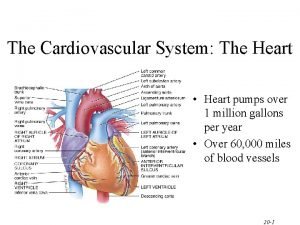
Heart Structure Heart located in mediastinum within the
















- Slides: 66
Heart Structure
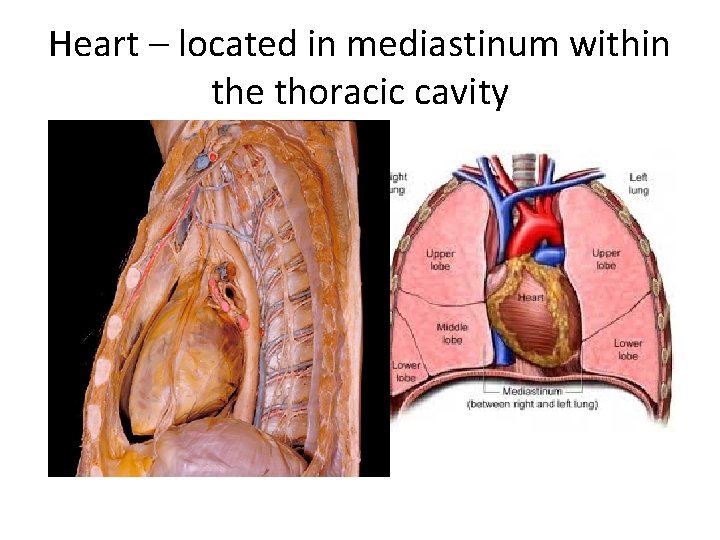
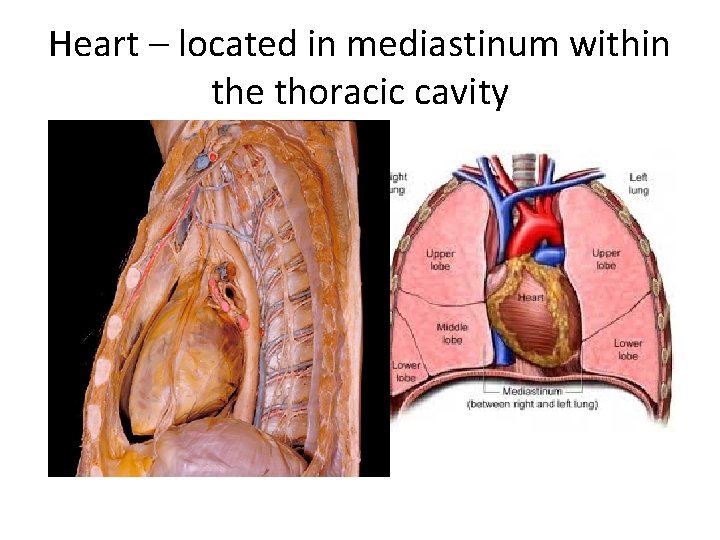
Heart – located in mediastinum within the thoracic cavity
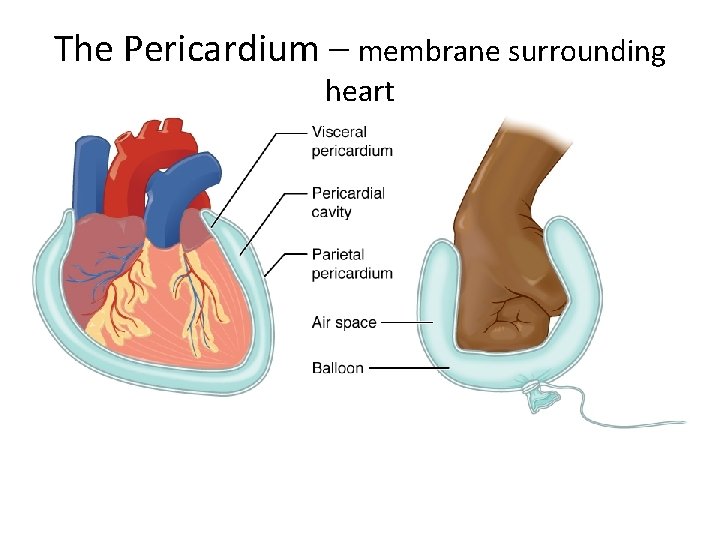
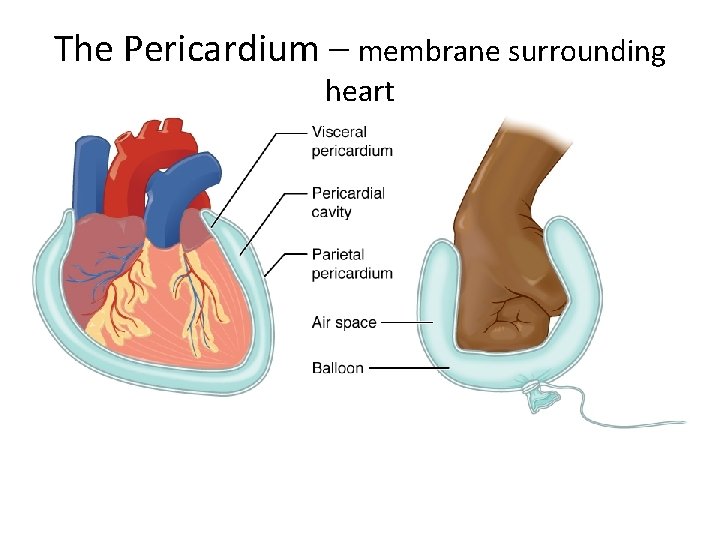
The Pericardium – membrane surrounding heart
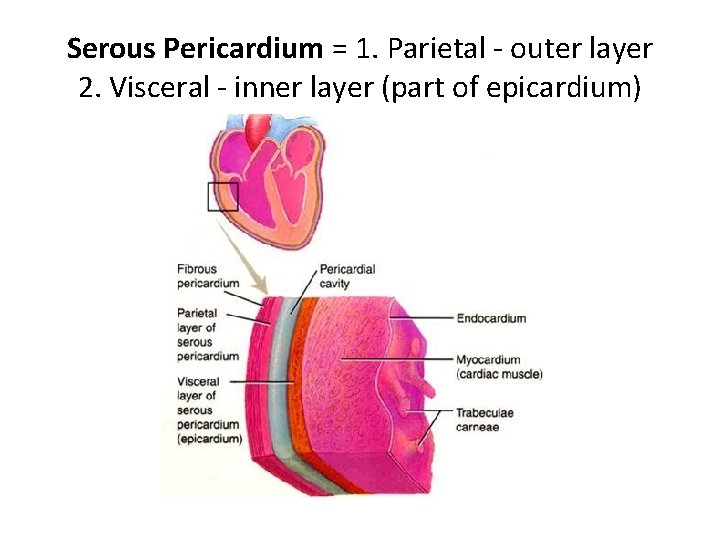
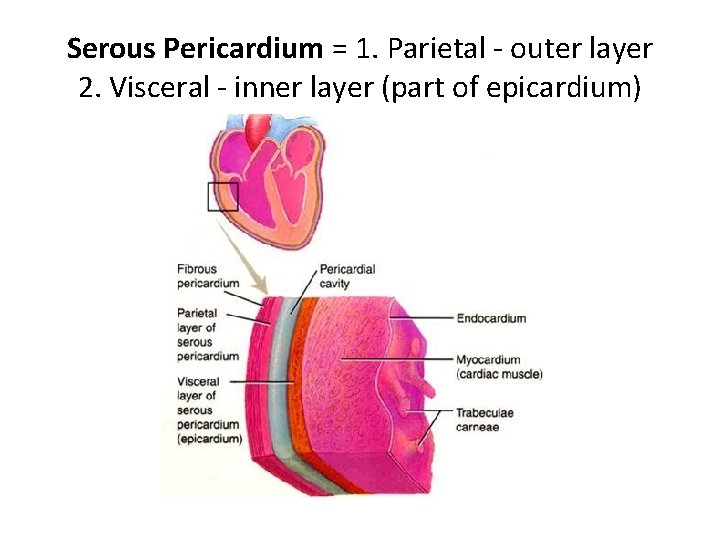
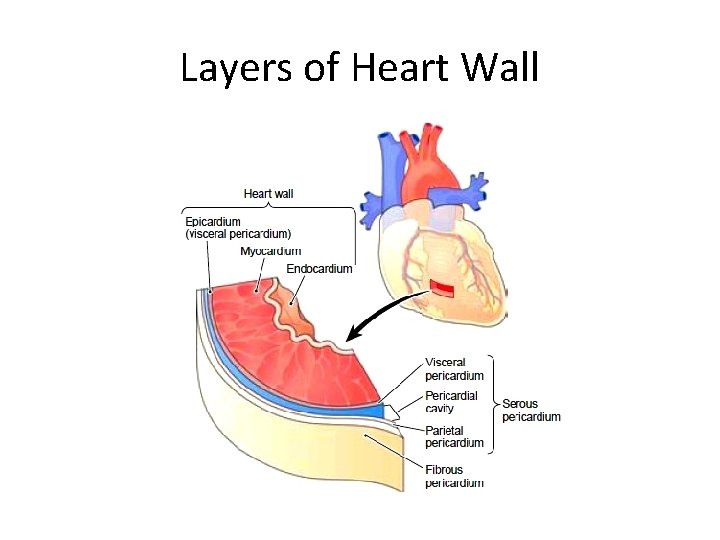
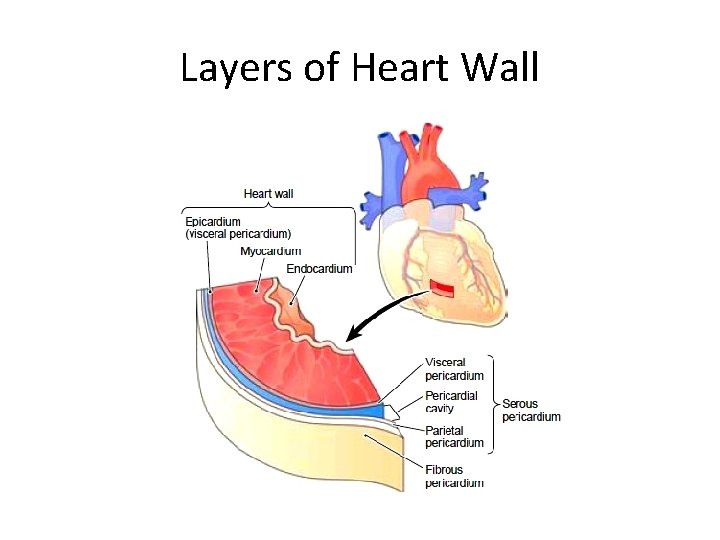
Serous Pericardium = 1. Parietal - outer layer 2. Visceral - inner layer (part of epicardium)
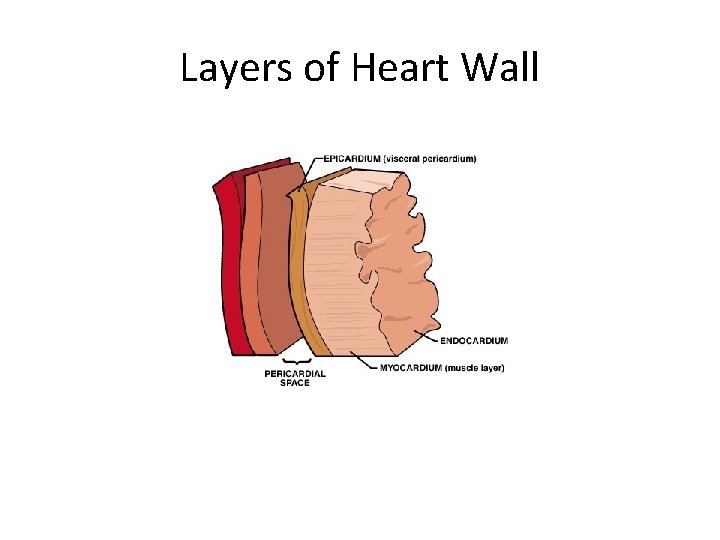
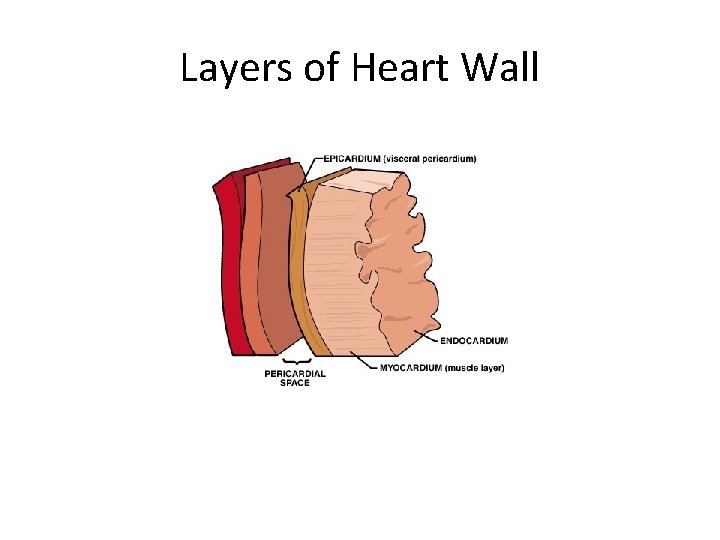
