ACUTE STROKE CARE FOR THE EMS PROVIDER Julie








- Slides: 67
ACUTE STROKE CARE FOR THE EMS PROVIDER Julie Berdis-RN, BSN, CNRN, Stroke Coordinator Providence Sacred Heart Medical Center Spokane, Washington
Disclosures § § § No financial disclosures Will be discussing off-label uses Always follow your local and regional protocols
Objectives n n n n Review the impact of stroke Recognize signs and symptoms of stroke Define risk factors for stroke Identify types of stroke Learn Pre-hospital recommendations for Dispatch Review stroke care in the field Review medical management and treatment options for stroke Review national/regional guidelines and recommendations for stroke
Key Points n n EMS play a critical role in the Emergency care of acute stroke patients. Over 400, 000 acute stroke patients are being transported annually by EMS providers. 50% of all stroke patients use EMS, but this is the majority of patients who present within the 3 hour treatment window EMS use decreases time to hospital arrival and the ability to implement acute stroke intervention.

The Impact of Stroke n n n n 795, 000 strokes in 2009 163, 000 die from stroke every year in America Stroke is the third leading cause of death Stroke is the leading cause of disability in adults 4. 4 million survivors; only 50 -75% of stroke survivors regain functional independence Estimated direct/indirect costs for 2007 - $62. 7 billion 14% of persons who survive a first stroke or TIA will have another within one year
Time is Brain! n n n Every second 32, 000 neurons die Every minute 1. 9 million neurons die Every hour 120 million neurons die Completed stroke: Loss of 1. 2 billion neurons Blockage of one blood vessel will cause ischemia within 5 minutes
What is our goal? Reduce stroke mortality v Improve quality of life for stroke survivors and their families v Focus: n Increasing public awareness n Timely initiation of 911 system n Deployment of informed EMS personnel n Delivery to a stroke center

Did You Know? n The average time from symptom onset to the ED is 17 -22 hours. n 42% of people over 50 do not recognize signs and symptoms of stroke n 17% of people over 50 can’t name a single stroke symptom n Only 38% call 9 -1 -1 Only 20 -25% arrive within 3 hours n
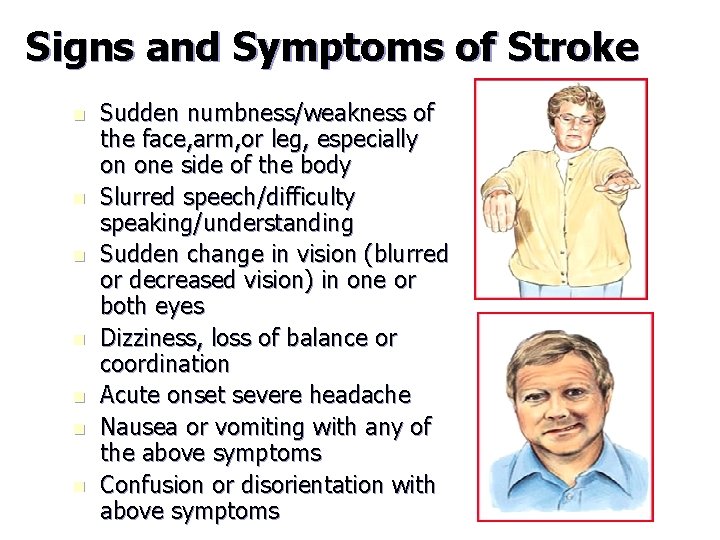
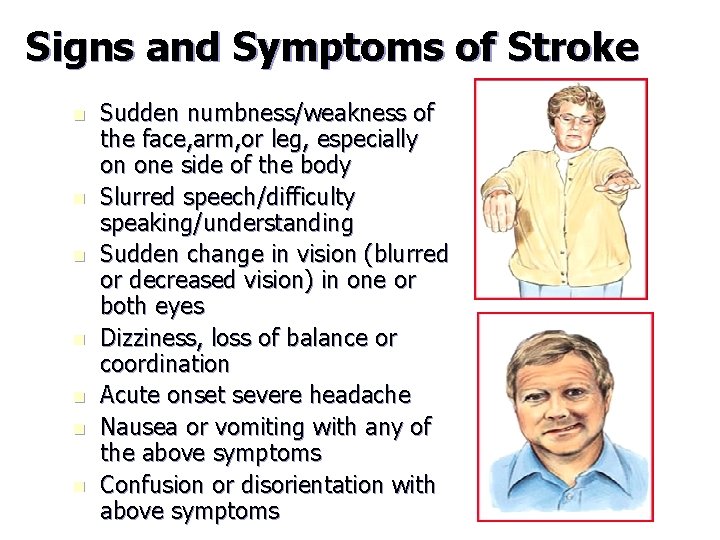
