis, Mycoplasma hominis, Ureaplasma urealyticum, and Gardnerella vaginalis. § General anesthesia § Cesarean delivery for multifetal gestation § Young maternal age and nulliparity, § Prolonged labor induction, § Obesity, § Meconium-stained amnionic fluid
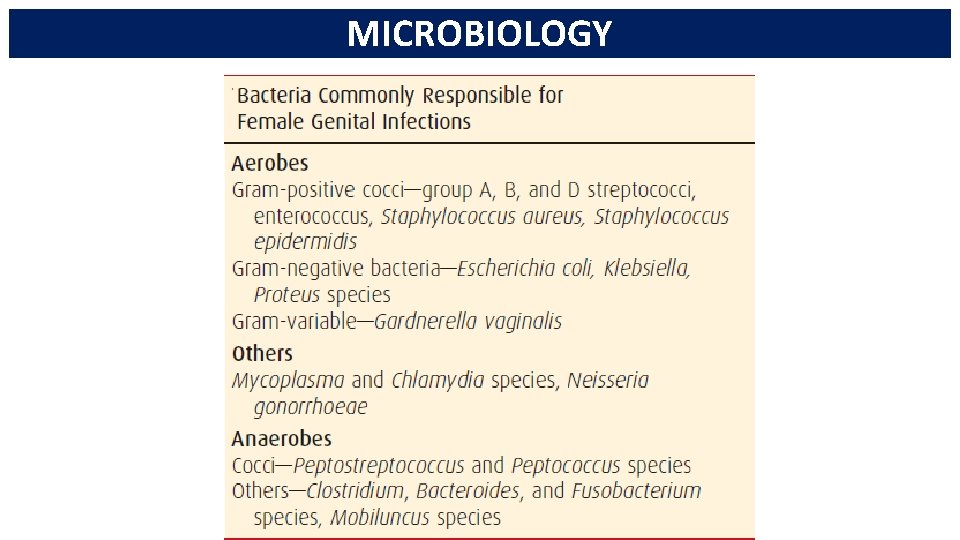
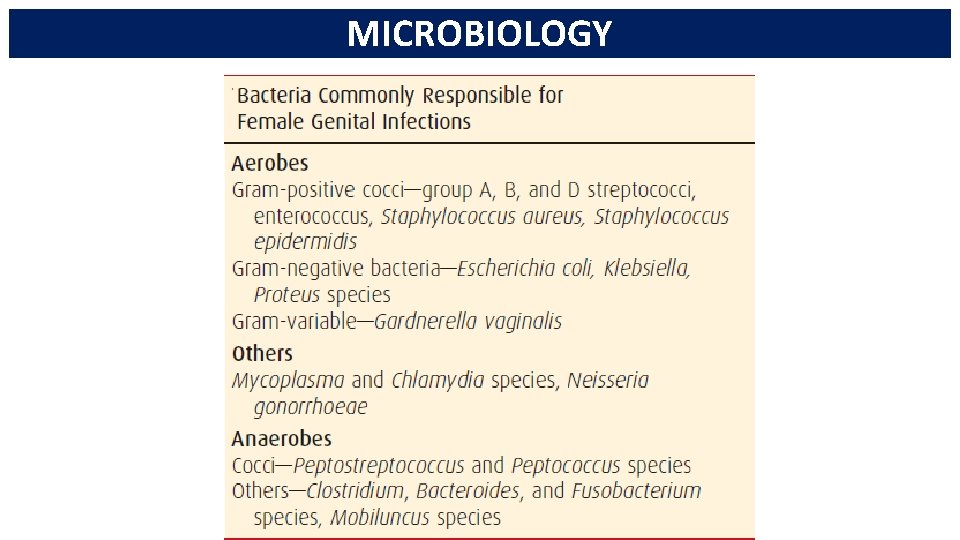
MICROBIOLOGY
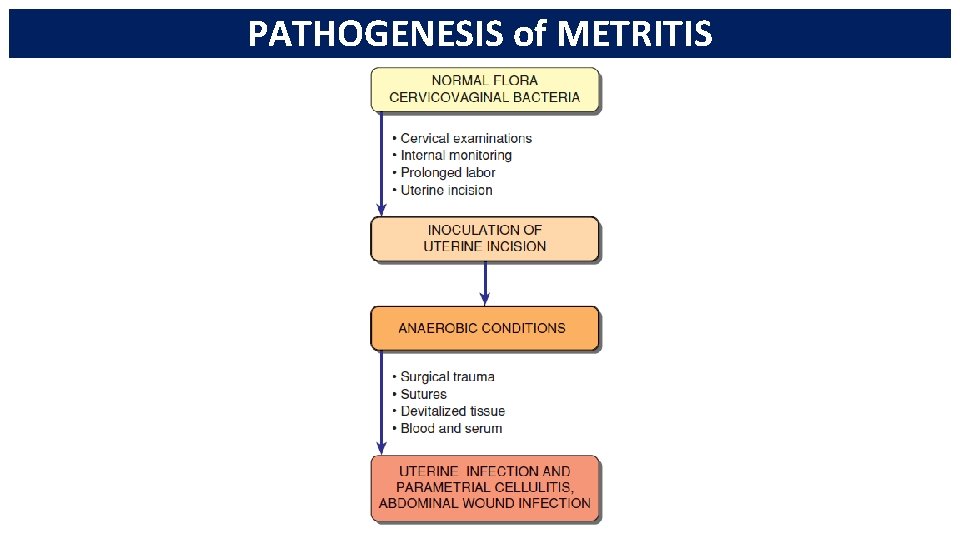
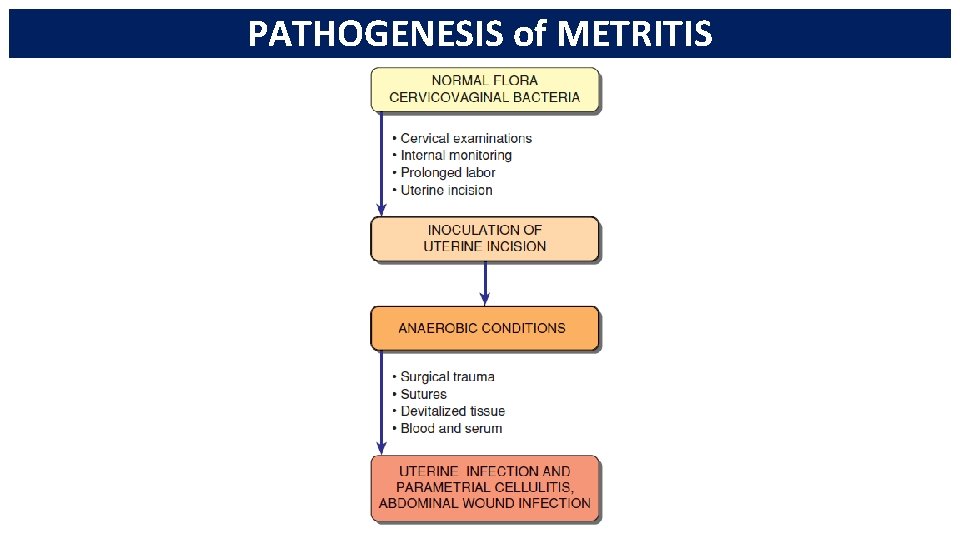
PATHOGENESIS of METRITIS
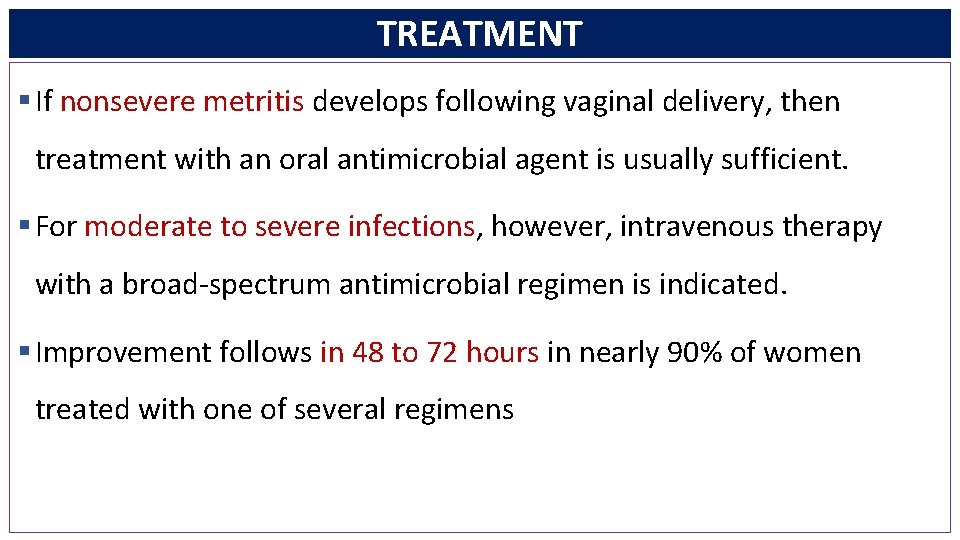
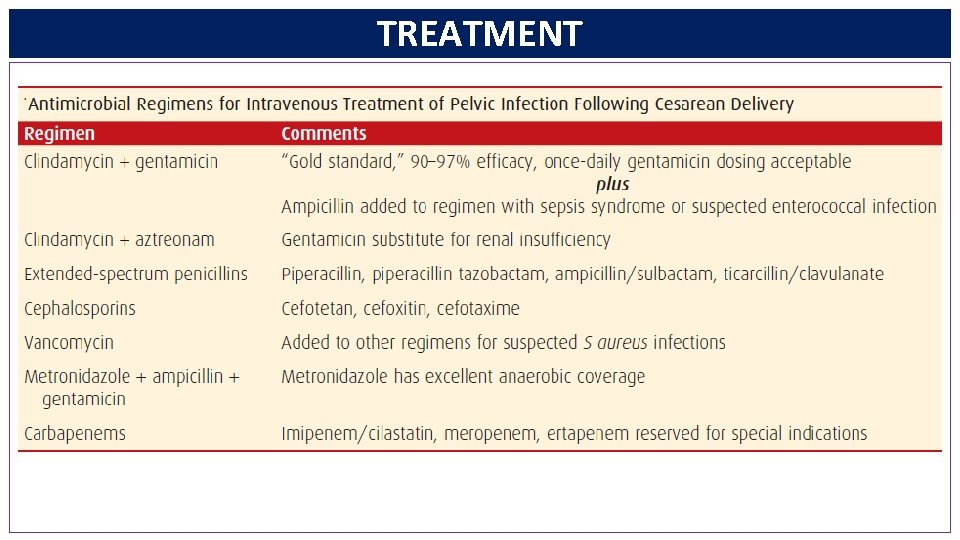
TREATMENT § If nonsevere metritis develops following vaginal delivery, then treatment with an oral antimicrobial agent is usually sufficient. § For moderate to severe