OSTEOPOROSIS An update May 2012 Osteoporosis Df A









- Slides: 31

OSTEOPOROSIS An update May 2012

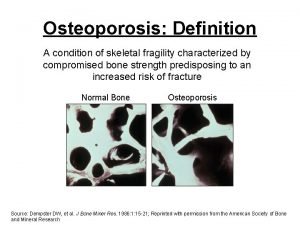
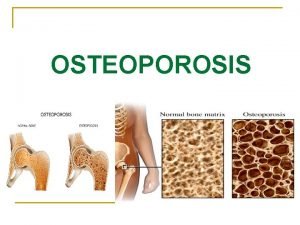
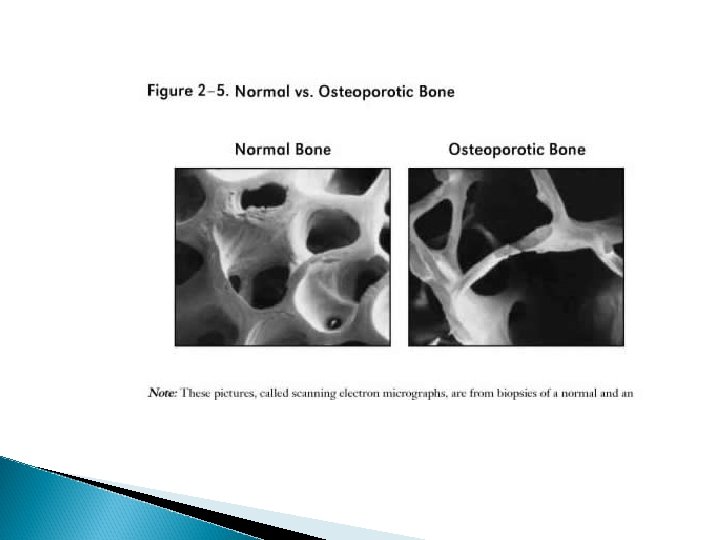
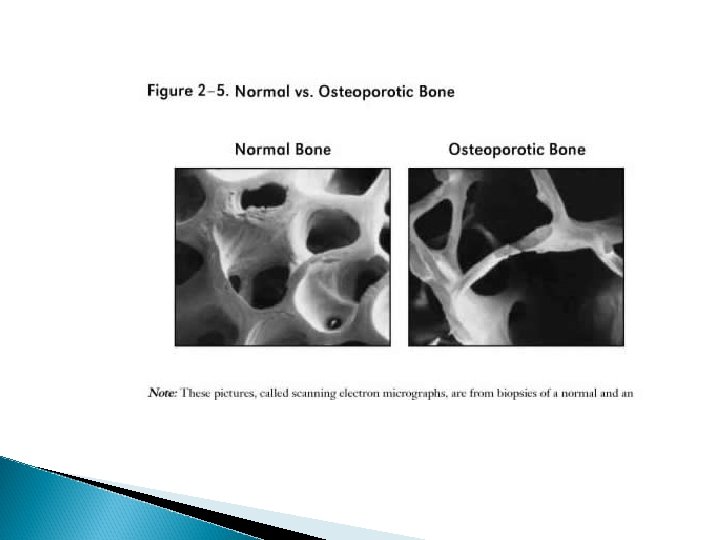
Osteoporosis Df: A progressive systemic skeletal disorder characterised by a low bone mass and microarchitectural deterioration of bone. T score of < -2. 5 when measuring bone mineral density on DEXA scan (Dual –energy x -ray absorptiometry) Osteopenia: T score -1 to -2. 5.

DEXA Scans Z score- bone strength compared to other people in your own age T score- compares bone density to that of a 25 year old. Measures bone mineral density using central hip and/or spine DEXA scanning and is expressed in the number of standard deviations below peak bone mineral density.
