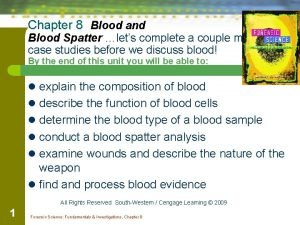
Components of Blood The Components of Blood 1
Components of Blood
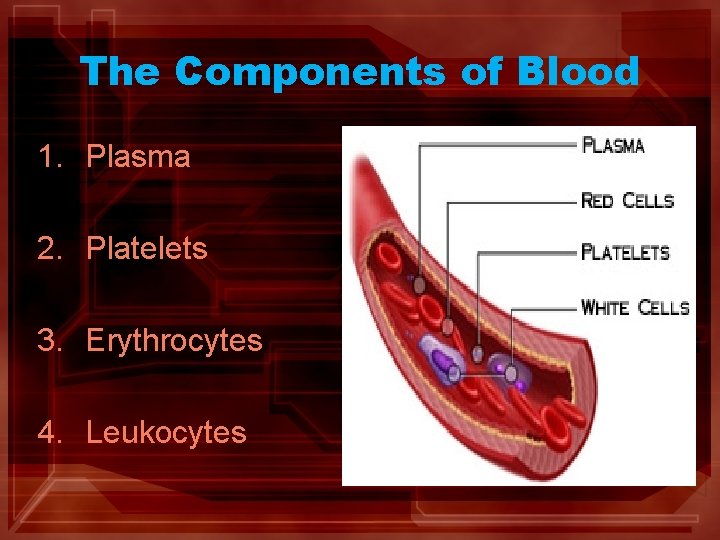
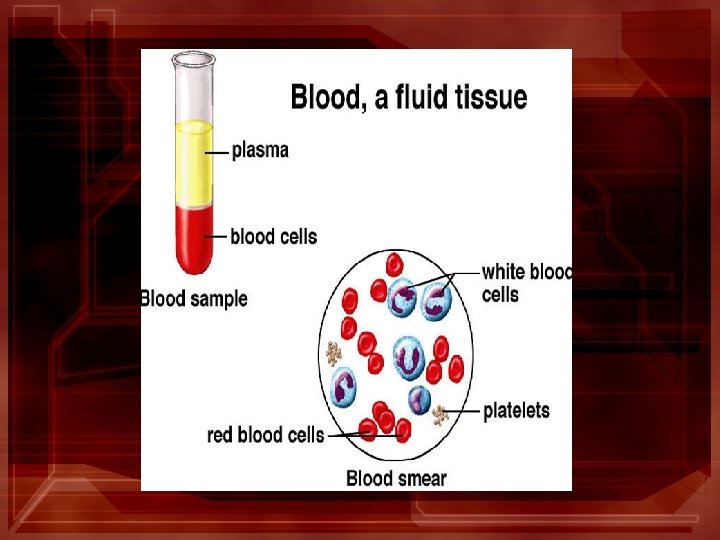
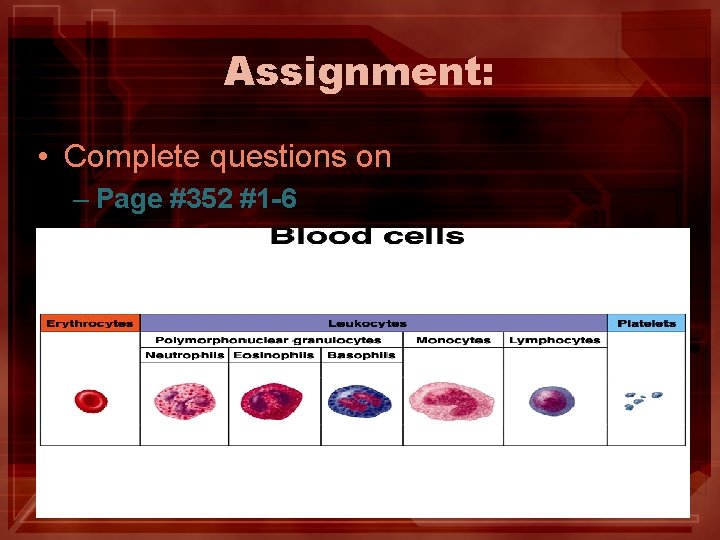
The Components of Blood 1. Plasma 2. Platelets 3. Erythrocytes 4. Leukocytes
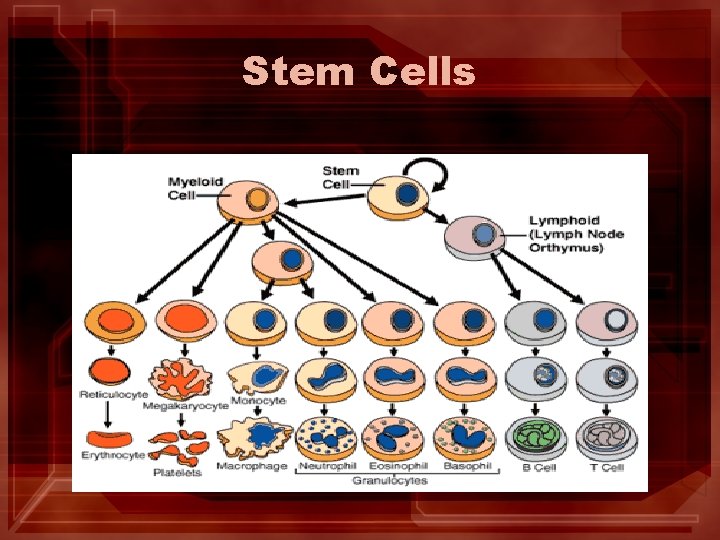
Stem Cells
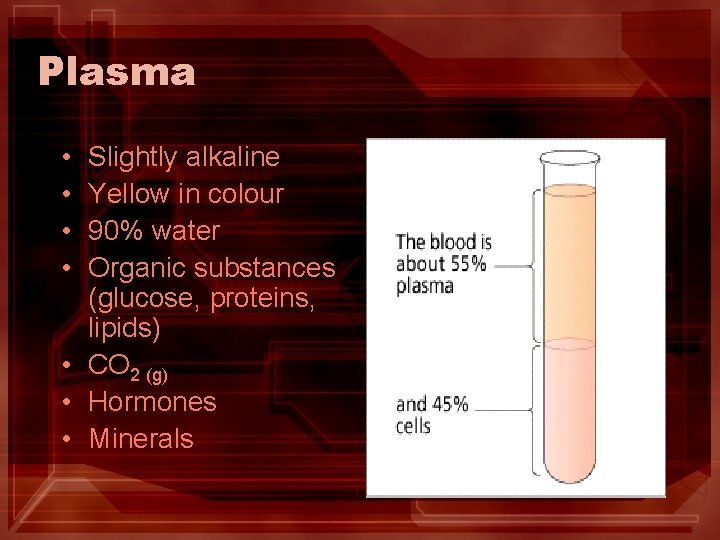
Plasma • • Slightly alkaline Yellow in colour 90% water Organic substances (glucose, proteins, lipids) • CO 2 (g) • Hormones • Minerals
Plasma Proteins • Albumins • Establishes the osmotic pressure that draws water back into the capillaries. • Globulins • Help provide protection against invading microbes. • Fibrinogen • Important in blood clotting.
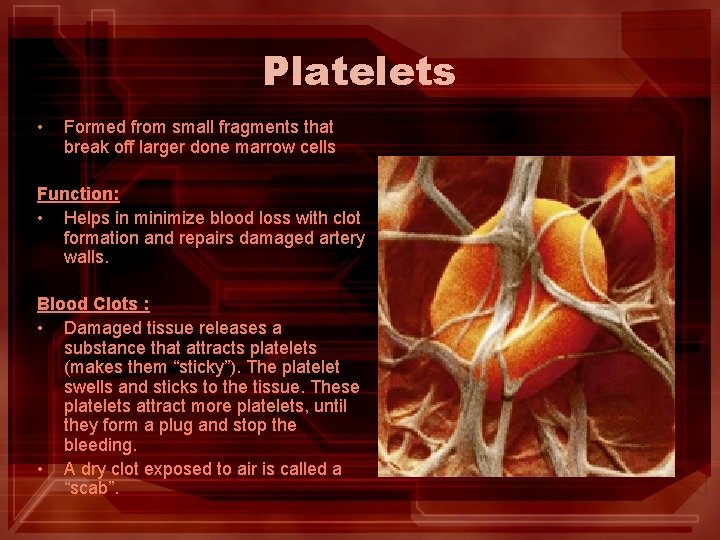
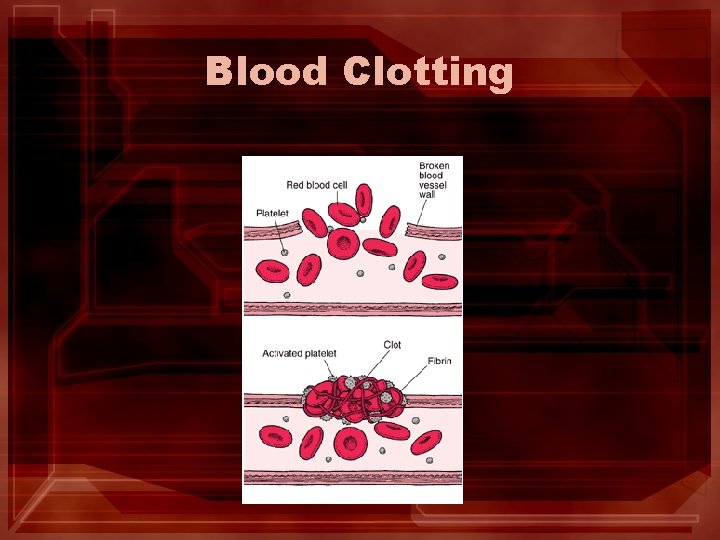
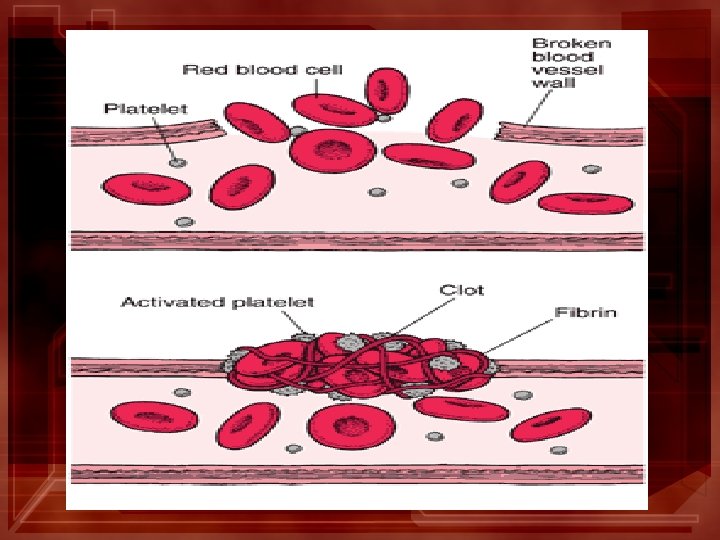
Platelets • Formed from small fragments that break off larger done marrow cells Function: • Helps in minimize blood loss with clot formation and repairs damaged artery walls. Blood Clots : • Damaged tissue releases a substance that attracts platelets (makes them “sticky”). The platelet swells and sticks to the tissue. These platelets attract more platelets, until they form a plug and stop the bleeding. • A dry clot exposed to air is called a “scab”.
