Asthma or COPD or ACOS Asthma COPD crossover
- Slides: 35
Asthma, or COPD, or ACOS (Asthma + COPD crossover Syndrome, or something else? And WHY does it matter which label? WECCG – time to Learn -- Respiratory 9 th July 2019
Some Treatment is the same • Asthma, COPD, ACOS, ILD etc: • ALL MUST have • Smoking cessation support • Agreed self management of exacerbations • Accurate diagnosis • Patient empowerment 9 th July 2019 WECCG 2
Some Treatment is different • Asthma – MUST have ICS • There is NO step 1 = SABA only • Mild COPD can be treated with LAMA/LABA – this can be fatal if patient has Asthma • Other Dx have different management 9 th July 2019 WECCG 3
Consider COPD if patient has: any of: • Dyspnoea • Chronic cough or sputum • Recurrent lower respiratory tract infections • Hx of exposure to risk (Smoke, weed, flour dust) 9 th July 2019 WECCG – GOLD Dx COPD 2019 4
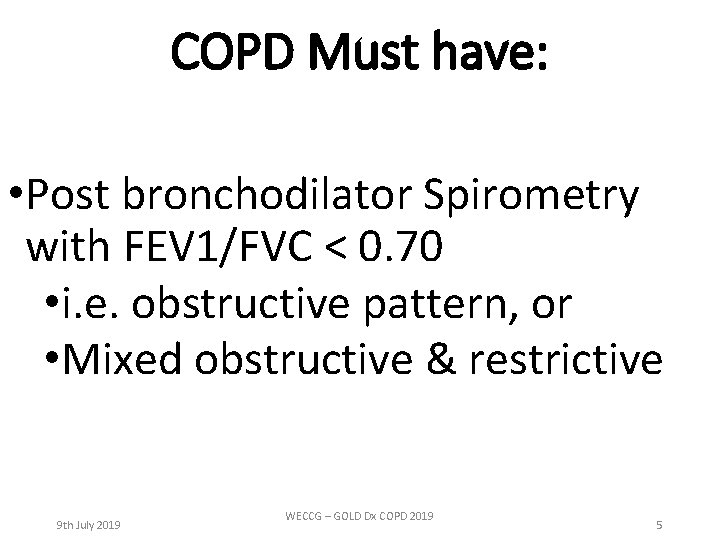
COPD Must have: • Post bronchodilator Spirometry with FEV 1/FVC < 0. 70 • i. e. obstructive pattern, or • Mixed obstructive & restrictive 9 th July 2019 WECCG – GOLD Dx COPD 2019 5
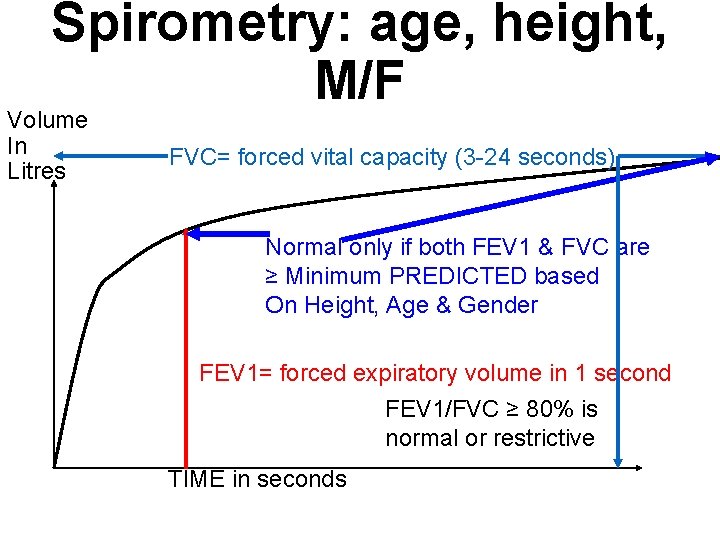
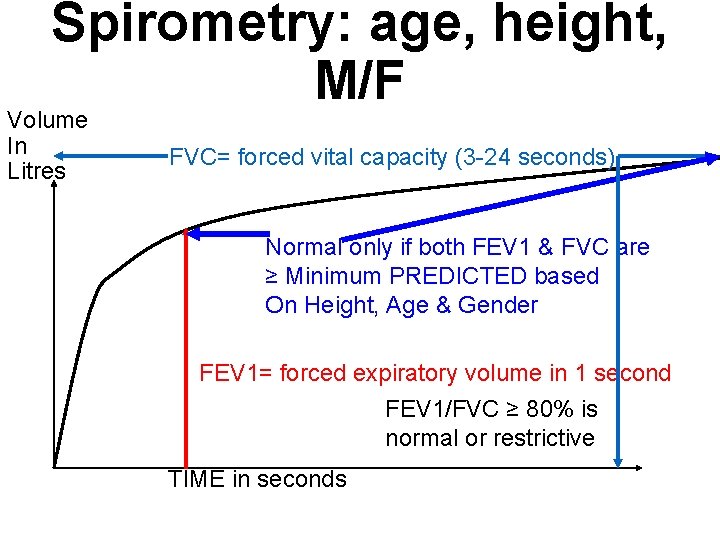