Layers of Heart Wall • Epicardium – outermost layer – synonymous with visceral portion of serous membrane • Myocardium – middle layer – Cardiac muscle – Pumping chamber • Endocardium – innermost layer – Smooth surface to reduce friction
Layers of Heart Wall
Layers of Heart Wall
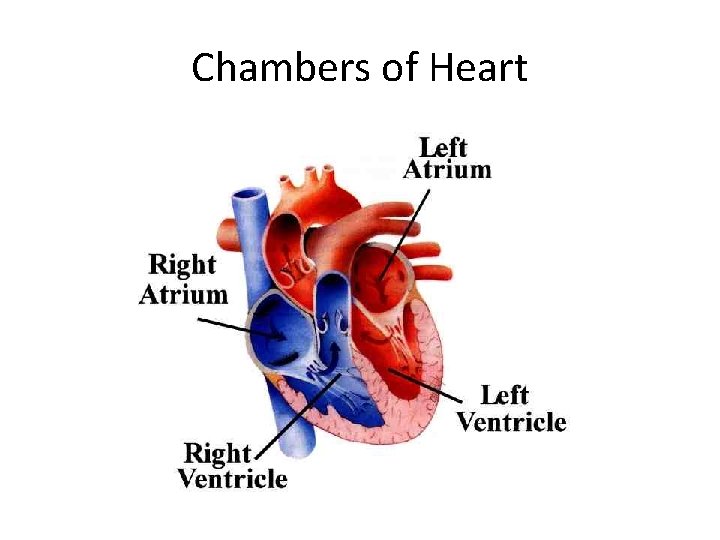
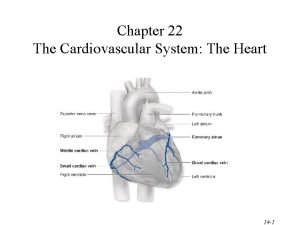
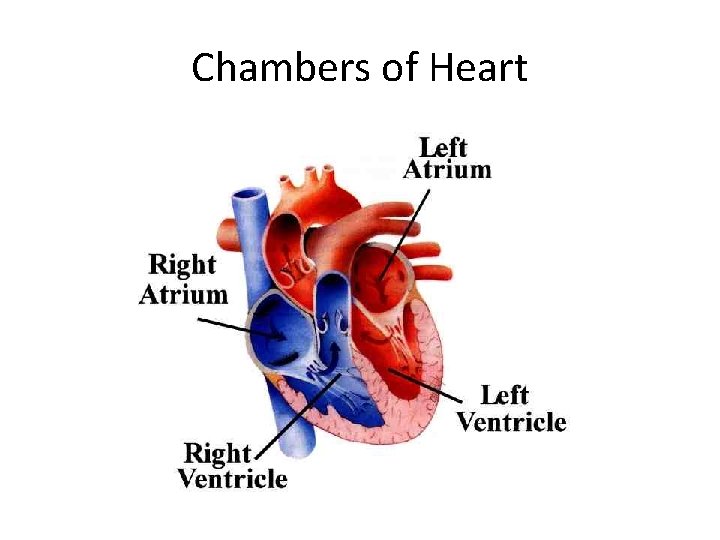
Chambers of Heart
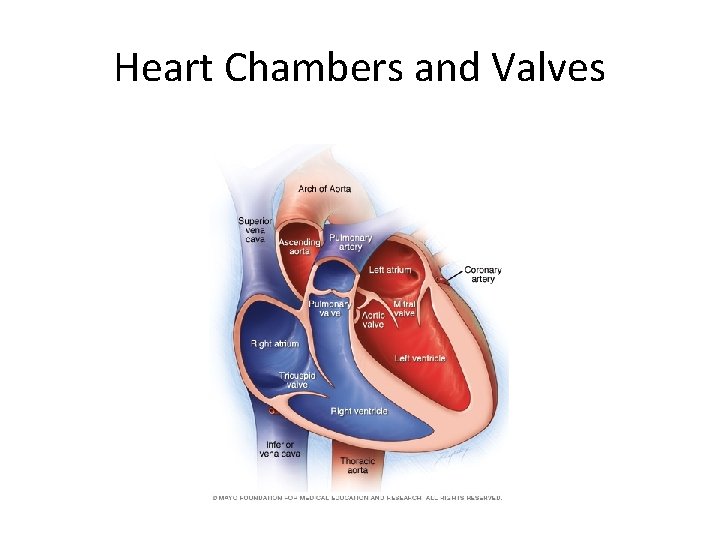
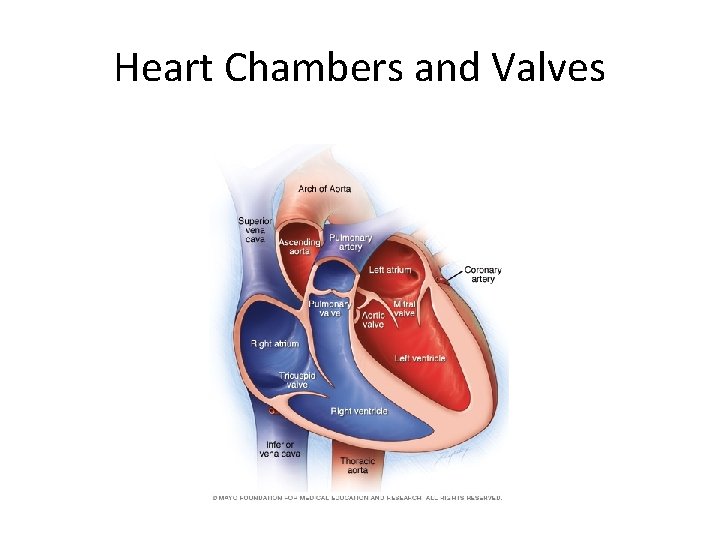
Heart Chambers and Valves
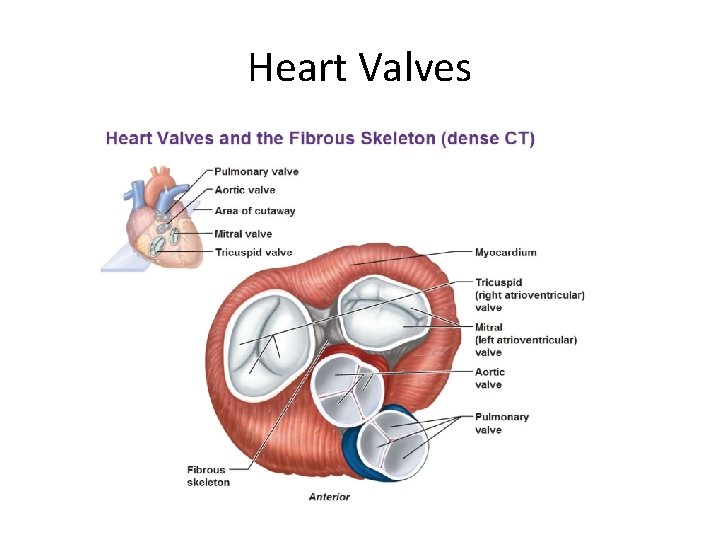
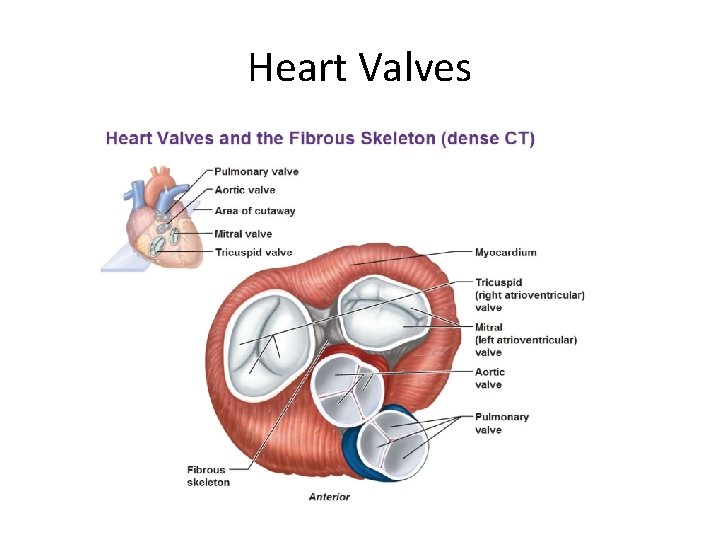
Heart Valves
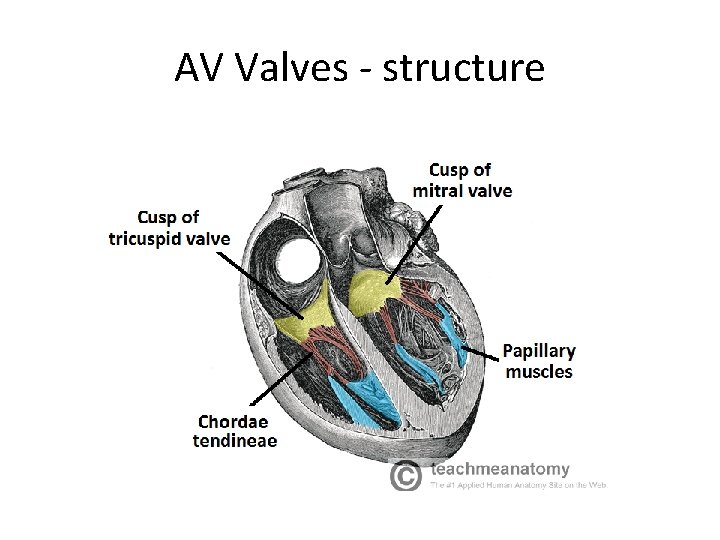
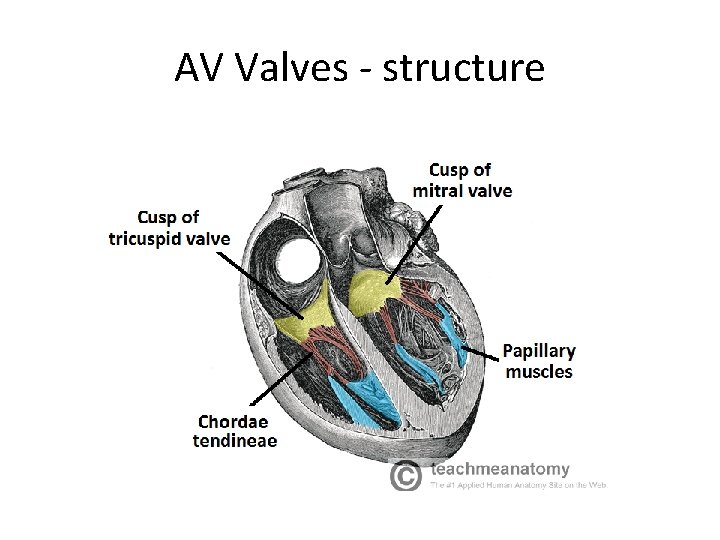
AV Valves - structure

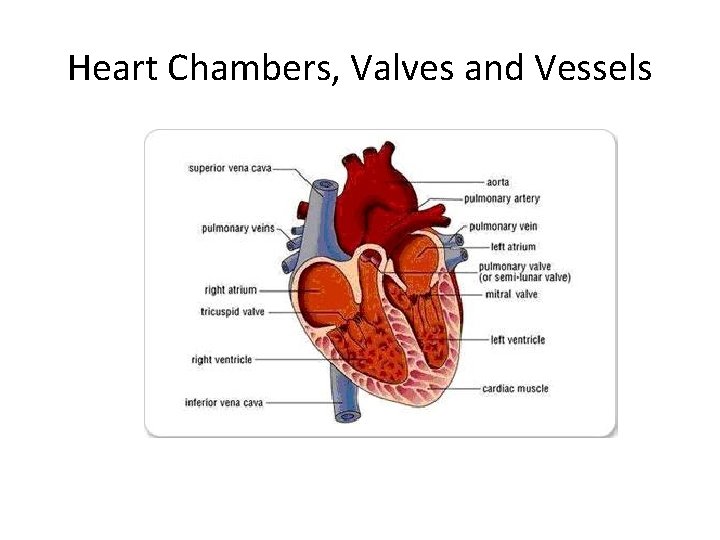
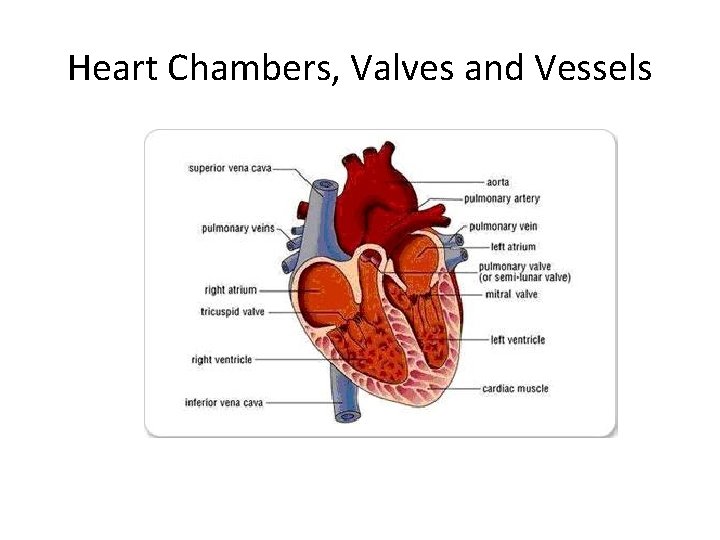
Heart Chambers, Valves and Vessels
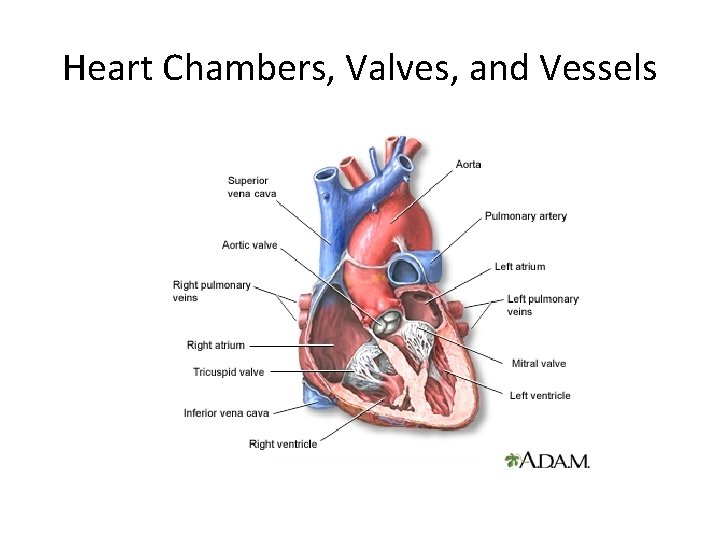