Signs and Symptoms of Stroke n n n n Sudden numbness/weakness of the face, arm, or leg, especially on one side of the body Slurred speech/difficulty speaking/understanding Sudden change in vision (blurred or decreased vision) in one or both eyes Dizziness, loss of balance or coordination Acute onset severe headache Nausea or vomiting with any of the above symptoms Confusion or disorientation with above symptoms
Additional stroke symptoms Decrease level of consciousness n Difficulty with swallowing and secretions n Respiratory distress n Pupil changes n Convulsions n
Modifiable Risk Factors n n n Hypertension Elevated cholesterol (statins reduce risk by 30%) Diabetes mellitus-independent risk factor Coronary Artery disease Heart disease-Valve disease/replacement, any factor that decreases ventricular contraction Atrial Fibrillation (3 -4 x risk) Previous stroke Obesity Excessive alcohol Smoking (2 x risk ischemic; 4 x risk hemorrhagic) Oral Contraceptives/HRT

Non-Modifiable Risk Factors n n n Age-Risk doubles per decade over 55 Gender-Men have greater risk, but women live longer. More women die from stroke (60% of stroke deaths) Race-African-American, Asian and Hispanic have greater risk, possibly due to hypertension Diabetes Mellitus- Exacerbated by hypertension or poor glucose control. Even diabetics with good control are at increased risk. Family history of stroke or TIA
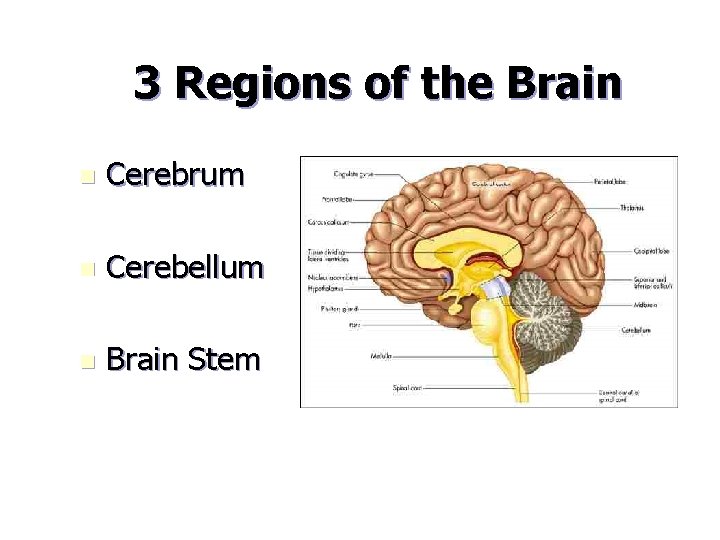
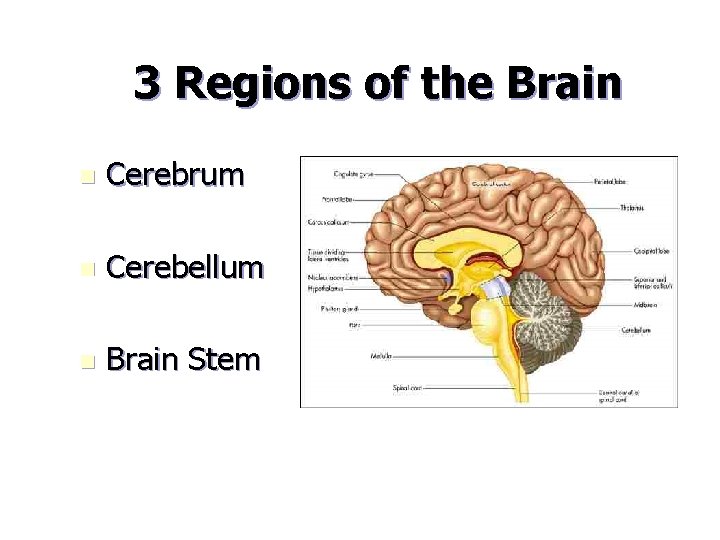
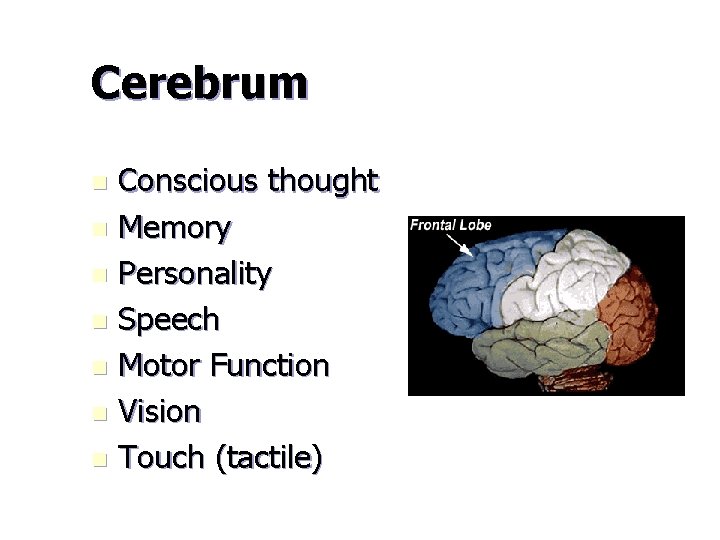
3 Regions of the Brain n Cerebrum n Cerebellum n Brain Stem
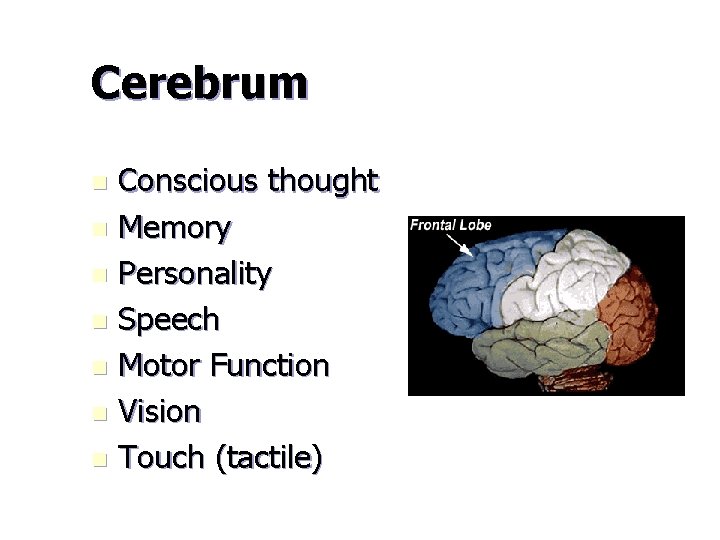
Cerebrum Conscious thought n Memory n Personality n Speech n Motor Function n Vision n Touch (tactile) n
Cerebellum Coordination n Balance n Fine motor control n Reflexes n Symptoms: dizziness, nausea, vomiting
Brain Stem n n Heart function Respiration Autonomic nervous system Digestion Symptoms: Involuntary life-support functions (breathing, heartbeat, blood pressure), eye movement, hearing, speech, swallow, mobility on one or both sides of the body
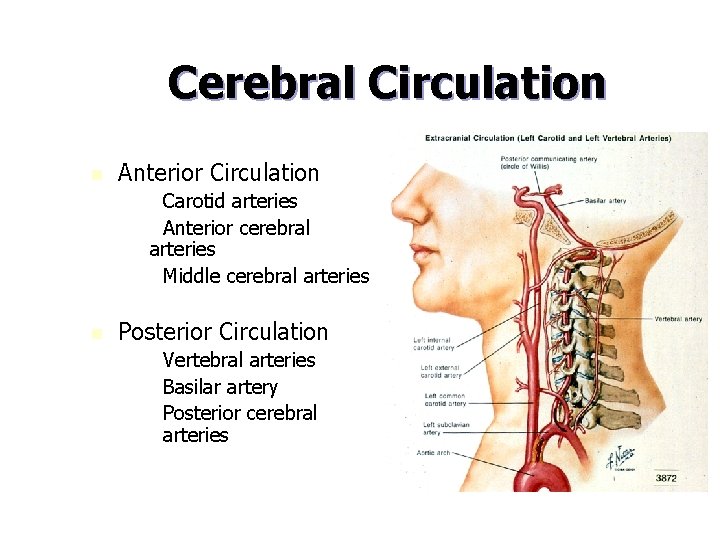
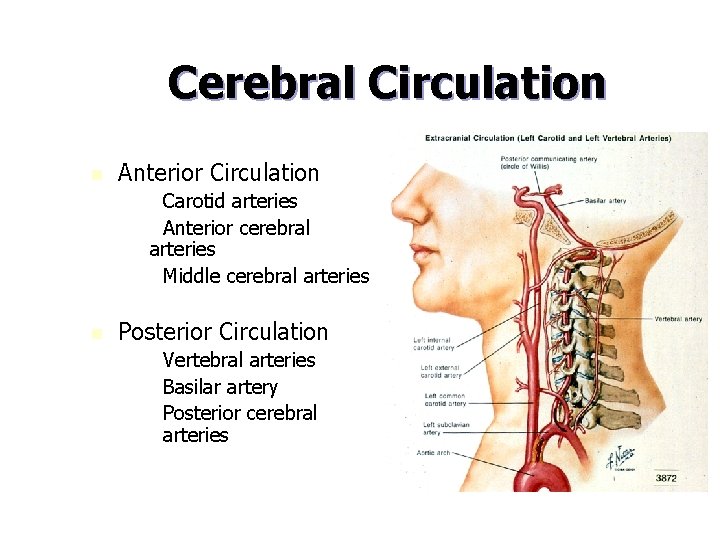
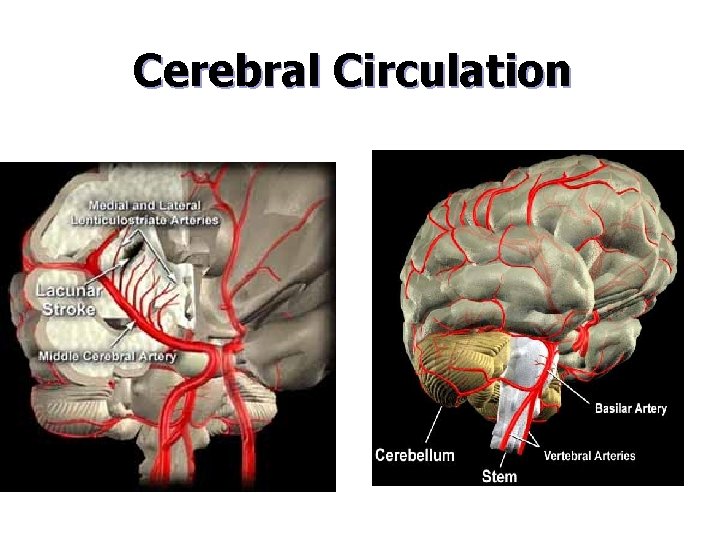
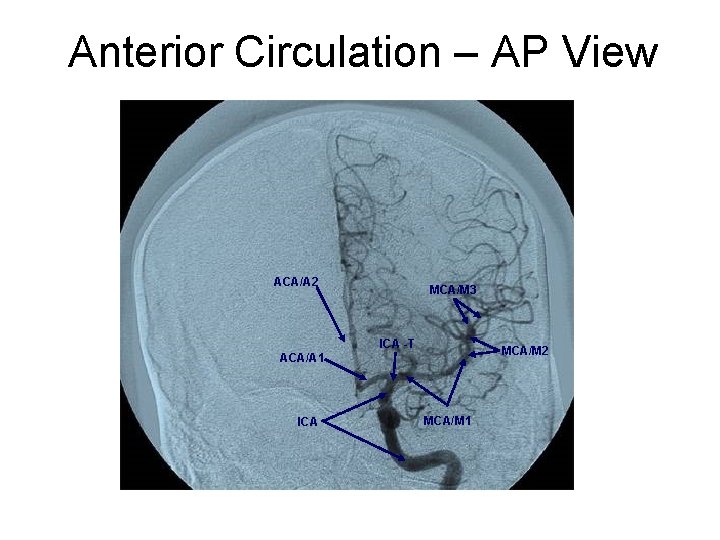
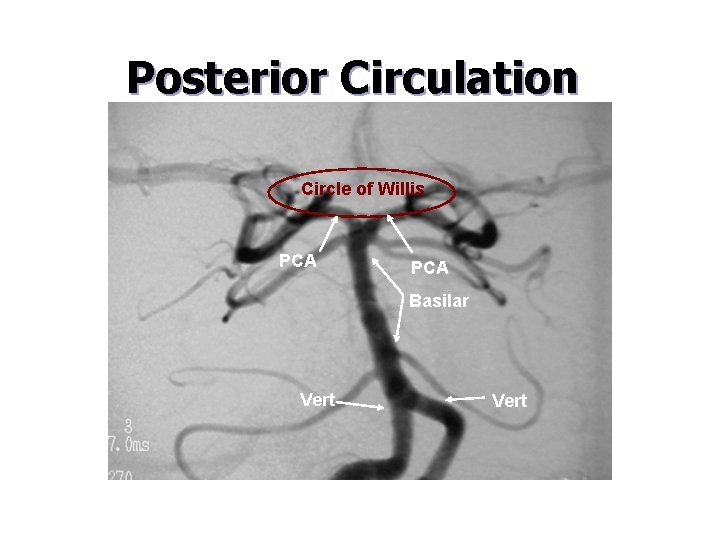