Platelets Change shape from round to spiky when release substances that attract more platelets.
Blood Clotting
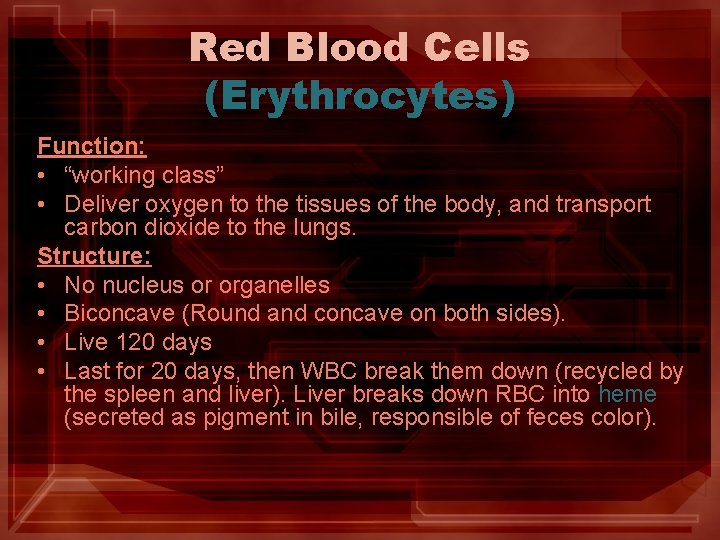
Red Blood Cells (Erythrocytes) Function: • “working class” • Deliver oxygen to the tissues of the body, and transport carbon dioxide to the lungs. Structure: • No nucleus or organelles • Biconcave (Round and concave on both sides). • Live 120 days • Last for 20 days, then WBC break them down (recycled by the spleen and liver). Liver breaks down RBC into heme (secreted as pigment in bile, responsible of feces color).
Red Blood Cells
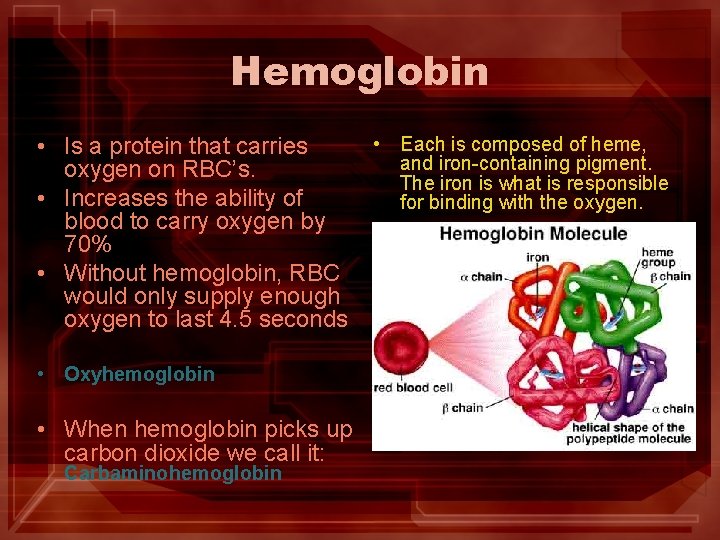
Hemoglobin • Is a protein that carries oxygen on RBC’s. • Increases the ability of blood to carry oxygen by 70% • Without hemoglobin, RBC would only supply enough oxygen to last 4. 5 seconds • Oxyhemoglobin • When hemoglobin picks up carbon dioxide we call it: Carbaminohemoglobin • Each is composed of heme, and iron-containing pigment. The iron is what is responsible for binding with the oxygen.
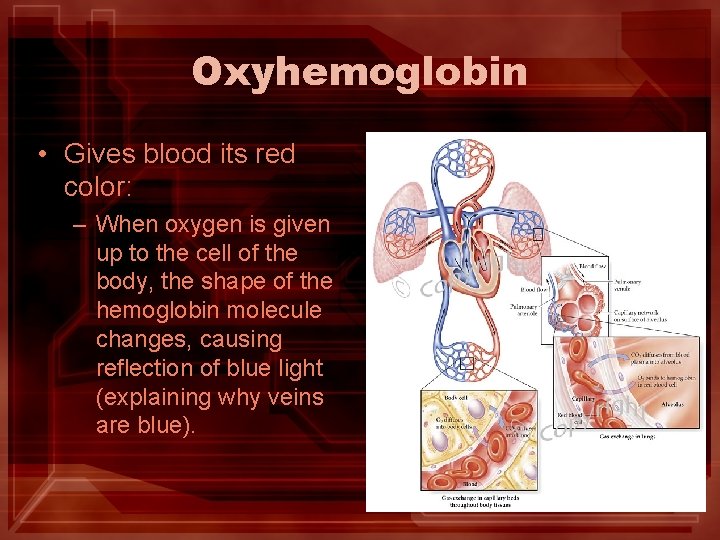
Oxyhemoglobin • Gives blood its red color: – When oxygen is given up to the cell of the body, the shape of the hemoglobin molecule changes, causing reflection of blue light (explaining why veins are blue).
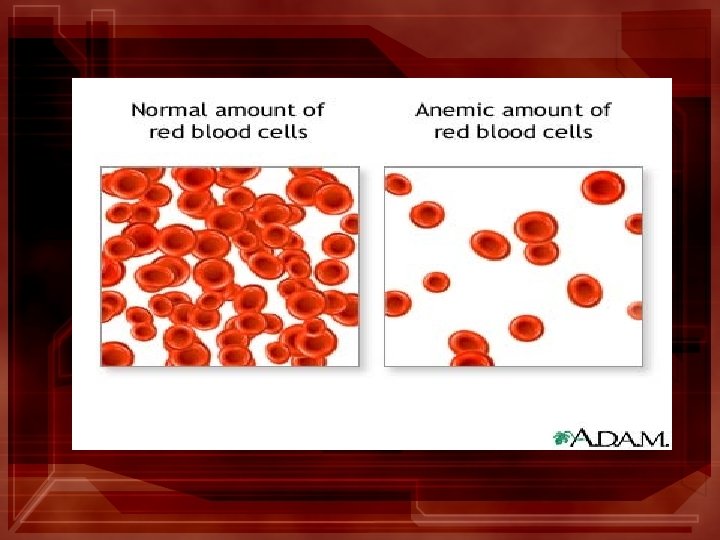
Anemia • Lack of oxygen delivery to tissues. • Results when there is a deficiency in hemoglobin or red blood cells (will have low iron levels as well). • Characterized by low energy levels. • Most common cause of low RBC count is hemorrhage. – Also: physical injury, bleeding ulcer, bleeding lungs b/c of tuberculosis, and iron deficiency).
White Blood Cells (Leukocytes) Function: • “fighting elite” • Important in defending the body against infections and foreign substances (via phagocytosis and antibodies). Structure: • Have a nucleus. • Located in your lymphatic system and circulatory system.
