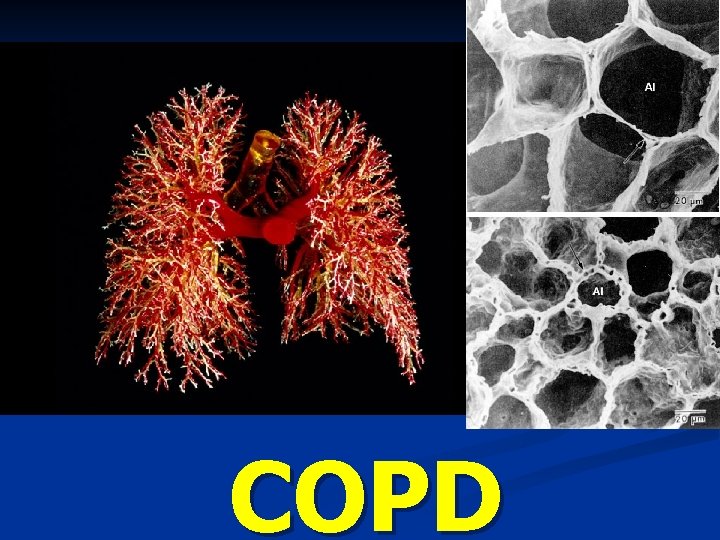
COPD Respiratory System 22 1 Figure Respiratory System







- Slides: 121
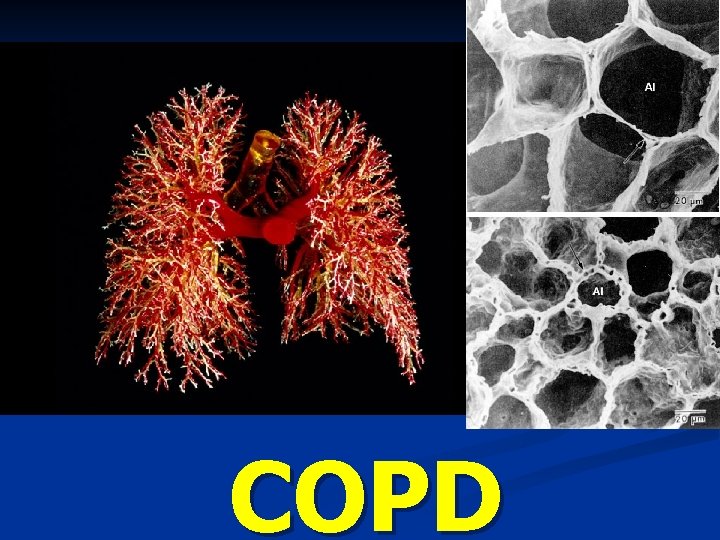
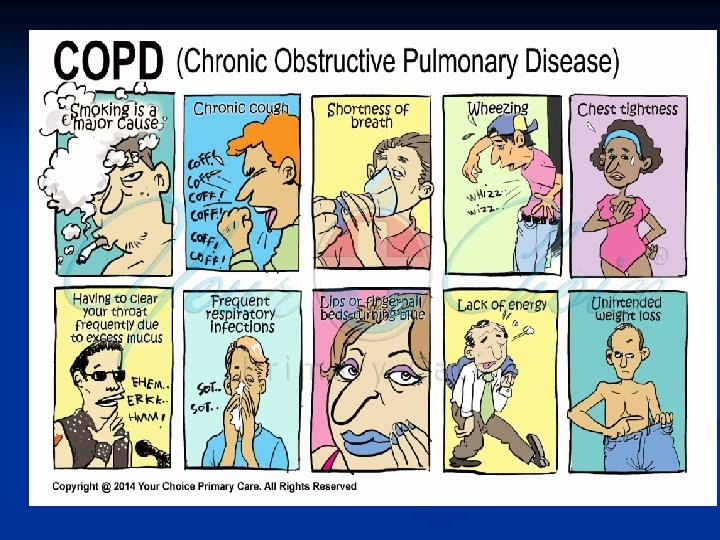
COPD
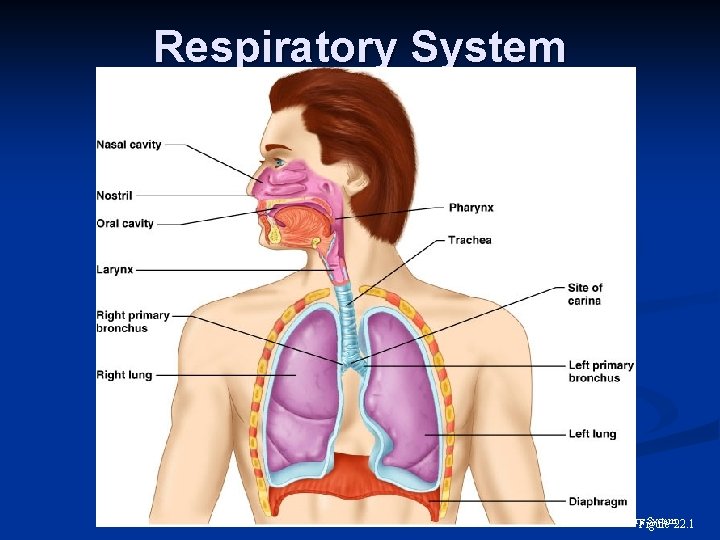
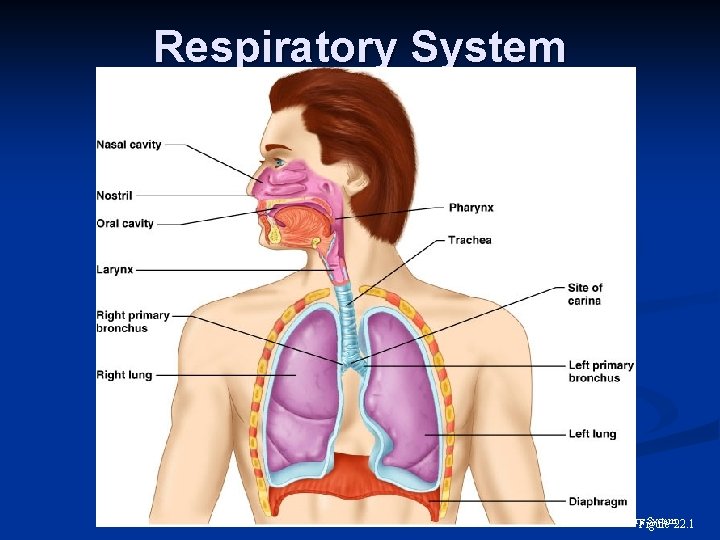
Respiratory System 22. 1 Figure
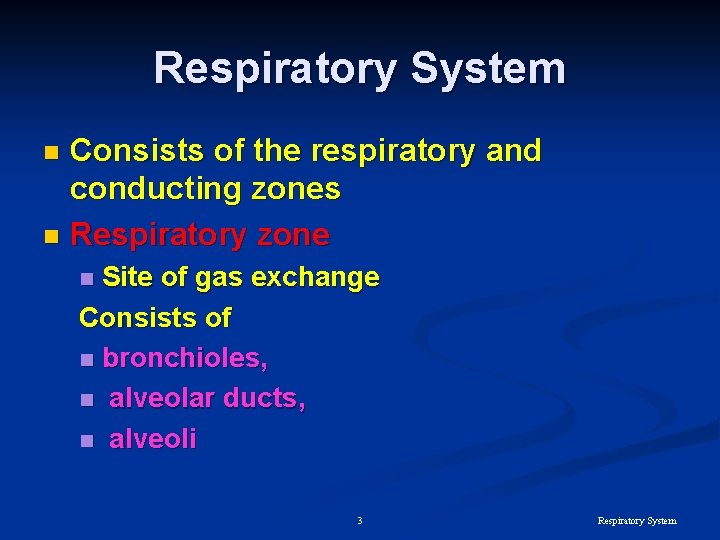
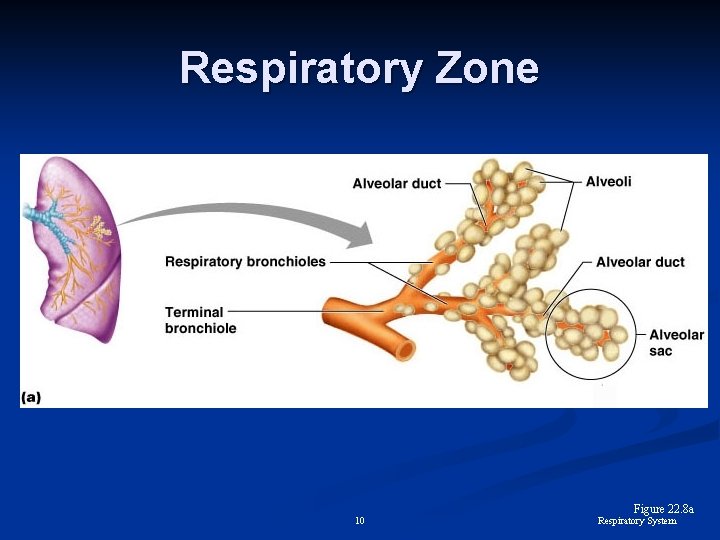
Respiratory System Consists of the respiratory and conducting zones n Respiratory zone n Site of gas exchange Consists of n bronchioles, n alveolar ducts, n alveoli n 3 Respiratory System
Respiratory System n Conducting zone Provides rigid conduits for air to reach the sites of gas exchange n all other respiratory structures (e. g. , nose, nasal cavity, pharynx, trachea) n n Respiratory muscles – diaphragm and other muscles that promote ventilation 4 Respiratory System
Major Functions of the Respiratory System To supply the body with oxygen and dispose of carbon dioxide n Respiration – four distinct processes n Pulmonary ventilation – moving air into and out of the lungs n External respiration – gas exchange between the lungs and the blood n 5 Respiratory System
Major Functions of the Respiratory System n Internal respiration – gas exchange between systemic blood vessels and tissues 6 Respiratory System
Larynx (Voice Box) Attaches to the hyoid bone n Continuous with the trachea posteriorly three functions n n To provide a patent airway n To act as a switching mechanism to route air and food into the proper channels n To function in voice production 7 Respiratory System
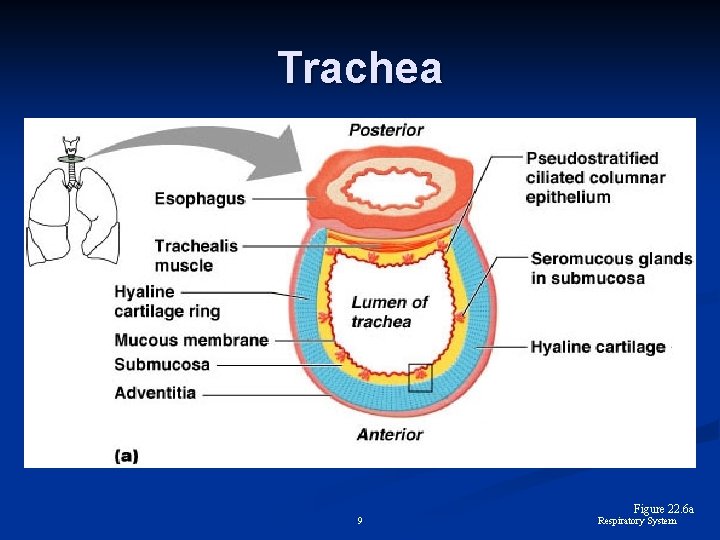
Trachea Flexible and mobile tube extending from the larynx into the mediastinum n Composed of three layers n Mucosa – made up of goblet cells and ciliated epithelium n Submucosa – connective tissue deep to the mucosa n Adventitia – outermost layer made of Cshaped rings of hyaline cartilage n 8 Respiratory System
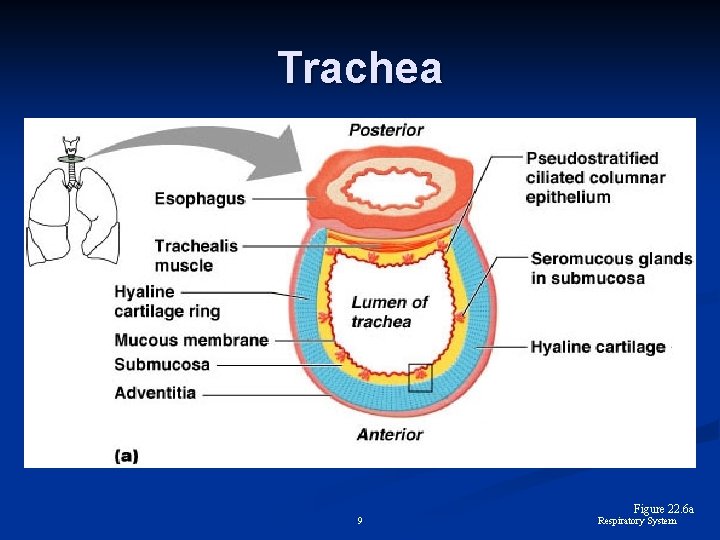
Trachea 9 Figure 22. 6 a Respiratory System
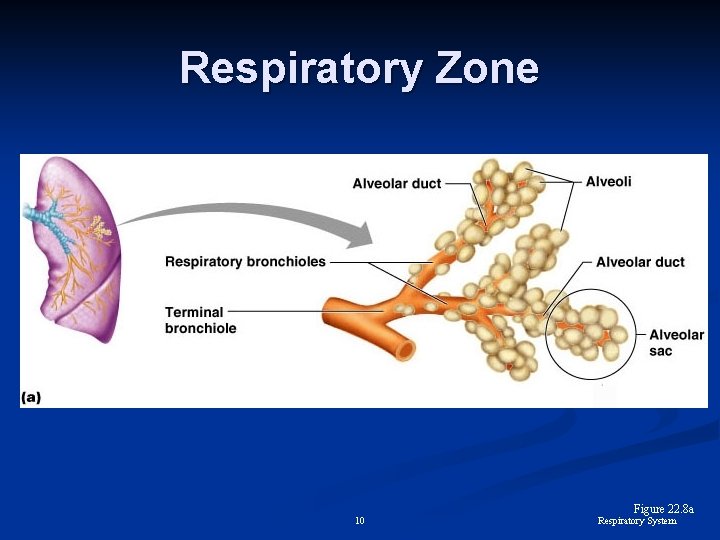
Respiratory Zone 10 Figure 22. 8 a Respiratory System
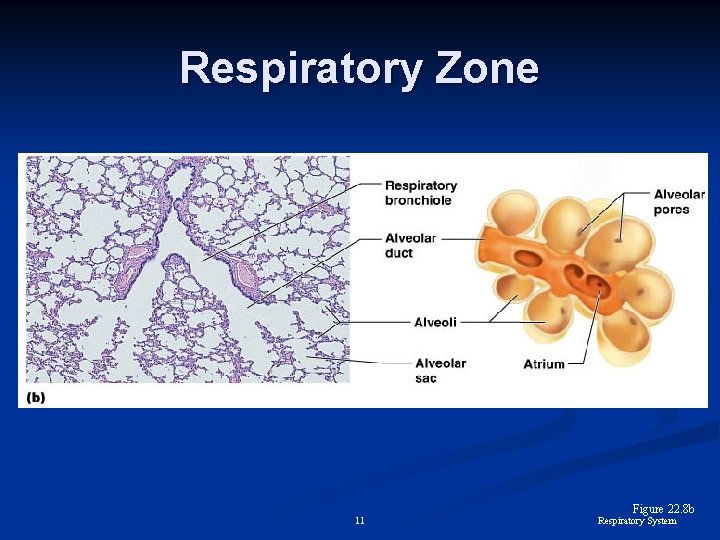
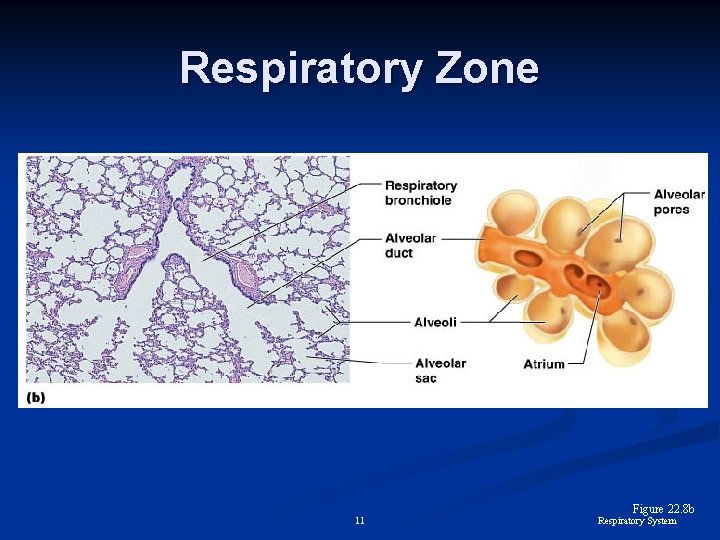
Respiratory Zone 11 Figure 22. 8 b Respiratory System
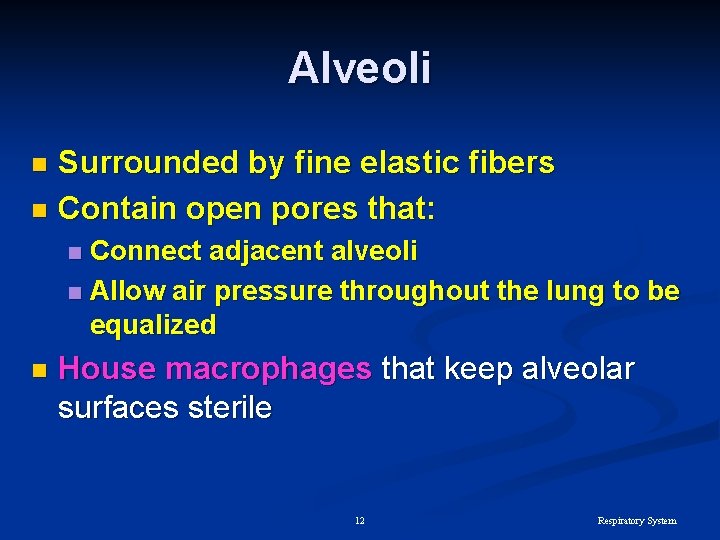
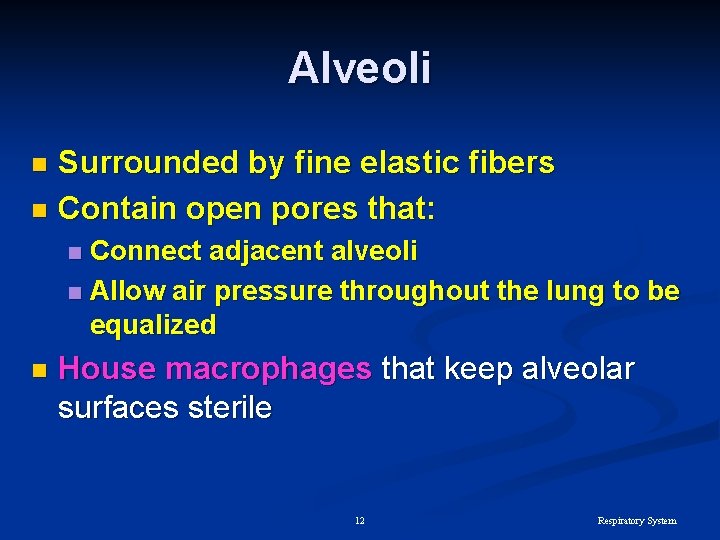
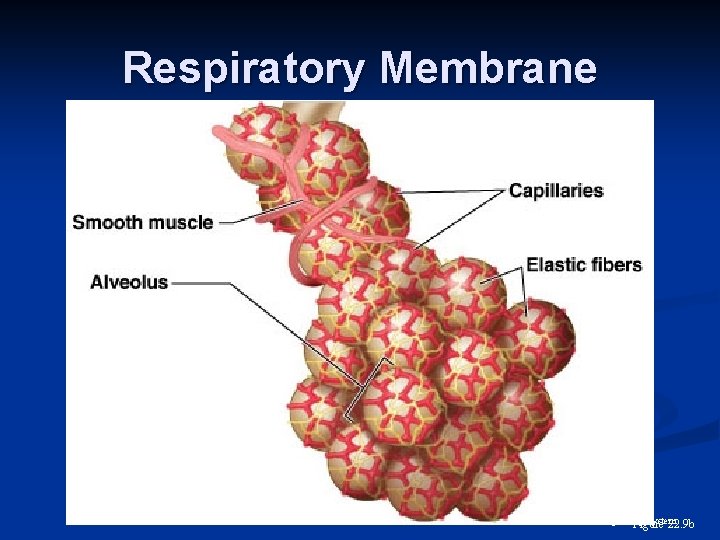
Alveoli Surrounded by fine elastic fibers n Contain open pores that: n Connect adjacent alveoli n Allow air pressure throughout the lung to be equalized n n House macrophages that keep alveolar surfaces sterile 12 Respiratory System
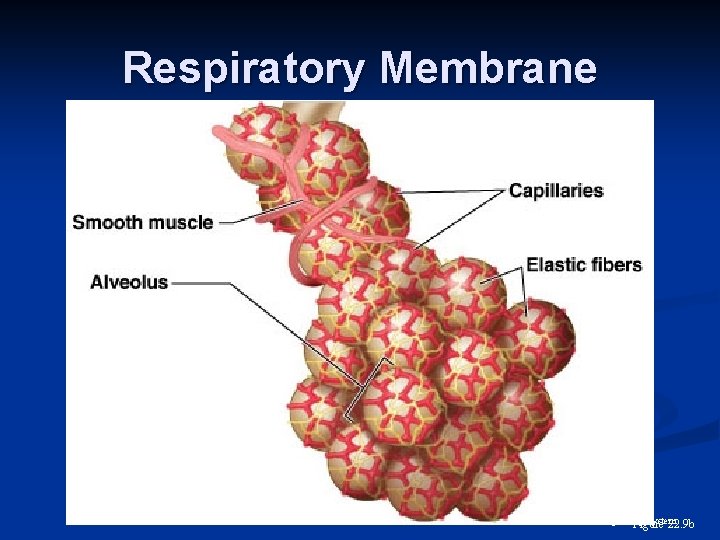
Respiratory Membrane 13 Respiratory System Figure 22. 9 b
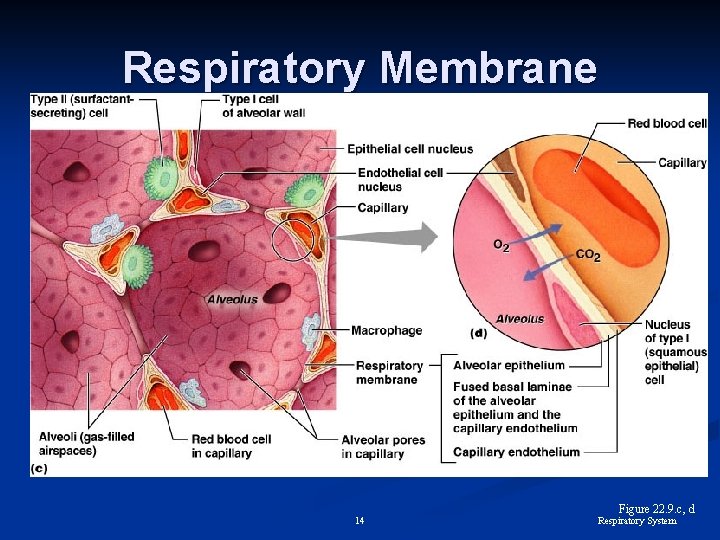
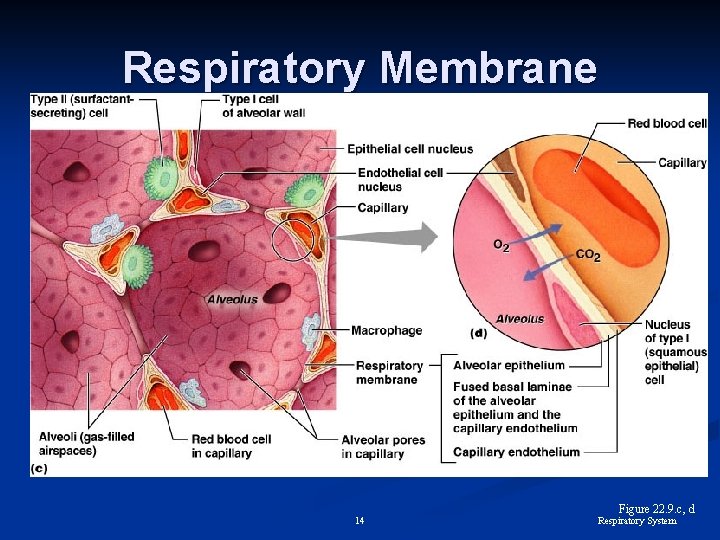
Respiratory Membrane 14 Figure 22. 9. c, d Respiratory System
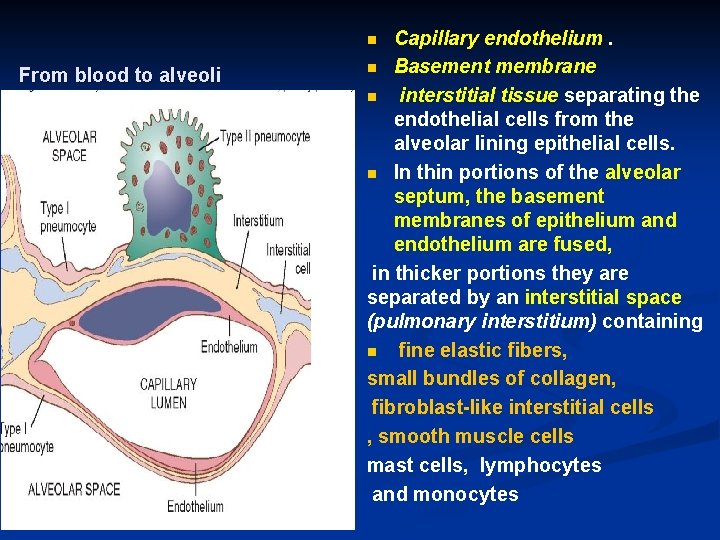
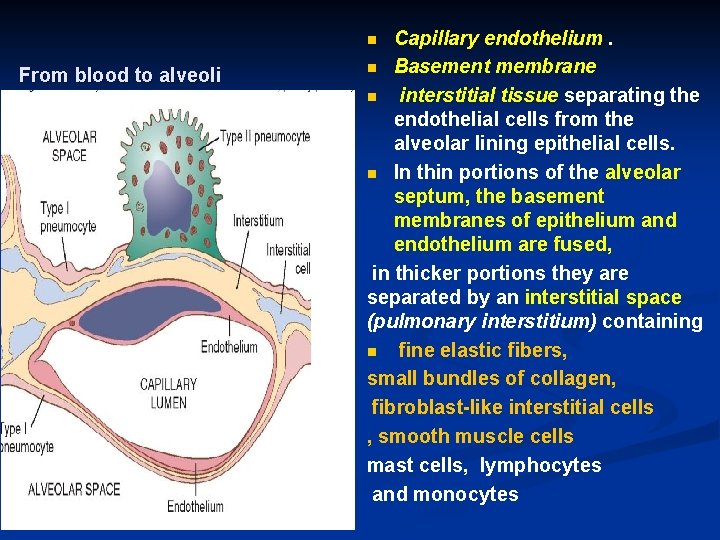
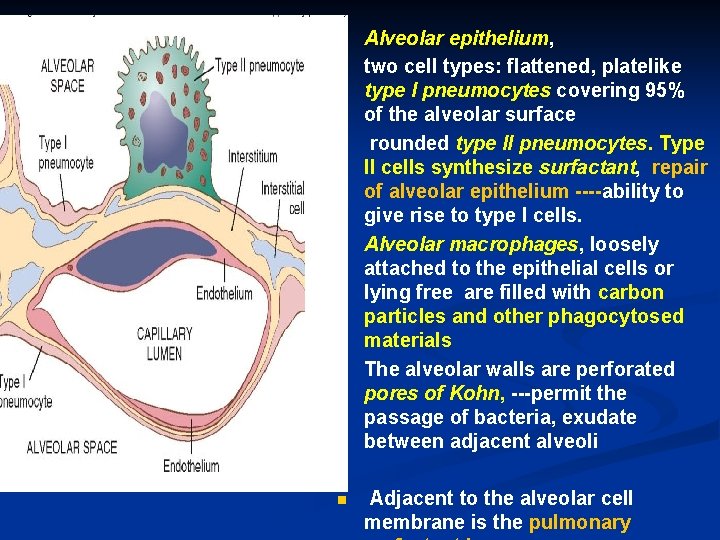
Capillary endothelium. n Basement membrane n interstitial tissue separating the endothelial cells from the alveolar lining epithelial cells. n In thin portions of the alveolar septum, the basement membranes of epithelium and endothelium are fused, in thicker portions they are separated by an interstitial space (pulmonary interstitium) containing n fine elastic fibers, small bundles of collagen, fibroblast-like interstitial cells , smooth muscle cells mast cells, lymphocytes and monocytes n From blood to alveoli
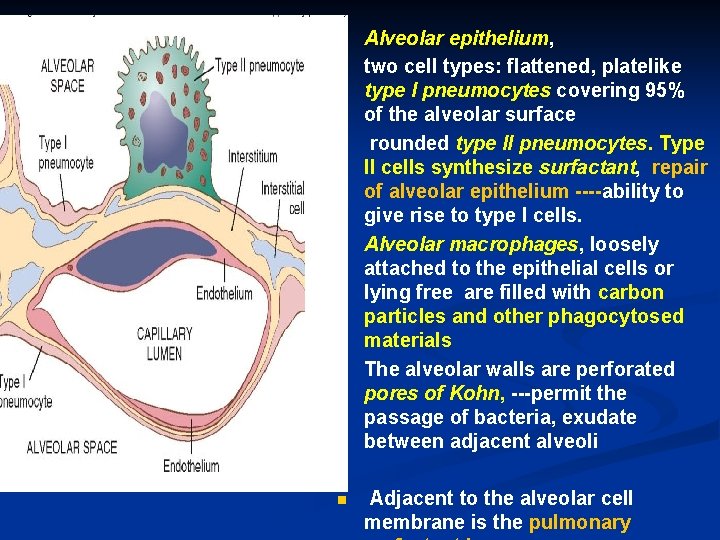
n n n Alveolar epithelium, two cell types: flattened, platelike type I pneumocytes covering 95% of the alveolar surface rounded type II pneumocytes. Type II cells synthesize surfactant, repair of alveolar epithelium ----ability to give rise to type I cells. Alveolar macrophages, loosely attached to the epithelial cells or lying free are filled with carbon particles and other phagocytosed materials The alveolar walls are perforated pores of Kohn, ---permit the passage of bacteria, exudate between adjacent alveoli Adjacent to the alveolar cell membrane is the pulmonary
