Osteoporosis an underestimated disease Definition of osteoporosis a

- Slides: 36
Osteoporosis an underestimated disease

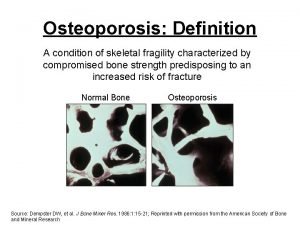
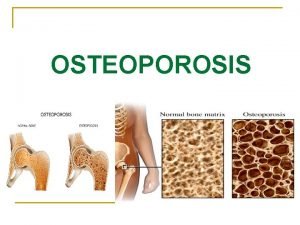
Definition of osteoporosis …a systemic skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue leading to enhanced bone fragility and a consequent increase in fracture risk. World Health Organization (WHO). Technical Report Series 843, Geneva 1994 Update TRS 921, 2003
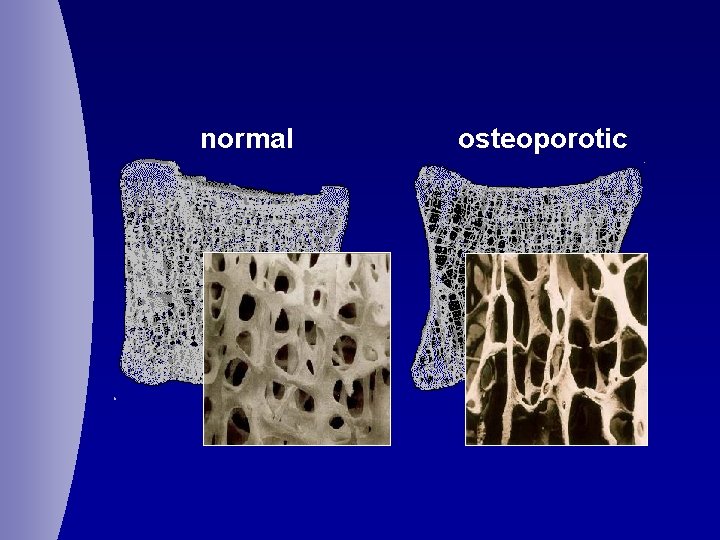
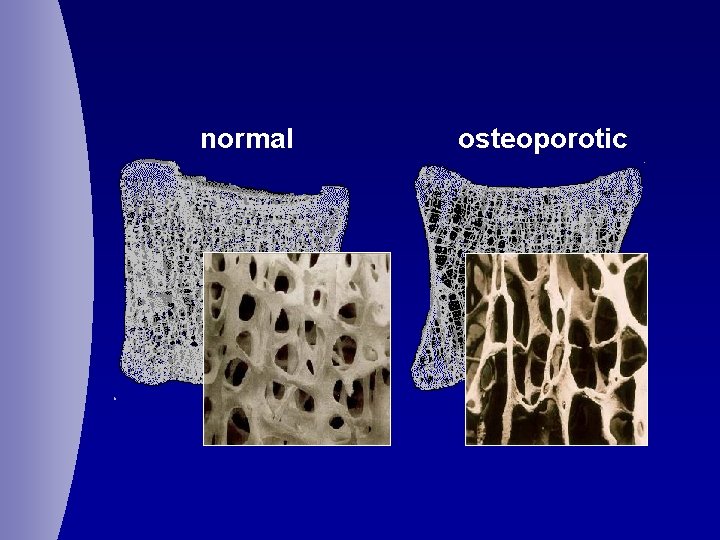
normal osteoporotic
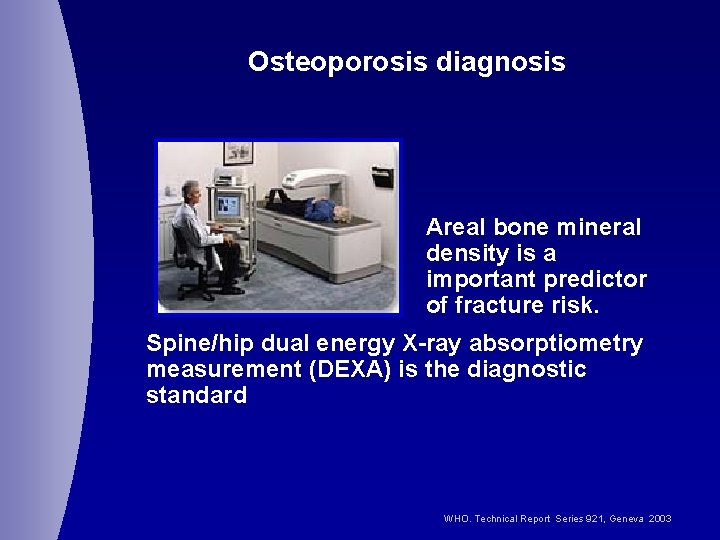
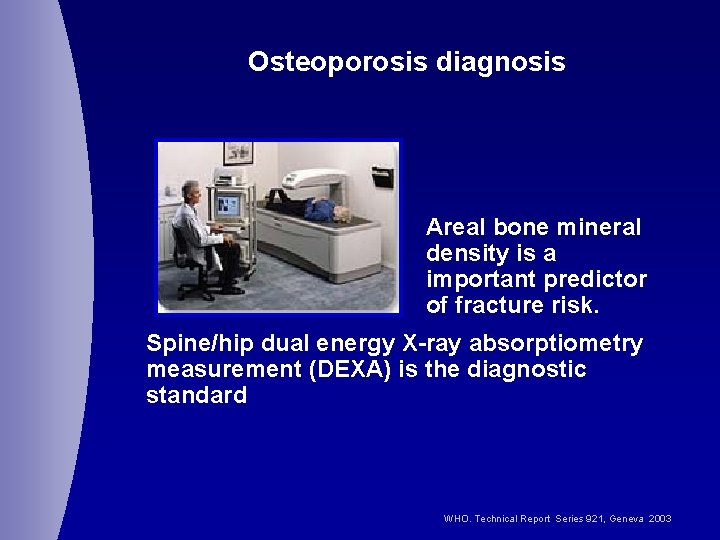
Osteoporosis diagnosis Areal bone mineral density is a important predictor of fracture risk. Spine/hip dual energy X-ray absorptiometry measurement (DEXA) is the diagnostic standard WHO. Technical Report Series 921, Geneva 2003
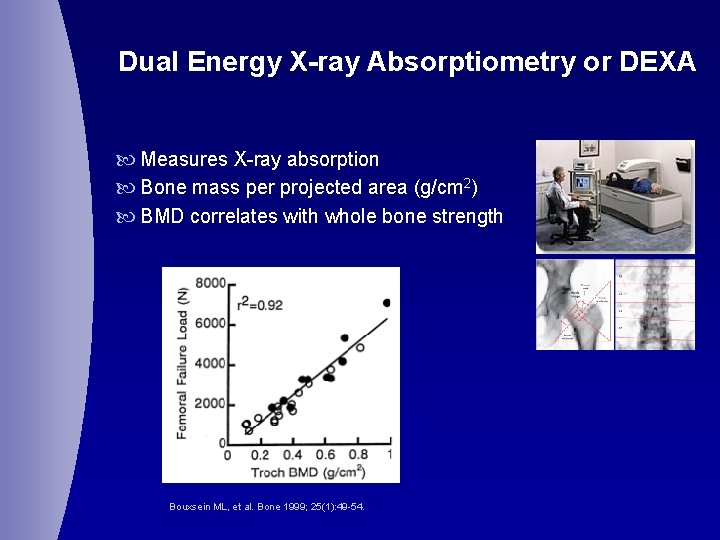
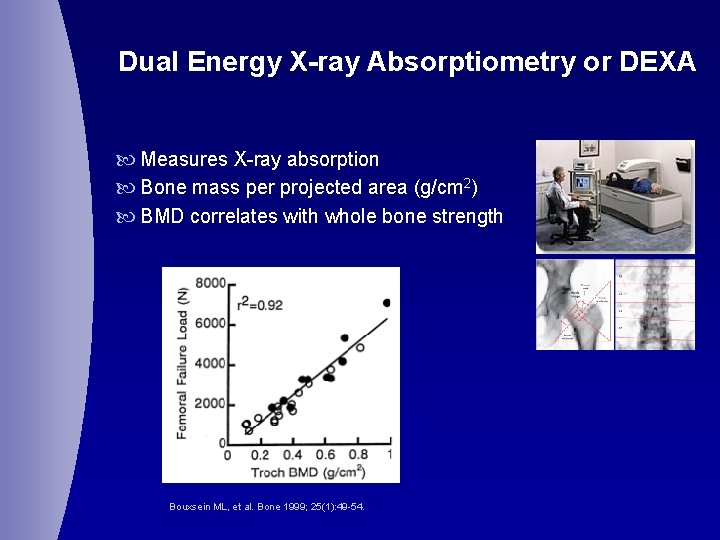
Dual Energy X-ray Absorptiometry or DEXA Measures X-ray absorption Bone mass per projected area (g/cm 2) BMD correlates with whole bone strength Bouxsein ML, et al. Bone 1999; 25(1): 49 -54.
