Osteoporosis Osteopenia 2016 06 27 Osteoporosis Osteoporosis is










- Slides: 22
Osteoporosis/ Osteopenia 2016. 06. 27. 학생집담회
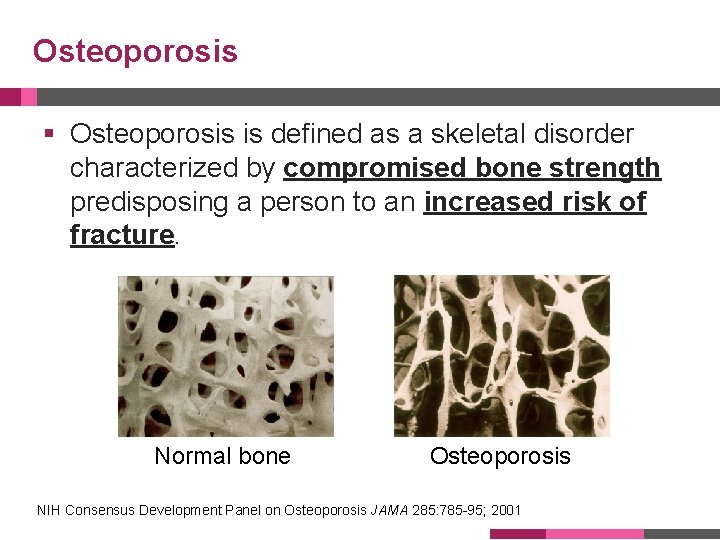
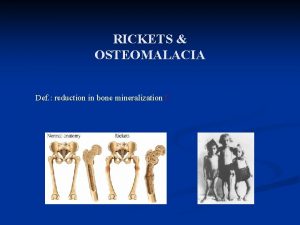
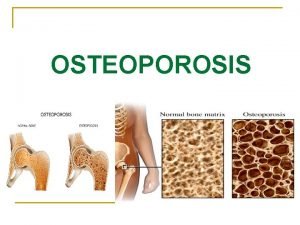
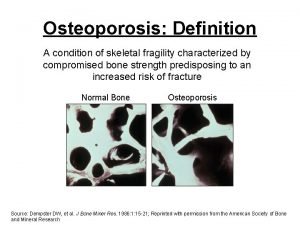
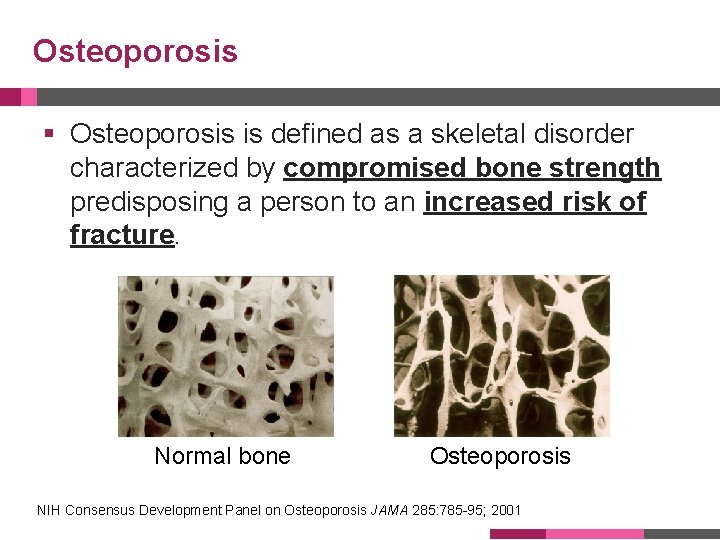
Osteoporosis § Osteoporosis is defined as a skeletal disorder characterized by compromised bone strength predisposing a person to an increased risk of fracture. Normal bone Osteoporosis NIH Consensus Development Panel on Osteoporosis JAMA 285: 785 -95; 2001
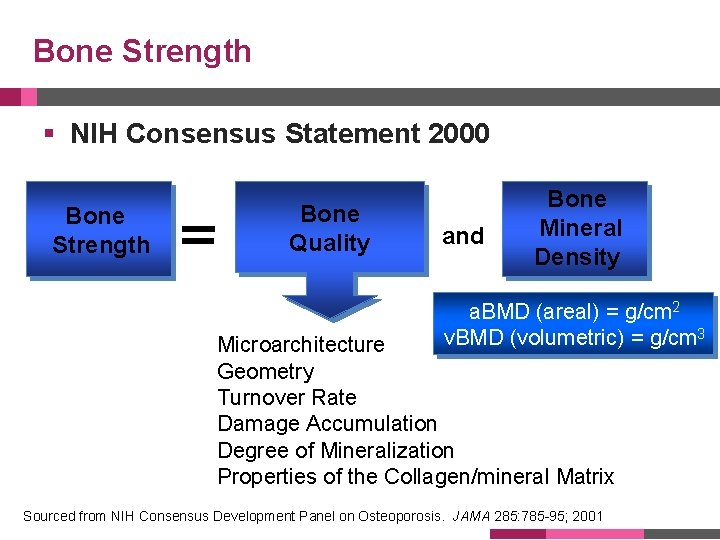
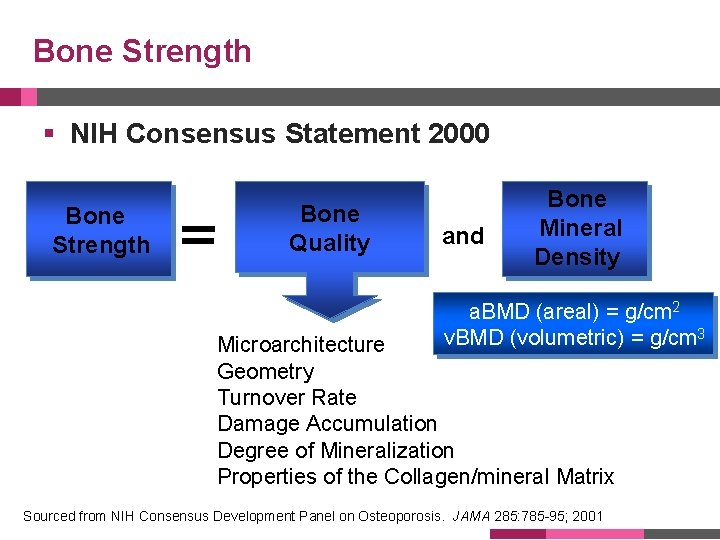
Bone Strength § NIH Consensus Statement 2000 Bone Strength Bone Quality and Bone Mineral Density a. BMD (areal) = g/cm 2 v. BMD (volumetric) = g/cm 3 Microarchitecture Geometry Turnover Rate