infections, however, intravenous therapy with a broad-spectrum antimicrobial regimen is indicated. § Improvement follows in 48 to 72 hours in nearly 90% of women treated with one of several regimens
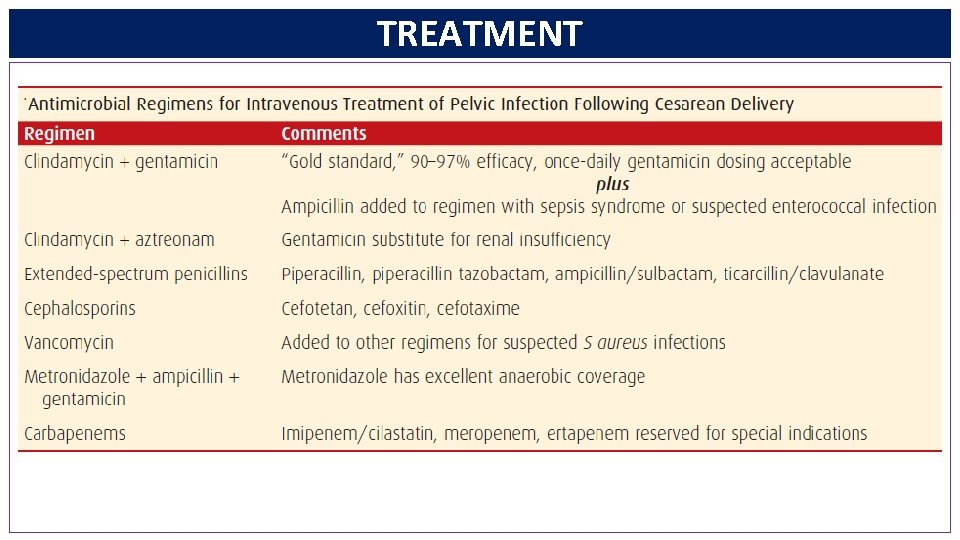
TREATMENT
PERIOPERATIVE PROPHYLAXIS § Administration of antimicrobial prophylaxis at the time of cesarean delivery has remarkably reduced the postoperative pelvic and wound infection rates. § Single-dose prophylaxis with ampicillin or a first-generation cephalosporin is ideal, and both are as effective as broadspectrum agents or a multipledose regimen. § There may be additive salutary effects of preoperative vaginal cleansing with povidone-iodine or application of metronidazole gel.
