The Child with Fever Dr Mohamed Hesham Professor























- Slides: 79
The Child with Fever Dr Mohamed Hesham Professor of Pediatrics Rabigh-Medical college
Objectives • Definition and measurement of normal body temperature • Definition and pathogenesis of fever • Causes and types of febrile illnesses • Clinical assessment of febrile patient • Pharmacologic and non pharmacologic management of fever
Normal body temperature • The average normal body temperature is (37°C). • It usually rises during the day from a low of 36. 3°C in the morning to a high of (37. 6°C) in the late afternoon. • Each child has a normal temperature range that may be different from another child's. • Mild increases to 38°C can be caused by exercising, wearing too many clothes, taking a hot bath, or being outside in hot weather.
Normal body temperature • Rectal temperatures are usually (0. 6 C) higher than oral temperatures. • Rectal and tympanic temperatures can be considered equivalent, but a rectal temperature is the current standard. • Temperature normally rises and falls during the day. It is usually at its lowest point between 4 am and 6 am and at it highest point between 4 pm and 6 pm
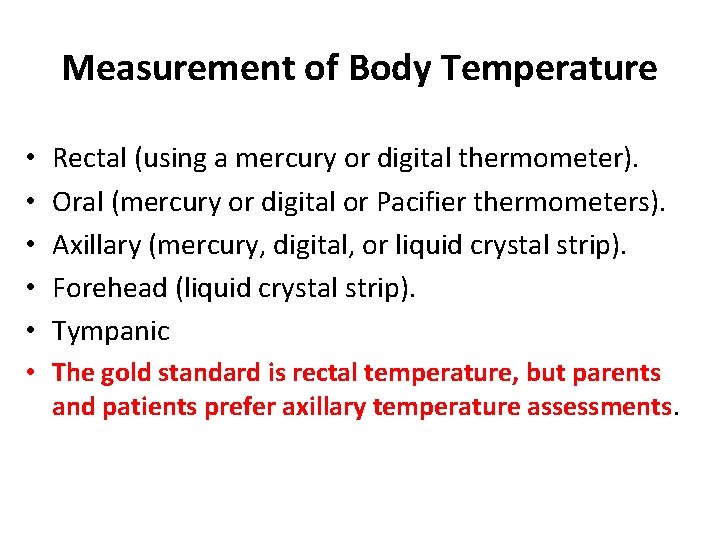
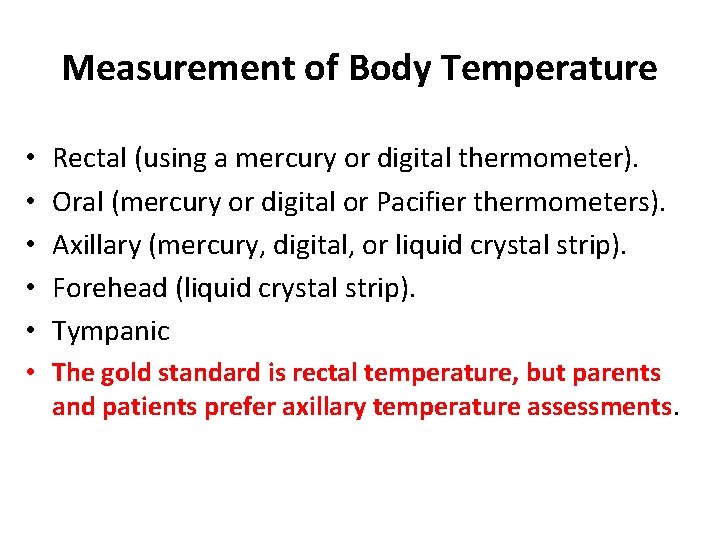
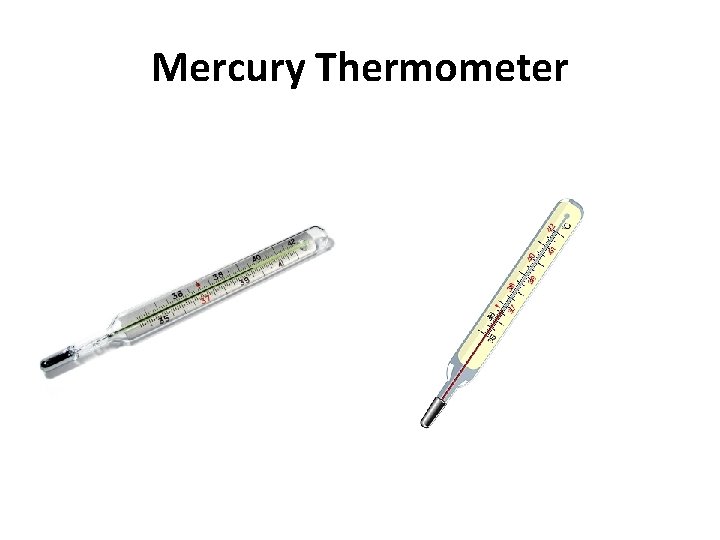
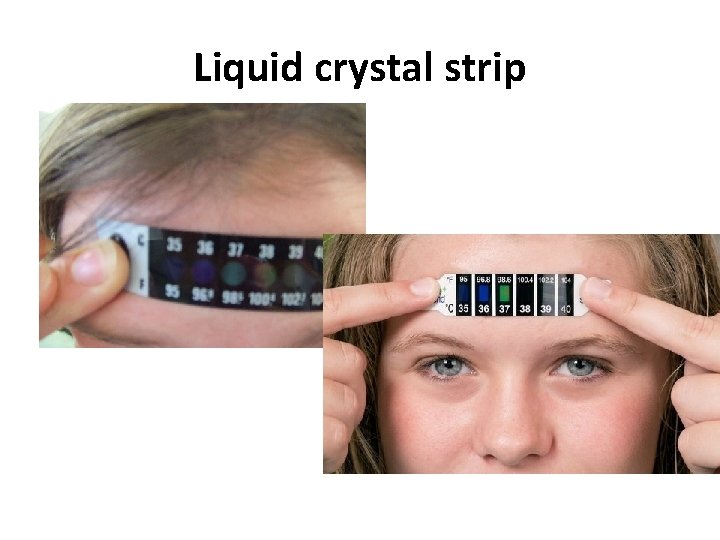
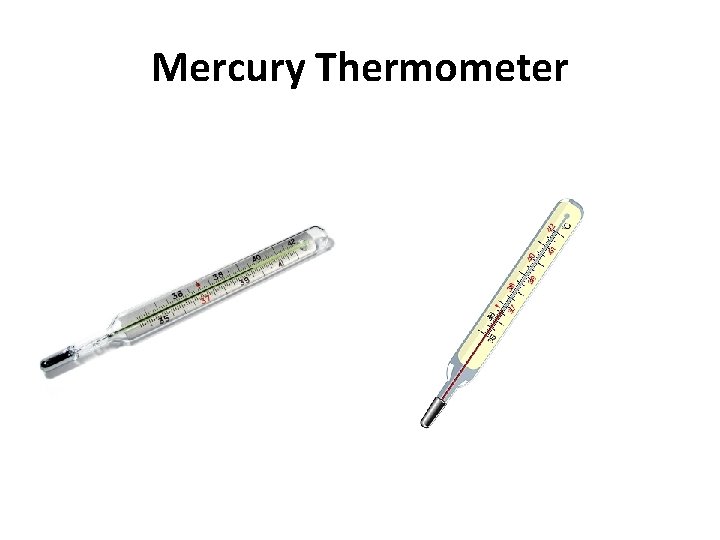
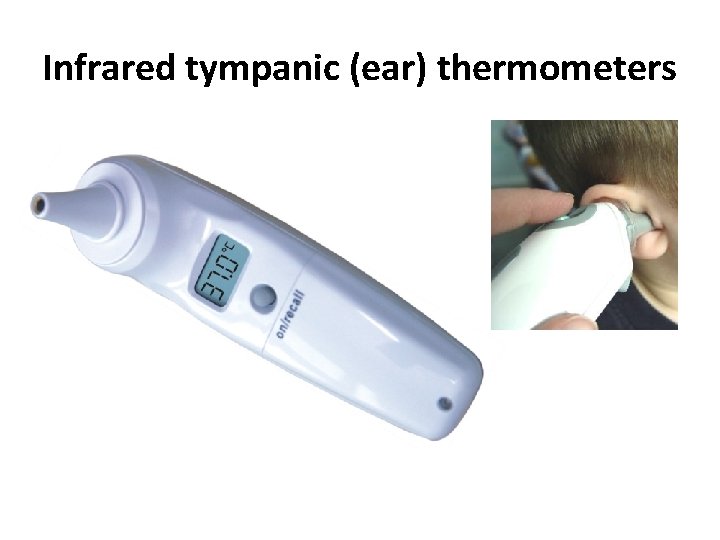
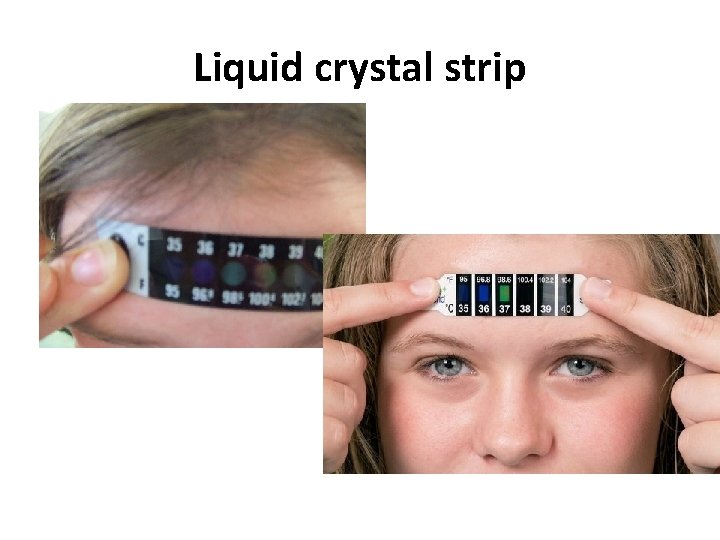
Measurement of Body Temperature • • • Rectal (using a mercury or digital thermometer). Oral (mercury or digital or Pacifier thermometers). Axillary (mercury, digital, or liquid crystal strip). Forehead (liquid crystal strip). Tympanic • The gold standard is rectal temperature, but parents and patients prefer axillary temperature assessments.
Mercury Thermometer

