Measles and Neonatal Tetanus Clinical Signsand and Treatment





- Slides: 34
Measles and Neonatal Tetanus: Clinical. Signsand and. Treatment Clinical Prof. Pushpa Raj Sharma Institute of Medicine Kathmandu
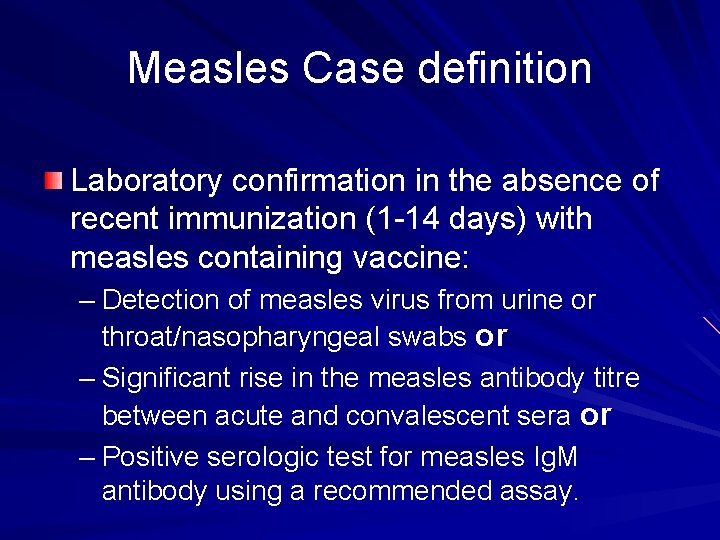
Measles Case definition Laboratory confirmation in the absence of recent immunization (1 -14 days) with measles containing vaccine: – Detection of measles virus from urine or throat/nasopharyngeal swabs or – Significant rise in the measles antibody titre between acute and convalescent sera or – Positive serologic test for measles Ig. M antibody using a recommended assay.
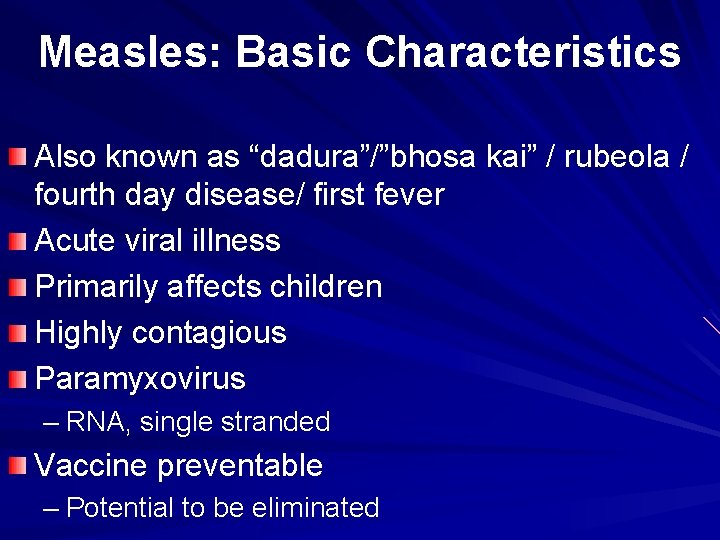
Measles: Basic Characteristics Also known as “dadura”/”bhosa kai” / rubeola / fourth day disease/ first fever Acute viral illness Primarily affects children Highly contagious Paramyxovirus – RNA, single stranded Vaccine preventable – Potential to be eliminated
Measles: Signs and Symptoms Incubation period: 10 -12 days (8 -16 range) Prodrome – Cough NP, worsens over 4 days, then improves Lasts through entire illness (7 -10 days) – Conjunctivitis (purulent), coryza May include photophobia Lasts 6 -8 days – Fever: 38 -40 o C: subsides after 1 week – Diarrhea Chronic, serious if previously malnourished