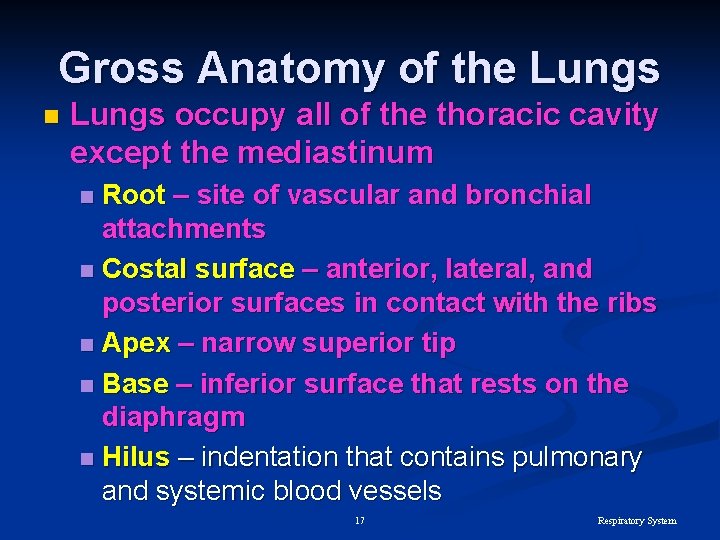
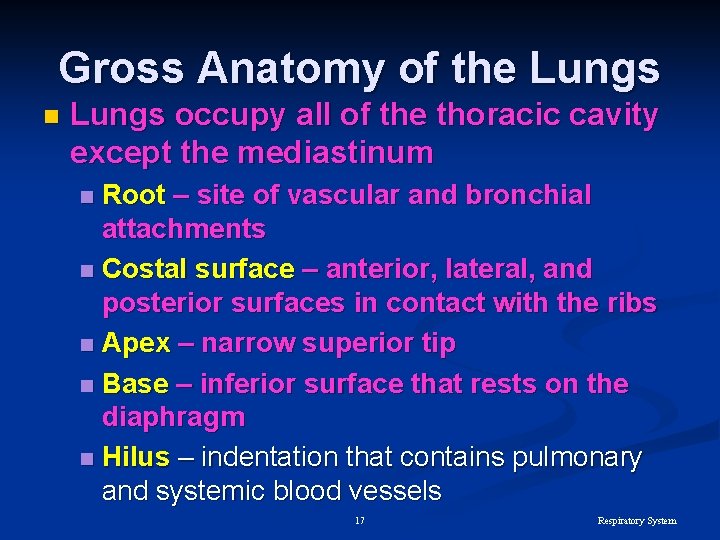
Gross Anatomy of the Lungs n Lungs occupy all of the thoracic cavity except the mediastinum Root – site of vascular and bronchial attachments n Costal surface – anterior, lateral, and posterior surfaces in contact with the ribs n Apex – narrow superior tip n Base – inferior surface that rests on the diaphragm n Hilus – indentation that contains pulmonary and systemic blood vessels n 17 Respiratory System
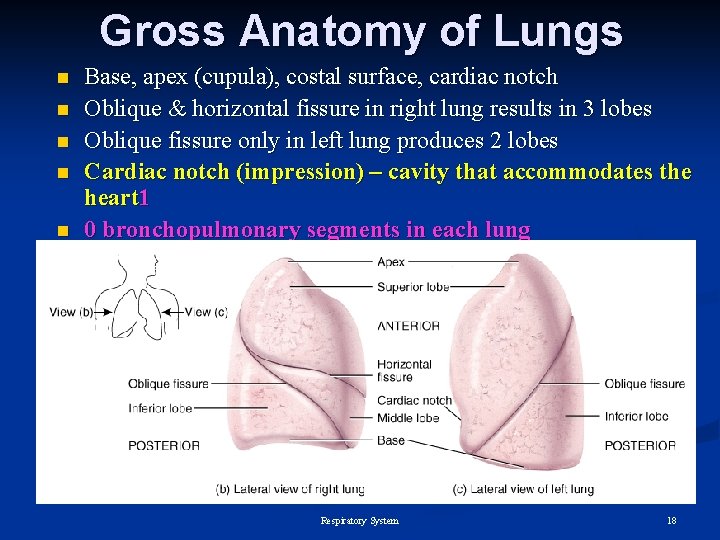
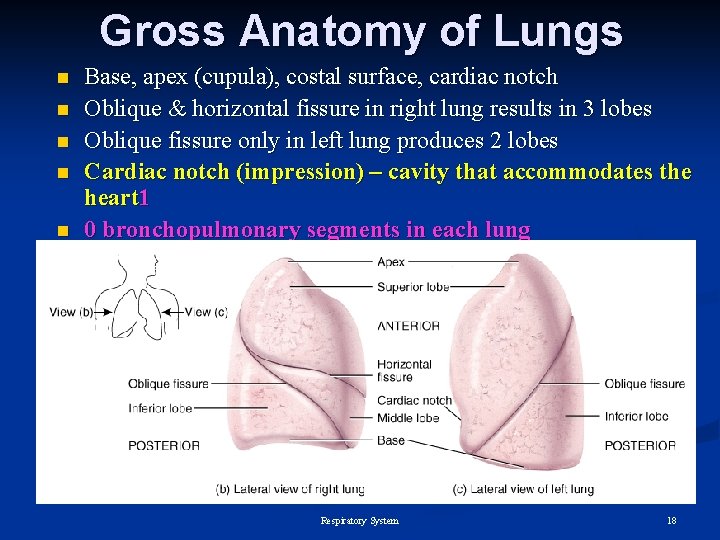
Gross Anatomy of Lungs n n n Base, apex (cupula), costal surface, cardiac notch Oblique & horizontal fissure in right lung results in 3 lobes Oblique fissure only in left lung produces 2 lobes Cardiac notch (impression) – cavity that accommodates the heart 1 0 bronchopulmonary segments in each lung Respiratory System 18
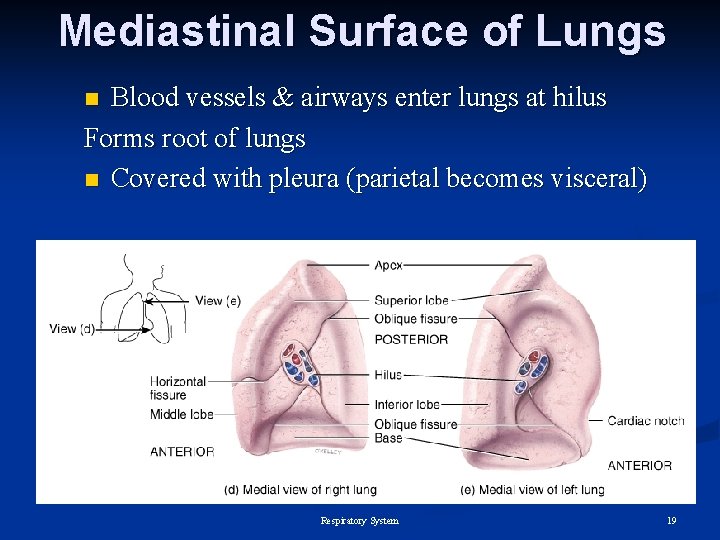
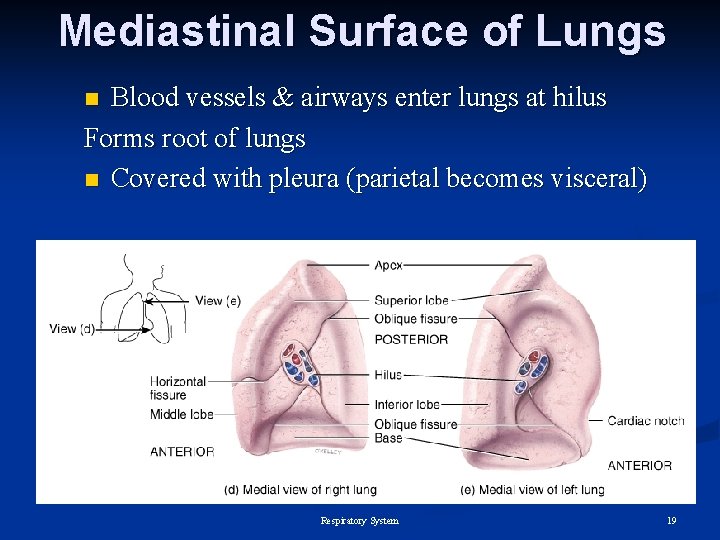
Mediastinal Surface of Lungs Blood vessels & airways enter lungs at hilus Forms root of lungs n Covered with pleura (parietal becomes visceral) n Respiratory System 19
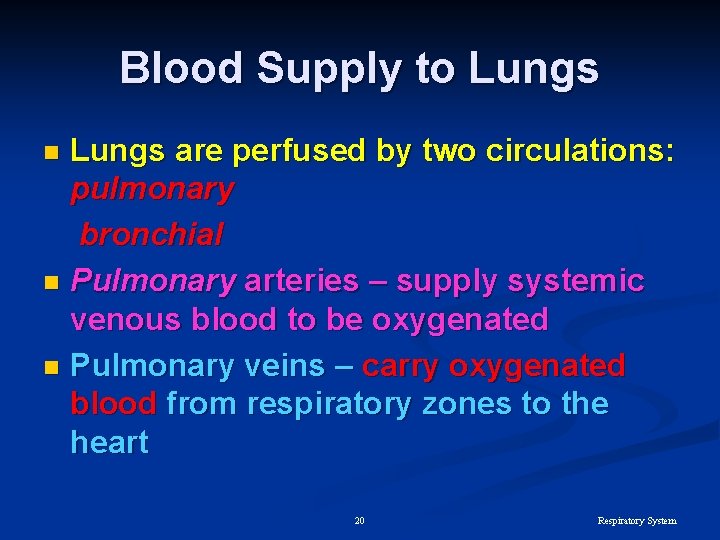
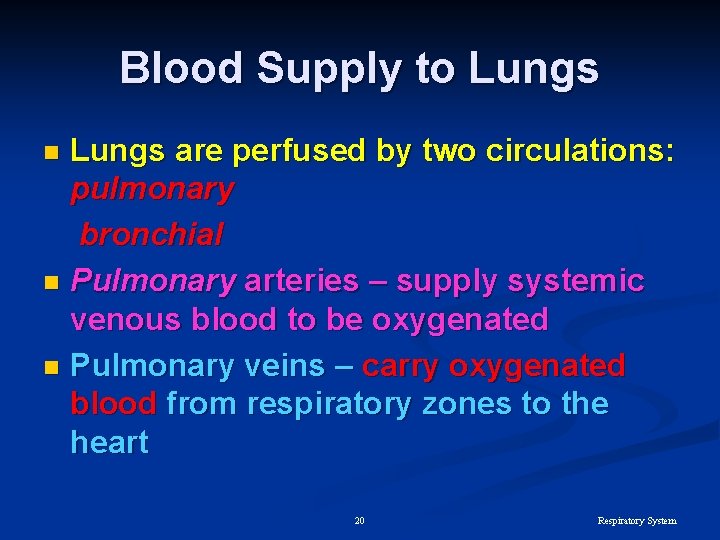
Blood Supply to Lungs are perfused by two circulations: pulmonary bronchial n Pulmonary arteries – supply systemic venous blood to be oxygenated n Pulmonary veins – carry oxygenated blood from respiratory zones to the heart n 20 Respiratory System
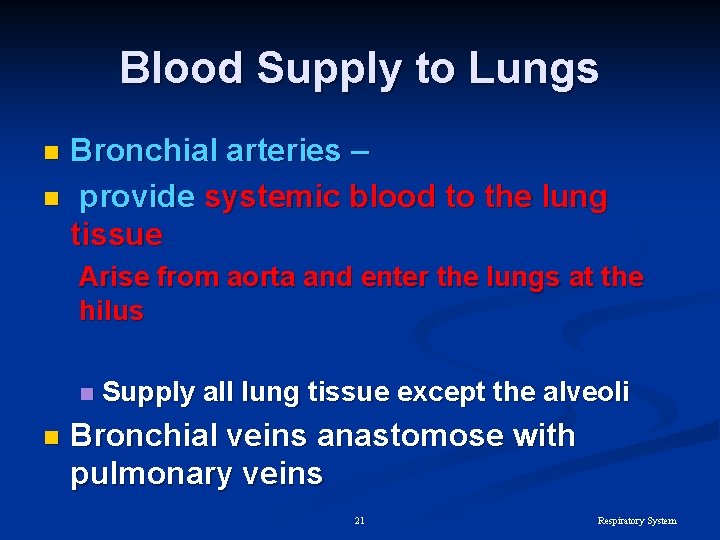
Blood Supply to Lungs Bronchial arteries – n provide systemic blood to the lung tissue n Arise from aorta and enter the lungs at the hilus n n Supply all lung tissue except the alveoli Bronchial veins anastomose with pulmonary veins 21 Respiratory System
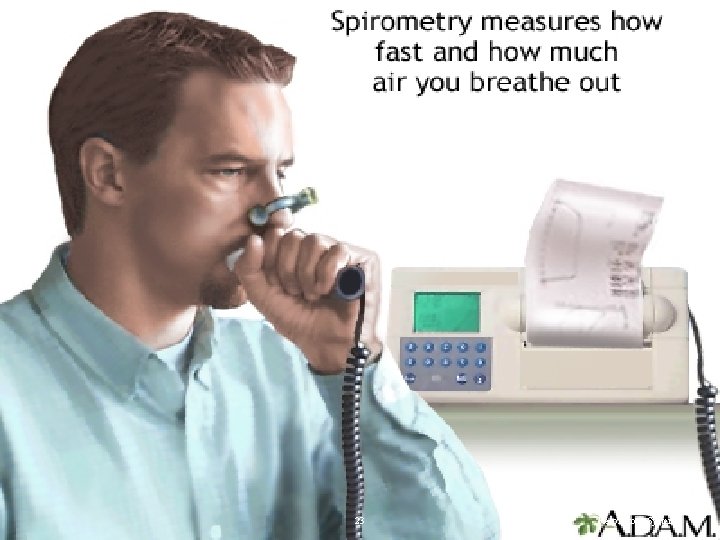
Pulmonary Function Tests Spirometer – an instrument consisting of a hollow bell inverted over water, used to evaluate respiratory function n Spirometry can distinguish between: n Obstructive pulmonary disease – increased airway resistance n Restrictive disorders – reduction in total lung capacity from structural or functional lung changes n 22 Respiratory System
23 Respiratory System
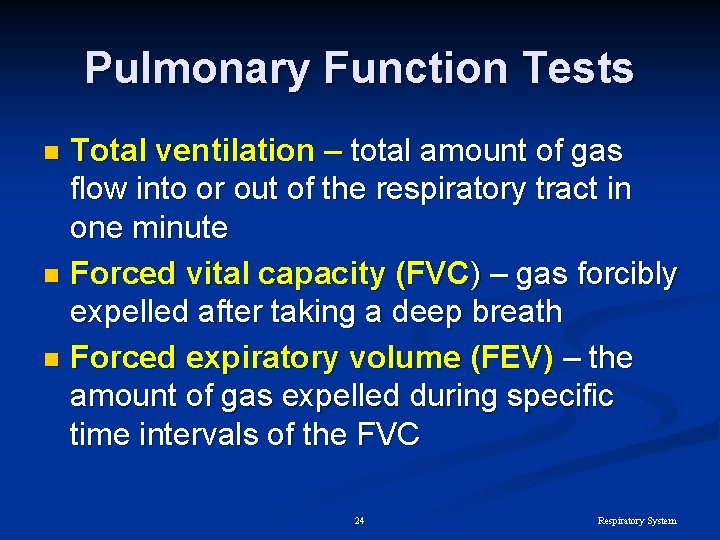
Pulmonary Function Tests Total ventilation – total amount of gas flow into or out of the respiratory tract in one minute n Forced vital capacity (FVC) – gas forcibly expelled after taking a deep breath n Forced expiratory volume (FEV) – the amount of gas expelled during specific time intervals of the FVC n 24 Respiratory System
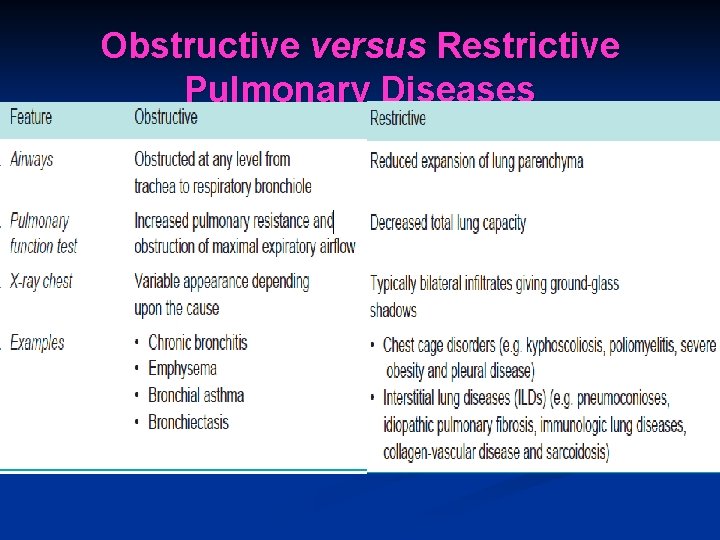
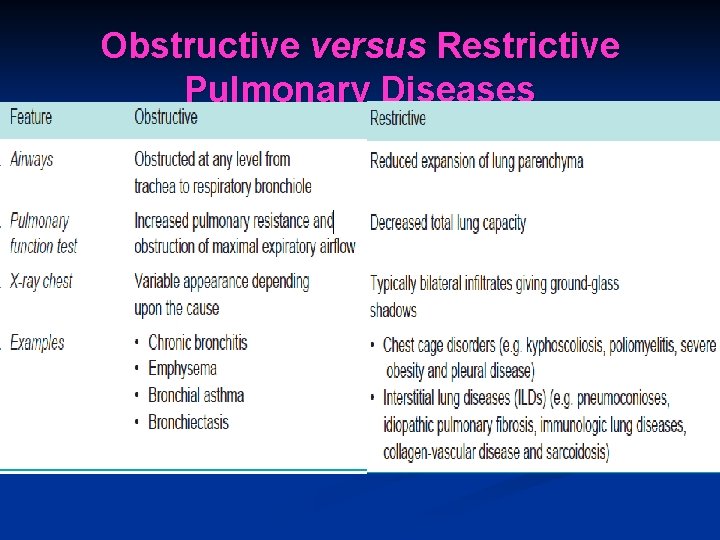
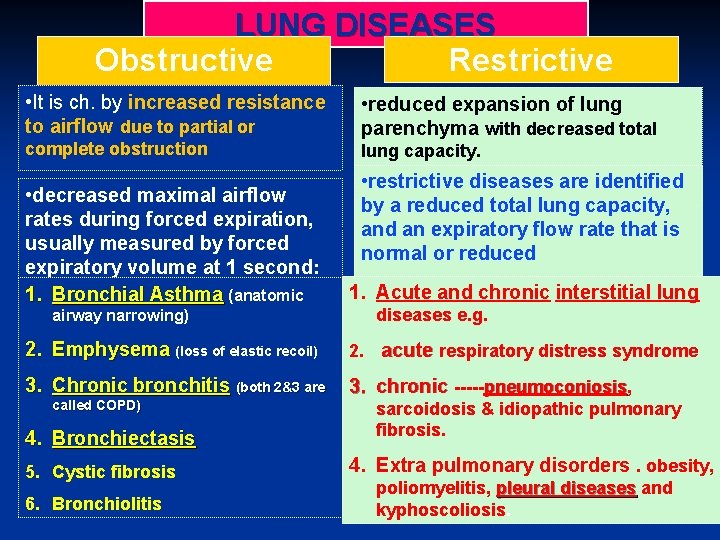
Obstructive versus Restrictive Pulmonary Diseases
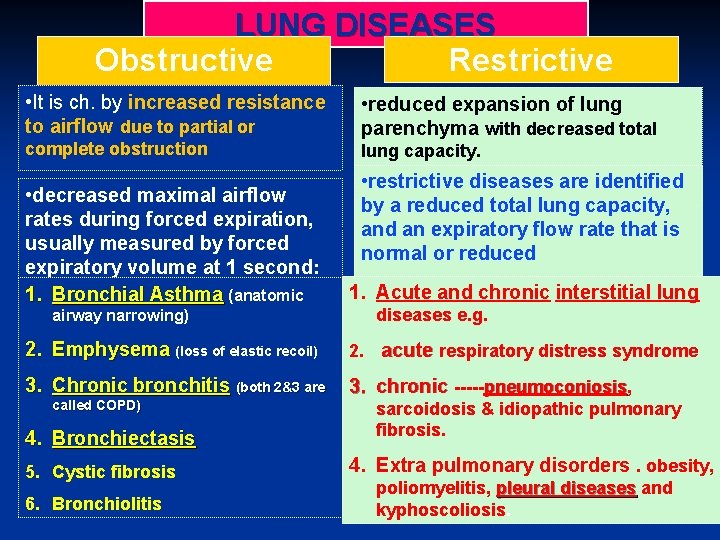
LUNG DISEASES Obstructive Restrictive • It is ch. by Disease increased resistance • reduced expansion of lung to airflow due to partial or complete obstruction • decreased maximal airflow rates during forced expiration, usually measured by forced expiratory volume at 1 second: 1. Bronchial Asthma (anatomic airway narrowing) parenchyma with decreased total lung capacity. • restrictive diseases are identified by a reduced total lung capacity, and an expiratory flow rate that is normal or reduced . interstitial lung 1. proportionately Acute and chronic diseases e. g. 2. Emphysema (loss of elastic recoil) 2. acute respiratory distress syndrome 3. Chronic bronchitis (both 2&3 are 3. chronic -----pneumoconiosis, pneumoconiosis called COPD) 4. Bronchiectasis 5. Cystic fibrosis 6. Bronchiolitis sarcoidosis & idiopathic pulmonary fibrosis. 4. Extra pulmonary disorders. obesity, poliomyelitis, pleural diseases and kyphoscoliosis.

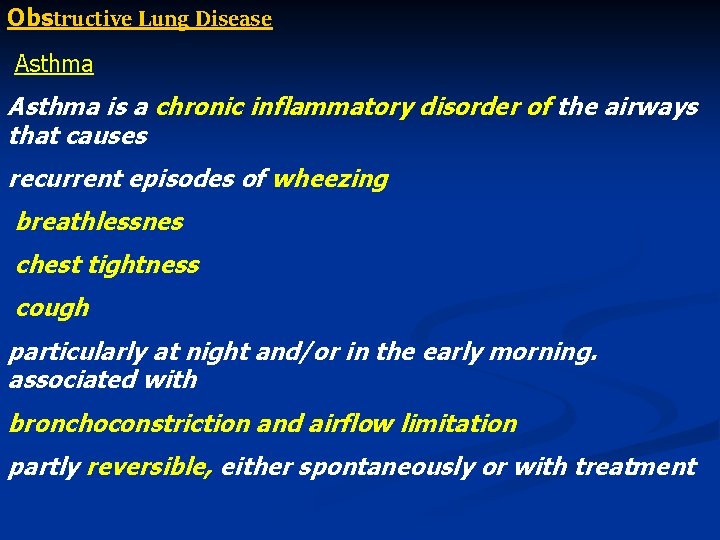
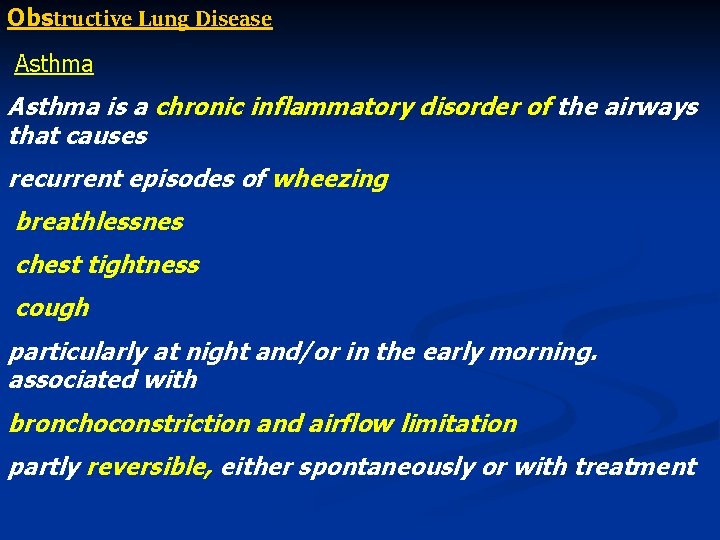
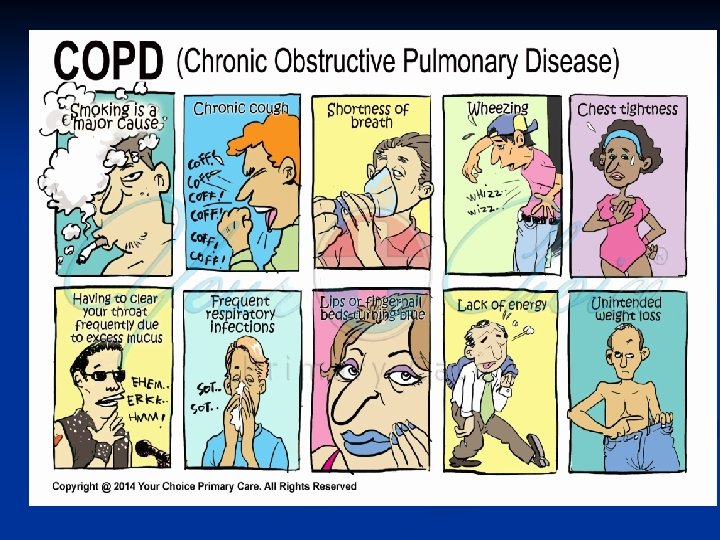
Obstructive Lung Disease Asthma is a chronic inflammatory disorder of the airways that causes recurrent episodes of wheezing breathlessnes chest tightness cough particularly at night and/or in the early morning. associated with bronchoconstriction and airflow limitation partly reversible, either spontaneously or with treatment