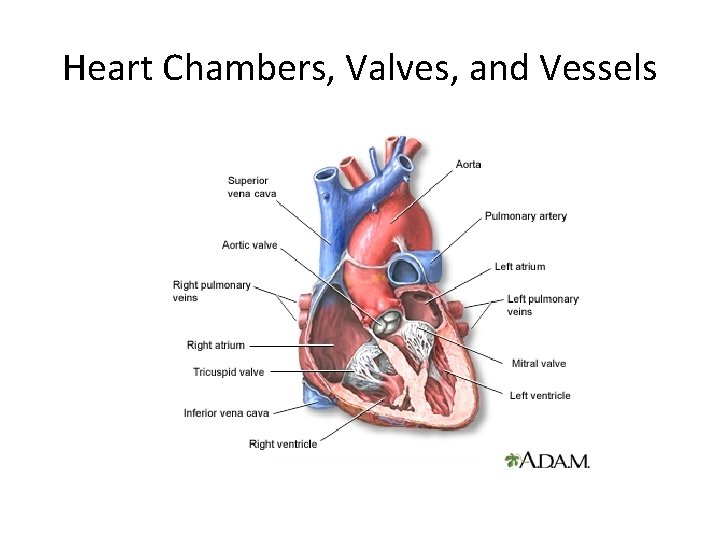
Heart Chambers, Valves, and Vessels
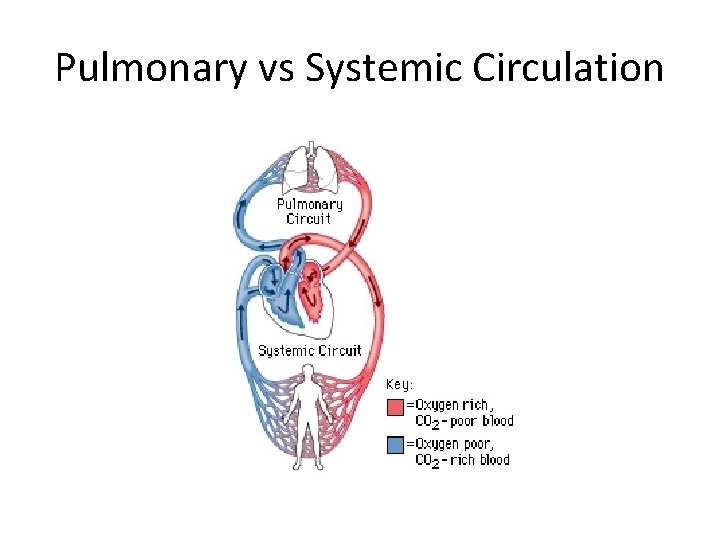
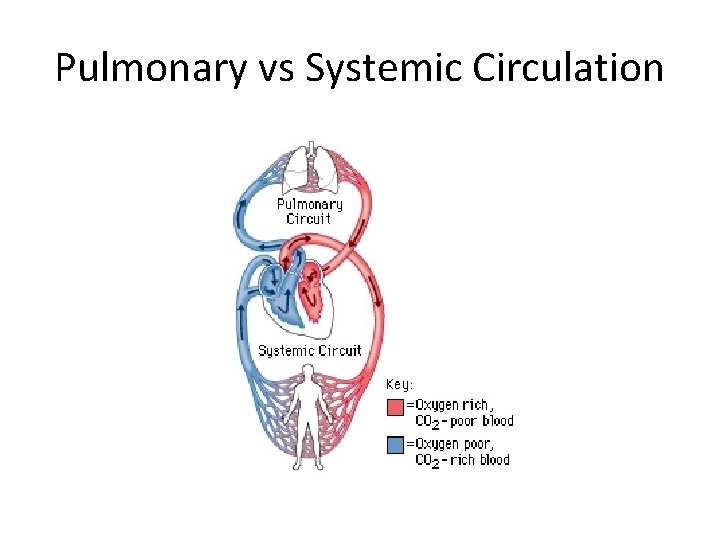
Pulmonary vs Systemic Circulation

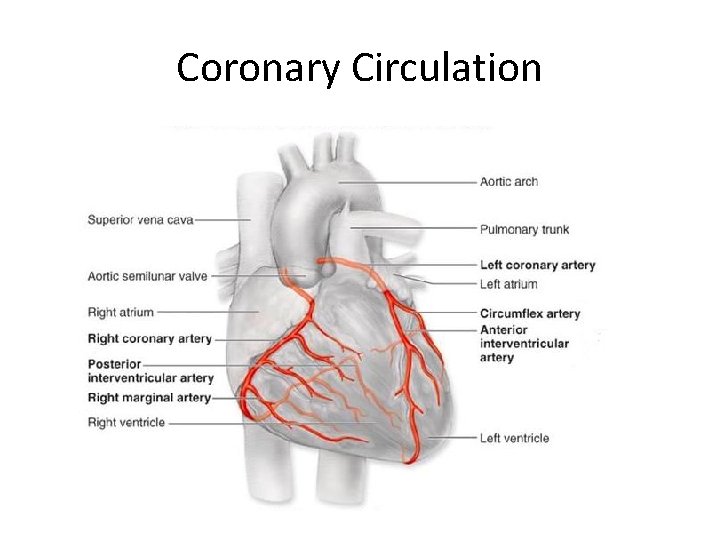
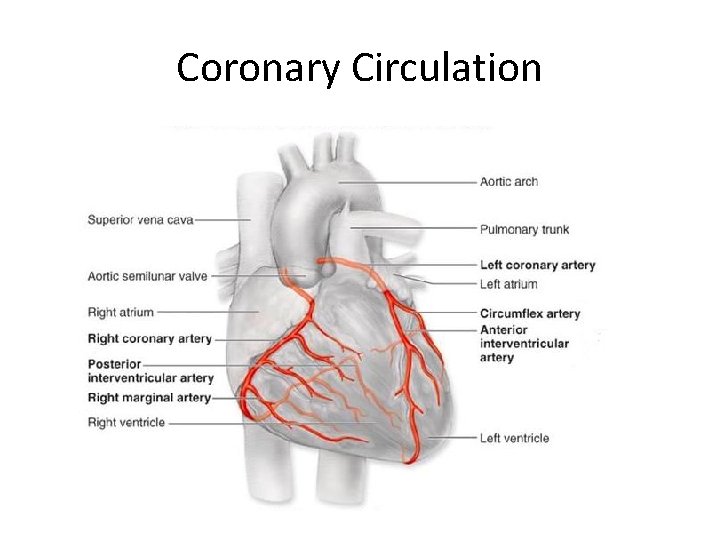
Coronary Circulation
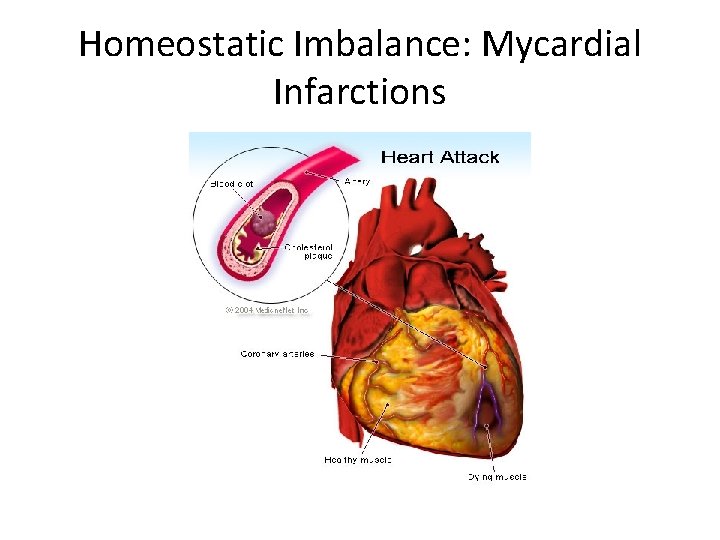
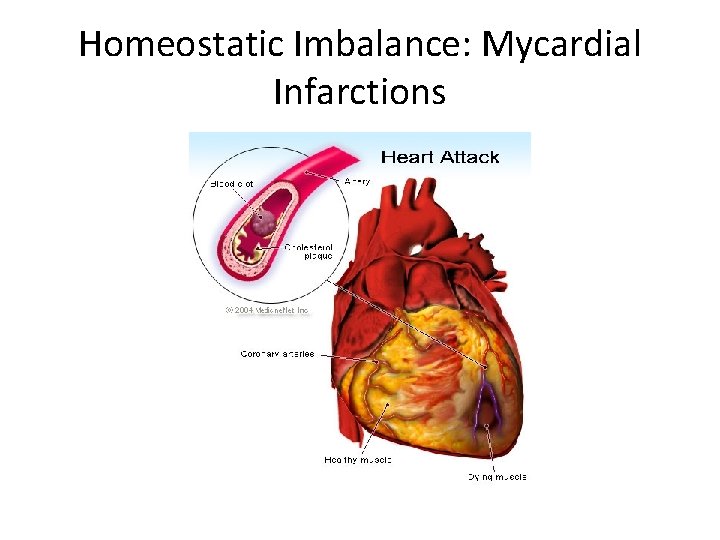
Homeostatic Imbalance: Mycardial Infarctions

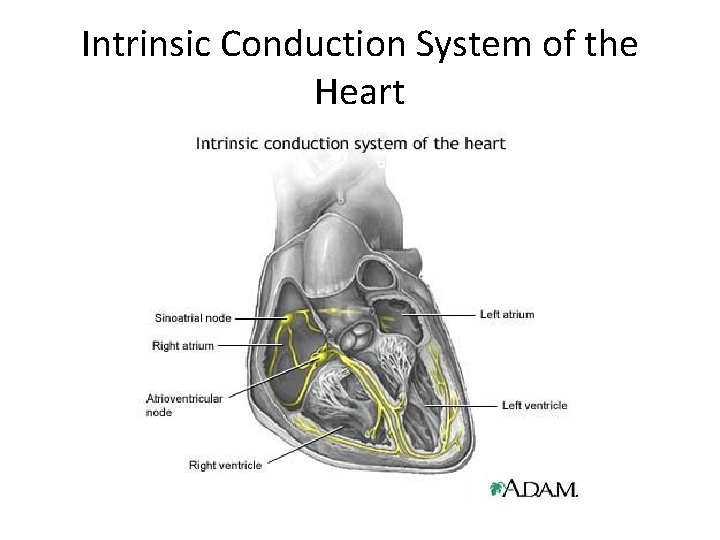
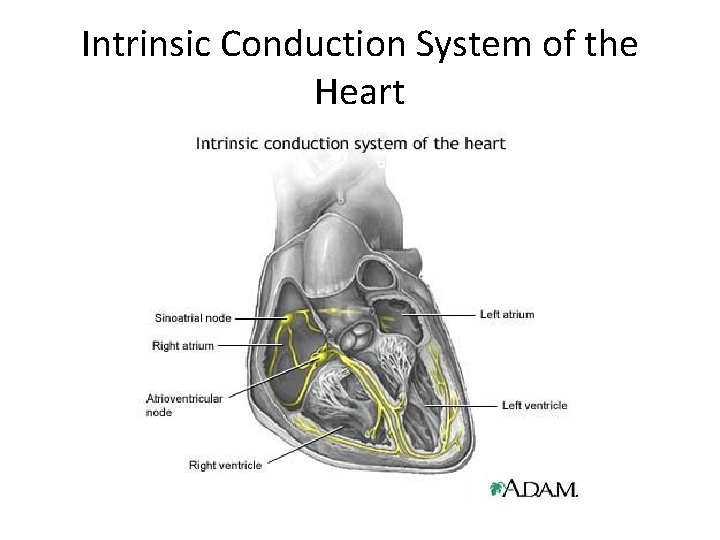
Intrinsic Conduction System of the Heart

Intrinsic Conduction System • Also called nodal system • Sinoatrial (SA) Node = pacemaker Atria Contract Atrioventricular (AV) Node • Brief Delay Atrioventricular bundle (bundle of His) Bundle branches Purkinje fibers Contraction of ventricle from bottom up Blood pushed out of ventricles