COMPLICATIONS OF UTERINE AND PELVIC INFECTIONS § In more than 90% of women, metritis responds to treatment within 48 to 72 hours. § In some of the remainder, any of several complications like wound infections, complex pelvic infections such as phlegmons or abscesses, and septic pelvic thrombophlebitis will rise.
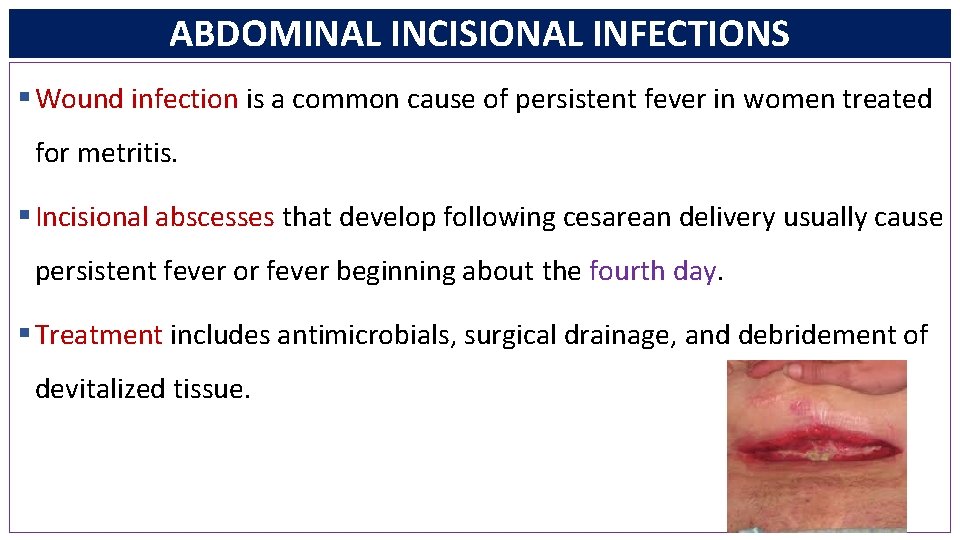
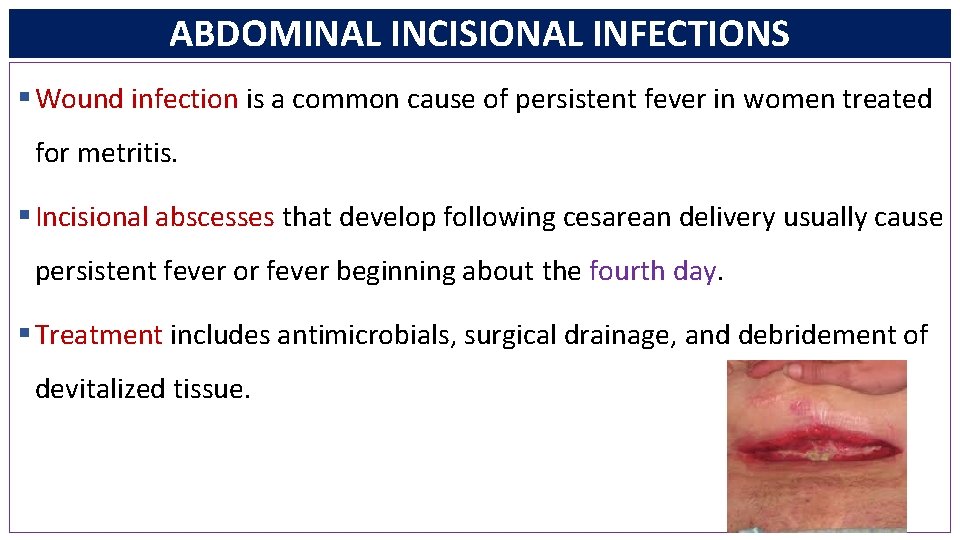
ABDOMINAL INCISIONAL INFECTIONS § Wound infection is a common cause of persistent fever in women treated for metritis. § Incisional abscesses that develop following cesarean delivery usually cause persistent fever or fever beginning about the fourth day. § Treatment includes antimicrobials, surgical drainage, and debridement of devitalized tissue.