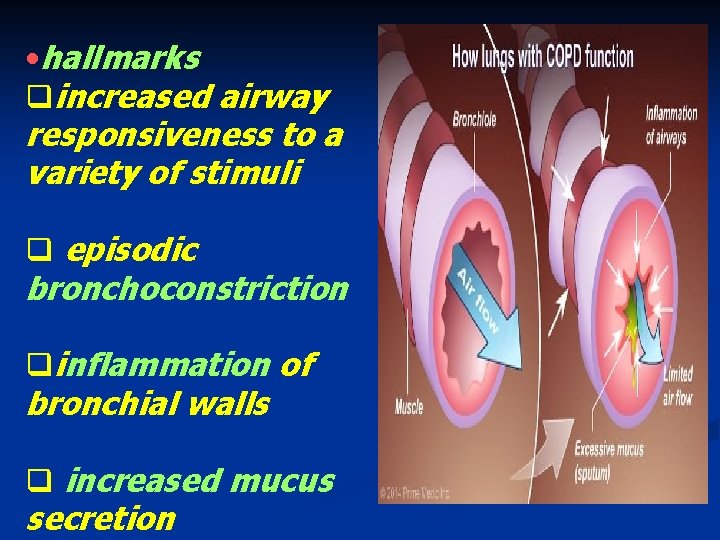
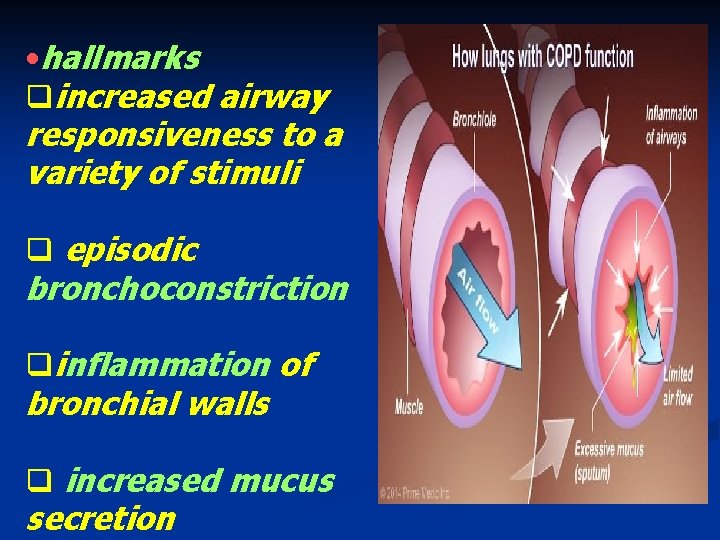
• hallmarks qincreased airway responsiveness to a variety of stimuli q episodic bronchoconstriction qinflammation of bronchial walls q increased mucus secretion
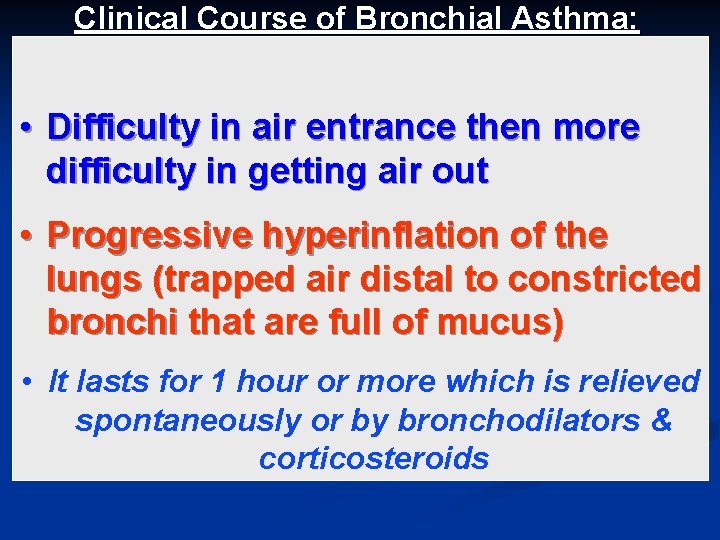
Clinical Course of Bronchial Asthma: • Difficulty in air entrance then more difficulty in getting air out • Progressive hyperinflation of the lungs (trapped air distal to constricted bronchi that are full of mucus) • It lasts for 1 hour or more which is relieved spontaneously or by bronchodilators & corticosteroids
status asthmaticus – a state of unremitting attacks, -----the severe acute paroxysm persists for days and even weeks, airflow obstruction might be so extreme ----cause severe cyanosis and fatal outcome between attacks asymptomatic
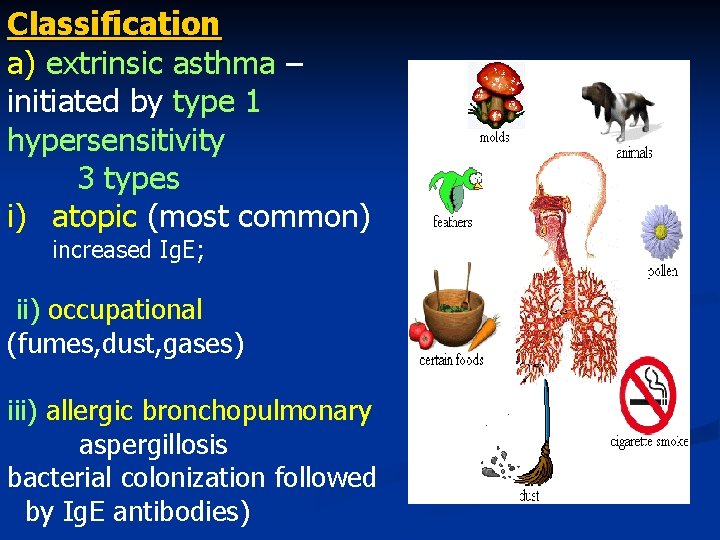
Classification a) extrinsic asthma – initiated by type 1 hypersensitivity 3 types i) atopic (most common) increased Ig. E; ii) occupational (fumes, dust, gases) iii) allergic bronchopulmonary aspergillosis bacterial colonization followed by Ig. E antibodies)
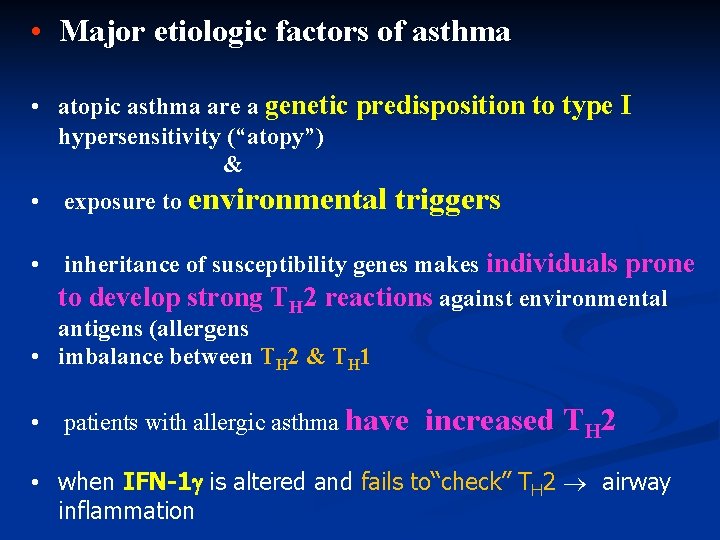
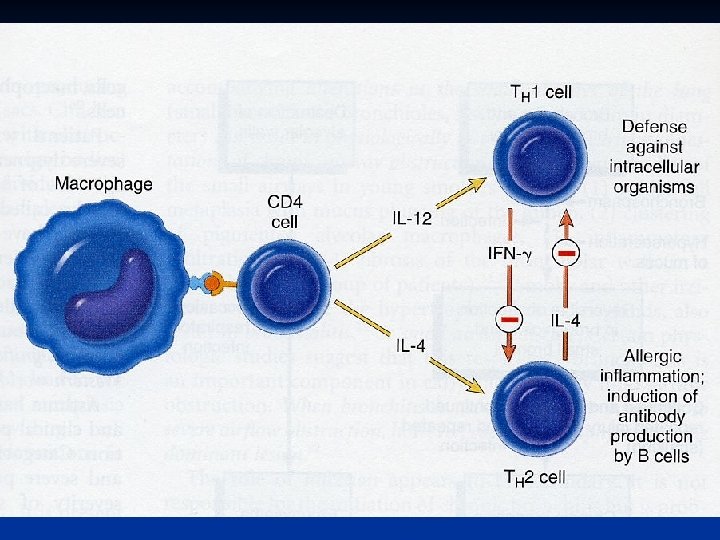
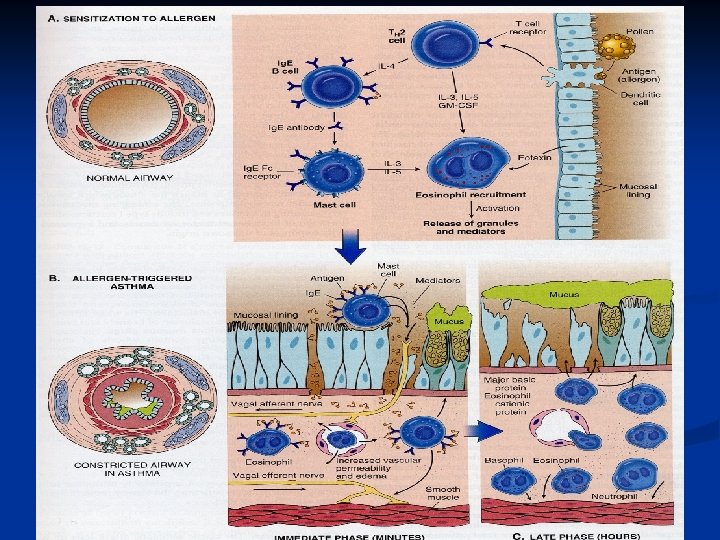
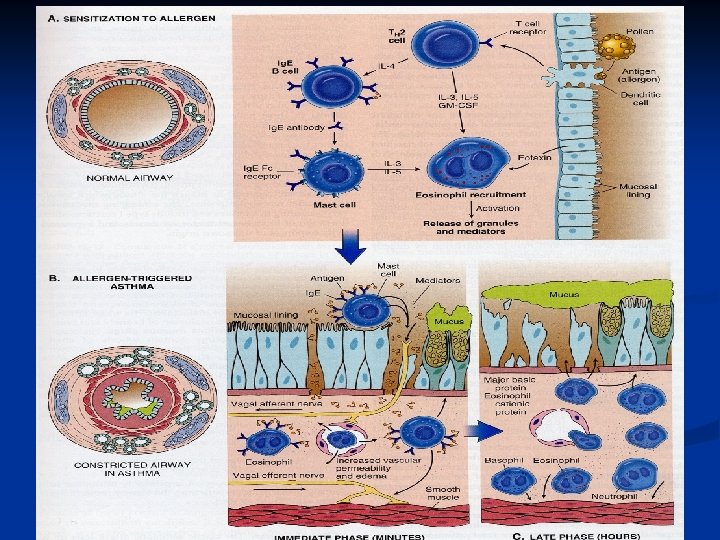
• Major etiologic factors of asthma • atopic asthma are a genetic predisposition to type I hypersensitivity (“atopy”) & • exposure to environmental triggers • inheritance of susceptibility genes makes individuals prone to develop strong TH 2 reactions against environmental antigens (allergens • imbalance between TH 2 & TH 1 • patients with allergic asthma have increased TH 2 • when IFN-1 is altered and fails to“check” TH 2 airway inflammation
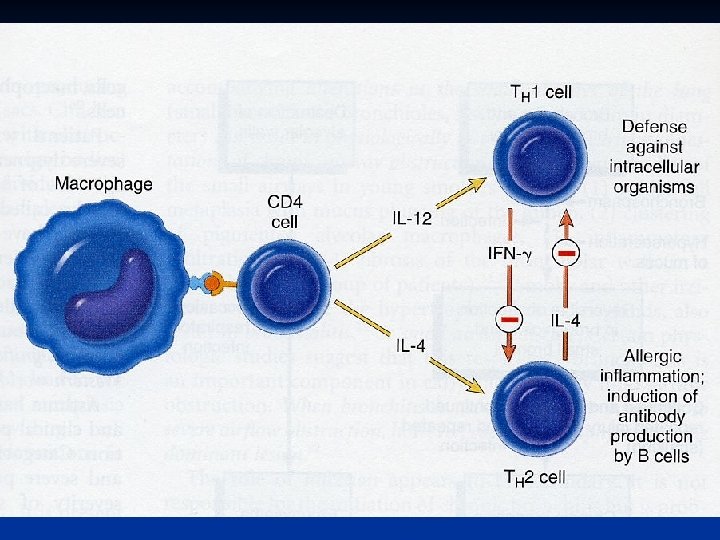
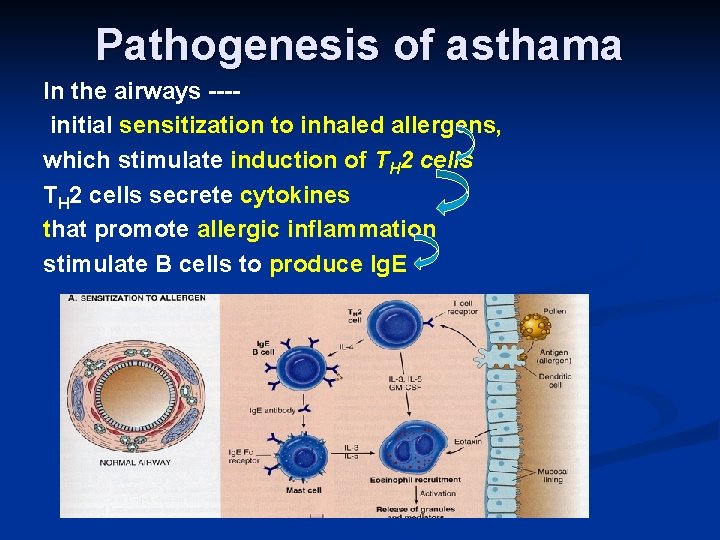
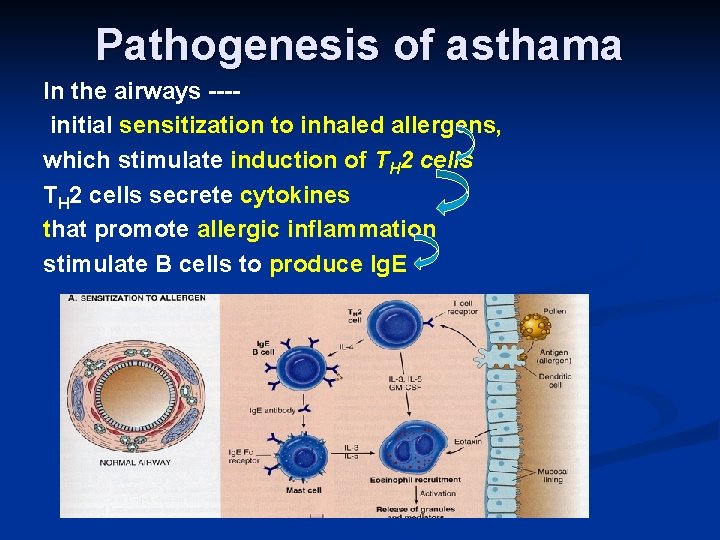
Pathogenesis of asthama In the airways ---initial sensitization to inhaled allergens, which stimulate induction of TH 2 cells secrete cytokines that promote allergic inflammation stimulate B cells to produce Ig. E
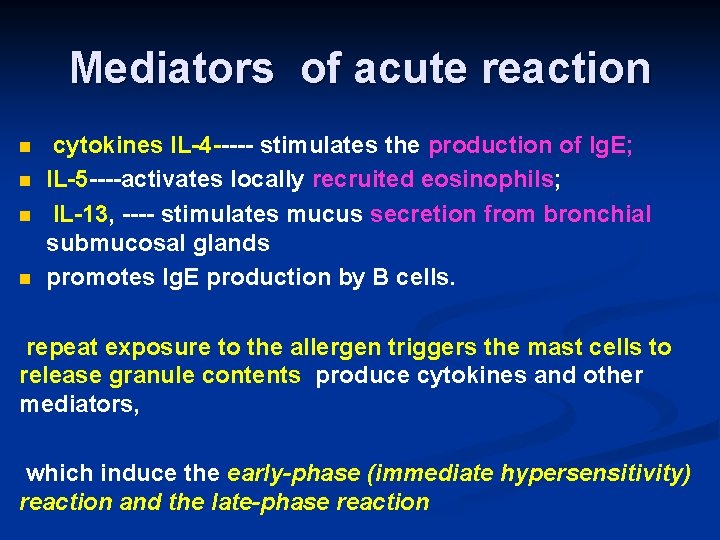
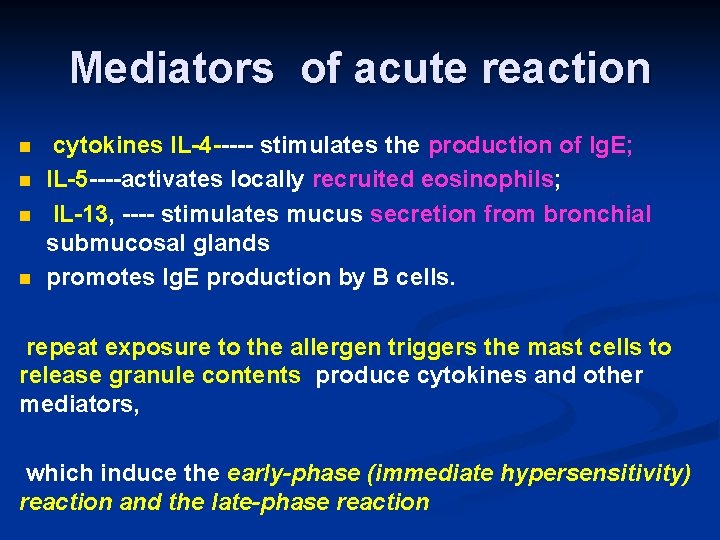
Mediators of acute reaction n n cytokines IL-4 ----- stimulates the production of Ig. E; IL-5 ----activates locally recruited eosinophils; IL-13, ---- stimulates mucus secretion from bronchial submucosal glands promotes Ig. E production by B cells. repeat exposure to the allergen triggers the mast cells to release granule contents produce cytokines and other mediators, which induce the early-phase (immediate hypersensitivity) reaction and the late-phase reaction
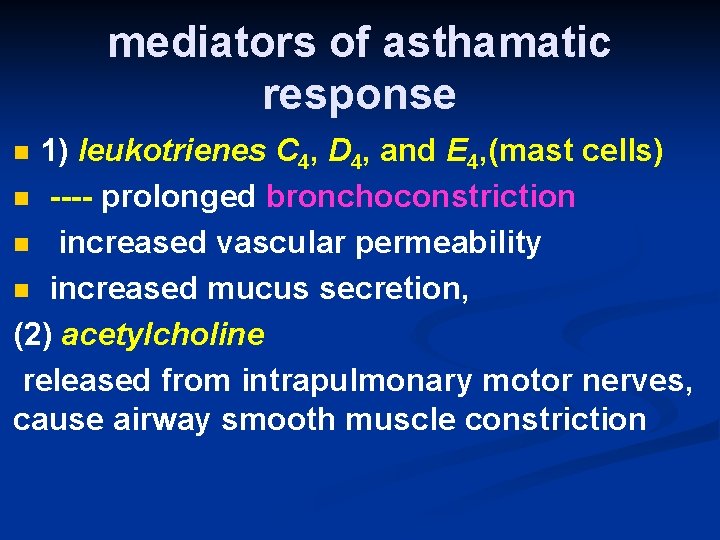
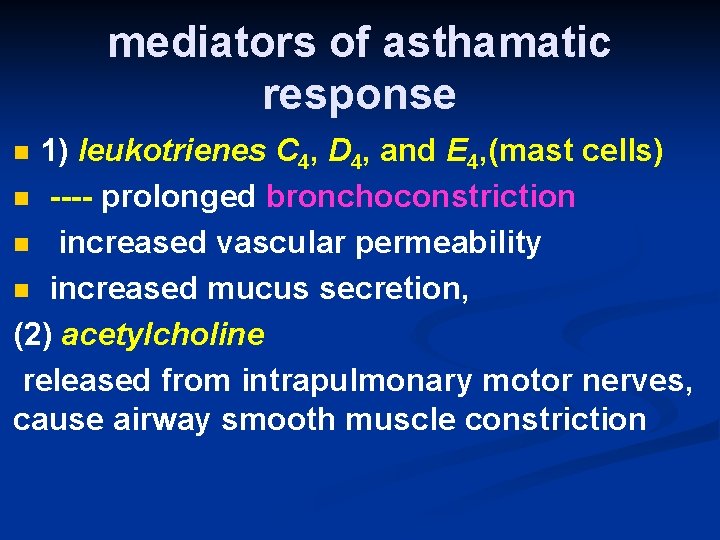
mediators of asthamatic response 1) leukotrienes C 4, D 4, and E 4, (mast cells) n ---- prolonged bronchoconstriction n increased vascular permeability n increased mucus secretion, (2) acetylcholine released from intrapulmonary motor nerves, cause airway smooth muscle constriction n
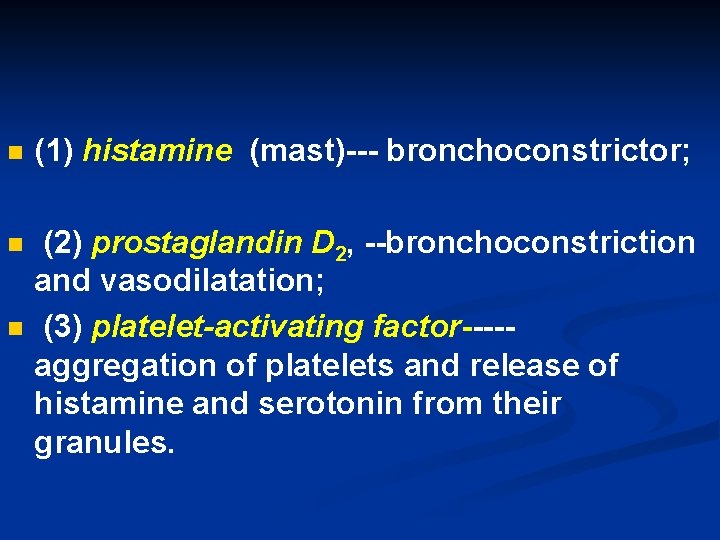
n (1) histamine (mast)--- bronchoconstrictor; n (2) prostaglandin D 2, --bronchoconstriction and vasodilatation; (3) platelet-activating factor----aggregation of platelets and release of histamine and serotonin from their granules. n
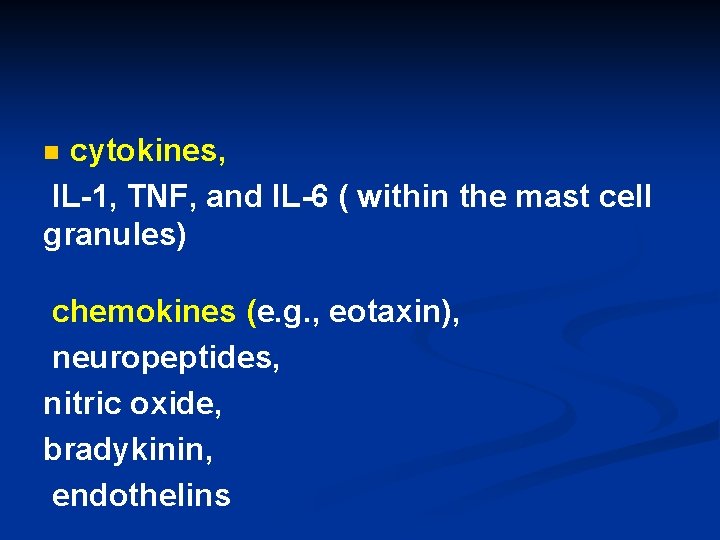
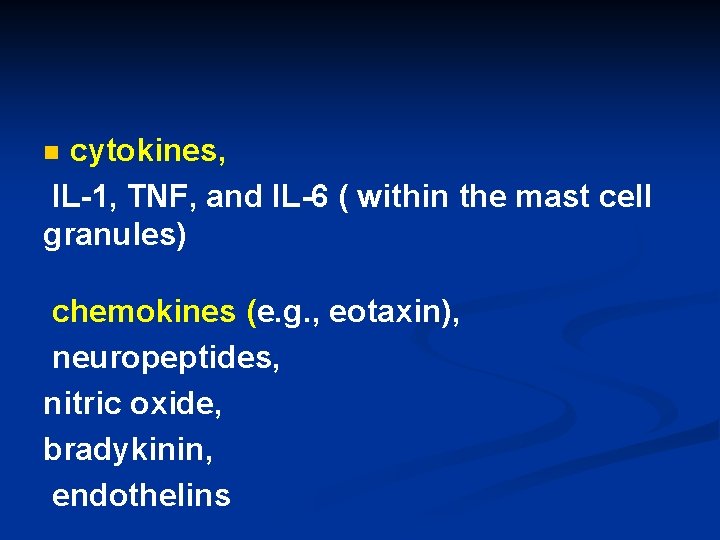
cytokines, IL-1, TNF, and IL-6 ( within the mast cell granules) n chemokines (e. g. , eotaxin), neuropeptides, nitric oxide, bradykinin, endothelins
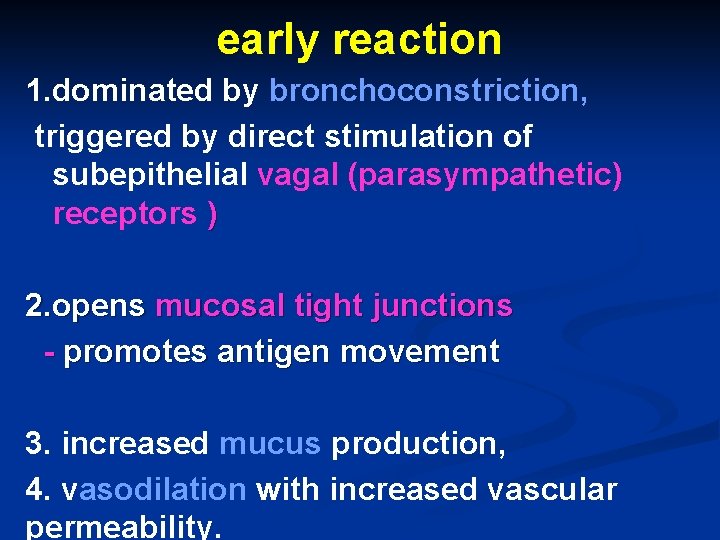
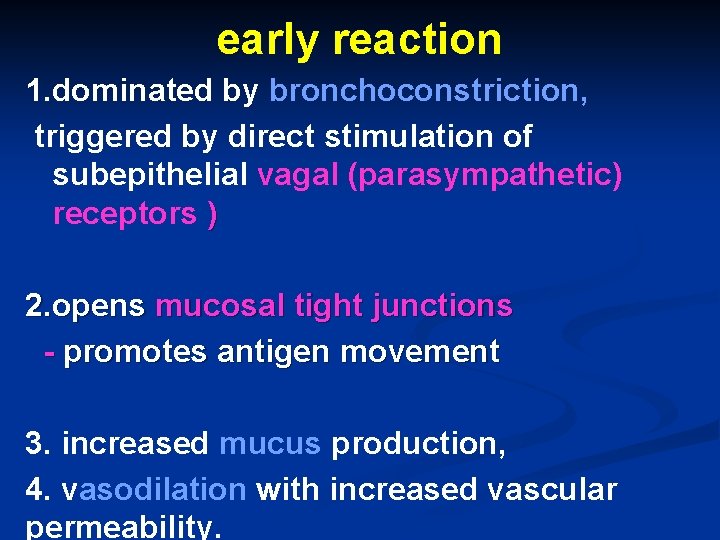
early reaction 1. dominated by bronchoconstriction, triggered by direct stimulation of subepithelial vagal (parasympathetic) receptors ) 2. opens mucosal tight junctions - promotes antigen movement 3. increased mucus production, 4. vasodilation with increased vascular permeability.
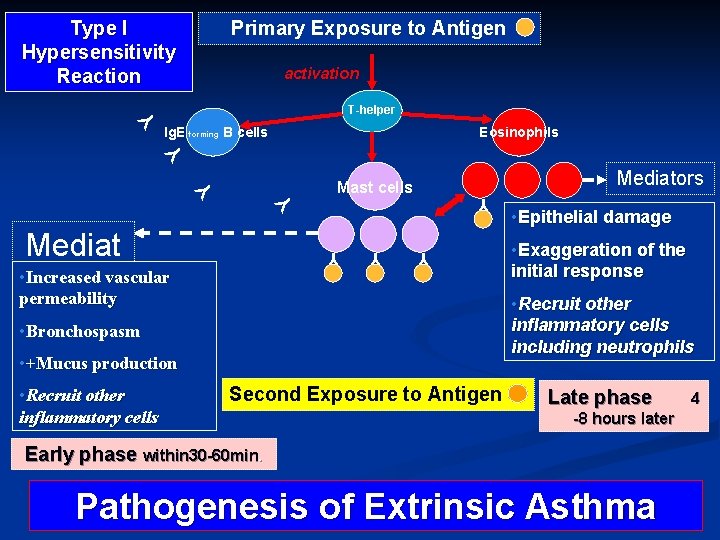
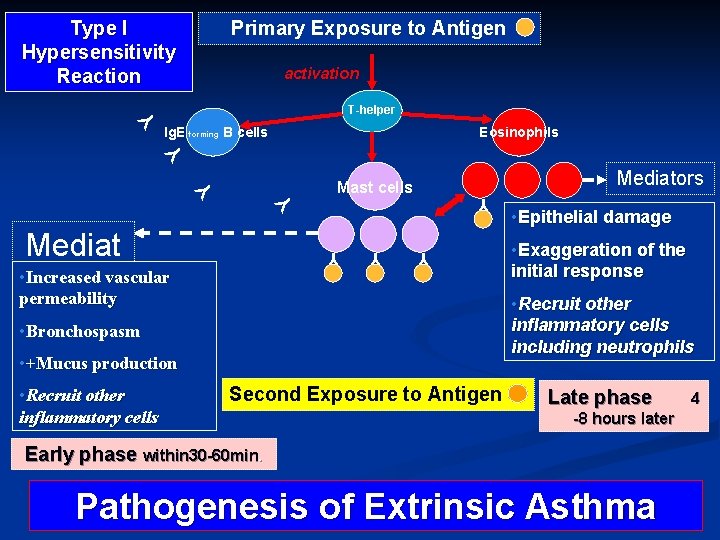
