Blood Bank Conclusion Open Discussion and Recommendations Safe
Blood Bank Conclusion, Open Discussion, and Recommendations
Safe Blood Donation • Voluntary blood donation. • Unpaid blood donation. • Absence of profit.
Donor Categories • “Allergenic”, “homologous” and “random donor” terms used for blood donated by individuals for anyone’s use • Autologous – donate blood for your own use only • Recipient Specific Directed donation – donor called in because blood/blood product is needed for a specific patient • Directed Donor – patient selects their own donors • Therapeutic bleeding – blood removed for medical purposes such as in polycythemia vera. NOT used for transfusion.

Donor Categories • Safest is autologous, blood is your own, no risk of disease acquisition • Most dangerous is Directed Donor, you select a donor who may, unknown to you, be in a high risk category but feels obligated to follow through and donate
Blood donation reactions and complications • Mild Reactions: - ( Anxiety, Increase respiration, Rapid Pulls, Pallor and mild Sweating. • Moderate Reactions: - Loss of Consciousness (faint), Slow Pulls (Difficult to feel ). • Sever Reactions: - Faint, Convulsion, ----
How To Manage Donation Reaction Mild) 1 - Discontinue Donation. 2 - Raise Legs and Lower Head. 3 - Loose or Remove tight. 4 - Keep the donor Cool. 5 - After recover offer him a cool drink. 6 - Record the reaction at the BB recording. Ensure that he is full recovered before leaving.
How To Manage Donation Reaction (Moderate) • • As before in addition to: 1 - Remove him to another room for privacy 2 - Chick the pulls, the appearance. 3 - release him when full recovered.
How To Manage Donation Reaction (Sever) • As before in addition to: • 1 - Turn the donor to a lateral position to maintain a clear airway. • 2 - Gently restrain the donor to prevent any injury. • 3 - Ensure that he is full recovered before leaving. • 4 - Advise him not to donate blood again and contact a doctor.