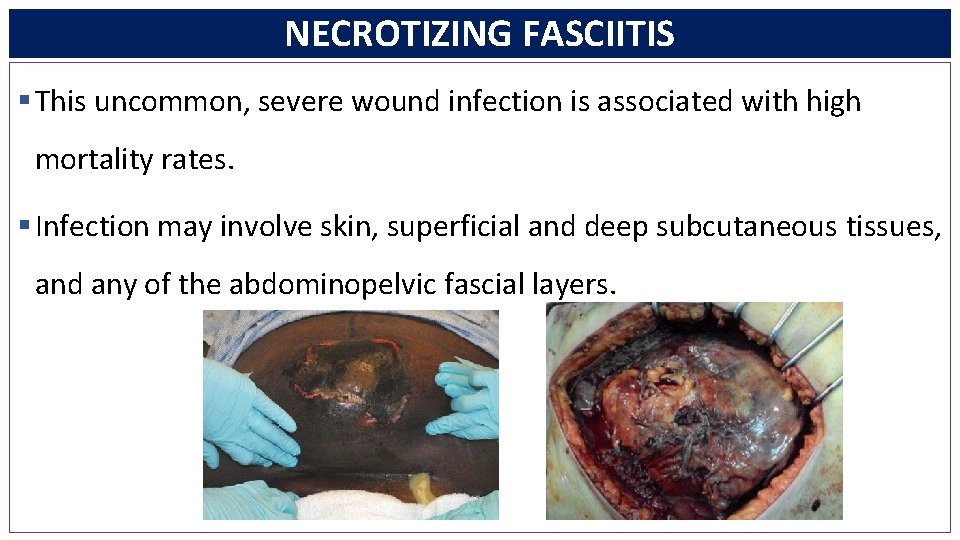
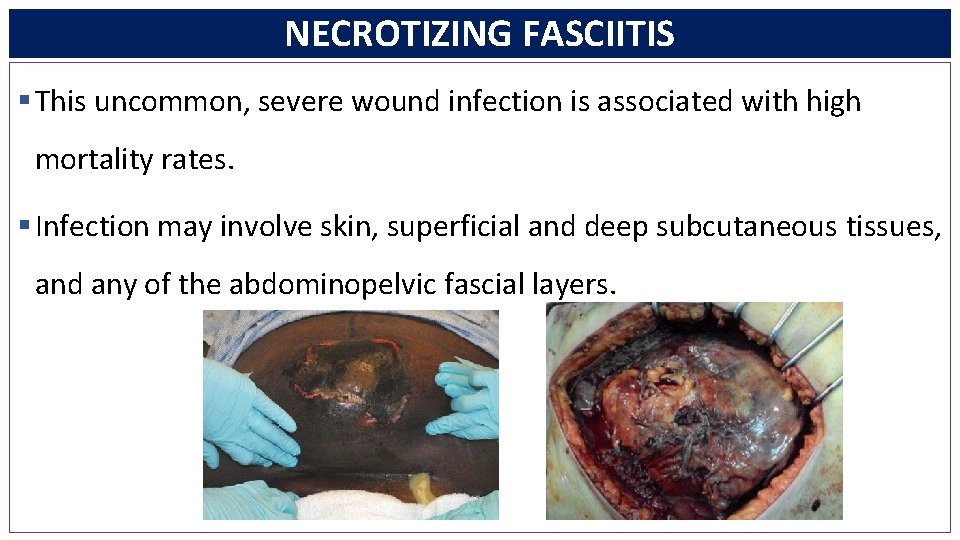
NECROTIZING FASCIITIS § This uncommon, severe wound infection is associated with high mortality rates. § Infection may involve skin, superficial and deep subcutaneous tissues, and any of the abdominopelvic fascial layers.
NECROTIZING FASCIITIS § Early diagnosis, surgical debridement, antimicrobials, and intensive care paramount to successfully treat necrotizing soft-tissue infections. § Death is virtually universal without surgical treatment, and rates approach 50% even if extensive debridement is performed.
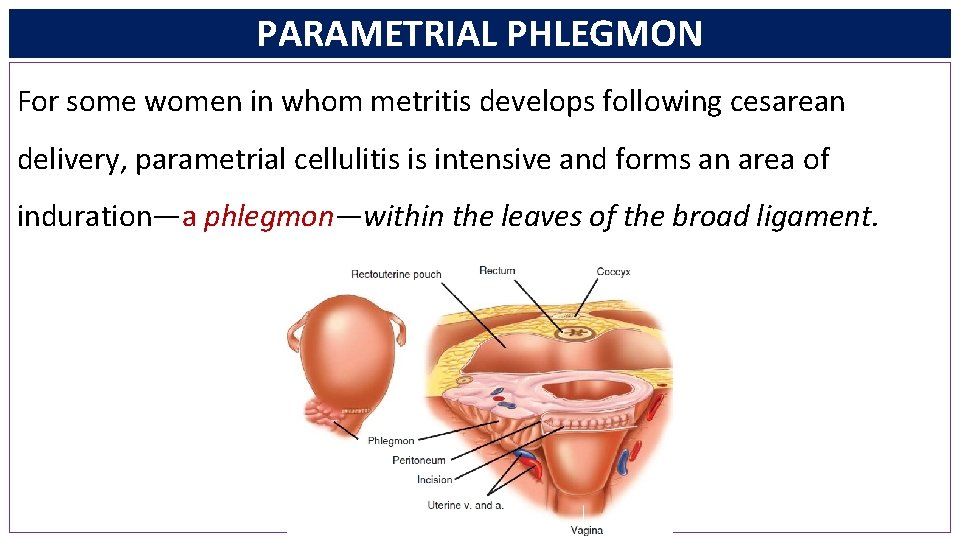
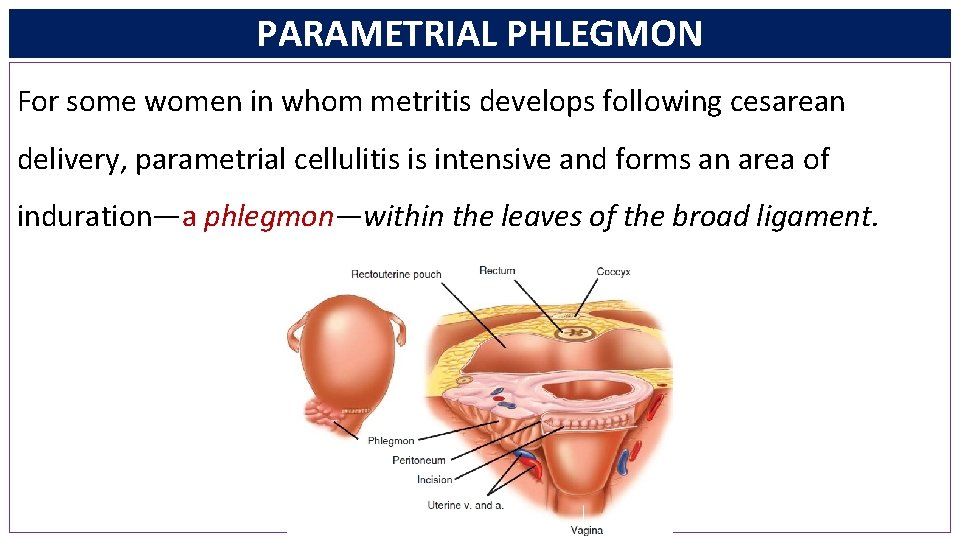
PARAMETRIAL PHLEGMON For some women in whom metritis develops following cesarean delivery, parametrial cellulitis is intensive and forms an area of induration—a phlegmon—within the leaves of the broad ligament.