Assignment: • Complete questions on – Page #352 #1 -6
Blood Clotting
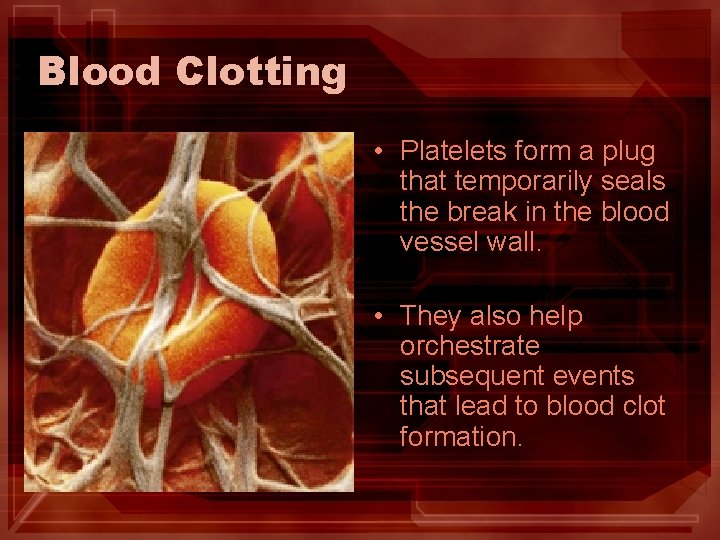
Blood Clotting • Platelets form a plug that temporarily seals the break in the blood vessel wall. • They also help orchestrate subsequent events that lead to blood clot formation.
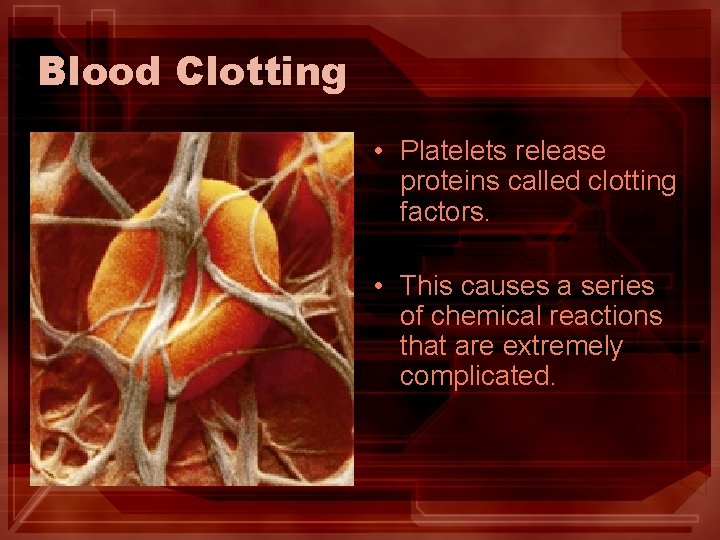
Blood Clotting • Platelets release proteins called clotting factors. • This causes a series of chemical reactions that are extremely complicated.
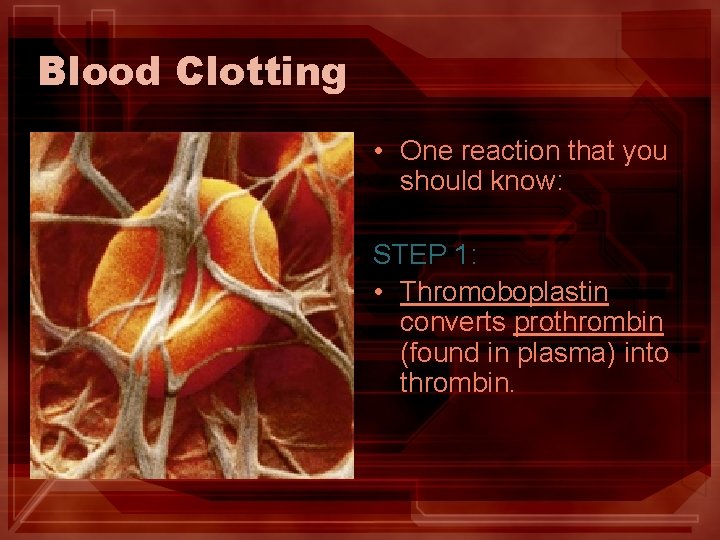
Blood Clotting • One reaction that you should know: STEP 1: • Thromoboplastin converts prothrombin (found in plasma) into thrombin.
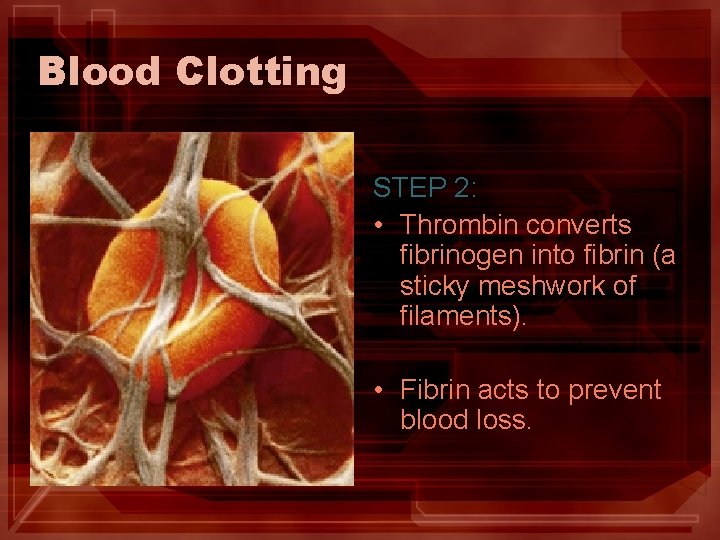
Blood Clotting STEP 2: • Thrombin converts fibrinogen into fibrin (a sticky meshwork of filaments). • Fibrin acts to prevent blood loss.
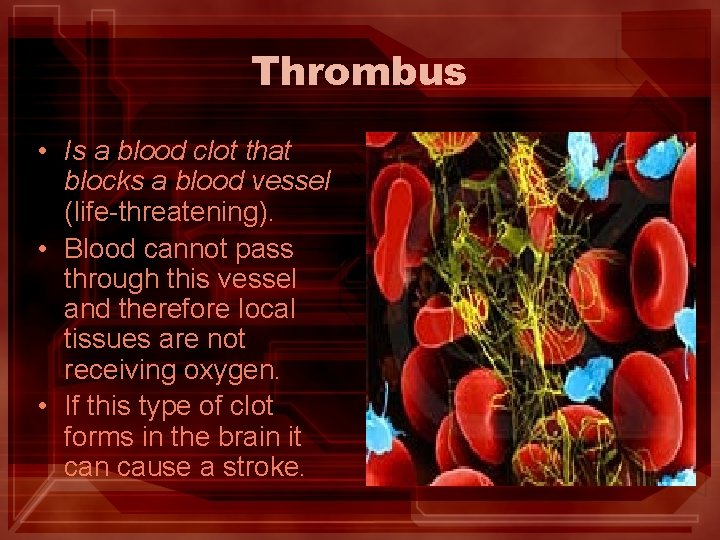
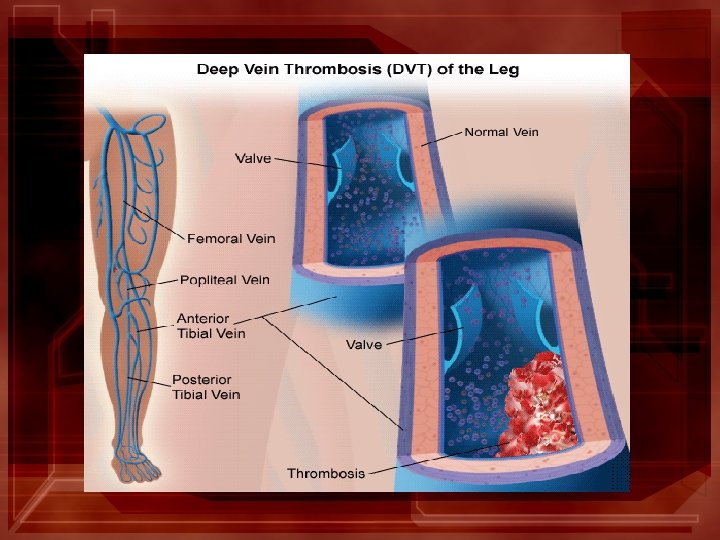
Thrombus • Is a blood clot that blocks a blood vessel (life-threatening). • Blood cannot pass through this vessel and therefore local tissues are not receiving oxygen. • If this type of clot forms in the brain it can cause a stroke.
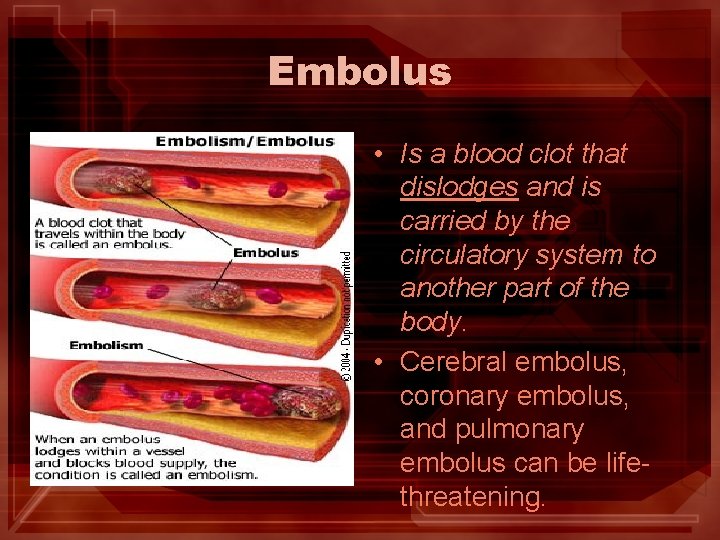
Embolus • Is a blood clot that dislodges and is carried by the circulatory system to another part of the body. • Cerebral embolus, coronary embolus, and pulmonary embolus can be lifethreatening.
