Y L 2018 Clinical Practice Guidelines N O








- Slides: 38
Y L 2018 Clinical Practice Guidelines N O E S U L A In-Hospital Management of N O S R Diabetes PE Chapter 16 Janine Malcolm MD FRCPC, Ilana Halperin MD FRCPC, David Miller MD FRCPC, Sarah Moore RN(EC) BSc. N MN, Kara Nerenberg MD FRCPC, Vincent Woo MD FRCPC, Catherine Yu MD FRCPC
Disclaimer All Content contained on this slide deck is the property of Diabetes Canada, its content suppliers or its licensors as the case may be, and is protected by Canadian and international copyright, trademark, and other applicable laws. Diabetes Canada grants personal, limited, revocable, non-transferable and non-exclusive license to access and read content in this slide deck for personal, non-commercial and not-for-profit use only. The slide deck is made available for lawful, personal use only and not for commercial use. The unauthorized reproduction, distribution of this copyrighted work is not permitted. For permission to use this slide deck for commercial or any use other than personal, please contact guidelines@diabetes. ca
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Changes 2018 • New recommendations for: • screening hospitalized patients with newly diagnosed hyperglycemia, diabetes risk factors, or pre-existing Y L N diabetes with A 1 C O ECBG monitoring • frequency and timing of bedside S U L • use of IV insulin infusion. Afor perioperative management NCABG to prevent surgical site of patients undergoing O S R infections E P • post-operative protocols using basal/bolus therapy in patients with diabetes requiring insulin therapy • New glycemic targets for various categories of inhospital people with diabetes CBG, capillary blood glucose monitoring; IV, intravenous PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes In-hospital Management Checklist üCHECK A 1 C if it has not been done in the last 3 months Y L üCONTINUE pre-hospital diabetes regimen if appropriate, N O E otherwise … S U L A of choice N üUSE insulin as the treatment O S R E üDO NOT use sliding scale insulin alone P üDO use BASAL + BOLUS + CORRECTION insulin regimen üAVOID hypoglycemia PERSONAL USE ONLY