Post-Phlebotomy Care • Donor applies pressure for 5 minutes • Check and bandage site • Have donor sit up for few minutes • Have donor report to refreshment area for additional 15 minutes of monitoring
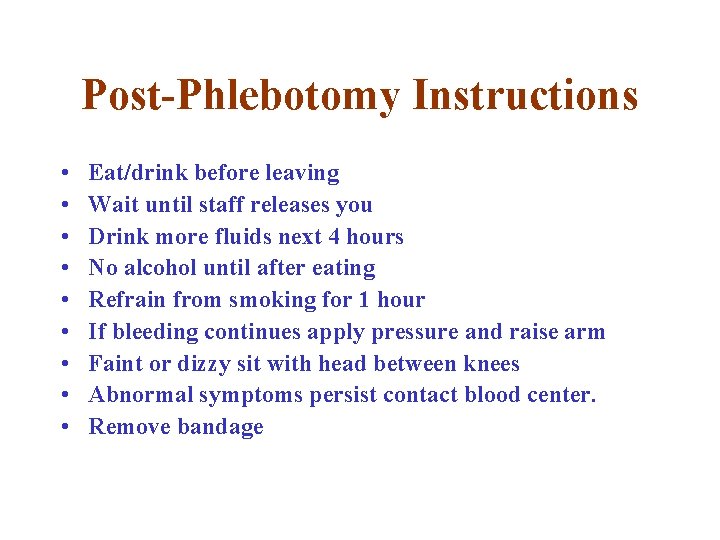
Post-Phlebotomy Instructions • • • Eat/drink before leaving Wait until staff releases you Drink more fluids next 4 hours No alcohol until after eating Refrain from smoking for 1 hour If bleeding continues apply pressure and raise arm Faint or dizzy sit with head between knees Abnormal symptoms persist contact blood center. Remove bandage
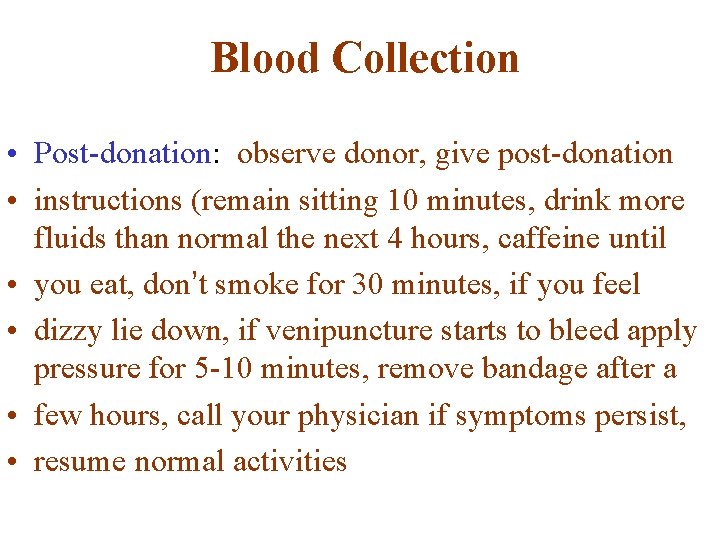
Blood Collection • Post-donation: observe donor, give post-donation • instructions (remain sitting 10 minutes, drink more fluids than normal the next 4 hours, caffeine until • you eat, don’t smoke for 30 minutes, if you feel • dizzy lie down, if venipuncture starts to bleed apply pressure for 5 -10 minutes, remove bandage after a • few hours, call your physician if symptoms persist, • resume normal activities
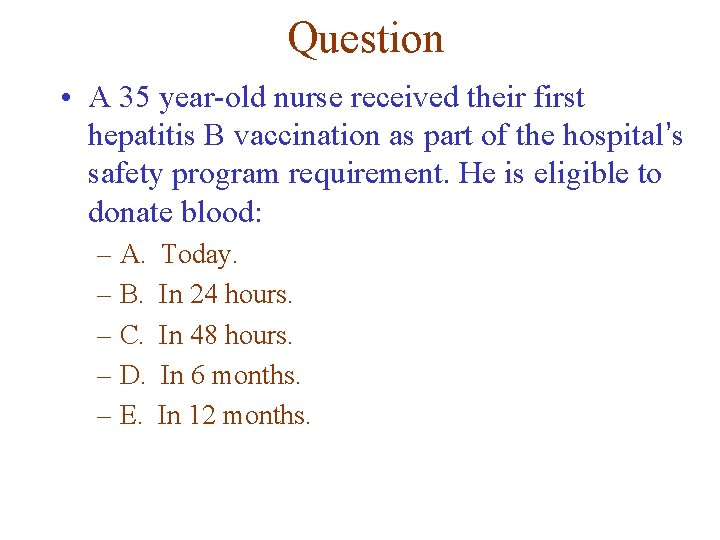
Question • A 35 year-old nurse received their first hepatitis B vaccination as part of the hospital’s safety program requirement. He is eligible to donate blood: – A. – B. – C. – D. – E. Today. In 24 hours. In 48 hours. In 6 months. In 12 months.
Question • A contact person to HBV, or HCV patient is not eligible to donate blood for : • • A- Two months • B- 6 months • C- Four month
Question • During Your Councilling, a blood donor before collecting his blood , he prevails that he is a diabetic patient. Would you accept or differed him?
Specimen Considerations – Recipient Specimen must be clearly and accurately identified Labeled with patient’s first and last name, hospital ID, date specimen drawn, who drew the specimen. Information on request for crossmatch must exactly match information on patient ID. Never rely on door tag, bed tag, patient chart for ID
Blood Typing (Reverse method) • There are 2 components to blood typing: – Test unknown cells with known antibodies – Test unknown serum/plasma with known RBc’s • The patterns are compared and the blood • group is determined.
