Osteoporosis The silent killer Michele T Glasgow MD
- Slides: 55
Osteoporosis: The silent killer � Michele T. Glasgow, MD � Midwest Orthopaedic Institute � Bone Health Center � 2111 Midlands Court � Sycamore, Illinois
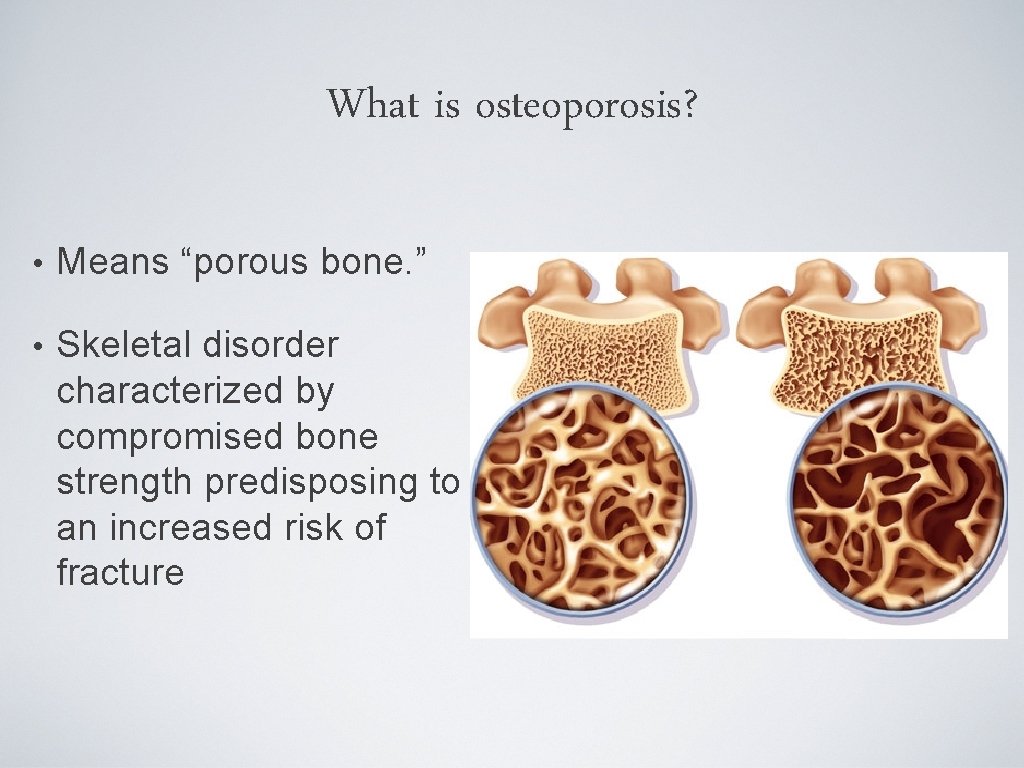
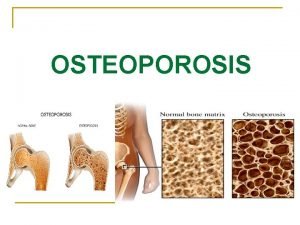
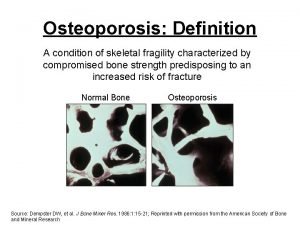
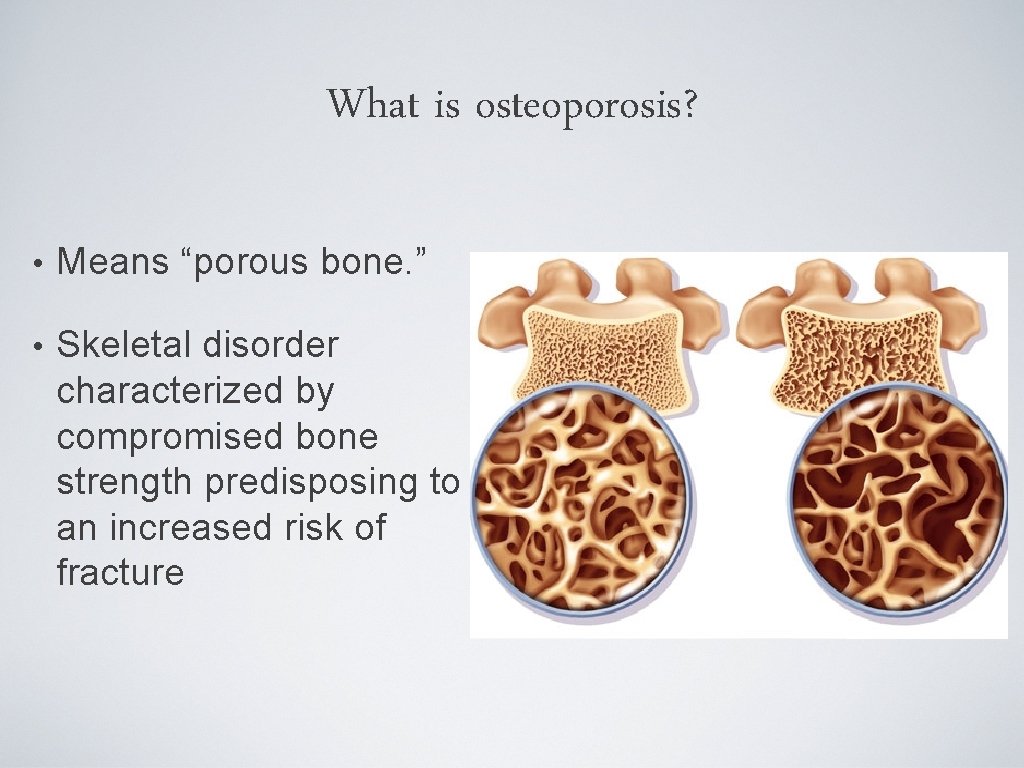
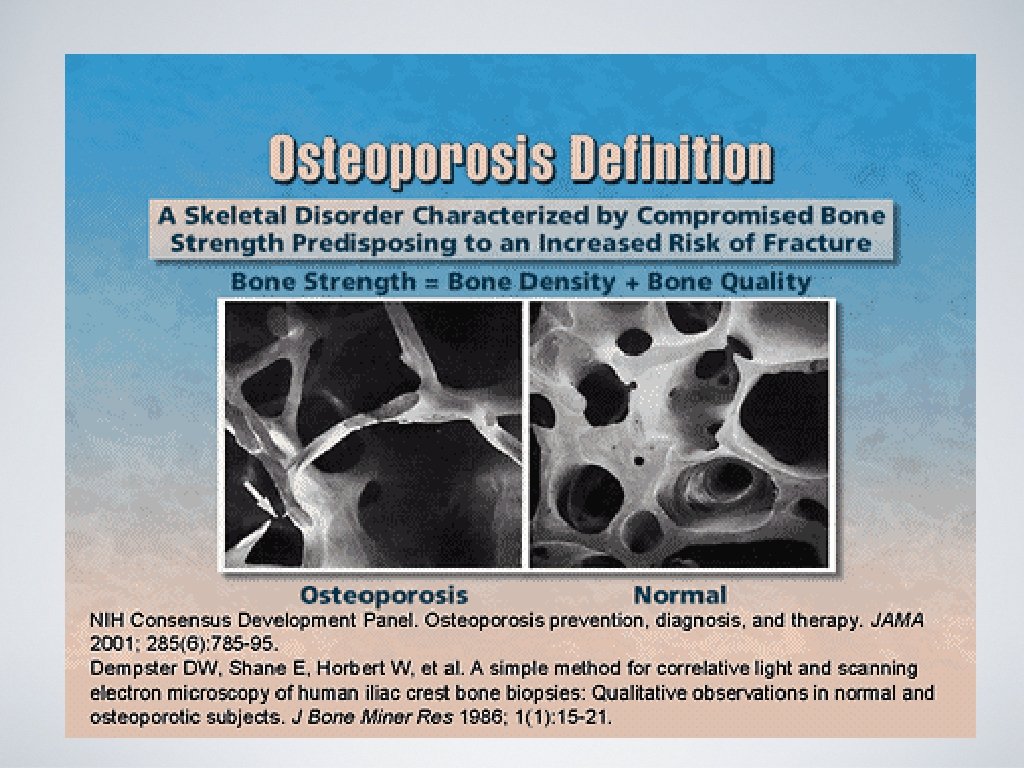
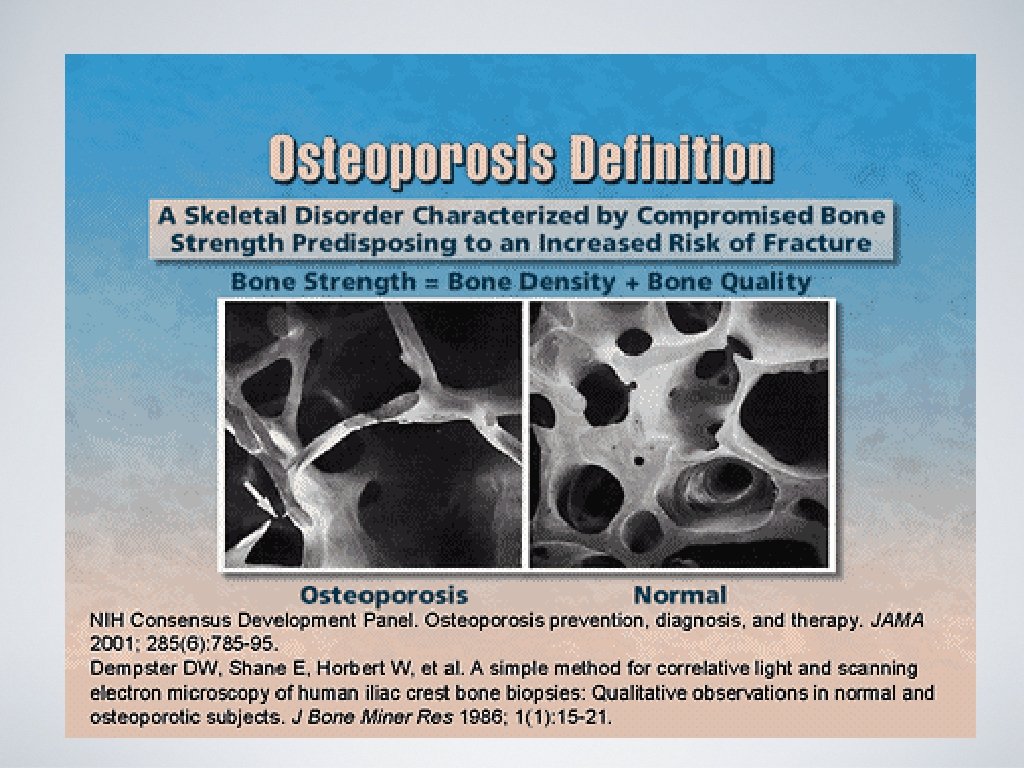
What is osteoporosis? • Means “porous bone. ” • Skeletal disorder characterized by compromised bone strength predisposing to an increased risk of fracture
Osteoporosis is Common • 9 million Americans have osteoporosis (~80% women) • 200 million people worldwide • 1 in 2 women and 1 in 4 men >50 yo will have an osteoporosis fracture in their lifetime • By 2020, it is projected that there will be ~14 million Americans with osteoporosis.
Osteoporosis is Costly • Responsible for 2 million fractures annually • $19 billion in related costs per year • By 2025, experts estimate osteoporosis will be responsible for ~3 million fractures and $25. 3 billion in costs each year
Osteoporosis is Serious • 20% of hip fractures die within one year REGARDLESS OF REPAIR from complications related to surgery or other co-morbidities • ~50% of hip fracture survivors require long term nursing home care and have some degree of permanent disability
