Imaging modalities History Energy Source The earliest medical





- Slides: 93
Imaging modalities
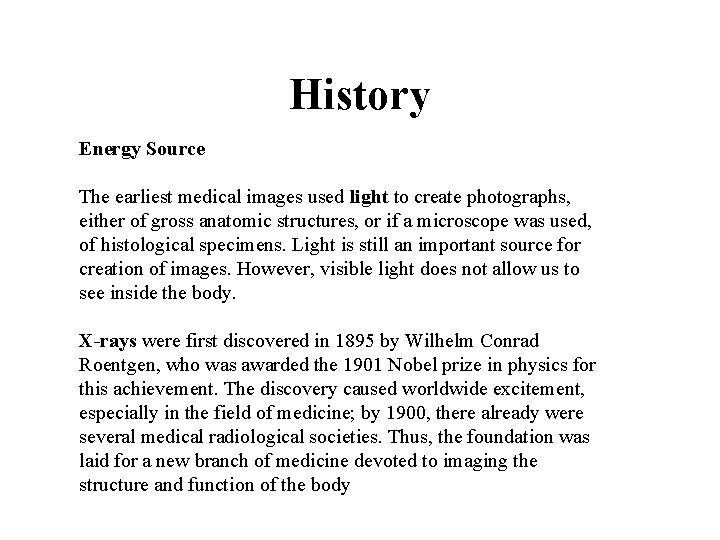
History Energy Source The earliest medical images used light to create photographs, either of gross anatomic structures, or if a microscope was used, of histological specimens. Light is still an important source for creation of images. However, visible light does not allow us to see inside the body. X-rays were first discovered in 1895 by Wilhelm Conrad Roentgen, who was awarded the 1901 Nobel prize in physics for this achievement. The discovery caused worldwide excitement, especially in the field of medicine; by 1900, there already were several medical radiological societies. Thus, the foundation was laid for a new branch of medicine devoted to imaging the structure and function of the body
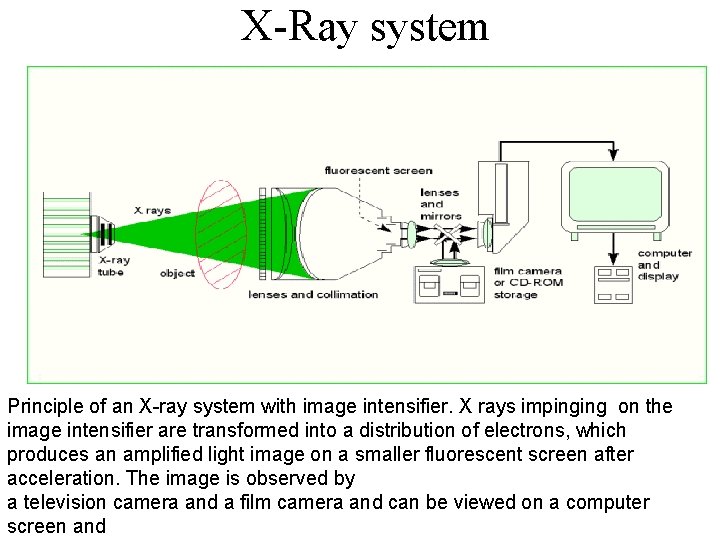
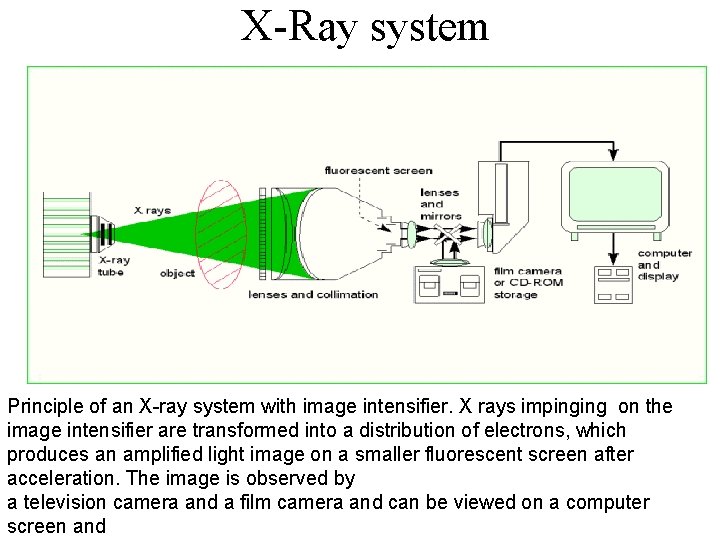
X-Ray system Principle of an X-ray system with image intensifier. X rays impinging on the image intensifier are transformed into a distribution of electrons, which produces an amplified light image on a smaller fluorescent screen after acceleration. The image is observed by a television camera and a film camera and can be viewed on a computer screen and
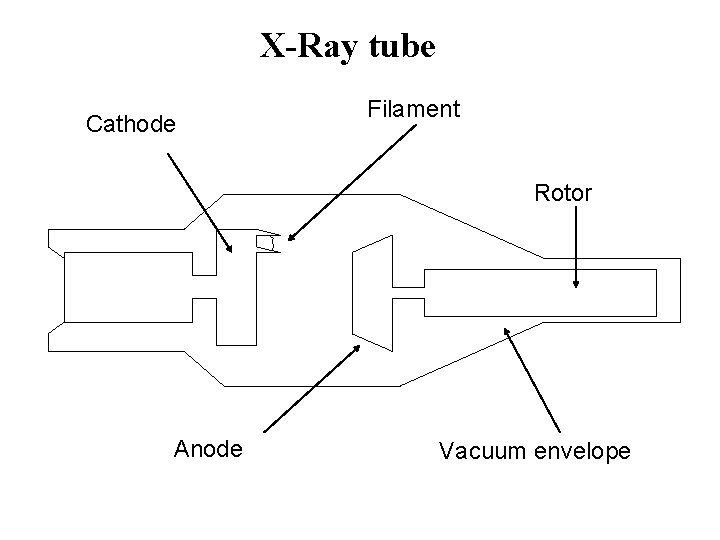
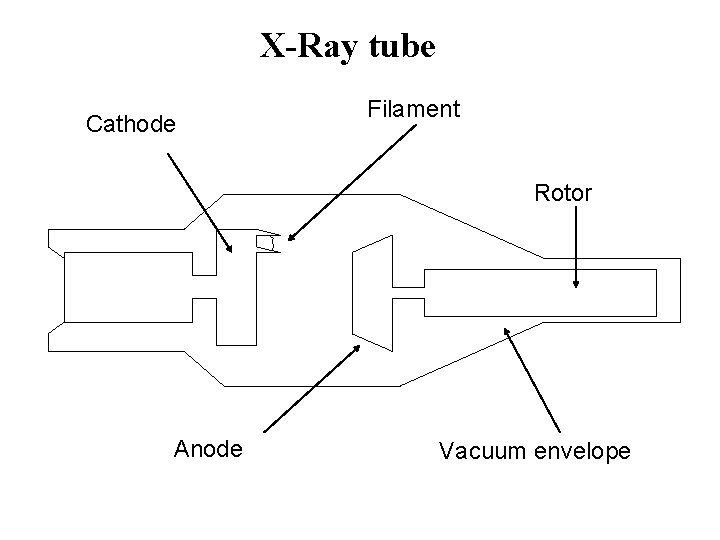
X-Ray tube Cathode Filament Rotor Anode Vacuum envelope
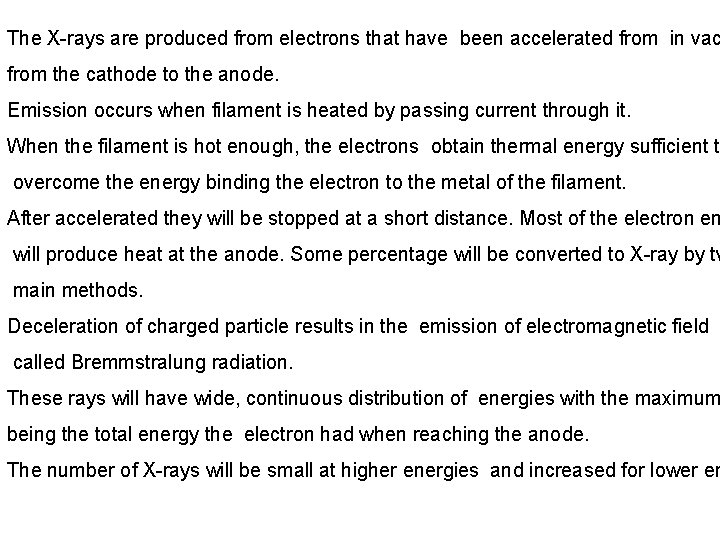
The X-rays are produced from electrons that have been accelerated from in vac from the cathode to the anode. Emission occurs when filament is heated by passing current through it. When the filament is hot enough, the electrons obtain thermal energy sufficient to overcome the energy binding the electron to the metal of the filament. After accelerated they will be stopped at a short distance. Most of the electron en will produce heat at the anode. Some percentage will be converted to X-ray by tw main methods. Deceleration of charged particle results in the emission of electromagnetic field called Bremmstralung radiation. These rays will have wide, continuous distribution of energies with the maximum being the total energy the electron had when reaching the anode. The number of X-rays will be small at higher energies and increased for lower en
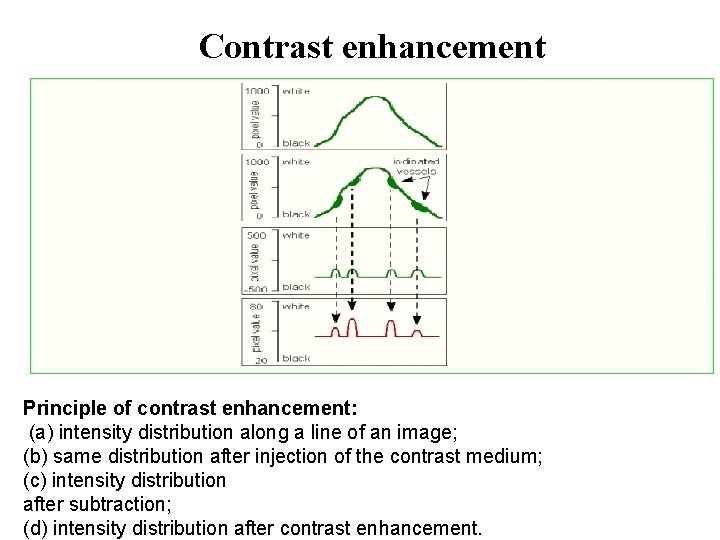
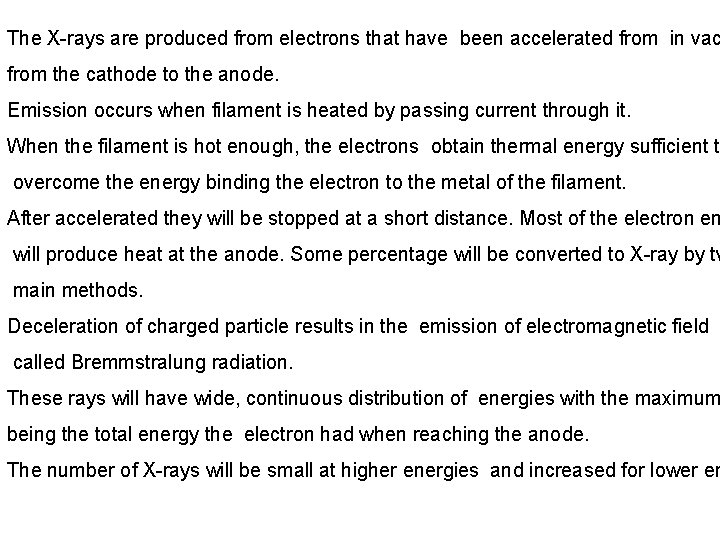
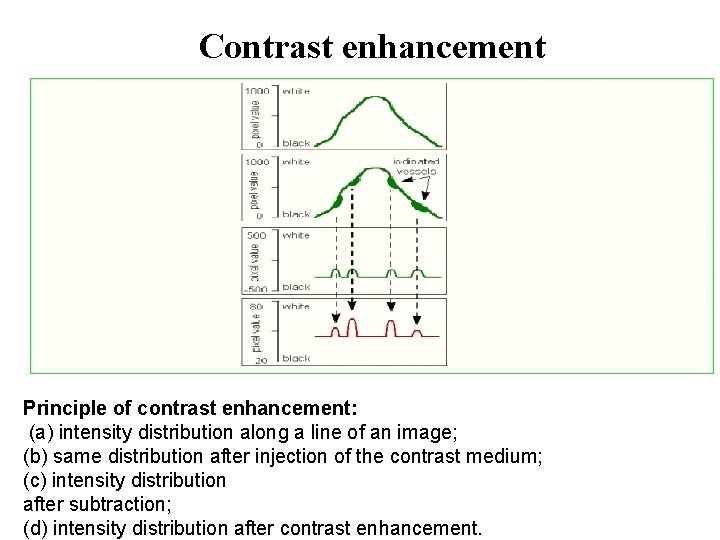
Contrast enhancement Principle of contrast enhancement: (a) intensity distribution along a line of an image; (b) same distribution after injection of the contrast medium; (c) intensity distribution after subtraction; (d) intensity distribution after contrast enhancement.
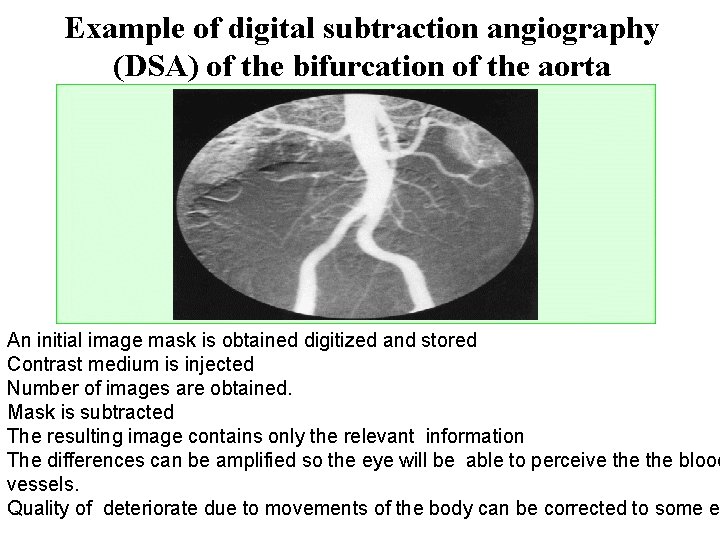
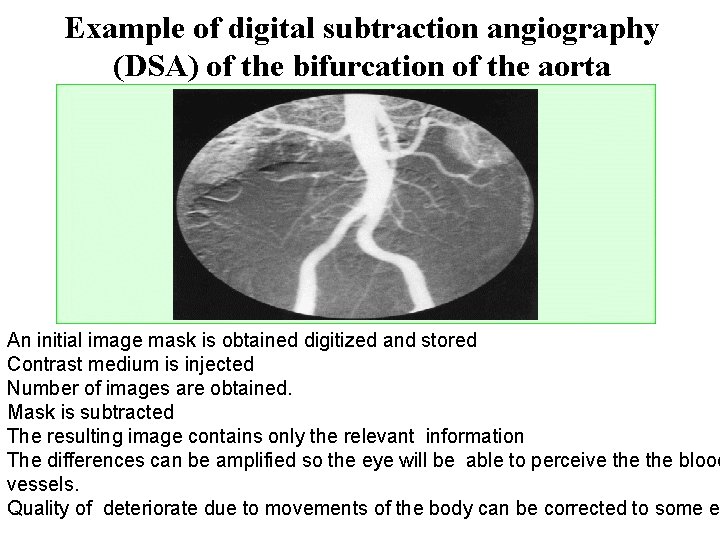
Example of digital subtraction angiography (DSA) of the bifurcation of the aorta An initial image mask is obtained digitized and stored Contrast medium is injected Number of images are obtained. Mask is subtracted The resulting image contains only the relevant information The differences can be amplified so the eye will be able to perceive the blood vessels. Quality of deteriorate due to movements of the body can be corrected to some e
Mammography; The mammogram is an X-ray shadowgram from a quasi-point source irradiate the breast and the transmitted X-rays are recorded by an image receptor. A region of reduced transmission corresponding to a structure of interest such as a tumor, a calcification or normal fibroglandular tissue. The imaging system must have a sufficient spatial resolution to delineate the edges of fine structures in the breast. Structural detail small as 50 m must be resolved adequately. Because the breast is sensitive to ionization radiation, which at least at high doses is known to cause breast cancer, it is desirable to use the lowest radiation dose compatible with excellent image quality.
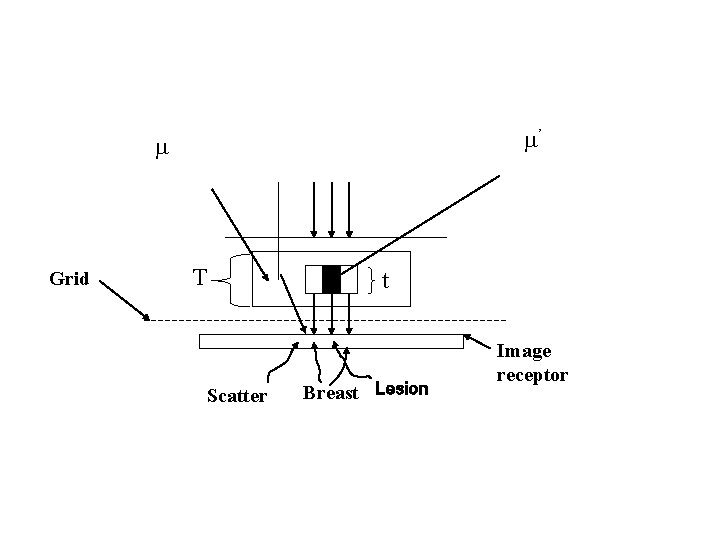
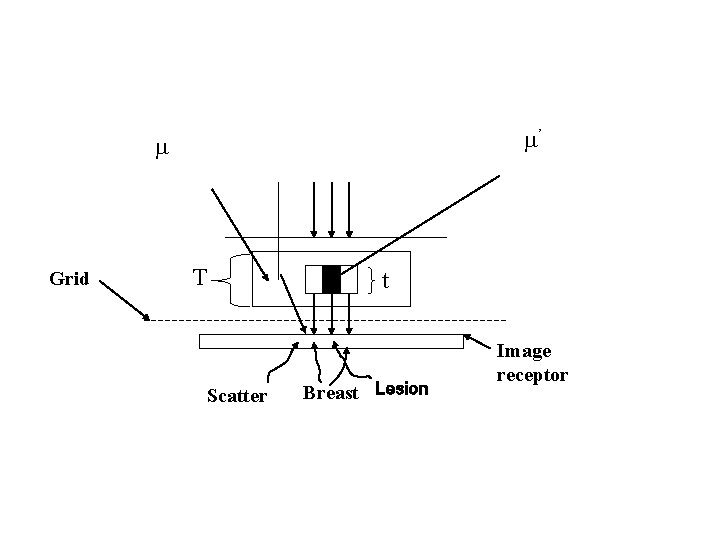
’ Grid T Scatter t Breast Lesion Image receptor
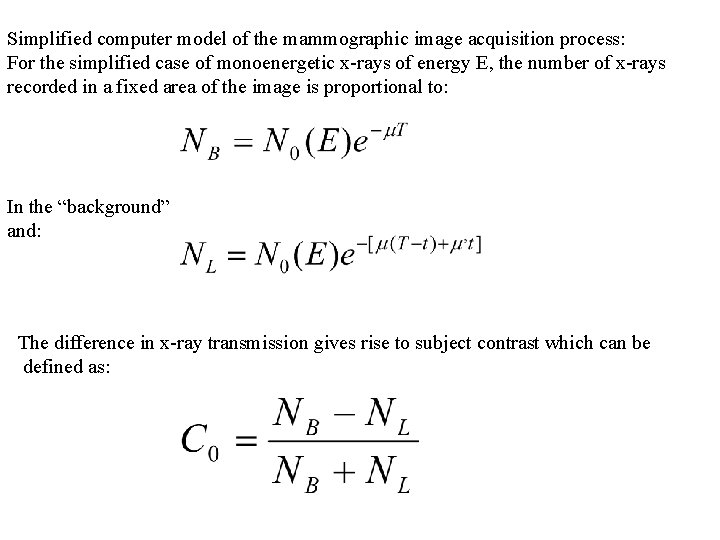
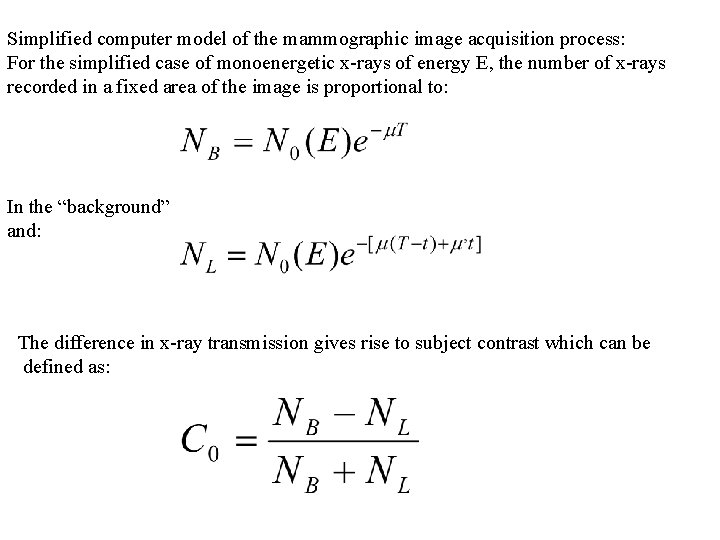
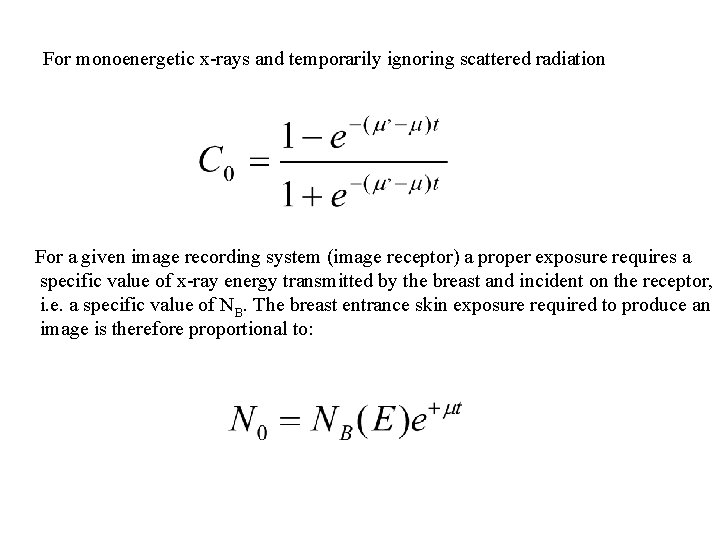
Simplified computer model of the mammographic image acquisition process: For the simplified case of monoenergetic x-rays of energy E, the number of x-rays recorded in a fixed area of the image is proportional to: In the “background” and: The difference in x-ray transmission gives rise to subject contrast which can be defined as:
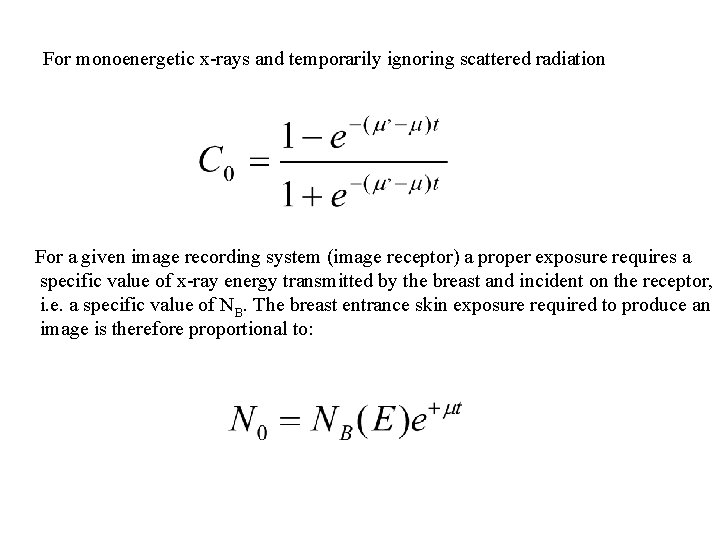
For monoenergetic x-rays and temporarily ignoring scattered radiation For a given image recording system (image receptor) a proper exposure requires a specific value of x-ray energy transmitted by the breast and incident on the receptor, i. e. a specific value of NB. The breast entrance skin exposure required to produce an image is therefore proportional to:
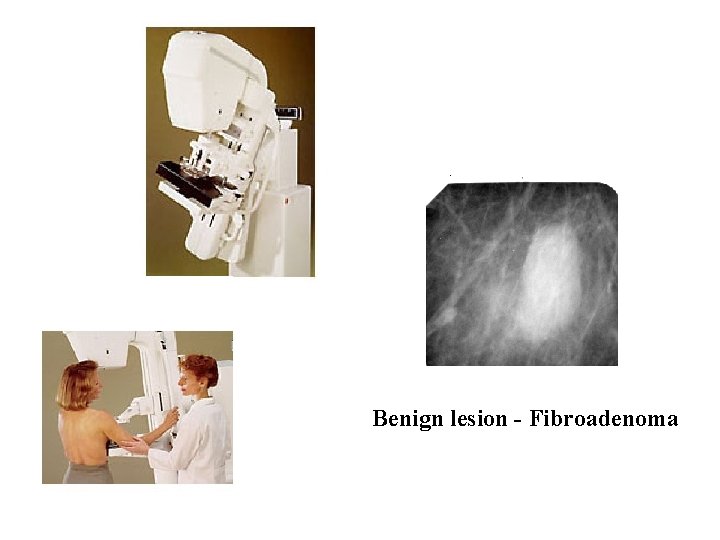
What Can Diagnostic Mammography Show? Diagnostic mammography may show that an abnormality (lesion) has a high likelihood of being benign (not cancer). For these, it is common to ask the woman to return earlier than usual for a recheck, usually in 6 months. A diagnostic mammogram may show that the abnormality is not worrisome at all and the woman can then return to routine yearly screening mammography. In some cases, patients with a cyst (fluid filled pocket) or other abnormality will also receive ultrasound imaging to obtain further diagnostic information. Finally, the diagnostic work-up may suggest that biopsy (tissue sampling) is needed to tell whether or not the abnormality is cancerous. A recommendation for biopsy does not necessarily mean that the abnormality is cancer. About 65% of all breast lesions that are evaluated with biopsy are found to be benign (non-cancerous) when evaluated under the microscope.