Homeostatic Imbalances • Heart block = Damage to AV node which allows ventricles to pump at own rate, which is typically slower than normal • Fibrillation = rapid uncoordinated shuddering of heart muscle, makes heart useless, major cause of death from heart attacks • Tachycardia = rapid heart rate +100 bpm • Bradycardia = slow heart rate < 60 bpm
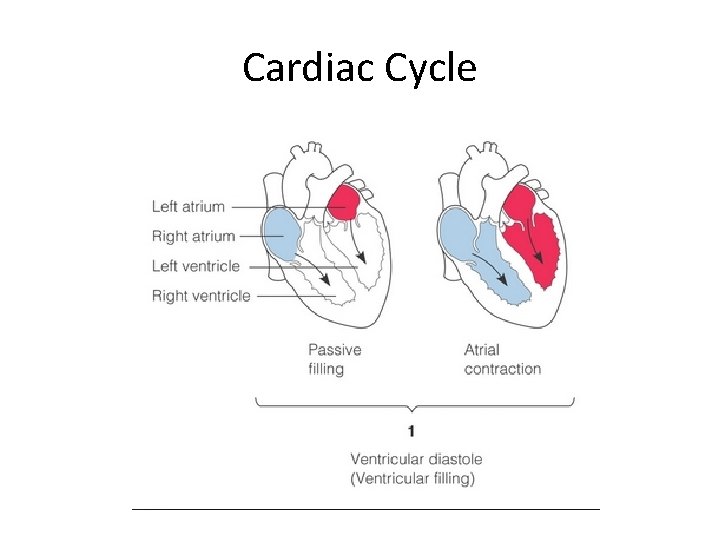
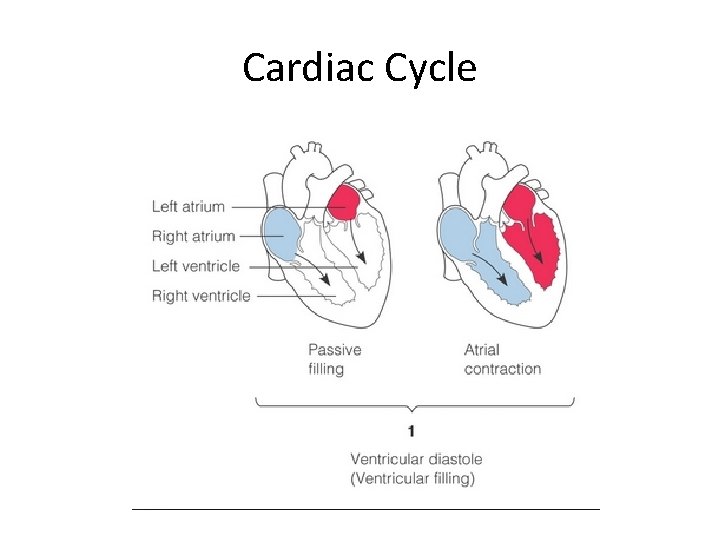
Cardiac Cycle =. 8 seconds • Sequence of Events in one heartbeat – Contraction of both atria – Contraction of both ventricles • • Systole = contraction – of ventricle Diastole = relaxation – of ventricle Lub = closing of AV valves Dub = closing of semilunar valves
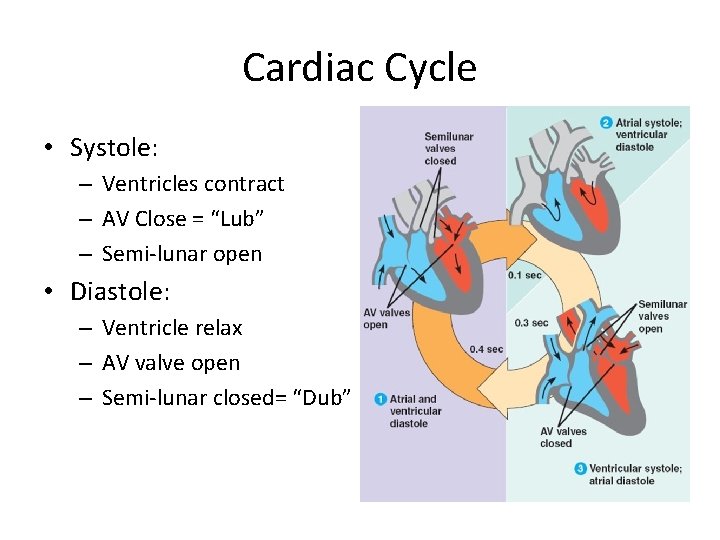
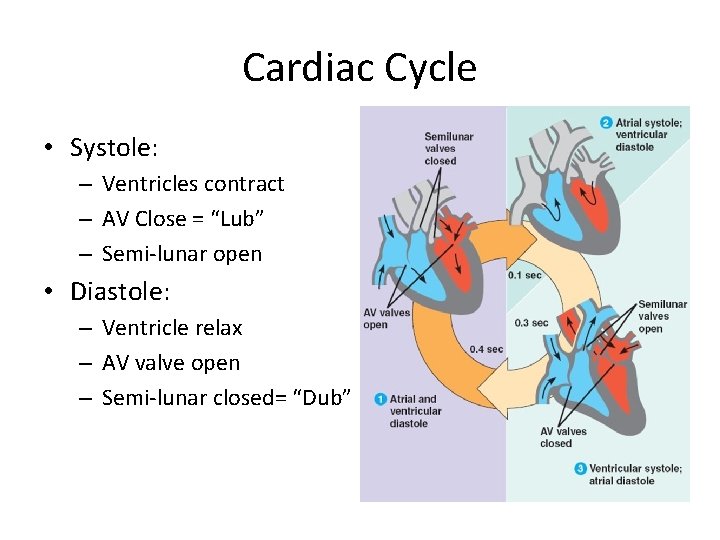