Osteoporosis is “Silent” • Bone loss occurs without symptoms • Often it is not detected until a fracture occurs • Compression fractures of the spine often occur without trauma and may present with back pain, kyphosis, or simple height loss
Osteoporosis = TICKING TIME BOMB!!
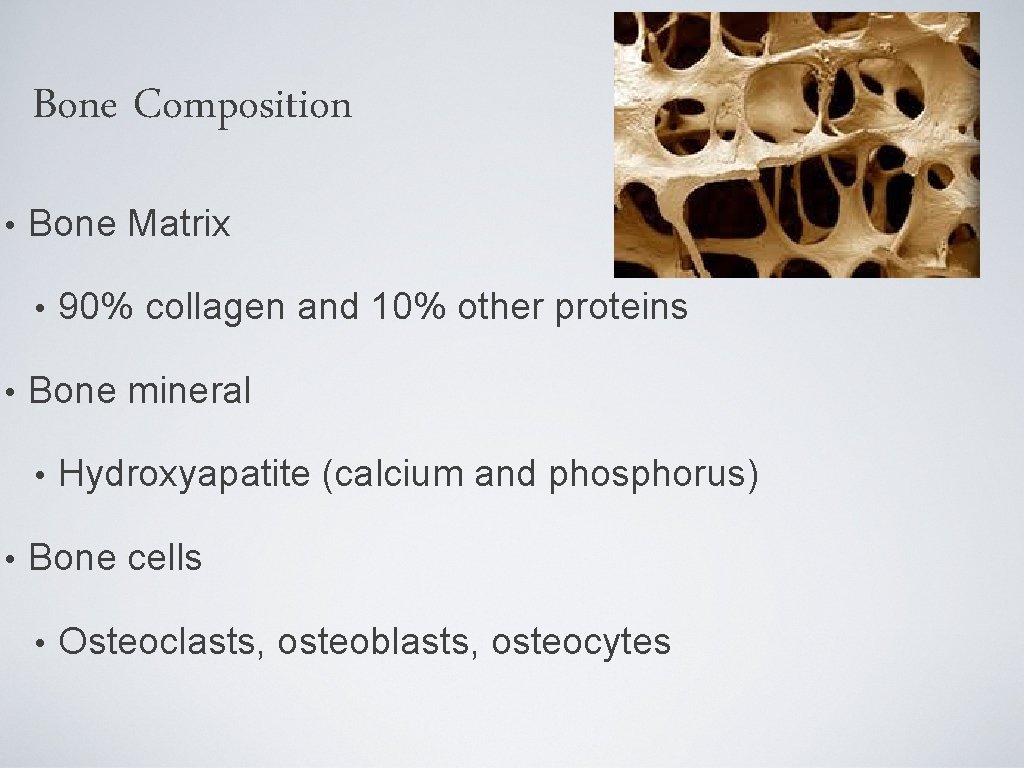
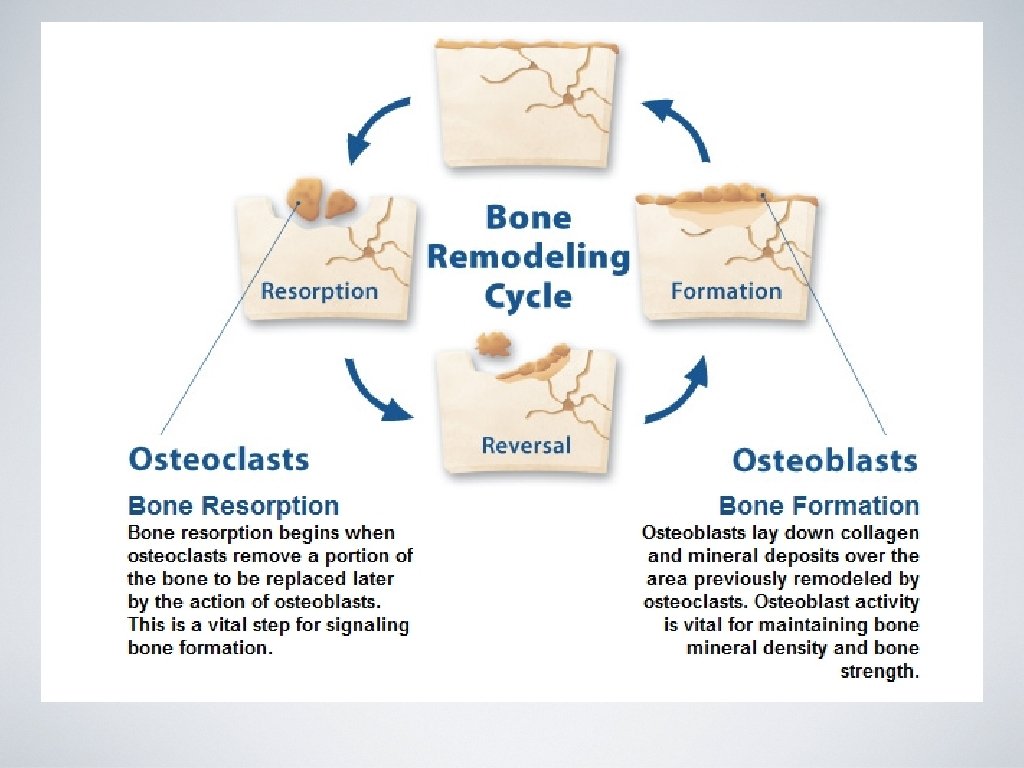
Bone Composition • Bone Matrix • • Bone mineral • • 90% collagen and 10% other proteins Hydroxyapatite (calcium and phosphorus) Bone cells • Osteoclasts, osteoblasts, osteocytes
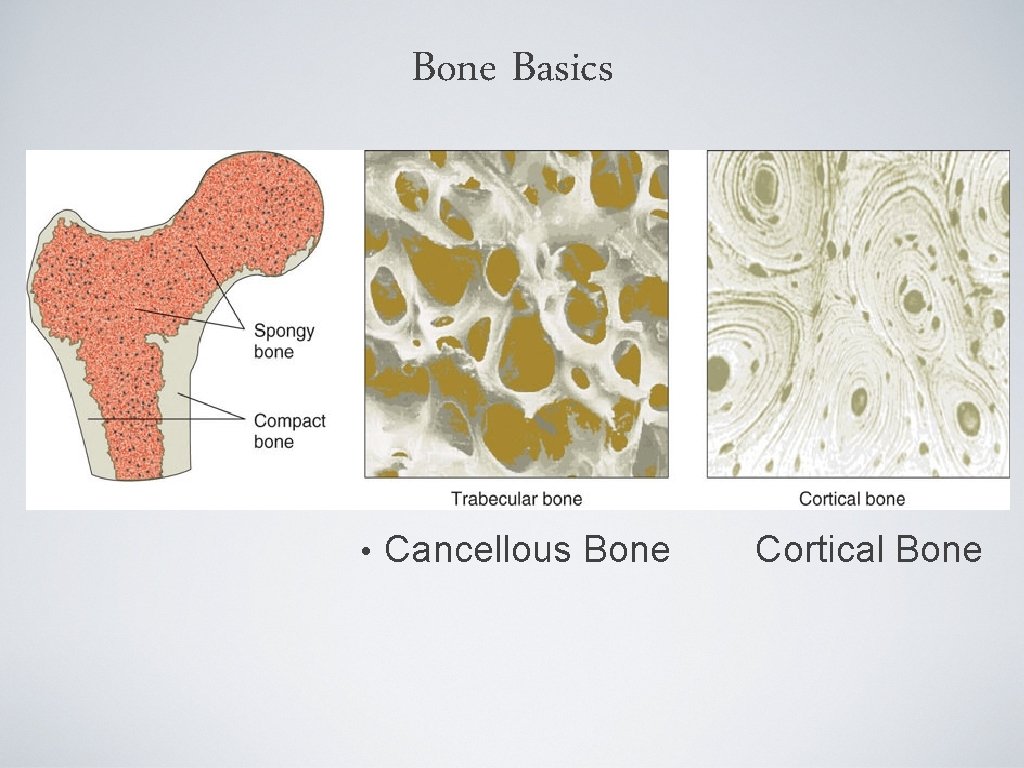
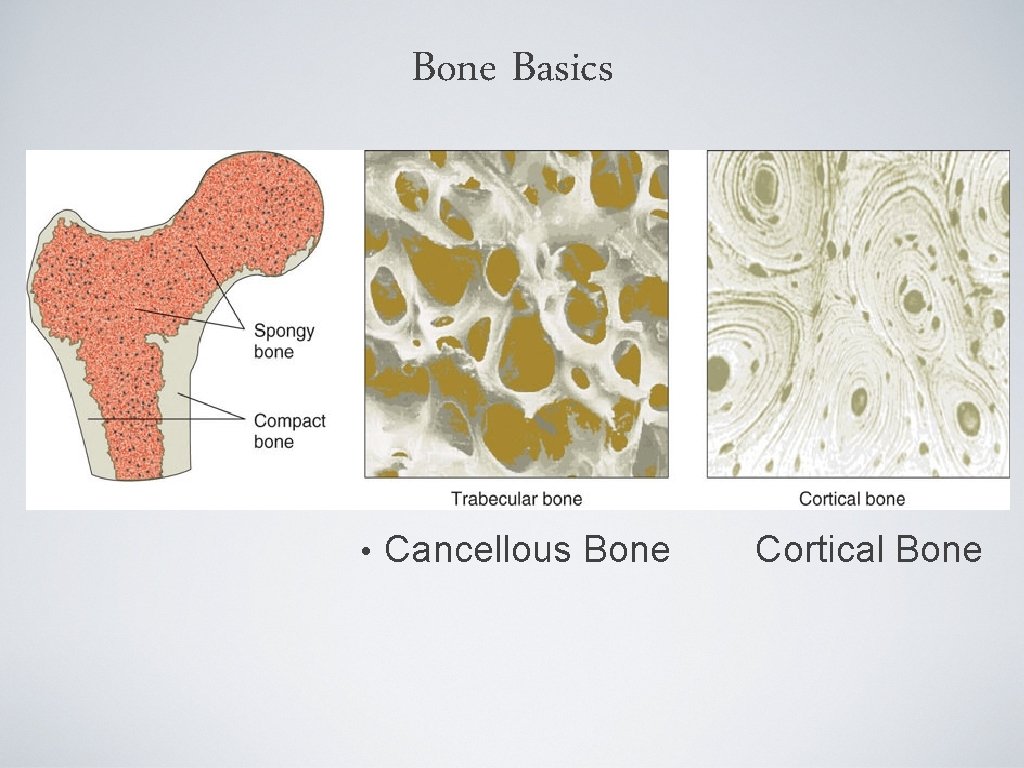
Bone Basics • Cancellous Bone Cortical Bone
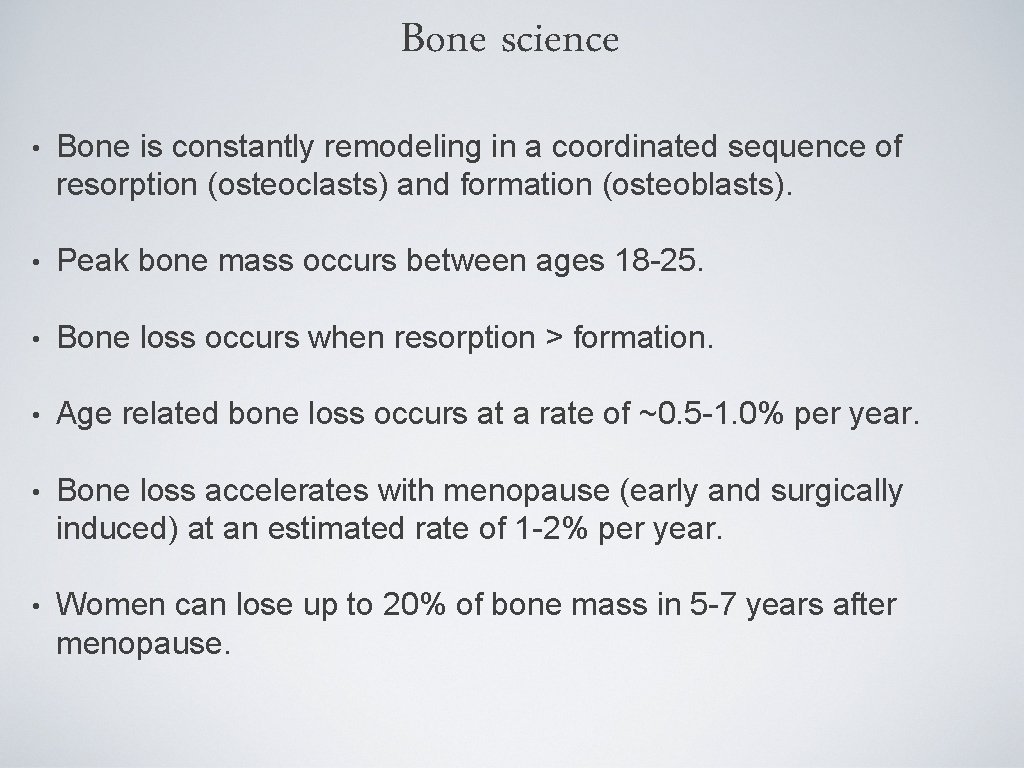
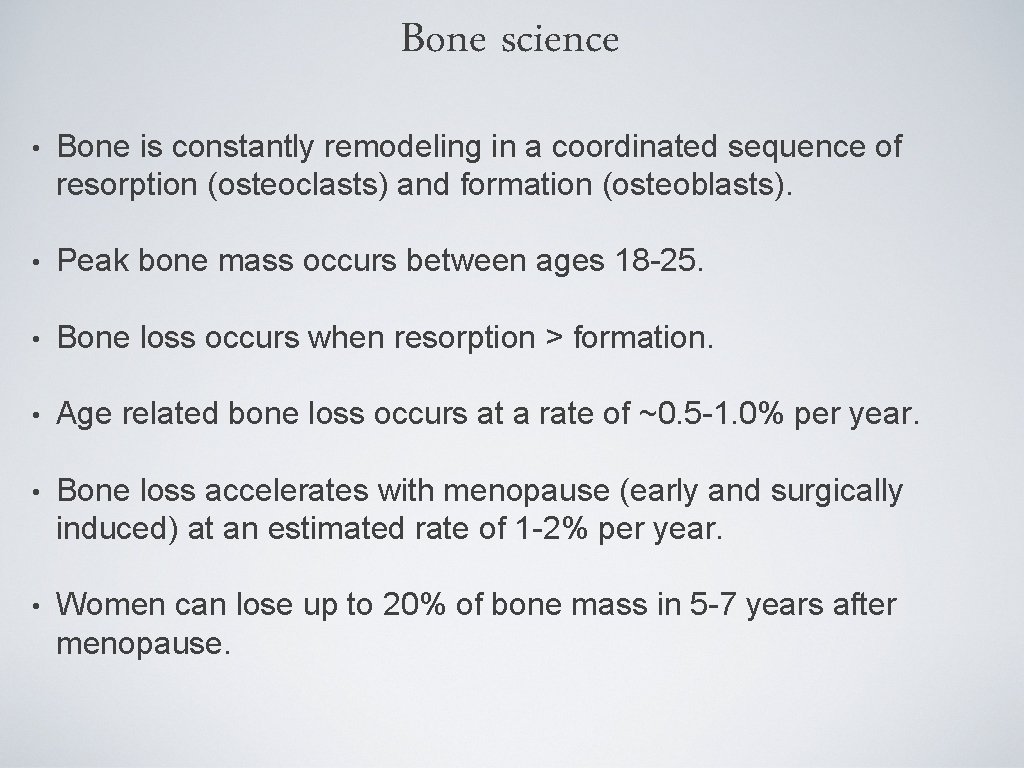
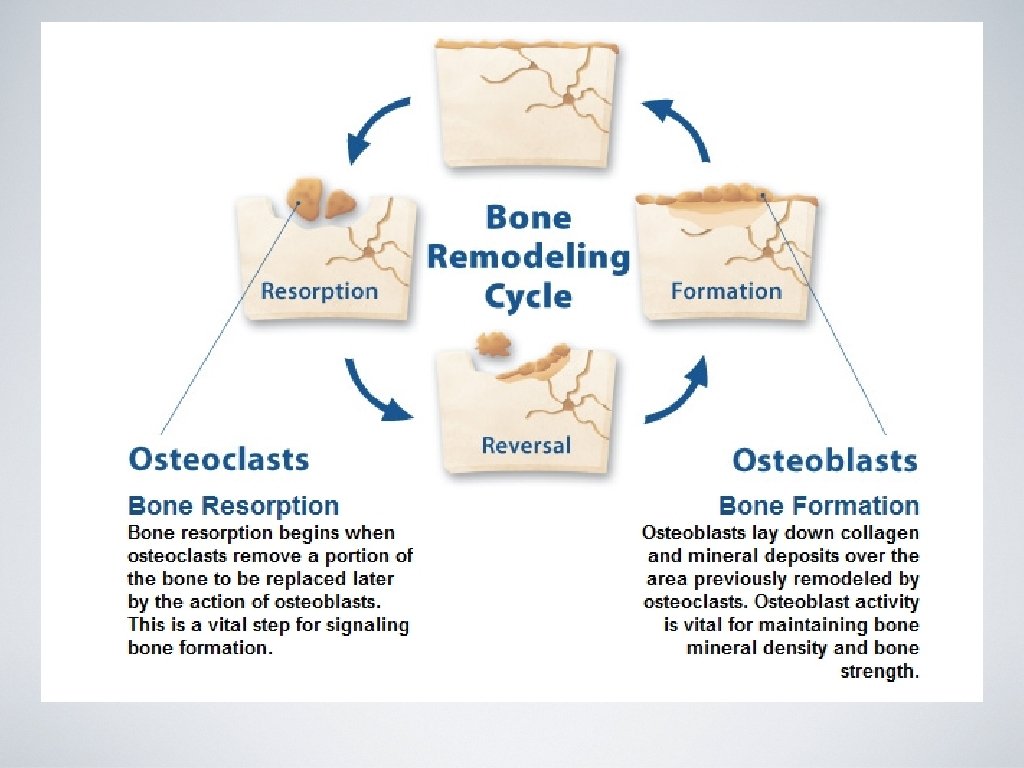
Bone science • Bone is constantly remodeling in a coordinated sequence of resorption (osteoclasts) and formation (osteoblasts). • Peak bone mass occurs between ages 18 -25. • Bone loss occurs when resorption > formation. • Age related bone loss occurs at a rate of ~0. 5 -1. 0% per year. • Bone loss accelerates with menopause (early and surgically induced) at an estimated rate of 1 -2% per year. • Women can lose up to 20% of bone mass in 5 -7 years after menopause.
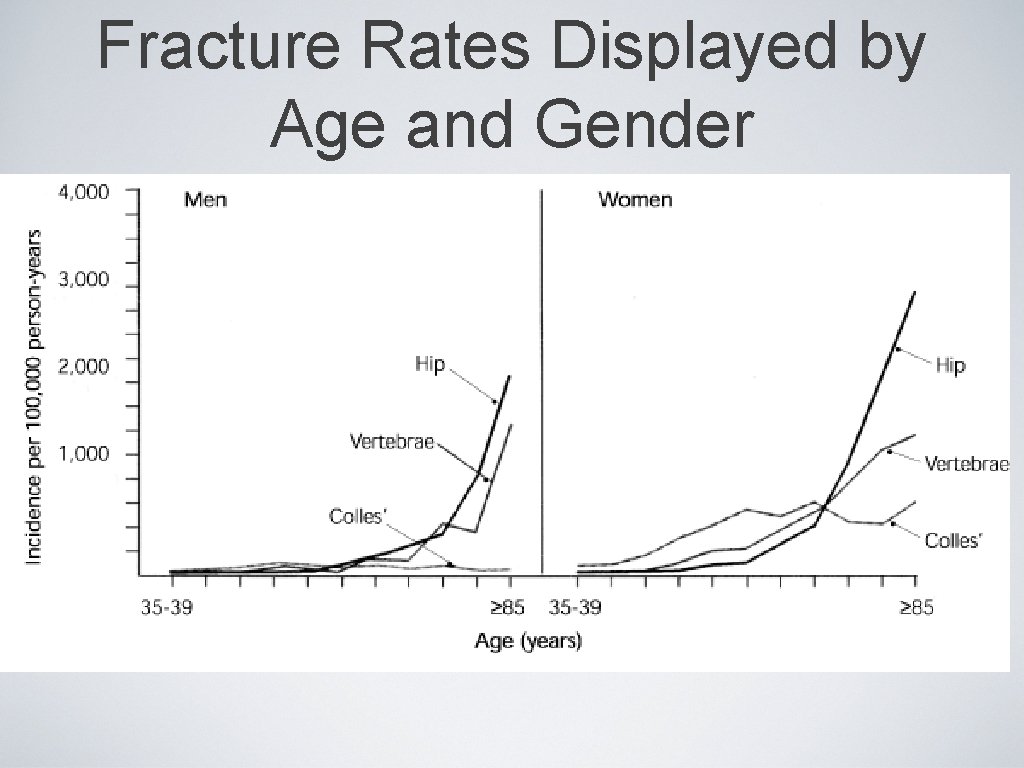
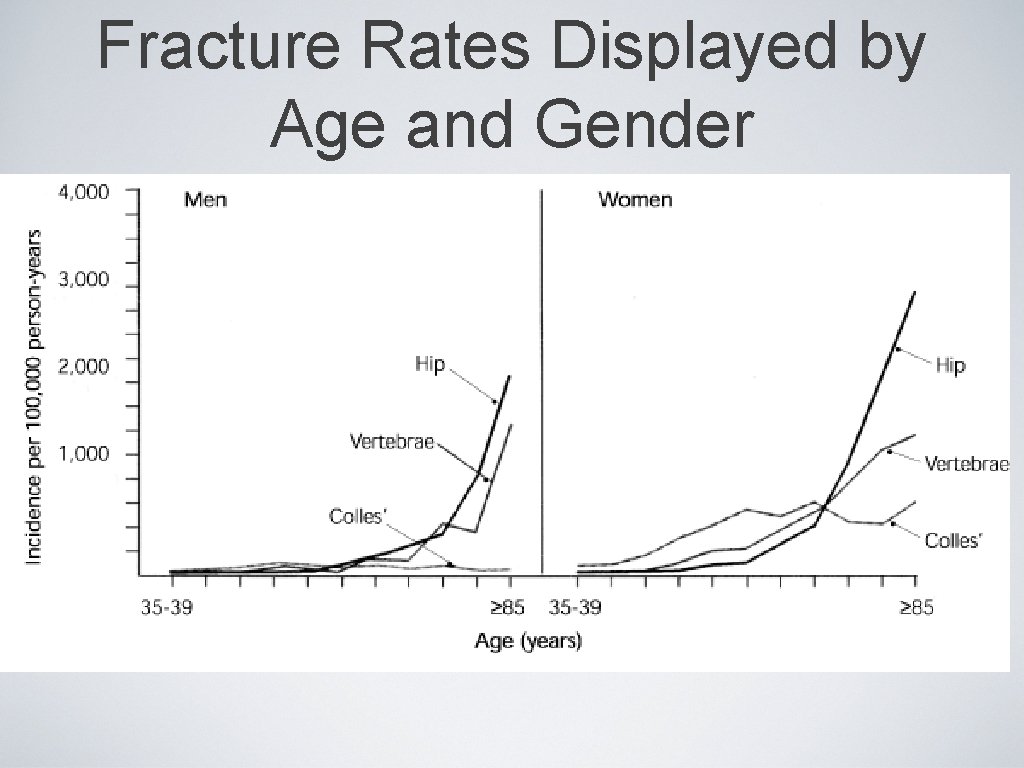
Fracture Rates Displayed by Age and Gender
Who needs to be screened? ASK YOUR DOCTOR!!
