In the name of GOD Principles of MECHANICAL






- Slides: 128
In the name of GOD Principles of MECHANICAL VENTILATION 1
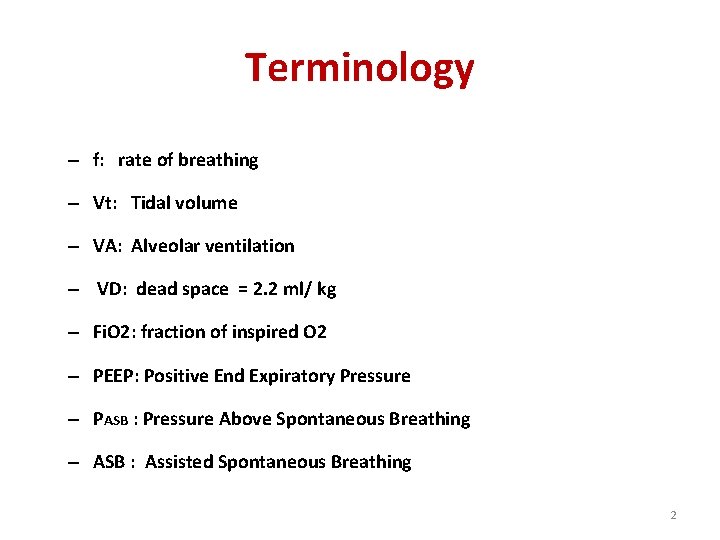
Terminology – f: rate of breathing – Vt: Tidal volume – VA: Alveolar ventilation – VD: dead space = 2. 2 ml/ kg – Fi. O 2: fraction of inspired O 2 – PEEP: Positive End Expiratory Pressure – PASB : Pressure Above Spontaneous Breathing – ASB : Assisted Spontaneous Breathing 2
Basic pulmonary physiology �Air that moves in and out of a patient's lungs per minute that is 7 -10 L/min Minute volume (MV) �MV =Vt x f � Alveolar ventilation (VA) in contact with the alveolar-capillary gas exchange interface �VA = (Vt - VD ) x f �Volume-pressure relation: P = V/C 3
Plateau pressure (static pressure) • … is the pressure at the end of inspiration with a short breath hold • It should not be exceed 30 cm. H 2 O • P plateau ~ 1/compliance (P = V/C) • volume = P plateau 4
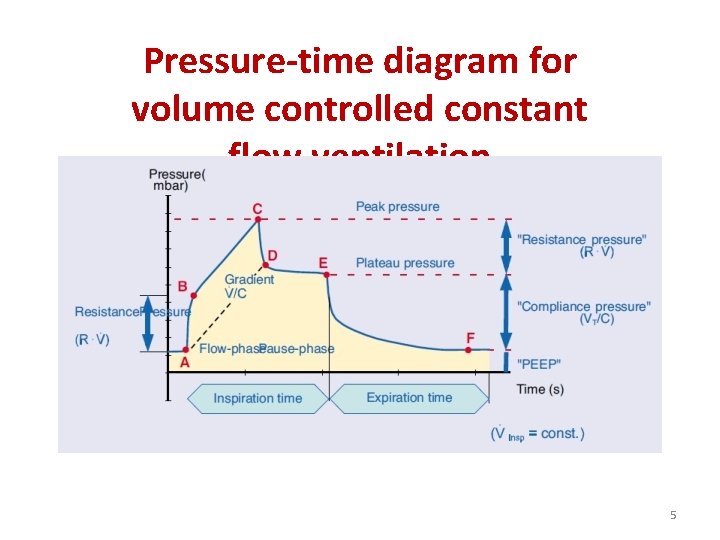
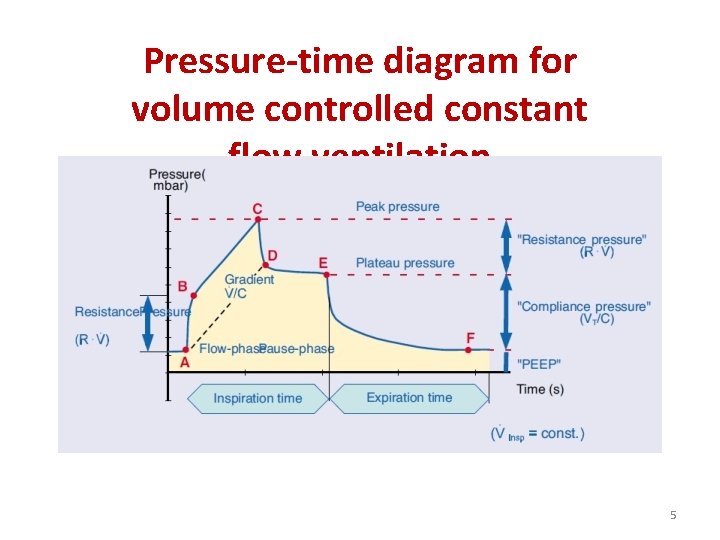
Pressure-time diagram for volume controlled constant flow ventilation 5
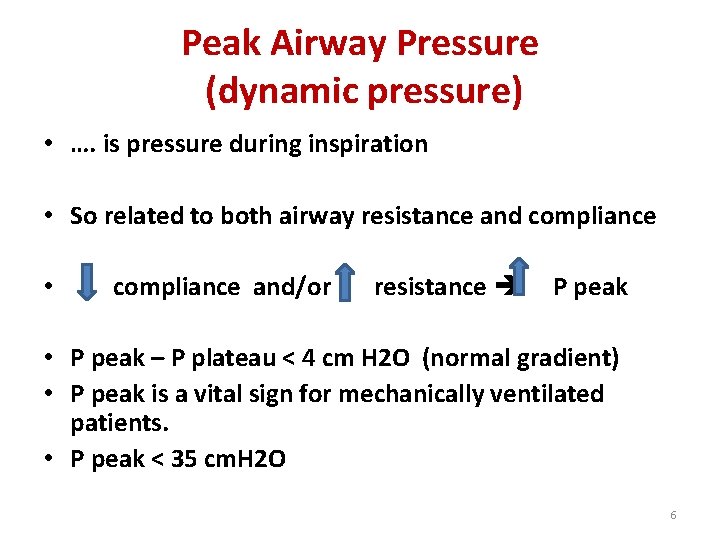
Peak Airway Pressure (dynamic pressure) • …. is pressure during inspiration • So related to both airway resistance and compliance • compliance and/or resistance P peak • P peak – P plateau < 4 cm H 2 O (normal gradient) • P peak is a vital sign for mechanically ventilated patients. • P peak < 35 cm. H 2 O 6
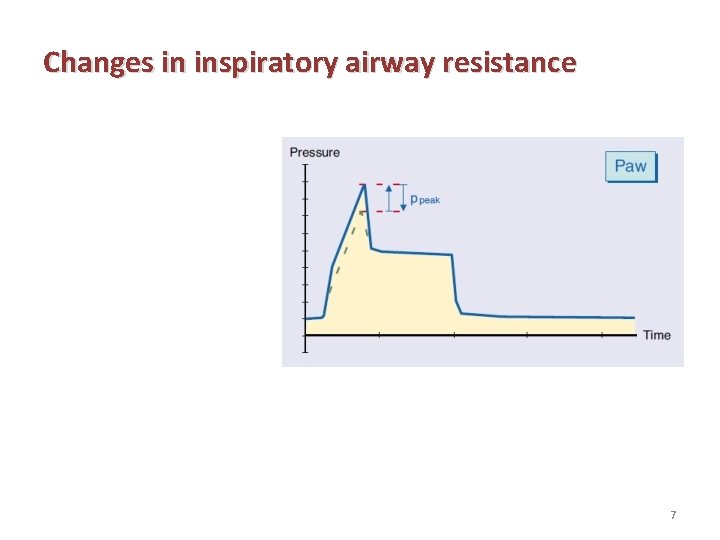
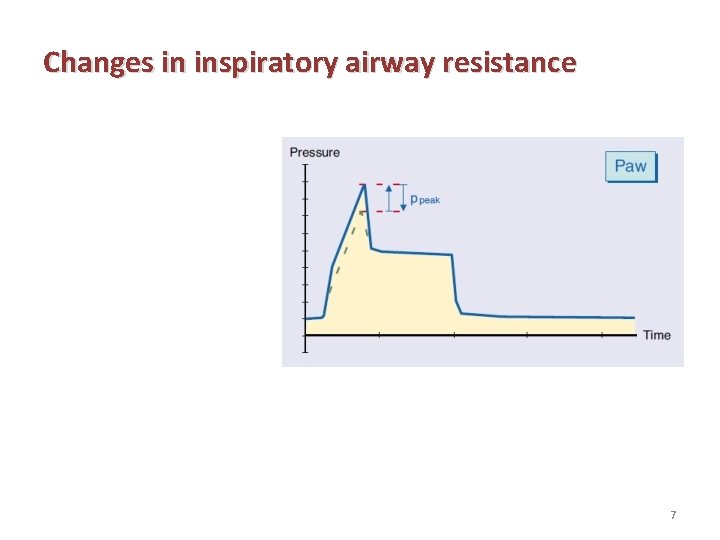
Changes in inspiratory airway resistance 7
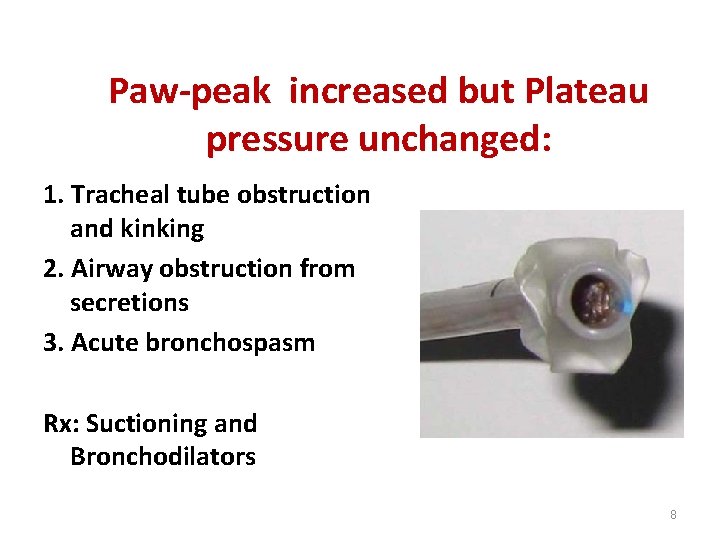
Paw-peak increased but Plateau pressure unchanged: 1. Tracheal tube obstruction and kinking 2. Airway obstruction from secretions 3. Acute bronchospasm Rx: Suctioning and Bronchodilators 8
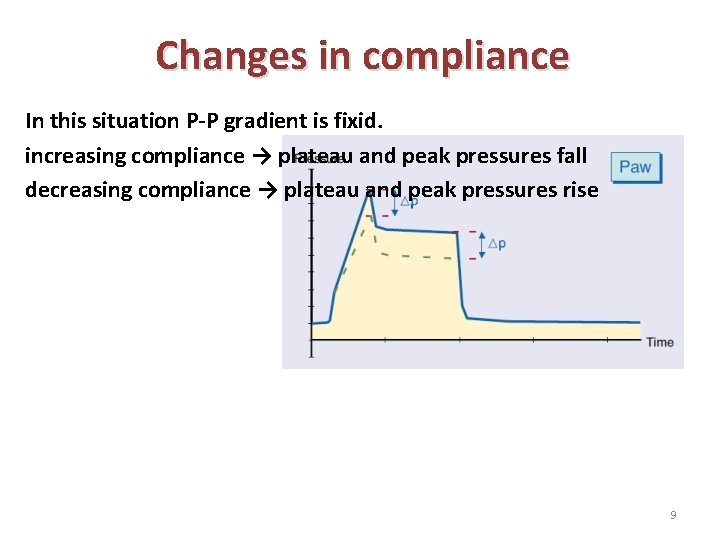
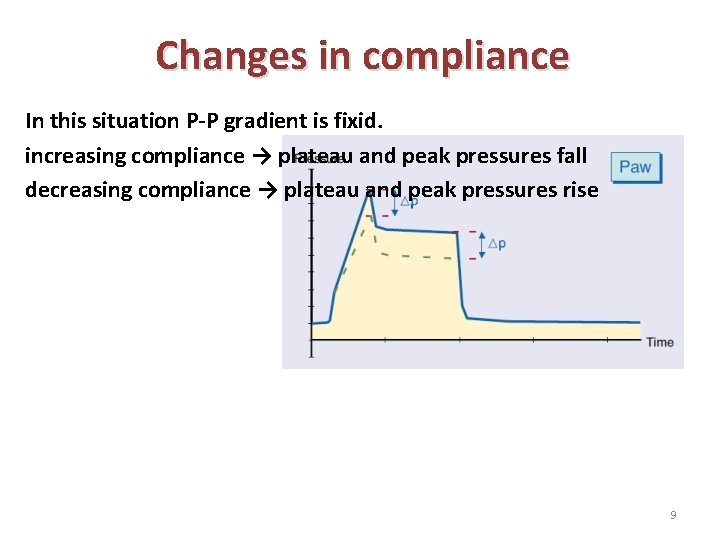
Changes in compliance In this situation P-P gradient is fixid. increasing compliance → plateau and peak pressures fall decreasing compliance → plateau and peak pressures rise 9
Paw-peak and Plateau pressure are both increased: 1. Pneumothorax 2. Lobar atelectasis 3. Acute pulmonary edema 4. Worsening pneumonia 5. ARDS 6. COPD with tachypnea and Auto-PEEP 7. Increased abdominal pressure 8. Asynchronous breathing 10
Decreased Paw-peak: 1. Inadequate gas supply, inadvertent change in setting, system air leak, Tubing disconnection, cuff leak, unintended extubation and failure of the ventilator Rx: Manual inflation, listen for leak 2. Hyperventilation: Enough negative intrathoracic pressure to pull air into lungs may drop Paw. Peak 11
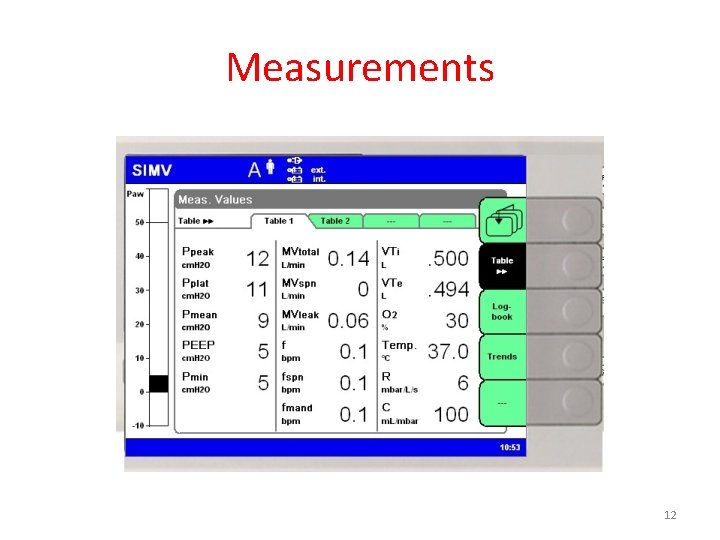
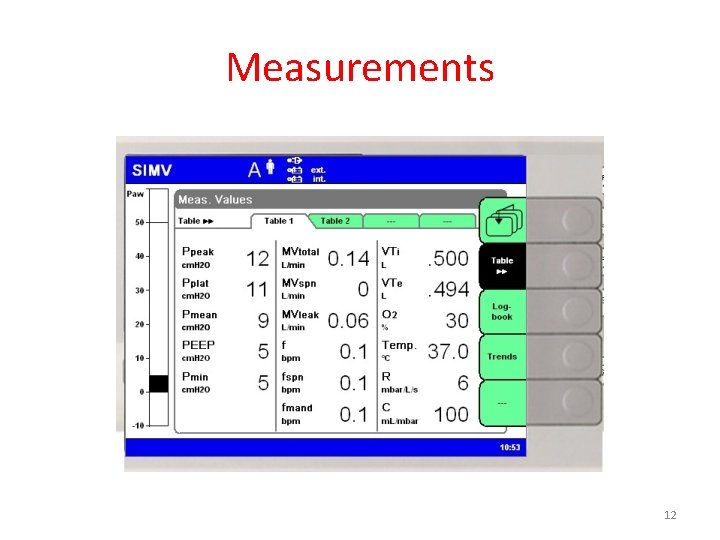
Measurements 12
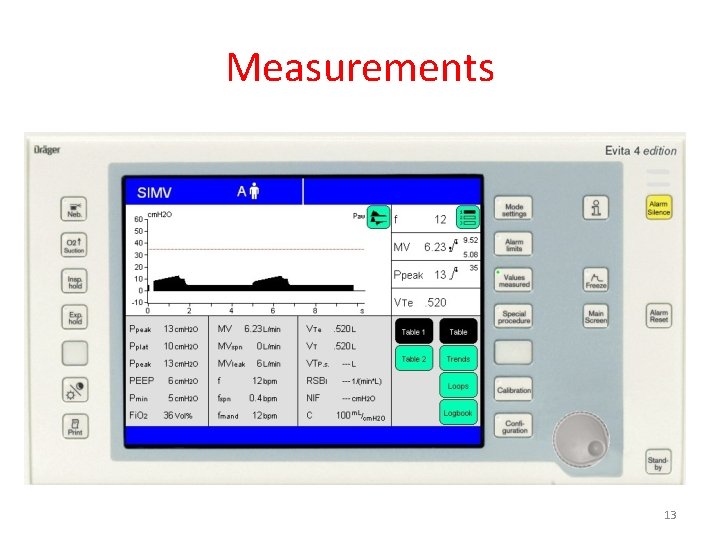
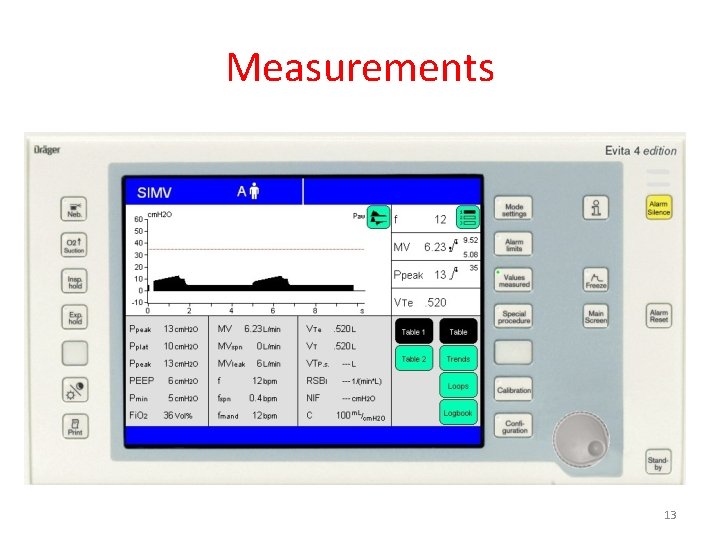
Measurements 13
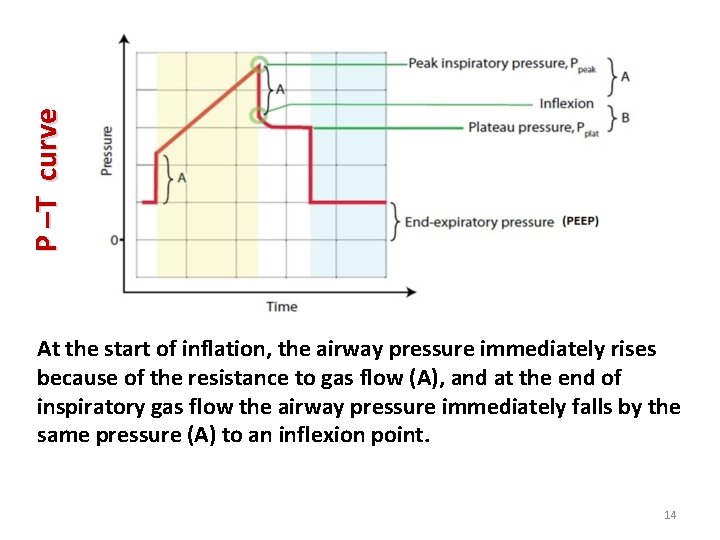
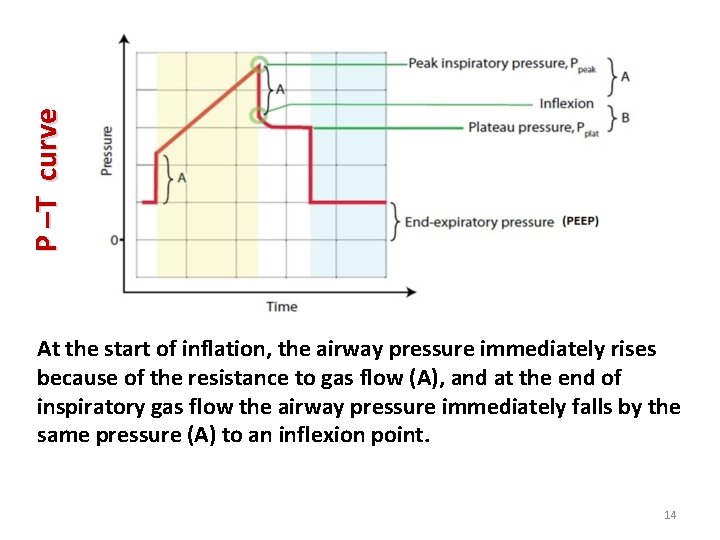
P –T curve At the start of inflation, the airway pressure immediately rises because of the resistance to gas flow (A), and at the end of inspiratory gas flow the airway pressure immediately falls by the same pressure (A) to an inflexion point. 14