Cerebral Circulation n Anterior Circulation – – Carotid arteries Anterior cerebral arteries – Middle cerebral arteries n Posterior Circulation – – – Vertebral arteries Basilar artery Posterior cerebral arteries
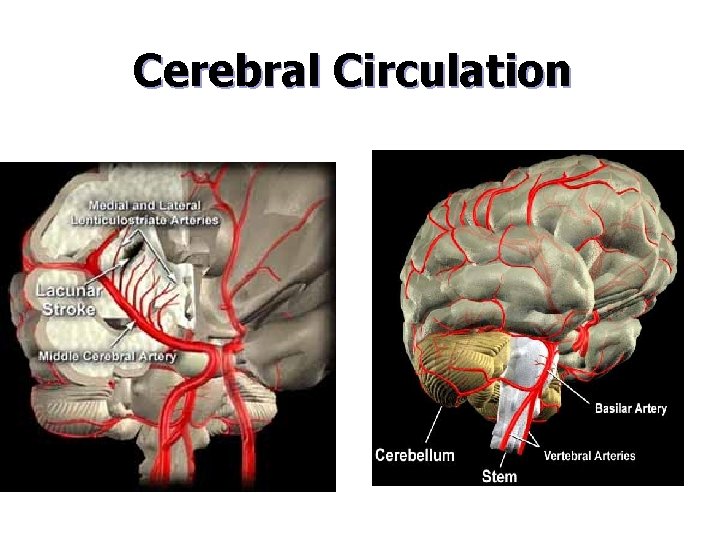
Cerebral Circulation
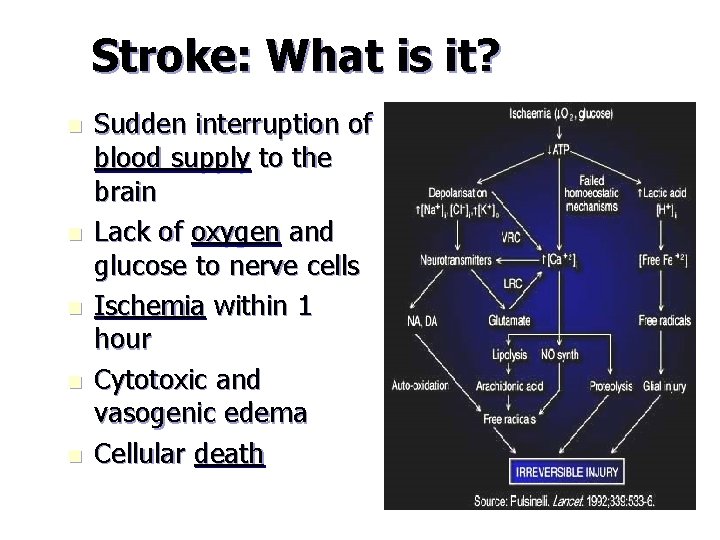
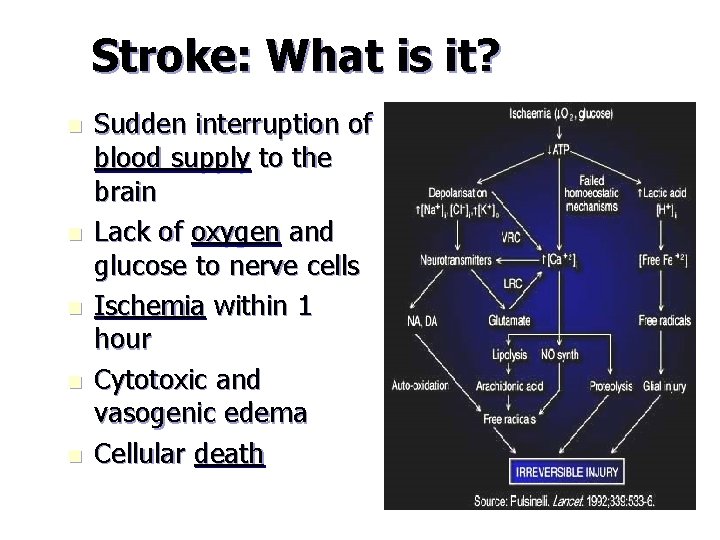
Stroke: What is it? n n n Sudden interruption of blood supply to the brain Lack of oxygen and glucose to nerve cells Ischemia within 1 hour Cytotoxic and vasogenic edema Cellular death
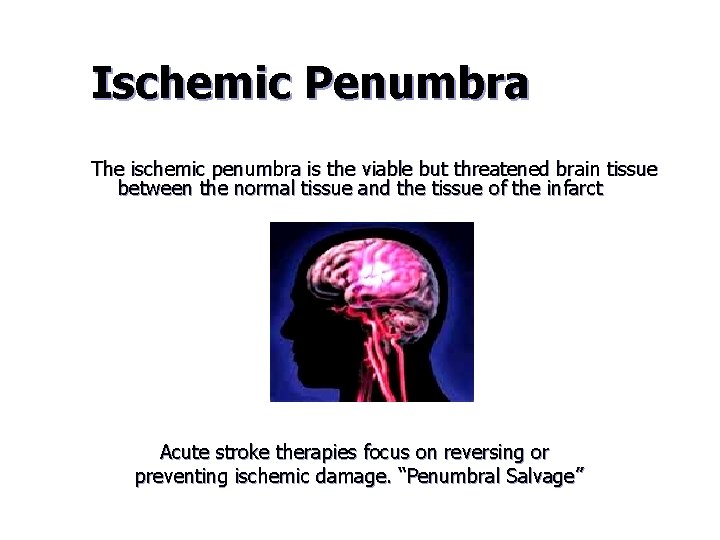
Ischemic Penumbra The ischemic penumbra is the viable but threatened brain tissue between the normal tissue and the tissue of the infarct Acute stroke therapies focus on reversing or preventing ischemic damage. “Penumbral Salvage”
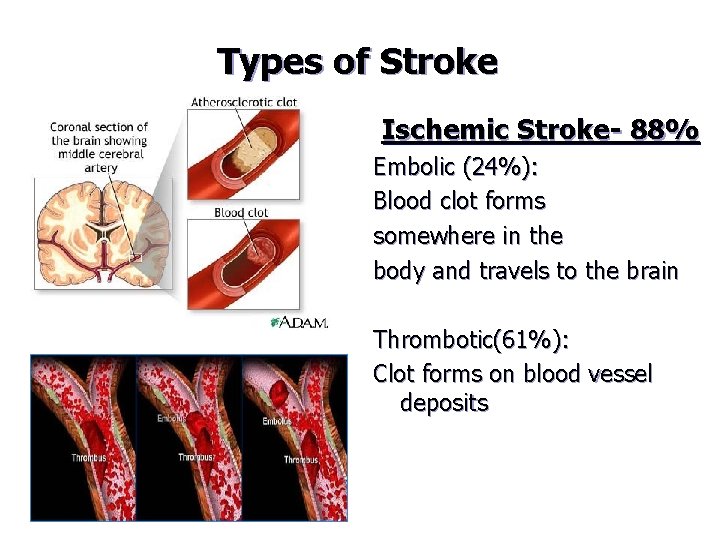
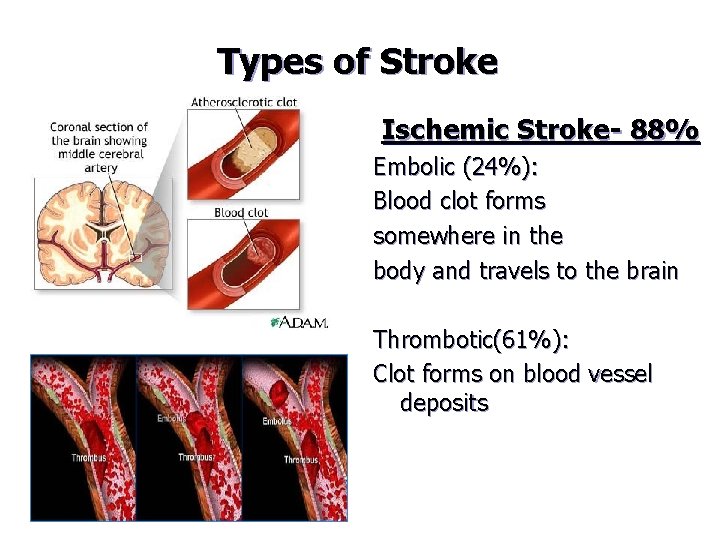
Types of Stroke Ischemic Stroke- 88% Embolic (24%): Blood clot forms somewhere in the body and travels to the brain Thrombotic(61%): Clot forms on blood vessel deposits
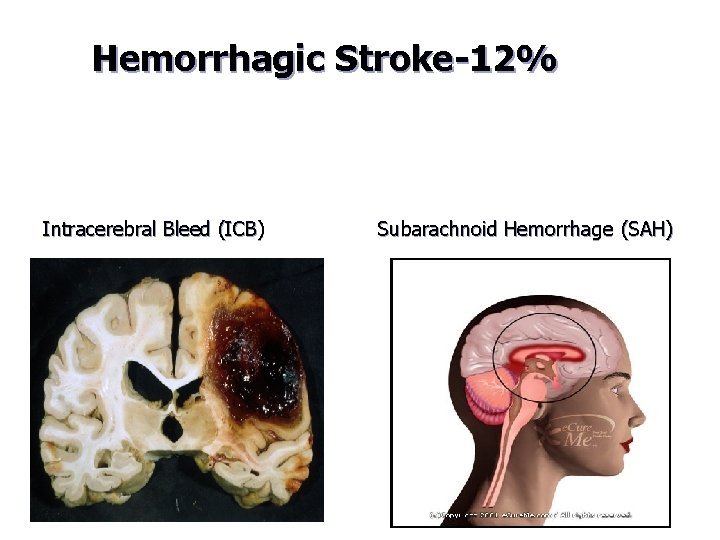
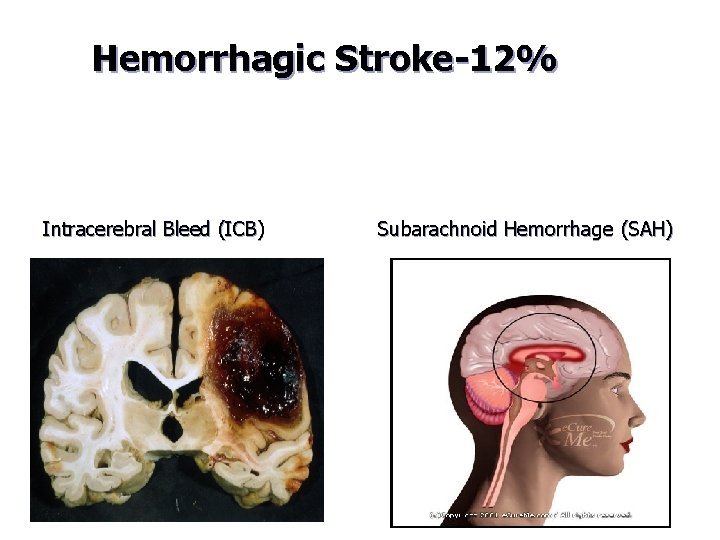
Hemorrhagic Stroke-12% Intracerebral Bleed (ICB) Subarachnoid Hemorrhage (SAH)
Hemorrhagic Stroke n n Responsible for 30% of stroke deaths Intracerebral-within the brain tissue. Most commonly from high blood pressure Subarachnoid-around the brain’s surface and under its protective layer-Most commonly from aneurysm rupture Risk factors: hypertension, alcohol, drug abuse, anti-clotting medication and blood clotting disorders
The Problem With TIA’s (Transient Ischemic Attack) n A “TIA” has sudden onset and rapid resolution Rule of Thumb: The event should last 2 -20 minutes n If the event lasts more than 1 hour it is probably a minor stroke n The likelihood of stroke is greatest in the first 48 hours after the event n More than 1/3 of all persons who experience TIA’s will go on to have a stroke
The Problem with TIA’s TIAs should not be ignored n Patients need to seek immediate medical attention in order to prevent a possible full blown stroke n MRI may be needed to determine TIA VS. Stroke n

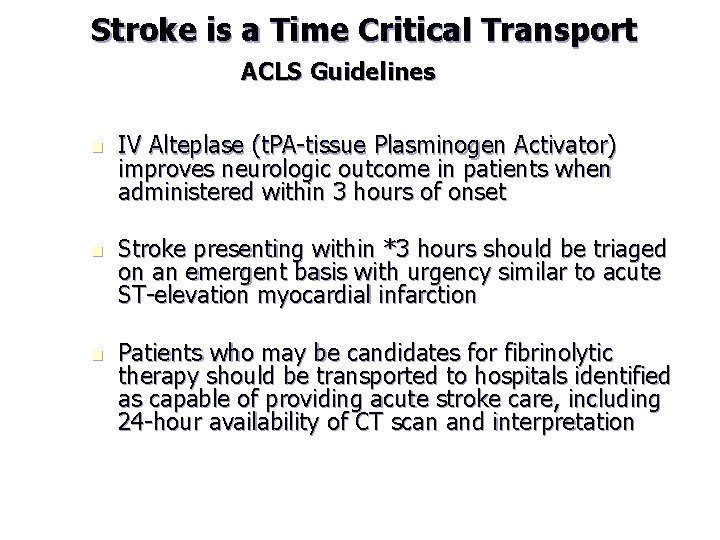