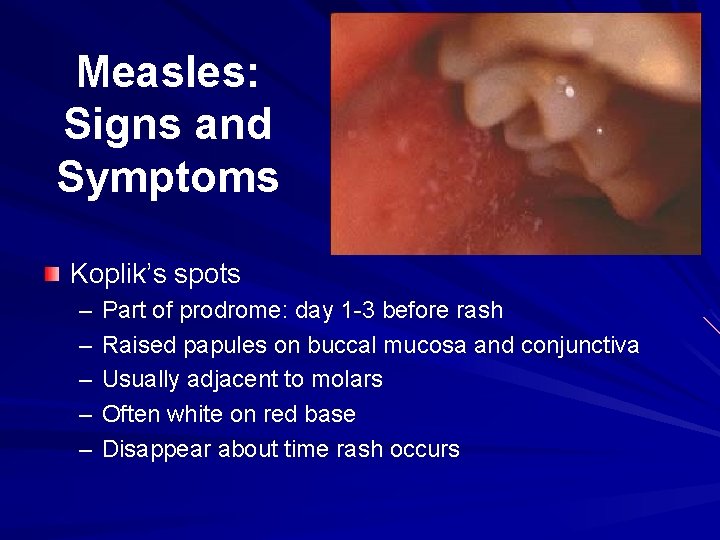
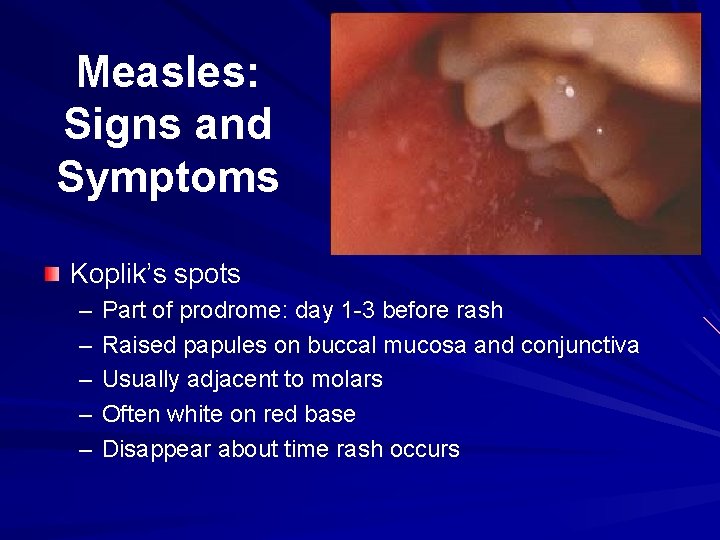
Measles: Signs and Symptoms Koplik’s spots – – – Part of prodrome: day 1 -3 before rash Raised papules on buccal mucosa and conjunctiva Usually adjacent to molars Often white on red base Disappear about time rash occurs
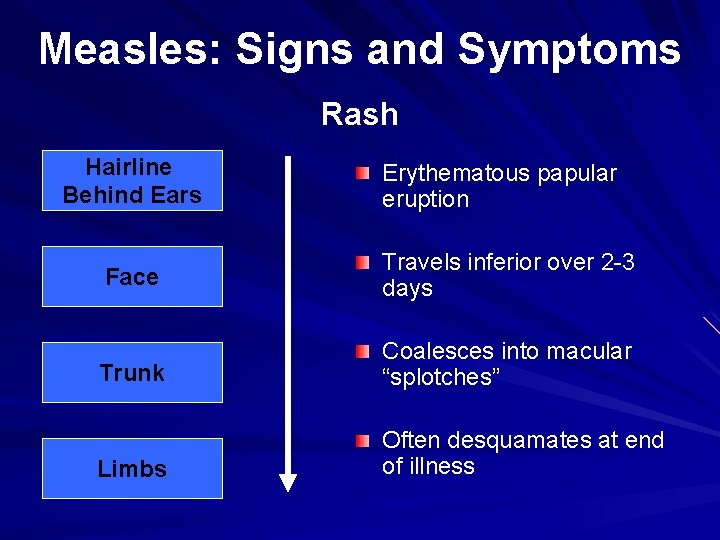
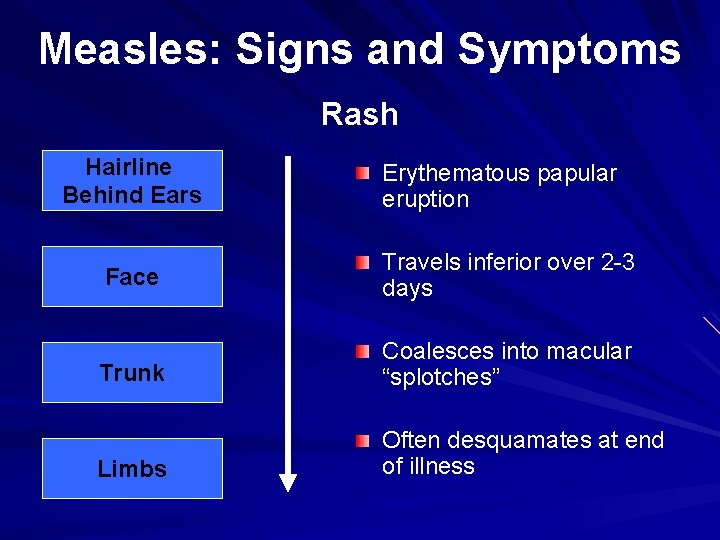
Measles: Signs and Symptoms Rash Hairline Behind Ears Erythematous papular eruption Face Travels inferior over 2 -3 days Trunk Coalesces into macular “splotches” Limbs Often desquamates at end of illness
Measles: Signs and Symptoms Peak of Illness – 2 -4 days after onset of rash Other signs and symptoms – Anorexia, malaise, hemorrhagic, Resolution – Rapid improvement at end of febrile period (1 week) – Complete recovery in 10 -14 days
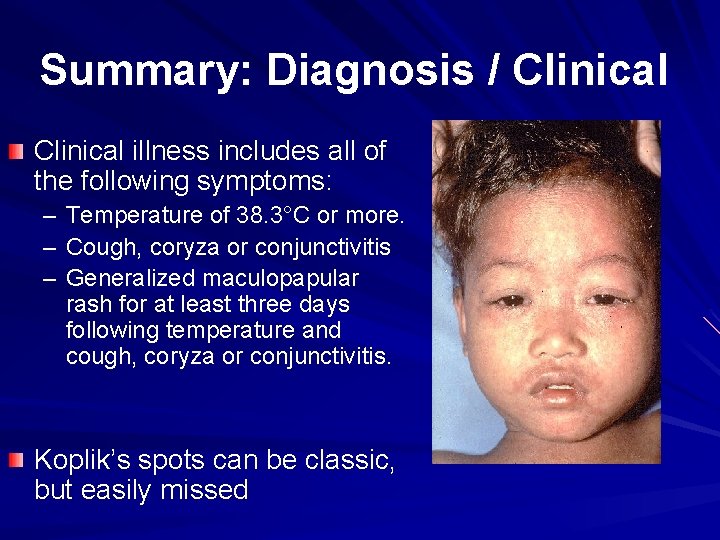
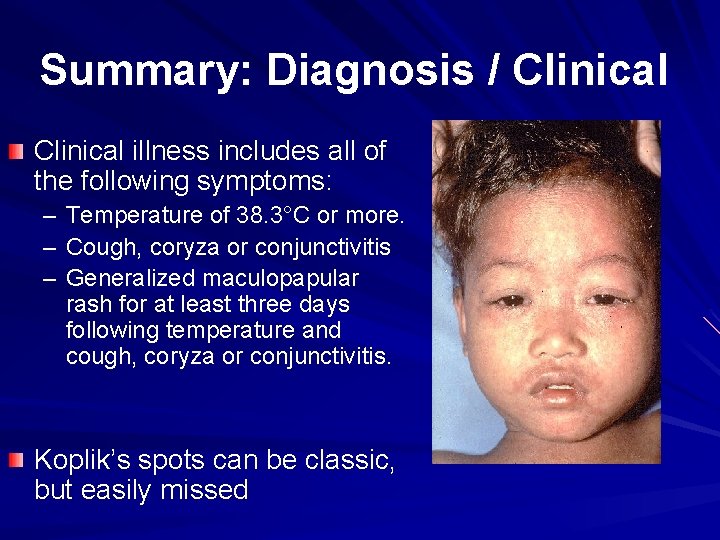
