ASTHMA AND COPD Respiratory Emergency 3 ASTHMA EPIDEMIOLOGY


![기출 문제 01] (2012) 천식 환자에서 risk가 낮은 환 자? 가) 베타 흡입제 1달에 기출 문제 01] (2012) 천식 환자에서 risk가 낮은 환 자? 가) 베타 흡입제 1달에](https://slidetodoc.com/presentation_image/48015bca88b3b9ac6fcfc10235a78d27/image-33.jpg)
![기출 문제 [01] (2012) COPD 환자가 호흡곤란으로 내원하였다. 가장 심한 상태인 것 은? 1)FEV 기출 문제 [01] (2012) COPD 환자가 호흡곤란으로 내원하였다. 가장 심한 상태인 것 은? 1)FEV](https://slidetodoc.com/presentation_image/48015bca88b3b9ac6fcfc10235a78d27/image-35.jpg)
![기출 문제 <03 -04> 1. Chlamydophila pneumoniae [03] (2012) COPD 환자가 기침, 화농성 2. 기출 문제 <03 -04> 1. Chlamydophila pneumoniae [03] (2012) COPD 환자가 기침, 화농성 2.](https://slidetodoc.com/presentation_image/48015bca88b3b9ac6fcfc10235a78d27/image-37.jpg)
- Slides: 43
ASTHMA AND COPD Respiratory Emergency #3

ASTHMA
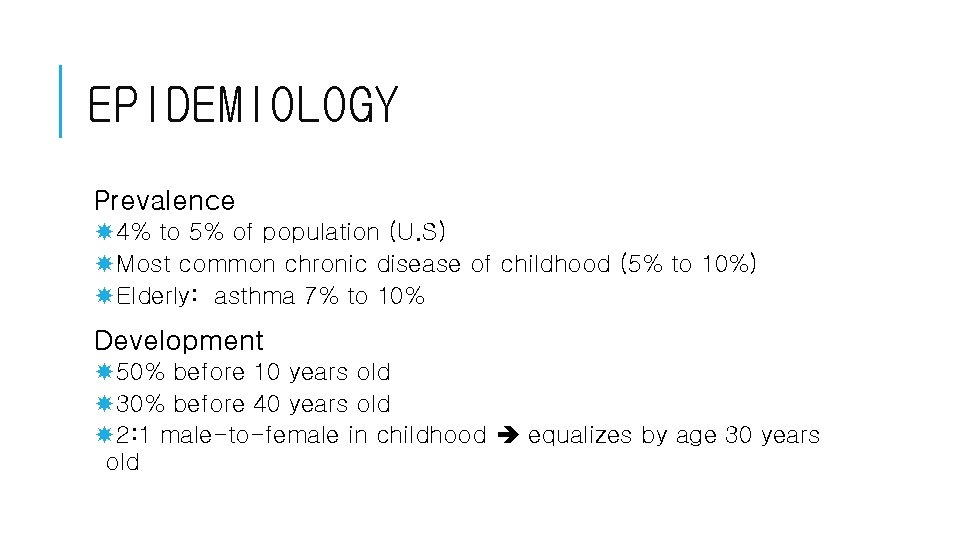
EPIDEMIOLOGY Prevalence 4% to 5% of population (U. S) Most common chronic disease of childhood (5% to 10%) Elderly: asthma 7% to 10% Development 50% before 10 years old 30% before 40 years old 2: 1 male-to-female in childhood equalizes by age 30 years old
http: //www. nhlbi. nih. gov/files/docs/guidelines/asthgdln. pdf
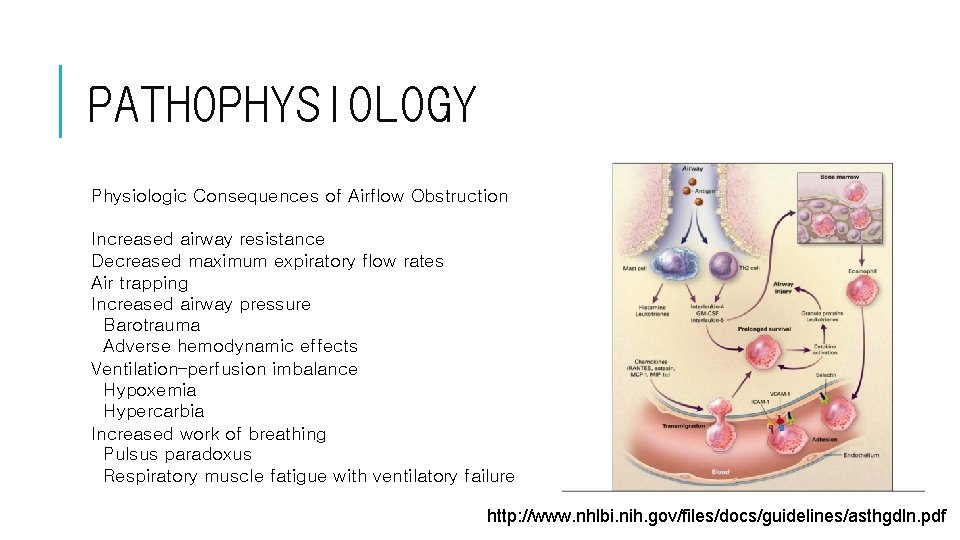
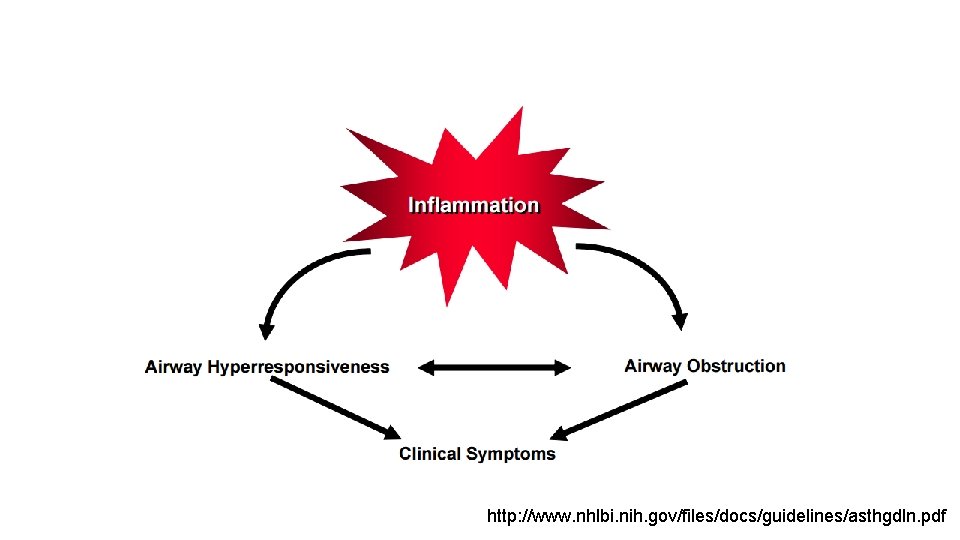
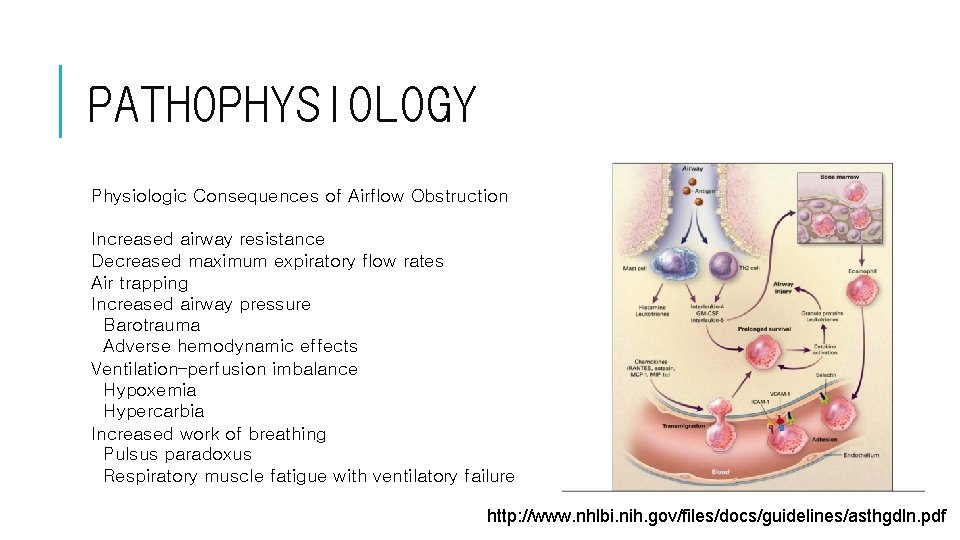
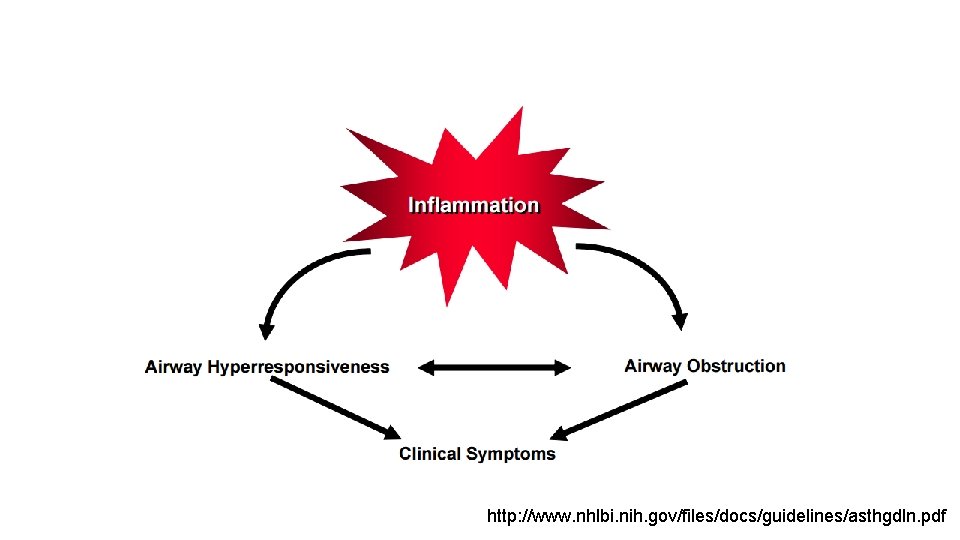
PATHOPHYSIOLOGY Physiologic Consequences of Airflow Obstruction Increased airway resistance Decreased maximum expiratory flow rates Air trapping Increased airway pressure Barotrauma Adverse hemodynamic effects Ventilation–perfusion imbalance Hypoxemia Hypercarbia Increased work of breathing Pulsus paradoxus Respiratory muscle fatigue with ventilatory failure http: //www. nhlbi. nih. gov/files/docs/guidelines/asthgdln. pdf
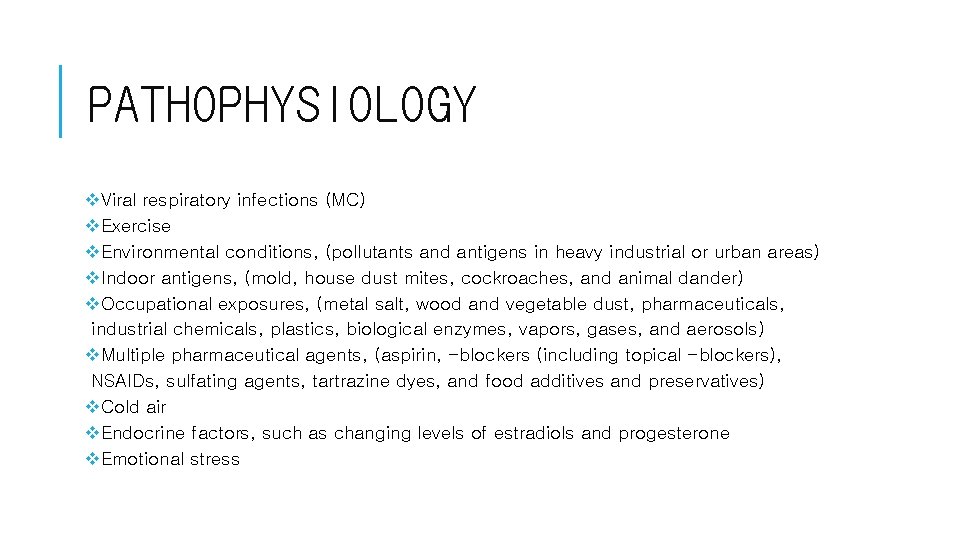
PATHOPHYSIOLOGY v. Viral respiratory infections (MC) v. Exercise v. Environmental conditions, (pollutants and antigens in heavy industrial or urban areas) v. Indoor antigens, (mold, house dust mites, cockroaches, and animal dander) v. Occupational exposures, (metal salt, wood and vegetable dust, pharmaceuticals, industrial chemicals, plastics, biological enzymes, vapors, gases, and aerosols) v. Multiple pharmaceutical agents, (aspirin, -blockers (including topical -blockers), NSAIDs, sulfating agents, tartrazine dyes, and food additives and preservatives) v. Cold air v. Endocrine factors, such as changing levels of estradiols and progesterone v. Emotional stress