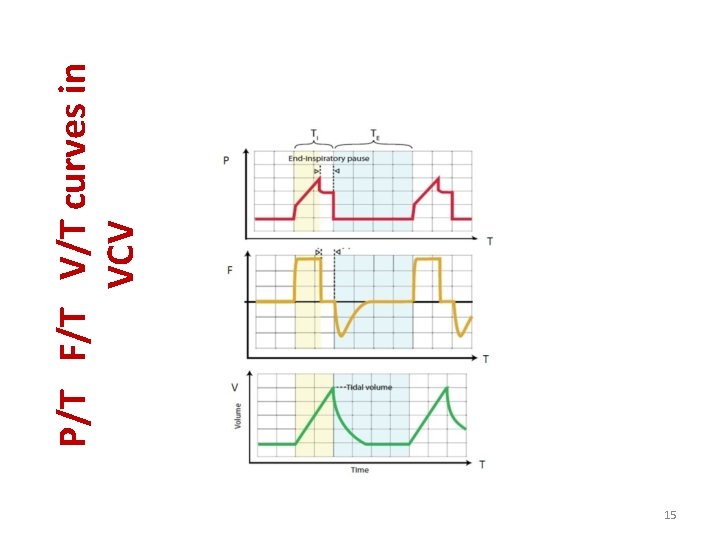
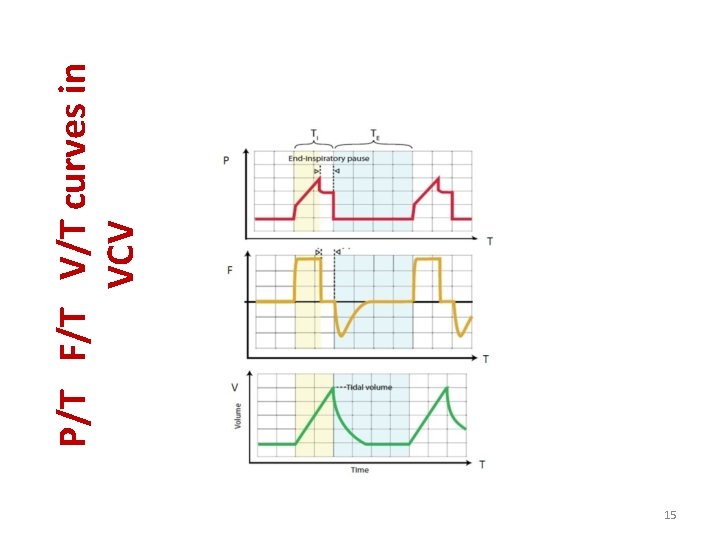
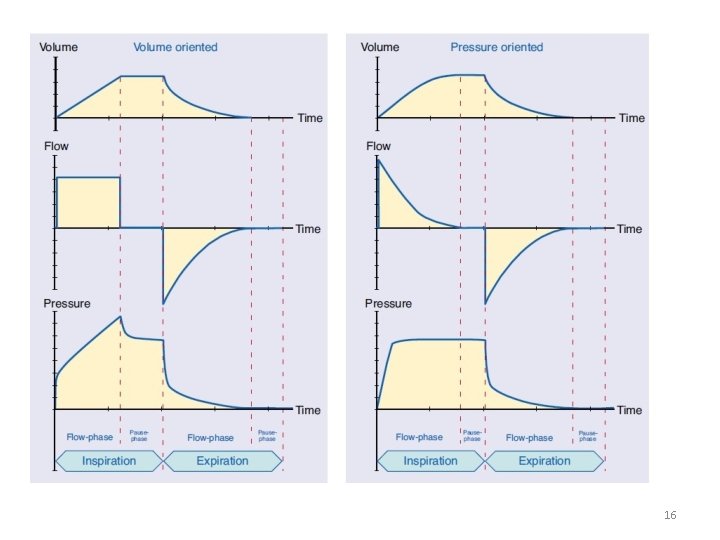
15 P/T F/T V/T curves in VCV
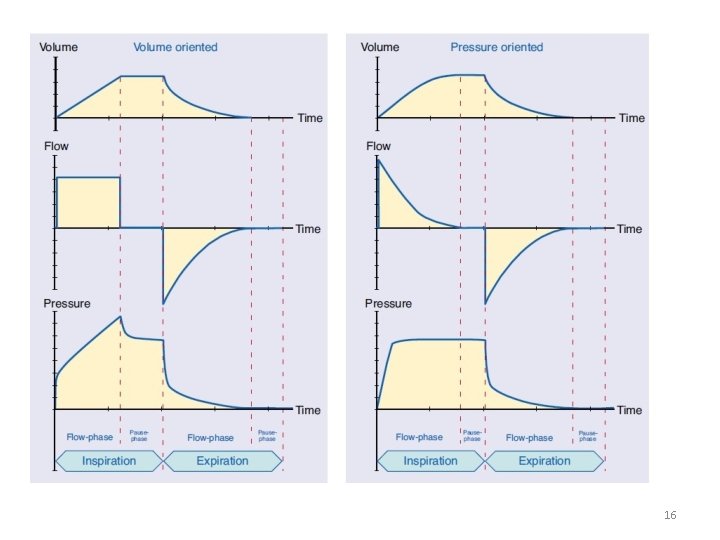
16
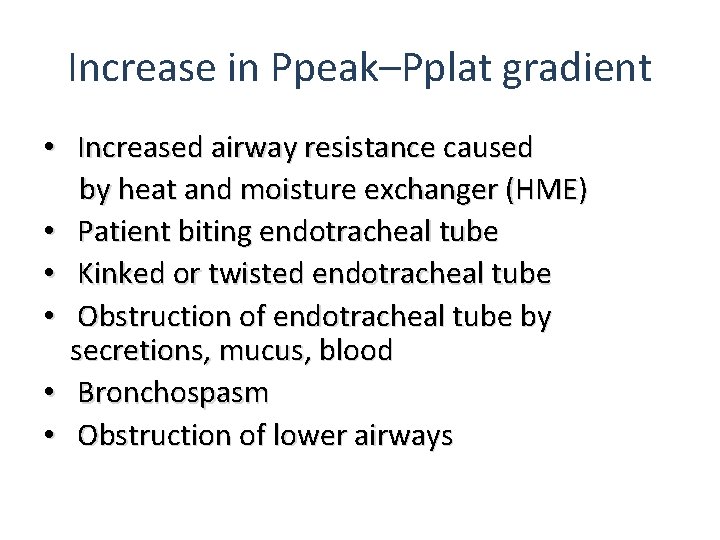
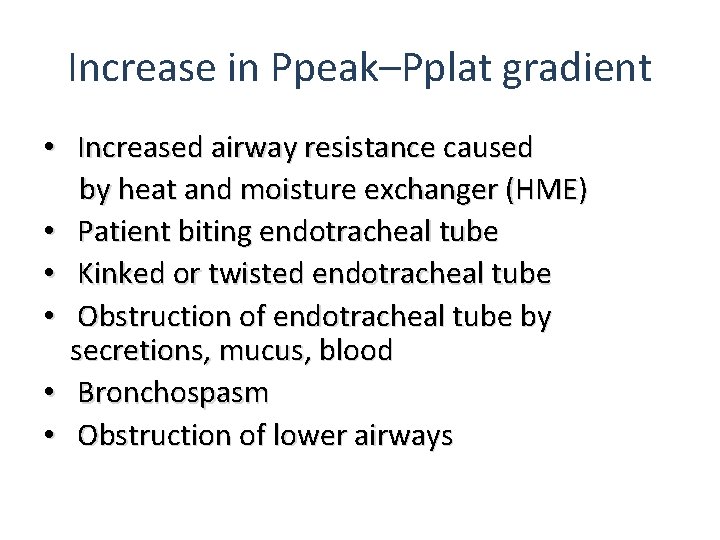
Increase in Ppeak–Pplat gradient • Increased airway resistance caused by heat and moisture exchanger (HME) • Patient biting endotracheal tube • Kinked or twisted endotracheal tube • Obstruction of endotracheal tube by secretions, mucus, blood • Bronchospasm • Obstruction of lower airways
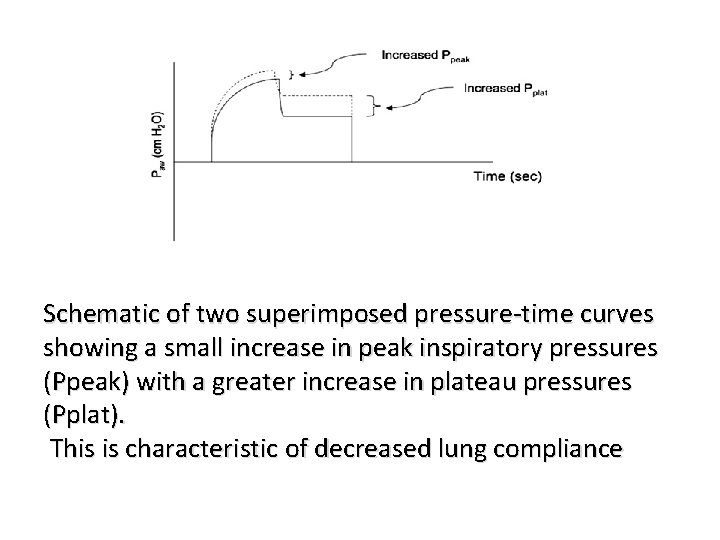
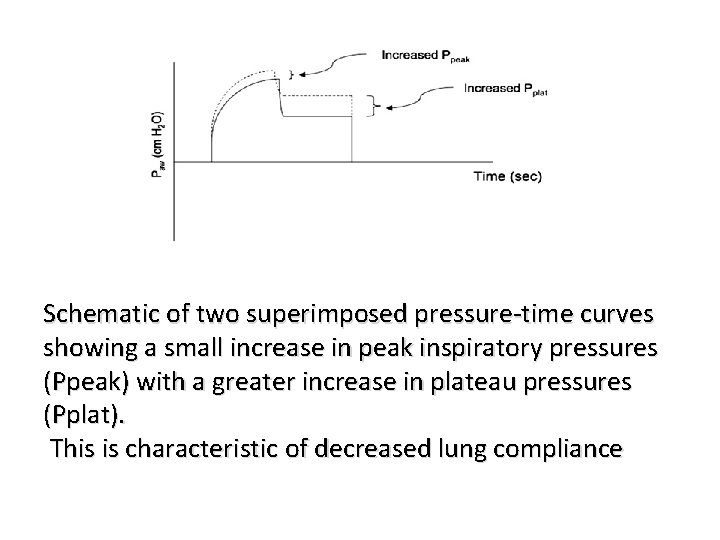
Schematic of two superimposed pressure-time curves showing a small increase in peak inspiratory pressures (Ppeak) with a greater increase in plateau pressures (Pplat). This is characteristic of decreased lung compliance
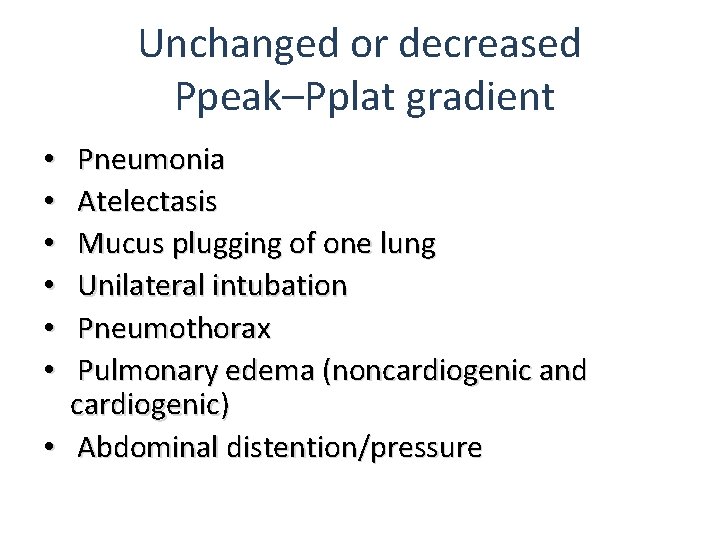
Unchanged or decreased Ppeak–Pplat gradient Pneumonia Atelectasis Mucus plugging of one lung Unilateral intubation Pneumothorax Pulmonary edema (noncardiogenic and cardiogenic) • Abdominal distention/pressure • • •
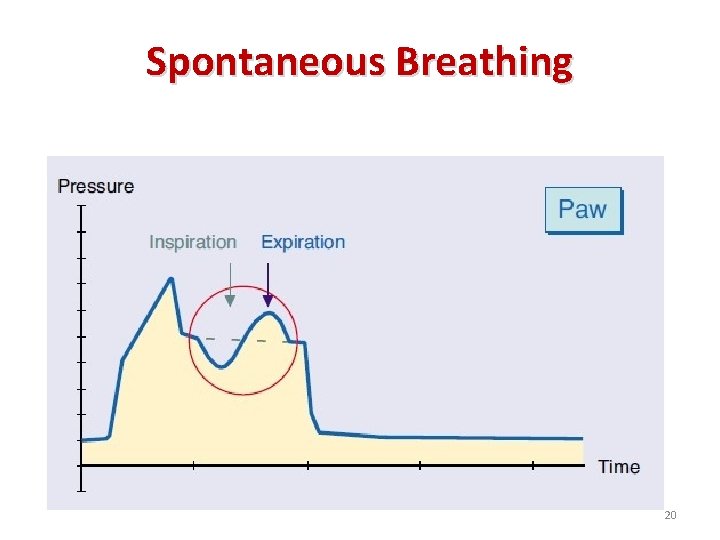
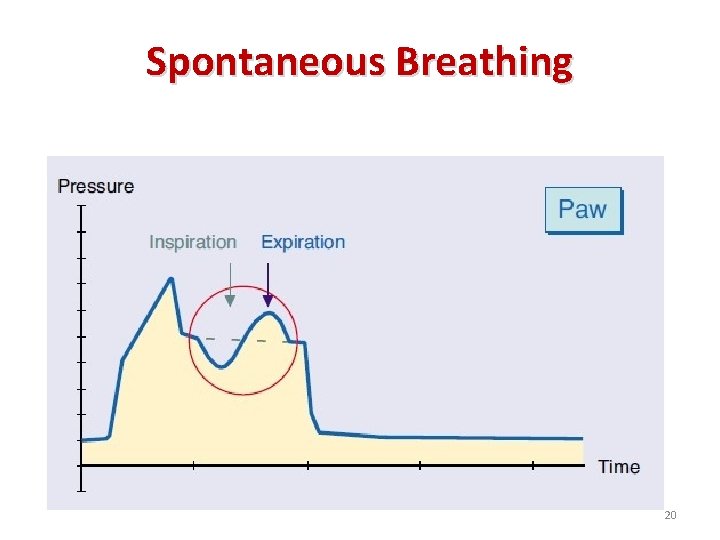
Spontaneous Breathing 20
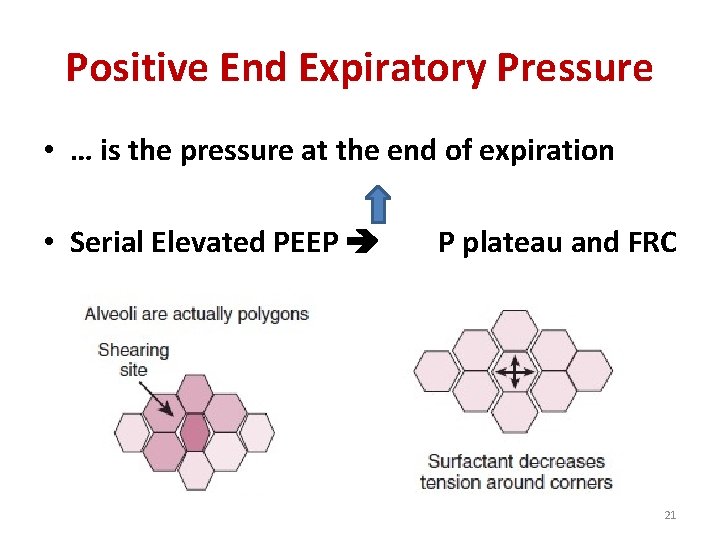
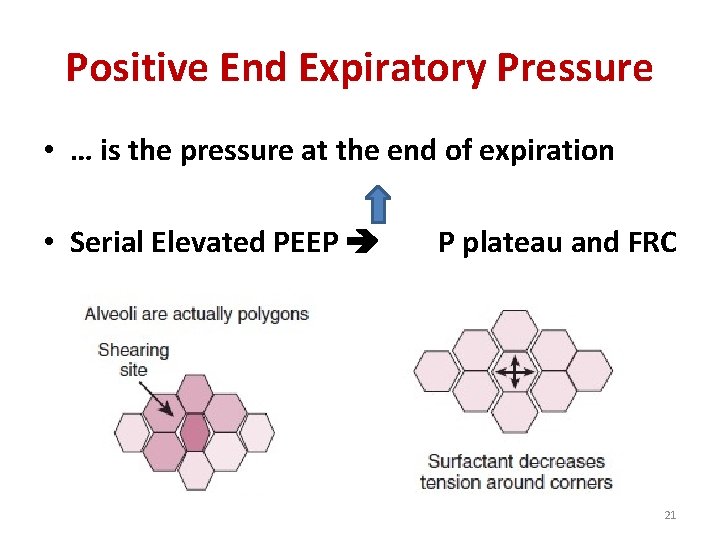
Positive End Expiratory Pressure • … is the pressure at the end of expiration • Serial Elevated PEEP P plateau and FRC 21
1 - Extrinsic PEEP (applied PEEP by MV) • • 3 - 20 cm H 2 O and be started on 5 cm H 2 O It improves the oxygenation not CO 2 removal It may be increased 3 -5 cm. H 2 O Q 10 -15 min It has some side effects: biotraumas and hemodynamic compromise • What is the optimal PEEP? 1 - increasing PEEP until a complication occurs 2 - assessing P plateau 22
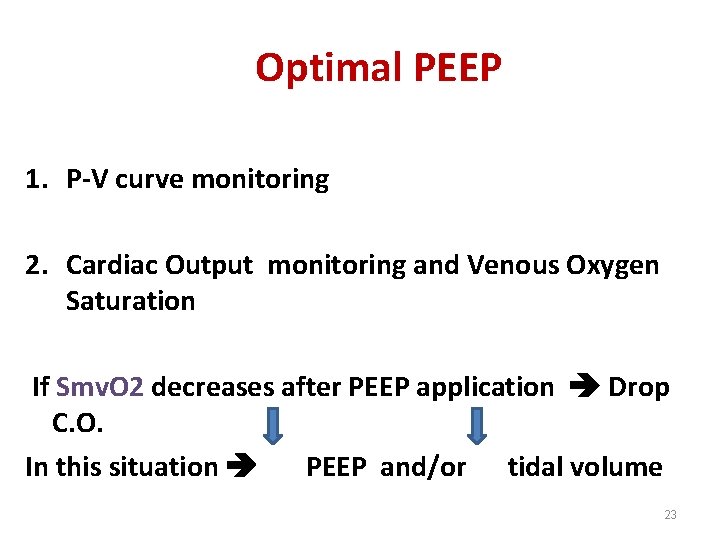
Optimal PEEP 1. P-V curve monitoring 2. Cardiac Output monitoring and Venous Oxygen Saturation If Smv. O 2 decreases after PEEP application Drop C. O. In this situation PEEP and/or tidal volume 23
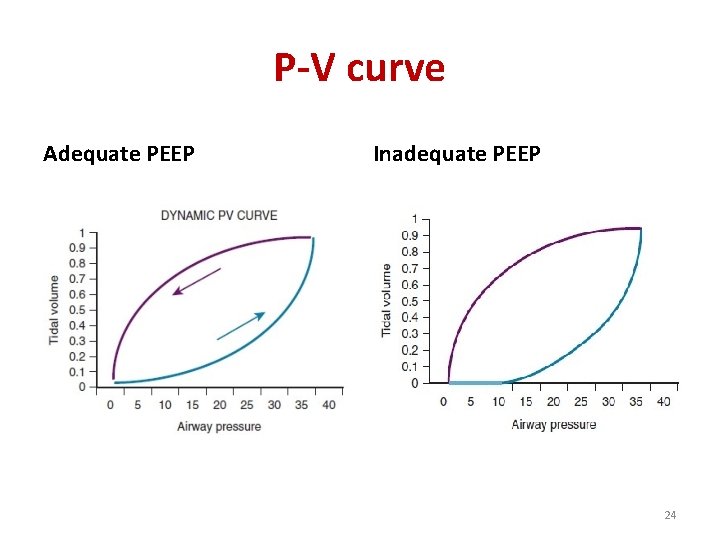
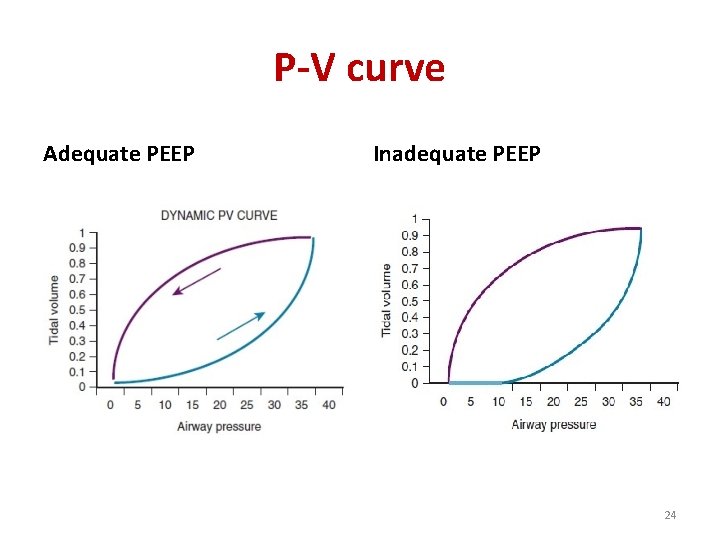
P-V curve Adequate PEEP Inadequate PEEP 24
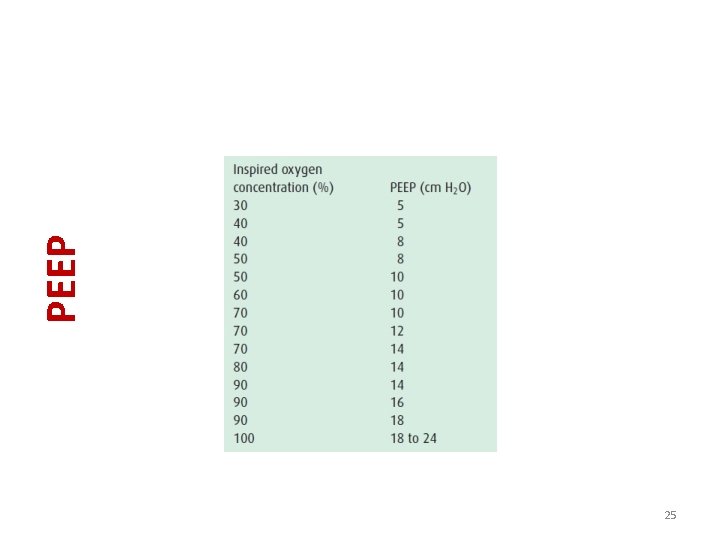
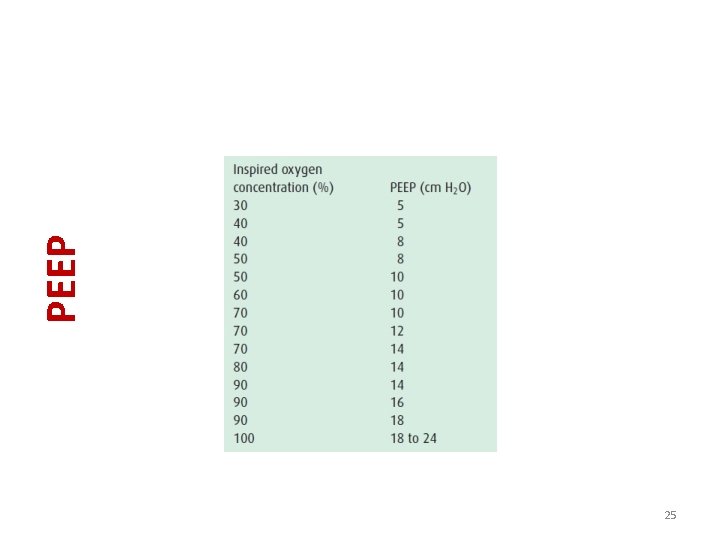
25 PEEP
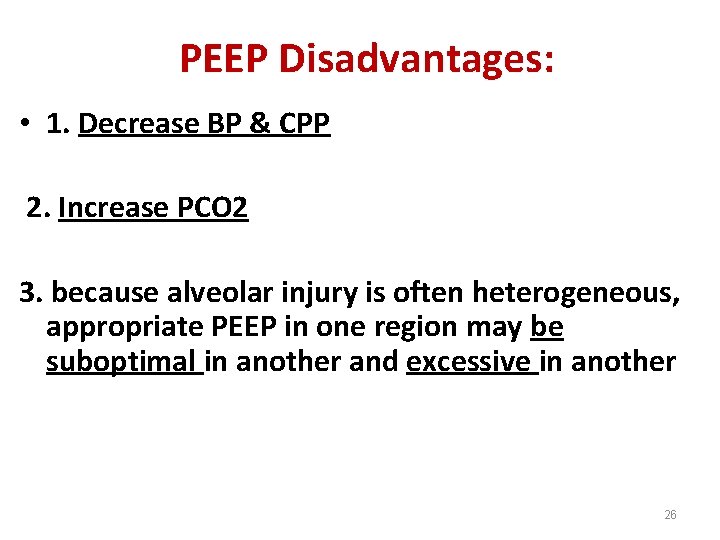
PEEP Disadvantages: • 1. Decrease BP & CPP 2. Increase PCO 2 3. because alveolar injury is often heterogeneous, appropriate PEEP in one region may be suboptimal in another and excessive in another 26
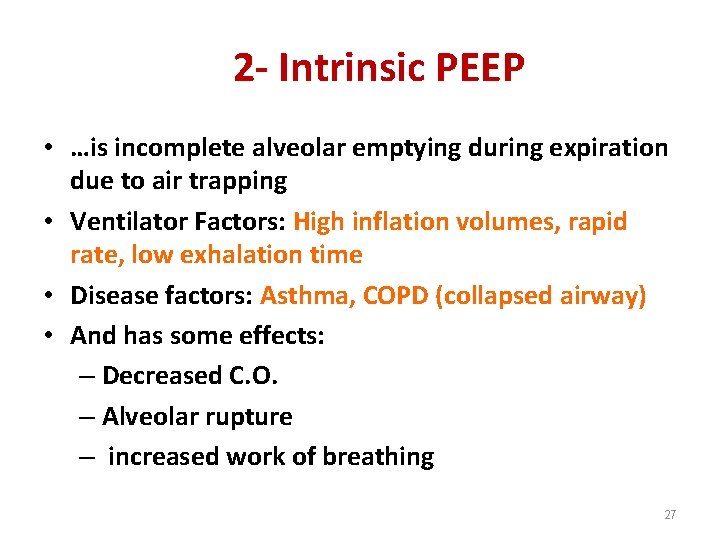
2 - Intrinsic PEEP • …is incomplete alveolar emptying during expiration due to air trapping • Ventilator Factors: High inflation volumes, rapid rate, low exhalation time • Disease factors: Asthma, COPD (collapsed airway) • And has some effects: – Decreased C. O. – Alveolar rupture – increased work of breathing 27
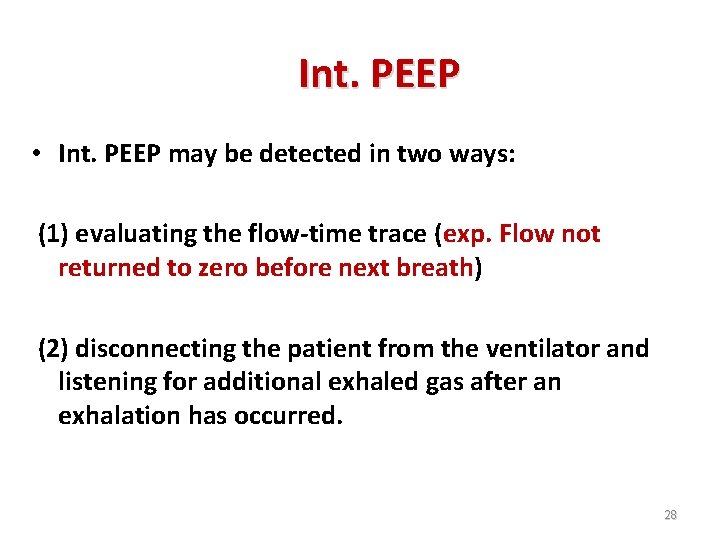
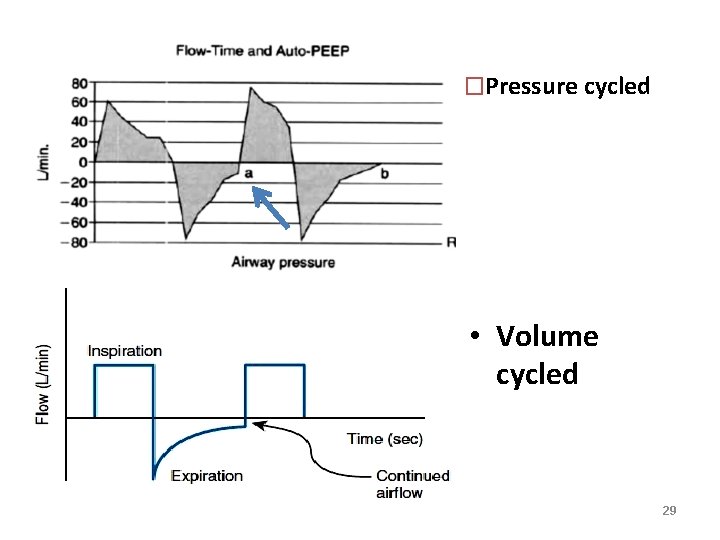
Int. PEEP • Int. PEEP may be detected in two ways: (1) evaluating the flow-time trace (exp. Flow not returned to zero before next breath) (2) disconnecting the patient from the ventilator and listening for additional exhaled gas after an exhalation has occurred. 28
