Marseilles fever Marseilles fever a disease common in





- Slides: 25

Marseilles fever

• Marseilles fever - a disease (common in India and around the Mediterranean area) caused by a rickettsia that is transmitted to humans by a reddish brown tick (ixodid) that lives on dogs and other mammals.
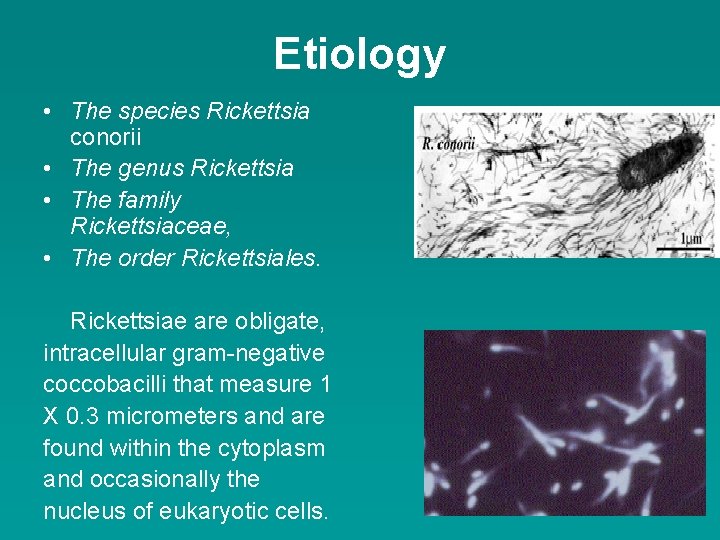
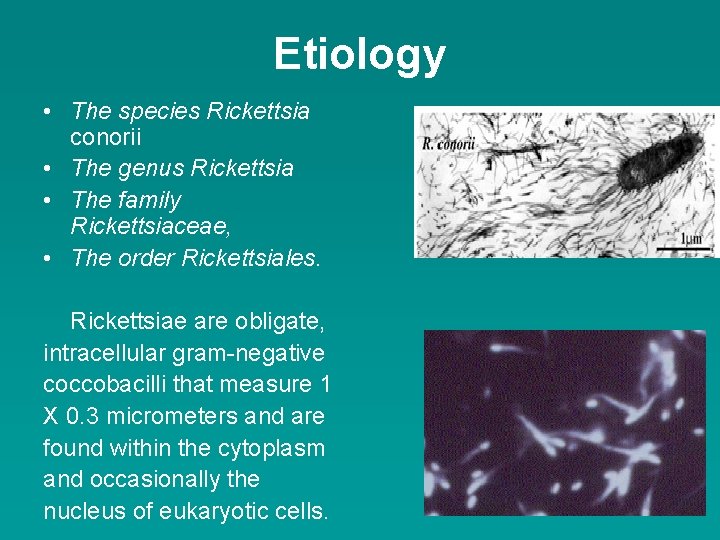
Etiology • The species Rickettsia conorii • The genus Rickettsia • The family Rickettsiaceae, • The order Rickettsiales. Rickettsiae are obligate, intracellular gram-negative coccobacilli that measure 1 X 0. 3 micrometers and are found within the cytoplasm and occasionally the nucleus of eukaryotic cells.