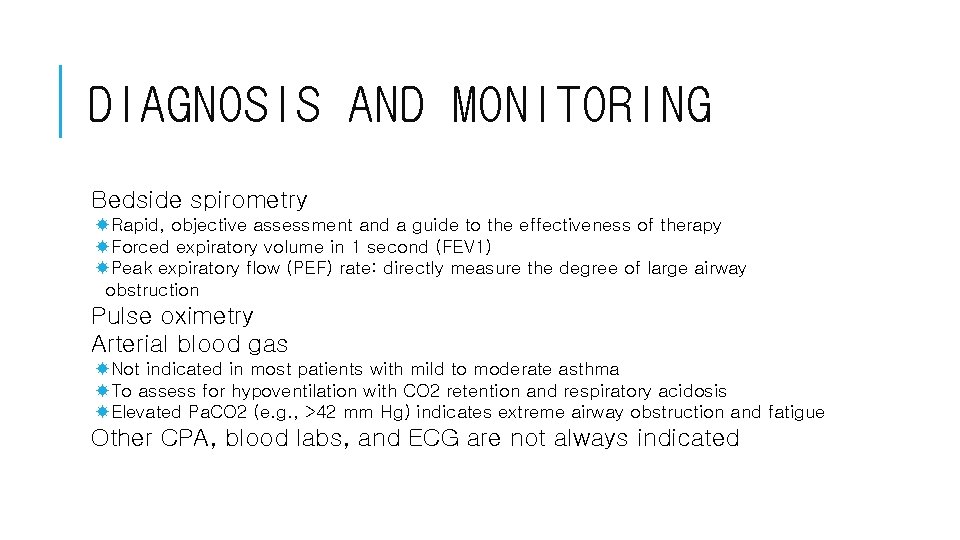
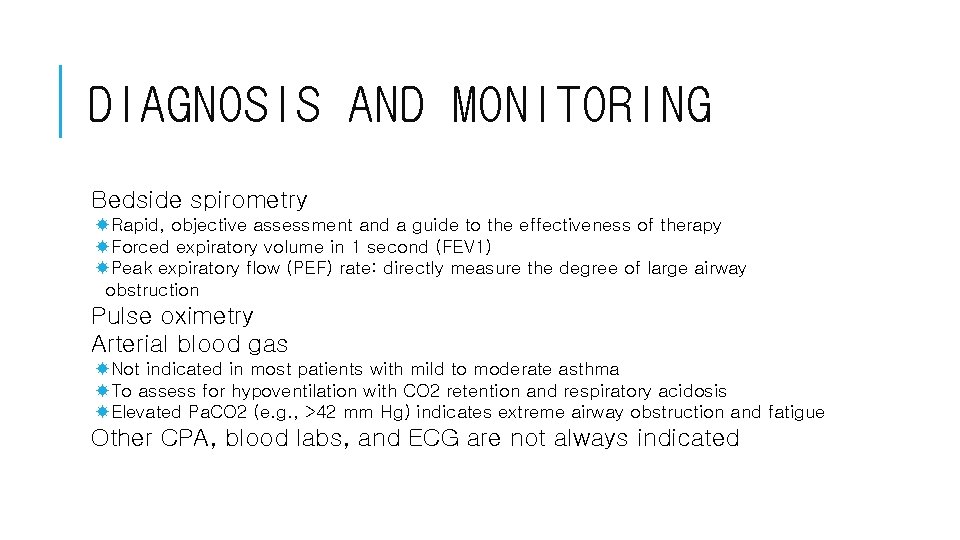
DIAGNOSIS AND MONITORING Bedside spirometry Rapid, objective assessment and a guide to the effectiveness of therapy Forced expiratory volume in 1 second (FEV 1) Peak expiratory flow (PEF) rate: directly measure the degree of large airway obstruction Pulse oximetry Arterial blood gas Not indicated in most patients with mild to moderate asthma To assess for hypoventilation with CO 2 retention and respiratory acidosis Elevated Pa. CO 2 (e. g. , >42 mm Hg) indicates extreme airway obstruction and fatigue Other CPA, blood labs, and ECG are not always indicated
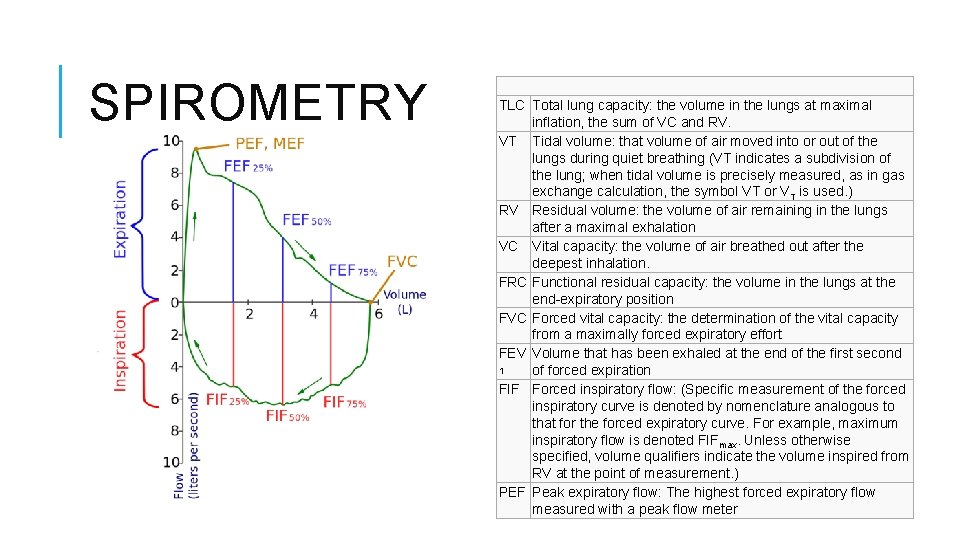
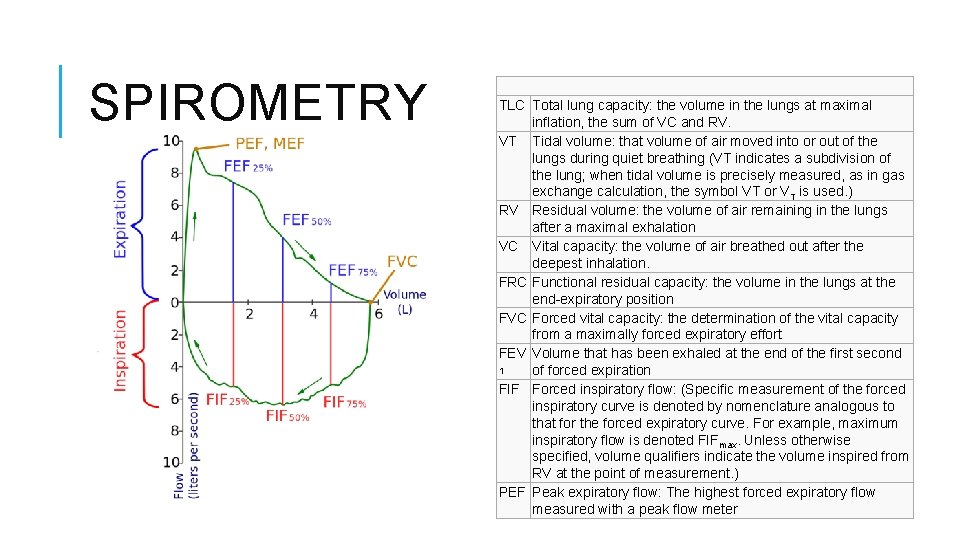
SPIROMETRY TLC Total lung capacity: the volume in the lungs at maximal inflation, the sum of VC and RV. VT Tidal volume: that volume of air moved into or out of the lungs during quiet breathing (VT indicates a subdivision of the lung; when tidal volume is precisely measured, as in gas exchange calculation, the symbol VT or VT is used. ) RV Residual volume: the volume of air remaining in the lungs after a maximal exhalation VC Vital capacity: the volume of air breathed out after the deepest inhalation. FRC Functional residual capacity: the volume in the lungs at the end-expiratory position FVC Forced vital capacity: the determination of the vital capacity from a maximally forced expiratory effort FEV Volume that has been exhaled at the end of the first second 1 of forced expiration FIF Forced inspiratory flow: (Specific measurement of the forced inspiratory curve is denoted by nomenclature analogous to that for the forced expiratory curve. For example, maximum inspiratory flow is denoted FIFmax. Unless otherwise specified, volume qualifiers indicate the volume inspired from RV at the point of measurement. ) PEF Peak expiratory flow: The highest forced expiratory flow measured with a peak flow meter
