CHAPTER I Osteoporosis evaluation of risks Osteoporosis evaluation
- Slides: 20
CHAPTER I Osteoporosis: evaluation of risks
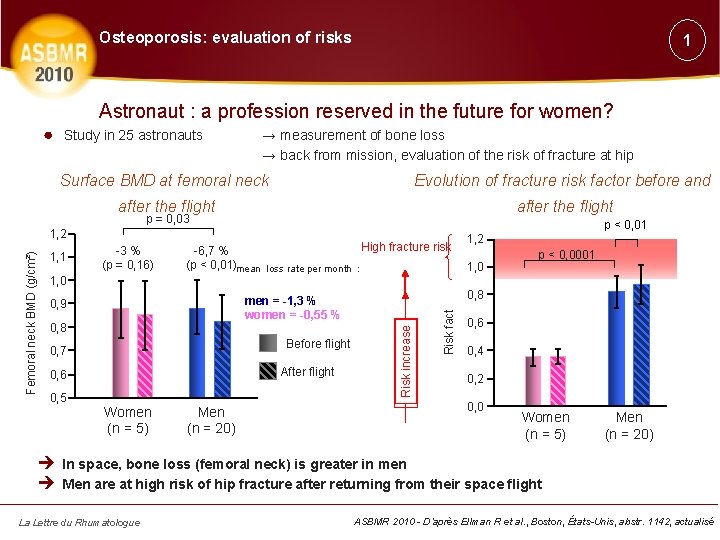
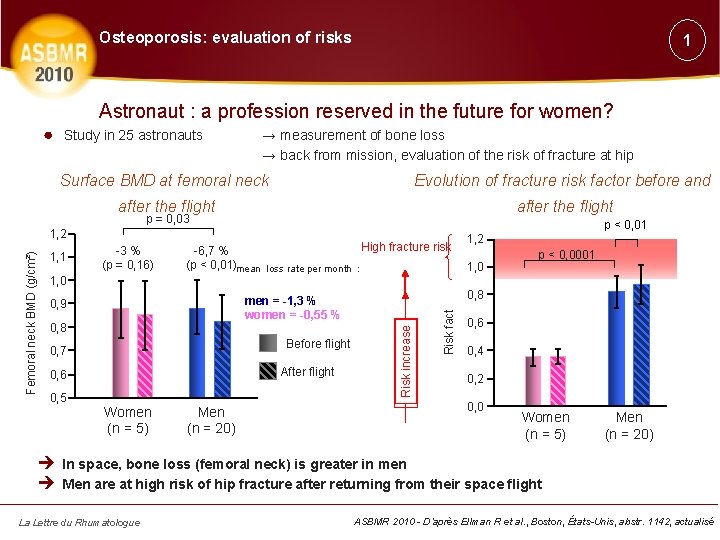
Osteoporosis: evaluation of risks 1 Astronaut : a profession reserved in the future for women? ● Study in 25 astronauts → measurement of bone loss → back from mission, evaluation of the risk of fracture at hip Surface BMD at femoral neck Evolution of fracture risk factor before and after the flight p = 0, 03 -3 % (p = 0, 16) 1, 0 High fracture risk -6, 7 % (p < 0, 01)mean loss rate per month : 0, 8 Before flight 0, 7 After flight 0, 6 0, 5 Women (n = 5) Men (n = 20) 1, 2 1, 0 p < 0, 0001 0, 8 men = -1, 3 % women = -0, 55 % 0, 9 Risk fact 1, 1 p < 0, 01 Increasing risk Risk increase Femoral neck BMD (g/cm²) 1, 2 0, 6 0, 4 0, 2 0, 0 Women (n = 5) Men (n = 20) è In space, bone loss (femoral neck) is greater in men è Men are at high risk of hip fracture after returning from their space flight La Lettre du Rhumatologue ASBMR 2010 - D’après Ellman R et al. , Boston, États-Unis, abstr. 1142, actualisé
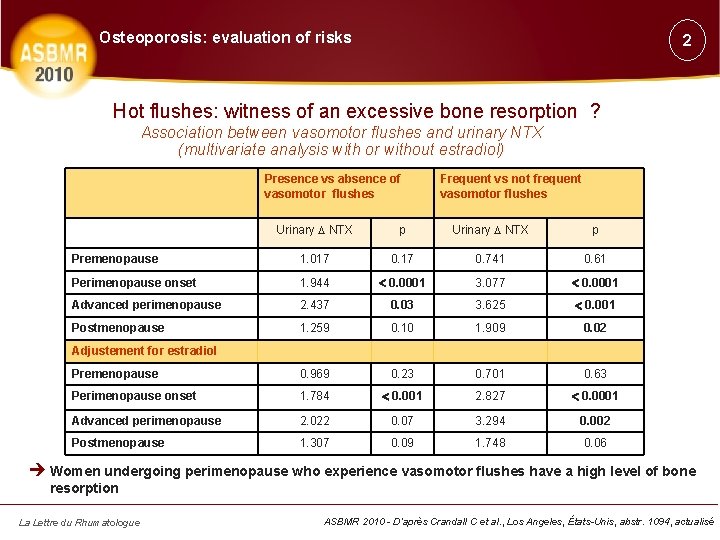
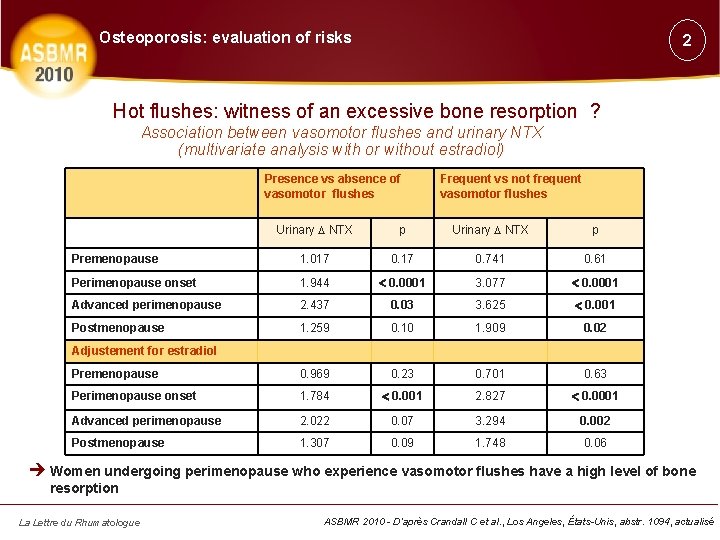
Osteoporosis: evaluation of risks 2 Hot flushes: witness of an excessive bone resorption ? Association between vasomotor flushes and urinary NTX (multivariate analysis with or without estradiol) Presence vs absence of vasomotor flushes Frequent vs not frequent vasomotor flushes Urinary NTX p Premenopause 1. 017 0. 741 0. 61 Perimenopause onset 1. 944 0. 0001 3. 077 0. 0001 Advanced perimenopause 2. 437 0. 03 3. 625 0. 001 Postmenopause 1. 259 0. 10 1. 909 0. 02 Premenopause 0. 969 0. 23 0. 701 0. 63 Perimenopause onset 1. 784 0. 001 2. 827 0. 0001 Advanced perimenopause 2. 022 0. 07 3. 294 0. 002 Postmenopause 1. 307 0. 09 1. 748 0. 06 Adjustement for estradiol è Women undergoing perimenopause who experience vasomotor flushes have a high level of bone resorption La Lettre du Rhumatologue ASBMR 2010 - D’après Crandall C et al. , Los Angeles, États-Unis, abstr. 1094, actualisé
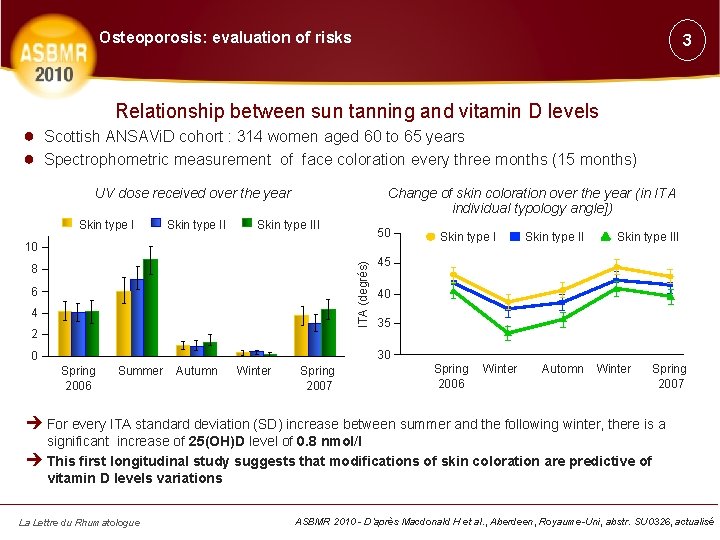
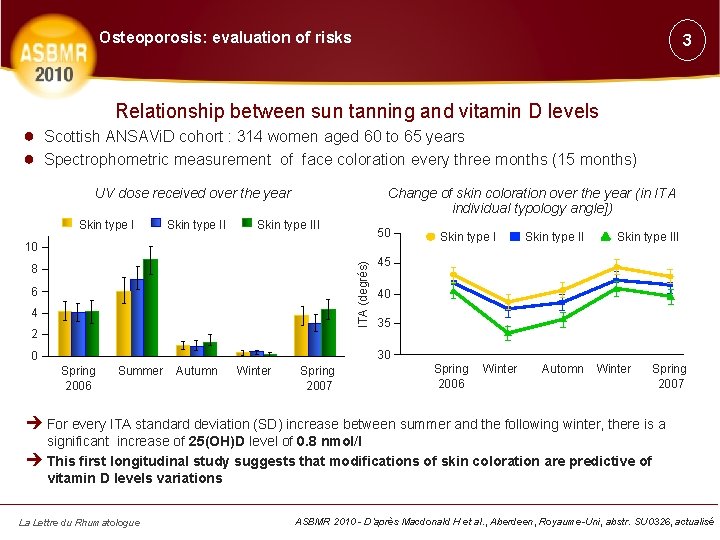