Electrical Digital thermometers
Infrared tympanic (ear) thermometers

Infrared tympanic (ear) thermometers
Liquid crystal strip

Phase-change (dot matrix) thermometers

Infant Pacifier Thermometer

Infant Pacifier Thermometer
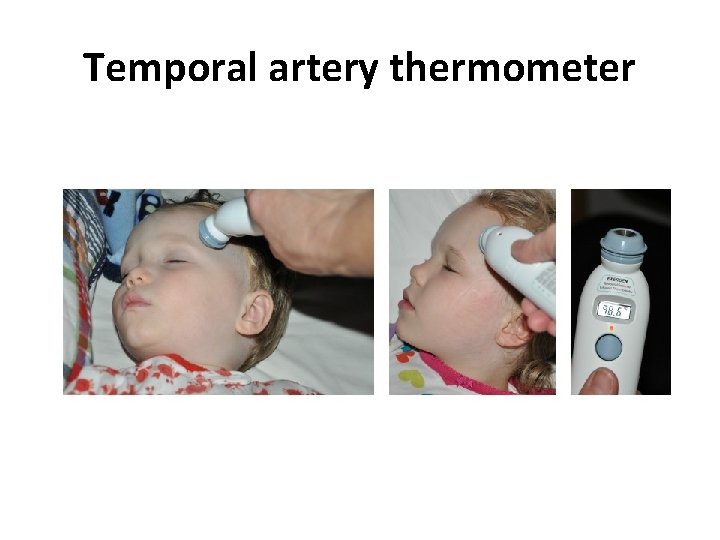
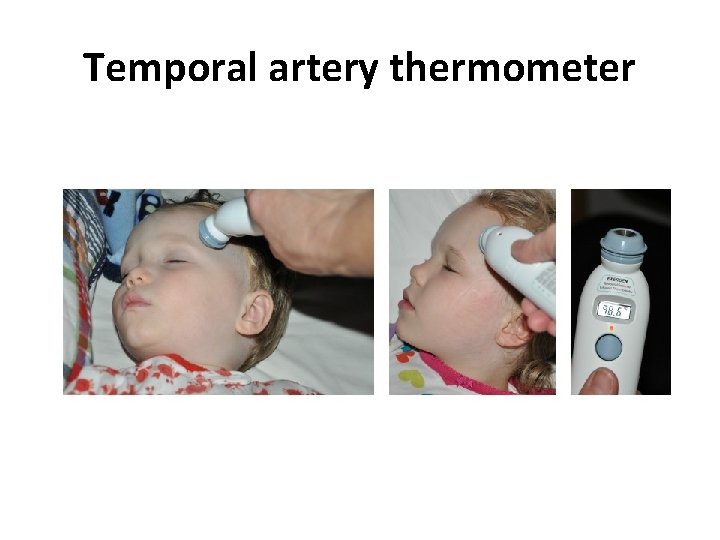
Temporal artery thermometer
Temporal artery thermometer

