In the name of God Tetanus Lockjaw Tetanus












- Slides: 74
In the name of God
Tetanus (Lockjaw) • Tetanus is a neurologic disorder, characterized by increased muscle tone and spasms, that is caused by Tetanospasmin, a powerful protein toxin elaborated by Clostridium tetani.
Clinical forms • Generalized • Neonatal • Localized(Cephalic)
Etiologic agent • Anaerobic, motile gram-positive rod, resembling tennis racket or drumstick.

Etiologic agent • Is found worldwide in soil, in the inanimate environment, in animal feces, and occasionally in human feces. • Spores may survive for years in some environments and are resistant to various disinfectants. • Tetanospasmin is formed in vegetative cells.
Pathogenesis • Contamination of wounds with spores of C. tetani is probably a frequent occurrence. • Germination and toxin production, however, take place only in wounds with low oxidation- reduction potentials such as those with devitalized tissue, foreign bodies, or active infection.
Pathogenesis • Generalized tetanus occurs when toxin released in the wound enters the lymphatics and blood stream and is spread widely to distant nerve terminals; the blood brain barrier (BBB) blocks direct entry into the central nervous system (CNS).
Pathogenesis • If it is assumed that intraneuronal transport times are equal for all nerves. • Short nerves are affected before long nerves: This fact explains the sequential involvement of nerves of the head, trunk, and extremities in generalized tetanus.
Pathogenesis • Toxin released in the wound binds to peripheral motor neuron terminals, enters the axon, and is transported to the nervecell body in the brainstem and spinal cord by retrograde intraneuronal transport
Pathogenesis • The toxin then migrates across the synapse to presynaptic terminals, where it blocks release of inhibitory neurotransmitters glycine and γaminobutiric acid(GABA)
Pathogenesis • Loss of inhibition may also affect preganglionic synapthetic neurons in the lateral gray matter of the spinal cord and produce sympathetic hyperactivity and high circulating catecholamine levels.
Pathogenesis • In local tetanus, only the nerves supplying the affected muscles are involved.
Clinical manifestations • Generalized tetanus, the most common form of the disease, is characterized by increased muscle tone and generalized spasms.


Clinical Manifestations • Generalized tetanus • Increased muscle tone and generalized spasms. • Trismus (lockjaw) increased tone in masseter muscle. • Dysphagia or stiffness or pain in the neck, shoulder, and back muscles appear concurrently or soon thereafter.
Clinical manifestations • Typically, the patient first notices increased tone in masseter muscle (Trismus , Lockjaw)
Clinical manifestations • Dysphagia or stiffness or pain in the neck, shoulder, and back muscles appear concurrently or soon thereafter. • The subsequent involvement of other muscles produces a rigid abdomen and stiff proximal limb muscles; the hands and feet are relatively spared.
Clinical manifestations • Sustained contraction of the facial muscles result in a grimace or sneer (Risus sardinius). • Contraction of the back muscles produces an arched back(Opisthotonos). • Some patients develop paroxysmal, violent, painful, generalized muscle spasms that may cause cyanosis and threaten ventilation.






Clinical manifestations • These spasms occur repetitively and may be spontaneous or provoked by even the slightest stimulation. • A constant threat during generalized spasms is reduced ventilation or apnea or laryngospasm.
Clinical manifestation • Mild: muscle rigidity and few or no spasms • Moderate: Trismus, dysphagia, rigidity, and spasms. • Severe: frequent explosive paroxysms.
Clinical Manifestations • • The patients may be febrile. Mentation is unimpaired. Deep tendon reflexes may be increased. Dysphagia or ileus may preclude oral feeding.
Clinical manifestations • Autonomic dysfunction commonly complicates severe cases and is characterized by labile or sustained hypertension, tachycardia, dysrythmia, hyperpyrexia, or profuse sweating, peripheral vasoconstriction, and increased plasma and urinary catecholamine levels.