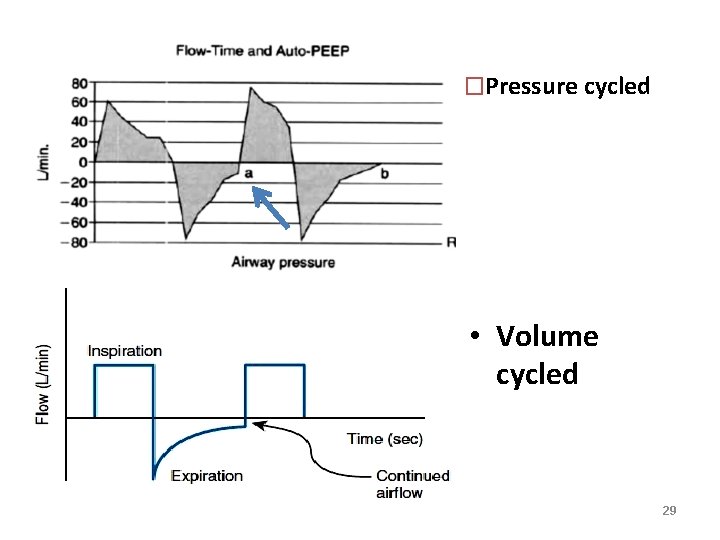
�Pressure cycled • Volume cycled 29
Indications for mechanical ventilation 30
�No absolute contraindications �Loss of airway anatomy �Loss airway protection �Respiratory and cardiac Failure �Apnea / Respiratory Arrest �Inadequate ventilation (acute vs. chronic) �Inadequate oxygenation �Eliminate work of breathing �Reduce oxygen consumption �Neurologic dysfunction �Central hypoventilation/ frequent apnea �Comatose patient, GCS < 8 �Inability to protect airway 31
Control Mechanisms 32
Control mechanisms 1. Spontaneous breathing (PSV) 2. Pressure targeted ventilation 3. Volume targeted ventilation 33
1. Spontaneous breathing: • Setting: Fi. O 2 and PEEP • Flow and f is dictated by patient 34
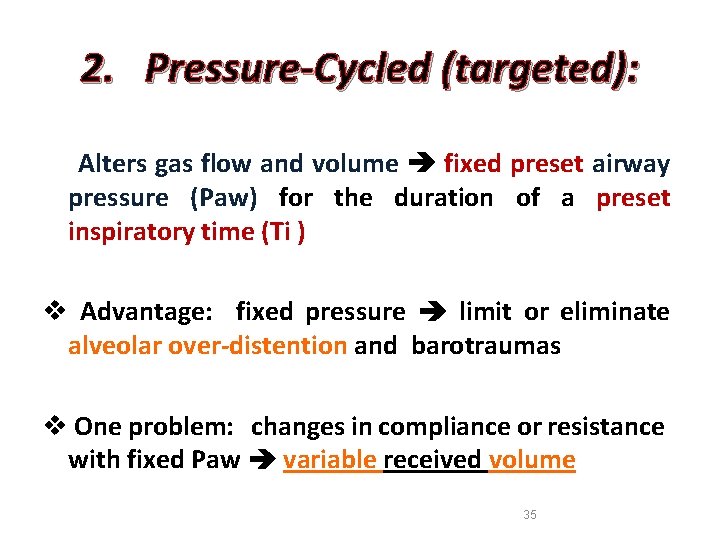
2. Pressure-Cycled (targeted): Alters gas flow and volume fixed preset airway pressure (Paw) for the duration of a preset inspiratory time (Ti ) v Advantage: fixed pressure limit or eliminate alveolar over-distention and barotraumas v One problem: changes in compliance or resistance with fixed Paw variable received volume 35
3. Volume/ Flow-Cycled (targeted) § Deliver a preset volume of gas ( VT) Paw is variable v. Advantage: delivery a constant VT changes in compliance or resistance with fixed volume changes airway pressure 36
• There are no clinical outcome studies showing benefit of one breath-targeting strategy over the other. • Pressure-targeting provide a variable flow tends to synchronize better with patient effort. 37
Modes 38
1. Controlled Mechanical Ventilation /Assist Control (CMV/AC) 2. Intermittent Mechanical Ventilation (IMV)/Synchronized IMV (SIMV). 3. Continuous Positive Airway Pressure (CPAP) /pressure support ventilation (PSV) 39

1. Controlled Mechanical Ventilation (CMV) Assist Control (AC) 40
v. Control Mode Ventilation v. Continuous mandatory ventilation v. Continuous mechanical ventilation v. Controlled mandatory ventilation v Intermittent Positive Pressure Ventilation (Dräger) � …is a full support mode (machine breaths) �All breaths are supported regardless of initiation of breathing and can be set to VCV and PCV �Used for: apneic patients, respiratory muscle weakness and LV dysfunction 41
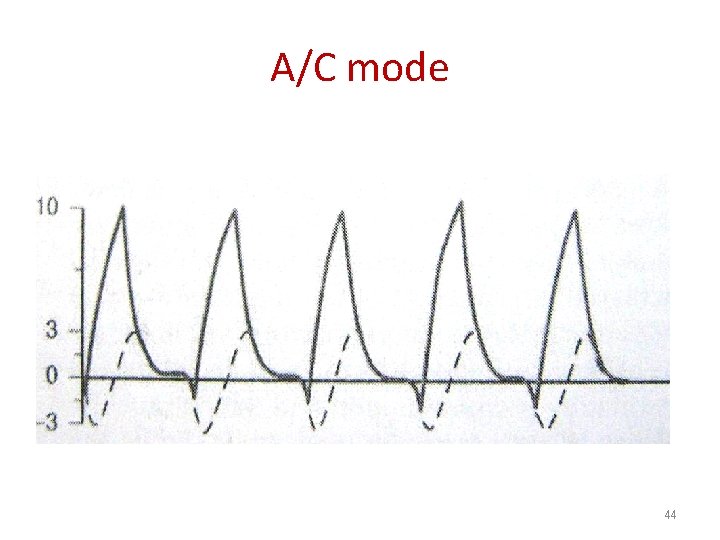
(CMV/AC ) �Sensitivity pressure 0. 5 to 2 cm H 2 O (1 -3 cm H 2 O Tintinalli) �The higher sensitivity the greater work of breathing �After spontaneous breath the ventilator`s timer resets from this time 42
(CMV /AC) �CMV preferred and most commonly used initial mode for acute phase of respiratory failure in ED � but CMV : 1. Poor toleration in awake patients 2. Worsening of volume retention in COPD / asthma 43
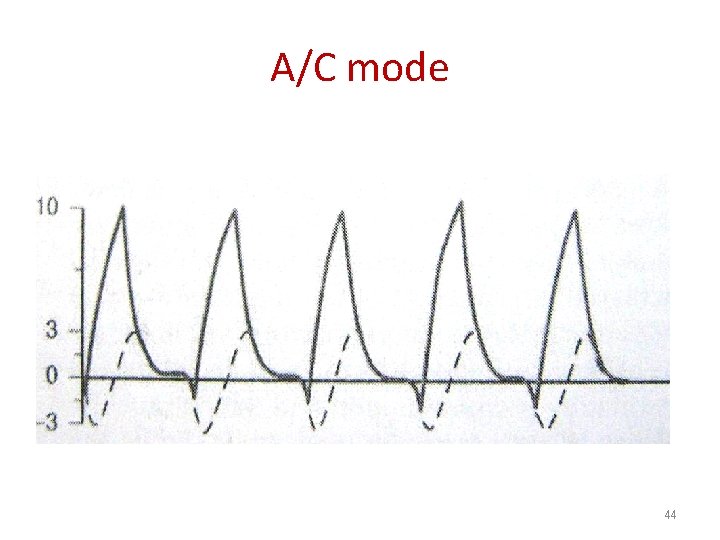
A/C mode 44
2. Intermittent Mechanical Ventilation (IMV) Synchronized IMV (SIMV) 45
v. SIMV (Dräger, Hamilton) v. SIMV (VC) + PS (Maquet) v VCV-SIMV (Puritan-Bennett, Respironics) v. Volume SIMV (Viasys) v. Intermittent demand ventilation �IMV combination of spontaneous vent. and AC �IMV is a partial support mode �This ventilator mode provides breaths at a preset rate (machine breath) similar to the AC mode �Can be set to PCV and VCV 46