Spirometry: age, height, M/F Volume In Litres FVC= forced vital capacity (3 -24 seconds) Normal only if both FEV 1 & FVC are ≥ Minimum PREDICTED based On Height, Age & Gender FEV 1= forced expiratory volume in 1 second FEV 1/FVC ≥ 80% is normal or restrictive TIME in seconds
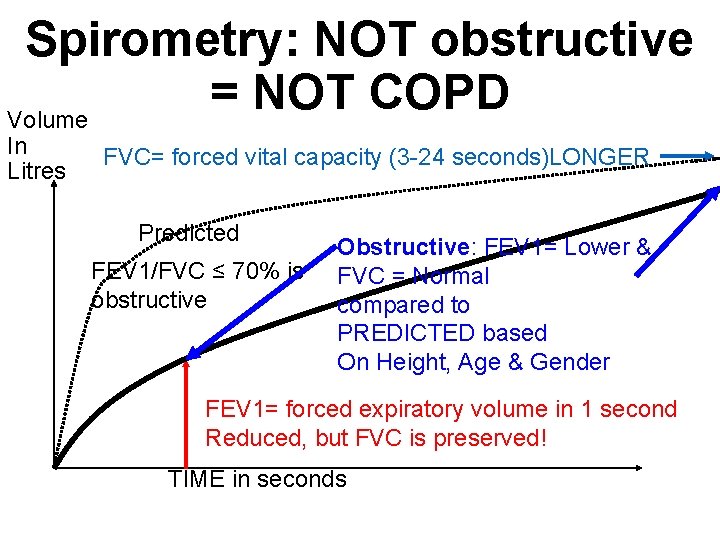
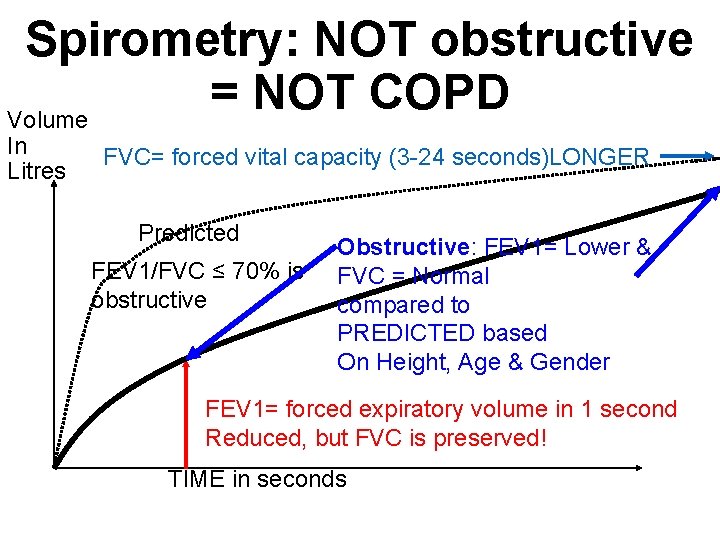
Spirometry: NOT obstructive = NOT COPD Volume In Litres FVC= forced vital capacity (3 -24 seconds)LONGER Predicted FEV 1/FVC ≤ 70% is obstructive Obstructive: FEV 1= Lower & FVC = Normal compared to PREDICTED based On Height, Age & Gender FEV 1= forced expiratory volume in 1 second Reduced, but FVC is preserved! TIME in seconds
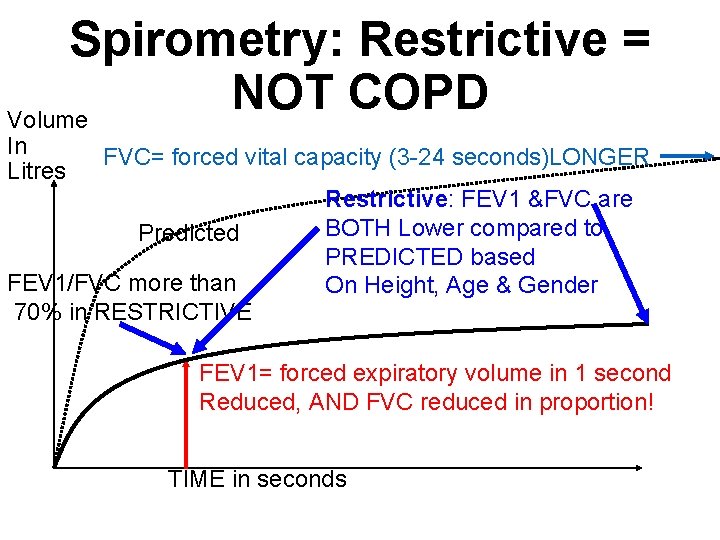
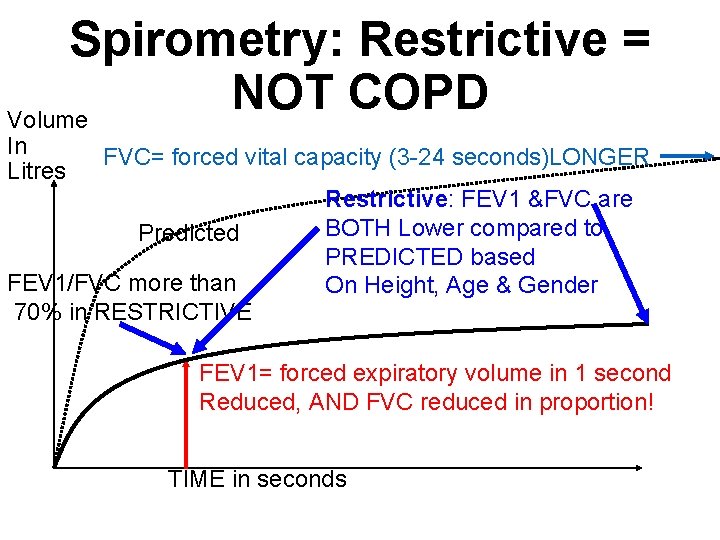
Spirometry: Restrictive = NOT COPD Volume In Litres FVC= forced vital capacity (3 -24 seconds)LONGER Predicted FEV 1/FVC more than 70% in RESTRICTIVE Restrictive: FEV 1 &FVC are BOTH Lower compared to PREDICTED based On Height, Age & Gender FEV 1= forced expiratory volume in 1 second Reduced, AND FVC reduced in proportion! TIME in seconds
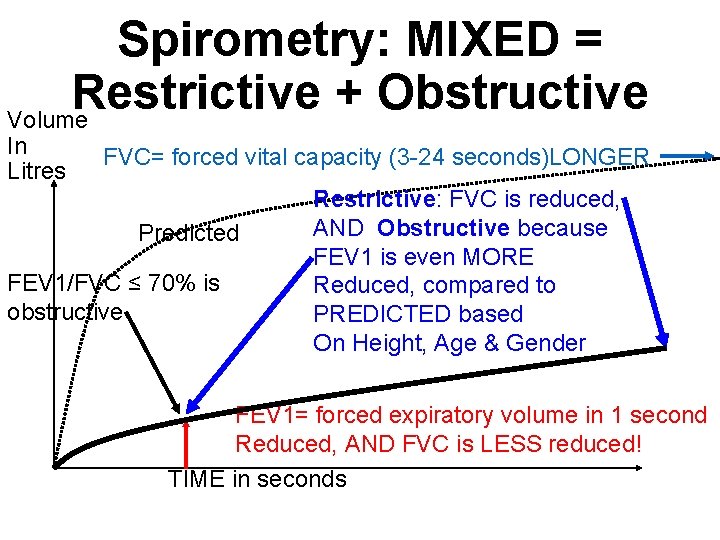