Stroke is a Time Critical Transport ACLS Guidelines n IV Alteplase (t. PA-tissue Plasminogen Activator) improves neurologic outcome in patients when administered within 3 hours of onset n Stroke presenting within *3 hours should be triaged on an emergent basis with urgency similar to acute ST-elevation myocardial infarction n Patients who may be candidates for fibrinolytic therapy should be transported to hospitals identified as capable of providing acute stroke care, including 24 -hour availability of CT scan and interpretation
Goals for EMS Response and Acute Intervention Rapid Recognition and Reaction to Stroke warning signs n Rapid EMS Dispatch n Rapid EMS transport and hospital prenotification n Rapid diagnosis and treatment n
Emergency Dispatch n n n Use of 911 system is recommended for symptoms of stroke Many callers do not use the word “stroke” Dispatchers should recognize the seriousness of stroke and be familiar with stroke symptoms. Strokes should be dispatched as a high priority call, send closest unit- similar to acute MI or trauma An EMD call-receiving algorithm is recommended to ask appropriate questions to callers
Emergency Dispatch n n n Dispatch should ask the caller when (what time) the patient was last seen normal (without weakness, facial droop, loss of speech)? Try to determine pertinent past medical history Relay information to Responder Request feedback from Responder regarding outcome Dispatchers should receive education recognizing stroke symptoms
EMS Stroke Care n n n Rapid Identification of stroke as the cause of the patient’s findings Elimination of conditions that could mimic stroke Stabilization Rapid transportation of the patient to the closest appropriate ED Pre notification to the receiving hospital about impending arrival of a patient with suspected stroke
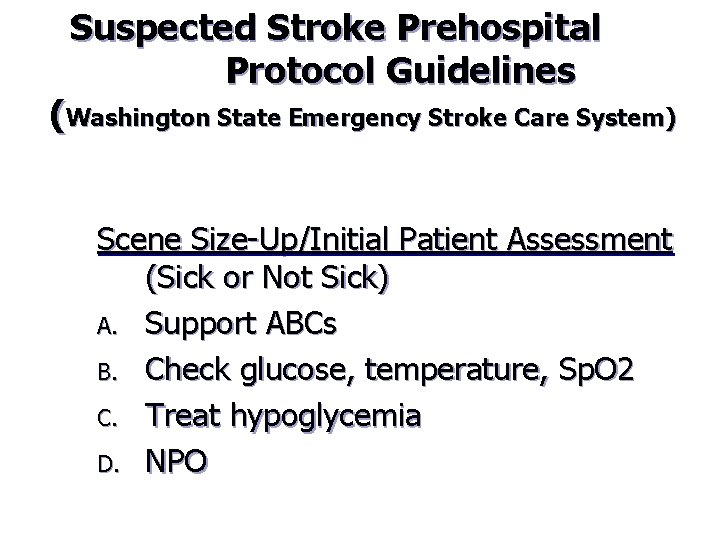
Suspected Stroke Prehospital Protocol Guidelines (Washington State Emergency Stroke Care System) Scene Size-Up/Initial Patient Assessment (Sick or Not Sick) A. Support ABCs B. Check glucose, temperature, Sp. O 2 C. Treat hypoglycemia D. NPO
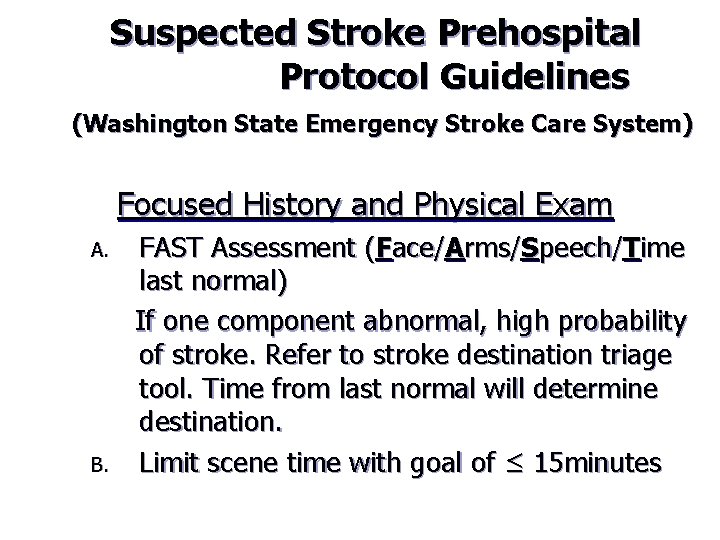
Suspected Stroke Prehospital Protocol Guidelines (Washington State Emergency Stroke Care System) Focused History and Physical Exam A. B. FAST Assessment (Face/Arms/Speech/Time last normal) If one component abnormal, high probability of stroke. Refer to stroke destination triage tool. Time from last normal will determine destination. Limit scene time with goal of ≤ 15 minutes
Time is Brain and you must act FAST!