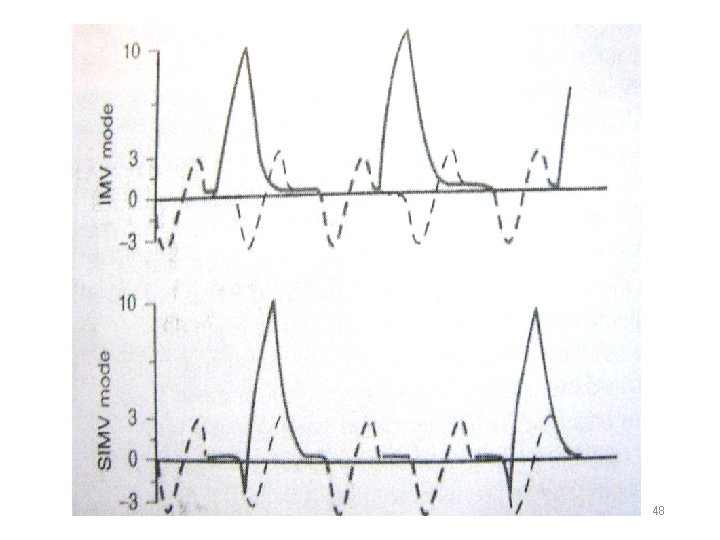
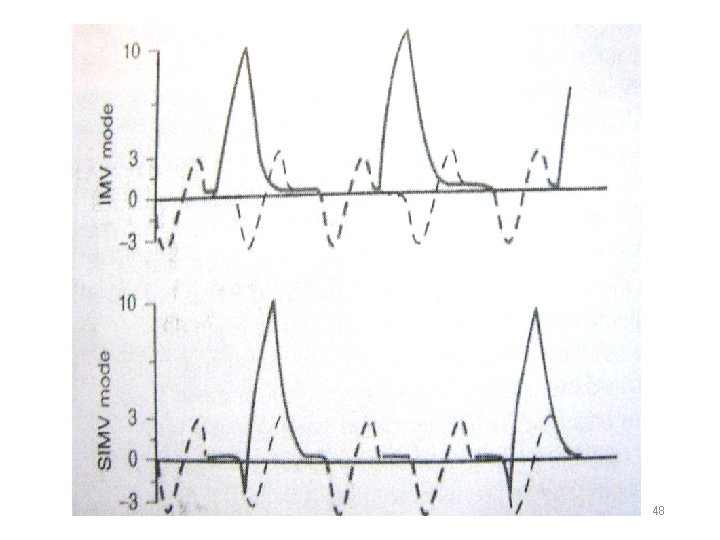
(IMV / SIMV ) v But in spontaneous breath only receive a spontaneous VT with no support from the ventilator and has a high work of breathing v The synchronized version of IMV spontaneous and machine breaths coordination v SIMV: 1. To prevent excess VT delivered (stacking) decreased hyperinflation, barotrauma 2. During exhalation from a spontaneous breath exhalation compromised 47
48

49
3. Continuous Positive Airway Pressure (CPAP) pressure support ventilation (PSV) 50
v. Assisted Spontaneous Breathing(Dräger) v. Spontaneous mode(Hamilton, Puritan-Bennett) v. Pressure support (Maquet) v. CPAP (Respironic) v. Pressure Support Ventilation (Viasys) vcontinuous positive-pressure breathing (CPPB ) v. EPAP �Is a partial support mode �Breathing control by the patient (spontaneous mode ) , and peak Paw control by machine (pressure targeted) 51
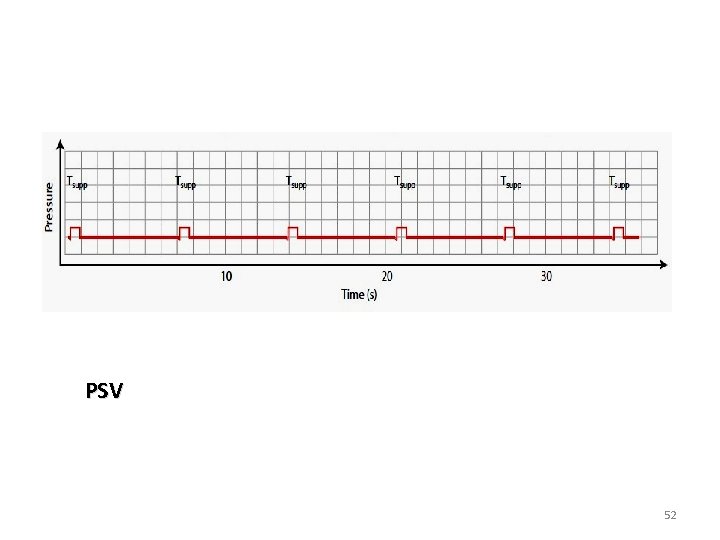
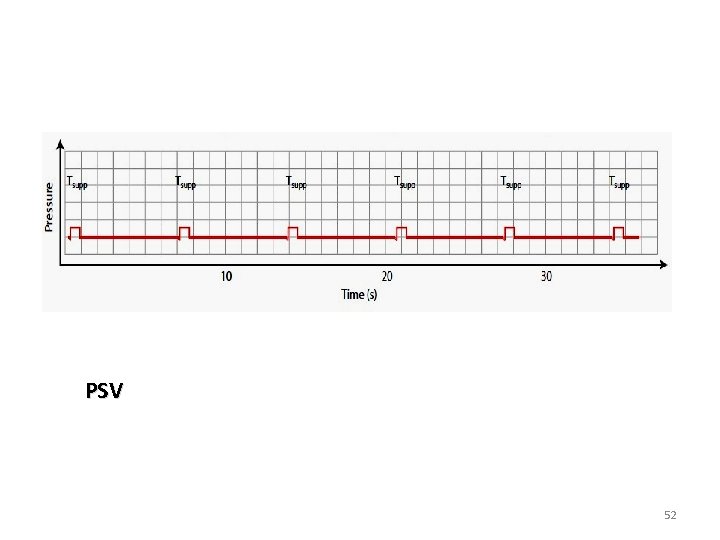
PSV 52
PSV / ASB / CPAP § Help the patient overcome the resistance of the circuit decreased work of breathing § This is not useful in apnea 53
CPAP / PSV / ASB �CPAP the least amount of support and used with IPPV or NIPPV �Most commonly used in (COPD) , CHF and obstructive sleep apnea with NIPPV ( via a tightfitting nasal or full face-mask) 54
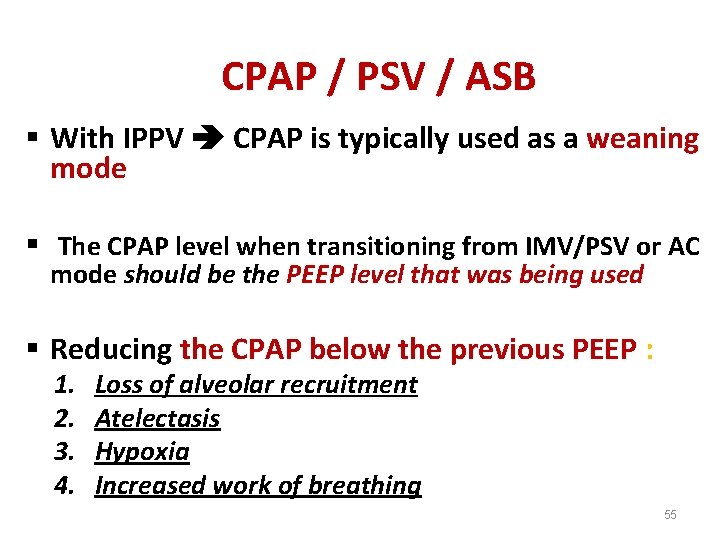
CPAP / PSV / ASB § With IPPV CPAP is typically used as a weaning mode § The CPAP level when transitioning from IMV/PSV or AC mode should be the PEEP level that was being used § Reducing the CPAP below the previous PEEP : 1. 2. 3. 4. Loss of alveolar recruitment Atelectasis Hypoxia Increased work of breathing 55
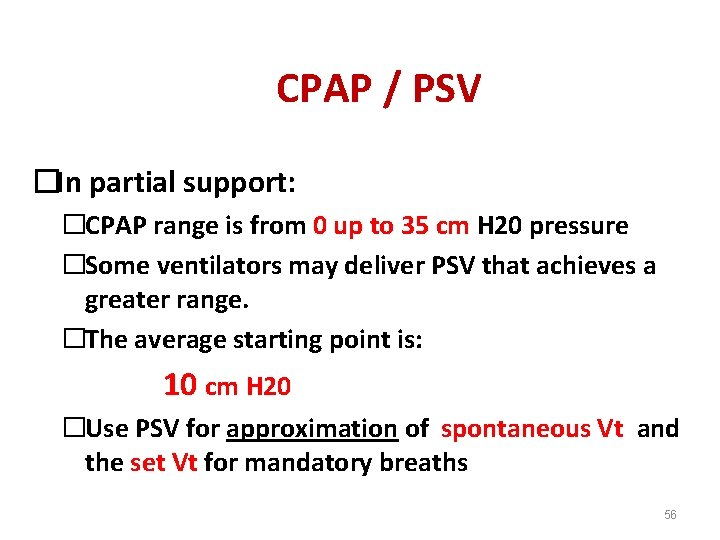
CPAP / PSV �In partial support: �CPAP range is from 0 up to 35 cm H 20 pressure �Some ventilators may deliver PSV that achieves a greater range. �The average starting point is: 10 cm H 20 �Use PSV for approximation of spontaneous Vt and the set Vt for mandatory breaths 56
(CPAP) benefits �Eliminate the work of breathing �To aid in weaning from IMV-base ventilation and is frequently part of a transition strategy from IMV to CPAP 57
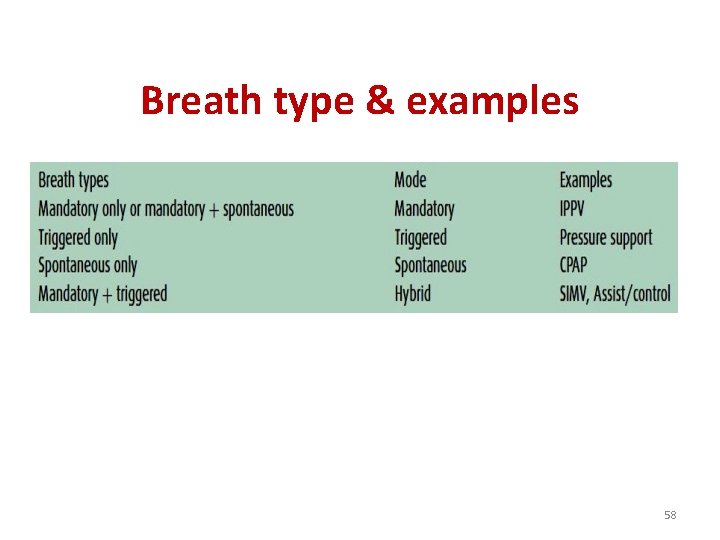
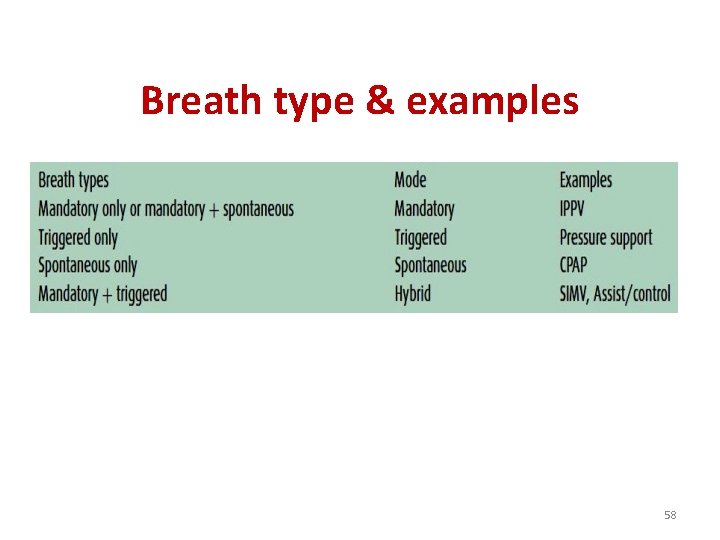
Breath type & examples 58
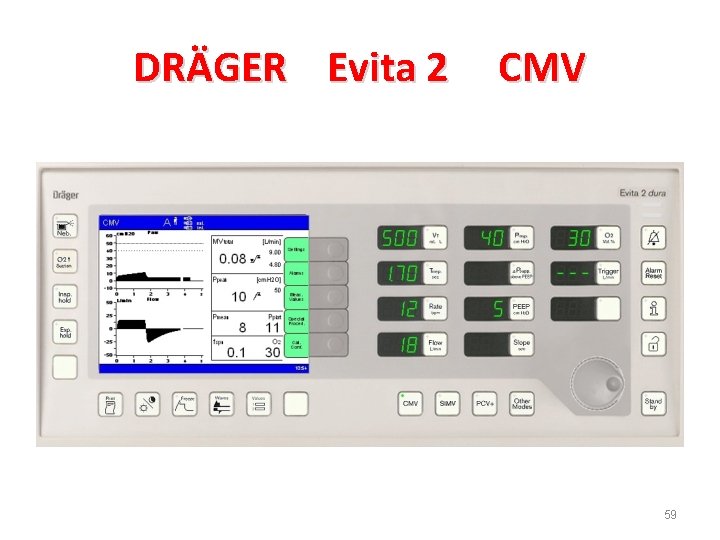
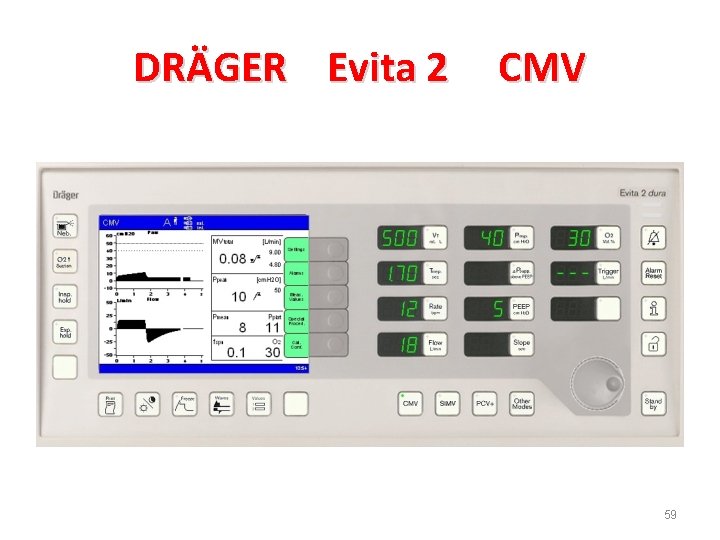
DRÄGER Evita 2 CMV 59
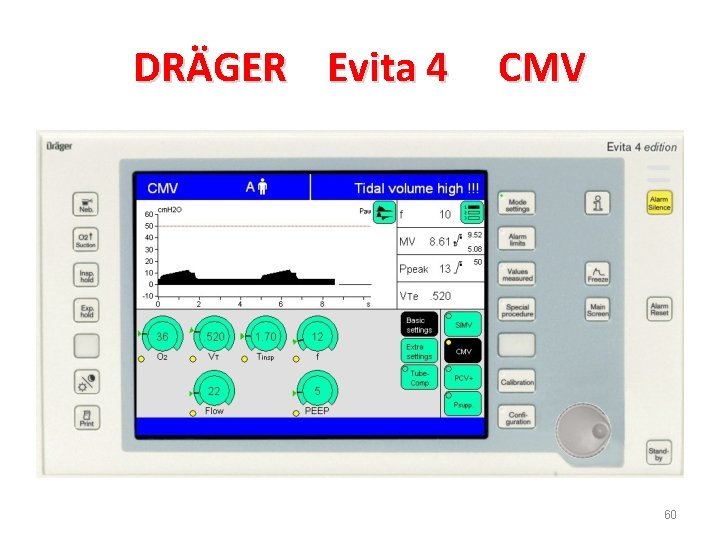
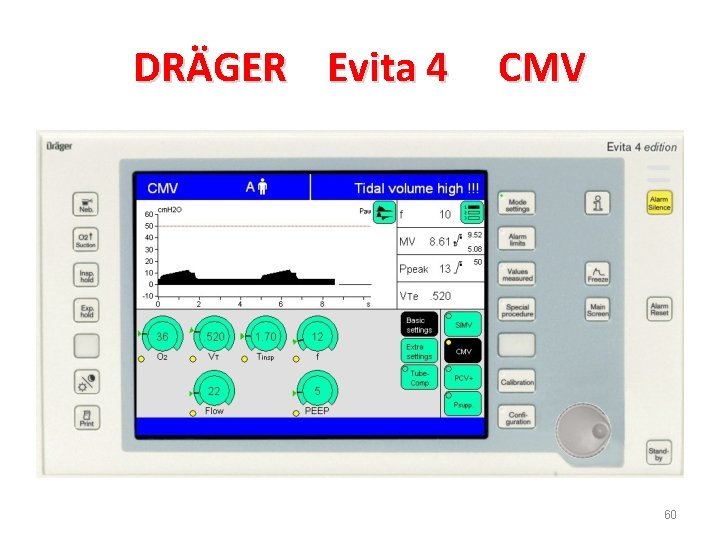
DRÄGER Evita 4 CMV 60

DRÄGER Evita 2 SIMV 61
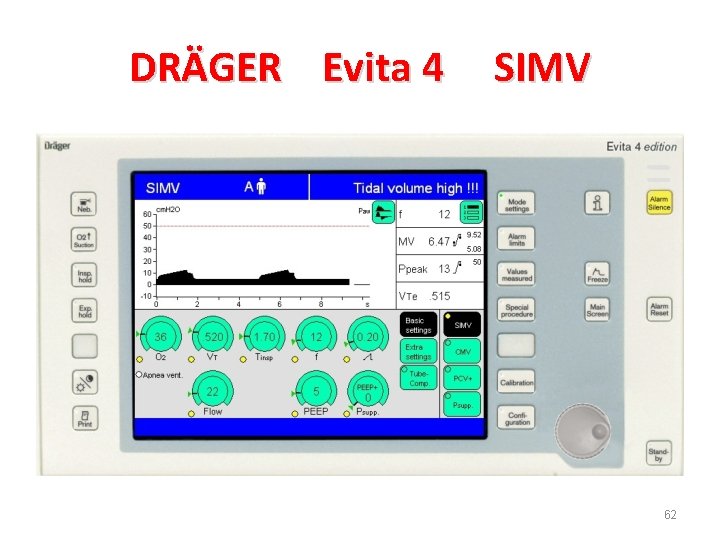
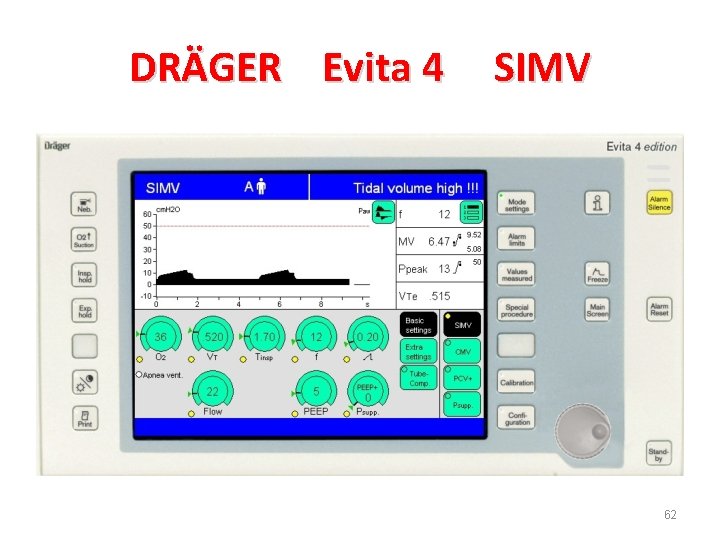
DRÄGER Evita 4 SIMV 62

DRÄGER Evita 2 CPAP 63
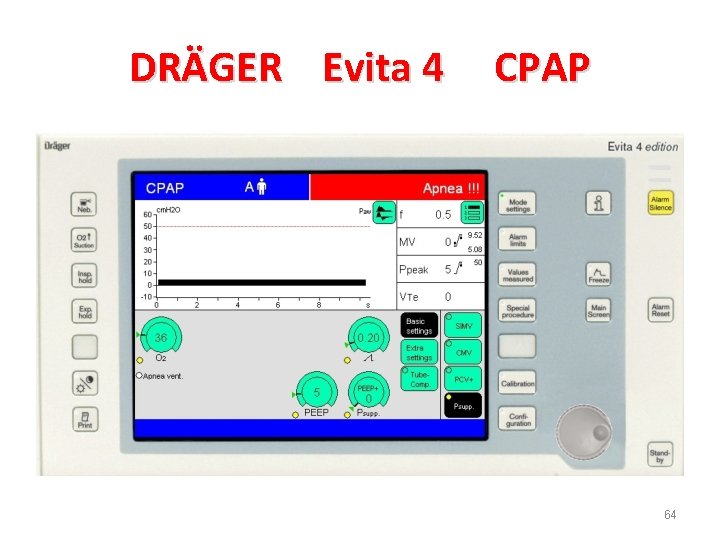
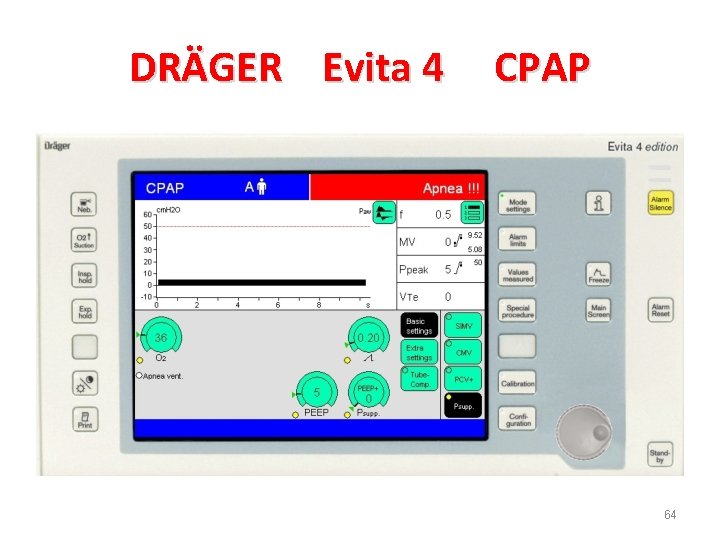
DRÄGER Evita 4 CPAP 64

DRÄGER Evita 2 PCV 65

DRÄGER Evita 4 PCV 66
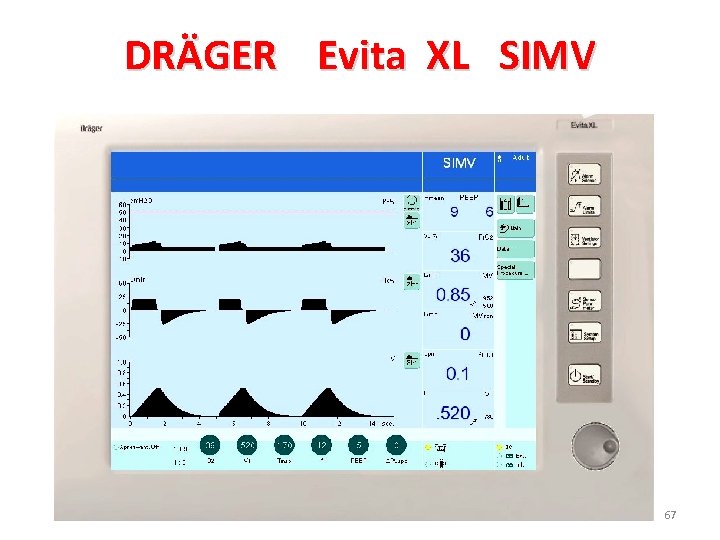
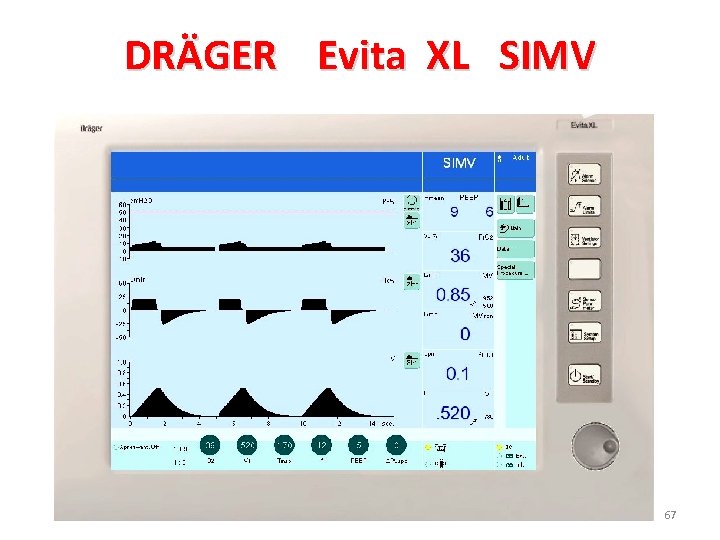
DRÄGER Evita XL SIMV 67
Adjunct Ventilator Settings and curves 68