Hemophilia - a genetic disorder that involves a defect in one of the clotting factor genes. - Hemophiliacs may bleed uncontrollably from even small cuts or scrapes. - They are given transfusions of clotting factors and platelets in order to reduce potential bleeding.
Artificial Blood Biology 20
Use of Artificial Blood • Fluosol, is a non-toxic artificial blood developed in Japan. • The ‘blood’ can maintain adequate oxygen levels until bone marrow begins to replenish RBC (transfusion) • Does not carry any viruses or diseases • Disadvantage: lacks ability to clot and protect the body (immunity).
ABO Blood Types Biology 20
In the 17 th century, Jean-Baptiste Denis performed the first blood transfusion by injecting sheep's blood into a young boy. The youth survived, but a repeat experiment, on an older man, proved disastrous– the man died almost immediately. “Why do some blood transfusions help, while others kill? ”
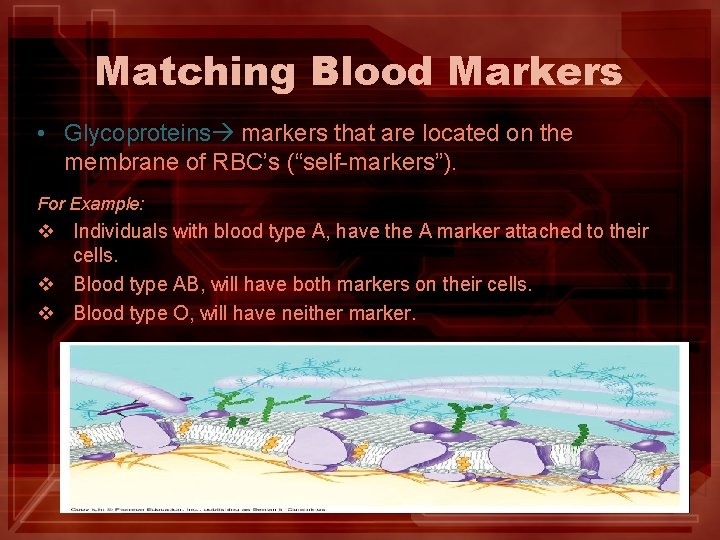
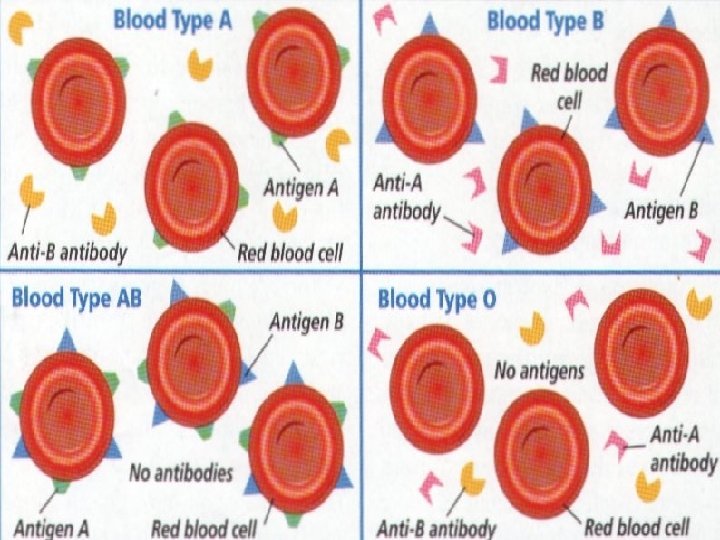
Matching Blood Markers • Glycoproteins markers that are located on the membrane of RBC’s (“self-markers”). For Example: v Individuals with blood type A, have the A marker attached to their cells. v Blood type AB, will have both markers on their cells. v Blood type O, will have neither marker.
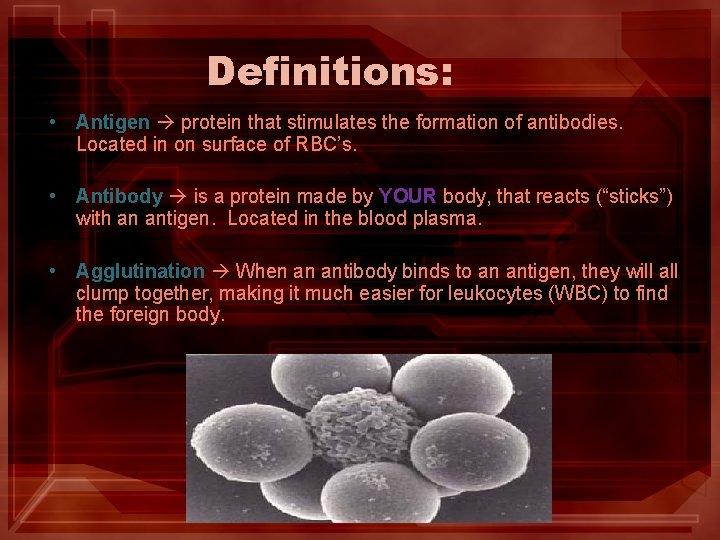
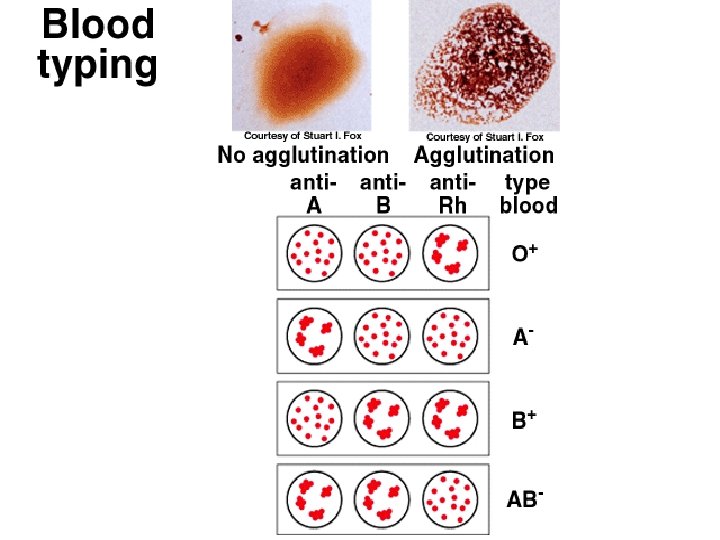
Definitions: • Antigen protein that stimulates the formation of antibodies. Located in on surface of RBC’s. • Antibody is a protein made by YOUR body, that reacts (“sticks”) with an antigen. Located in the blood plasma. • Agglutination When an antibody binds to an antigen, they will all clump together, making it much easier for leukocytes (WBC) to find the foreign body.
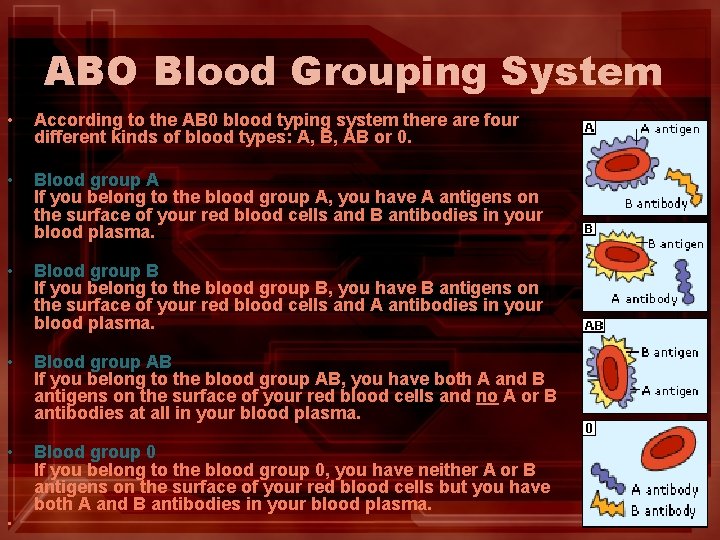
ABO Blood Grouping System • According to the AB 0 blood typing system there are four different kinds of blood types: A, B, AB or 0. • Blood group A If you belong to the blood group A, you have A antigens on the surface of your red blood cells and B antibodies in your blood plasma. • Blood group B If you belong to the blood group B, you have B antigens on the surface of your red blood cells and A antibodies in your blood plasma. Blood group AB If you belong to the blood group AB, you have both A and B antigens on the surface of your red blood cells and no A or B antibodies at all in your blood plasma. • • Blood group 0 If you belong to the blood group 0, you have neither A or B antigens on the surface of your red blood cells but you have both A and B antibodies in your blood plasma. •
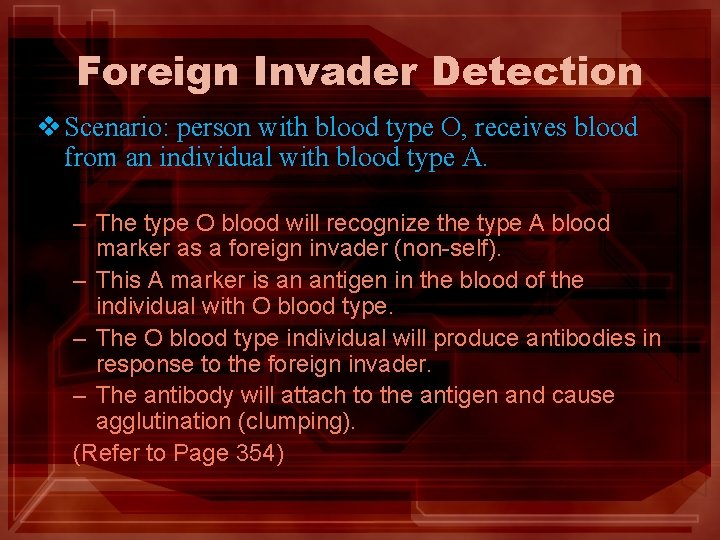
Foreign Invader Detection v Scenario: person with blood type O, receives blood from an individual with blood type A. – The type O blood will recognize the type A blood marker as a foreign invader (non-self). – This A marker is an antigen in the blood of the individual with O blood type. – The O blood type individual will produce antibodies in response to the foreign invader. – The antibody will attach to the antigen and cause agglutination (clumping). (Refer to Page 354)
Agglutination • The importance of a correct transfusion is emphasized by the fact that agglutinated blood can no longer pass through capillaries; therefore, clogging tissues and preventing the delivery of oxygen and nutrients.