F–A–S–T n Face – smile n Arm raise n Say a phrase n Time – Time Last Normal
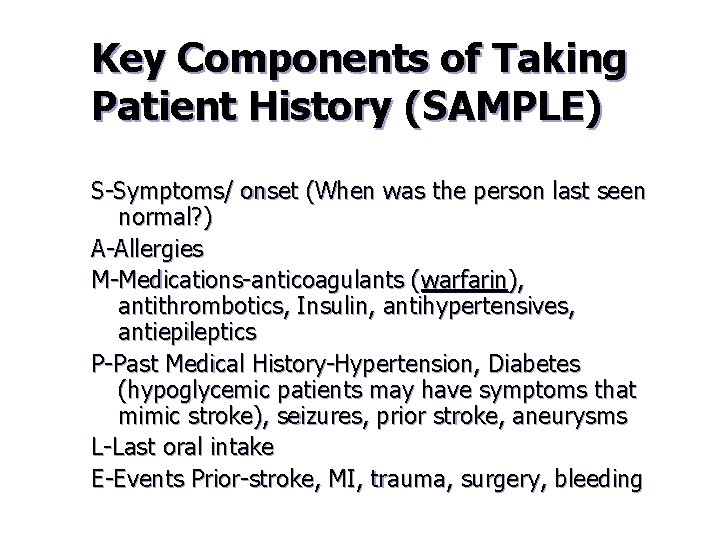
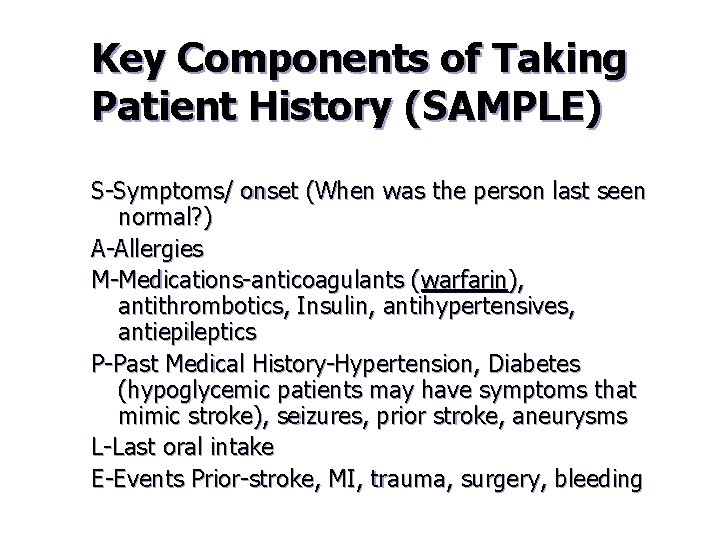
Key Components of Taking Patient History (SAMPLE) S-Symptoms/ onset (When was the person last seen normal? ) A-Allergies M-Medications-anticoagulants (warfarin), antithrombotics, Insulin, antihypertensives, antiepileptics P-Past Medical History-Hypertension, Diabetes (hypoglycemic patients may have symptoms that mimic stroke), seizures, prior stroke, aneurysms L-Last oral intake E-Events Prior-stroke, MI, trauma, surgery, bleeding

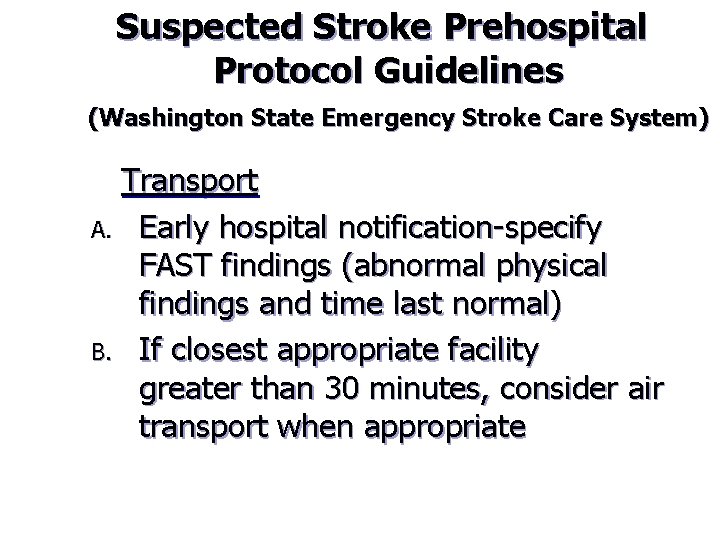
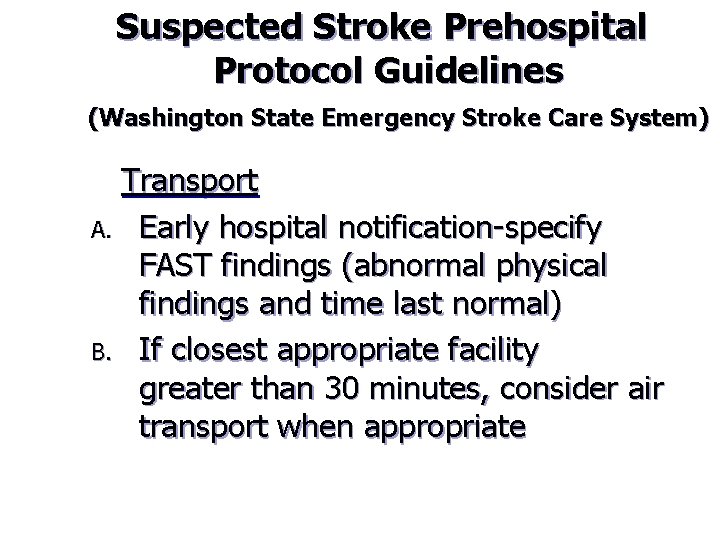
Suspected Stroke Prehospital Protocol Guidelines (Washington State Emergency Stroke Care System) Transport A. Early hospital notification-specify FAST findings (abnormal physical findings and time last normal) B. If closest appropriate facility greater than 30 minutes, consider air transport when appropriate
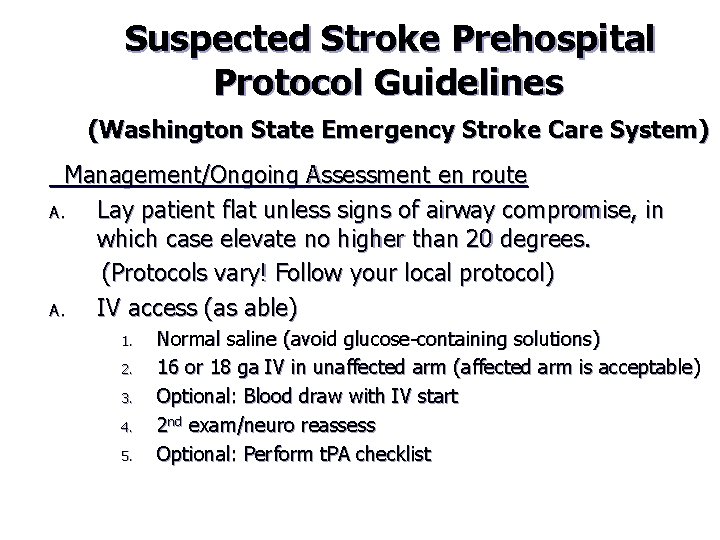
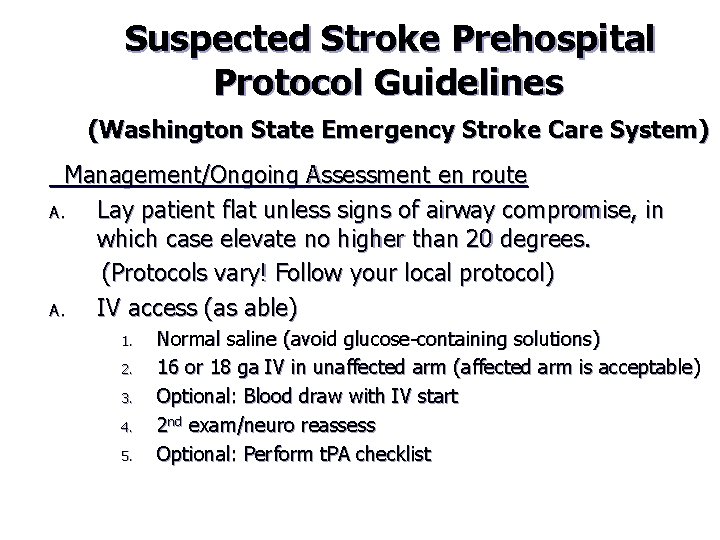
Suspected Stroke Prehospital Protocol Guidelines (Washington State Emergency Stroke Care System) Management/Ongoing Assessment en route A. Lay patient flat unless signs of airway compromise, in which case elevate no higher than 20 degrees. (Protocols vary! Follow your local protocol) A. IV access (as able) 1. 2. 3. 4. 5. Normal saline (avoid glucose-containing solutions) 16 or 18 ga IV in unaffected arm (affected arm is acceptable) Optional: Blood draw with IV start 2 nd exam/neuro reassess Optional: Perform t. PA checklist
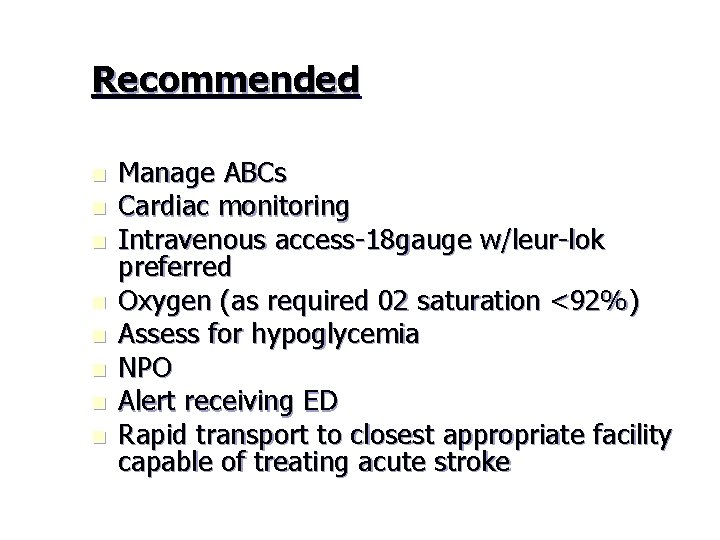
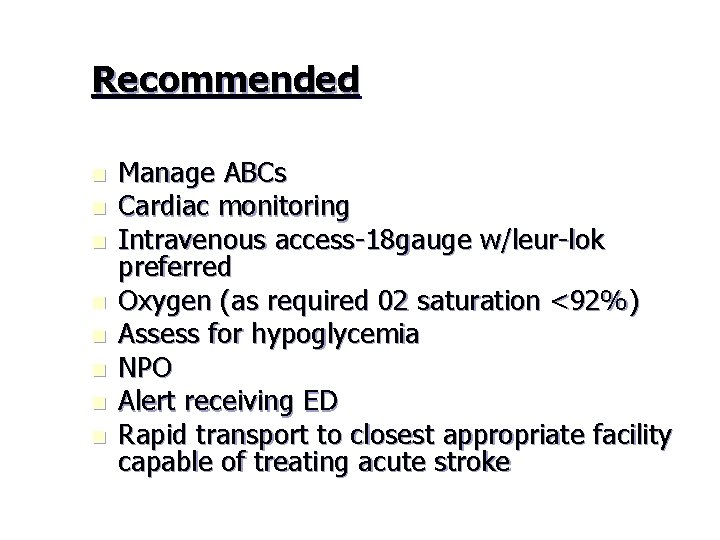
Recommended n n n n Manage ABCs Cardiac monitoring Intravenous access-18 gauge w/leur-lok preferred Oxygen (as required 02 saturation <92%) Assess for hypoglycemia NPO Alert receiving ED Rapid transport to closest appropriate facility capable of treating acute stroke

Not Recommended Dextrose-containing fluids in nonhypoglycemic patients n Excessive blood pressure reduction (can cause hypotension, decrease cerebral perfusion and worsen stroke) n Excessive intravenous fluids (can cause increased intracranial pressure) n
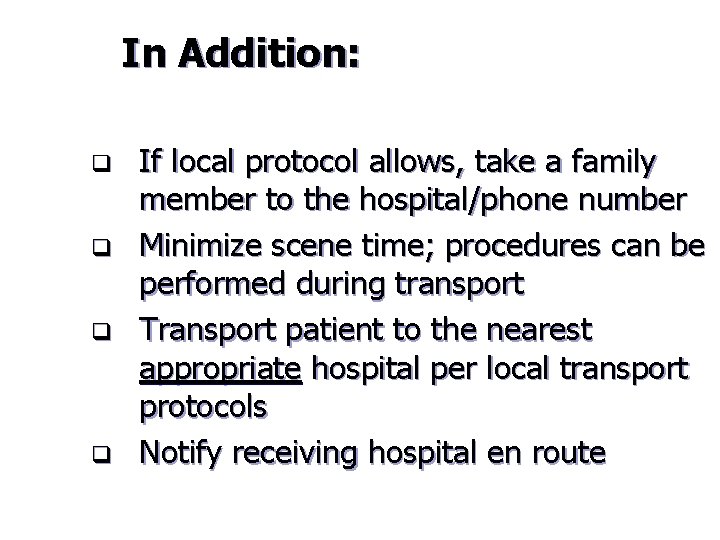