Summary: Diagnosis / Clinical illness includes all of the following symptoms: – Temperature of 38. 3°C or more. – Cough, coryza or conjunctivitis – Generalized maculopapular rash for at least three days following temperature and cough, coryza or conjunctivitis. Koplik’s spots can be classic, but easily missed
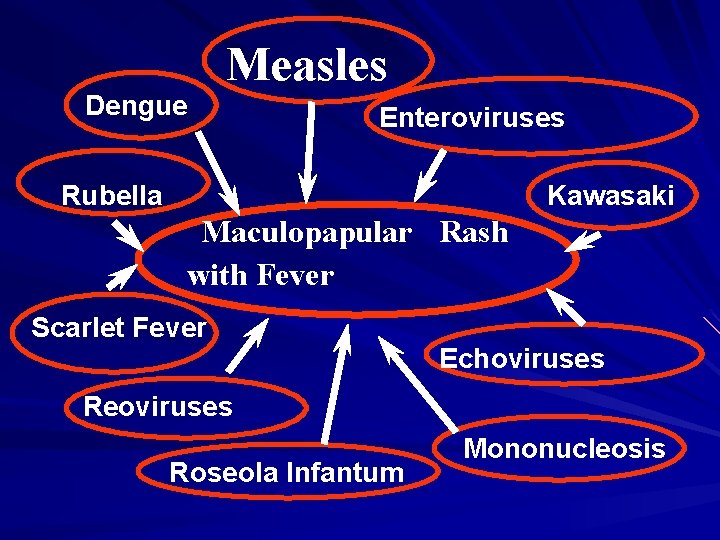
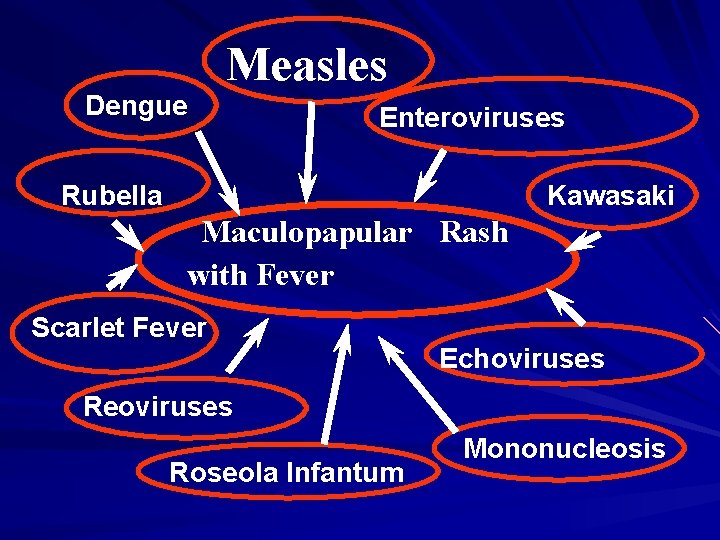
Dengue Measles Enteroviruses Rubella Kawasaki Maculopapular Rash with Fever Scarlet Fever Echoviruses Reoviruses Roseola Infantum Mononucleosis

Six Case Studies
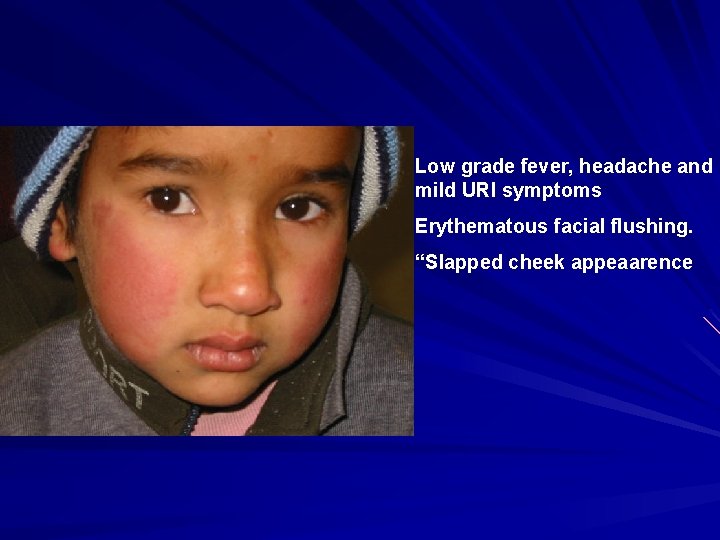
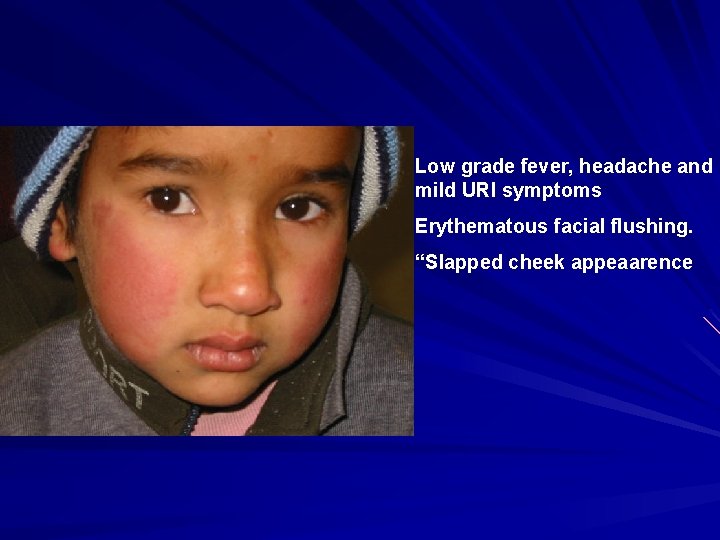
Low grade fever, headache and mild URI symptoms Erythematous facial flushing. “Slapped cheek appeaarence
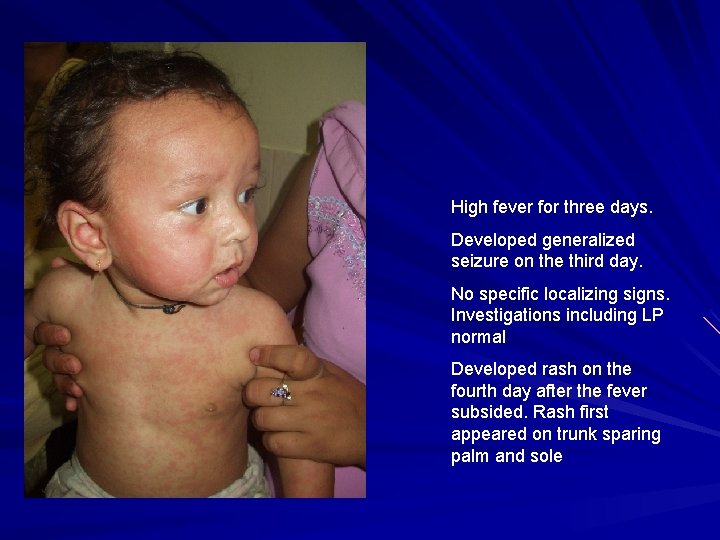
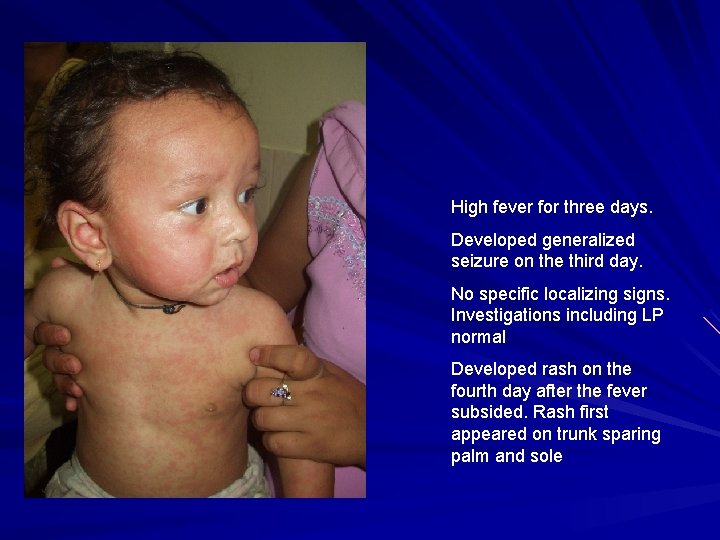
High fever for three days. Developed generalized seizure on the third day. No specific localizing signs. Investigations including LP normal Developed rash on the fourth day after the fever subsided. Rash first appeared on trunk sparing palm and sole

Presented with Jaundice and drowsiness, ascitis Started ampicillin Developed rash on 4 th day.