Clinical manifestations • Periods of bradycardia and hypertension may also be documentated. • Sudden cardiac arrest sometimes occurs, but it basis is unknown.
Clinical manifestations • Other complications include: Aspiration pneumonia, fractures, muscle rupture, deepvein thrombophelebitis(DVT), pulmonary emboli(PE), decubitus ulcer, rhabdomyolysis.
Diagnosis • The diagnosis of tetanus is based entirely on clinical findings. • Differential diagnosis: strychnine poisoning, dystonic drug reactions(e. g. , phenotyazines, and metocolpramide) and hypocalcemic tetany • Other conditions sometimes confused: meningitis/ encephalitis, rabies,
Treatment • General measures: the goals of therapy are to eliminate the source of toxin, neutralize unbound toxin, and prevent muscle spasms, monitoring the patient’s condition and providing support – especially respiratory support – until recovery. • Patients should be admitted to a quiet room in an ICU.
Treatment • Observation and cardiopulmonary monitoring should be maintained continuously but stimulation should be minimized. • Protection of the airway is vital. • Wounds should be explored , carefully cleansed, and thoroughly debrided.
Antibiotic therapy • Although of unproven value, antibiotic therapy is administered to eradicate vegetative cellsthe source of toxin. • Penicillin( 10 -12 million units IV for 10 days. • Metronidazole 500 mg qid or 1 gram BID. • (Is preferred by some experts)
Antitoxin • Given to neutralize circulating toxin and unbound toxin in the wound. • Antitoxin effectively lowers mortality. • Toxin already bound to neural tissue is unaffected. • Human Tetanus Immunoglobin(TIG) is the preparation of choice and should be given promptly. • The dose is 3000 -6000 units IM, usually in divided doses, because the volume is large.
Antitoxin • The optimal dose is not known. • Pooled IVIG may be an alternative. • It may be best to administer antitoxin before manipulating the wound. • The value of injecting a dose proximal to the wound or infiltrating the wound is unclear.
Antitoxin • Additional doses are unnecessary because the half-life of antitoxin is long. • Antibody does not penetrate the Blood. Brain Barrier. • Interathecal administration should be considered experimental.
Control of muscle spasms • Many agents, alone and in combination, have been used to treat the muscle spasms of tetanus, which is painful and can threaten ventilation by causing laryngospasm or sustained contraction of ventilatory muscle. • The ideal therapeutic regimen would abolish spasmodic activity without causing oversedation & hypoventilation.
Control of muscle spasms • Diazepam: (a benzodiazepine and GABA agonist), is in wide use. • The dose is titrated, and large doses (≥ 250 mg/ day) may be required. • Lorazepam, with a longer duration of action, midazolam, with a short half-life, are other options.
Control of muscle spasms • Barbiturates and chlorpromazine are considered second - line agents. • Therapeutic paralysis with a non depolarizing neuromascular blocking agent and mechanical ventilation may be required for treatment of spasms unresponsive to medication or spasms that threaten ventilation.
Control of spasms • • Dantrolen Intrathecal baclofen Succinilcholine Magnesium sulfate
Respiratory care • Intubation or tracheostomy, with or without mechanical ventilation , may be required foe hypoventilation due to oversedation or laryngospasm or for avoidance of aspiration.