1. Oxygen �The fraction of inspired O 2 (Fi. O 2) is set in a range from 21% (room air; not generally indicated) to 100% �In the ED it is common to start at 100% Fi. O 2 to ensure adequate oxygenation and titrate the Fi. O 2 down to nontoxic levels (Fi. O 2< 60%) following the Sa. O 2 via the pulse oximeter (Sa. O 2> 90%) during first 72 h. �some practitioners recommend using 95% O 2 as the upper limit of Fi. O 2 69
2. Inspiration : Expiration (I: E) Ratio • The normal I: E ratio in a spontaneously breathing, non intubated patient is 1: 4 • Intubated patients commonly achieve I: E ratios of 1: 2 70
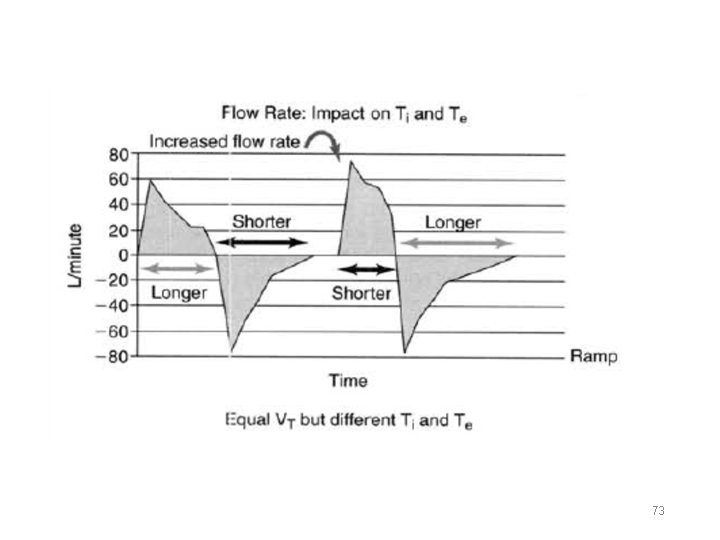
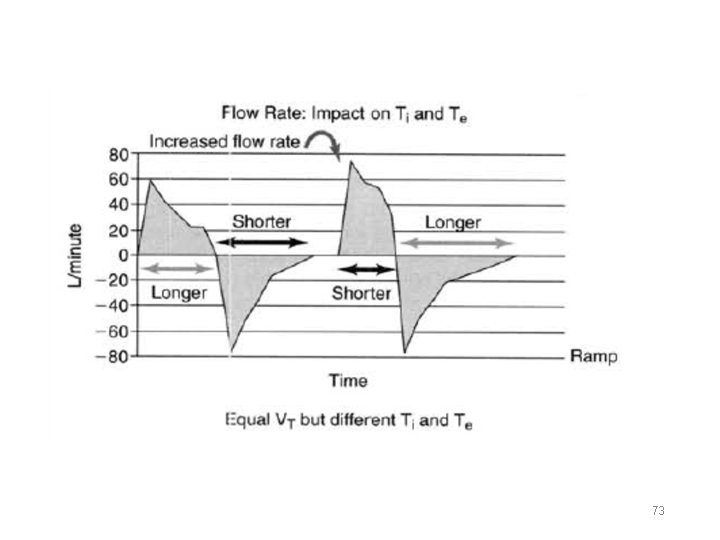
3. Flow rate (Q ) • This is the rate of gas delivery (L/min). • The range of flows that can be achieved by current ventilation is from 10 to 160 L/min. • Common flow settings are from 40 to 75 L/min. • The higher the flow rate, the faster the ventilator will reach its set volume or pressure. • Start at Q=60 L/ min • A faster flow rate decreased ins. time • A slower flow rate decreased exp. time 71
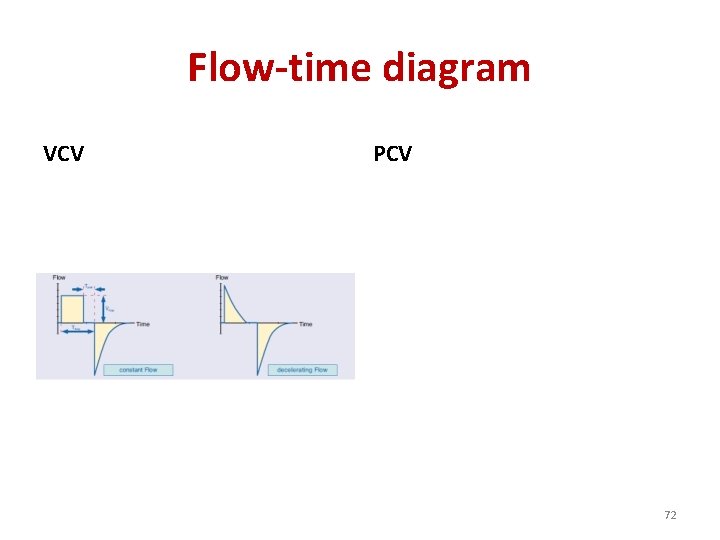
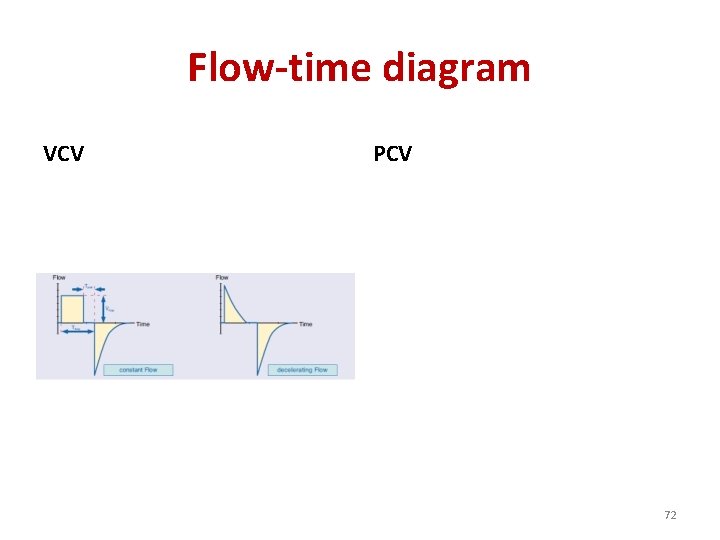
Flow-time diagram VCV PCV 72
73
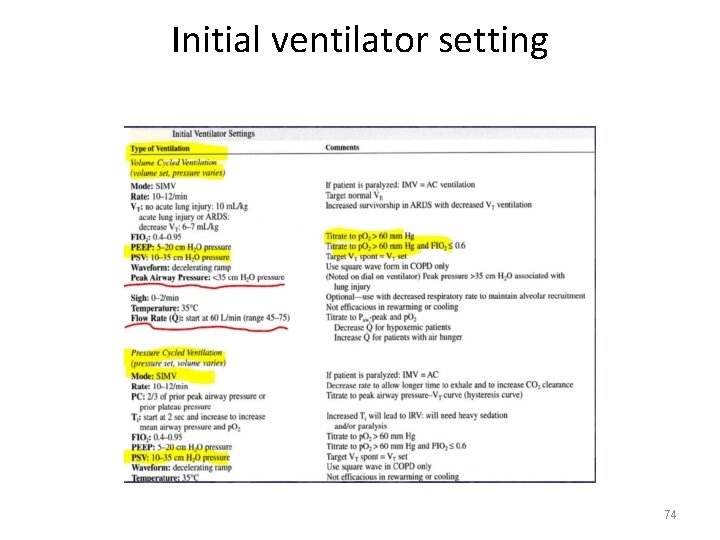
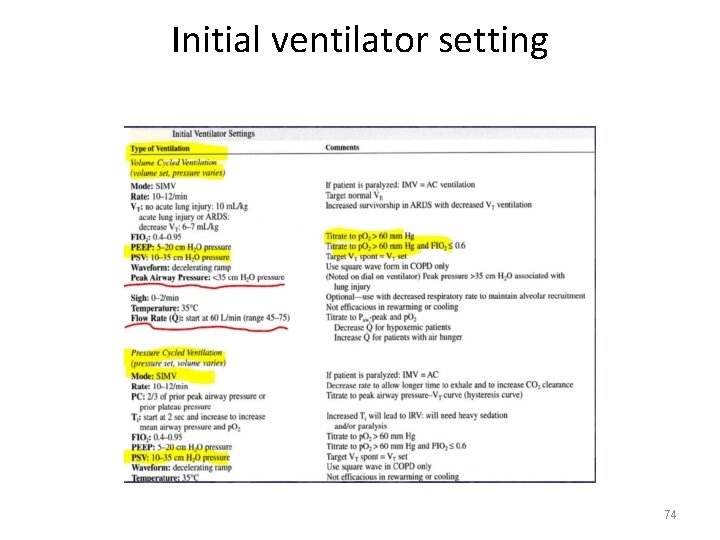
Initial ventilator setting 74
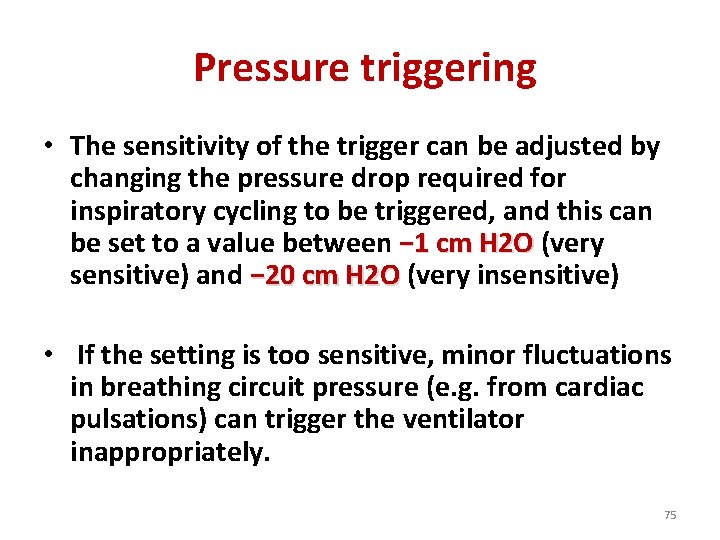
Pressure triggering • The sensitivity of the trigger can be adjusted by changing the pressure drop required for inspiratory cycling to be triggered, and this can be set to a value between − 1 cm H 2 O (very − 1 cm H 2 O sensitive) and − 20 cm H 2 O (very insensitive) − 20 cm H 2 O • If the setting is too sensitive, minor fluctuations in breathing circuit pressure (e. g. from cardiac pulsations) can trigger the ventilator inappropriately. 75
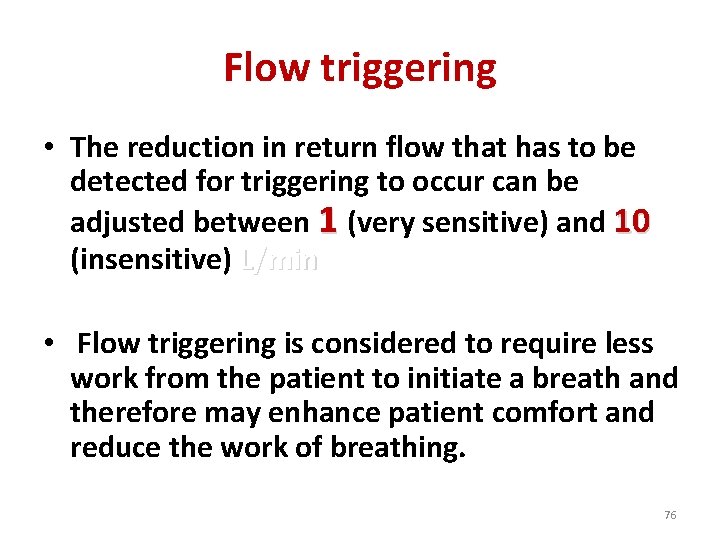
Flow triggering • The reduction in return flow that has to be detected for triggering to occur can be adjusted between 1 (very sensitive) and 10 (insensitive) L/min • Flow triggering is considered to require less work from the patient to initiate a breath and therefore may enhance patient comfort and reduce the work of breathing. 76
Advanced modes • BREATH TO BREATH – Pressure-regulated volume control (PRVC) – Auto flow – Volume control plus (VC+) – Adaptive pressure ventilation (APV) – Variable-pressure control (VPC) • WITHIN A BREATH – Volume-assured pressure support ventilation (VAPSV) – Pressure augmentation 77
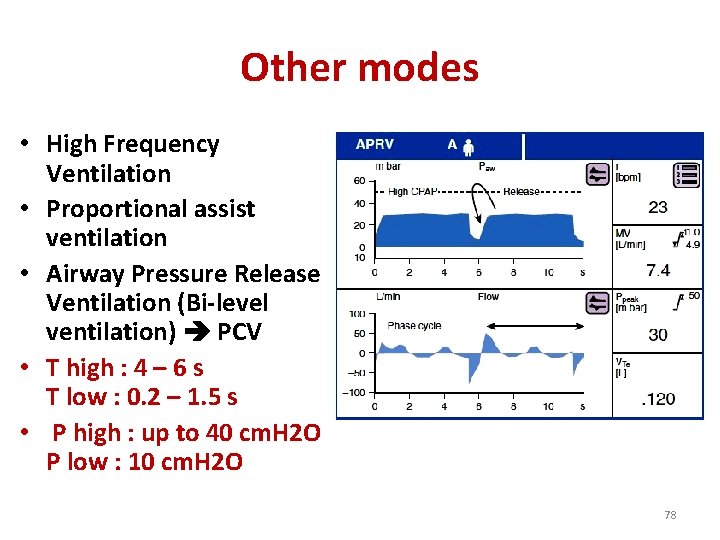
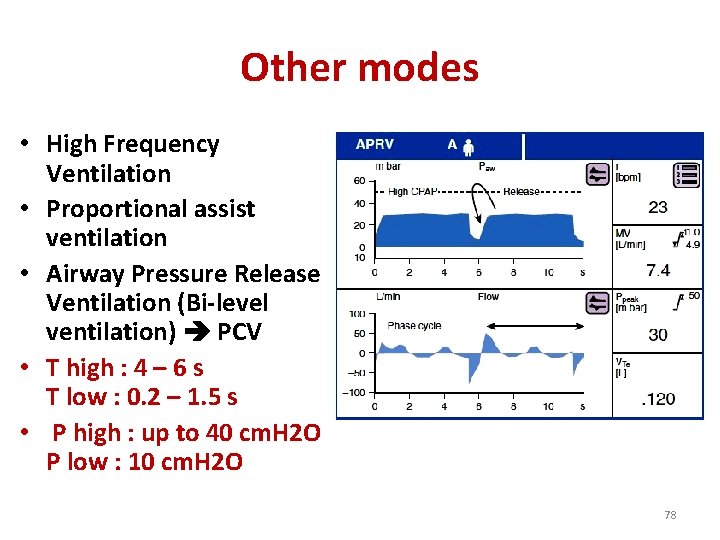
Other modes • High Frequency Ventilation • Proportional assist ventilation • Airway Pressure Release Ventilation (Bi-level ventilation) PCV • T high : 4 – 6 s T low : 0. 2 – 1. 5 s • P high : up to 40 cm. H 2 O P low : 10 cm. H 2 O 78
NON INVASIVE VENTILATION TUMS 79
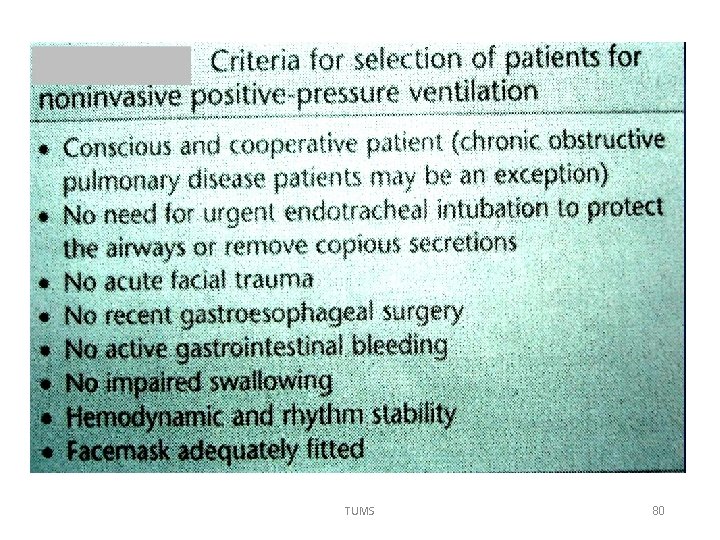
TUMS 80
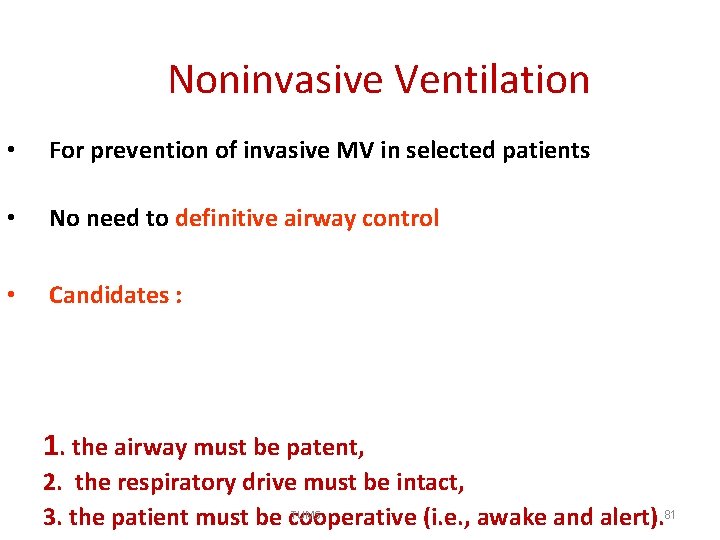
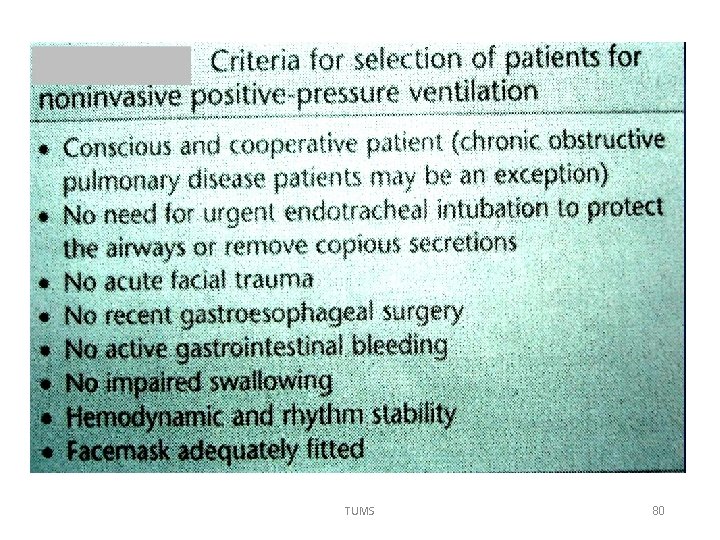
Noninvasive Ventilation • For prevention of invasive MV in selected patients • No need to definitive airway control • Candidates : COPD, CHF, Asthma, hypoxia, DNR patients and Immunocompromised patients 1. the airway must be patent, 2. the respiratory drive must be intact, TUMS 81 3. the patient must be cooperative (i. e. , awake and alert).