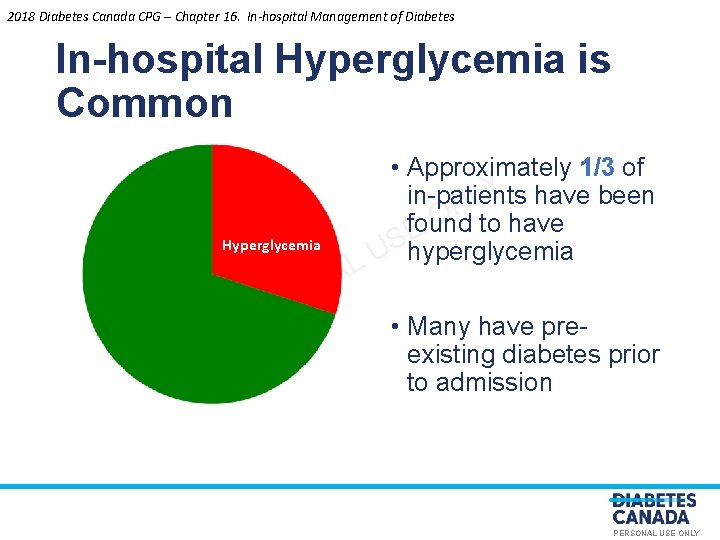
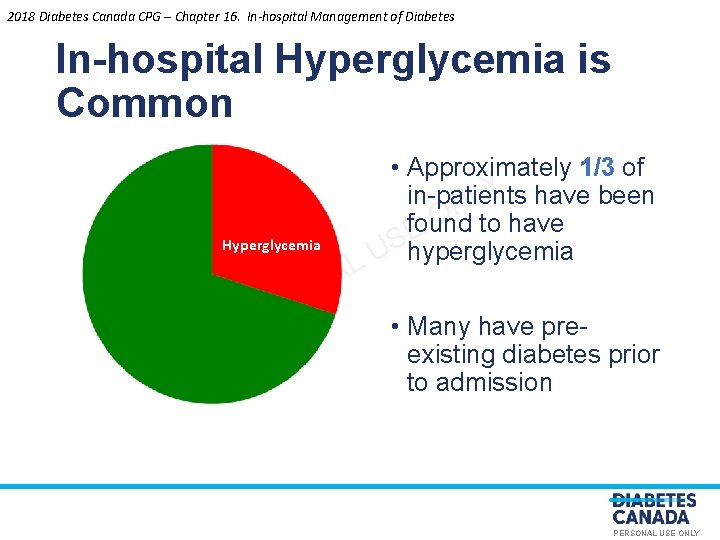
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes In-hospital Hyperglycemia is Common Hyperglycemia O S R E P L A N • Approximately 1/3 of Y have been in-patients L N O found to have E UShyperglycemia • Many have preexisting diabetes prior to admission PERSONAL USE ONLY
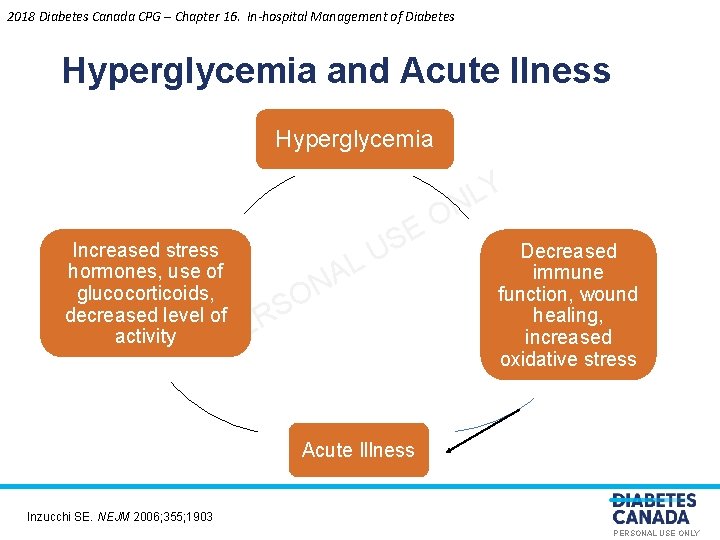
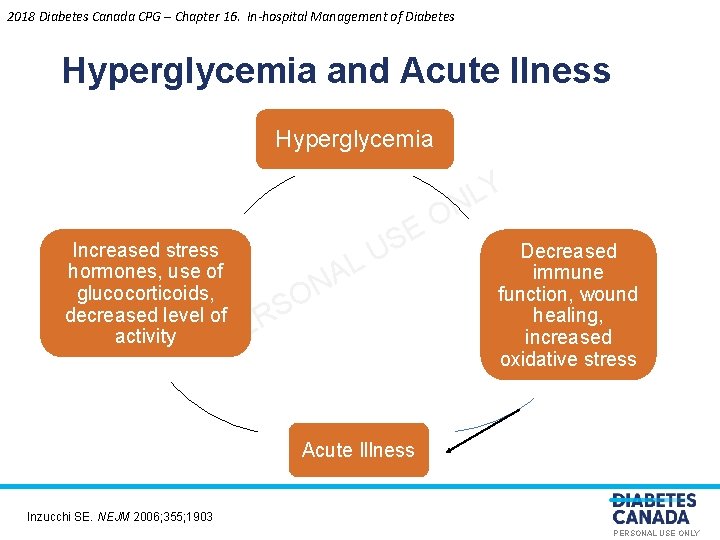
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Hyperglycemia and Acute Ilness Hyperglycemia Increased stress L hormones, use of A N glucocorticoids, O S decreased level of R activity PE O E US Y L N Decreased immune function, wound healing, increased oxidative stress Acute Illness Inzucchi SE. NEJM 2006; 355; 1903 PERSONAL USE ONLY
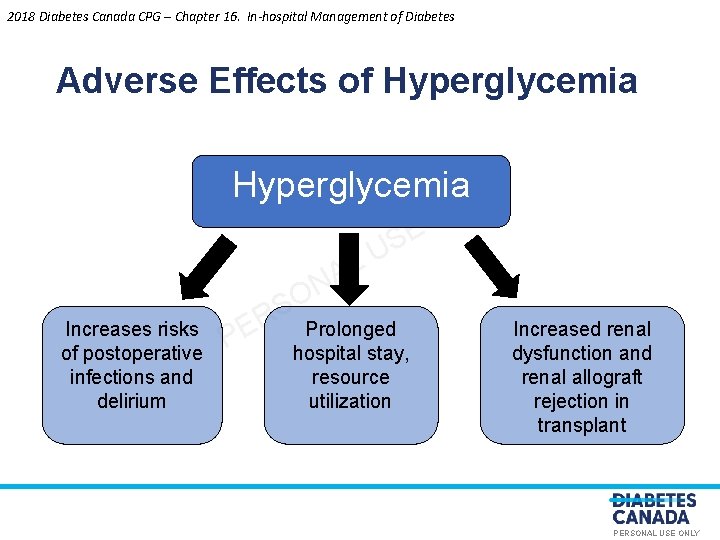
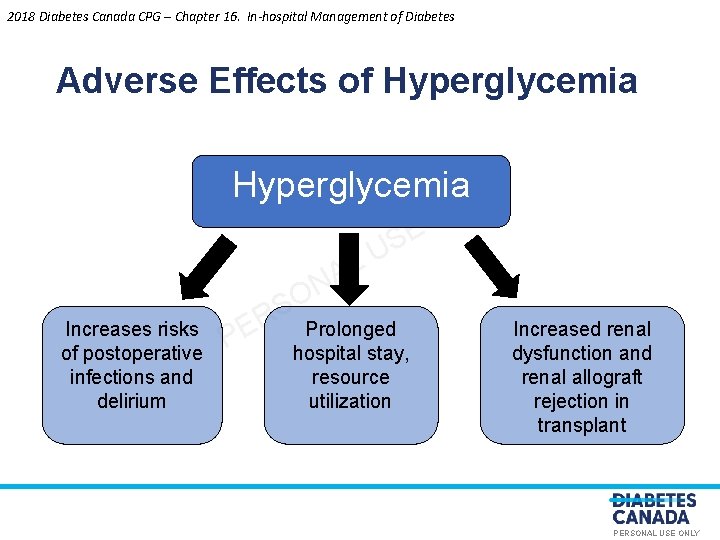
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Adverse Effects of Hyperglycemia LY N O E S U L A N O Increases risks of postoperative infections and delirium S R PE Prolonged hospital stay, resource utilization Increased renal dysfunction and renal allograft rejection in transplant PERSONAL USE ONLY
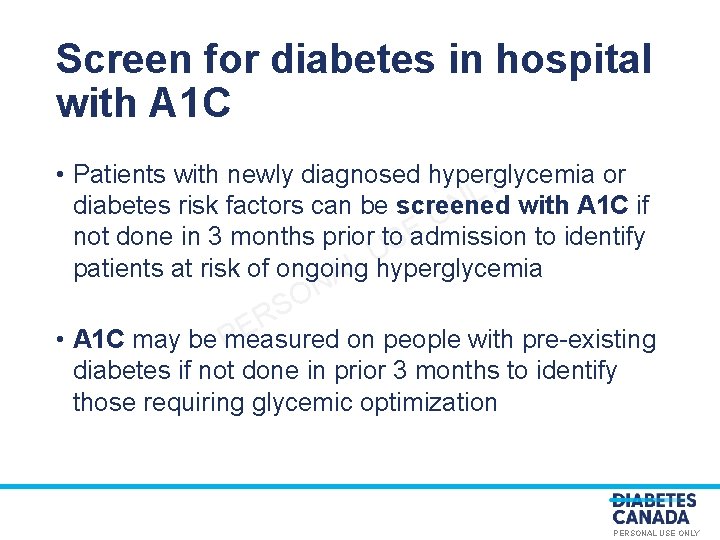
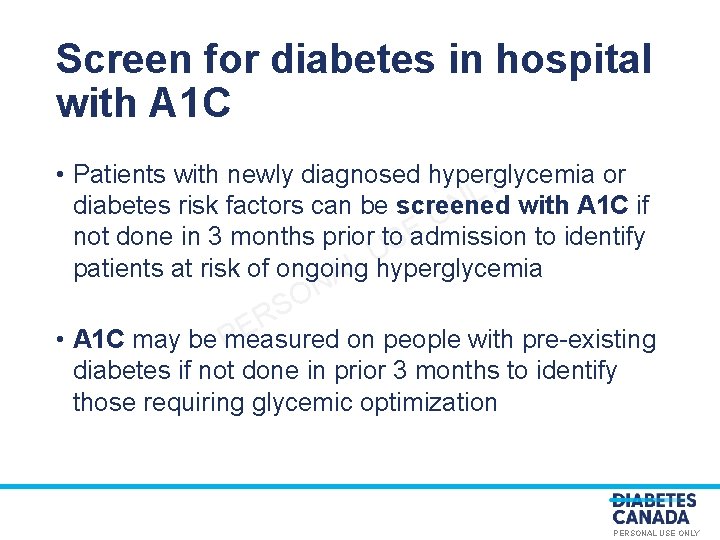
Screen for diabetes in hospital with A 1 C • Patients with newly diagnosed hyperglycemia or Y L diabetes risk factors can be screened N with A 1 C if O not done in 3 months prior to. SE admission to identify U L patients at risk of ongoing A hyperglycemia N O S R E • A 1 C may be measured on people with pre-existing P diabetes if not done in prior 3 months to identify those requiring glycemic optimization PERSONAL USE ONLY
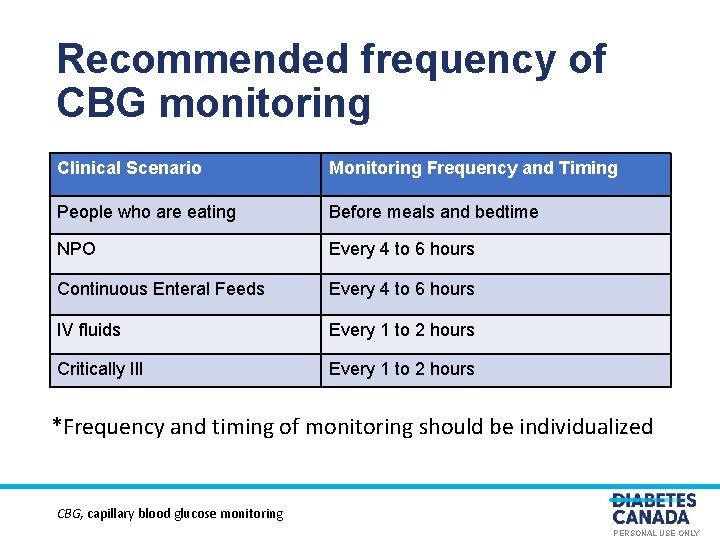
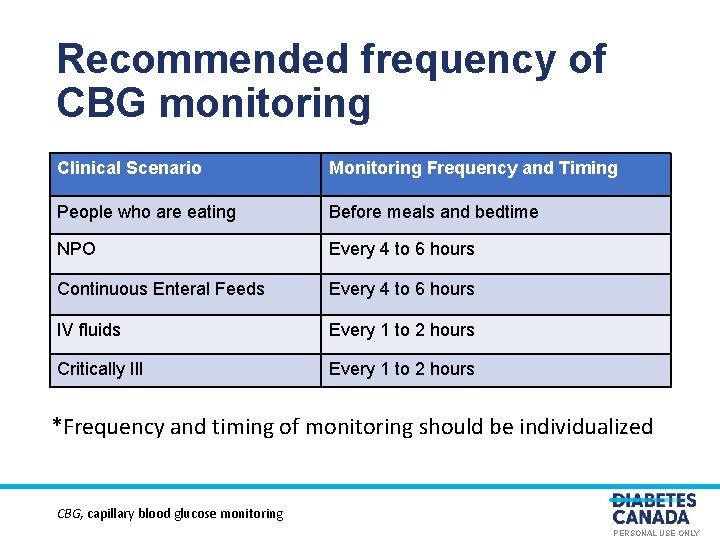
Recommended frequency of CBG monitoring Clinical Scenario Monitoring Frequency and Timing People who are eating Y L N bedtime Before meals and O E Every. U 4 S to 6 hours L A ONEvery 4 to 6 hours NPO Continuous Enteral Feeds IV fluids S R PE Critically Ill Every 1 to 2 hours *Frequency and timing of monitoring should be individualized CBG, capillary blood glucose monitoring PERSONAL USE ONLY
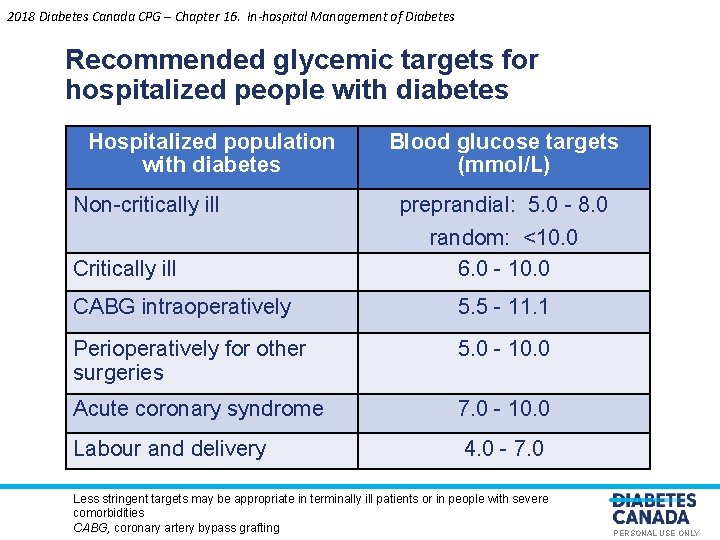