Type I Hypersensitivity Reaction Primary Exposure to Antigen activation Y T-helper Eosinophils Y Y Y Mediat • Increased vascular oors permeability Mediators Mast cells Y Y Y Ig. E forming B cells • Exaggeration of the initial response Y • Recruit other inflammatory cells including neutrophils • Bronchospasm • +Mucus production • Recruit other inflammatory cells • Epithelial damage Second Exposure to Antigen Late phase -8 hours later Early phase within 30 -60 min. Pathogenesis of Extrinsic Asthma 4
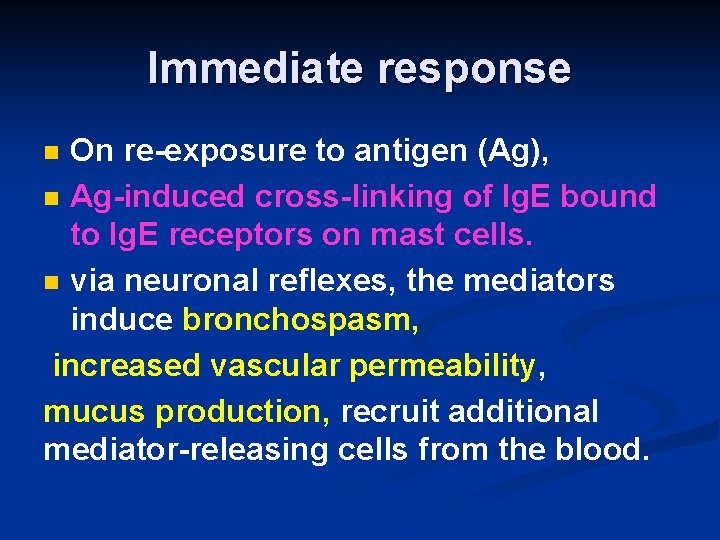
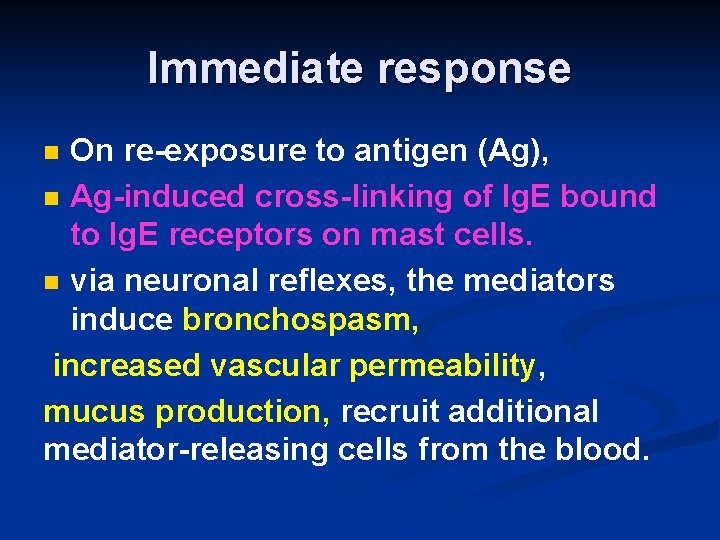
Immediate response On re-exposure to antigen (Ag), n Ag-induced cross-linking of Ig. E bound to Ig. E receptors on mast cells. n via neuronal reflexes, the mediators induce bronchospasm, increased vascular permeability, mucus production, recruit additional mediator-releasing cells from the blood. n
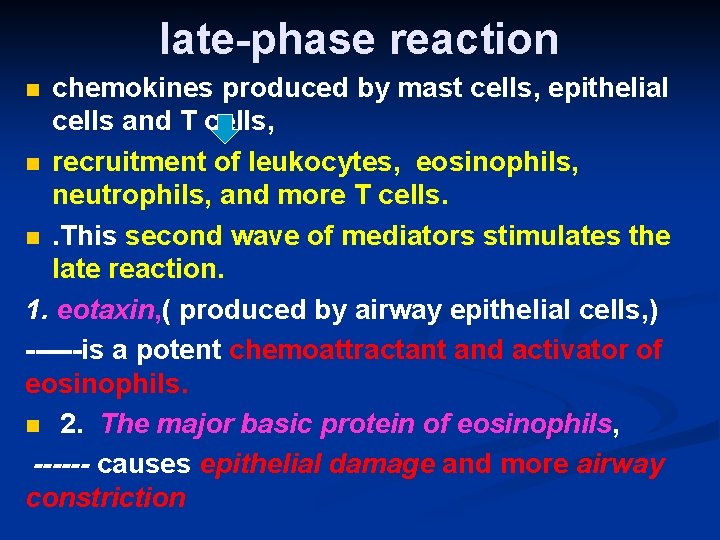
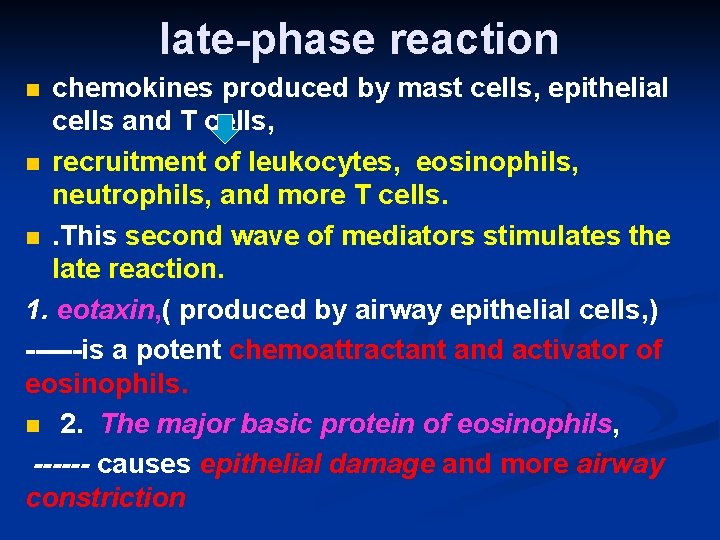
late-phase reaction chemokines produced by mast cells, epithelial cells and T cells, n recruitment of leukocytes, eosinophils, neutrophils, and more T cells. n. This second wave of mediators stimulates the late reaction. 1. eotaxin, ( produced by airway epithelial cells, ) ------is a potent chemoattractant and activator of eosinophils. n 2. The major basic protein of eosinophils, ------ causes epithelial damage and more airway constriction n
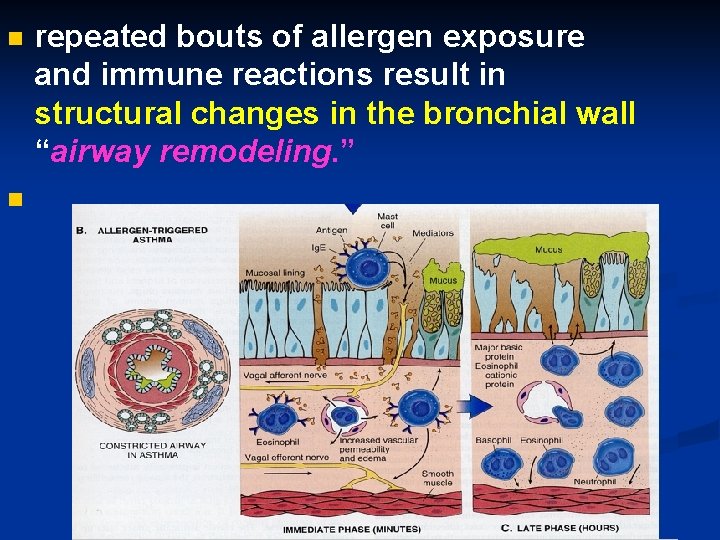
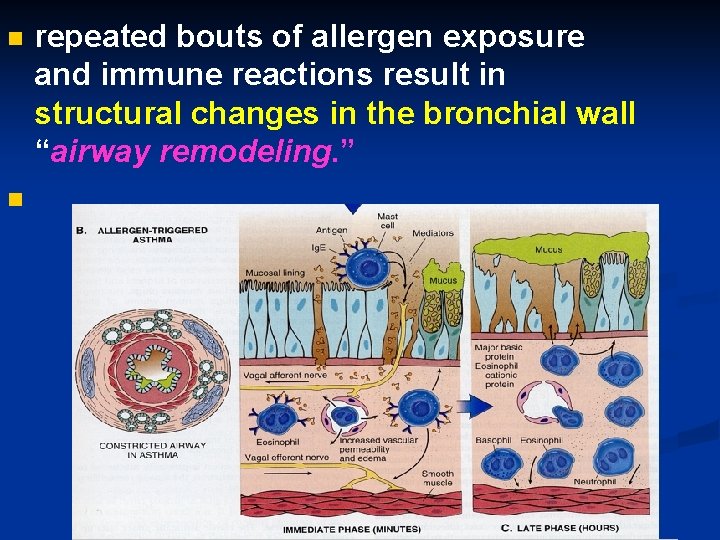
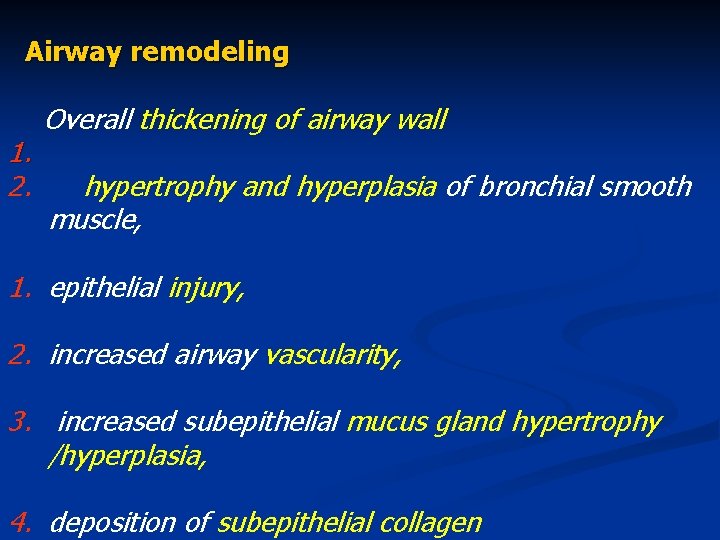
n n repeated bouts of allergen exposure and immune reactions result in structural changes in the bronchial wall “airway remodeling. ”
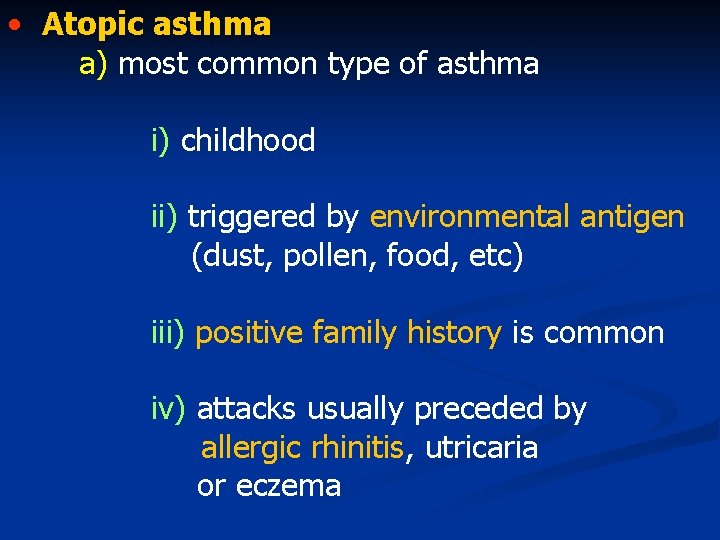
• Atopic asthma a) most common type of asthma i) childhood ii) triggered by environmental antigen (dust, pollen, food, etc) iii) positive family history is common iv) attacks usually preceded by allergic rhinitis, utricaria or eczema
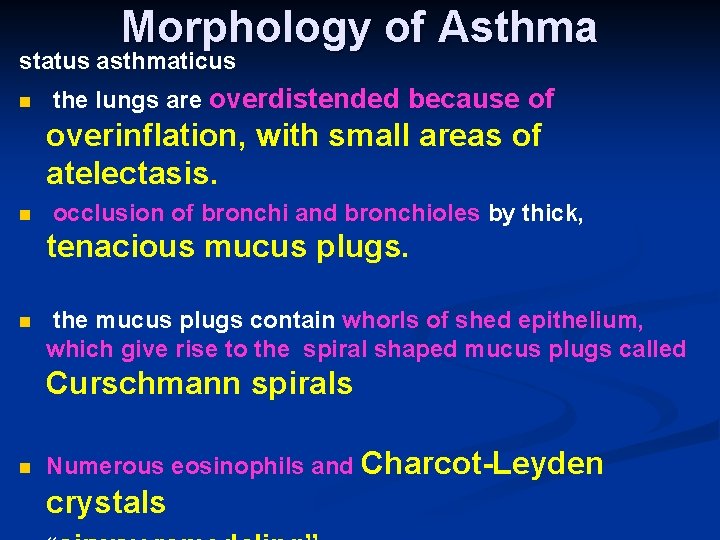
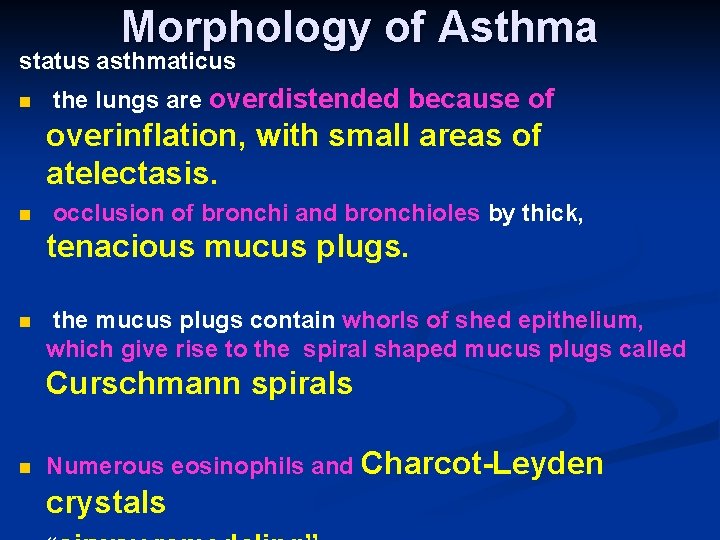
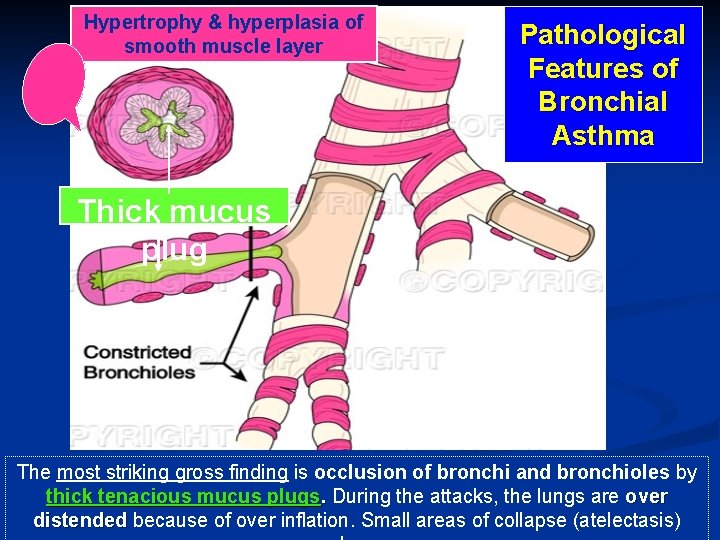
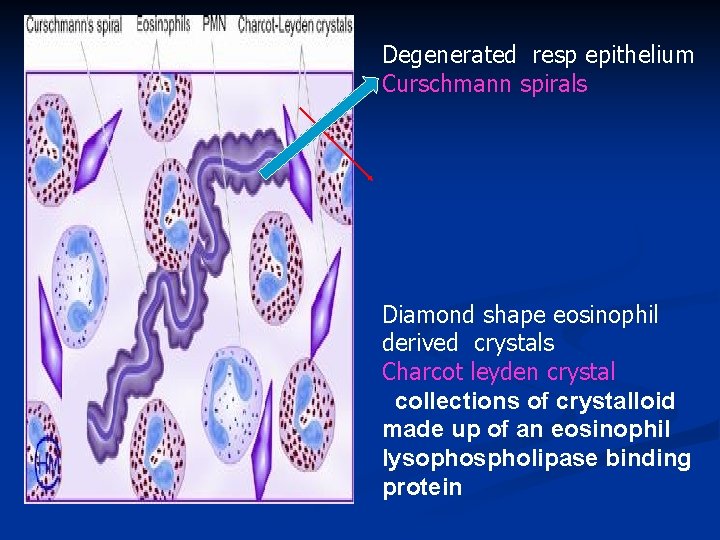
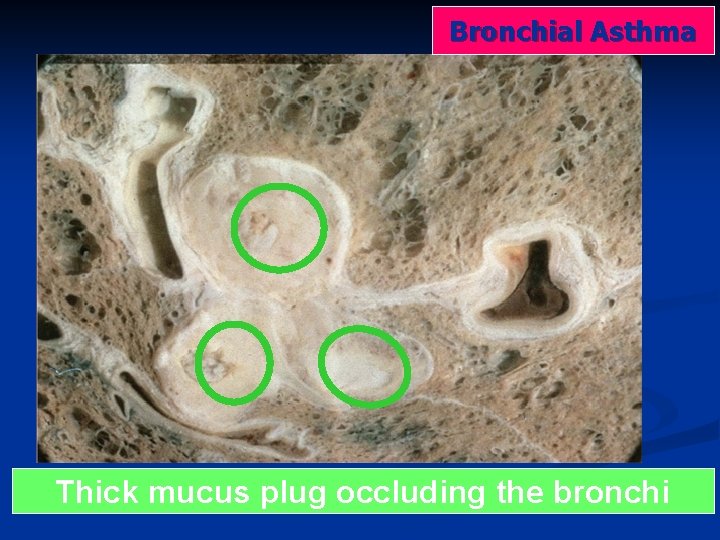
Morphology of Asthma status asthmaticus n the lungs are overdistended because of overinflation, with small areas of atelectasis. n occlusion of bronchi and bronchioles by thick, tenacious mucus plugs. n the mucus plugs contain whorls of shed epithelium, which give rise to the spiral shaped mucus plugs called Curschmann spirals n Numerous eosinophils and Charcot-Leyden crystals
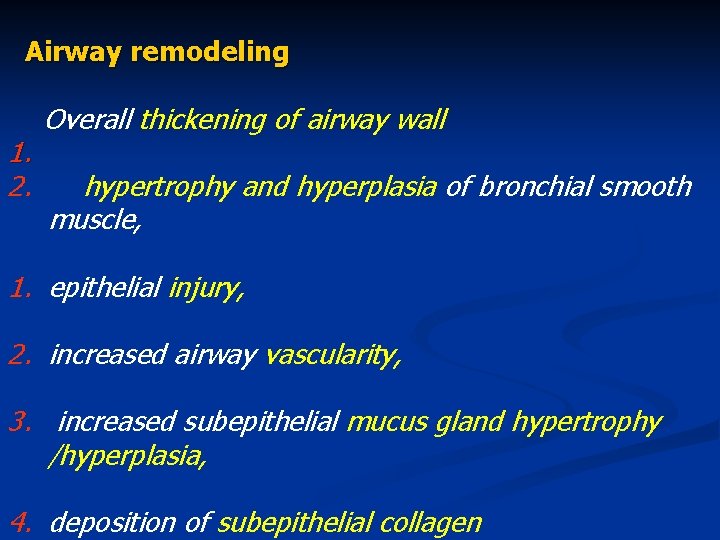
Airway remodeling 1. 2. Overall thickening of airway wall hypertrophy and hyperplasia of bronchial smooth muscle, 1. epithelial injury, 2. increased airway vascularity, 3. increased subepithelial mucus gland hypertrophy /hyperplasia, 4. deposition of subepithelial collagen
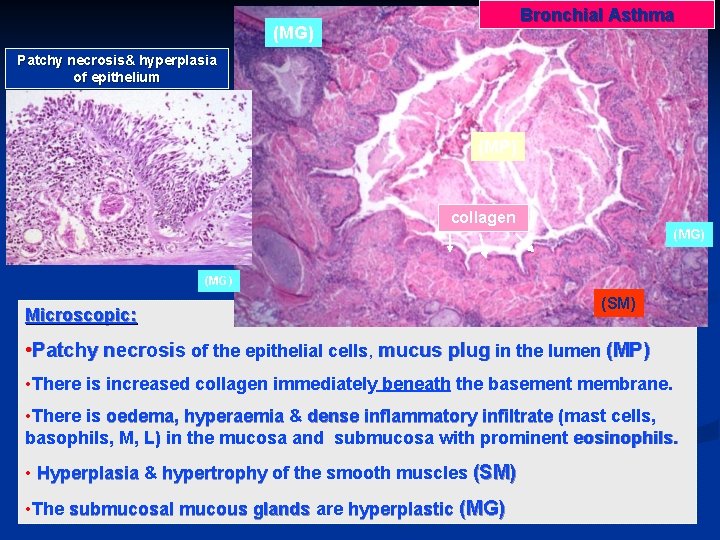
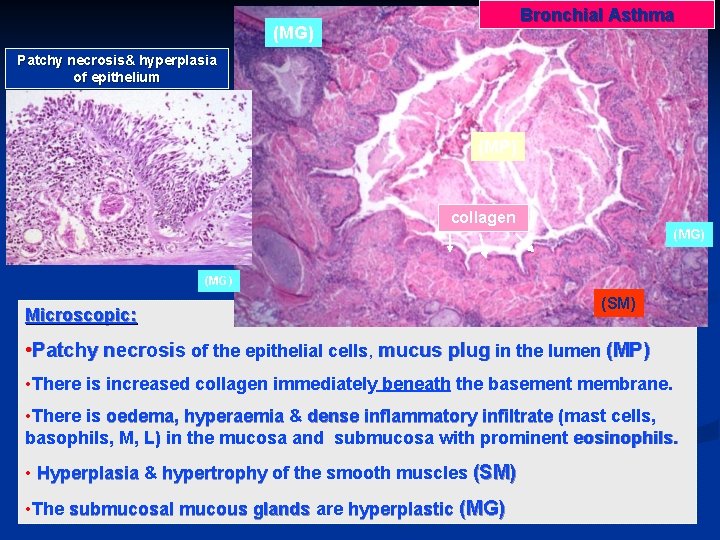
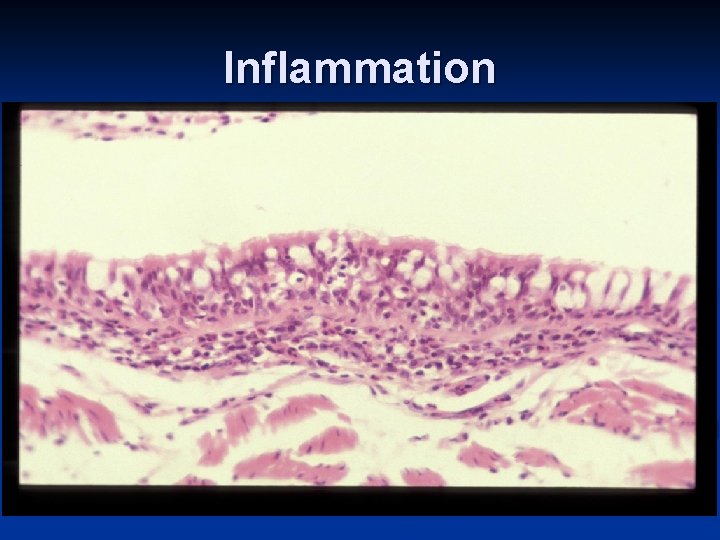
Bronchial Asthma (MG) Patchy necrosis& hyperplasia of epithelium (MP) collagen (MG) Microscopic: (SM) • Patchy necrosis of the epithelial cells, mucus plug in the lumen (MP) • There is increased collagen immediately beneath the basement membrane. • There is oedema, hyperaemia & dense inflammatory infiltrate (mast cells, basophils, M, L) in the mucosa and submucosa with prominent eosinophils. • Hyperplasia & hypertrophy of the smooth muscles (SM) • The submucosal mucous glands are hyperplastic (MG)
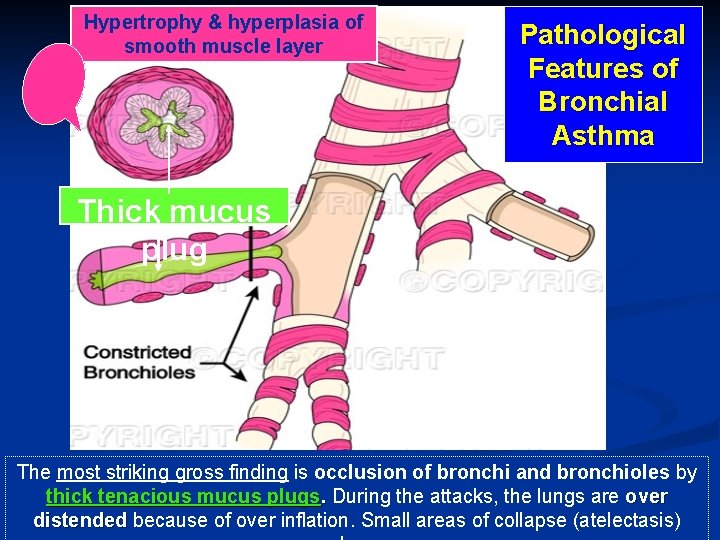
Hypertrophy & hyperplasia of smooth muscle layer Pathological Features of Bronchial Asthma Thick mucus plug The most striking gross finding is occlusion of bronchi and bronchioles by thick tenacious mucus plugs. During the attacks, the lungs are over distended because of over inflation. Small areas of collapse (atelectasis)
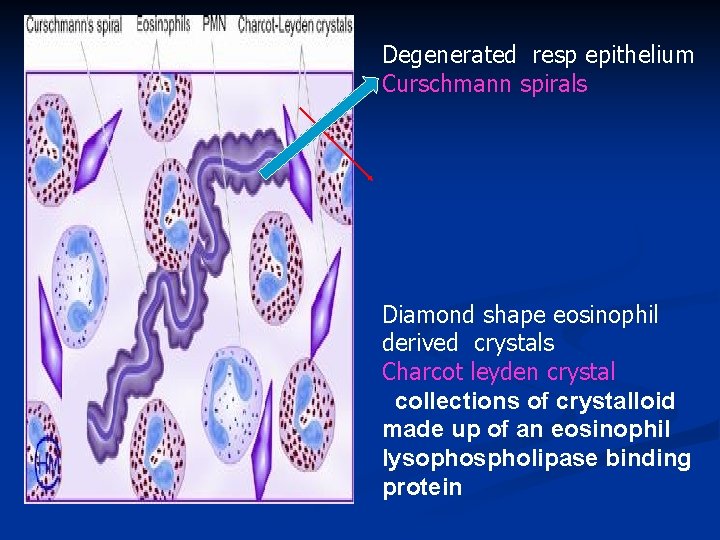
Degenerated resp epithelium Curschmann spirals Diamond shape eosinophil derived crystals Charcot leyden crystal collections of crystalloid made up of an eosinophil lysophospholipase binding protein
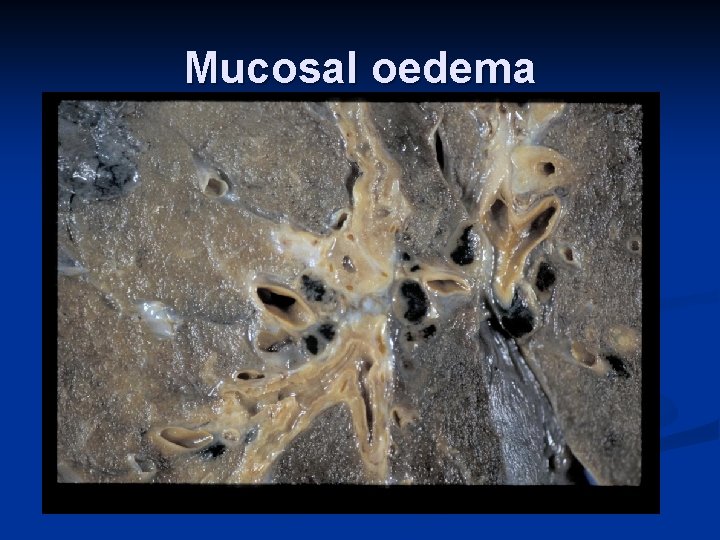