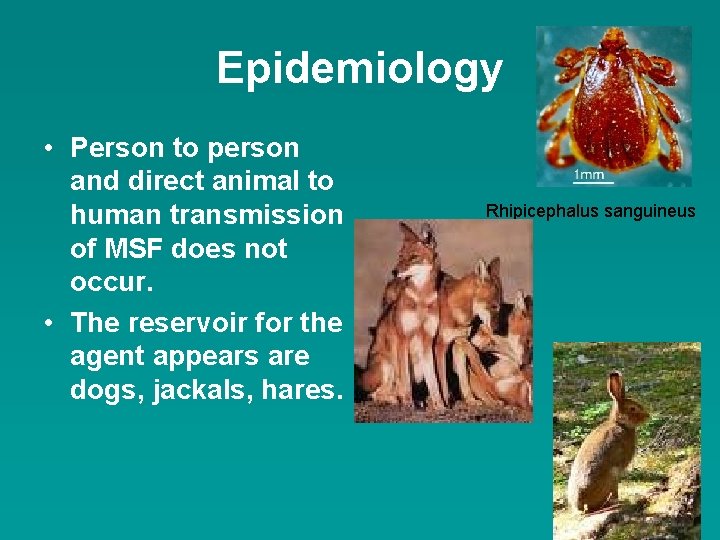
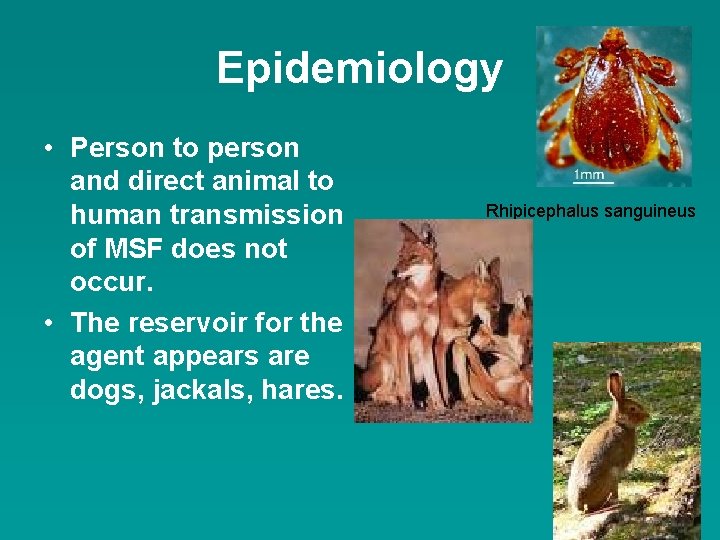
Epidemiology • Person to person and direct animal to human transmission of MSF does not occur. • The reservoir for the agent appears are dogs, jackals, hares. Rhipicephalus sanguineus
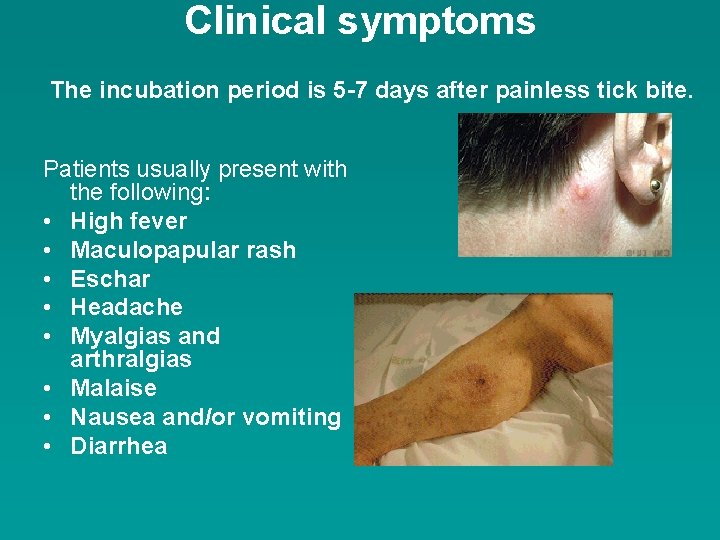
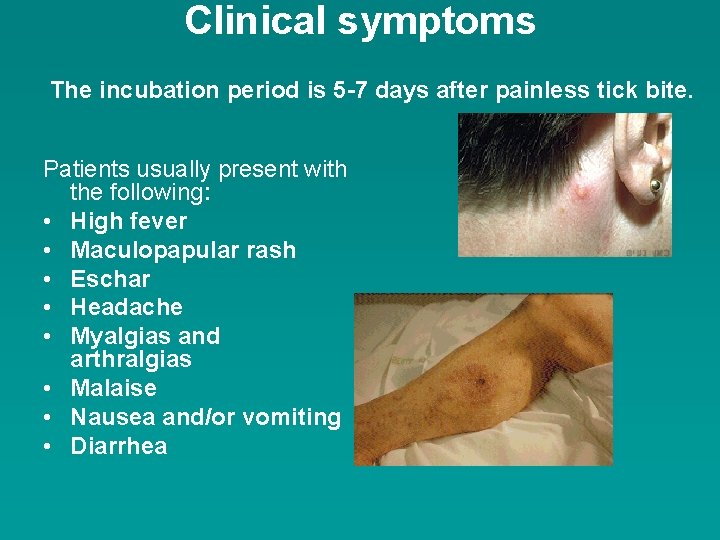
Clinical symptoms The incubation period is 5 -7 days after painless tick bite. Patients usually present with the following: • High