Osteoporosis: evaluation of risks 3 Relationship between sun tanning and vitamin D levels ● Scottish ANSAVi. D cohort : 314 women aged 60 to 65 years ● Spectrophometric measurement of face coloration every three months (15 months) UV dose received over the year Skin type II Change of skin coloration over the year (in ITA individual typology angle]) Skin type III 50 ITA (degrés) 10 8 6 4 2 Skin type III 45 40 35 30 0 Spring 2006 Summer Autumn Winter Spring 2007 Spring 2006 Winter Automn Winter Spring 2007 è For every ITA standard deviation (SD) increase between summer and the following winter, there is a significant increase of 25(OH)D level of 0. 8 nmol/l è This first longitudinal study suggests that modifications of skin coloration are predictive of vitamin D levels variations La Lettre du Rhumatologue ASBMR 2010 - D’après Macdonald H et al. , Aberdeen, Royaume-Uni, abstr. SU 0326, actualisé
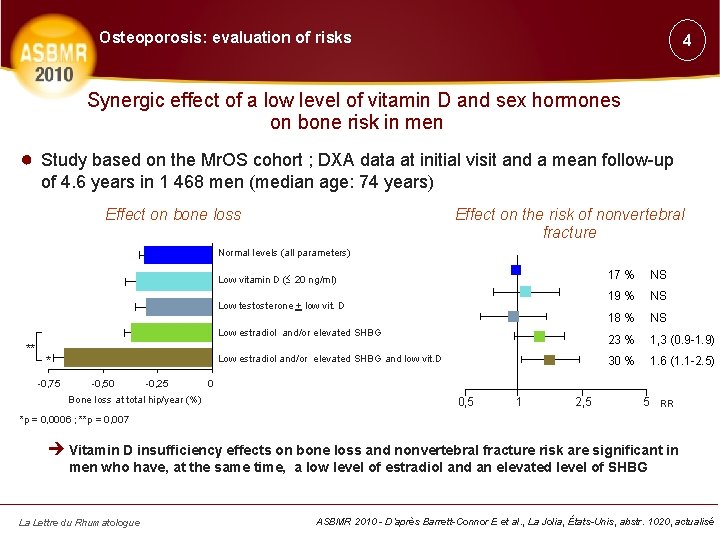
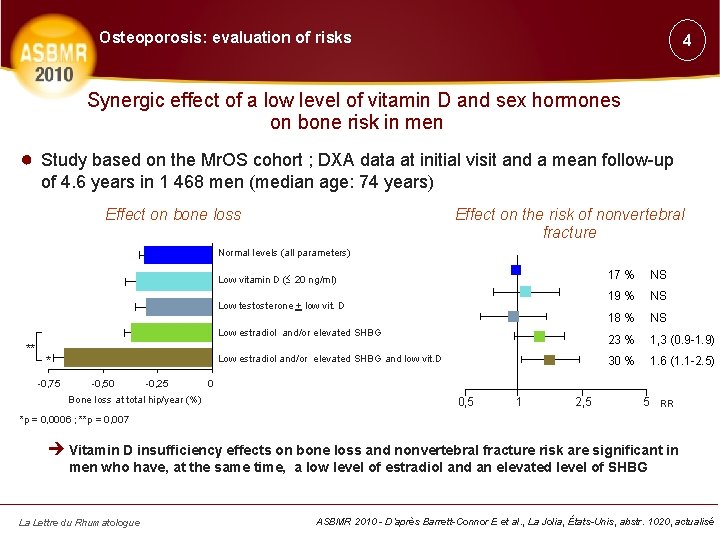
Osteoporosis: evaluation of risks 4 Synergic effect of a low level of vitamin D and sex hormones on bone risk in men ● Study based on the Mr. OS cohort ; DXA data at initial visit and a mean follow-up of 4. 6 years in 1 468 men (median age: 74 years) Effect on bone loss Effect on the risk of nonvertebral fracture Normal levels (all parameters) Low vitamin D ( 20 ng/ml) Low testosterone + low vit. D Low estradiol and/or elevated SHBG ** Low estradiol and/or elevated SHBG and low vit. D * -0, 75 -0, 50 -0, 25 Bone loss at total hip/year (%) 17 % NS 19 % NS 18 % NS 23 % 1, 3 (0. 9 -1. 9) 30 % 1. 6 (1. 1 -2. 5) 0 0, 5 1 2, 5 5 RR *p = 0, 0006 ; **p = 0, 007 è Vitamin D insufficiency effects on bone loss and nonvertebral fracture risk are significant in men who have, at the same time, a low level of estradiol and an elevated level of SHBG La Lettre du Rhumatologue ASBMR 2010 - D’après Barrett-Connor E et al. , La Jolia, États-Unis, abstr. 1020, actualisé
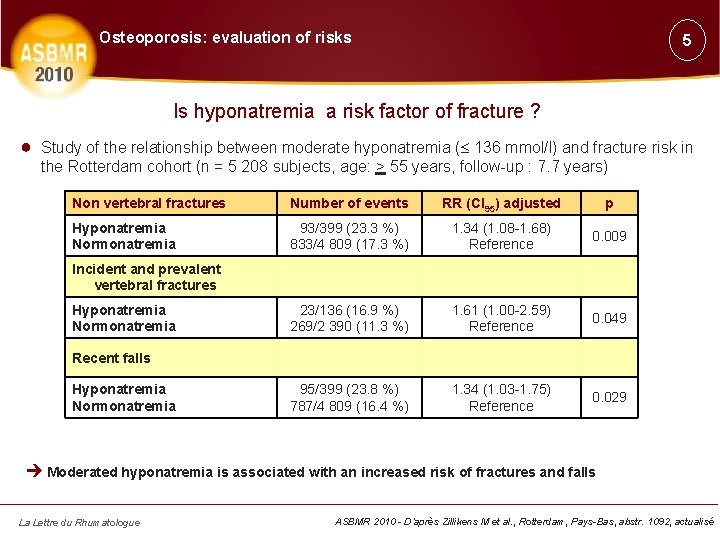
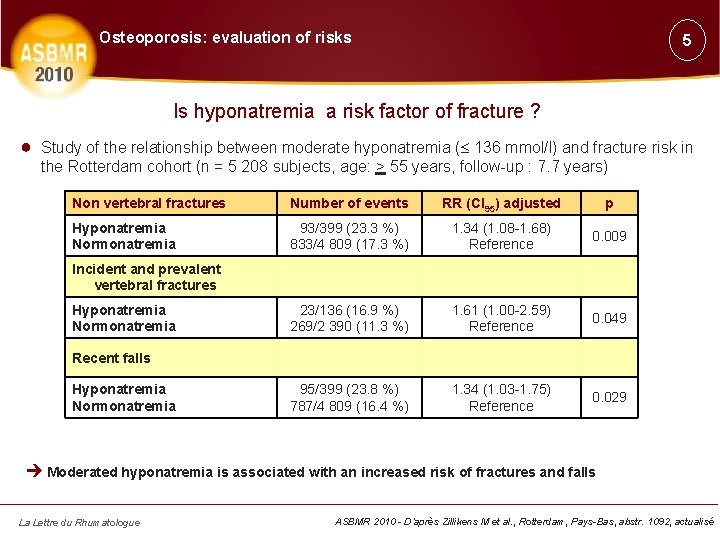
Osteoporosis: evaluation of risks 5 Is hyponatremia a risk factor of fracture ? ● Study of the relationship between moderate hyponatremia ( 136 mmol/l) and fracture risk in the Rotterdam cohort (n = 5 208 subjects, age: > 55 years, follow-up : 7. 7 years) Non vertebral fractures Number of events RR (CI 95) adjusted p Hyponatremia Normonatremia 93/399 (23. 3 %) 833/4 809 (17. 3 %) 1. 34 (1. 08 -1. 68) Reference 0. 009 23/136 (16. 9 %) 269/2 390 (11. 3 %) 1. 61 (1. 00 -2. 59) Reference 0. 049 95/399 (23. 8 %) 787/4 809 (16. 4 %) 1. 34 (1. 03 -1. 75) Reference 0. 029 Incident and prevalent vertebral fractures Hyponatremia Normonatremia Recent falls Hyponatremia Normonatremia è Moderated hyponatremia is associated with an increased risk of fractures and falls La Lettre du Rhumatologue ASBMR 2010 - D’après Zillikens M et al. , Rotterdam, Pays-Bas, abstr. 1092, actualisé