Mucosal oedema
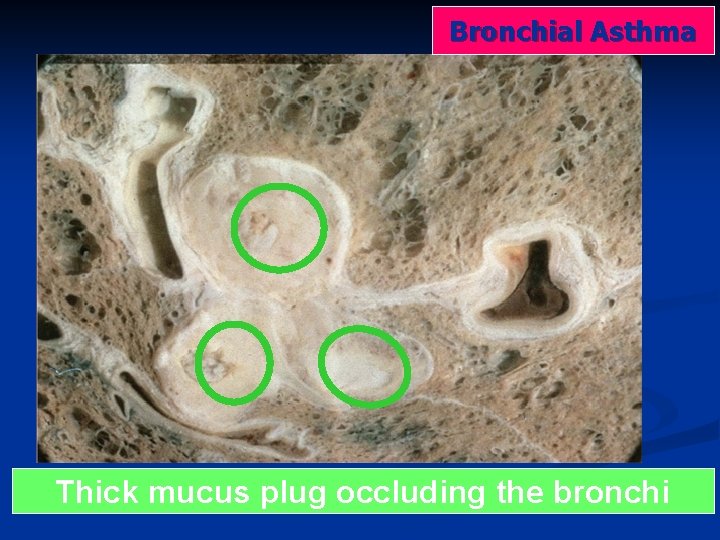
Bronchial Asthma Thick mucus plug occluding the bronchi
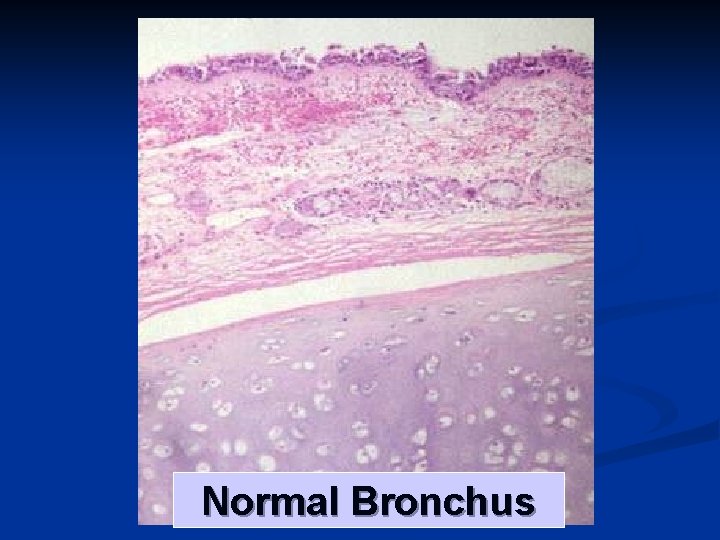
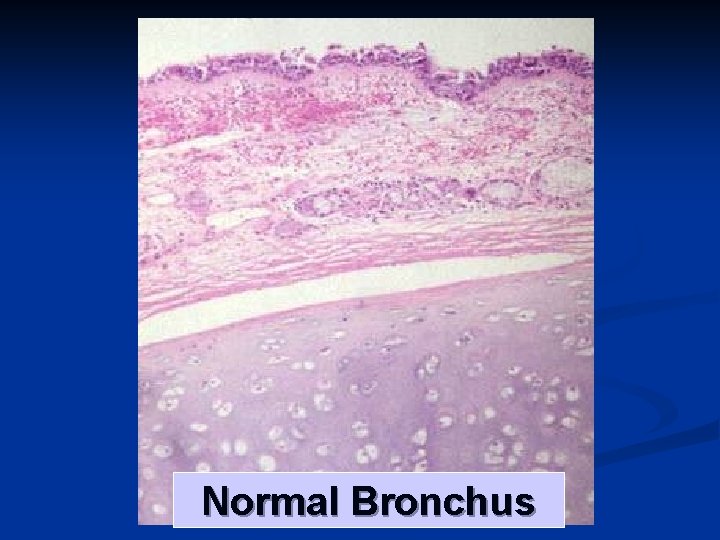
Normal Bronchus
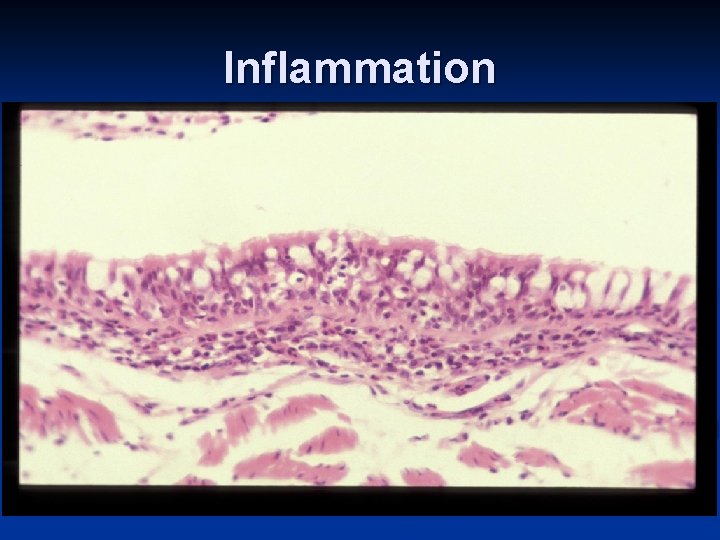
Inflammation
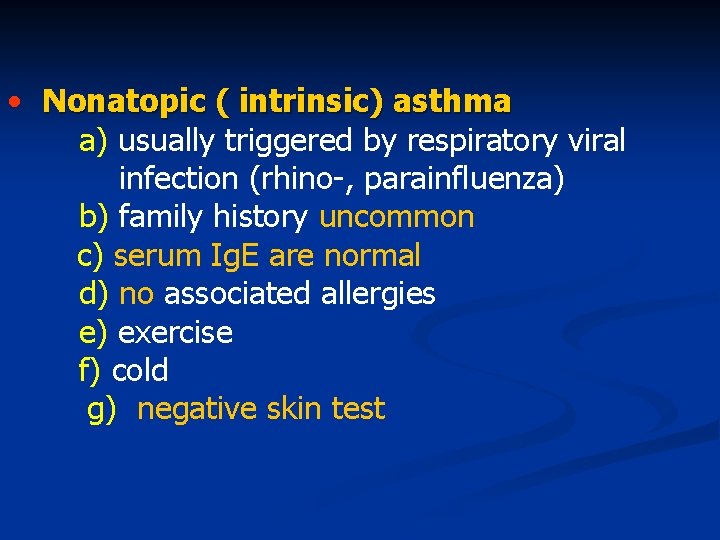
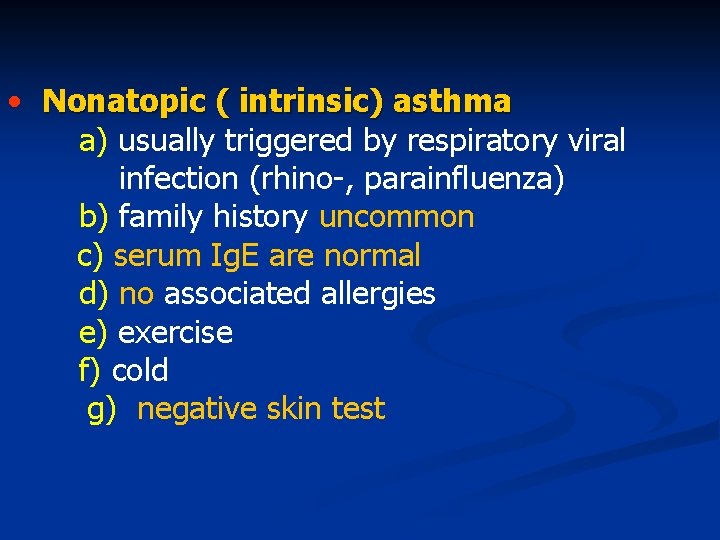
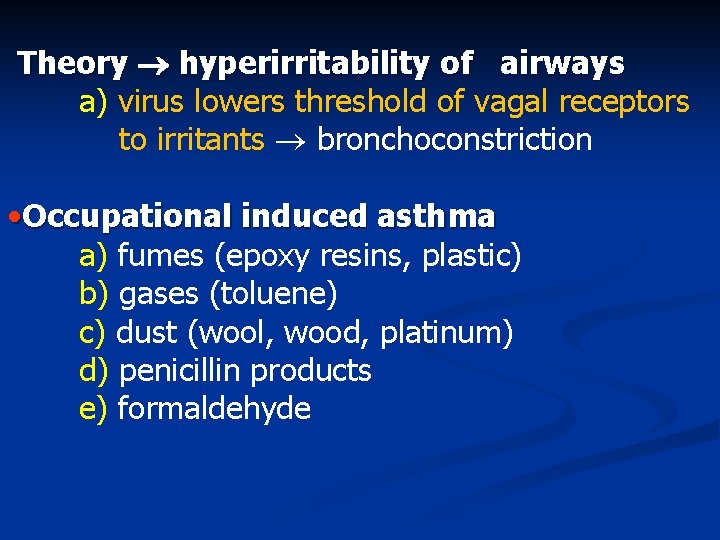
• Nonatopic ( intrinsic) asthma a) usually triggered by respiratory viral infection (rhino-, parainfluenza) b) family history uncommon c) serum Ig. E are normal d) no associated allergies e) exercise f) cold g) negative skin test
Theory hyperirritability of airways a) virus lowers threshold of vagal receptors to irritants bronchoconstriction • Occupational induced asthma a) fumes (epoxy resins, plastic) b) gases (toluene) c) dust (wool, wood, platinum) d) penicillin products e) formaldehyde
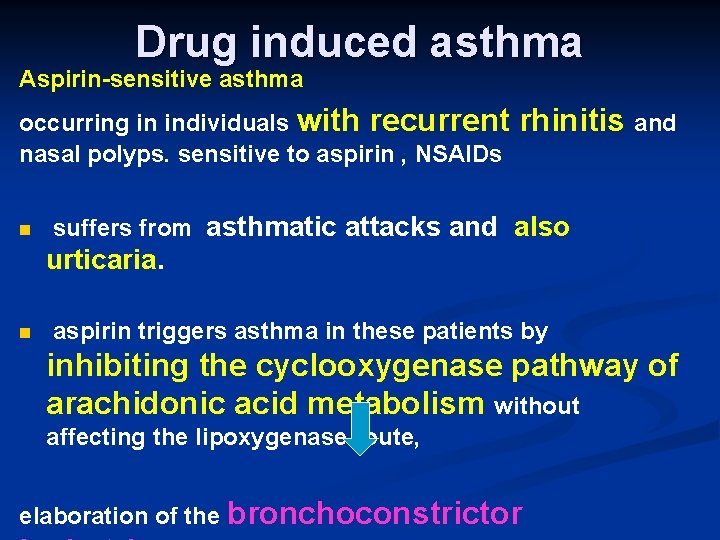
Drug induced asthma Aspirin-sensitive asthma occurring in individuals with recurrent nasal polyps. sensitive to aspirin , NSAIDs n rhinitis and suffers from asthmatic attacks and also urticaria. n aspirin triggers asthma in these patients by inhibiting the cyclooxygenase pathway of arachidonic acid metabolism without affecting the lipoxygenase route, elaboration of the bronchoconstrictor
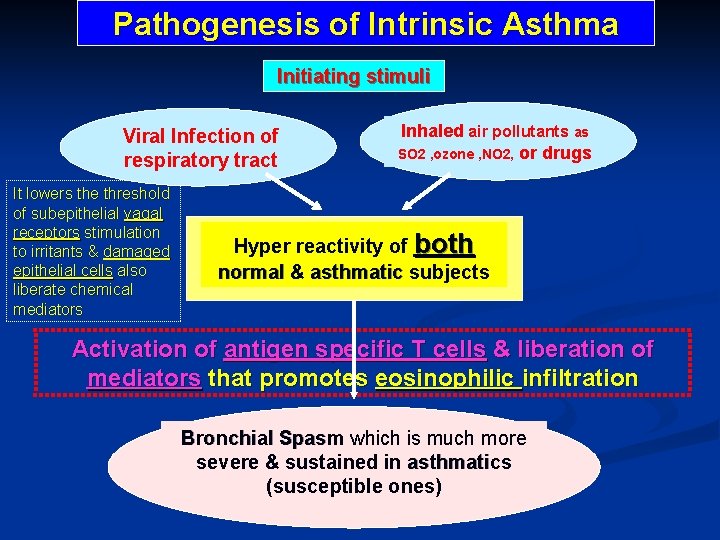
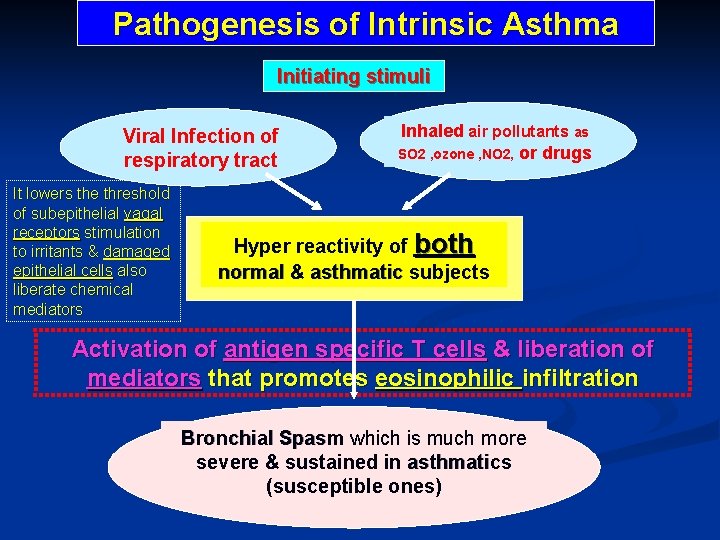
Pathogenesis of Intrinsic Asthma Initiating stimuli Viral Infection of respiratory tract It lowers the threshold of subepithelial vagal receptors stimulation to irritants & damaged epithelial cells also liberate chemical mediators Inhaled air pollutants as SO 2 , ozone , NO 2, or drugs Hyper reactivity of both normal & asthmatic subjects Activation of antigen specific T cells & liberation of mediators that promotes eosinophilic infiltration Bronchial Spasm which is much more severe & sustained in asthmatics (susceptible ones)
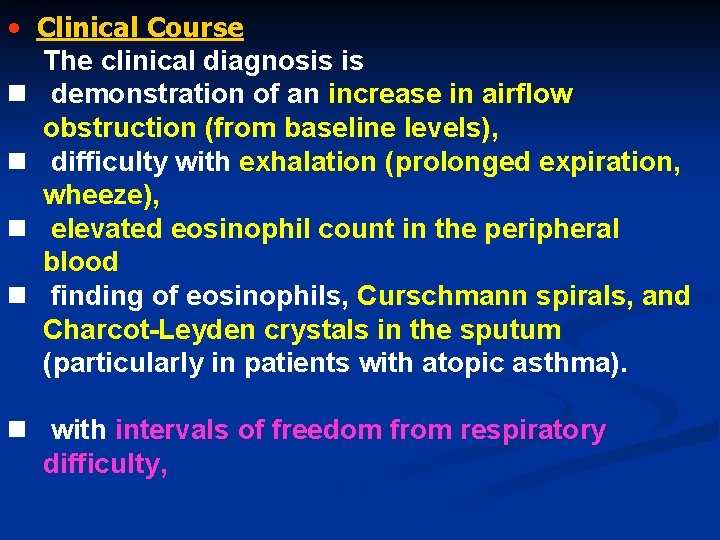
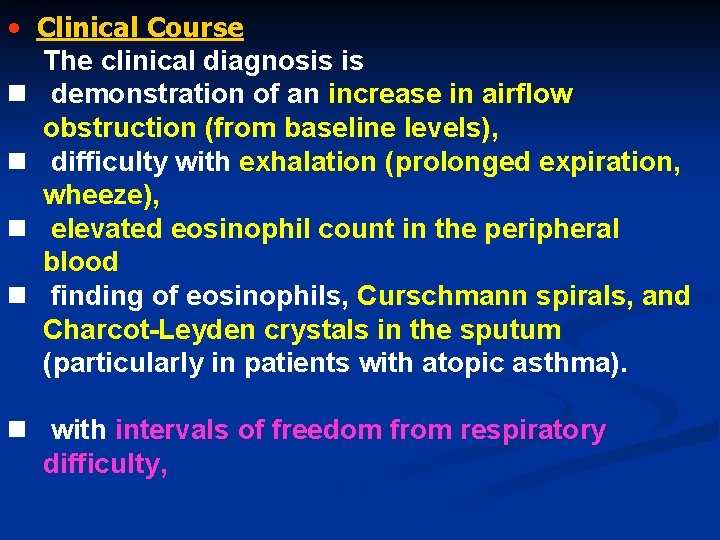
• Clinical Course The clinical diagnosis is n demonstration of an increase in airflow obstruction (from baseline levels), n difficulty with exhalation (prolonged expiration, wheeze), n elevated eosinophil count in the peripheral blood n finding of eosinophils, Curschmann spirals, and Charcot-Leyden crystals in the sputum (particularly in patients with atopic asthma). n with intervals of freedom from respiratory difficulty,
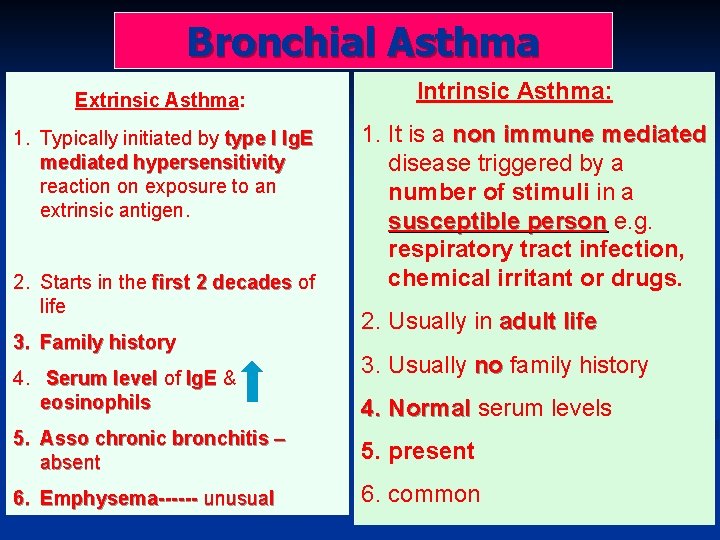
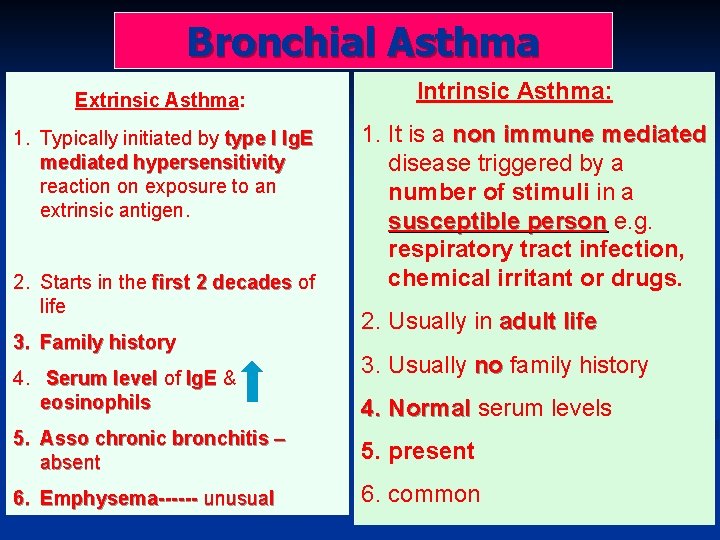
Bronchial Asthma Extrinsic Asthma: 1. Typically initiated by type I Ig. E mediated hypersensitivity reaction on exposure to an extrinsic antigen. 2. Starts in the first 2 decades of life 3. Family history 4. Serum level of Ig. E & eosinophils Intrinsic Asthma: 1. It is a non immune mediated disease triggered by a number of stimuli in a susceptible person e. g. respiratory tract infection, chemical irritant or drugs. 2. Usually in adult life 3. Usually no family history 4. Normal serum levels 5. Asso chronic bronchitis – absent 5. present 6. Emphysema------ unusual 6. common
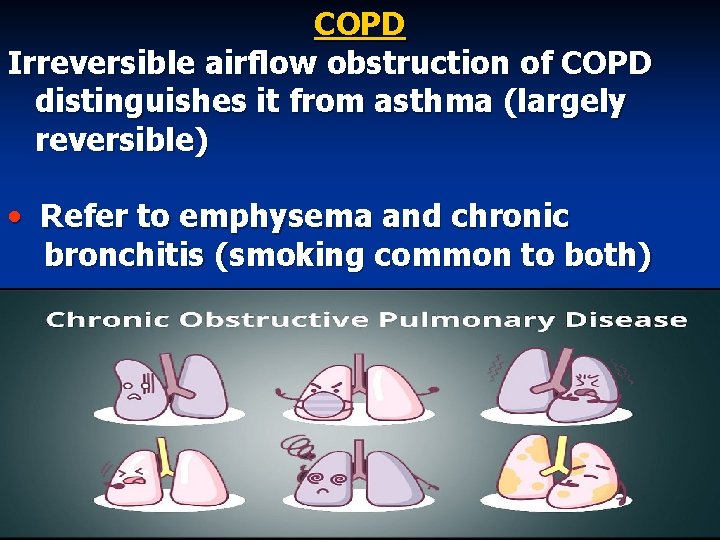
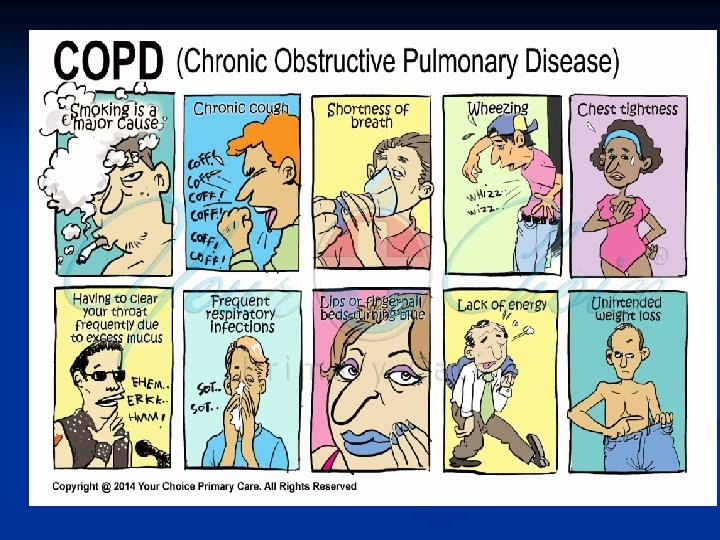
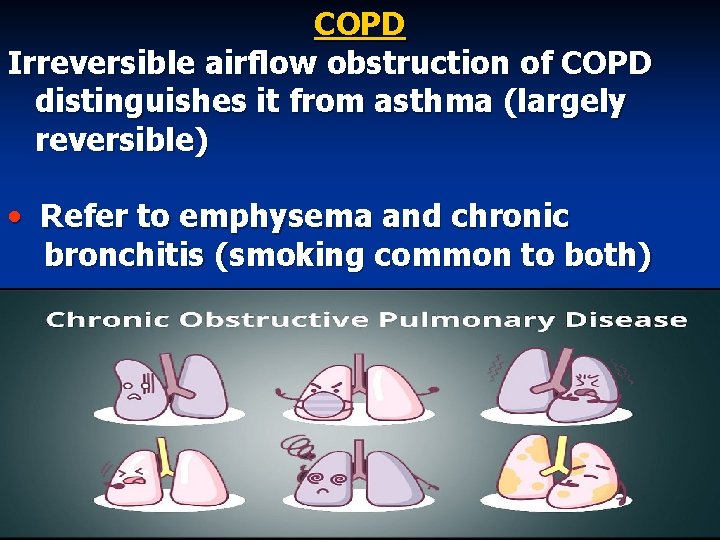
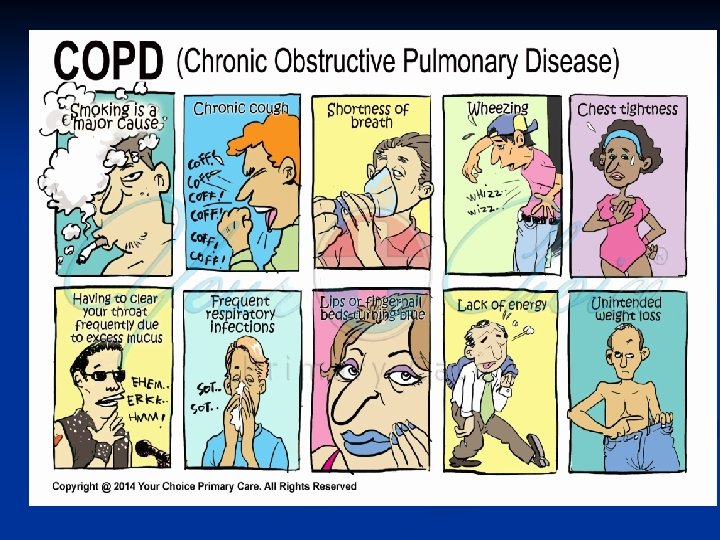
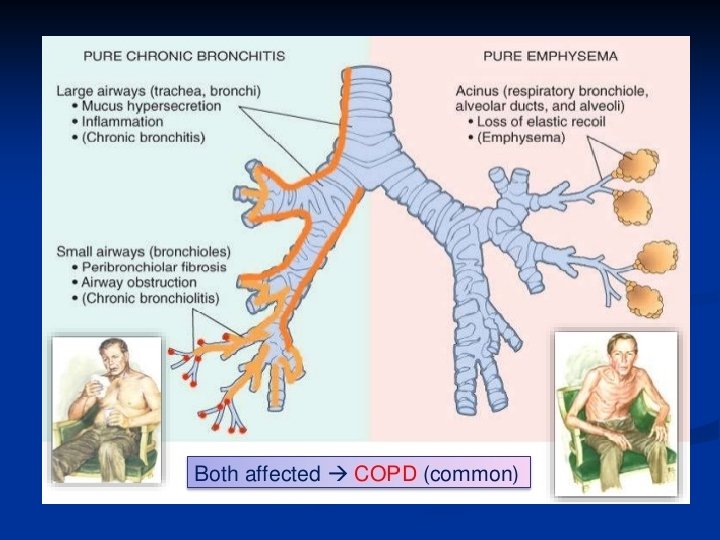
COPD Irreversible airflow obstruction of COPD distinguishes it from asthma (largely reversible) • Refer to emphysema and chronic bronchitis (smoking common to both)
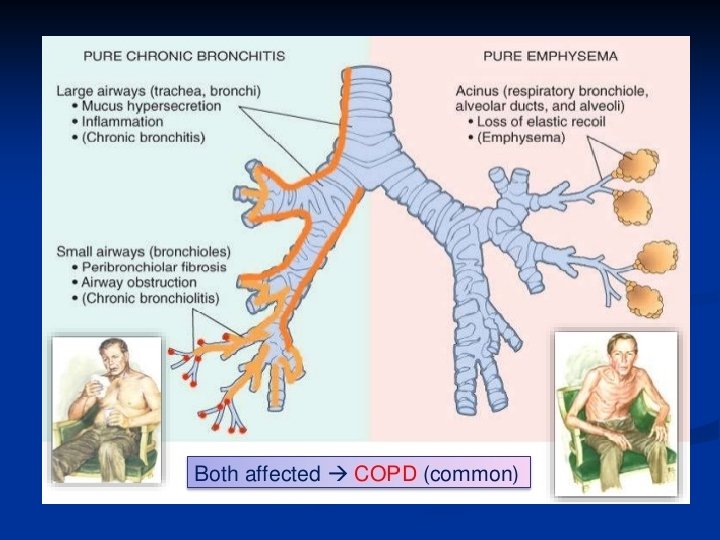
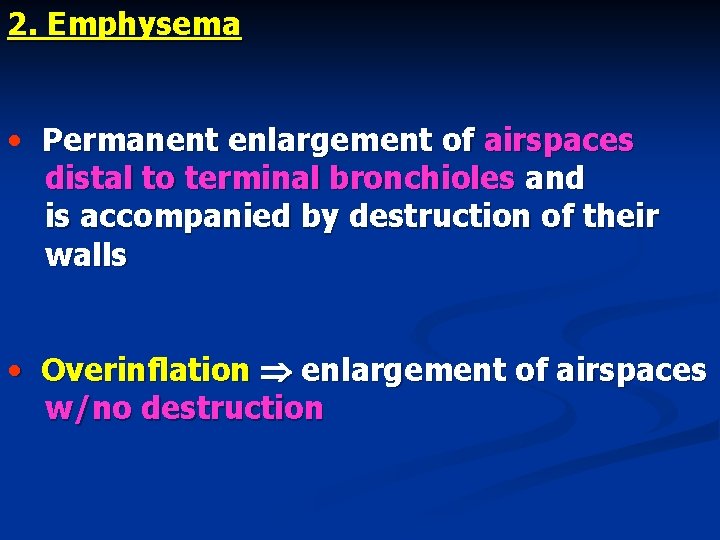
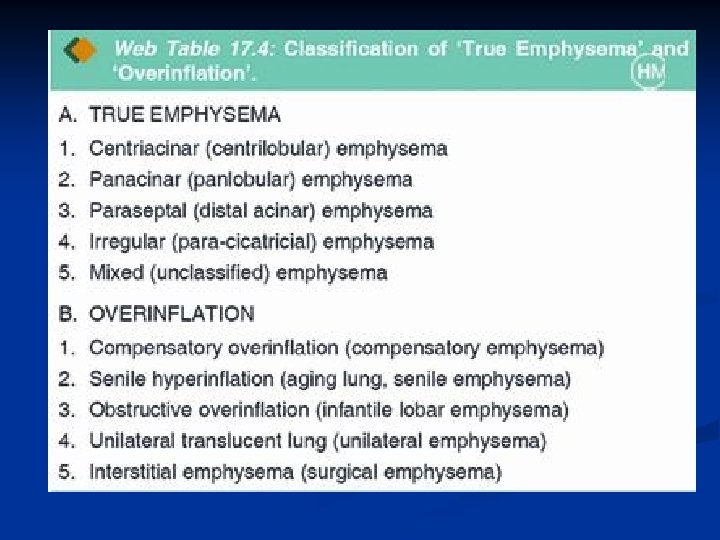
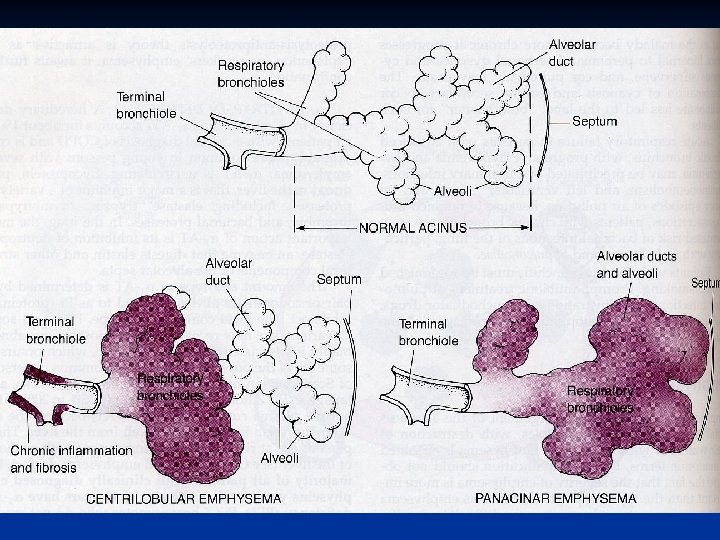
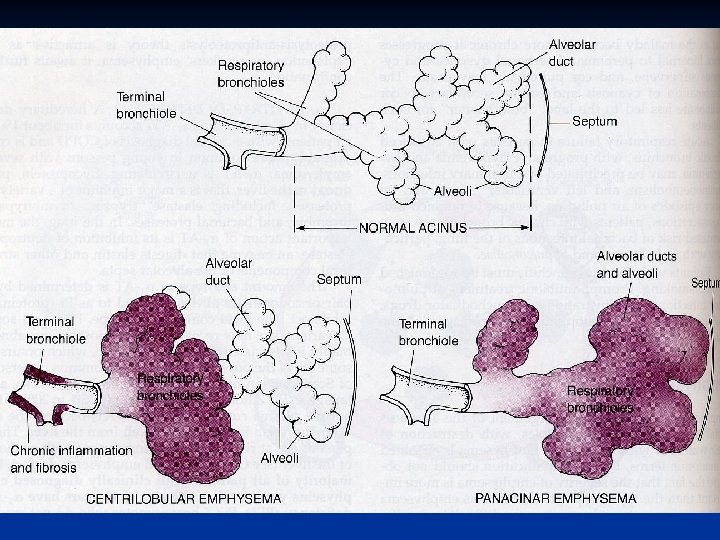
2. Emphysema • Permanent enlargement of airspaces distal to terminal bronchioles and is accompanied by destruction of their walls • Overinflation enlargement of airspaces w/no destruction
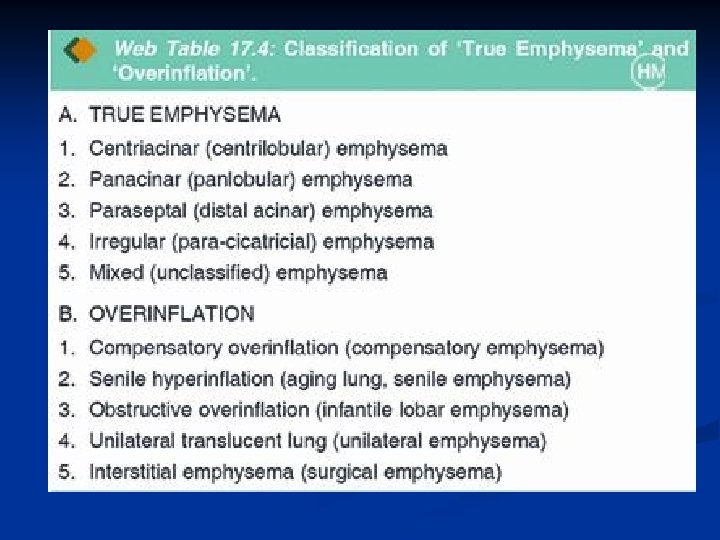
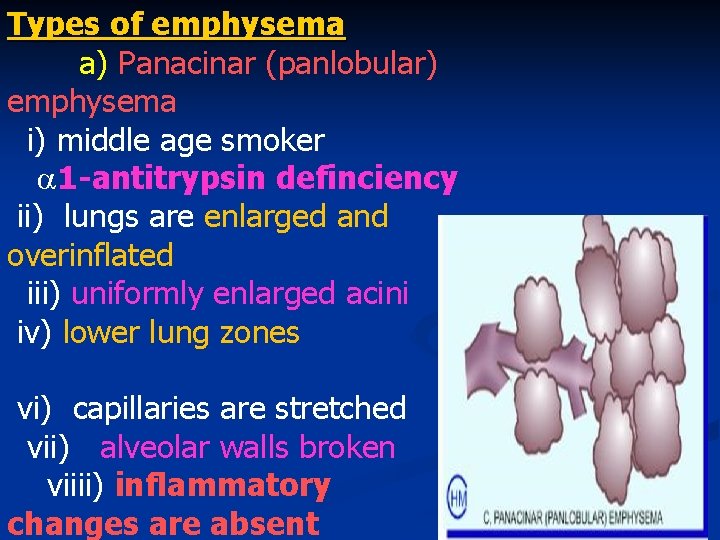
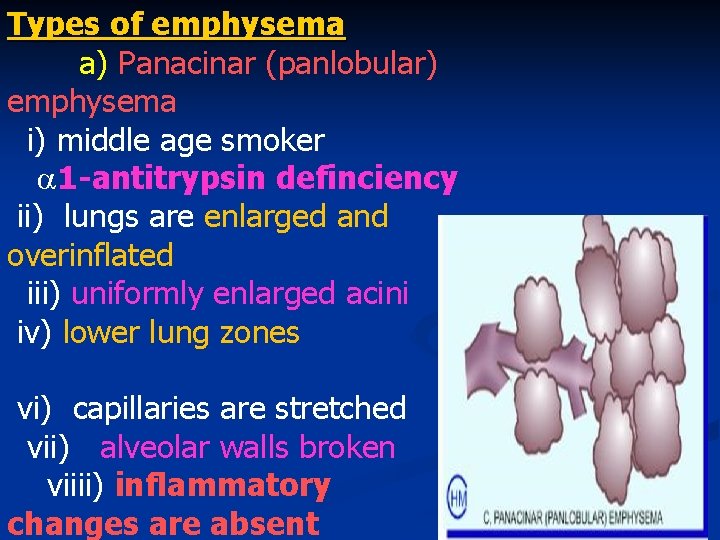
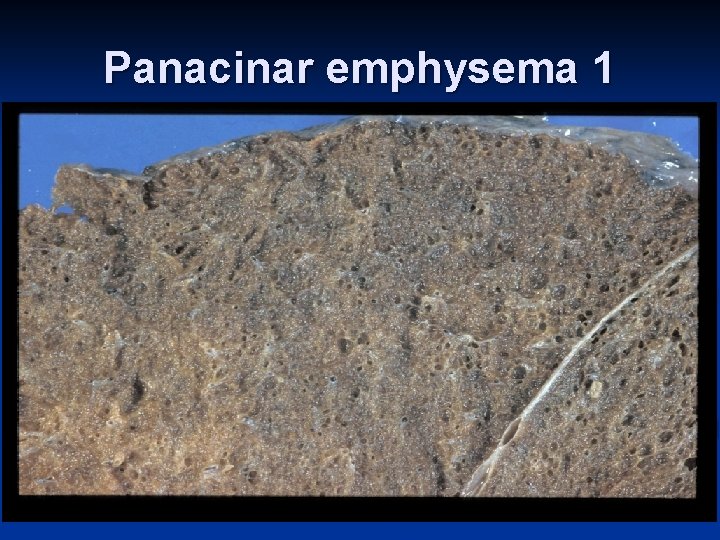
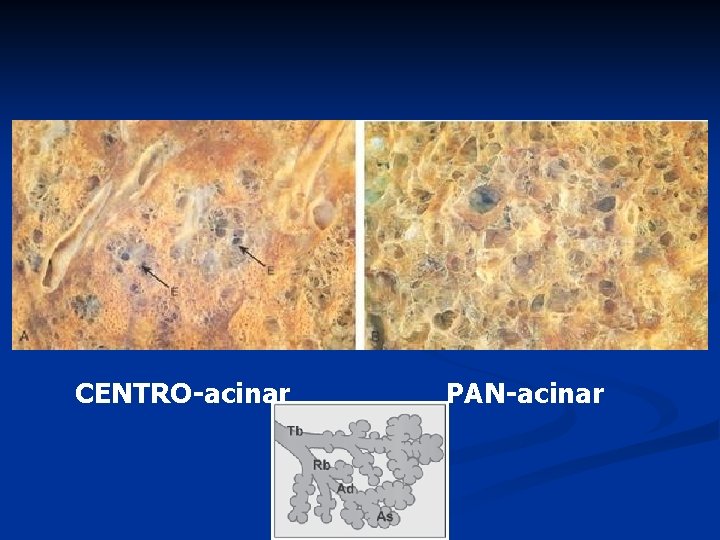