Temporal artery thermometer
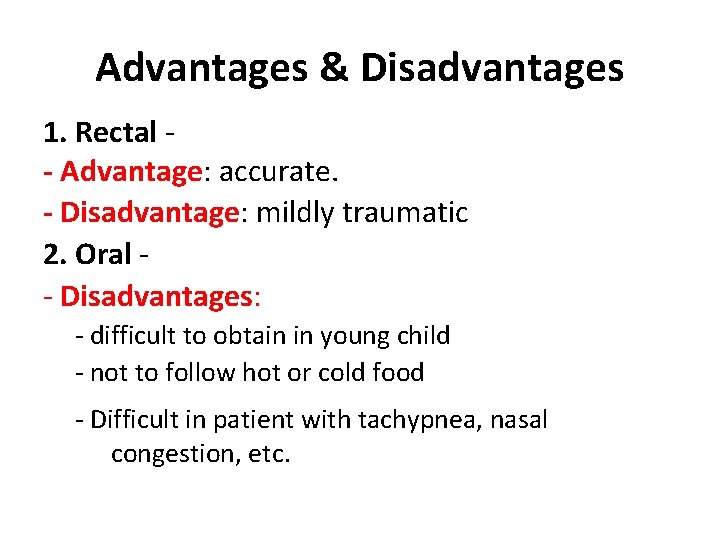
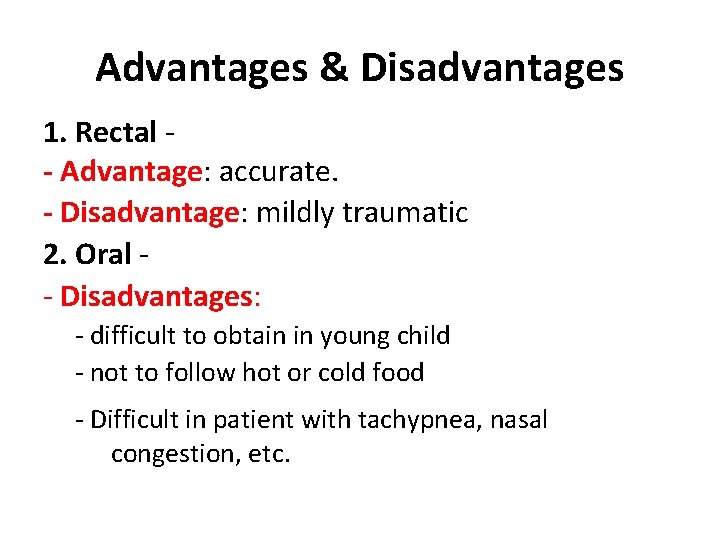
Advantages & Disadvantages 1. Rectal - Advantage: accurate. - Disadvantage: mildly traumatic 2. Oral - Disadvantages: - difficult to obtain in young child - not to follow hot or cold food - Difficult in patient with tachypnea, nasal congestion, etc.
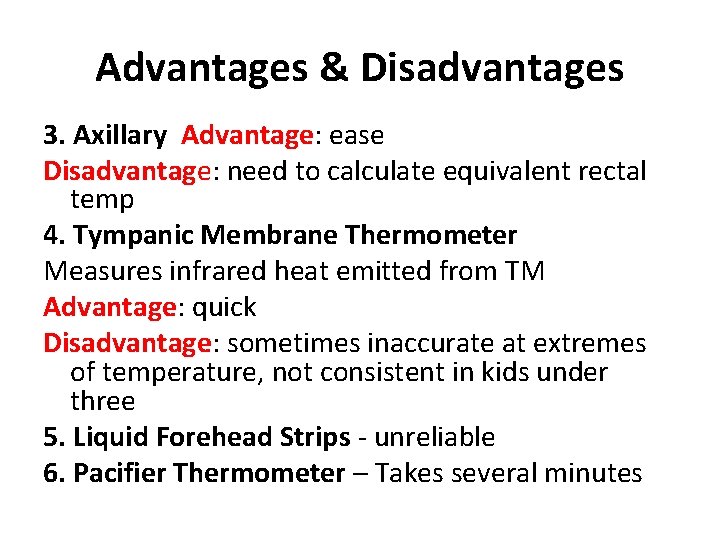
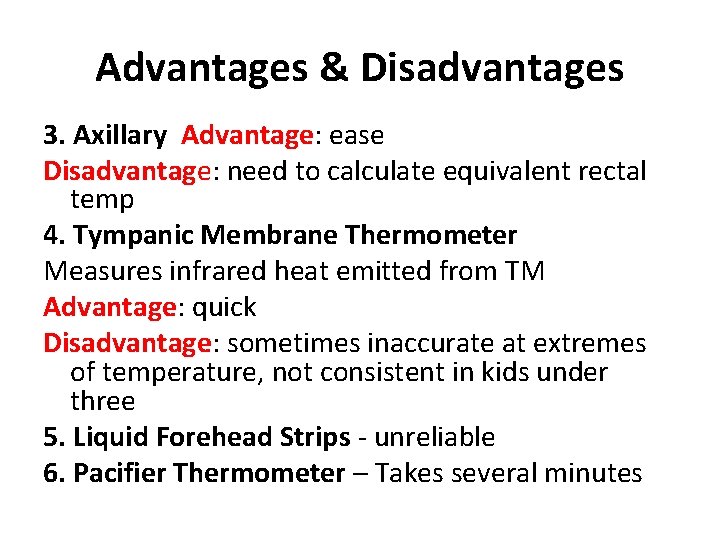
Advantages & Disadvantages 3. Axillary Advantage: ease Disadvantage: need to calculate equivalent rectal temp 4. Tympanic Membrane Thermometer Measures infrared heat emitted from TM Advantage: quick Disadvantage: sometimes inaccurate at extremes of temperature, not consistent in kids under three 5. Liquid Forehead Strips - unreliable 6. Pacifier Thermometer – Takes several minutes

Definition and General Concepts • Fever is the body's normal and healthy reaction to infection and other illnesses, both minor and serious. • Fevers help the body fight infection. • Fever is a symptom, not a disease!
Definition and General Concepts • Fever remains the most common concern for which parents bring their child to the emergency department. • The most common reason for pediatric consultations • Definition: Rectal temperature of 38°C or above. • Temperatures measured at other sites are usually lower.