Cardiac Cycle • Systole: – Ventricles contract – AV Close = “Lub” – Semi-lunar open • Diastole: – Ventricle relax – AV valve open – Semi-lunar closed= “Dub”
Cardiac Cycle



Cardiac Output • Cardiac Output = amount of blood pumped out by EACH side of the heart in 1 minute • CO = HR X SV • HR = heart rate or beats per minute • SV = stroke volume = amount of blood pumped out be each ventricle with each heartbeat • If either HR or SV varies, the other tries to compensate to keep the cardiac output stable

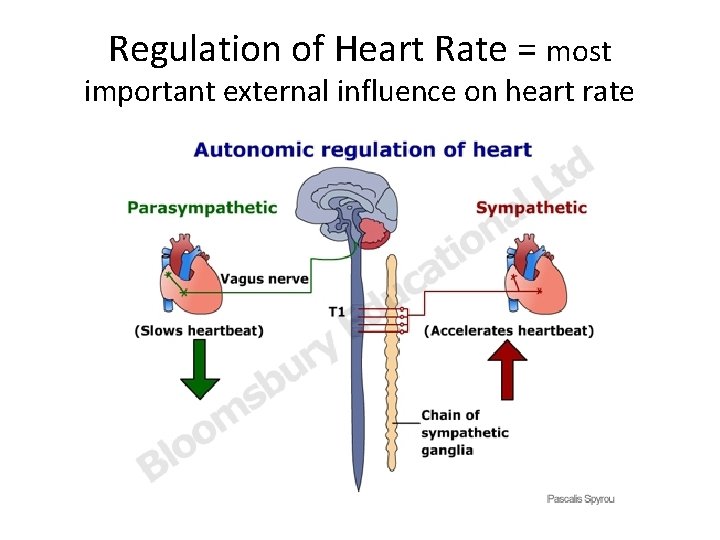
Factors Affecting Heartrate • Autonomic NS – most important external influence on heart – Sympathetic – increase heart rate – Parasympathetic – slow and steady heartrate (vagus nerve) • Hormones – Epinephrine and thyroxine – increase heartrate • Physical factors – Age, gender, exercise, body temperature