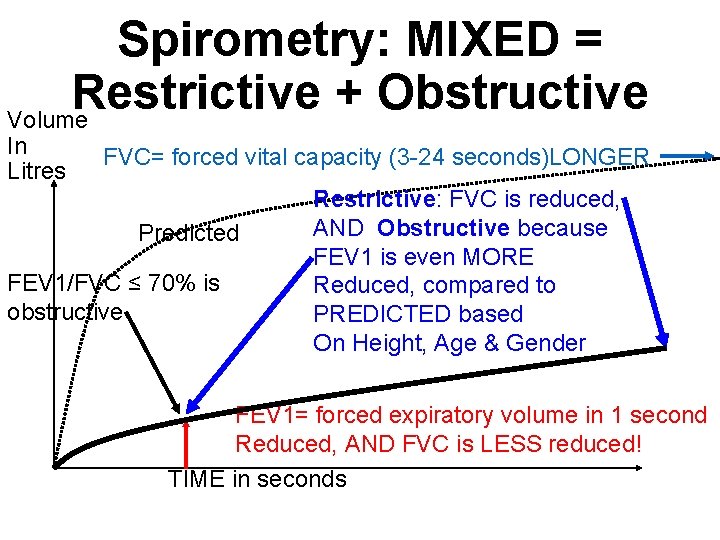
Spirometry: MIXED = Restrictive + Obstructive Volume In Litres FVC= forced vital capacity (3 -24 seconds)LONGER Predicted FEV 1/FVC ≤ 70% is obstructive Restrictive: FVC is reduced, AND Obstructive because FEV 1 is even MORE Reduced, compared to PREDICTED based On Height, Age & Gender FEV 1= forced expiratory volume in 1 second Reduced, AND FVC is LESS reduced! TIME in seconds
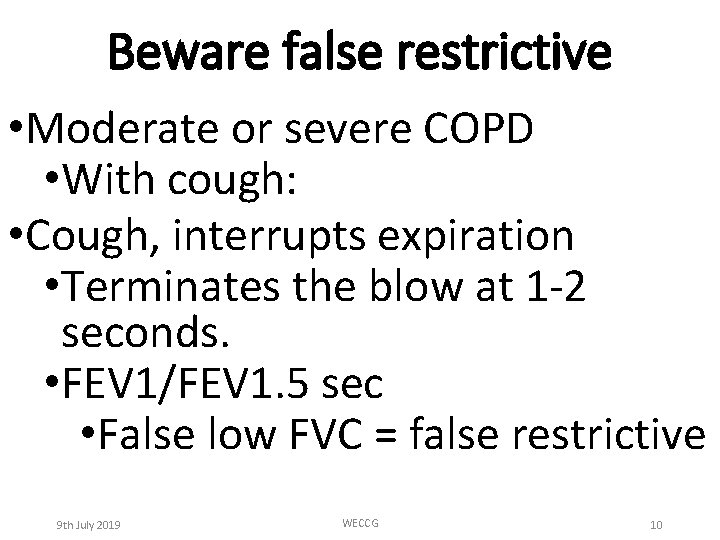
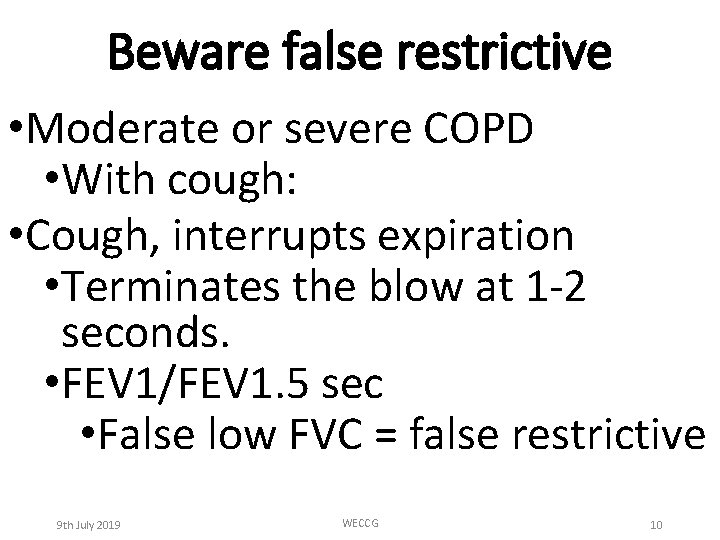
Beware false restrictive • Moderate or severe COPD • With cough: • Cough, interrupts expiration • Terminates the blow at 1 -2 seconds. • FEV 1/FEV 1. 5 sec • False low FVC = false restrictive 9 th July 2019 WECCG 10
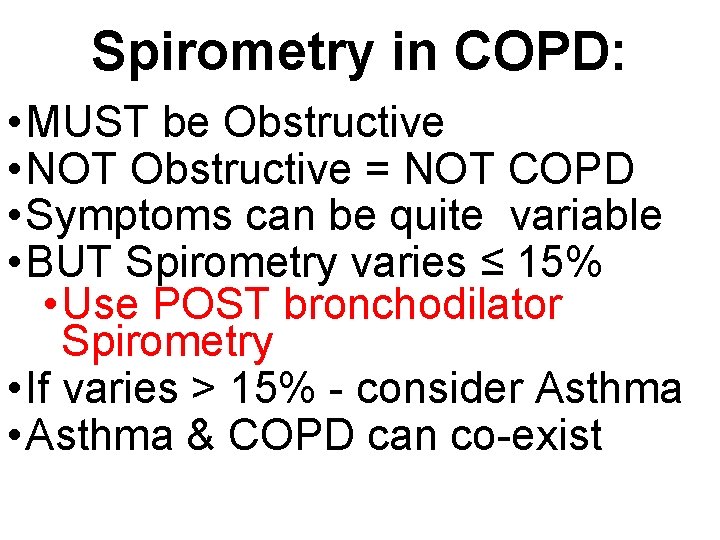
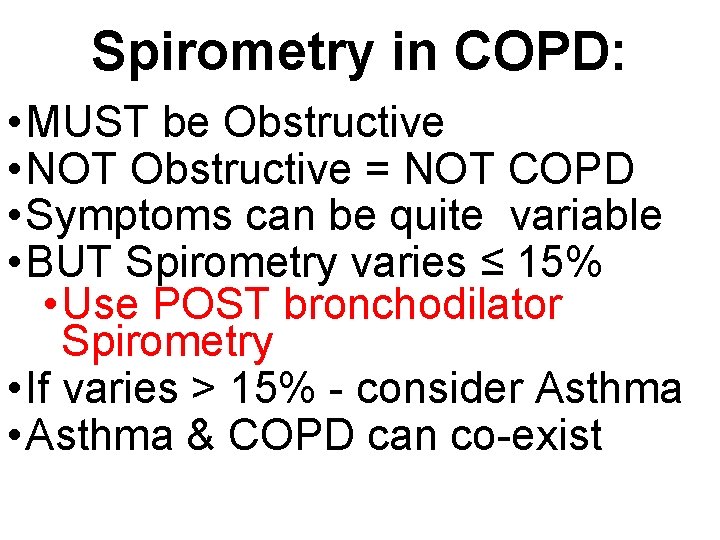
Spirometry in COPD: • MUST be Obstructive • NOT Obstructive = NOT COPD • Symptoms can be quite variable • BUT Spirometry varies ≤ 15% • Use POST bronchodilator Spirometry • If varies > 15% - consider Asthma • Asthma & COPD can co-exist
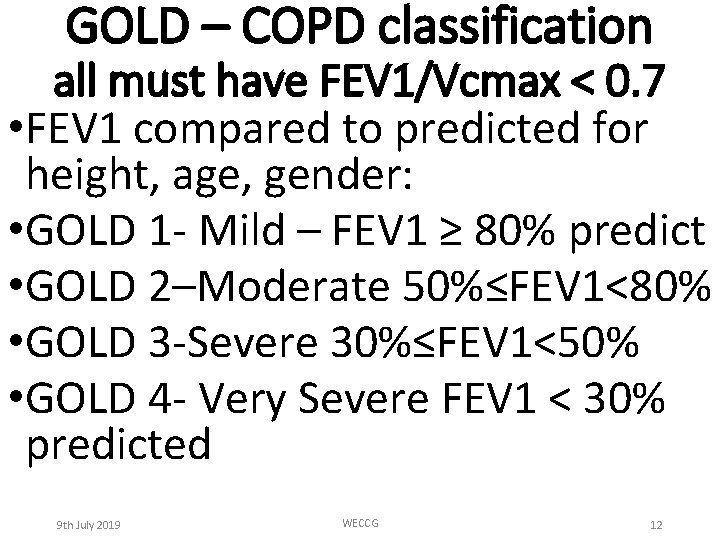
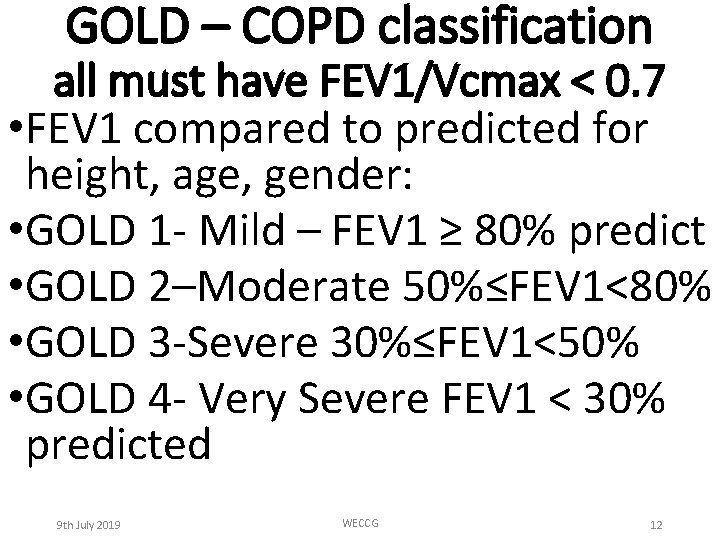
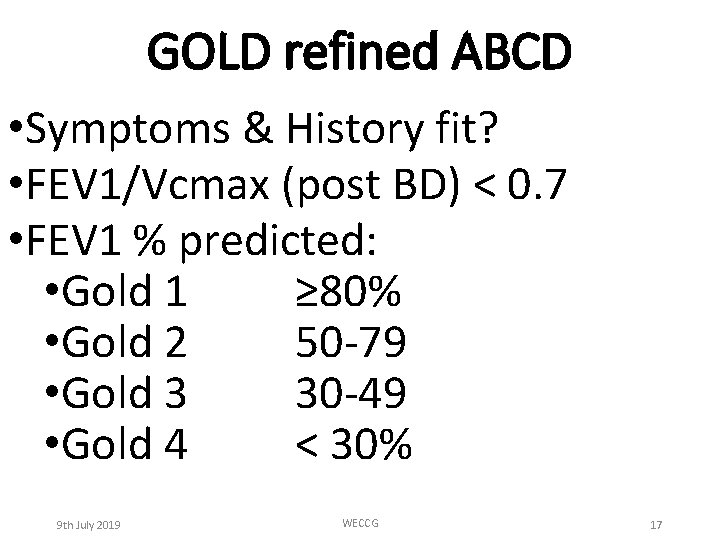