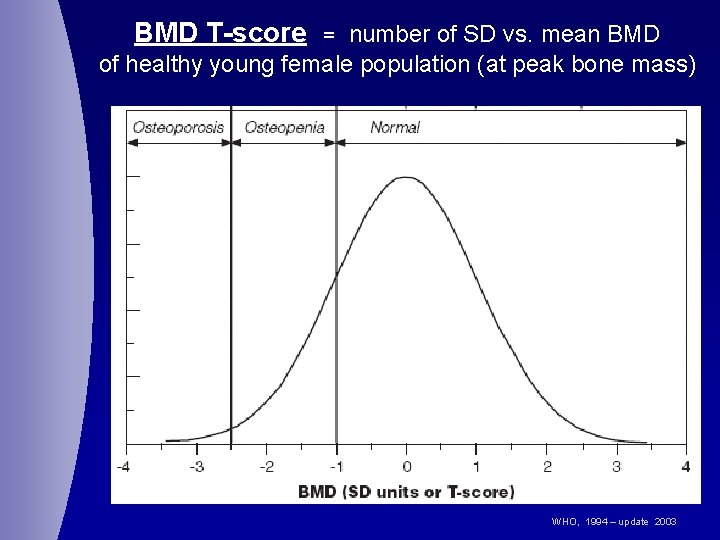
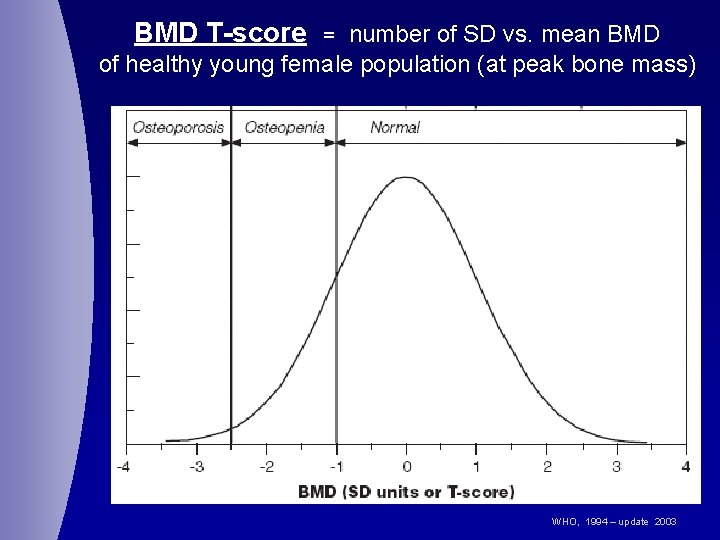
BMD T-score number of SD vs. mean BMD of healthy young female population (at peak bone mass) = WHO, 1994 – update 2003
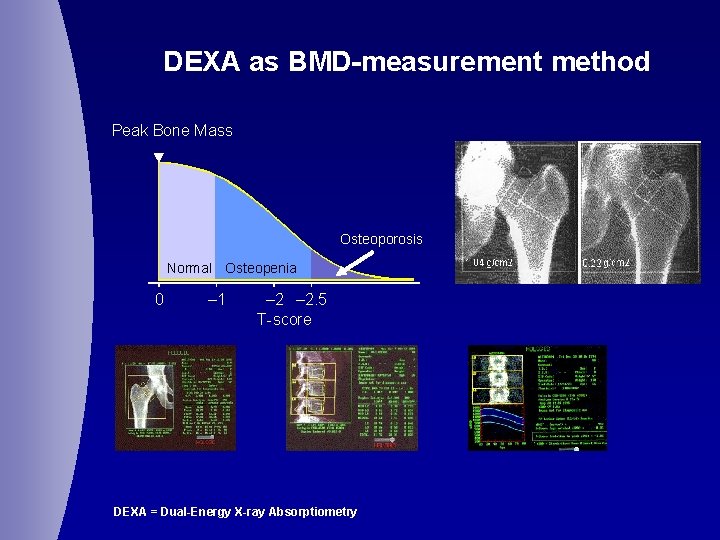
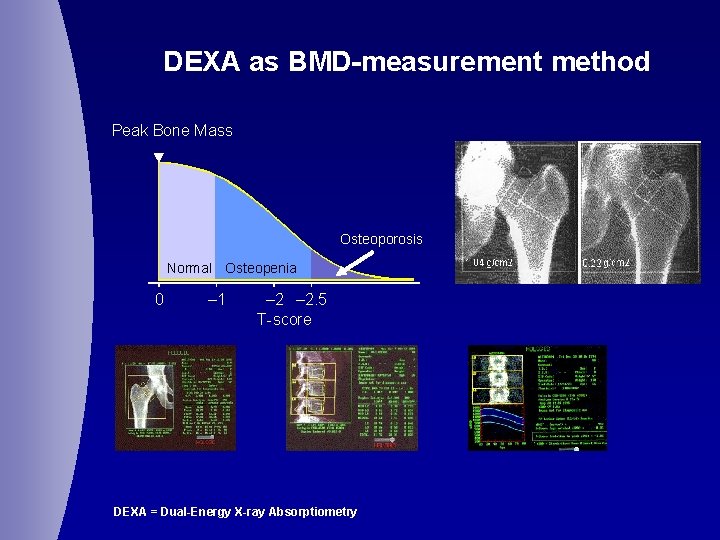
DEXA as BMD-measurement method Peak Bone Mass Osteoporosis Normal Osteopenia 0 – 1 – 2. 5 T-score DEXA = Dual-Energy X-ray Absorptiometry
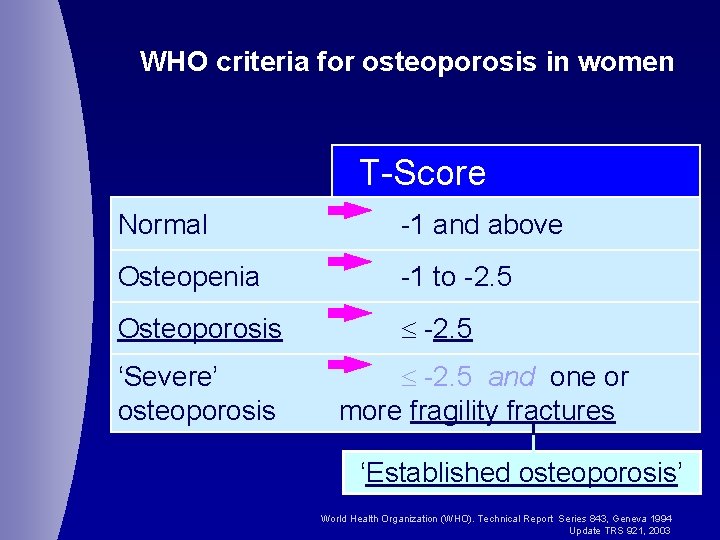
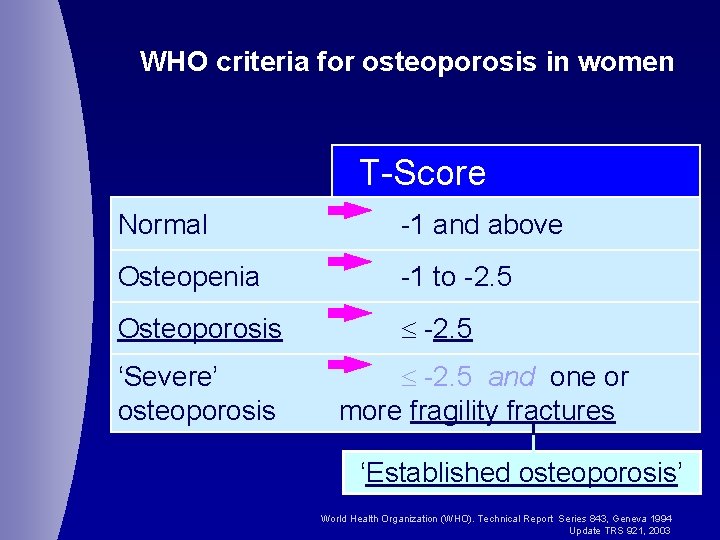
WHO criteria for osteoporosis in women T-Score Normal -1 and above Osteopenia -1 to -2. 5 Osteoporosis -2. 5 ‘Severe’ osteoporosis -2. 5 and one or more fragility fractures ‘Established osteoporosis’ World Health Organization (WHO). Technical Report Series 843, Geneva 1994 Update TRS 921, 2003
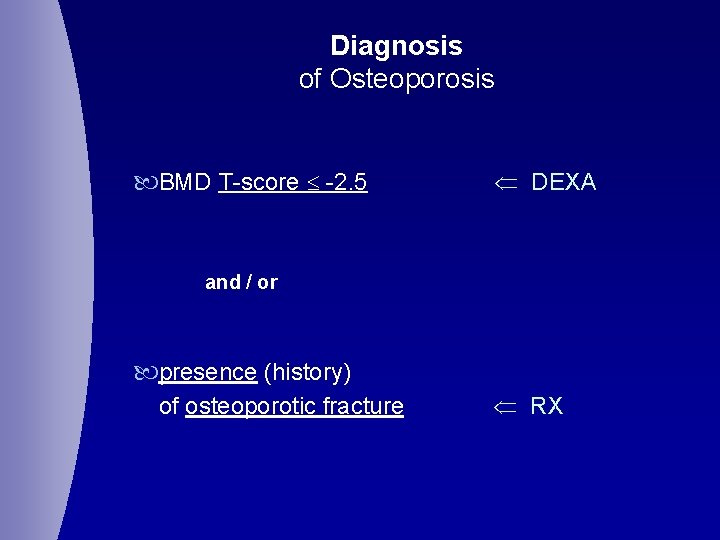
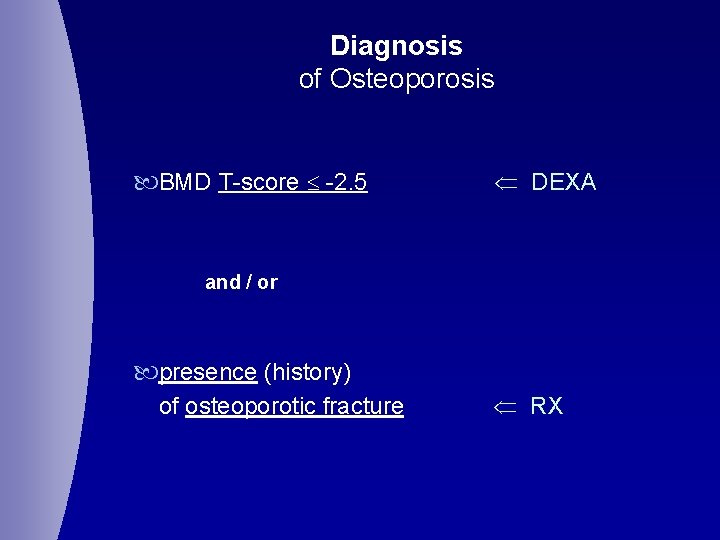
Diagnosis of Osteoporosis BMD T-score -2. 5 DEXA and / or presence (history) of osteoporotic fracture RX
Post-menopausal Osteoporosis
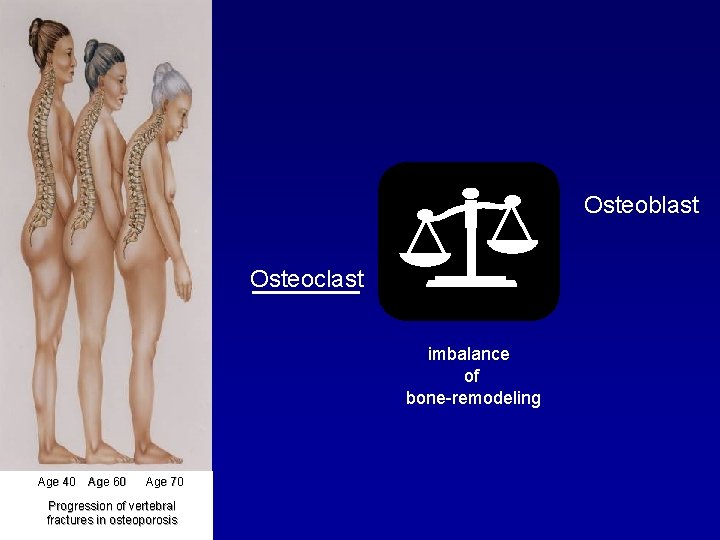
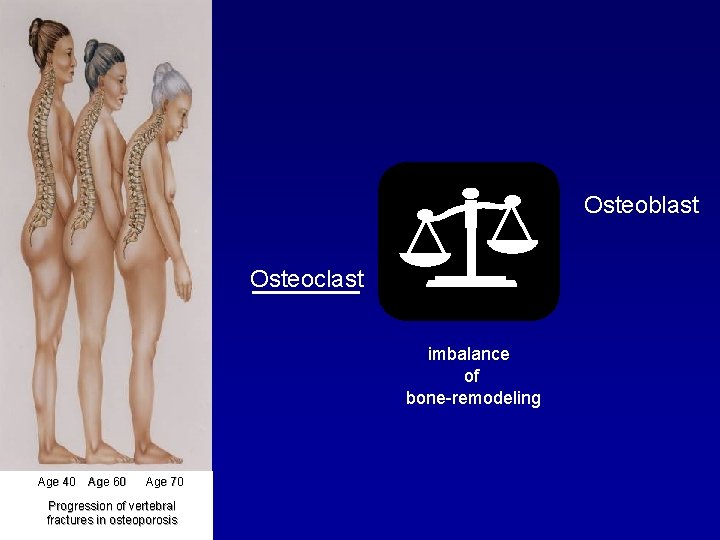