Definition and General Concepts • Fever itself is not life-threatening unless it is extremely and persistently high, such as greater than 107 F (41. 6 C) when measured rectally. • Fever may indicate the presence of a serious illness, but usually a fever is caused by common infections which are not serious.
“Fever Phobia” • Primary fears – Brain damage – Coma – Seizures – Blindness – Death • Other contributors – School – Pharmaceuticals
Benefits of Fever Protective role in the immune system • Inhibition of growth and replication of microorganisms • Aids in body’s acute phase reaction • Enhanced immunologic function of WBCs – lymphocyte response to mitogens – bactericidal activity of neutrophils – production of interferon • Promotion of monocyte maturation into macrophages • Promotion of lymphocyte activation and antibody production • Decreased availability of free iron for bacterial replication
Benefits of fever • “Fever is nature’s engine which she brings into the field to remove her enemy” Thomas Sydenham English Physician 1624 – 1689 It is not the fever that is harmful but the underlying disease. The associated fever may be protective How patient is acting is generally more important than degree of temperature elevation
Pathogenesis of Fever • The part of the brain called the hypothalamus controls body temperature. • The hypothalamus increases the body's temperature as a way to fight the infection. • However, many conditions other than infections may cause a fever

Pathogenesis of Fever • Exogenous pyrogens (infection/inflammation) • Endogenous pyrogens(interleukin-1, tumor necrosis factor, and interferon) by macrophages • Anterior hypothalamus (raise thermostat) • Prostaglandin-E 2 • FEVER • Antipyretics are anti-prostaglandins

Causes of Fever • Infections (bacterial, viral, fungal, …) • Inflammatory diseases ( collagen vascular, IBD) • Malignancies (lymphoma, leukemia, …. . ) • Others – Hyperthyroidism – Diabetes inspidus – Drugs – CNS dysfunction – Factitious fever – etc……………. .

Causes of Fever Short febrile illness (duration < 7 days): Simple focal infections: • The most common of all cause e. g. tonsillitis, bronchitis, • Easily diagnosed by history & exam Serious focal infections: • Like pneumonia, meningitis, peritonitis • Relevant clinical signs are important for diagnosis Fever without a focus ( Non-localizing fever) Classified using general clinical assessment 1) Appetite, activity, and reaction (parents) 2) Consciousness, look, and reaction (doctor)

Fever and Teething……? ? ? • Teething does not cause a fever. If a baby is teething and has a fever, look for other symptoms that may need to be evaluated