PARAMETRIAL PHLEGMON § These infections should be considered when fever persists longer than 72 hours despite intravenous antimicrobial therapy!!! § Unilateral, and they frequently are limited to the parametrium § For most, hysterectomy and surgical debridement are needed
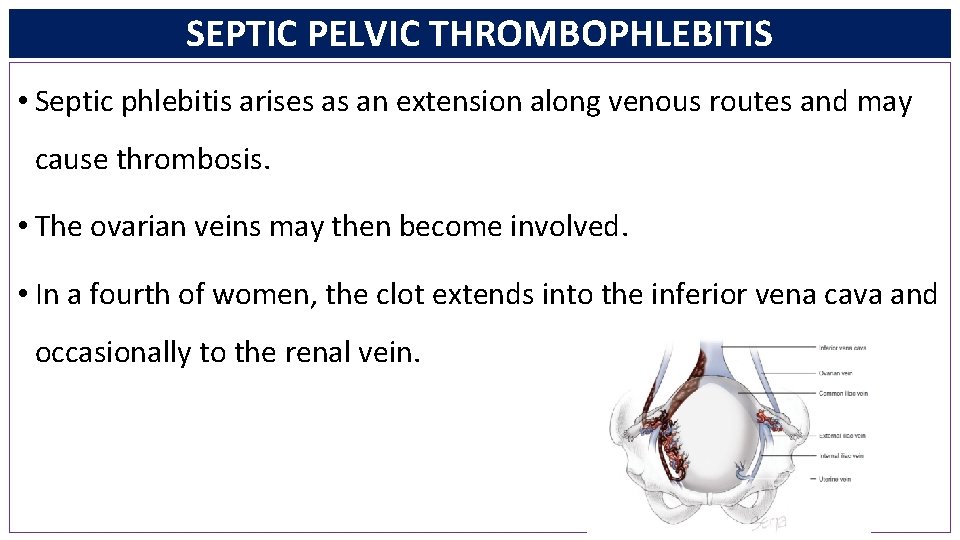
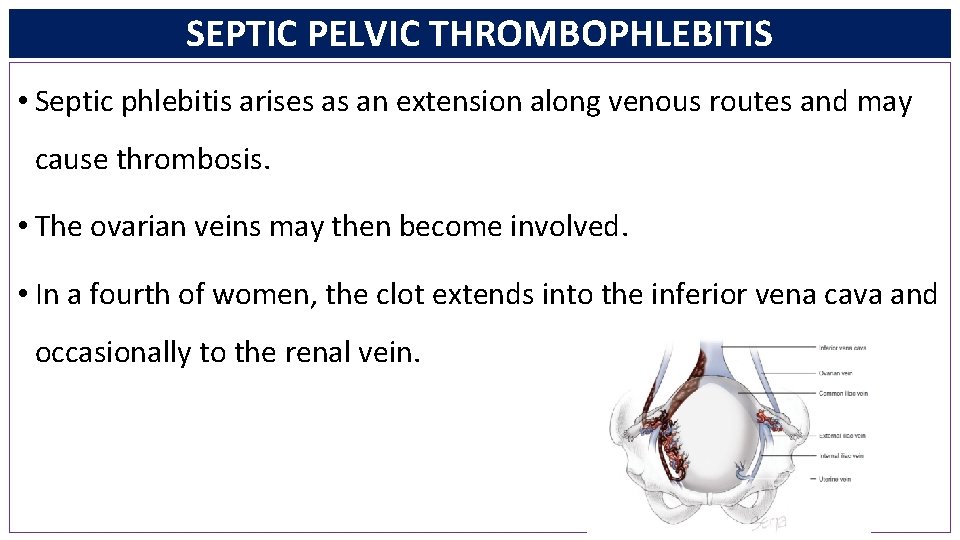
SEPTIC PELVIC THROMBOPHLEBITIS • Septic phlebitis arises as an extension along venous routes and may cause thrombosis. • The ovarian veins may then become involved. • In a fourth of women, the clot extends into the inferior vena cava and occasionally to the renal vein.
SEPTIC PELVIC THROMBOPHLEBITIS • Incidence: • 1 per 9000 following vaginal delivery and • 1 per 800 with cesarean delivery. • Women with septic thrombophlebitis usually have symptomatic improvement with antimicrobial treatment, however, they continue to have fever !!!