Damage Accumulation Degree of Mineralization Properties of the Collagen/mineral Matrix Sourced from NIH Consensus Development Panel on Osteoporosis. JAMA 285: 785 -95; 2001
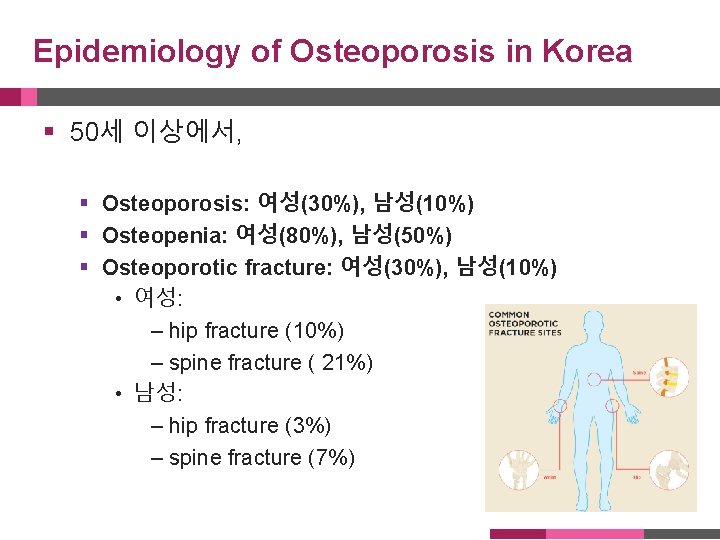
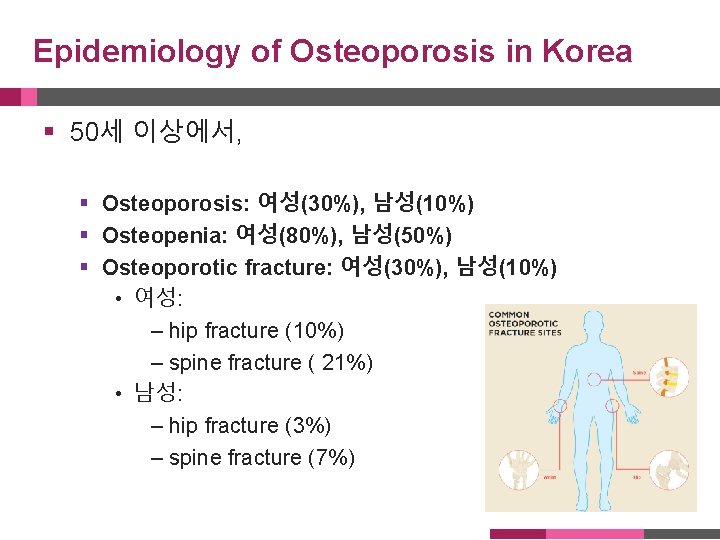
Epidemiology of Osteoporosis in Korea § 50세 이상에서, § Osteoporosis: 여성(30%), 남성(10%) § Osteopenia: 여성(80%), 남성(50%) § Osteoporotic fracture: 여성(30%), 남성(10%) • 여성: – hip fracture (10%) – spine fracture ( 21%) • 남성: – hip fracture (3%) – spine fracture (7%)
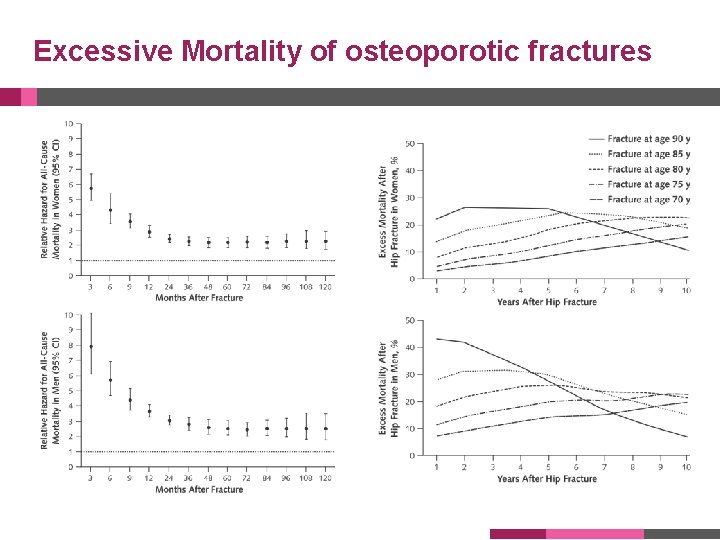
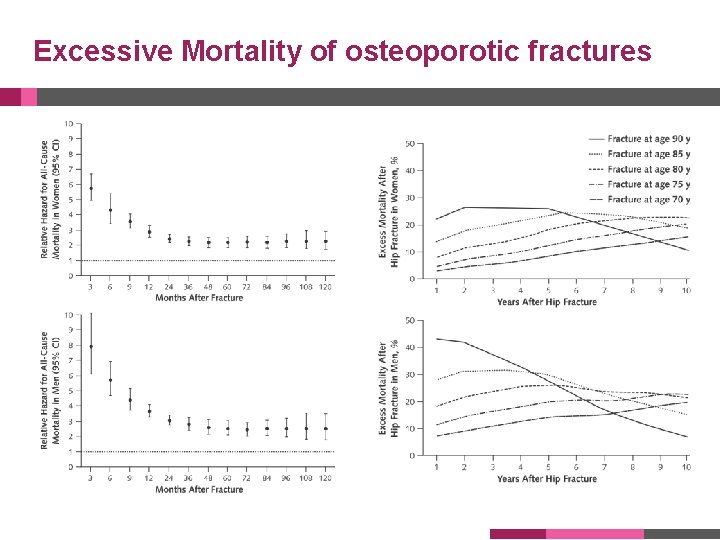
Excessive Mortality of osteoporotic fractures
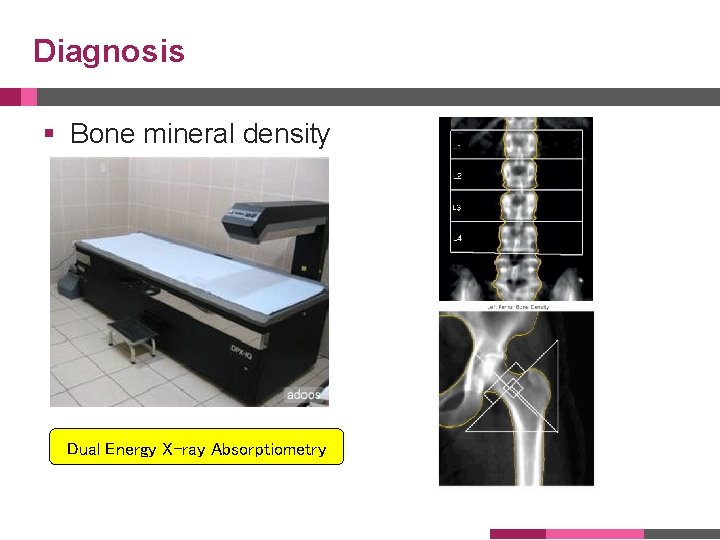
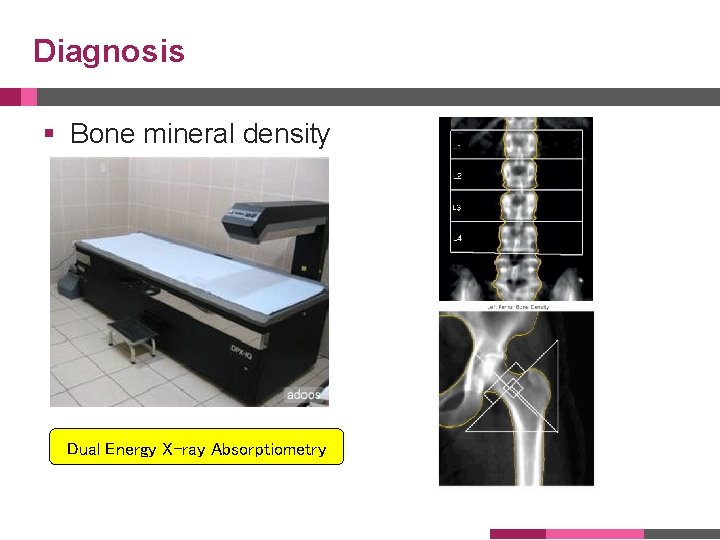
Diagnosis § Bone mineral density Dual Energy X-ray Absorptiometry








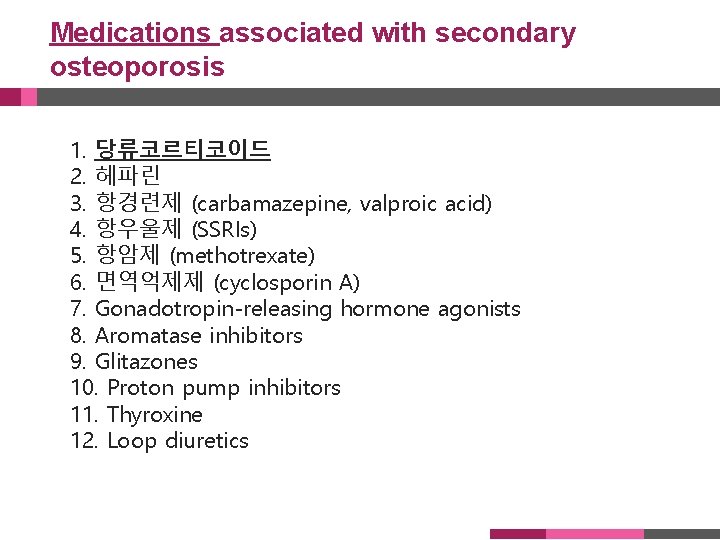
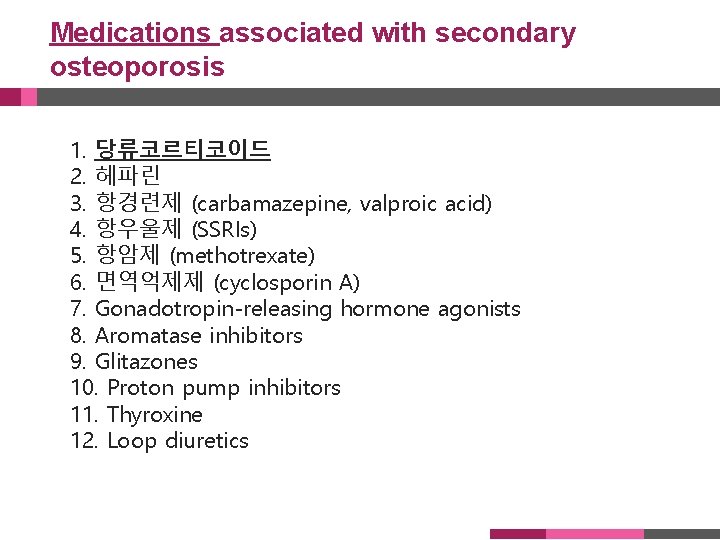