GOLD – COPD classification all must have FEV 1/Vcmax < 0. 7 • FEV 1 compared to predicted for height, age, gender: • GOLD 1 - Mild – FEV 1 ≥ 80% predict • GOLD 2–Moderate 50%≤FEV 1<80% • GOLD 3 -Severe 30%≤FEV 1<50% • GOLD 4 - Very Severe FEV 1 < 30% predicted 9 th July 2019 WECCG 12
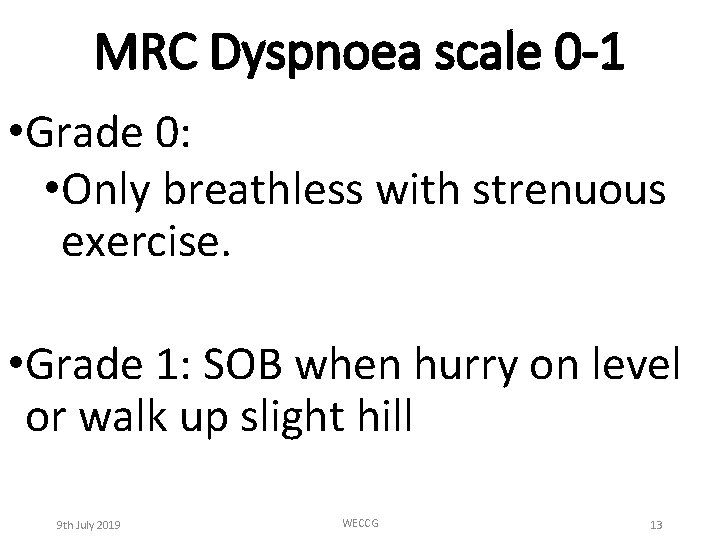
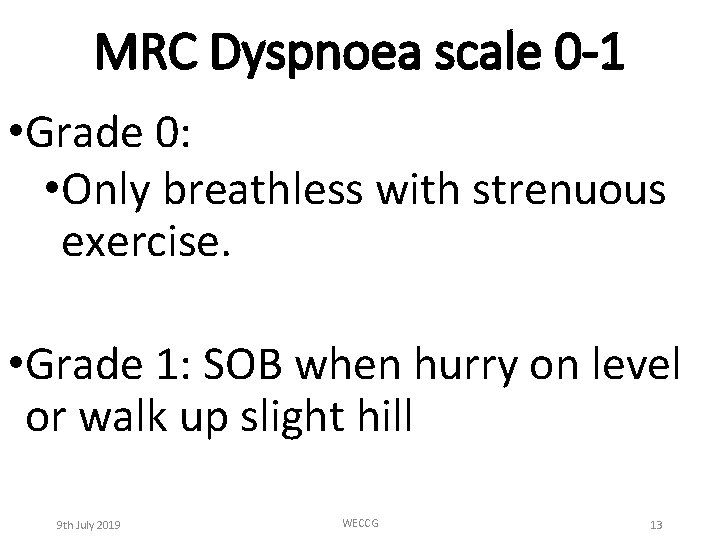
MRC Dyspnoea scale 0 -1 • Grade 0: • Only breathless with strenuous exercise. • Grade 1: SOB when hurry on level or walk up slight hill 9 th July 2019 WECCG 13
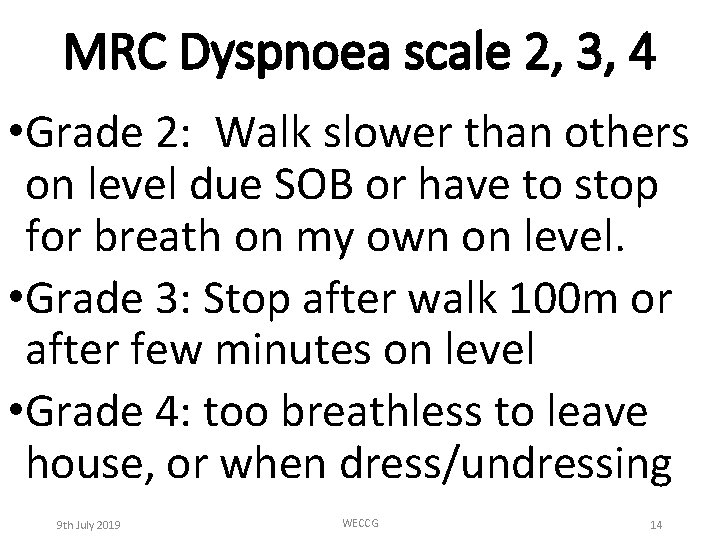
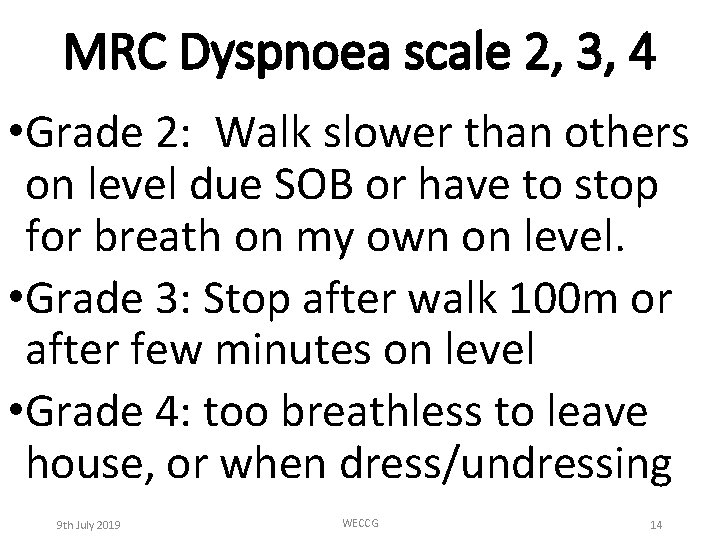
MRC Dyspnoea scale 2, 3, 4 • Grade 2: Walk slower than others on level due SOB or have to stop for breath on my own on level. • Grade 3: Stop after walk 100 m or after few minutes on level • Grade 4: too breathless to leave house, or when dress/undressing 9 th July 2019 WECCG 14
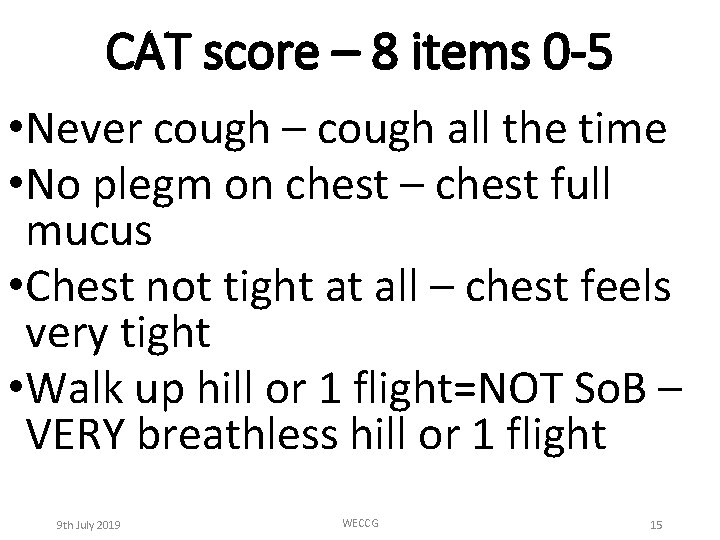
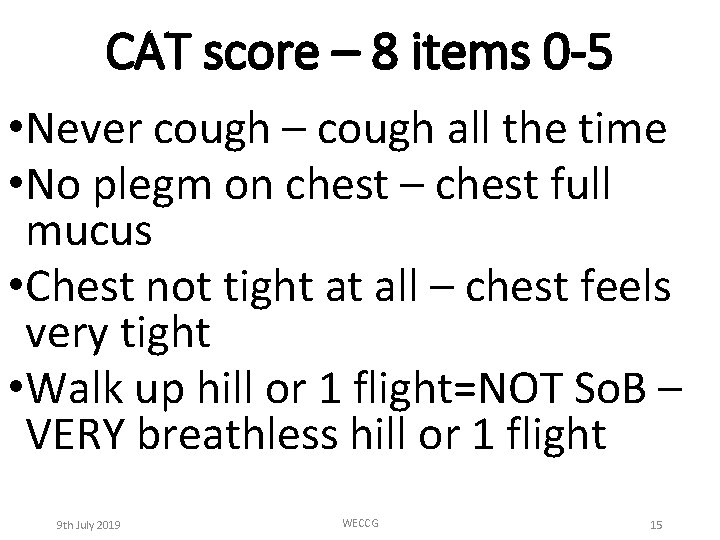
CAT score – 8 items 0 -5 • Never cough – cough all the time • No plegm on chest – chest full mucus • Chest not tight at all – chest feels very tight • Walk up hill or 1 flight=NOT So. B – VERY breathless hill or 1 flight 9 th July 2019 WECCG 15