Clinical assessment of febrile patient (i) How is fever identified in children? (ii) How old is the child? (iii) Are there risk factors for infection? (iv) How ill is the child? (v) Is there a rash? (vi) Is there a focus for infection?
(i) How is fever identified in children? • Parents usually know if their child has been febrile. • In hospital, it is measured: – < 4 weeks old by electronic thermometer in the axilla – 4 wk to 5 yrs by electronic or chem dot thermometer in the axilla or infrared tympanic thermometer. – In general, axillary temperatures underestimate body temperature by 0. 5°C.
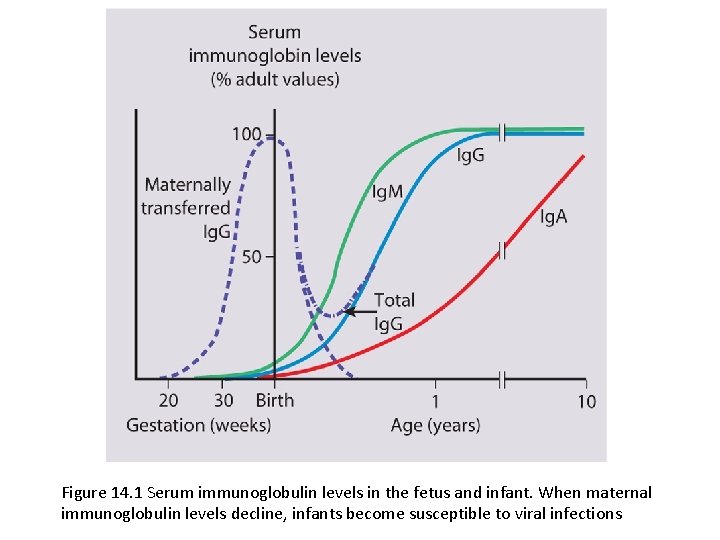
(ii) How old is the child? • Febrile infants <3 months present with non-specific clinical features and clinical examination alone is unreliable. • It is uncommon for them to have common viral infections because of passive immunity from their mothers. • Unless a clear cause for the fever is identified, they require urgent investigation with a septic screen and intravenous antibiotic therapy given immediately to avoid the illness becoming more severe and to prevent rapid spread to other sites of the body.
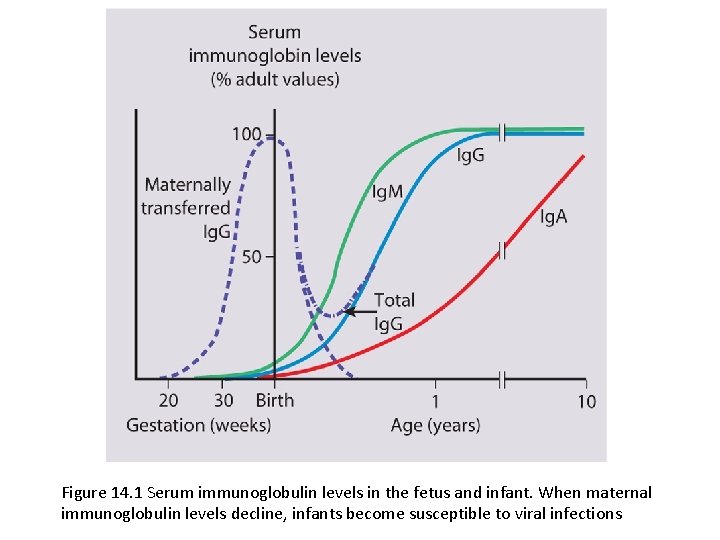
Figure 14. 1 Serum immunoglobulin levels in the fetus and infant. When maternal immunoglobulin levels decline, infants become susceptible to viral infections
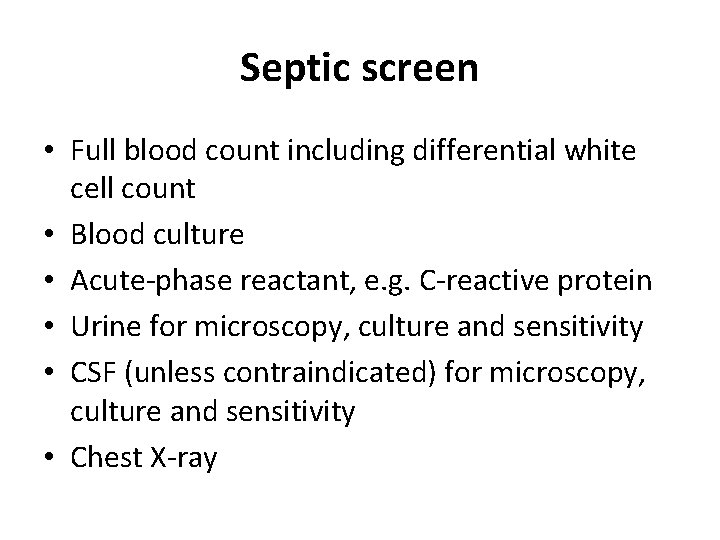
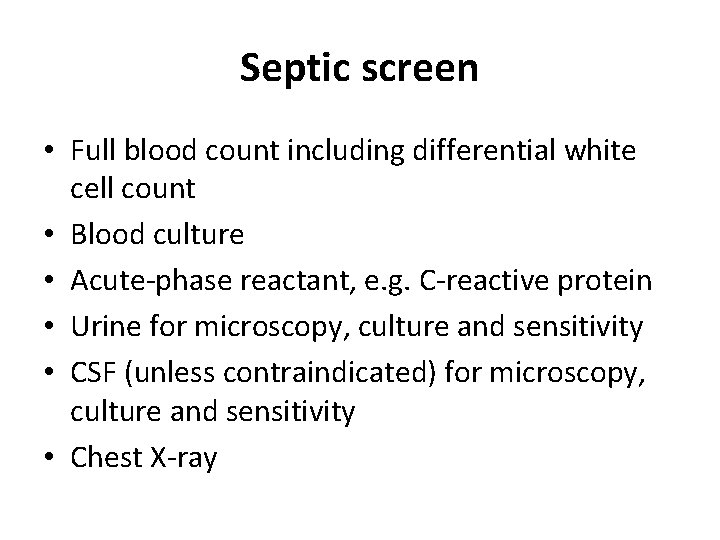
Septic screen • Full blood count including differential white cell count • Blood culture • Acute-phase reactant, e. g. C-reactive protein • Urine for microscopy, culture and sensitivity • CSF (unless contraindicated) for microscopy, culture and sensitivity • Chest X-ray
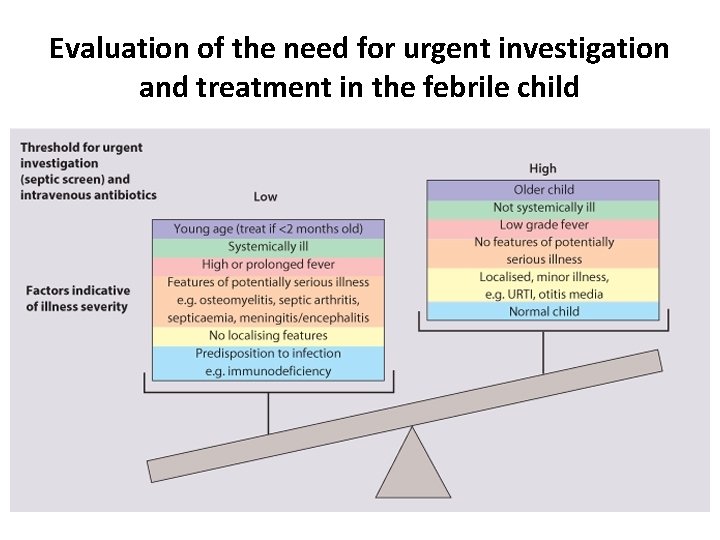
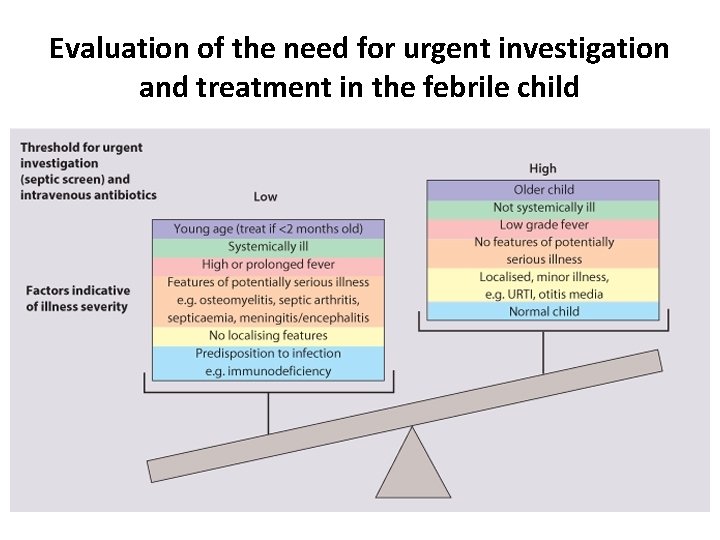
Evaluation of the need for urgent investigation and treatment in the febrile child

• Most children aged 0– 36 months without an obvious focus of infection have viral infections, but • they may harbor two important serious bacterial infections (SBI): urinary tract infection or bacteremia.
• Febrile neonates and ill-looking children, regardless of age, are at high risk for SBI and need antibiotic coverage, hospital admission, and comprehensive septic work-up. • This entails blood and urine cultures, full blood cell count (FBC), C-reactive protein (CRP), and, when indicated, chest X-ray, LP and stool studies.
• Children aged 1– 36 months without a focus may be treated more selectively: if the temperature is >39°C, WBC count is >15, 000 mm− 3 and CRP is >40 mg L− 1; urine and blood cultures should be ordered; and a thirdgeneration cephalosporin (ceftriaxone or cefotaxime) considered.