Slide Blood Typing - continued • The slide is divided into halves. • On one side a drop of anti-A is added, this will attach to and cause clumping of RBcs possessing the A antigen. • On the other side a drop of anti-B is added which will cause clumping of RBcs with the B antigen. • A drop of RBcs is added to each side and mixed well with the reagent. • The slide is tilted back and forth for one minute and observed for agglutination (clumping) of the RBcs
Slide Blood Typing • Very rudimentary method for determining blood groups. • CANNOT be used for transfusion purposes as false positives and negatives do occur. • A “false positive” is when agglutination occurs not because the antigen is present, but cells may already be clumpled. • A “false negative” is one in which the cells are not clumped because there are too many cells or not enough reagent.
ABO Compatibility Best to give ABO group specific blood Should not give ABO non-specific whole blood In Packed Red Cells small amount of antibodies remaining in plasma are diluted by patient’s system are inconsequential Recipient blood is forward and reverse typed. Donor ABO group must be confirmed after ABO label is attached.
Cross-Reaction • If donor and recipient blood types not compatible: – Plasma antibody meets its specific surface antigen and blood will agglutinate and hemolyze
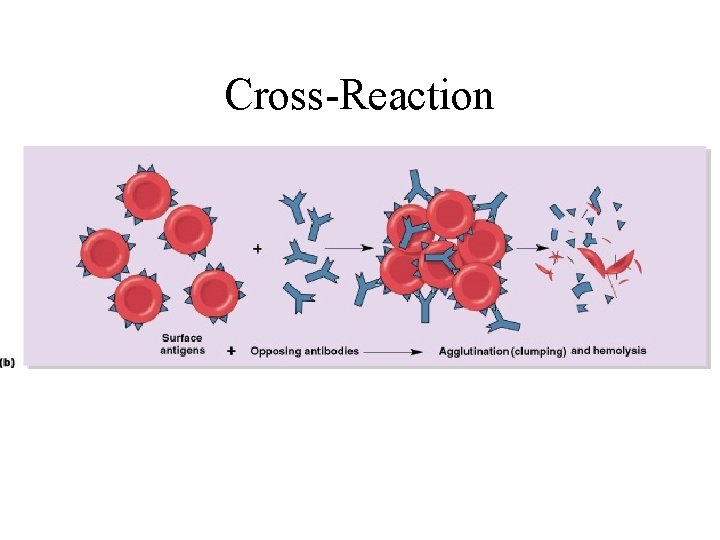
Cross-Reaction Figure 19– 6 b
Blood Storage • • Blood Donated is stored in low temp ( 1 -6 C) To slow or stop al biochemical activities, and keep blood cells active, and avoid contamination.
Blood Transfusion Request • It should provide the following information's: • . Date of Request. • . Patients full name, date of birth, sex, hospital No, word, address, blood group if known. • . provisional diagnosis. • . Presence of antibodies. • . History of previous transfusion, and reaction if happened. • . No of previous pregnancies (female) • . No and type of units of blood and blood products required. • . Reason of transfusion. • Signature of doctor requesting the blood. • • • . . .
Blood transfusion reaction 1. Stop transfusion immediately 2. Continue IV infusion with normal saline 3. Notify physician of client’s signs and symptoms 4. Provide care for client as indicated 5. Complete reaction form according to institution protocol. 6. Obtain urine specimen from client and send for free hemoglobin.