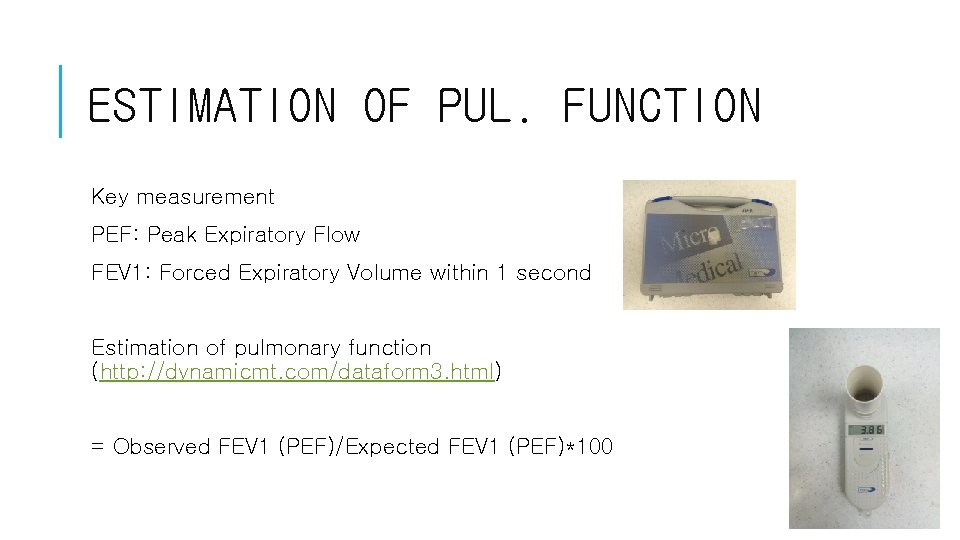
ESTIMATION OF PUL. FUNCTION Key measurement PEF: Peak Expiratory Flow FEV 1: Forced Expiratory Volume within 1 second Estimation of pulmonary function (http: //dynamicmt. com/dataform 3. html) = Observed FEV 1 (PEF)/Expected FEV 1 (PEF)*100
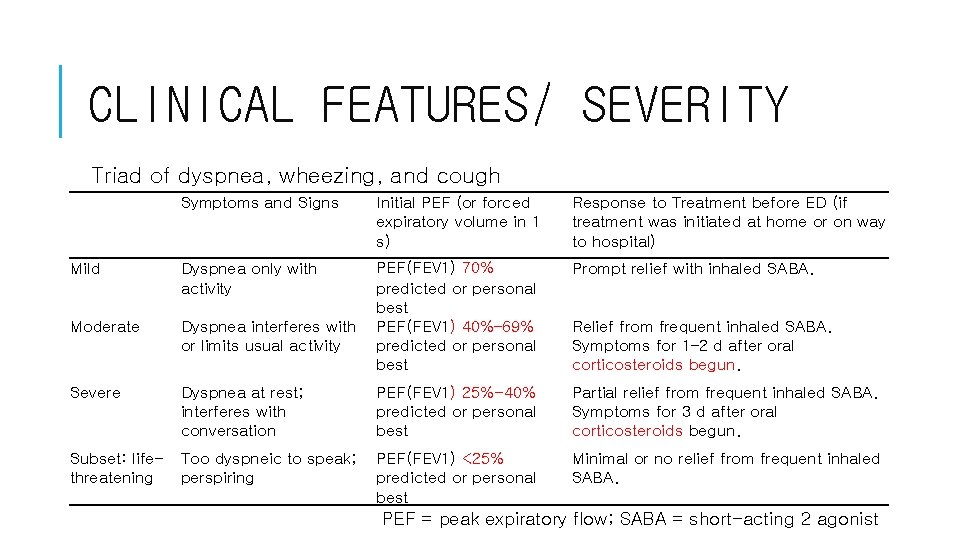
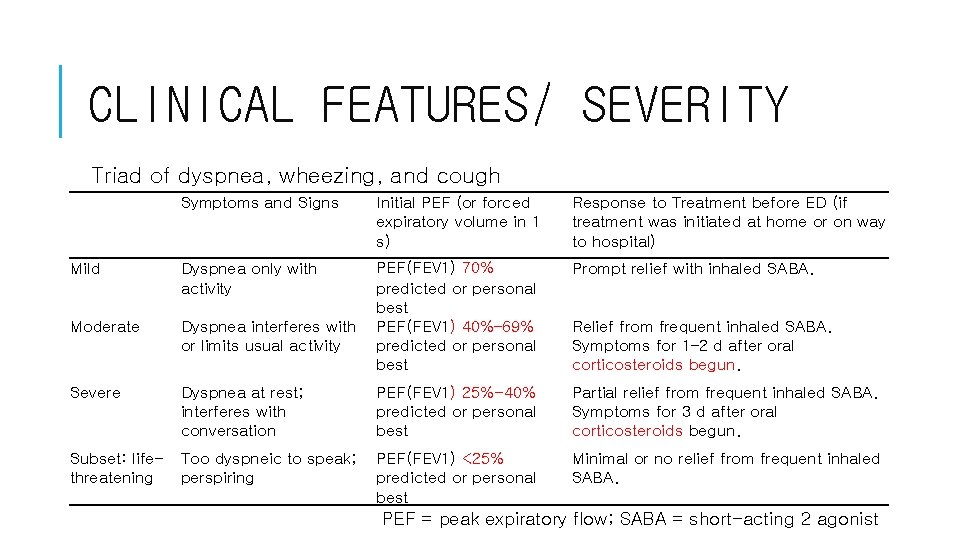
CLINICAL FEATURES/ SEVERITY Triad of dyspnea, wheezing, and cough Symptoms and Signs Mild Dyspnea only with activity Initial PEF (or forced expiratory volume in 1 s) Response to Treatment before ED (if treatment was initiated at home or on way to hospital) PEF(FEV 1) 70% predicted or personal best Dyspnea interferes with PEF(FEV 1) 40%– 69% or limits usual activity predicted or personal best Prompt relief with inhaled SABA. Dyspnea at rest; interferes with conversation PEF(FEV 1) 25%-40% predicted or personal best Partial relief from frequent inhaled SABA. Symptoms for 3 d after oral corticosteroids begun. Subset: life- Too dyspneic to speak; PEF(FEV 1) <25% threatening perspiring predicted or personal best Minimal or no relief from frequent inhaled SABA. Moderate Severe Relief from frequent inhaled SABA. Symptoms for 1– 2 d after oral corticosteroids begun. PEF = peak expiratory flow; SABA = short-acting 2 agonist
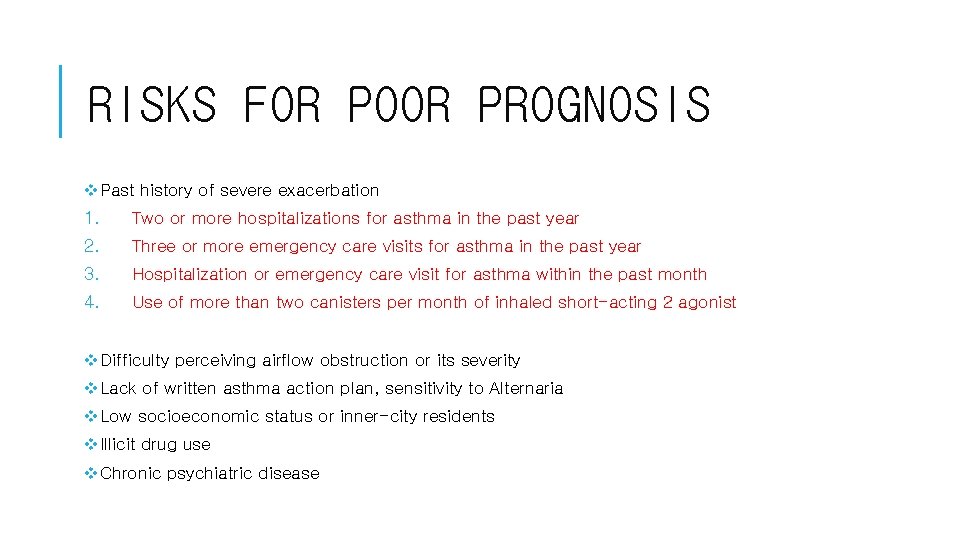
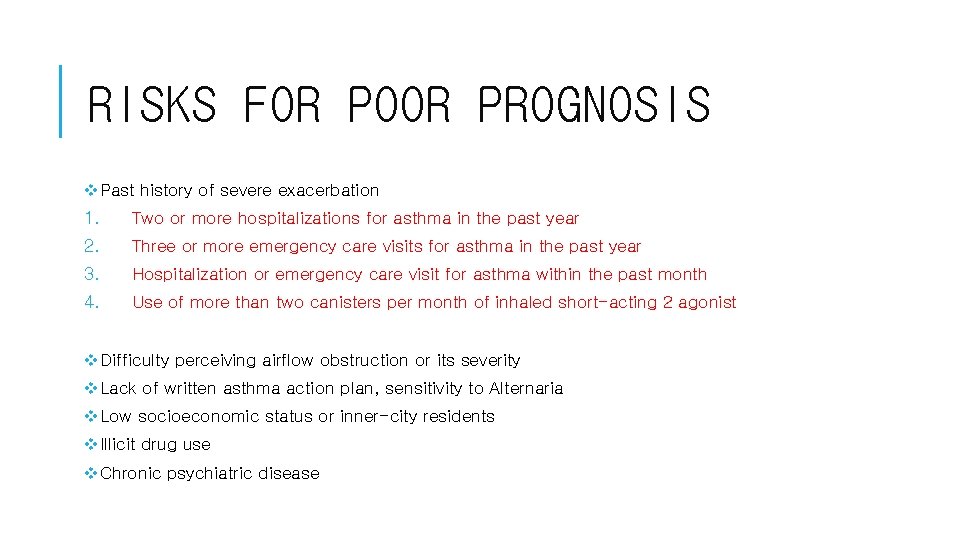
RISKS FOR POOR PROGNOSIS v. Past history of severe exacerbation 1. Two or more hospitalizations for asthma in the past year 2. Three or more emergency care visits for asthma in the past year 3. Hospitalization or emergency care visit for asthma within the past month 4. Use of more than two canisters per month of inhaled short-acting 2 agonist v. Difficulty perceiving airflow obstruction or its severity v. Lack of written asthma action plan, sensitivity to Alternaria v. Low socioeconomic status or inner-city residents v. Illicit drug use v. Chronic psychiatric disease
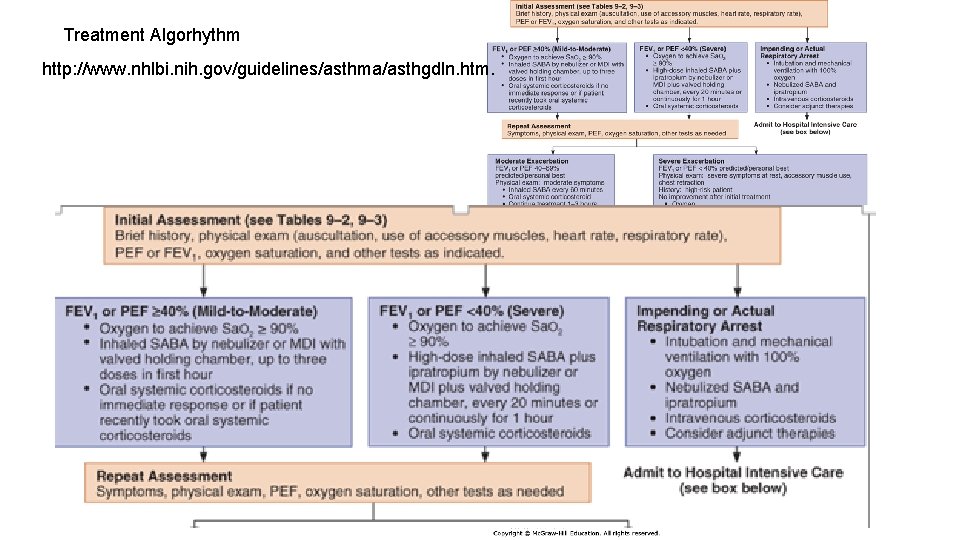
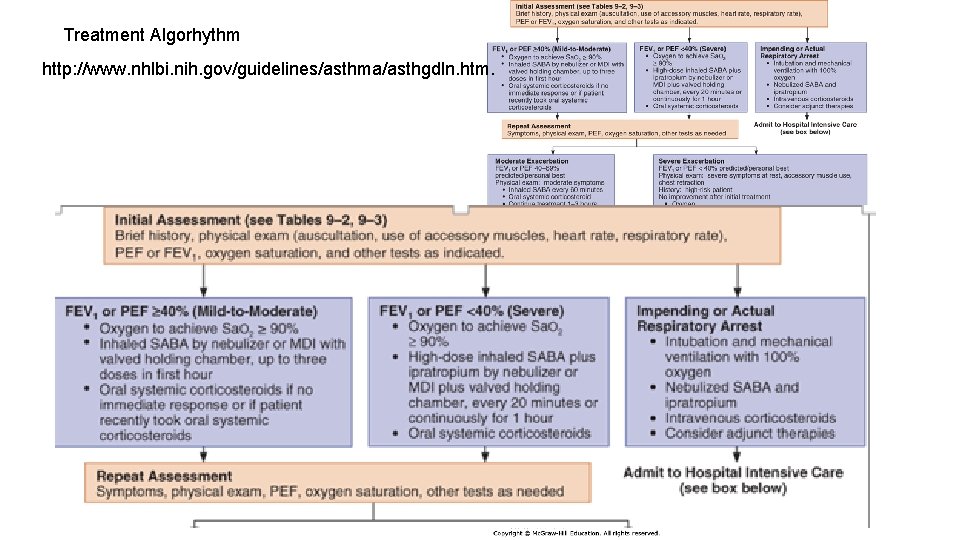
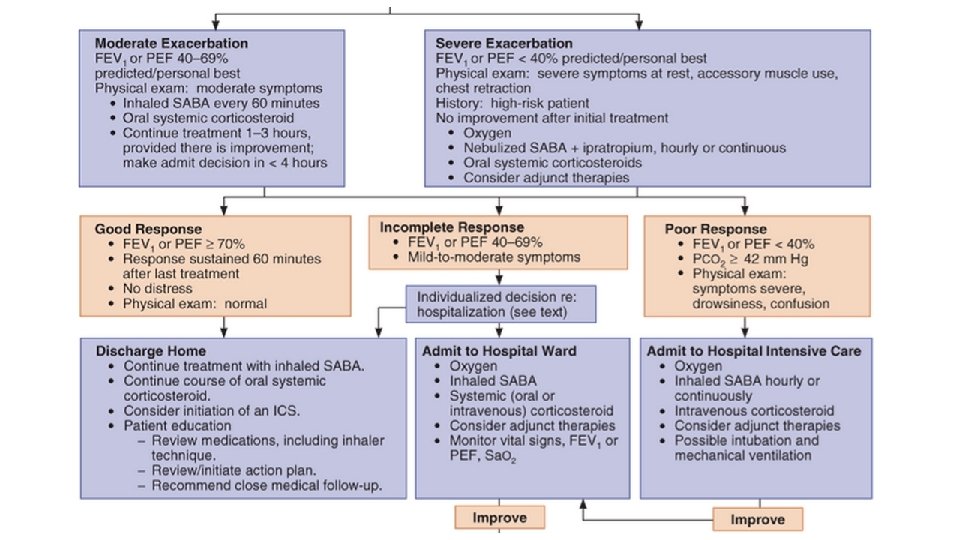
Treatment Algorhythm http: //www. nhlbi. nih. gov/guidelines/asthma/asthgdln. htm.