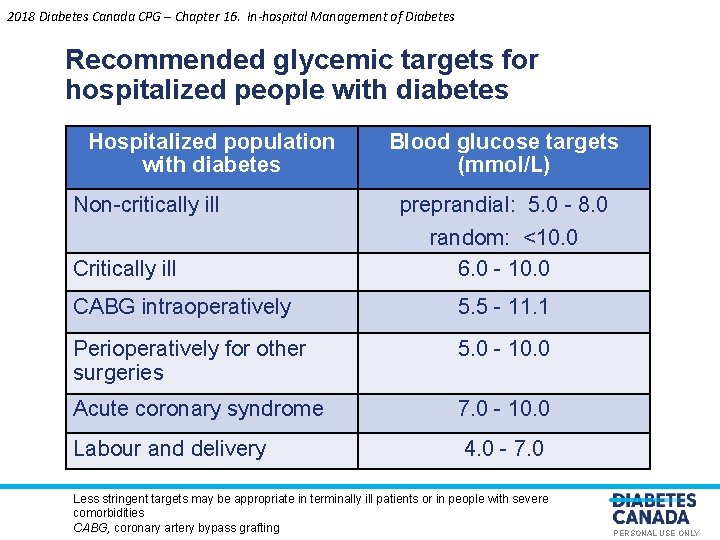
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommended glycemic targets for hospitalized people with diabetes Hospitalized population with diabetes Blood glucose targets (mmol/L) Non-critically ill Y L preprandial: 5. 0 - 8. 0 N O SE random: <10. 0 Critically ill N O CABG intraoperatively S R E P Perioperatively for other surgeries U L A 6. 0 - 10. 0 5. 5 - 11. 1 5. 0 - 10. 0 Acute coronary syndrome 7. 0 - 10. 0 Labour and delivery 4. 0 - 7. 0 Less stringent targets may be appropriate in terminally ill patients or in people with severe comorbidities CABG, coronary artery bypass grafting PERSONAL USE ONLY
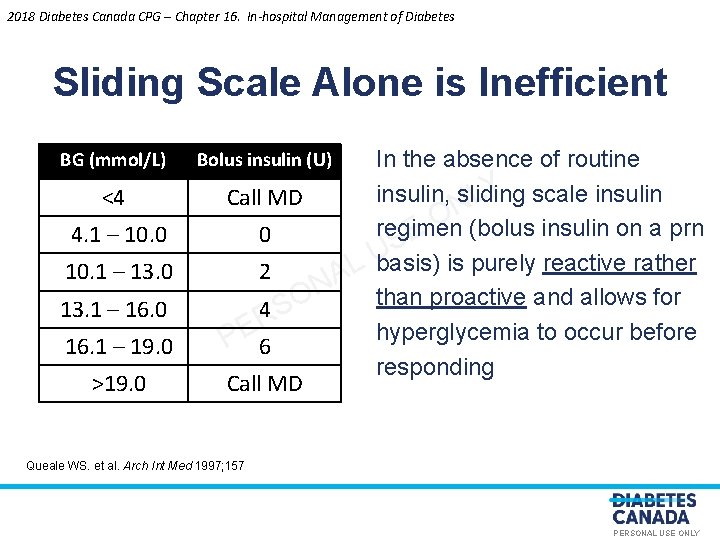
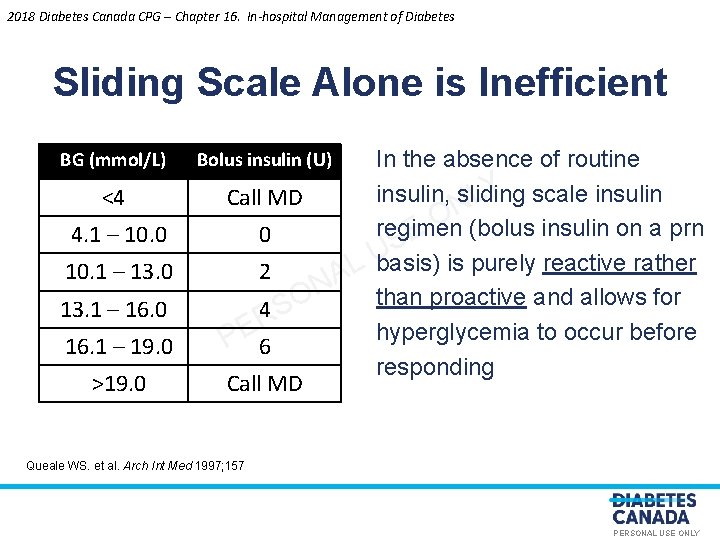
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Sliding Scale Alone is Inefficient BG (mmol/L) Bolus insulin (U) <4 Call MD 4. 1 – 10. 0 0 10. 1 – 13. 0 2 16. 1 – 19. 0 O S R E P >19. 0 Call MD L A N 13. 1 – 16. 0 4 6 In the absence of routine Y scale insulin, sliding L N O regimen E (bolus insulin on a prn S U basis) is purely reactive rather than proactive and allows for hyperglycemia to occur before responding Queale WS. et al. Arch Int Med 1997; 157 PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Sliding Scale Insulin Alone Results in Variable Glucose Control BG (mmol/L) 16. 5 What do you do? +6 U 14. 0 +4 U O E Y L N S U L 10. 0 A N O S R PE 6. 0 4. 0 What do you do? 0 U 0 U Breakfast Lunch Dinner Sliding Scale alone BG (mmol/L) Bolus insulin (U) <4 Call MD 4. 1 – 10. 0 0 10. 1 – 13. 0 2 13. 1 – 16. 0 4 16. 1 – 19. 0 6 > 19. 0 Call MD 3. 0 Bedtime Bolus insulin QID, four times daily; SSI, sliding-scale insulin; BG, blood glucose PERSONAL USE ONLY
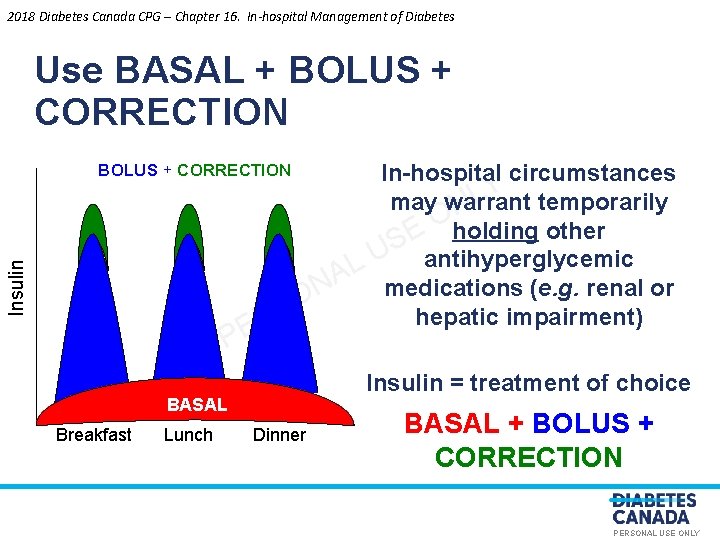
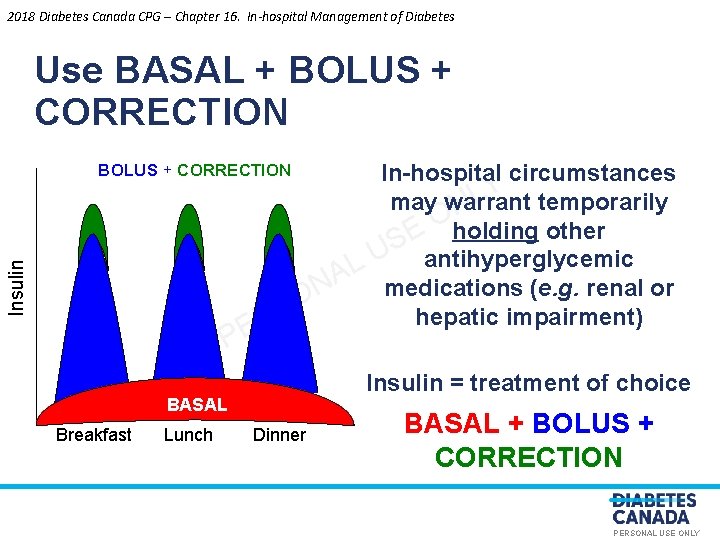
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Use BASAL + BOLUS + CORRECTION Insulin L A N O S R E P Insulin = treatment of choice BASAL Breakfast Lunch In-hospital circumstances Y temporarily L may warrant N O E holding other S U antihyperglycemic medications (e. g. renal or hepatic impairment) Dinner BASAL + BOLUS + CORRECTION PERSONAL USE ONLY