Fever without a focus a) Viremia • Fever not high + assessment is fair • Treatment by antipyretics & re-evaluation b) Bacteremia • High fever + assessment is sick • Investigations: CBC, CRP, ESR • Treatment by broad spectrum antibiotic and re-evaluate c) Septicemia • High fever + assessment is seriously ill • Urgent hospitalization, & investigations ( CBC, CRP, ESR, CSF, and cultures)
Criteria of sepsis • Leukocytosis> 15. 000 • Bandemia> 10% • Toxic granulation • Elevated ESR • Elevated CRP Treatment Combined Parenteral antibiotics (Ampicillin and gentamicin plus very close observation for complications)
Complications of septicemia: • Serious focal infections like meningitis • Septic shock, acute renal failure • Acute hemolytic anemia, DIC • Toxic enchephalopathy • Sclerema
(iii) Are there risk factors for infection? • • • Illness of other family members If a specific illness is prevalent in the community Unimmunized Recent travel abroad, e. g. malaria, typhoid Contact with animals, e. g. brucellosis. Increased susceptibility from immunodeficiency. – post-autosplenectomy in SCD or splenectomy – nephrotic syndrome, steroid therapy – primary immune deficiency.
(iv) How ill is the child? • • • Red Flag features suggesting serious illness and the need for urgent investigation and treatment are: Fever >38°C if <3 months, >39°C if 3 -6 months Colour - pale, mottled, blue Level of consciousness is reduced, neck stiffness, bulging fontanelle, status epilepticus, focal neurological signs or seizures Significant respiratory distress Bile-stained vomiting Severe dehydration or shock
Definitions of Terms • Fever …. . Rectal temperature of 38°C. • Fever without source ……Acute febrile illness in which the etiology of the fever is not apparent after a careful history and physical examination • Serious bacterial infection …. . Meningitis, sepsis, bone and joint infections, urinary tract infections, pneumonia, enteritis • Toxic appearance …. Clinical presentation characterized by lethargy, evidence of poor perfusion, cyanosis, hypoventilation or hyperventilation • Lethargy …. . Poor or absent eye contact; failure of child to recognize parents or to interact with persons or objects in the environment

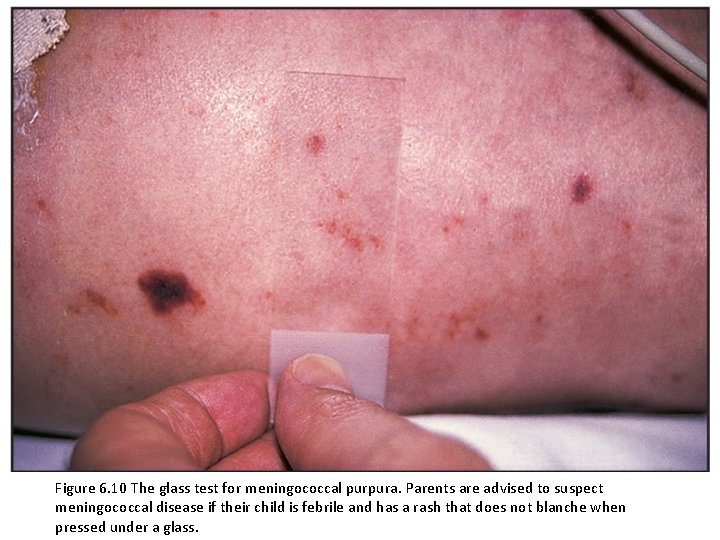
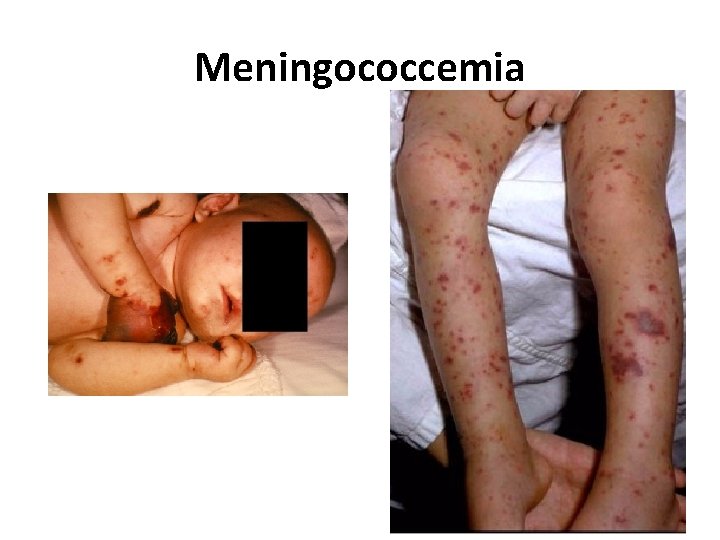
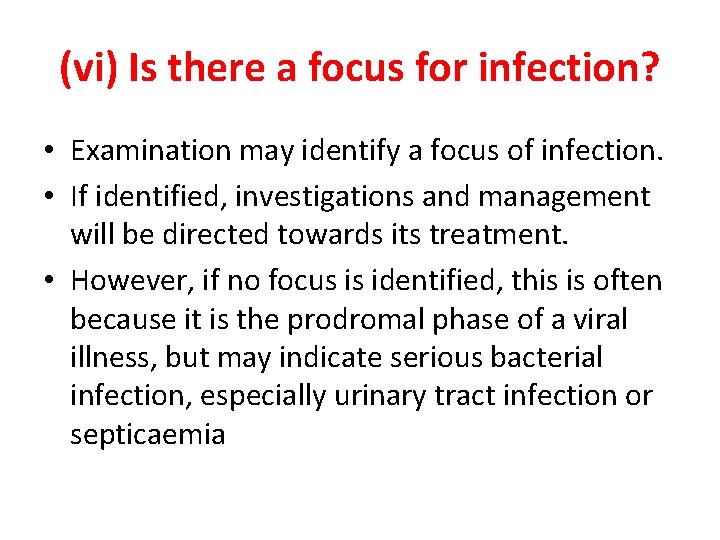
(v) Is there a rash? • Rashes often accompany febrile illnesses. • In some, the characteristics of the rash and other clinical features lead to a diagnosis, e. g. meningococcal septicemia.
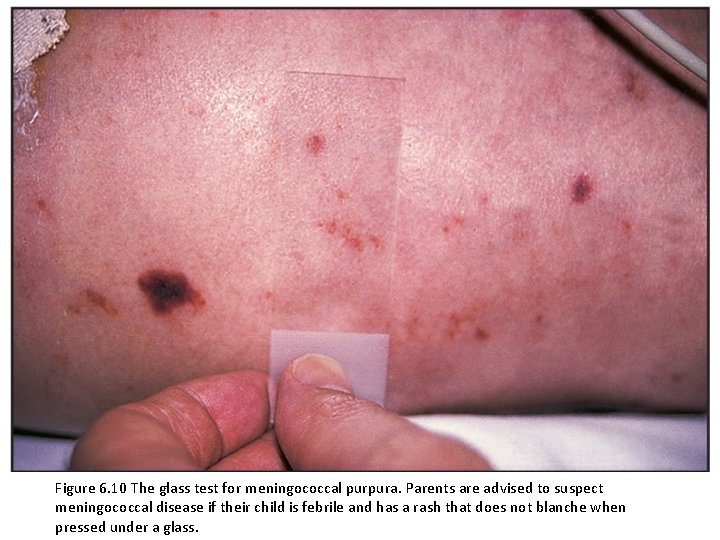
Figure 6. 10 The glass test for meningococcal purpura. Parents are advised to suspect meningococcal disease if their child is febrile and has a rash that does not blanche when pressed under a glass.
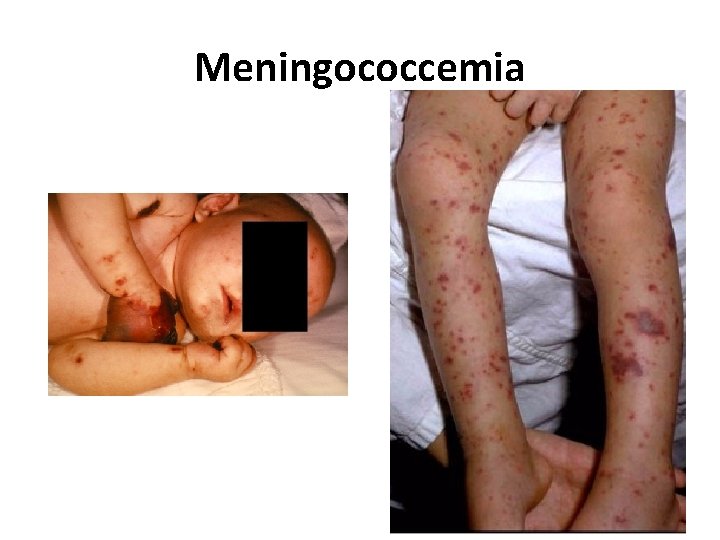
Meningococcemia