Donors and Recipients Blood Type O • “Universal Donor” • This is because is can be received by individuals of all blood types ( no antigens on RBC’s). • Can only receive blood from type “O” individuals. Blood Type AB • These individuals can receive blood from any donor. • Can only donate blood to individuals with AB blood types.
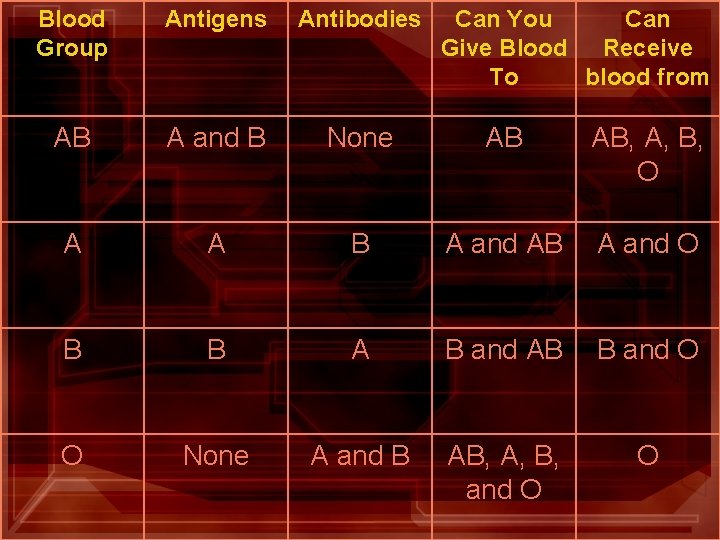
Blood Group Antigens Antibodies Can You Can Give Blood Receive To blood from AB A and B None AB AB, A, B, O A A B A and AB A and O B B A B and AB B and O O None A and B AB, A, B, and O O
Rhesus Factor Biology 20
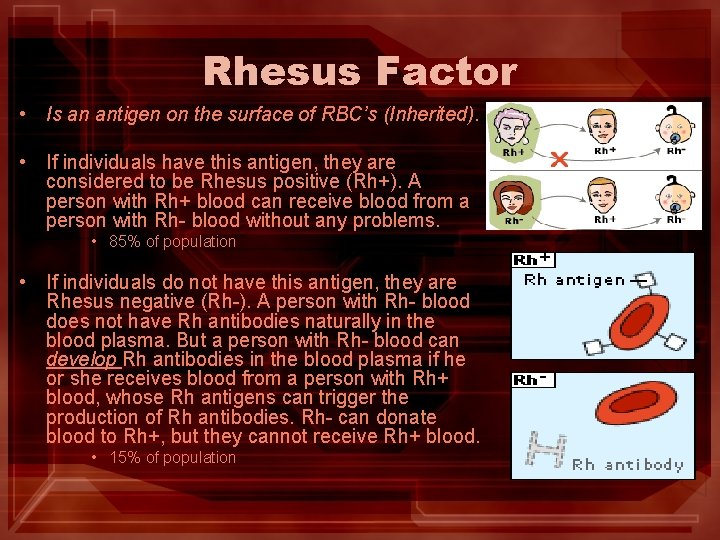
Rhesus Factor • Is an antigen on the surface of RBC’s (Inherited). • If individuals have this antigen, they are considered to be Rhesus positive (Rh+). A person with Rh+ blood can receive blood from a person with Rh- blood without any problems. • 85% of population • If individuals do not have this antigen, they are Rhesus negative (Rh-). A person with Rh- blood does not have Rh antibodies naturally in the blood plasma. But a person with Rh- blood can develop Rh antibodies in the blood plasma if he or she receives blood from a person with Rh+ blood, whose Rh antigens can trigger the production of Rh antibodies. Rh- can donate blood to Rh+, but they cannot receive Rh+ blood. • 15% of population
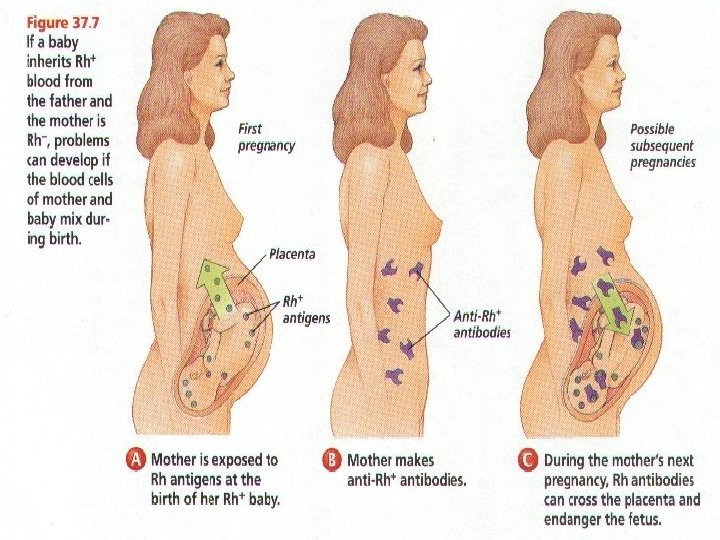
Erythroblastosis Fetalis 1 st Child • A condition that occurs when a mother’s antibodies against Rh+ blood enter the Rh+ blood of her fetus (baby inherits the Rh+ from the father). • Therefore, only important with Rh+ babies and Rh- mothers. • 1 st child is not affected b/c the mothers and babies blood is separated by the placenta, until after birth. • Capillary beds rupture when the placenta is shed from the uterus in birth, this is the first time blood is mixed. • The mothers immune system will recognized the Rh+ antigens and this will trigger the production of antibodies. These antibodies will not effect the baby, because by the time they are produced the baby will no longer be attached to the placenta.
Erythroblastosis Fetalis 2 nd Child • Mother has retained Rh+ antibodies from the first exposure to the antigen (1 st born). • With second birth, the mothers antigens will cross the placenta and attack the baby’s RBC’s.
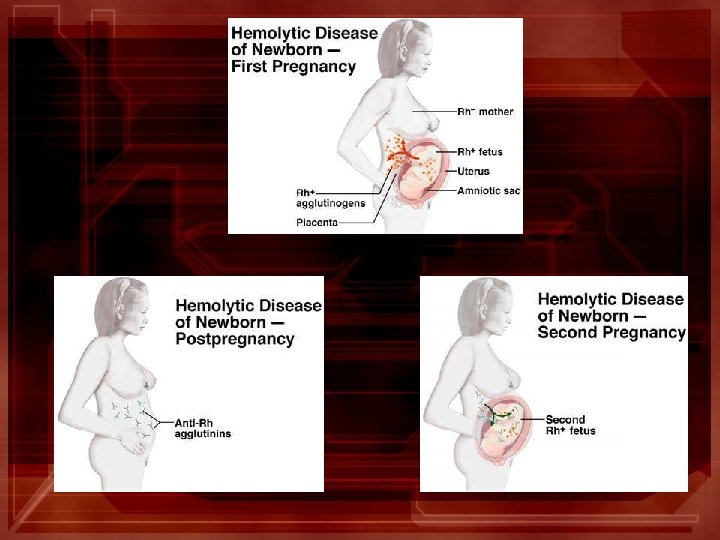
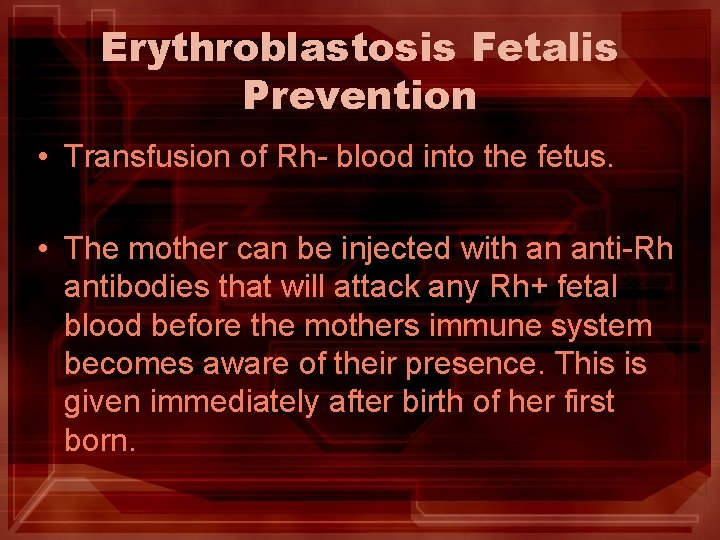
Erythroblastosis Fetalis Prevention • Transfusion of Rh- blood into the fetus. • The mother can be injected with an anti-Rh antibodies that will attack any Rh+ fetal blood before the mothers immune system becomes aware of their presence. This is given immediately after birth of her first born.