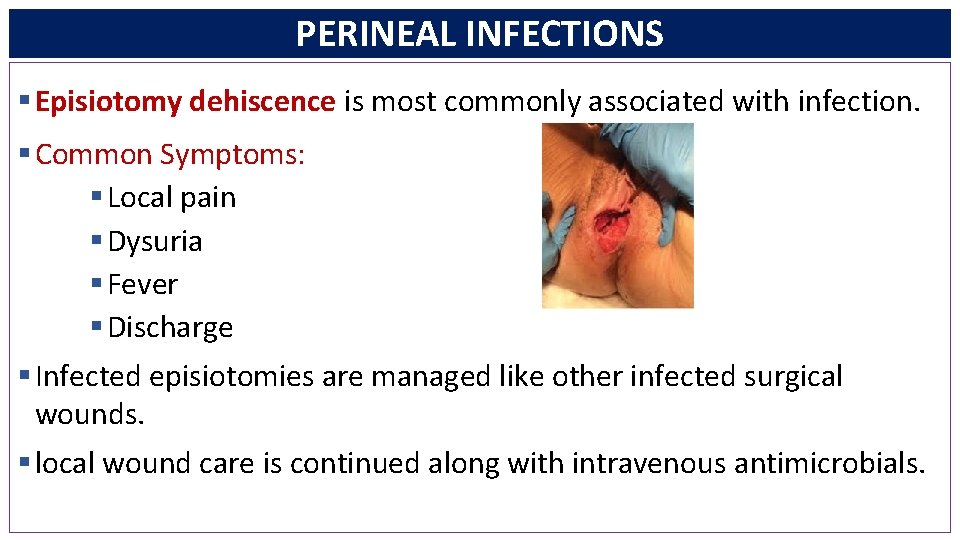
PERINEAL INFECTIONS § Episiotomy dehiscence is most commonly associated with infection. § Common Symptoms: § Local pain § Dysuria § Fever § Discharge § Infected episiotomies are managed like other infected surgical wounds. § local wound care is continued along with intravenous antimicrobials.
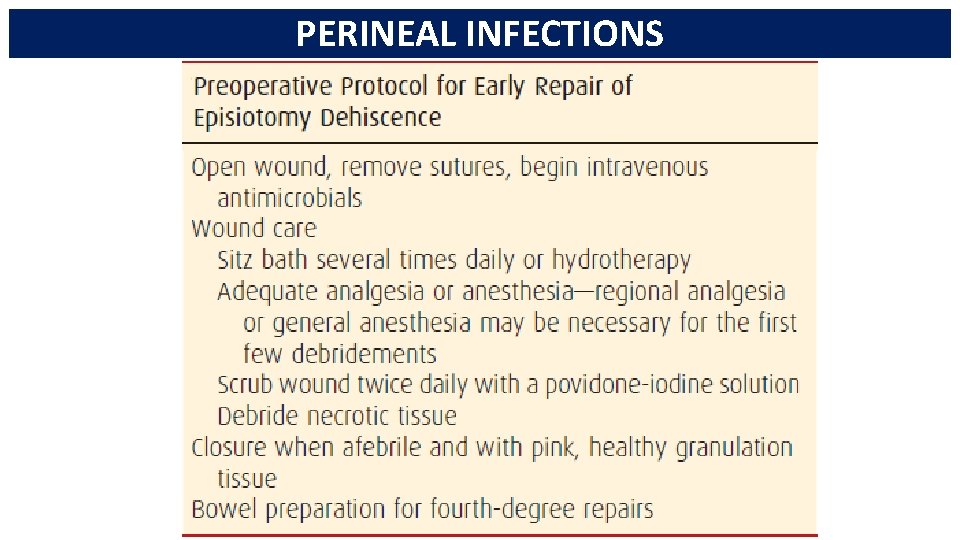
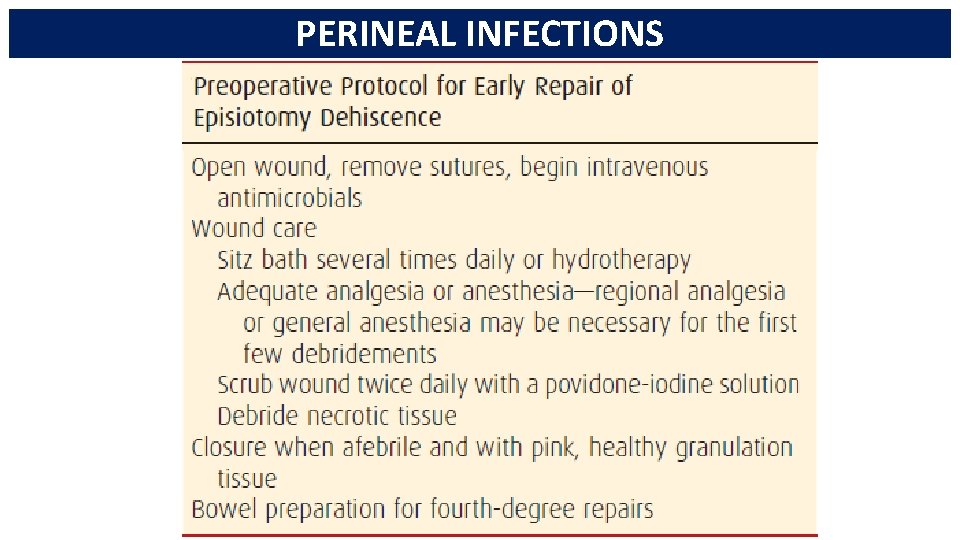
PERINEAL INFECTIONS
TOXIC SHOCK SYNDROME § There is usually fever, headache, mental confusion, diffuse macular erythematous rash, subcutaneous edema, nausea, vomiting, watery diarrhea, and marked hemoconcentration. § Staphylococcus aureus with endotoxin; toxic shock syndrome toxin-1 (TSST-1) was recovered from almost all afflicted persons.