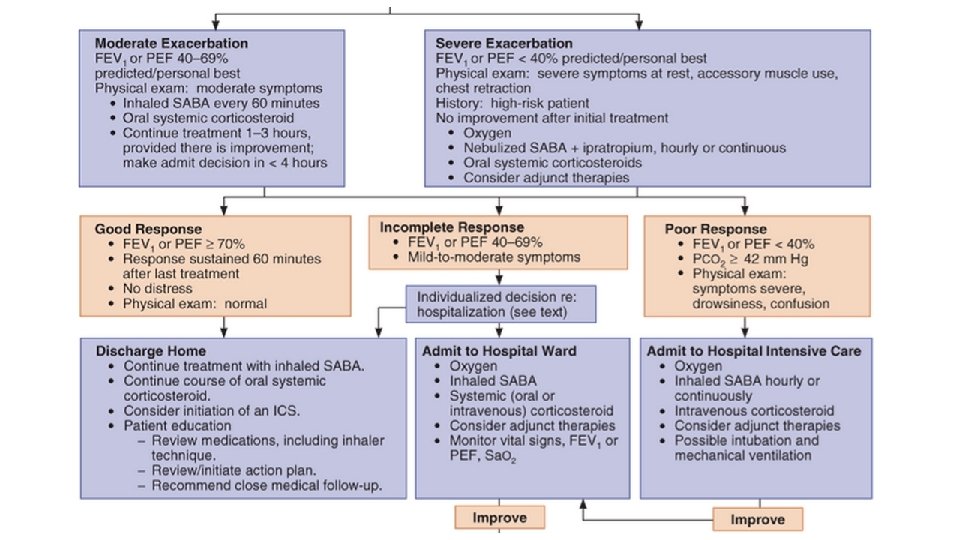
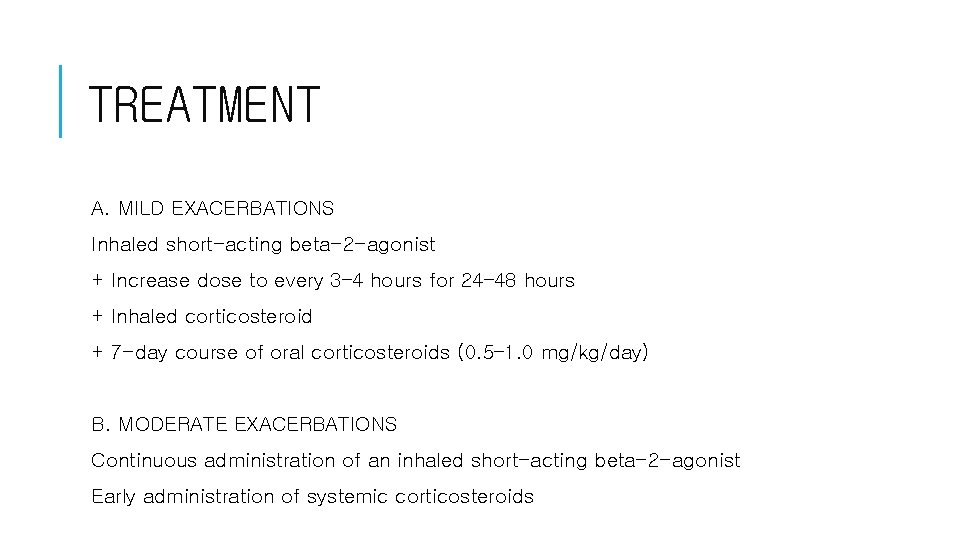
TREATMENT A. MILD EXACERBATIONS Inhaled short-acting beta-2 -agonist + Increase dose to every 3– 4 hours for 24– 48 hours + Inhaled corticosteroid + 7 -day course of oral corticosteroids (0. 5– 1. 0 mg/kg/day) B. MODERATE EXACERBATIONS Continuous administration of an inhaled short-acting beta-2 -agonist Early administration of systemic corticosteroids
TREATMENT C. SEVERE EXACERBATIONS 1. Oxygen: Sa. O 2 greater than 90% or a Pa. O 2 greater than 60 mm Hg 2. Frequent high doses of an inhaled short-acting beta-2 -agonist (60 -90 min. ): MDI and nebulizer (Ipratropium bromide) 3. Systemic corticosteroids 4. IV magnesium sulfate (2 g intravenously over 20 minutes) 5. Intubation and mechanical ventilation *Cautions Mucolytic agents (eg, acetylcysteine, potassium iodide) may worsen cough or airflow obstruction Anxiolytic and hypnotic drugs contraindicated
COPD
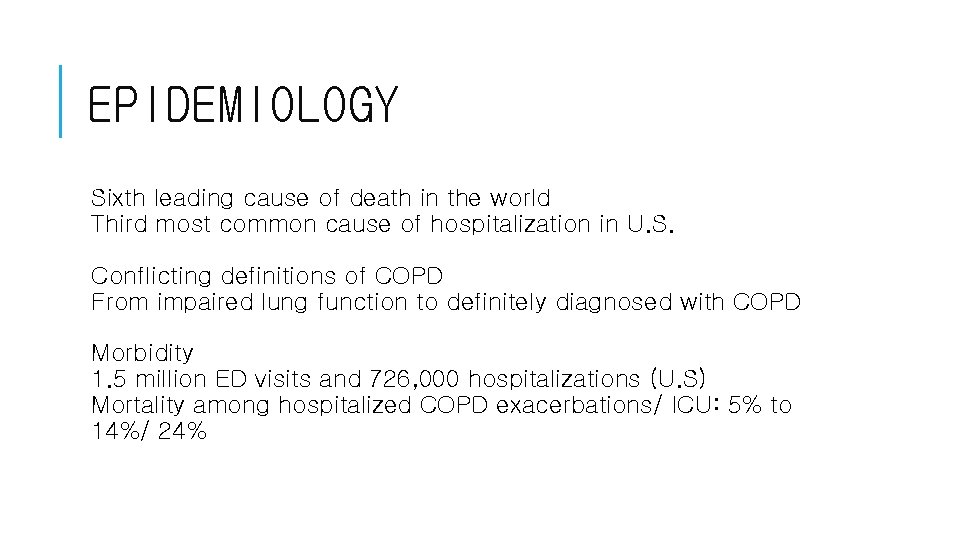
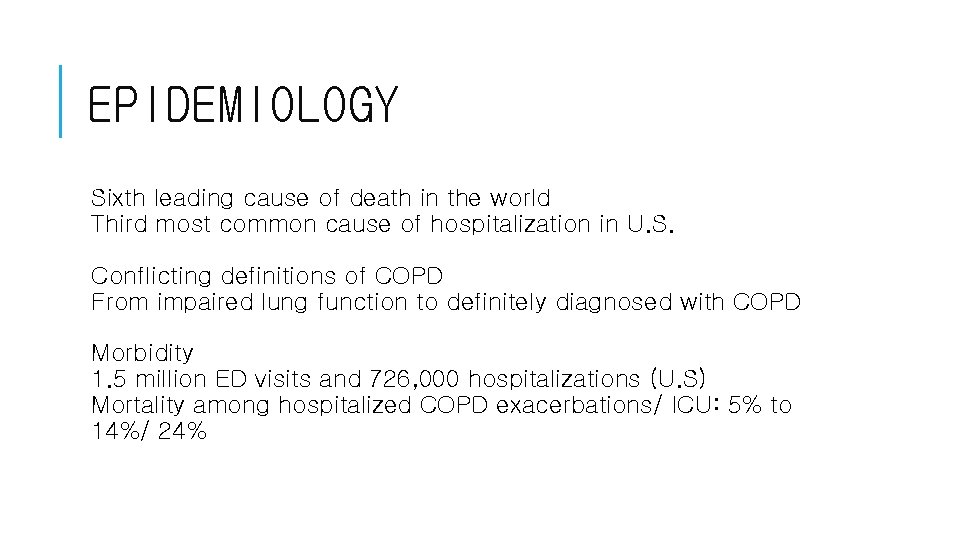
EPIDEMIOLOGY Sixth leading cause of death in the world Third most common cause of hospitalization in U. S. Conflicting definitions of COPD From impaired lung function to definitely diagnosed with COPD Morbidity 1. 5 million ED visits and 726, 000 hospitalizations (U. S) Mortality among hospitalized COPD exacerbations/ ICU: 5% to 14%/ 24%
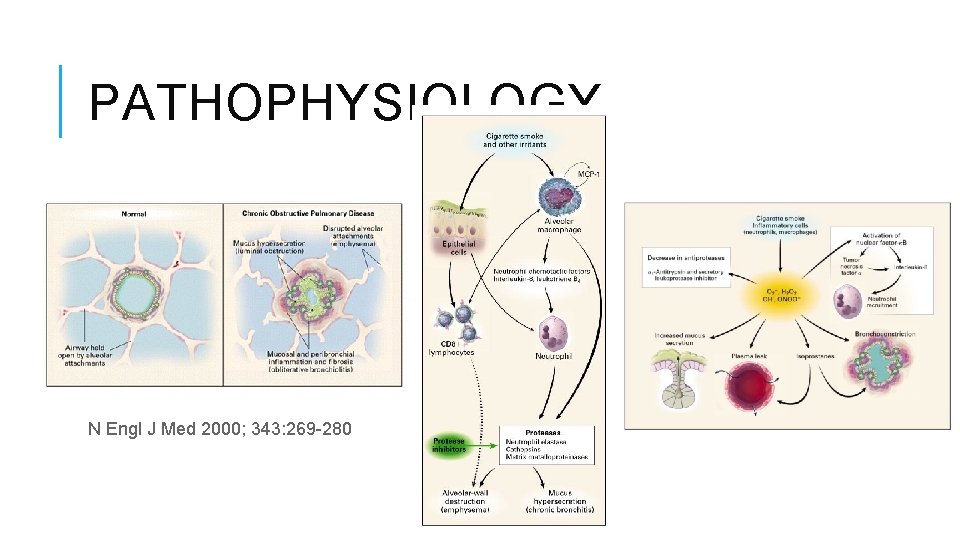
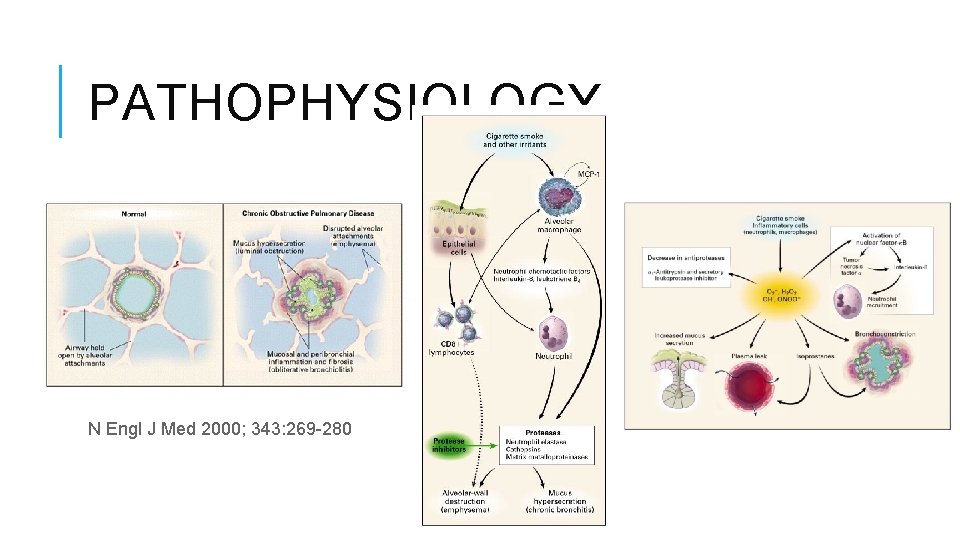
PATHOPHYSIOLOGY N Engl J Med 2000; 343: 269 -280
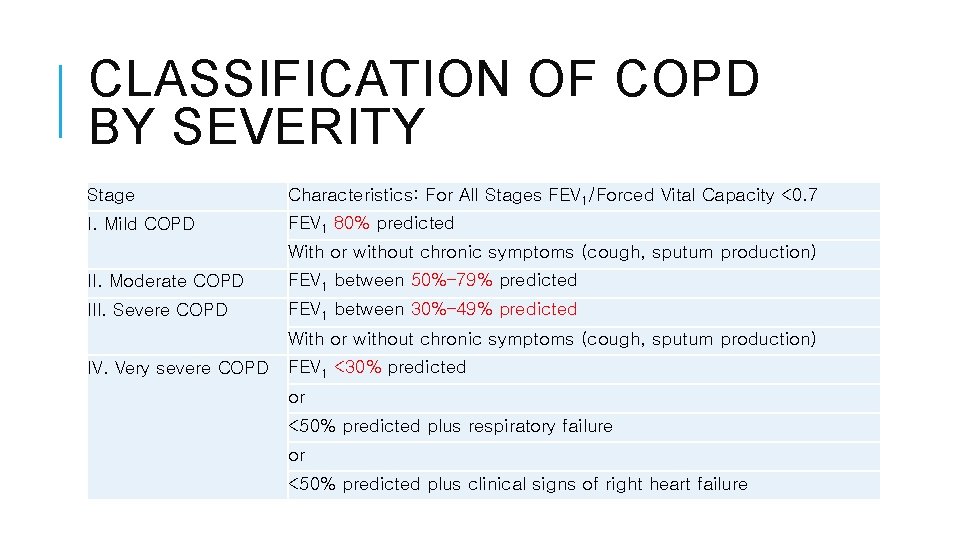
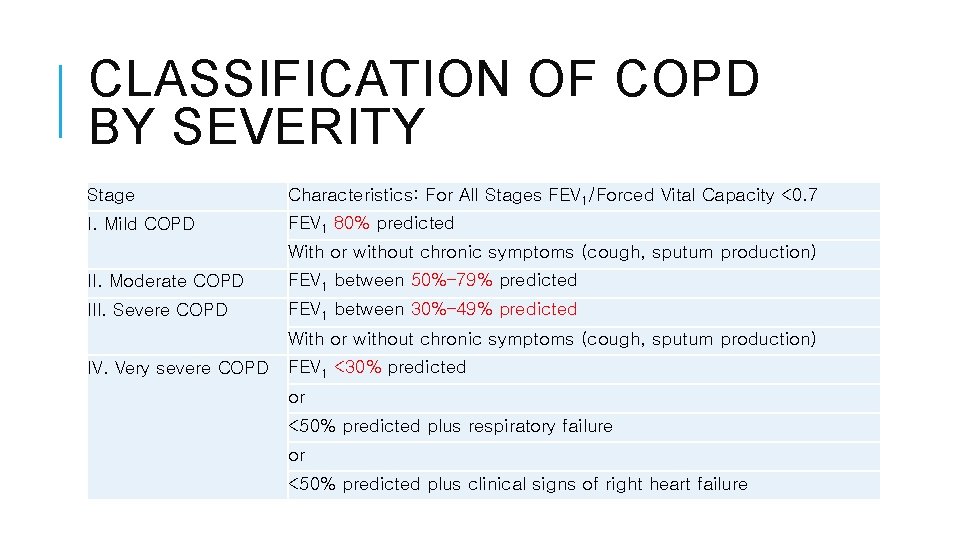
CLASSIFICATION OF COPD BY SEVERITY Stage Characteristics: For All Stages FEV 1/Forced Vital Capacity <0. 7 I. Mild COPD FEV 1 80% predicted With or without chronic symptoms (cough, sputum production) II. Moderate COPD FEV 1 between 50%– 79% predicted III. Severe COPD FEV 1 between 30%– 49% predicted With or without chronic symptoms (cough, sputum production) IV. Very severe COPD FEV 1 <30% predicted or <50% predicted plus respiratory failure or <50% predicted plus clinical signs of right heart failure