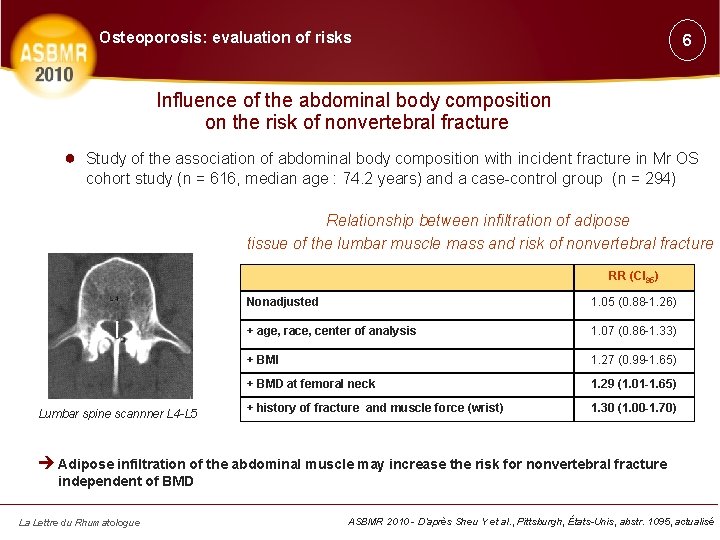
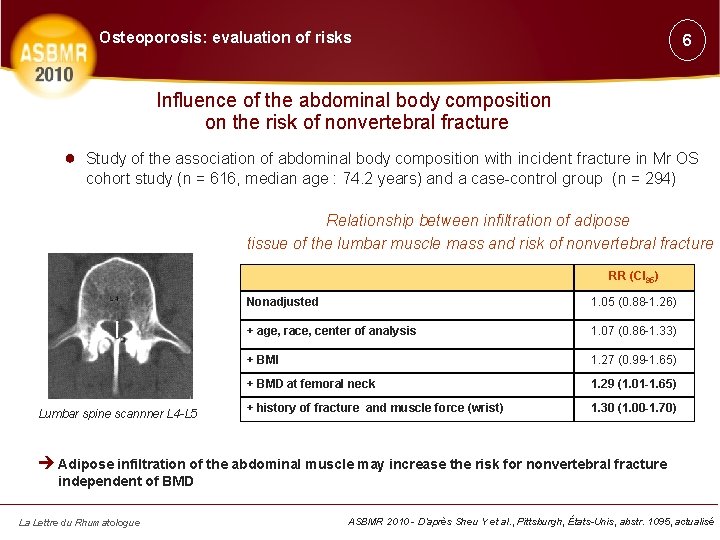
Osteoporosis: evaluation of risks 6 Influence of the abdominal body composition on the risk of nonvertebral fracture ● Study of the association of abdominal body composition with incident fracture in Mr OS cohort study (n = 616, median age : 74. 2 years) and a case-control group (n = 294) Relationship between infiltration of adipose tissue of the lumbar muscle mass and risk of nonvertebral fracture RR (CI 95) Lumbar spine scannner L 4 -L 5 Nonadjusted 1. 05 (0. 88 -1. 26) + age, race, center of analysis 1. 07 (0. 86 -1. 33) + BMI 1. 27 (0. 99 -1. 65) + BMD at femoral neck 1. 29 (1. 01 -1. 65) + history of fracture and muscle force (wrist) 1. 30 (1. 00 -1. 70) è Adipose infiltration of the abdominal muscle may increase the risk for nonvertebral fracture independent of BMD La Lettre du Rhumatologue ASBMR 2010 - D’après Sheu Y et al. , Pittsburgh, États-Unis, abstr. 1095, actualisé
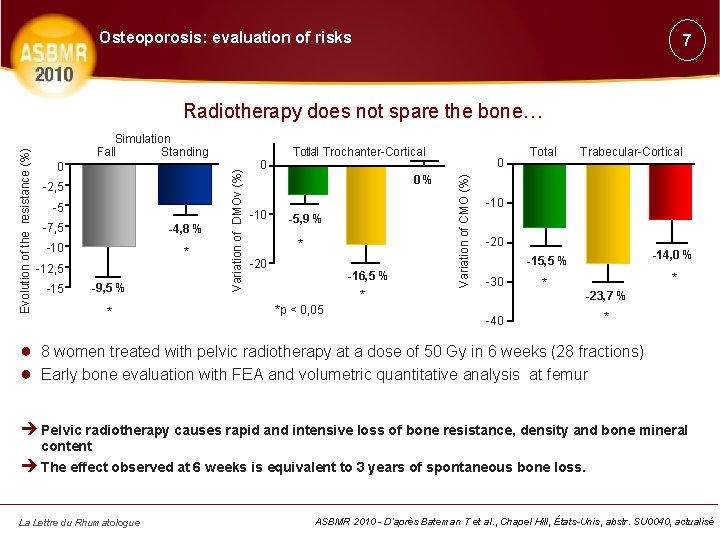
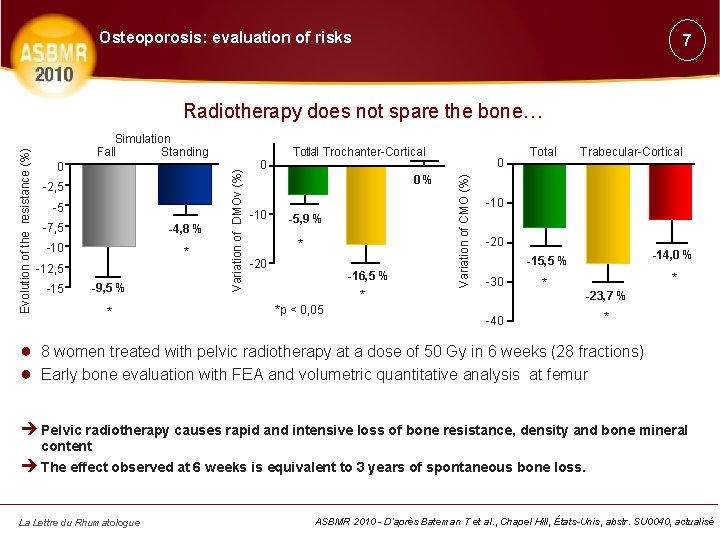
Osteoporosis: evaluation of risks 7 0 -2, 5 -5 -7, 5 -4, 8 % -10 * -12, 5 -15 -9, 5 % * 0 Total l l Trochanter-Cortical 0% -10 -5, 9 % * -20 -16, 5 % * *p < 0, 05 0 Variation of CMO (%) Simulation Fall Standing Variation of DMOv (%) Evolution of the resistance (%) Radiotherapy does not spare the bone… Total Trabecular-Cortical -10 -20 -30 -15, 5 % -14, 0 % * * -40 -23, 7 % * ● 8 women treated with pelvic radiotherapy at a dose of 50 Gy in 6 weeks (28 fractions) ● Early bone evaluation with FEA and volumetric quantitative analysis at femur è Pelvic radiotherapy causes rapid and intensive loss of bone resistance, density and bone mineral content è The effect observed at 6 weeks is equivalent to 3 years of spontaneous bone loss. La Lettre du Rhumatologue ASBMR 2010 - D’après Bateman T et al. , Chapel Hill, États-Unis, abstr. SU 0040, actualisé
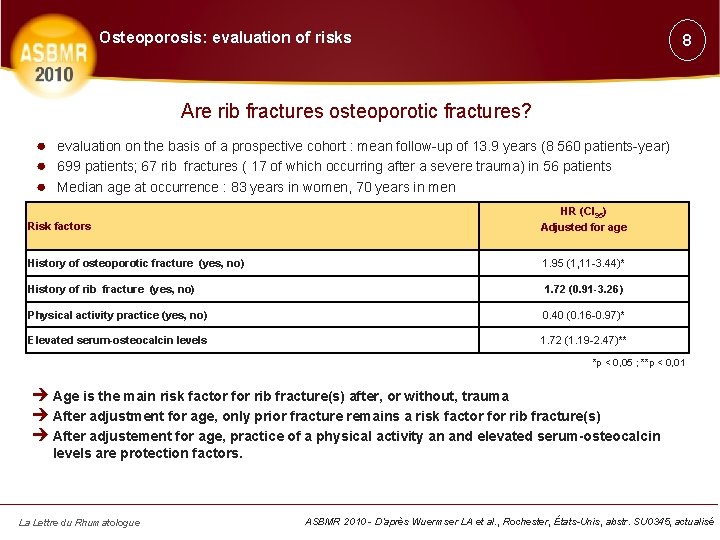
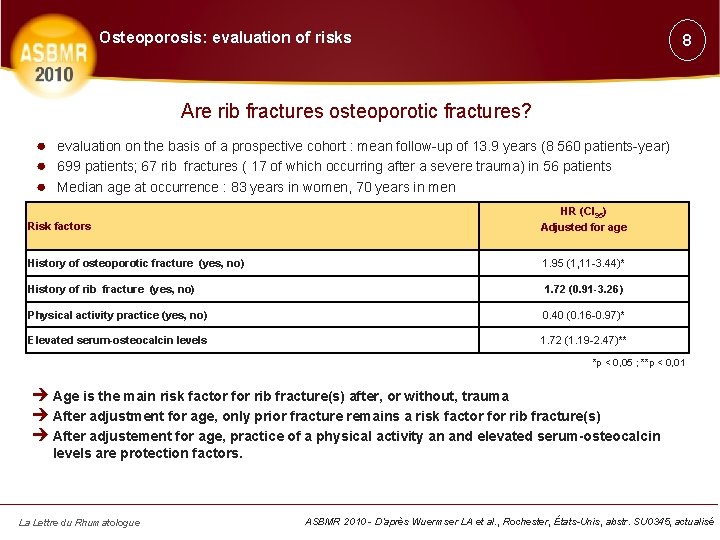
Osteoporosis: evaluation of risks 8 Are rib fractures osteoporotic fractures? ● evaluation on the basis of a prospective cohort : mean follow-up of 13. 9 years (8 560 patients-year) ● 699 patients; 67 rib fractures ( 17 of which occurring after a severe trauma) in 56 patients ● Median age at occurrence : 83 years in women, 70 years in men Risk factors HR (CI 95) Adjusted for age History of osteoporotic fracture (yes, no) 1. 95 (1, 11 -3. 44)* History of rib fracture (yes, no) 1. 