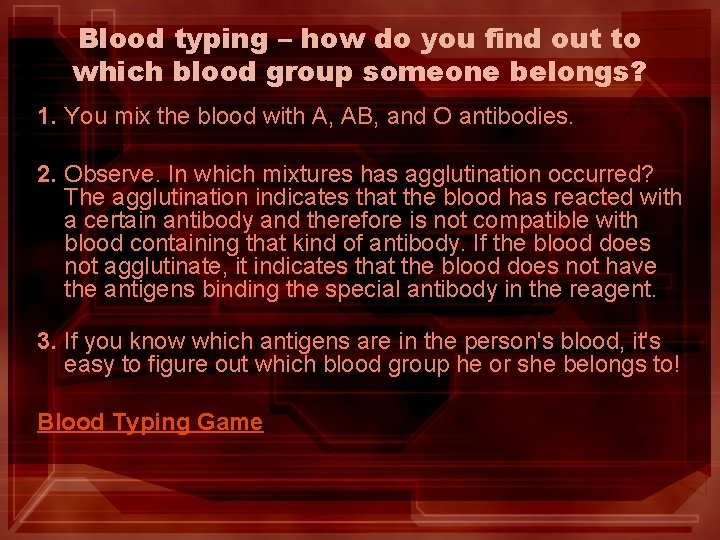
Blood typing – how do you find out to which blood group someone belongs? 1. You mix the blood with A, AB, and O antibodies. 2. Observe. In which mixtures has agglutination occurred? The agglutination indicates that the blood has reacted with a certain antibody and therefore is not compatible with blood containing that kind of antibody. If the blood does not agglutinate, it indicates that the blood does not have the antigens binding the special antibody in the reagent. 3. If you know which antigens are in the person's blood, it's easy to figure out which blood group he or she belongs to! Blood Typing Game
Vaccines • Living attenuated microbes: These are mutants of microbes that have lost the ability, either naturally or by treatment in the laboratory, to produce the dangerous, clinical disease. • These vaccination s infect you with a living microbe which then produces a limited infection. Because these microbes are weak, the immune system of normal healthy people quickly kill and eliminate them from the body. • Now possess the necessary antibodies against the disease/virus • Dead Microbes: These vaccines are manipulated in the lab. • They use disease-producing microbe , but killing them in such a way that they retain their ability to stimulate the body to produce antibodies. • Examples: include anthrax and rabies vaccine.
Assignment: 1. Complete questions on Page 356 #15 -18 2. Find 3 people who you could receive a successful blood transfusion from (at least 1 family member).
The Body’s Lines of Defense Biology 20
The Body’s Line of Defense • Three lines of defense have evolved to help resist infection and possible death. • First two lines of defense non-specific immunity Third line of defense specific immunity •
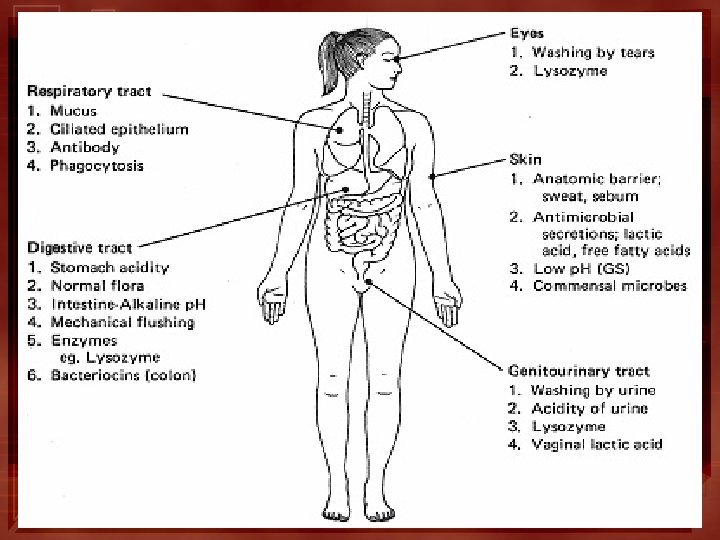
The First Line of Defense • Physical Barriers – skin and mucous membranes. Examples: • Lysozyme, an antimicrobial enzymes secreted in tears, saliva, mucous secretion, and sweat, destroys the cells walls of the bacteria. • The respiratory tract has mucous and cilia (hairlike structures), which trap foreign debris. Coughing expels them. • Acidity in the stomach destroys invaders.
The Second Line of Defense • Activated if invaders take up residence within the body. • Leukocytes, or WBC’s, may engulf invading microbes or produce antibodies. • Non-specific defense mechanisms relay on Phagocytosis. • Phagocytosis the process by which a white blood cell engulfs and chemically destroys a microbe.
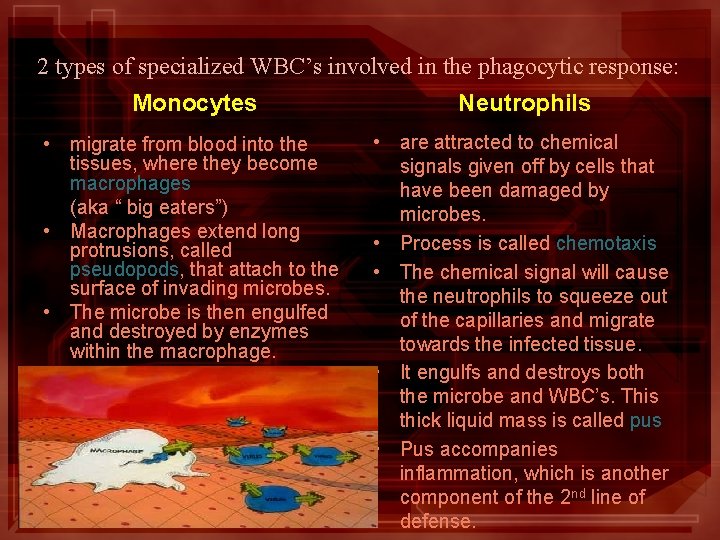
2 types of specialized WBC’s involved in the phagocytic response: Monocytes Neutrophils • migrate from blood into the tissues, where they become macrophages (aka “ big eaters”) • Macrophages extend long protrusions, called pseudopods, that attach to the surface of invading microbes. • The microbe is then engulfed and destroyed by enzymes within the macrophage. • are attracted to chemical signals given off by cells that have been damaged by microbes. • Process is called chemotaxis • The chemical signal will cause the neutrophils to squeeze out of the capillaries and migrate towards the infected tissue. • It engulfs and destroys both the microbe and WBC’s. This thick liquid mass is called pus • Pus accompanies inflammation, which is another component of the 2 nd line of defense.
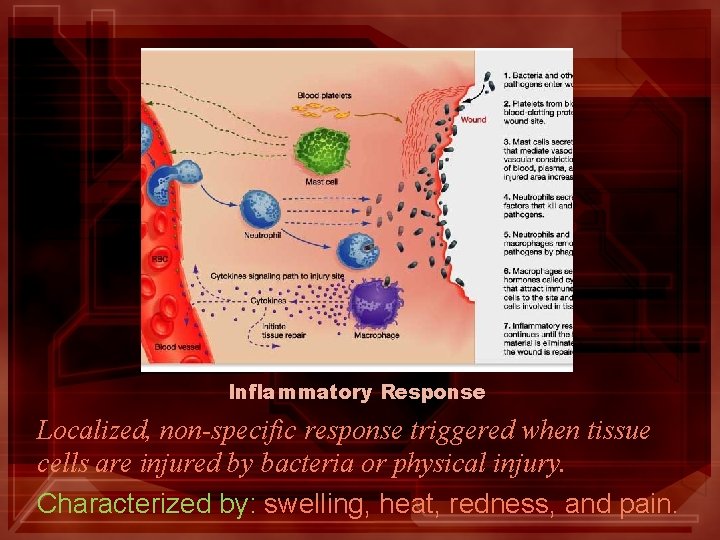
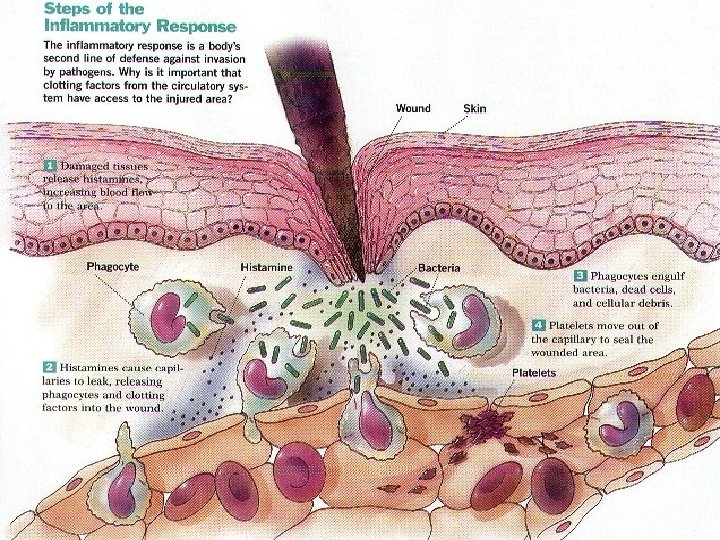
Inflammatory Response Localized, non-specific response triggered when tissue cells are injured by bacteria or physical injury. Characterized by: swelling, heat, redness, and pain.