Why is it important? 70, 000 hip and 120, 000 spine and 50, 000 wrist # a yr due to osteoporosis. 1 > 1/3 rd of women sustain a # relating to osteoporosis. 2 Costing NHS > 940 M a yr. 2
Quick revision Bone remodelling predominates 15 -17 yrs (once longitudinal growth ceases) Consists of: i. bone dissolution/resorption by osteoclasts + ii. bone formation by osteoblasts Adults, remodelling cycle is balanced so resorption = bone formation (90 -130 days)
i) ii) However remodelling can become imbalanced so result in significant bone loss Age-related bone loss starts in 40’s/50’s as a result of: ↑ed bone breakdown by osteoclasts ↓ed bone formation by osteblasts

Risk Factors 1. 2. 3. Hormonal. Late menarche, early menopause, long hx of oligomenorrhoea. During menopause oestrogen deprivation ↑ed bone resorption, so→ bone loss. Smoking Excessive alcohol intake
4. Lack of weight bearing exercise 5. Vitamin D deficiency 6. Glucocorticoid exposure. ↓ Ca absorption, ↑ bone resorption, ↓ bone formation, thus → bone loss.
Investigations 1. < 75 yrs DEXA scan 2. Bloods: Ø Ø 3 FBC, ESR, TSH, U+E’s, bone and LFTs. Consider checking serum paraproteins /urinary Bence Jones proteins to exclude other causes for # such as:
Ø 1. 2. 3. Other possible causes of #: Malignancy, Osteomalacia, Hyperparathyroidism 4
If ≥ 75 yrs + DEXA clinically inappropriate clincial assessment is sufficient for diagnosis. 3