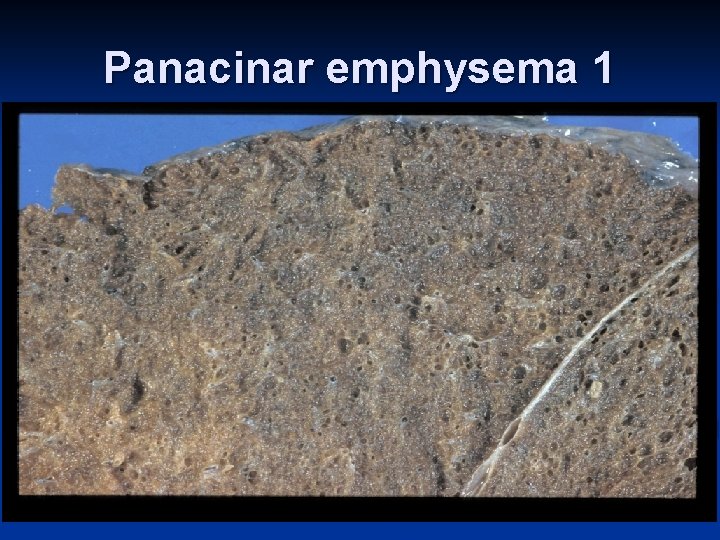
Types of emphysema a) Panacinar (panlobular) emphysema i) middle age smoker 1 -antitrypsin definciency ii) lungs are enlarged and overinflated iii) uniformly enlarged acini iv) lower lung zones vi) capillaries are stretched vii) alveolar walls broken viiii) inflammatory changes are absent
Panacinar emphysema 1
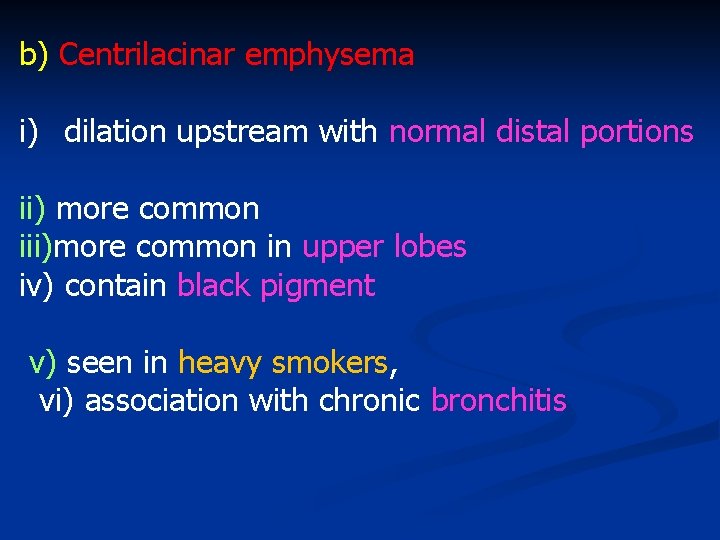
b) Centrilacinar emphysema i) dilation upstream with normal distal portions ii) more common iii)more common in upper lobes iv) contain black pigment v) seen in heavy smokers, vi) association with chronic bronchitis
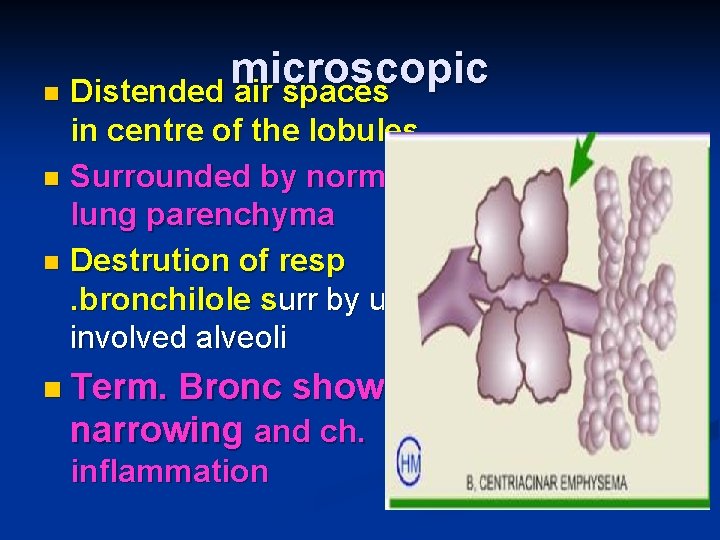
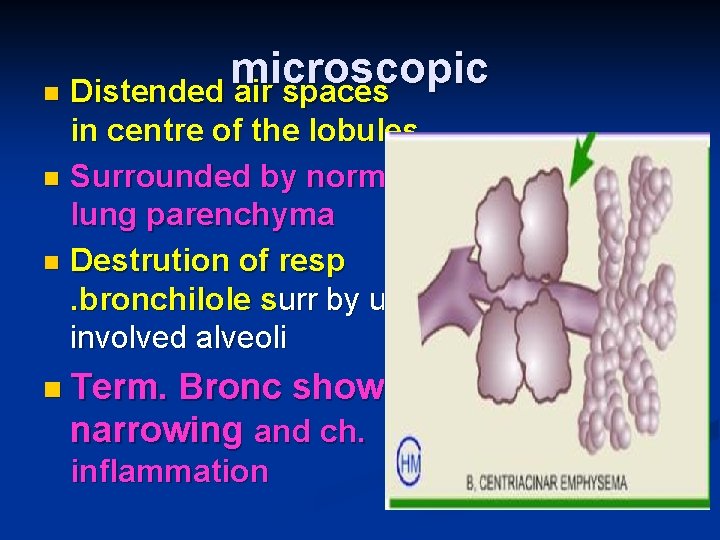
microscopic n Distended air spaces in centre of the lobules n Surrounded by normal lung parenchyma n Destrution of resp. bronchilole surr by un involved alveoli n Term. Bronc show narrowing and ch. inflammation
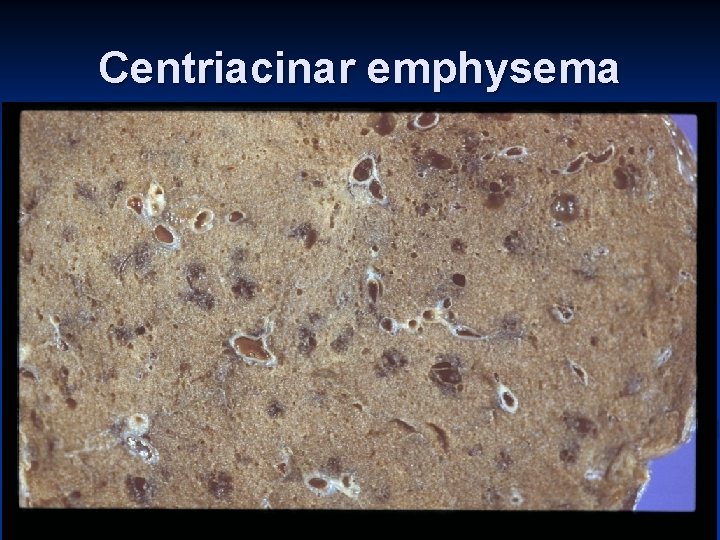
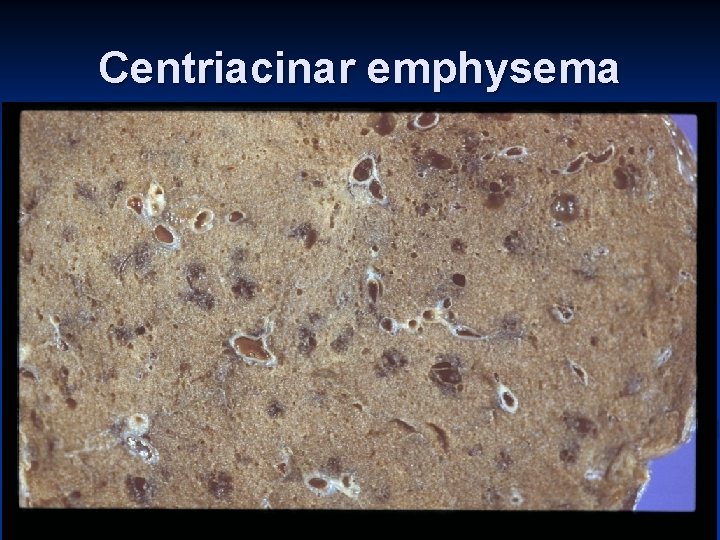
Centriacinar emphysema

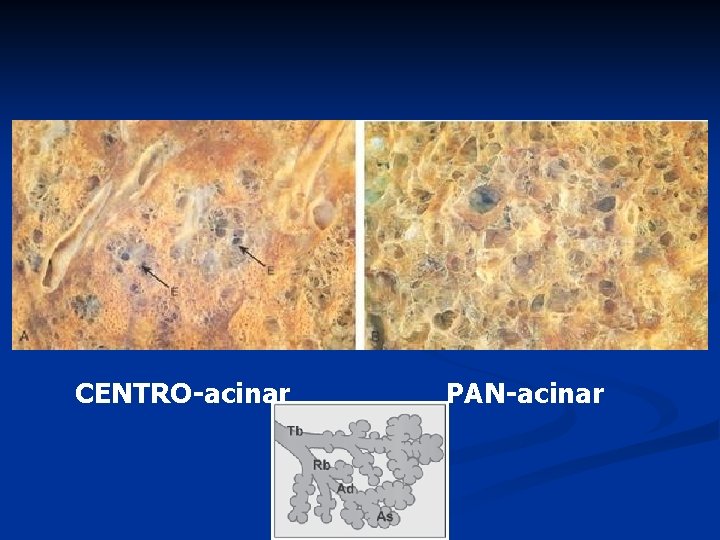
CENTRO-acinar PAN-acinar
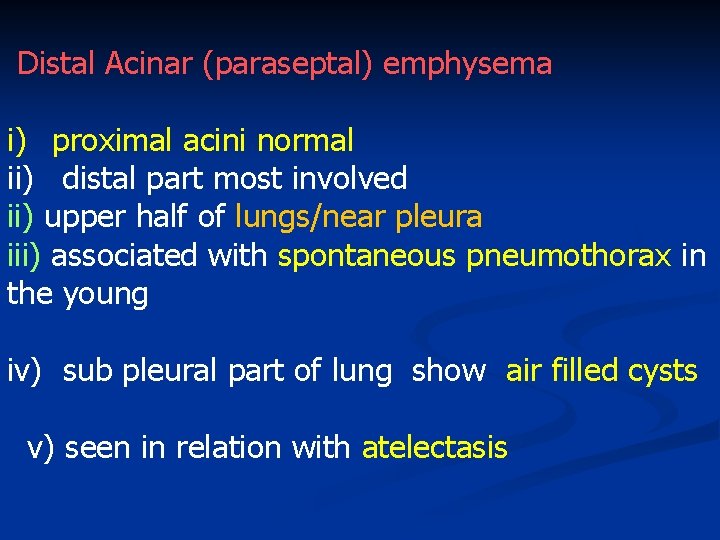
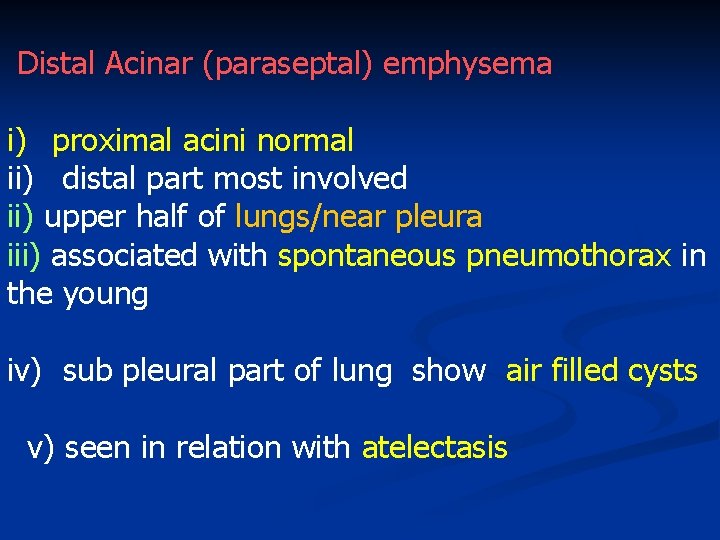
Distal Acinar (paraseptal) emphysema i) proximal acini normal ii) distal part most involved ii) upper half of lungs/near pleura iii) associated with spontaneous pneumothorax in the young iv) sub pleural part of lung show air filled cysts v) seen in relation with atelectasis
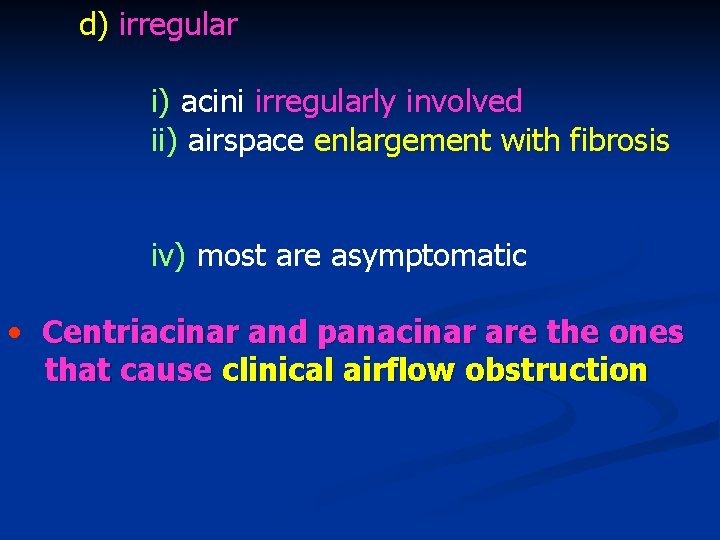
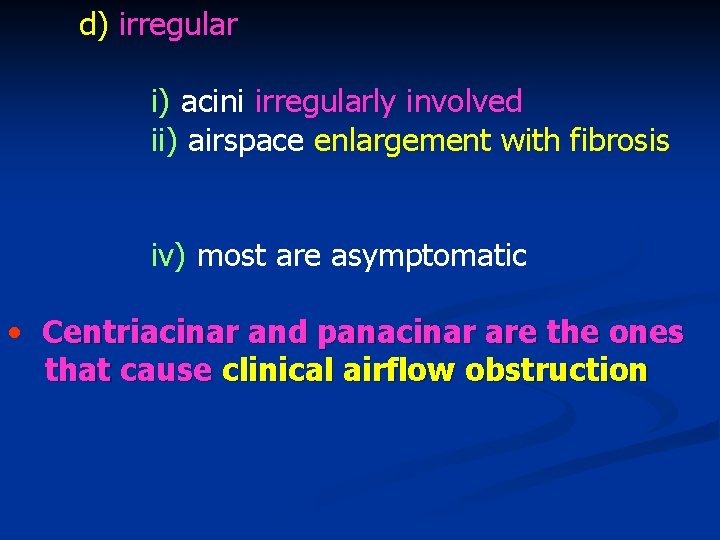
d) irregular i) acini irregularly involved ii) airspace enlargement with fibrosis iv) most are asymptomatic • Centriacinar and panacinar are the ones that cause clinical airflow obstruction
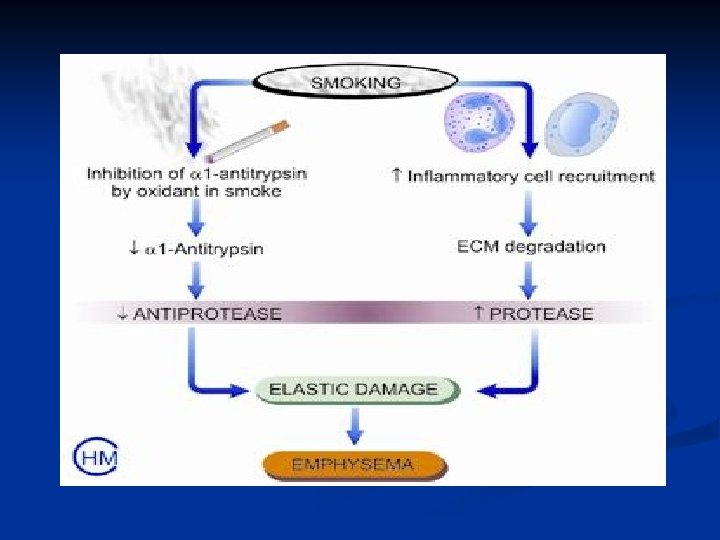
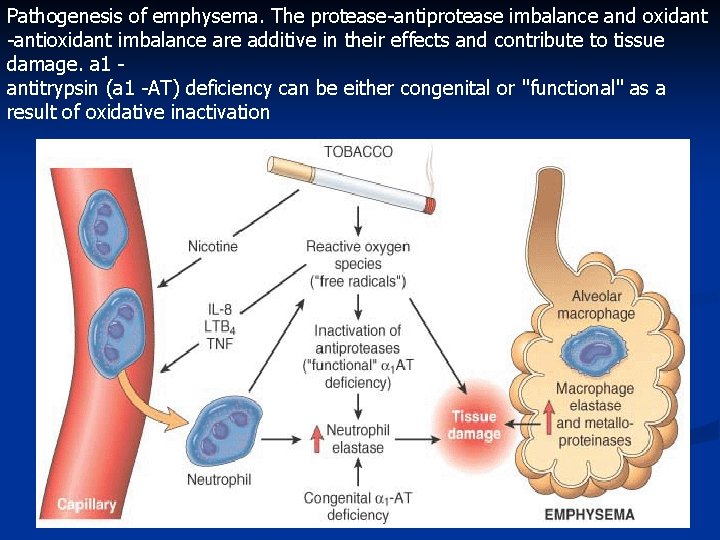
• pathogenesis by 2 Theories i) protease-antiprotease imbalance ii) oxidant-antioxidant imbalance
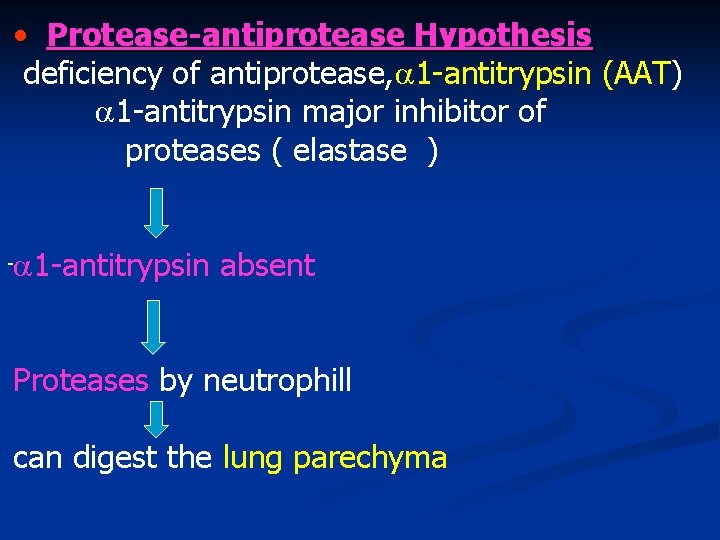
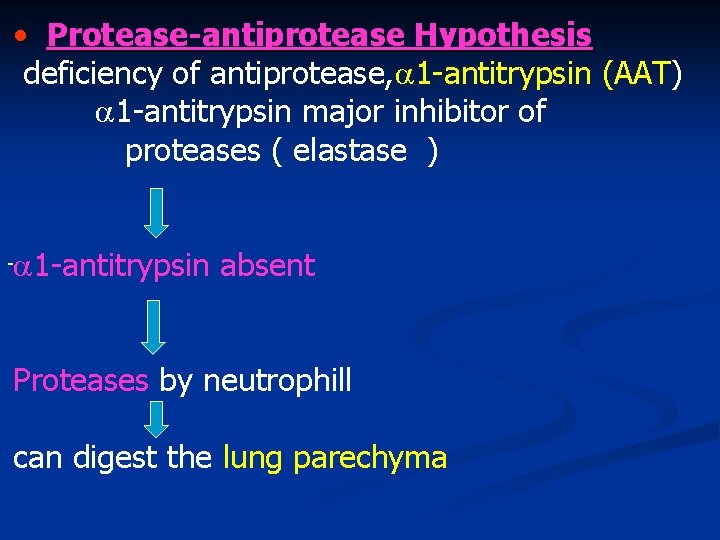
• Protease-antiprotease Hypothesis deficiency of antiprotease, 1 -antitrypsin (AAT) 1 -antitrypsin major inhibitor of proteases ( elastase ) 1 -antitrypsin absent - Proteases by neutrophill can digest the lung parechyma
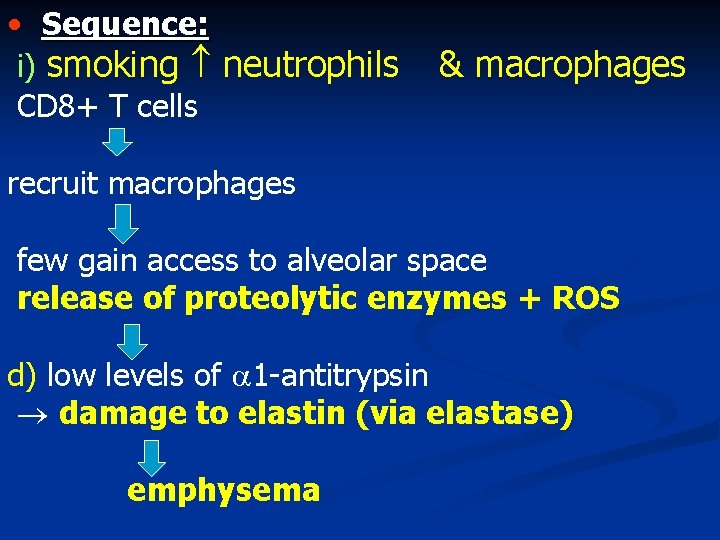
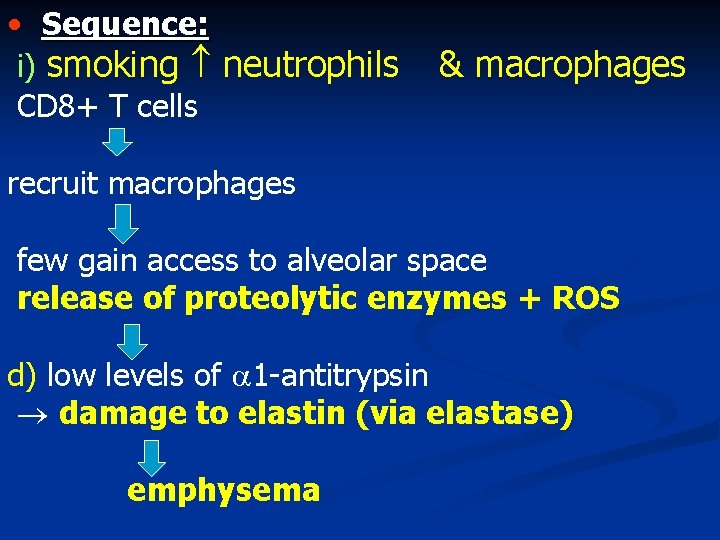
• Sequence: i) smoking neutrophils CD 8+ T cells & macrophages recruit macrophages few gain access to alveolar space release of proteolytic enzymes + ROS d) low levels of 1 -antitrypsin damage to elastin (via elastase) emphysema
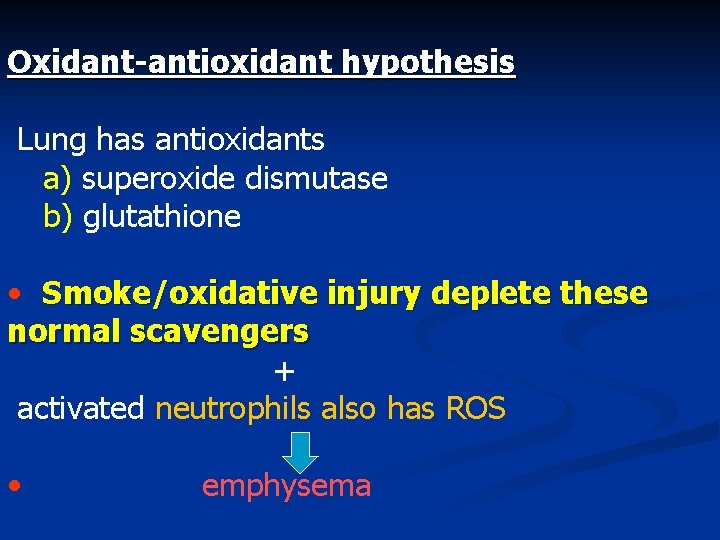
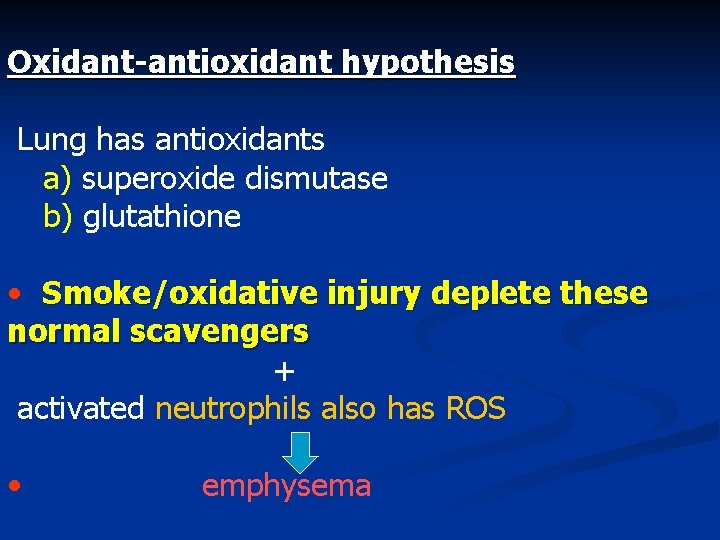
Oxidant-antioxidant hypothesis Lung has antioxidants a) superoxide dismutase b) glutathione • Smoke/oxidative injury deplete these normal scavengers + activated neutrophils also has ROS • emphysema
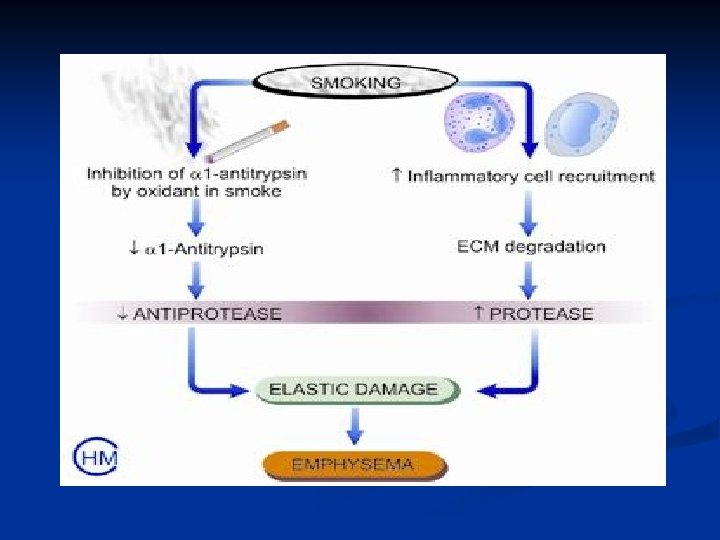
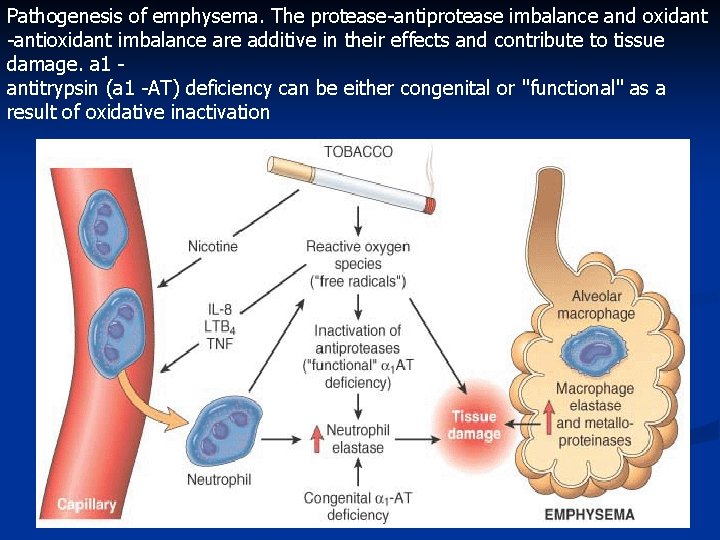
Pathogenesis of emphysema. The protease-antiprotease imbalance and oxidant -antioxidant imbalance are additive in their effects and contribute to tissue damage. a 1 antitrypsin (a 1 -AT) deficiency can be either congenital or "functional" as a result of oxidative inactivation
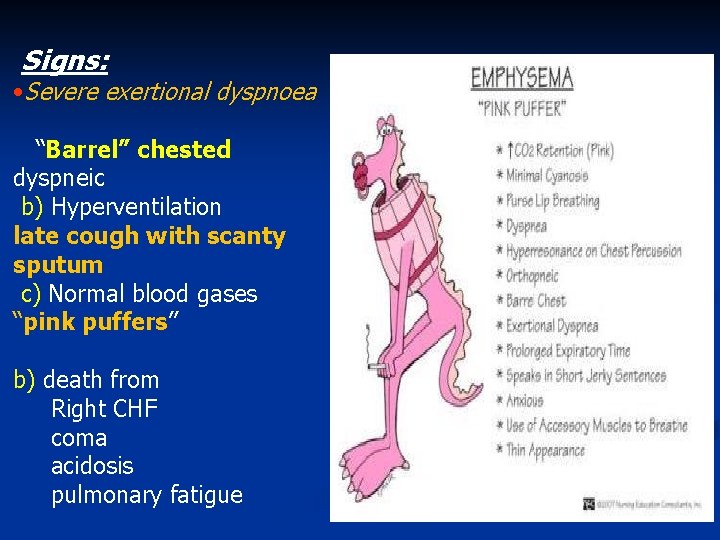
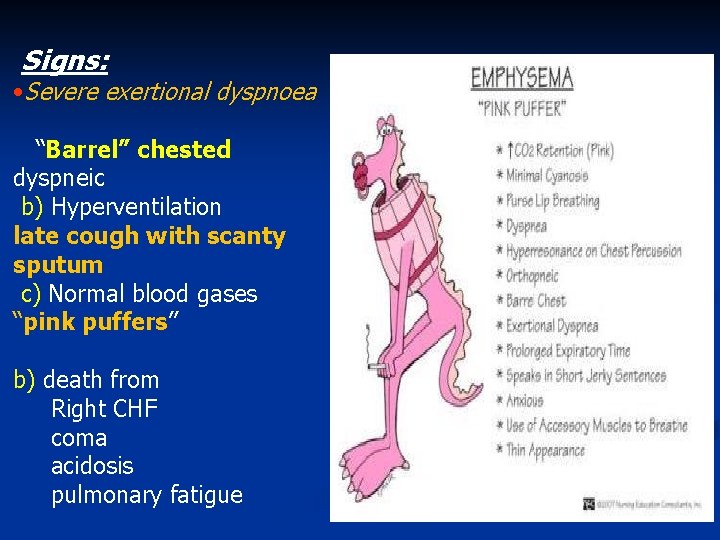
Signs: • Severe exertional dyspnoea “Barrel” chested dyspneic b) Hyperventilation late cough with scanty sputum c) Normal blood gases “pink puffers” b) death from Right CHF coma acidosis pulmonary fatigue
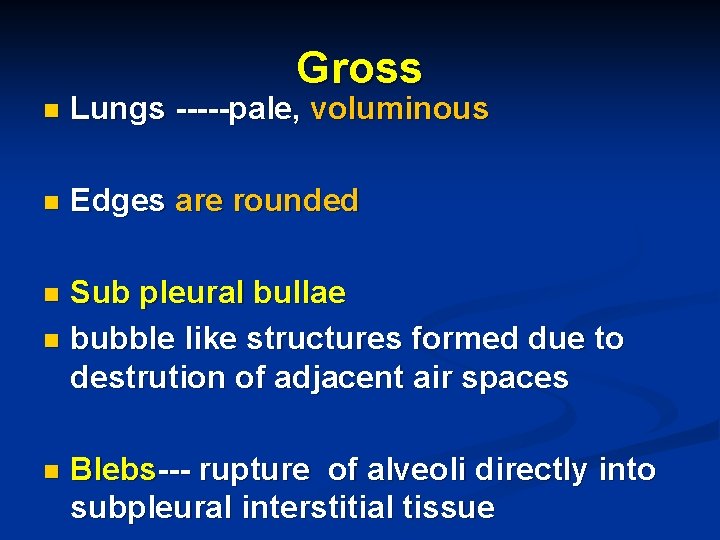
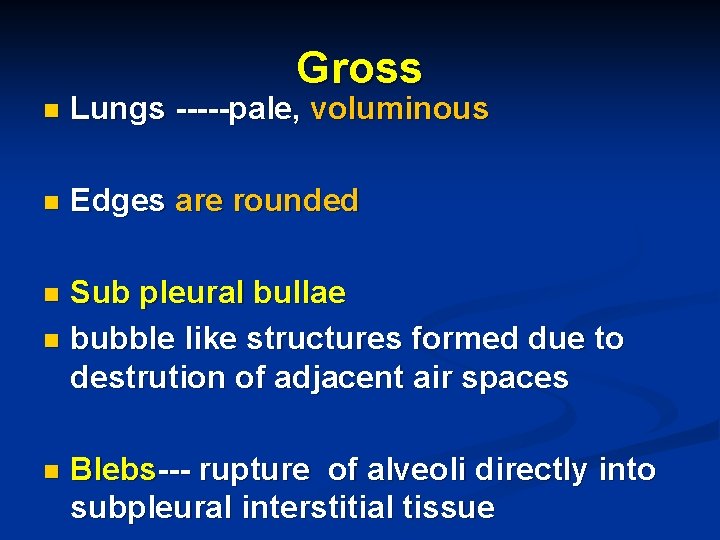
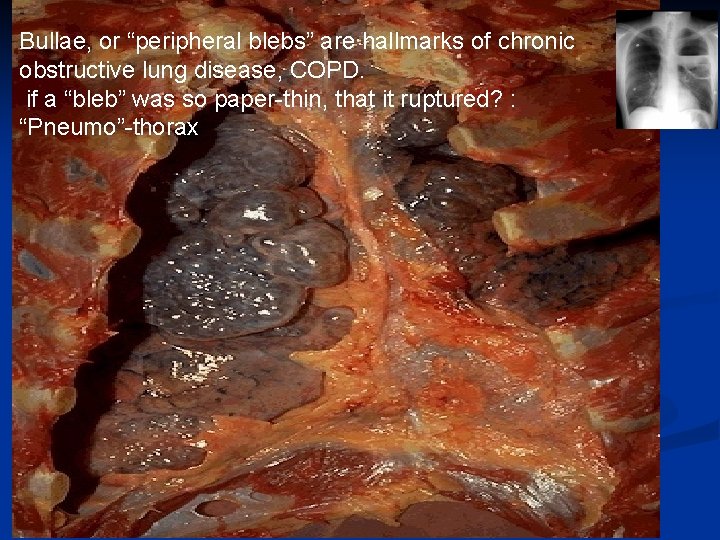
Gross n Lungs -----pale, voluminous n Edges are rounded Sub pleural bullae n bubble like structures formed due to destrution of adjacent air spaces n n Blebs--- rupture of alveoli directly into subpleural interstitial tissue
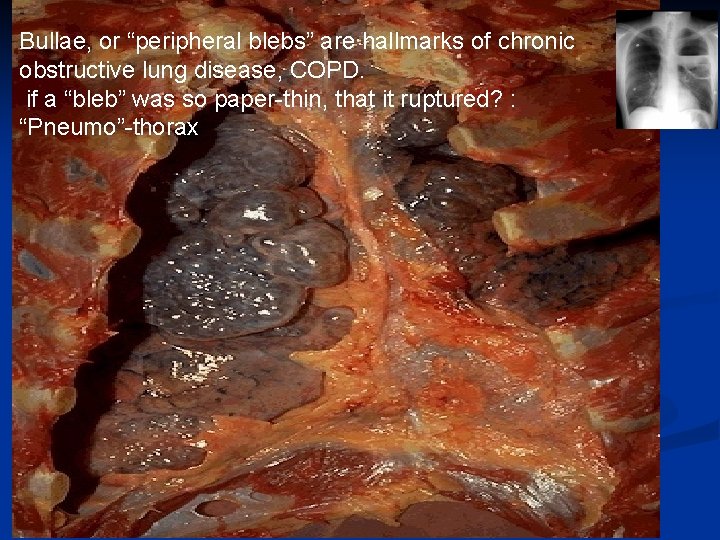
Bullae, or “peripheral blebs” are hallmarks of chronic obstructive lung disease, COPD. if a “bleb” was so paper-thin, that it ruptured? : “Pneumo”-thorax

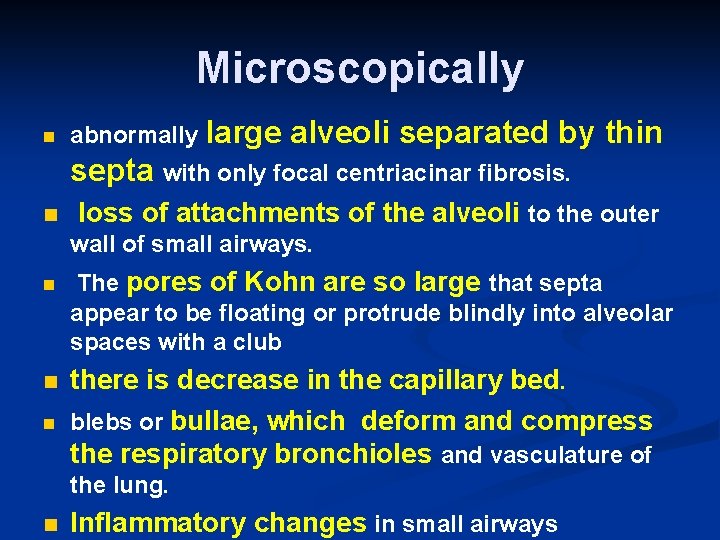
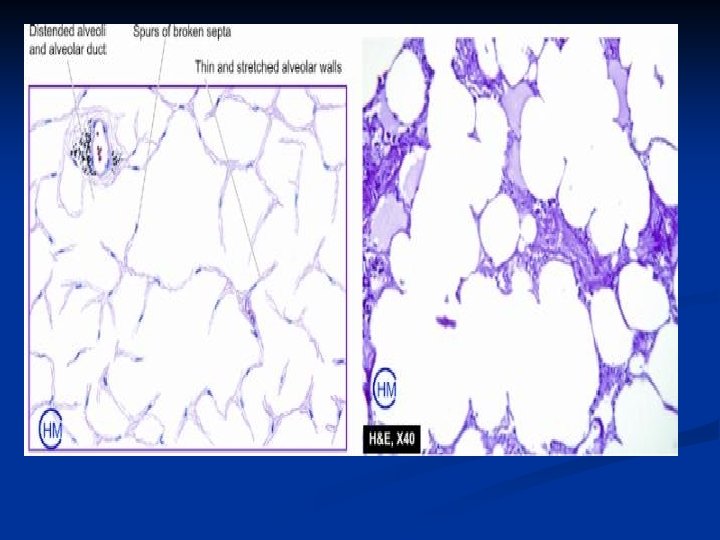
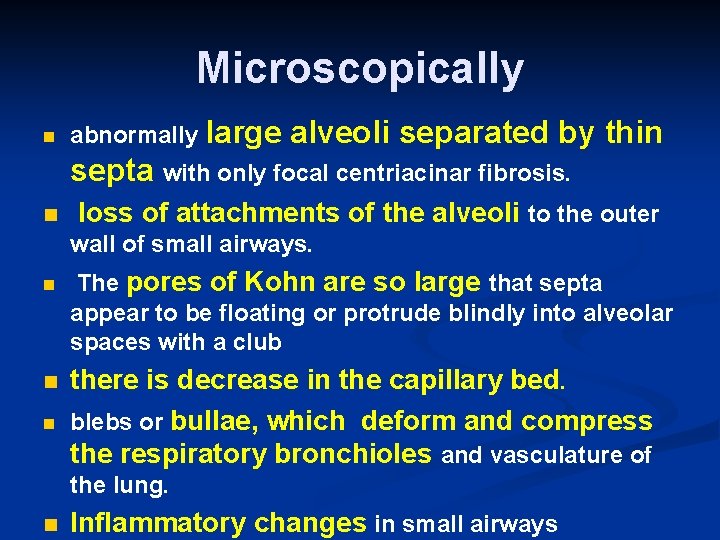