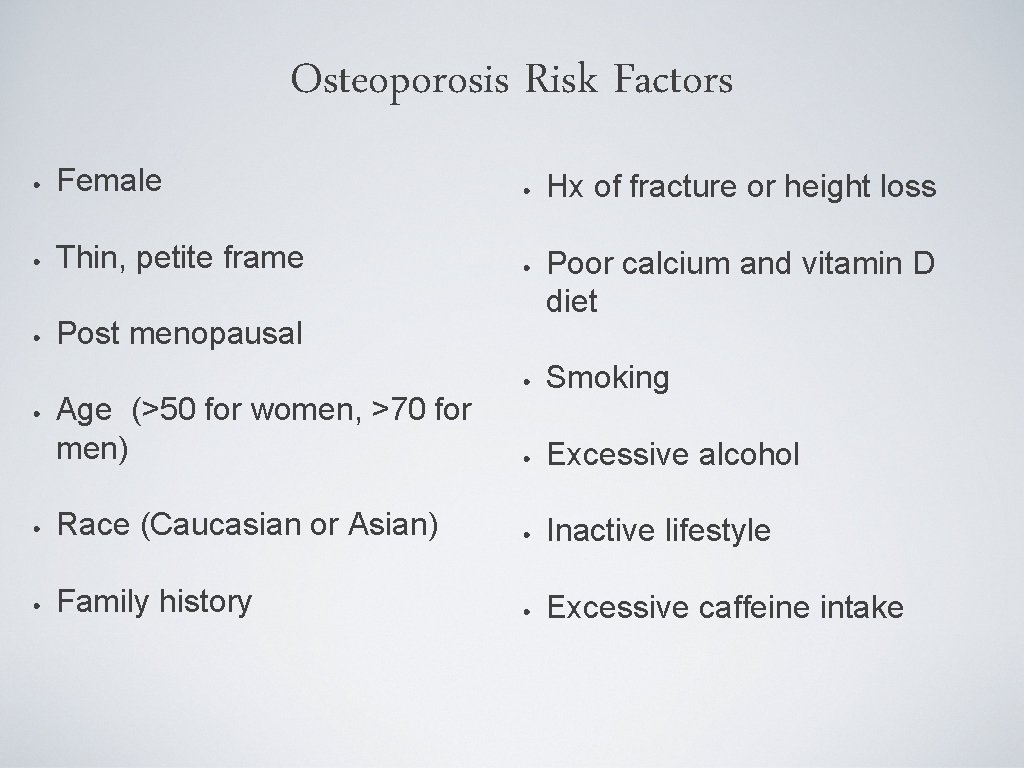
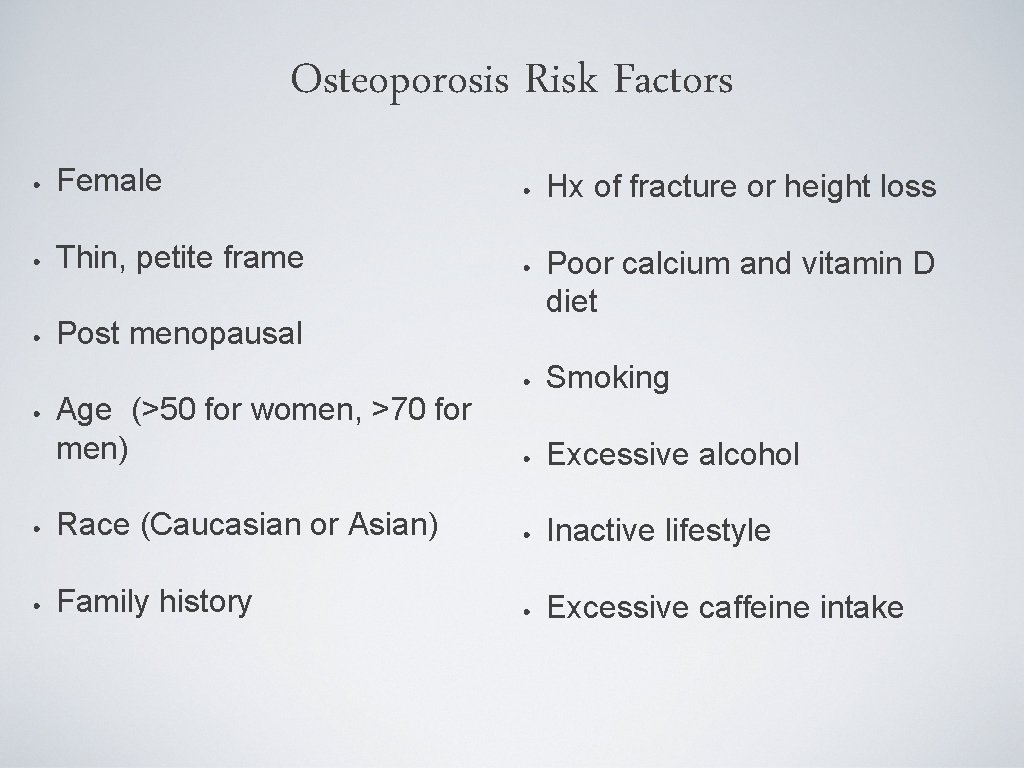
Osteoporosis Risk Factors • Female • Thin, petite frame • Post menopausal • Age (>50 for women, >70 for men) • Race (Caucasian or Asian) • Family history • Hx of fracture or height loss • Poor calcium and vitamin D diet • Smoking • Excessive alcohol • Inactive lifestyle • Excessive caffeine intake
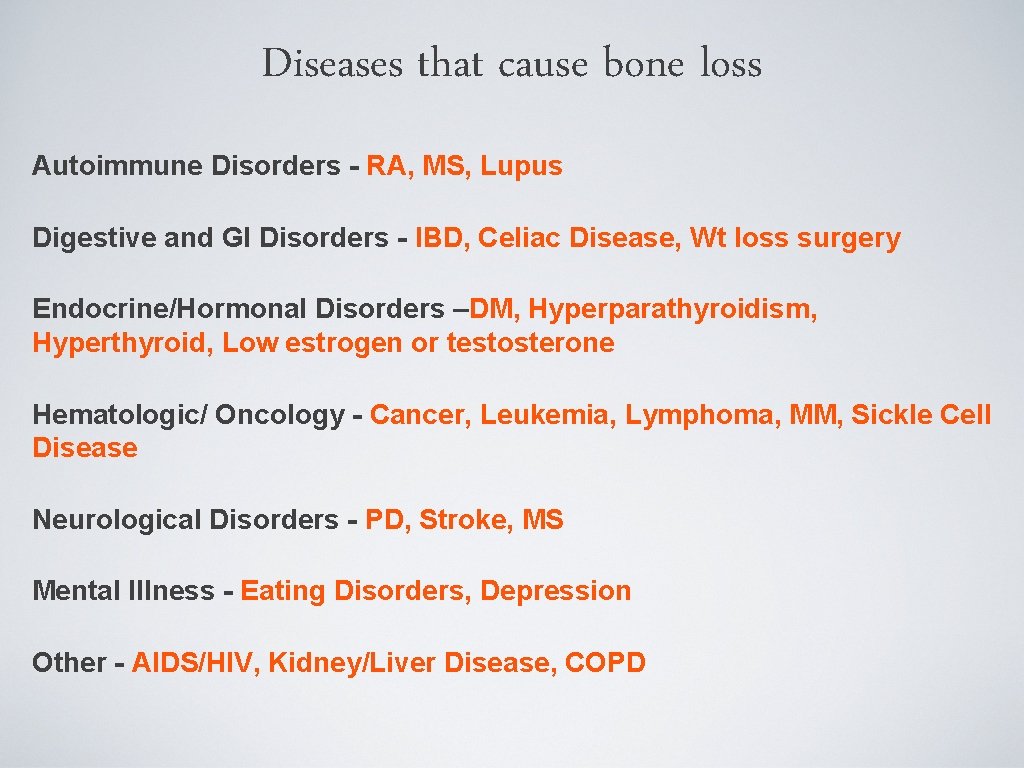
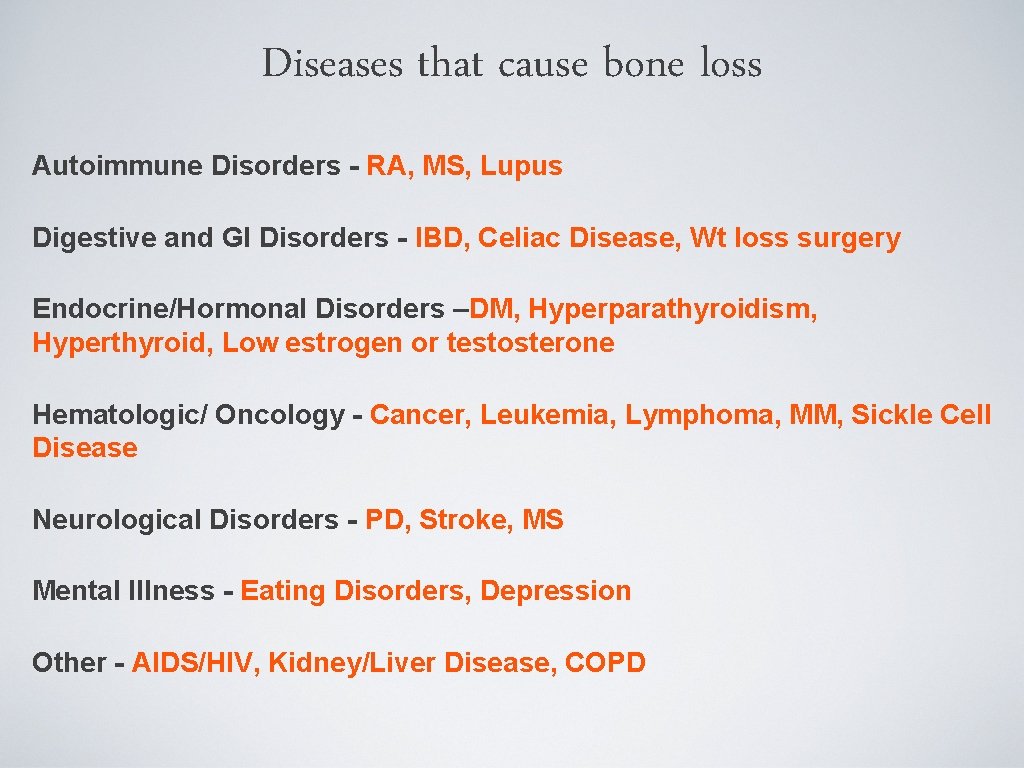
Diseases that cause bone loss Autoimmune Disorders - RA, MS, Lupus Digestive and GI Disorders - IBD, Celiac Disease, Wt loss surgery Endocrine/Hormonal Disorders –DM, Hyperparathyroidism, Hyperthyroid, Low estrogen or testosterone Hematologic/ Oncology - Cancer, Leukemia, Lymphoma, MM, Sickle Cell Disease Neurological Disorders - PD, Stroke, MS Mental Illness - Eating Disorders, Depression Other - AIDS/HIV, Kidney/Liver Disease, COPD
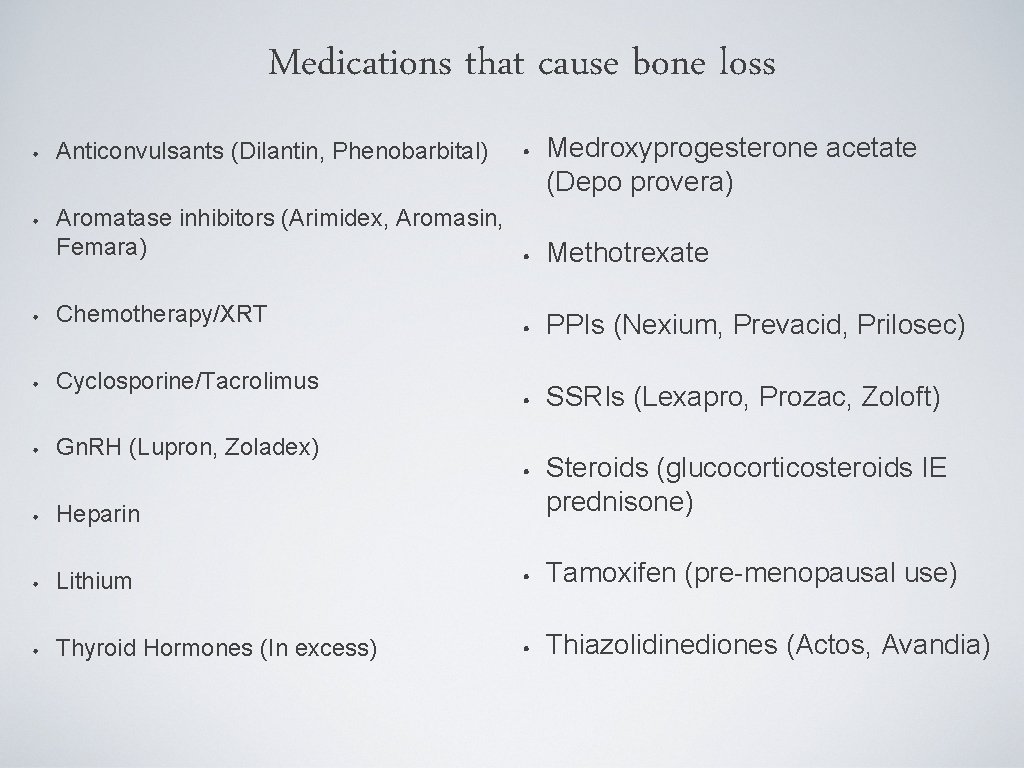
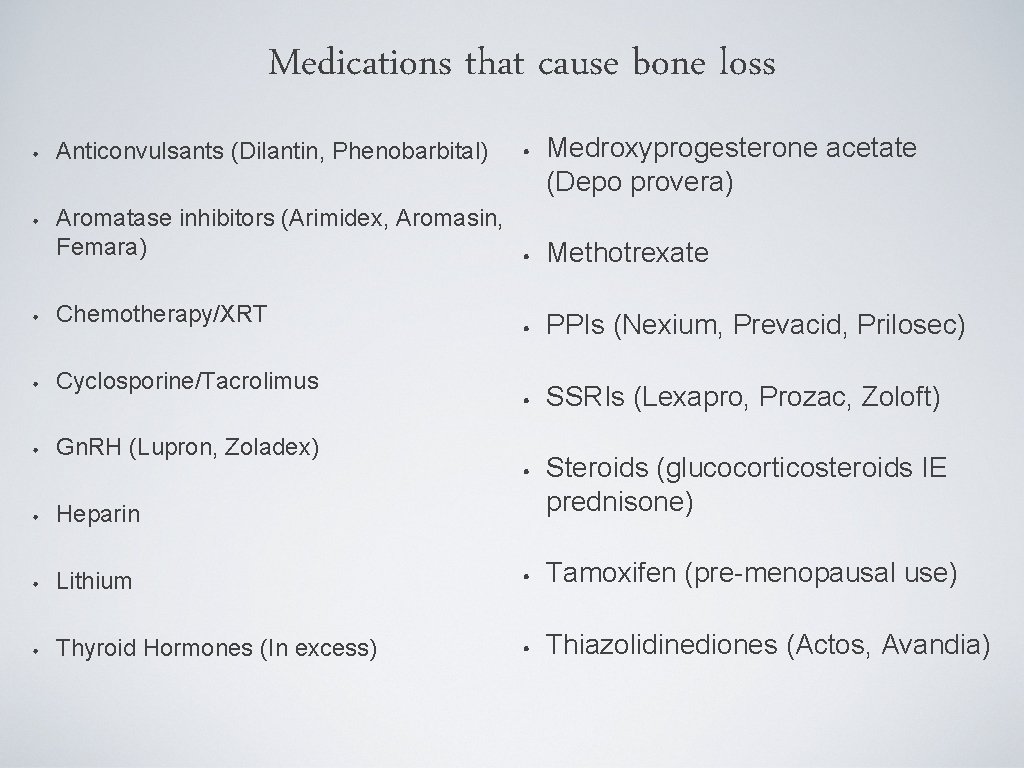
Medications that cause bone loss Medroxyprogesterone acetate (Depo provera) • Anticonvulsants (Dilantin, Phenobarbital) • Aromatase inhibitors (Arimidex, Aromasin, Femara) • Methotrexate • Chemotherapy/XRT • Cyclosporine/Tacrolimus • Gn. RH (Lupron, Zoladex) • Heparin • • PPIs (Nexium, Prevacid, Prilosec) • SSRIs (Lexapro, Prozac, Zoloft) • Steroids (glucocorticosteroids IE prednisone) Lithium • Tamoxifen (pre-menopausal use) Thyroid Hormones (In excess) • Thiazolidinediones (Actos, Avandia)
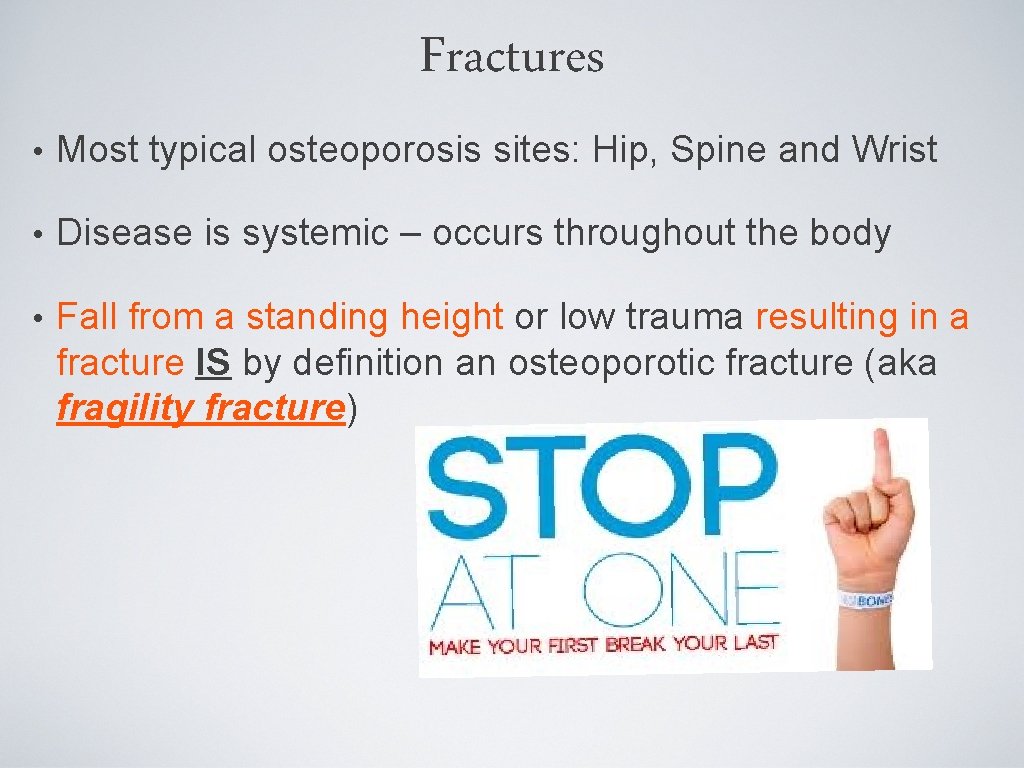
Fractures • Most typical osteoporosis sites: Hip, Spine and Wrist • Disease is systemic – occurs throughout the body • Fall from a standing height or low trauma resulting in a fracture IS by definition an osteoporotic fracture (aka fragility fracture)