Meningococcemia

Meningococcemia
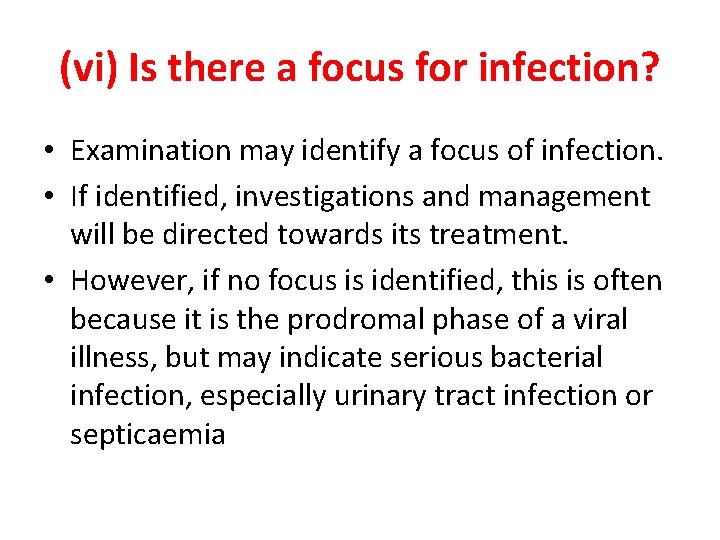
(vi) Is there a focus for infection? • Examination may identify a focus of infection. • If identified, investigations and management will be directed towards its treatment. • However, if no focus is identified, this is often because it is the prodromal phase of a viral illness, but may indicate serious bacterial infection, especially urinary tract infection or septicaemia

Fever - Symptoms • Signs and symptoms of fever may be obvious or subtle. • The younger the child, the more subtle the symptoms
Infants - Symptoms • • • Irritable Fussy Lethargic Quiet Feel warm or hot Not feed normally • Cry • Breathe rapidly • Exhibit changes in sleeping or eating habits • Seizure
Verbal children - Symptoms • Feeling hotter or colder than others in the room who feel comfortable • Body aches • Headache • Having difficulty sleeping or sleeping more • Poor appetite
Febrile seizure and lumbar puncture (LP) • LP strongly suggested in the first seizure in infants less than 12 month because signs and symptoms of meningitis may be absent in this age group • 12 -18 months LP strongly suggested because sign of meningitis may be subtle in this age group • 18+ months LP only if signs and symptoms of meningitis
Management • Children who are not seriously ill can be managed at home with regular review by the parents, as long as they are given clear instructions (e. g. what clinical features should prompt reassessment by a doctor). • Children who are significantly unwell, particularly if there is no focus of infection, will require investigations and observation or treatment in a pediatric assessment unit or A&E department or children's ward. A septic screen will be required.
Management • Parenteral antibiotics are given immediately to seriously unwell children, e. g. a third-generation cephalosporin such as cefotaxime or ceftriaxone if >3 months old. • In infants 1 -3 months old, cefotaxime (in case of septicemia or meningitis) and ampicillin (in case of Listeria infection) are usually given. • Acyclovir is given if herpes simplex encephalitis is suspected. Supportive care is given as indicated
Antipyretic Measures • Many parents aim for “normal” temperature – Daycare, school & work can drive this • Antipyretic therapy DOES NOT – Reduce morbidity or mortality from a febrile illness – Decrease the recurrence of febrile seizures • Antipyretic DOES – Relieve discomfort – Decrease insensible fluid loss