Medications associated with secondary osteoporosis 1. 당류코르티코이드 2. 헤파린 3. 항경련제 (carbamazepine, valproic acid) 4. 항우울제 (SSRIs) 5. 항암제 (methotrexate) 6. 면역억제제 (cyclosporin A) 7. Gonadotropin-releasing hormone agonists 8. Aromatase inhibitors 9. Glitazones 10. Proton pump inhibitors 11. Thyroxine 12. Loop diuretics
Clinical Risk factors for fractures § § § § Age BMD; 1 SD 2 fold increase of fracture risk BMI History of fragility fracture Family history of fragility fracture Cigarette smoking Glucocorticoids (>5 mg prednisolone daily or equivalent for 3 months or more) § Alcohol (≥ 3 units daily intake, dose-dependent increase in risk) § Rheumatoid arthritis

http: //www. shef. ac. uk/FRAX/tool. jsp? country=25
Pharmacologic therapy Who should be considered for treatment? § Postmenopausal women and men age 50 and older presenting with the following should be considered for treatment: § A hip or vertebral fracture (There is abundant data that patients with spine and hip fractures will have reduced fracture risk if treated with pharmacologic therapy) § T-score ≤ -2. 5 at the femoral neck, total hip or lumbar spine (There is abundant evidence that patients with osteoporosis by BMD have an elevated risk of fracture and reduced fracture risk with pharmacotherapy) § Low bone mass (T-score between -1. 0 and -2. 5 at the femoral neck or lumbar spine) and a 10 -year probability of a hip fracture ≥ 3% or a major osteoporosis-related fracture ≥ 20%)
Pharmacologic Intervention § Calcium & Vitamin D § Antiresorptive (anticatabolic) agent § § § Hormone therapy SERM (Raloxifene) Tibolon Calcitonin Bisphophonates (Alendronate, Risedronate, Ibandronate, Zoledronate) § Bone forming (Anabolic) agent § rh. PTH (Teriparatide)