What Abnormalities Does Mammography Detect and Diagnose? Mammography is used to detect a number of abnormalities, the two main ones being calcifications and masses. Calcifications are tiny mineral deposits within the breast tissue that appear as small white spots on the films. Calcifications are divided into two categories, macrocalcifications and microcalcifications. A mass is any group of cells clustered together more densely than the surrounding tissue. A cyst or fluid collection may also appear as a mass on mammography. The difference between a solid mass and a cyst can often be shown with ultrasound.
Calcifications: Macrocalcifications are coarse (larger) calcium deposits that are often associated with fibrocystic change or with degenerative changes in the breasts, such as aging of the bre arteries, old injuries, or inflammation. Macrocalcification deposits are associated with benign (noncancerous) conditions and do not require a biopsy. Macrocalcifications are in about 50 % of women over the age of 50. Microcalcifications are tiny (less than 1/50 of an inch) specks of calcium in the breast. When many microcalcifications are seen in one area, they are referred to as a cluster an indicate a small cancer. About half of the cancers detected by mammography appear as of microcalcifications. Microcalcifications are the most common mammographic sign of ductal carcinoma in s (meaning the cancer has not spread or invade neighboring tissue). Almost 90% of cases of ductal carcinoma in situ are associated with microcalcifications. An area of microcalcifications seen on a mammogram does not always mean that is present. The shape and arrangement of microcalcifications help the radiologist the likelihood of cancer being present. In some cases, the microcalcifications do not indicate a need for a biopsy. Instead, a doctor may advise a follow-up mammogram with months. In other cases, the microcalcifications are more suspicious and a stereotactic bi is recommended. Only 17% of calcifications requiring biopsy are cancerous.
Masses: Another important change seen on a mammogram is the presence of a mass, wh may occur with or without associated calcifications. A mass is any group of cells clustered together more densely than the surrounding tissue. Masses can be due to many things, in cysts, which are non-cancerous collections of fluid in the breast. A cyst cannot be diagnos by physical exam alone nor can it be diagnosed by mammography alone, although certain can suggest the presence of a cyst or cysts. To confirm that a mass is a cyst, either breast ultrasound or aspiration with a needle is required. If a mass is not a cyst, then further imag may be obtained. As with calcifications, a mass can be caused by benign breast condition By breast cancer. Some masses can be monitored with periodic mammography while othe may require biopsy. The size, shape, and margins (edges) of the mass help the radiol in evaluating the likelihood of cancer. Breast ultrasound is often helpful. Prior mammog may help show that a mass is unchanged for many years, indicating a benign condition an helping to avoid unnecessary biopsy. Having prior mammograms available to the radiologi as discussed above, is very important. Mammography alone cannot prove that an abnormal area is cancer although some abnormalities are very characteristic of malignancy. If mammography raises a significant suspicion of cancer, tissue must be removed for examination under the microscope to tell if it is cancer. This can be done with one of several breast biopsy techniques. Ductography, also know as a Galactogram, is special type of contrast enhanced mammog used for imaging the breast ducts. Ductography can aid in diagnosing the cause of an abn nippledischarge and is valuable in diagnosing intraductal papillomas.
Digital Mammography One of the most recent advances in x-ray mammography is digital mammography. Digital (computerized) mammography is similar to standard mammography in that x-rays are use produce detailed images of the breast. Digital mammography uses essentially the same mammography system as conventional mammography, but the system is equipped with a receptor and a computer instead of a film cassette. Several studies have demonstrated th Mammography is at least as accurate as standard mammography. Digital spot view mammography allows faster and more accurate stereotactic biopsy. This in shorter examination times and significantly improved patient comfort and convenience s the time the patient must remain still is much shorter. With digital spot-view mammography images are acquired digitally and displayed immediately on the system monitor. Spot-view systems have been approved by the U. S. Food and Drug Administration (FDA) for use in g breast biopsy. Traditional stereotactic biopsy requires a mammogram film be exposed, dev and then reviewed, greatly increasing the time before the breast biopsy can be completed In addition to spot-view digital mammography, the FDA has recently approved a "full-field" digital mammography system to screen for and diagnose breast cancer. Currently, only ha copy printouts of the digital mammographic images maybe used by radiologists. With cont improvements, the "full-field" mammography systems may eventually replace traditional mammography.
How Does Digital Mammography Differ From Standard Mammography? In standard mammography, images are recorded on film using an x-ray cassette. The film viewed by the radiologist using a "light box" and then stored in a jacket in the facility’s arch With digital mammography, the breast image is captured using a special electronic x-ray detector, which converts the image into a digital picture for review on a computer mo The digital mammogram is then stored on a computer. With digital mammography, the magnification, orientation, brightness, and contrast of the image may be altered after the e completed to help the radiologist more clearly see certain areas. Digital mammography provides many benefits over standard mammography equipment. These benefits include: • faster image acquisition • shorter exam time • easier image storage • physician manipulation of breast images for more accurate detection of breast cancer • transmittal of images over phone lines or a computer network for remote consultati other physicians Digital mammography has the potential to significantly reduce the amount of time required acquire a mammogram from 10 to 15 minutes to less than a minute. This will provide a sh more comfortable exam for the woman and possibly allow mammography facilities to cond more mammograms in a day. Digital images can also be manipulated to correct for under over exposure. If under or over exposure occurs with a standard film-based mammograph System women have to undergo a repeat mammogram before leaving the facility.
Many radiologists support digital mammography as an effective tool to screen for breast cancer. The contrast resolution of these devices is inherently better, "In addition, the extra features digital mammography will ultimately provide, such as telemammography, tomosynthesis, a computer-aided diagnosis will prove invaluable to patients and their doctors, ” Telemammography (also called teleradiology) allows radiologists to share digital images vi phone or network connection for remote consultation with other physicians; tomosynthesis allows radiologists to add or subtract digital mammography images using a computer workstation for enhanced diagnostic capability. Computer-aided detection (CAD) was approved by the FDA in June 1999. CAD helps radiologists more accurately detect breast cancer by marking suspicious areas on digitized mammograms. Promising Developments in Digital Mammography The FDA has approved the first "full-field" digital mammography scanner to screen for and diagnose breast cancer in February 2000. Before applying for FDA certification, data was gathered from 662 patients at four institutions: the University of Colorado, the University of Massachusetts Medical Center, Massachusetts General Hospital, and the Hospital of th University of Pennsylvania. The data compared hard copies of digital breast images on film conventional mammography films finding that digital mammography is as effective at detec breast cancer as standard film mammograms. A separate study revealed that the digital mammography scanner showed a slight advantage in the visibility of breast tissue at the sk
Disadvantages to Digital Mammography While digital mammography is quite promising, it still has additional hurdles to undergo b it replaces conventional mammography. Digital mammography must: provide higher detail resolution (as standard mammography does) become less expensive (currently several times more costly than conventional mammography) provide a method to efficiently compare digital mammogram images with existing mammography films on computer monitors Standard mammography using film cassettes has the benefit of providing very high deta resolution (image sharpness), which is especially useful for imaging microcalcifications (tiny calcium deposits) and very small abnormalities that may indicate early breast cancer. While full-field digital mammography may lack the spatial resolution of film, clinic trials have shown digital mammography to be at least equivalent to standard film screeni mammography. This is because digital mammography has the benefit of providing impro contrast resolution, which may make abnormalities easier to see. Various manufacturers trying to develop digital mammography systems with detail resolution equivalent to standard film mammography while also providing the benefits of digital mammography n above. The high cost of digital mammography is a major obstacle. Digital mammography system costs roughly four to five times as much as standard mammography equipment. Standar mammography systemsare currently installed in over 10, 000 locations across the United It may take years for this current equipment to be updated or replaced and for digital mammography to become widespread after its approval by the FDA.
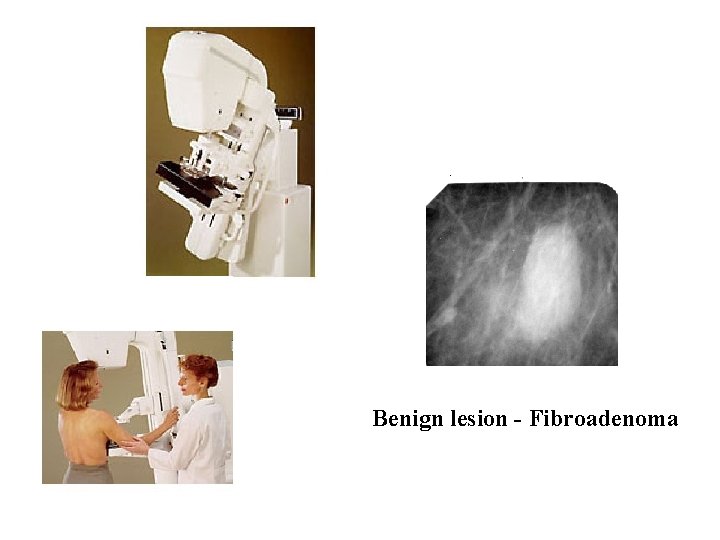
Benign lesion - Fibroadenoma
Computerized Tomography Imaging of a cross sectional slice of the body using X-rays. Invented by Dr. G. N. Housfield in 1971. Received the Nobel prize in medicine in 1979. The method is constructing images from large number of measurements of x-ray transmission through the patient. The resulting images are tomographic maps of the X-ray linear attenuation coefficient.
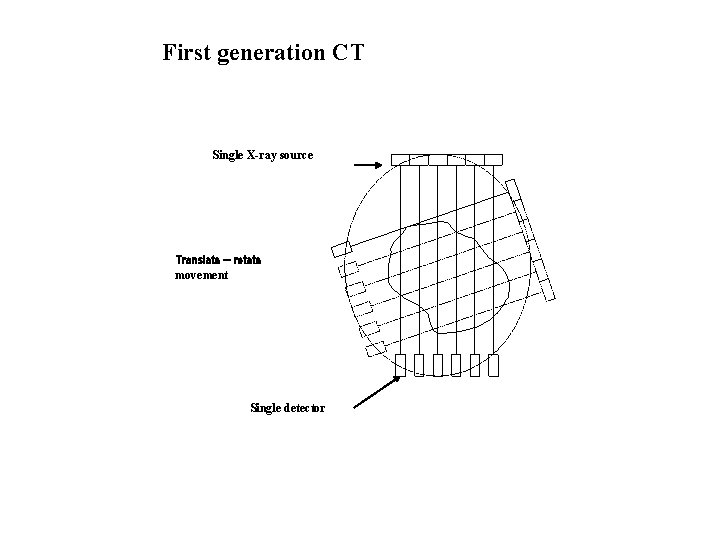
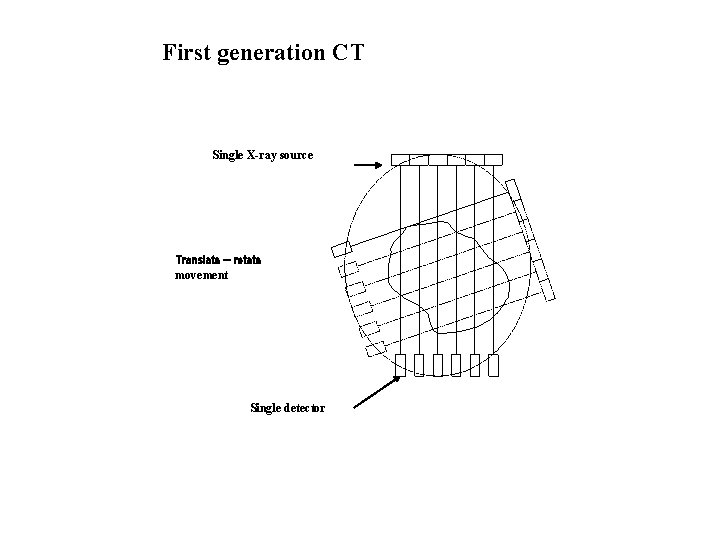
First generation CT Single X-ray source Translate – rotate movement Single detector
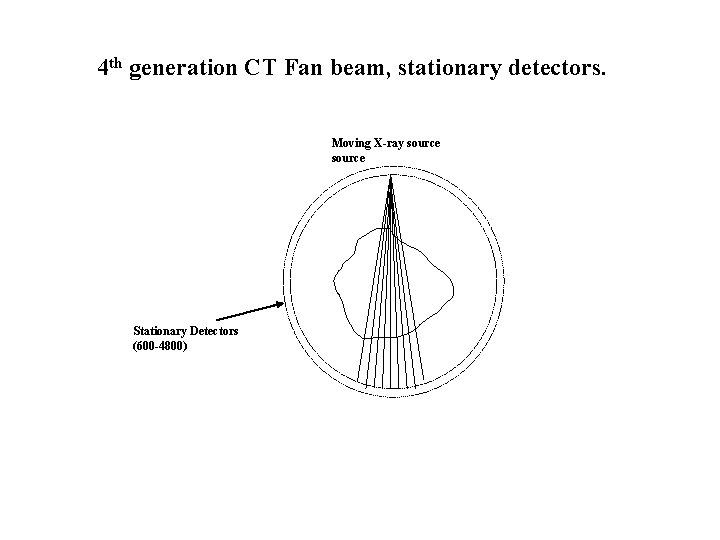
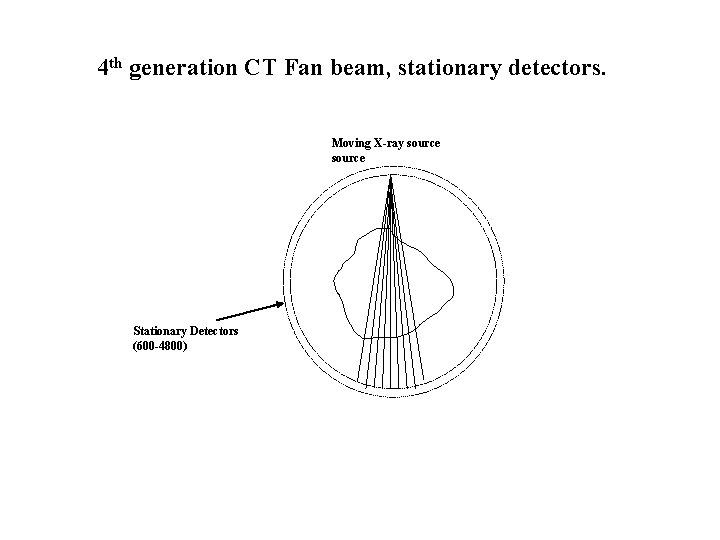
4 th generation CT Fan beam, stationary detectors. Moving X-ray source Stationary Detectors (600 -4800)
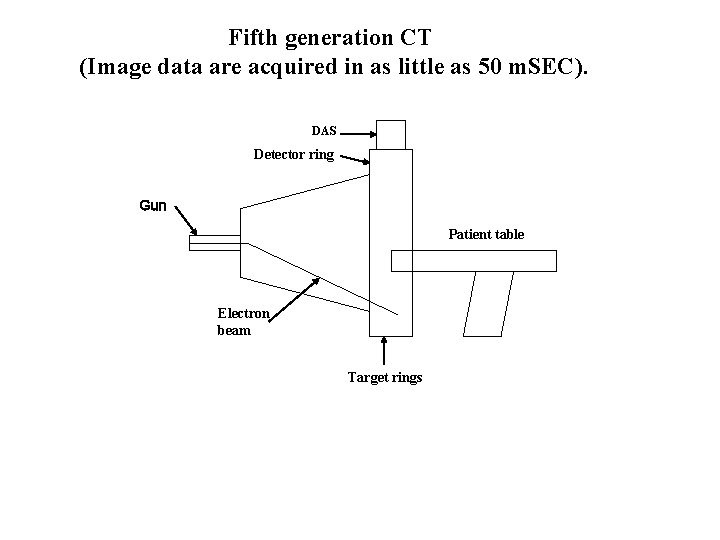
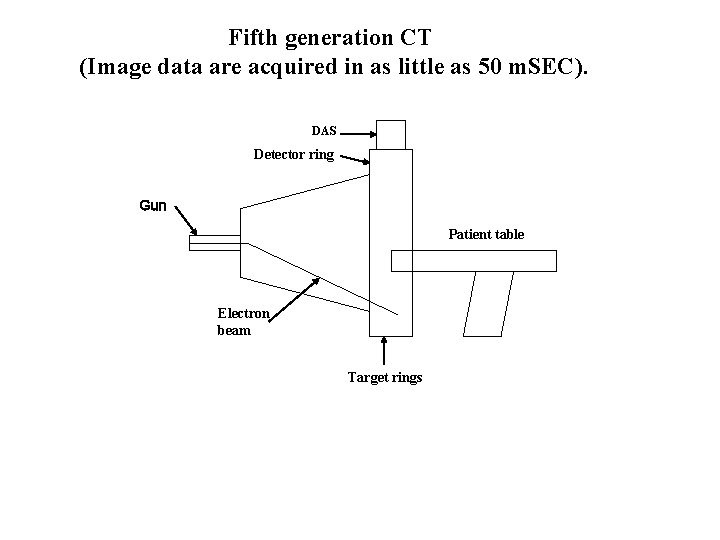
Fifth generation CT (Image data are acquired in as little as 50 m. SEC). DAS Detector ring Gun Patient table Electron beam Target rings
CT (by Picker) Colonoscopy with spiral CT Spiral scan
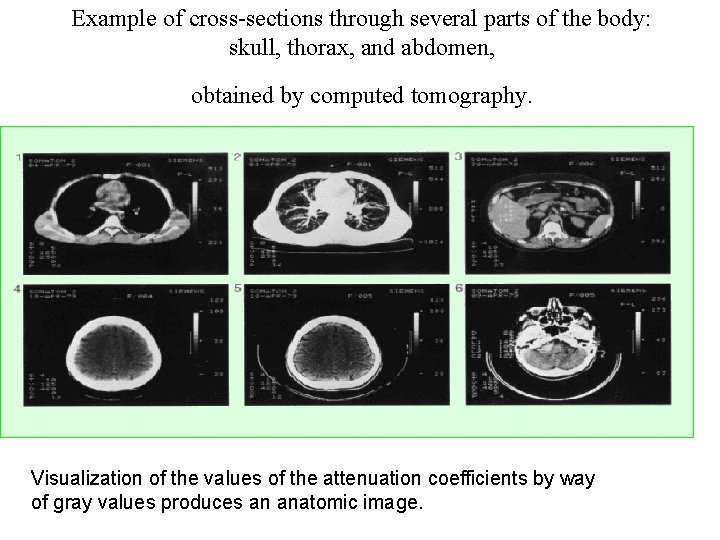
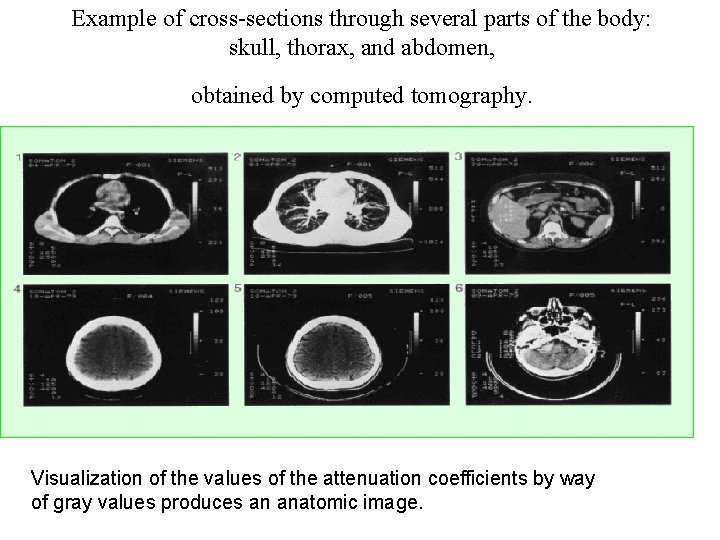
Example of cross-sections through several parts of the body: skull, thorax, and abdomen, obtained by computed tomography. Visualization of the values of the attenuation coefficients by way of gray values produces an anatomic image.