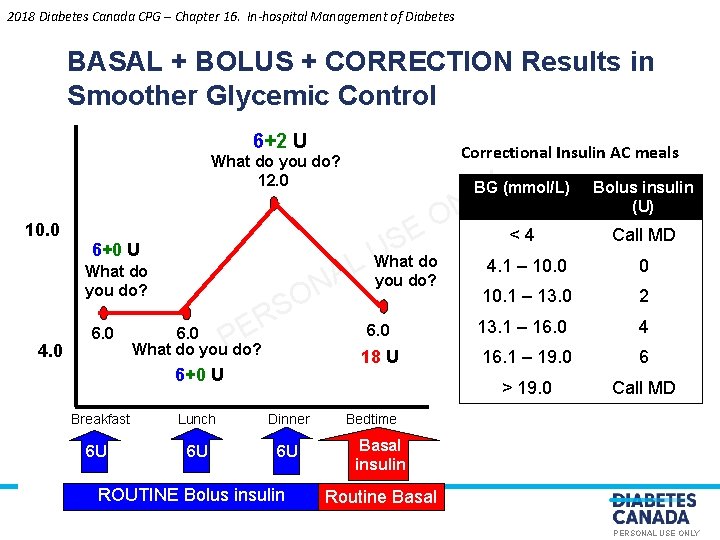
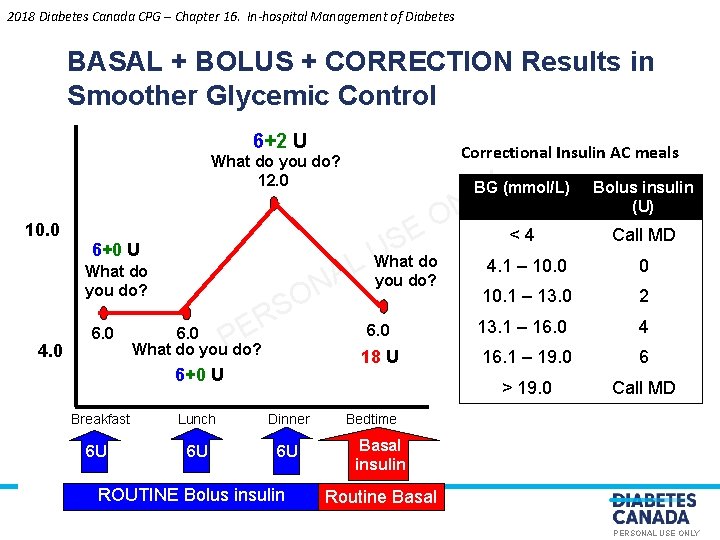
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes BASAL + BOLUS + CORRECTION Results in Smoother Glycemic Control 6+2 U Correctional Insulin AC meals What do you do? 12. 0 10. 0 O E 6+0 U What do you do? 4. 0 6. 0 R E P N O S 6. 0 What do you do? 6+0 U Breakfast 6 U Lunch Dinner 6 U 6 U ROUTINE Bolus insulin US What do L A you do? 6. 0 18 U BG Y(mmol/L) L N Bolus insulin (U) <4 Call MD 4. 1 – 10. 0 0 10. 1 – 13. 0 2 13. 1 – 16. 0 4 16. 1 – 19. 0 6 > 19. 0 Call MD Bedtime Basal insulin Routine Basal PERSONAL USE ONLY
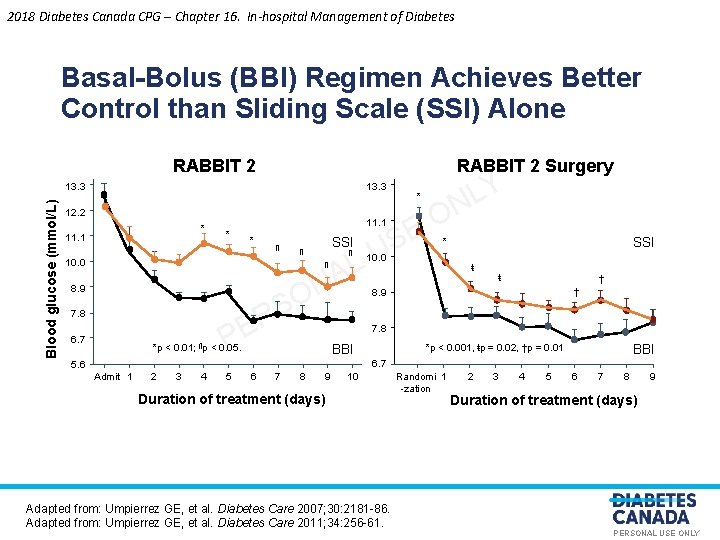
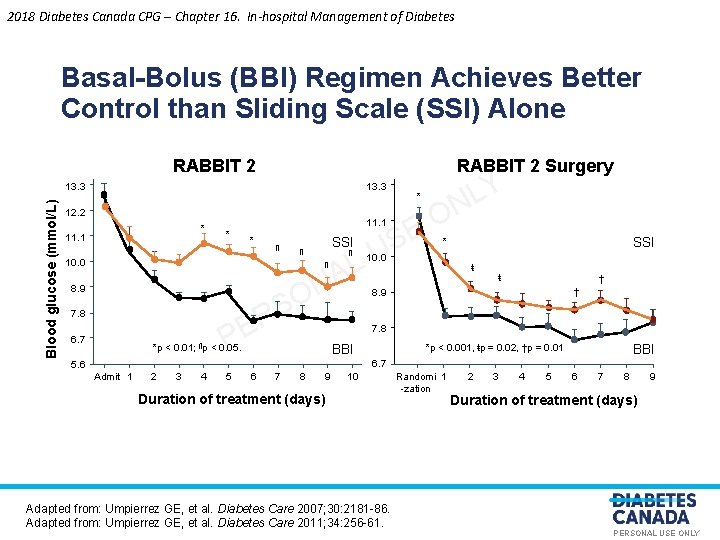
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Basal-Bolus (BBI) Regimen Achieves Better Control than Sliding Scale (SSI) Alone RABBIT 2 Surgery Blood glucose (mmol/L) 13. 3 12. 2 * 11. 1 * * ¶ SSI ¶ 10. 0 ¶ 8. 9 R E P 7. 8 6. 7 AL ¶ N O S *p < 0. 01; ¶p < 0. 05. * O E US Y L N SSI * 10. 0 ŧ ŧ † † 8. 9 7. 8 *p < 0. 001, ŧp = 0. 02, †p = 0. 01 BBI 6. 7 5. 6 Admit 1 2 3 4 5 6 7 8 9 10 Duration of treatment (days) Adapted from: Umpierrez GE, et al. Diabetes Care 2007; 30: 2181 -86. Adapted from: Umpierrez GE, et al. Diabetes Care 2011; 34: 256 -61. Randomi 1 -zation 2 3 4 5 6 7 8 9 Duration of treatment (days) PERSONAL USE ONLY
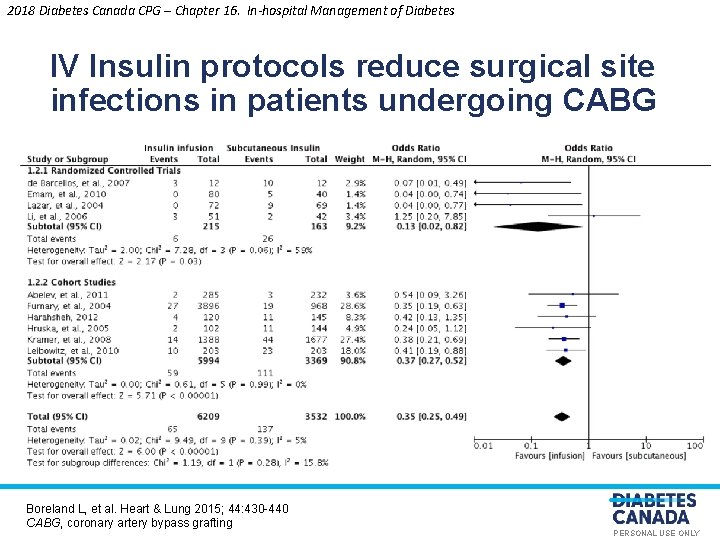
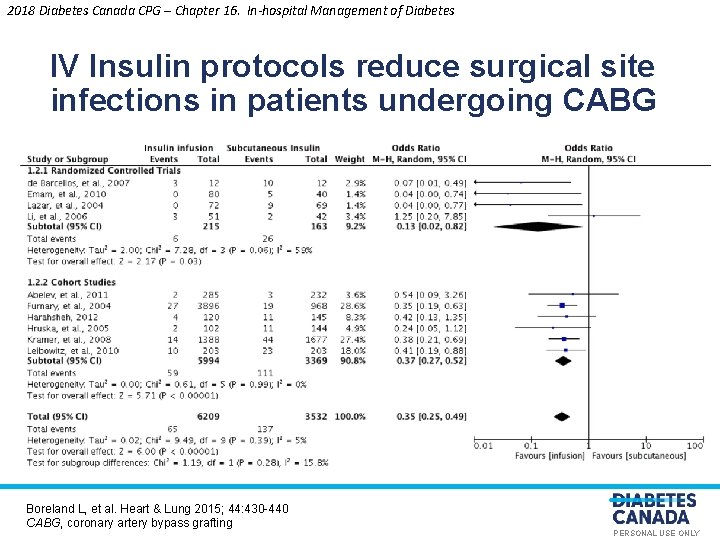
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes IV Insulin protocols reduce surgical site infections in patients undergoing CABG O E Y L N S U L A N O S R PE Boreland L, et al. Heart & Lung 2015; 44: 430 -440 CABG, coronary artery bypass grafting PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Avoid Hypoglycemia • Protocols for hypoglycemia avoidance, recognition and management should be implemented. Ywith nursing. L N initiated treatment O E S U • Patients at risk of hypoglycemia should have ready L A N access to an appropriate source of glucose at all times O S R • Insulin protocols PE and order sets may be used to improve adherence to optimal insulin use and glycemic control PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Organization of Care • Institution wide programs with the following Yin in-hospital elements can result in improvements L N O glycemic control: E S Ubased care • Inter-professional team L A N O • Health-care professional development focused S R E on in-hospital P diabetes management • Algorithms, order sets and decision support • Comprehensive quality assurance initiatives PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 1 1. 2018 An A 1 C should be measured if not done in the 3 months prior to admission on: • All hospitalized people with a history of diabetes to identify Y L N optimization individuals that would benefit from glycemic [Grade D, Consensus] • • O E S U All hospitalized people with. L newly diagnosed Awith diabetes risk factors to hyperglycemia or those N Orisk for ongoing dysglycemia [Grade C, identify individuals. Sat R Level 3] E P Repeat screening should be performed 6 to 8 weeks post hospital discharge for individuals with an A 1 C 6. 0%-6. 4% [Grade D, Consensus] • In-hospital CBG monitoring should be initiated for individuals with an A 1 C ≥ 6. 5% [Grade D, Consensus] CBG, capillary blood glucose monitoring PERSONAL USE ONLY
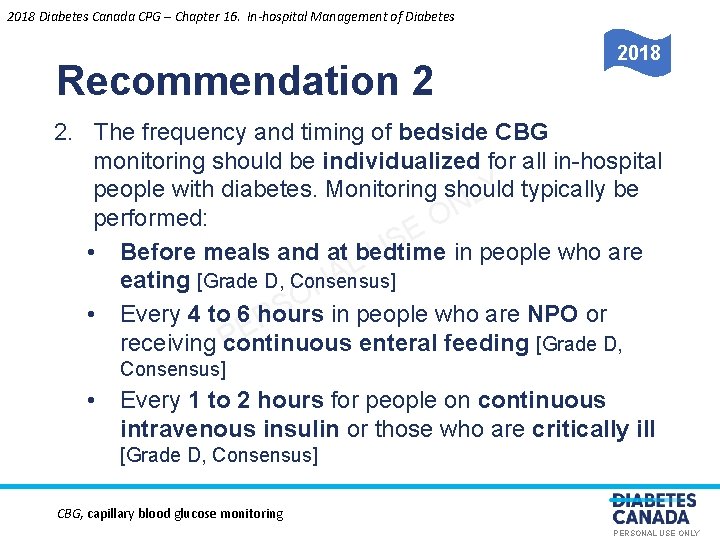
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 2 2018 2. The frequency and timing of bedside CBG monitoring should be individualized for all in-hospital Y typically be people with diabetes. Monitoring should L N performed: O E S • Before meals and at bedtime in people who are U L A eating [Grade D, Consensus] N O S in people who are NPO or • Every 4 to 6 hours R PE receiving continuous enteral feeding [Grade D, Consensus] • Every 1 to 2 hours for people on continuous intravenous insulin or those who are critically ill [Grade D, Consensus] CBG, capillary blood glucose monitoring PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 3 3. Provided that their medical conditions, dietary intake Y with diabetes and glycemic control are stable, people L N O should be maintained on their pre-hospitalization E S non-insulin antihyperglycemic agents or insulin U L A regimens [Grade D, Consensus] N O S R E P PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 4 4. For hospitalized