Management Non-pharmacological Pharmacological
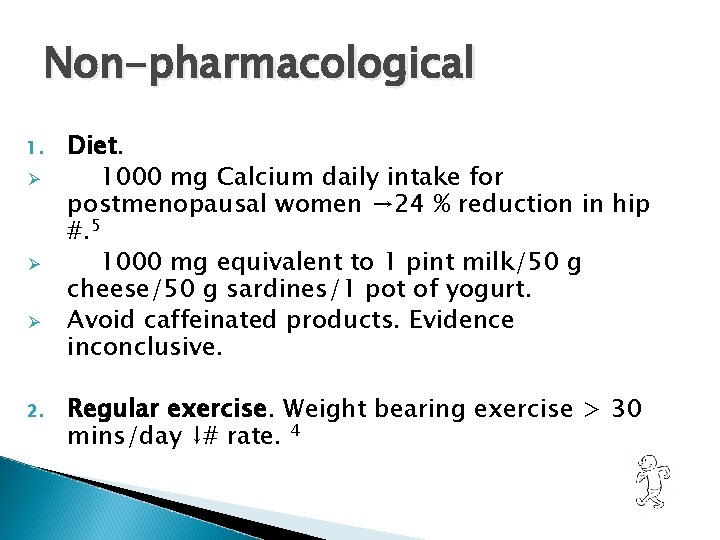
Non-pharmacological 1. Ø Ø Ø 2. Diet. 1000 mg Calcium daily intake for postmenopausal women → 24 % reduction in hip #. 5 1000 mg equivalent to 1 pint milk/50 g cheese/50 g sardines/1 pot of yogurt. Avoid caffeinated products. Evidence inconclusive. Regular exercise. Weight bearing exercise > 30 mins/day ↓# rate. 4
3. Stop smoking. Pre-menopause leads to 25 % ↓# rate postmenopausal 4 4. ↓alcohol consumption to < 21 units/wk male, <14 units/wk women 4
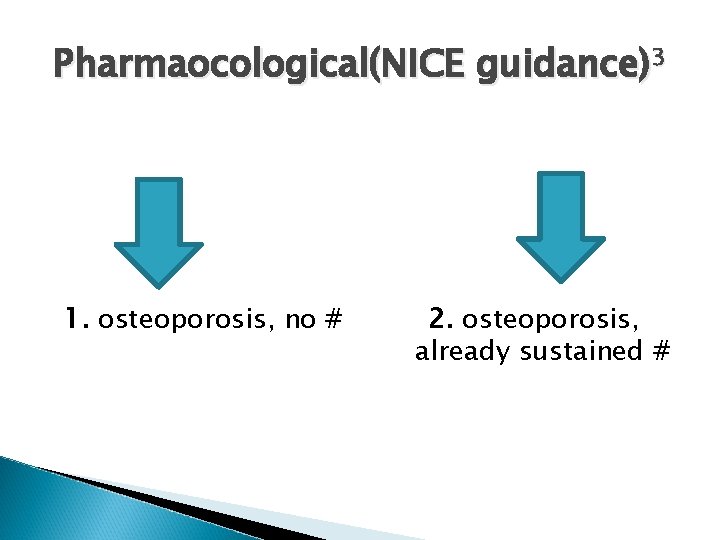
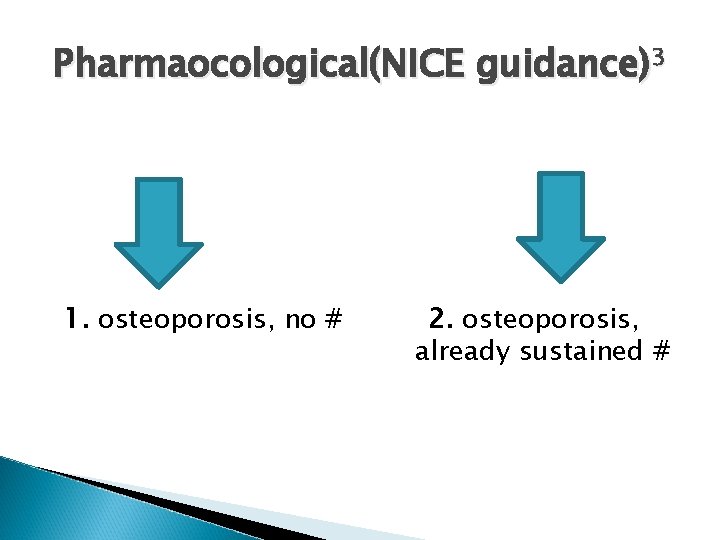
Pharmaocological(NICE guidance)3 1. osteoporosis, no # 2. osteoporosis, already sustained #

1 o prevention of osteoporotic # in PM women 1 st line Alendronate 2 nd line Risedronate and Etidronate 3 rd line Strontium Ranelate 4 th line Denosumab
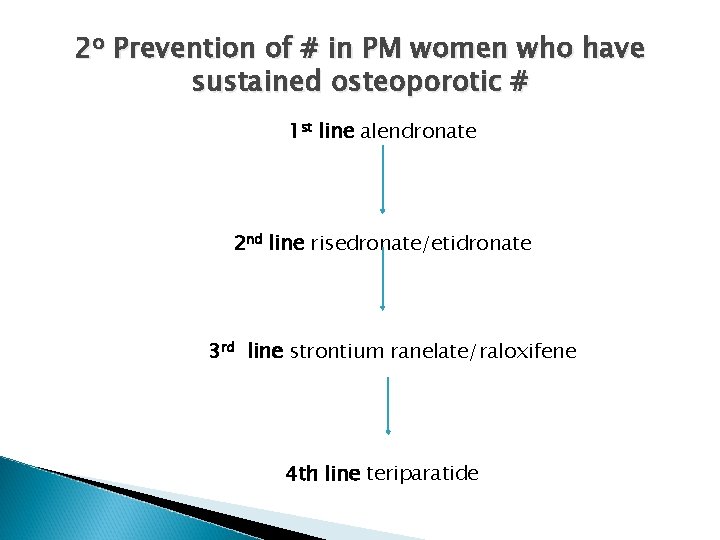
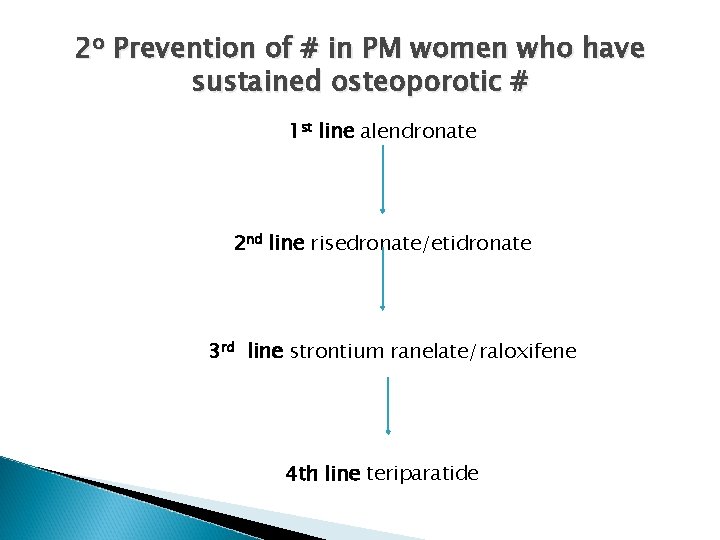
2 o Prevention of # in PM women who have sustained osteoporotic # 1 st line alendronate 2 nd line risedronate/etidronate 3 rd line strontium ranelate/raloxifene 4 th line teriparatide

If there are contraindications, intolerances or side effects then the next line of treatment should be tried. As an adjunct to treatment calcium and vitamin D supplementation should be considered in patients with a diagnosis of osteoporosis.