Osteoblast Osteoclast imbalance of bone-remodeling Age 40 Age 60 Age 70 Progression of vertebral fractures in osteoporosis
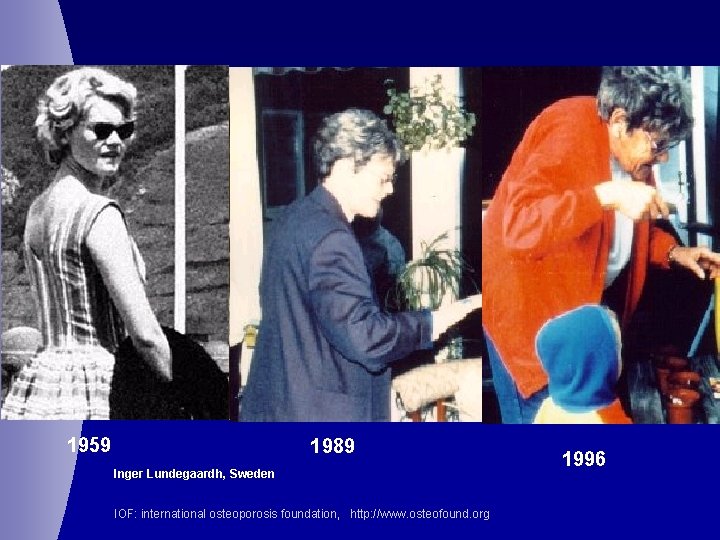
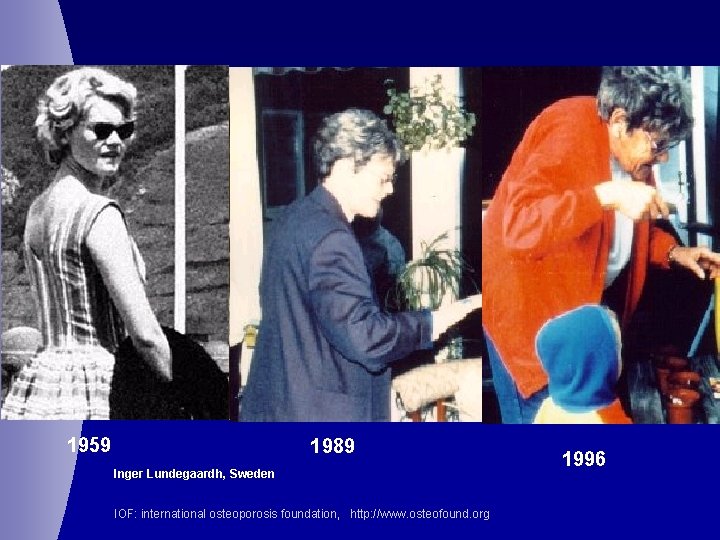
1959 1989 Inger Lundegaardh, Sweden IOF: international osteoporosis foundation, http: //www. osteofound. org 1996
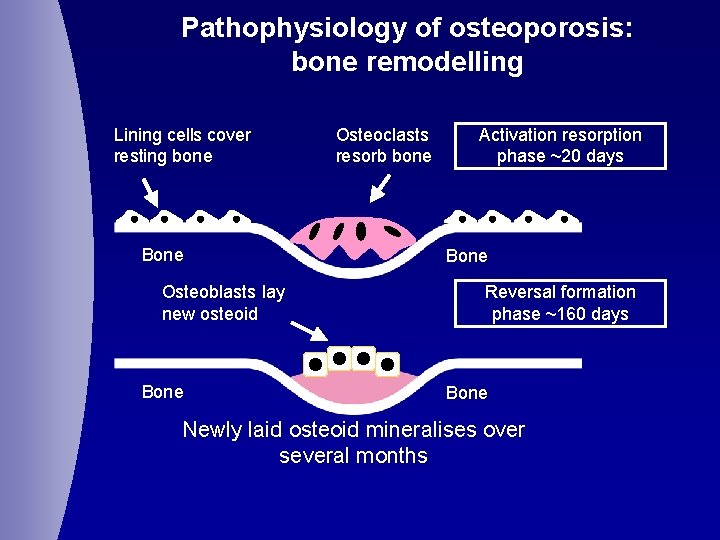
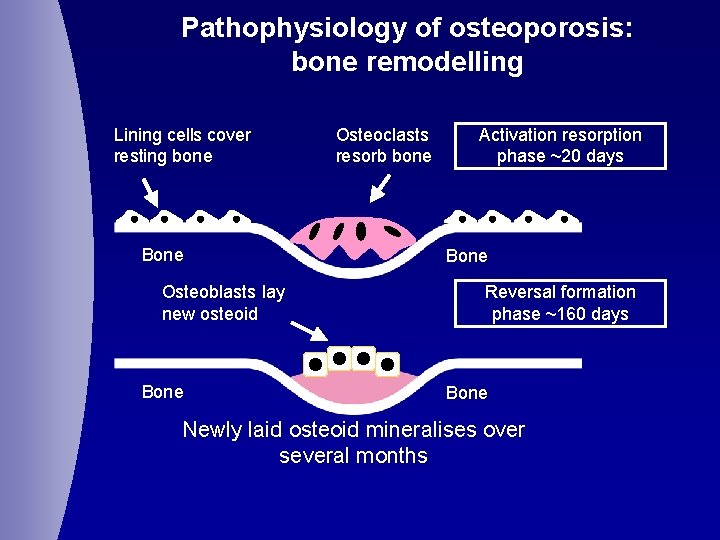
Pathophysiology of osteoporosis: bone remodelling Lining cells cover resting bone Bone Osteoblasts lay new osteoid Bone Osteoclasts resorb bone Activation resorption phase ~20 days Bone Reversal formation phase ~160 days Bone Newly laid osteoid mineralises over several months
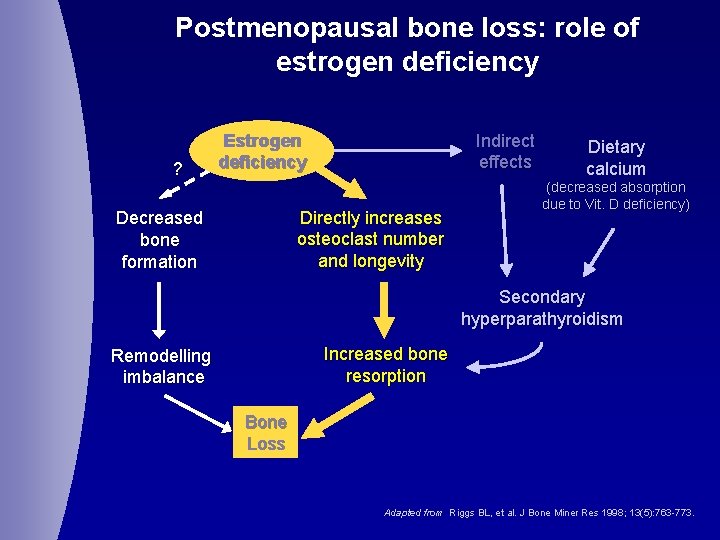
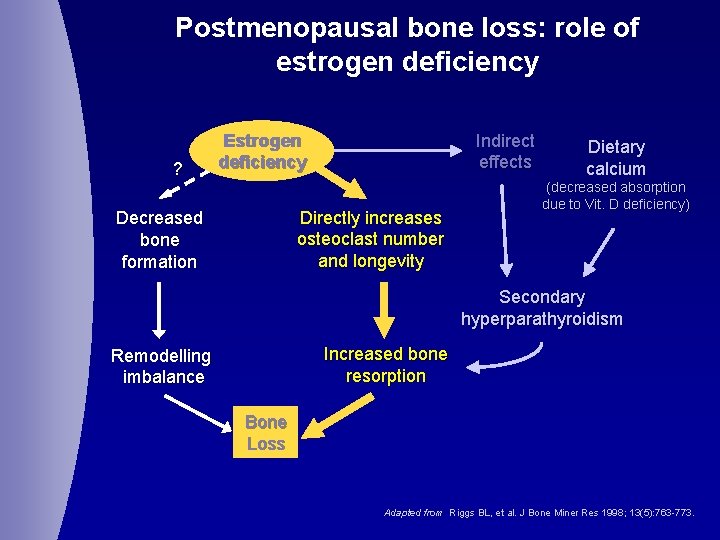
Postmenopausal bone loss: role of estrogen deficiency ? Indirect effects Estrogen deficiency Directly increases osteoclast number and longevity Decreased bone formation Dietary calcium (decreased absorption due to Vit. D deficiency) Secondary hyperparathyroidism Increased bone resorption Remodelling imbalance Bone Loss Adapted from Riggs BL, et al. J Bone Miner Res 1998; 13(5): 763 -773.