fever • Maculopapular rash • Eschar • Headache • Myalgias and arthralgias • Malaise • Nausea and/or vomiting • Diarrhea
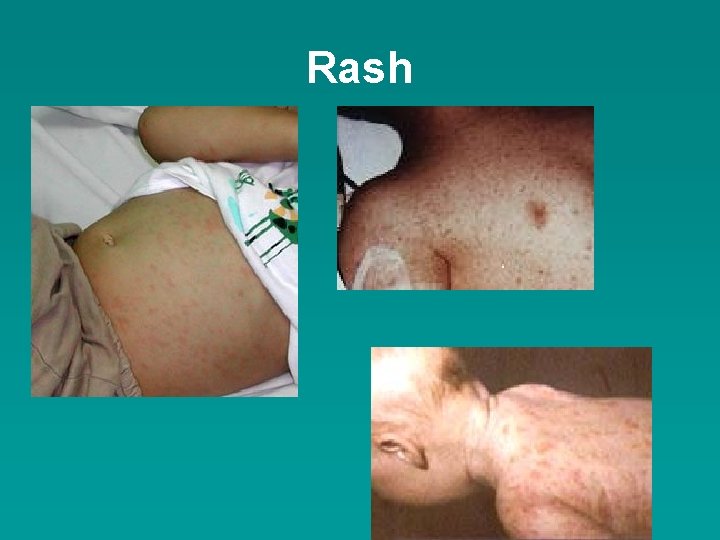
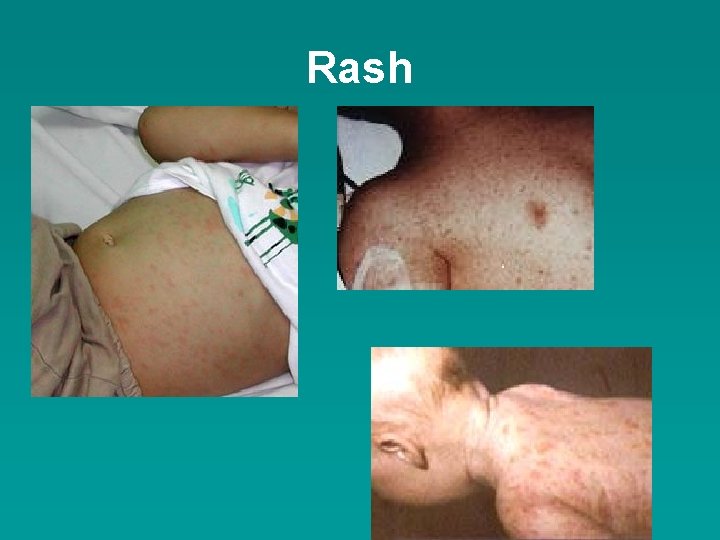
Rash
Pigmentation
Laboratory diagnostics • Serologic assays sometimes are difficult to interpret, since extensive cross-reactivity exists between members of the spotted fever group. • Occasionally, the organism can be isolated from blood or skin biopsy at the eschar site.