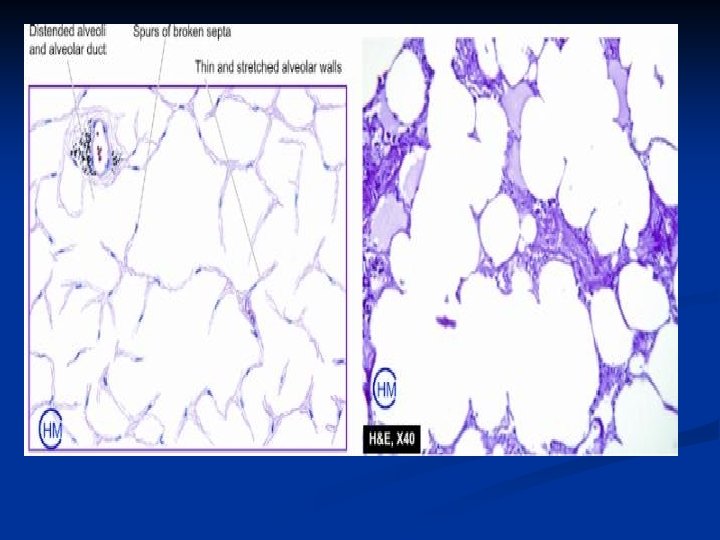
Microscopically n abnormally large alveoli separated by thin septa with only focal centriacinar fibrosis. n loss of attachments of the alveoli to the outer wall of small airways. n n n The pores of Kohn are so large that septa appear to be floating or protrude blindly into alveolar spaces with a club there is decrease in the capillary bed. blebs or bullae, which deform and compress the respiratory bronchioles and vasculature of the lung. n Inflammatory changes in small airways
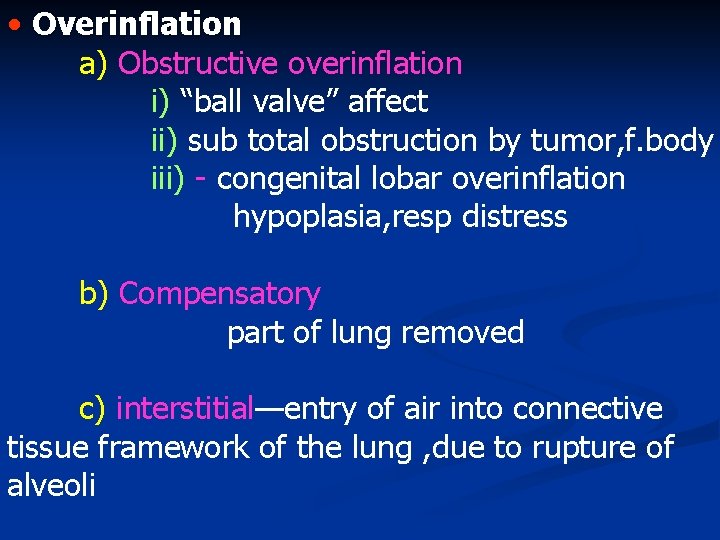
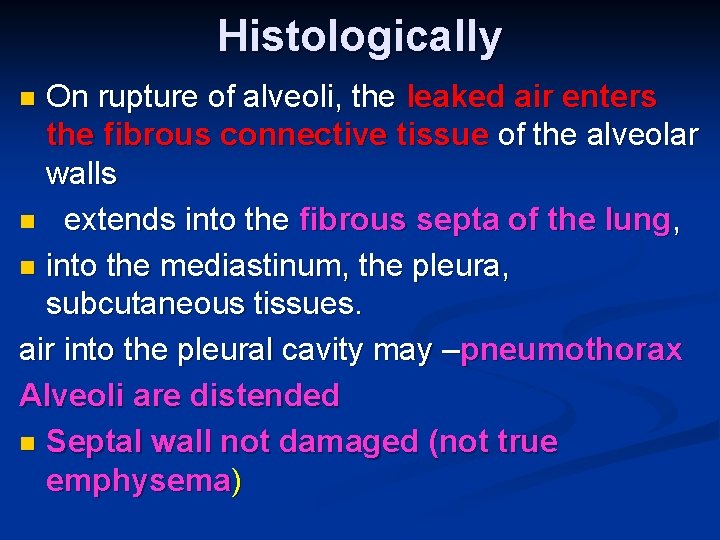
• Overinflation a) Obstructive overinflation i) “ball valve” affect ii) sub total obstruction by tumor, f. body iii) - congenital lobar overinflation hypoplasia, resp distress b) Compensatory part of lung removed c) interstitial—entry of air into connective tissue framework of the lung , due to rupture of alveoli
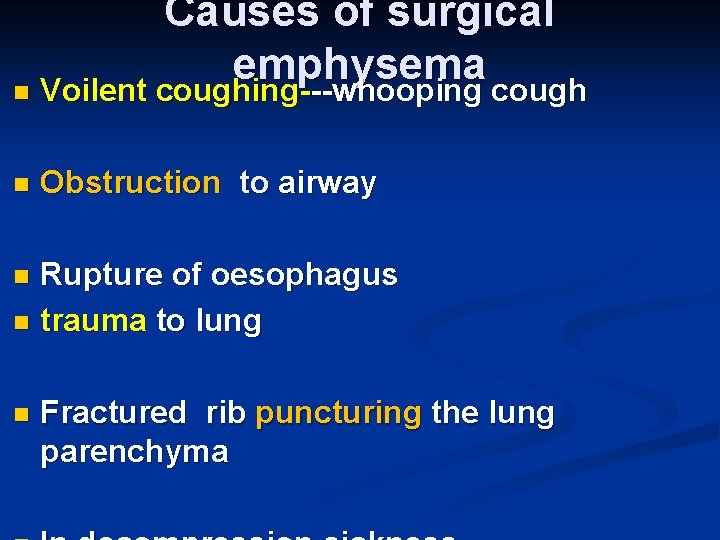
Causes of surgical emphysema n Voilent coughing---whooping cough n Obstruction to airway Rupture of oesophagus n trauma to lung n n Fractured rib puncturing the lung parenchyma
Histologically On rupture of alveoli, the leaked air enters the fibrous connective tissue of the alveolar walls n extends into the fibrous septa of the lung, n into the mediastinum, the pleura, subcutaneous tissues. air into the pleural cavity may –pneumothorax Alveoli are distended n Septal wall not damaged (not true emphysema) n
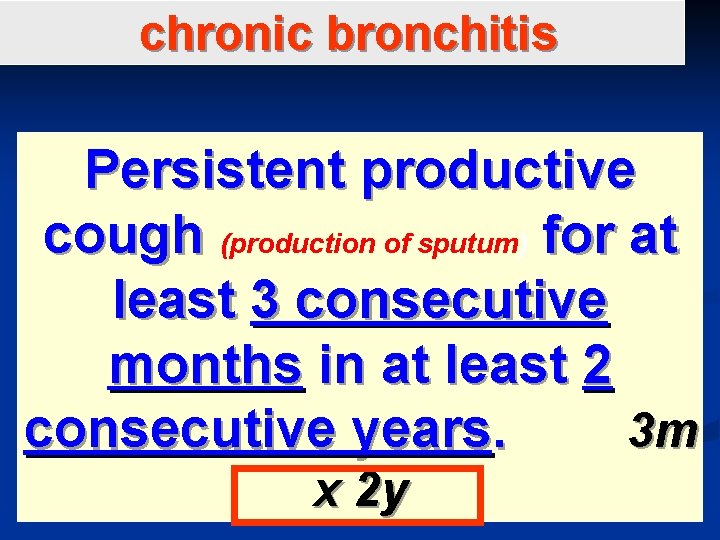
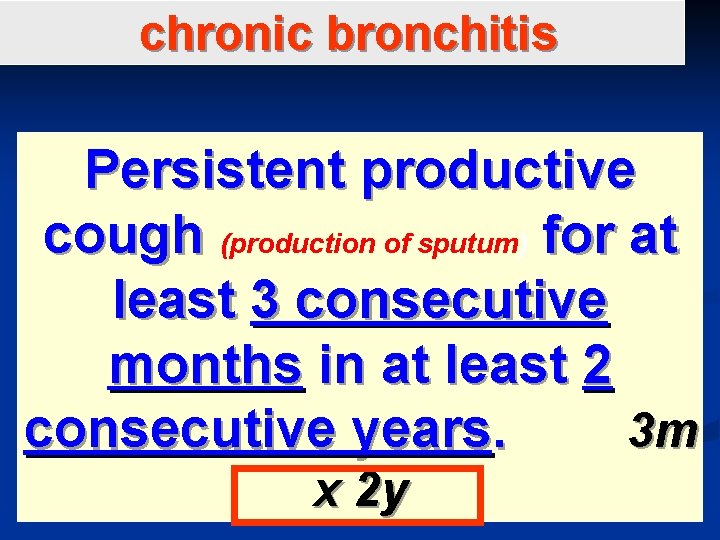
chronic bronchitis Persistent productive cough (production of sputum) for at least 3 consecutive months in at least 2 consecutive years. 3 m x 2 y
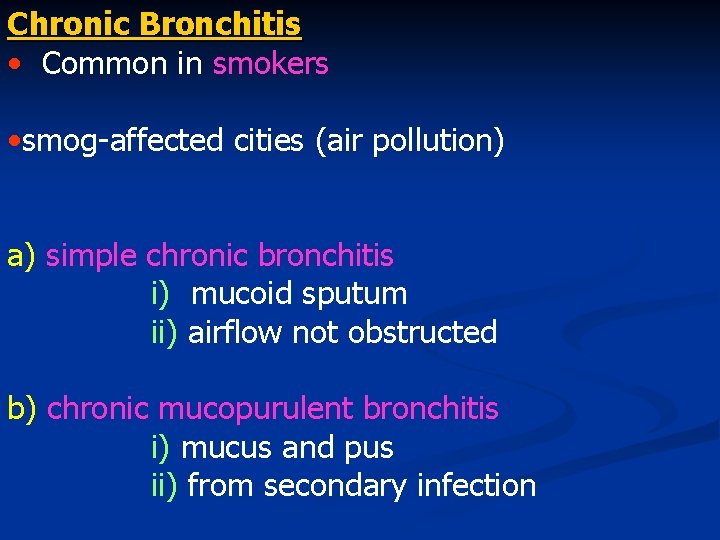
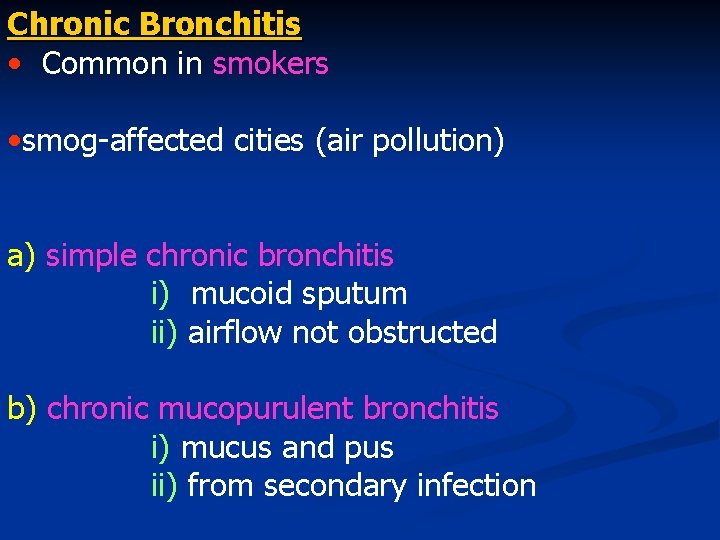
Chronic Bronchitis • Common in smokers • smog-affected cities (air pollution) a) simple chronic bronchitis i) mucoid sputum ii) airflow not obstructed b) chronic mucopurulent bronchitis i) mucus and pus ii) from secondary infection
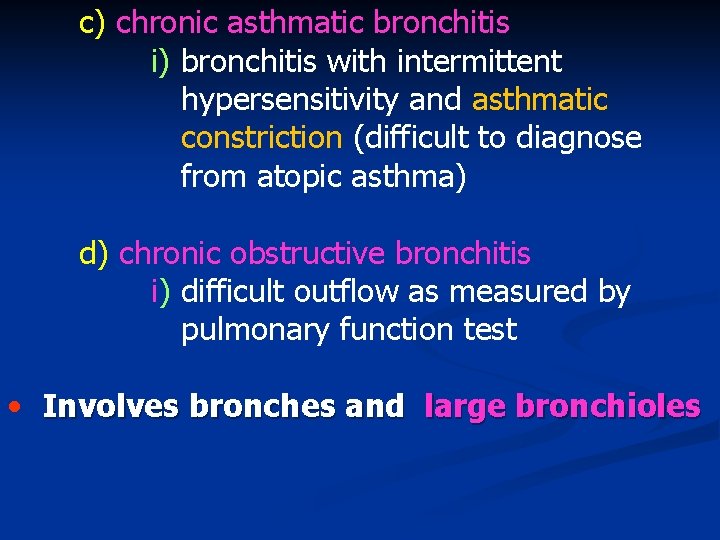
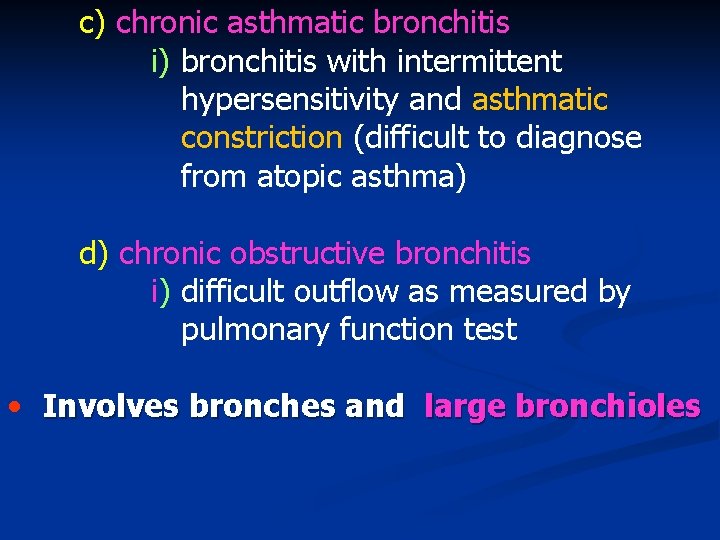
c) chronic asthmatic bronchitis i) bronchitis with intermittent hypersensitivity and asthmatic constriction (difficult to diagnose from atopic asthma) d) chronic obstructive bronchitis i) difficult outflow as measured by pulmonary function test • Involves bronches and large bronchioles
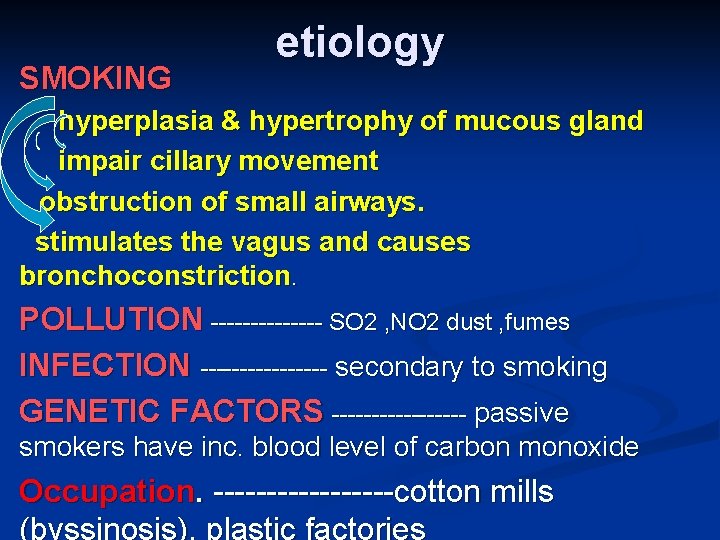
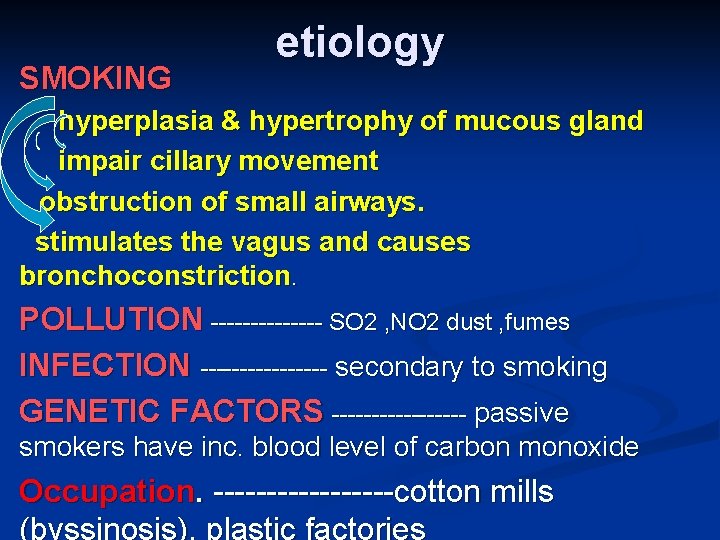
SMOKING etiology hyperplasia & hypertrophy of mucous gland impair cillary movement obstruction of small airways. stimulates the vagus and causes bronchoconstriction. POLLUTION ------- SO 2 , NO 2 dust , fumes INFECTION -------- secondary to smoking GENETIC FACTORS --------- passive smokers have inc. blood level of carbon monoxide Occupation. ---------cotton mills (byssinosis), plastic factories
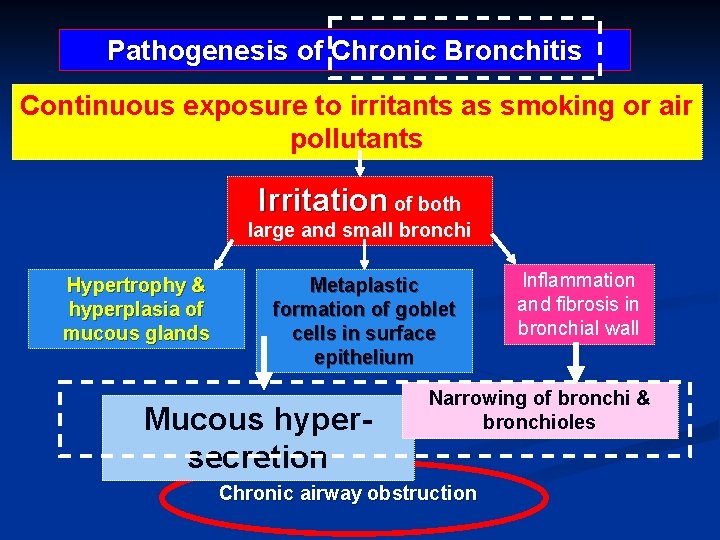
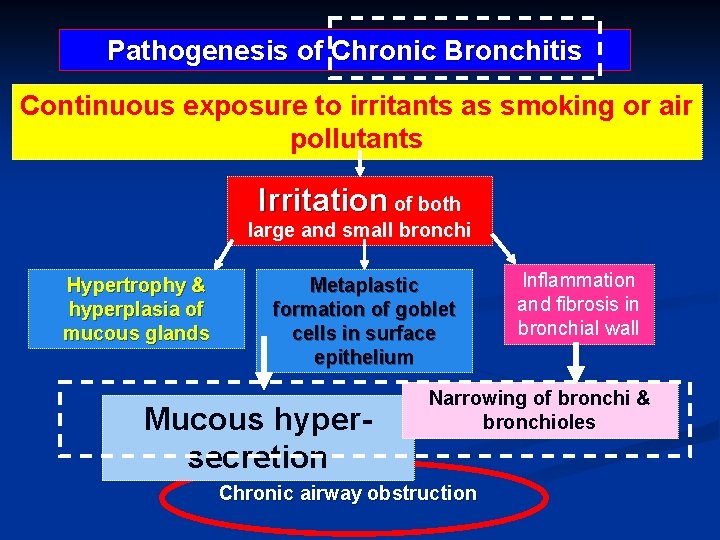
Pathogenesis of Chronic Bronchitis Continuous exposure to irritants as smoking or air pollutants Irritation of both large and small bronchi Hypertrophy & hyperplasia of mucous glands Metaplastic formation of goblet cells in surface epithelium Mucous hypersecretion Inflammation and fibrosis in bronchial wall Narrowing of bronchi & bronchioles Chronic airway obstruction
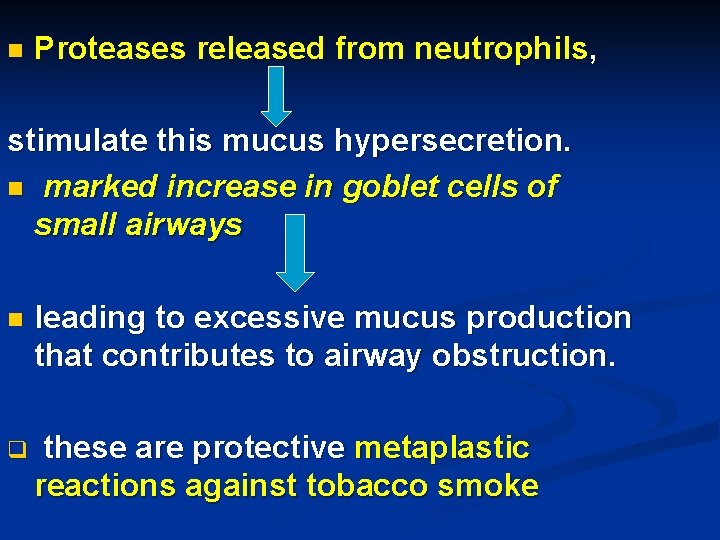
n Proteases released from neutrophils, stimulate this mucus hypersecretion. n marked increase in goblet cells of small airways n leading to excessive mucus production that contributes to airway obstruction. q these are protective metaplastic reactions against tobacco smoke
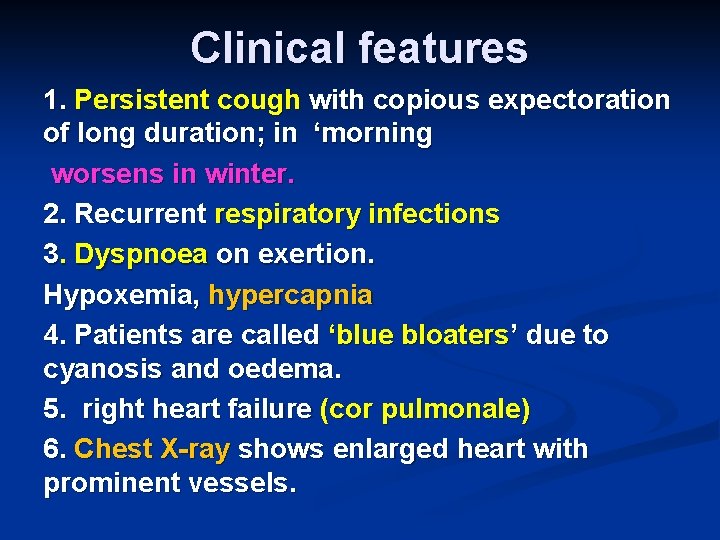
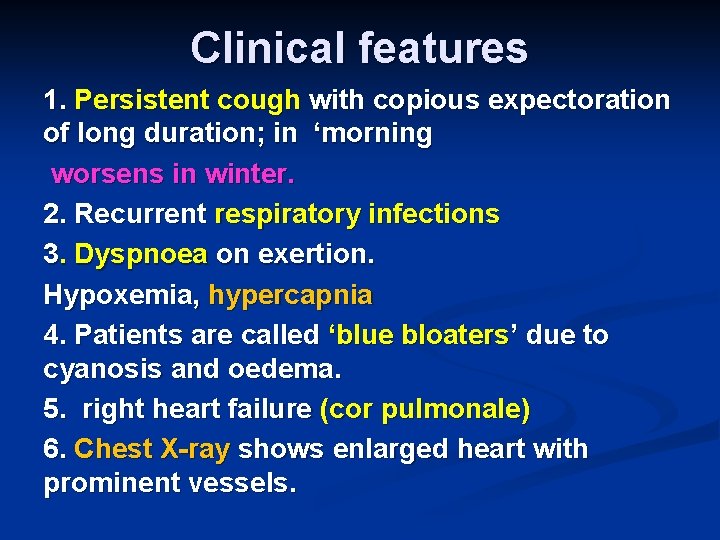
Clinical features 1. Persistent cough with copious expectoration of long duration; in ‘morning worsens in winter. 2. Recurrent respiratory infections 3. Dyspnoea on exertion. Hypoxemia, hypercapnia 4. Patients are called ‘blue bloaters’ due to cyanosis and oedema. 5. right heart failure (cor pulmonale) 6. Chest X-ray shows enlarged heart with prominent vessels.