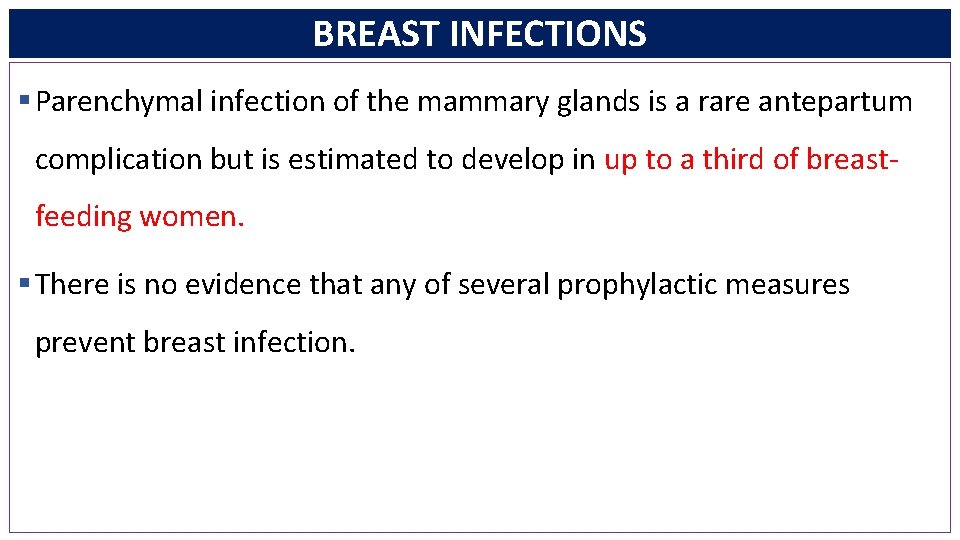
BREAST INFECTIONS § Parenchymal infection of the mammary glands is a rare antepartum complication but is estimated to develop in up to a third of breastfeeding women. § There is no evidence that any of several prophylactic measures prevent breast infection.
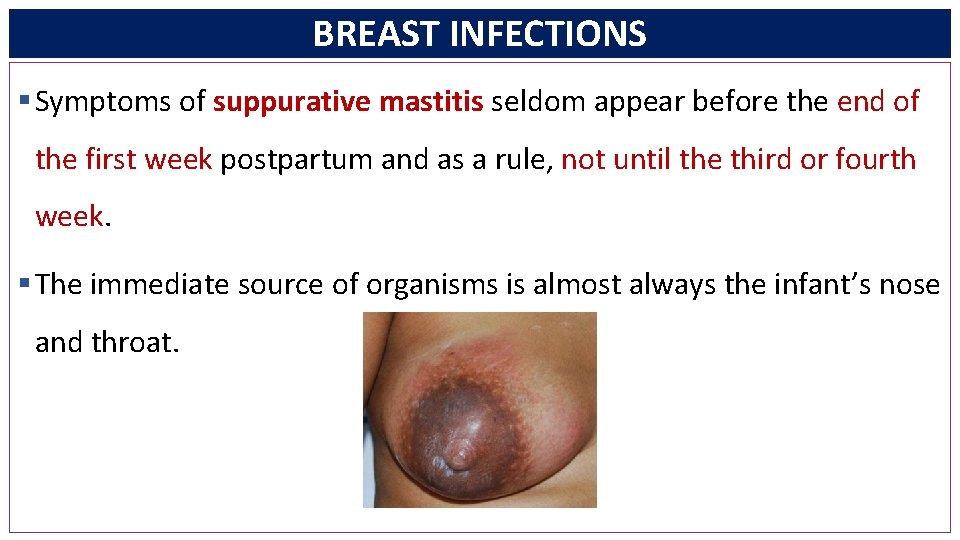
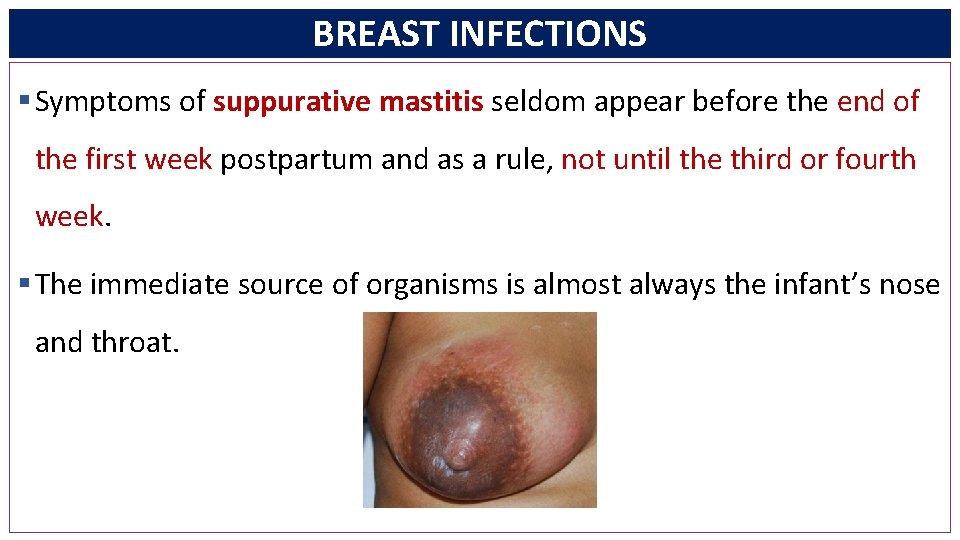
BREAST INFECTIONS § Symptoms of suppurative mastitis seldom appear before the end of the first week postpartum and as a rule, not until the third or fourth week. § The immediate source of organisms is almost always the infant’s nose and throat.
BREAST INFECTIONS § Staphylococcus aureus, especially its methicillin-resistant strain, is the most commonly isolated organism. § Provided that appropriate therapy for mastitis is started before suppuration begins, the infection usually resolves within 48 hours. § Dicloxacillin, 500 mg orally four times daily, may be started empirically.