people with diabetes treated with Y basal, insulin, a proactive approach that includes L N insulin, O bolus and correction (supplemental) E S along with pattern management, should be used to U L improve glycemic control, A reduce adverse events and N O instead of only correcting high BG with short- or rapid S R A, Level 1 A] E -acting insulin [Grade P BG, blood glucose PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 5 5. For the majority of non-critically ill hospitalized Ytargets should people with diabetes, preprandial BG L N with random BG O be 5. 0 to 8. 0 mmol/L in conjunction E S values <10. 0 mmol/L, as U long as these targets can LD, Consensus] A be safely achieved [Grade N O S R E P BG, blood glucose PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 6 6. For most medical/surgical critically ill hospitalized Y a people with diabetes with hyperglycemia, L N O continuous intravenous insulin infusion should be E S used to maintain BG <10. 0 Ummol/L [Grade B, Level 2] L A and >6. 0 mmol/L [Grade N D, Consensus] O S R E P BG, blood glucose PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 7 2018 7. For people with diabetes undergoing CABG, a Y targeting continuous IV insulin infusion protocol L N O intraoperative glycemic levels between 5. 5 and 11. 1 E S than subcutaneous mmol/L should be used, rather U L A insulin, to prevent postoperative infections [Grade A, N Level 1 A] O S R E P CABG, coronary artery bypass grafting PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 8 2018 8. In hospitalized people with diabetes requiring insulin Y with/without therapy, protocols using basal insulin L N bolus insulin should be used for. Opostoperative E S glycemic management [Grade U B, Level 2] L A N O S R E P PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 9 9. In hospitalized people with diabetes, hypoglycemia should be minimized. Protocols for hypoglycemia Y should be L avoidance, recognition and management N O implemented with nurse-initiated E treatment, S U hypoglycemia when including glucagon for severe L A readily available [Grade D, intravenous access. Ois. Nnot S Consensus]. Hospitalized people with diabetes