Osteoporosis What is Osteoporosis A disease that causes



- Slides: 21
Osteoporosis

What is Osteoporosis? • A disease that causes bones to become brittle and fragile • Literally means “porous bone” • The consequence of long-term bone demineralization
Who gets it and why? • There are different types of osteoporosis classified by the cause • Primary Osteoporosis: type I and type II • Secondary Osteoporosis
Primary Osteoporosis Type I : Post-menopausal • 25% of Post-menopausal women will develop it • Due to drop in estrogen • Most common between 50 -70 yrs • Incidence increases with age
Primary Osteoporosis Type II: Age Related • Bone loss due to aging process • Men and women generally over 70 yrs

Secondary Osteoporosis May be caused by: • Steroids (corticosteroids) • Anticoagulant • Anticonvulsants • Result of disease or disorders (kidney disease, anorexia, hyperthyroidism) • Impairment of calcium absorption • Immobilization • Inflammatory arthritis
Risk Factors • • Low calcium intake Sedentary lifestyles Tobacco use Being underweight Amenorrhea Estrogen deficiency Decreased bone-mass mineral content, as detected by a bone-mass density test • Genetics/family history
Prevention • Weight bearing exercise (walking is the easiest form) • Important to start during developing years, before 25, to build strong dense bones • Continue into adulthood to prevent density loss • Diet • High calcium and vitamin D to help absorb the calcium • Vitamin supplementation · Maintain appropriate body weight • Being too thin increases risk
Signs of Osteoporosis • • • Decreased height over time Hunched back Broken bones Back pain Tooth loss
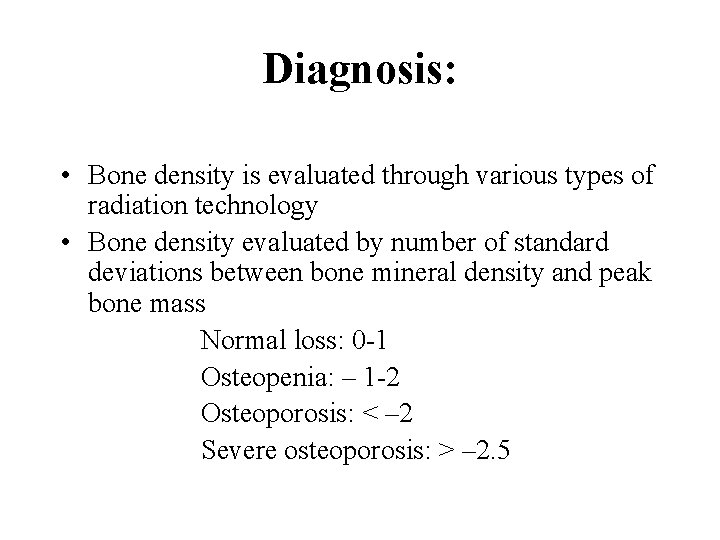
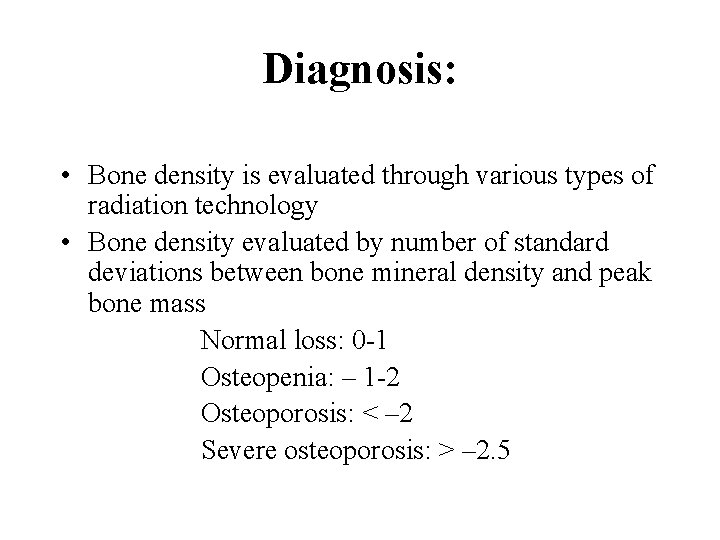
Diagnosis: • Bone density is evaluated through various types of radiation technology • Bone density evaluated by number of standard deviations between bone mineral density and peak bone mass Normal loss: 0 -1 Osteopenia: – 1 -2 Osteoporosis: < – 2 Severe osteoporosis: > – 2. 5

Symptoms of Osteoporosis • • Joint pain swelling Fractures due to minor trauma Bone deformity Debilitation
Treatment • There a wide range of treatment options • Once out of developmental years (past 25 years), reversal is unlikely, but goal is to prevent further loss • Various drug treatments in combination with weigh bearing exercise and dietary adjustments to include vitamin D and calcium are most common