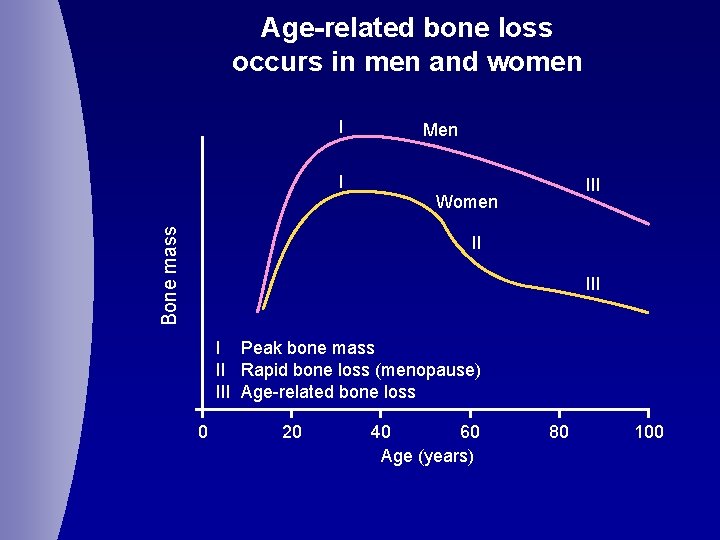
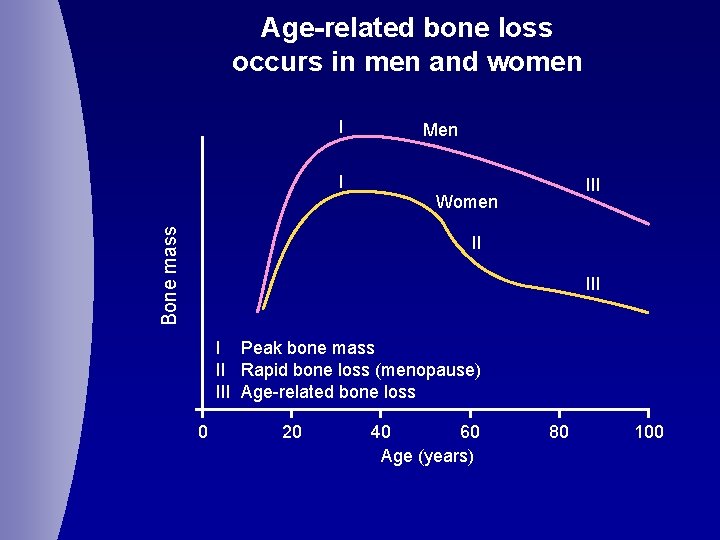
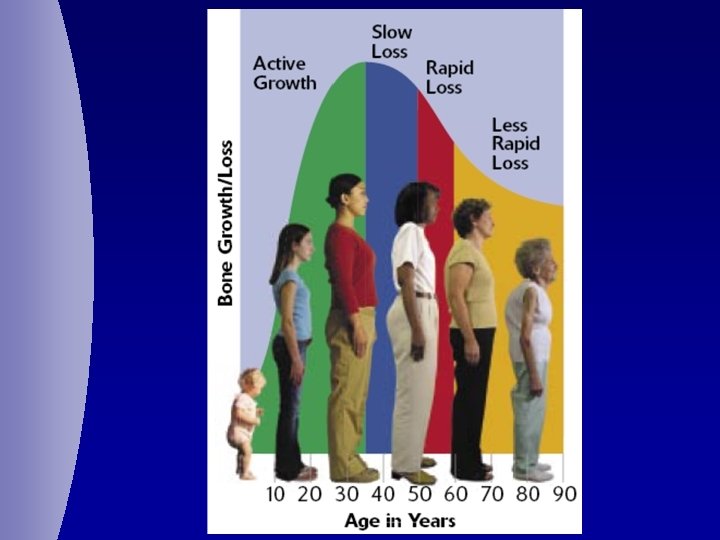
Age-related bone loss occurs in men and women I Bone mass I Men III Women II I Peak bone mass II Rapid bone loss (menopause) III Age-related bone loss 0 20 40 60 Age (years) 80 100
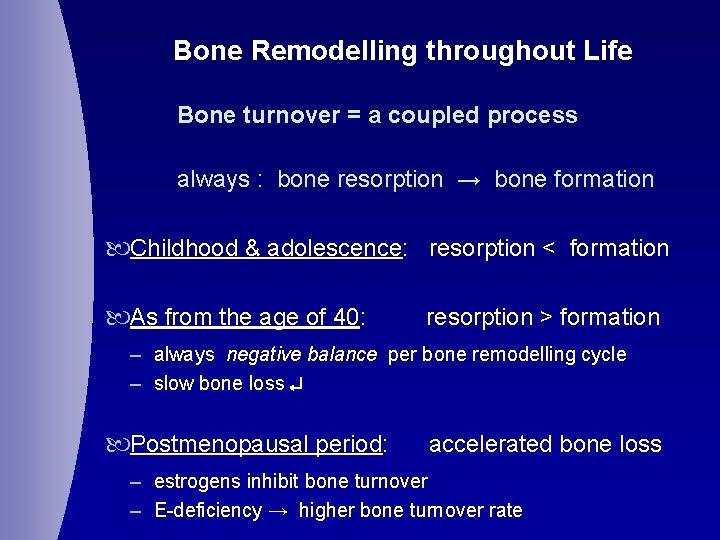
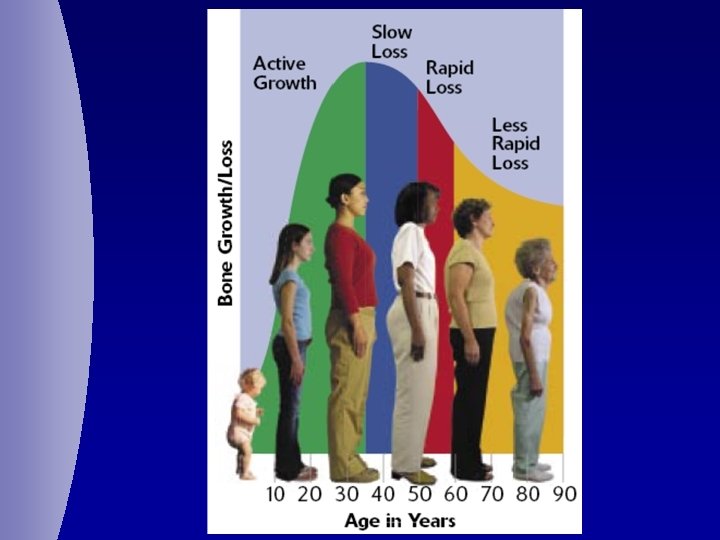
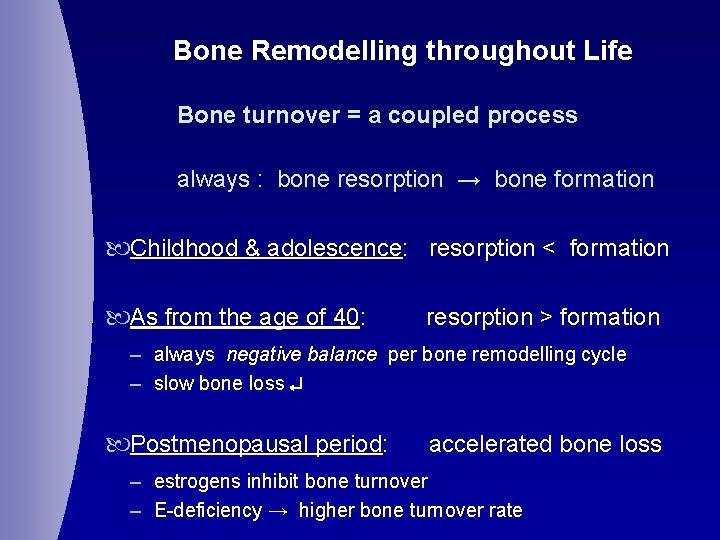
Bone Remodelling throughout Life Bone turnover = a coupled process always : bone resorption → bone formation Childhood & adolescence: resorption < formation As from the age of 40: resorption > formation – always negative balance per bone remodelling cycle – slow bone loss Postmenopausal period: accelerated bone loss – estrogens inhibit bone turnover – E-deficiency → higher bone turnover rate
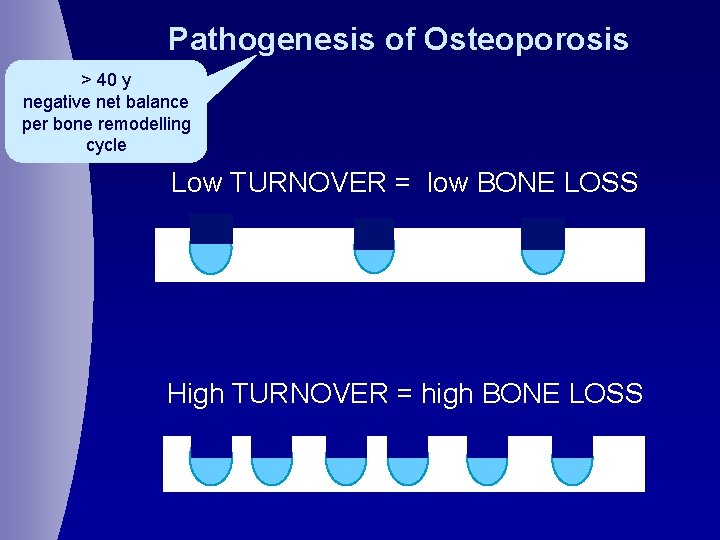
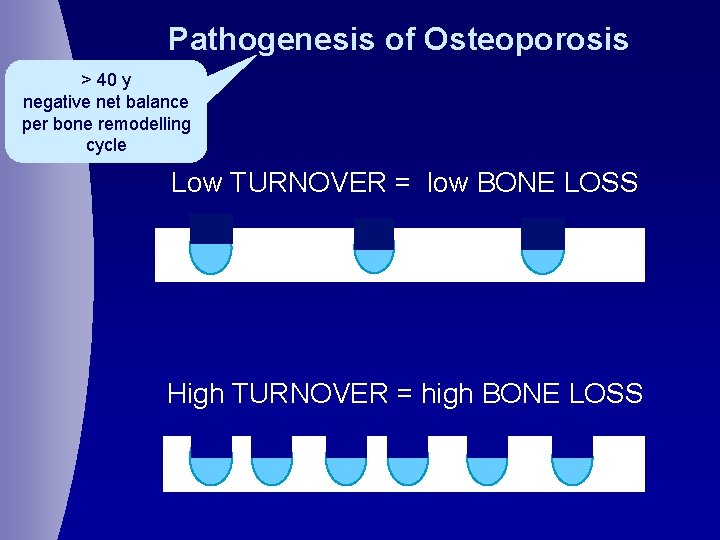
Pathogenesis of Osteoporosis > 40 y negative net balance per bone remodelling cycle Low TURNOVER = low BONE LOSS High TURNOVER = high BONE LOSS
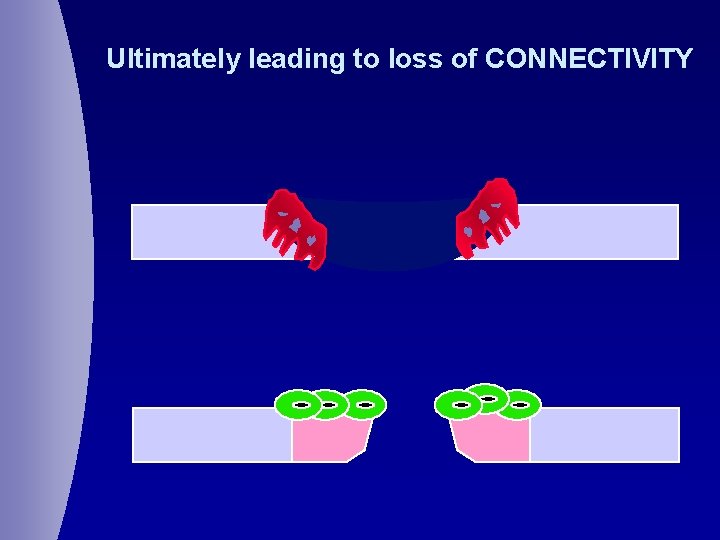
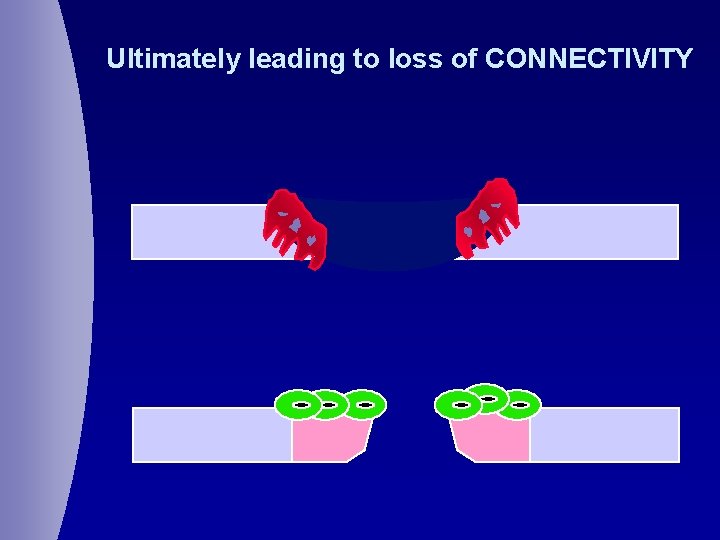
Ultimately leading to loss of CONNECTIVITY