Prevention • Balanced diet of calcium and vitamin D • Regular weight bearing and muscle strengthening exercise • Healthy lifestyle, avoid excess alcohol, caffeine, soda • Bone density testing and medication when appropriate • Fall prevention
Detection • DXA or bone density scan can: • Detect osteoporosis before a fracture occurs • Predict your chances of fracturing in the future • Determine your rate of bone loss and/or monitor the effects of treatment if the test is conducted at intervals of a year or more • Paid for by Medicare every two years
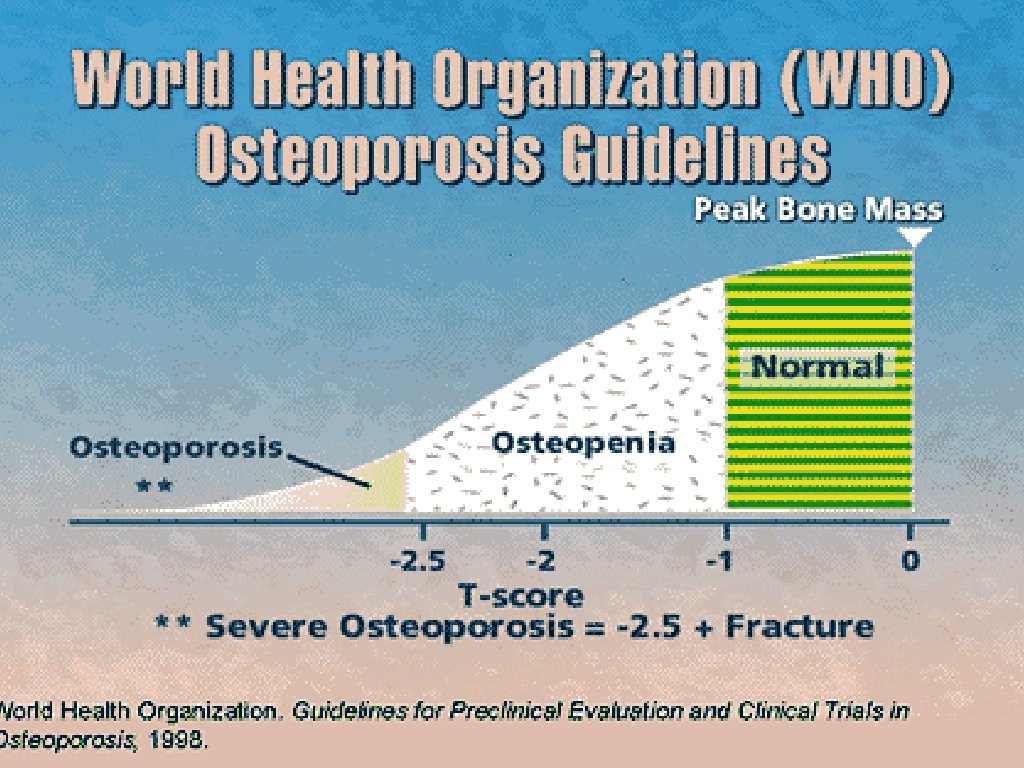
Diagnosis • Central dual-energy DXA (GOLD STANDARD) • In the absence of a fracture, T-score > -2. 5 in the spine, femoral neck or total hip. • Fracture of the hip or spine • AACE American Association of Clinical Endocrinologists) Guidelines for Diagnosis and Treatment of Osteoporosis 2010
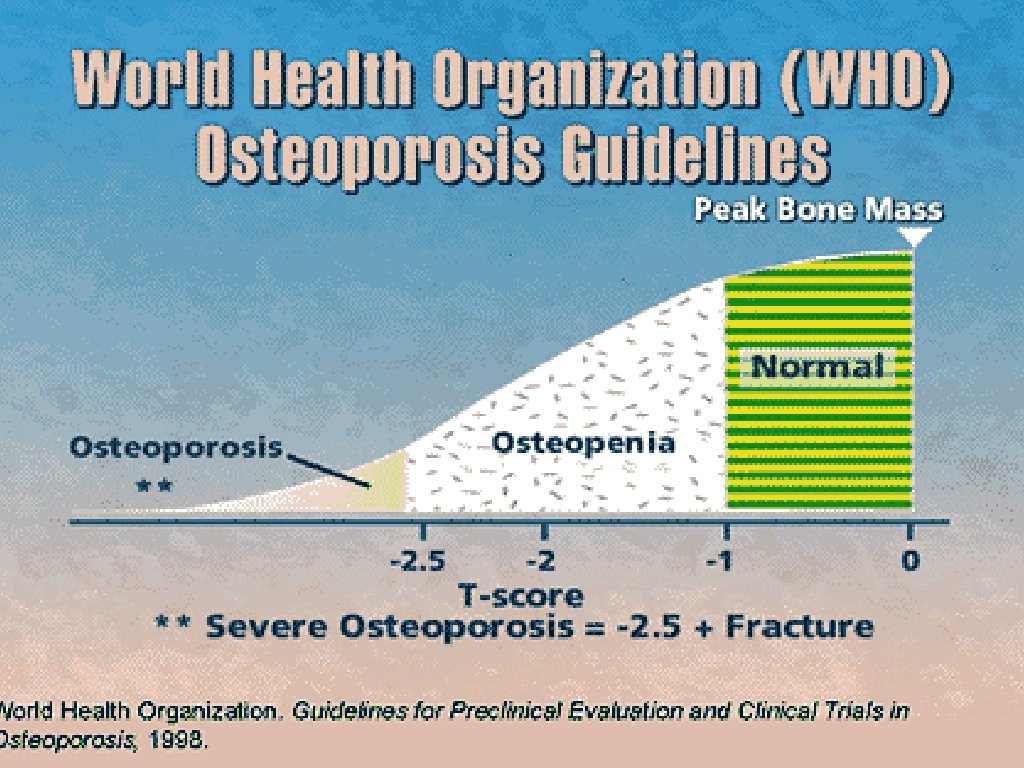
Limitations of World Health Organization Definition • Established in post-menopausal osteoporosis • Does not recognize fragility fractures and therefore may have a “normal result” in patients with osteoporotic fractures • Only for central DXA and forearm • REMEMBER: This is a SCREENING TOOL!! It is in conjunction with clinical information and judgement
Alternative Tools: Peripheral DXA Should NOT be used for monitoring patient’s response to therapy Ease and availability Often used as a screening tool
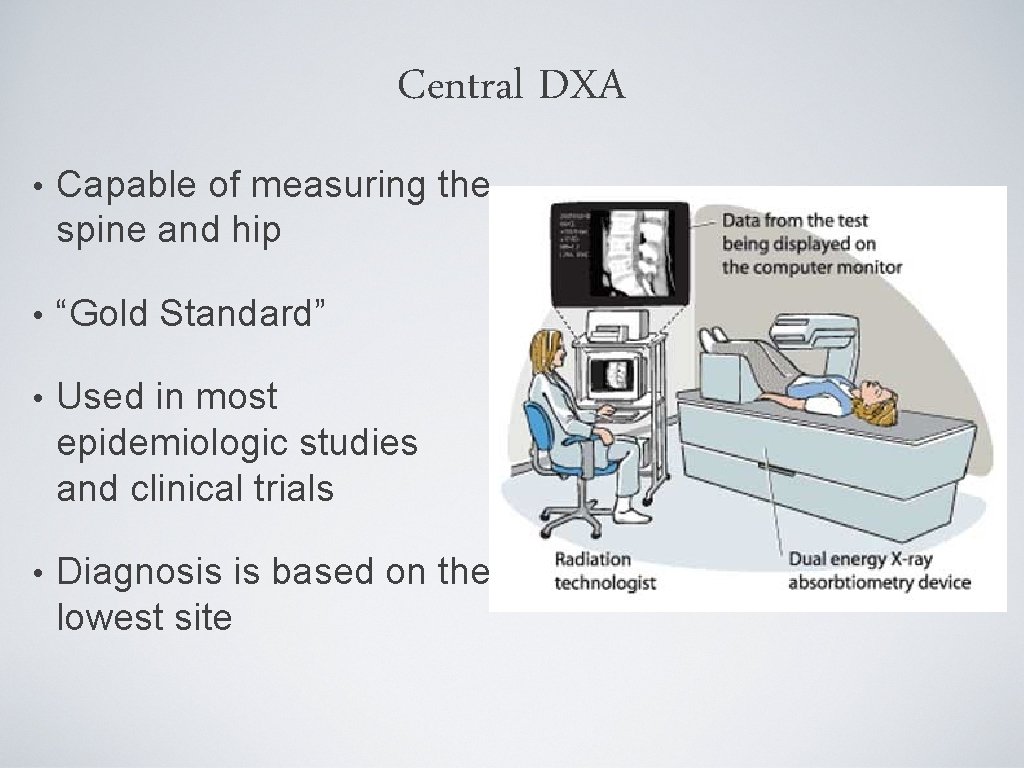
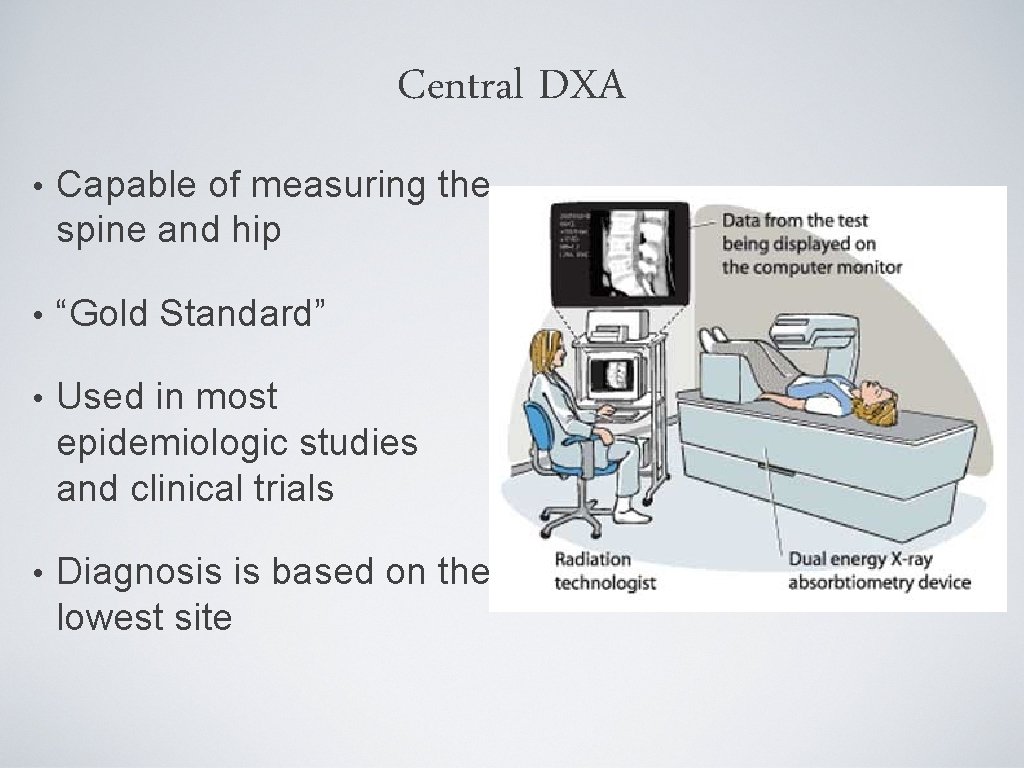
Central DXA • Capable of measuring the spine and hip • “Gold Standard” • Used in most epidemiologic studies and clinical trials • Diagnosis is based on the lowest site
Contraindications for central DXA • Pregnancy • Recent contrast study or nuclear medicine scan (wait 72 hours) • Calcium supplements taken day of the study • Extensive orthopaedic instrumentation • Severe obesity