72 (0. 91 -3. 26) Physical activity practice (yes, no) 0. 40 (0. 16 -0. 97)* Elevated serum-osteocalcin levels 1. 72 (1. 19 -2. 47)** *p < 0, 05 ; **p < 0, 01 è Age is the main risk factor for rib fracture(s) after, or without, trauma è After adjustment for age, only prior fracture remains a risk factor for rib fracture(s) è After adjustement for age, practice of a physical activity an and elevated serum-osteocalcin levels are protection factors. La Lettre du Rhumatologue ASBMR 2010 - D’après Wuermser LA et al. , Rochester, États-Unis, abstr. SU 0345, actualisé
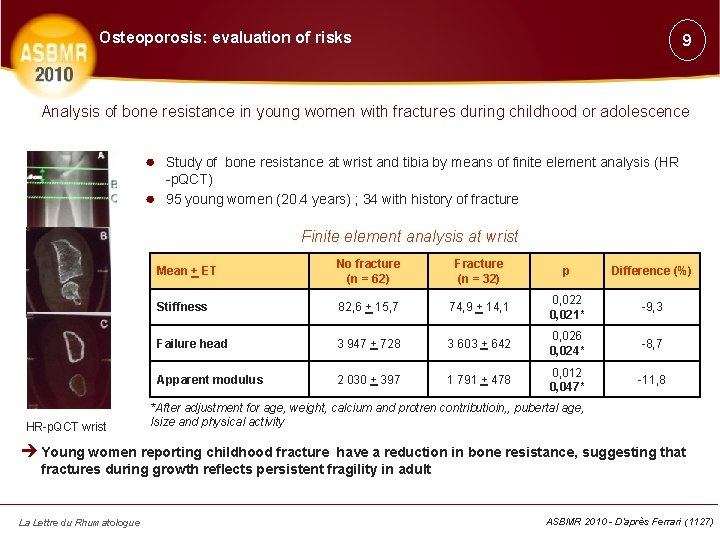
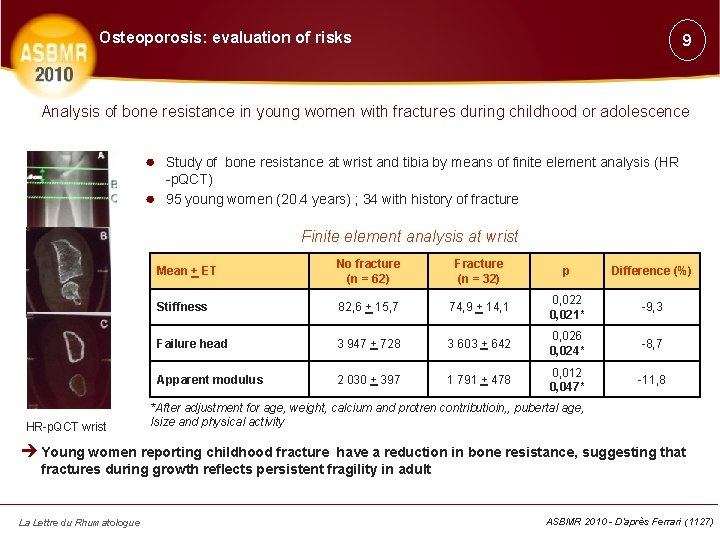
Osteoporosis: evaluation of risks 9 Analysis of bone resistance in young women with fractures during childhood or adolescence ● Study of bone resistance at wrist and tibia by means of finite element analysis (HR ● -p. QCT) 95 young women (20. 4 years) ; 34 with history of fracture Finite element analysis at wrist HR-p. QCT wrist Mean + ET No fracture (n = 62) Fracture (n = 32) p Difference (%) Stiffness 82, 6 + 15, 7 74, 9 + 14, 1 0, 022 0, 021* -9, 3 Failure head 3 947 + 728 3 603 + 642 0, 026 0, 024* -8, 7 Apparent modulus 2 030 + 397 1 791 + 478 0, 012 0, 047* -11, 8 *After adjustment for age, weight, calcium and protren contributioin, , pubertal age, lsize and physical activity è Young women reporting childhood fracture have a reduction in bone resistance, suggesting that fractures during growth reflects persistent fragility in adult La Lettre du Rhumatologue ASBMR 2010 - D’après Ferrari (1127)
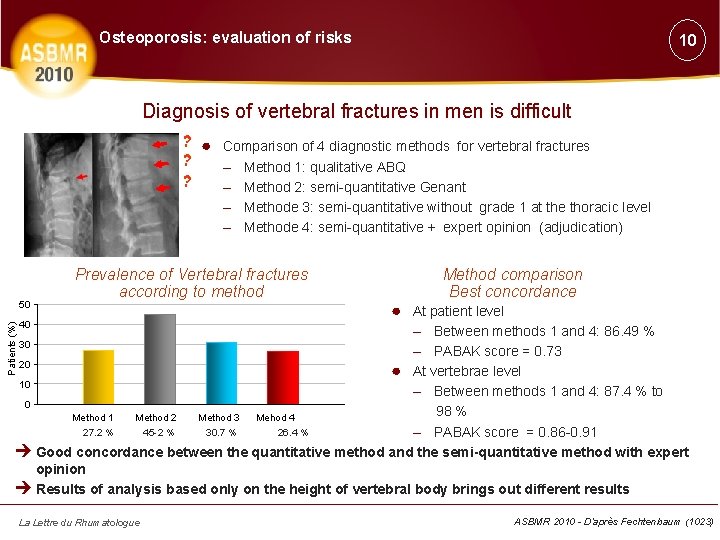
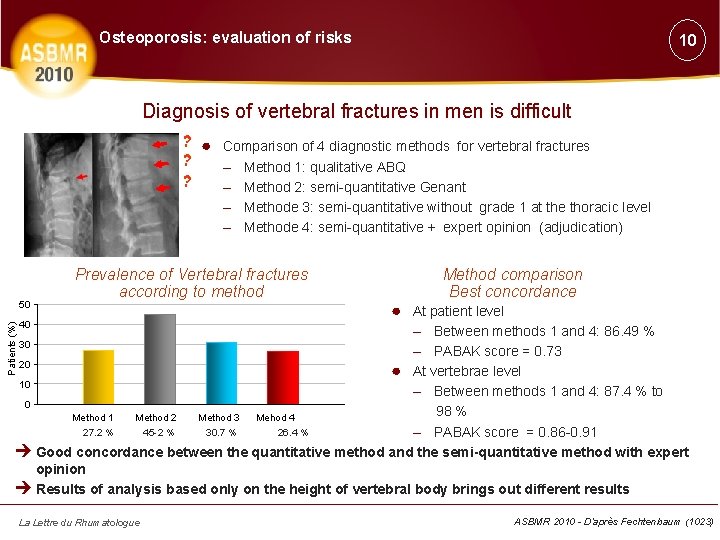
Osteoporosis: evaluation of risks 10 Diagnosis of vertebral fractures in men is difficult ? ● Comparison of 4 diagnostic methods for vertebral fractures ? – Method 1: qualitative ABQ ? – Method 2: semi-quantitative Genant – Methode 3: semi-quantitative without grade 1 at the thoracic level – Methode 4: semi-quantitative + expert opinion (adjudication) Patients (%) 50 Prevalence of Vertebral fractures according to method Method comparison Best concordance ● At patient level 40 – Between methods 1 and 4: 86. 49 % – PABAK score = 0. 73 20 ● At vertebrae level 10 – Between methods 1 and 4: 87. 4 % to 0 98 % Method 1 Method 2 Method 3 Mehod 4 27. 2 % 45 -2 % 30. 7 % 26. 4 % – PABAK score = 0. 86 -0. 91 è Good concordance between the quantitative method and the semi-quantitative method with expert opinion è Results of analysis based only on the height of vertebral body brings out different results 30 La Lettre du Rhumatologue ASBMR 2010 - D’après Fechtenbaum (1023)