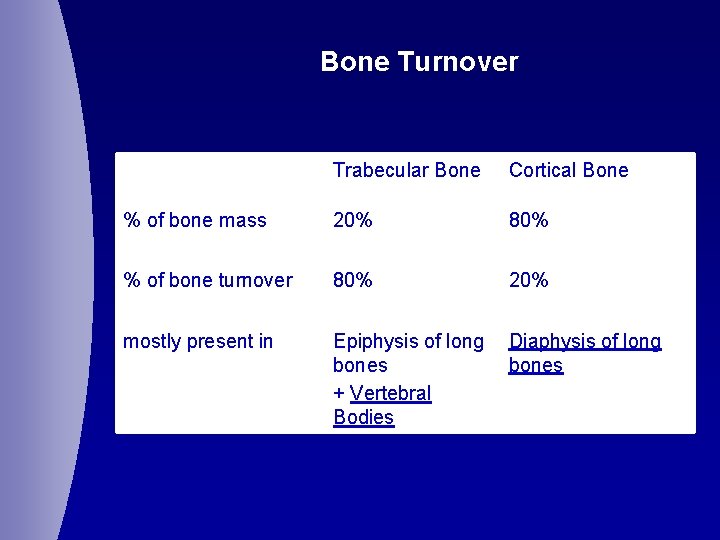
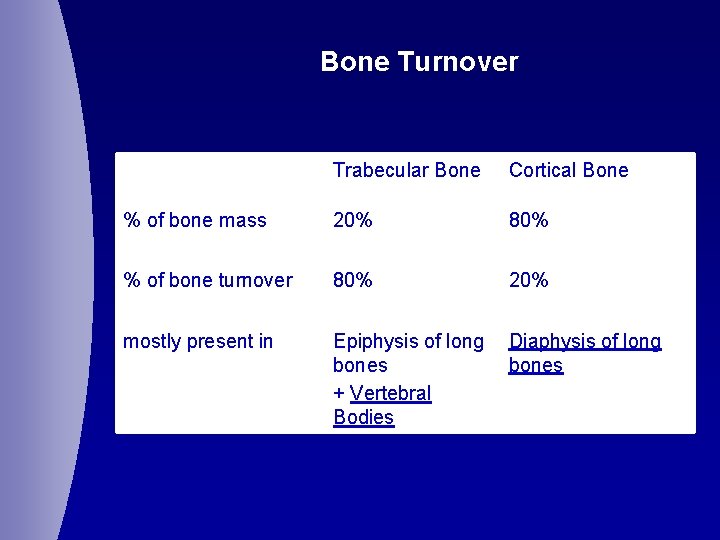
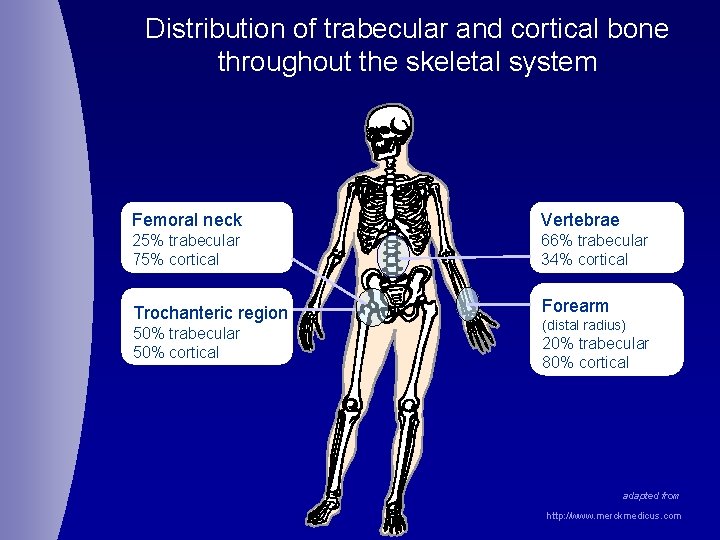
Bone Turnover Trabecular Bone Cortical Bone % of bone mass 20% 80% % of bone turnover 80% 20% mostly present in Epiphysis of long bones + Vertebral Bodies Diaphysis of long bones
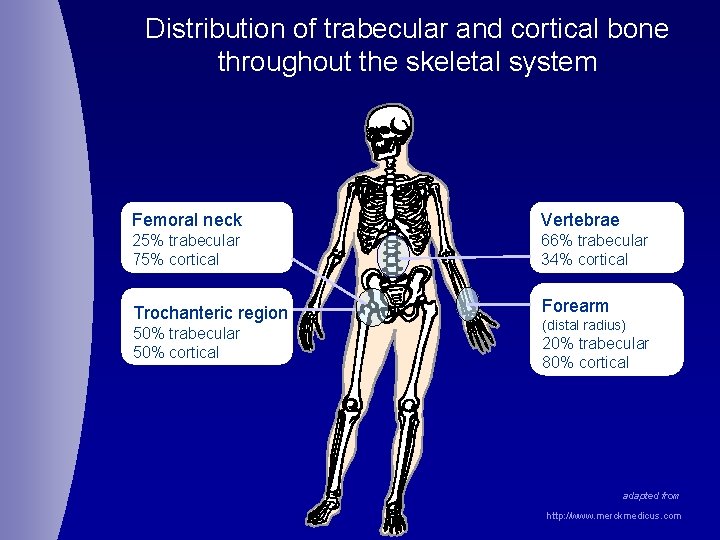
Distribution of trabecular and cortical bone throughout the skeletal system Femoral neck Vertebrae 25% trabecular 75% cortical 66% trabecular 34% cortical Trochanteric region Forearm 50% trabecular 50% cortical (distal radius) 20% trabecular 80% cortical adapted from http: //www. merckmedicus. com
Consequences of Postmenopausal Osteoporosis
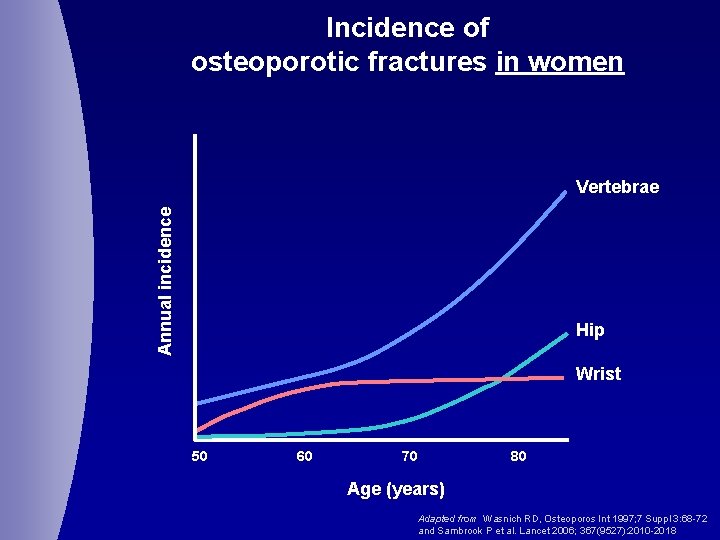
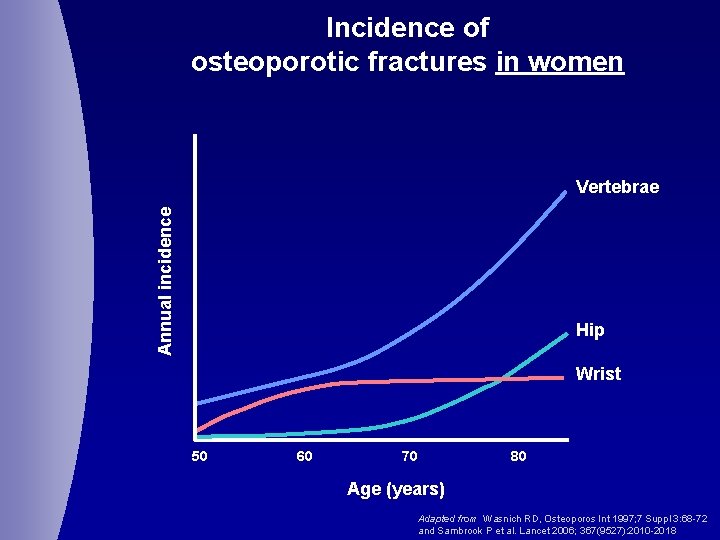
Incidence of osteoporotic fractures in women Annual incidence Vertebrae Hip Wrist 50 60 70 80 Age (years) Adapted from Wasnich RD, Osteoporos Int 1997; 7 Suppl 3: 68 -72 and Sambrook P et al. Lancet 2006; 367(9527): 2010 -2018
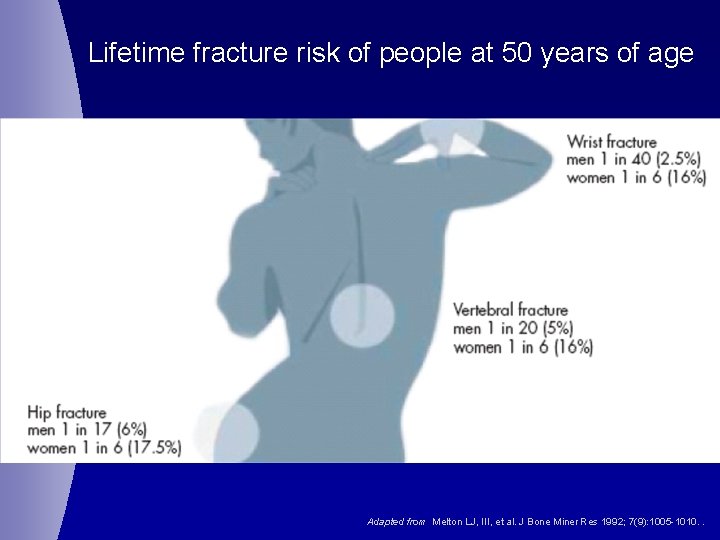
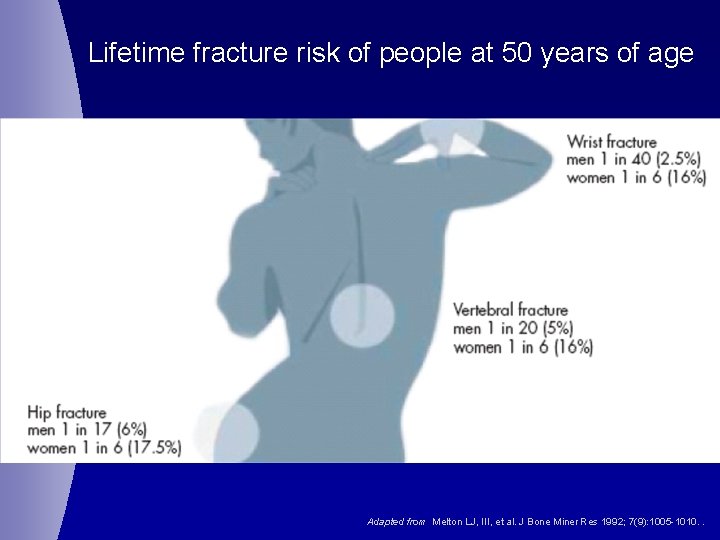
Lifetime fracture risk of people at 50 years of age Adapted from Melton LJ, III, et al. J Bone Miner Res 1992; 7(9): 1005 -1010. .