Autonomic dysfunction • The optimal therapy for sympathetic overactivity has not been defined. • Labetalol, (α- and β- adrenergic blocking agent ) • Esmolol(β- adrenergic blocking agent ) • Clonidine ( a central – acting antiadrenergic)

Recommended childhood immunization schedule- IRAN • • • Birth : HBV, OPV, BCG 2 months : HBV, DTP, OPV 4 months : OPV, DTP 6 months : HBV, DTP, OPV 12 months : MMR 18 months : OPV, DTP 6 years : MMR, DTP, OPV 14 -16 years: Td Td every ten years
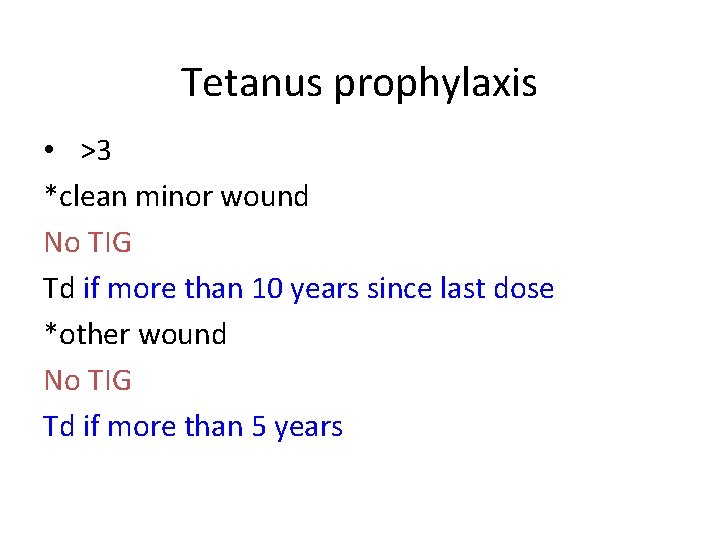
Tetanus prophylaxis • >3 *clean minor wound No TIG Td if more than 10 years since last dose *other wound No TIG Td if more than 5 years
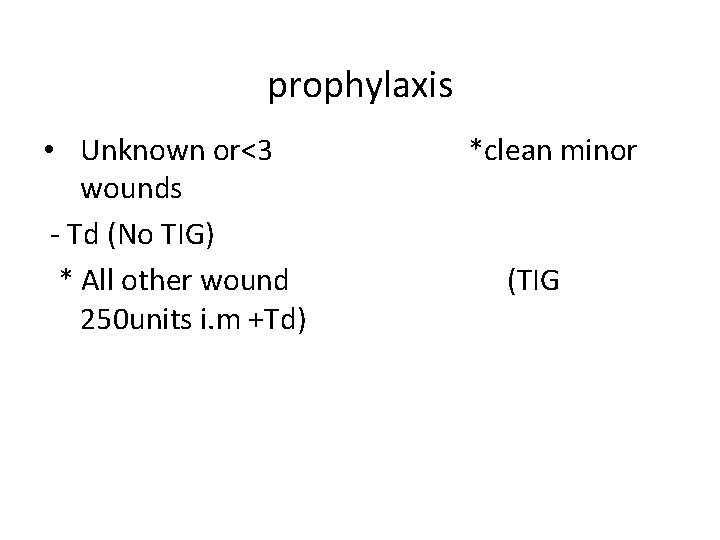
prophylaxis • Unknown or<3 wounds - Td (No TIG) * All other wound 250 units i. m +Td) *clean minor (TIG

Botulism • Botulism is a paralytic disease caused by potent protein neurotoxin elaborated by Clostridium botulinum. • Illness begins with cranial nerve involvement, and progression proceeds caudally to involved extremities.

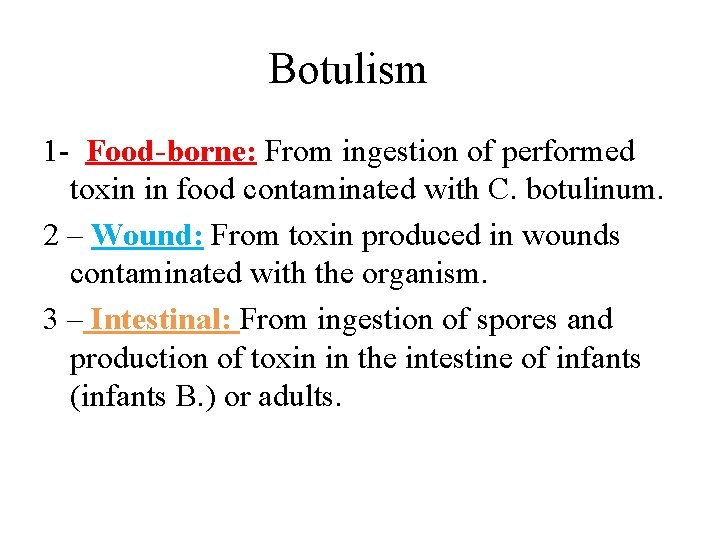
Botulism 1 - Food-borne: From ingestion of performed toxin in food contaminated with C. botulinum. 2 – Wound: From toxin produced in wounds contaminated with the organism. 3 – Intestinal: From ingestion of spores and production of toxin in the intestine of infants (infants B. ) or adults.