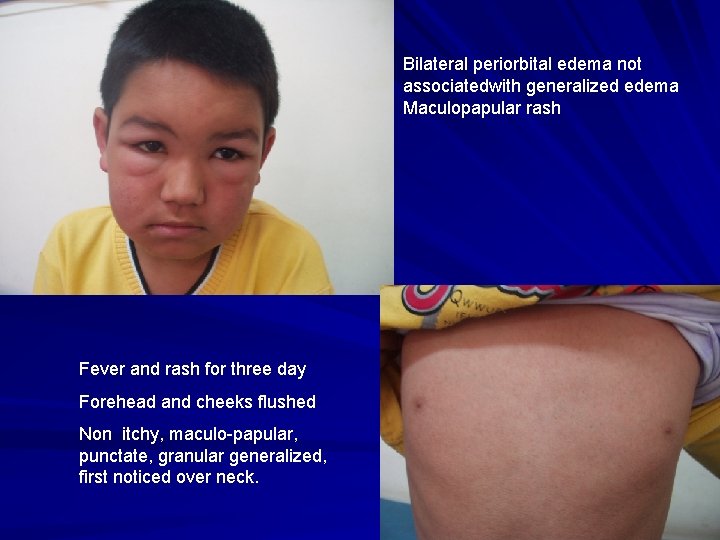
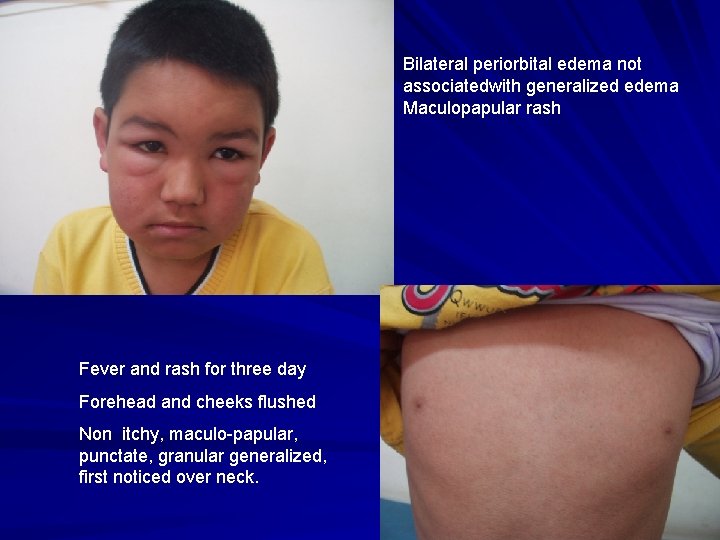
Bilateral periorbital edema not associatedwith generalized edema Maculopapular rash Fever and rash for three day Forehead and cheeks flushed Non itchy, maculo-papular, punctate, granular generalized, first noticed over neck.

Mild fever and cough for two days Developed rash on the second day of fever which appeared on face first and spread allover in one day. Fever: 99. 2 axillary; enanthem on the soft palate; tender discrete lymph nodes over retro auricular, sub occipital and posterior cervical region. Rash cleared on third day.
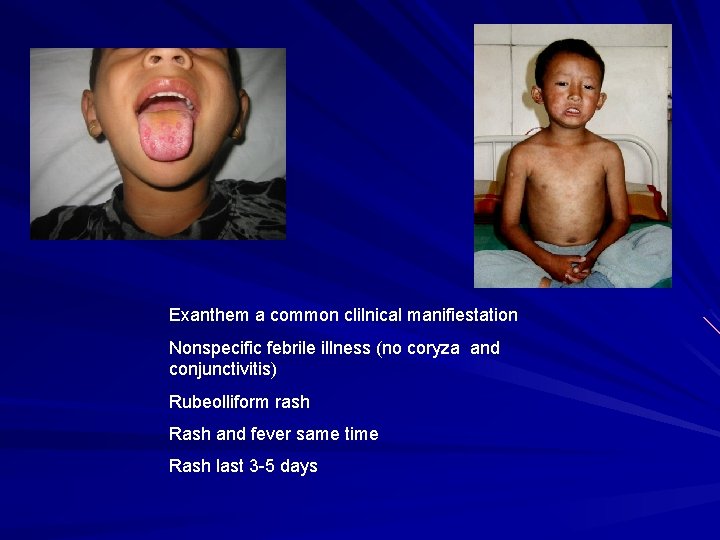
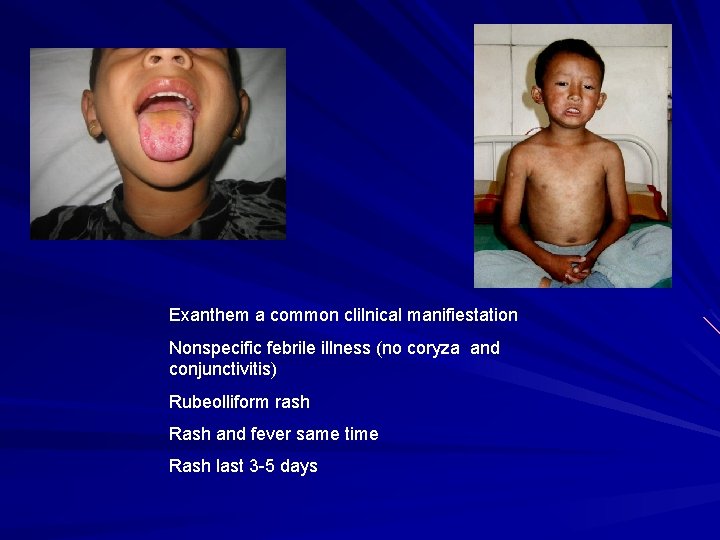
Exanthem a common clilnical manifiestation Nonspecific febrile illness (no coryza and conjunctivitis) Rubeolliform rash Rash and fever same time Rash last 3 -5 days

Case history: Five years , child – moderate fever, a hacking cough, runny nose, red eyes for three days. On examination – enanthem was present on the hard and soft palate. Grayish white dots were seen opposite the lower molars. On fourth day – temperature: 104ºF. Faint macules on the upper lateral parts of neck, behind the ears, along the hair line, and on the posterior parts of neck was noticed.