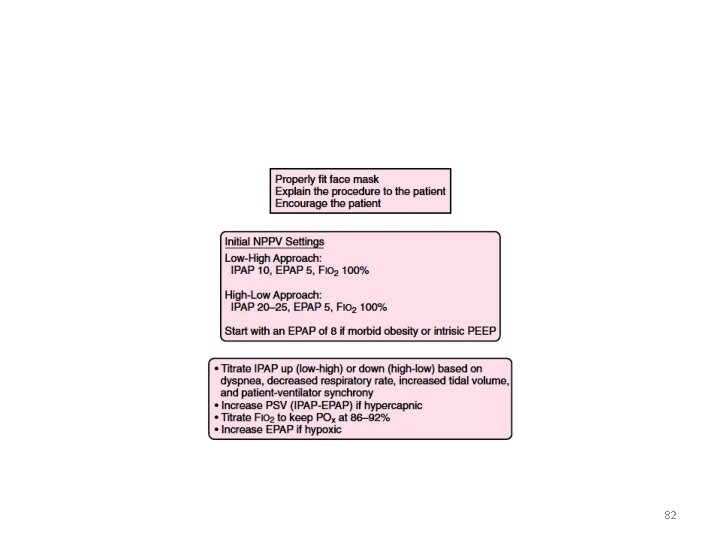
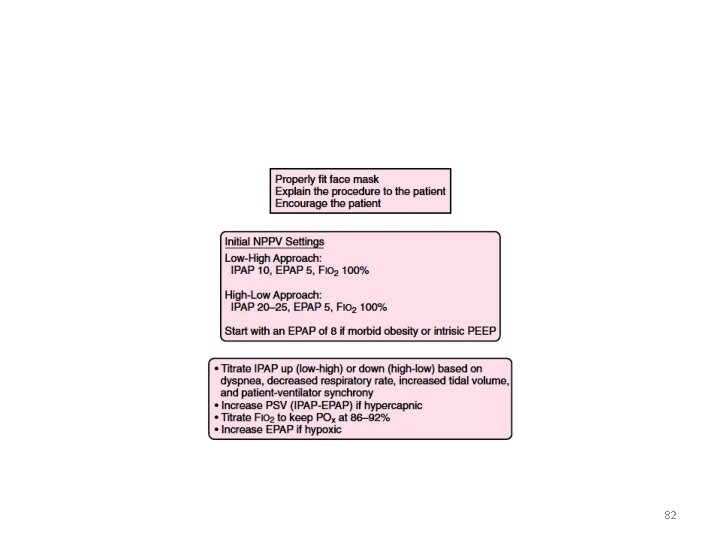
82
• Serial assessment and close monitoring Q 30 min • ABG Q 1 -2 h • Contraindications: – Near arrest – Severe GIB – Anatomic defect of face – Up airway obstruction – AMS – Risk of aspiration and defect in secretion clearance 83
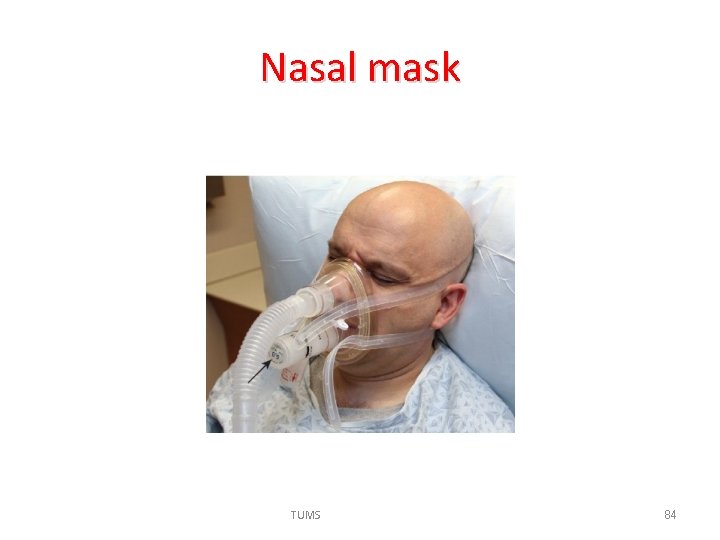
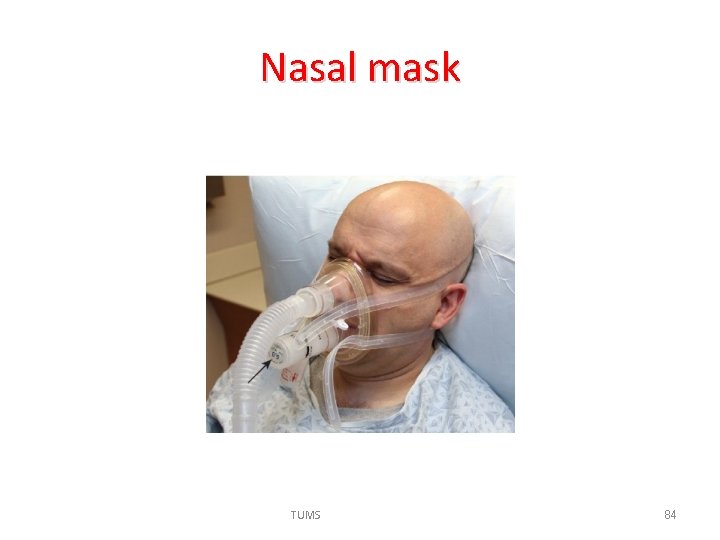
Nasal mask TUMS 84
Advantages of NIV The potential benefits of NIV over MV are: 1. 2. 3. 4. a decrease in potential airway injury decrease in VAP probably a shorter length of stay Eating and speech reserved TUMS 85
Disadvantages of NIV 1. Pulmonary baro-trauma (volu-trauma) 2. pressure necrosis of the facial skin, subcutaneous tissue and musculature and patient discomfort 3. aerophgia gastric dilation vomiting and aspiration 4. hemodynamic compromise TUMS 86
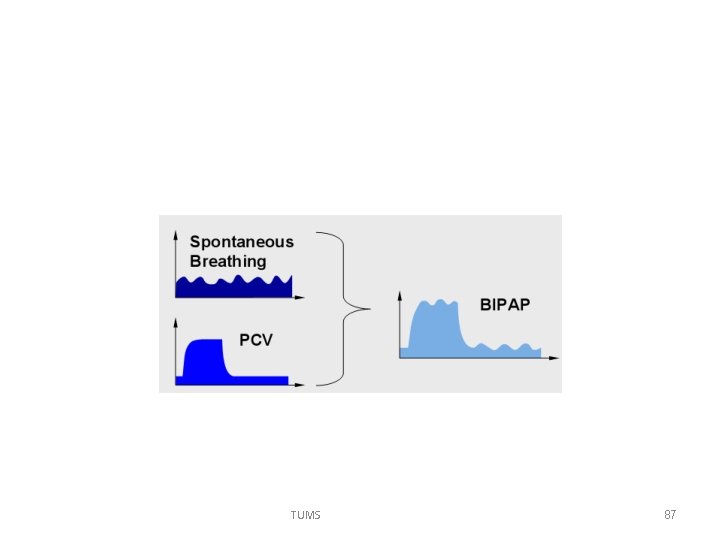
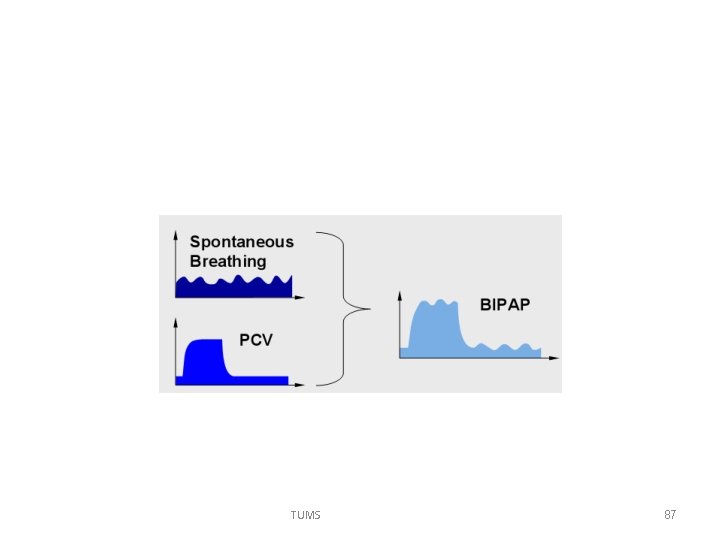
TUMS 87
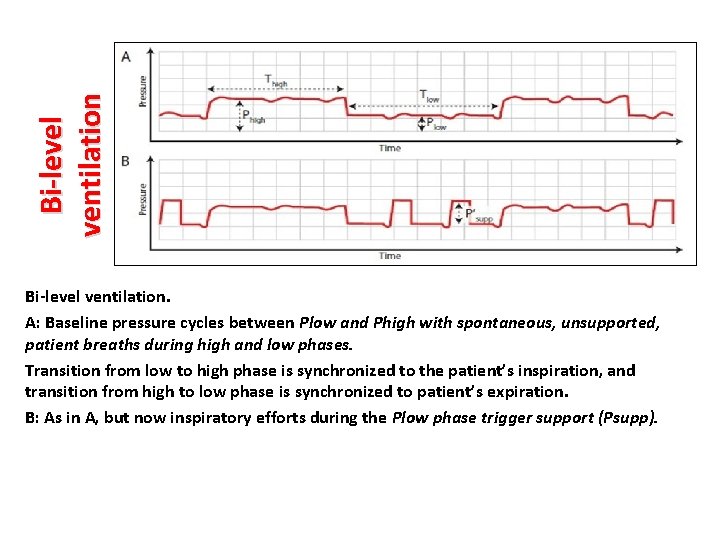
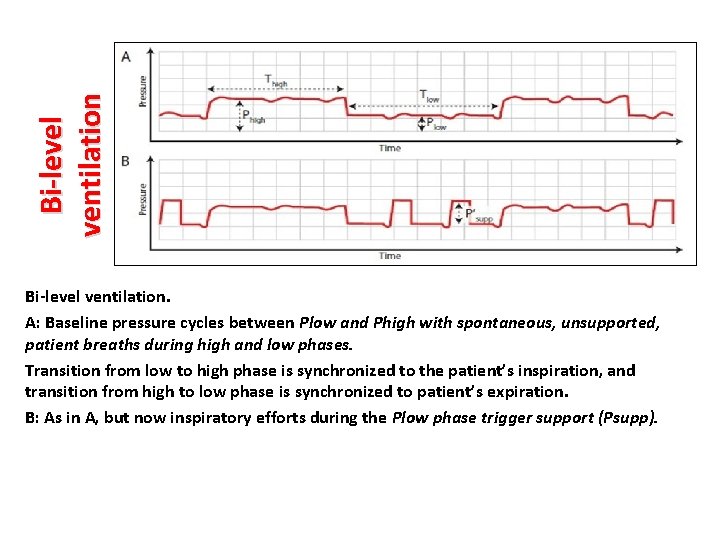
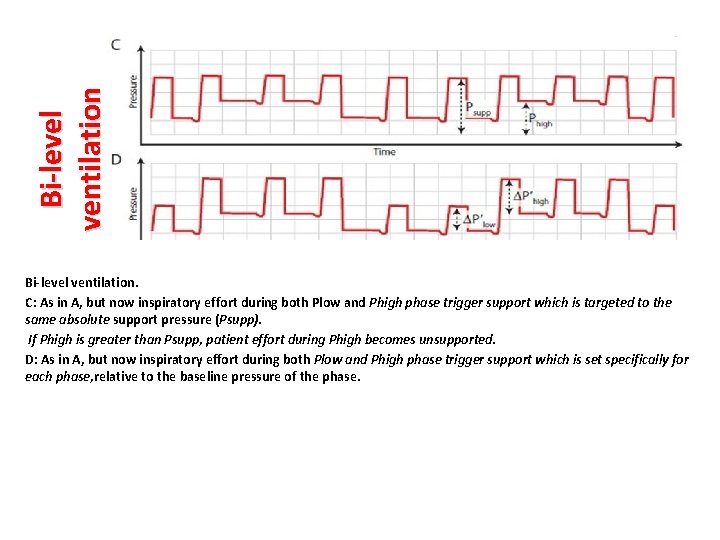
Bi-level ventilation. A: Baseline pressure cycles between Plow and Phigh with spontaneous, unsupported, patient breaths during high and low phases. Transition from low to high phase is synchronized to the patient’s inspiration, and transition from high to low phase is synchronized to patient’s expiration. B: As in A, but now inspiratory efforts during the Plow phase trigger support (Psupp).
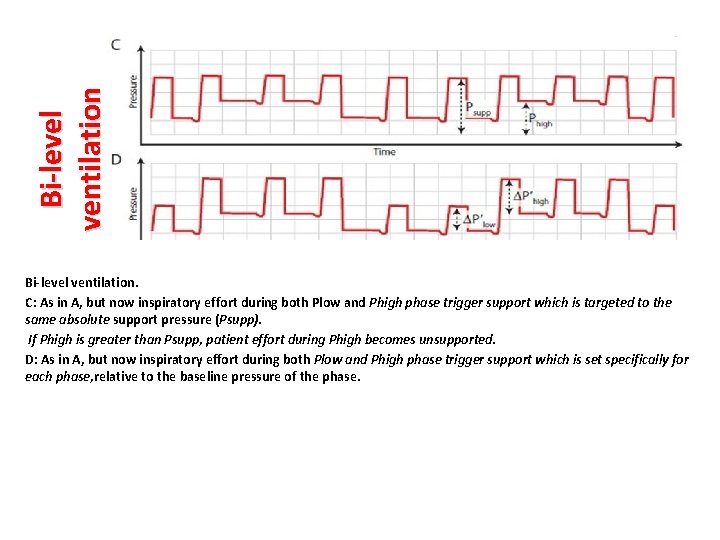
Bi-level ventilation. C: As in A, but now inspiratory effort during both Plow and Phigh phase trigger support which is targeted to the same absolute support pressure (Psupp). If Phigh is greater than Psupp, patient effort during Phigh becomes unsupported. D: As in A, but now inspiratory effort during both Plow and Phigh phase trigger support which is set specifically for each phase, relative to the baseline pressure of the phase.
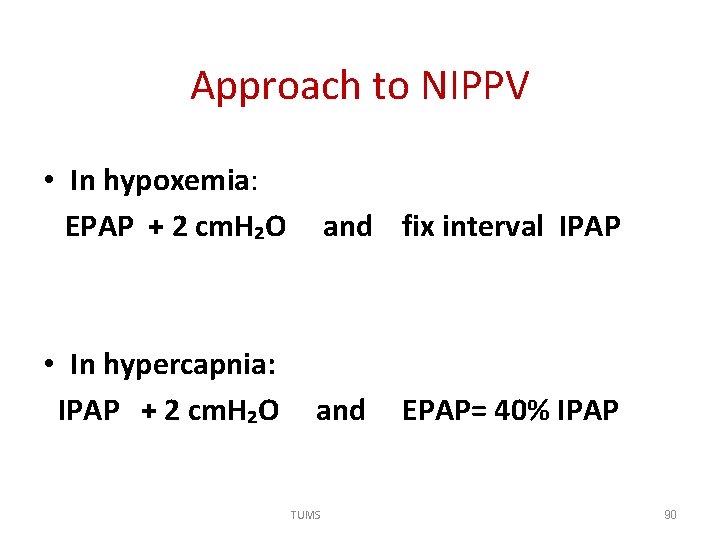
Approach to NIPPV • In hypoxemia: EPAP + 2 cm. H₂O and fix interval IPAP • In hypercapnia: IPAP + 2 cm. H₂O and EPAP= 40% IPAP TUMS 90
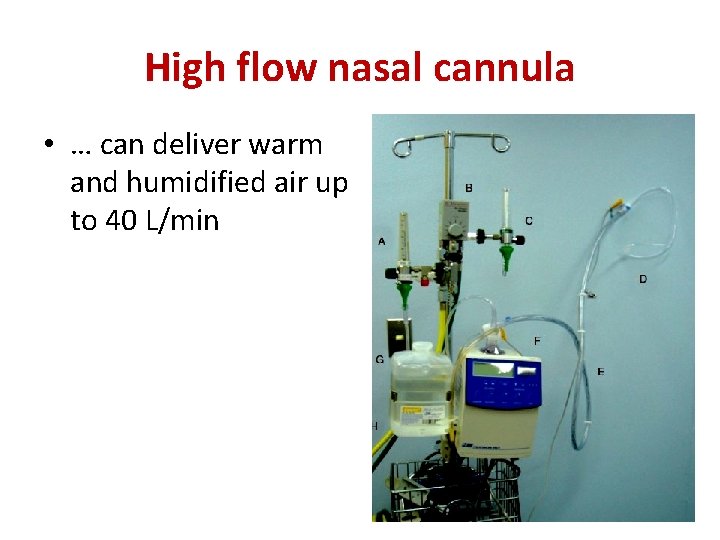
High flow nasal cannula • … can deliver warm and humidified air up to 40 L/min 91
5 Special Circumstances and applying ventilatory support TUMS 92
1. Severe Acute Lung Injury and ARDS • Preferred PCV • consider permissive hypercapnia. If able to achieve P 02> 60 mm Hg on Fi. O 2<60%, the PCO 2 may be allowed to be >40 mm Hg if p. H> 7. 25. if needed, use Na. HCO 3 • • Tv 6 – 8 ml / kg F 20 – 25 / min PEEP 8 Monitor P plateau: if > 30 cm H 2 O Tv : 4 ml/kg TUMS 93
2. Severe Asthma and COPD • The defect is decreased gas flow. • In conventional ventilation use higher flow rate and lower respiratory rate to allow more time for exhalation. • Tv 5 -8 ml / kg • F 8 – 10 / min • Q 80 l/min • PEEP 5 (50 - 80% intrinsic PEEP) • Detection of intrinsic PEEP with wean and chest compression • Optimal P plateau < 30 cm. H 2 O TUMS 94
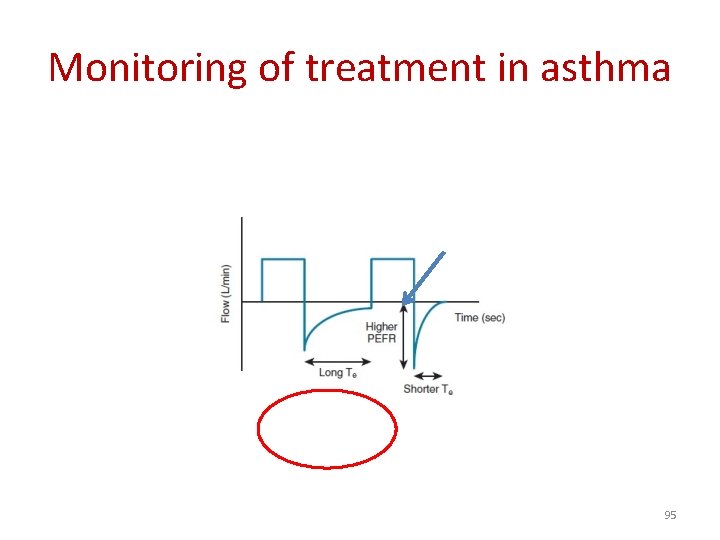
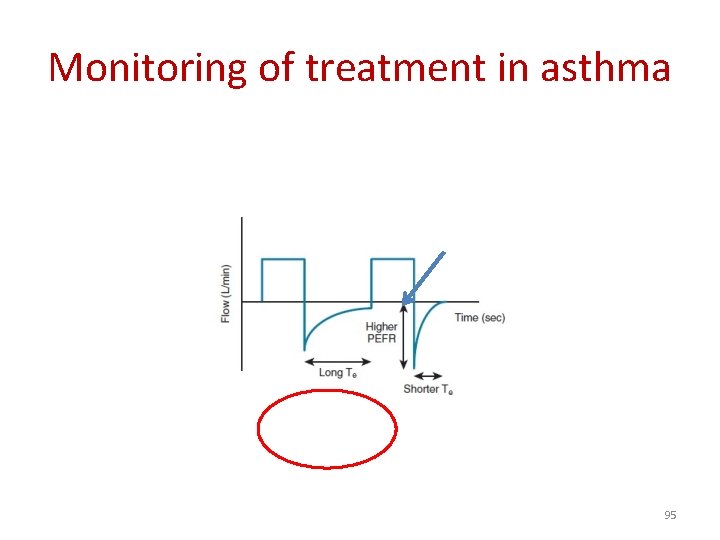
Monitoring of treatment in asthma 95
3. Pulmonary edema • • • NIPPV is preferred If the patient is intubated PEEP is useful But in hypotensive patients min. PEEP with continuous evaluation TUMS 96
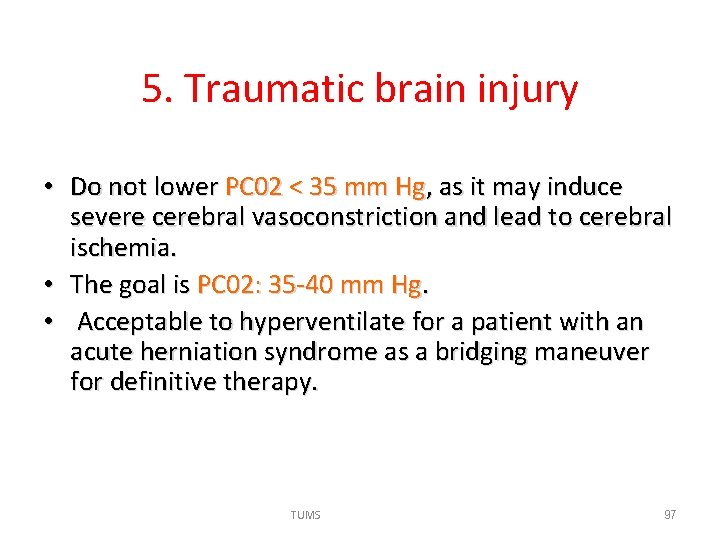
5. Traumatic brain injury • Do not lower PC 02 < 35 mm Hg, as it may induce severe cerebral vasoconstriction and lead to cerebral ischemia. • The goal is PC 02: 35 -40 mm Hg. • Acceptable to hyperventilate for a patient with an acute herniation syndrome as a bridging maneuver for definitive therapy. TUMS 97
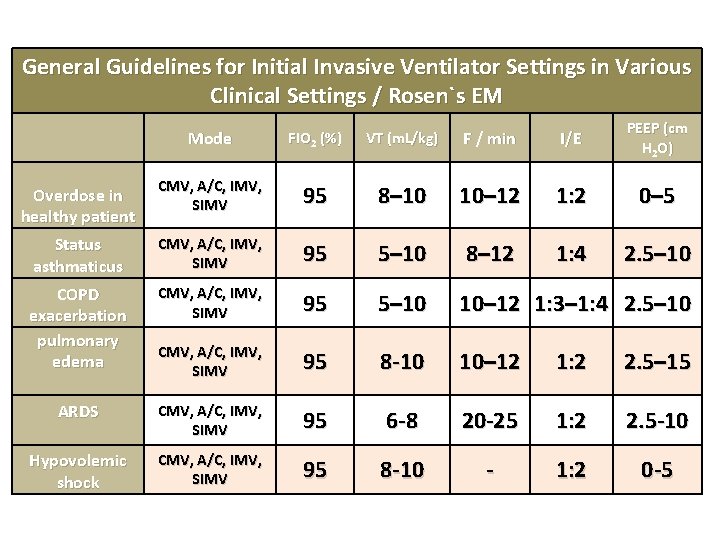
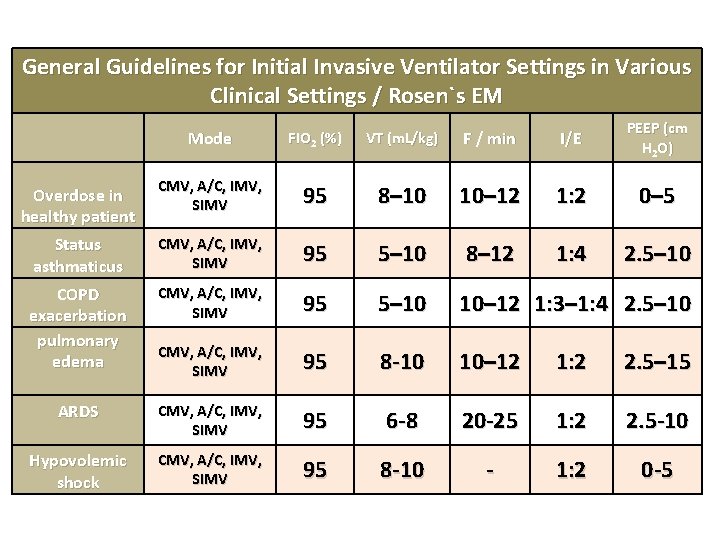
General Guidelines for Initial Invasive Ventilator Settings in Various Clinical Settings / Rosen`s EM Mode FIO 2 (%) VT (m. L/kg) F / min I/E PEEP (cm H 2 O) Overdose in healthy patient CMV, A/C, IMV, SIMV 95 8– 10 10– 12 1: 2 0– 5 Status asthmaticus CMV, A/C, IMV, SIMV 95 5– 10 8– 12 1: 4 2. 5– 10 COPD exacerbation pulmonary edema CMV, A/C, IMV, SIMV 95 5– 10 10– 12 1: 3– 1: 4 2. 5– 10 CMV, A/C, IMV, SIMV 95 8 -10 10– 12 1: 2 2. 5– 15 ARDS CMV, A/C, IMV, SIMV 95 6 -8 20 -25 1: 2 2. 5 -10 Hypovolemic shock CMV, A/C, IMV, SIMV 95 8 -10 - 1: 2 0 -5
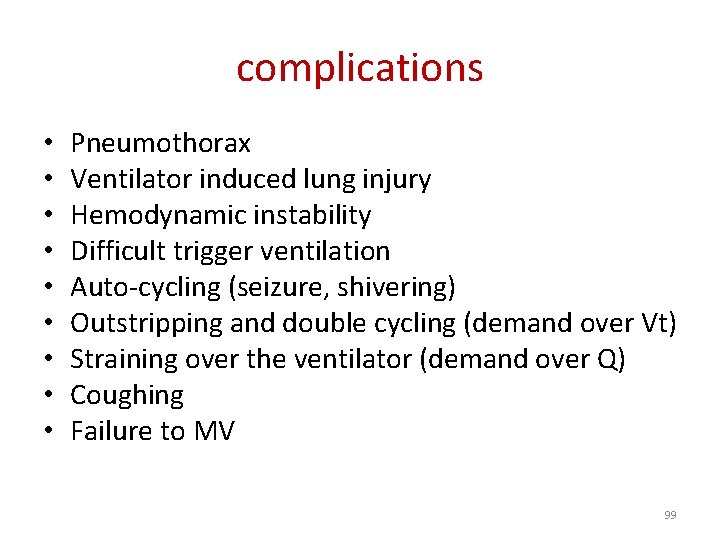
complications • • • Pneumothorax Ventilator induced lung injury Hemodynamic instability Difficult trigger ventilation Auto-cycling (seizure, shivering) Outstripping and double cycling (demand over Vt) Straining over the ventilator (demand over Q) Coughing Failure to MV 99
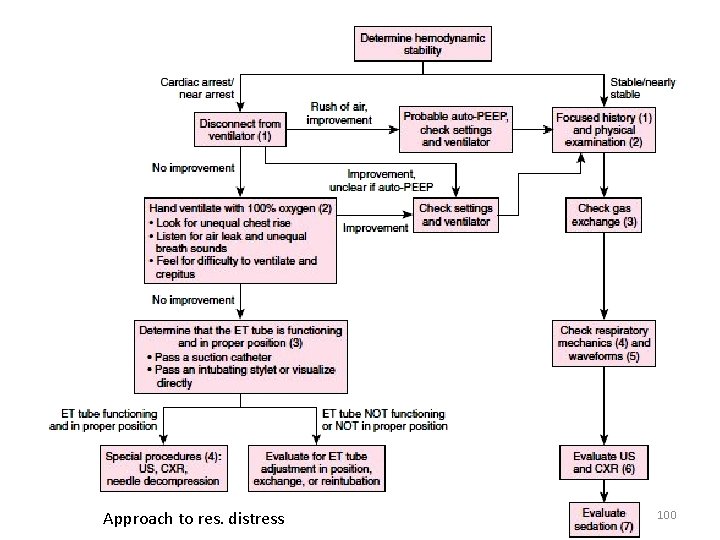
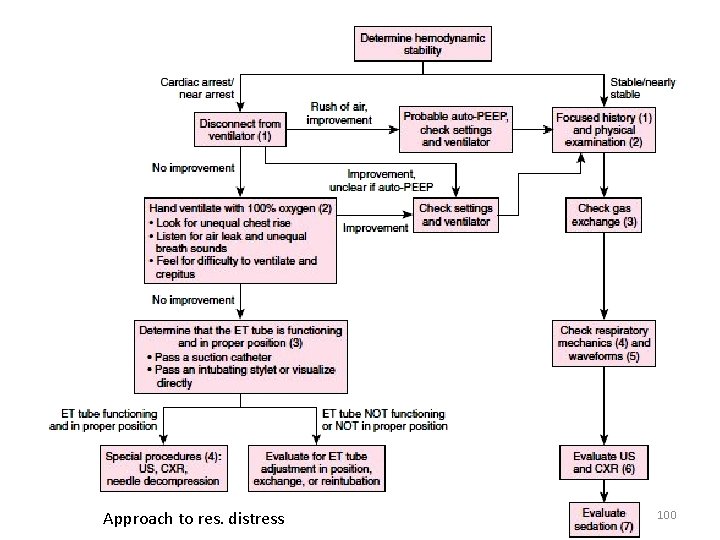
Approach to res. distress 100
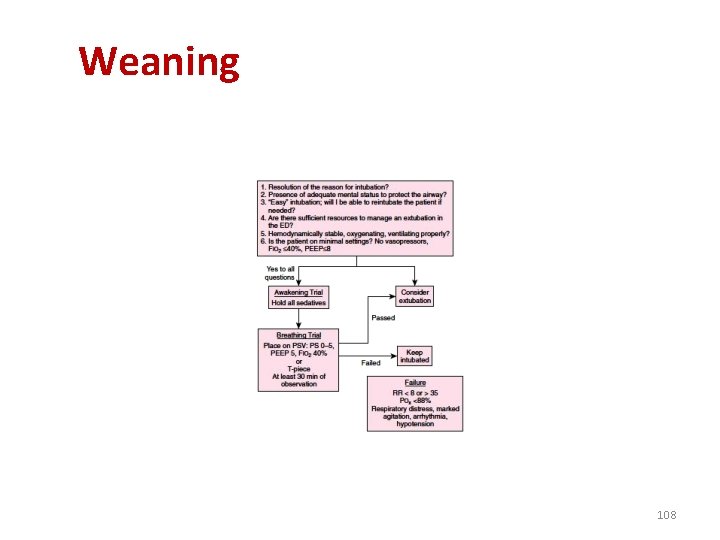
Weaning 101
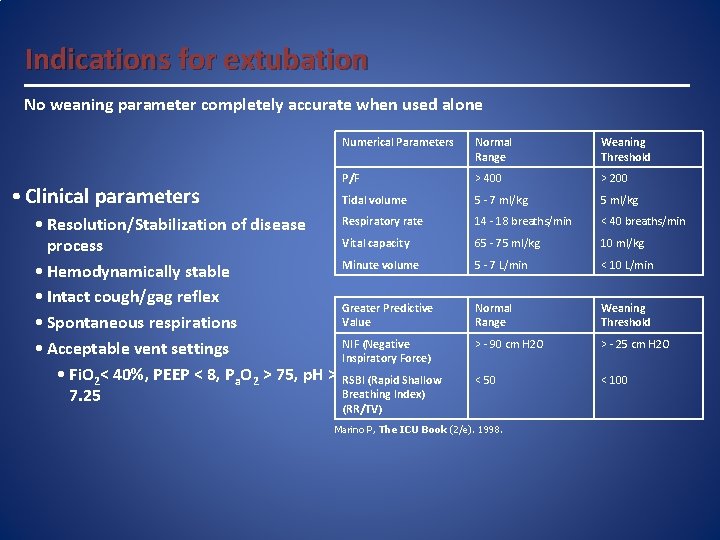
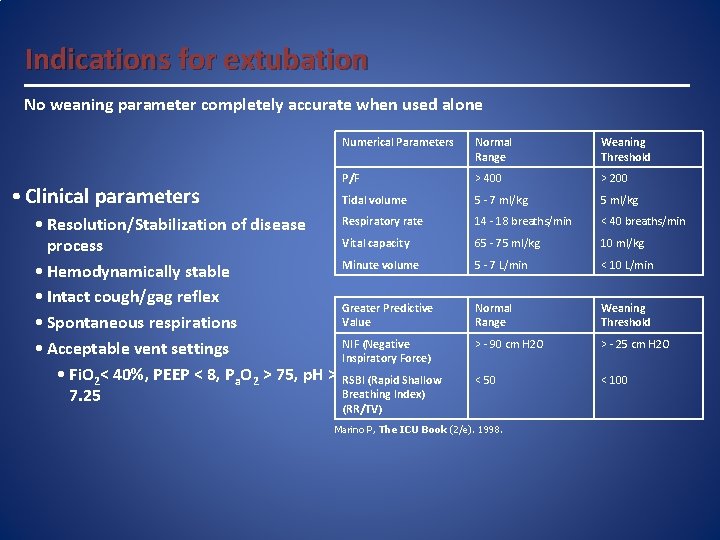
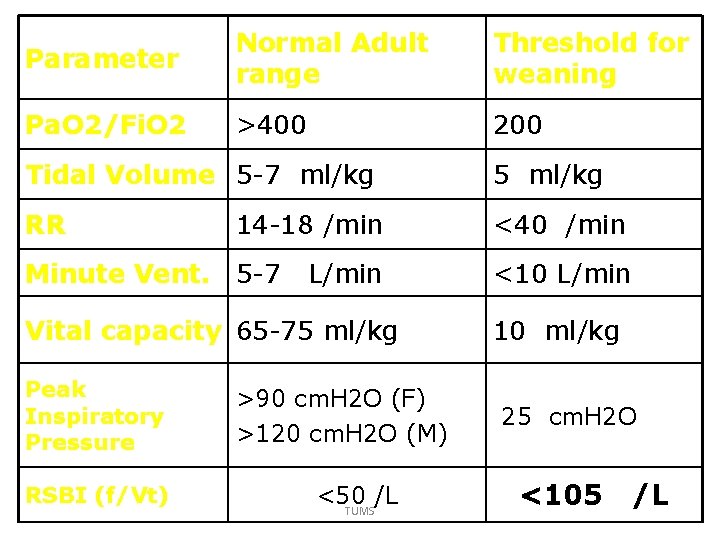
Indications for extubation No weaning parameter completely accurate when used alone • Clinical parameters Numerical Parameters Normal Range Weaning Threshold P/F > 400 > 200 Tidal volume 5 - 7 ml/kg 5 ml/kg 14 - 18 breaths/min < 40 breaths/min 65 - 75 ml/kg 10 ml/kg 5 - 7 L/min < 10 L/min Normal Range Weaning Threshold > - 90 cm H 2 O > - 25 cm H 2 O < 50 < 100 Respiratory rate • Resolution/Stabilization of disease Vital capacity process Minute volume • Hemodynamically stable • Intact cough/gag reflex Greater Predictive Value • Spontaneous respirations NIF (Negative • Acceptable vent settings Inspiratory Force) • Fi. O 2< 40%, PEEP < 8, Pa. O 2 > 75, p. H > RSBI (Rapid Shallow Breathing Index) 7. 25 (RR/TV) Marino P, The ICU Book (2/e). 1998.
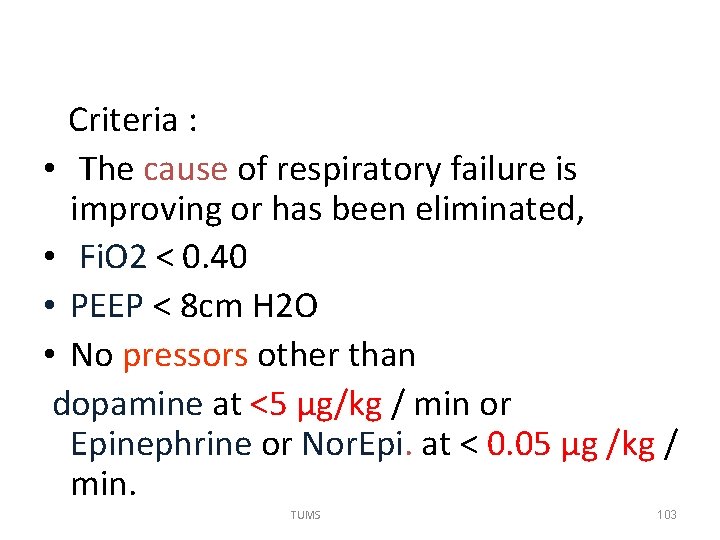
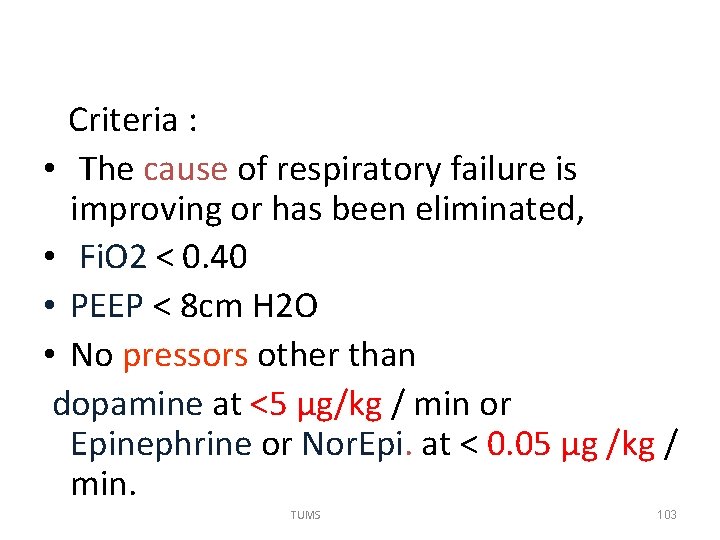
Criteria : • The cause of respiratory failure is improving or has been eliminated, • Fi. O 2 < 0. 40 • PEEP < 8 cm H 2 O • No pressors other than dopamine at <5 μg/kg / min or Epinephrine or Nor. Epi. at < 0. 05 µg /kg / min. TUMS 103
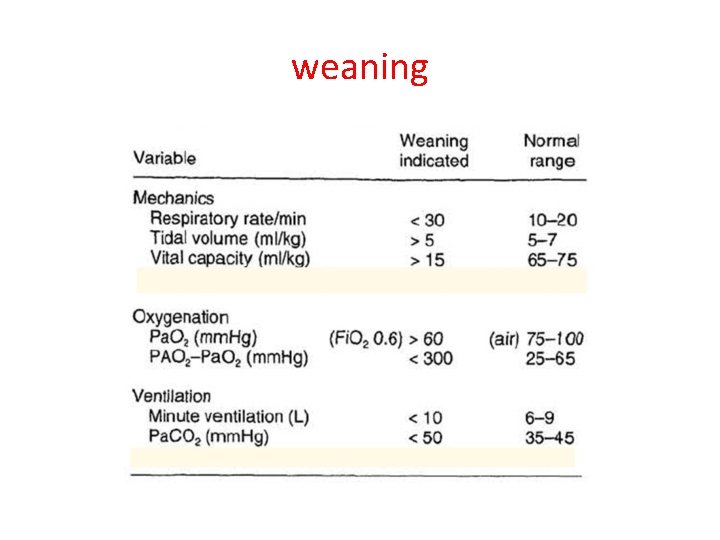
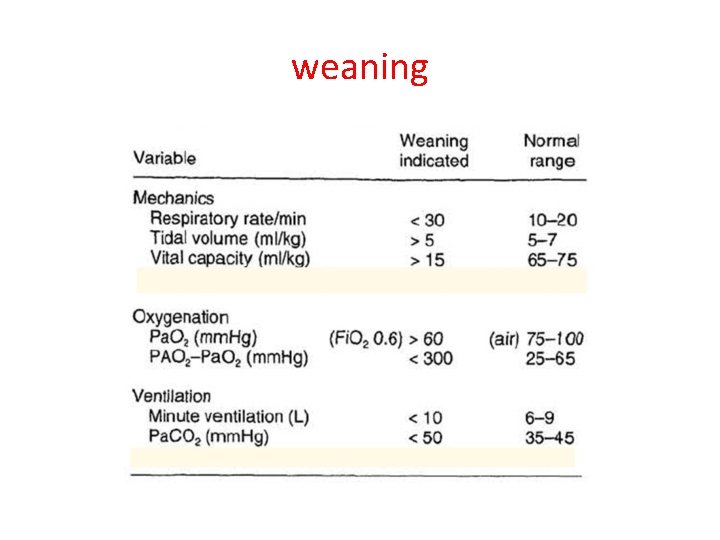
weaning
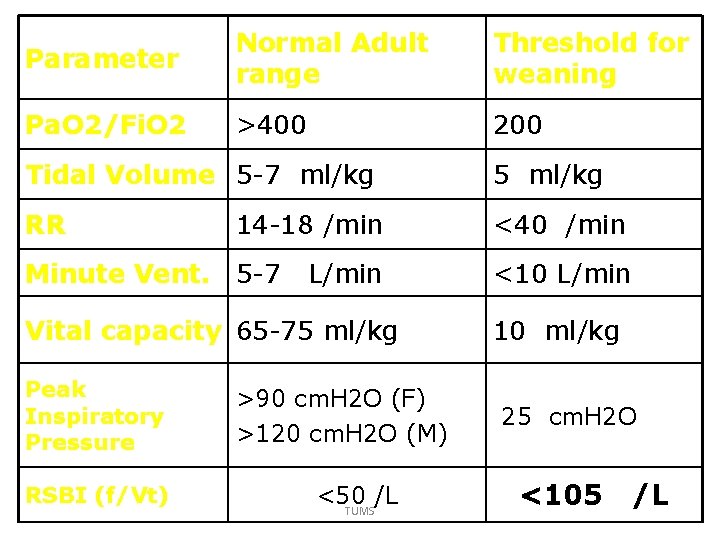