Antipyretic Measures • The child should not be overdressed. • The use of antipyretic agents should be considered in children with fever who appear distressed or unwell. • They should not be given if the child is otherwise well. • Either paracetamol or ibuprofen can be used. • They can be given alternatively if unresponsive to a single agent. • Evidence that antipyretics prevent febrile seizures is lacking.
Fever in Children - Treatment Self-Care at Home • The three goals of home care 1) Control the temperature 2) Prevent dehydration 3) Monitor for serious or life-threatening illness
1) Control the temperature • A warm water bath can also be helpful but should be used for no more than 10 minutes each hour. • Acetaminophen (10 -15 mg/kg/dose) and ibuprofen (5 -10 mg /kg/dose) are used to reduce fever
• Do not use aspirin to treat fever in children, especially for a fever with chickenpox or other viral infection. • Aspirin has been linked to liver failure in some children (Reye syndrome). • Children should not be overdressed indoors, even in the winter.
• Adjunctive measures – Rest – Comfortable surroundings: temperature (22 o C) – Not bundled in extra clothing or blankets – Sponging with tepid water (temperature around 27 o C) – Ice baths or alcohol should be avoided
2) Prevent dehydration • Encourage the child to drink clear fluids (not water). Water does not contain the necessary electrolytes and glucose. • Reduce the child's temperature & give enough clear fluids
3) Monitor for serious or lifethreatening illness • If child still appears ill…. . Ask for medical help

Fever of unknown origin Definition • Fever > 10 -14 days without evident cause despite H/O & exam • Documentation is the first step • Accurate history, careful exam and directed investigations • Non specific criteria of significant illness are anorexia, wt loss, toxic look, pallor
Management of FUO 1) Hospitalization : Observation/ no drugs 2) Investigations Initial : • CBC, ESR, CRP • Cultures of blood& urine • Chest x-ray, Widal test, monospot(IMN) Further • US abdomen, echocardiography • BM exam, LN biopsy

Management of FUO 3) Blind empirical therapy • Better avoided • Blind antibiotic treatment in sick septic patients with –ve cultures • Blind anti-TB treatment in sick patients with suspected unproven TB
Key points Fever is a normal physiologic response Most fevers are of short duration and benign Treat discomfort NOT fever Monitor for signs/symptoms that require an intervention or suggest a more serious illness • Provide education at well-child visits • •
Key points • Serious bacterial infection must be considered if there is no focus of infection, especially urinary tract infection or septicemia, or there are Red Flag features of life-threatening illness • The younger the child, the lower the threshold for performing a septic screen and starting antibiotics
Key points • Infections are the most common cause of fever in children • During assessment of a child with fever, pay close attention to vital sign changes, overall appearance, and potential sites of infection • Closely monitor for clinical decompensation after antibiotic administration, particularly in patients at high-risk of developing sepsis
Questions • Practical ways of checking body temperature in a small infant include the following EXCEPT: a) Tympanic b) Oral c) Axillary d) Rectal
Case Study • A 7 -month-old infant presents with fever, evolving purpura and poor peripheral perfusion. Intravenous access is obtained with difficulty and a bolus of normal saline is given. • Q: What is the best first action to be taken next? a) Perform a lumbar puncture b) Start intravenous antibiotics c) Prescribe chemoprophylaxis for the staff d) Take a swab from a purpuric lesion
• The following antibiotics will effectively cross the blood/brain barrier and can be given intravenously to treat bacterial meningitis EXCEPT: a) Benzyl penicillin b) Gentamicin c) Cefotaxime d) Chloramphenicol

Thank You
 Maitre hesham
Maitre hesham Professor nasser mohamed
Professor nasser mohamed Promotion from associate professor to professor
Promotion from associate professor to professor Left child right child tree representation
Left child right child tree representation Mohamed merchant
Mohamed merchant Mohamed homayed death
Mohamed homayed death Mohamed younis umbc
Mohamed younis umbc Mohamed salah
Mohamed salah Mohamed fayad sjsu
Mohamed fayad sjsu Mohammad diab md
Mohammad diab md Orhán
Orhán Mohamed dahoui
Mohamed dahoui Parallel computing nyu
Parallel computing nyu Abdelrahman mohamed
Abdelrahman mohamed Mohamed samir design
Mohamed samir design Mohamed akel
Mohamed akel Muhamed computer technology
Muhamed computer technology Mr mohamed chafik el idrissi
Mr mohamed chafik el idrissi Mohamed akel
Mohamed akel Abukar mohamed
Abukar mohamed Mohamed younis umbc
Mohamed younis umbc Yahye mohamed omar
Yahye mohamed omar Omar requirements
Omar requirements Lodacain
Lodacain Henintsoa georges
Henintsoa georges Dr mohamed bashar shala
Dr mohamed bashar shala Mohamed hassoun
Mohamed hassoun Hassan fareed physics
Hassan fareed physics Mohamed el merouani
Mohamed el merouani Mohamed hmiden
Mohamed hmiden Mohamed akel
Mohamed akel Mohamed
Mohamed Mohamed younis umbc
Mohamed younis umbc Mohamed younis umbc
Mohamed younis umbc Dr mohamed eldeib
Dr mohamed eldeib Dr mohamed nasr
Dr mohamed nasr Parallel computing nyu
Parallel computing nyu Mohamed kossentini
Mohamed kossentini Dr alboushi
Dr alboushi Fahma mohamed
Fahma mohamed Hopital mohamed seghir nekkache
Hopital mohamed seghir nekkache Prophet pbuh family tree
Prophet pbuh family tree Mohamed akel
Mohamed akel Riham mohamed aly
Riham mohamed aly Bouhicha mohamed
Bouhicha mohamed Mohamed younis umbc
Mohamed younis umbc Diana spencer accident de voiture
Diana spencer accident de voiture Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ độ dài liên kết
độ dài liên kết Voi kéo gỗ như thế nào
Voi kéo gỗ như thế nào Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau điện thế nghỉ
điện thế nghỉ Một số thể thơ truyền thống
Một số thể thơ truyền thống Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Ng-html
Ng-html Hệ hô hấp
Hệ hô hấp Các số nguyên tố
Các số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Tư thế worms-breton
Tư thế worms-breton ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Tư thế ngồi viết
Tư thế ngồi viết Cái miệng nó xinh thế
Cái miệng nó xinh thế Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Bổ thể
Bổ thể Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Tư thế ngồi viết
Tư thế ngồi viết V. c c
V. c c Thơ thất ngôn tứ tuyệt đường luật
Thơ thất ngôn tứ tuyệt đường luật Hát lên người ơi alleluia
Hát lên người ơi alleluia Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Diễn thế sinh thái là
Diễn thế sinh thái là đại từ thay thế
đại từ thay thế Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Phép trừ bù
Phép trừ bù