Important Considerations for Physical Activity • Par-Q and medical release must be completed • Adjust loading if osteoporosis is present due to increased risk of fractures (Include resistance often hip or wrist) • Include strength training/weight bearing activity in programs for all ages, in all populations for prevention • Target Extensor groups to prevent common deformity
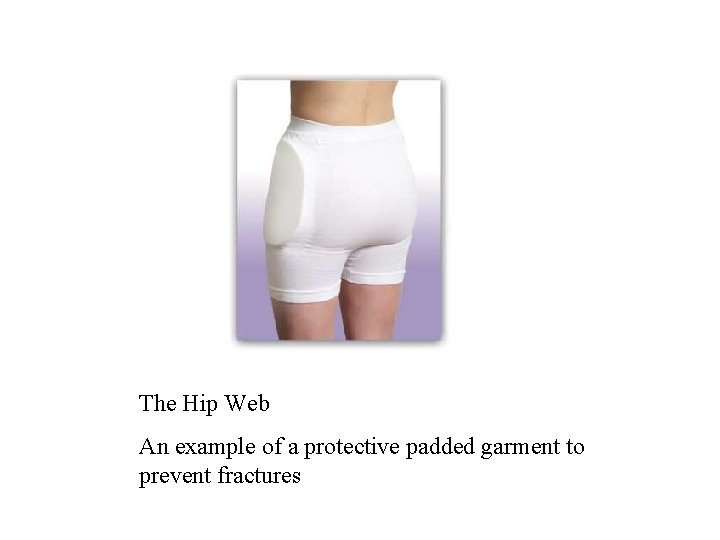
Contraindications to Physical Activity? • It is widely accepted that physical activity helps to prevent further bone loss and helps to increase flexibility, balance, and strength helping to decrease the chance of falls • However, precautions must be taken to avoid fractures: • • • Avoid Twisting and bouncing movements Avoid heavy lifting Use proper lifting technique, even for light loads Stop immediately if pain is experienced Age considerations (older adult population exercise contradictions from pervious week) • Use padded garments
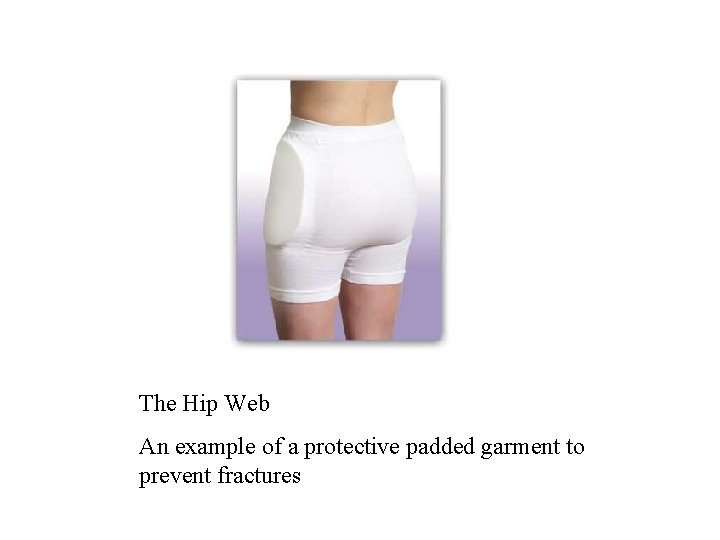
The Hip Web An example of a protective padded garment to prevent fractures
Special Considerations • Although most common in older women, Osteoporosis is not gender or age specific • When prescribing exercise may encounter: • Individuals immobilized for long periods of time • Female athletes • Corticosteroid users
Immobilization • May Cause Disuse Osteoporosis • Long term immobilization may cause degeneration of bone • Due to limited weight bearing and muscle activity • Bone loss can be detected as early as 2 weeks after immobilization • Prevention: • Isotonic and isometric exercises during immobilization • Treatment: • Losses may be regained after remobilization with increased weight bearing exercise
Female Athletes The Female Triad • Triad of disorders commonly found in young female athletes • Disordered Eating, Amenorrhea, Osteoporosis • Most common in sports requiring ideal body weight (gymnastics, figure skating, cross-country running, diving, swimming, and ballet) • Does not only effect female athletes • Usually caused by desire to be ultra thin to improve performance or physical appearance
Female Athletes • How it works: • Eating disorders cause amenorrhea and lack of minerals and vitamins for bone growth • Amenorrhea with continued lack of vitamin intake accelerates bone loss causing osteoporosis • Prevention: • • • Education Early recognition of eating disorder Counseling Monitor body weight (maintain healthy weight) Supplementation
Corticosteroids • What are they? • Drugs used to alleviate swelling, redness, warmth, and pain or joints or organs • Who uses them? • Most commonly arthritics and asthmatics • Adverse Effects: • Long term use may cause sever bone density loss • Up to 7. 5 mg/day for 6 months may decrease trabecular bone volume up to 20%, with continued but slower loss if longer use • Side effects are not age specific