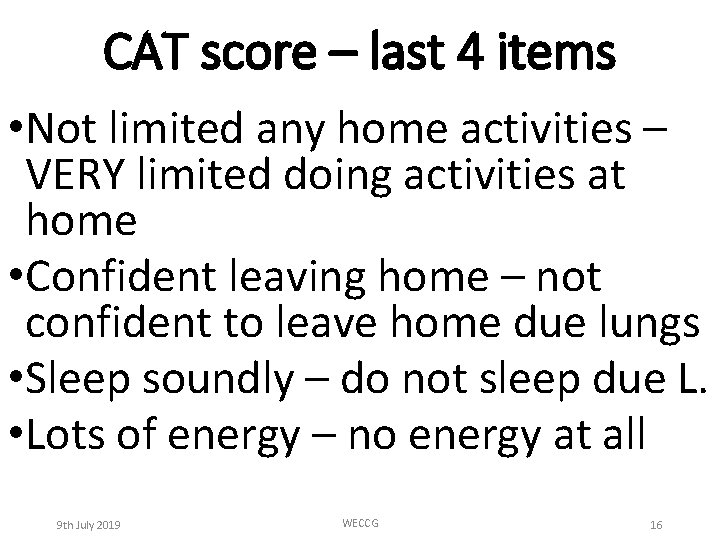
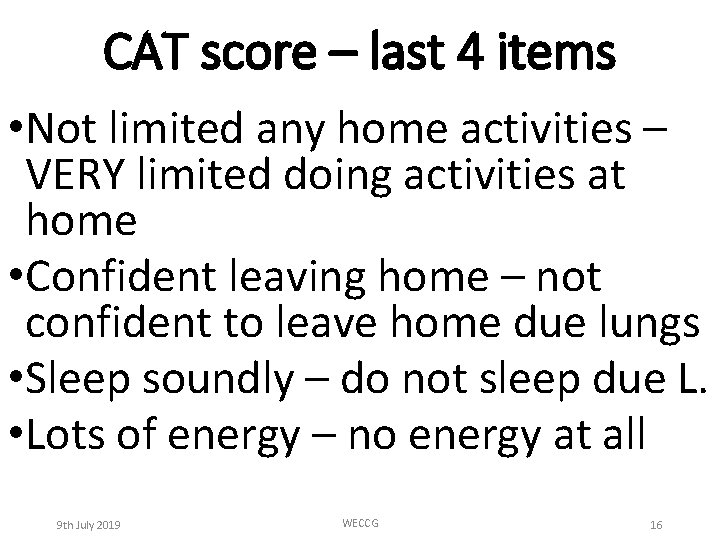
CAT score – last 4 items • Not limited any home activities – VERY limited doing activities at home • Confident leaving home – not confident to leave home due lungs • Sleep soundly – do not sleep due L. • Lots of energy – no energy at all 9 th July 2019 WECCG 16
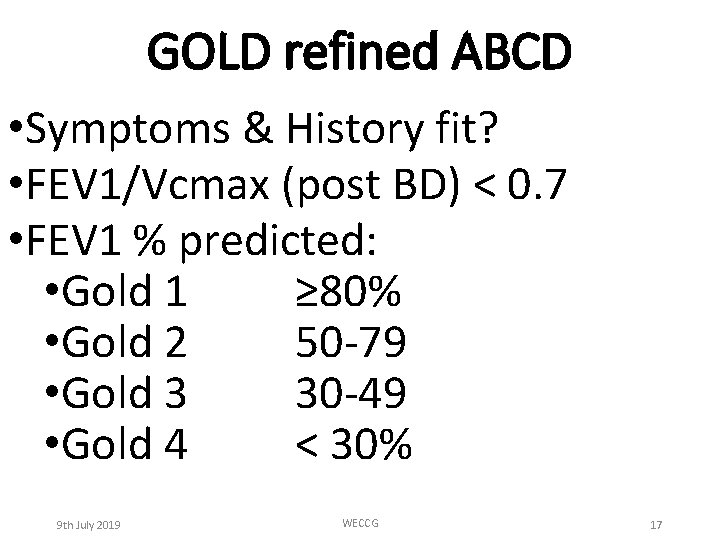
GOLD refined ABCD • Symptoms & History fit? • FEV 1/Vcmax (post BD) < 0. 7 • FEV 1 % predicted: • Gold 1 ≥ 80% • Gold 2 50 -79 • Gold 3 30 -49 • Gold 4 < 30% 9 th July 2019 WECCG 17
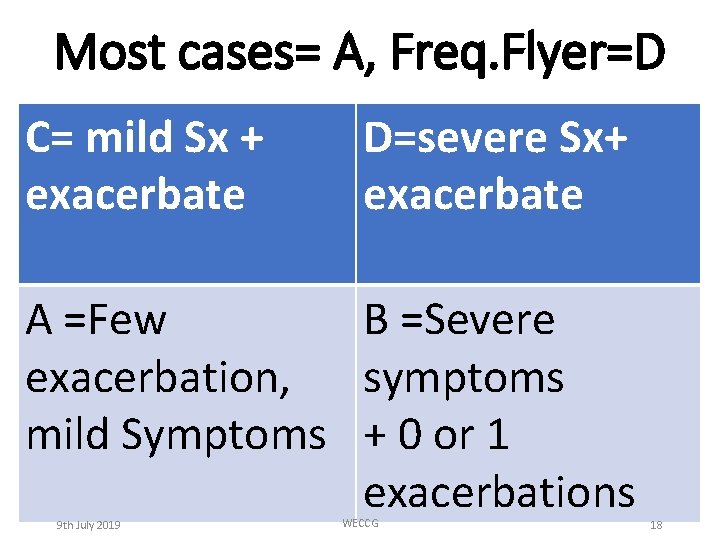
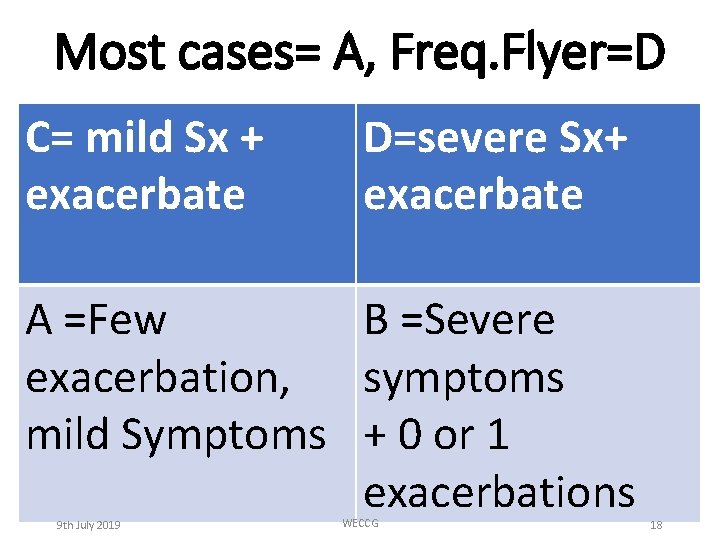
Most cases= A, Freq. Flyer=D C= mild Sx + exacerbate D=severe Sx+ exacerbate A =Few B =Severe exacerbation, symptoms mild Symptoms + 0 or 1 exacerbations 9 th July 2019 WECCG 18
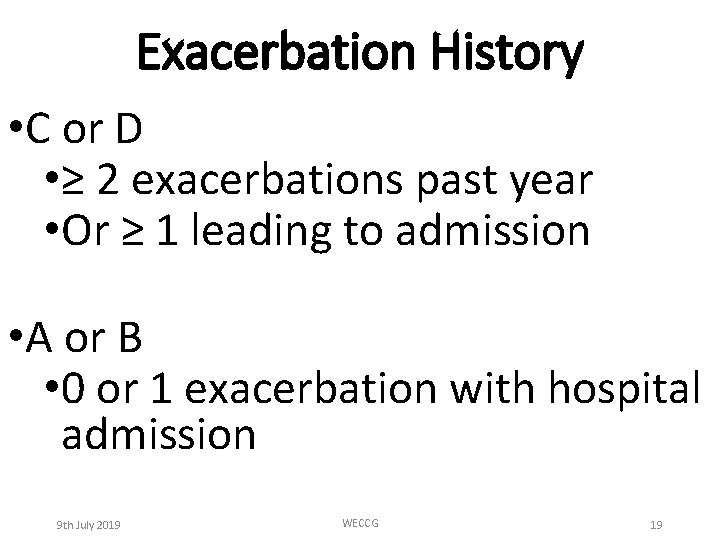
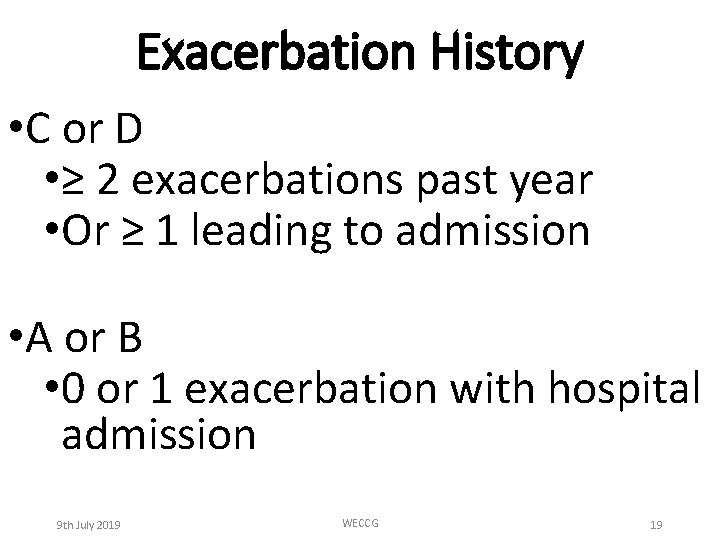
Exacerbation History • C or D • ≥ 2 exacerbations past year • Or ≥ 1 leading to admission • A or B • 0 or 1 exacerbation with hospital admission 9 th July 2019 WECCG 19
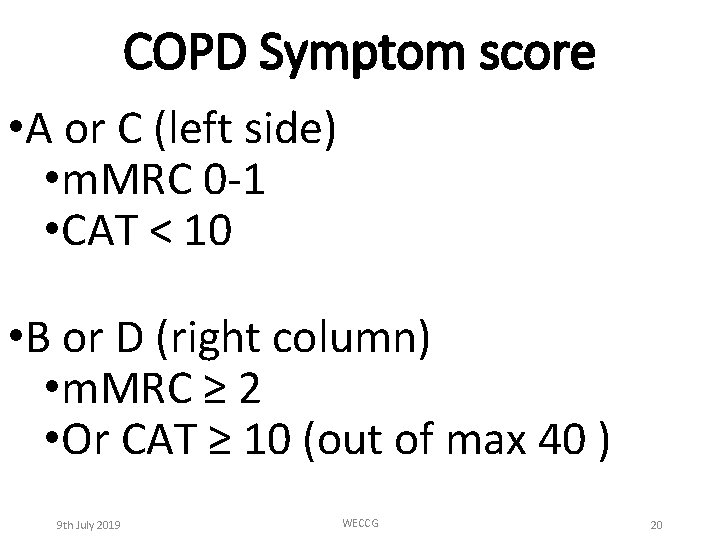