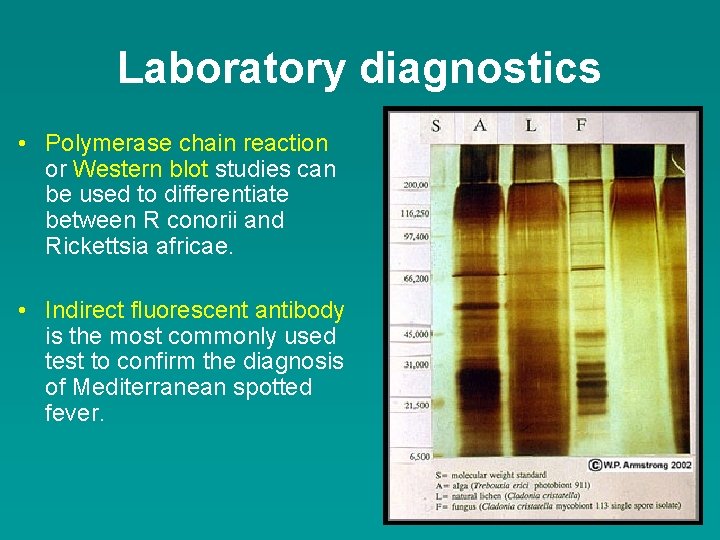
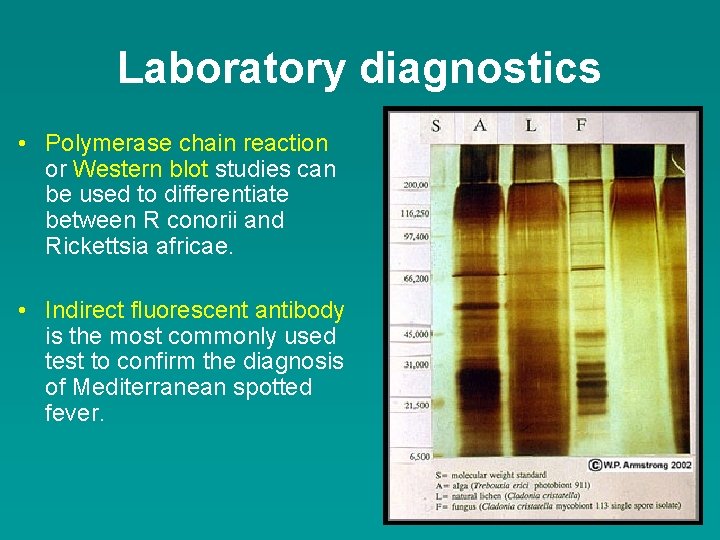
Laboratory diagnostics • Polymerase chain reaction or Western blot studies can be used to differentiate between R conorii and Rickettsia africae. • Indirect fluorescent antibody is the most commonly used test to confirm the diagnosis of Mediterranean spotted fever.
Laboratory diagnostics • R conorii may be cultured from blood samples using Vero cells, primary chicken embryo, fibroblast, and other cell lines or by intraperitoneal inoculation of adult male guinea pigs.
The treatment • Doxycycline (100 mg PO q 12 h). • Other effective treatments include the following: • Ciprofloxacin (200 mg IV q 12 h or 750 mg PO q 12 h) • Levofloxacin (500 mg PO qd) • Chloramphenicol (50 -60 mg/kg/d PO q 6 h in 4 divided doses) • Macrolides such as azithromycin (500 mg PO qd) and clarithromycin (500 mg PO bid) have been shown to be efficacious in children and can be used as alternatives to doxycycline in adults.
Prevention • To prevent infection by rickettsiae, precautions should be taken to avoid contact with ticks. • Protective clothing should be worn, preferably impregnated with permethrin or another pyrethroid. • Topical repellents can be used on any exposed skin; however, frequent application is recommended because of short-lasting effect of approximately 1 -2 hours per application. • Daily self-checks and removal of ticks should be performed during travel.

Q fever (Coxiella burnetii infections) • Q fever is a disease caused by infection with Coxiella burnetii, a bacterium that affects both humans and animals.