Factors Affecting Stroke Volume • How much cardiac muscle stretched before contraction • More stretch = more contraction • Venous return determines amount of stretch • Greater venous return = Greater SV • Increase SV – Slow Heartrate – Exercise • Decrease SV – Severe blood loss – Very Rapid heartrate

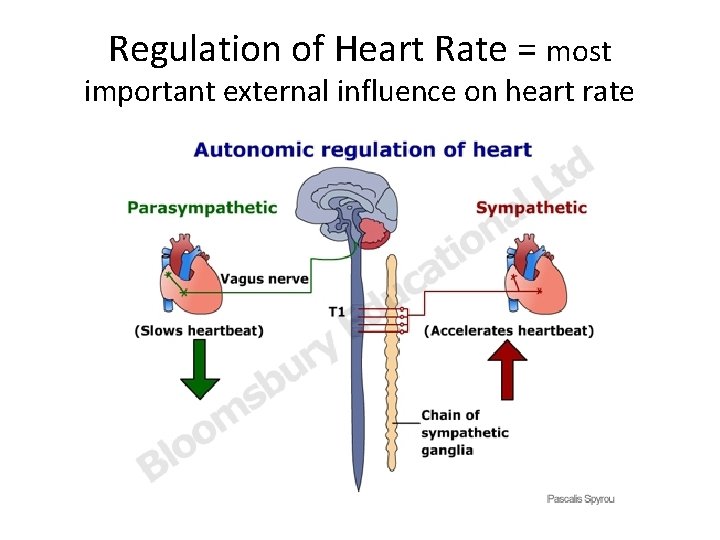
Regulation of Heart Rate = most important external influence on heart rate
Homeostatic Imbalance: Congestive Heart Failure • When the pumping efficiency of the heart is depressed so that circulation is inadequate to meet tissue needs • Usually progressive condition that reflects weakening of the heart by atherosclerosis, persistent high blood pressure, or multiple myocardial infarctions