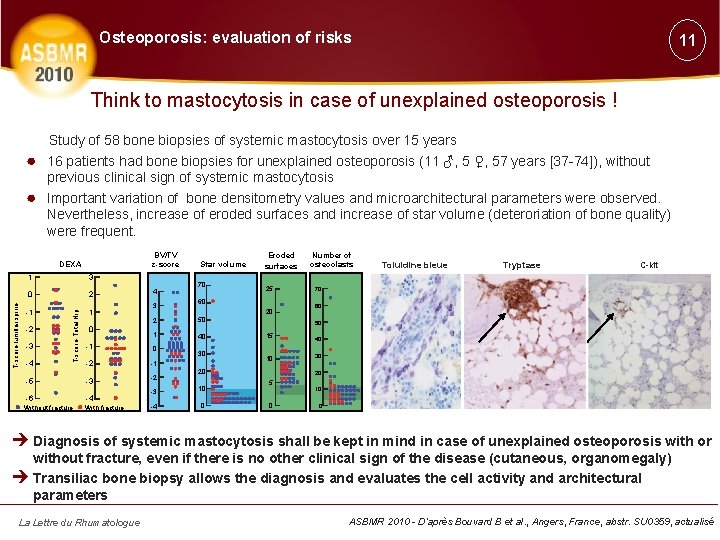
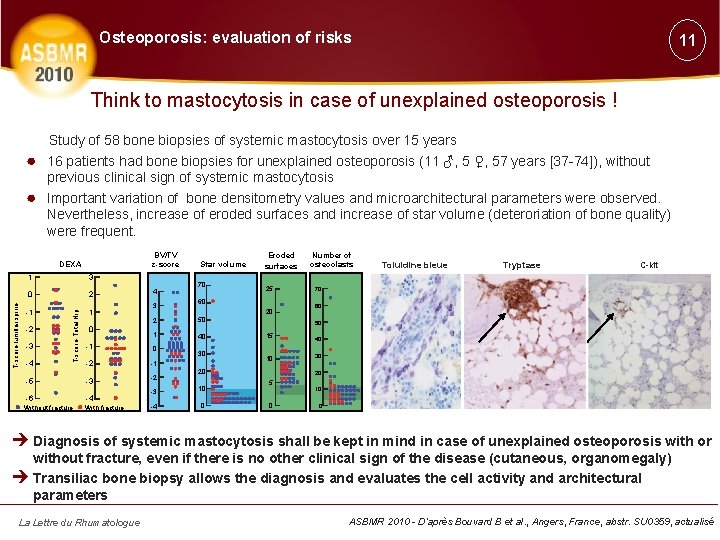
Osteoporosis: evaluation of risks 11 Think to mastocytosis in case of unexplained osteoporosis ! ● ● Study of 58 bone biopsies of systemic mastocytosis over 15 years 16 patients had bone biopsies for unexplained osteoporosis (11 ♂, 5 ♀, 57 years [37 -74]), without previous clinical sign of systemic mastocytosis Important variation of bone densitometry values and microarchitectural parameters were observed. Nevertheless, increase of eroded surfaces and increase of star volume (deteroriation of bone quality) were frequent. BV/TV z-score 1 3 0 2 -1 1 -2 -3 T-score Total Hip T-score lumbar spine DEXA 0 4 3 70 50 1 40 0 -2 -1 -5 -3 -2 -6 -4 Without fracture With fracture Eroded surfaces 25 60 2 -1 -4 Star volume 30 20 10 -4 0 Toluidine bleue Tryptase C-kit 70 60 50 15 10 20 -3 Number of osteoclasts 40 30 20 5 0 10 0 è Diagnosis of systemic mastocytosis shall be kept in mind in case of unexplained osteoporosis with or without fracture, even if there is no other clinical sign of the disease (cutaneous, organomegaly) è Transiliac bone biopsy allows the diagnosis and evaluates the cell activity and architectural parameters La Lettre du Rhumatologue ASBMR 2010 - D’après Bouvard B et al. , Angers, France, abstr. SU 0359, actualisé
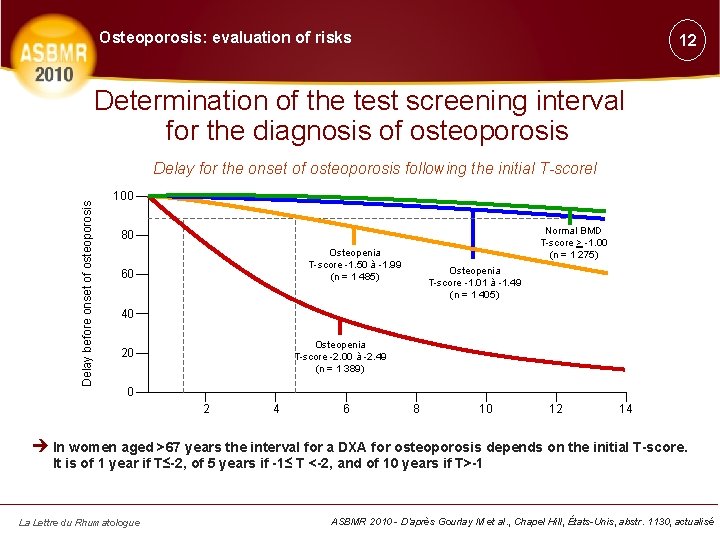
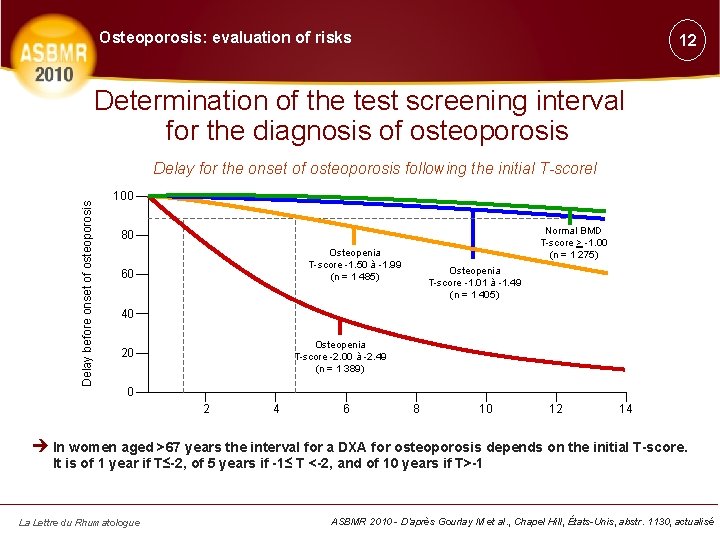
Osteoporosis: evaluation of risks 12 Determination of the test screening interval for the diagnosis of osteoporosis Delay before onset of osteoporosis Delay for the onset of osteoporosis following the initial T-scorel 100 Normal BMD T-score > -1. 00 (n = 1 275) 80 Osteopenia T-score -1. 50 à -1. 99 (n = 1 485) 60 Osteopenia T-score -1. 01 à -1. 49 (n = 1 405) 40 Osteopenia T-score -2. 00 à -2. 49 (n = 1 389) 20 0 2 4 6 8 10 12 14 è In women aged >67 years the interval for a DXA for osteoporosis depends on the initial T-score. It is of 1 year if T≤-2, of 5 years if -1≤ T <-2, and of 10 years if T>-1 La Lettre du Rhumatologue ASBMR 2010 - D’après Gourlay M et al. , Chapel Hill, États-Unis, abstr. 1130, actualisé
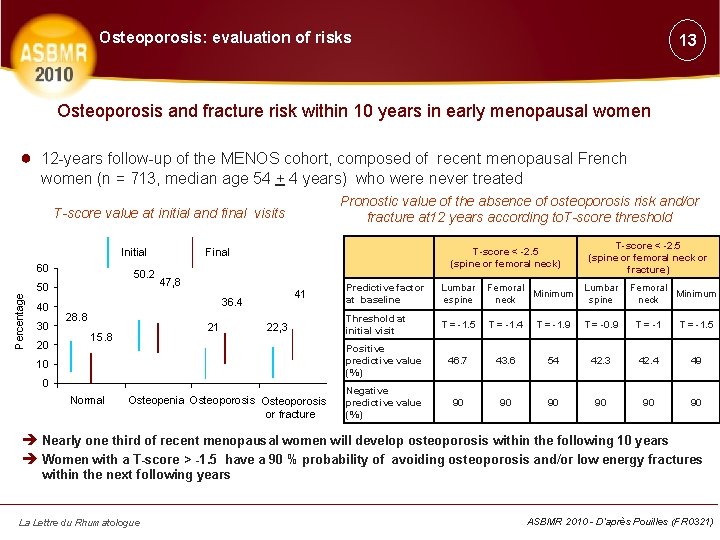
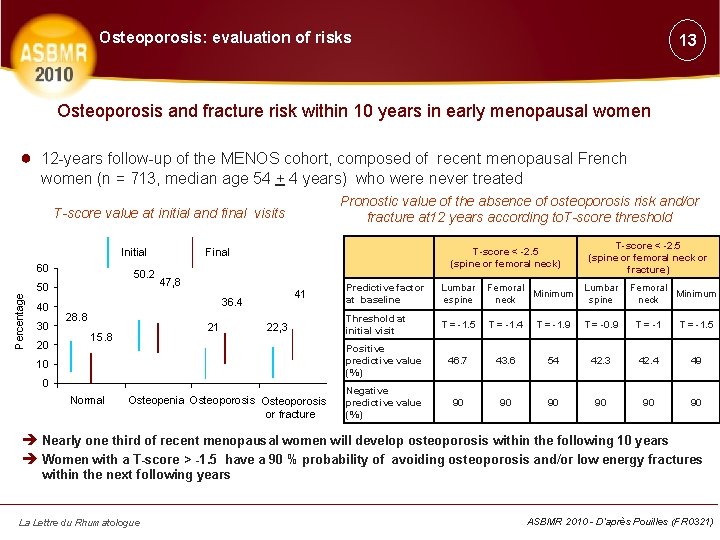