References Anderson, Hall, and Martin. (2005). Foundations of Athletic Training: Prevention, assessment, and management(3 rd ed). Pennsylvania: Lippincott Williams & Wilkins Black, J. M. , Hawks, J. H. (2005). Medical-surgical nursing: Clinical Management for positive outcomes (7 th ed. ). Missouri: W. B. Saunders. Earle RW, and Baechle TR. (2004). NSCA’s essentials of personal training. Windsor: Human Kinetics. Jordan, K. , Cooper, C. (2002). Epidemiology of Osteoporosis. Best Practice & Research Clinical Rheumatology, 16(5), 803. Klippel, JH (Ed. ) (1997). Primer on the Rheumatic Diseases(11 th ed). Georga: Arthritis Foundation. The Osteoporosis Society of Canada. (2005). About Osteoporosis. Retrieved February 23, 2005, from http: //www. osteoporosis. ca/english/about%20 osteoporosis/default. asp? s=1 The Osteoporosis Society of Canada. (2005). Programs and Resources. Retrieved February 23, 2005, from http: //www. osteoporosis. ca/english/program%20 and%20 resources/default. asp? s=1 Minister of Public Works and Government Services Canada. (2001). Osteoporosis Info-Sheet for Seniors. Retrieved February 23, 2005, from http: //www. phac-aspc. gc. ca/seniorsaines/pubs/info_sheets/osteoporosis/osteo_e. htm
 Con hãy đưa tay khi thấy người vấp ngã
Con hãy đưa tay khi thấy người vấp ngã Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Tôn thất thuyết là ai
Tôn thất thuyết là ai Phân độ lown ngoại tâm thu
Phân độ lown ngoại tâm thu Chiến lược kinh doanh quốc tế của walmart
Chiến lược kinh doanh quốc tế của walmart Gây tê cơ vuông thắt lưng
Gây tê cơ vuông thắt lưng Block xoang nhĩ
Block xoang nhĩ Tìm vết của đường thẳng
Tìm vết của đường thẳng Sau thất bại ở hồ điển triệt
Sau thất bại ở hồ điển triệt Thể thơ truyền thống
Thể thơ truyền thống Bharathi viswanathan
Bharathi viswanathan Upper lobe blood diversion
Upper lobe blood diversion Economic importance of radiolarians
Economic importance of radiolarians Causes of valvular heart disease
Causes of valvular heart disease Dopamine uses
Dopamine uses Food poisoning cause
Food poisoning cause Parkinson's disease causes
Parkinson's disease causes Site:slidetodoc.com
Site:slidetodoc.com Rheumatic heart disease causes
Rheumatic heart disease causes What causes addisons disease
What causes addisons disease Giardia causes what disease
Giardia causes what disease Proximate and ultimate causes of behaviour
Proximate and ultimate causes of behaviour