Inflammatory Response 1. Initiated by a chemical signal (Histamine and Prostaglandins). Causes dilation and permeability of nearby capillaries. 2. Blood clotting elements activated. 3. Phagocytic cells migrate to area and consumes the pathogens and cell debris. Page 358 Figure 2 (very important)
It’s gettin’ hot in here! • When you are infected with a cold or flu, neutrophils and macrophages will destroy the microbes and release chemicals into the blood. • When these chemicals are detected by the hypothalamus, they cause an increase in the bodies temperature aka Fever. • Why increase body temperature? • The higher temperature helps prevent the spread (reproduction) of the microbe
Third Line of Defense (The Immune Response) • Complement proteins plasma proteins that help defend against invading microbes
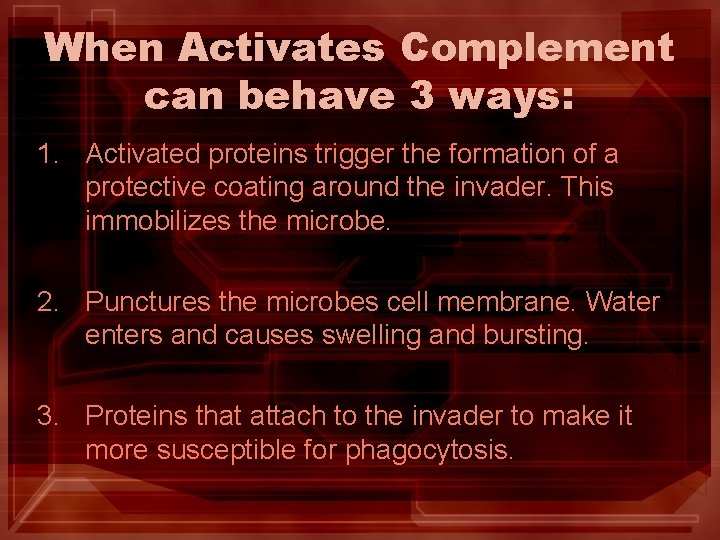
When Activates Complement can behave 3 ways: 1. Activated proteins trigger the formation of a protective coating around the invader. This immobilizes the microbe. 2. Punctures the microbes cell membrane. Water enters and causes swelling and bursting. 3. Proteins that attach to the invader to make it more susceptible for phagocytosis.
Lymphocytes • A type of WBC that produces antibodies. • Foreign protein markers activate the production of antibodies. • The cell membranes of the bacterium contain many different antigens. • Two types of Lymphocytes – T cells – B cells
T cells • Produced in the bone marrow and stored in the thymus gland. • Function: find invader and signal the attack. • Once T cells find the invader and identify the antigen, another T cell passes the information to the B cells. 1. Helper T cells present infected cells to killer T cells and B cells. 2. Killer T cells cause lysis of the infected cell. 3. Suppressor T cells once the invader is removed, this cell turns the immune system off.
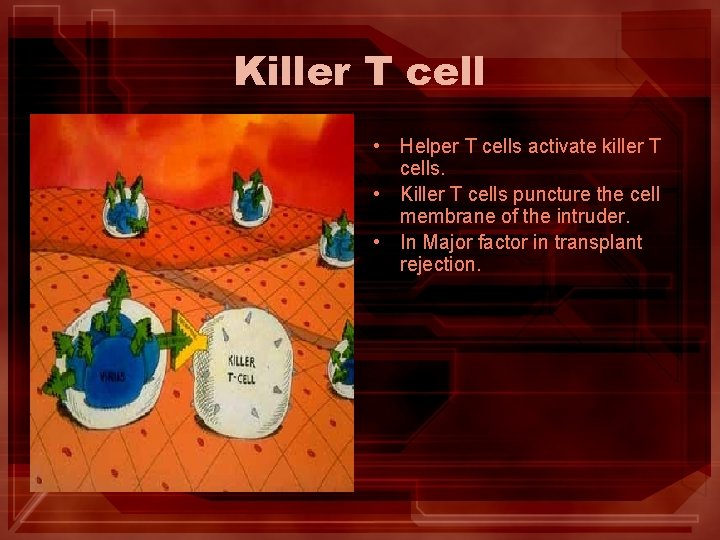
Killer T cell • Helper T cells activate killer T cells. • Killer T cells puncture the cell membrane of the intruder. • In Major factor in transplant rejection.
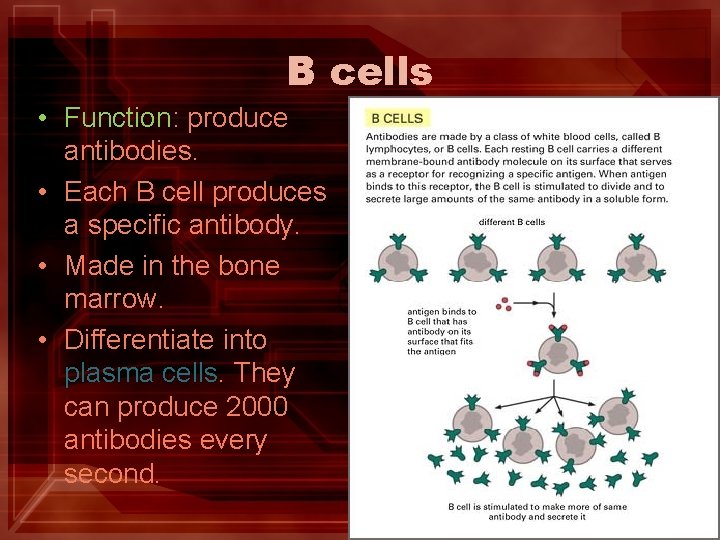
B cells • Function: produce antibodies. • Each B cell produces a specific antibody. • Made in the bone marrow. • Differentiate into plasma cells. They can produce 2000 antibodies every second.
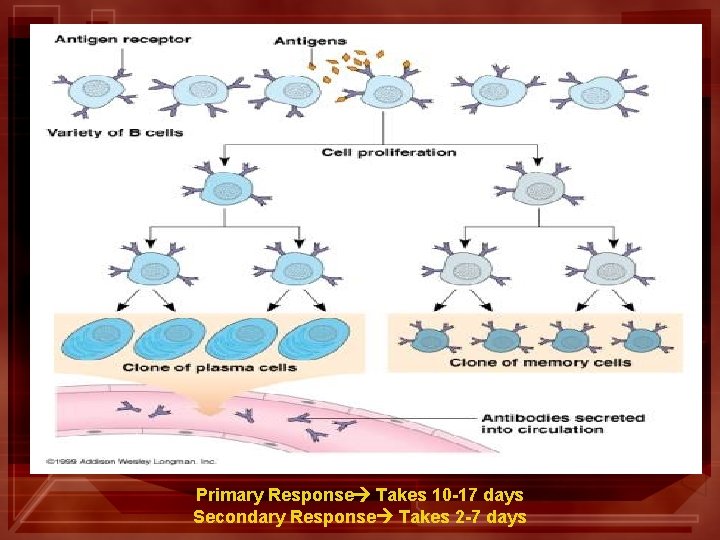
Primary Response Takes 10 -17 days Secondary Response Takes 2 -7 days
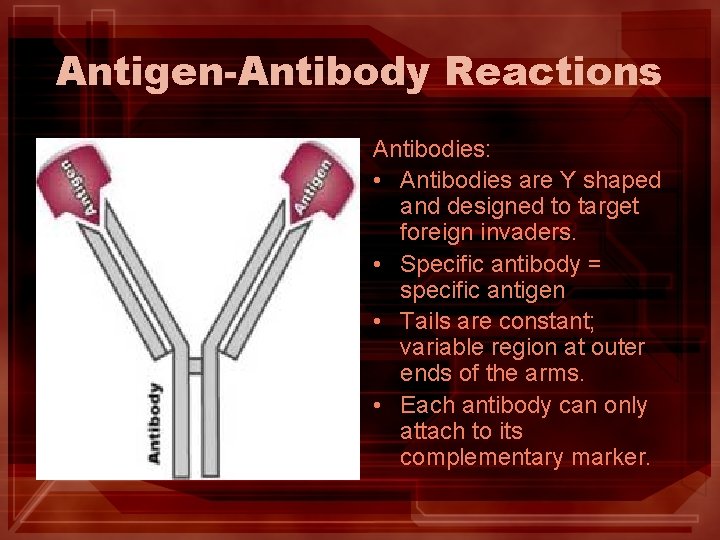
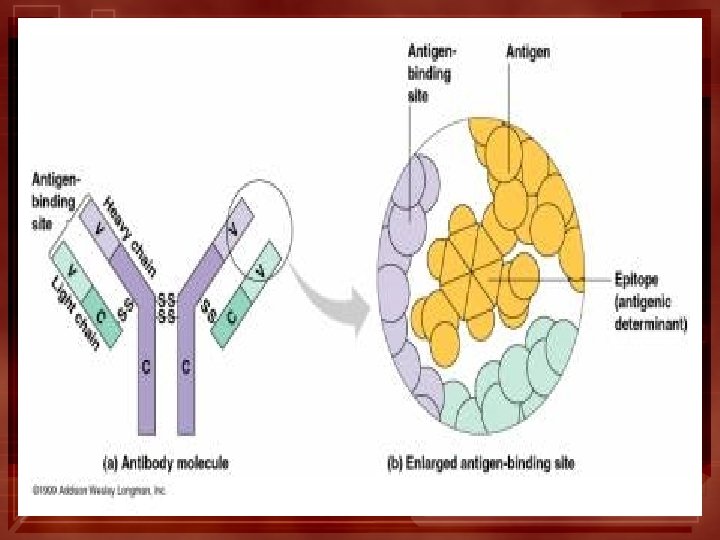
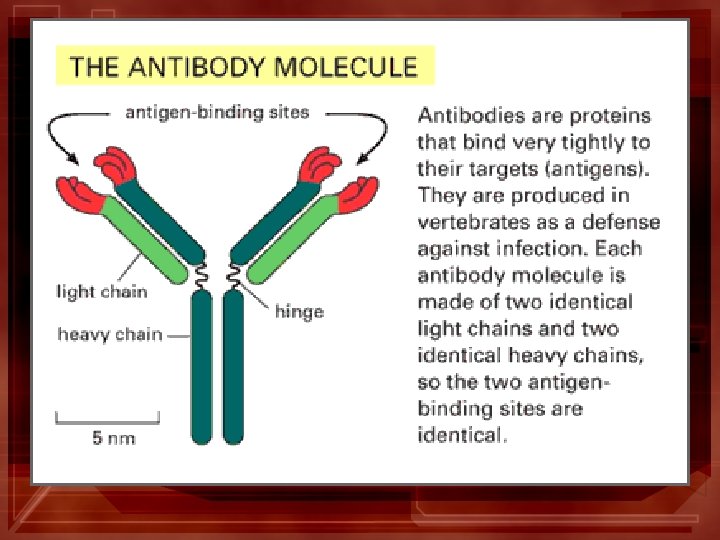
Antigen-Antibody Reactions Antibodies: • Antibodies are Y shaped and designed to target foreign invaders. • Specific antibody = specific antigen • Tails are constant; variable region at outer ends of the arms. • Each antibody can only attach to its complementary marker.