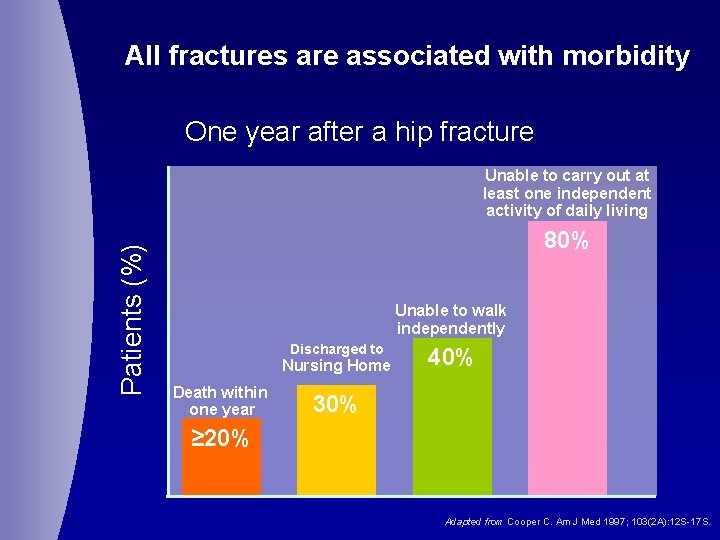
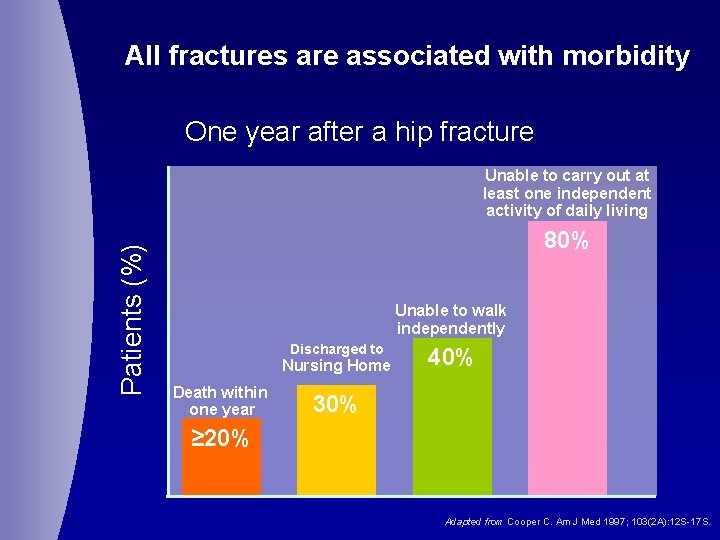
All fractures are associated with morbidity One year after a hip fracture Patients (%) Unable to carry out at least one independent activity of daily living 80% Unable to walk independently Discharged to Nursing Home Death within one year 40% 30% ≥ 20% Adapted from Cooper C. Am J Med 1997; 103(2 A): 12 S-17 S.
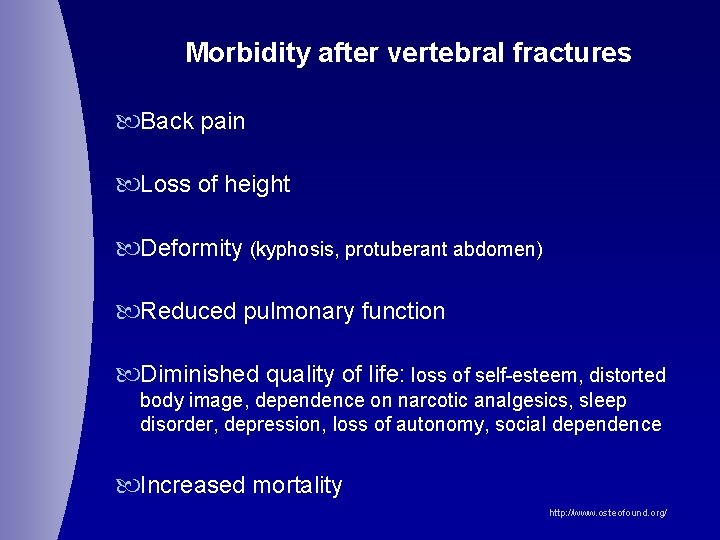
Morbidity after vertebral fractures Back pain Loss of height Deformity (kyphosis, protuberant abdomen) Reduced pulmonary function Diminished quality of life: loss of self-esteem, distorted body image, dependence on narcotic analgesics, sleep disorder, depression, loss of autonomy, social dependence Increased mortality http: //www. osteofound. org/
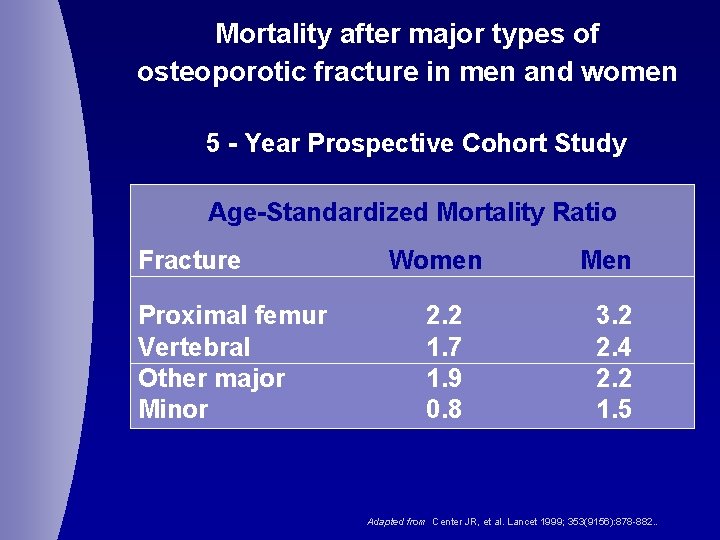
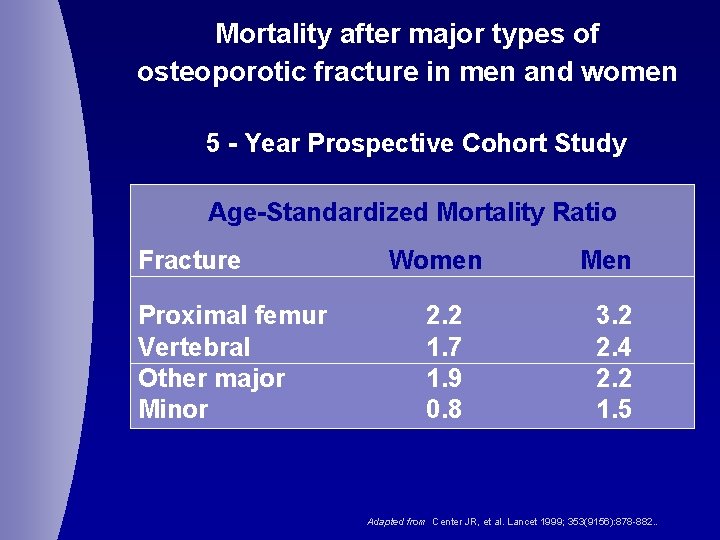
Mortality after major types of osteoporotic fracture in men and women 5 - Year Prospective Cohort Study Age-Standardized Mortality Ratio Fracture Proximal femur Vertebral Other major Minor Women 2. 2 1. 7 1. 9 0. 8 Men 3. 2 2. 4 2. 2 1. 5 Adapted from Center JR, et al. Lancet 1999; 353(9156): 878 -882. .