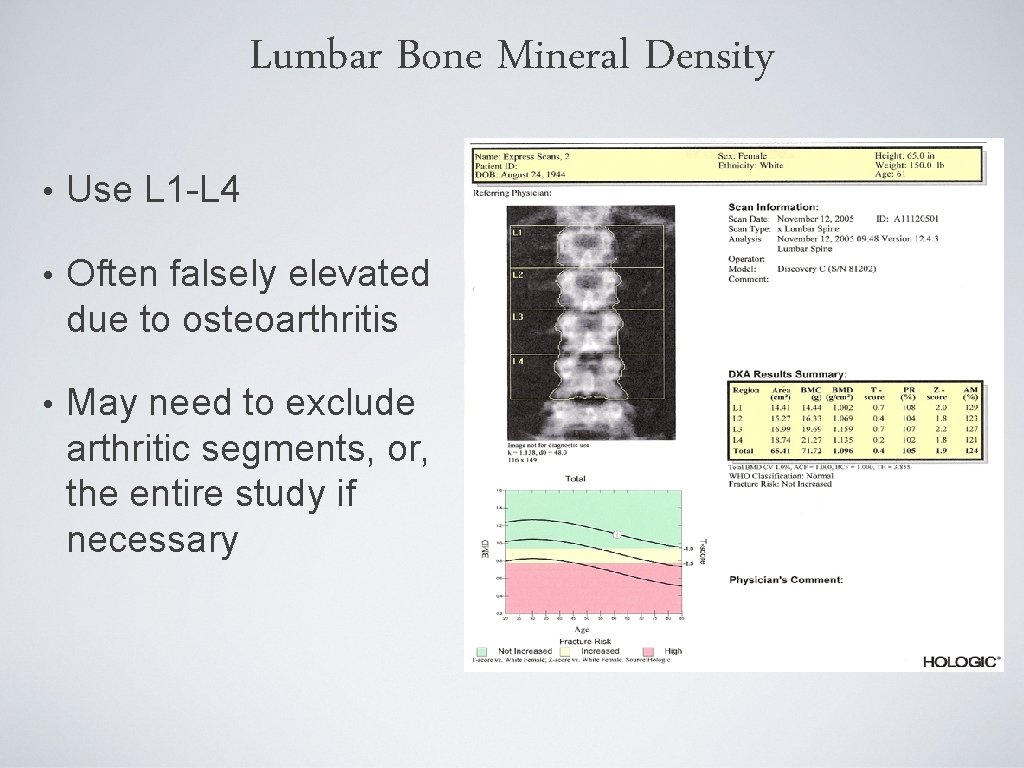
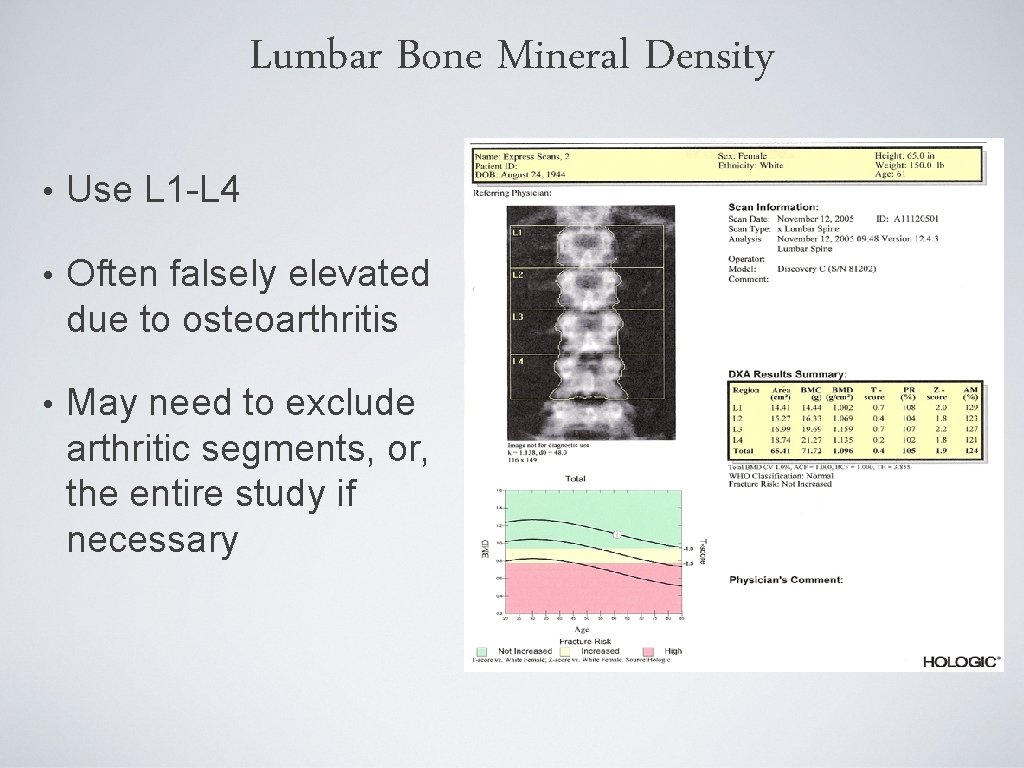
Lumbar Bone Mineral Density • Use L 1 -L 4 • Often falsely elevated due to osteoarthritis • May need to exclude arthritic segments, or, the entire study if necessary
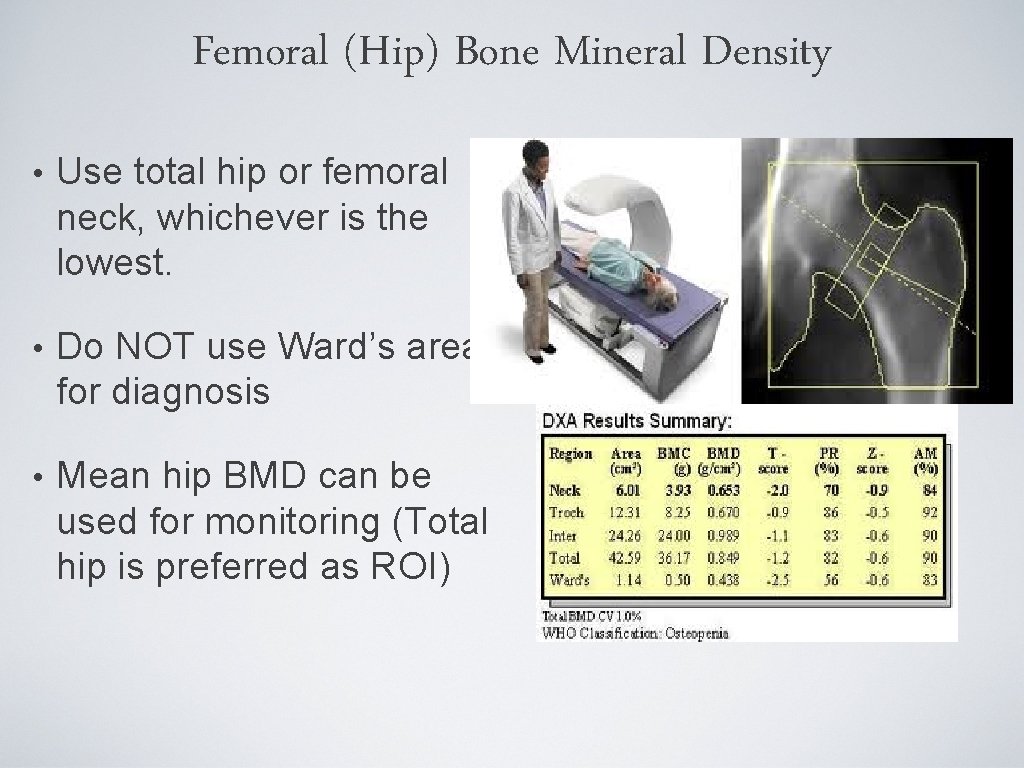
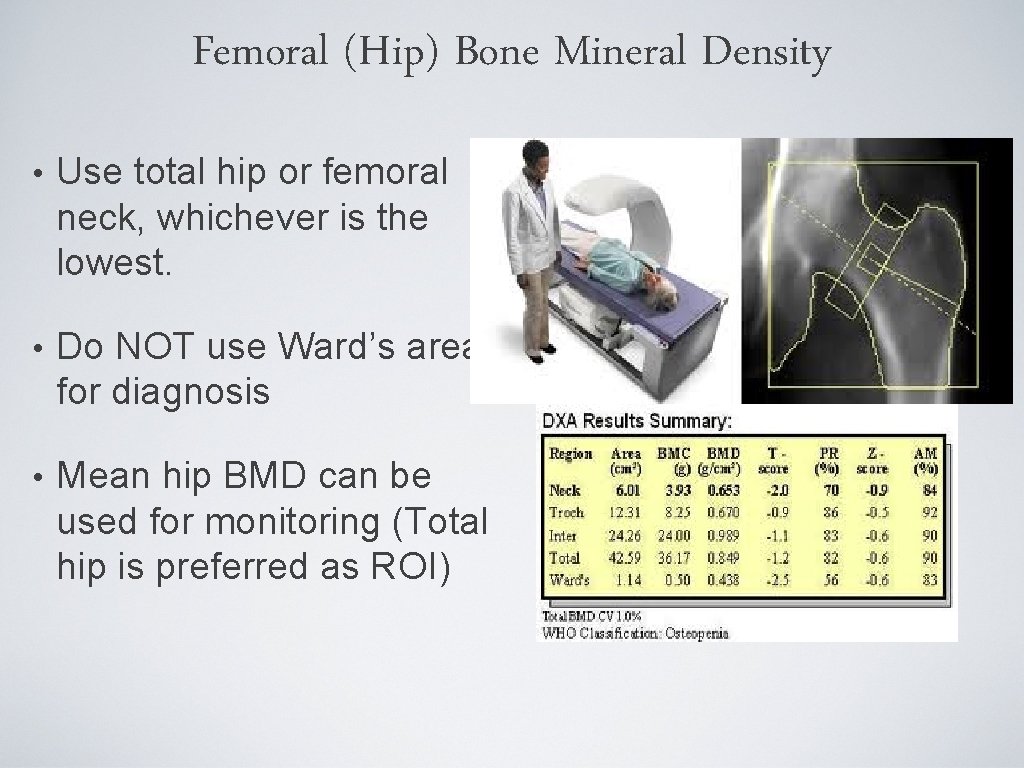
Femoral (Hip) Bone Mineral Density • Use total hip or femoral neck, whichever is the lowest. • Do NOT use Ward’s area for diagnosis • Mean hip BMD can be used for monitoring (Total hip is preferred as ROI)
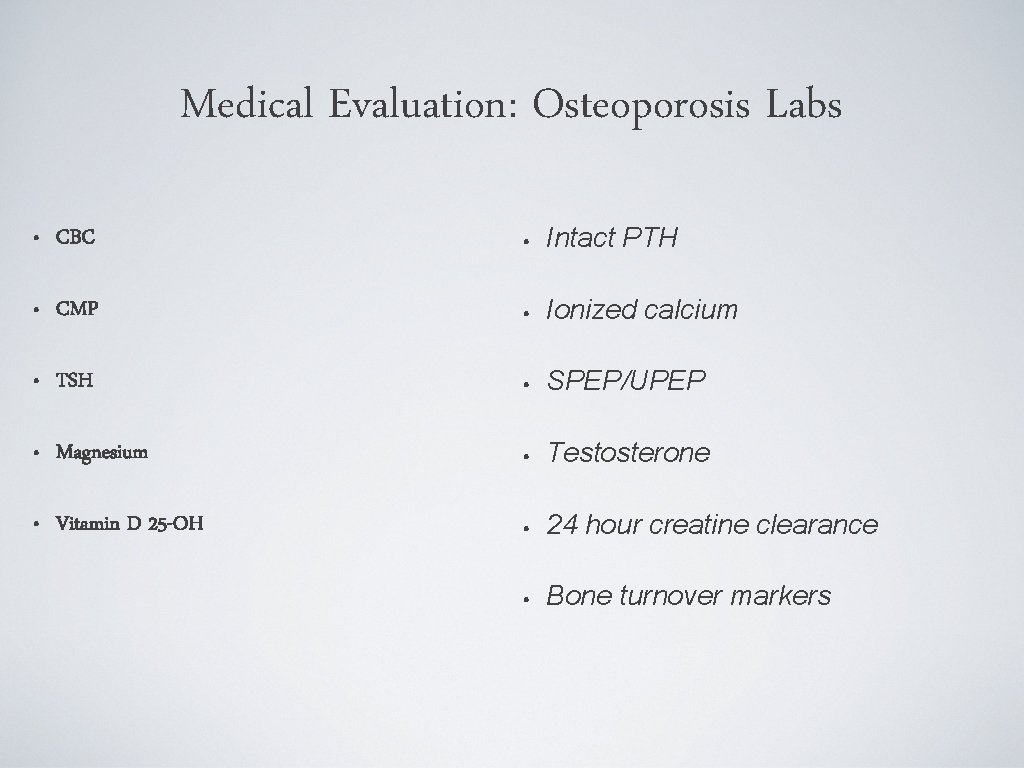
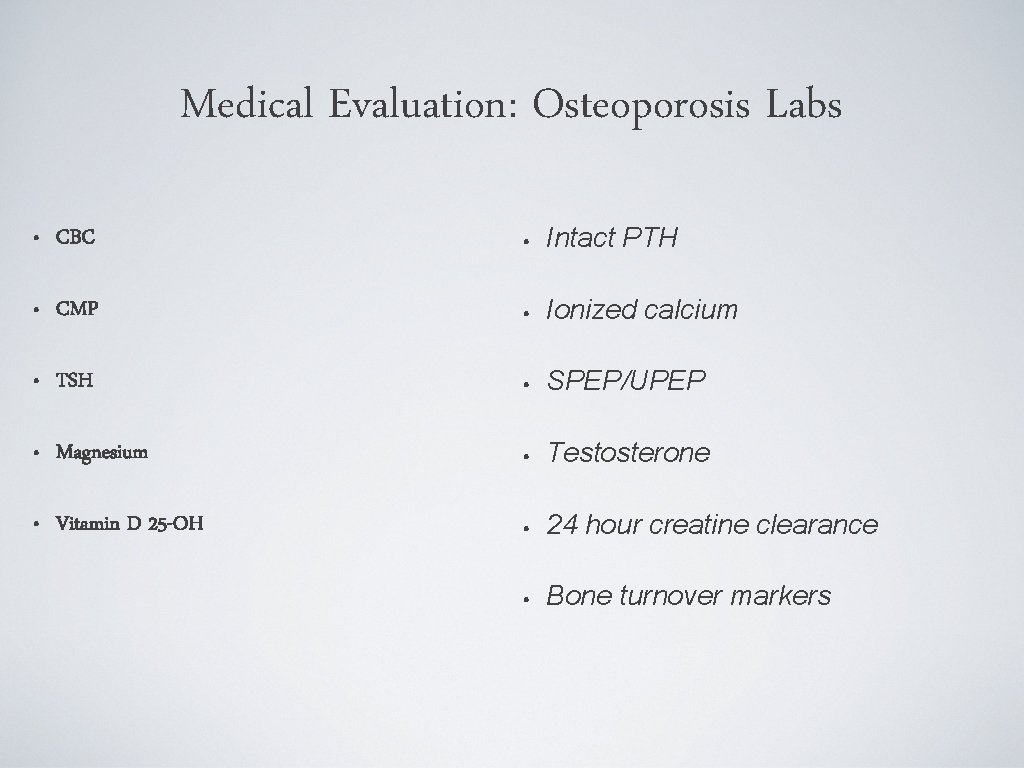
Medical Evaluation: Osteoporosis Labs • CBC • Intact PTH • CMP • Ionized calcium • TSH • SPEP/UPEP • Magnesium • Testosterone • Vitamin D 25 -OH • 24 hour creatine clearance • Bone turnover markers
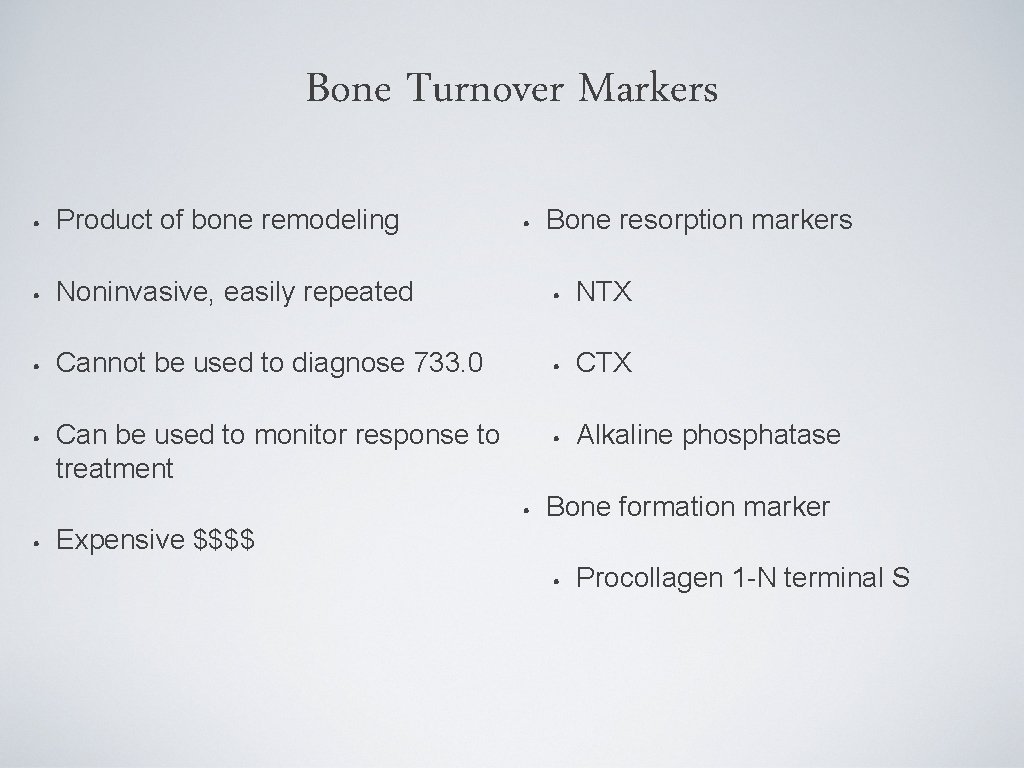
Bone Turnover Markers • Product of bone remodeling • Noninvasive, easily repeated • NTX • Cannot be used to diagnose 733. 0 • CTX • Can be used to monitor response to treatment • Alkaline phosphatase • Expensive $$$$ • • Bone resorption markers Bone formation marker • Procollagen 1 -N terminal S
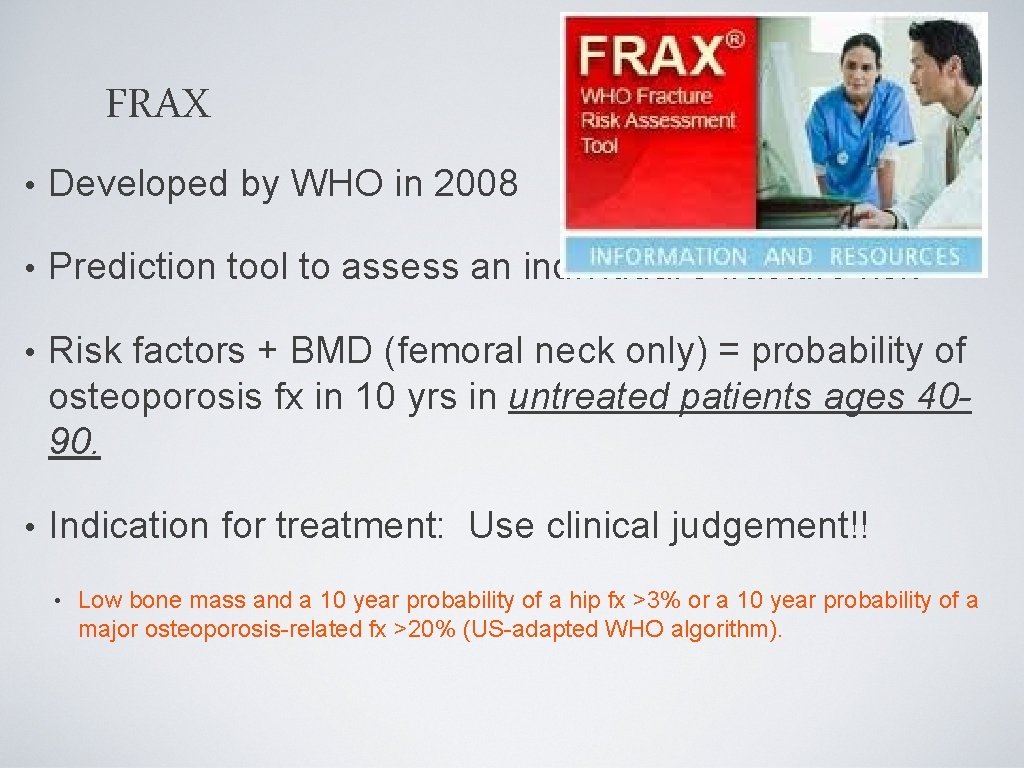
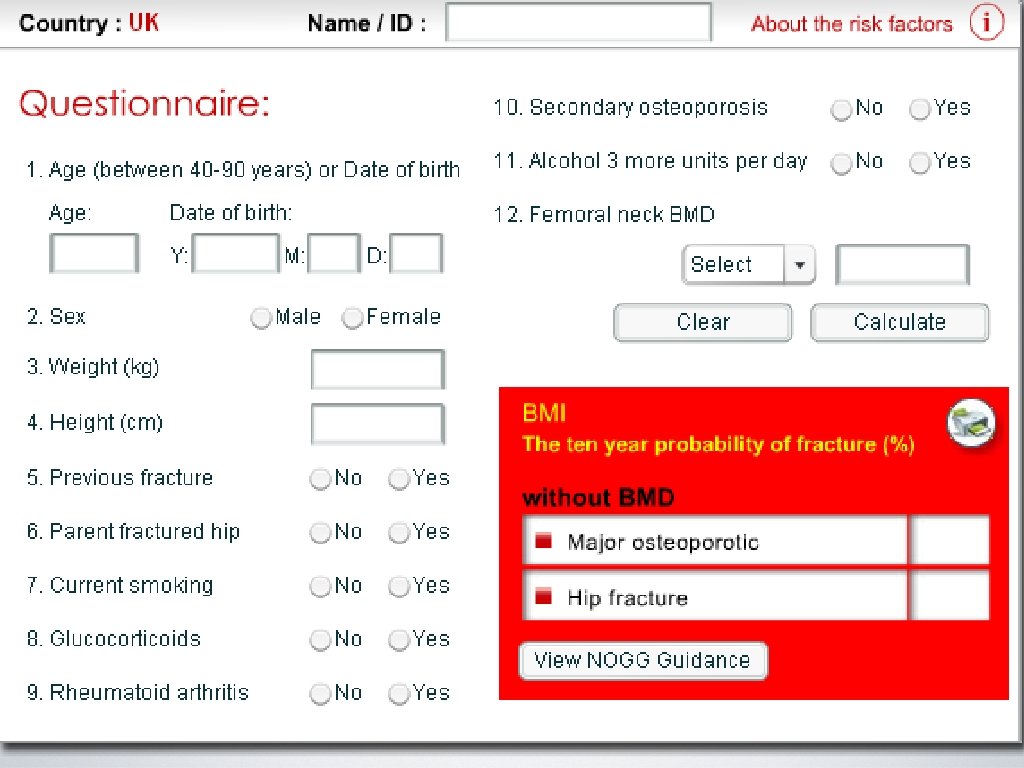
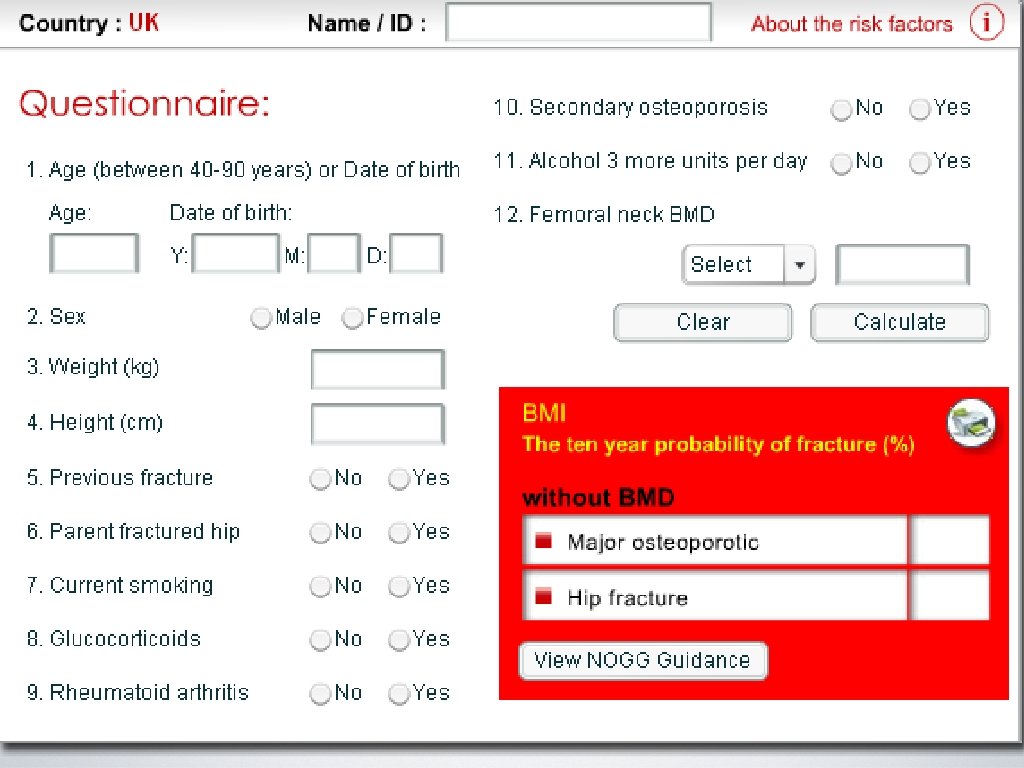
FRAX • Developed by WHO in 2008 • Prediction tool to assess an individual’s fracture risk • Risk factors + BMD (femoral neck only) = probability of osteoporosis fx in 10 yrs in untreated patients ages 4090. • Indication for treatment: Use clinical judgement!! • Low bone mass and a 10 year probability of a hip fx >3% or a 10 year probability of a major osteoporosis-related fx >20% (US-adapted WHO algorithm).