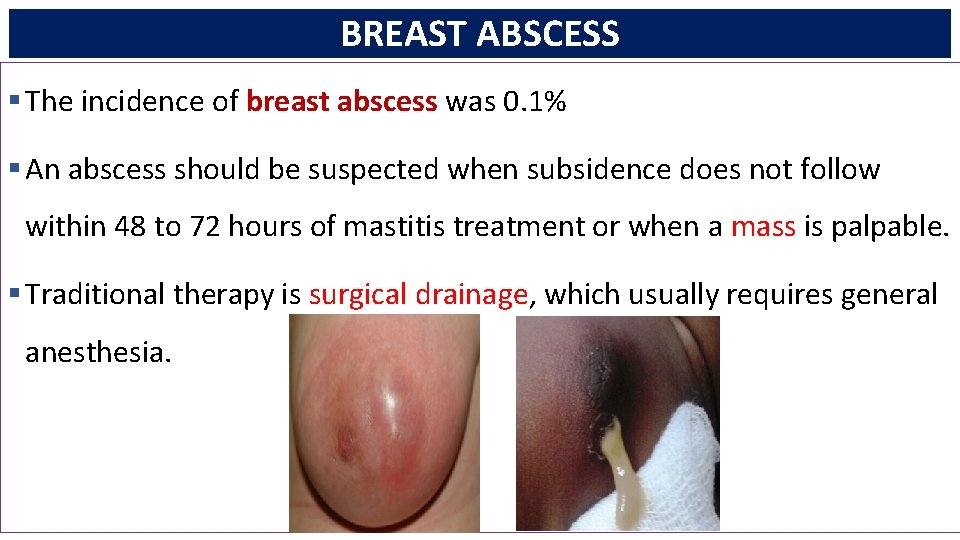
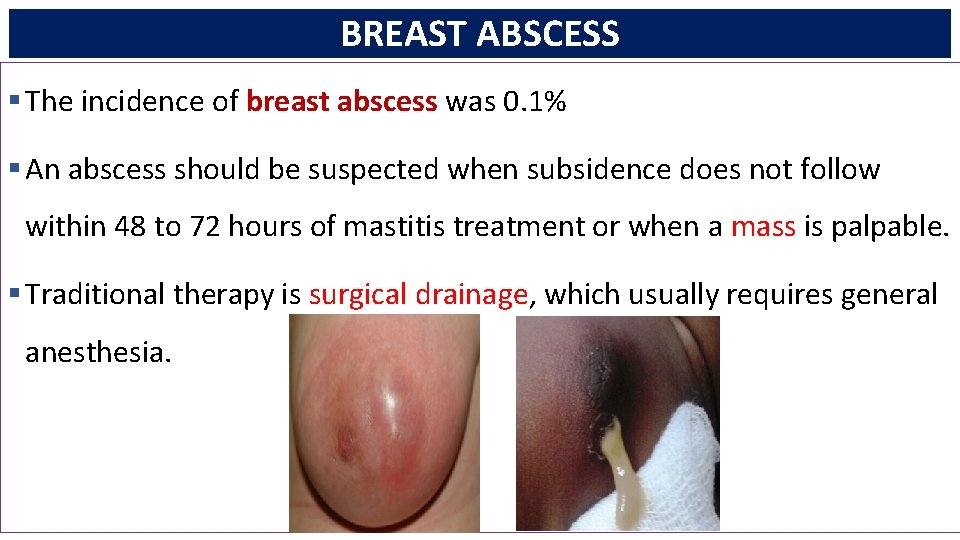
BREAST ABSCESS § The incidence of breast abscess was 0. 1% § An abscess should be suspected when subsidence does not follow within 48 to 72 hours of mastitis treatment or when a mass is palpable. § Traditional therapy is surgical drainage, which usually requires general anesthesia.
REFERENCES 1. Michael S. Baggish, Atlas of Pelvic Anatomy and Gynecologic Surgery, Third Edition, California, Saunders Elsevier, 2011 2. Williams Obstetrics 24. th edition-Cunningham et al. The Mc. Graw-Hill Companies-2014 3. Gabbe: Obstetrics: Normal and Problem Pregnancies, 6 th ed. , 2013 4. Current Obstetrics & Gyneacology , Mc. Graw. Hill, Lange, 12 th edition 2015 5. Creasy And Resnik’s Maternal-fetal Medicine, Seventh Edition, Elsevier
 Seluk sport
Seluk sport Lactating women meaning
Lactating women meaning Management of puerperium
Management of puerperium Reva rubin scale
Reva rubin scale Dr nihal harris
Dr nihal harris Twin icd 10
Twin icd 10 Adverse events in hospital
Adverse events in hospital Tratamento mastite puerperal
Tratamento mastite puerperal Puerperal sepsis
Puerperal sepsis Prevention of puerperal sepsis
Prevention of puerperal sepsis Acute gingival infections
Acute gingival infections Neurosiphyllis
Neurosiphyllis Opportunistic infections
Opportunistic infections Genital infections
Genital infections Storch infections
Storch infections Johnson and johnson botnet infections
Johnson and johnson botnet infections Bacterial vaginosis
Bacterial vaginosis Methotrexate yeast infection
Methotrexate yeast infection Genital infections
Genital infections Storch infections
Storch infections Postpartum infections
Postpartum infections Opportunistic infections
Opportunistic infections Innate immunity first line of defense
Innate immunity first line of defense Bone and joint infections
Bone and joint infections Retroviruses and opportunistic infections
Retroviruses and opportunistic infections A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Diễn thế sinh thái là
Diễn thế sinh thái là Thế nào là giọng cùng tên?
Thế nào là giọng cùng tên? Phép trừ bù
Phép trừ bù Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chúa yêu trần thế
Chúa yêu trần thế Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ đại từ thay thế
đại từ thay thế Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công của trọng lực
Công của trọng lực Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Lời thề hippocrates
Lời thề hippocrates Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Frameset trong html5
Frameset trong html5 Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Sơ đồ cơ thể người
Sơ đồ cơ thể người Tư thế ngồi viết
Tư thế ngồi viết đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5