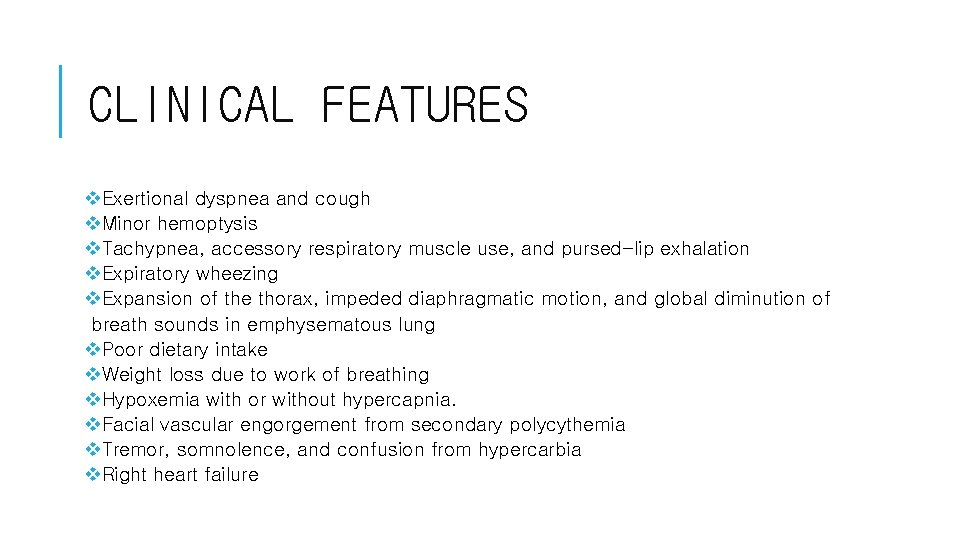
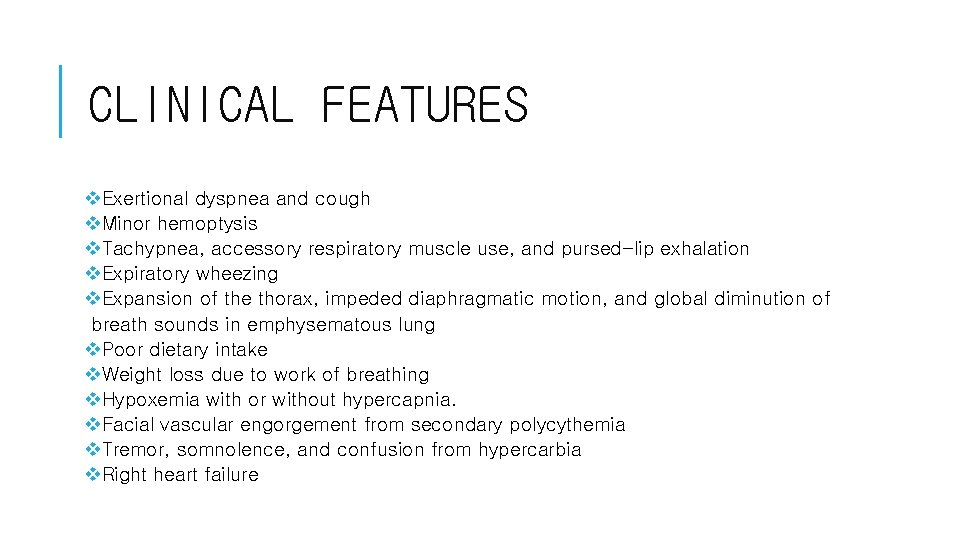
CLINICAL FEATURES v. Exertional dyspnea and cough v. Minor hemoptysis v. Tachypnea, accessory respiratory muscle use, and pursed-lip exhalation v. Expiratory wheezing v. Expansion of the thorax, impeded diaphragmatic motion, and global diminution of breath sounds in emphysematous lung v. Poor dietary intake v. Weight loss due to work of breathing v. Hypoxemia with or without hypercapnia. v. Facial vascular engorgement from secondary polycythemia v. Tremor, somnolence, and confusion from hypercarbia v. Right heart failure
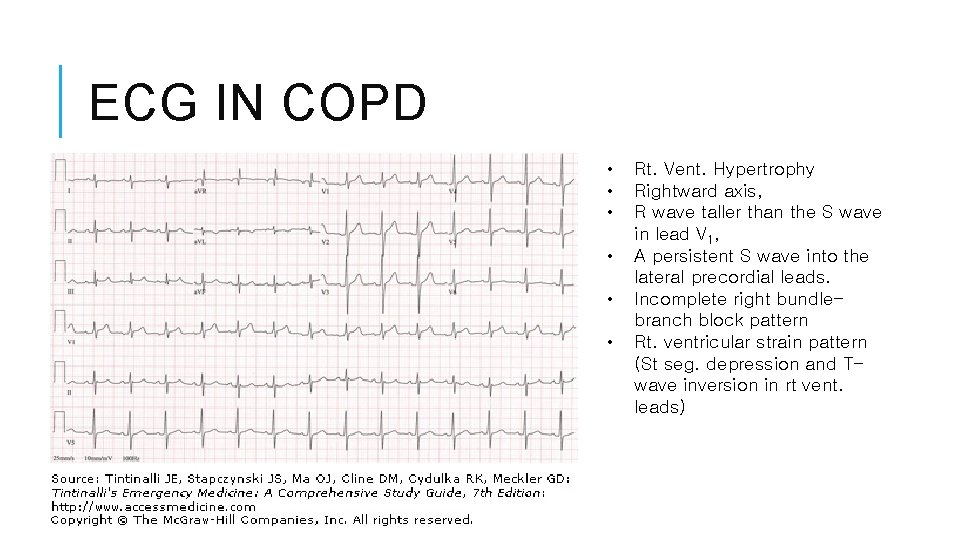
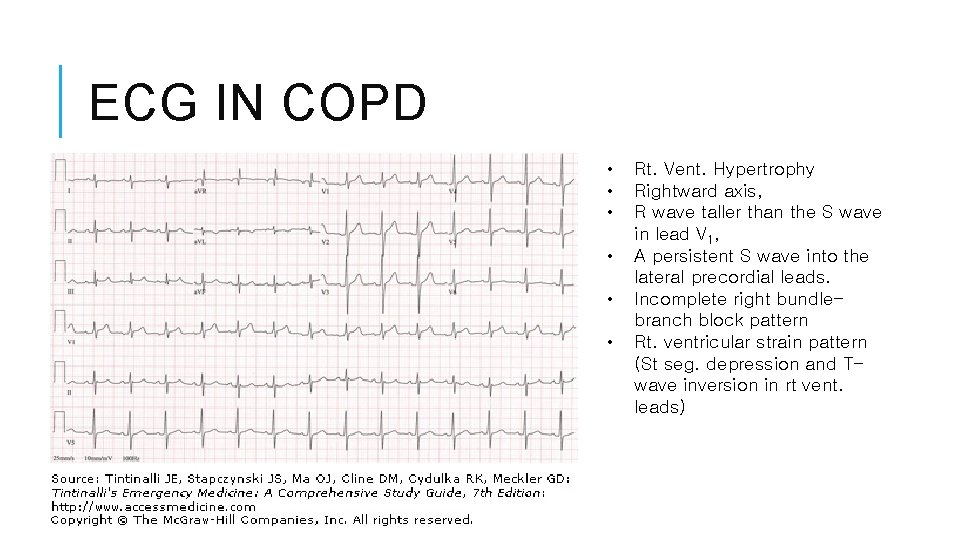
ECG IN COPD • • • Rt. Vent. Hypertrophy Rightward axis, R wave taller than the S wave in lead V 1, A persistent S wave into the lateral precordial leads. Incomplete right bundlebranch block pattern Rt. ventricular strain pattern (St seg. depression and Twave inversion in rt vent. leads)
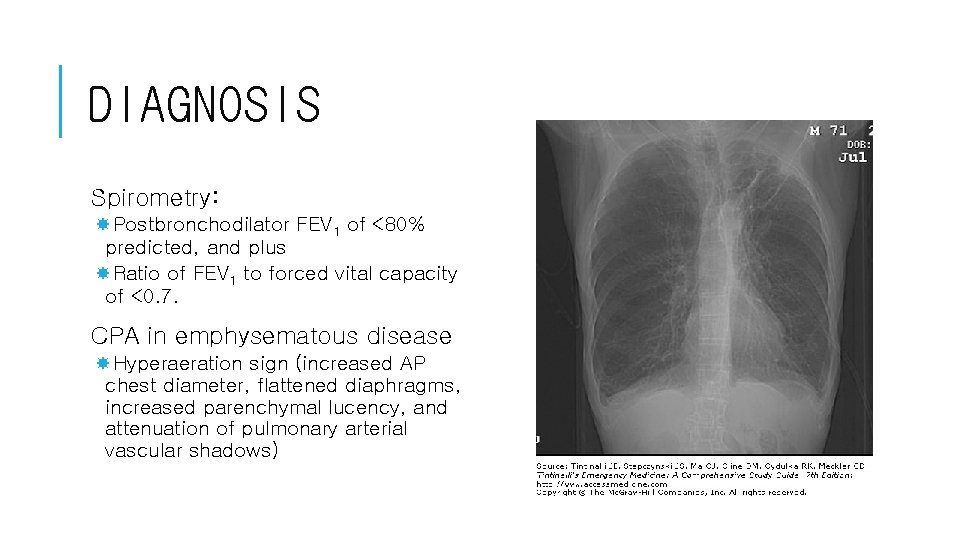
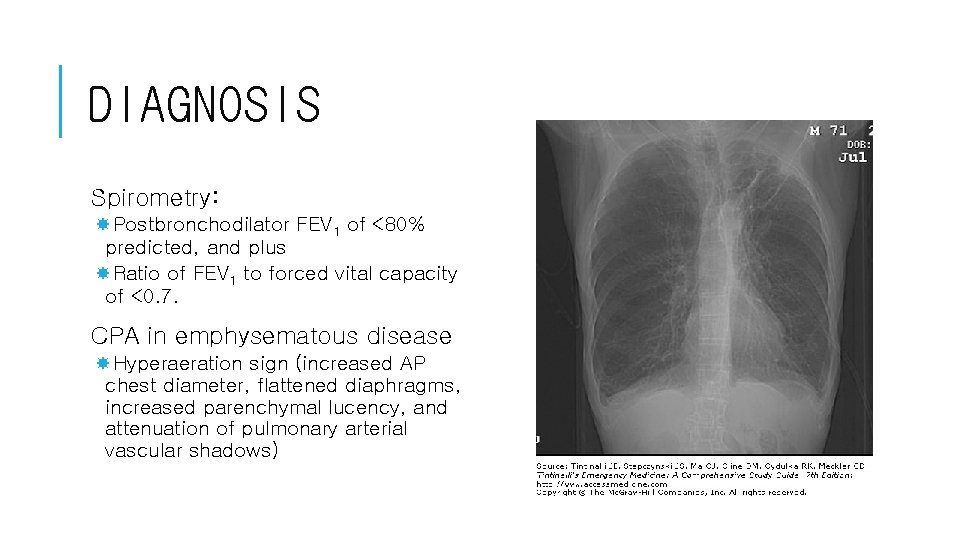
DIAGNOSIS Spirometry: Postbronchodilator FEV 1 of <80% predicted, and plus Ratio of FEV 1 to forced vital capacity of <0. 7. CPA in emphysematous disease Hyperaeration sign (increased AP chest diameter, flattened diaphragms, increased parenchymal lucency, and attenuation of pulmonary arterial vascular shadows)
ACUTE EXACERBATION v. Hypoxemia: Sa. O 2 <90% v Tachypnea, tachycardia, systemic hypertension, cyanosis, and a change in mental status v. Increased work of breathing, muscle production of CO 2 increases, and CO 2 retention and respiratory acidosis. v. Sitting-up-and-forward position, pursed-lip exhalation, and accessory muscle use. v. Assess Oxygenation and Acid-Base Status v. Respiratory acidosis : p. H 7. 35 and PCO 2 44 mm. Hg v. Acute hypercapnia. HCO 3– increases 1 m. Eq/L for every 10 mm Hg increase in Pa. CO 2, or 1: 10. v. Chronic hypercapnia. HCO 3– increases 3. 5 m. Eq/L for each 10 mm Hg increase in Pa. CO 2 or 3. 5: 10.