Botulism • C. botulinum, a species encompassing a heterogeneous group of anaerobic grampositive organisms that form sub terminal spores. • C. botulinum is found in soil and marine environments throughout the world and elaborates the most potent bacterial toxin known.
Botulinum • Organisms of types A through G have been distinguished by antigenic specificities of their toxins. • Rare strains of other clostridial species – C. butyricum and C baratii – have also been found to produce toxin.
Does the appearance of food change? • C. botulinum strains with proteolytic activity can digest food and produce a spoiled appearance ; nonproteolytic types leave the appearance of food unchanged.
Toxin types • Of the eight distinct toxin types described ( A, B, C 1, C 2, D, E, F, and G), all except C 2 are neurotoxin; C 2 is a cytotoxin of unknown clinical significance. • Toxin types A, B, E, and rarely F cause human diseases. • Type G (from C. argentinese) has been associated with sudden death, but not with neuroparalytic illness.
4 steps in neurotoxin activity • 1 – Specific binding to presynaptic nerve cell in endocytic vesicles • 2 - Internalization of toxin inside the nerve cell in endocytic vesicles. • 3 – Translocation of the toxin into cytosol. • 4 – Proteolysis by toxin ( a Zinc endopepticase) of components of the neuroexocytosis apparatus curtailing release of the neurotransmitter acetylcoline.
Clinical manifestations • Food-Borne: After ingestion of food containing toxin, illness varies from a mild condition for which no medical advice is sought to very severe disease than can result in death within 24 h.
Food- borne B. ° Incubation period is usually 18 - 36 h but depending on toxin dose, can extend from a few hours to several days.
Food- Borne B. • Symmetric descending paralysis is characteristic and can lead to respiratory failure and death.
Food-borne B. • Cranial nerve involvement, which almost always marks the onset of symptoms, usually produces diplopia, dysarthria, dysphonia, and /or dysphagia.
Food-borne B. • Weakness progresses, often rapidly, from the head to involve the neck, arms, thorax, and legs; occasionally, weakness is asymmetric. • Nausea, vomiting, and abdominal pain may precede or follow the onset of paralysis.
Food- borne B • Dizziness, blurred vision , dry mouth, and very dry, occasionally sore throat are common. • Patients are usually alert and oriented, but they may be drowsy, agitated, and anxious. • Typically they have NO fever.
Food- borne B. • Ptosis is frequent • Pupillary reflexes may be depressed. • Fixed or dilated pupils are noted in half of patients. • Gag reflex may be suppressed. • Deep tendon reflexes may be normal or decreasesd. • Sensory findings are usually absent. • Paralytic illeus, severe constipation, and urinary retention are common.
Wound B. • Occurs when the spores contaminating a wound germinate and form vegetative organisms that produce toxin. • This rare condition resembles food-borne illness except that the incubation period is longer (averaging 10 days), and GI symptoms are lacking.
Wound B. • • Contamination with soil. IVDU( black –tar heroin) C. Section delivery The wound may appear benign.
Intestinal B. • Germination of ingested spores. • Infant B. is the most common form. • Mild illness with failure to thrive → to fulminant severe paralysis with respiratory failure. • One cause of sudden death.