Parameter Normal Adult range Threshold for weaning Pa. O 2/Fi. O 2 >400 200 Tidal Volume 5 -7 ml/kg 5 ml/kg RR <40 /min 14 -18 /min Minute Vent. 5 -7 L/min Vital capacity 65 -75 ml/kg Peak Inspiratory Pressure RSBI (f/Vt) >90 cm. H 2 O (F) >120 cm. H 2 O (M) <50 /L TUMS <10 L/min 10 ml/kg 25 cm. H 2 O <105 /L
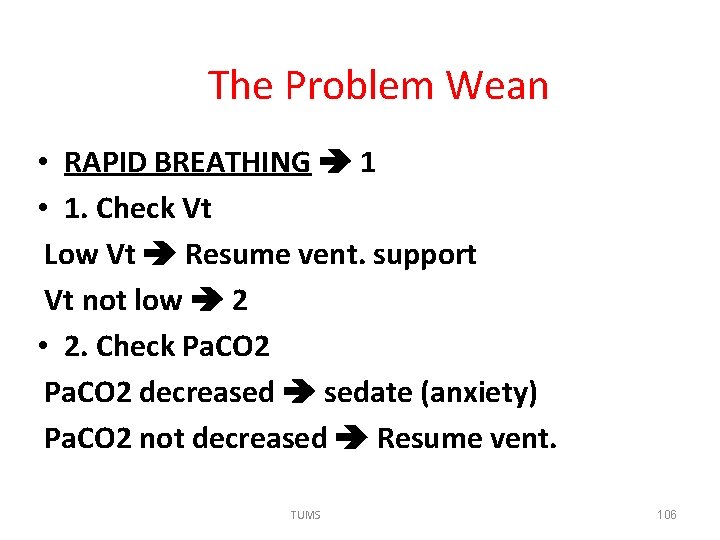
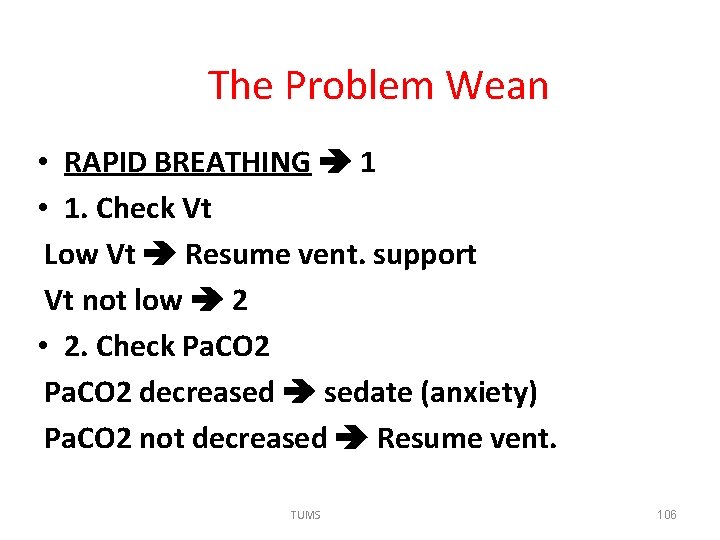
The Problem Wean • RAPID BREATHING 1 • 1. Check Vt Low Vt Resume vent. support Vt not low 2 • 2. Check Pa. CO 2 decreased sedate (anxiety) Pa. CO 2 not decreased Resume vent. TUMS 106
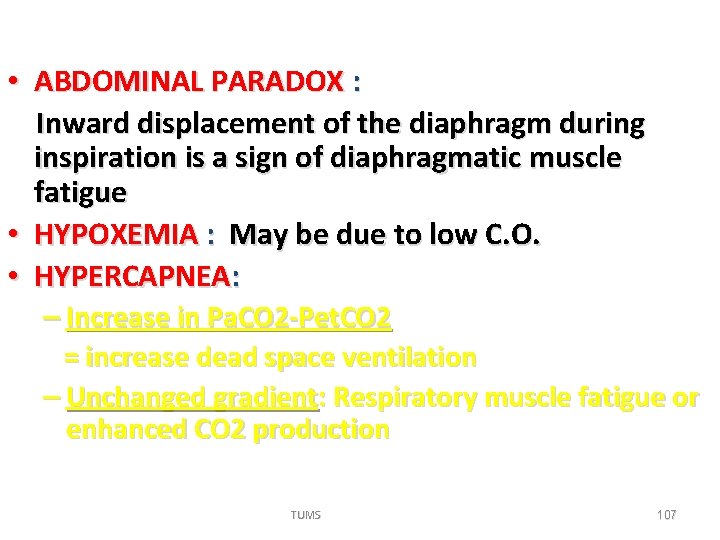
• ABDOMINAL PARADOX : Inward displacement of the diaphragm during inspiration is a sign of diaphragmatic muscle fatigue • HYPOXEMIA : May be due to low C. O. • HYPERCAPNEA: – Increase in Pa. CO 2 -Pet. CO 2 = increase dead space ventilation – Unchanged gradient: Respiratory muscle fatigue or enhanced CO 2 production TUMS 107
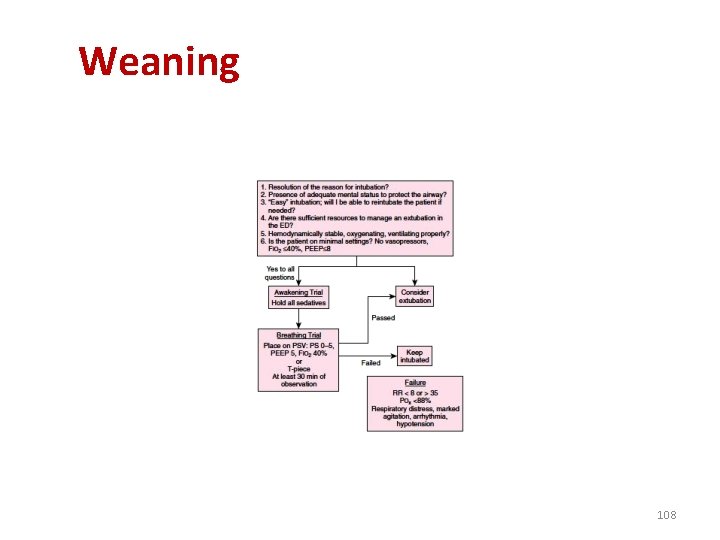
Weaning 108
Tracheal Decannulation • Successful weaning is not synonymous with tracheal decannulation • If weaned and not fully awake or unable to clear secretions, leave ETT in place • Tracheal decannulation increases the work of breathing due to laryngeal edema and secretions • Do not perform tracheal decannulation to reduce work of breathing TUMS 109
Inspiratory Stridor • Post extubation inspiratory stridor is a sign of severe obstruction and should prompt re-intubation • Laryngeal edema (post-ext) may respond to aerosolized epinephrine in children • Steroids have no role • Most need reintubation followed by tracheostomy TUMS 110
TUMS 111
Case management TUMS 112
Case 1 • An l 8 -year-old otherwise healthy 60 -kg female presents with an overdose of benzodiazepines. • She requires intubation for airway protection and ventilatory support. • There is no evidence of aspiration or an intrinsic lung problem. TUMS 113
With VCV setting Target Vm = 7. 2 L / min It is reasonable to assume a normal need for Vm since she has no evidence of hypoperfusion or infection, and she has not ingested an medications known to cause a metabolic acidosis that would require a higher Vm to buffer by induced hypocarbia. TUMS 114
Dräger ev. Aita 2 Patient data Ventilator setting Alarm setting TUMS 115
Vt and f • F= 12 /min • Vt = 600 m. L (7 -10 m. L/kg) • This setting will guarantee the desired Vm even if the patient continues to develop respiratory depression from the benzodiazepine ingestion. TUMS 116
Pressure Support Ventilation. • Initiate PSV at 10 cm H 20 pressure, and then titrate up or down to achieve a spontaneous breath Vt approximately equal to that of the set Vt. TUMS 117
• Gas Delivery Waveform: Begin with a decelerating waveform. • Maximal Inspiratory Flow : Set the initial Q at 60 L/min. lower Q(Q = 50 L/min) in hypoxemia higher flow (Q = 70 L/min) in exhalation obstruction (e. g. COPD), then evaluate the resultant Paw-peak. TUMS 118
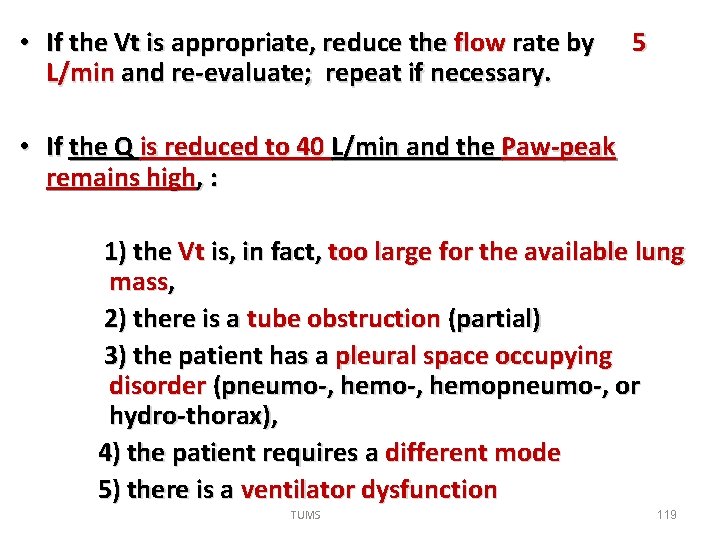
• If the Vt is appropriate, reduce the flow rate by 5 L/min and re-evaluate; repeat if necessary. • If the Q is reduced to 40 L/min and the Paw-peak remains high, : 1) the Vt is, in fact, too large for the available lung mass, 2) there is a tube obstruction (partial) 3) the patient has a pleural space occupying disorder (pneumo-, hemopneumo-, or hydro-thorax), 4) the patient requires a different mode 5) there is a ventilator dysfunction TUMS 119
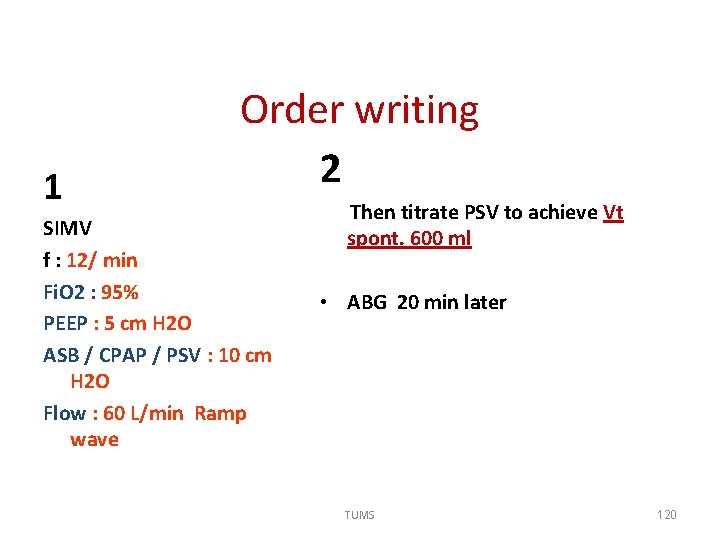
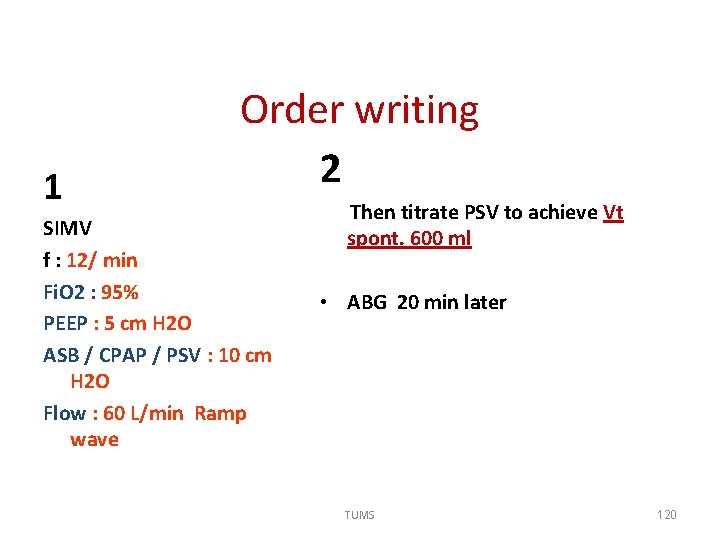
1 Order writing 2 SIMV f : 12/ min Fi. O 2 : 95% PEEP : 5 cm H 2 O ASB / CPAP / PSV : 10 cm H 2 O Flow : 60 L/min Ramp wave Then titrate PSV to achieve Vt spont. 600 ml • ABG 20 min later TUMS 120
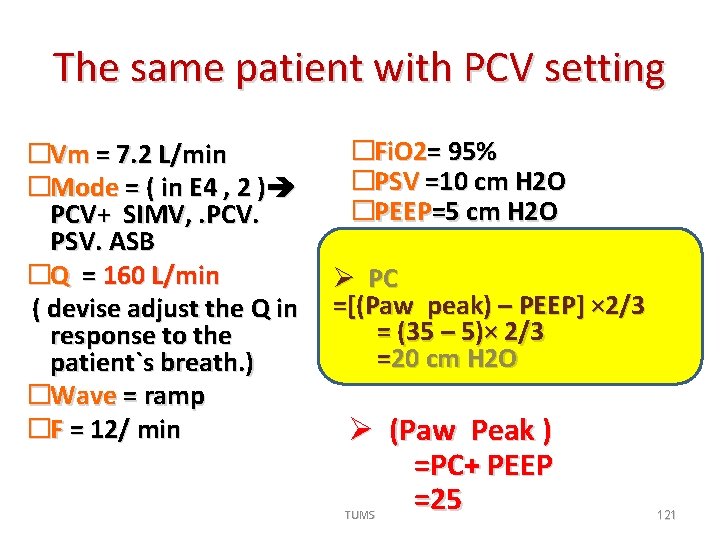
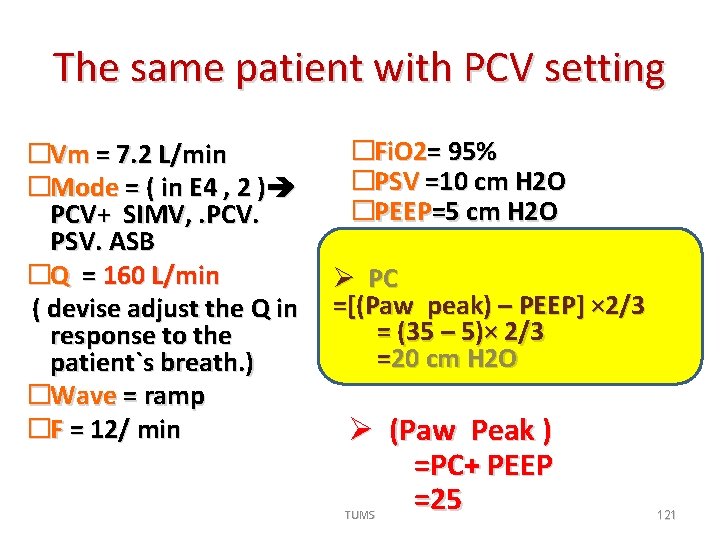
The same patient with PCV setting �Vm = 7. 2 L/min �Mode = ( in E 4 , 2 ) PCV+ SIMV, . PCV. PSV. ASB �Q = 160 L/min ( devise adjust the Q in response to the patient`s breath. ) �Wave = ramp �F = 12/ min �Fi. O 2= 95% �PSV =10 cm H 2 O �PEEP=5 cm H 2 O Ø PC =[(Paw peak) – PEEP] × 2/3 = (35 – 5)× 2/3 =20 cm H 2 O Ø (Paw Peak ) =PC+ PEEP =25 TUMS 121
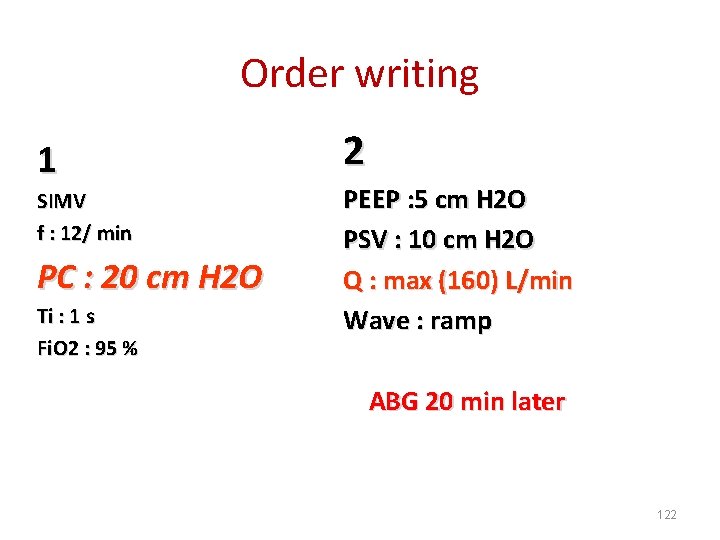
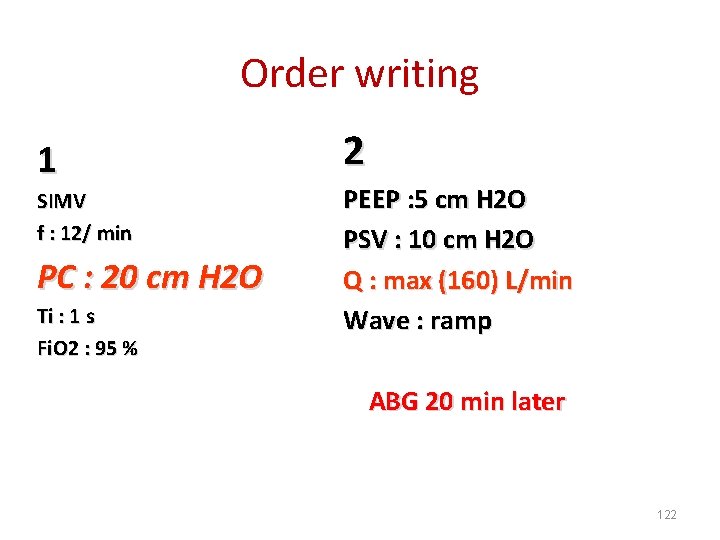
Order writing 1 SIMV f : 12/ min PC : 20 cm H 2 O Ti : 1 s Fi. O 2 : 95 % 2 PEEP : 5 cm H 2 O PSV : 10 cm H 2 O Q : max (160) L/min Wave : ramp ABG 20 min later 122
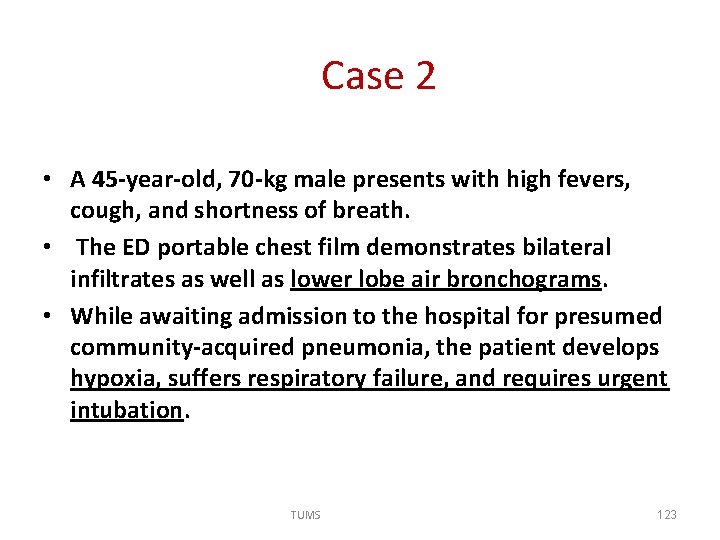
Case 2 • A 45 -year-old, 70 -kg male presents with high fevers, cough, and shortness of breath. • The ED portable chest film demonstrates bilateral infiltrates as well as lower lobe air bronchograms. • While awaiting admission to the hospital for presumed community-acquired pneumonia, the patient develops hypoxia, suffers respiratory failure, and requires urgent intubation. TUMS 123
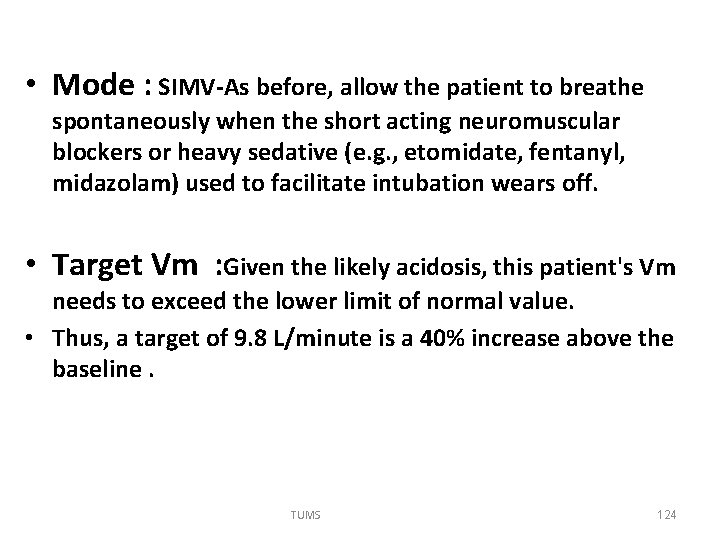
• Mode : SIMV-As before, allow the patient to breathe spontaneously when the short acting neuromuscular blockers or heavy sedative (e. g. , etomidate, fentanyl, midazolam) used to facilitate intubation wears off. • Target Vm : Given the likely acidosis, this patient's Vm needs to exceed the lower limit of normal value. • Thus, a target of 9. 8 L/minute is a 40% increase above the baseline. TUMS 124
• initial f= 14 / min • Vt = 700 ml • One must evaluate the resultant Paw-peak after starting at this setting. • One may also need to reduce the tidal volume and increase the rate if the Paw-peak is high and no other mode of ventilation is available. TUMS 125
• Fi 02 : Begin with Fi. O 2 : 95% then titrate. • PEEP : ≥ 5 (to maintain FRC and alveolar recruitment with V/S consideration ) • Flow: • A longer Ti is ideal for alveolar recruitment and a slow flow rate will complement the decelerating waveform and further prolong the Ti. • Then start with a Q of 50 L/min TUMS 126
• Start with a higher PSV because the pulmonary compliance is less than the normal lungs. • Initiate PSV at 15 cm H 20 and titrate to achieve similar Vt with the machine and spontaneous breaths. • In PCV : the same MODE & Vm … • Only set the Ti & PC (longer Ti) • Then reevaluate the patient`s condition TUMS 127