In Addition: q q If local protocol allows, take a family member to the hospital/phone number Minimize scene time; procedures can be performed during transport Transport patient to the nearest appropriate hospital per local transport protocols Notify receiving hospital en route
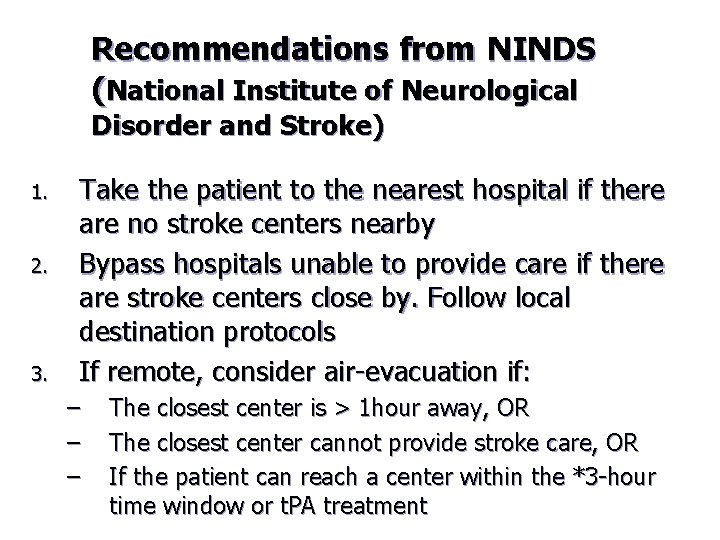
Recommendations from NINDS (National Institute of Neurological Disorder and Stroke) 1. 2. 3. Take the patient to the nearest hospital if there are no stroke centers nearby Bypass hospitals unable to provide care if there are stroke centers close by. Follow local destination protocols If remote, consider air-evacuation if: – – – The closest center is > 1 hour away, OR The closest center cannot provide stroke care, OR If the patient can reach a center within the *3 -hour time window or t. PA treatment
Destination Protocols Coming soon! Washington State destination protocols for stroke
Northwest Medstar Response Times
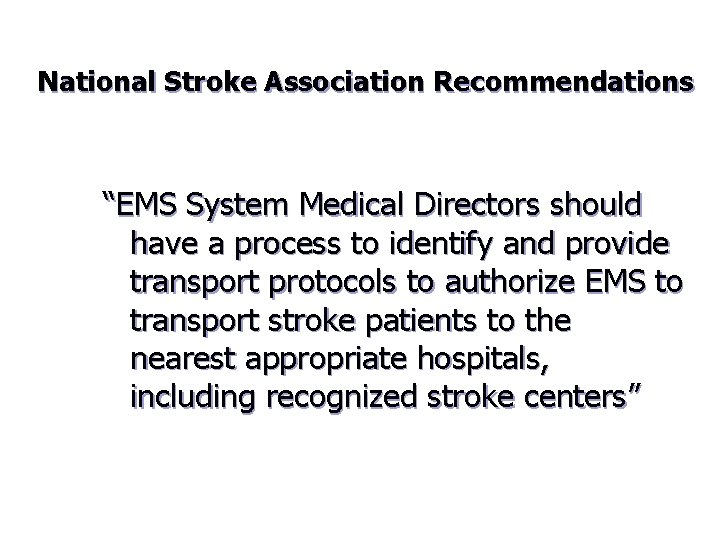
National Stroke Association Recommendations “EMS System Medical Directors should have a process to identify and provide transport protocols to authorize EMS to transport stroke patients to the nearest appropriate hospitals, including recognized stroke centers”
Evaluation of Current Systems n n n What is your general EMS environment in your state? What processes are in place that provide rapid access to EMS for patients with acute stroke? What are your EMS dispatch protocols? Where are suspected stroke patients transported? What communications occur between local hospitals and EMS systems?
Stroke is a time critical n IV t. PA (Alteplase)-Time from last normal to 3 hours. (Extended window 3 -4. 5 hours) n Dose is based on patient’s weight. 10% of determined dose as an IV bolus, remaining 90% over one hour n May cause intracranial bleeding but has not been shown to increase mortality
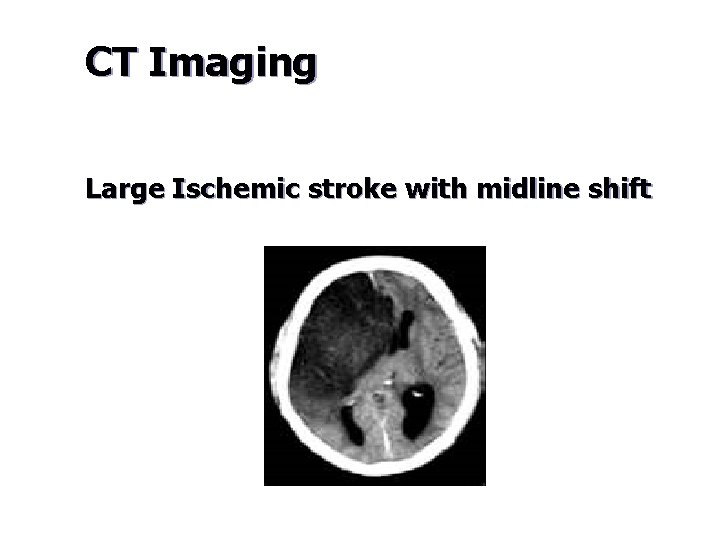
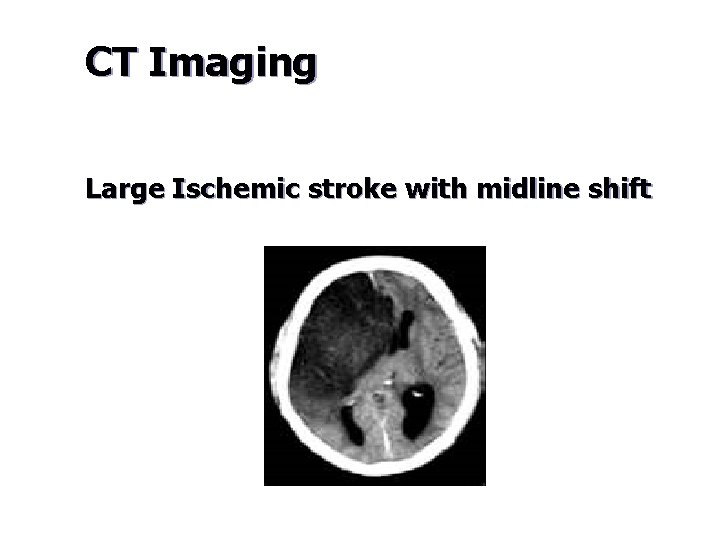
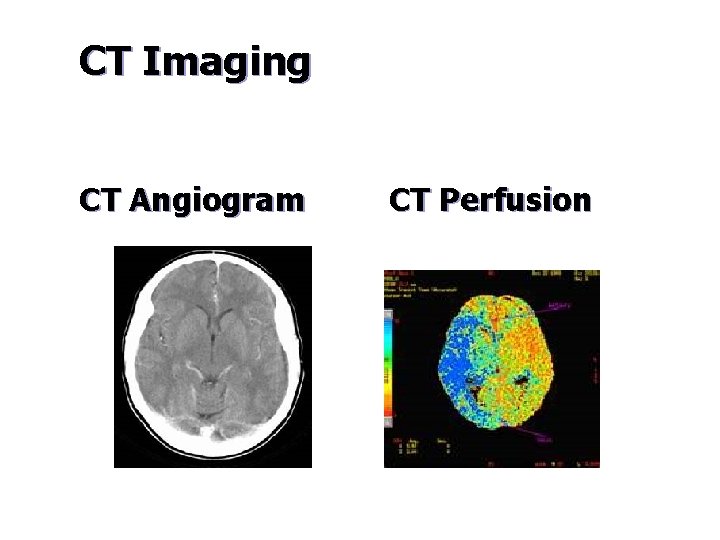
CT Imaging Large Ischemic stroke with midline shift
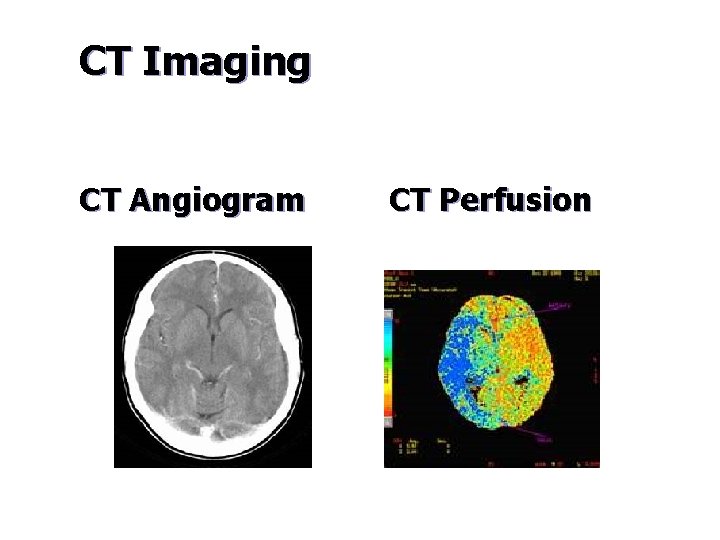
CT Imaging CT Angiogram CT Perfusion
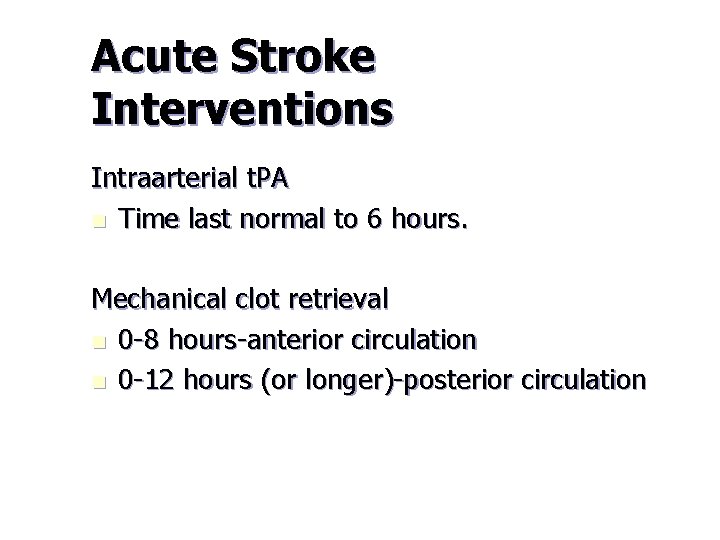
Acute Stroke Interventions Intraarterial t. PA n Time last normal to 6 hours. Mechanical clot retrieval n 0 -8 hours-anterior circulation n 0 -12 hours (or longer)-posterior circulation

Merci™-Mechanical Clot Retrieval Device
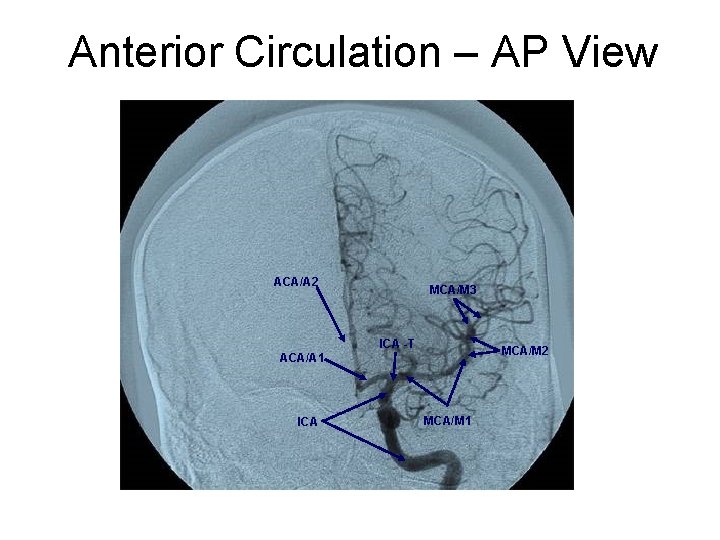