Bisphonates Ø Alendronic acid/risedronate/etidronate Ø MOA: adsorbed onto hydroxyapatite crystals in bone, slowing both their rate of growth + dissolution so ↓ the rate of bone turn over. 6 Ø Poorly absorbed. 1 -5 % of oral dose actually absorbed. 5

Ø Special § § To be swallowed whole, with water while sitting or standing on an empty stomach 30 mins before breakfast. Pt should then stand or sit upraight for at least 30 mins after taking the tablet. Ø Side § instructions: effects: oesophageal reactionsoesophagitis/ulcers/stricture/erosions.
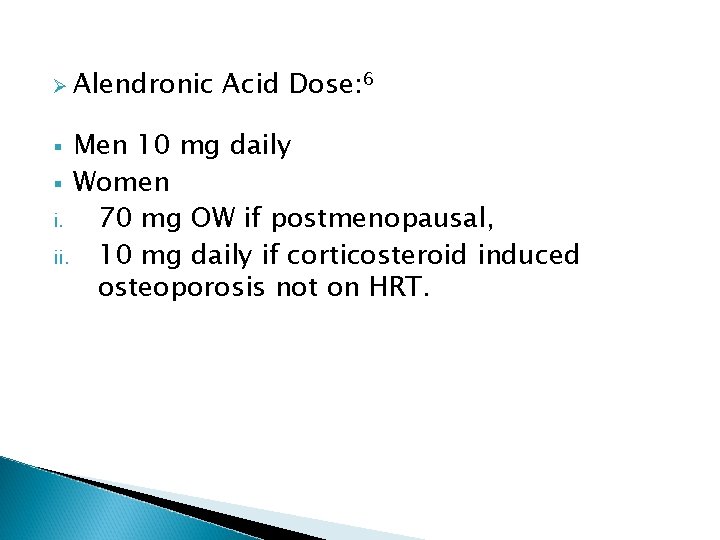
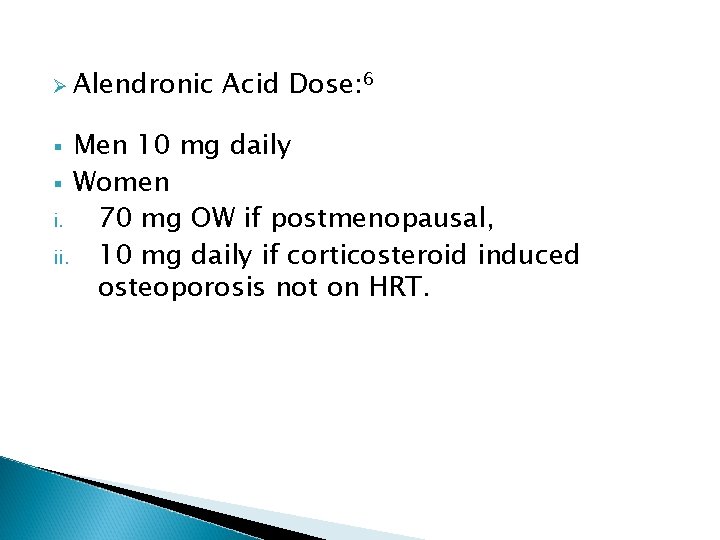
Ø Alendronic Acid Dose: 6 Men 10 mg daily § Women i. 70 mg OW if postmenopausal, ii. 10 mg daily if corticosteroid induced osteoporosis not on HRT. §
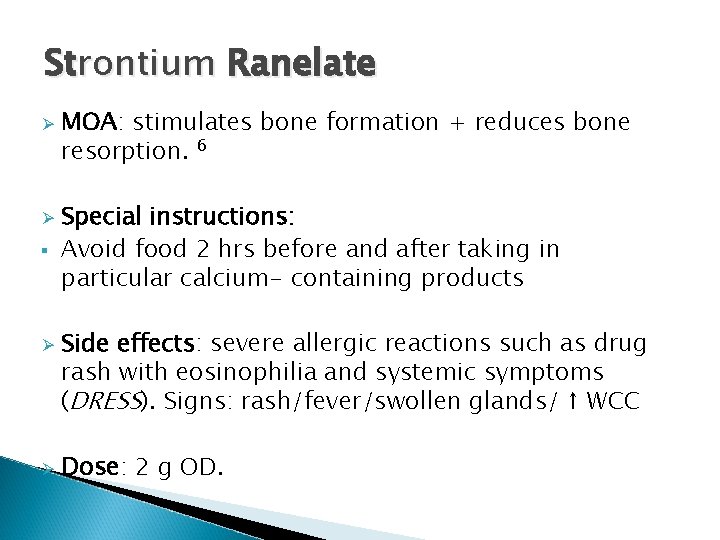
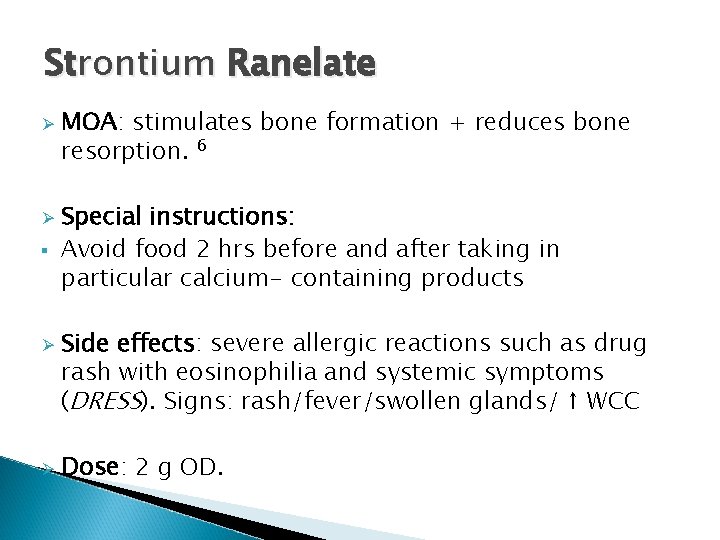
Strontium Ranelate Ø Ø § Ø Ø MOA: stimulates bone formation + reduces bone resorption. 