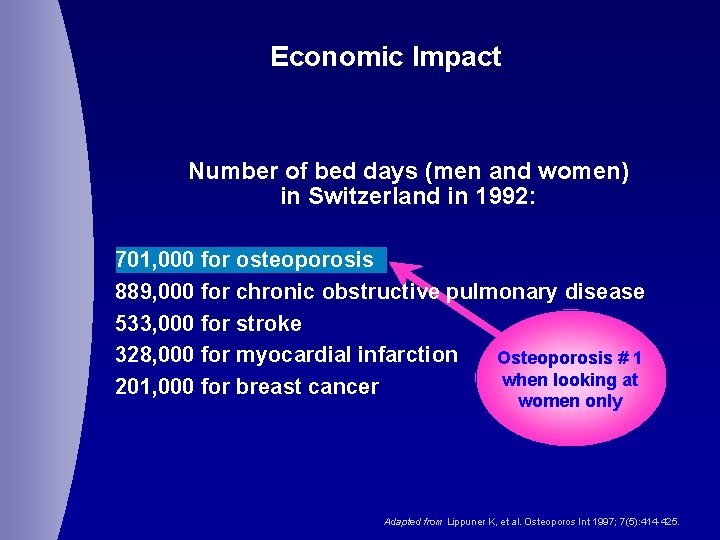
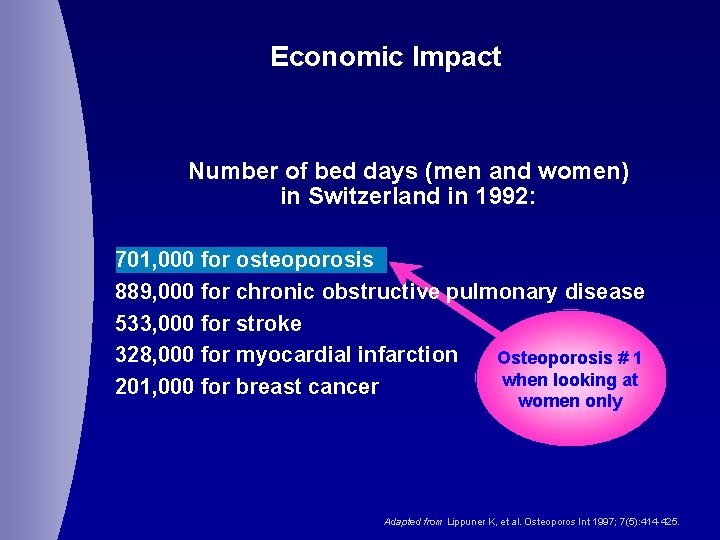
Economic Impact Number of bed days (men and women) in Switzerland in 1992: 701, 000 for osteoporosis 889, 000 for chronic obstructive pulmonary disease 533, 000 for stroke 328, 000 for myocardial infarction Osteoporosis # 1 when looking at 201, 000 for breast cancer women only Adapted from Lippuner K, et al. Osteoporos Int 1997; 7(5): 414 -425.
Risk factors for Osteoporosis ‘Case-finding’
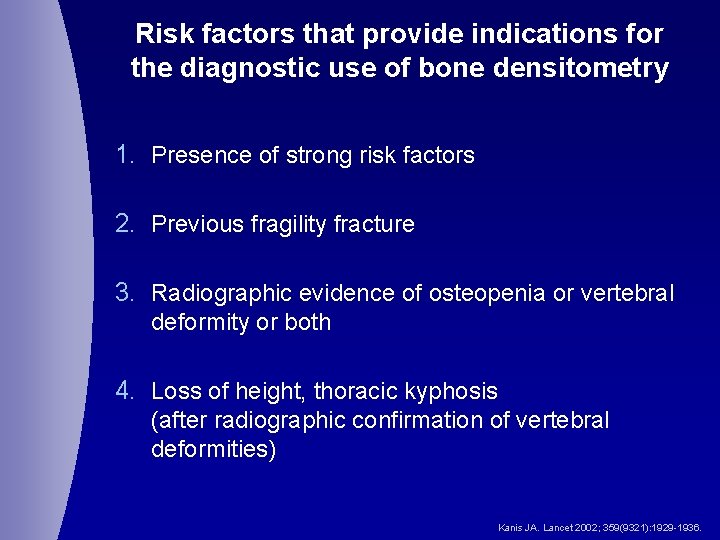
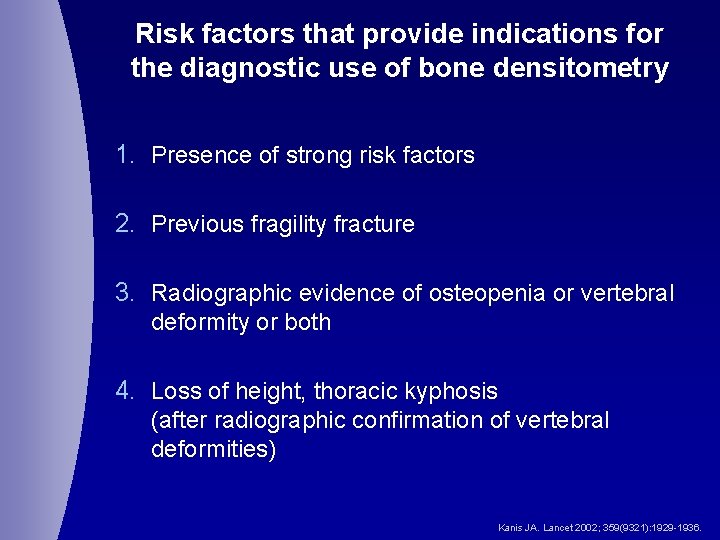
Risk factors that provide indications for the diagnostic use of bone densitometry 1. Presence of strong risk factors 2. Previous fragility fracture 3. Radiographic evidence of osteopenia or vertebral deformity or both 4. Loss of height, thoracic kyphosis (after radiographic confirmation of vertebral deformities) Kanis JA. Lancet 2002; 359(9321): 1929 -1936.
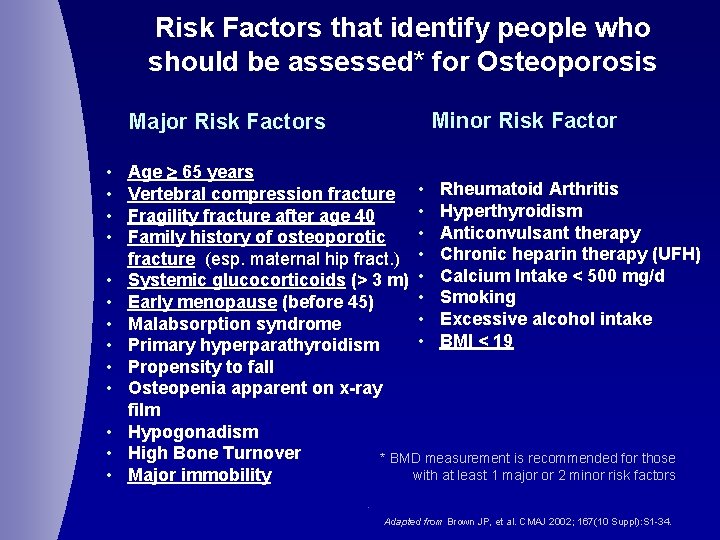
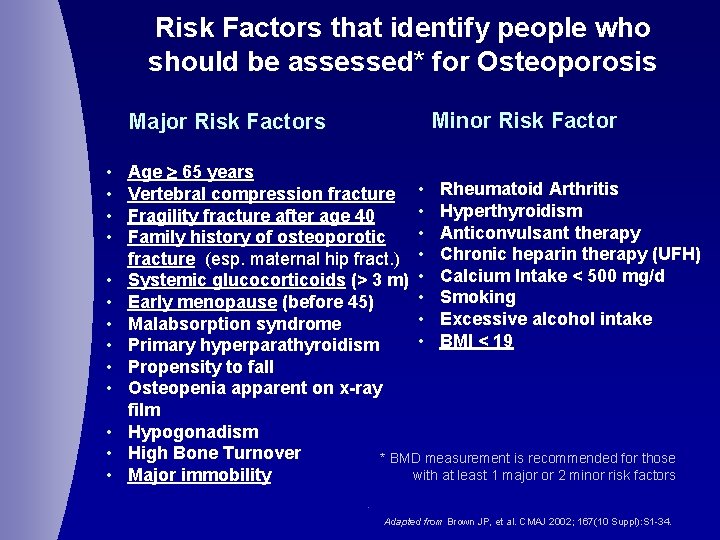
Risk Factors that identify people who should be assessed* for Osteoporosis Minor Risk Factor Major Risk Factors • • • • Age 65 years Vertebral compression fracture • Rheumatoid Arthritis • Hyperthyroidism Fragility fracture after age 40 • Anticonvulsant therapy Family history of osteoporotic fracture (esp. maternal hip fract. ) • Chronic heparin therapy (UFH) Systemic glucocorticoids (> 3 m) • Calcium Intake < 500 mg/d • Smoking Early menopause (before 45) ( • Excessive alcohol intake Malabsorption syndrome • BMI < 19 Primary hyperparathyroidism Propensity to fall Osteopenia apparent on x-ray film Hypogonadism High Bone Turnover * BMD measurement is recommended for those with at least 1 major or 2 minor risk factors Major immobility. Adapted from Brown JP, et al. CMAJ 2002; 167(10 Suppl): S 1 -34.