at risk R E P should have ready access to an of hypoglycemia appropriate source of glucose (oral or IV) at all times, particularly when NPO or during diagnostic procedures [Grade D, Consensus] PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Recommendation 10 2018 10. Programs consisting of the following elements should be implemented for optimal inpatient diabetes care: • • • Y Interprofessional team-based approach [Grade B, Level 2] L N regarding in-hospital O Health-care professional development E diabetes management [Grade D, S Level 4] U L Algorithms, order sets. A and decision support [Grade C, Level 3] • N O S Rquality assurance initiatives including Comprehensive E P BG monitoring systems, inpatient education, institution-wide and transition/continuity of care and discharge planning [Grade D, Consensus] BG, blood glucose PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages • Hyperglycemia is common in hospitalized people, Y even among those without a previous Lhistory of N O diabetes, and is associated with increased in-hospital E complications, longer length USof stay, and mortality L A N O S R E P PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages • Insulin is the most appropriate pharmacologic agent for effectively controlling glycemia in hospital. Y L N O • A proactive approach to glycemic E management using S Ucorrection scheduled basal, bolus and L A the preferred method. (supplemental) insulin is N O S R PE • The use of correction (supplemental) only insulin, which treats hyperglycemia only after it has occurred, should be discouraged as the sole modality for treating elevated blood glucose levels. PERSONAL USE ONLY

2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages • Glycemic targets for the majority of non-critically ill hospitalized people with diabetes are: • preprandial 5. 0 to 8. 0 mmol/L, in conjunction with Y Las these targets N random BG <10. 0 mmol/L, as long O can be safely achieved. SE U L A N O • For critically ill hospitalized people with diabetes, BG S R levels should be. PE maintained between 6. 0 and 10. 