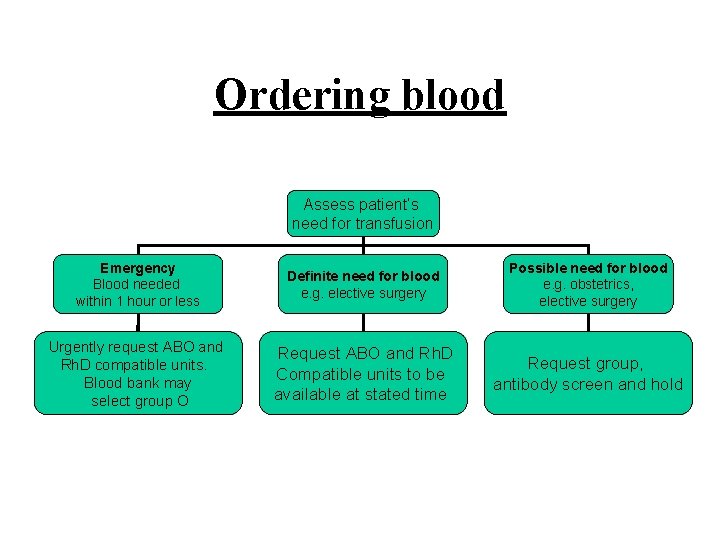
Ordering blood Assess patient’s need for transfusion Emergency Blood needed within 1 hour or less Definite need for blood e. g. elective surgery Possible need for blood e. g. obstetrics, elective surgery Urgently request ABO and Rh. D compatible units. Blood bank may select group O Request ABO and Rh. D Compatible units to be available at stated time Request group, antibody screen and hold
Urgent Release of Blood Requesting physician must document that the clinical situation was urgent to require release of uncross matched blood. Usually give O neg unless ABO type/Rh of recipient has been determined (can't use previous records). Units must be labeled to make it clear that testing was incomplete
Personnel 1. Does the facility have qualified personnel with appropriate education, training and experience-competent performance of assigned duties 2. Effective job description
Personnel Well defined program Orientation of new employees Regular scheduled competency evaluation of staff: To ensure that their skills are maintained
DOCUMENTATION If you have not documented it, You have NOT done it.
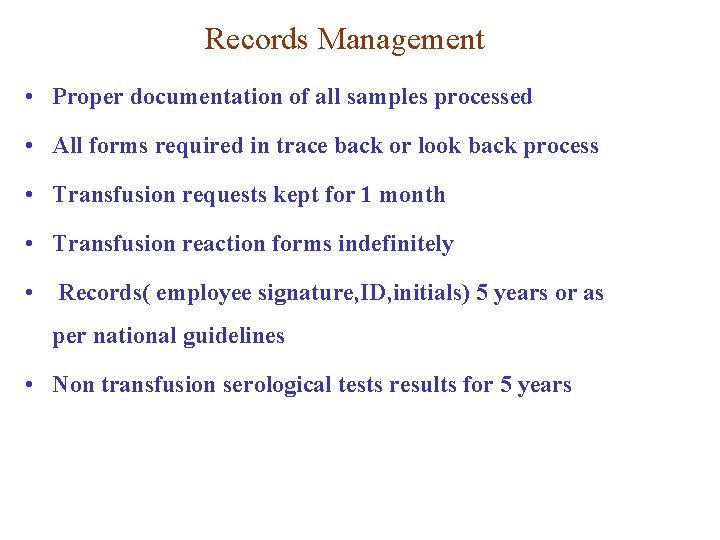
Records Management • Proper documentation of all samples processed • All forms required in trace back or look back process • Transfusion requests kept for 1 month • Transfusion reaction forms indefinitely • Records( employee signature, ID, initials) 5 years or as per national guidelines • Non transfusion serological tests results for 5 years
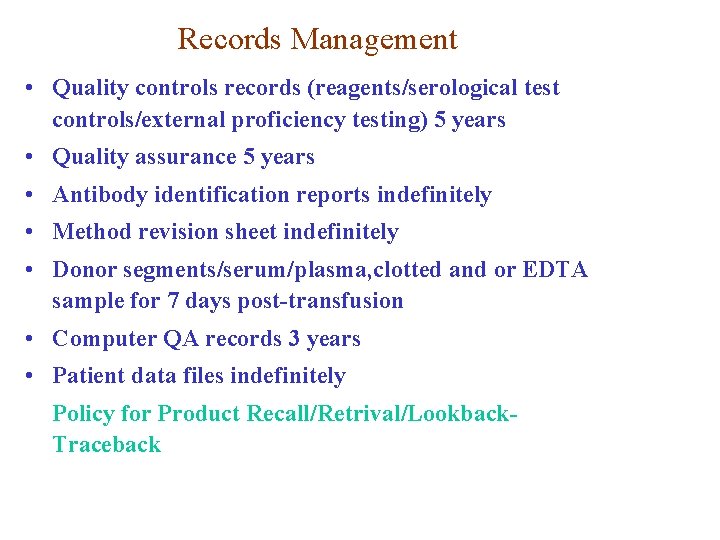