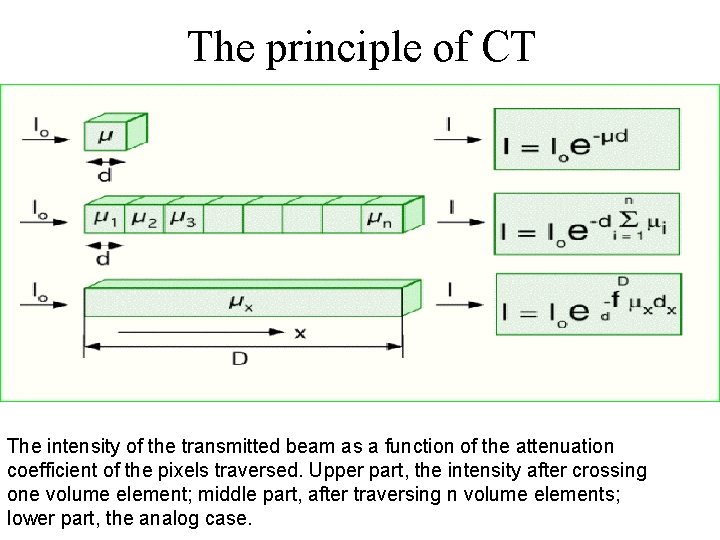
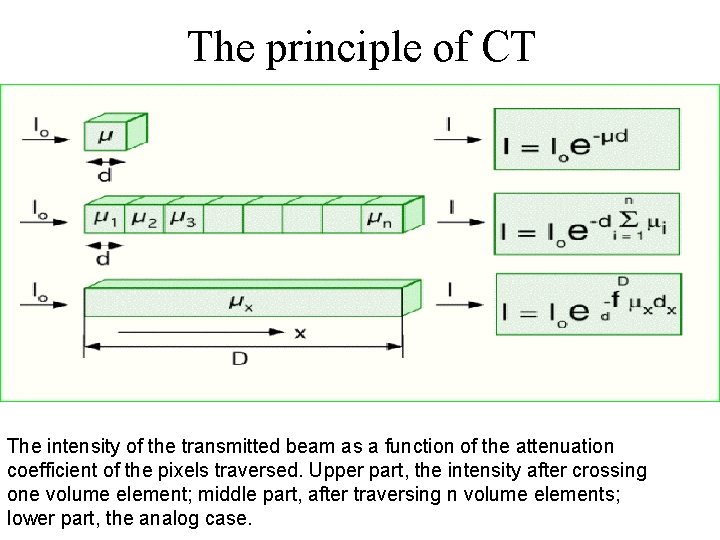
The principle of CT The intensity of the transmitted beam as a function of the attenuation coefficient of the pixels traversed. Upper part, the intensity after crossing one volume element; middle part, after traversing n volume elements; lower part, the analog case.
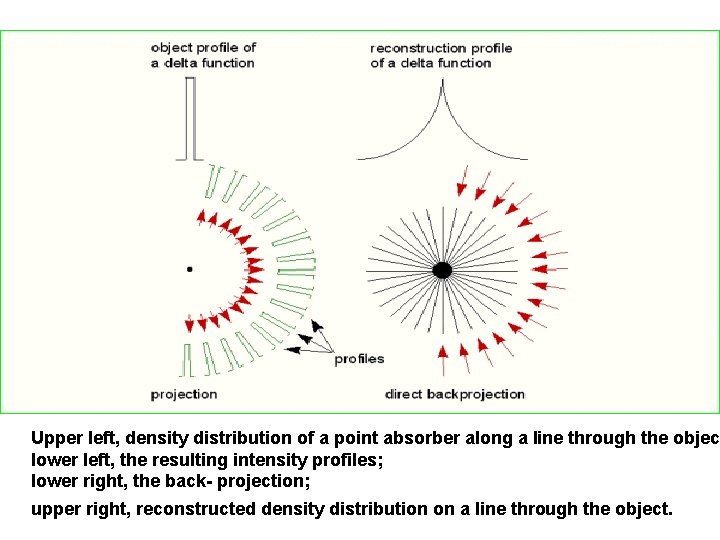
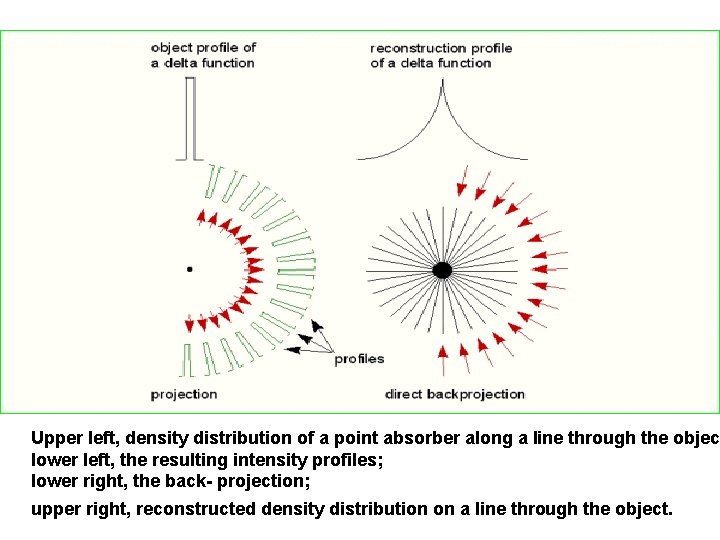
Upper left, density distribution of a point absorber along a line through the objec lower left, the resulting intensity profiles; lower right, the back- projection; upper right, reconstructed density distribution on a line through the object.
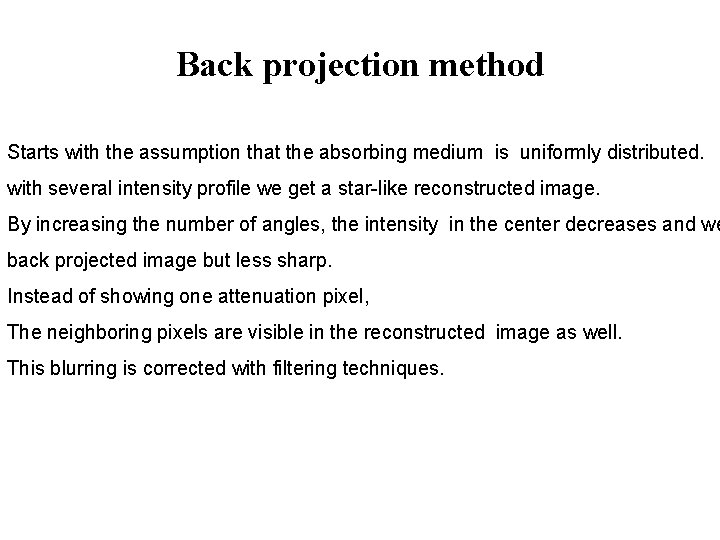
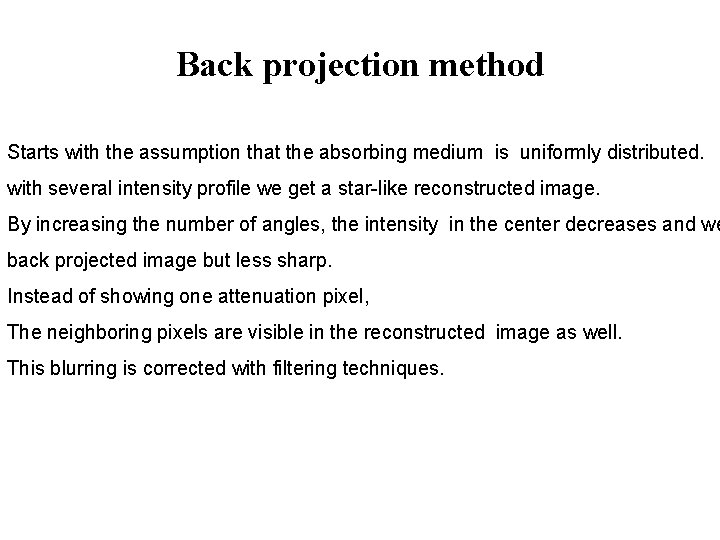
Back projection method Starts with the assumption that the absorbing medium is uniformly distributed. with several intensity profile we get a star-like reconstructed image. By increasing the number of angles, the intensity in the center decreases and we back projected image but less sharp. Instead of showing one attenuation pixel, The neighboring pixels are visible in the reconstructed image as well. This blurring is corrected with filtering techniques.
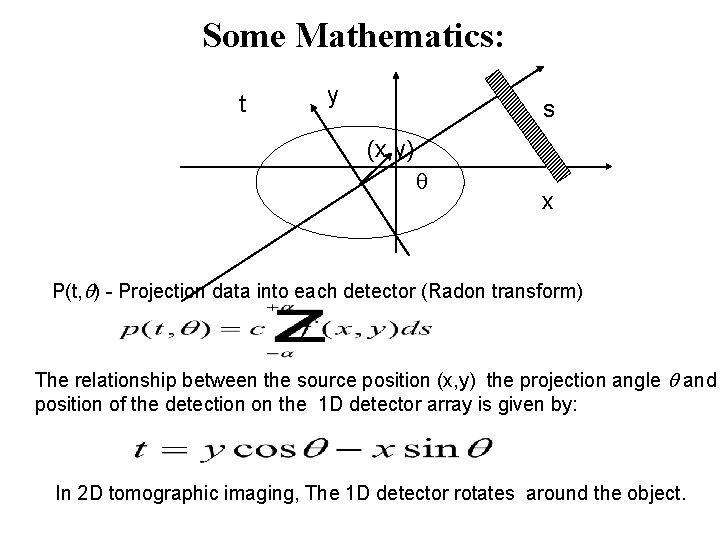
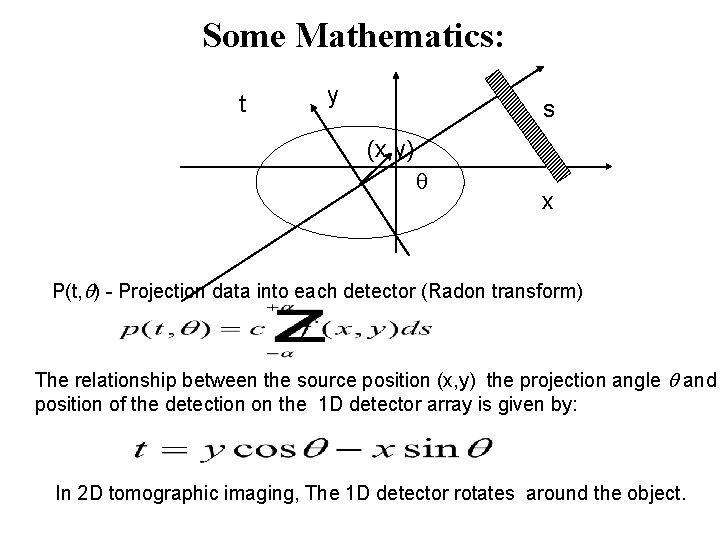
Some Mathematics: t y s (x, y) x P(t, ) - Projection data into each detector (Radon transform) The relationship between the source position (x, y) the projection angle and position of the detection on the 1 D detector array is given by: In 2 D tomographic imaging, The 1 D detector rotates around the object.
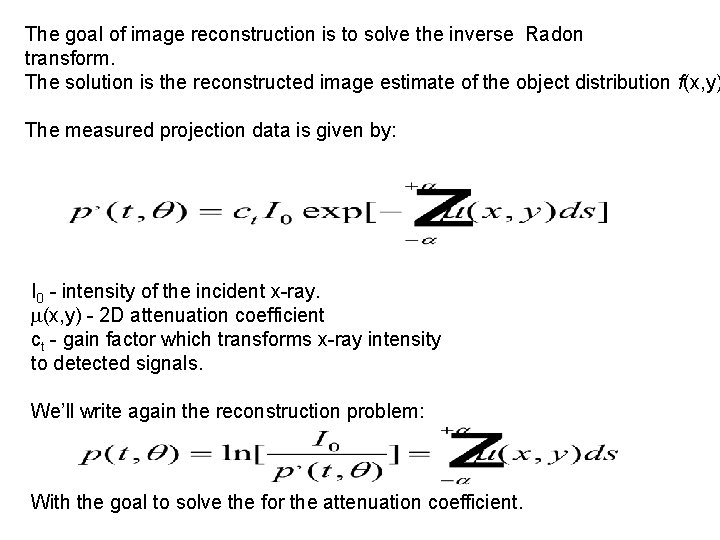
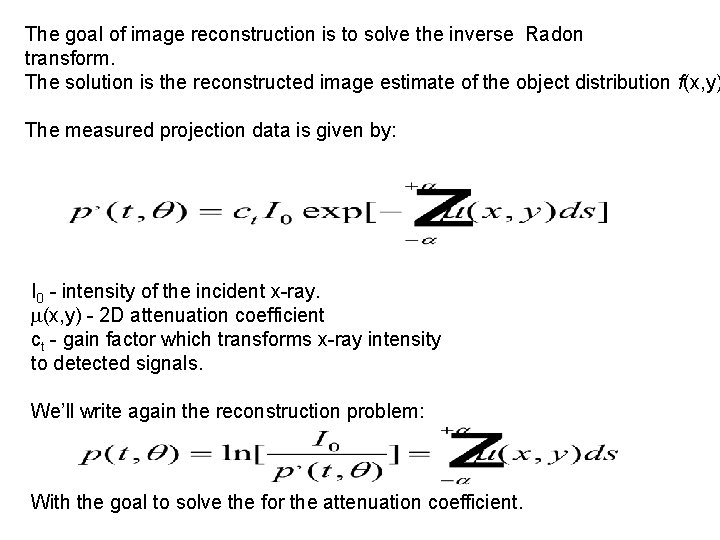
The goal of image reconstruction is to solve the inverse Radon transform. The solution is the reconstructed image estimate of the object distribution f(x, y) The measured projection data is given by: I 0 - intensity of the incident x-ray. (x, y) - 2 D attenuation coefficient ct - gain factor which transforms x-ray intensity to detected signals. We’ll write again the reconstruction problem: With the goal to solve the for the attenuation coefficient.
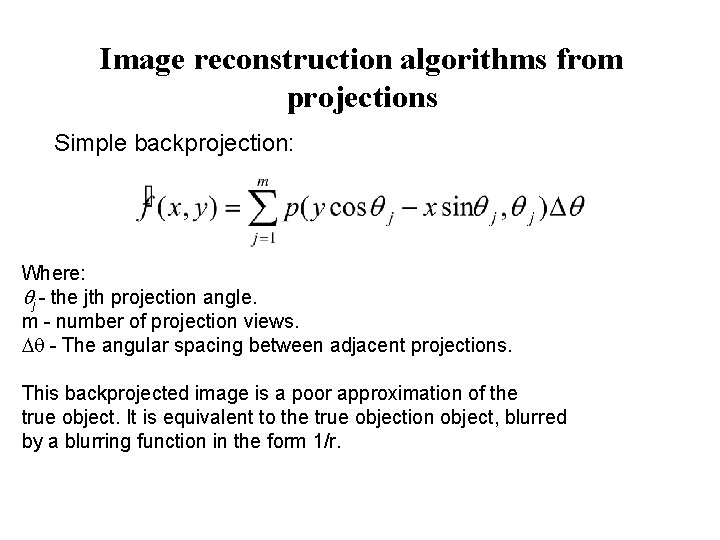
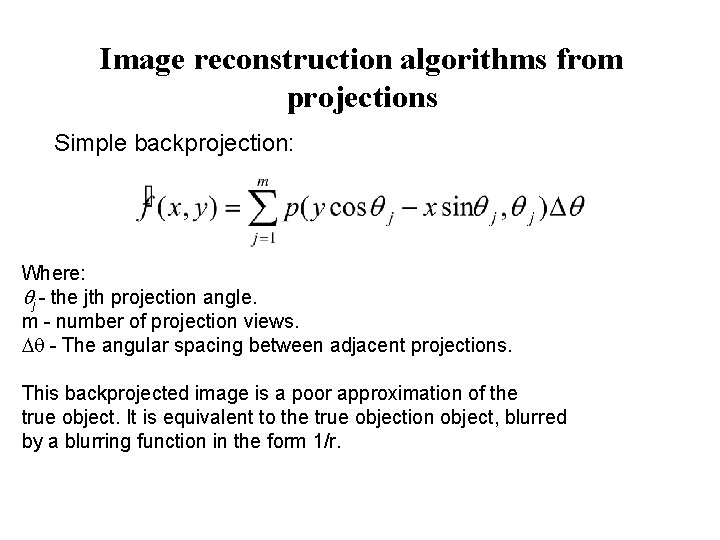
Image reconstruction algorithms from projections Simple backprojection: Where: j - the jth projection angle. m - number of projection views. - The angular spacing between adjacent projections. This backprojected image is a poor approximation of the true object. It is equivalent to the true objection object, blurred by a blurring function in the form 1/r.
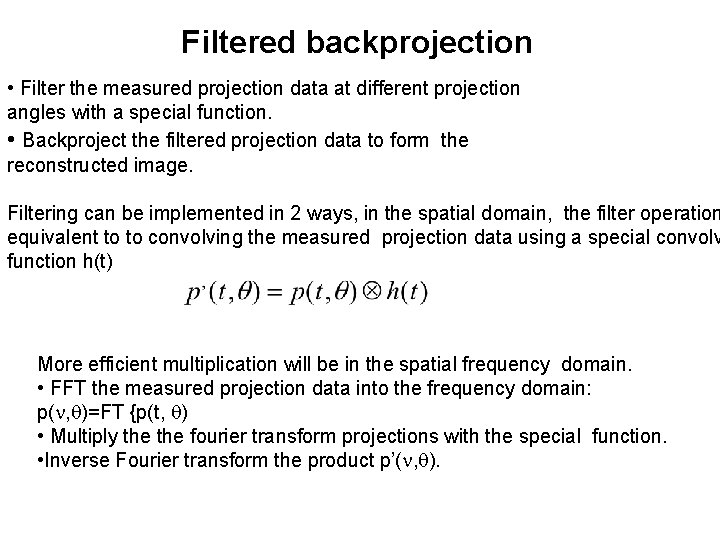
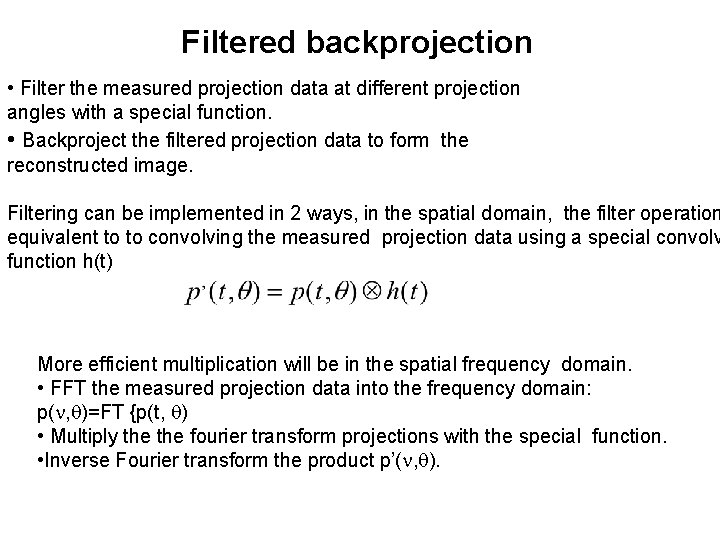
Filtered backprojection • Filter the measured projection data at different projection angles with a special function. • Backproject the filtered projection data to form the reconstructed image. Filtering can be implemented in 2 ways, in the spatial domain, the filter operation equivalent to to convolving the measured projection data using a special convolv function h(t) More efficient multiplication will be in the spatial frequency domain. • FFT the measured projection data into the frequency domain: p( , )=FT {p(t, ) • Multiply the fourier transform projections with the special function. • Inverse Fourier transform the product p’( , ).