Anterior Circulation – AP View ACA/A 2 MCA/M 3 ICA -T MCA/M 2 ACA/A 1 MCA/M 1 ICA APM 0189/B/3073, 2007 -12 © Concentric Medical 2007 56
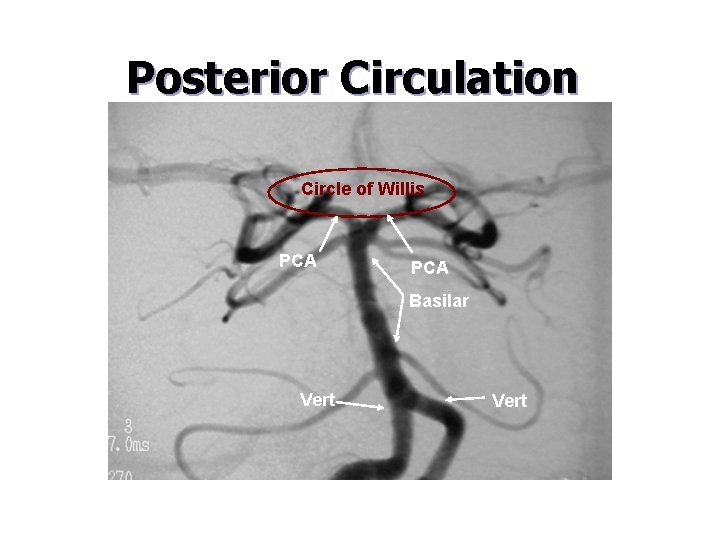
Posterior Circulation Circle of Willis PCA Basilar Vert APM 0189/B/3073, 2007 -12 © Concentric Medical 2007 Vert 57
Patient History n n n n 47 year old male, history of excessive alcohol abuse Last seen normal at midnight, found at 4 am unable to move his right side and unable to speak Family called 911, transfer to stroke center Not a candidate for IV t-PA, symptom onset >3 hours ER Physicians notified interventional team and arranged for transfer Patient arrived to and was in the angiography suite by 6: 30 am Clinical Neurologic exam: unable to move right arm and leg, confused and unable to express language, NIHSS 18 (0 – 42) APM 0189/B/3073, 2007 -12 © Concentric Medical 2007 Patient not a candidate for IV t-PA as symptom onset >3 hours. He was identified as a candidate for intervention. 58
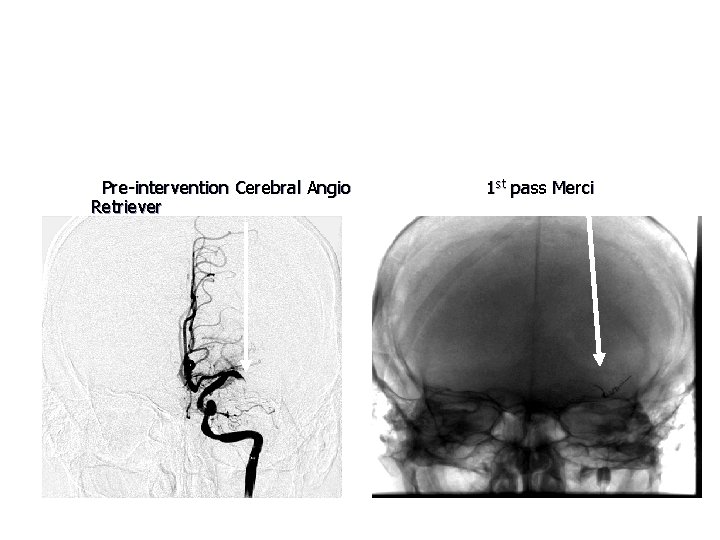
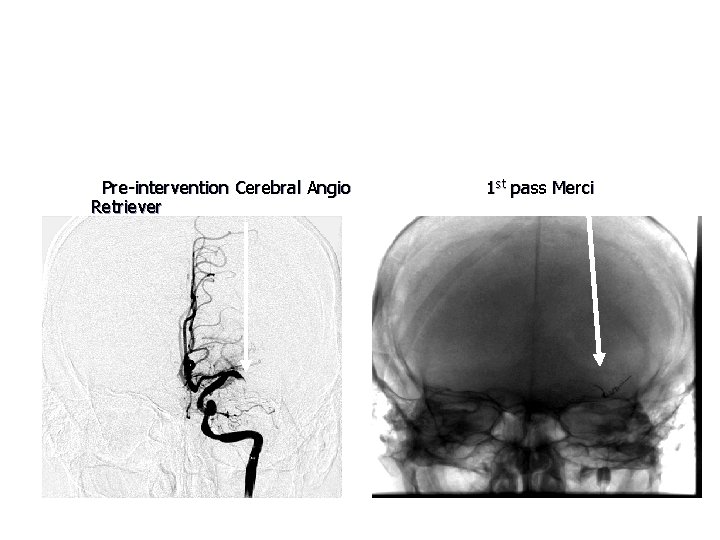
Intervention with Merci Retriever Clot completely blocking flow in the left middle cerebral artery Merci Retriever positioned in the left middle cerebral artery Pre-intervention Cerebral Angio Retriever APM 0189/B/3073, 2007 -12 © Concentric Medical 2007 59 1 st pass Merci
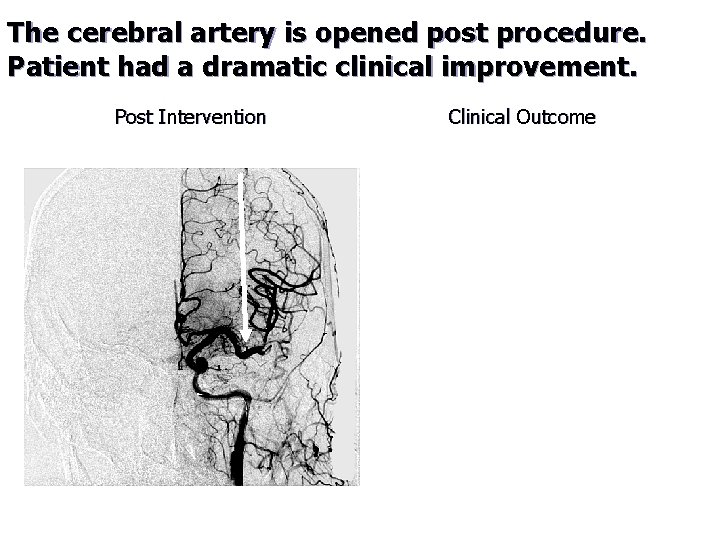
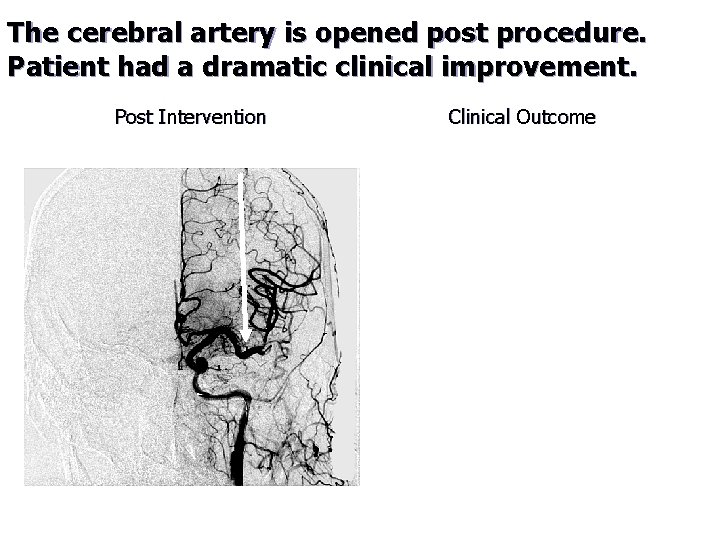
The cerebral artery is opened post procedure. Patient had a dramatic clinical improvement. Post Intervention Clinical Outcome First division of the left middle cerebral artery is open Neurologic Exam after interventional procedure: • Alert and oriented, moving all extremities with subtle right sided weakness and mild language difficulties • Following day NIHSS 3 decreased from 18 • Discharged to rehab • Awaiting home transfer with 24/7 supervision • Ambulates with quad cane and has some persistent mixed aphasia APM 0189/B/3073, 2007 -12 © Concentric Medical 2007 60
EMS Role in Research n n n Identification of an effective neuroprotective therapy may further expand the role of EMS in the treatment of acute stroke. Hypothermia-Reduces cytotoxic cascade, Stabilizes blood-brain barrier, Reduces freeradical formation, May prevent neurotoxicity of t. PA IV Magnesium-(FASTMAG Trial) IV Magnesium loading dose given in the field. Cytoprotective and vasodilating effects.