Osteoporosis Tools: DXA, labs, FRAX, clinical judgement
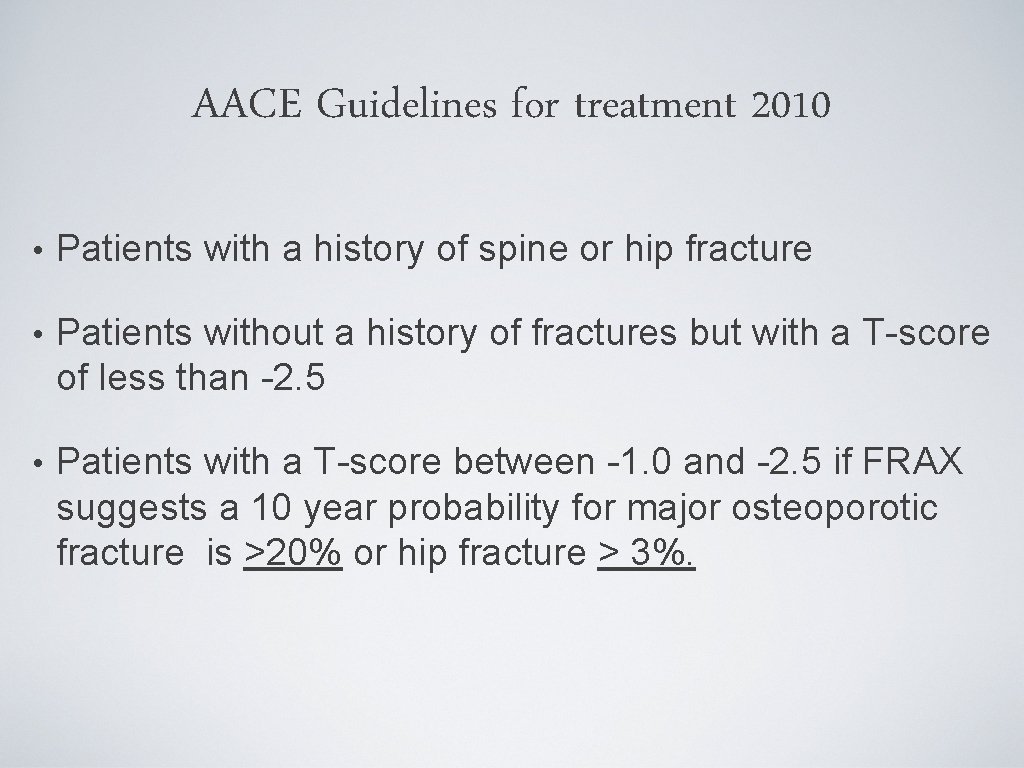
AACE Guidelines for treatment 2010 • Patients with a history of spine or hip fracture • Patients without a history of fractures but with a T-score of less than -2. 5 • Patients with a T-score between -1. 0 and -2. 5 if FRAX suggests a 10 year probability for major osteoporotic fracture is >20% or hip fracture > 3%.
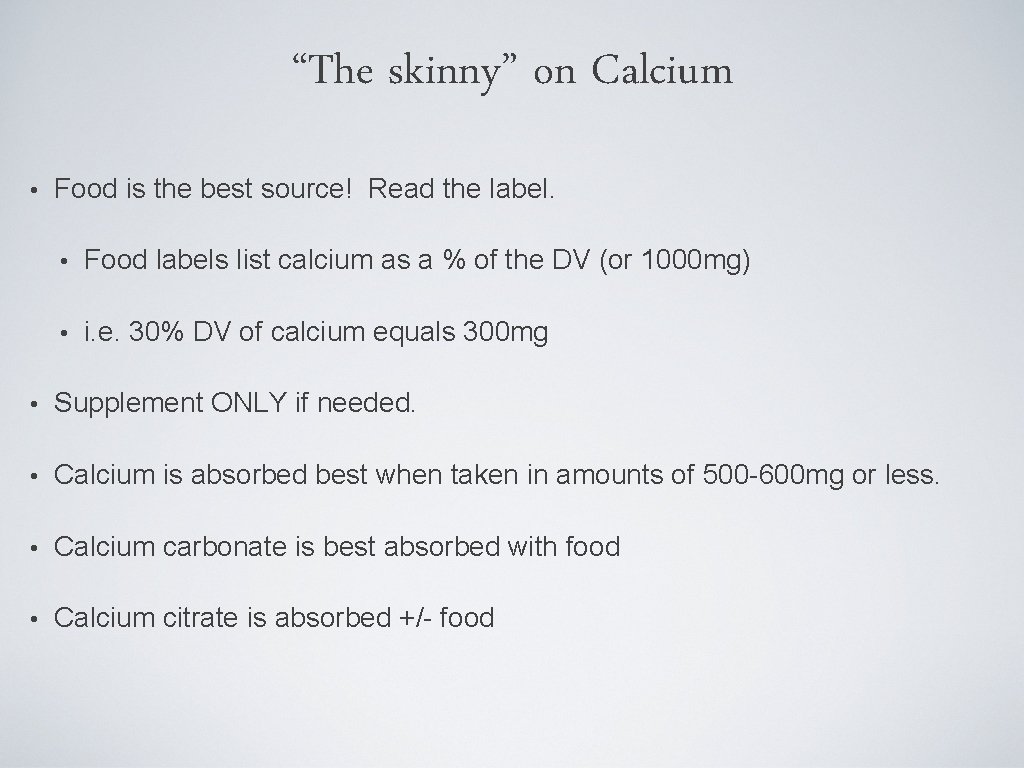
“The skinny” on Calcium • Food is the best source! Read the label. • Food labels list calcium as a % of the DV (or 1000 mg) • i. e. 30% DV of calcium equals 300 mg • Supplement ONLY if needed. • Calcium is absorbed best when taken in amounts of 500 -600 mg or less. • Calcium carbonate is best absorbed with food • Calcium citrate is absorbed +/- food
The Sunshine Vitamin: Vitamin D • 3 Sources: Sunlight, Food, Supplements • Promotes calcium absorption • Maintains serum Ca and PO 4 (bone mineralization) • Needed for bone growth and remodeling
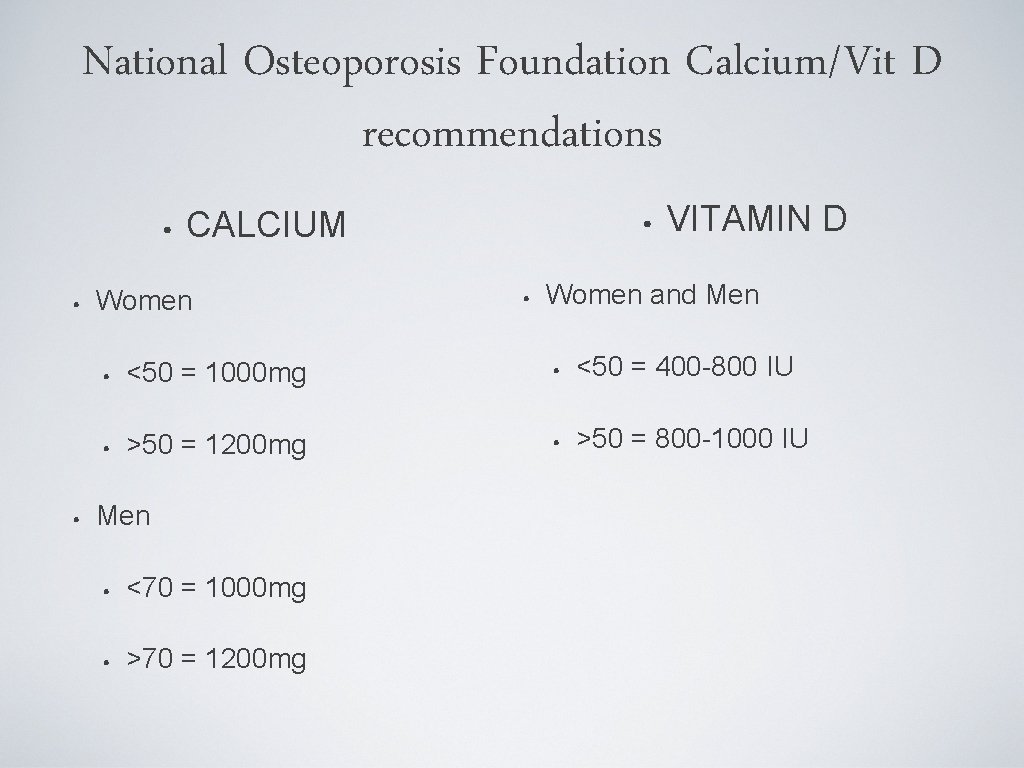
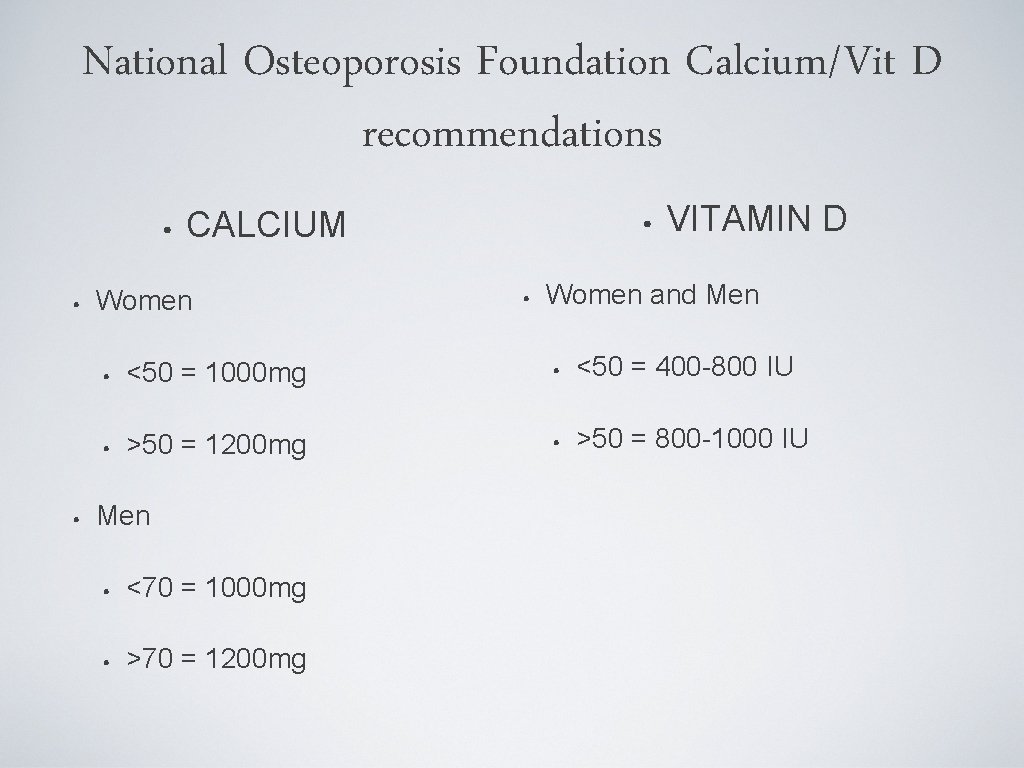
National Osteoporosis Foundation Calcium/Vit D recommendations • • • CALCIUM Women • • VITAMIN D Women and Men • <50 = 1000 mg • <50 = 400 -800 IU • >50 = 1200 mg • >50 = 800 -1000 IU Men • <70 = 1000 mg • >70 = 1200 mg
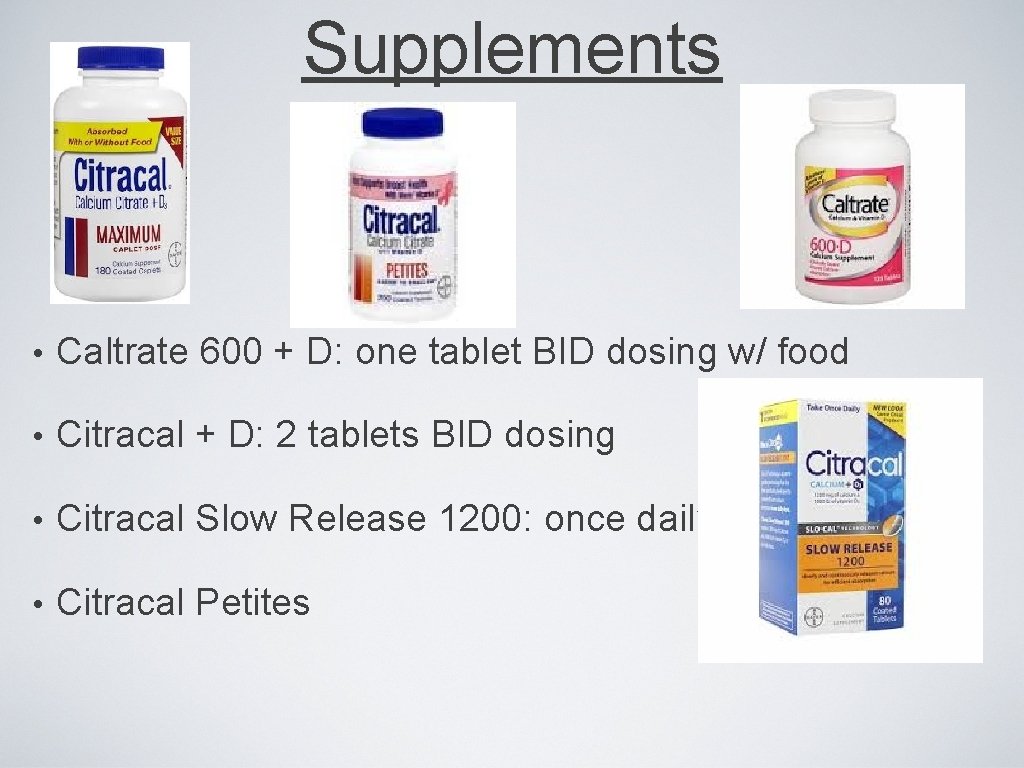
Supplements • Caltrate 600 + D: one tablet BID dosing w/ food • Citracal + D: 2 tablets BID dosing • Citracal Slow Release 1200: once daily • Citracal Petites
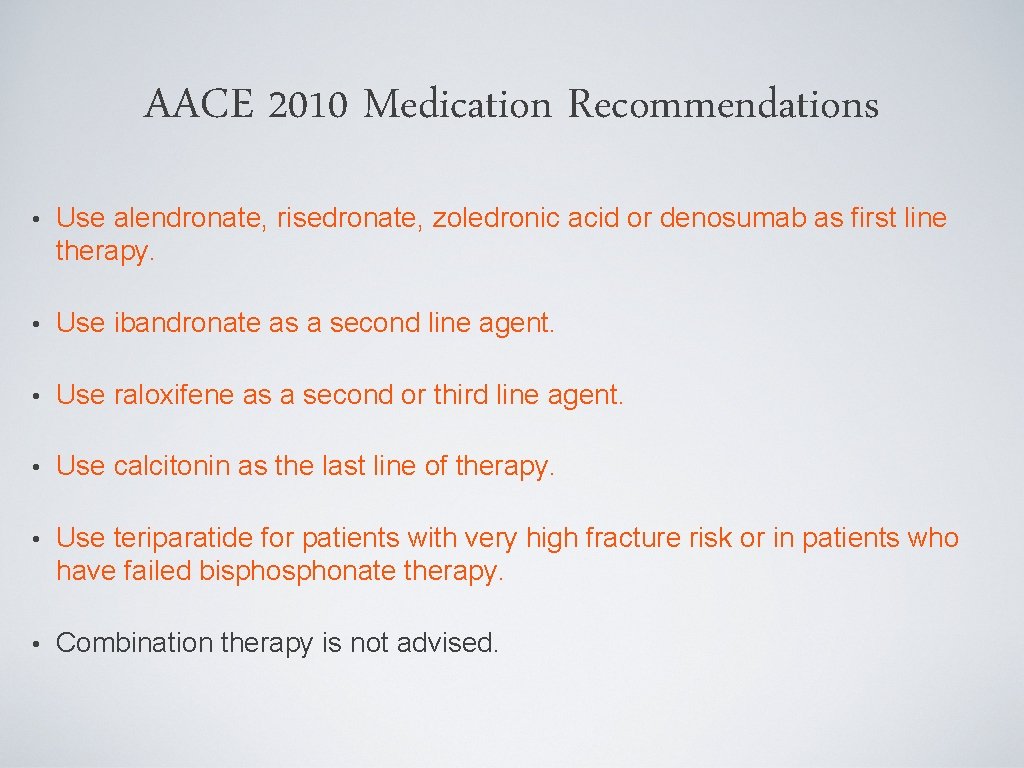
AACE 2010 Medication Recommendations • Use alendronate, risedronate, zoledronic acid or denosumab as first line therapy. • Use ibandronate as a second line agent. • Use raloxifene as a second or third line agent. • Use calcitonin as the last line of therapy. • Use teriparatide for patients with very high fracture risk or in patients who have failed bisphonate therapy. • Combination therapy is not advised.