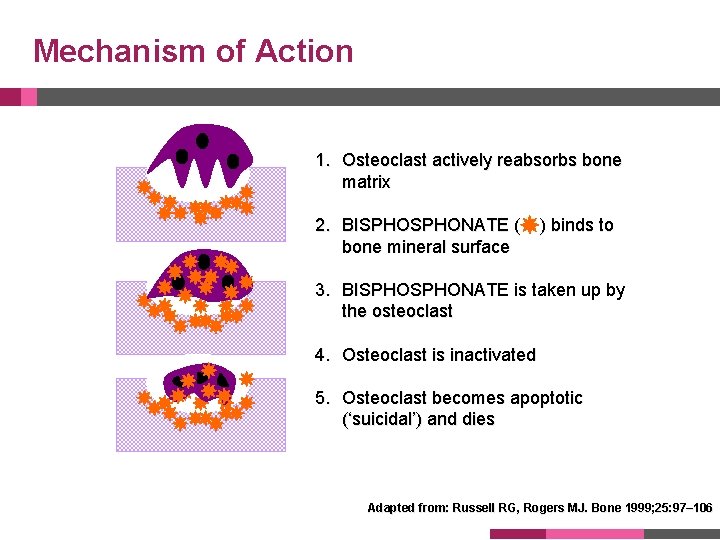
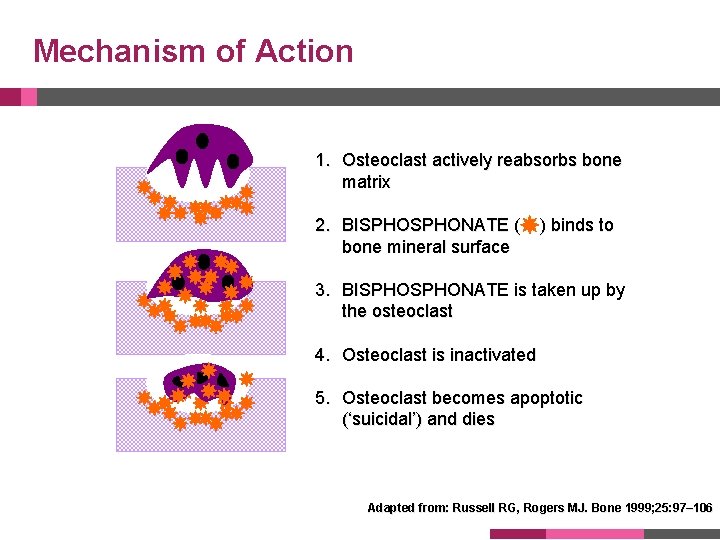
Mechanism of Action 1. Osteoclast actively reabsorbs bone matrix 2. BISPHONATE ( bone mineral surface ) binds to 3. BISPHONATE is taken up by the osteoclast 4. Osteoclast is inactivated 5. Osteoclast becomes apoptotic (‘suicidal’) and dies Adapted from: Russell RG, Rogers MJ. Bone 1999; 25: 97– 106

Mechanism of Action
 Osteopenia of prematurity ppt
Osteopenia of prematurity ppt Engrosamiento sinovial
Engrosamiento sinovial Osteoporosis
Osteoporosis T score osteoporosis
T score osteoporosis Osteoporosis definition
Osteoporosis definition Pathway hiperkalemia
Pathway hiperkalemia Dr eva decroli
Dr eva decroli International osteoporosis foundation
International osteoporosis foundation Is osteoporosis hypokinetic or hyperkinetic
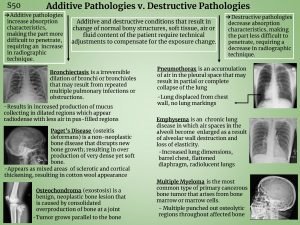
Is osteoporosis hypokinetic or hyperkinetic Additive pathology examples
Additive pathology examples Osteoporosis definition
Osteoporosis definition Loss defination
Loss defination Whole muscle
Whole muscle Royal osteoporosis society leaflets
Royal osteoporosis society leaflets Pes statement for osteoporosis
Pes statement for osteoporosis Tbs osteoporosis
Tbs osteoporosis Subjective data for osteoporosis
Subjective data for osteoporosis 2016 tni standard checklist
2016 tni standard checklist Se dirjen cipta karya no 86 tahun 2016
Se dirjen cipta karya no 86 tahun 2016 Como colocar borda no word 2016
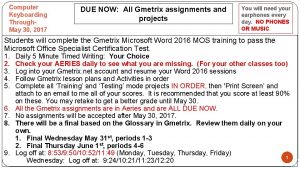
Como colocar borda no word 2016 Word 2016 session 2 post assessment
Word 2016 session 2 post assessment Forrester identity management
Forrester identity management Www.gcflearnfree.org/excel 2016
Www.gcflearnfree.org/excel 2016