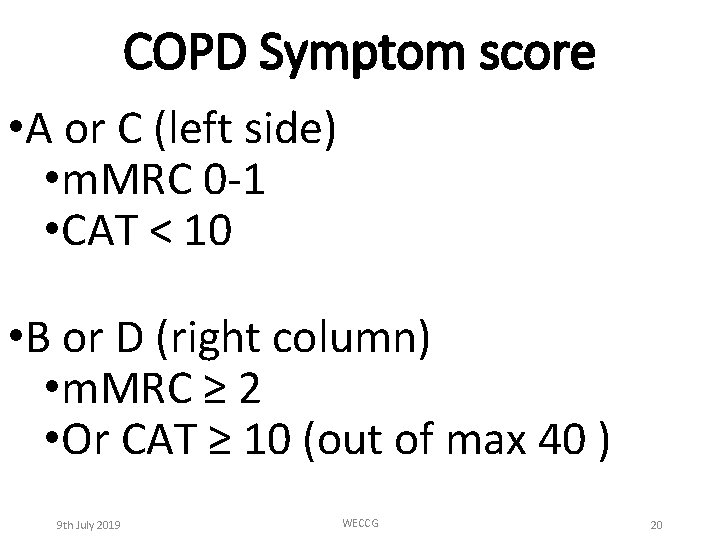
COPD Symptom score • A or C (left side) • m. MRC 0 -1 • CAT < 10 • B or D (right column) • m. MRC ≥ 2 • Or CAT ≥ 10 (out of max 40 ) 9 th July 2019 WECCG 20
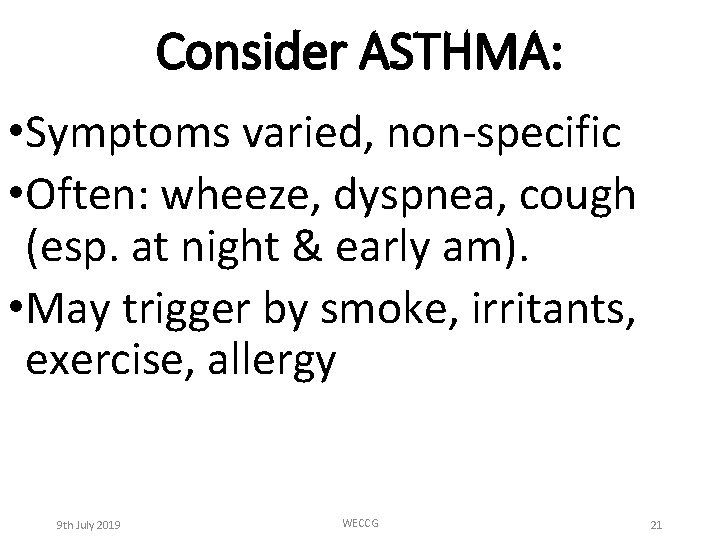
Consider ASTHMA: • Symptoms varied, non-specific • Often: wheeze, dyspnea, cough (esp. at night & early am). • May trigger by smoke, irritants, exercise, allergy 9 th July 2019 WECCG 21
Spirometry in Asthma • May or may not show reversability at any one time • Can be any pattern- restrict/obs • Variability is key 9 th July 2019 WECCG 22
Action point: • Do NOT cancel spirometry when patient arrives symptomatic and / or with recent chest infecrion. • This does not save resources (apt already consumed) but robs us of information on reversability. 9 th July 2019 WECCG 23
When is it “Pure COPD? ” • First onset > 40 years old. • ≥ 20 pack years smoking exposure • Symptoms vary, but FEV 1 & PEF vary less than 10% • (do get spiro when symptomatic) • MUST have obstructive post BD spirometry 9 th July 2019 WECCG 24
Suspect asthma element? ? • Onset of symptoms before 40 • Hx of atopy, hay fever, marked allergy • Eosinophilia, or high Ig. E • Variability • Wheezing & cough esp. at night 9 th July 2019 WECCG 25