6 Special instructions: Avoid food 2 hrs before and after taking in particular calcium- containing products Side effects: severe allergic reactions such as drug rash with eosinophilia and systemic symptoms (DRESS). Signs: rash/fever/swollen glands/ ↑ WCC Dose: 2 g OD.
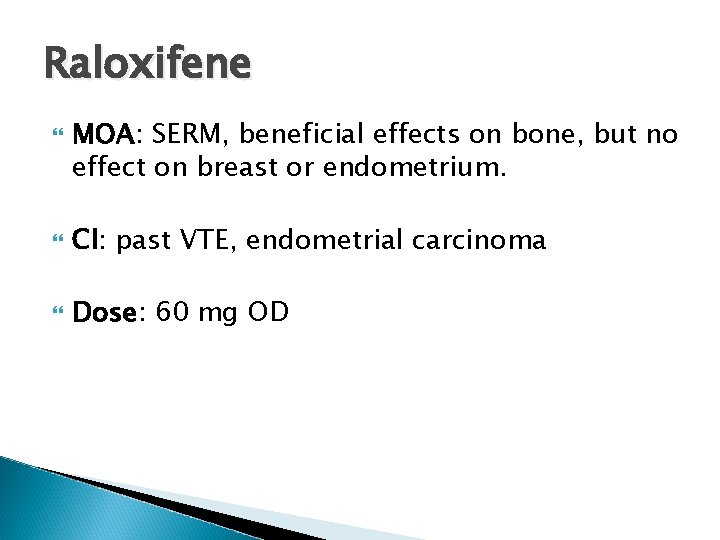
Raloxifene MOA: SERM, beneficial effects on bone, but no effect on breast or endometrium. CI: past VTE, endometrial carcinoma Dose: 60 mg OD
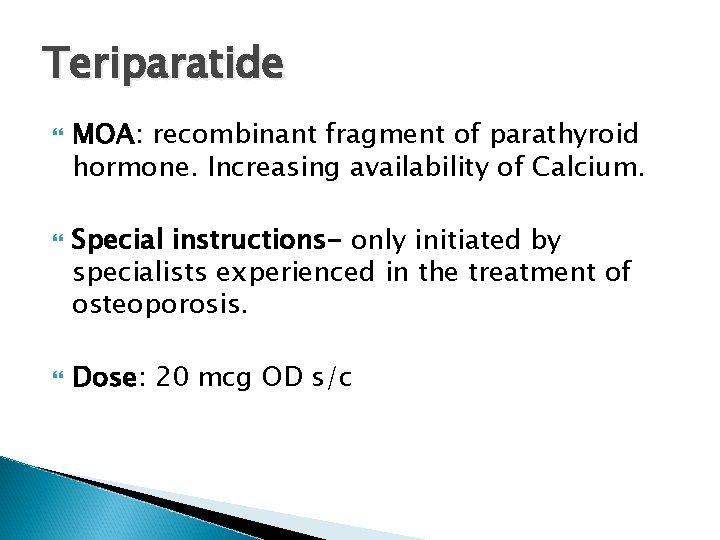
Teriparatide MOA: recombinant fragment of parathyroid hormone. Increasing availability of Calcium. Special instructions- only initiated by specialists experienced in the treatment of osteoporosis. Dose: 20 mcg OD s/c
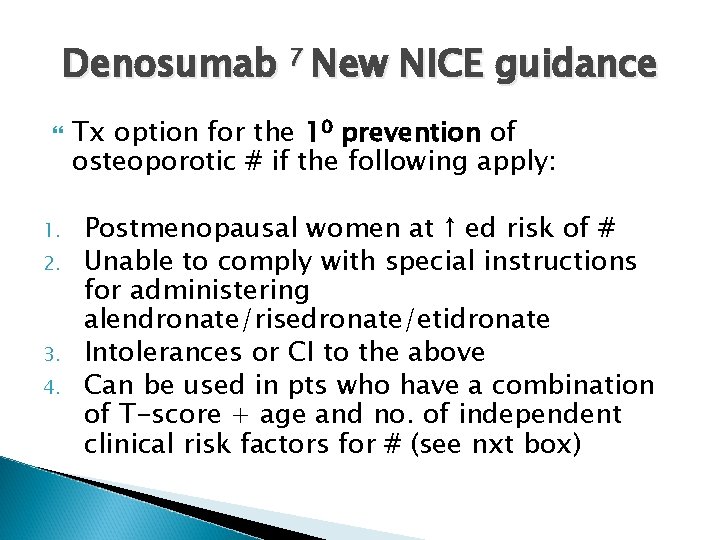
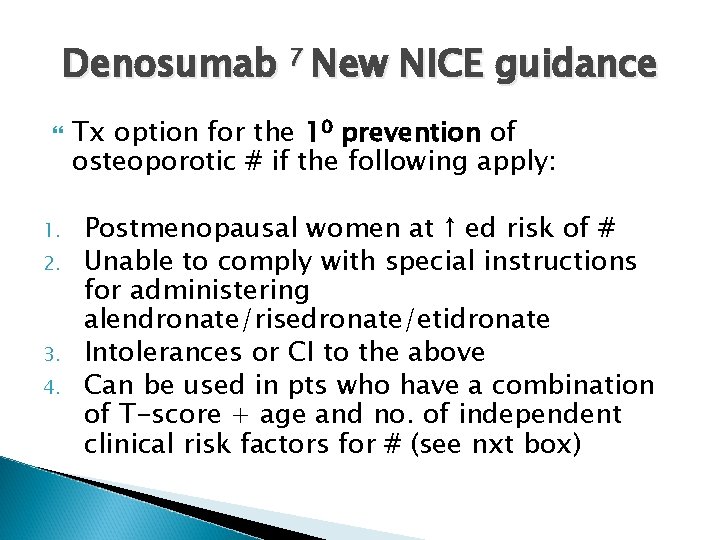
Denosumab 7 New NICE guidance 1. 2. 3. 4. Tx option for the 10 prevention of osteoporotic # if the following apply: Postmenopausal women at ↑ ed risk of # Unable to comply with special instructions for administering alendronate/risedronate/etidronate Intolerances or CI to the above Can be used in pts who have a combination of T-score + age and no. of independent clinical risk factors for # (see nxt box)