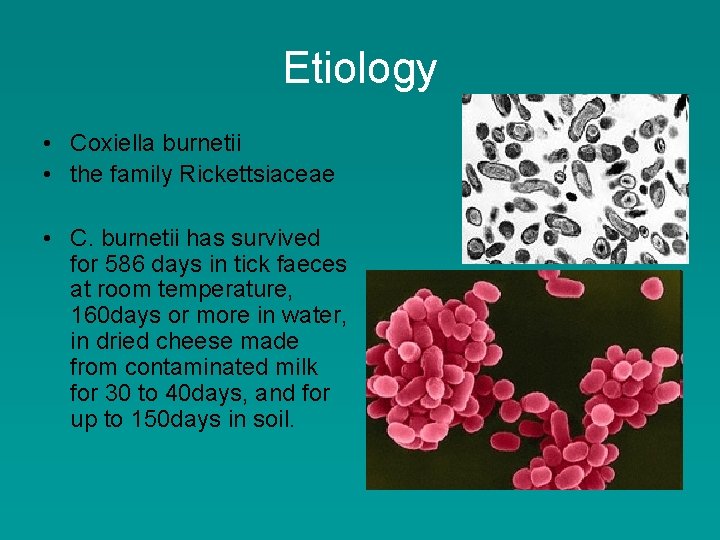
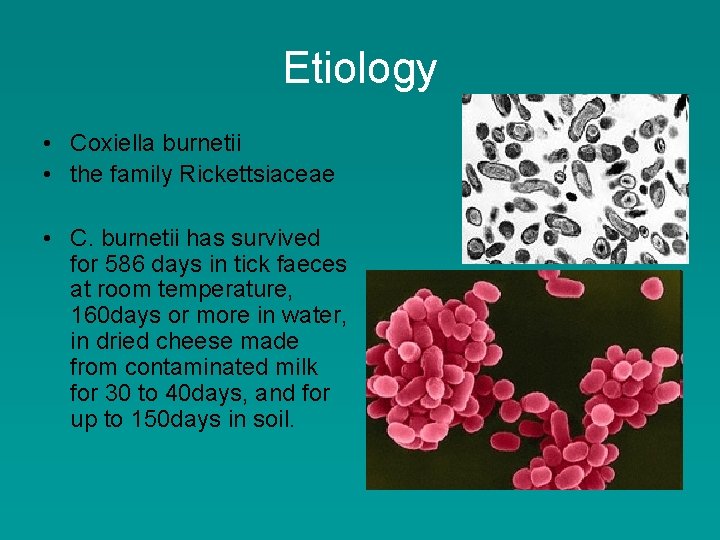
Etiology • Coxiella burnetii • the family Rickettsiaceae • C. burnetii has survived for 586 days in tick faeces at room temperature, 160 days or more in water, in dried cheese made from contaminated milk for 30 to 40 days, and for up to 150 days in soil.
Epidemiology • Q fever is a zoonosis. • There is an extensive wild-life and arthropod (mainly ticks) reservoir of C. burnetii. • Domestic animals are infected through inhalation of contaminated aerosols or by ingestion of infected material. • These animals rarely become ill but abortion and stillbirths may occur. • Infected cows have shed C. burnetii in milk for up to 32 months while sheep shed the organism in faeces for 11 to 18 days postpartum. • Infected cattle, sheep, and goats are the animals primarily responsible for transmitting C. burnetii to man. • In Atlantic Canada, infected parturient cats spread this microorganism to man.

The group of risk • • • veterinary personnel stockyard workers farmers shearers animal transporters laboratory workers handling potentially infected veterinary samples or visiting abattoirs • people who cull and process kangaroos • hide (tannery) workers.
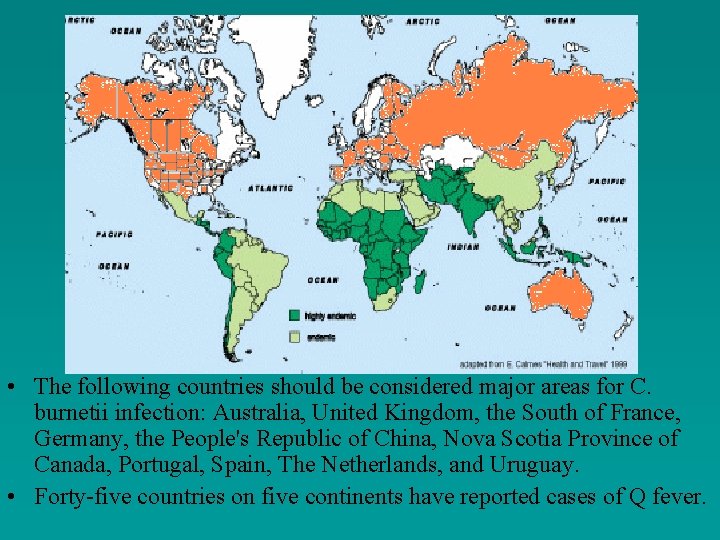
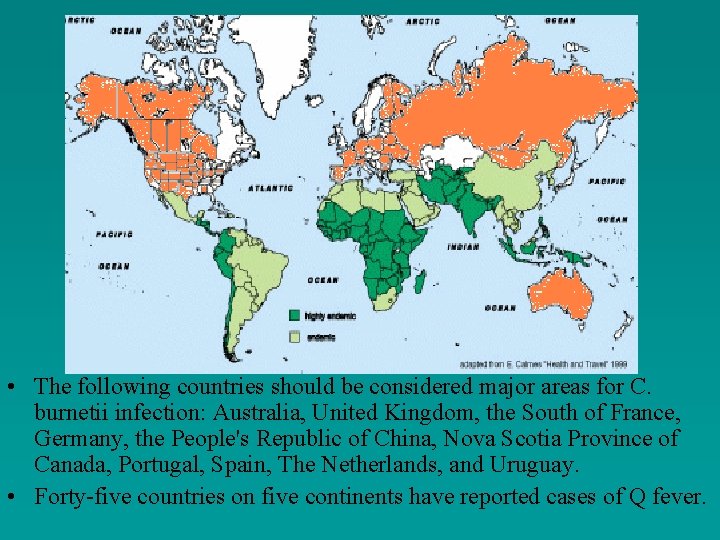
• The following countries should be considered major areas for C. burnetii infection: Australia, United Kingdom, the South of France, Germany, the People's Republic of China, Nova Scotia Province of Canada, Portugal, Spain, The Netherlands, and Uruguay. • Forty-five countries on five continents have reported cases of Q fever.