Osteoporosis: evaluation of risks 13 Osteoporosis and fracture risk within 10 years in early menopausal women ● 12 -years follow-up of the MENOS cohort, composed of recent menopausal French women (n = 713, median age 54 + 4 years) who were never treated Pronostic value of the absence of osteoporosis risk and/or fracture at 12 years according to. T-score threshold T-score value at initial and final visits Initial Percentage 60 50. 2 50 40 30 20 T-score < -2. 5 (spine or femoral neck) Final 47, 8 41 36. 4 28. 8 21 15. 8 22, 3 10 0 Normal Osteopenia Osteoporosis or fracture T-score < -2. 5 (spine or femoral neck or fracture) Predictive factor at baseline Lumbar espine Femoral Minimum neck Lumbar spine Femoral Minimum neck Threshold at initial visit T = -1. 5 T = -1. 4 T = -1. 9 T = -0. 9 T = -1. 5 Positive predictive value (%) 46. 7 43. 6 54 42. 3 42. 4 49 Negative predictive value (%) 90 90 90 è Nearly one third of recent menopausal women will develop osteoporosis within the following 10 years è Women with a T-score > -1. 5 have a 90 % probability of avoiding osteoporosis and/or low energy fractures within the next following years La Lettre du Rhumatologue ASBMR 2010 - D’après Pouilles (FR 0321)
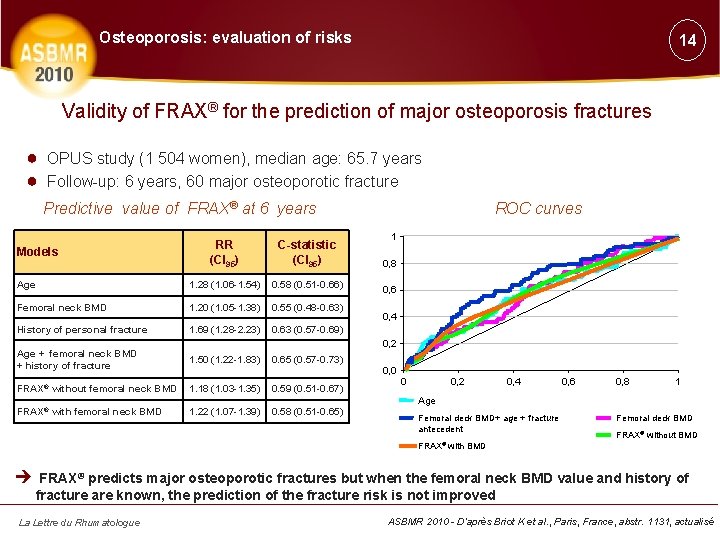
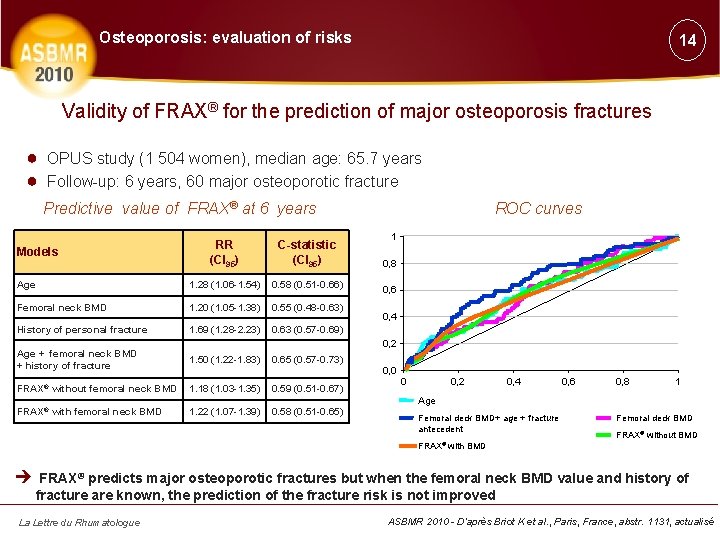
Osteoporosis: evaluation of risks 14 Validity of FRAX® for the prediction of major osteoporosis fractures ● OPUS study (1 504 women), median age: 65. 7 years ● Follow-up: 6 years, 60 major osteoporotic fracture Predictive value of FRAX® at 6 years RR (CI 95) C-statistic (CI 95) Age 1. 28 (1. 06 -1. 54) 0. 58 (0. 51 -0. 66) Femoral neck BMD 1. 20 (1. 05 -1. 38) 0. 55 (0. 48 -0. 63) History of personal fracture 1. 69 (1. 28 -2. 23) 0. 63 (0. 57 -0. 69) Models ROC curves 1 0, 8 0, 6 0, 4 0, 2 Age + femoral neck BMD + history of fracture 1. 50 (1. 22 -1. 83) 0. 65 (0. 57 -0. 73) FRAX® without femoral neck BMD 1. 18 (1. 03 -1. 35) 0. 59 (0. 51 -0. 67) FRAX® with femoral neck BMD 1. 22 (1. 07 -1. 39) 0. 58 (0. 51 -0. 65) 0, 0 0 0, 2 0, 4 0, 6 0, 8 1 Age Femoral deck BMD+ age + fracture antecedent FRAX® with Femoral deck BMD FRAX® without BMD è FRAX® predicts major osteoporotic fractures but when the femoral neck BMD value and history of fracture are known, the prediction of the fracture risk is not improved La Lettre du Rhumatologue ASBMR 2010 - D’après Briot K et al. , Paris, France, abstr. 1131, actualisé
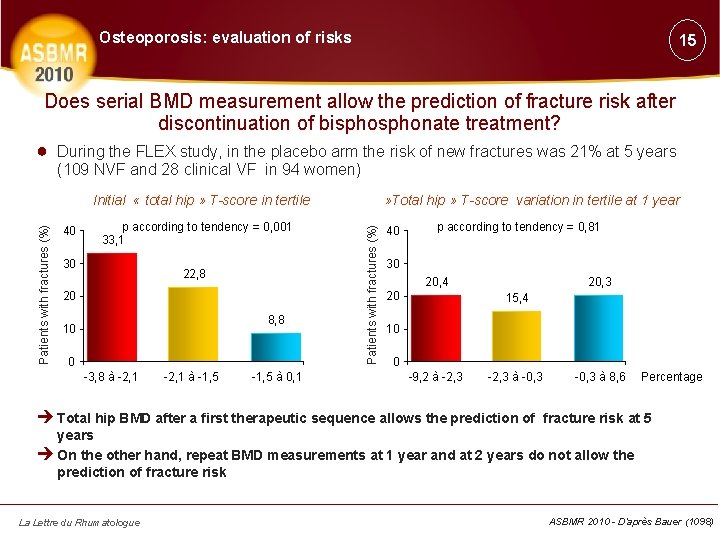
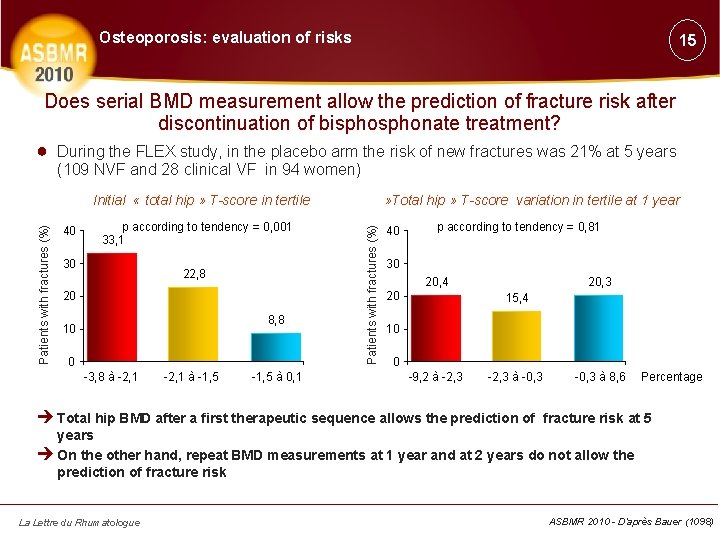