Intestinal B. • The identification of contaminated honey as one source of spores has led to the recommendation that honey not be fed to children < 12 months of age. • Cases usually involve infants < 6 months.
Diagnosis • Symmetric descending paralysis who are febrile and mentally intact. • Toxin in serum by bioassay • Demonstration of toxin in vomitus, gastric fluid, or stool is strongly suggestive. • Isolation of the organism from food without toxin is insufficient grounds for the diagnosis.
Diagnosis • Wound cultures yielding the organism are suggestive of botulism. • Tensilon test (Edrophonium chloride ) for myasthenia gravis may be falsely positive but is usually less dramatically positive than the former condition. • NCV is normal. • Single – fiber EMG may be helpful.
Treatment • Patients should be hospitalized and monitored closely, both clinically and by spirometry, pulse oxitometry, and measurment of ABG for incipient respiratory failure.
Treatment • Intubation and mechanical ventilation should be strongly considered when the vital capacity is< 30% of predicted, especially when paralysis is progressing rapidly and hypoxemia with absolute or relative hypercapnia is documented.
Treatment • In food-borne illness, equine antitoxin should be administered as soon as possible after specimen are obtained for laboratory analysis. • Previous: Trivalent antitoxin(type A, B, and E) • Biovalent: A, B • Monovalent: type E
B. Antitoxin • Botulism antitoxin E monovalent • 20 ml / 100 ml normal saline / infusion over 30 min • After 4 h, 100 ml • After 12 - 24 • Prevention 20 ml / IM
Treatment • If there is no ileus, cathartics, and enemas may be given to purge the gut of toxin; emetics or gastric lavage can also be used if the time since ingestion is brief (Only a few hours).
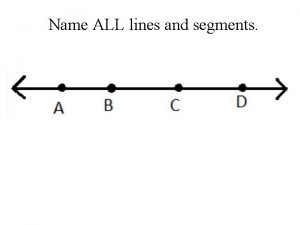
 Name all the lines
Name all the lines Sulcus nasolabialis
Sulcus nasolabialis Spasme
Spasme Muscle physiology
Muscle physiology The staircase phenomenon
The staircase phenomenon Horst allerdist
Horst allerdist Oppervlakkige hondenbeet tetanus
Oppervlakkige hondenbeet tetanus Incomplete tetanus muscle contraction
Incomplete tetanus muscle contraction Incomplete tetanus muscle contraction
Incomplete tetanus muscle contraction Charles bell tetanus
Charles bell tetanus Tetanus pathogenesis
Tetanus pathogenesis Prophalaxysis
Prophalaxysis Tetanus
Tetanus Tetanus shot osha recordable
Tetanus shot osha recordable Tetanus
Tetanus Tetanus
Tetanus Vlnitý tetanus
Vlnitý tetanus Laatjevaccineren.be/tetanus-klem
Laatjevaccineren.be/tetanus-klem Fajar tetanua
Fajar tetanua Agedema
Agedema Hondenbeet tetanus
Hondenbeet tetanus Tetanus symptoms
Tetanus symptoms Phenotyazine
Phenotyazine Lactation tetany
Lactation tetany Vrbanac kod svinja liječenje
Vrbanac kod svinja liječenje Tetanus def
Tetanus def 5u1 cjepivo
5u1 cjepivo Tetanus neonatorum ppt
Tetanus neonatorum ppt Latch state smooth muscle
Latch state smooth muscle Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Chúa yêu trần thế alleluia
Chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng từ chạy
Môn thể thao bắt đầu bằng từ chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tiính động năng
Công thức tiính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Nguyên nhân của sự mỏi cơ sinh 8
Nguyên nhân của sự mỏi cơ sinh 8 đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Số nguyên tố là gì
Số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Our god is an awesome god vine
Our god is an awesome god vine My god is an awesome god he reigns
My god is an awesome god he reigns Awesome god medley
Awesome god medley God is good god is great speed
God is good god is great speed