TREATMENT Oxygen To increase the baseline Pa. O 2 to 60 mm Hg or the Sa. O 2>90% at rest. Pharmacotherapy Long-acting inhaled 2 agonists (salmeterol and formoterol) Short-acting inhaled 2 agonists Anticholinergic agents (cause bronchodilation): Ipratropium bromide Systemic steroid: Not recommend long-term systemic corticosteroid therapy Antibiotics in sputum ++: Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis. Theophylline recommended as an adjunct therapy. Secretion Mobilization Limit the use of antihistamines, antitussives, and decongestants. Smoking Cessation and Pulmonary Rehabilitation Pneumococcal vaccination
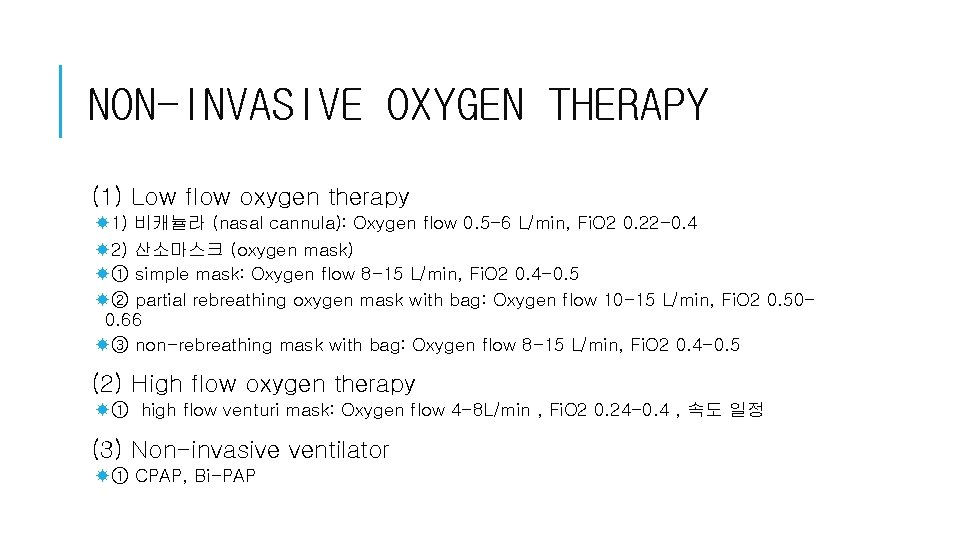
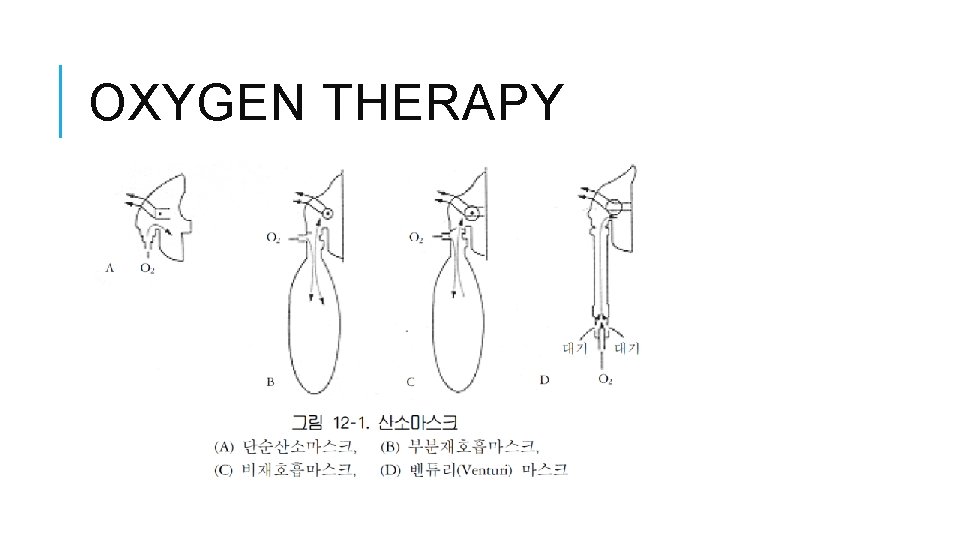
NON-INVASIVE OXYGEN THERAPY (1) Low flow oxygen therapy 1) 비캐뉼라 (nasal cannula): Oxygen flow 0. 5 -6 L/min, Fi. O 2 0. 22 -0. 4 2) 산소마스크 (oxygen mask) ① simple mask: Oxygen flow 8 -15 L/min, Fi. O 2 0. 4 -0. 5 ② partial rebreathing oxygen mask with bag: Oxygen flow 10 -15 L/min, Fi. O 2 0. 500. 66 ③ non-rebreathing mask with bag: Oxygen flow 8 -15 L/min, Fi. O 2 0. 4 -0. 5 (2) High flow oxygen therapy ① high flow venturi mask: Oxygen flow 4 -8 L/min , Fi. O 2 0. 24 -0. 4 , 속도 일정 (3) Non-invasive ventilator ① CPAP, Bi-PAP
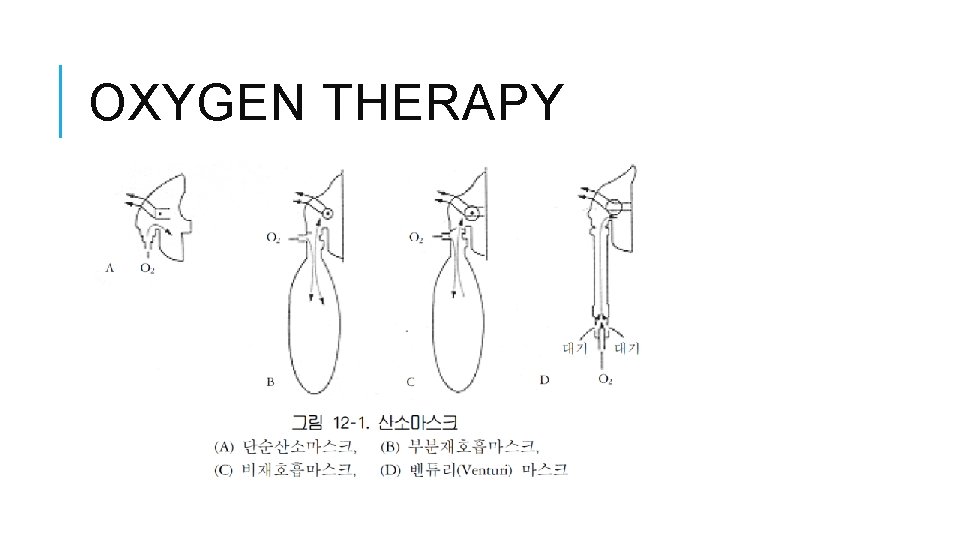
OXYGEN THERAPY
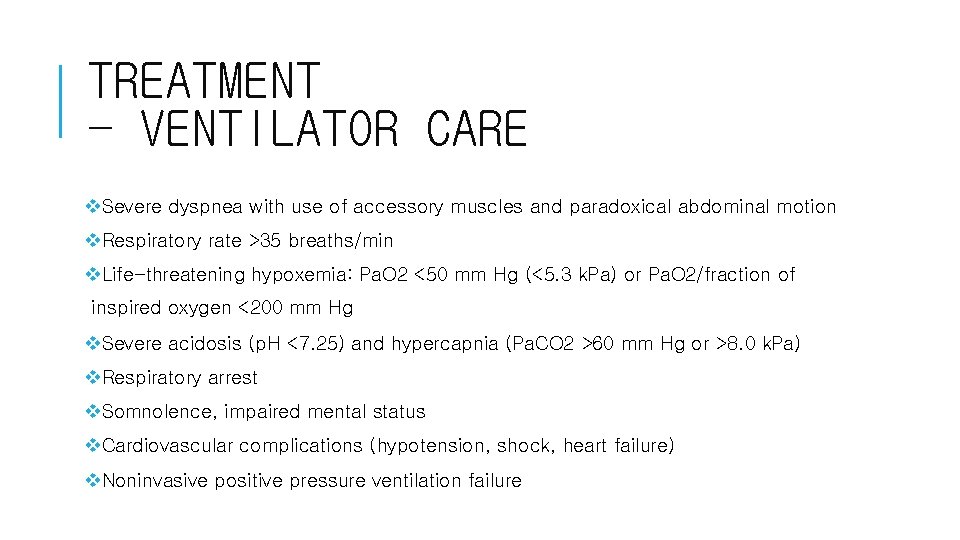
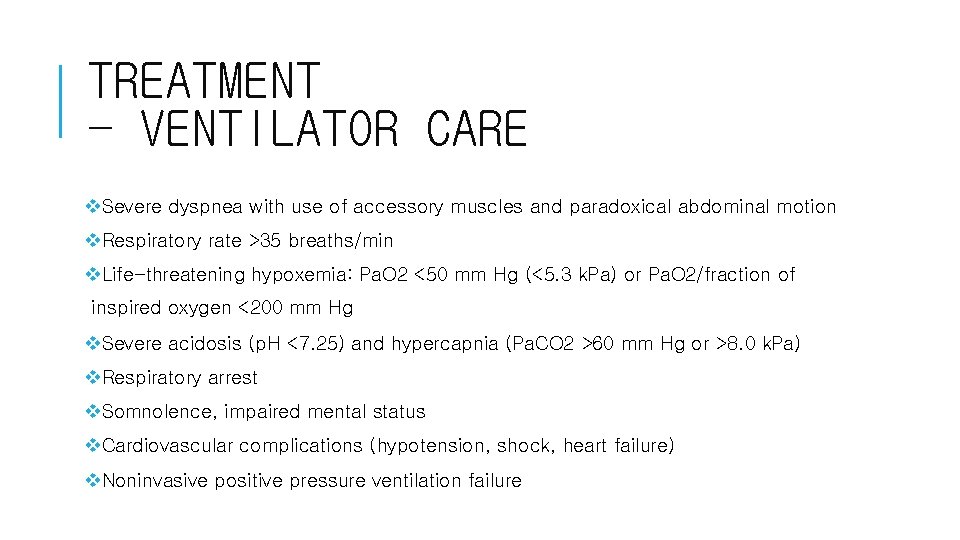
TREATMENT - VENTILATOR CARE v. Severe dyspnea with use of accessory muscles and paradoxical abdominal motion v. Respiratory rate >35 breaths/min v. Life-threatening hypoxemia: Pa. O 2 <50 mm Hg (<5. 3 k. Pa) or Pa. O 2/fraction of inspired oxygen <200 mm Hg v. Severe acidosis (p. H <7. 25) and hypercapnia (Pa. CO 2 >60 mm Hg or >8. 0 k. Pa) v. Respiratory arrest v. Somnolence, impaired mental status v. Cardiovascular complications (hypotension, shock, heart failure) v. Noninvasive positive pressure ventilation failure
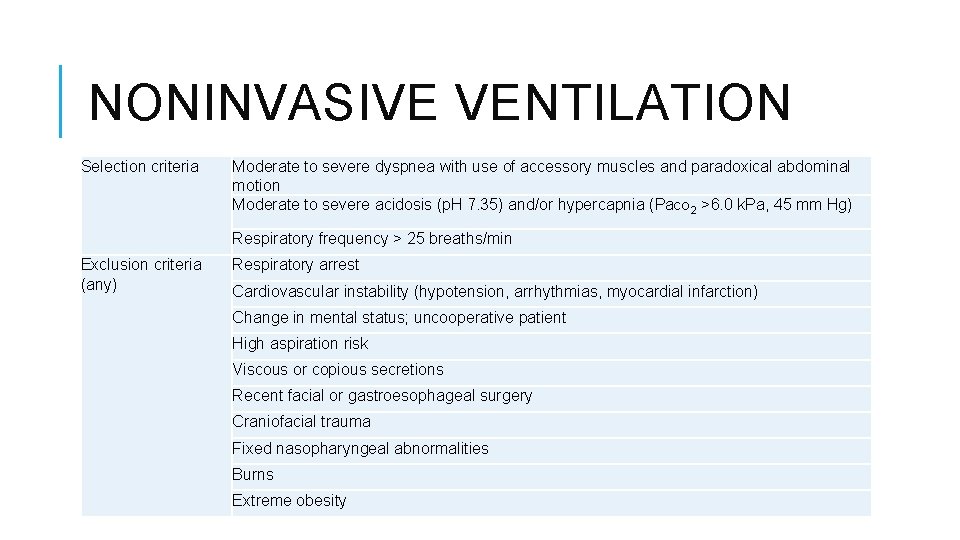
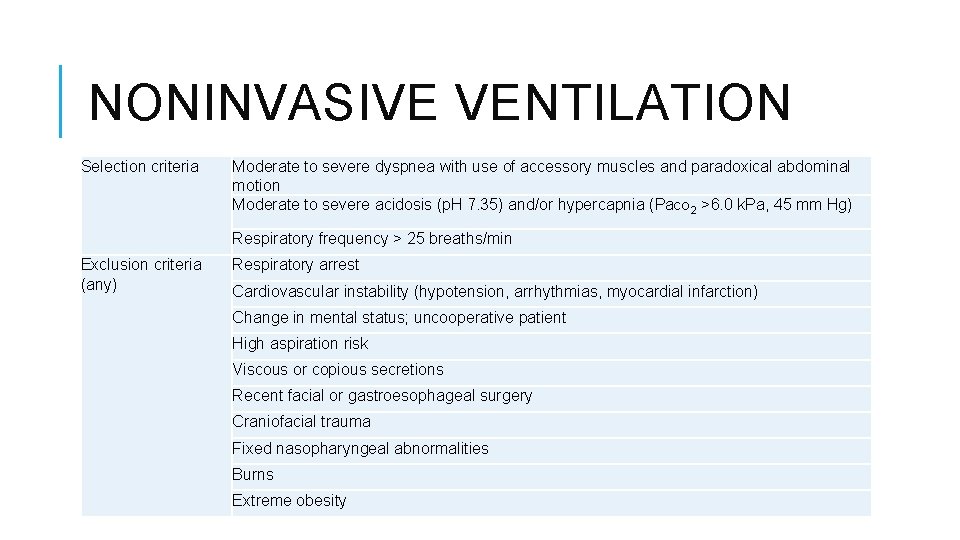
NONINVASIVE VENTILATION Selection criteria Moderate to severe dyspnea with use of accessory muscles and paradoxical abdominal motion Moderate to severe acidosis (p. H 7. 35) and/or hypercapnia (Pa. CO 2 >6. 0 k. Pa, 45 mm Hg) Respiratory frequency > 25 breaths/min Exclusion criteria (any) Respiratory arrest Cardiovascular instability (hypotension, arrhythmias, myocardial infarction) Change in mental status; uncooperative patient High aspiration risk Viscous or copious secretions Recent facial or gastroesophageal surgery Craniofacial trauma Fixed nasopharyngeal abnormalities Burns Extreme obesity