The end TUMS 128
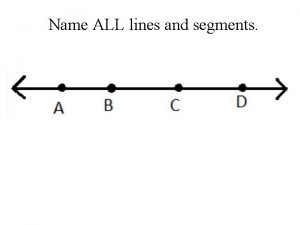
 Name a point that is collinear with the given points
Name a point that is collinear with the given points Actual mechanical advantage vs ideal mechanical advantage
Actual mechanical advantage vs ideal mechanical advantage Mechanical principles
Mechanical principles Headgear force intermittent
Headgear force intermittent Principles of tooth preparation
Principles of tooth preparation Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Tư thế worms-breton
Tư thế worms-breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cong thức tính động năng
Cong thức tính động năng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ V cc
V cc Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Thế nào là số nguyên tố
Thế nào là số nguyên tố Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Our god is an awesome god vine
Our god is an awesome god vine Our god is an awesome god
Our god is an awesome god God is an awesome god and greatly to be praised
God is an awesome god and greatly to be praised God is good god is great speed
God is good god is great speed O god you are my god earnestly i seek you
O god you are my god earnestly i seek you God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. God-given virtues that direct us to our loving, triune god.
God-given virtues that direct us to our loving, triune god. My god's bigger than your god
My god's bigger than your god How to know god personally four spiritual principles
How to know god personally four spiritual principles Don't covet your neighbor's
Don't covet your neighbor's First i must honor god second honor his name
First i must honor god second honor his name O lord our lord how excellent your name is
O lord our lord how excellent your name is In the name of god amen
In the name of god amen In the name of god most gracious most merciful
In the name of god most gracious most merciful You are my all in all images
You are my all in all images 12 roman gods
12 roman gods Asymmetry
Asymmetry In the name of god the beneficent the merciful
In the name of god the beneficent the merciful In the name of god most gracious most merciful
In the name of god most gracious most merciful Hercules scar rug
Hercules scar rug Deity titles
Deity titles God name
God name Our god saves
Our god saves In the name of god most gracious prayer
In the name of god most gracious prayer In the name of god the merciful
In the name of god the merciful His name is the word of god
His name is the word of god The rich is not what it
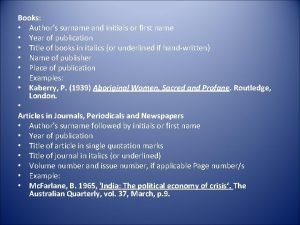
The rich is not what it Authors last name first name initial
Authors last name first name initial Name above every other name
Name above every other name Square shape names
Square shape names Class person string name person(string name)
Class person string name person(string name) What is her name
What is her name Name of presentation company name
Name of presentation company name Name of presentation company name
Name of presentation company name Name teachers name class date
Name teachers name class date Hello my name is betty
Hello my name is betty What's your name and how old are you
What's your name and how old are you What is your class teacher name answer
What is your class teacher name answer Student id name department name
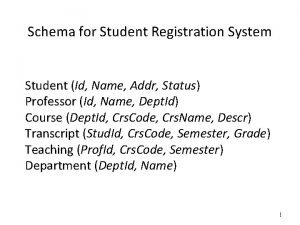
Student id name department name Git config user name
Git config user name Lecturer's name
Lecturer's name Agile inception planning
Agile inception planning Name date class
Name date class First name last name tpu
First name last name tpu Stock name and classical name of elements
Stock name and classical name of elements Ytu erasmus ofisi
Ytu erasmus ofisi What are the cutting tools
What are the cutting tools Kinetic energy definition
Kinetic energy definition Mechanical machine
Mechanical machine Two wheels of different sizes that rotate together
Two wheels of different sizes that rotate together How does mechanical advantage work
How does mechanical advantage work Example of a wheel and axle
Example of a wheel and axle What is an example of mechanical energy
What is an example of mechanical energy Mechanical isolation
Mechanical isolation Aidan kaminski
Aidan kaminski Organic solidarity
Organic solidarity Physical weathering and chemical weathering venn diagram
Physical weathering and chemical weathering venn diagram Weathering erosion
Weathering erosion Mechanical and chemical weathering venn diagram
Mechanical and chemical weathering venn diagram Identify three agents of mechanical weathering
Identify three agents of mechanical weathering Vertical wave
Vertical wave Lowest point of a wave
Lowest point of a wave Characteristics of mechanical waves
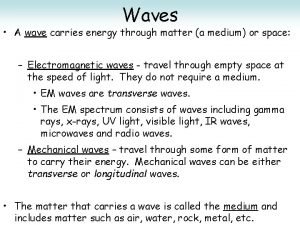
Characteristics of mechanical waves Carries energy through matter
Carries energy through matter Designspark.com
Designspark.com Transfer of energy when a wave disappears into a surface
Transfer of energy when a wave disappears into a surface Pusher vs non pusher mechanical seal
Pusher vs non pusher mechanical seal Type of mechanical waves
Type of mechanical waves Nps mechanical engineering
Nps mechanical engineering Mechanical transducer
Mechanical transducer Organic solidarity
Organic solidarity Quantum mechanical atom model
Quantum mechanical atom model Mechanical reasoning test gears
Mechanical reasoning test gears Pathway of digestion
Pathway of digestion Mechanical and chemical digestion
Mechanical and chemical digestion Mechanical hazard
Mechanical hazard Sterilization by mechanical methods
Sterilization by mechanical methods Habitat isolation.
Habitat isolation. Mechanical isolation in plants
Mechanical isolation in plants Law of conservation of energy
Law of conservation of energy Criticism of conflict theory
Criticism of conflict theory Mechanical advantage of a ramp
Mechanical advantage of a ramp