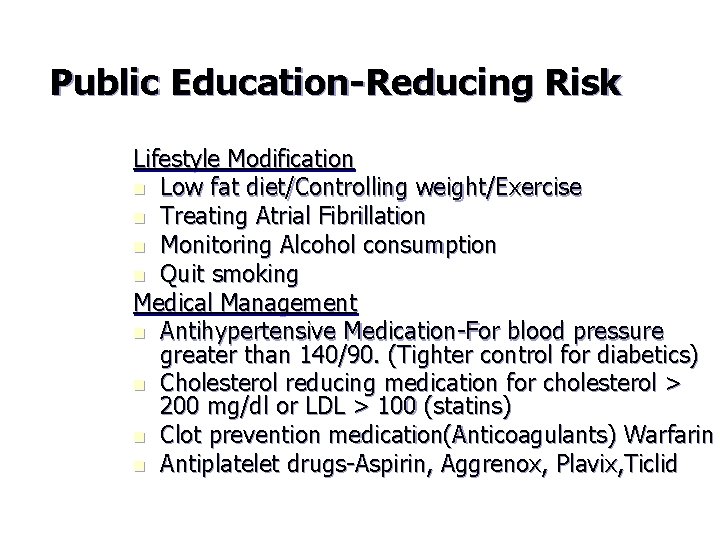
Public Education-Reducing Risk Lifestyle Modification n Low fat diet/Controlling weight/Exercise n Treating Atrial Fibrillation n Monitoring Alcohol consumption n Quit smoking Medical Management n Antihypertensive Medication-For blood pressure greater than 140/90. (Tighter control for diabetics) n Cholesterol reducing medication for cholesterol > 200 mg/dl or LDL > 100 (statins) n Clot prevention medication(Anticoagulants) Warfarin n Antiplatelet drugs-Aspirin, Aggrenox, Plavix, Ticlid
Questions?
Donald Rumsfeld n There are knowns. These are things we know that we know. There are known unknowns. That is to say, there are things that we know we don't know. But there also unknowns. There are things we don't know.
References n n n n American Stroke Association. Guidelines for the Early Management of Adults With Ischemic Stroke May 2007. “Prehospital Management and Field Treatment”. American Heart Association/ACLS Provider Manual. 2006 National Institute of Neurological Disorders and Stroke (NINDS) Concentric Medical-Merci Retrieval device Genentec-Alteplase National Stroke Association-EMS Provider information Thanks to Michael Day-Trauma Services Coordinator Sacred Heart Medical Center Northwest Regional Stroke Network-Destination protocols, EMS Online Training
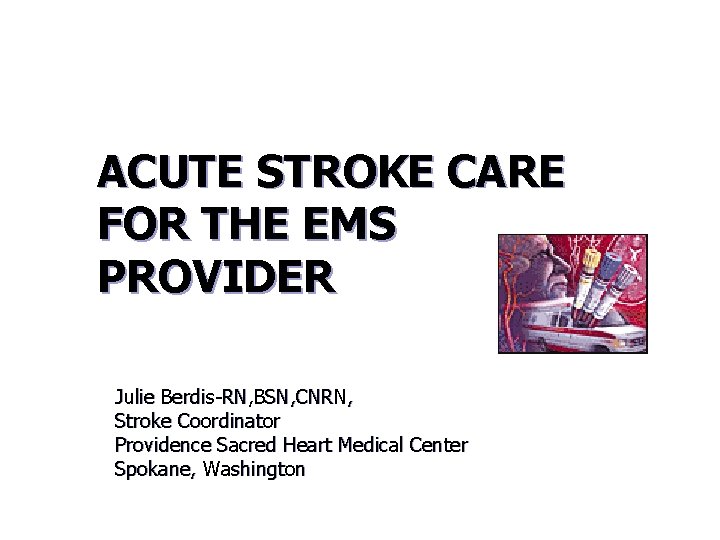
Super Secret Question You are dispatched to a call of a 75 -year-old female with sudden onset of trouble walking; she has become dizzy and very nauseated. She cannot walk without holding onto furniture. Her blood pressure is 160/90. Her blood sugar is normal. The cardiac monitor shows sinus rhythm. She has no c/o chest pain. She is a nondrinker/non-smoker, but takes medication for high blood pressure. She has no facial droop or arm weakness. You suspect this could be stroke. What area of the brain could give you these symptoms?
Questions? Contact: Carolyn Stovall 509 -242 -4263 1 -866 -630 -4033 stovalc@inhs. org Fax: 509 -232 -8168
 Anterior stroke vs posterior stroke
Anterior stroke vs posterior stroke Stroke algorithm
Stroke algorithm Acute stroke ready certification
Acute stroke ready certification Levels of nursing care primary secondary tertiary
Levels of nursing care primary secondary tertiary 8 ds of stroke care
8 ds of stroke care Acute care collaboration
Acute care collaboration Rcp acute care toolkit
Rcp acute care toolkit Hepatitis a incubation period
Hepatitis a incubation period Care provider background screening clearinghouse
Care provider background screening clearinghouse Lakeland care provider portal
Lakeland care provider portal Iso 22301 utbildning
Iso 22301 utbildning Typiska novell drag
Typiska novell drag Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Returpilarna
Returpilarna Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Underlag för särskild löneskatt på pensionskostnader
Underlag för särskild löneskatt på pensionskostnader Tidbok för yrkesförare
Tidbok för yrkesförare Anatomi organ reproduksi
Anatomi organ reproduksi Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Stig kerman
Stig kerman Hur skriver man en tes
Hur skriver man en tes Delegerande ledarskap
Delegerande ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Lufttryck formel
Lufttryck formel Offentlig förvaltning
Offentlig förvaltning Kyssande vind
Kyssande vind Presentera för publik crossboss
Presentera för publik crossboss Vad är ett minoritetsspråk
Vad är ett minoritetsspråk Kanaans land
Kanaans land Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Mjälthilus
Mjälthilus Claes martinsson
Claes martinsson Cks
Cks Lågenergihus nyproduktion
Lågenergihus nyproduktion Mat för idrottare
Mat för idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referatmarkeringar
Referatmarkeringar Redogör för vad psykologi är
Redogör för vad psykologi är Matematisk modellering eksempel
Matematisk modellering eksempel Tack för att ni har lyssnat
Tack för att ni har lyssnat Borra hål för knoppar
Borra hål för knoppar Vilken grundregel finns det för tronföljden i sverige?
Vilken grundregel finns det för tronföljden i sverige? Relativ standardavvikelse formel
Relativ standardavvikelse formel Tack för att ni har lyssnat
Tack för att ni har lyssnat Steg för steg rita
Steg för steg rita Vad är verksamhetsanalys
Vad är verksamhetsanalys Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Blomman för dagen drog
Blomman för dagen drog Handledning reflektionsmodellen
Handledning reflektionsmodellen Egg för emanuel
Egg för emanuel Elektronik för barn
Elektronik för barn Mantel som bars av kvinnor i antikens rom
Mantel som bars av kvinnor i antikens rom Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Kung som dog 1611
Kung som dog 1611 Humanitr
Humanitr Ro i rom pax
Ro i rom pax Tack för att ni lyssnade
Tack för att ni lyssnade Matte större än tecken
Matte större än tecken Dikter
Dikter Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Rbk fuktmätning
Rbk fuktmätning