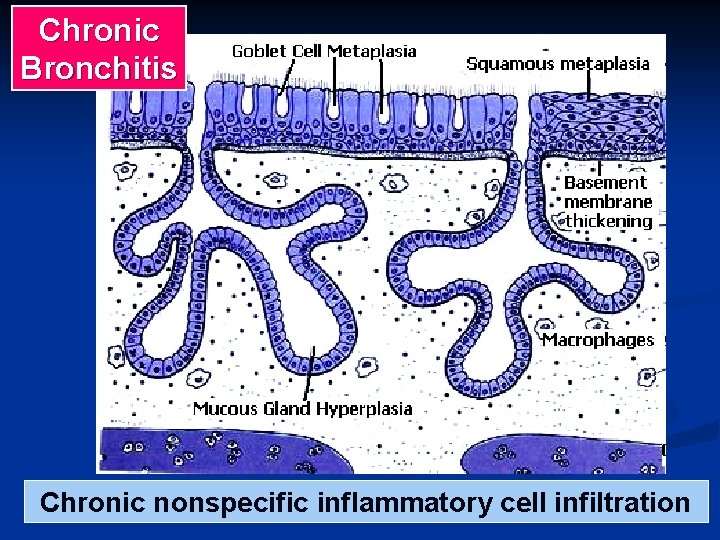
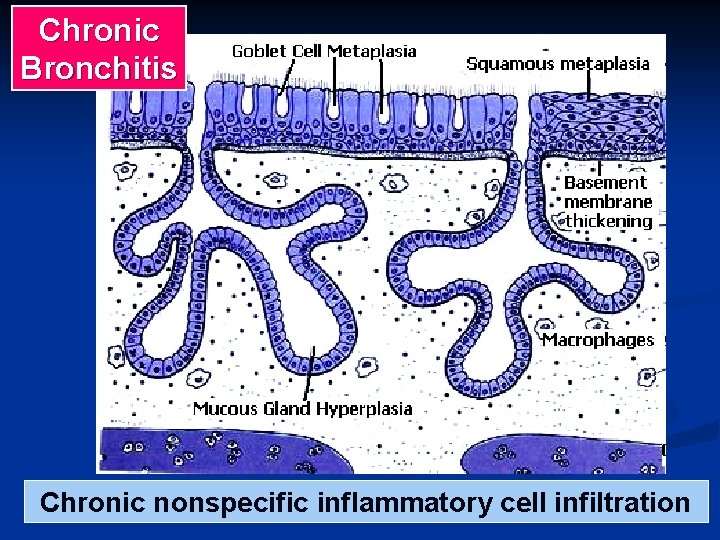
Chronic Bronchitis Chronic nonspecific inflammatory cell infiltration
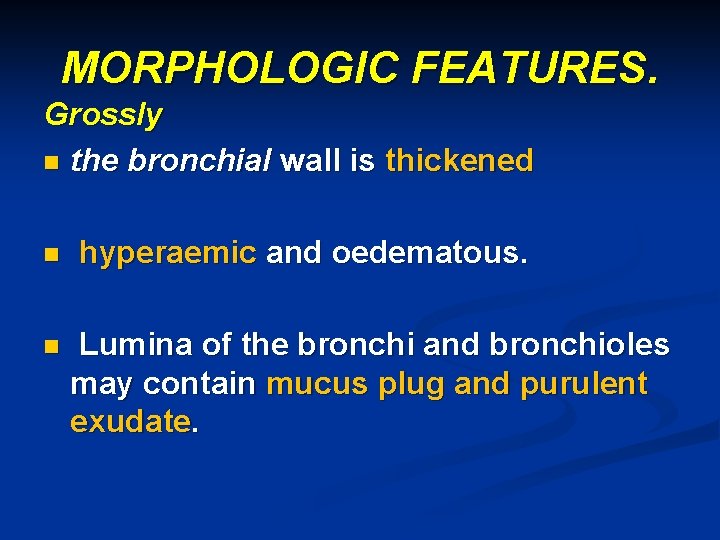
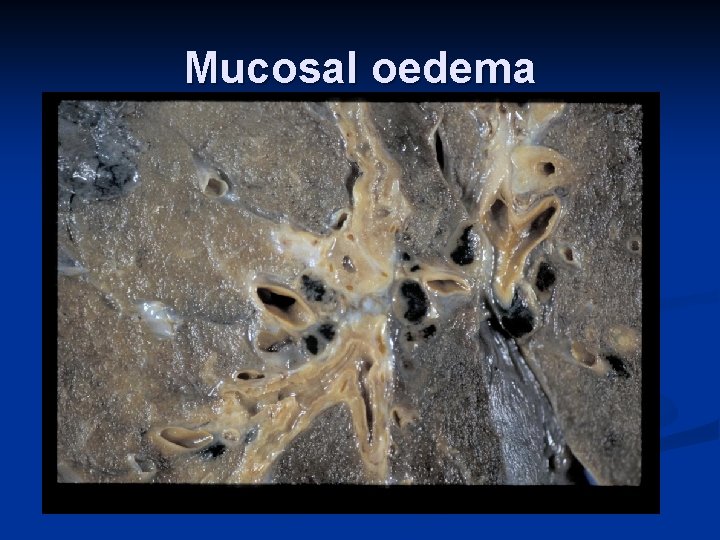
MORPHOLOGIC FEATURES. Grossly n the bronchial wall is thickened n n hyperaemic and oedematous. Lumina of the bronchi and bronchioles may contain mucus plug and purulent exudate.
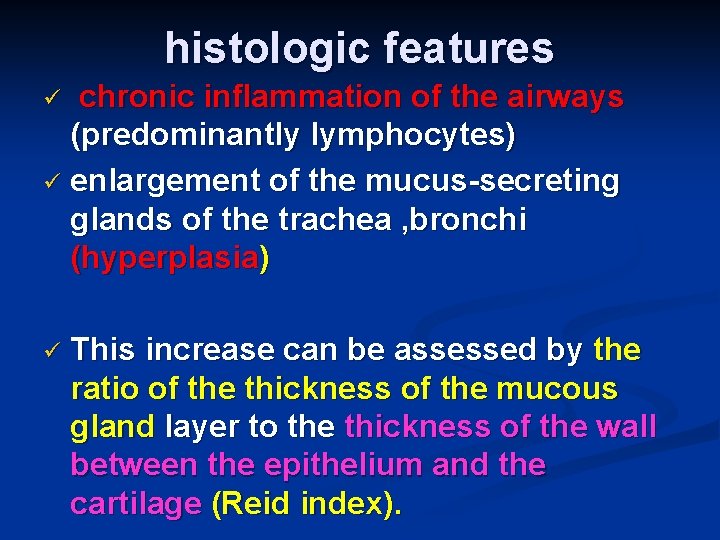
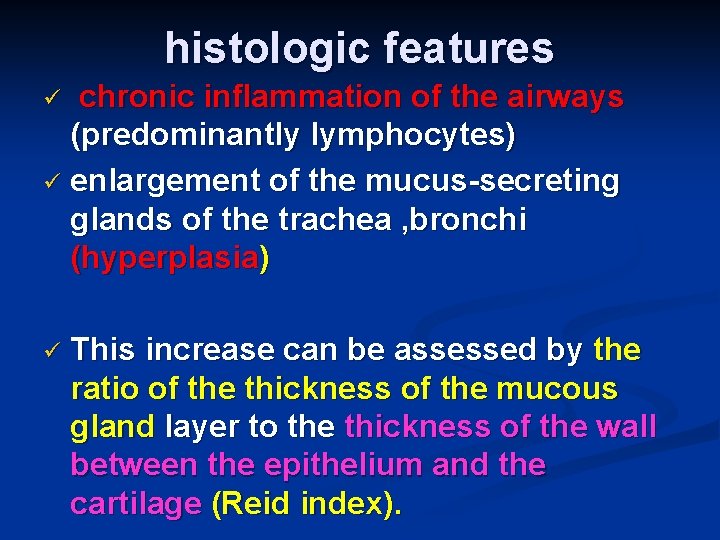
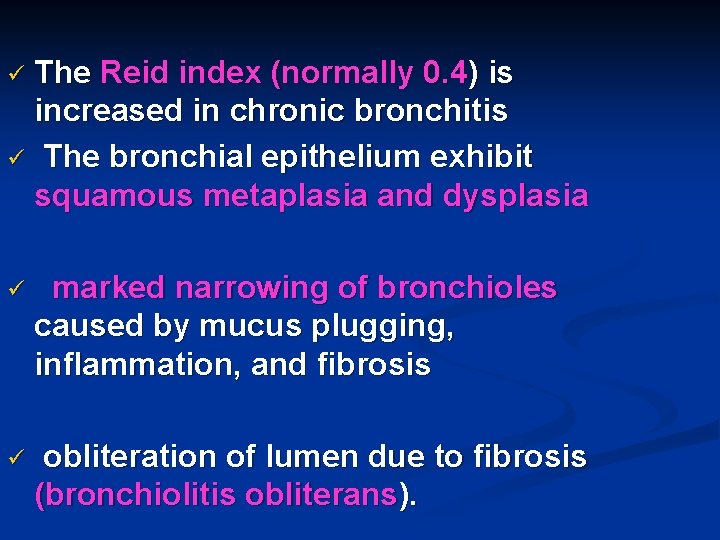
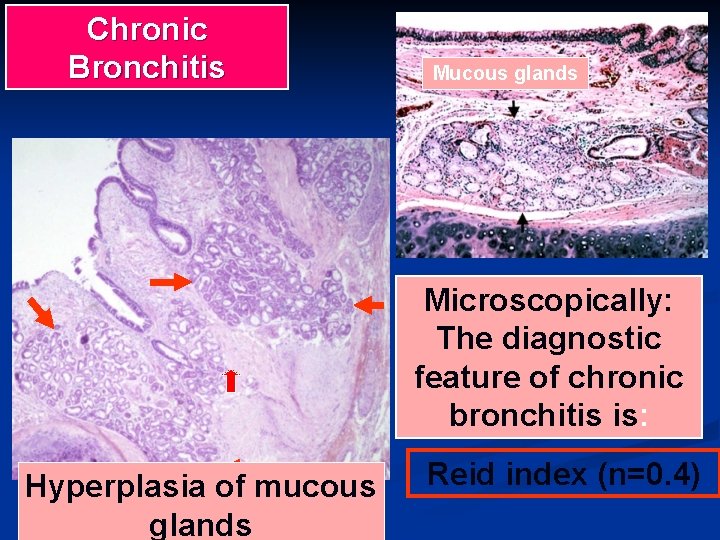
histologic features chronic inflammation of the airways (predominantly lymphocytes) ü enlargement of the mucus-secreting glands of the trachea , bronchi (hyperplasia) ü ü This increase can be assessed by the ratio of the thickness of the mucous gland layer to the thickness of the wall between the epithelium and the cartilage (Reid index).
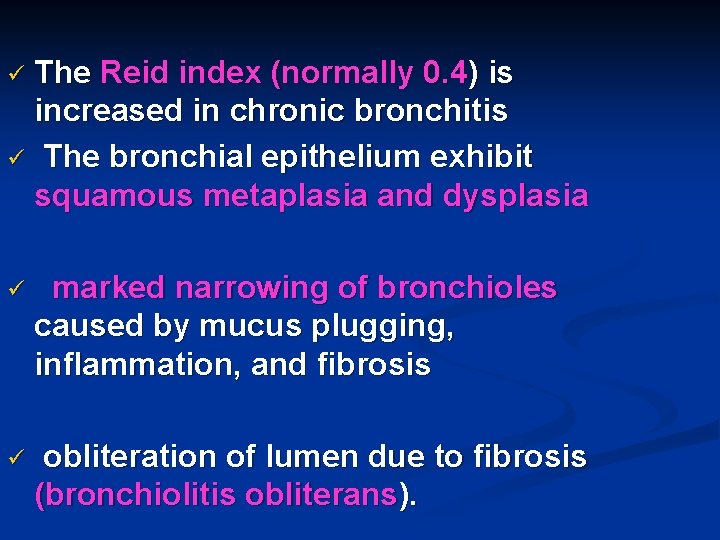
The Reid index (normally 0. 4) is increased in chronic bronchitis ü The bronchial epithelium exhibit squamous metaplasia and dysplasia ü ü marked narrowing of bronchioles caused by mucus plugging, inflammation, and fibrosis ü obliteration of lumen due to fibrosis (bronchiolitis obliterans).

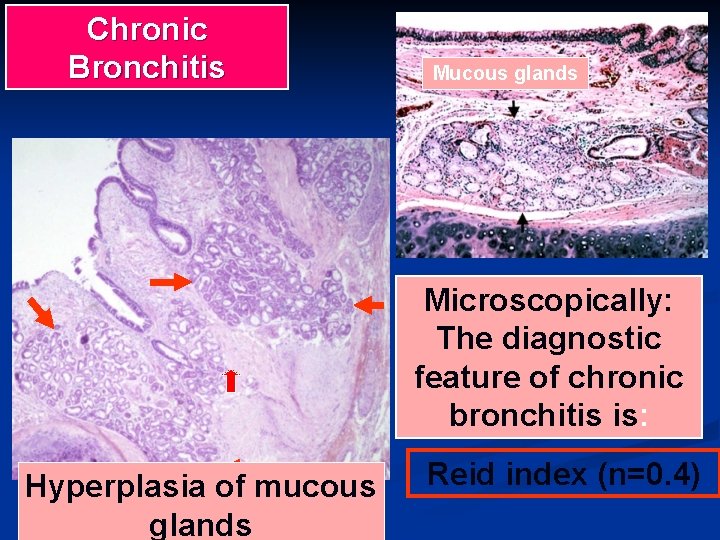
Chronic Bronchitis Mucous glands Microscopically: The diagnostic feature of chronic bronchitis is: Hyperplasia of mucous glands Reid index (n=0. 4)
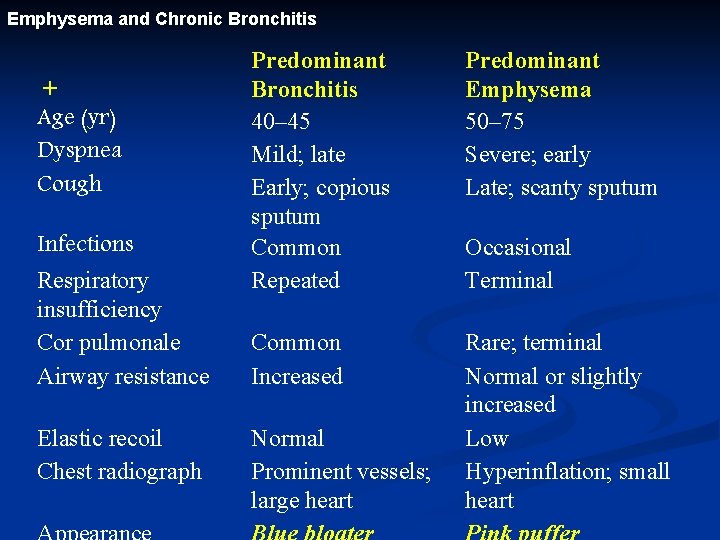
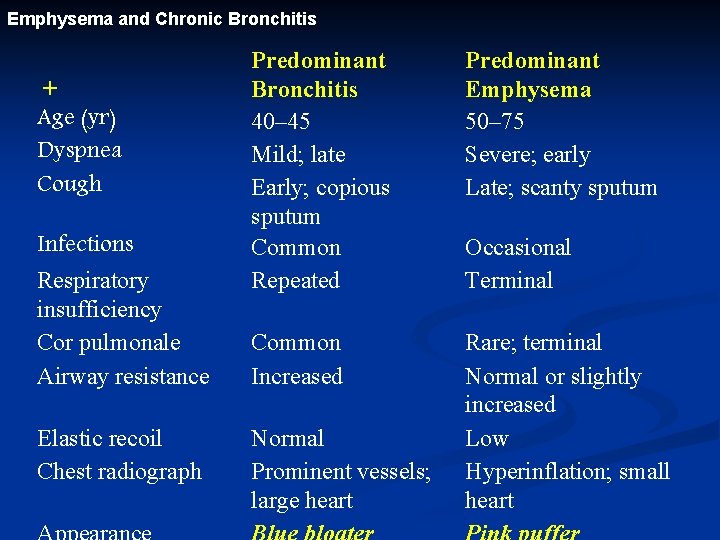
Emphysema and Chronic Bronchitis + Age (yr) Dyspnea Cough Infections Respiratory insufficiency Cor pulmonale Airway resistance Elastic recoil Chest radiograph Predominant Bronchitis 40– 45 Mild; late Early; copious sputum Common Repeated Predominant Emphysema 50– 75 Severe; early Late; scanty sputum Common Increased Rare; terminal Normal or slightly increased Low Hyperinflation; small heart Normal Prominent vessels; large heart Occasional Terminal

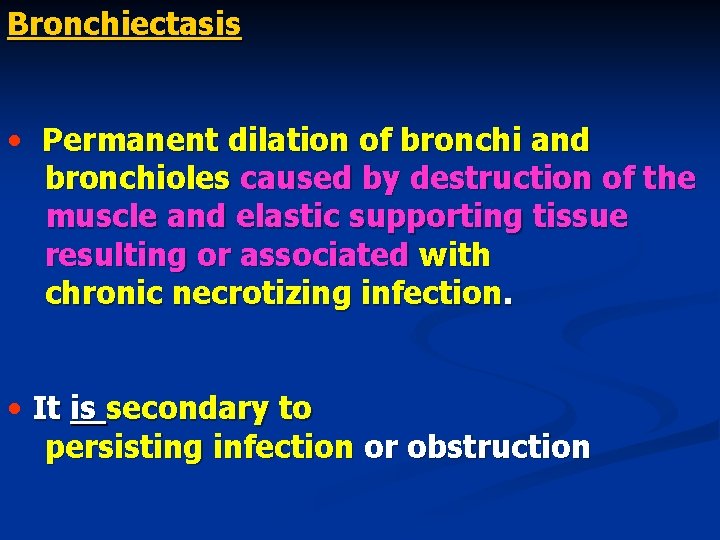
Bronchiectasis • Permanent dilation of bronchi and bronchioles caused by destruction of the muscle and elastic supporting tissue resulting or associated with chronic necrotizing infection. • It is secondary to persisting infection or obstruction
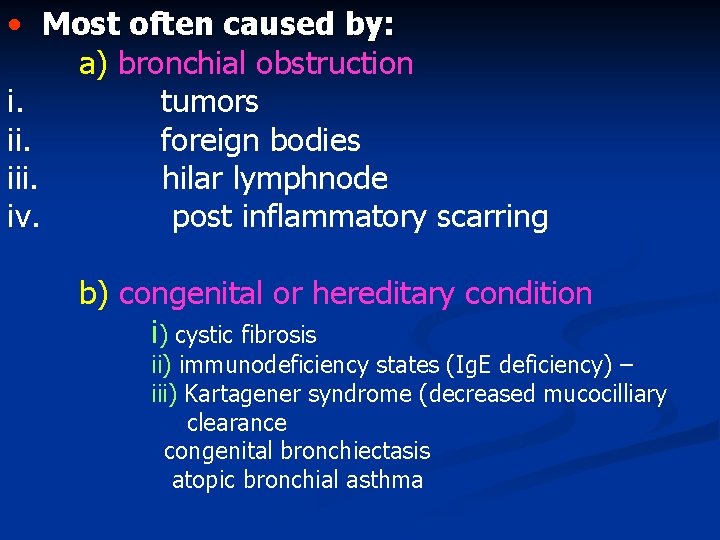
• Most often caused by: a) bronchial obstruction i. tumors ii. foreign bodies iii. hilar lymphnode iv. post inflammatory scarring b) congenital or hereditary condition i) cystic fibrosis ii) immunodeficiency states (Ig. E deficiency) – iii) Kartagener syndrome (decreased mucocilliary clearance congenital bronchiectasis atopic bronchial asthma
c) Secondry complication 1. necrotizing pneumonia (S. aureus, K. pneumoniae) 2. post tubercular bronchiectasis
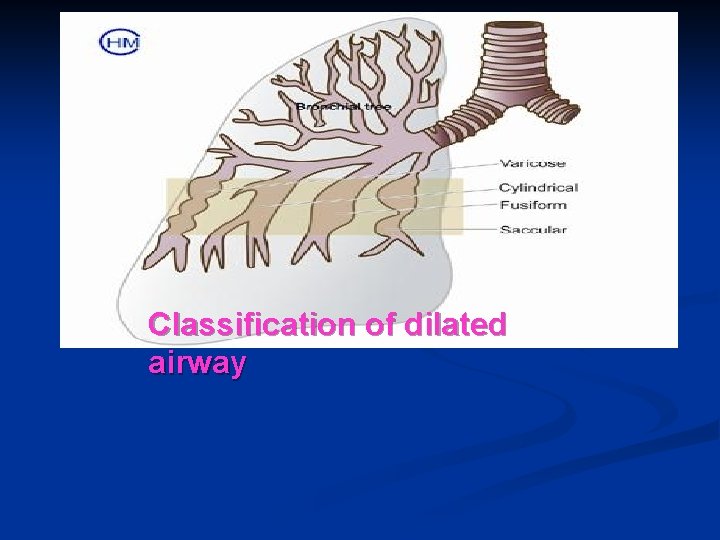
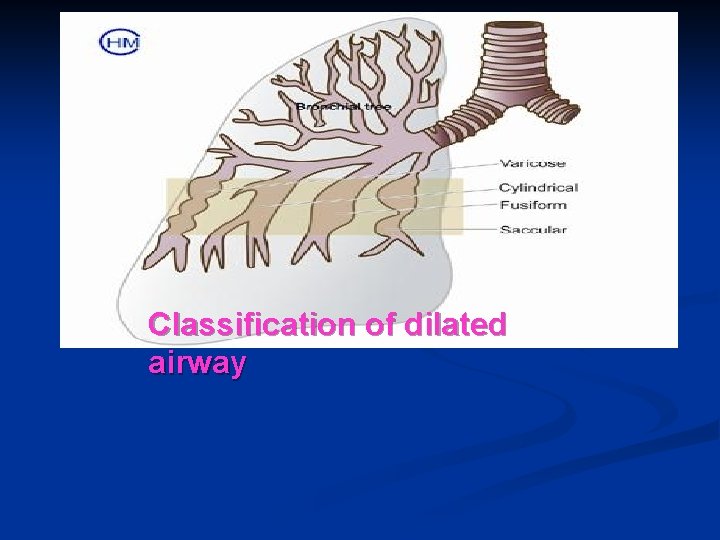
Classification of dilated airway
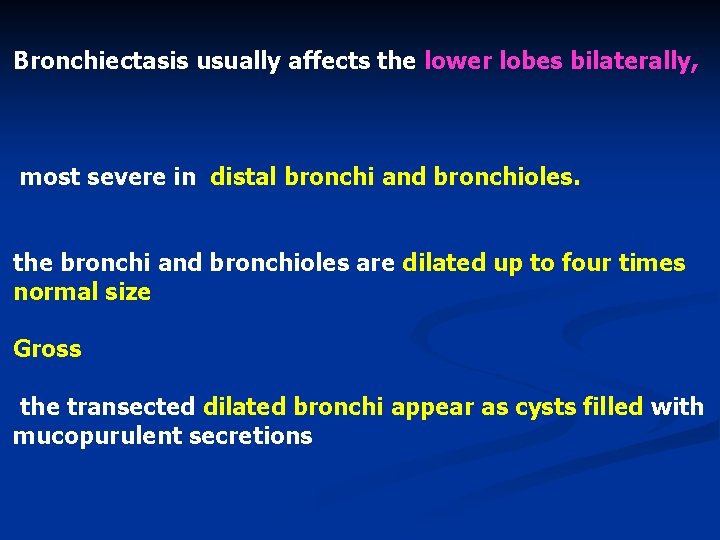
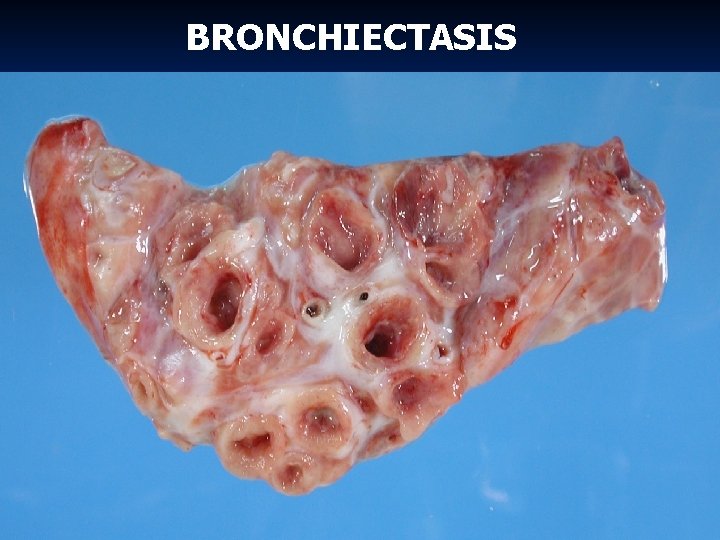
Bronchiectasis usually affects the lower lobes bilaterally, most severe in distal bronchi and bronchioles. the bronchi and bronchioles are dilated up to four times normal size Gross the transected dilated bronchi appear as cysts filled with mucopurulent secretions
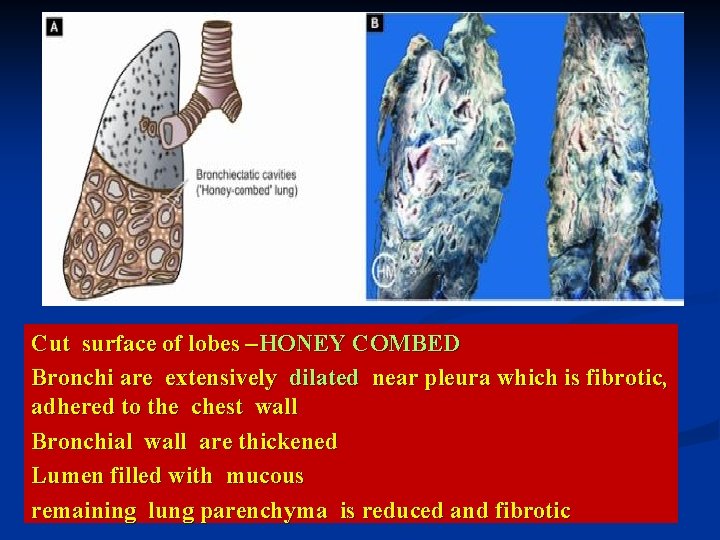
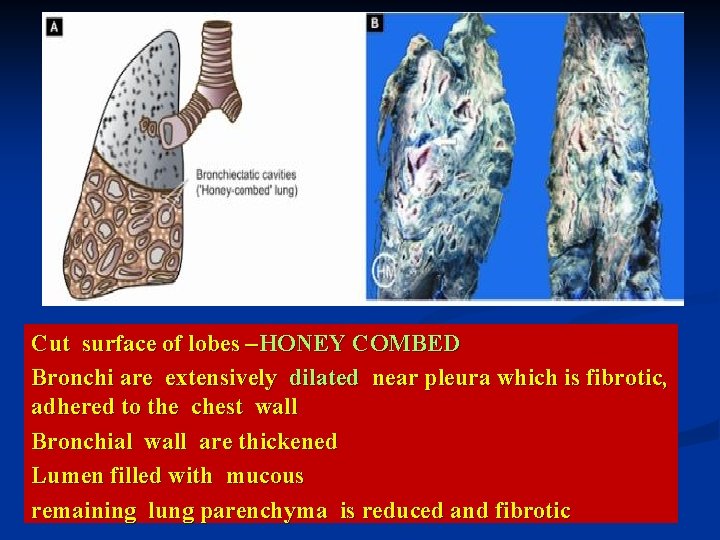
Cut surface of lobes –HONEY COMBED Bronchi are extensively dilated near pleura which is fibrotic, adhered to the chest wall Bronchial wall are thickened Lumen filled with mucous remaining lung parenchyma is reduced and fibrotic
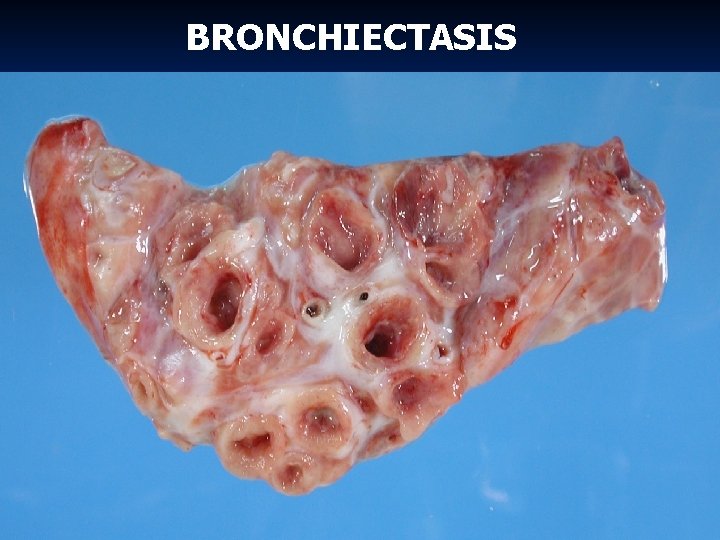
BRONCHIECTASIS
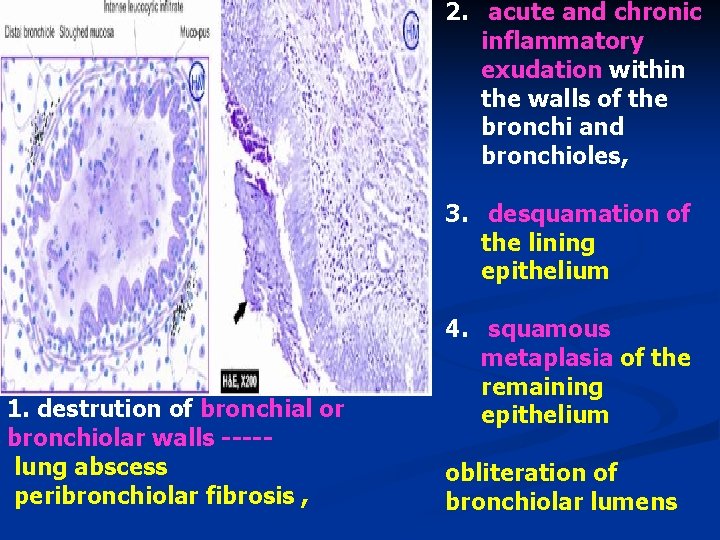
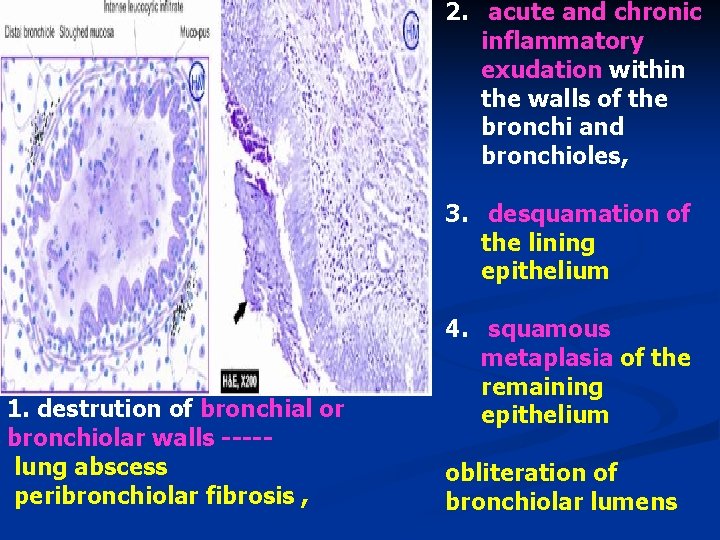
2. acute and chronic inflammatory exudation within the walls of the bronchi and bronchioles, 3. desquamation of the lining epithelium 1. destrution of bronchial or bronchiolar walls ----lung abscess peribronchiolar fibrosis , 4. squamous metaplasia of the remaining epithelium obliteration of bronchiolar lumens
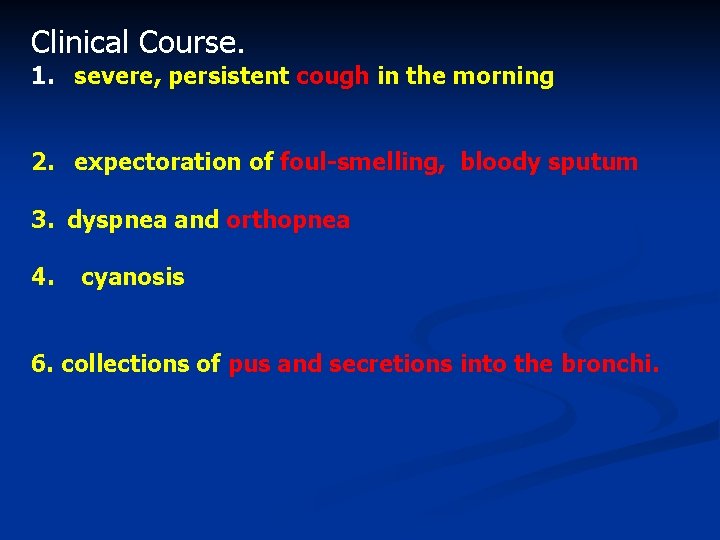
Clinical Course. 1. severe, persistent cough in the morning 2. expectoration of foul-smelling, bloody sputum 3. dyspnea and orthopnea 4. cyanosis 6. collections of pus and secretions into the bronchi.
complications of bronchiectasis Cor pulmonale brain abscesses amyloidosis


Important questions for COPD Q 1 -- ENUMERATE VARIOUS CAUSES OF COPD n Q 2 -- WRITE DOWN THE ETIOPATHOGENESIS OF EMPHYSEMA n Q 3—WRITE BRIEFLY ABOUT bronchiectasis n Q 4 WRITE SHORT NOTE ON EXTRINSIC ASTHAMA n
WRITE DOWN THE DIFFERENCES IN BETWEEN Q 1 - Differences between extrinsic and intrinsic asthma n Q 2 - Differentiate between chronic bronchitis and emphysema n Q 3 - Differences between centriacinar and panacinar emphysema n Q 4 - Obstructive versus Restrictive Pulmonary Diseases n