Congestive Heart Failure Pulmonary Congestions Peripheral Congestion • Left side failure • Right side pumps to lungs • Left side cannot pump to body • Blood pressure inside lungs increases and fluid leaks into lung tissue • Pulmonary edema • Person can suffocate • Right side failure • Blood backs up in systemic circulation • Edema in most distal parts of body

Review Questions – True of False The ventricles contract in diastole The AV valves are open during systole The SA node is the pacemaker of the heart Increased venous return will decrease stroke volume • Parasympathetic NS keeps heartrate slow and steady • •
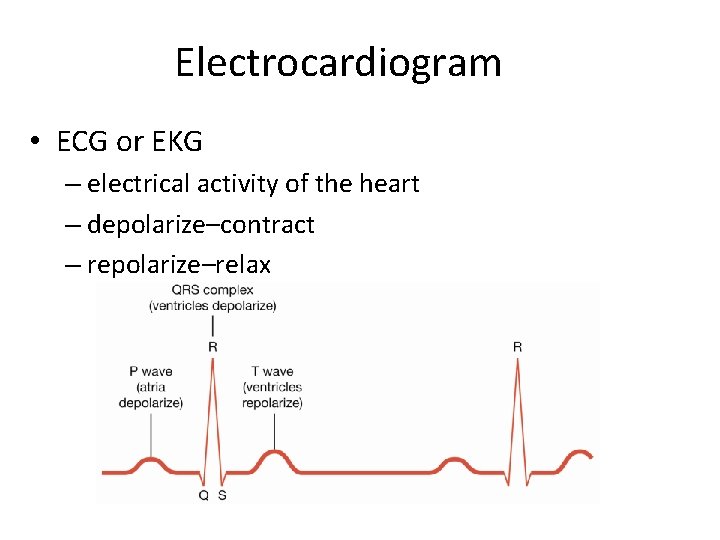
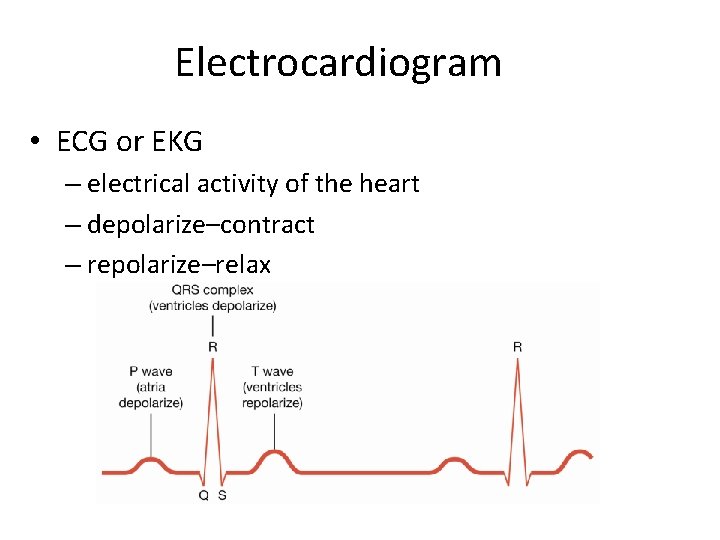
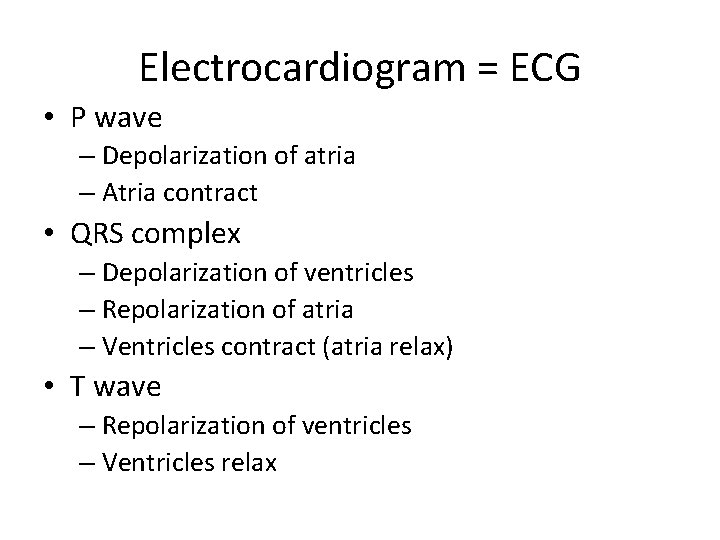
Electrocardiogram • ECG or EKG – electrical activity of the heart – depolarize–contract – repolarize–relax
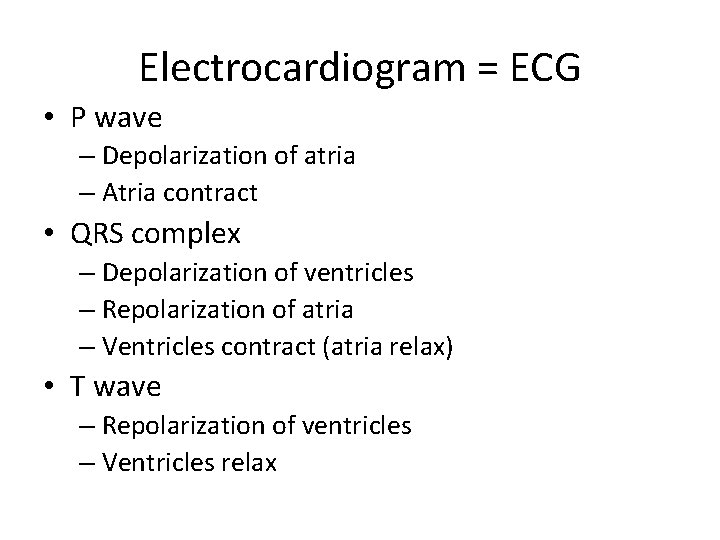