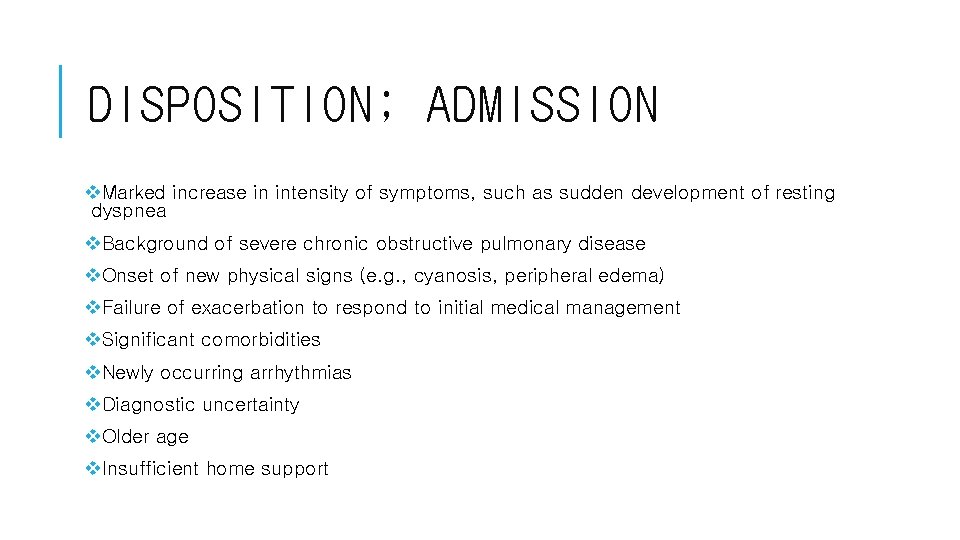
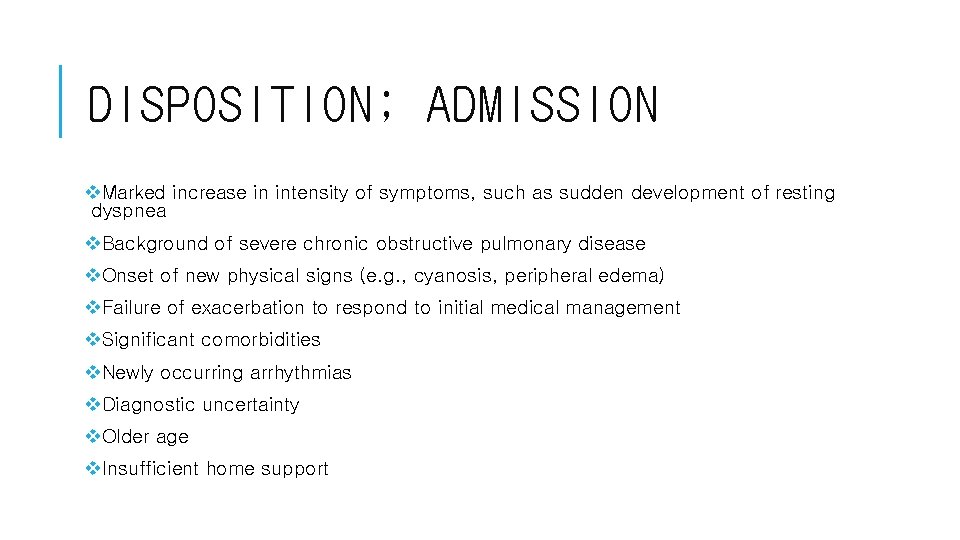
DISPOSITION; ADMISSION v. Marked increase in intensity of symptoms, such as sudden development of resting dyspnea v. Background of severe chronic obstructive pulmonary disease v. Onset of new physical signs (e. g. , cyanosis, peripheral edema) v. Failure of exacerbation to respond to initial medical management v. Significant comorbidities v. Newly occurring arrhythmias v. Diagnostic uncertainty v. Older age v. Insufficient home support

![기출 문제 01 2012 천식 환자에서 risk가 낮은 환 자 가 베타 흡입제 1달에 기출 문제 01] (2012) 천식 환자에서 risk가 낮은 환 자? 가) 베타 흡입제 1달에](https://slidetodoc.com/presentation_image/48015bca88b3b9ac6fcfc10235a78d27/image-33.jpg)
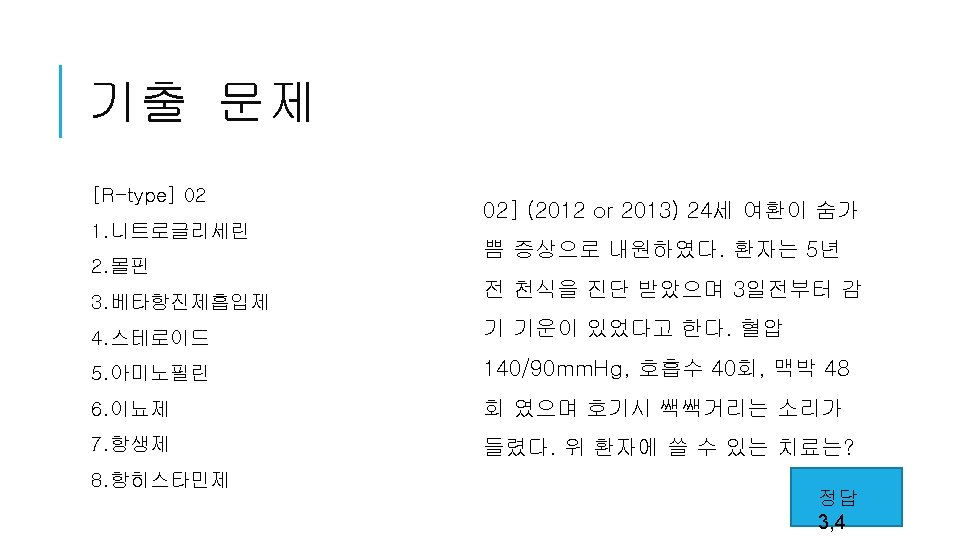
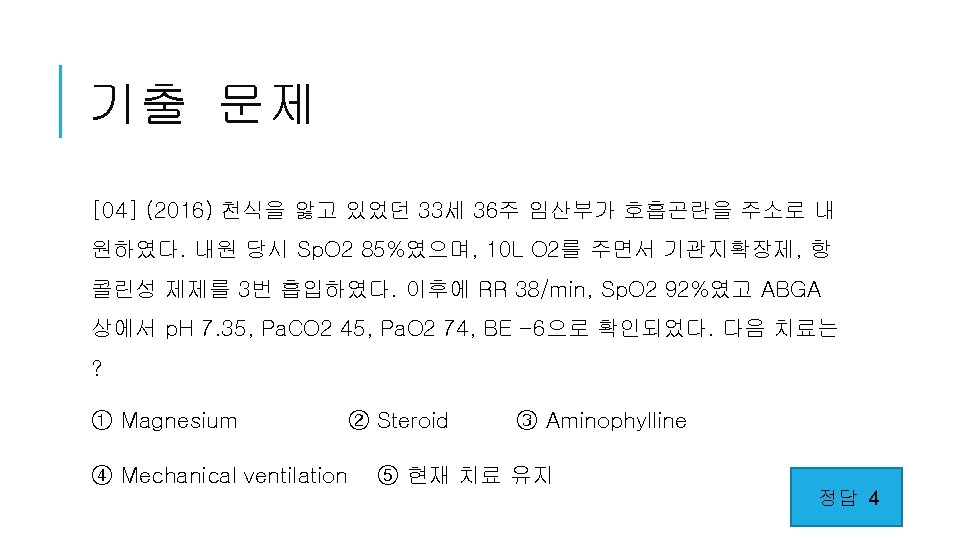
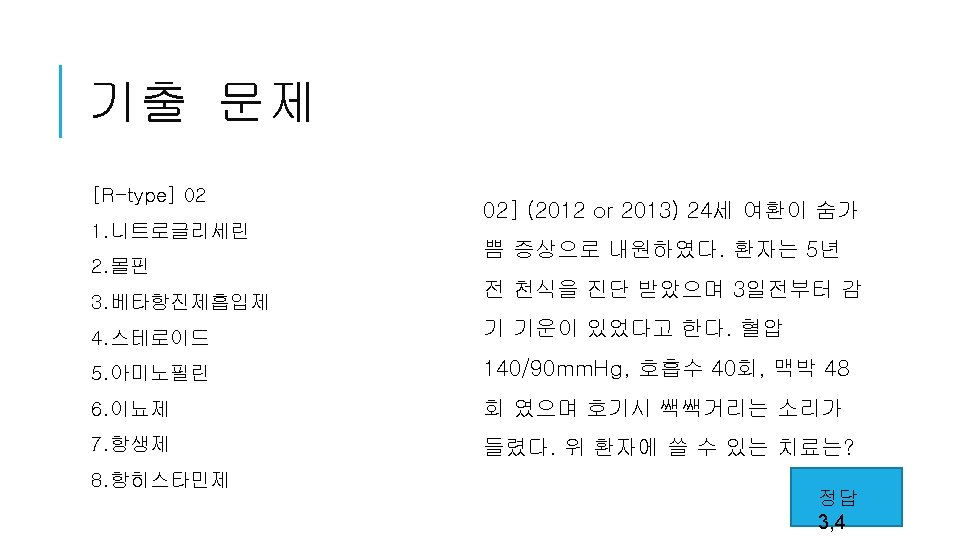
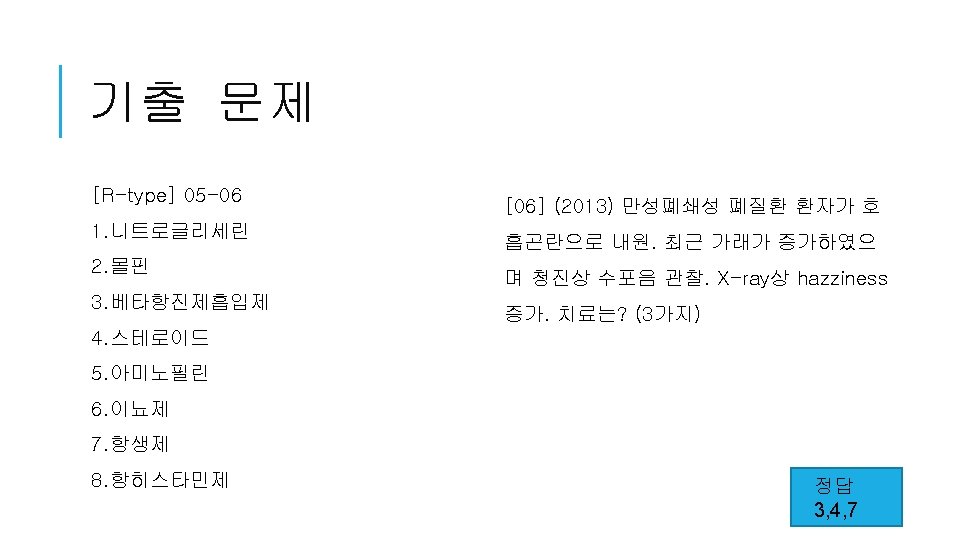
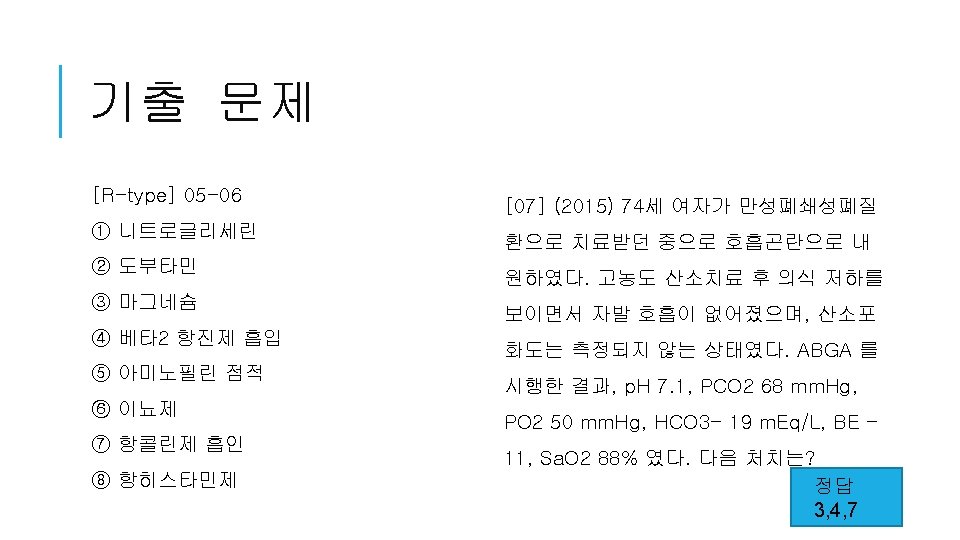
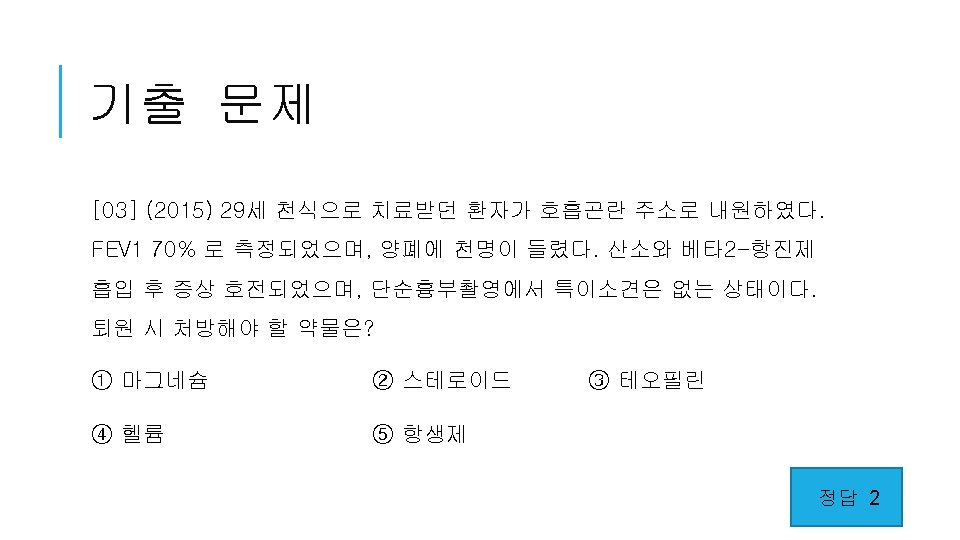
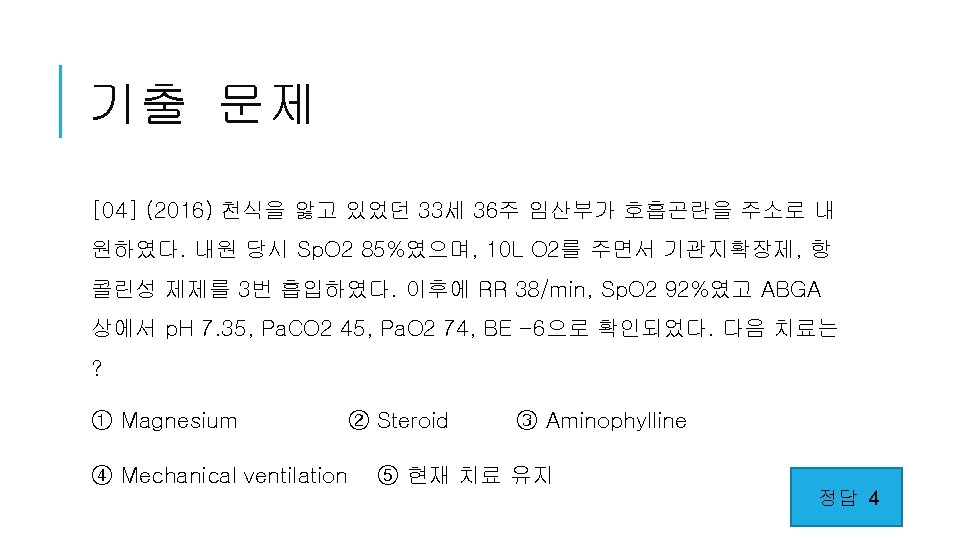
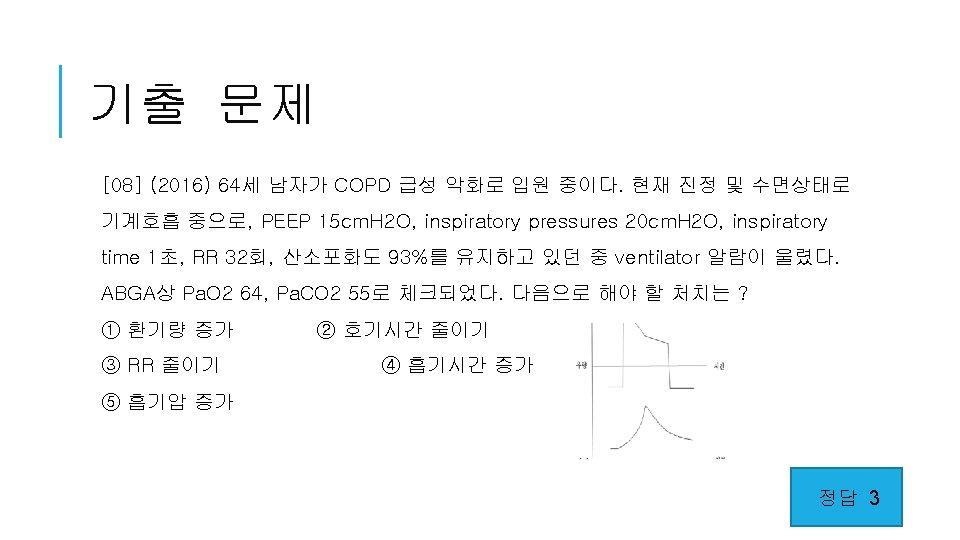
기출 문제 01] (2012) 천식 환자에서 risk가 낮은 환 자? 가) 베타 흡입제 1달에 3통 흡입 나) 2주전 응급실 내원 다) 1년에 입원 3번 라) 6개월전 2개월전 응급실 방문 마) 1년 입원 2회 Tin. 7 th p. 505 Table 72 -2 < Risk factor for death from asthma > # Past history of severe exacerbation # Two or more hospitalizations for asthma in the past year # Three or more emergency care visits for asthma in the past year # Hospitalization or emergency care visit for asthma within the past month # Use of more than two canisters per month of inhaled short-acting 2 agonist # Difficulty perceiving airflow obstruction or its severity # Lack of written asthma action plan, sensitivity to Alternaria # Low socioeconomic status or inner-city residents # Illicit drug use 정답 라 # Chronic psychiatric disease
![기출 문제 01 2012 COPD 환자가 호흡곤란으로 내원하였다 가장 심한 상태인 것 은 1FEV 기출 문제 [01] (2012) COPD 환자가 호흡곤란으로 내원하였다. 가장 심한 상태인 것 은? 1)FEV](https://slidetodoc.com/presentation_image/48015bca88b3b9ac6fcfc10235a78d27/image-35.jpg)
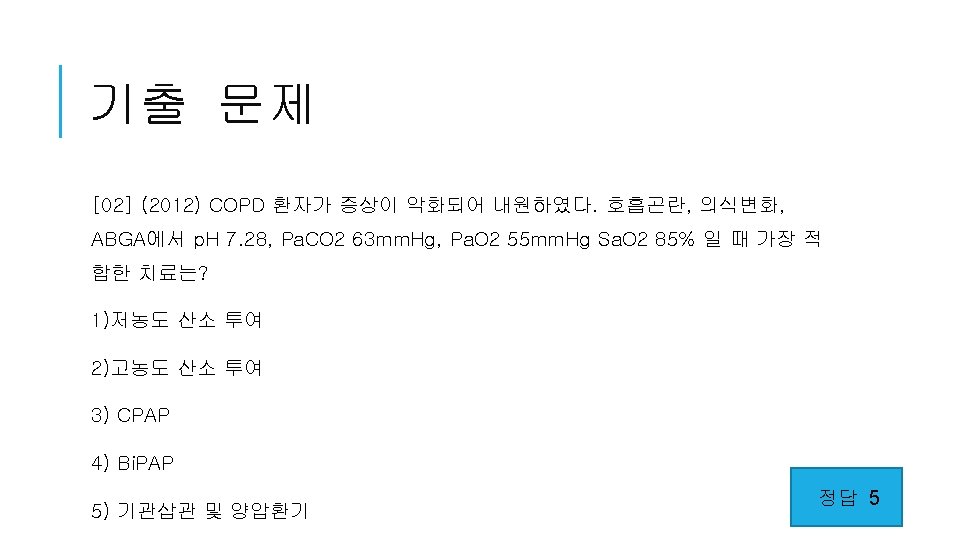
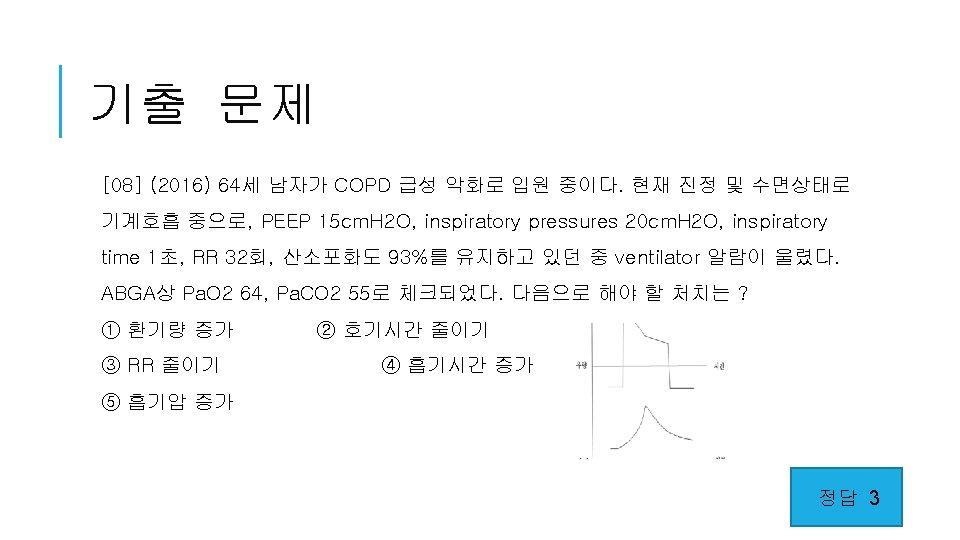
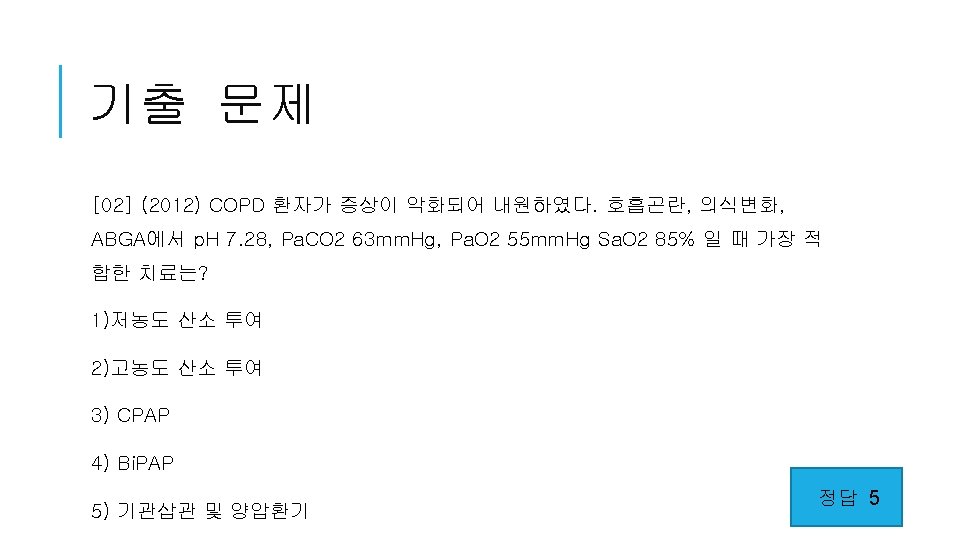
기출 문제 [01] (2012) COPD 환자가 호흡곤란으로 내원하였다. 가장 심한 상태인 것 은? 1)FEV 1 <30% predicted 2)FEV 1 <40% predicted 3)FEV 1 <50% predicted 4)FEV 1 <60% predicted 5)FEV 1 <70% predicted 정답 1