Spirometry in Asthma • If Asthma is the only Diagnosis: • Then Must have normal spiro between exacerbations • When symptomatic, • can be nearly normal, • Usually restrictive, can be obstructive • Occasionaly mixed (consider Asthma+COPD)
Fixed Restrictive Spirometry • Wide differential diagnosis • CXR, repeat, then refer to Hospital • Differential Diagnosis (Diff. Dx): • CCF (Heart failure) PE • Pneumothorax Chest wall disease • Lung cancer Lobectomy • Scaring, old MTB (Tuberculosis), interstial lung disease, • Pneumonia Pleural Disease
Adult Bronchiectasis • High mucous production • Sometimes so thick cannot get it out • Grows unusual/resistant Bugs • DO sputum cultures frequently • Longer & prompt rescue packs • Antibiotics AND steroids • Get HRCT 9 th July 2019 WECCG 28
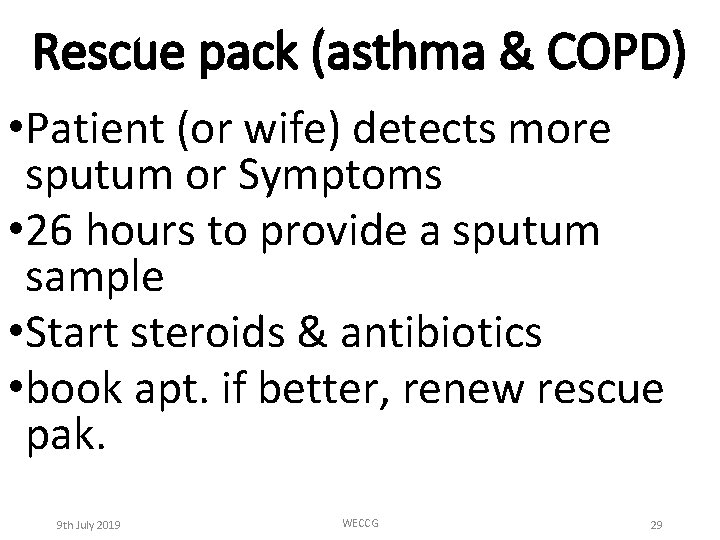
Rescue pack (asthma & COPD) • Patient (or wife) detects more sputum or Symptoms • 26 hours to provide a sputum sample • Start steroids & antibiotics • book apt. if better, renew rescue pak. 9 th July 2019 WECCG 29
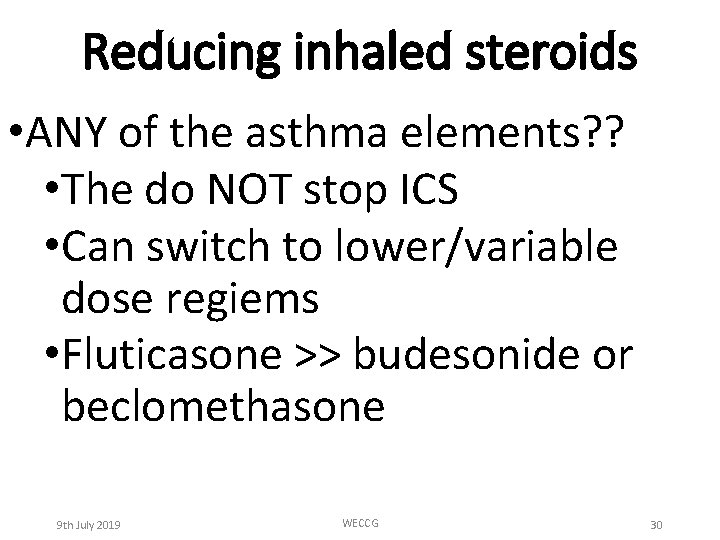