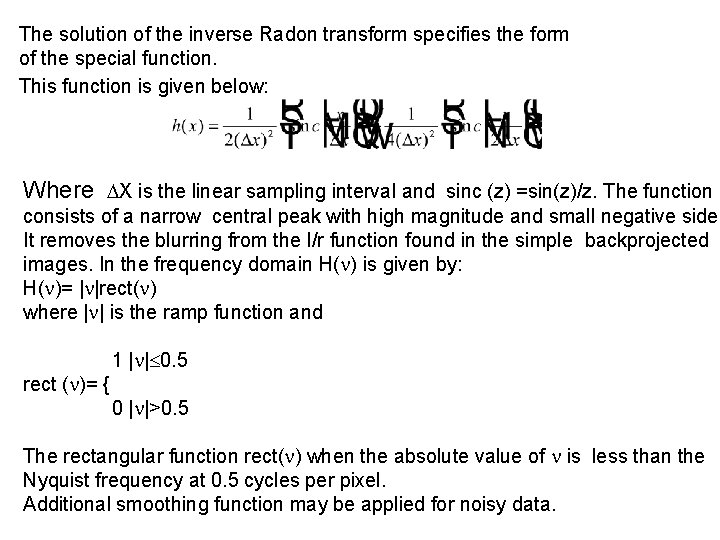
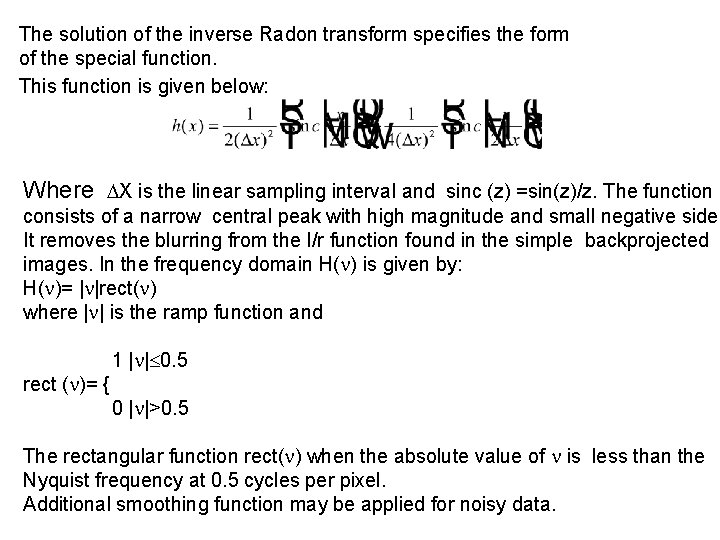
The solution of the inverse Radon transform specifies the form of the special function. This function is given below: Where X is the linear sampling interval and sinc (z) =sin(z)/z. The function h consists of a narrow central peak with high magnitude and small negative side It removes the blurring from the I/r function found in the simple backprojected images. In the frequency domain H( ) is given by: H( )= | |rect( ) where | | is the ramp function and 1 | | 0. 5 rect ( )= { 0 | |>0. 5 The rectangular function rect( ) when the absolute value of is less than the Nyquist frequency at 0. 5 cycles per pixel. Additional smoothing function may be applied for noisy data.
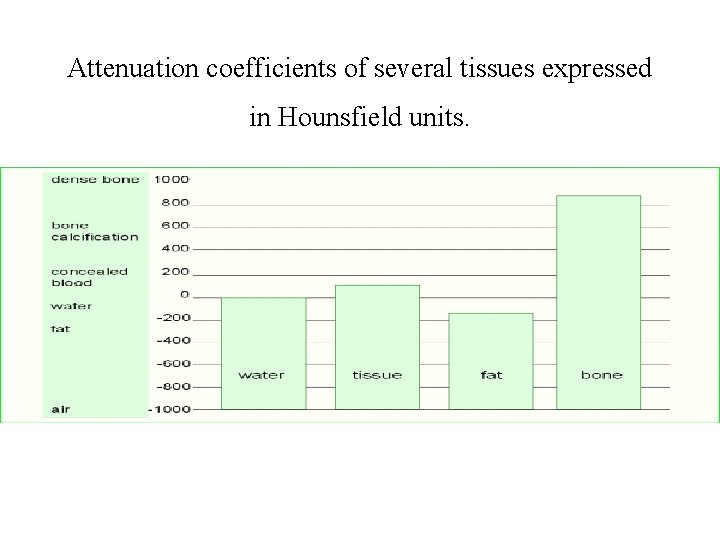
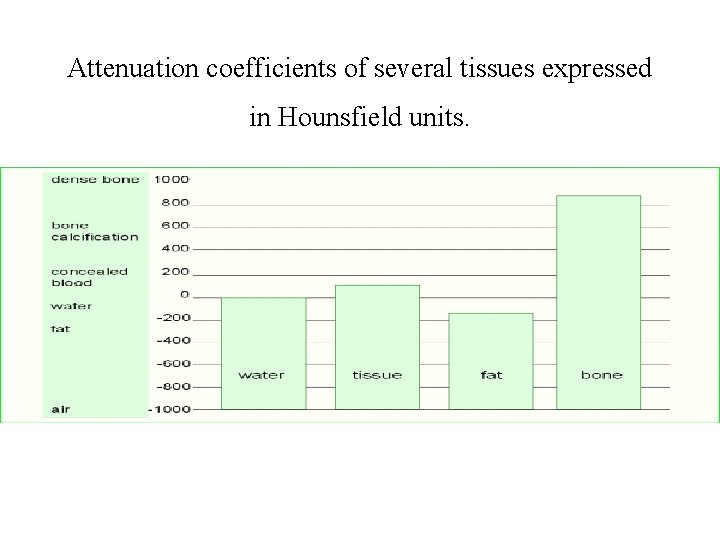
Attenuation coefficients of several tissues expressed in Hounsfield units.
Magnetic resonance imaging (MRI)
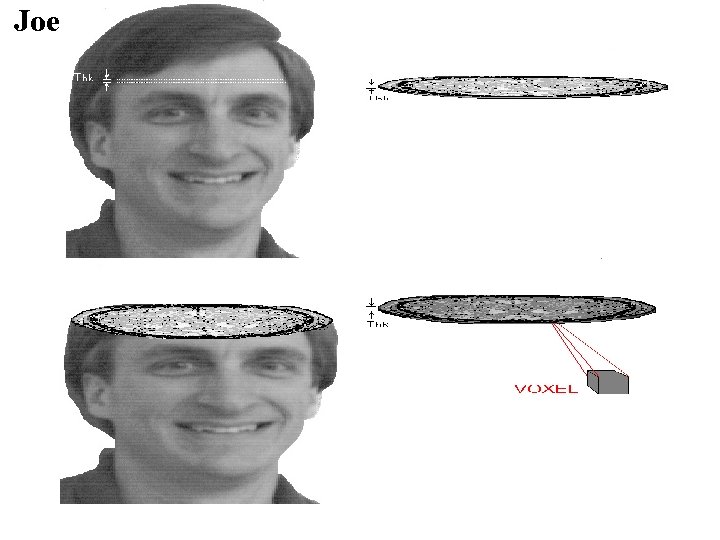
Joe

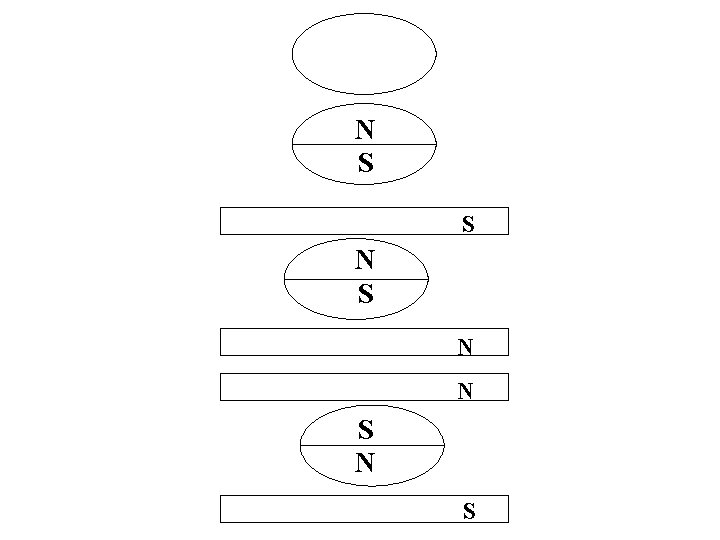
N S S N N S

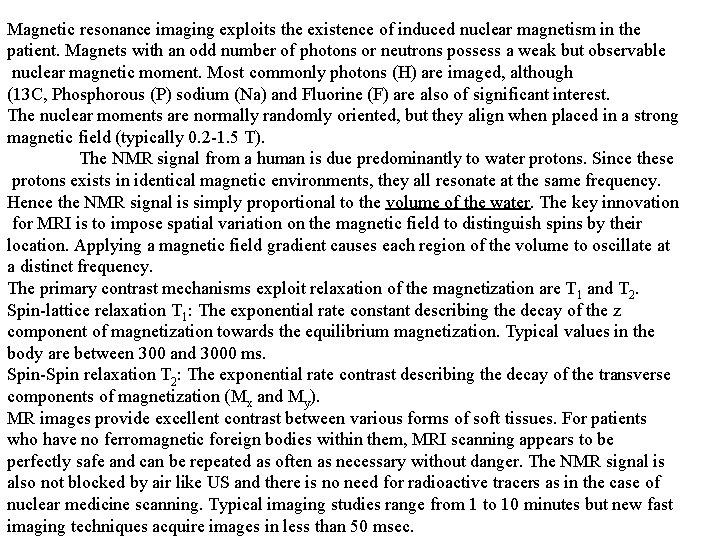
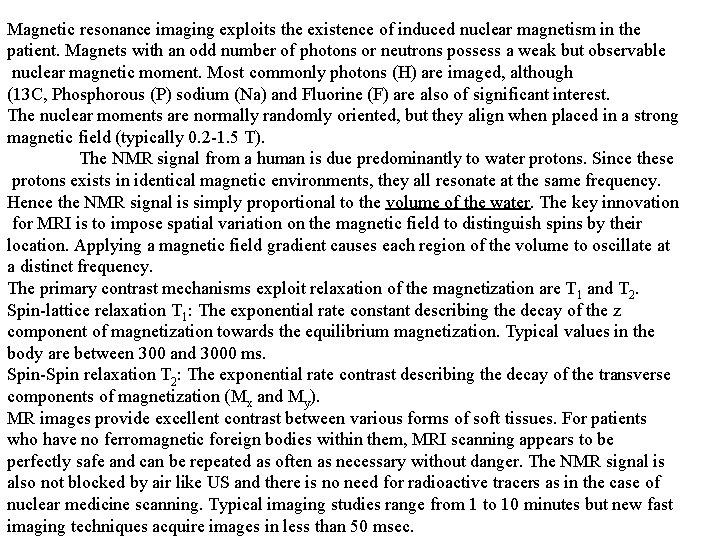
Magnetic resonance imaging exploits the existence of induced nuclear magnetism in the patient. Magnets with an odd number of photons or neutrons possess a weak but observable nuclear magnetic moment. Most commonly photons (H) are imaged, although (13 C, Phosphorous (P) sodium (Na) and Fluorine (F) are also of significant interest. The nuclear moments are normally randomly oriented, but they align when placed in a strong magnetic field (typically 0. 2 -1. 5 T). The NMR signal from a human is due predominantly to water protons. Since these protons exists in identical magnetic environments, they all resonate at the same frequency. Hence the NMR signal is simply proportional to the volume of the water. The key innovation for MRI is to impose spatial variation on the magnetic field to distinguish spins by their location. Applying a magnetic field gradient causes each region of the volume to oscillate at a distinct frequency. The primary contrast mechanisms exploit relaxation of the magnetization are T 1 and T 2. Spin-lattice relaxation T 1: The exponential rate constant describing the decay of the z component of magnetization towards the equilibrium magnetization. Typical values in the body are between 300 and 3000 ms. Spin-Spin relaxation T 2: The exponential rate contrast describing the decay of the transverse components of magnetization (Mx and My). MR images provide excellent contrast between various forms of soft tissues. For patients who have no ferromagnetic foreign bodies within them, MRI scanning appears to be perfectly safe and can be repeated as often as necessary without danger. The NMR signal is also not blocked by air like US and there is no need for radioactive tracers as in the case of nuclear medicine scanning. Typical imaging studies range from 1 to 10 minutes but new fast imaging techniques acquire images in less than 50 msec.

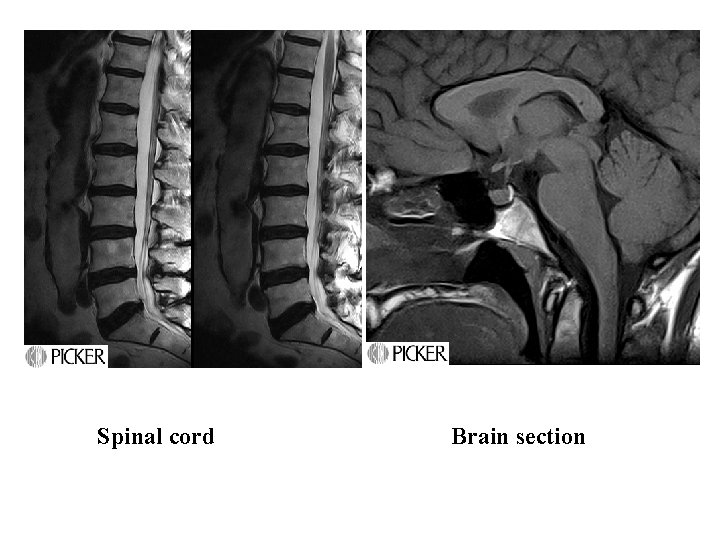
MRI by Picker
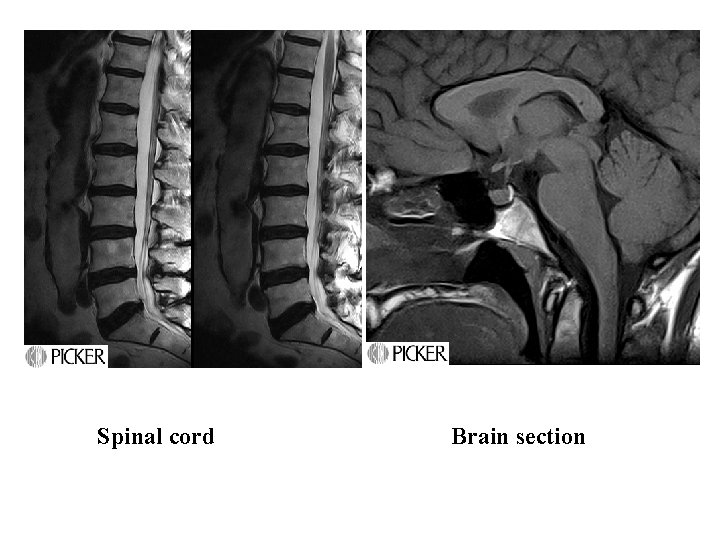
Spinal cord Brain section
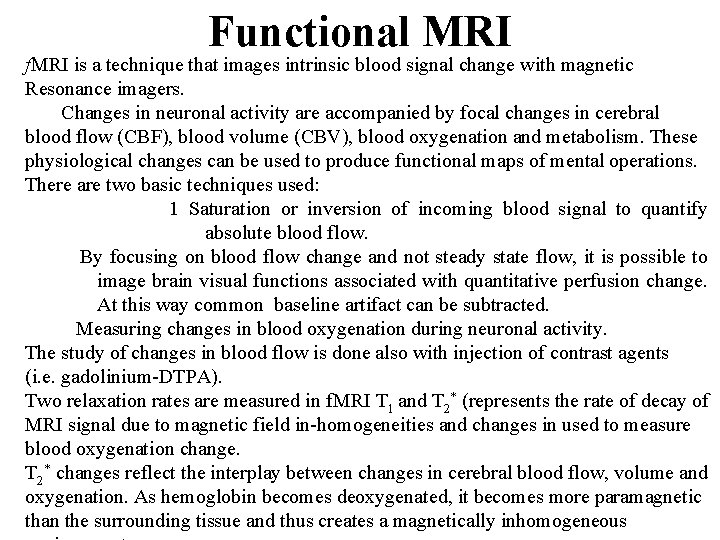
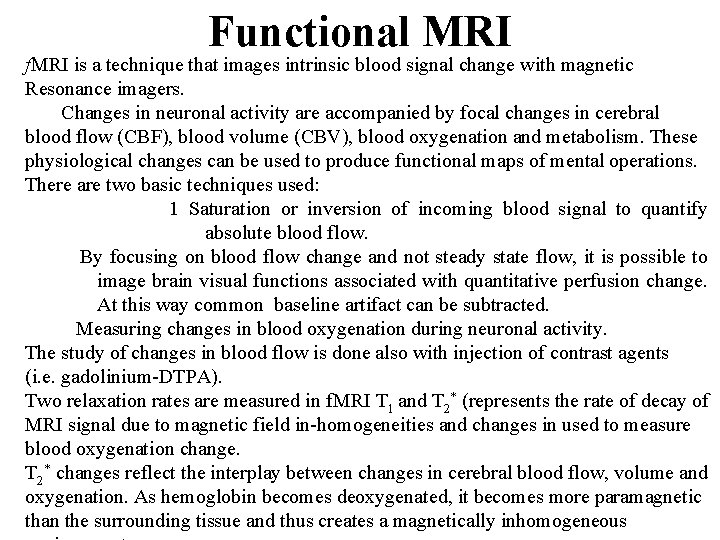
Functional MRI f. MRI is a technique that images intrinsic blood signal change with magnetic Resonance imagers. Changes in neuronal activity are accompanied by focal changes in cerebral blood flow (CBF), blood volume (CBV), blood oxygenation and metabolism. These physiological changes can be used to produce functional maps of mental operations. There are two basic techniques used: 1 Saturation or inversion of incoming blood signal to quantify absolute blood flow. By focusing on blood flow change and not steady state flow, it is possible to image brain visual functions associated with quantitative perfusion change. At this way common baseline artifact can be subtracted. Measuring changes in blood oxygenation during neuronal activity. The study of changes in blood flow is done also with injection of contrast agents (i. e. gadolinium-DTPA). Two relaxation rates are measured in f. MRI T 1 and T 2* (represents the rate of decay of MRI signal due to magnetic field in-homogeneities and changes in used to measure blood oxygenation change. T 2* changes reflect the interplay between changes in cerebral blood flow, volume and oxygenation. As hemoglobin becomes deoxygenated, it becomes more paramagnetic than the surrounding tissue and thus creates a magnetically inhomogeneous
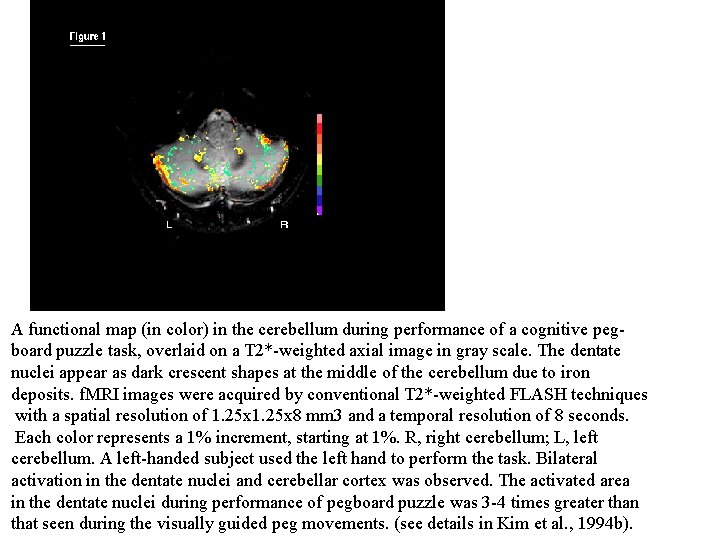
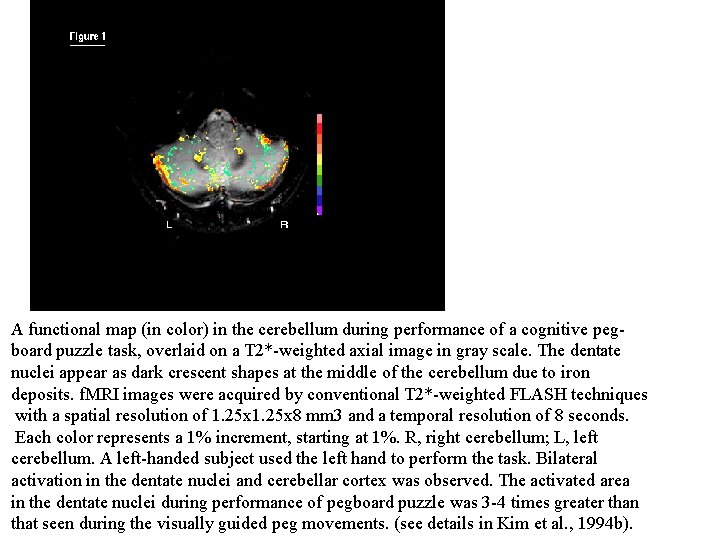
A functional map (in color) in the cerebellum during performance of a cognitive pegboard puzzle task, overlaid on a T 2*-weighted axial image in gray scale. The dentate nuclei appear as dark crescent shapes at the middle of the cerebellum due to iron deposits. f. MRI images were acquired by conventional T 2*-weighted FLASH techniques with a spatial resolution of 1. 25 x 8 mm 3 and a temporal resolution of 8 seconds. Each color represents a 1% increment, starting at 1%. R, right cerebellum; L, left cerebellum. A left-handed subject used the left hand to perform the task. Bilateral activation in the dentate nuclei and cerebellar cortex was observed. The activated area in the dentate nuclei during performance of pegboard puzzle was 3 -4 times greater than that seen during the visually guided peg movements. (see details in Kim et al. , 1994 b).