Osteoporosis: evaluation of risks 15 Does serial BMD measurement allow the prediction of fracture risk after discontinuation of bisphonate treatment? ● During the FLEX study, in the placebo arm the risk of new fractures was 21% at 5 years (109 NVF and 28 clinical VF in 94 women) 40 p according to tendency = 0, 001 33, 1 30 22, 8 20 8, 8 10 0 -3, 8 à -2, 1 à -1, 5 à 0, 1 » Total hip » T-score variation in tertile at 1 year Patients with fractures (%) Initial « total hip » T-score in tertile 40 p according to tendency = 0, 81 30 20, 4 20 20, 3 15, 4 10 0 -9, 2 à -2, 3 à -0, 3 à 8, 6 Percentage è Total hip BMD after a first therapeutic sequence allows the prediction of fracture risk at 5 years è On the other hand, repeat BMD measurements at 1 year and at 2 years do not allow the prediction of fracture risk La Lettre du Rhumatologue ASBMR 2010 - D’après Bauer (1098)
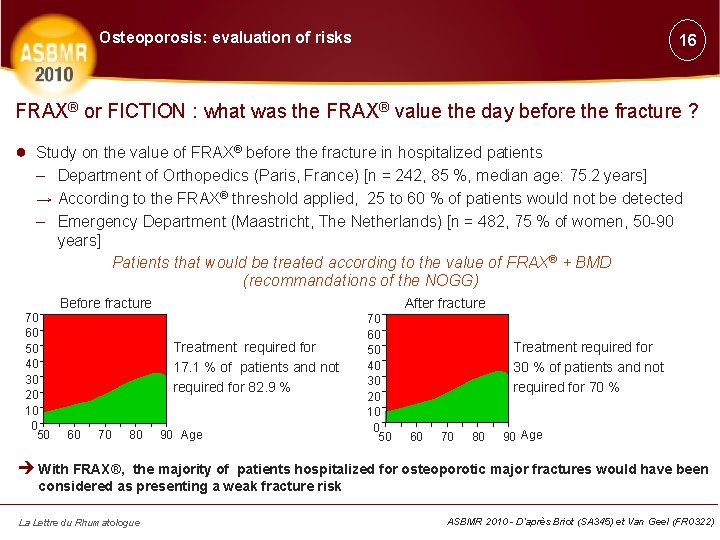
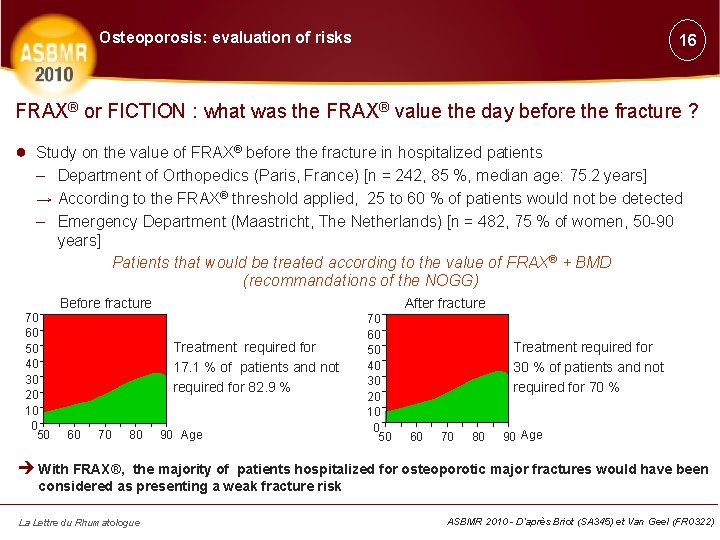
Osteoporosis: evaluation of risks 16 FRAX® or FICTION : what was the FRAX® value the day before the fracture ? ● Study on the value of FRAX® before the fracture in hospitalized patients – Department of Orthopedics (Paris, France) [n = 242, 85 %, median age: 75. 2 years] → According to the FRAX® threshold applied, 25 to 60 % of patients would not be detected – Emergency Department (Maastricht, The Netherlands) [n = 482, 75 % of women, 50 -90 years] Patients that would be treated according to the value of FRAX® + BMD (recommandations of the NOGG) 70 60 50 40 30 20 10 0 50 Before fracture After fracture Treatment required for 17. 1 % of patients and not required for 82. 9 % 60 70 80 90 Age 70 60 50 40 30 20 10 0 50 Treatment required for 30 % of patients and not required for 70 % 60 70 80 90 Age è With FRAX®, the majority of patients hospitalized for osteoporotic major fractures would have been considered as presenting a weak fracture risk La Lettre du Rhumatologue ASBMR 2010 - D’après Briot (SA 345) et Van Geel (FR 0322)
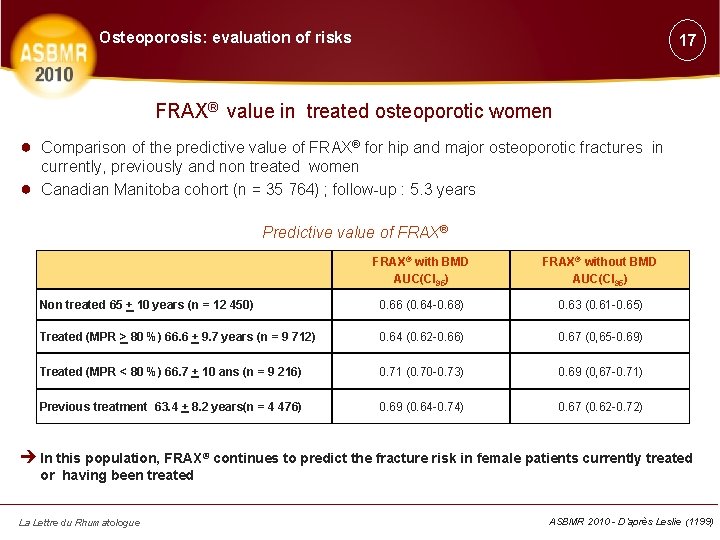
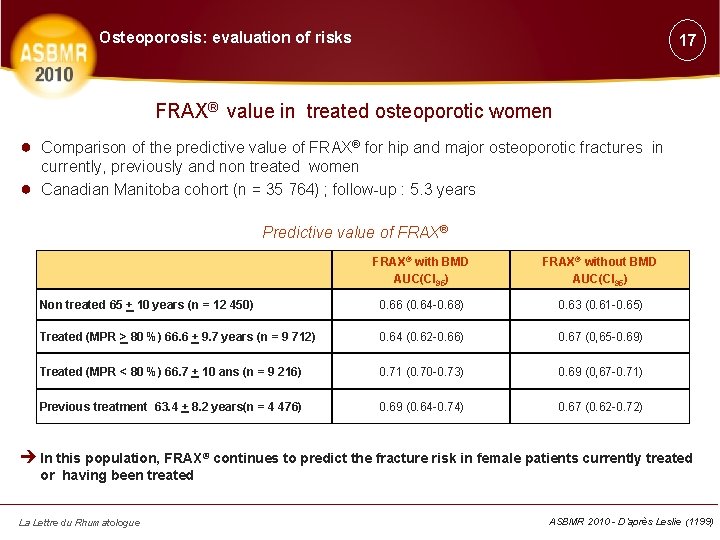
Osteoporosis: evaluation of risks 17 FRAX® value in treated osteoporotic women ● Comparison of the predictive value of FRAX® for hip and major osteoporotic fractures in ● currently, previously and non treated women Canadian Manitoba cohort (n = 35 764) ; follow-up : 5. 3 years Predictive value of FRAX® with BMD AUC(CI 95) FRAX® without BMD AUC(CI 95) Non treated 65 + 10 years (n = 12 450) 0. 66 (0. 64 -0. 68) 0. 63 (0. 61 -0. 65) Treated (MPR > 80 %) 66. 6 + 9. 7 years (n = 9 712) 0. 64 (0. 62 -0. 66) 0. 67 (0, 65 -0. 69) Treated (MPR < 80 %) 66. 7 + 10 ans (n = 9 216) 0. 71 (0. 70 -0. 73) 0. 69 (0, 67 -0. 71) Previous treatment 63. 4 + 8. 2 years(n = 4 476) 0. 69 (0. 64 -0. 74) 0. 67 (0. 62 -0. 72) è In this population, FRAX® continues to predict the fracture risk in female patients currently treated or having been treated La Lettre du Rhumatologue ASBMR 2010 - D’après Leslie (1199)