![기출 문제 03 04 1 Chlamydophila pneumoniae 03 2012 COPD 환자가 기침 화농성 2 기출 문제 <03 -04> 1. Chlamydophila pneumoniae [03] (2012) COPD 환자가 기침, 화농성 2.](https://slidetodoc.com/presentation_image/48015bca88b3b9ac6fcfc10235a78d27/image-37.jpg)
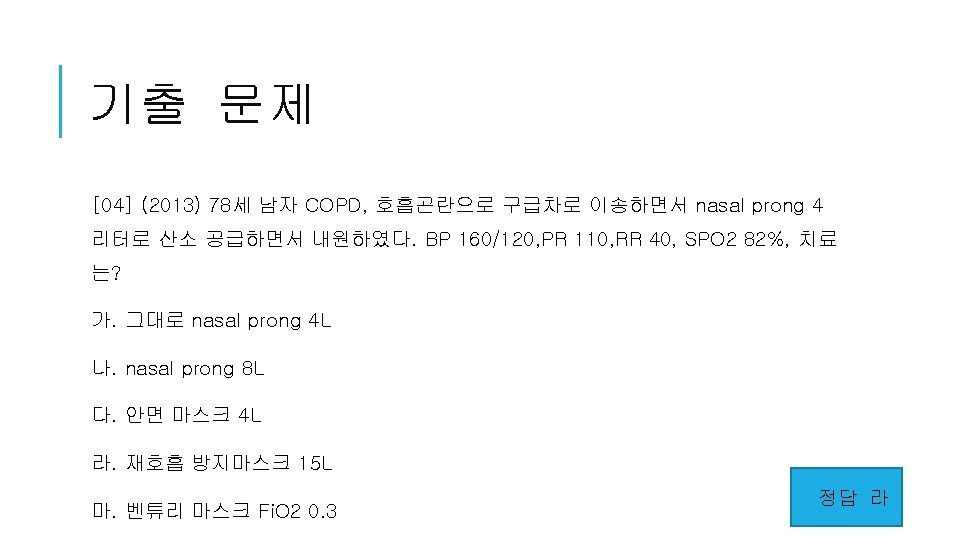
기출 문제 <03 -04> 1. Chlamydophila pneumoniae [03] (2012) COPD 환자가 기침, 화농성 2. Haemophilus influenzae 가래를 보일 때 원인균 3가지를 고르시 3. Klebsiella pneumoniae 4. Legionella pneumonia 오. 5. Moraxella catarrhalis 6. Mycoplasma pneumoniae 7. Pneumocystis carinii 8. Pseudomonas aeruginosa 9. Staphylococcus aureus 10. Streptococcus pneumoniae 정답 2, 5, 10
 Spirometry
Spirometry Copd vs asthma
Copd vs asthma Asthmatic lung x ray
Asthmatic lung x ray Conducting zone of the respiratory system function
Conducting zone of the respiratory system function Difference between descriptive and analytic epidemiology
Difference between descriptive and analytic epidemiology Nutrition epidemiology definition
Nutrition epidemiology definition Descriptive vs analytical epidemiology
Descriptive vs analytical epidemiology Incidence and prevalence meaning
Incidence and prevalence meaning Cbic recertification
Cbic recertification Descriptive epidemiology
Descriptive epidemiology Sbar copd
Sbar copd Interstitialis rajzolat a tüdőben
Interstitialis rajzolat a tüdőben Niv modes and settings
Niv modes and settings Cat score copd
Cat score copd Blue and white inhaler
Blue and white inhaler Tiêu chuẩn anthonisen
Tiêu chuẩn anthonisen Gina guidelines
Gina guidelines Non pharmacological treatment for copd
Non pharmacological treatment for copd Copd netwerk
Copd netwerk Lets be copd
Lets be copd Sbar copd
Sbar copd Barrel chested
Barrel chested Copd exacerbation nursing management
Copd exacerbation nursing management Copd 저농도 산소
Copd 저농도 산소 Copd national action plan
Copd national action plan Bitemporal wasting in copd
Bitemporal wasting in copd Hyprcapnia
Hyprcapnia Copd abcd assessment
Copd abcd assessment Ibratropium
Ibratropium Exacerbatie copd
Exacerbatie copd Terminale copd
Terminale copd Eindstadium copd
Eindstadium copd Copd pink puffer
Copd pink puffer Mucoid sputum
Mucoid sputum Copd lungs images
Copd lungs images Restrictive lung disease
Restrictive lung disease Copd types
Copd types Fever in copd
Fever in copd Fever in copd
Fever in copd Cv rizikó
Cv rizikó Verpleegplan copd
Verpleegplan copd Copd obstruktionsgrad
Copd obstruktionsgrad Ukuran asosiasi
Ukuran asosiasi Logistic regression epidemiology
Logistic regression epidemiology