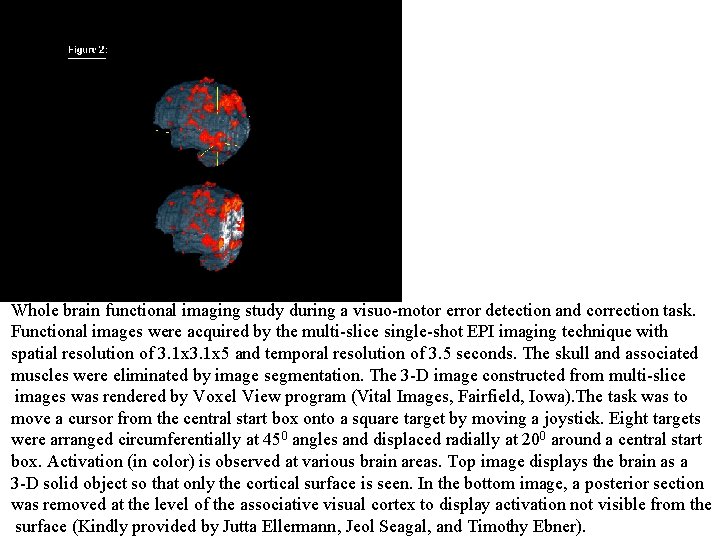
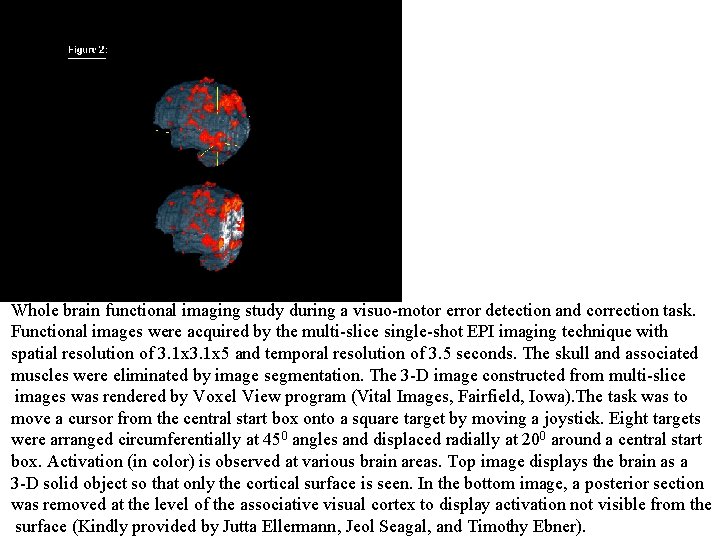
Whole brain functional imaging study during a visuo-motor error detection and correction task. Functional images were acquired by the multi-slice single-shot EPI imaging technique with spatial resolution of 3. 1 x 5 and temporal resolution of 3. 5 seconds. The skull and associated muscles were eliminated by image segmentation. The 3 -D image constructed from multi-slice images was rendered by Voxel View program (Vital Images, Fairfield, Iowa). The task was to move a cursor from the central start box onto a square target by moving a joystick. Eight targets were arranged circumferentially at 450 angles and displaced radially at 200 around a central start box. Activation (in color) is observed at various brain areas. Top image displays the brain as a 3 -D solid object so that only the cortical surface is seen. In the bottom image, a posterior section was removed at the level of the associative visual cortex to display activation not visible from the surface (Kindly provided by Jutta Ellermann, Jeol Seagal, and Timothy Ebner).
Open MRI units
Nuclear Imaging Use of G rays, Radionuclides and Radiopharmaceuticals in medical imaging.
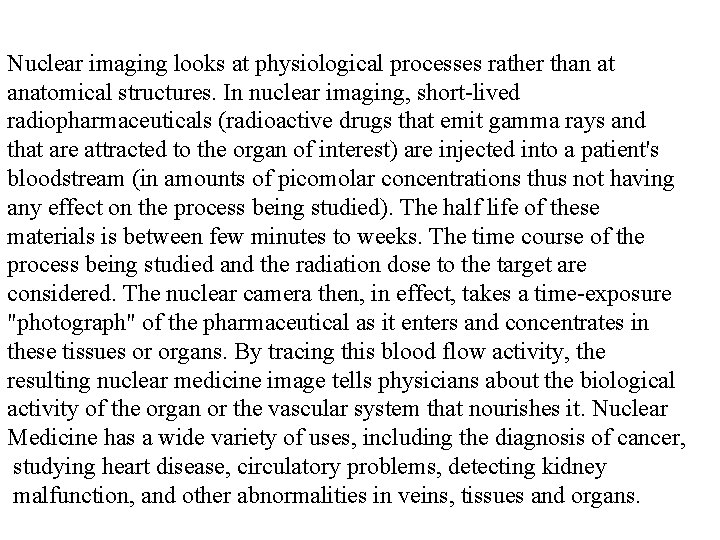
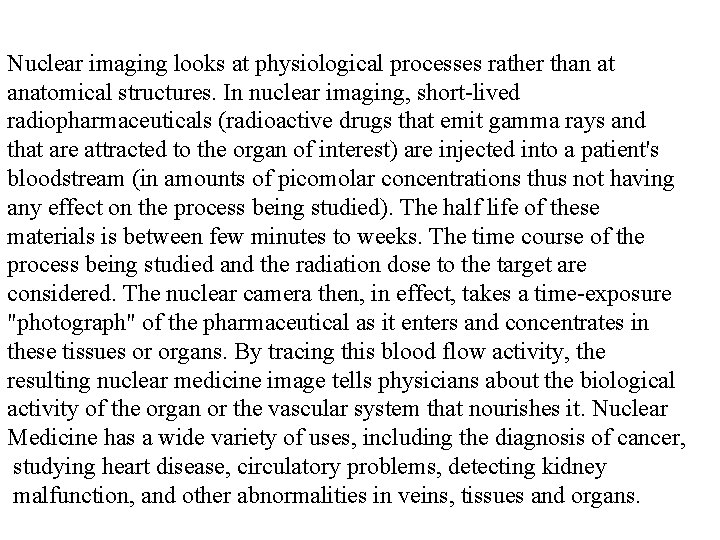
Nuclear imaging looks at physiological processes rather than at anatomical structures. In nuclear imaging, short-lived radiopharmaceuticals (radioactive drugs that emit gamma rays and that are attracted to the organ of interest) are injected into a patient's bloodstream (in amounts of picomolar concentrations thus not having any effect on the process being studied). The half life of these materials is between few minutes to weeks. The time course of the process being studied and the radiation dose to the target are considered. The nuclear camera then, in effect, takes a time-exposure "photograph" of the pharmaceutical as it enters and concentrates in these tissues or organs. By tracing this blood flow activity, the resulting nuclear medicine image tells physicians about the biological activity of the organ or the vascular system that nourishes it. Nuclear Medicine has a wide variety of uses, including the diagnosis of cancer, studying heart disease, circulatory problems, detecting kidney malfunction, and other abnormalities in veins, tissues and organs.
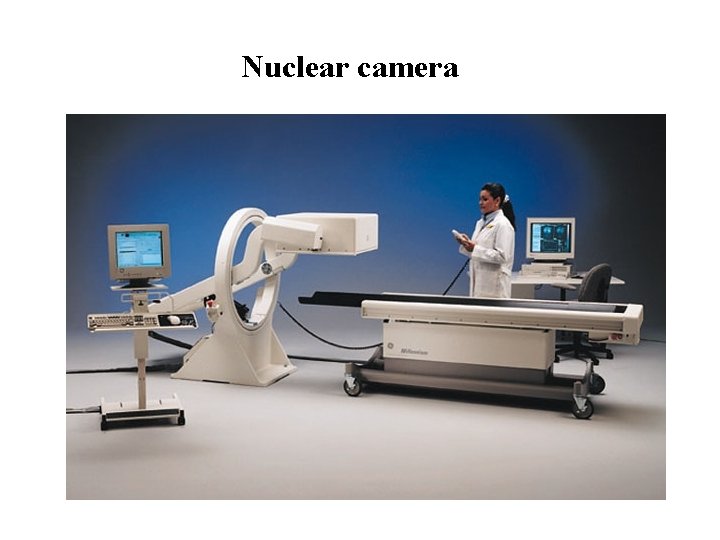
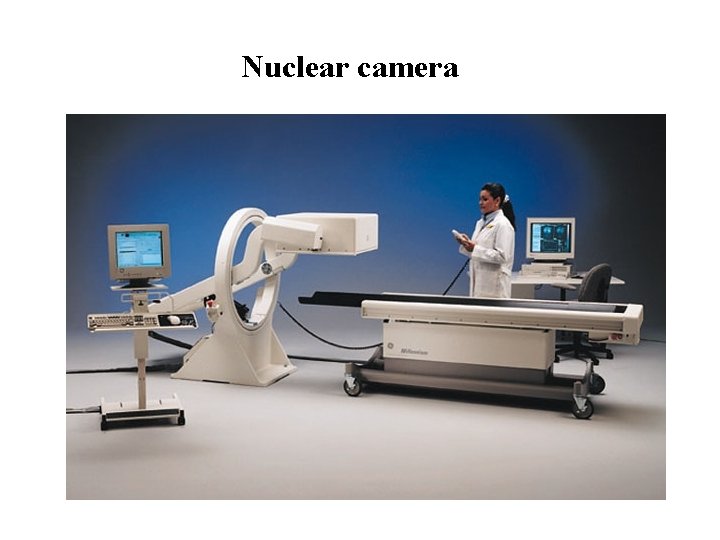
Nuclear camera
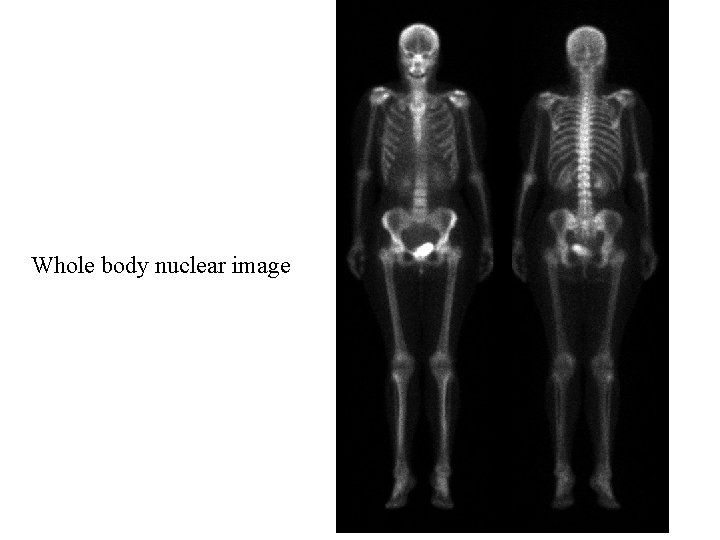
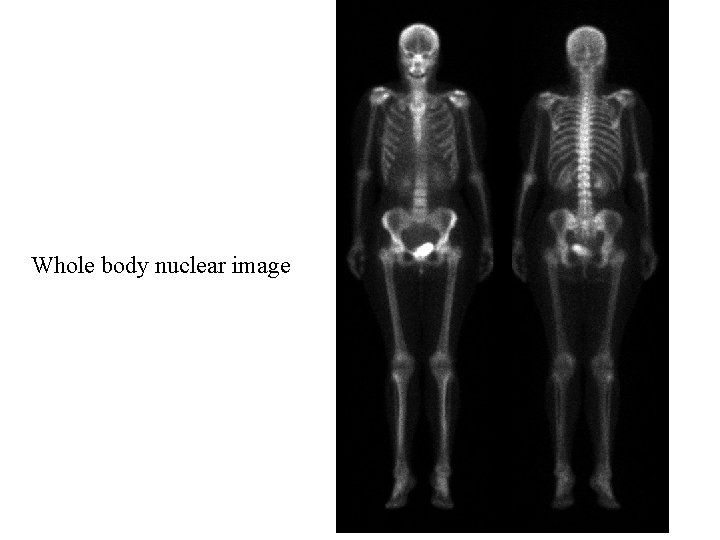
Whole body nuclear image
SPECT (single photon emission computerized tomography SPECT is based on the conventional nuclear imaging technique and tomographic reconstruction methods.
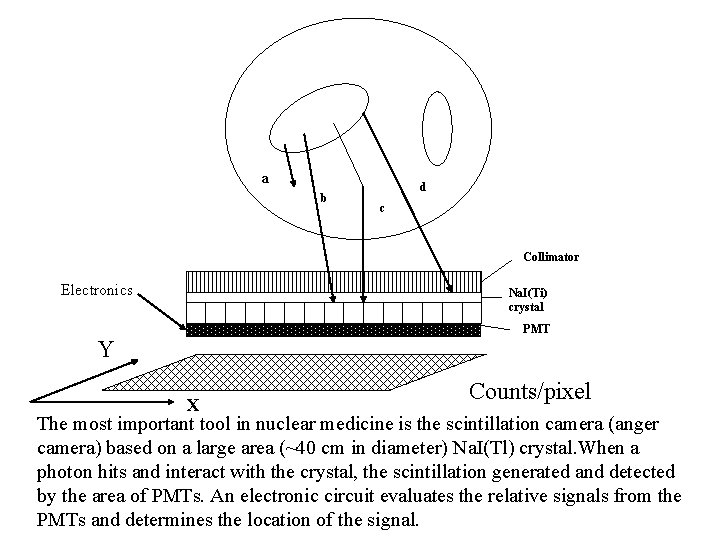
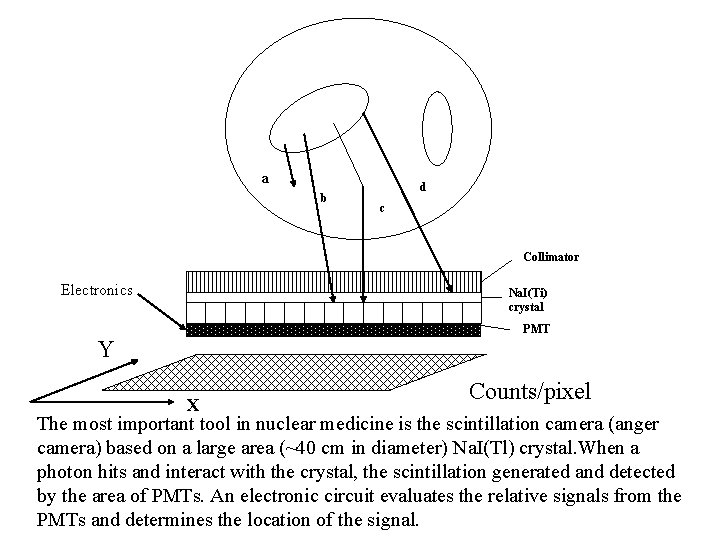
a b d c Collimator Electronics Na. I(Ti) crystal PMT Y X Counts/pixel The most important tool in nuclear medicine is the scintillation camera (anger camera) based on a large area (~40 cm in diameter) Na. I(Tl) crystal. When a photon hits and interact with the crystal, the scintillation generated and detected by the area of PMTs. An electronic circuit evaluates the relative signals from the PMTs and determines the location of the signal.
Performance characteristics of Nuclear Imaging Systems Spatial resolution - A measure for the degree of detail the final reconstructed image provides and hence the size of lesions that m potentially be detected. In other words: how fine the details are that be separated. Sensitivity, dead time - describes how well the radioactive decays tracer distribution are exploited to form image counts. A source radiated isotropically into all directions. The camera collec part that is entering into its solid angle less the photon which will impinge the collimators. Some of the events are lost because the system is still processing a previous event (dead time).
Signal to Noise ratio (SNR) - The relative strength of the informatio and the noise. If the lesion is small compared with the spatial resol the contrast is reduced because the high lesion activity blurred int neighborhood by the detector response. Uniformity, Linearity - The image of an object should be independe of its position in the field of view. This is not true in real systems. This can be assessed in calibration measurements to derive correc factors. This reduces non-uniformity from 10% to 3%.
The conventional nuclear medicine imaging process. Typical radionuclides used are 140 Ke. V Tc-99 m and 70 Ke. V photons from Tl-201. The gamma ray photons emitted from the radiopharmaceutical penetrate through the patient body and are detected by a set of collimated radiation detectors. The emitted photon experience interaction within the body by the photoelectric effect which stops their emergence from the body or compton scattering which transfers part of the energy to free electrons and the photon is scattered into a new direction. These photons are also detected by the camera and cause blurring of the image if un-treated with image reconstruction and processing tools.
In SPECT projection data are acquired from different views around the patient. Similar to X-ray CT, image processing and reconstruction methods are used to obtain transaxial or cross sectional images from multiview projection data.
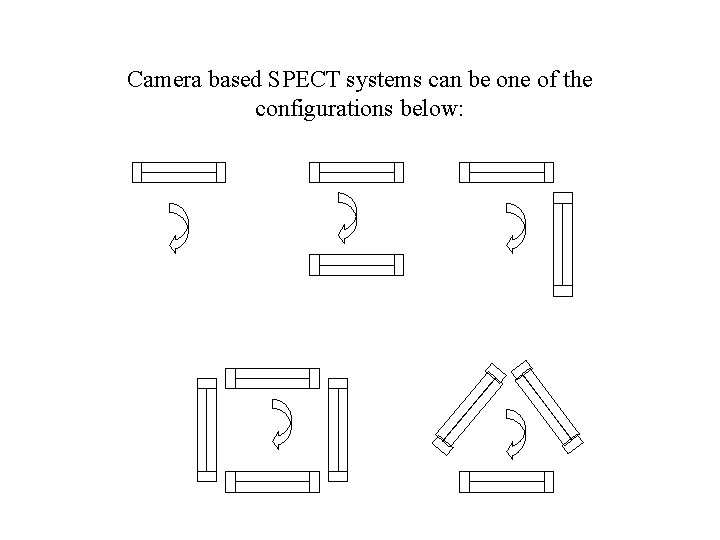
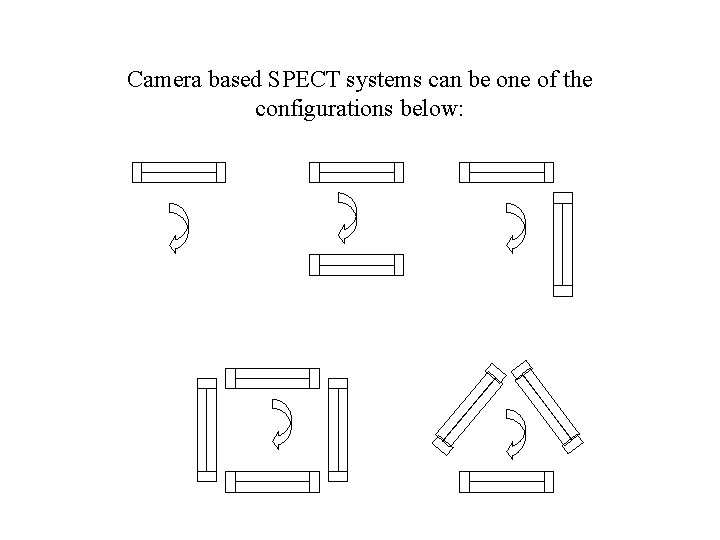
Camera based SPECT systems can be one of the configurations below:
SPECT Machine
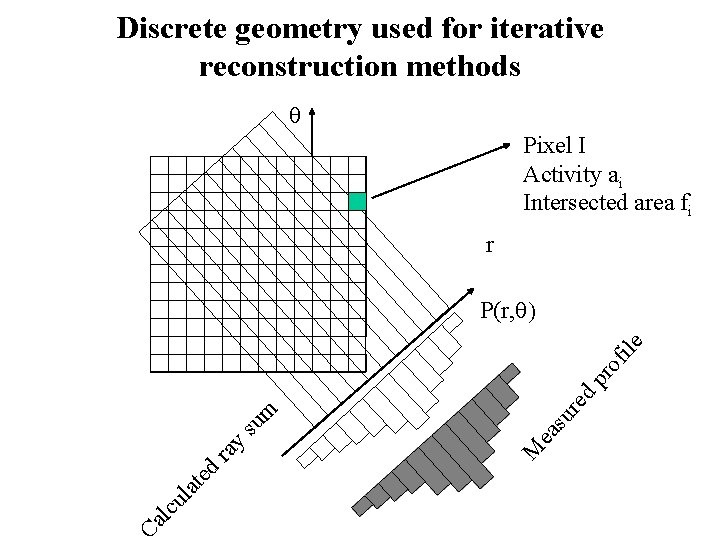
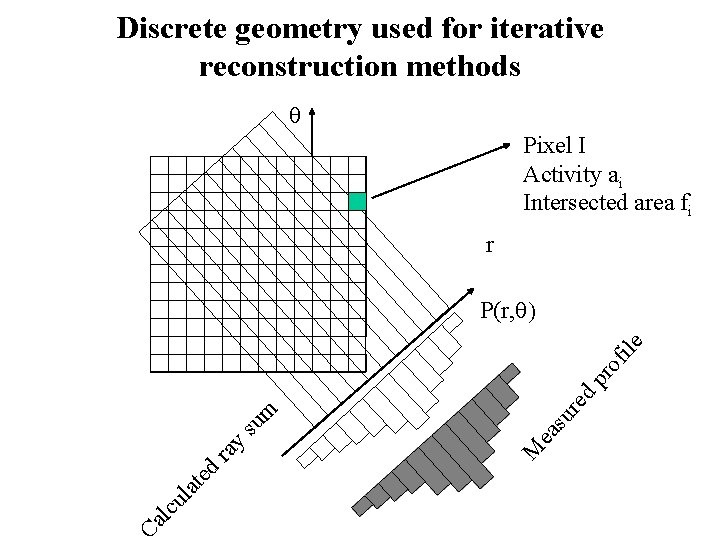
Discrete geometry used for iterative reconstruction methods Pixel I Activity ai Intersected area fi r Ca l cu l at ed re d su M ea ra y su m p ro f ile P(r, )
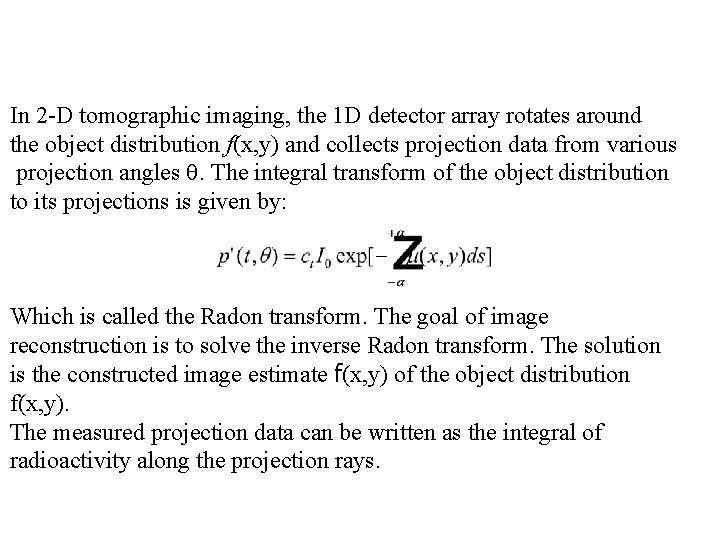
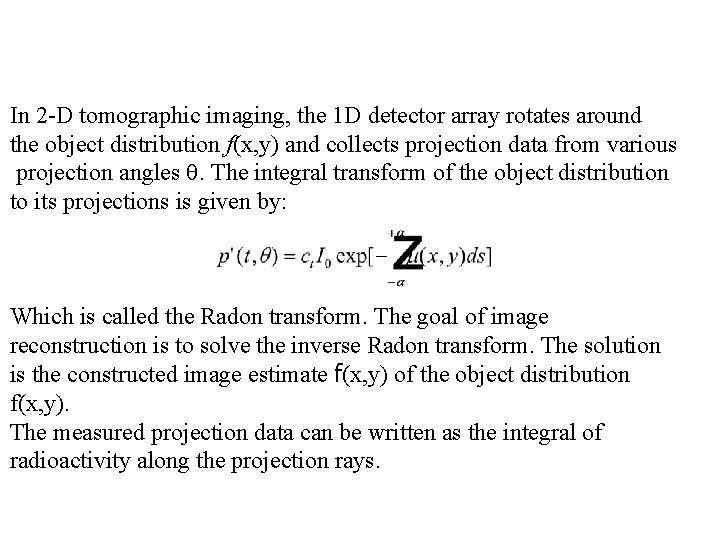
In 2 -D tomographic imaging, the 1 D detector array rotates around the object distribution f(x, y) and collects projection data from various projection angles . The integral transform of the object distribution to its projections is given by: Which is called the Radon transform. The goal of image reconstruction is to solve the inverse Radon transform. The solution is the constructed image estimate f(x, y) of the object distribution f(x, y). The measured projection data can be written as the integral of radioactivity along the projection rays.