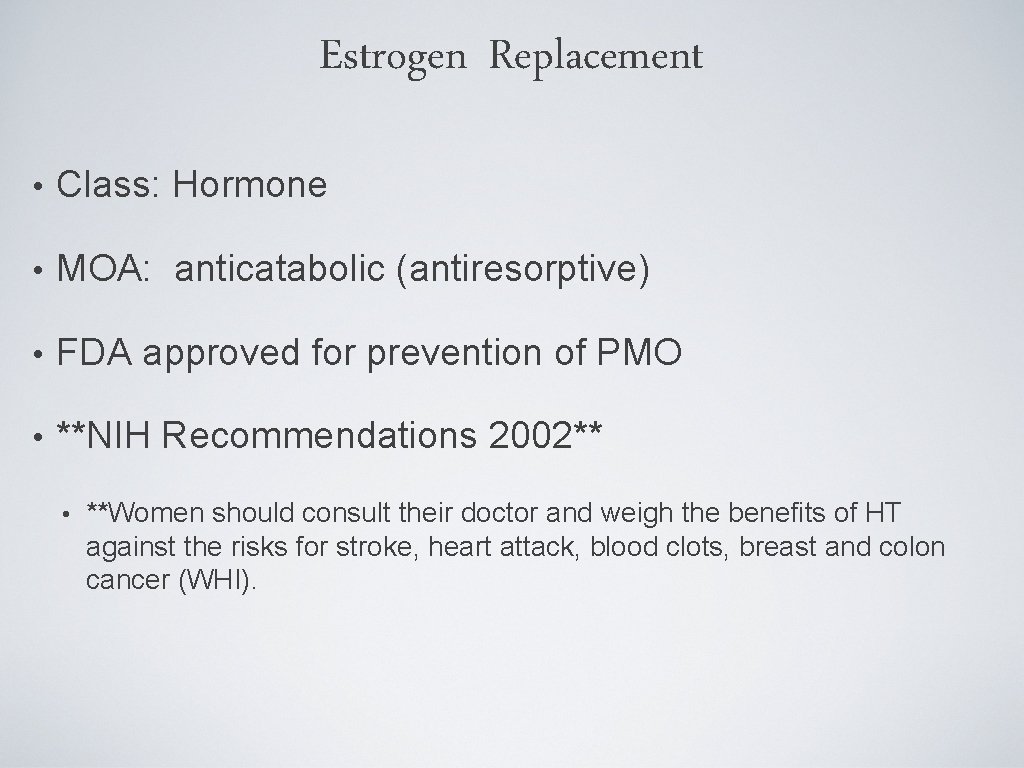
Estrogen Replacement • Class: Hormone • MOA: anticatabolic (antiresorptive) • FDA approved for prevention of PMO • **NIH Recommendations 2002** • **Women should consult their doctor and weigh the benefits of HT against the risks for stroke, heart attack, blood clots, breast and colon cancer (WHI).
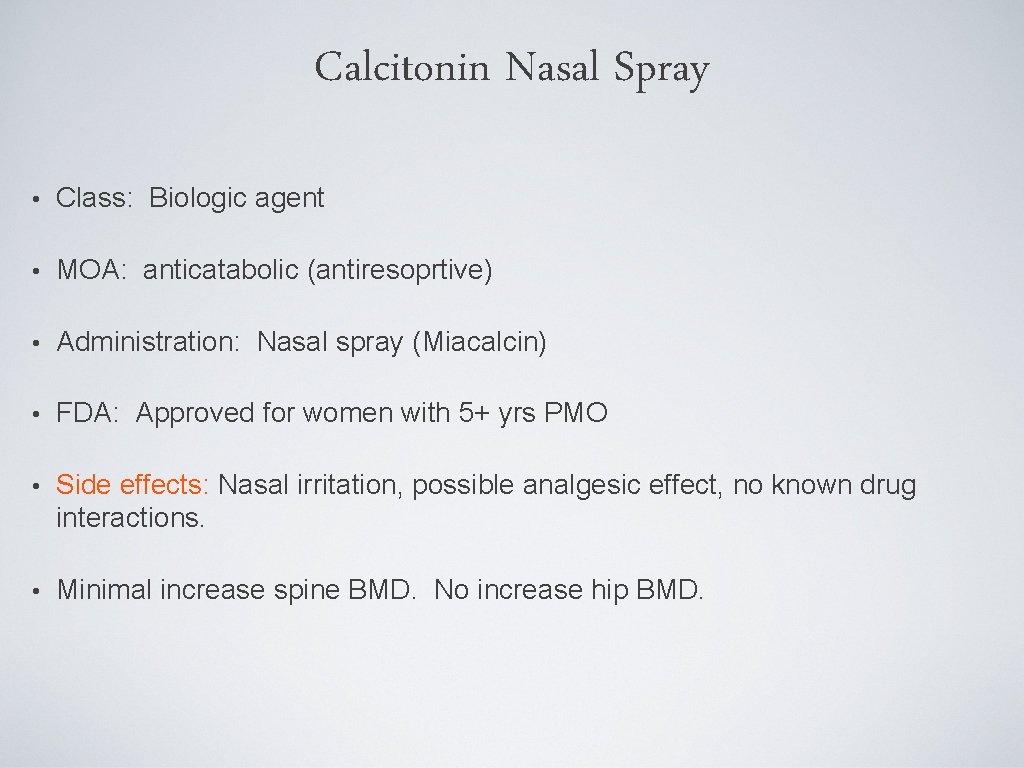
Calcitonin Nasal Spray • Class: Biologic agent • MOA: anticatabolic (antiresoprtive) • Administration: Nasal spray (Miacalcin) • FDA: Approved for women with 5+ yrs PMO • Side effects: Nasal irritation, possible analgesic effect, no known drug interactions. • Minimal increase spine BMD. No increase hip BMD.
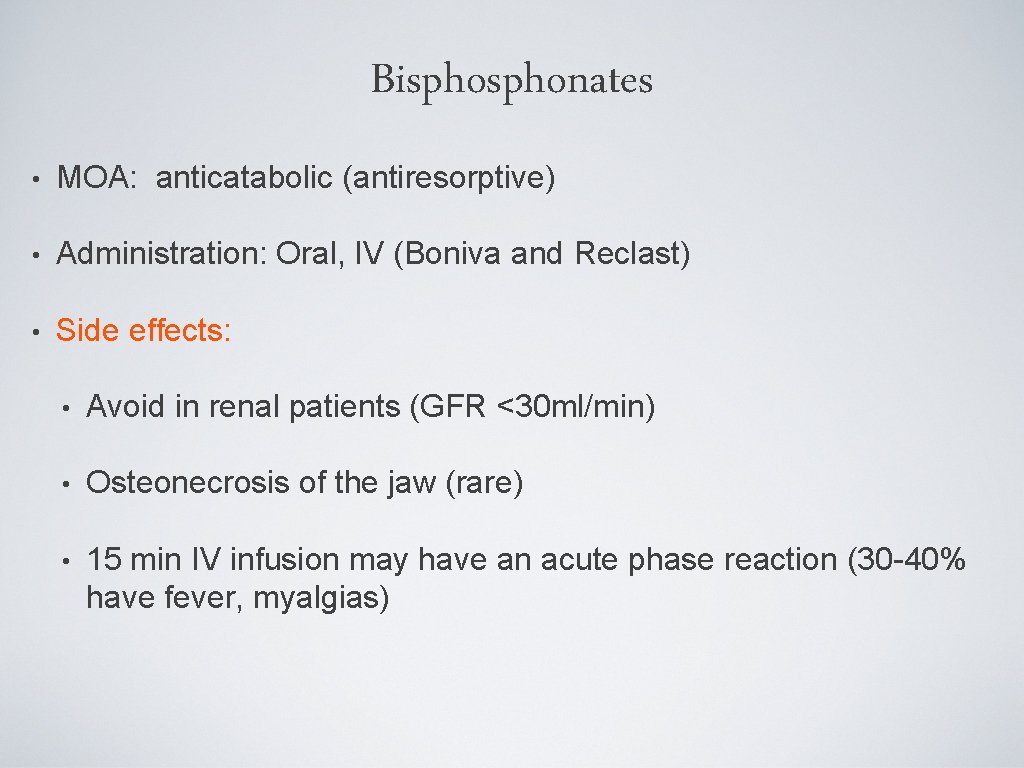
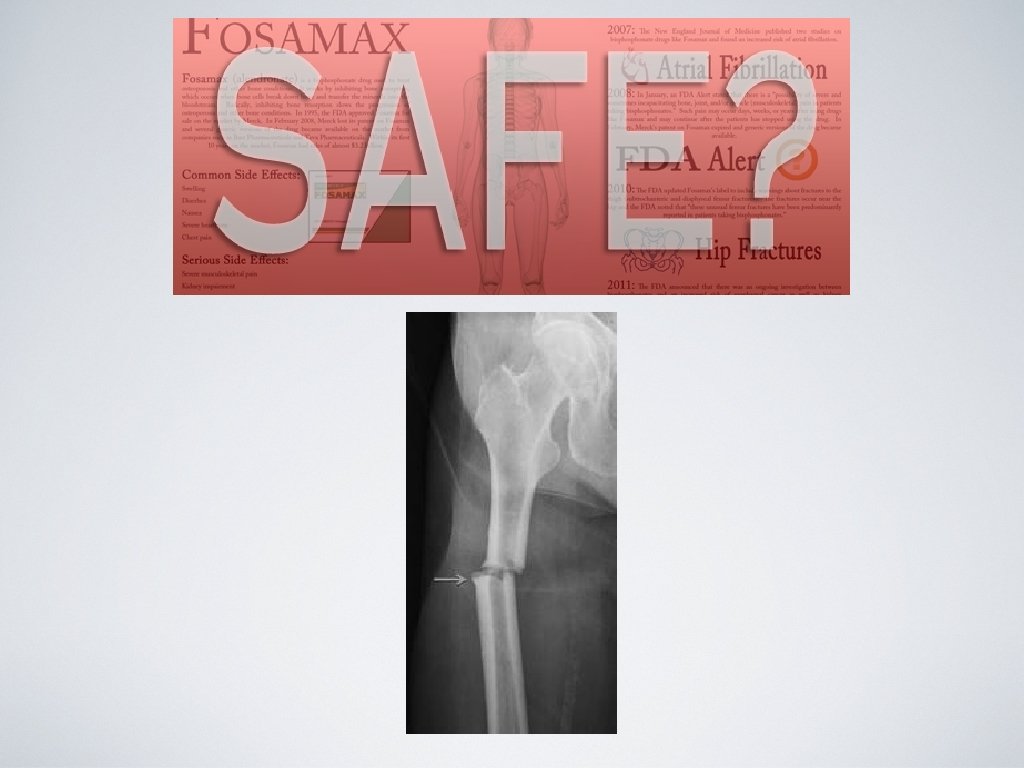
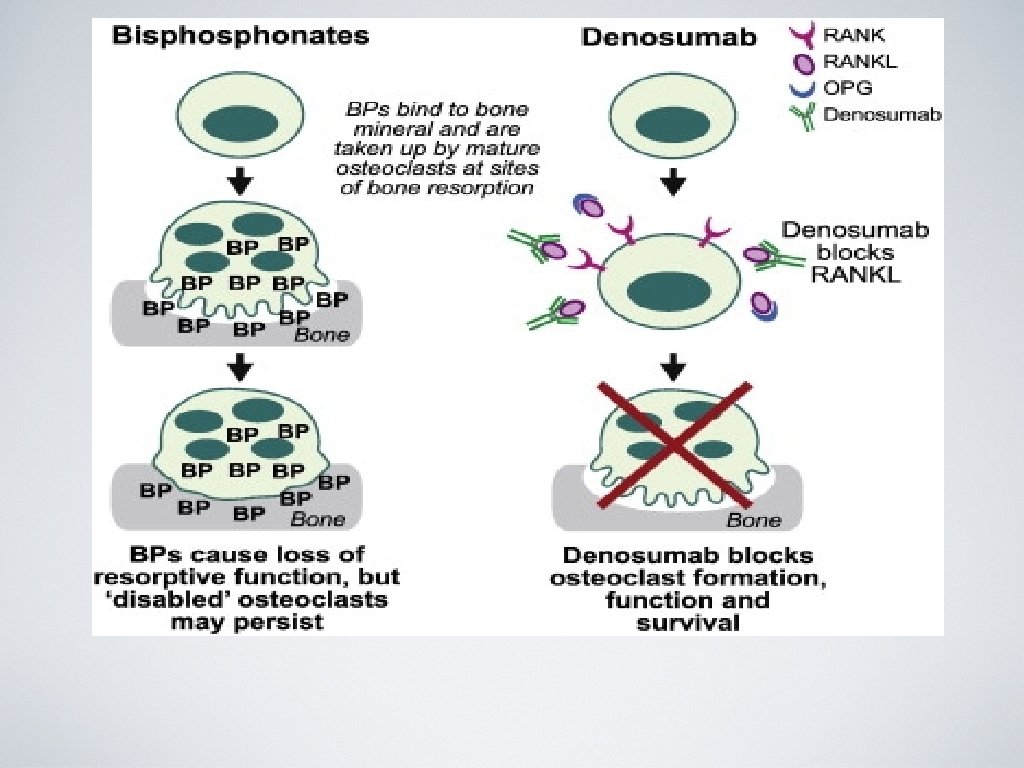
Bisphonates • MOA: anticatabolic (antiresorptive) • Administration: Oral, IV (Boniva and Reclast) • Side effects: • Avoid in renal patients (GFR <30 ml/min) • Osteonecrosis of the jaw (rare) • 15 min IV infusion may have an acute phase reaction (30 -40% have fever, myalgias)
Bisphonates • Fosamax (Alendronate) • Actonel (Risedronate) • Boniva (Ibandronate) • Reclast (Zolendronic Acid)
AACE Stance on Bisphonates 2010 • Consider a drug holiday after 4 -5 years of stability on bisphonate therapy. • Follow BMD and bone turnover markers during a drug holiday. • Reinitiate therapy if bone declines sustantially, bone turnover markers increase or fracture occurs.