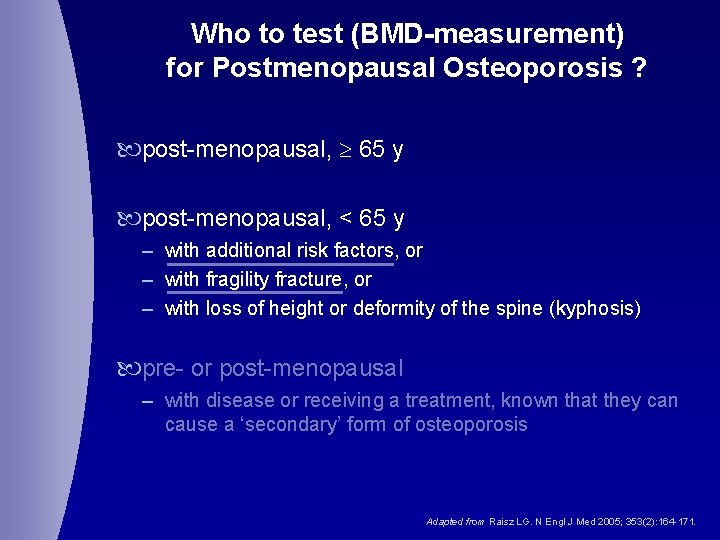
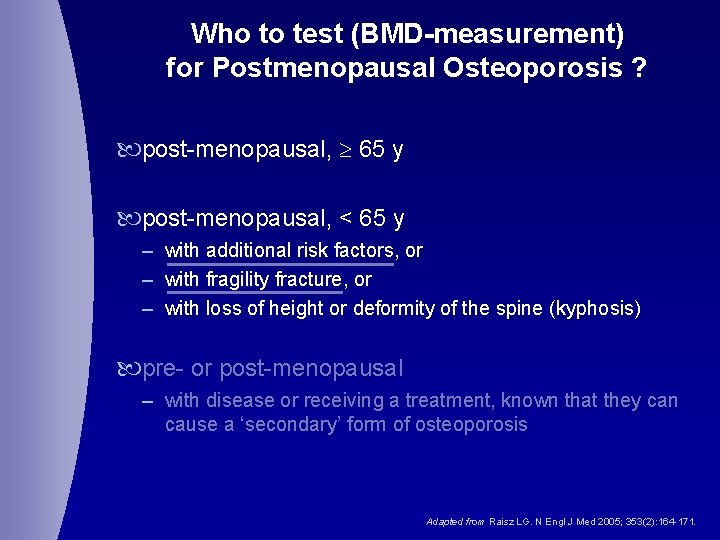
Who to test (BMD-measurement) for Postmenopausal Osteoporosis ? post-menopausal, 65 y post-menopausal, < 65 y – with additional risk factors, or – with fragility fracture, or – with loss of height or deformity of the spine (kyphosis) pre- or post-menopausal – with disease or receiving a treatment, known that they can cause a ‘secondary’ form of osteoporosis Adapted from Raisz LG. N Engl J Med 2005; 353(2): 164 -171.
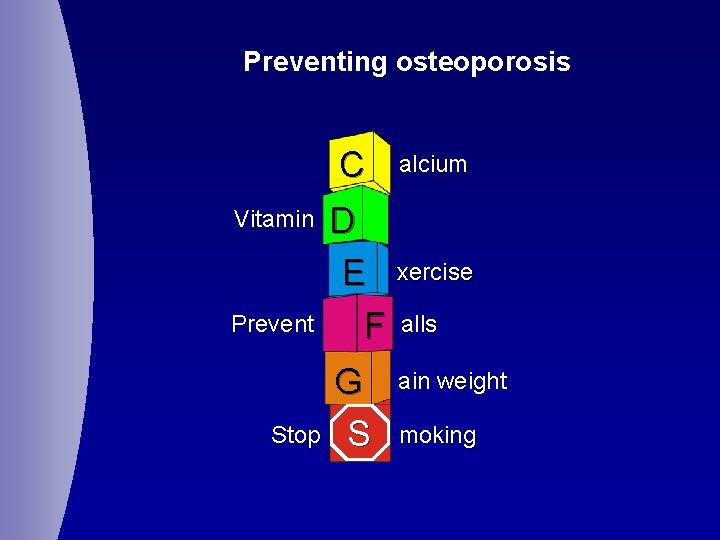
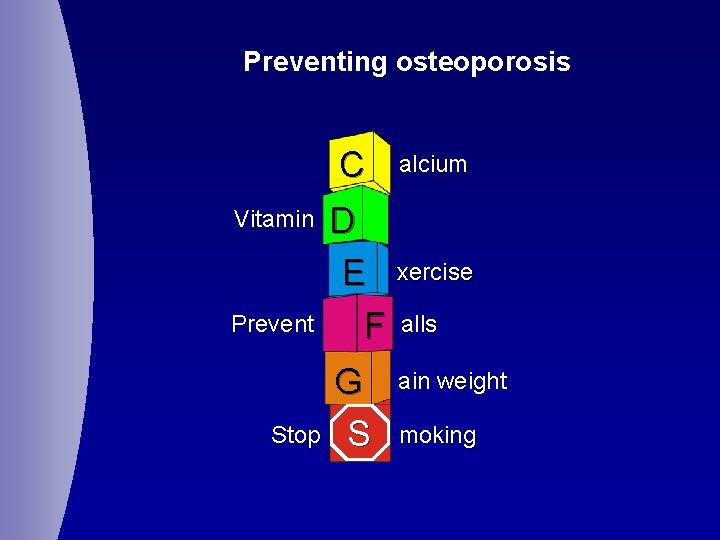
Preventing osteoporosis C Vitamin Prevent Stop alcium D E xercise F alls G S ain weight moking
TREATMENT of OSTEOPOROSIS in order to prevent (new) fractures
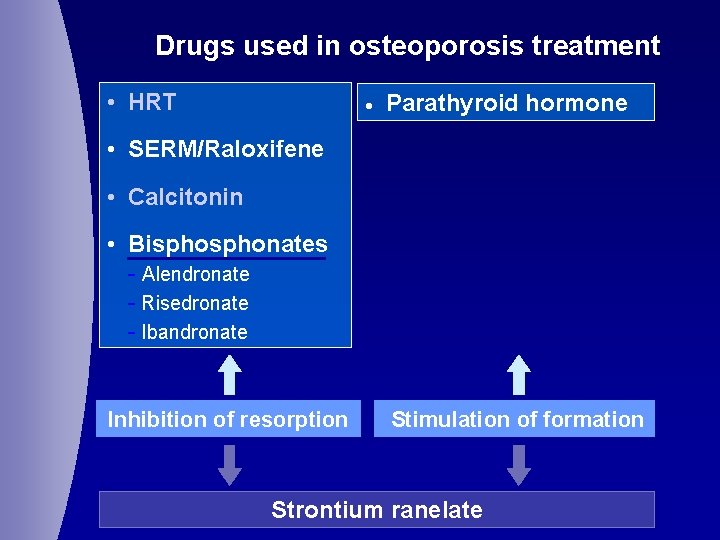
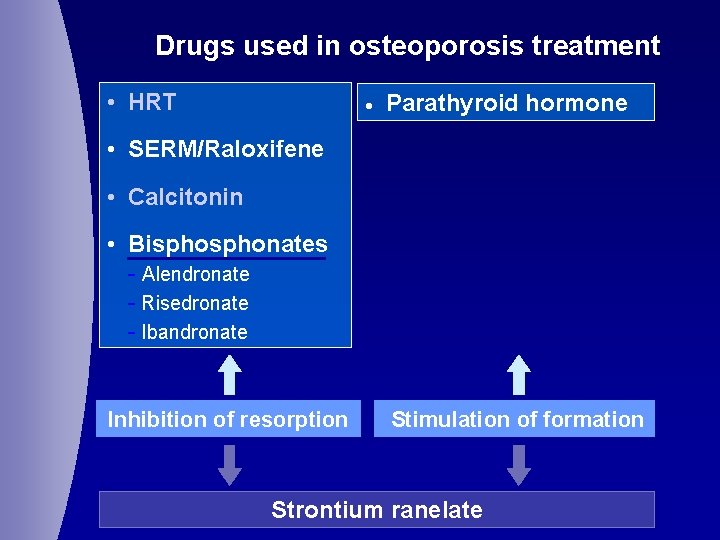
Drugs used in osteoporosis treatment • HRT · Parathyroid hormone • SERM/Raloxifene • Calcitonin • Bisphonates - Alendronate - Risedronate - Ibandronate Inhibition of resorption Stimulation of formation Strontium ranelate
 Definition of underestimated
Definition of underestimated Alendronate mechanism
Alendronate mechanism Osteoporosis
Osteoporosis Bharathi viswanathan
Bharathi viswanathan Pes statement for osteoporosis
Pes statement for osteoporosis Dual energy x ray absorptiometry (dexa)
Dual energy x ray absorptiometry (dexa) Is osteoporosis hypokinetic or hyperkinetic
Is osteoporosis hypokinetic or hyperkinetic Defination of osteoporosis
Defination of osteoporosis Nursing diagnosis for osteoporosis
Nursing diagnosis for osteoporosis Pathway hiperkalemia
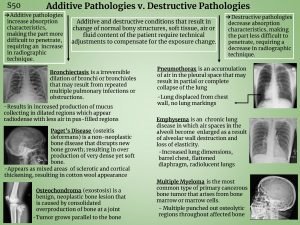
Pathway hiperkalemia Additive pathology
Additive pathology Royal osteoporosis society leaflets
Royal osteoporosis society leaflets Osteoporosis
Osteoporosis Eva decroli
Eva decroli Tbs osteoporosis
Tbs osteoporosis International osteoporosis foundation
International osteoporosis foundation Whole muscle
Whole muscle Periradicular disease
Periradicular disease Bulky desease
Bulky desease Copd exacerbation nursing management
Copd exacerbation nursing management Alzheimer disease definition
Alzheimer disease definition Ulcers in the antrum
Ulcers in the antrum Salpingitis
Salpingitis Dopamine blockers
Dopamine blockers Disease-specific workflows
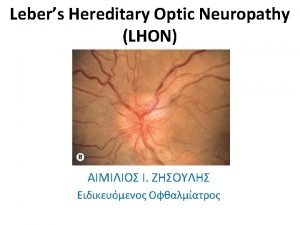
Disease-specific workflows Lhon disease
Lhon disease Gastroenterology board review
Gastroenterology board review Prion disease symptoms
Prion disease symptoms Disease betekenis
Disease betekenis Factors that affect disease transmission
Factors that affect disease transmission Types of diseases
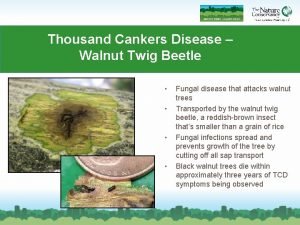
Types of diseases Thousand cankers disease map
Thousand cankers disease map Legg calve perthes disease vs scfe
Legg calve perthes disease vs scfe Deficiency disease of protein
Deficiency disease of protein Raynaud's disease lupus
Raynaud's disease lupus Disease specific mortality rate formula
Disease specific mortality rate formula What causes lungs pain
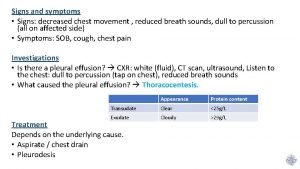
What causes lungs pain