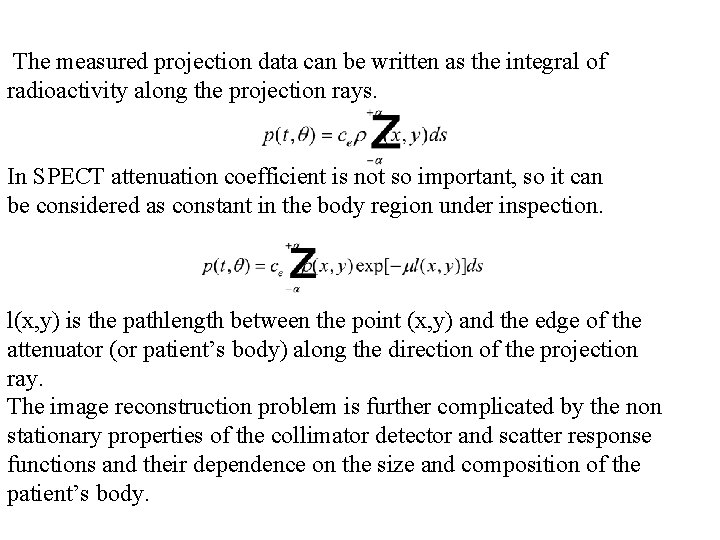
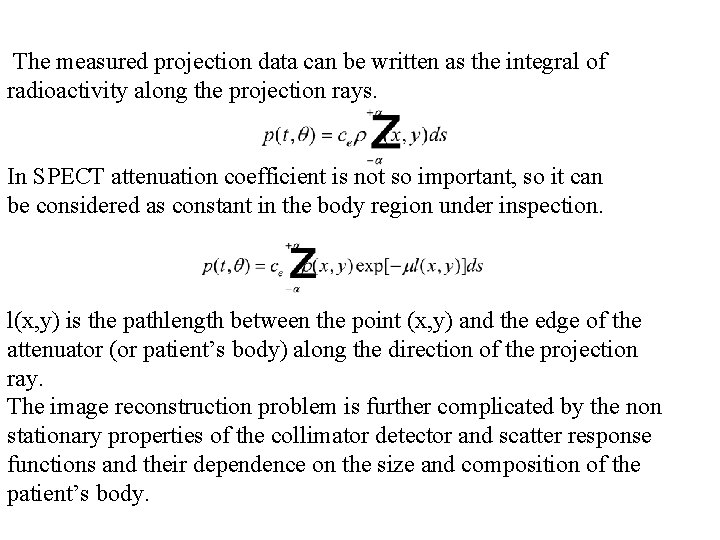
The measured projection data can be written as the integral of radioactivity along the projection rays. In SPECT attenuation coefficient is not so important, so it can be considered as constant in the body region under inspection. l(x, y) is the pathlength between the point (x, y) and the edge of the attenuator (or patient’s body) along the direction of the projection ray. The image reconstruction problem is further complicated by the non stationary properties of the collimator detector and scatter response functions and their dependence on the size and composition of the patient’s body.
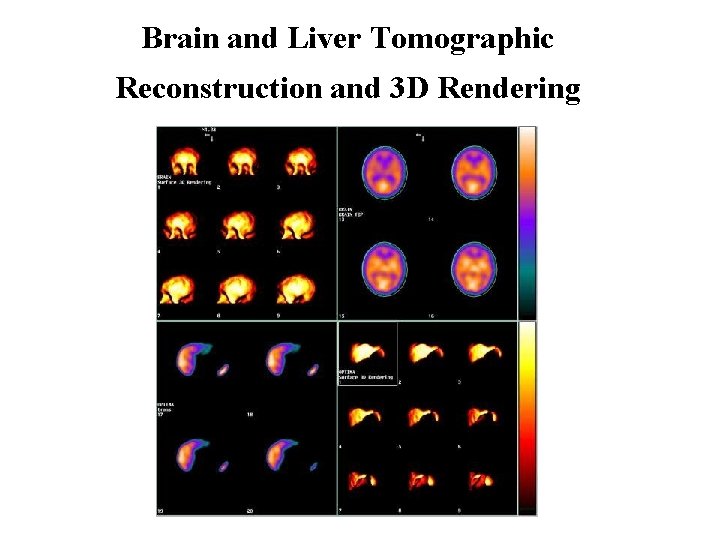
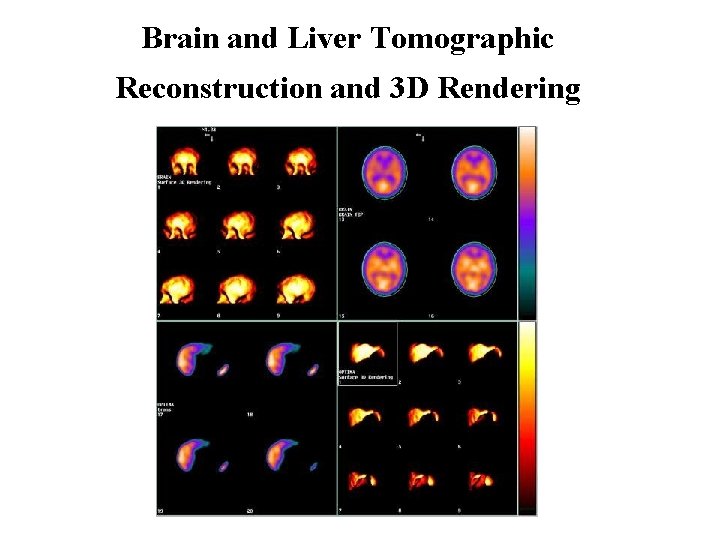
Brain and Liver Tomographic Reconstruction and 3 D Rendering
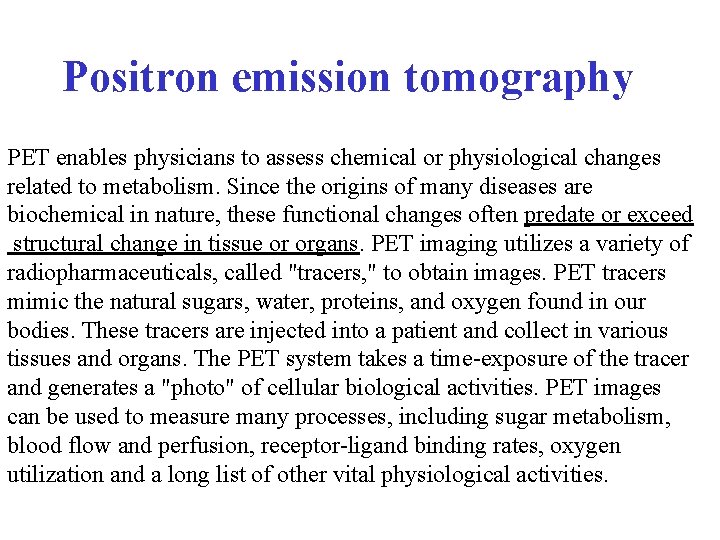
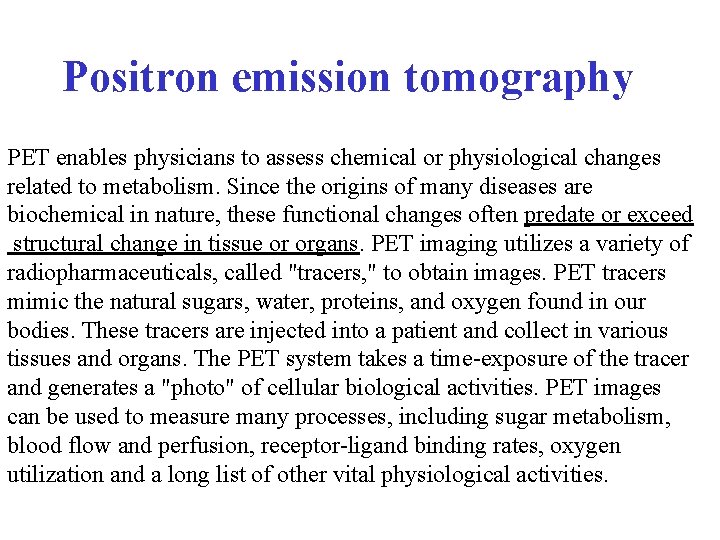
Positron emission tomography PET enables physicians to assess chemical or physiological changes related to metabolism. Since the origins of many diseases are biochemical in nature, these functional changes often predate or exceed structural change in tissue or organs. PET imaging utilizes a variety of radiopharmaceuticals, called "tracers, " to obtain images. PET tracers mimic the natural sugars, water, proteins, and oxygen found in our bodies. These tracers are injected into a patient and collect in various tissues and organs. The PET system takes a time-exposure of the tracer and generates a "photo" of cellular biological activities. PET images can be used to measure many processes, including sugar metabolism, blood flow and perfusion, receptor-ligand binding rates, oxygen utilization and a long list of other vital physiological activities.

PET TRACER PRODUCTION SYSTEMS PET scanning uses artificial radioactive tracers and radionuclides. Their lifetime is usually rather short, thus they need to be produced on site.
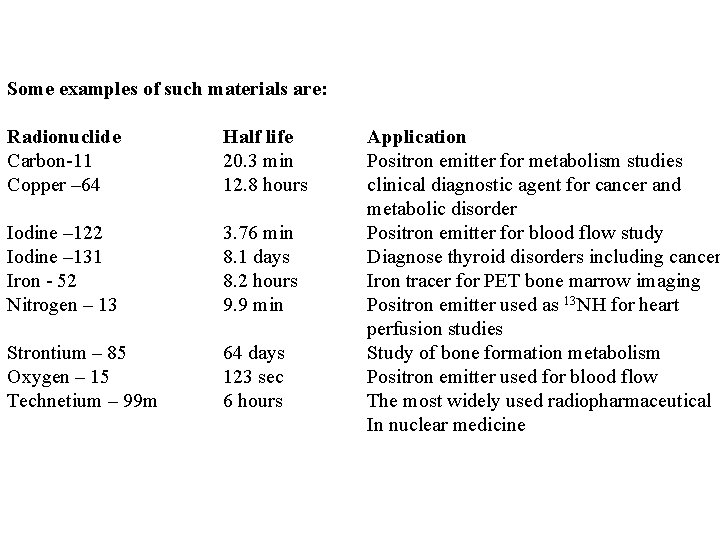
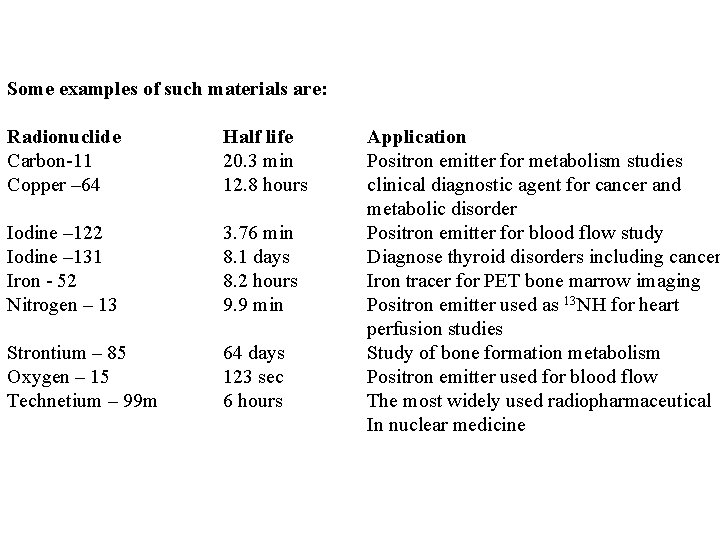
Some examples of such materials are: Radionuclide Half life Carbon-11 20. 3 min Copper – 64 12. 8 hours Iodine – 122 Iodine – 131 Iron - 52 Nitrogen – 13 3. 76 min 8. 1 days 8. 2 hours 9. 9 min Strontium – 85 Oxygen – 15 Technetium – 99 m 64 days 123 sec 6 hours Application Positron emitter for metabolism studies clinical diagnostic agent for cancer and metabolic disorder Positron emitter for blood flow study Diagnose thyroid disorders including cancer Iron tracer for PET bone marrow imaging Positron emitter used as 13 NH for heart perfusion studies Study of bone formation metabolism Positron emitter used for blood flow The most widely used radiopharmaceutical In nuclear medicine
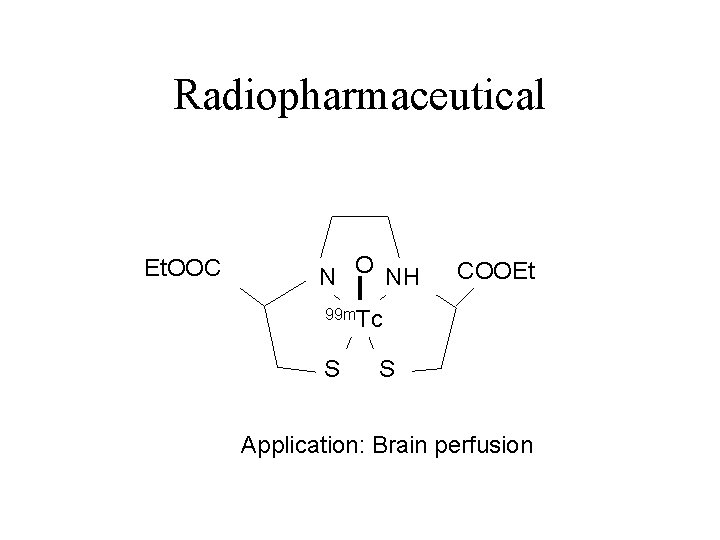
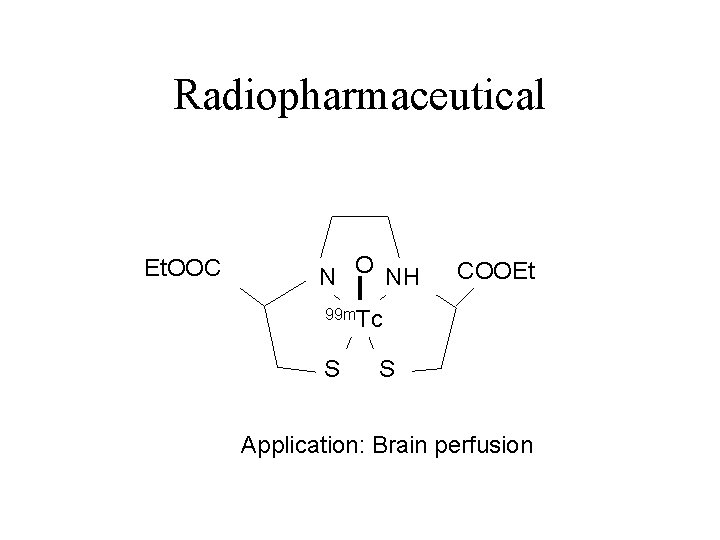
Radiopharmaceutical Et. OOC N O NH COOEt 99 m. Tc S S Application: Brain perfusion
PET has a million fold sensitivity advantage over MRI in tracer study and its chemical specificity, PET is used to study neuroreceptors in the brain and other body tissues. It is efficient in the nanomolar range where much of the receptor proteins in the body. Clinical studies include tumors of the brain, breast, lung, lower GI tract. Additional study of Alzheimer’s disease, Parkinson’s disease, epilepsy and coronary artery disease affecting heart muscle metabolism and flow.
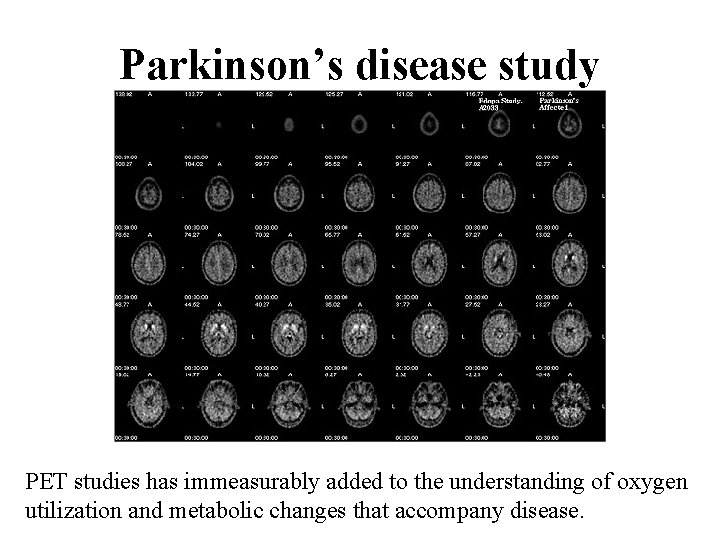
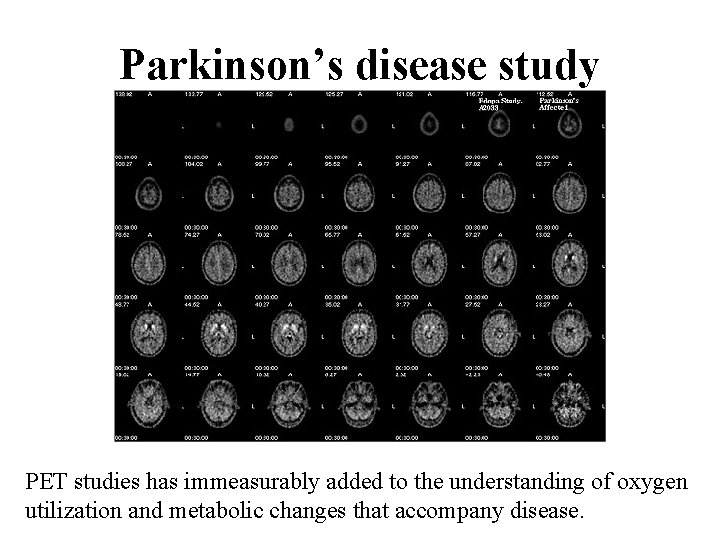
Parkinson’s disease study PET studies has immeasurably added to the understanding of oxygen utilization and metabolic changes that accompany disease.
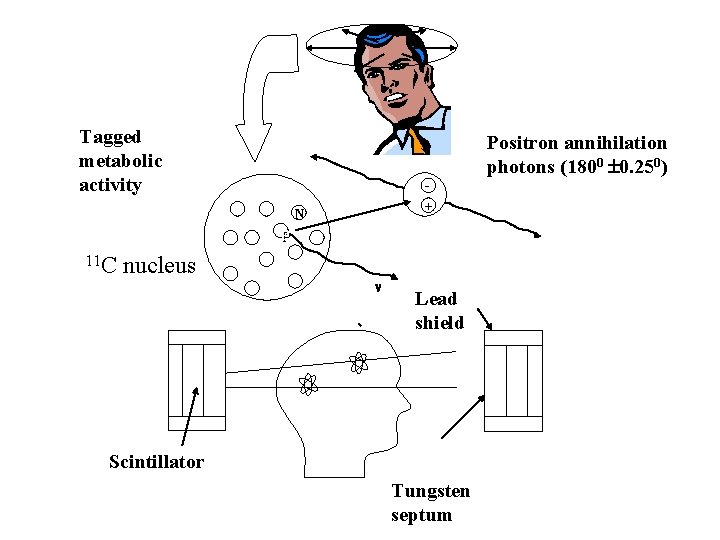
Theory PET imaging starts with the injection of metabolically active tracer – a biologic molecule that carries with it a positron emitting isotope. Over a few minutes the isotope accumulates in an area of the body for which the molecule has an affinity. i. e. glucose labeled with 11 C or glucose analogue labeled with 18 F, accumulates in the brain or tumors, where glucose is used as the primary source of energy. The radioactive nuclei then decay by positron emission. In positron (positive electron) , a nuclear proton changes into a positive electron and a neutron. The atom maintains its atomic mass but decreases its atomic number by 1. The ejected positron combines with an electron almost instantaneously, and these 2 particles undergo the process of annihilation. The energy associated with the masses of the positron and electron particles is 12. 022 Me. V in accordance with E=MC 2. This energy is divided equally between 2 photons which fly away from one another at 1800 angle. Each photon has an energy of 511 ke. V. These high energy gamma rays emerge from the body in opposite directions and recorded simultaneously by pair of detectors.
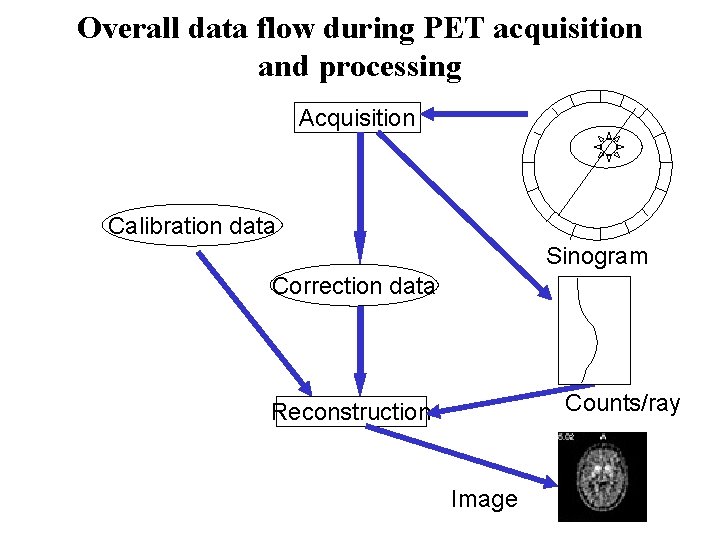
The annihilation event that gave rise to them must have occurred somewhere along the line connecting the detectors. Of course if one of the photons is scattered, then the line of coincidence will be incorrect. After 100, 000 or more annihilation events are detected, the distribution of the positron-emitting tracer is calculated by tomographic reconstruction procedures. PET reconstructs a 2 dimensional image from the one dimensional projections seen at different angles. 3 -D reconstructions can be done using 2 D projections from multiple angles.
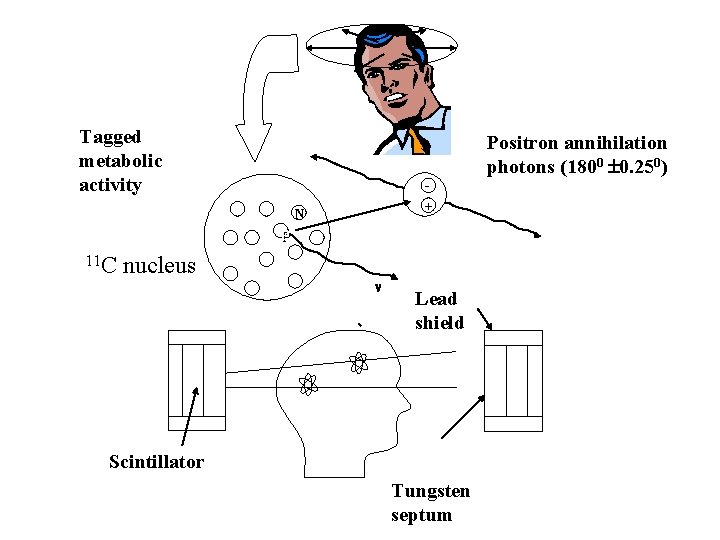
Tagged metabolic activity Positron annihilation photons (1800 0. 250) + N PP 11 C nucleus Lead shield Scintillator Tungsten septum
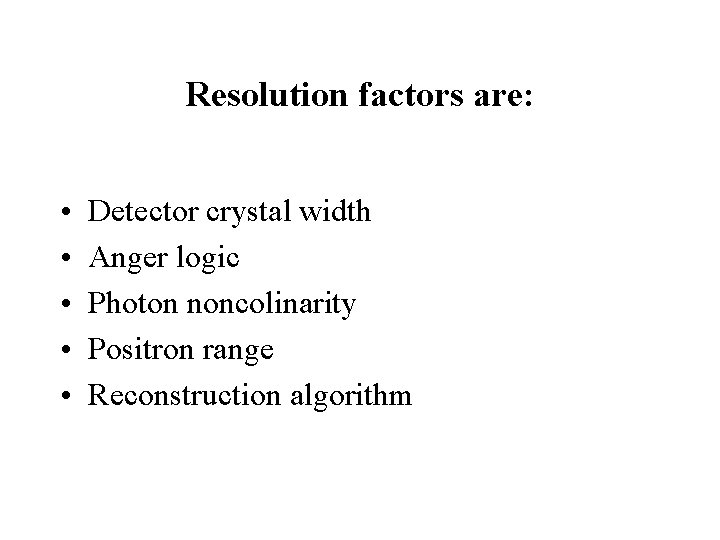
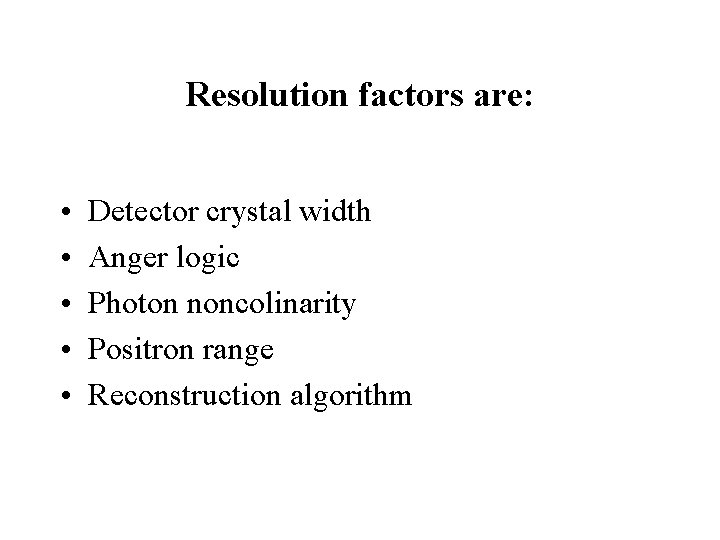
Resolution factors are: • • • Detector crystal width Anger logic Photon noncolinarity Positron range Reconstruction algorithm
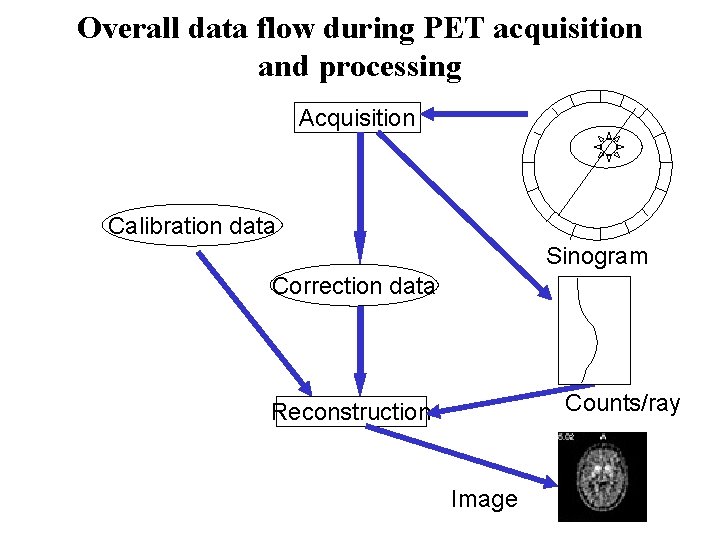
Overall data flow during PET acquisition and processing Acquisition Calibration data Sinogram Correction data Counts/ray Reconstruction Image
Whole body PET
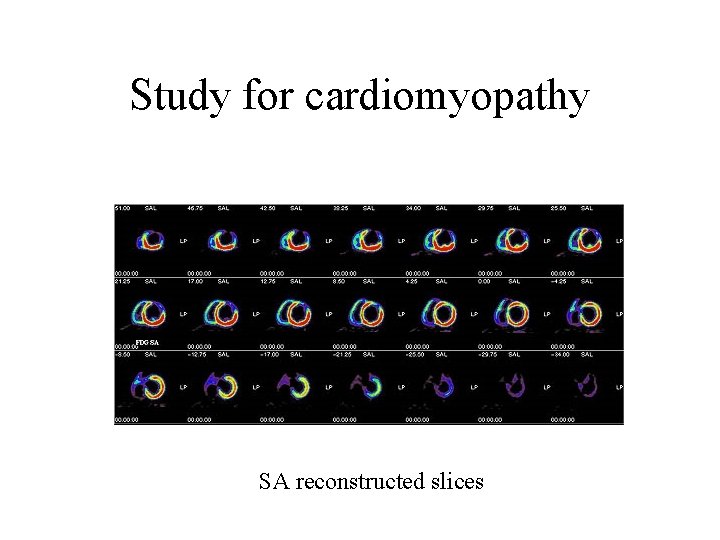
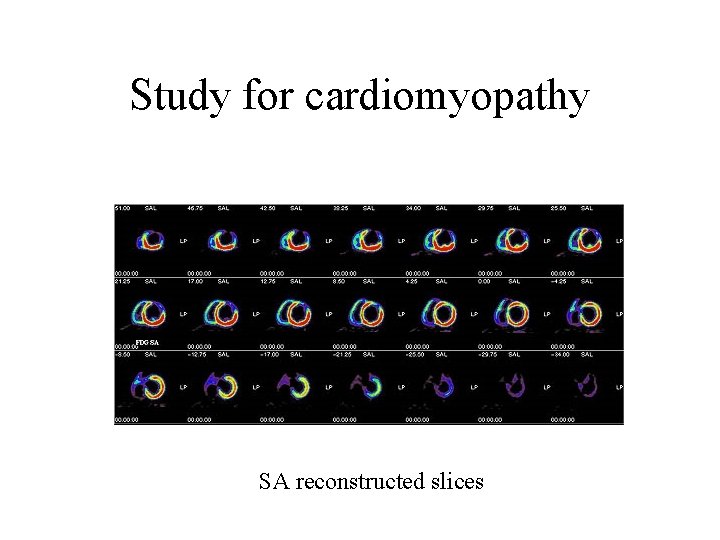
Study for cardiomyopathy SA reconstructed slices
Measurements: • Blood volumes • Oxygen consumption • Perfusion • Glucose consumption
Ultrasound Imaging
Ultrasound operates much the same as sonar, using high-frequency sound waves as its imaging source. Ultrasound is the reflection of a sound wave as it collides with the anatomy being studied. The resulting pattern of that reflection is converted into diagnostic information via a hand-held transducer passed over the area being imaged. First utilized some 50 years ago, this medical technology's non-radioactive nature has made it the modality of choice for ob-gyn procedures; in fact, it is most commonly associated with fetal imaging. Advances in ultrasound technology have resulted in applications that extend far beyond fetal imaging to include cardiac, vascular and breast imaging, as well as cyst identification and guidance of a variety of surgical and otherapeutic procedures.
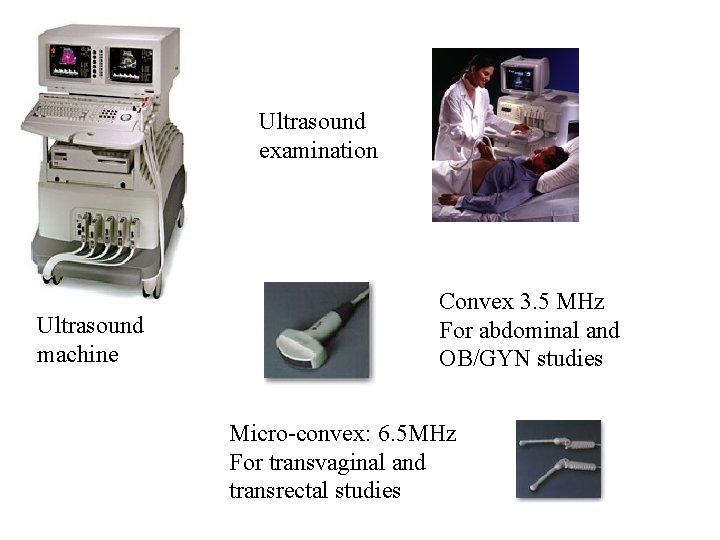
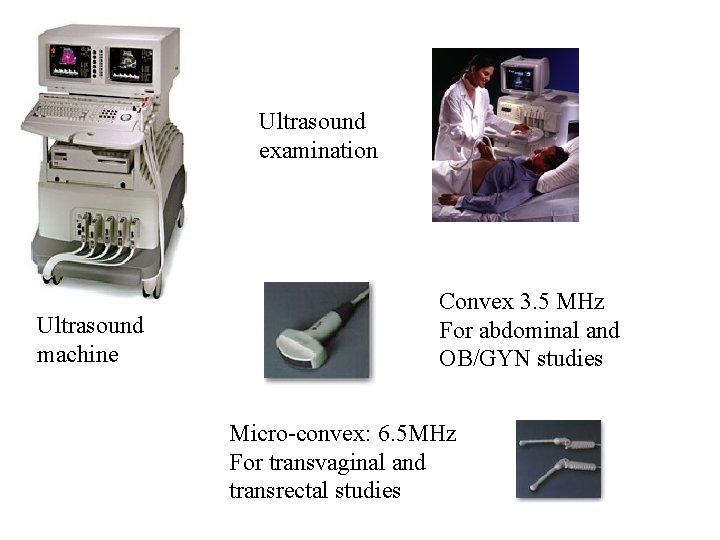
Ultrasound examination Ultrasound machine Convex 3. 5 MHz For abdominal and OB/GYN studies Micro-convex: 6. 5 MHz For transvaginal and transrectal studies
Ultrasound transducers generate acoustic waves by converting magnetic, thermal, or electric energy into mechanical energy. The most efficient technique for medical ultrasound uses the piezoelectric effect. Applying stress on a crystal creates electrical potential and vise versa. The transducer developed when linear arrays were developed. To implement real time imaging, rapid steer of the acoustic beam is needed. Linear sequential arrays were designed to electronically focus the beam in a rectangular image region. Linear phased area transducers were designed to electronically steer and focus the beam at high speed in a sector image format. The standard material fot medical ultrasound for many years is the ferroelectric ceramic lead-zirconate-titanate (PZT) it has a high electromechanical conversion efficiency and low intrinsic losses. The properties of the PZT can be adjusted by modifying the ratio of zirconium to titanium and introducing small amounts of other substances, such as Tantalum. PZT is mechanically strong and can operate at temperatures up to 100 0 C and it’s stable for a long period of time. The disadvantage is high acoustic impedance (Z=30 Mrayls) compared with body tissue (1. 5 Mrayls). This is compensated with acoustic matching layers. Other materials are used as well (i. e. PVDF-Polyvinylidene difluoride).
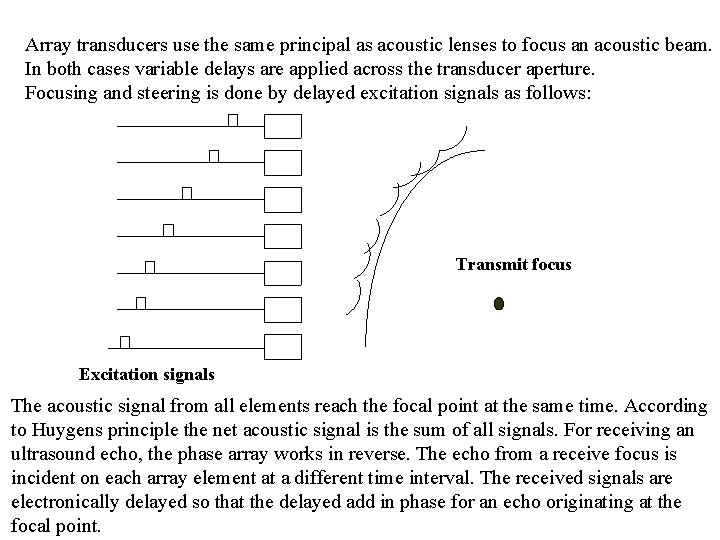
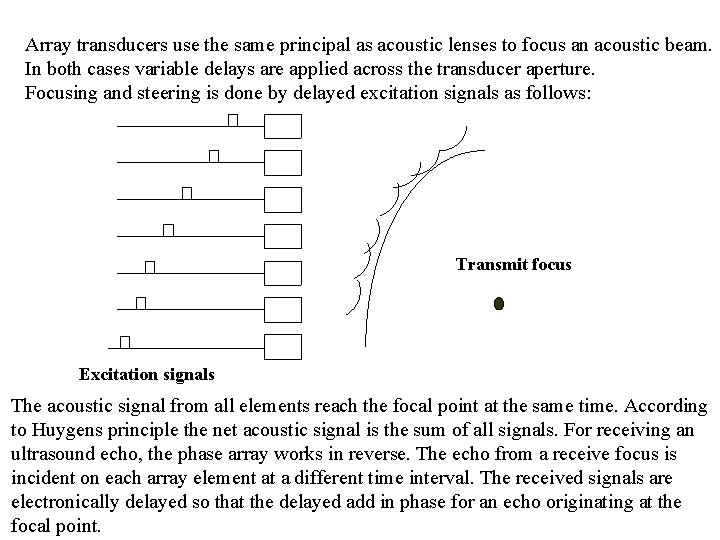
Array transducers use the same principal as acoustic lenses to focus an acoustic beam. In both cases variable delays are applied across the transducer aperture. Focusing and steering is done by delayed excitation signals as follows: Transmit focus Excitation signals The acoustic signal from all elements reach the focal point at the same time. According to Huygens principle the net acoustic signal is the sum of all signals. For receiving an ultrasound echo, the phase array works in reverse. The echo from a receive focus is incident on each array element at a different time interval. The received signals are electronically delayed so that the delayed add in phase for an echo originating at the focal point.
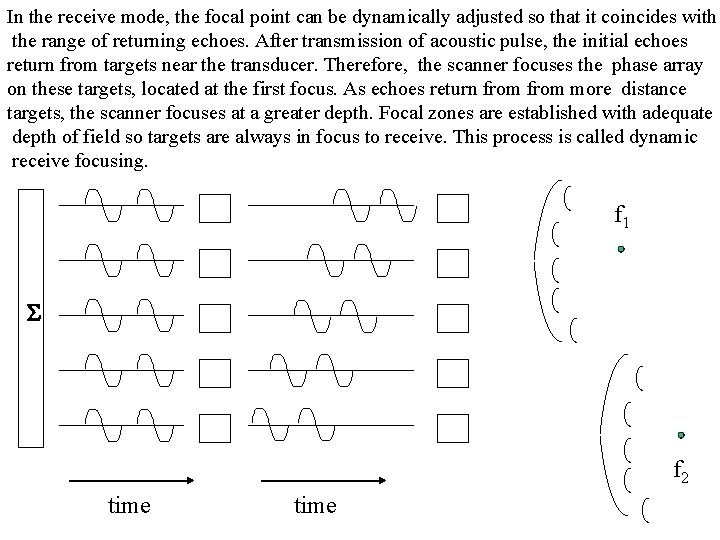
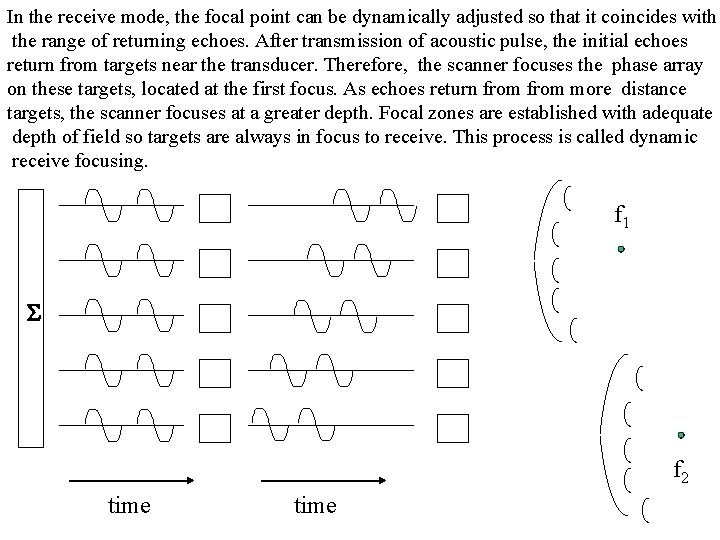
In the receive mode, the focal point can be dynamically adjusted so that it coincides with the range of returning echoes. After transmission of acoustic pulse, the initial echoes return from targets near the transducer. Therefore, the scanner focuses the phase array on these targets, located at the first focus. As echoes return from more distance targets, the scanner focuses at a greater depth. Focal zones are established with adequate depth of field so targets are always in focus to receive. This process is called dynamic receive focusing. f 1 S f 2 time
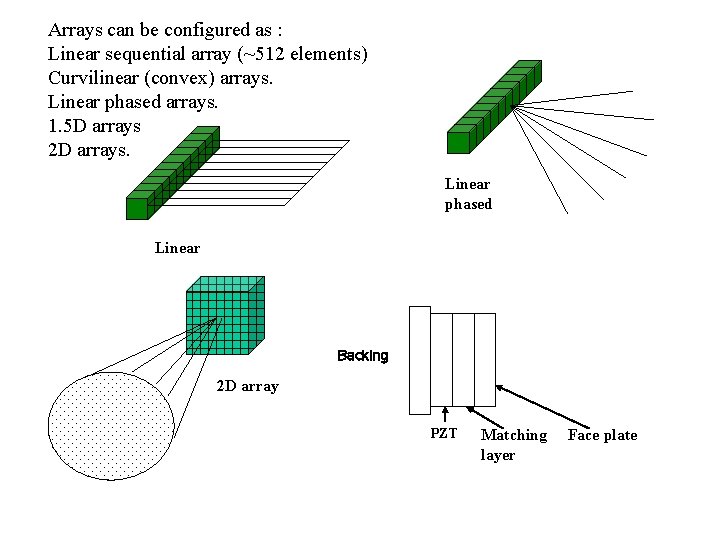
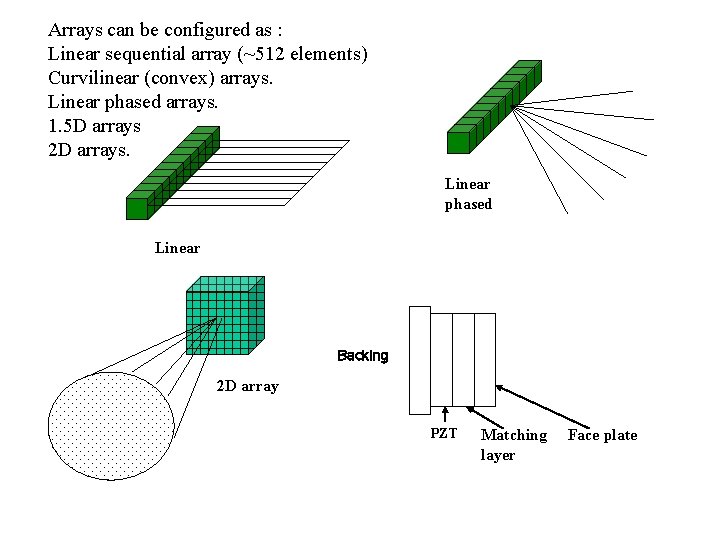
Arrays can be configured as : Linear sequential array (~512 elements) Curvilinear (convex) arrays. Linear phased arrays. 1. 5 D arrays 2 D arrays. Linear phased Linear Backing 2 D array PZT Matching layer Face plate
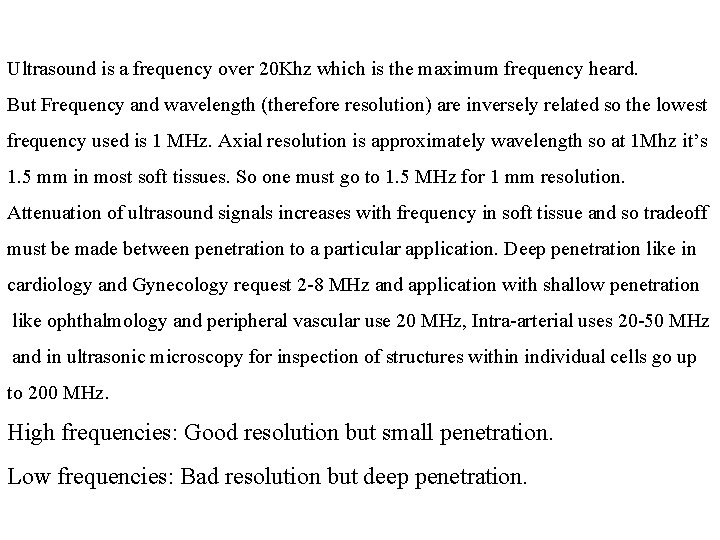
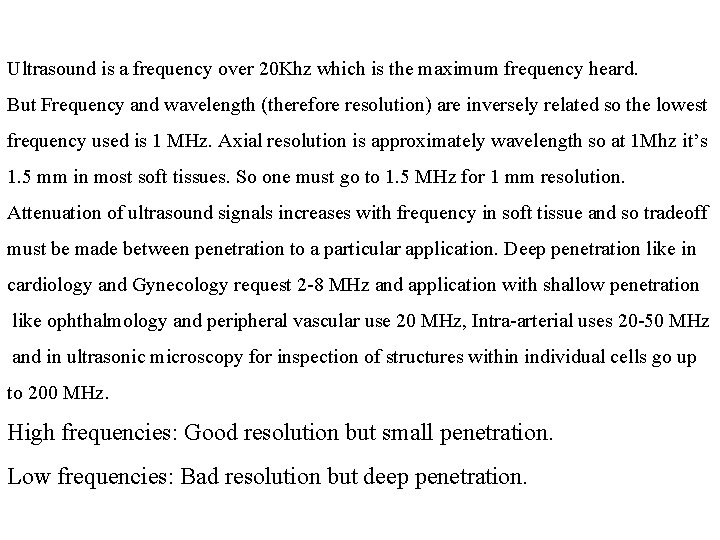
Ultrasound is a frequency over 20 Khz which is the maximum frequency heard. But Frequency and wavelength (therefore resolution) are inversely related so the lowest frequency used is 1 MHz. Axial resolution is approximately wavelength so at 1 Mhz it’s 1. 5 mm in most soft tissues. So one must go to 1. 5 MHz for 1 mm resolution. Attenuation of ultrasound signals increases with frequency in soft tissue and so tradeoff must be made between penetration to a particular application. Deep penetration like in cardiology and Gynecology request 2 -8 MHz and application with shallow penetration like ophthalmology and peripheral vascular use 20 MHz, Intra-arterial uses 20 -50 MHz and in ultrasonic microscopy for inspection of structures within individual cells go up to 200 MHz. High frequencies: Good resolution but small penetration. Low frequencies: Bad resolution but deep penetration.
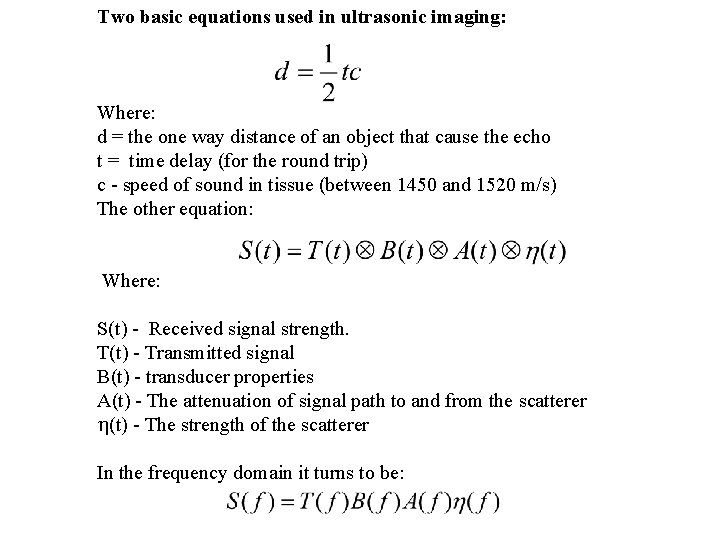
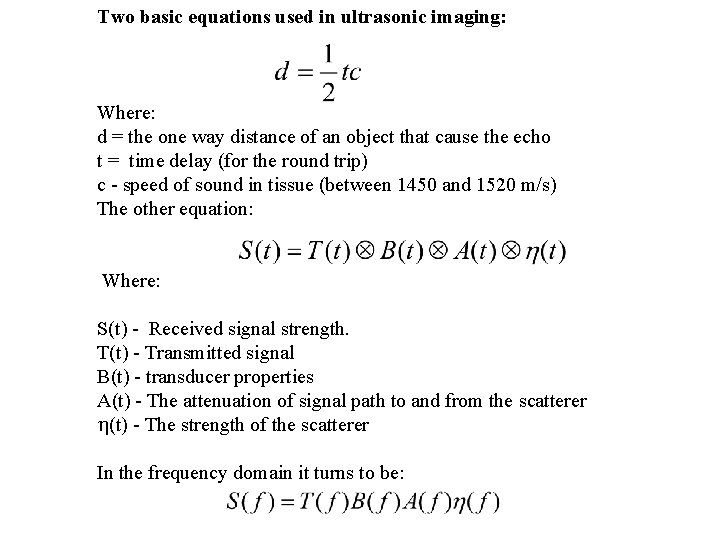
Two basic equations used in ultrasonic imaging: Where: d = the one way distance of an object that cause the echo t = time delay (for the round trip) c - speed of sound in tissue (between 1450 and 1520 m/s) The other equation: Where: S(t) - Received signal strength. T(t) - Transmitted signal B(t) - transducer properties A(t) - The attenuation of signal path to and from the scatterer (t) - The strength of the scatterer In the frequency domain it turns to be:
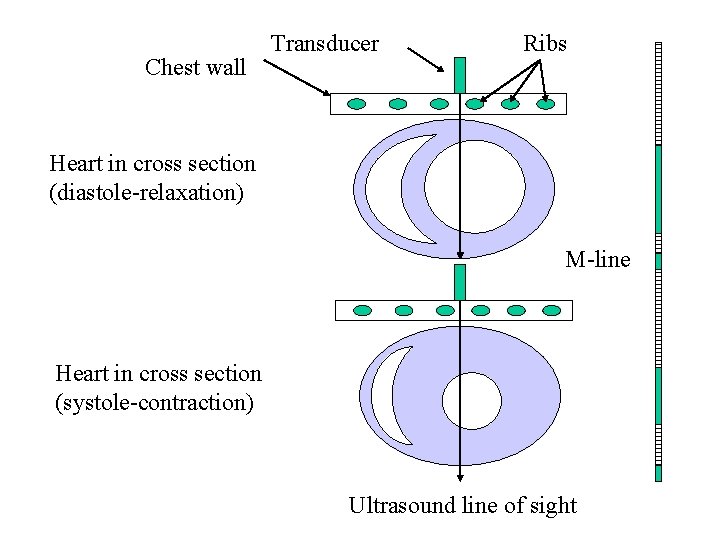
Definition of terms: A-mode - The original display mode of ultrasound measurements, in which the amplitude of the returned echoes along a single line is displayed on an oscilloscope. B-mode (2 -D) - The current display mode of choice. This is produced by sweeping the transducer from side to side and displaying the strength of the returned echoes as bright spots in their geometrically correct direction and distance. M-mode - Followed A mode by recording the strength of the echoes as dark spots on moving light sensitive paper. Object that move, such as the heart cause standard patters of motion to be displayed. And a lot of diagnostic information such as valve closure rates, whether valves opened and closed completely, and wall thickness could be obtained from this mode.
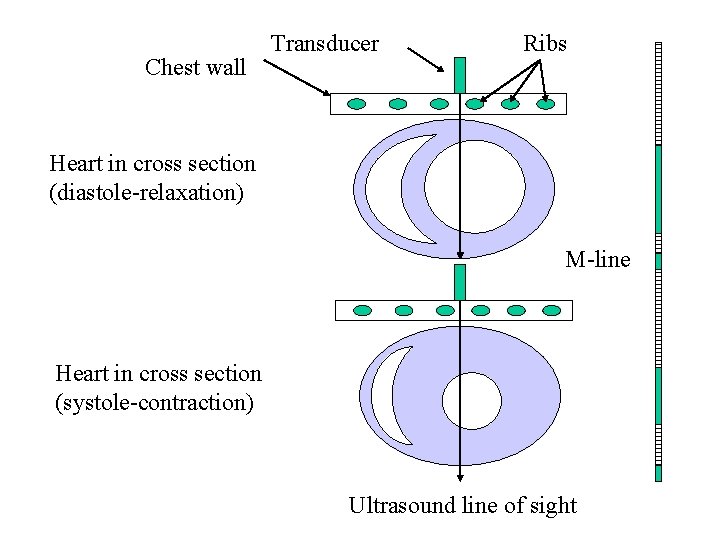
Chest wall Transducer Ribs Heart in cross section (diastole-relaxation) M-line Heart in cross section (systole-contraction) Ultrasound line of sight
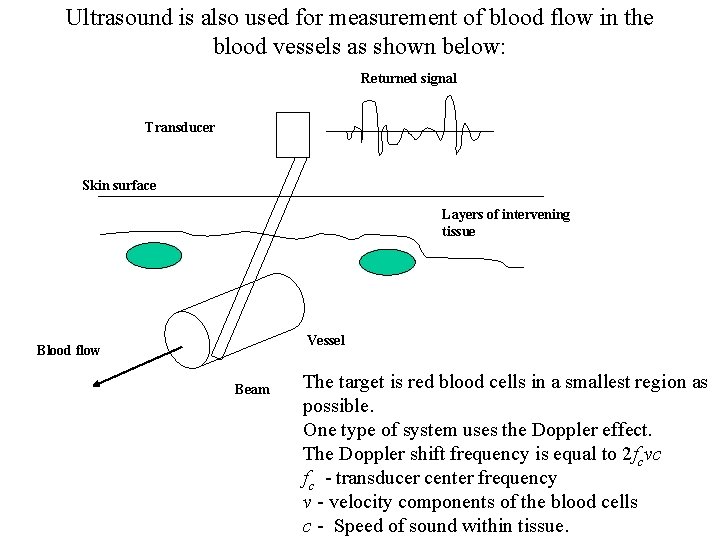
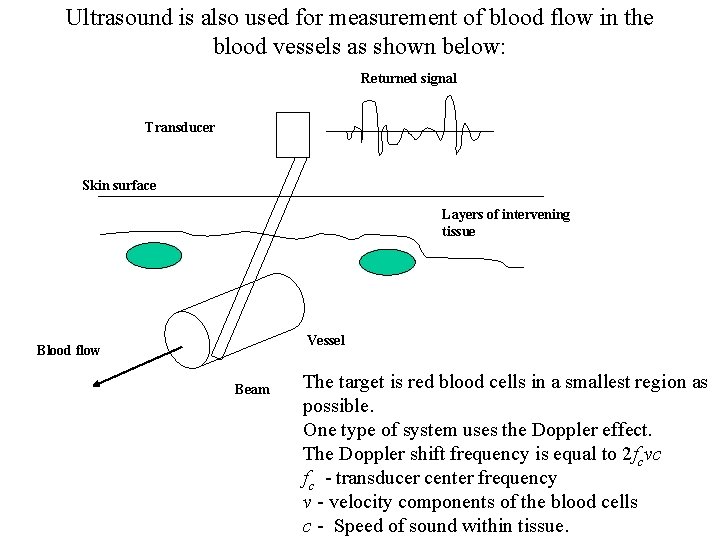
Ultrasound is also used for measurement of blood flow in the blood vessels as shown below: Returned signal Transducer Skin surface Layers of intervening tissue Vessel Blood flow Beam The target is red blood cells in a smallest region as possible. One type of system uses the Doppler effect. The Doppler shift frequency is equal to 2 fcvc fc - transducer center frequency v - velocity components of the blood cells c - Speed of sound within tissue.
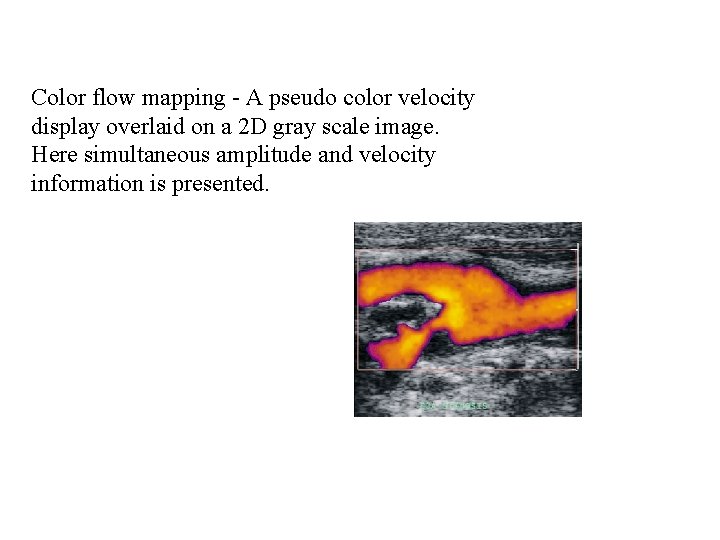
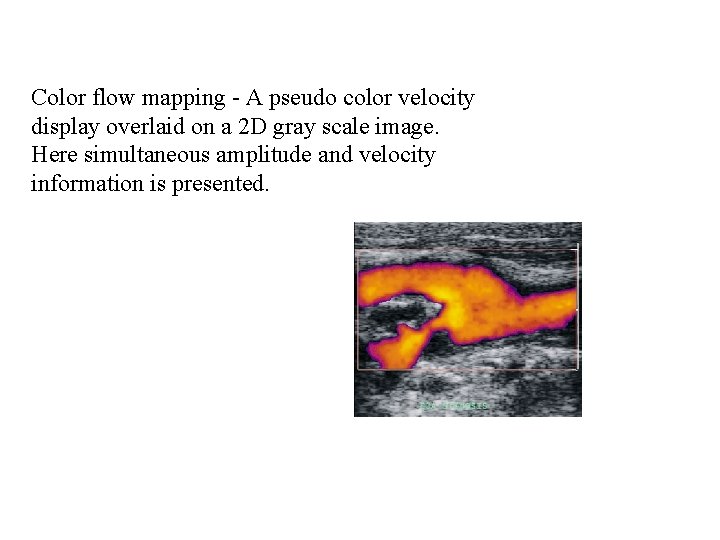
Color flow mapping - A pseudo color velocity display overlaid on a 2 D gray scale image. Here simultaneous amplitude and velocity information is presented.
Ultrasound contrast agents Reflection of sound waves depend on the acoustic impedance which are defined by its density and the velocity of sound in the medium. Acoustic impedances differences are very small between soft tissues. Echofarnaceuticals (US Cas) have been proposed to increase acoustic impedance differences at tissue interfaces. Secondly to increase the respective echo intensities. The most effective principle by far that has emerged is the diffraction of ultrasonic waves on gas bubbles (microbubble containing solutions ) and colloidal, sometimes temperature dependent diphasic systems.

Ultrasound contrast agents Form Substances Properties, Indications Solutions Shaken saline Indocyanine green Gas bubbles, short half life, difficult reproducabilty, cavitation and shaking effects Colloidal emulsions (foam) Perfluorooctylbromide, High density, low acoustic lipid emulsions velocity, lower solubilty in blood, prolongs Doppler enhancement. Colloidal suspensions Iodipamide, ethyl ester, Aqueous microparticles suspension with very fine gas bubbles. Suspensions with gas microbubbles Galactose microparticles suspension forming microbubbles Right heart disease diagnostics
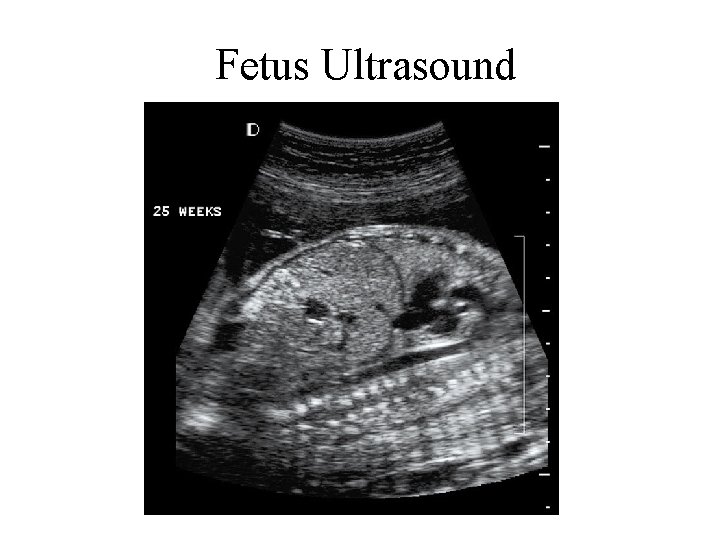
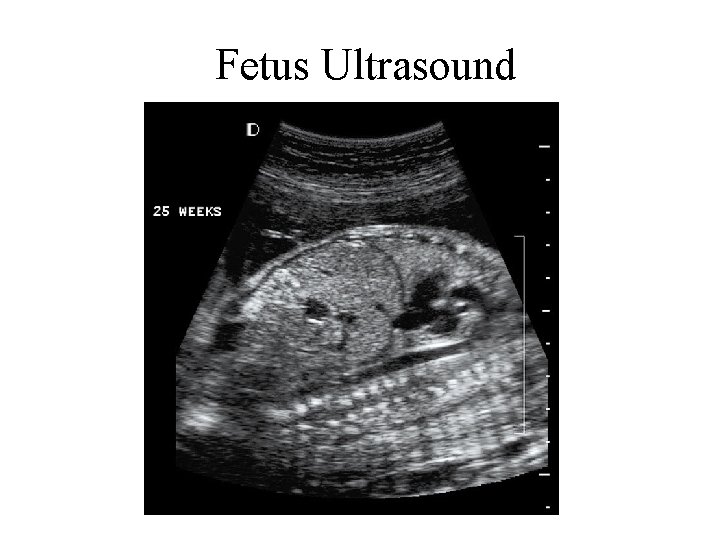
Fetus Ultrasound
 Frc driver station mac
Frc driver station mac Chapter 41 musculoskeletal care modalities
Chapter 41 musculoskeletal care modalities Superficial and deep heating modalities
Superficial and deep heating modalities Thermotherapy indications
Thermotherapy indications Cervical hivd
Cervical hivd Thermal modalities
Thermal modalities Mechanical modalities
Mechanical modalities Cscc medical imaging
Cscc medical imaging Spie medical imaging
Spie medical imaging Medical terminology radiology
Medical terminology radiology Fourier transform
Fourier transform Medical imaging software
Medical imaging software Medical imaging workstations
Medical imaging workstations Body quadrants and organs
Body quadrants and organs Define urban hierarchy
Define urban hierarchy Earliest urban hearths
Earliest urban hearths The are our earliest literature
The are our earliest literature The earliest bridges consisted mainly of
The earliest bridges consisted mainly of Prometheus background
Prometheus background Myllokunmingia
Myllokunmingia Earliest urban hearths
Earliest urban hearths Earliest start time formula
Earliest start time formula Childhood days in tagalog
Childhood days in tagalog The earliest known grecian epics were written by____ .
The earliest known grecian epics were written by____ . Short history of tennis
Short history of tennis Gymnastics history
Gymnastics history The earliest fossils date back to about when?
The earliest fossils date back to about when? Earliest earth
Earliest earth Where did the earliest civilizations develop
Where did the earliest civilizations develop Types of noise according to dean barnlund
Types of noise according to dean barnlund Earliest comedian
Earliest comedian The earliest civilization in asia arose in
The earliest civilization in asia arose in The earliest texans lived in shelters made of wood.
The earliest texans lived in shelters made of wood. The earliest start time rule
The earliest start time rule The earliest aegean civilization was located
The earliest aegean civilization was located Energy energy transfer and general energy analysis
Energy energy transfer and general energy analysis Energy energy transfer and general energy analysis
Energy energy transfer and general energy analysis Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Frameset trong html5
Frameset trong html5 Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Thang điểm glasgow
Thang điểm glasgow Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Các môn thể thao bắt đầu bằng từ đua
Các môn thể thao bắt đầu bằng từ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư tọa độ 5x5
Mật thư tọa độ 5x5 101012 bằng
101012 bằng Phản ứng thế ankan
Phản ứng thế ankan Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế
Cái miệng nó xinh thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Ví dụ giọng cùng tên
Ví dụ giọng cùng tên Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Số nguyên tố là gì
Số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ đẻ mỗi lứa mấy con
Hổ đẻ mỗi lứa mấy con Khi nào hổ mẹ dạy hổ con săn mồi
Khi nào hổ mẹ dạy hổ con săn mồi Hệ hô hấp
Hệ hô hấp Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi California medical license for foreign medical graduates
California medical license for foreign medical graduates Gbmc infoweb
Gbmc infoweb Hepburn osteometric board
Hepburn osteometric board Torrance memorial medical center medical records
Torrance memorial medical center medical records Cartersville medical center medical records
Cartersville medical center medical records Windows imaging acquisition
Windows imaging acquisition Quantum imaging with undetected photons
Quantum imaging with undetected photons Affordable hyperspectral imaging
Affordable hyperspectral imaging Live cell imaging applications
Live cell imaging applications Salt for concave mirrors
Salt for concave mirrors Focused imaging learning
Focused imaging learning Direct imaging subsystem
Direct imaging subsystem Hardware independent imaging
Hardware independent imaging Digital imagery definition
Digital imagery definition Digital imaging artist
Digital imaging artist