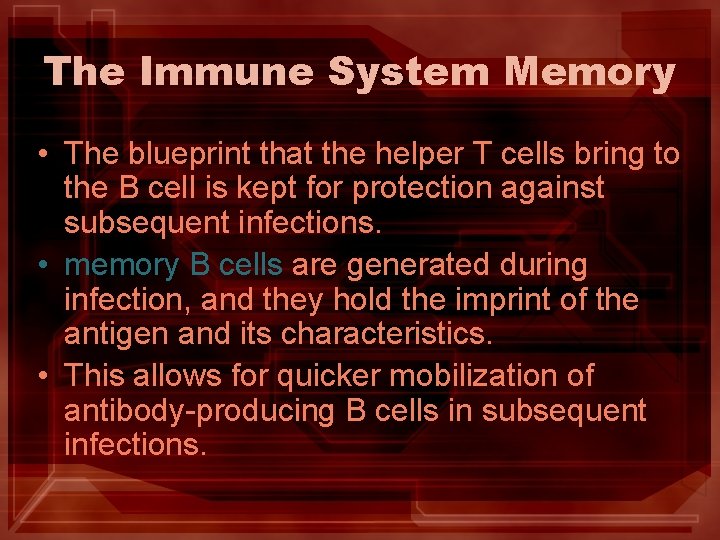
The Immune System Memory • The blueprint that the helper T cells bring to the B cell is kept for protection against subsequent infections. • memory B cells are generated during infection, and they hold the imprint of the antigen and its characteristics. • This allows for quicker mobilization of antibody-producing B cells in subsequent infections.
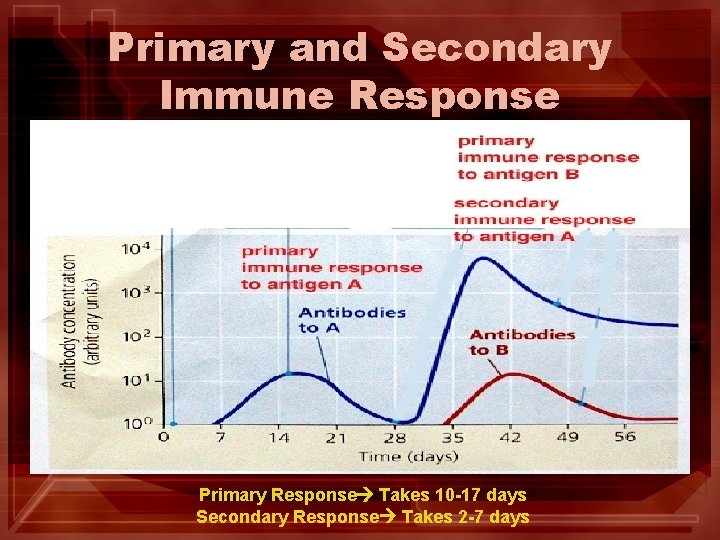
Primary and Secondary Immune Response Primary Response Takes 10 -17 days Secondary Response Takes 2 -7 days
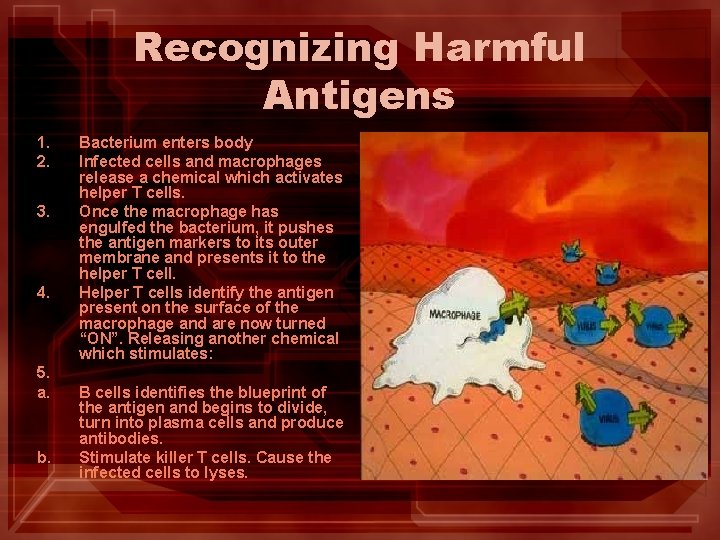
Recognizing Harmful Antigens 1. 2. 3. 4. 5. a. b. Bacterium enters body Infected cells and macrophages release a chemical which activates helper T cells. Once the macrophage has engulfed the bacterium, it pushes the antigen markers to its outer membrane and presents it to the helper T cell. Helper T cells identify the antigen present on the surface of the macrophage and are now turned “ON”. Releasing another chemical which stimulates: B cells identifies the blueprint of the antigen and begins to divide, turn into plasma cells and produce antibodies. Stimulate killer T cells. Cause the infected cells to lyses.
How do antibodies protect against poisons or toxins, from destroying cells? • Receptor sites are ports along the cell membranes in which hormones, nutrients, and other needed materials fit. • Toxins can dock on these sites and be engulfed in to the cell. • Antibodies interfere with the attachment of toxins to the cell membrane receptor sites by binding to the toxins.
AIDS is an immunodeficiency disease caused by a virus • “Acquired Immunodeficiency Syndrome” • Human immunodeficiency virus (HIV) is the causative agent of AIDS. Probably evolved from a similar virus in chimpanzees. • Virus infects helper T cells.
Malfunctions of the Immune System Biology 20
Allergies • Occurs when your immune system mistakes harmless antigens for harmful invaders. • For example: If you are allergic to peanuts, your body recognizes one of the proteins in peanuts as dangerous. • Tissue swelling, mucous secretions and sometimes closed airways are a part of the immune response. • Dust, ragweed, strawberries and leaf moulds can be life threatening.
Anaphylactic Reactions (severe allergic rxns) • These reactions involve the circulatory or respiratory systems; accompanied by swelling, hives, and itching. • When you ingest something (food or medicine) that your body believes is dangerous, it releases a chemical messenger bradykinin. The chemical stimulates the release of histamine.
The Effect of Histamine • Histamine increase capillary permeability. • Proteins and WBC’s leave the capillaries in search of invader; this alters the osmotic pressure. – Less water is absorbed and tissue swells. Ø Anaphylactic shock can occur very quickly (weakness, sweating, and difficulty breathing are indicators). Ø Epinephrine or antihistamines
Autoimmune Diseases • Immune system attacks own body cells and tissues. • Mutated B and T cells; believed to be removed by suppressor T cells that enroll macrophages to remove these faulty cells. • The failure of suppressor T cells to control the renegade cell is an autoimmune disease (rheumatoid arthritis).
Multiple Sclerosis • Autoimmune disease in which T cells of the body initiate an attack on the myelin sheath of nerve cells. • In final stages can lead to paralysis.
Organ Transplant Matches • Major histocompatibility complex protein fingerprints unique to each individual. • Often look to close relatives for transplant. • Research of drugs that will stops the immune rejection of the transplant. Downfall, is that this increases patient risk for infection. • Transgenic transplants
Stem Cell Research • Stems cells can develop into a variety of different tissues and cells. • Embryonic stem cell research is particularly controversial because, with the present state of technology, starting an embryonic stem cell line requires the destruction of a human embryo and/or therapeutic cloning. • Some opponents of the research also argue that this practice is a slippery slope to reproductive cloning • Parkinson's – Michael J Fox – Political Commercial • Paralysis – Christopher Reeve
- Slides: 84