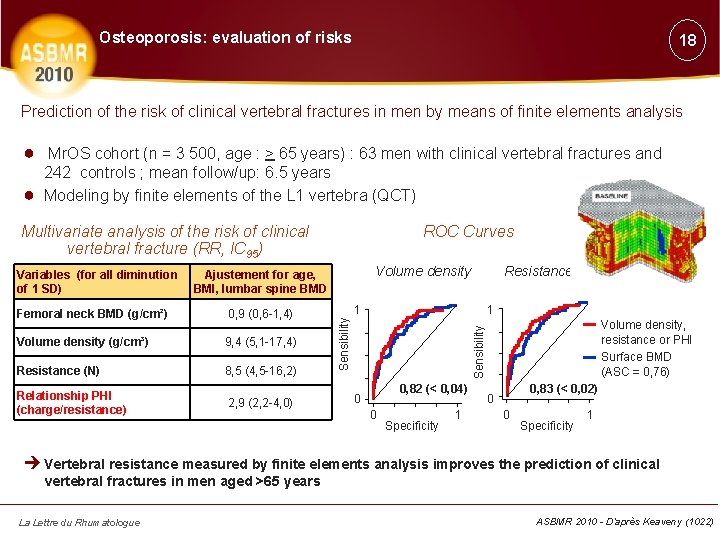
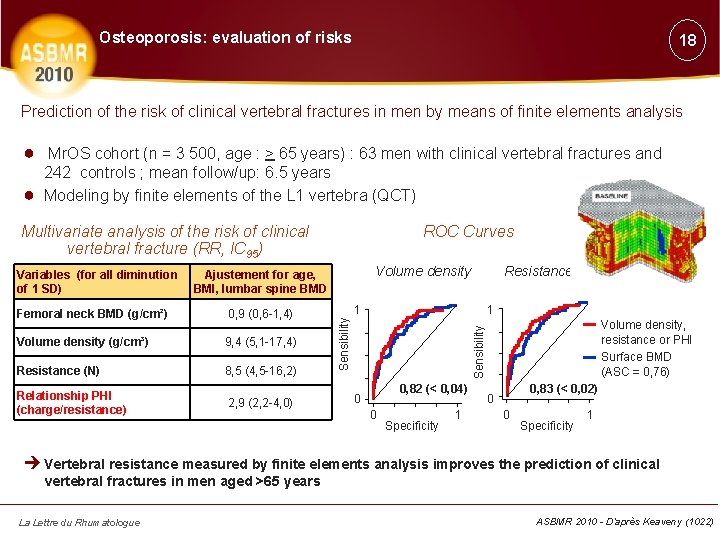
Osteoporosis: evaluation of risks 18 Prediction of the risk of clinical vertebral fractures in men by means of finite elements analysis ● Mr. OS cohort (n = 3 500, age : > 65 years) : 63 men with clinical vertebral fractures and ● 242 controls ; mean follow/up: 6. 5 years Modeling by finite elements of the L 1 vertebra (QCT) Multivariate analysis of the risk of clinical vertebral fracture (RR, IC 95) Volume density Ajustement for age, BMI, lumbar spine BMD 0, 9 (0, 6 -1, 4) Volume density (g/cm³) 9, 4 (5, 1 -17, 4) Resistance (N) 8, 5 (4, 5 -16, 2) Relationship PHI (charge/resistance) 2, 9 (2, 2 -4, 0) Resistancee 1 1 Volume density, resistance or PHI Surface BMD (ASC = 0, 76) Sensibility Femoral neck BMD (g/cm²) Sensibility Variables (for all diminution of 1 SD) ROC Curves 0, 82 (< 0, 04) 0 0 Specificity 1 0, 83 (< 0, 02) 0 0 Specificity 1 è Vertebral resistance measured by finite elements analysis improves the prediction of clinical vertebral fractures in men aged >65 years La Lettre du Rhumatologue ASBMR 2010 - D’après Keaveny (1022)
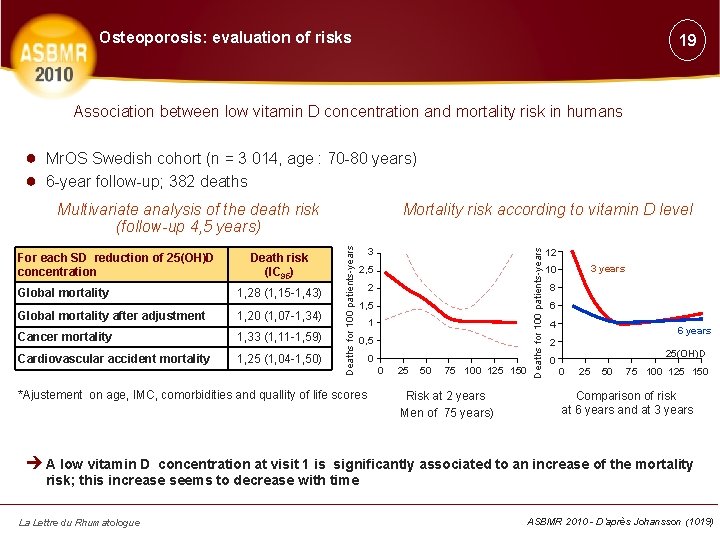
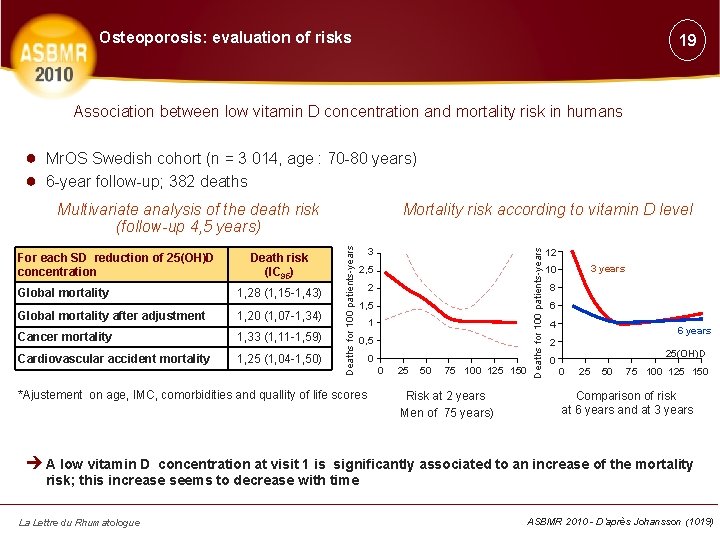
Osteoporosis: evaluation of risks 19 Association between low vitamin D concentration and mortality risk in humans ● Mr. OS Swedish cohort (n = 3 014, age : 70 -80 years) ● 6 -year follow-up; 382 deaths Death risk (IC 95) Global mortality 1, 28 (1, 15 -1, 43) Global mortality after adjustment 1, 20 (1, 07 -1, 34) Cancer mortality 1, 33 (1, 11 -1, 59) Cardiovascular accident mortality 1, 25 (1, 04 -1, 50) 3 2, 5 2 1, 5 1 0, 5 *Ajustement on age, IMC, comorbidities and quallity of life scores 0 0 25 50 75 100 125 150 Risk at 2 years Men of 75 years) Deaths for 100 patients-years For each SD reduction of 25(OH)D concentration Mortality risk according to vitamin D level Deaths for 100 patients-years Multivariate analysis of the death risk (follow-up 4, 5 years) 12 3 years 10 8 6 4 6 years 2 0 25(OH)D 0 25 50 75 100 125 150 Comparison of risk at 6 years and at 3 years è A low vitamin D concentration at visit 1 is significantly associated to an increase of the mortality risk; this increase seems to decrease with time La Lettre du Rhumatologue ASBMR 2010 - D’après Johansson (1019)