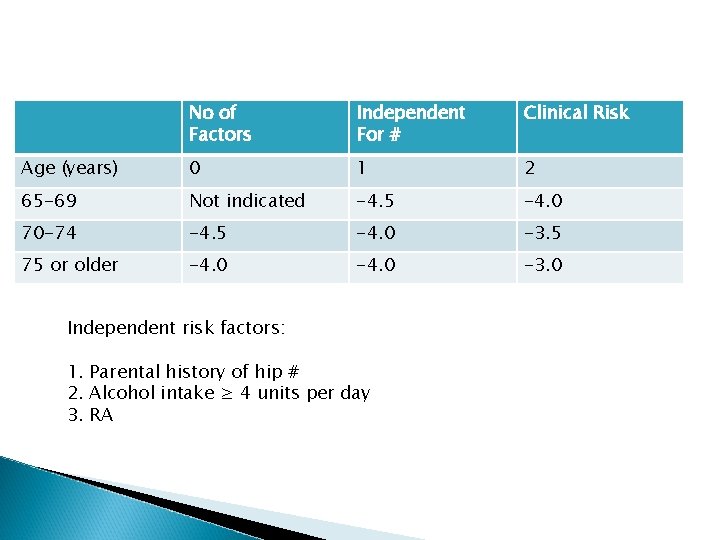
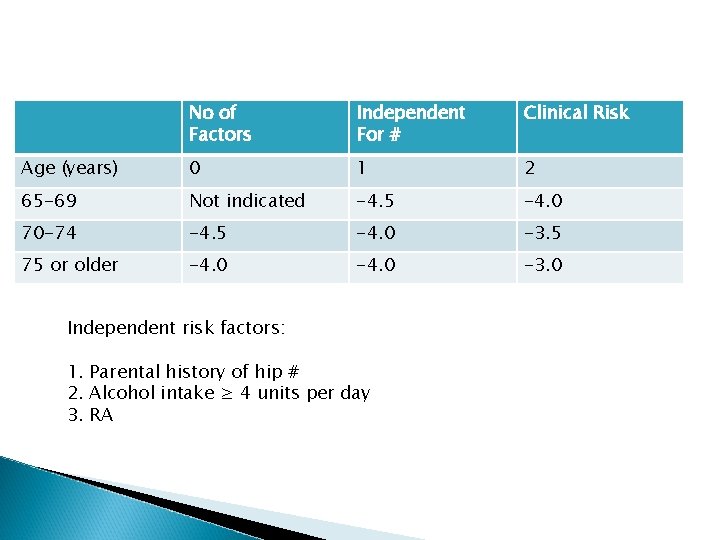
No of Factors Independent For # Clinical Risk Age (years) 0 1 2 65 -69 Not indicated -4. 5 -4. 0 70 -74 -4. 5 -4. 0 -3. 5 75 or older -4. 0 -3. 0 Independent risk factors: 1. Parental history of hip # 2. Alcohol intake ≥ 4 units per day 3. RA
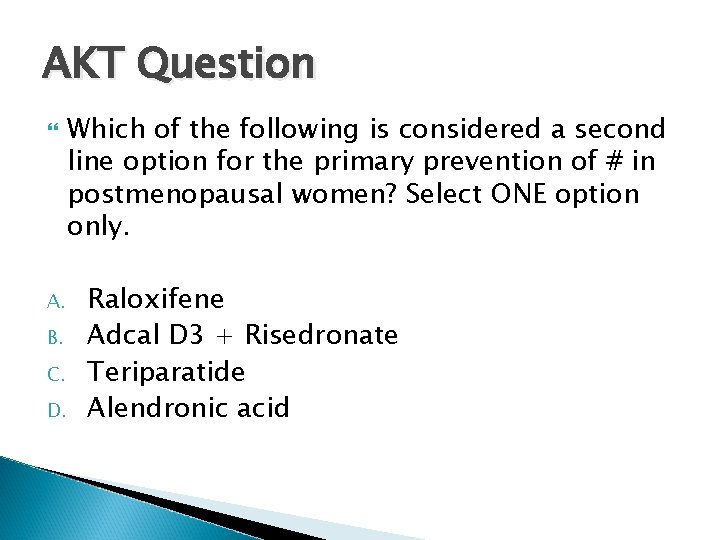
AKT Question A. B. C. D. Which of the following is considered a second line option for the primary prevention of # in postmenopausal women? Select ONE option only. Raloxifene Adcal D 3 + Risedronate Teriparatide Alendronic acid
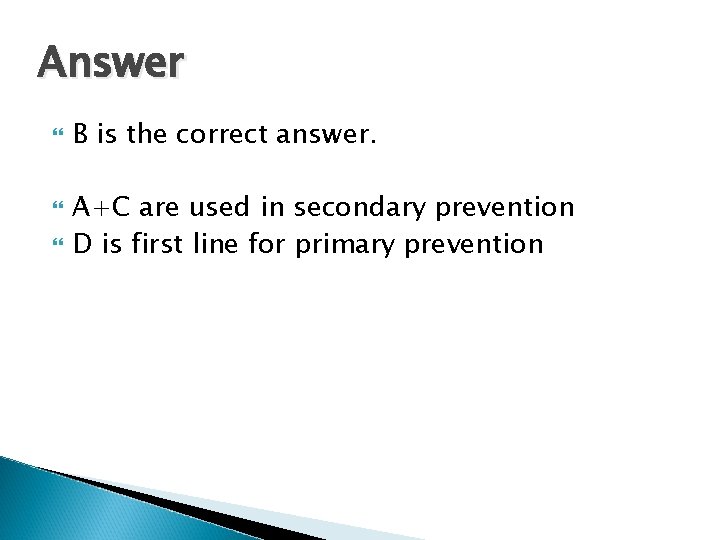
Answer B is the correct answer. A+C are used in secondary prevention D is first line for primary prevention
References 1. Osteoporosis. An Information booklet. www. arc. org. uk Updated May 2007. 2. Royal College of Physicians. Clinical Guidelines for the prevention and treatment of osteoporosis. www. rcplondon. ac. uk 3. NICE guidance Oct 2008 http: //www. nice. org. uk/nicemedia/live/11746/42 486/42486. pdf 4. Oxford Handbook of General Practice. P 568 -569