CLINICAL FEATURES • There is an incubation period of about 2 weeks (range 2 -29 days) following inhalation of C. burnetii. • The resulting illness in man can be divided into acute and chronic varieties.
Acute Q fever • fever, • fatigue, • headache, which may be very severe, occasionally so severe that it prompts a lumbar puncture. • A dry cough, • pleuritic chest pain, • nausea, vomiting, diarrhoea. • pneumonia • haematuria
Neurological manifestations • • • Encephalitis, encephalomyelitis, toxic confusional states, optic neuritis, demyelinating polyradiculoneuritis
Chronic Q fever • • endocarditis. fever Hepatomegaly or A purpuric rash Hyperglobulinaemia osteomyelitis, infection of aortic aneurysm, infection of vascular prosthetic grafts.
DIAGNOSIS • Serological tests: Øcomplement fixation, Ømicroimmunofluorescence, Øenzyme immunoassay.

X-ray Allergic test
TREATMENT • Tetracyclines and trimethoprimsulphamethoxazole. • Acute Q fever is treated with a 2 -week course of tetracycline, doxycycline, or trimethoprim-sulphamethoxazole. • Chronic Q fever should be treated with two antimicrobial agents for at least 2 years.
PREVENTION • A formalin-inactivated C. burnetii, wholecell vaccine - Q-Vax. • The intradermal vaccination is composed of killed Coxiella burnetii organisms. • control of ectoparasites on livestock.
 Marseilles fever
Marseilles fever Edith wharton mythology
Edith wharton mythology Dahilan ng paglalakbay ni rizal sa ibang bansa
Dahilan ng paglalakbay ni rizal sa ibang bansa Outline map of france bordeaux nantes paris marseilles
Outline map of france bordeaux nantes paris marseilles Communicable disease and non communicable disease
Communicable disease and non communicable disease Common factors of 12 and 42
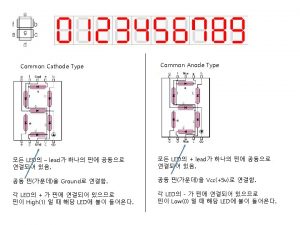
Common factors of 12 and 42 Common anode and common cathode
Common anode and common cathode Highest common factors and lowest common multiples
Highest common factors and lowest common multiples Factors of 72
Factors of 72 What are the factors for 54
What are the factors for 54 What is the greatest common factor of 18, 36, and 90?
What is the greatest common factor of 18, 36, and 90? Kinectio
Kinectio Sublingual temperature
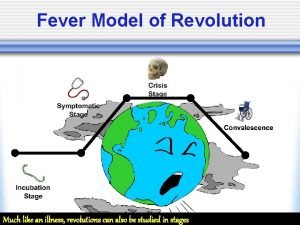
Sublingual temperature The fever model of revolutions
The fever model of revolutions Fever 1793 chapter 24
Fever 1793 chapter 24 Fever in copd
Fever in copd Rheumatic fever
Rheumatic fever Black water fever caused by
Black water fever caused by Typhoid symptoms
Typhoid symptoms Saturday night fever meaning
Saturday night fever meaning Introduction of typhoid fever
Introduction of typhoid fever Causes of viral hemorrhagic fever
Causes of viral hemorrhagic fever My love is as a fever
My love is as a fever Defenition of fever
Defenition of fever Post op fever day 1
Post op fever day 1 Stages of a fever
Stages of a fever