Records Management • Quality controls records (reagents/serological test controls/external proficiency testing) 5 years • Quality assurance 5 years • Antibody identification reports indefinitely • Method revision sheet indefinitely • Donor segments/serum/plasma, clotted and or EDTA sample for 7 days post-transfusion • Computer QA records 3 years • Patient data files indefinitely Policy for Product Recall/Retrival/Lookback. Traceback
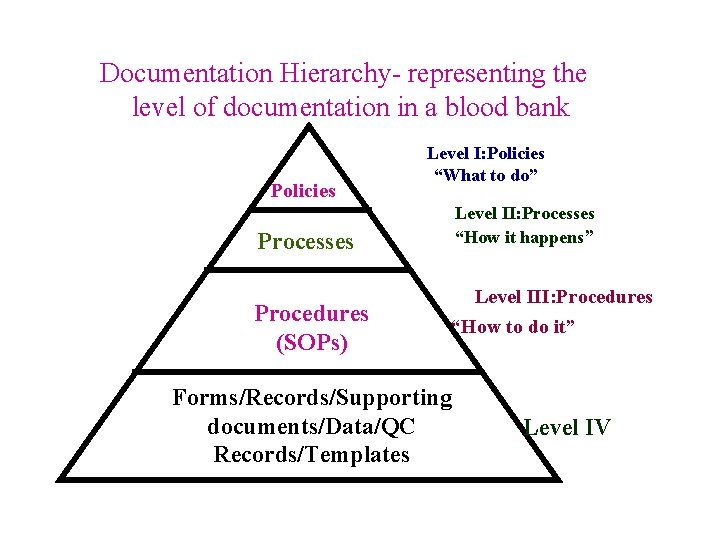
Documentation Hierarchy- representing the level of documentation in a blood bank Policies Level I: Policies “What to do” Level II: Processes “How it happens” Processes Procedures (SOPs) Level III: Procedures “How to do it” Forms/Records/Supporting documents/Data/QC Records/Templates Level IV
Documentation Are the records of incidents, errors, and accidents maintained ?
Types of Clerical Errors • • • Venipuncture of the wrong patient failure to identify patient correctly wrong name placed on sample blood taken to the wrong patient failure to properly identify the patient prior to transfusion
ERRORS ARE USEFUL INFORMATION v WE LEARN MORE FROM OUR FAILURES THAN WE MAY FROM SUCCESS “Give me a fruitful error anytime, full of seeds, bursting with its own corrections. You can keep your sterile truth for yourself” VILFRED PARETO v v CAN IMPROVE OUR PROCESS WHEN STUDIED BENIGN ERROR MAY PREDICT DISASTERS OR BAD OUTCOMES
Basic Blood Components • Red Blood Cells • Platelets • Fresh Frozen Plasma (FFP) • Cryoprecipitate Anti-hemophilic Factor • Granulocytes
BLOOD COMPONNET AND SEPARATION Blood components are packed Red Blood Cells, Platelets, Rich Plasma, Platelet concentrate, Fresh Plasma, Fresh Frozen Plasma, Cryoprecipitate, and Cryosupernant. Double, Triple and Quadruple blood bags are used for producing and separating components in closed system.
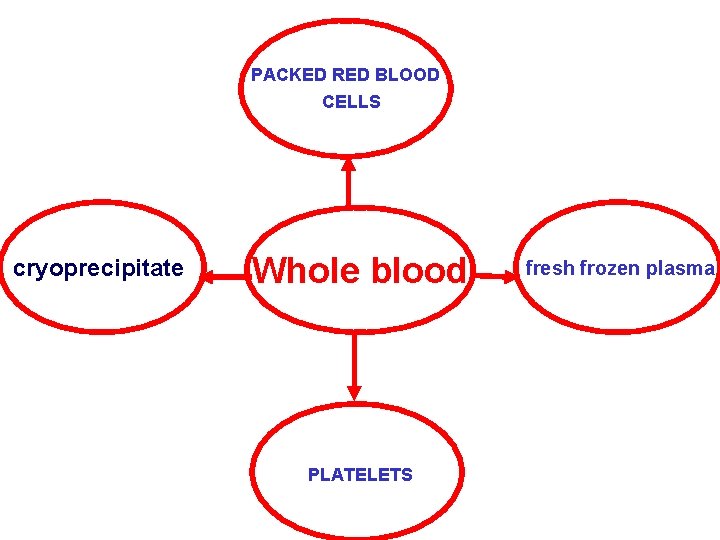
PACKED RED BLOOD CELLS cryoprecipitate Whole blood PLATELETS fresh frozen plasma
Terms to know: • Whole blood: blood collected before separation into components • Components: parts of whole blood that are separated • Closed system: a sterile system of blood collection • Open system: when the collection is exposed to air, decreasing expiration date
Collection basics • • • Blood is collected in a primary bag that contains anticoagulant-preservatives Satellite bags may also be attached, depending on what components are needed Anticoagulant-preservatives minimize biochemical changes and increase shelf life
WHY BLOOD COMPONENTS ? • TO CORRECT SPECIFIC DEFICIENCY • STORAGE CONSIDERATIONS
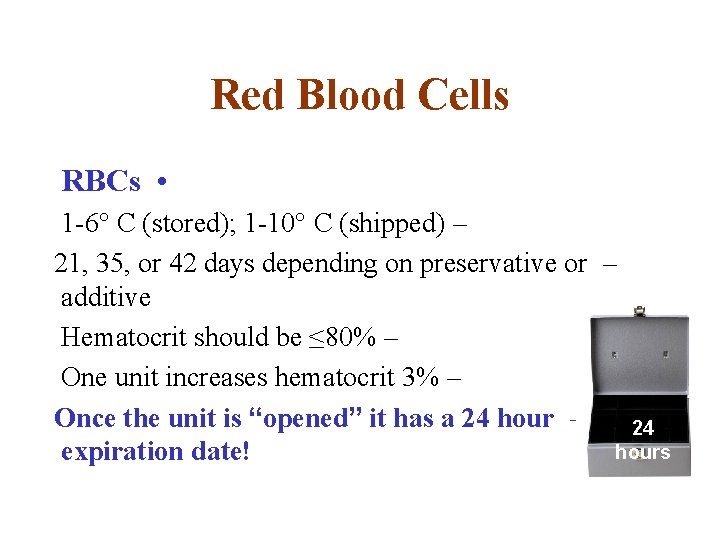
Red Blood Cells RBCs • 1 -6° C (stored); 1 -10° C (shipped) – 21, 35, or 42 days depending on preservative or – additive Hematocrit should be ≤ 80% – One unit increases hematocrit 3% – Once the unit is “opened” it has a 24 hour – 24 hours expiration date!
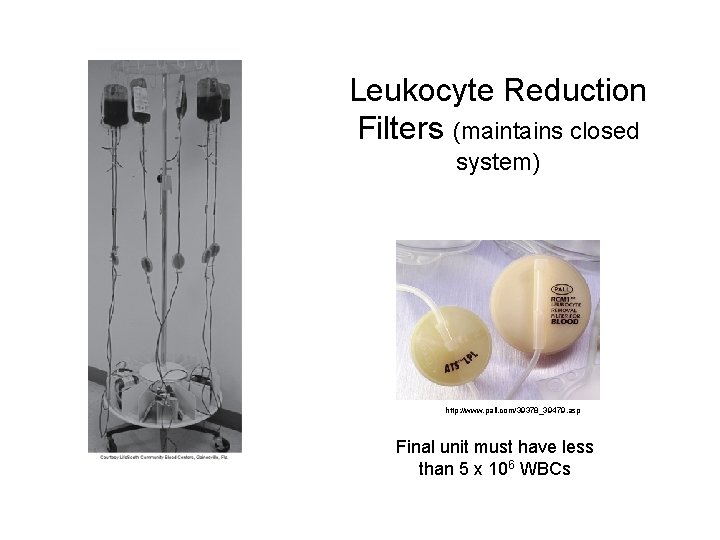
Leukocyte Reduction Filters (maintains closed system) http: //www. pall. com/39378_39479. asp Final unit must have less than 5 x 106 WBCs
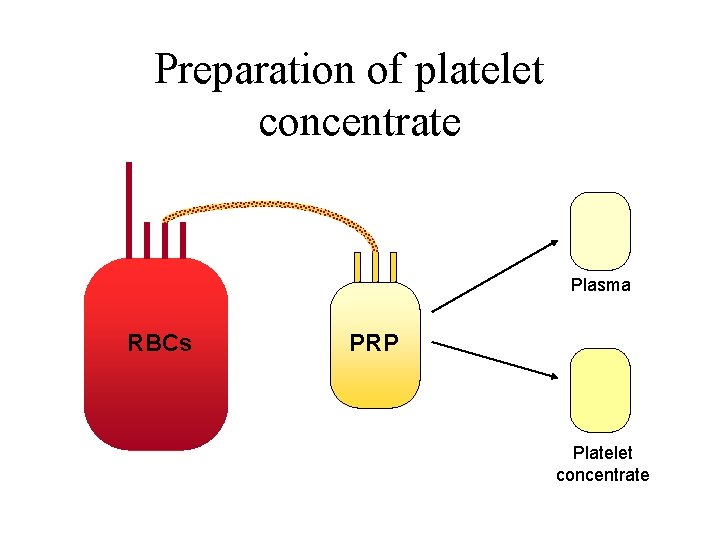
Preparation of platelet concentrate Plasma RBCs PRP Platelet concentrate
How platelets are processed • Requires 2 spins: – Soft – separates RBCs and WBCs from plasma and platelets – Heavy • platelets in platelet rich plasma (PRP) will be forced to the bottom of a satellite bag • 40 -60 m. L of plasma is expelled into another satellite bag, while the remaining bag contains platelet concentrate
Platelets • Important in maintaining hemostasis • Help stop bleeding and form a platelet plug (primary hemostasis) • People who need platelets: – Cancer patients – Bone marrow recipients – Postoperative bleeding
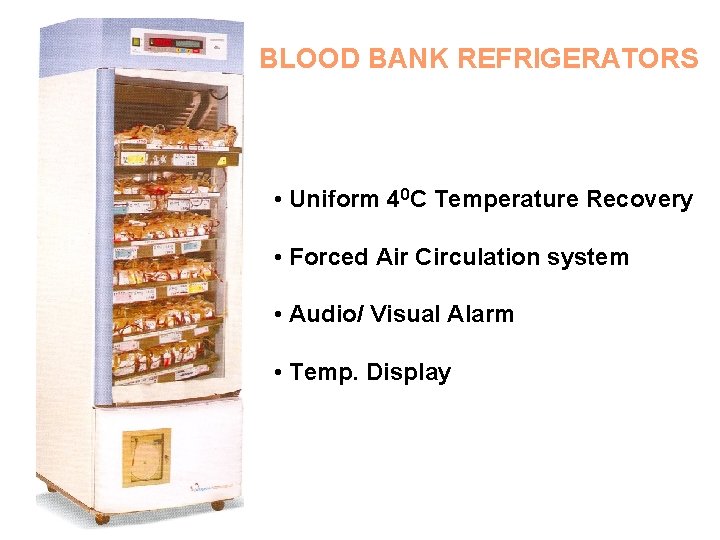
BLOOD BANK REFRIGERATORS • Uniform 40 C Temperature Recovery • Forced Air Circulation system • Audio/ Visual Alarm • Temp. Display
What is Apheresis The process of apheresis involves removal of whole blood from a patient or donor. Within an instrument that is essentially designed as a centrifuge, the components of whole blood are separated. One of the separated portions is then withdrawn and the remaining components are retransfused into the patient or donor
Plasma (plasmapheresis) Platelets (plateletpheresis) Leukocytes (leukapheresis)
Whatever the local system for the collection, screening and processing of blood, clinicians must be familiar with it and understand any limitations that it may impose on the safety or availability of blood.
Getting the right blood to the right patient at the right time
Blood products Key points 1 Safe blood products, used correctly, can be life-saving, However, even where quality standards are very high, transfusion carries some risks. If standards are poor or inconsistent, transfusion may be extremely risky. 2 No blood or blood product should be administered unless all nationally required tests have been carried out. 3 Each unit should be tested and labeled to show its ABO and Rh D group. 4 whole blood can be transfused to replace red cells in acute bleeding when there is also a need to correct hypo volaemia.
5. The preparation of blood components allows a single blood donation to provide treatment for two or three patients and also avoids the transfusion of elements of the whole blood that the patient may not require. Blood components can also be collected by apheresis. 6. Plasma can transmit most of the infections present in whole blood and there are very few indications for its transfusion. 7. Plasma derivatives are made by a pharmaceutical manufacturing process from large volumes of plasma comprising many individual blood donation. Plasma used in the process should be individually tested prior to pooling to minimize the risks of transmitting infection. 8. Factors VIII and IX and immunoglobulins are also made by recombinant DNA technology and are often favoured because there should be no risk of transmitting infectious agents to the patient. However, the costs are high and there have been some reported cases of complications.
Clinical transfusion procedures Key points 1. Every hospital should have standard operating procedures for each stage of the clinical transfusion process. All staff should be trained to follow them. 2. Clear communication and cooperation between clinical and blood bank staff are essential in ensuring the safety of blood issued for transfusion. 3. The blood bank should not issue blood for transfusion unless a blood sample label and blood request form have been correctly completed. The blood request form should include the reason for transfusion so that the most suitable product can be selected for compatibility testing. 4. Blood products should be kept within the correct storage conditions during transportation and in the clinical area before transfusion, in order to prevent loss of function or bacterial contamination.
5. The transfusion of an incompatible blood component is the most common cause of acute transfusion reaction, which may be fatal. The safe administration of blood depends on: § Accurate, unique identification of the patient. §Correct labeling of the blood sample for pre-transfusion testing. §A final identity check of the patient and the blood unit to ensure the administration of the right blood to the right patient. 6. For each unit of blood transfused, the patient should be monitored by a trained member of staff before, during and on completion of the transfusion.
Monitor and record daily blood stock and prevent shortages of specific group. The daily blood and blood component stock is monitored and checked by head of the sections, in case of specific group shortage the following actions is taken: 1. Phone call the donors with needed specific group. 2. Phone call the institute and establishments that held blood campaign 3. Communicate central blood bank society. 4. Call blood collection centers in other government hospitals. 5. Demand patient family to replace needed blood. 6. On top emergencies call the TV. and other media for public announcement.
Do not ever leave the donor during or after donation process until he or she leave the donation hall.
- Slides: 60