0 mmol/L BG, blood glucose PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages • Hypoglycemia is a major barrier to achieving targeted glycemic control in the hospital setting. LY N O • Health-care institutions should develop protocols for E S U of hypoglycemia the assessment and treatment L A N O S R E P PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages for People with Diabetes • If your admission to hospital is planned, talk with your healthcare providers in order to develop Yan in-hospital L N diabetes care plan that addresses O issues: E S • who will manage your diabetes in the hospital; U L NA • will you be able to. O self-manage your diabetes; S R • what adjustments to your diabetes medications or E P insulin doses may be necessary before and after medical procedures or surgery; and • if you use an insulin pump, are hospital staff familiar with pump therapy PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages for People with Diabetes Y in hospital than • Your blood glucose levels may be higher L ON of factors, your usual target range due to a. Evariety S medications, medical including the stress of your illness, U L A procedures and infections N O S R E P • Your diabetes medications may need to be changed during your hospital stay to manage the changes in blood glucose, or if medical conditions develop that make some medications no longer safe to use PERSONAL USE ONLY
2018 Diabetes Canada CPG – Chapter 16. In-hospital Management of Diabetes Key Messages for People with Diabetes • When you are discharged, make sure that you Y L have written instructions about: N O E S • changes in your dosage of medications or U L new medications or insulin injections N or. Aany O S treatments; R E P • how often to check your blood glucose; and • who to contact if you have difficulty managing your blood glucose levels PERSONAL USE ONLY

Visit guidelines. diabetes. ca O E Y L N S U L A N O S R PE PERSONAL USE ONLY
Or download the App O E Y L N S U L A N O S R PE PERSONAL USE ONLY
Diabetes Canada Clinical Practice Guidelines Y L http: //guidelines. diabetes. ca – for health-care N O providers E S U L A N O 1 -800 -BANTING (226 -8464) S R E P http: //diabetes. ca – for people with diabetes PERSONAL USE ONLY