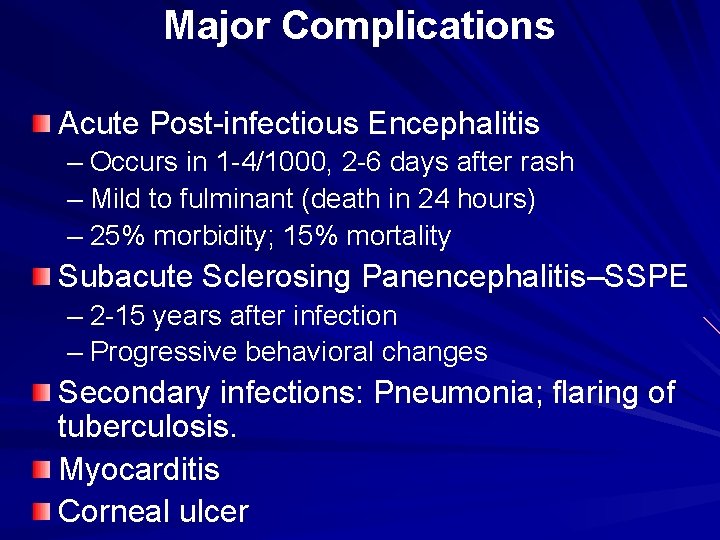
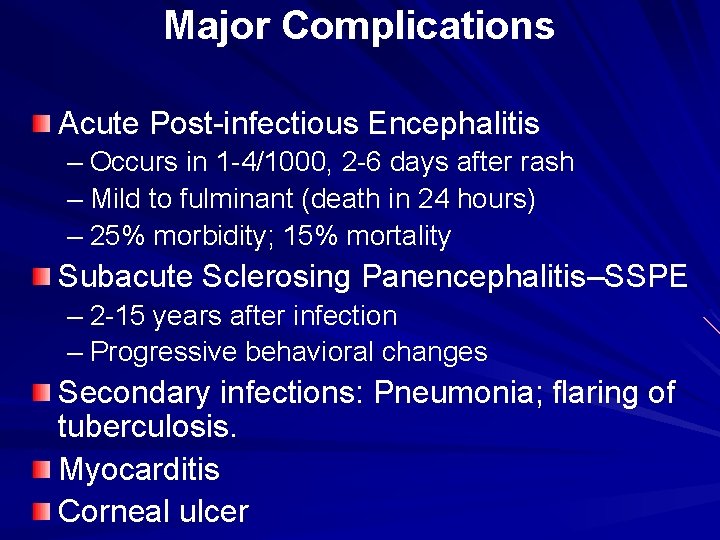
Major Complications Acute Post-infectious Encephalitis – Occurs in 1 -4/1000, 2 -6 days after rash – Mild to fulminant (death in 24 hours) – 25% morbidity; 15% mortality Subacute Sclerosing Panencephalitis–SSPE – 2 -15 years after infection – Progressive behavioral changes Secondary infections: Pneumonia; flaring of tuberculosis. Myocarditis Corneal ulcer
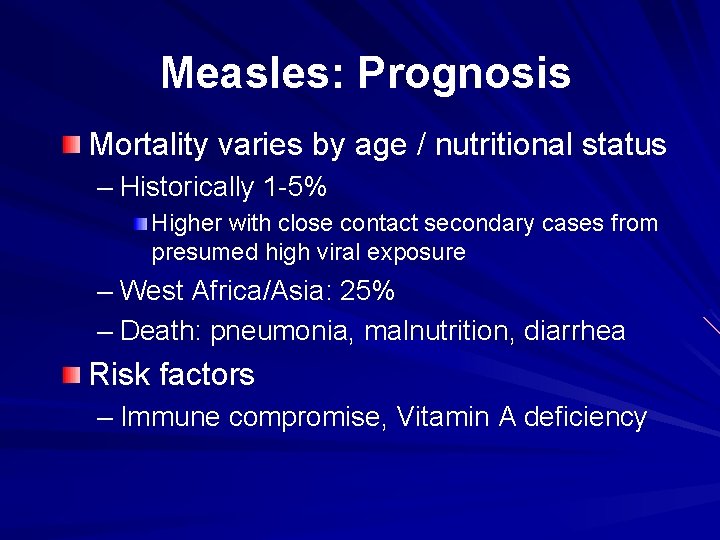
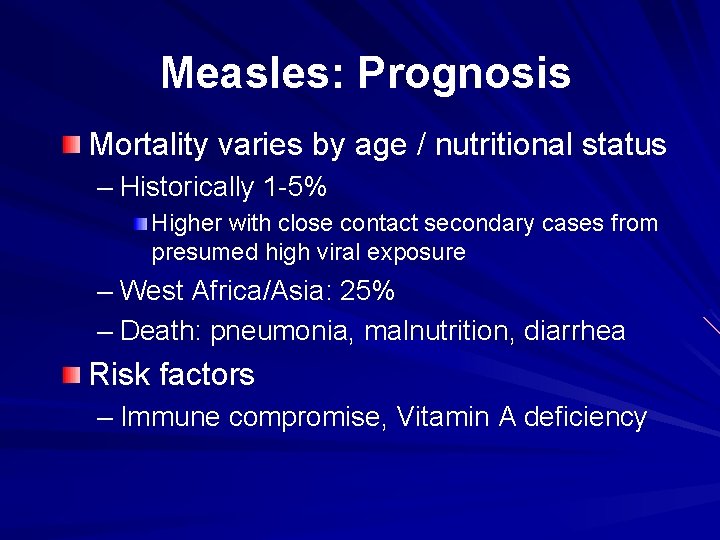
Measles: Prognosis Mortality varies by age / nutritional status – Historically 1 -5% Higher with close contact secondary cases from presumed high viral exposure – West Africa/Asia: 25% – Death: pneumonia, malnutrition, diarrhea Risk factors – Immune compromise, Vitamin A deficiency
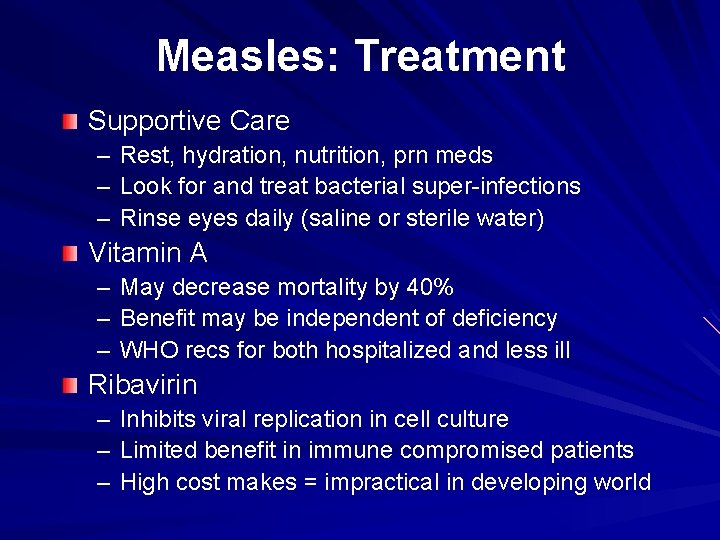
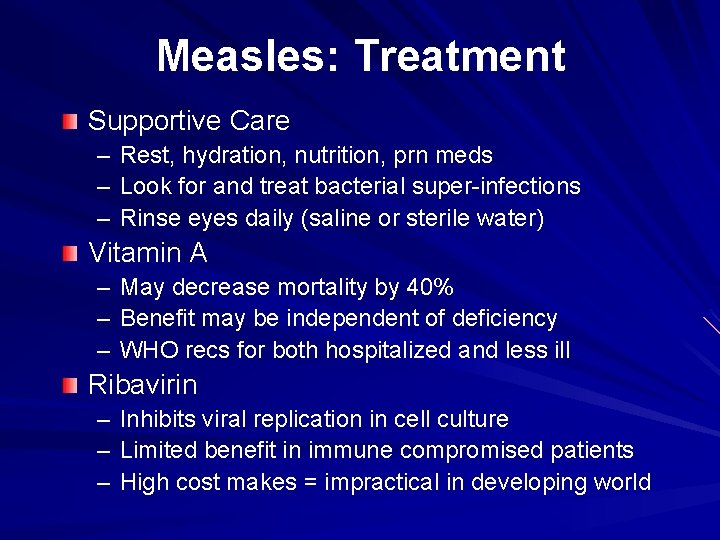
Measles: Treatment Supportive Care – Rest, hydration, nutrition, prn meds – Look for and treat bacterial super-infections – Rinse eyes daily (saline or sterile water) Vitamin A – May decrease mortality by 40% – Benefit may be independent of deficiency – WHO recs for both hospitalized and less ill Ribavirin – Inhibits viral replication in cell culture – Limited benefit in immune compromised patients – High cost makes = impractical in developing world
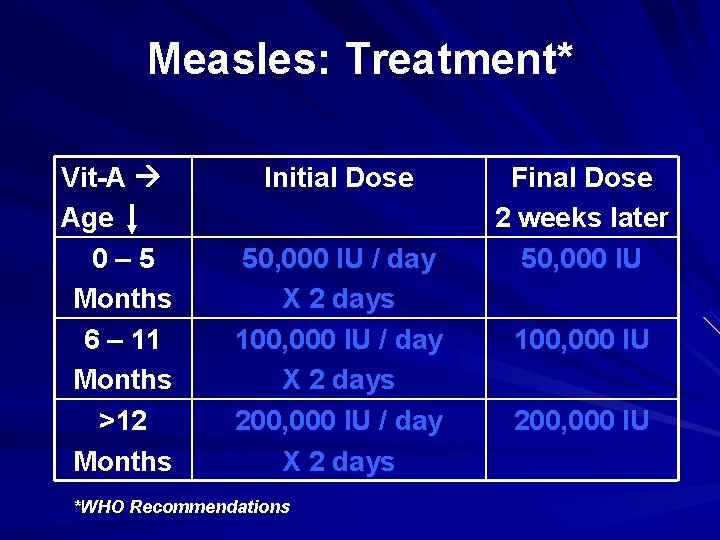
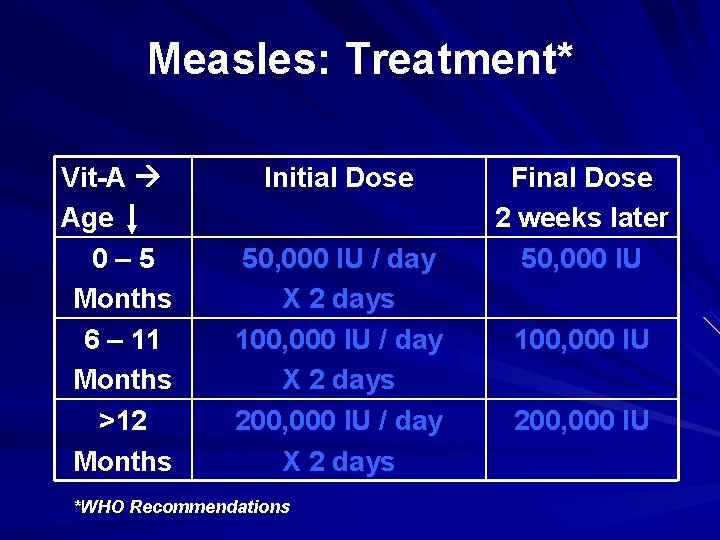
Measles: Treatment* Vit-A Age 0– 5 Months 6 – 11 Months >12 Months Initial Dose 50, 000 IU / day X 2 days 100, 000 IU / day X 2 days 200, 000 IU / day X 2 days *WHO Recommendations Final Dose 2 weeks later 50, 000 IU 100, 000 IU 200, 000 IU
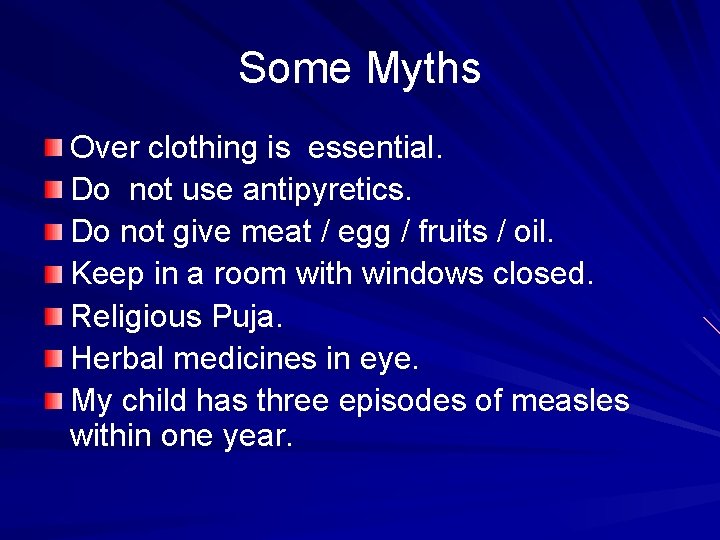
Some Myths Over clothing is essential. Do not use antipyretics. Do not give meat / egg / fruits / oil. Keep in a room with windows closed. Religious Puja. Herbal medicines in eye. My child has three episodes of measles within one year.
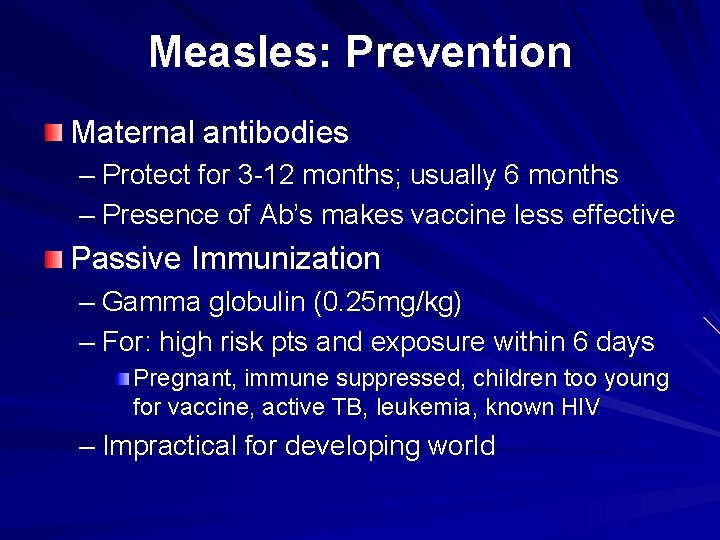
Measles: Prevention Maternal antibodies – Protect for 3 -12 months; usually 6 months – Presence of Ab’s makes vaccine less effective Passive Immunization – Gamma globulin (0. 25 mg/kg) – For: high risk pts and exposure within 6 days Pregnant, immune suppressed, children too young for vaccine, active TB, leukemia, known HIV – Impractical for developing world
Measles: Prevention Vaccine Immunization – Live attenuated vaccine – Efficacy (seroconversion) Lifelong immunity 9 months: 80 -85% Second dose with MMR at 16 months: >90% – Contraindications (live vaccine) Immune suppressed, leukemia, lymphoma, pregnancy, anaphylaxis to neomycin or gelatin Most recommend vaccinating HIV patients
Measles: Prevention Vitamin A – National Vit. A programme – Targets children >= 6 months old – Decrease mortality by improving nutrition – Benefit likely involves many infections, but measles is at the top
Neonatal Tetanus First described by Hippocrates Etiology discovered by Carle and Rattone in 1984 Passive immunity used for treatment and prophylaxis during World War I Tetanus toxoid first widely used during World War II
Tetanus Pathogenesis Anaerobic condition helps to germinate spores and production of toxins. Toxins binds to the central nervous system Interferes with the neurotransmitter release to block inhibitory impulses. Leads to unopposed muscle contraction and spasm.
Clinical Features Incubation period: 8 days (3 -21 days). Three clinical forms: –Local (not common) –Cephalilc (rare) –Generalised most common Descending symptoms of trismus, difficulty swallowing, muscle rigidity and spasm. Spasm continues ( consciousness retained)
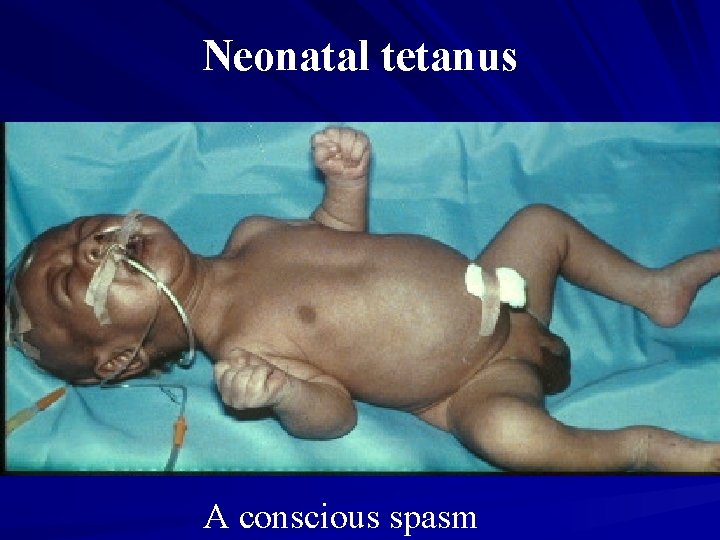
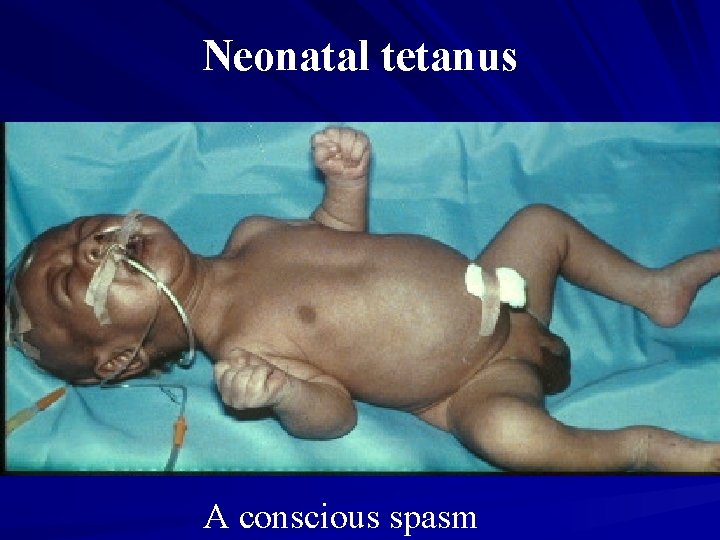
Neonatal tetanus A conscious spasm
Tetanus: complications Laryngospasm Hypoglycemia Nosocomial infections Myoglobinuria Aspiration Iatrogenic apnoea Death
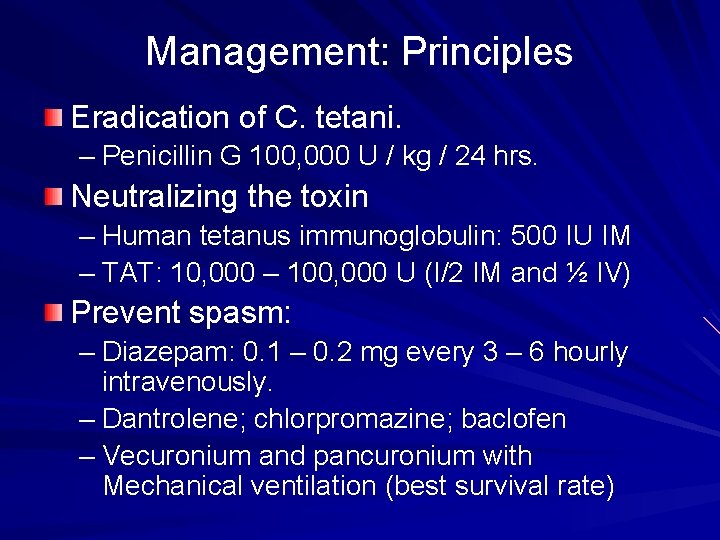
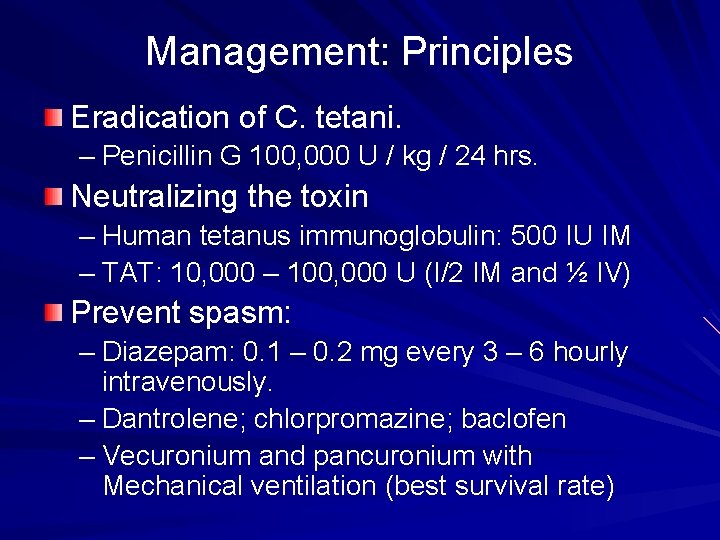
Management: Principles Eradication of C. tetani. – Penicillin G 100, 000 U / kg / 24 hrs. Neutralizing the toxin – Human tetanus immunoglobulin: 500 IU IM – TAT: 10, 000 – 100, 000 U (I/2 IM and ½ IV) Prevent spasm: – Diazepam: 0. 1 – 0. 2 mg every 3 – 6 hourly intravenously. – Dantrolene; chlorpromazine; baclofen – Vecuronium and pancuronium with Mechanical ventilation (best survival rate)
Management: contd. IV line. Nasogastric tube feeding. Minimal handling. A separate room.
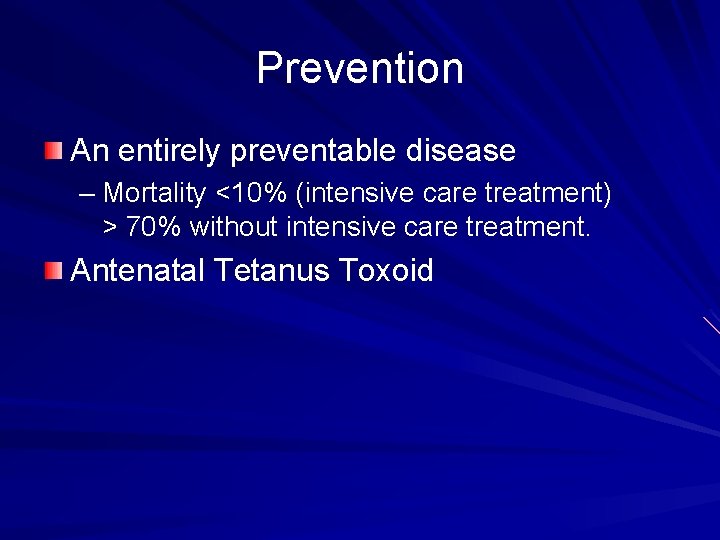
Prevention An entirely preventable disease – Mortality <10% (intensive care treatment) > 70% without intensive care treatment. Antenatal Tetanus Toxoid

www. prsharma. com. np
 Risus sardonicus
Risus sardonicus Mumps medicine
Mumps medicine Diff between measles and chickenpox
Diff between measles and chickenpox Pathophysiology of mumps
Pathophysiology of mumps Clostridium tetani
Clostridium tetani Measles mcq
Measles mcq Measles cdc
Measles cdc Measles cdc
Measles cdc Edge packing
Edge packing Measles cases
Measles cases Phase of dengue fever
Phase of dengue fever Branny desquamation measles
Branny desquamation measles Measles ppt 2020
Measles ppt 2020 Mrs measles
Mrs measles Sspe measles
Sspe measles Neuretic
Neuretic Fajar tetanua
Fajar tetanua Kepanjangan sdv paru
Kepanjangan sdv paru Muscle twitch
Muscle twitch Stair case phenomenon
Stair case phenomenon Tetanus lüge
Tetanus lüge Oppervlakkige hondenbeet tetanus
Oppervlakkige hondenbeet tetanus Incomplete tetanus muscle contraction
Incomplete tetanus muscle contraction Incomplete tetanus muscle contraction
Incomplete tetanus muscle contraction Clostridia family
Clostridia family Tetanus hondenbeet
Tetanus hondenbeet Tetanus
Tetanus Tetanus shot osha recordable
Tetanus shot osha recordable Tetanus
Tetanus Tetanus
Tetanus Sarkolema
Sarkolema Laatjevaccineren.be/tetanus-klem
Laatjevaccineren.be/tetanus-klem Fajar tetanua
Fajar tetanua Agedema
Agedema Hondenbeet tetanus
Hondenbeet tetanus