Evista (Raloxifene) • Class: SERM (selective estrogen receptor modulator) • MOA: anticatabolic (antiresorptive) • FDA approved for prevention and tx of PMO • FDA approved as an agent to reduce breast cancer • Reduces spine fractures **hip and non vertebral fractures not proven** (2 nd or 3 rd line agent) • Side effects: Increased risk of DVT, does not alleviate hot flashes
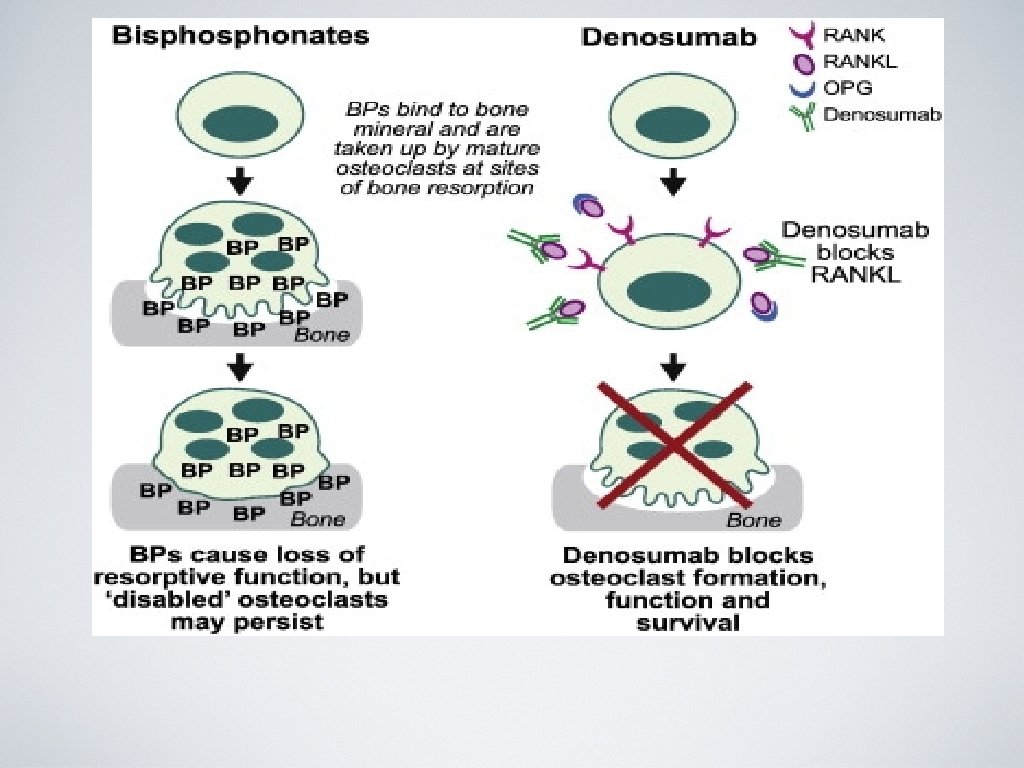
PROLIA (denosumab) • Class: anticatabolic (antiresorptive) • MOA: RANK ligand inhibitor • Administration: 60 mg SQ every 6 months • FDA approved for prevention and tx of osteoporosis in PMO and osteoporosis tx in men. • Good option in pts who have failed or are intolerant to other available osteoporosis therapy • Side effects: hypocalcemia, infection, dermatologic rxn, ONJ
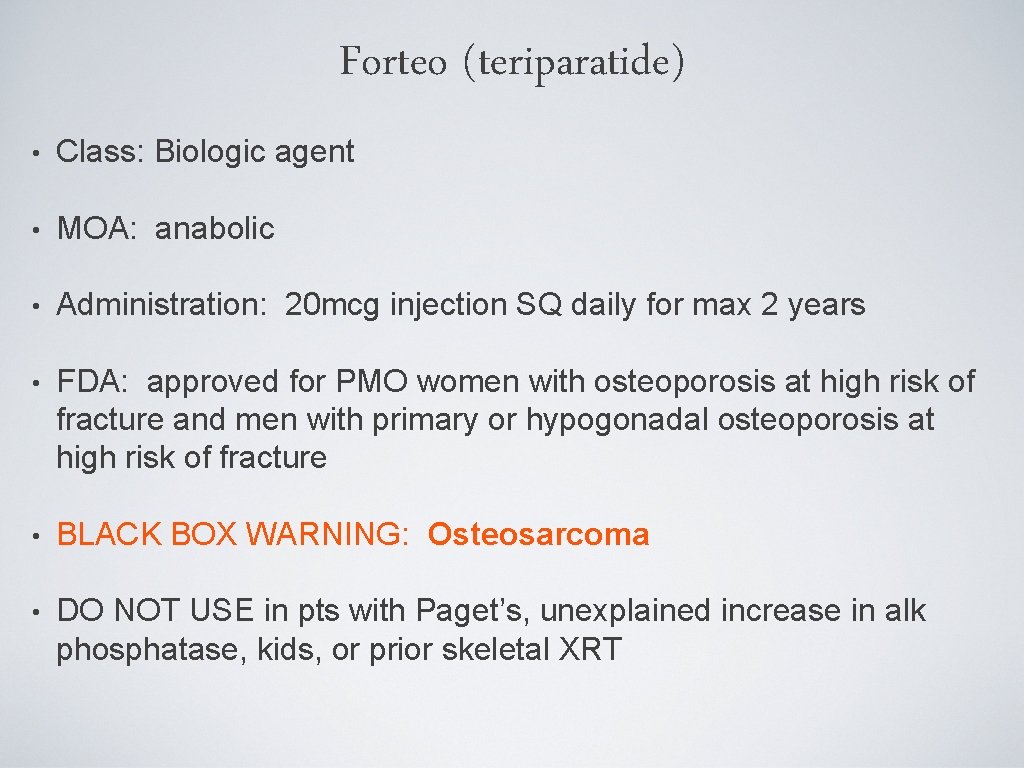
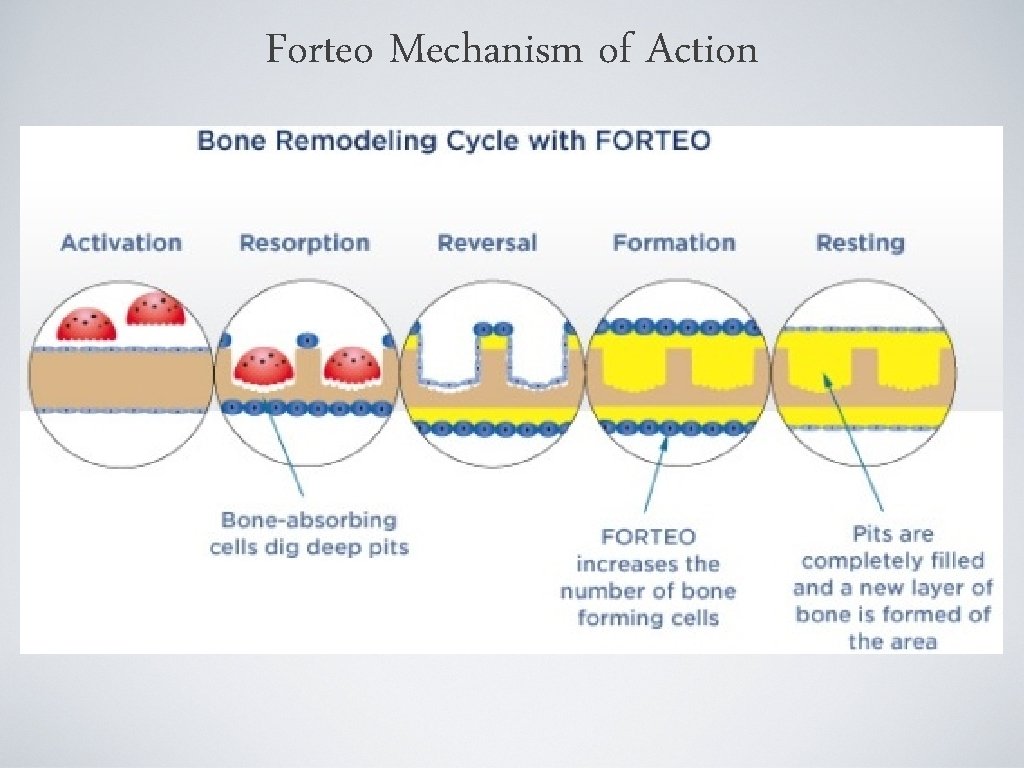
Forteo (teriparatide) • Class: Biologic agent • MOA: anabolic • Administration: 20 mcg injection SQ daily for max 2 years • FDA: approved for PMO women with osteoporosis at high risk of fracture and men with primary or hypogonadal osteoporosis at high risk of fracture • BLACK BOX WARNING: Osteosarcoma • DO NOT USE in pts with Paget’s, unexplained increase in alk phosphatase, kids, or prior skeletal XRT
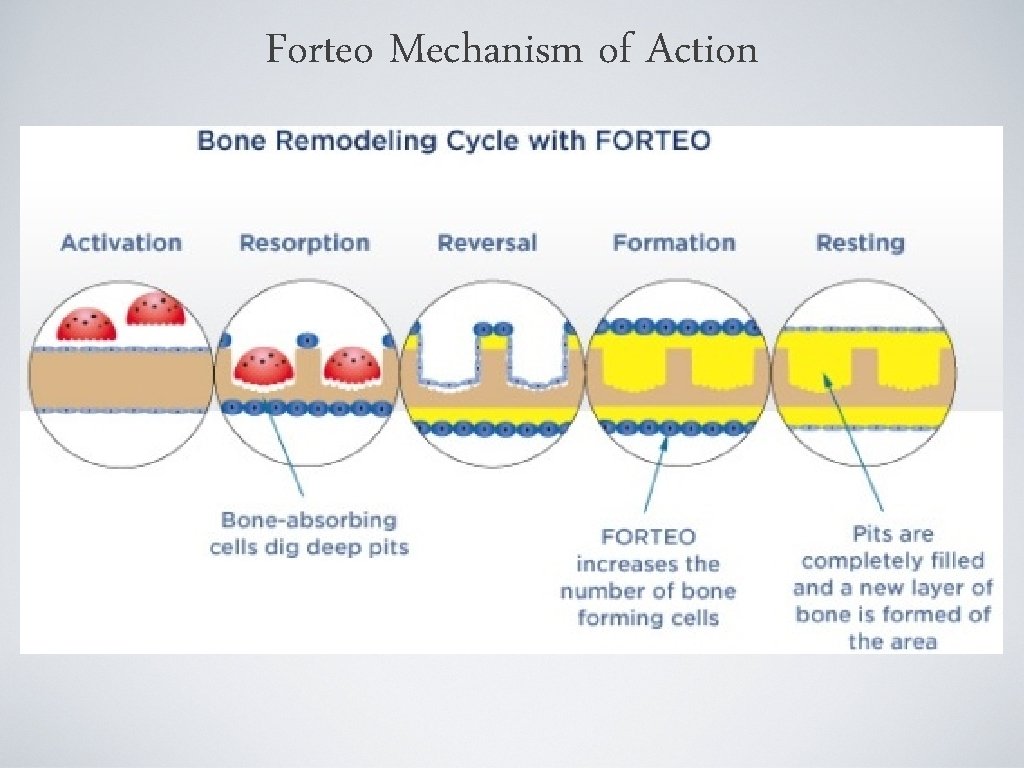
Forteo Mechanism of Action
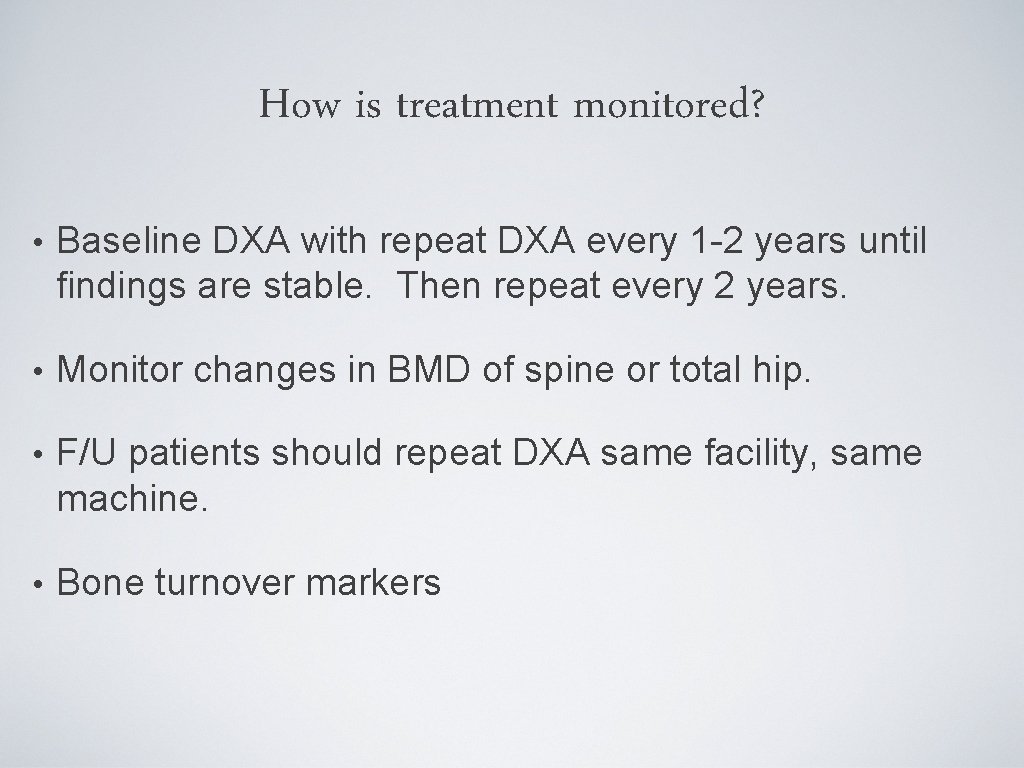
How is treatment monitored? • Baseline DXA with repeat DXA every 1 -2 years until findings are stable. Then repeat every 2 years. • Monitor changes in BMD of spine or total hip. • F/U patients should repeat DXA same facility, same machine. • Bone turnover markers
Defining successful treatment • BMD is stable or increasing and no fractures are present. • For patients on antiresorptive agents, bone turnover markers at or below the median value. • One fracture is NOT a sign of failure!! Consider alternate therapy, compliance, and reassess.
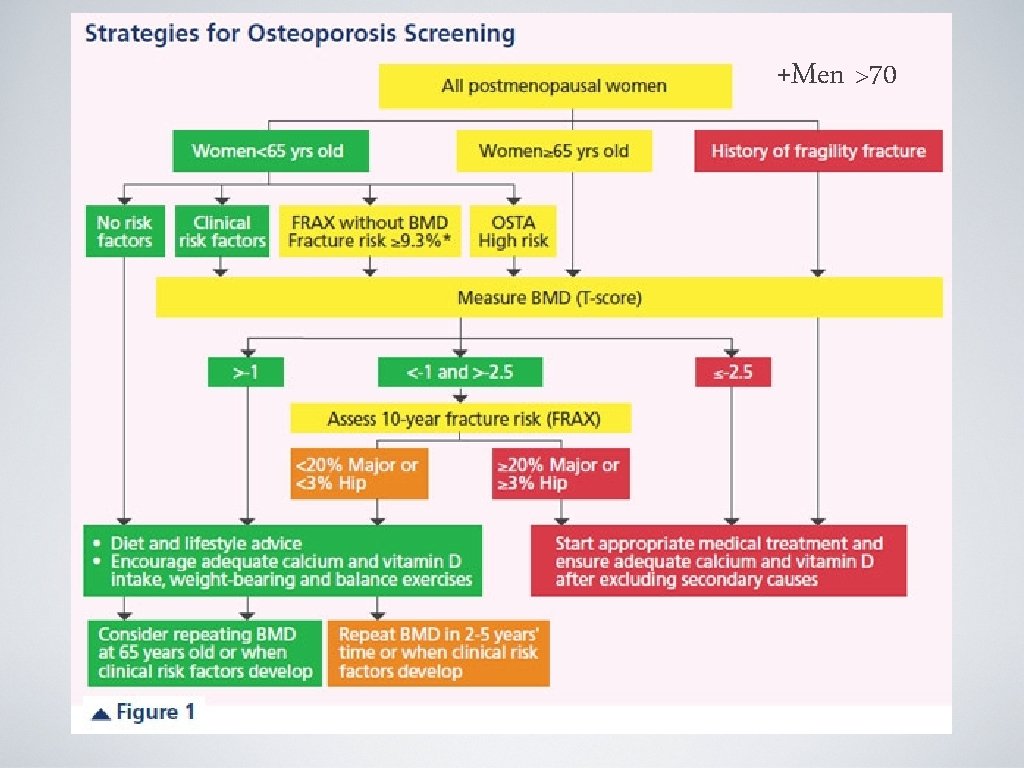
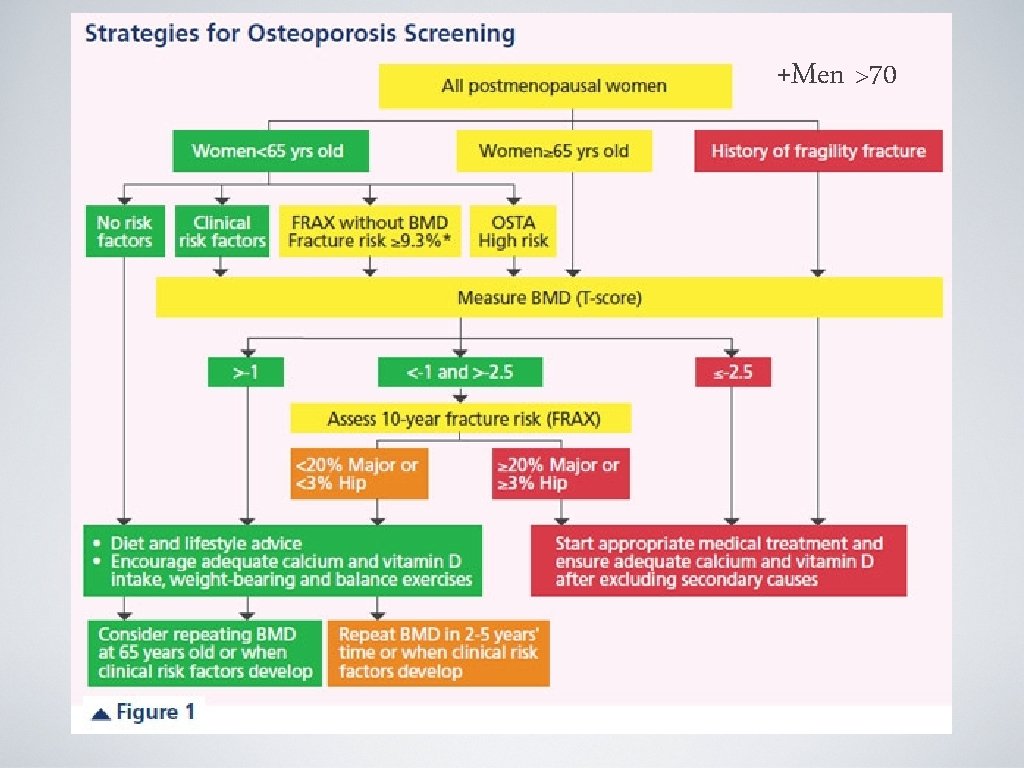
+Men >70
When to see the Bone Expert • Patient with normal BMD sustains a fracture without trauma. • Patients with recurrent fractures or continued bone loss despite therapy. • Severe osteoporosis. • When a patient has a condition that complicates management (ie. renal failure, hyperparathyroidism, malabsorption).
Thank you! Midwest Orthopaedic Institute Bone Health Center Michele T. Glasgow, MD Marie Rivers, PA-C
 Types of killer
Types of killer The way my mother speaks carol ann duffy
The way my mother speaks carol ann duffy Hepatitis b is a silent killer
Hepatitis b is a silent killer Defination of osteoporosis
Defination of osteoporosis Royal osteoporosis society leaflets
Royal osteoporosis society leaflets Pes statement for osteoporosis
Pes statement for osteoporosis Osteoporosis
Osteoporosis God bone
God bone Nursing diagnosis for osteoporosis
Nursing diagnosis for osteoporosis Osteoporosis
Osteoporosis Osteoporosis t scores
Osteoporosis t scores Bendaggio
Bendaggio Pathway hiperkalemia
Pathway hiperkalemia Eva decroli
Eva decroli Is osteoporosis hypokinetic or hyperkinetic
Is osteoporosis hypokinetic or hyperkinetic Whole muscle
Whole muscle Is osteoporosis additive or destructive
Is osteoporosis additive or destructive Osteoporosis definition
Osteoporosis definition Kể tên các môn thể thao
Kể tên các môn thể thao Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Dot
Dot Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ độ dài liên kết
độ dài liên kết Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan điện thế nghỉ
điện thế nghỉ Phối cảnh
Phối cảnh Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Frameset trong html5
Frameset trong html5 Hệ hô hấp
Hệ hô hấp Các số nguyên tố là gì
Các số nguyên tố là gì đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thang điểm glasgow
Thang điểm glasgow ưu thế lai là gì
ưu thế lai là gì Tư thế ngồi viết
Tư thế ngồi viết Thẻ vin
Thẻ vin Bàn tay mà dây bẩn
Bàn tay mà dây bẩn Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Diễn thế sinh thái là
Diễn thế sinh thái là Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Phép trừ bù
Phép trừ bù Công thức tính thế năng
Công thức tính thế năng Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi