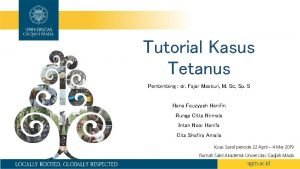
TETANUS INTRODUCTION Greek wordtetanos taut and stretched First











- Slides: 72
TETANUS
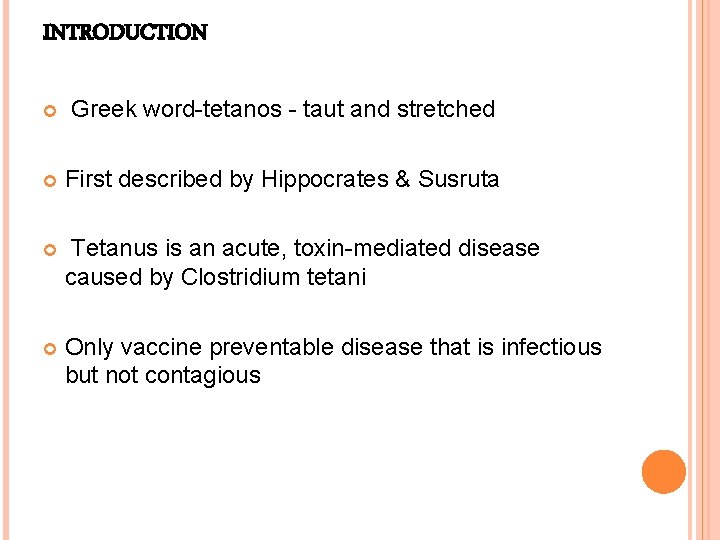
INTRODUCTION Greek word-tetanos - taut and stretched First described by Hippocrates & Susruta Tetanus is an acute, toxin-mediated disease caused by Clostridium tetani Only vaccine preventable disease that is infectious but not contagious
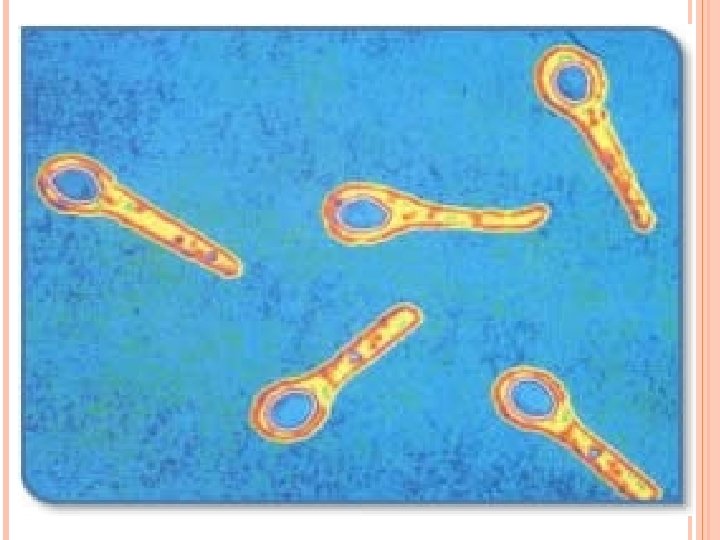
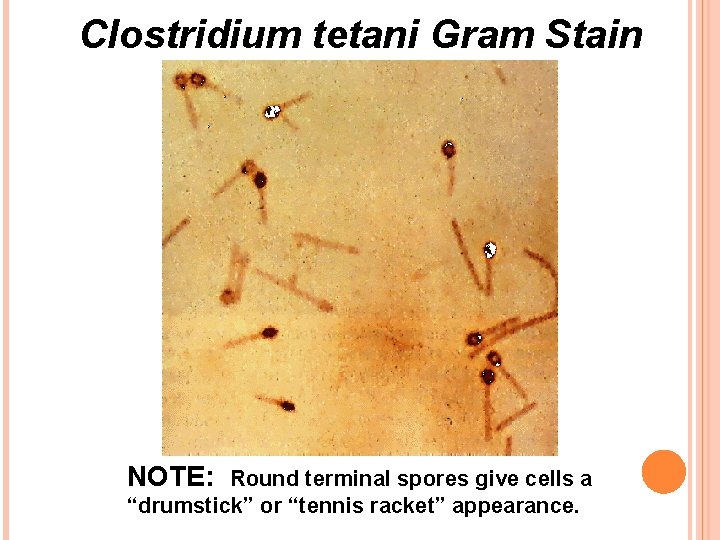
CAUSATIVE AGENT Caused by CLOSTRIDIUM TETANI Anaerobic Motile Gram positive bacilli Oval, colourless, terminal spores – tennis racket or drumstick shape. It is found worldwide in soil, in inanimate environment, in animal faeces & occasionally human faeces.
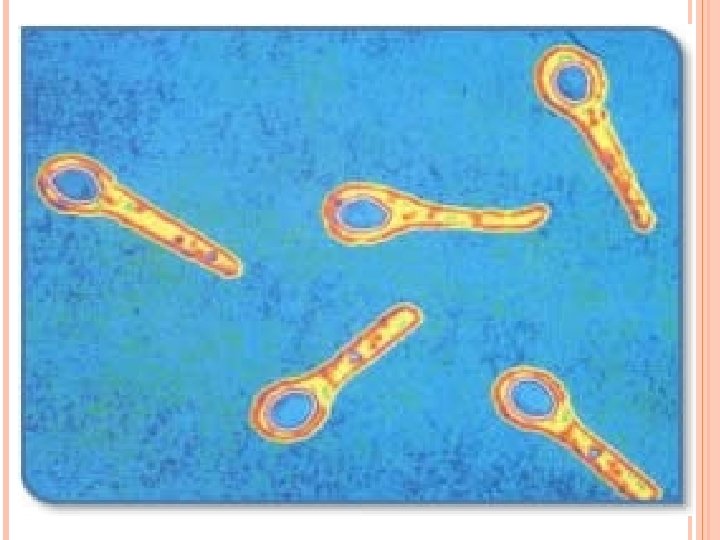
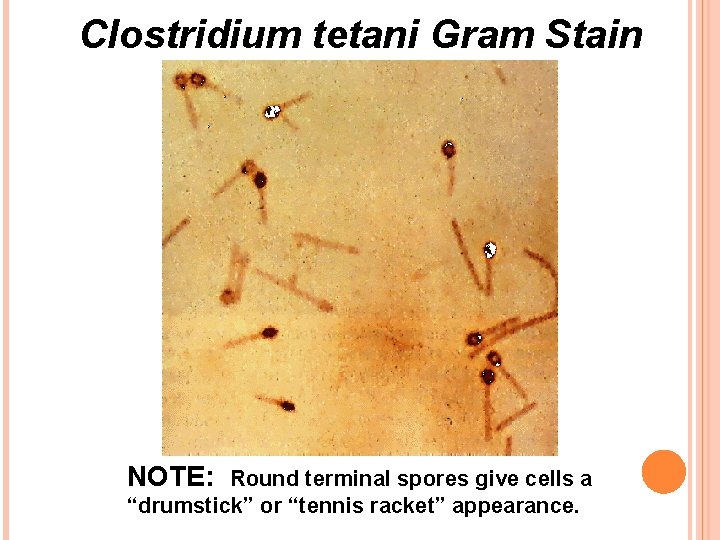
Clostridium tetani Gram Stain NOTE: Round terminal spores give cells a “drumstick” or “tennis racket” appearance.
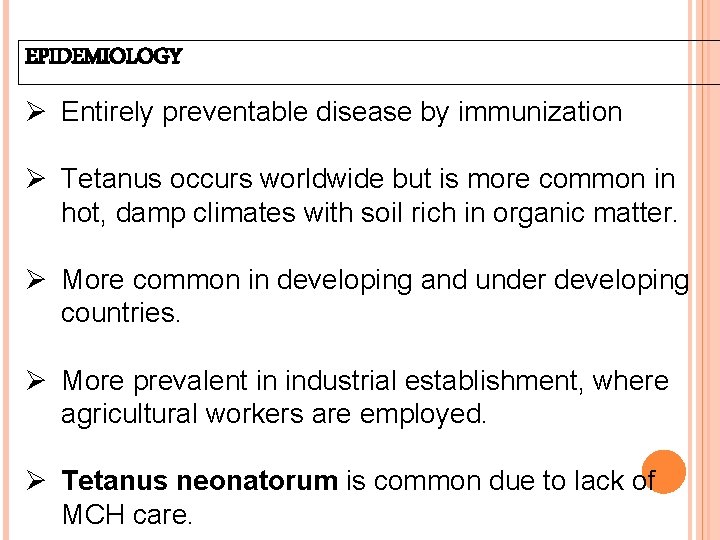
EPIDEMIOLOGY Ø Entirely preventable disease by immunization Ø Tetanus occurs worldwide but is more common in hot, damp climates with soil rich in organic matter. Ø More common in developing and under developing countries. Ø More prevalent in industrial establishment, where agricultural workers are employed. Ø Tetanus neonatorum is common due to lack of MCH care.
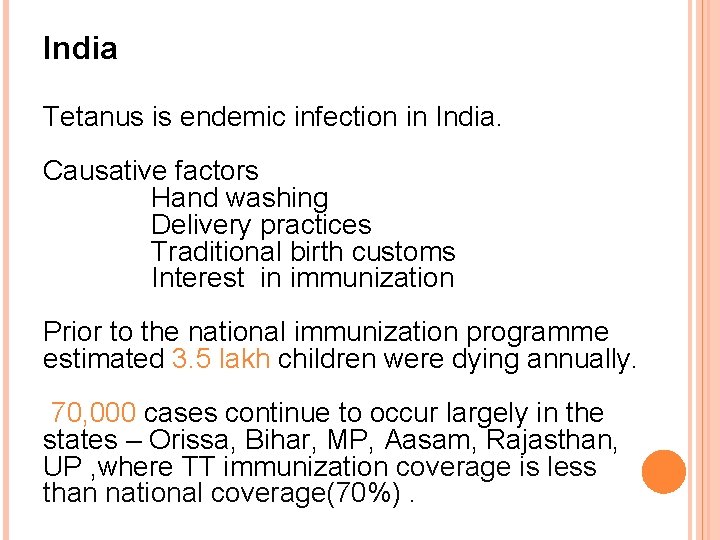
India Tetanus is endemic infection in India. Causative factors Hand washing Delivery practices Traditional birth customs Interest in immunization Prior to the national immunization programme estimated 3. 5 lakh children were dying annually. 70, 000 cases continue to occur largely in the states – Orissa, Bihar, MP, Aasam, Rajasthan, UP , where TT immunization coverage is less than national coverage(70%).
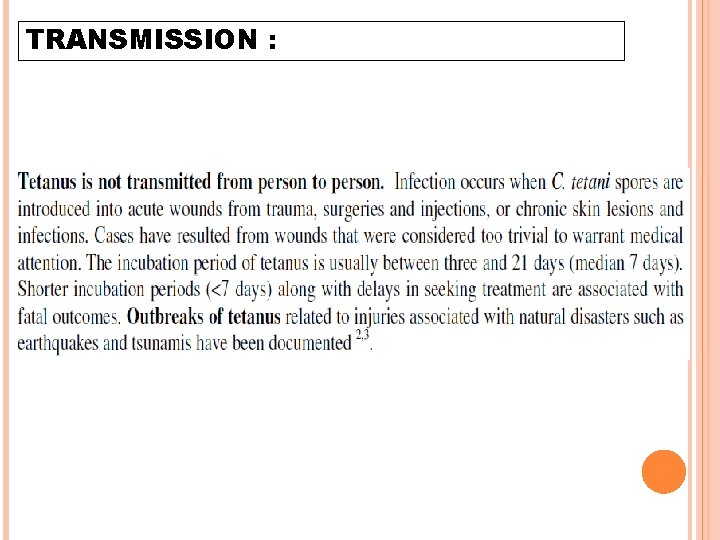
TRANSMISSION :
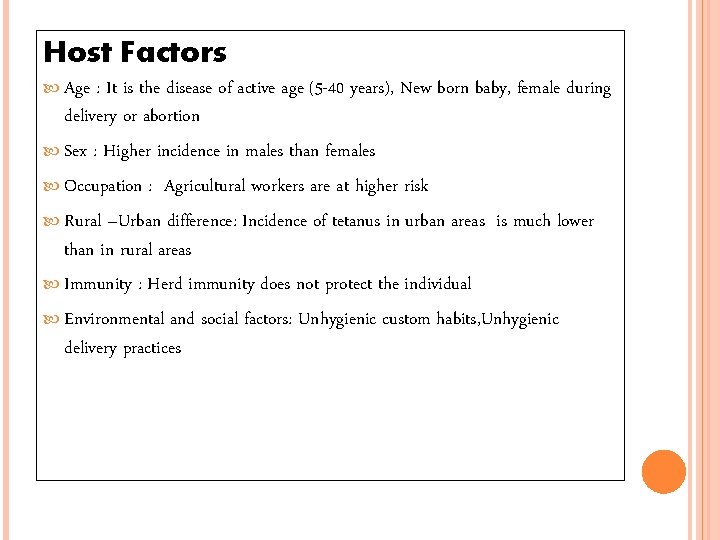
Host Factors Age : It is the disease of active age (5 -40 years), New born baby, female during delivery or abortion Sex : Higher incidence in males than females Occupation : Agricultural workers are at higher risk Rural –Urban difference: Incidence of tetanus in urban areas is much lower than in rural areas Immunity : Herd immunity does not protect the individual Environmental and social factors: Unhygienic custom habits, Unhygienic delivery practices
ROUTE OF ENTRY Apparently trivial injuries Animal bites/human bites Open fractures Burns Gangrene In neonates usually via infected umbilical stumps Abscess Parenteral drug abuse
TETANUS PRONE WOUND A wound sustained more than 6 hr before surgical treatment. A wound sustained at any interval after injury which is puncture type or shows much devitalised tissue or is septic or is contaminated with soil or manure.
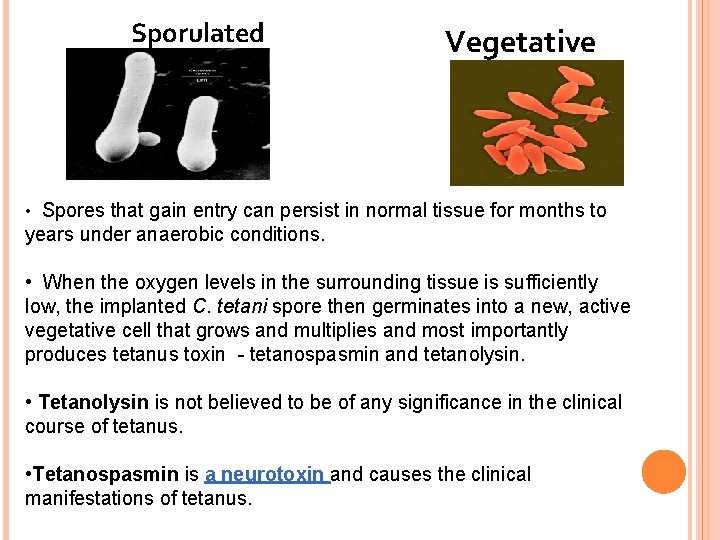
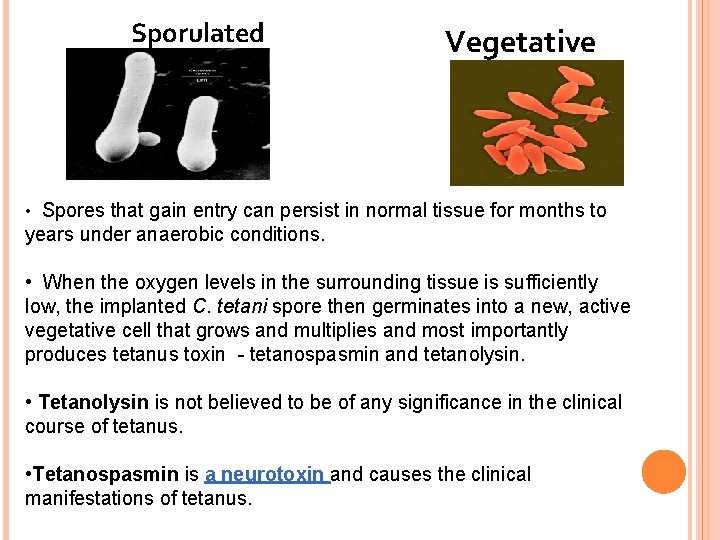
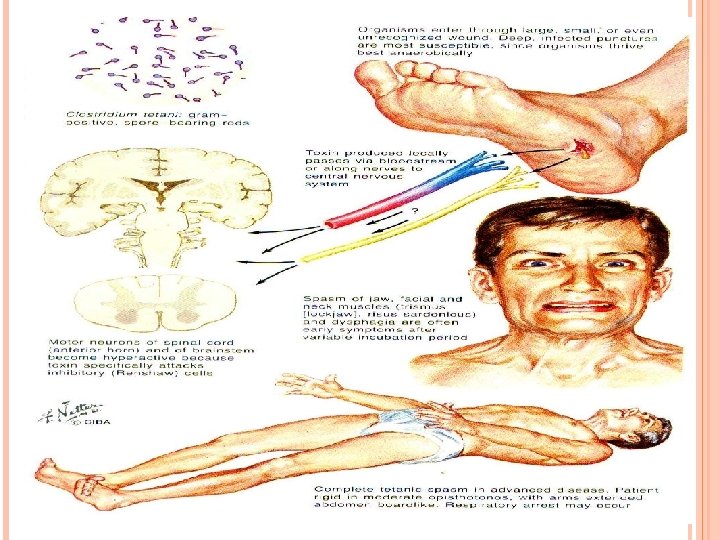
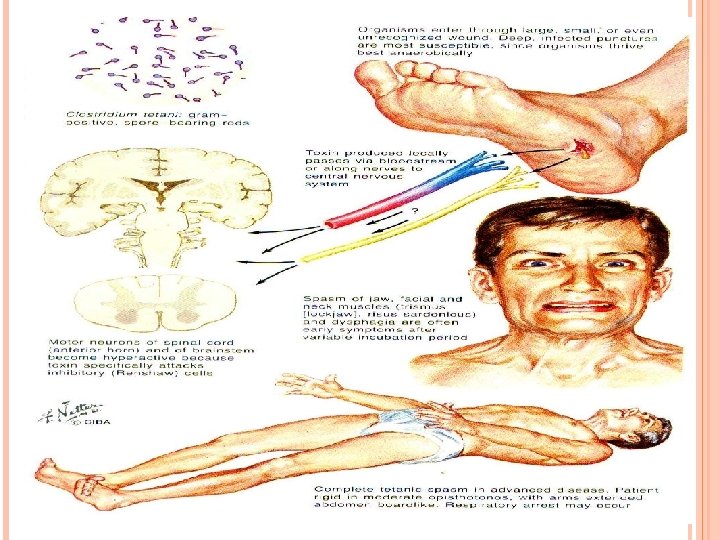
Sporulated Vegetative • Spores that gain entry can persist in normal tissue for months to years under anaerobic conditions. • When the oxygen levels in the surrounding tissue is sufficiently low, the implanted C. tetani spore then germinates into a new, active vegetative cell that grows and multiplies and most importantly produces tetanus toxin - tetanospasmin and tetanolysin. • Tetanolysin is not believed to be of any significance in the clinical course of tetanus. • Tetanospasmin is a neurotoxin and causes the clinical manifestations of tetanus.

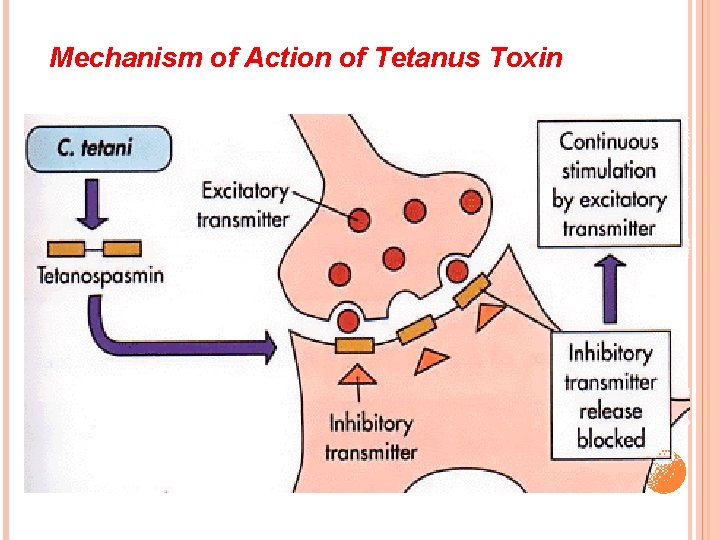
• The toxin migrates across the synapse (small space between nerve cells critical for transmission of signals among nerve cells) where it binds to presynaptic nerve terminals and inhibits or stops the release of certain inhibitory neurotransmitters (glycine and gamma-amino butyric acid). • Loss of inhibition of preganglionic sym neurons – sympathetic hyperactivity • These neurons become incapable to release neurotransmitter. The neurons, which release gammaaminobutyric acid (GABA) and glycine, the major inhibitory neurotransmitters, are particularly sensitive to tetanospasmin, leading to failure of inhibition of motor reflex responses to sensory stimulation.
Ø This results in generalized contractions of the agonist and antagonist musculature characteristic of a tetanic spasm. Ø The shortest peripheral nerves are the first to deliver the toxin to the CNS, which leads to the early symptoms of facial distortion and back and neck stiffness. Ø Once the toxin becomes fixed to neurons, it cannot be neutralized with antitoxin. Recovery of nerve function from tetanus toxins requires sprouting of new nerve terminals and formation of new synapses.
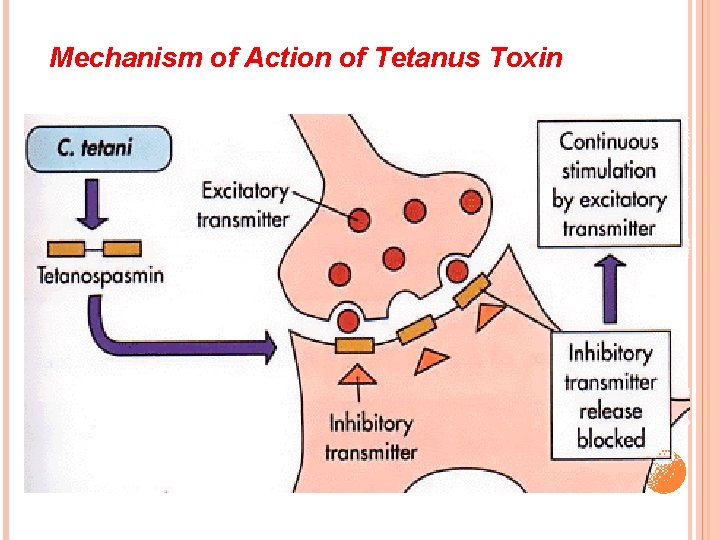
Mechanism of Action of Tetanus Toxin
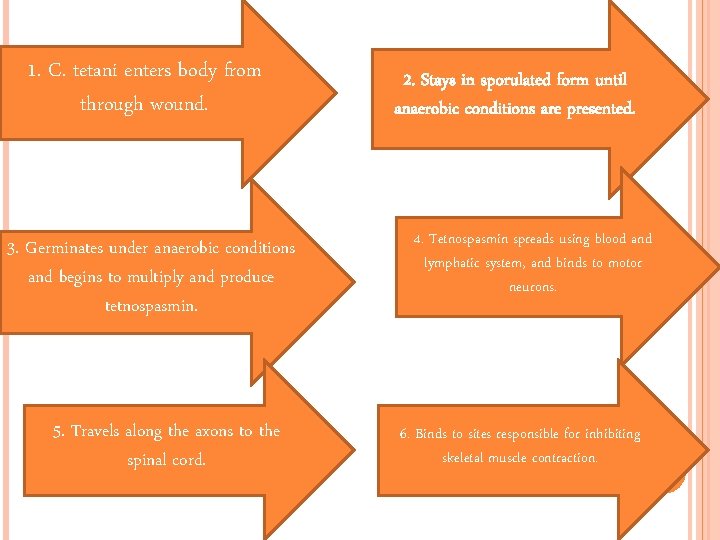
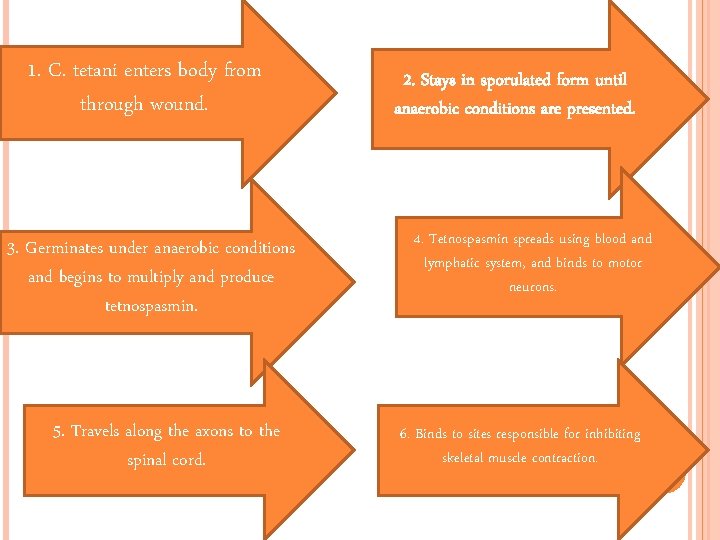
1. C. tetani enters body from through wound. 3. Germinates under anaerobic conditions and begins to multiply and produce tetnospasmin. 5. Travels along the axons to the spinal cord. 2. Stays in sporulated form until anaerobic conditions are presented. 4. Tetnospasmin spreads using blood and lymphatic system, and binds to motor neurons. 6. Binds to sites responsible for inhibiting skeletal muscle contraction.
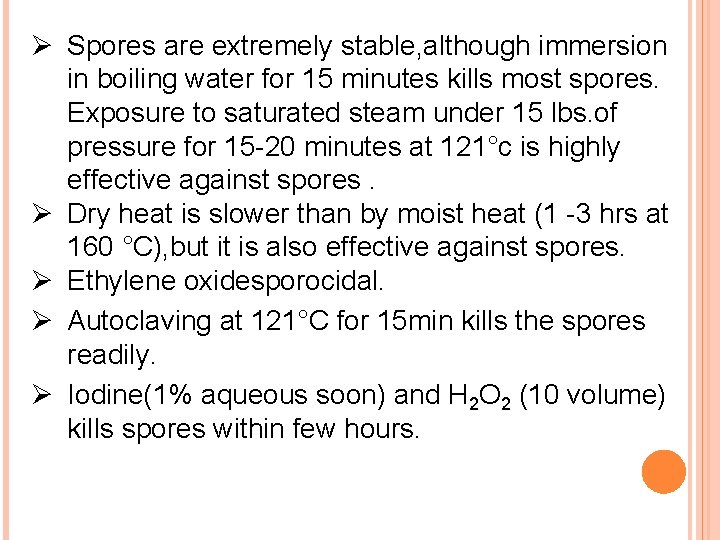
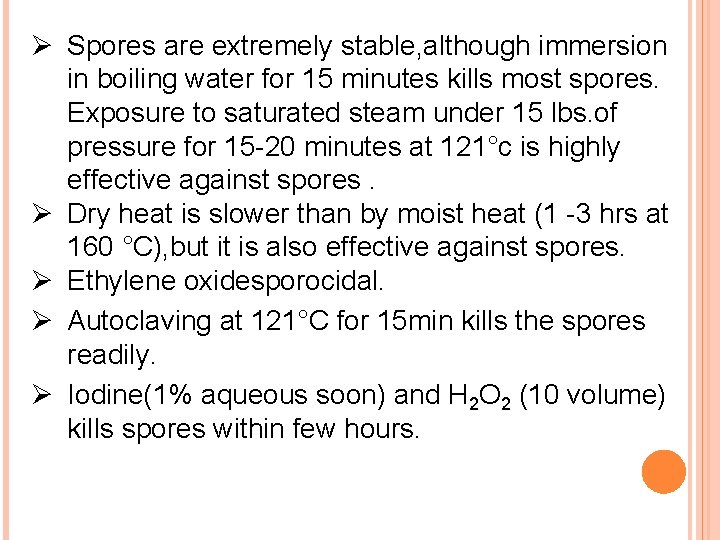
Ø Spores are extremely stable, although immersion in boiling water for 15 minutes kills most spores. Exposure to saturated steam under 15 lbs. of pressure for 15 -20 minutes at 121°c is highly effective against spores. Ø Dry heat is slower than by moist heat (1 -3 hrs at 160 °C), but it is also effective against spores. Ø Ethylene oxidesporocidal. Ø Autoclaving at 121°C for 15 min kills the spores readily. Ø Iodine(1% aqueous soon) and H 2 O 2 (10 volume) kills spores within few hours.
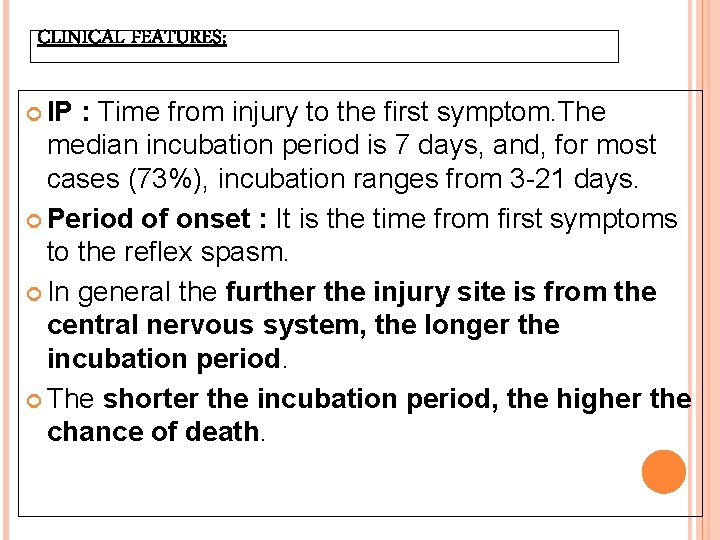
CLINICAL FEATURES: IP : Time from injury to the first symptom. The median incubation period is 7 days, and, for most cases (73%), incubation ranges from 3 -21 days. Period of onset : It is the time from first symptoms to the reflex spasm. In general the further the injury site is from the central nervous system, the longer the incubation period. The shorter the incubation period, the higher the chance of death.

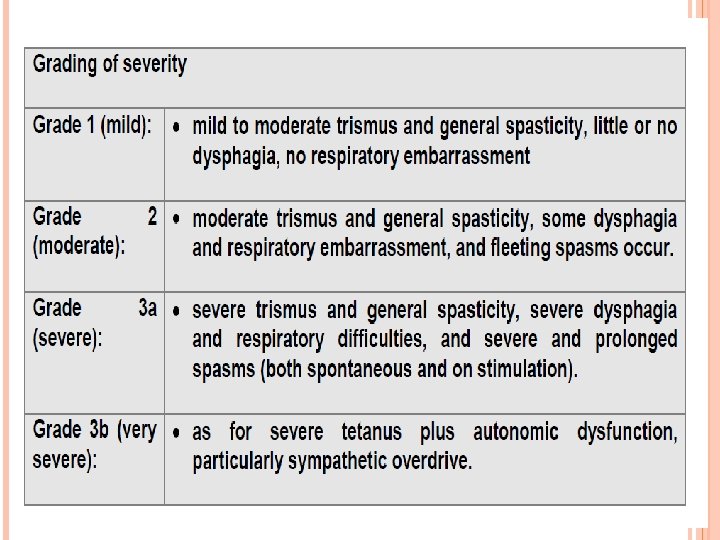
Triad of muscle rigidity, spasms & autonomic dysfunction Early symptoms are neck stiffness, sore throat and poor mouth opening. Patients with generalized tetanus present with trismus (ie, lockjaw) in 75% of cases. Other presenting complaints include stiffness, neck rigidity, dysphagia, restlessness, and reflex spasms. Spasms usually continue for 3 -4 weeks. Subsequently, muscle rigidity becomes the major manifestation. Rigid Abdomen. Muscle rigidity spreads in a descending pattern from the jaw and facial muscles over the next 24 -48 hours to the extensor muscles of the limbs – stiff proximal limb muscles & relatively sparing hand & feet.
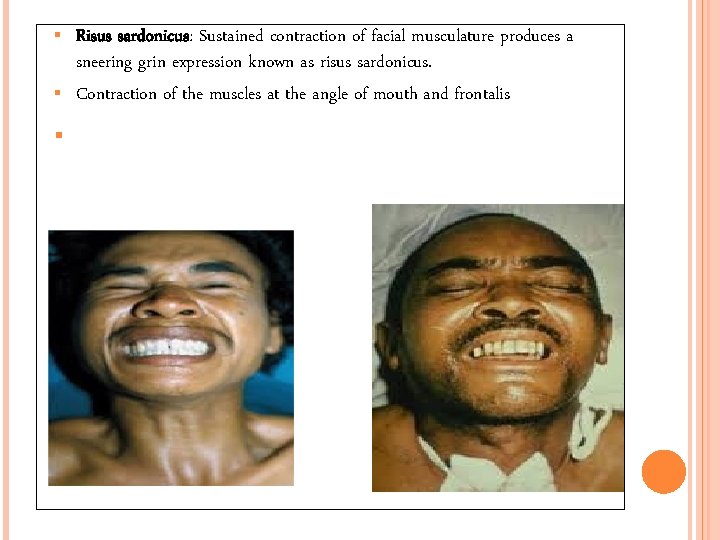
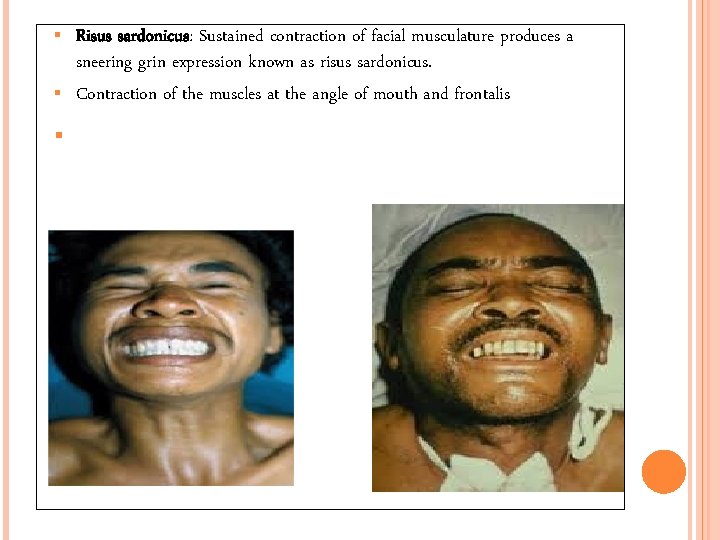
Risus sardonicus: Sustained contraction of facial musculature produces a sneering grin expression known as risus sardonicus. Contraction of the muscles at the angle of mouth and frontalis
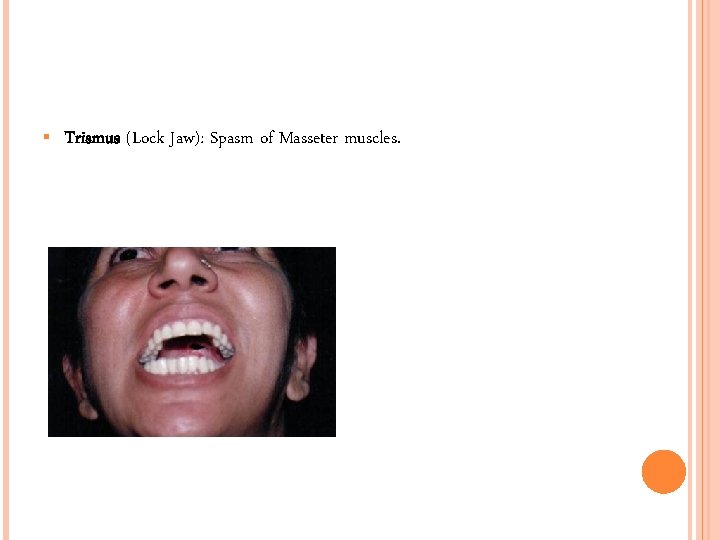
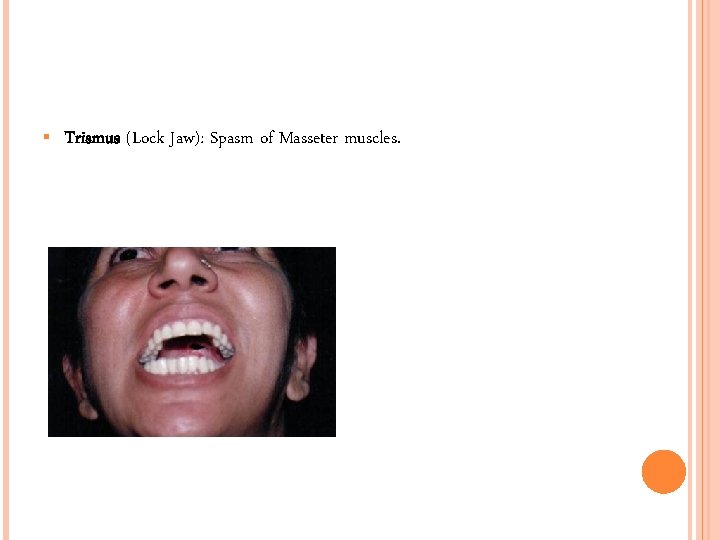
Trismus (Lock Jaw): Spasm of Masseter muscles.
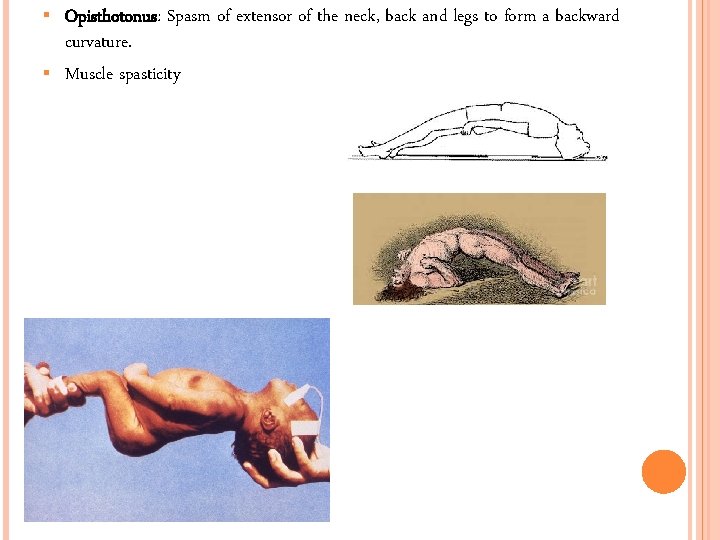
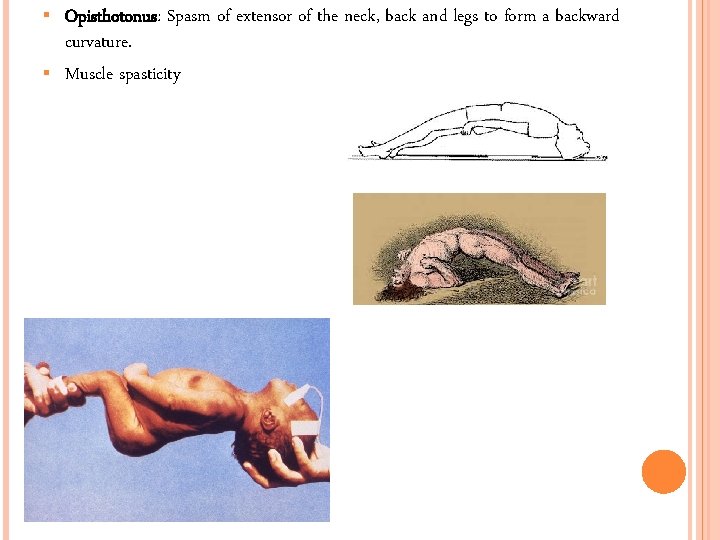
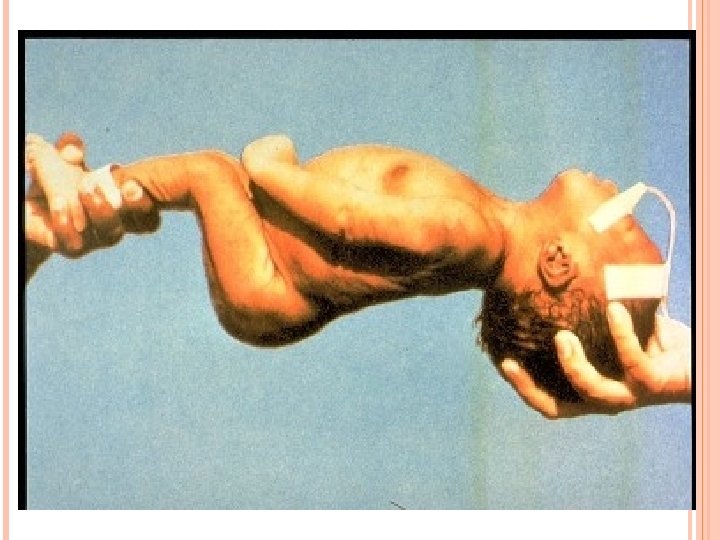
Opisthotonus: Spasm of extensor of the neck, back and legs to form a backward curvature. Muscle spasticity

Poor cough, inability to swallow, gastric stasis all increase the risk of aspiration. Respiratory failure continues to be a major cause of mortality in developing countries. whereas severe autonomic dysfunction causes most deaths in the developed world.
Dysphagia occurs in moderately severe tetanus due to pharyngeal muscle spasms. Reflex spasms triggered by minimal external stimuli such as noise, light, or touch. The spasms last seconds to minutes; become more intense; increase in frequency with disease progression; and can cause apnea, fractures, dislocations, and rhabdomyolysis. Laryngeal spasms can occur at any time and can result in asphyxia.
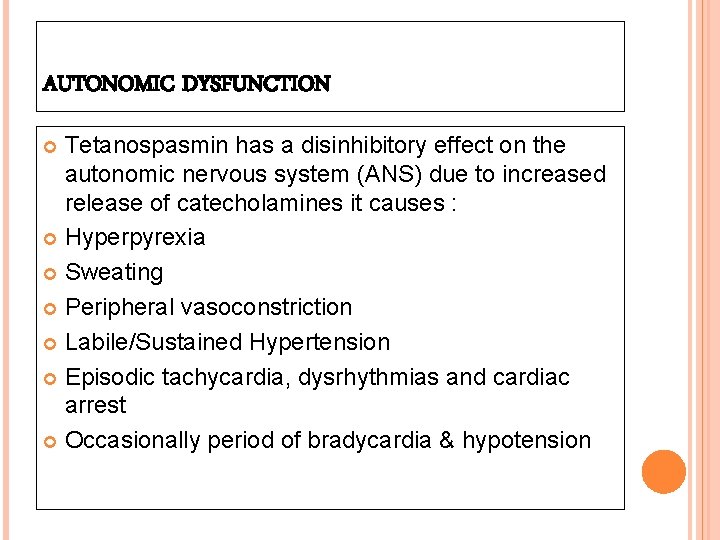
AUTONOMIC DYSFUNCTION Tetanospasmin has a disinhibitory effect on the autonomic nervous system (ANS) due to increased release of catecholamines it causes : Hyperpyrexia Sweating Peripheral vasoconstriction Labile/Sustained Hypertension Episodic tachycardia, dysrhythmias and cardiac arrest Occasionally period of bradycardia & hypotension
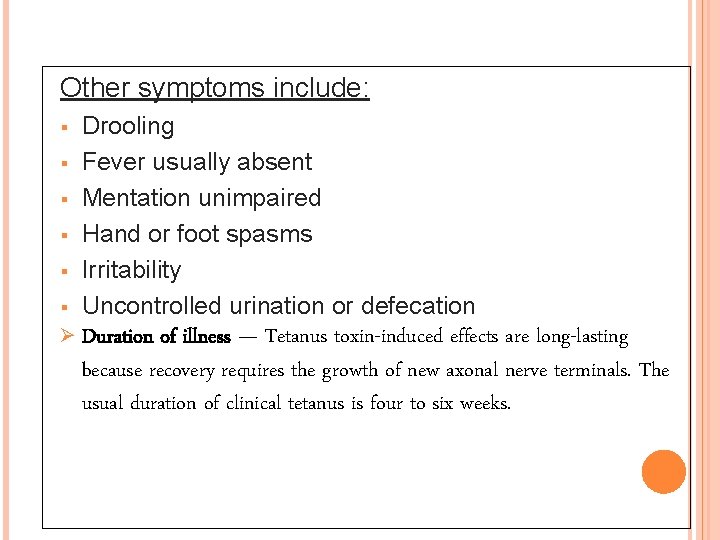
Other symptoms include: Drooling Fever usually absent Mentation unimpaired Hand or foot spasms Irritability Uncontrolled urination or defecation Ø Duration of illness — Tetanus toxin-induced effects are long-lasting because recovery requires the growth of new axonal nerve terminals. The usual duration of clinical tetanus is four to six weeks.
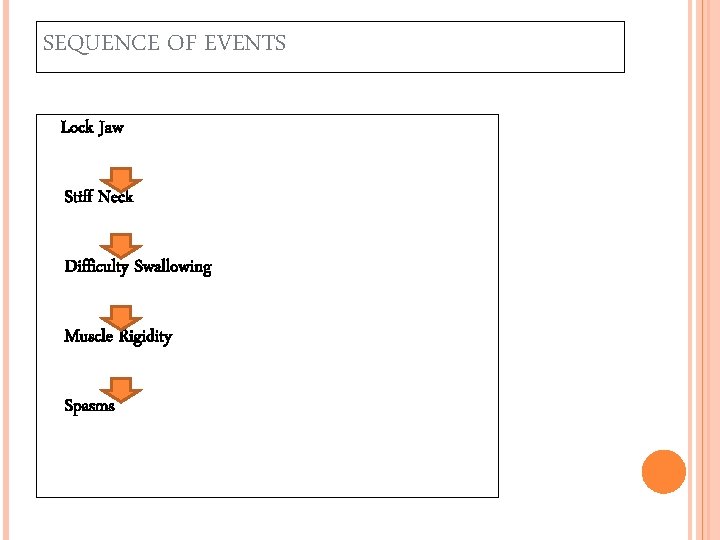
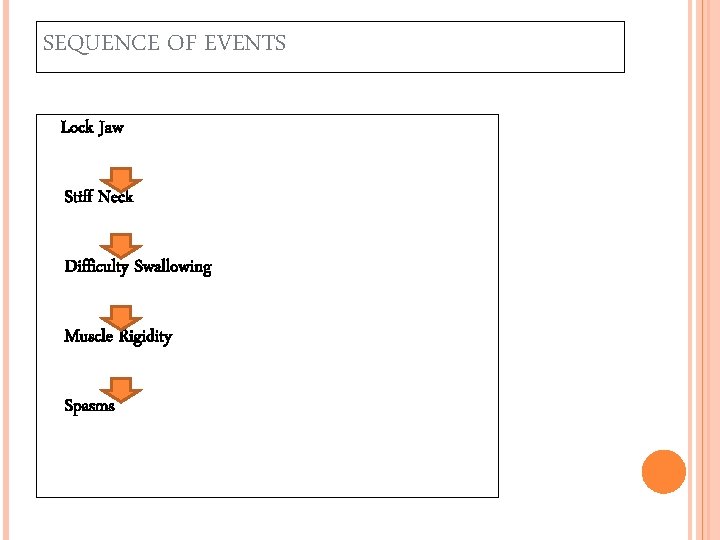
SEQUENCE OF EVENTS Lock Jaw Stiff Neck Difficulty Swallowing Muscle Rigidity Spasms
THANK YOU
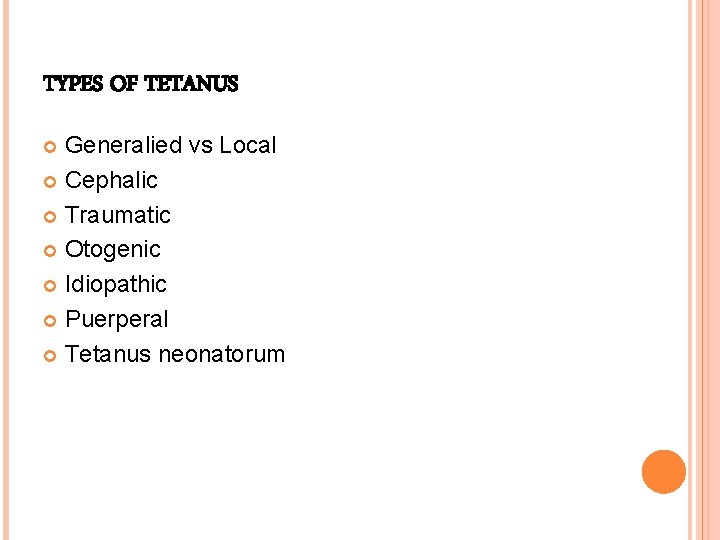
TYPES OF TETANUS Generalied vs Local Cephalic Traumatic Otogenic Idiopathic Puerperal Tetanus neonatorum
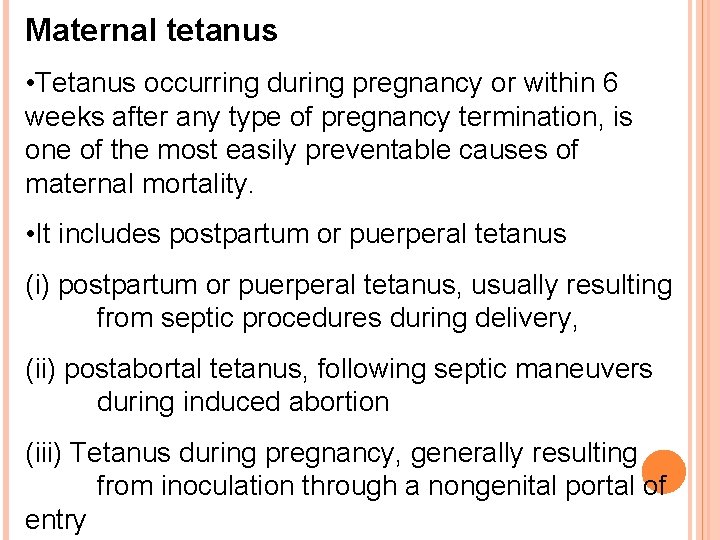
Maternal tetanus • Tetanus occurring during pregnancy or within 6 weeks after any type of pregnancy termination, is one of the most easily preventable causes of maternal mortality. • It includes postpartum or puerperal tetanus (i) postpartum or puerperal tetanus, usually resulting from septic procedures during delivery, (ii) postabortal tetanus, following septic maneuvers during induced abortion (iii) Tetanus during pregnancy, generally resulting from inoculation through a nongenital portal of entry
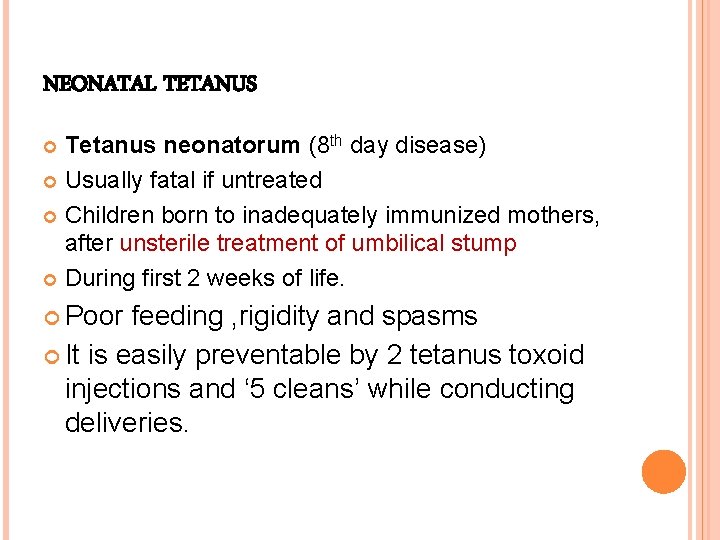
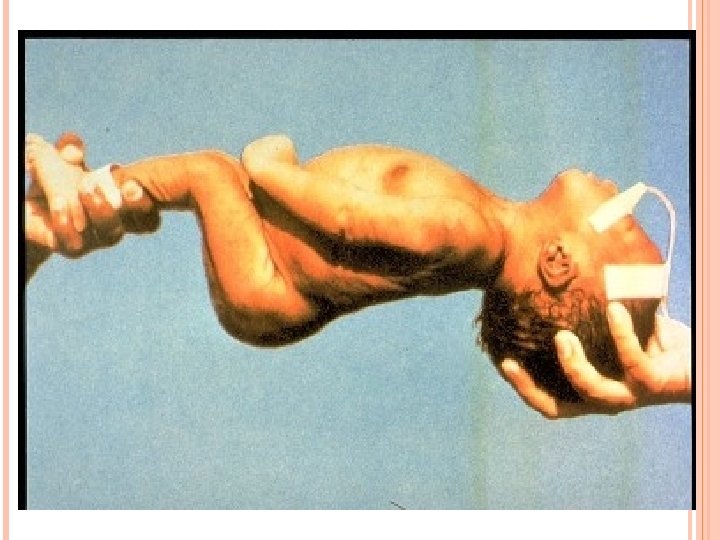
NEONATAL TETANUS Tetanus neonatorum (8 th day disease) Usually fatal if untreated Children born to inadequately immunized mothers, after unsterile treatment of umbilical stump During first 2 weeks of life. Poor feeding , rigidity and spasms It is easily preventable by 2 tetanus toxoid injections and ‘ 5 cleans’ while conducting deliveries.


LOCAL TETANUS Uncommon form Manifestations are restricted to muscles near the wound. Cramping and twisting in skeletal muscles surrounding the wound – local rigidity Prognosis – excellent
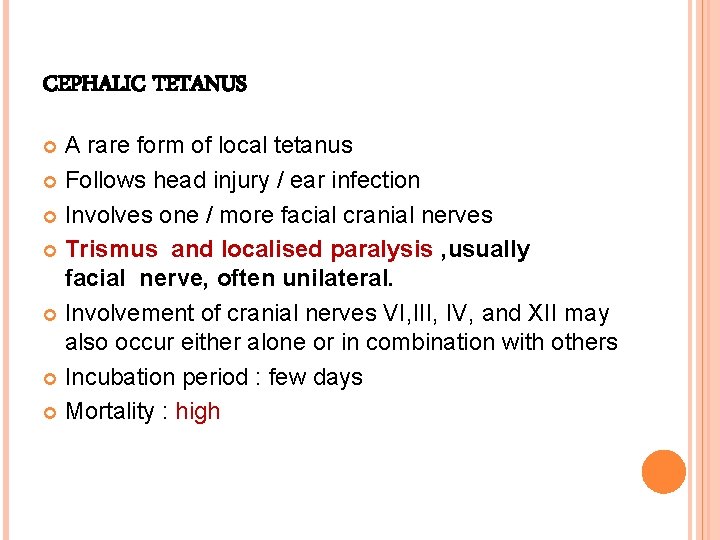
CEPHALIC TETANUS A rare form of local tetanus Follows head injury / ear infection Involves one / more facial cranial nerves Trismus and localised paralysis , usually facial nerve, often unilateral. Involvement of cranial nerves VI, III, IV, and XII may also occur either alone or in combination with others Incubation period : few days Mortality : high

Ophthalmoplegic tetanus is a variant that develops after penetrating eye injuries and results in CN III palsies and ptosis.
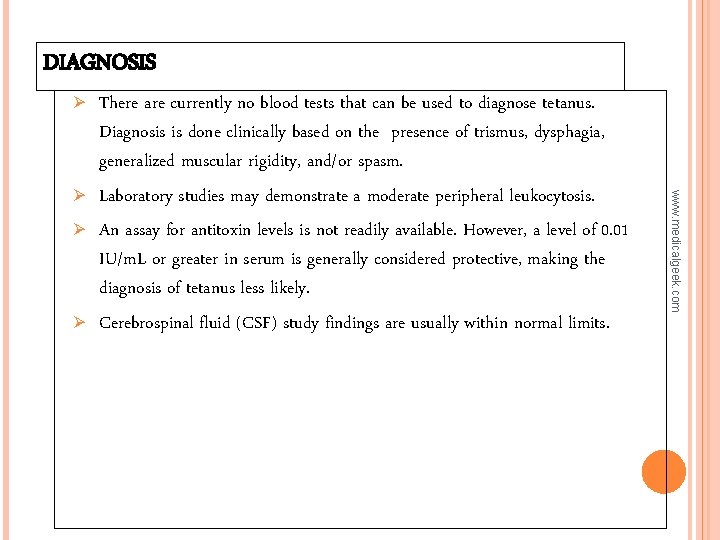
DIAGNOSIS Ø Ø Ø www. medicalgeek. com Ø There are currently no blood tests that can be used to diagnose tetanus. Diagnosis is done clinically based on the presence of trismus, dysphagia, generalized muscular rigidity, and/or spasm. Laboratory studies may demonstrate a moderate peripheral leukocytosis. An assay for antitoxin levels is not readily available. However, a level of 0. 01 IU/m. L or greater in serum is generally considered protective, making the diagnosis of tetanus less likely. Cerebrospinal fluid (CSF) study findings are usually within normal limits.
DIRECT SMEAR Show Gram-positive bacilli with drumstick appearance. Morphologically indistinguishable from similar nonpathogenic bacilli.

CULTURE Done in blood agar under anaerobic condition or in Robertson’s cooked meat medium. Produces swarming growth after 1 -2 days of incubation. In contaminated specimen heat at 80°C for 10 mins before culture to destroy non-sporing organisms.
ANIMAL INOCULATION To demonstrate toxigenicity. Positive case : test animal develops stiffness & spasm of tail & inoculated hind limb within 12 -24 hrs which spreads to rest of the body. Death occurs in 1 -2 days.
q Procedures: Ø The Ø Ø Ø spatula test is one diagnostic bedside test. This simple test involves touching the oropharynx with a spatula or tongue blade. This test typically elicits a gag reflex, and the patient tries to expel the spatula (ie, a negative test result). If tetanus is present, patients develop a reflex spasm of the masseters and bite the spatula (ie, a positive test result). Sensitivity of 94% and a specificity of 100%. [2] No adverse sequelae (eg, laryngeal spasm) from this procedure were reported
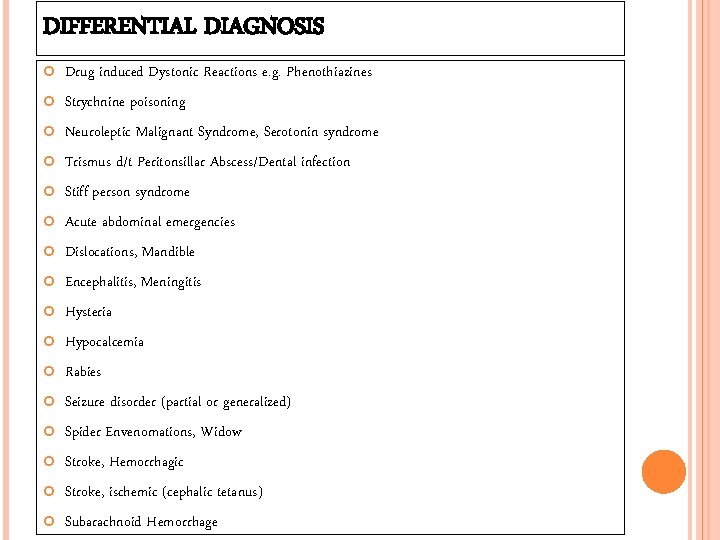
DIFFERENTIAL DIAGNOSIS Drug induced Dystonic Reactions e. g. Phenothiazines Strychnine poisoning Neuroleptic Malignant Syndrome, Serotonin syndrome Trismus d/t Peritonsillar Abscess/Dental infection Stiff person syndrome Acute abdominal emergencies Dislocations, Mandible Encephalitis, Meningitis Hysteria Hypocalcemia Rabies Seizure disorder (partial or generalized) Spider Envenomations, Widow Stroke, Hemorrhagic Stroke, ischemic (cephalic tetanus) Subarachnoid Hemorrhage
PRINCIPLE OF TREATMENT 1. Neutralization of unbound toxin -HTIG/ATS 2. Prevention of further toxin production -Wound debridement & antibiotics 3. Antibiotics 4. Control of spasm -Anticonvulsants, Sedatives, Muscle relaxants etc. 5. Management of autonomic dysfunction -MGSO 4, Betablockers etc. 6. Supportive care -Physiotherapy, Nutrition, Thromboembolism prophylaxis ABC etc…
1. NEUTRALIZATION OF UNBOUND TOXIN • • • www. medicalgeek. com • A single intramuscular dose of 3000 -5000 units (100 U/kg-half in each buttocks) is generally recommended for children and adults, with part of the dose infiltrated around the wound if it can be identified. The WHO recommends TIG 500 units by IM/IV (depending on the available preparation) as soon as possible; in addition, administer age-appropriate TTcontaining vaccine (Td, Tdap, DT, DPT, DTa. P, or TT depending on age or allergies), 0. 5 cc by intramuscular injection at separate site with HTIG. TIG can only help remove unbound tetanus toxin, but it cannot affect toxin bound to nerve endings. 250 U/vial available in our hospital, so 10 vial in each buttock is usual dose.
PRINCIPLE OF TREATMENT Admit patients to the intensive care unit (ICU). Because of the risk of reflex spasms, maintain a dark and quiet environment for the patient. Avoid unnecessary procedures and manipulations. Attempting endotracheal intubation may induce severe reflex laryngospasm; prepare for emergency tracheostomy. Seriously consider prophylactic tracheostomy in all patients with moderate-tosevere clinical manifestations. Intubation and ventilation are required in 67% of patients. Tracheostomy has also been recommended after onset of the first generalized seizure.
2. PREVENTION OF FURTHER TOXIN PRODUCTION • • Debridement of Wound to remove organisms and to create an aerobic environment. The current recommendation is to excise at least 2 cm of normal viableappearing tissue around the wound margins. Incise and drain abscesses. Delay any wound manipulation until several hours after administration of antitoxin due to risk of releasing tetanospasmin into the bloodstream.
3. ANTIBIOTICS Ø Ø Theoretically, antibiotics may prevent multiplication of C tetani, thus halting production of toxin. Penicillin G was the drug of choice initially but now Metronidazole is preffered drug. Penicillin G aqueous : (10 -12 MU IV in 2 -4 divided doses- 2 -4 MU IV every 4 to 6 hrs) Ø A 10 - to 14 -d course of treatment is recommended Ø Metronidazole: (5 oomg 6 hrly or 1 gm 12 hrly) Ø A 10 - to 14 -d course of treatment is recommended. Some consider this the DOC since penicillin G is also a GABA agonist, which may enhance effects of the toxin. Doxycycline, Clindamycin and Erythromycin are alternative for penicillin allergic patients who can not tolerate metronidazole. Ø
4. Control of spasm - Nursing in quiet environment, avoid unnecessary stimuli, Protecting the airway. - Drugs used to treat muscle spasm, rigidity, and tetanic seizures include sedativehypnotic agents, general anesthetics, centrally acting muscle relaxants, and neuromuscular blocking agents. - Anticonvulsants - Sedative-hypnotic agents are the mainstays of tetanus treatment. Benzodiazepines are the most effective primary agents for muscle spasm prevention and work by enhancing GABA inhibition. Diazepam : Mainstay of treatment of tetanic spasms and tetanic seizures. Depresses all levels of CNS, including limbic and reticular formation, possibly by increasing activity of GABA, a major inhibitory neurotransmitter.
Diazepam reduces anxiety, produces sedation, and relaxes muscles. Lorazepam is an effective alternative. Large amounts of either may be required (up to 600 mg/d). Diazepam or Midazolam can be used as 5 -10 mg iv/im every 1 -4 hrly. Midazolam can be given as an intravenous infusion (5 -15 mg/hr). Phenobarbitone (up to 200 mg IV or PO/NG 12 -hourly), and phenothiazines (usually chlorpromazine-25 mg/ml, 100 mg IM f/b 50 -100 mg 12 hrly) may be added as an adjunctive sedative. Propofol, dantrolene, intrathecal baclofen, succinylcholine & magnesium sulfate can be tried
Skeletal muscle relaxants: These agents can inhibit both monosynaptic and polysynaptic reflexes at spinal level, possibly by hyperpolarization of afferent terminals. Muscle relaxation is indicated where sedation alone is inadequate. Vecuronium (0. 1 mg/kg IV as needed) or atracurium (0. 5 mg/kg IV) are appropriate. Pancuronium may worsen autonomic instability by inhibiting catecholamine reuptake. Prolonged usage of aminosteroid muscle relaxants has been associated with critical illness neuropathy and myopathy.
BACLOFEN Intrathecal (IT) baclofen, a centrally acting muscle relaxant, has been used experimentally to wean patients off the ventilator and to stop diazepam infusion. IT baclofen is more potent than PO baclofen. May induce hyperpolarization of afferent terminals and inhibit both monosynaptic and polysynaptic reflexes at spinal level. Entire dose of baclofen is administered as a bolus injection. Dose may be repeated after 12 h or more if spontaneous paroxysms return. It can also be given as T. Baclofen 5 mg tds, increase 5 mg/day every 3 days, maximum dose 80 mg
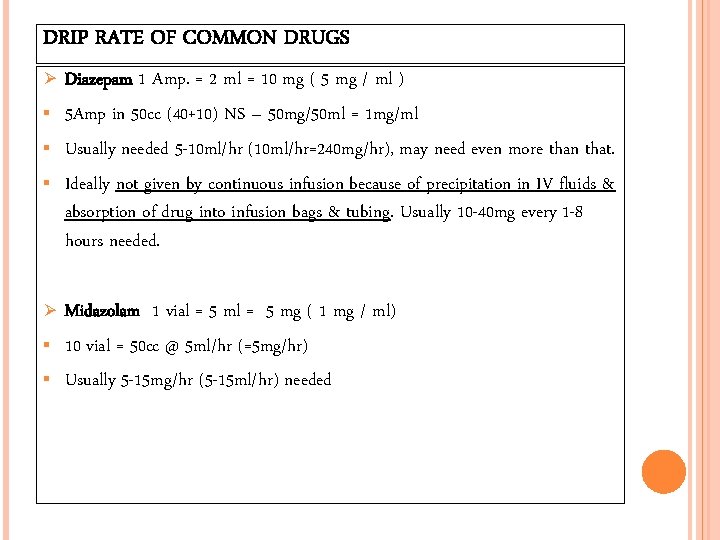
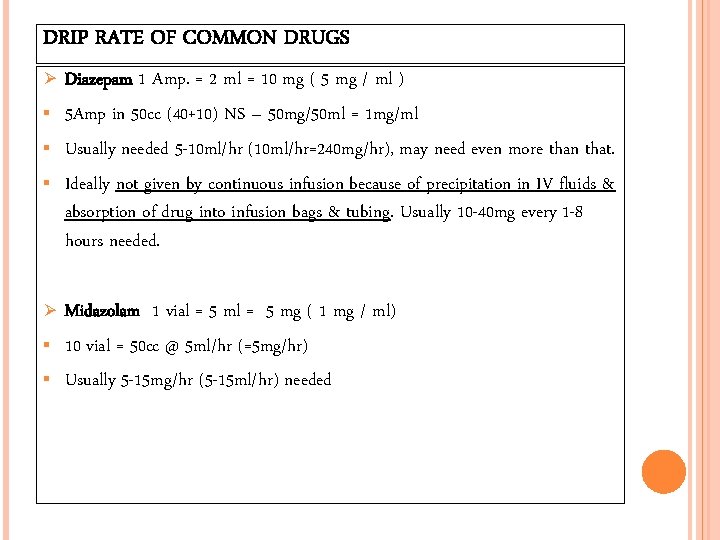
DRIP RATE OF COMMON DRUGS Ø Ø Diazepam 1 Amp. = 2 ml = 10 mg ( 5 mg / ml ) 5 Amp in 50 cc (40+10) NS – 50 mg/50 ml = 1 mg/ml Usually needed 5 -10 ml/hr (10 ml/hr=240 mg/hr), may need even more than that. Ideally not given by continuous infusion because of precipitation in IV fluids & absorption of drug into infusion bags & tubing. Usually 10 -40 mg every 1 -8 hours needed. Midazolam 1 vial = 5 mg ( 1 mg / ml) 10 vial = 50 cc @ 5 ml/hr (=5 mg/hr) Usually 5 -15 mg/hr (5 -15 ml/hr) needed
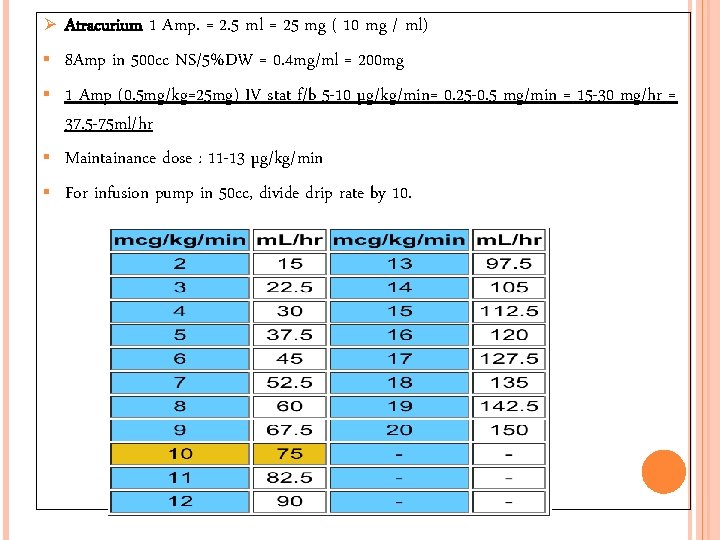
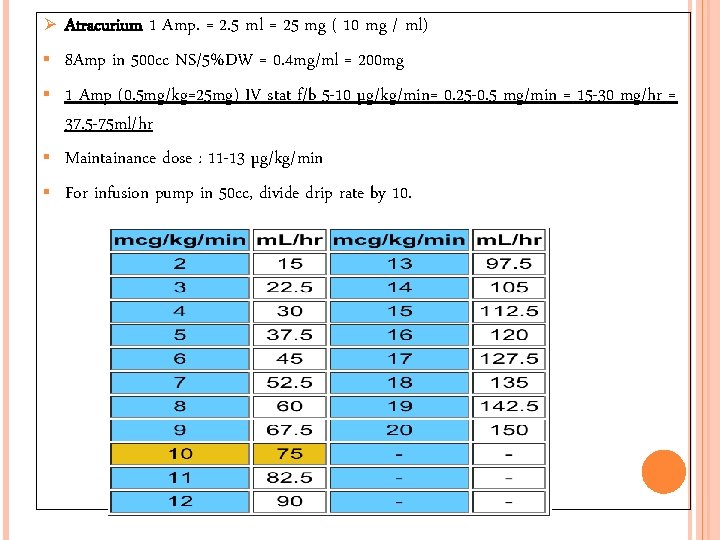
Ø Atracurium 1 Amp. = 2. 5 ml = 25 mg ( 10 mg / ml) 8 Amp in 500 cc NS/5%DW = 0. 4 mg/ml = 200 mg 1 Amp (0. 5 mg/kg=25 mg) IV stat f/b 5 -10 µg/kg/min= 0. 25 -0. 5 mg/min = 15 -30 mg/hr = 37. 5 -75 ml/hr Maintainance dose : 11 -13 µg/kg/min For infusion pump in 50 cc, divide drip rate by 10.
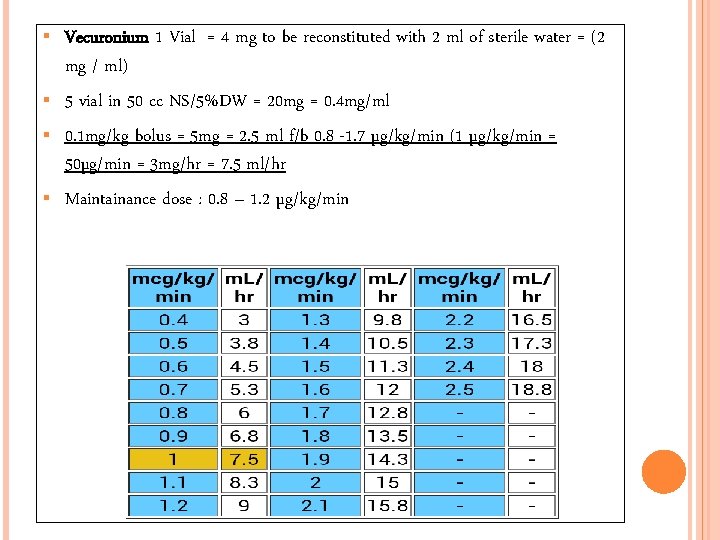
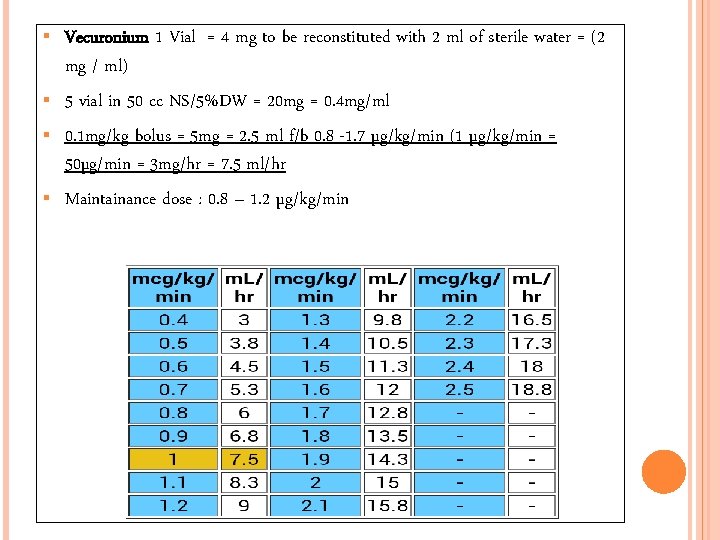
Vecuronium 1 Vial = 4 mg to be reconstituted with 2 ml of sterile water = (2 mg / ml) 5 vial in 50 cc NS/5%DW = 20 mg = 0. 4 mg/ml 0. 1 mg/kg bolus = 5 mg = 2. 5 ml f/b 0. 8 -1. 7 µg/kg/min (1 µg/kg/min = 50µg/min = 3 mg/hr = 7. 5 ml/hr Maintainance dose : 0. 8 – 1. 2 µg/kg/min
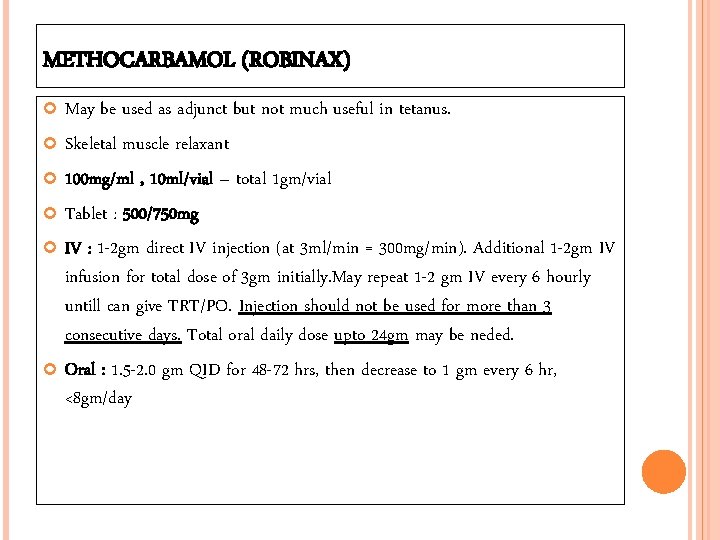
METHOCARBAMOL (ROBINAX) May be used as adjunct but not much useful in tetanus. Skeletal muscle relaxant 100 mg/ml , 10 ml/vial – total 1 gm/vial Tablet : 500/750 mg IV : 1 -2 gm direct IV injection (at 3 ml/min = 300 mg/min). Additional 1 -2 gm IV infusion for total dose of 3 gm initially. May repeat 1 -2 gm IV every 6 hourly untill can give TRT/PO. Injection should not be used for more than 3 consecutive days. Total oral daily dose upto 24 gm may be neded. Oral : 1. 5 -2. 0 gm QID for 48 -72 hrs, then decrease to 1 gm every 6 hr, <8 gm/day

5. MANAGEMENT OF AUTONOMIC DYSFUNCTION: Fluid loading is a useful in minimizing autonomic instability. Magnesium Sulphte: ØIt is an effective adjunct in relaxation , sedation & controlling the autonomic disturbance in tetanus. ØIt is a pre-syneptic neuromuscular blocker, reduces catecholemine release from nerves & adrenal medulla; and reduces responciveness to released catechlemines. ØA loading dose of 5 gm should be given over 20 minutes, followed by intravenous infusion of 2 gm/hr. the dose can be incresed by upto 0. 5 g/hr until spasms are relieved or the patellar reflex disappears.
Ø Ø If infusion devices are unavailable , give 2. 5 gm i. v. every 2 hours , titrating the frequency of administration to spasms. To avoid overdose, monitor patellar reflex as areflexia(absence of patellar reflex) occurs at the upper end of therapeutic range (4 mmol/L). If areflexia develops, dose should be decreased. By antagonizing the calcium metabolism Mg. SO 4 causes weakness & paralysis in overdose. Monitoring of serum magnesium level is important to prevent this: the normal serum magnesium level is 0. 7 - 1. 0 mmol/l & acceptable therapeutic level is 2 -3. 5 mmol/l. Another drugs: Labetalol Continuous infusion of esmolol Clonidine / verapamil Morphine
6. SUPPORTIVE CARE:
PREVENTION Tetanus is completely preventable by active tetanus immunization. Immunization is thought to provide protection for 10 years. Begins in infancy with the DTP series of shots. The DTP vaccine is a "3 -in-1" vaccine that protects against diphtheria, pertussis, and tetanus. www. medicalgeek. com

ACTIVE IMMUNIZATION 1 st dose 2 nd dose 3 rd dose 1 st booster 2 nd booster 3 rd booster - 6 th week (DPT) 10 th week (DPT) 14 th week (DPT) 18 th month (DPT) 6 th year (DT) 10 th year (TT)
MONOVALENT VACCINES Purified tetanus toxoid ( adsorbed ) supplanted the plain toxoid – higher & long lasting immunity response Primary course of immunization – 3 doses Each 0. 5 ml , injected into arm given at intervals of 0, 1, 6 months The longer the interval b/w two doses, better is the immune response Booster doses : After 1 yr f/b Every 10 yrs
Older teenagers and adults who have sustained injuries, especially puncture-type wounds, should receive booster immunization for tetanus if more than 10 years have passed since the last booster. Recovered clinical tetanus does not produce immunity to further attacks because very small amount of tetanus toxin produced can not elicit strong protective immune response. Therefore, even after recovery patients must receive a full course of tetanus toxoid.

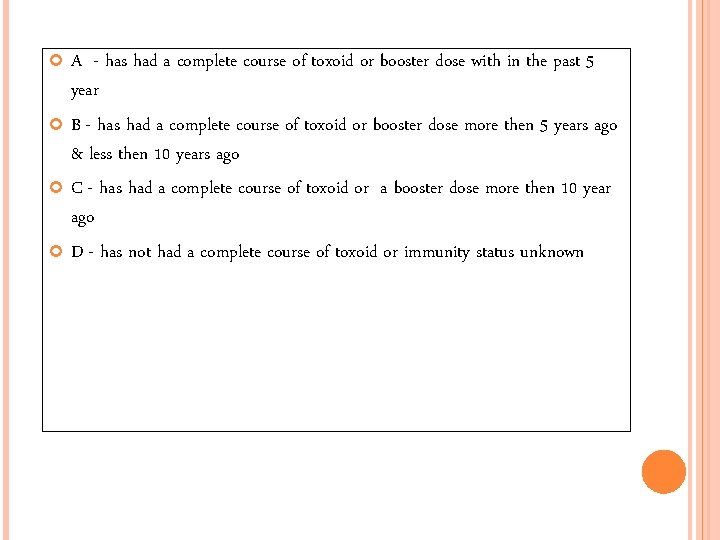
POSTEXPOSURE PROPHYLAXIS: All wound receive surgical toilet Wounds less then 6 hours other wounds Old , clean, non-penetrating, & with negligible tissue damage immunity treatment immunity category treatment category A nothing more required A B toxoid 1 dose C toxoid 1 dose + D toxoid complete course D nothing more required human tetanus Ig. toxoid complete course + human tetanus Ig
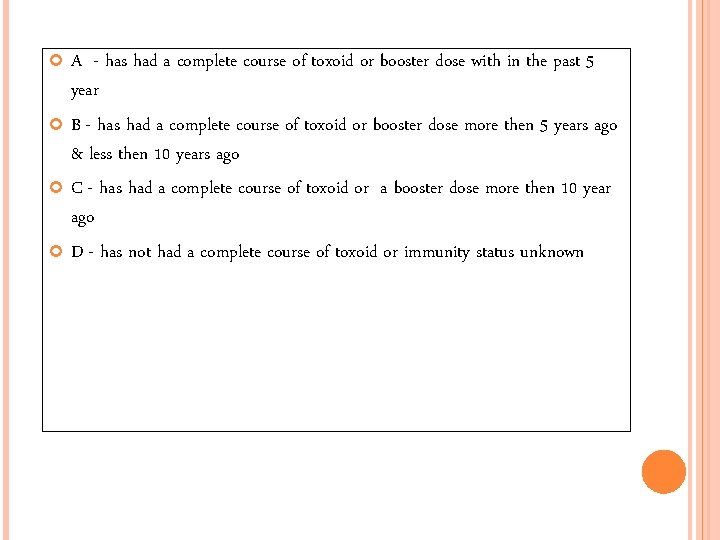
A - has had a complete course of toxoid or booster dose with in the past 5 year B - has had a complete course of toxoid or booster dose more then 5 years ago & less then 10 years ago C - has had a complete course of toxoid or a booster dose more then 10 year ago D - has not had a complete course of toxoid or immunity status unknown

PASSIVE IMMUNIZATION Temp protection – human tetanus immunoglobulin /ATS Human Tetanus Hyperimmunoglobulin : • 250 -500 IU • Produces protective antibody level for atleast 4 -6 weeks. • Does not cause serum sickness • Longer passive protection compared to horse ATS( 30 days / 7 -10 days )
PASSIVE IMMUNIZATION • • ATS ( EQUINE ) : 1500 IU s/c after sensitivity testing 7 – 10 days High risk of serum sickness It stimulates formation of antibodies to it , hence a person who has once received ATS tends to rapidly eliminate subsequent doses.
ACTIVE & PASSIVE IMMUNIZATION In non immunized persons 1500 IU of ATS / 250 -500 units of Human Ig in one arm & 0. 5 ml of adsorbed tetanus toxoid into other arm /gluteal region 6 wks later, 0. 5 ml of tetanus toxoid 1 yr later , 0. 5 ml of tetanus toxoid
PREVENTION OF NEONATAL TETANUS Clean delivery practices 3 cleans : clean hands, clean delivery surface, clean cord care Tetanus toxoid protects both mother & child Unimmunized pregnant women : 2 doses tetanus toxoid (16 th-36 th week) • 1 st dose as early as possible during pregnancy • 2 nd dose – at least a month later / 3 wks before delivery Immunized pregnant women : a booster is sufficient No need of booster in every consecutive pregnancy To newborn of unimmunized mother, 500 U HTIG within 6 hours of birth.
REFERECES: Ø Ø Ø Ø Harrison’s PRINCIPLES OF INTERNAL MEDICINE : Eighteenth Edition Textbook of preventive & social medicine – Park – 19 th Edition Up. To. Date (http: //www. uptodate. com) e. Medicine (http: //www. emedicine. com) Current recommendations for treatment of tetanus during humanitarian emergencies : WHO Technical Note World Federation of Societies of Anaesthesiologists - WFSA CDC Article - Tetanus
 Ndbpt
Ndbpt Stretched stem and leaf display
Stretched stem and leaf display Lactation tetany
Lactation tetany Transformations of linear functions
Transformations of linear functions Crack” went the bat as the pitcher hit a home run.
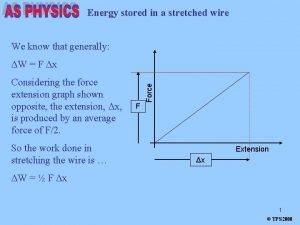
Crack” went the bat as the pitcher hit a home run. Wire stretch formula
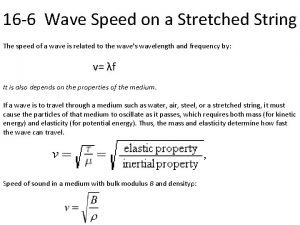
Wire stretch formula Wave speed on a stretched string
Wave speed on a stretched string Kafka stretch cluster
Kafka stretch cluster One's mind once stretched
One's mind once stretched Respiratory system zones
Respiratory system zones Philip score tetanus
Philip score tetanus Kepanjangan sdv paru
Kepanjangan sdv paru Treppe
Treppe What is staircase phenomenon
What is staircase phenomenon Tetanus lüge
Tetanus lüge Hondenbeet tetanus wanneer
Hondenbeet tetanus wanneer Incomplete tetanus muscle contraction
Incomplete tetanus muscle contraction Tetanus vs summation
Tetanus vs summation Charles bell tetanus
Charles bell tetanus Tetanus
Tetanus Prophalaxysis
Prophalaxysis Tetanus
Tetanus Osha log posting dates
Osha log posting dates Tetanus
Tetanus Clostridium perfringens lecithinase
Clostridium perfringens lecithinase Interkalárne disky
Interkalárne disky Laatjevaccineren.be/tetanus-klem
Laatjevaccineren.be/tetanus-klem Definisi tetanus
Definisi tetanus Nadia nour
Nadia nour Hondenbeet tetanus
Hondenbeet tetanus Tetanus symptoms
Tetanus symptoms Hondenbeet tetanus
Hondenbeet tetanus Vrbanac kod ljudi
Vrbanac kod ljudi Tetanus def
Tetanus def Tetanus
Tetanus Tetanus neonatorum ppt
Tetanus neonatorum ppt Latch state smooth muscle
Latch state smooth muscle What is the greek miracle in greek mythology
What is the greek miracle in greek mythology Entity framework 7 release date
Entity framework 7 release date Breadth first and depth first search
Breadth first and depth first search Ekkylema
Ekkylema Ekkylema
Ekkylema Greek tragedy definition
Greek tragedy definition Theatron greek theatre definition
Theatron greek theatre definition An introduction to greek philosophy
An introduction to greek philosophy Civilization
Civilization The maturity continuum 7 habits
The maturity continuum 7 habits Sdl first vs code first
Sdl first vs code first Habit 3 lesson plans
Habit 3 lesson plans Put first things first meaning
Put first things first meaning First to file vs first to invent
First to file vs first to invent Data structure stack
Data structure stack First in first out
First in first out First come first serve
First come first serve Put first things first definition
Put first things first definition Sjf cpu scheduling
Sjf cpu scheduling See-do-get model example
See-do-get model example Habit 3 activities
Habit 3 activities Put first things first video
Put first things first video Habit 3 activities
Habit 3 activities First aid merit badge first aid kit
First aid merit badge first aid kit What are the objectives of first aid?
What are the objectives of first aid? Put first things first
Put first things first A great introduction
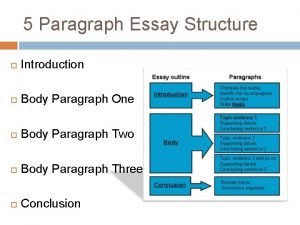
A great introduction Body paragraph structure
Body paragraph structure Greek and latin roots and affixes unit 1 answer key
Greek and latin roots and affixes unit 1 answer key Ante root word examples
Ante root word examples Root word dyna
Root word dyna Newton's first law and second law and third law
Newton's first law and second law and third law Newton's first law
Newton's first law First person second third examples
First person second third examples Neurological considerations in language acquisition
Neurological considerations in language acquisition