Reducing inhaled steroids • ANY of the asthma elements? ? • The do NOT stop ICS • Can switch to lower/variable dose regiems • Fluticasone >> budesonide or beclomethasone 9 th July 2019 WECCG 30
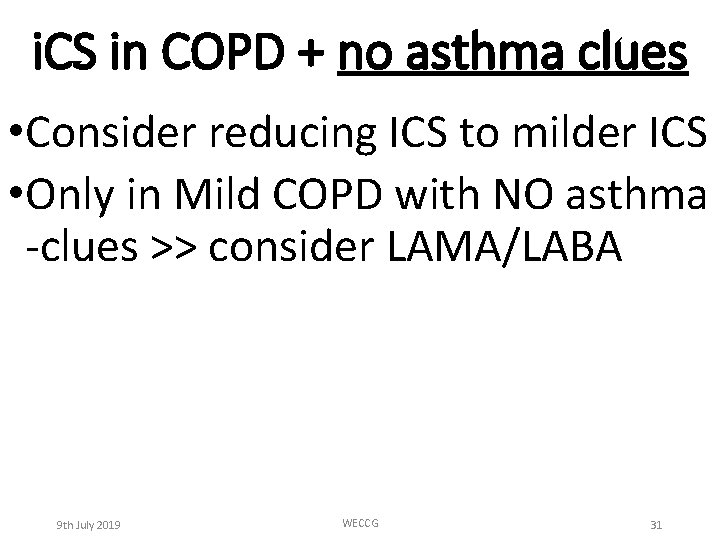
i. CS in COPD + no asthma clues • Consider reducing ICS to milder ICS • Only in Mild COPD with NO asthma -clues >> consider LAMA/LABA 9 th July 2019 WECCG 31
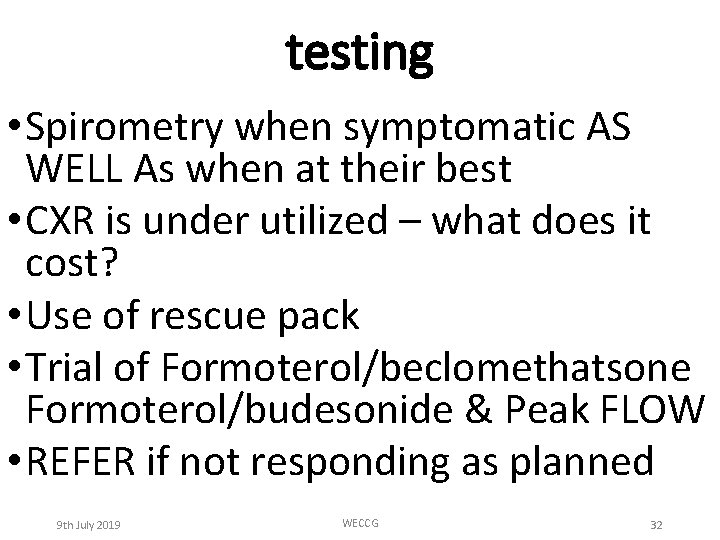
testing • Spirometry when symptomatic AS WELL As when at their best • CXR is under utilized – what does it cost? • Use of rescue pack • Trial of Formoterol/beclomethatsone Formoterol/budesonide & Peak FLOW • REFER if not responding as planned 9 th July 2019 WECCG 32
9 high impact interventions-1 -4 • Accurate Diagnosis • Co-morbidity (IHD prevention), frailty and end-of-life (if appropriate) • Flu Vaccine • CAT score, exacerbation & MRC dyspnoea 9 th July 2019 WECCG 33
9 high impact interventions-5 -9 • Smoking cessation • Pulmonary rehab • Optimize medication (include IHD prevention) • Self management / rescue pack • Patient empowerment & care navigation 9 th July 2019 WECCG 34
Your ideas? • What will you do differently? 9 th July 2019 WECCG 35