5. SIGN (Scottish intercollegiate guidelines network) guidelines for osteoporosis. http: //www. sign. ac. uk/guidelines updated 2004. 6. BNF Chapter 6. 6. 2 p 463. Bisphospahtes and other drugs affecting bone metabolism. 7. Denosumab for the prevention of osteoporotic fractures in postmenopausal women Nice Guidance, Oct 2010. http: //www. nice. org. uk/nicemedia/live/13251/51 329/51329. pdf
 Backup and recovery techniques
Backup and recovery techniques Dr eva decroli
Dr eva decroli Is osteoporosis hypokinetic or hyperkinetic
Is osteoporosis hypokinetic or hyperkinetic Whole muscle
Whole muscle International osteoporosis foundation
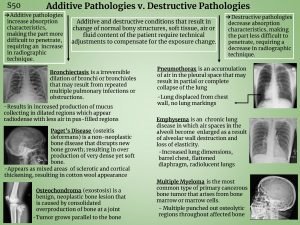
International osteoporosis foundation Additive pathology in radiography
Additive pathology in radiography Alendronate brand name
Alendronate brand name Osteoporosis defination
Osteoporosis defination Royal osteoporosis society leaflets
Royal osteoporosis society leaflets Pes statement for osteoporosis
Pes statement for osteoporosis God bone
God bone Subjective data for osteoporosis
Subjective data for osteoporosis Osteoporosis
Osteoporosis Osteoporosis t score
Osteoporosis t score Defination of osteoporosis
Defination of osteoporosis Woc osteoporosis
Woc osteoporosis Hci design patterns
Hci design patterns Windws update
Windws update Multiplicative update
Multiplicative update 508 refresh
508 refresh Rational clear quest
Rational clear quest Database commit is triggered by
Database commit is triggered by Mdh situation update
Mdh situation update Iso legislation update
Iso legislation update 811 locate request
811 locate request Gtcs professional update
Gtcs professional update Kb2533623 update for windows 7
Kb2533623 update for windows 7 Routing area update
Routing area update Game loop diagram
Game loop diagram Flowchart proses update secara berurutan adalah
Flowchart proses update secara berurutan adalah Fsu freight status update
Fsu freight status update Ffm update
Ffm update