Electrocardiogram = ECG • P wave – Depolarization of atria – Atria contract • QRS complex – Depolarization of ventricles – Repolarization of atria – Ventricles contract (atria relax) • T wave – Repolarization of ventricles – Ventricles relax
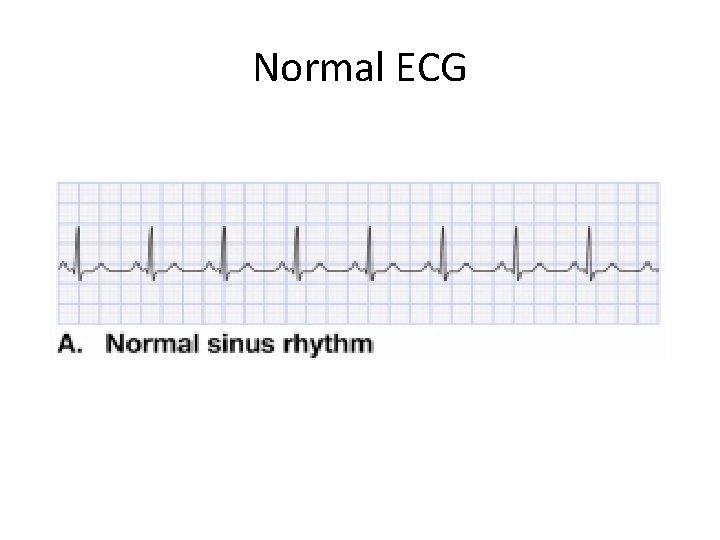
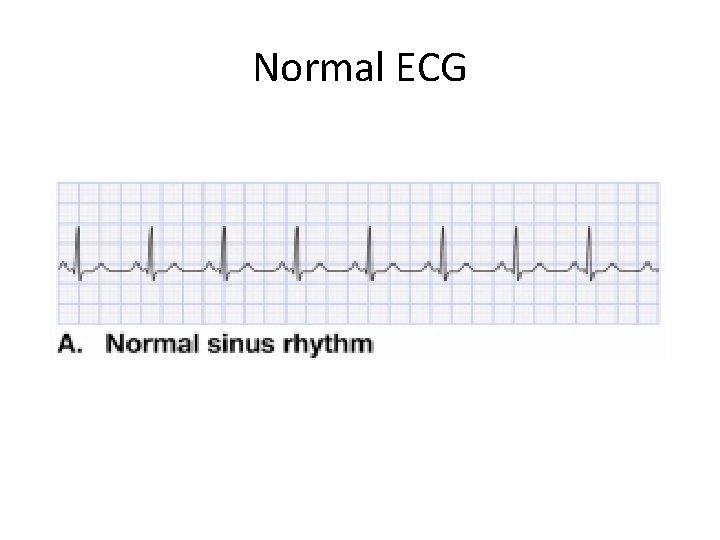
Normal ECG
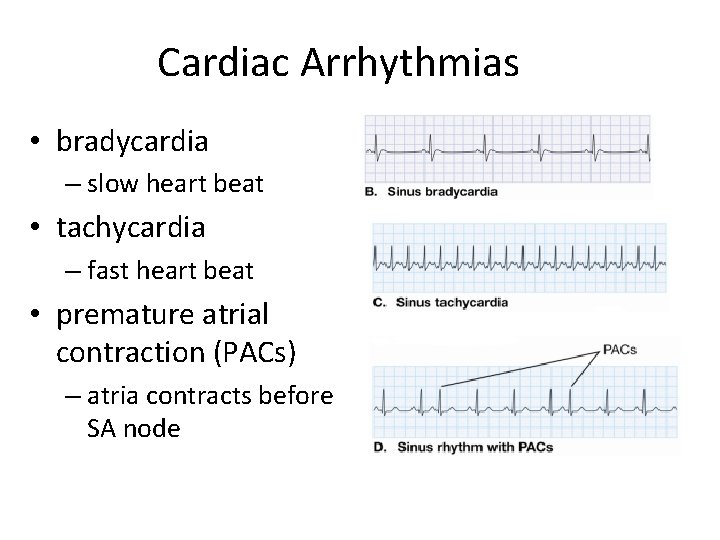
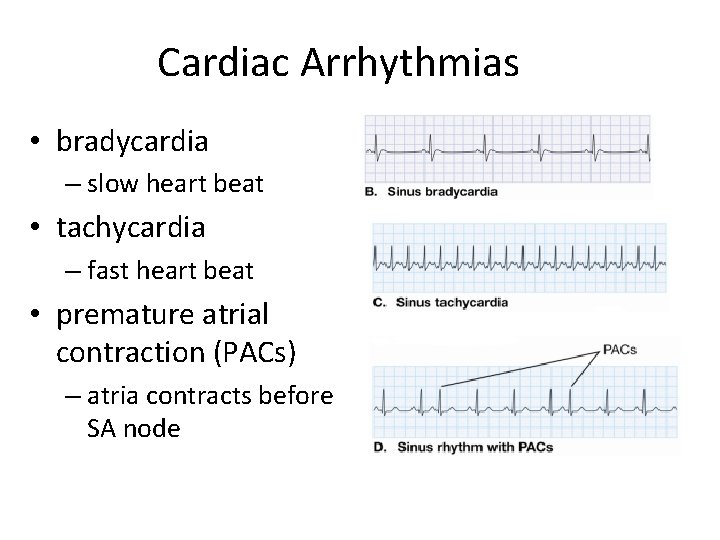
Cardiac Arrhythmias • bradycardia – slow heart beat • tachycardia – fast heart beat • premature atrial contraction (PACs) – atria contracts before SA node
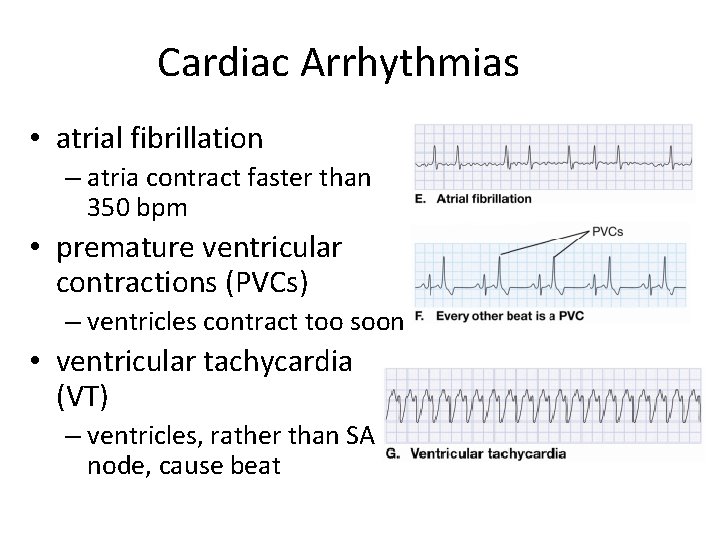
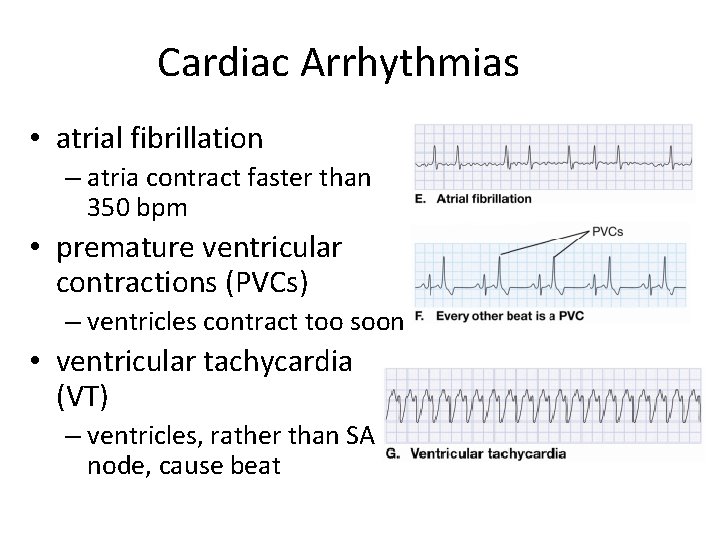
Cardiac Arrhythmias • atrial fibrillation – atria contract faster than 350 bpm • premature ventricular contractions (PVCs) – ventricles contract too soon • ventricular tachycardia (VT) – ventricles, rather than SA node, cause beat
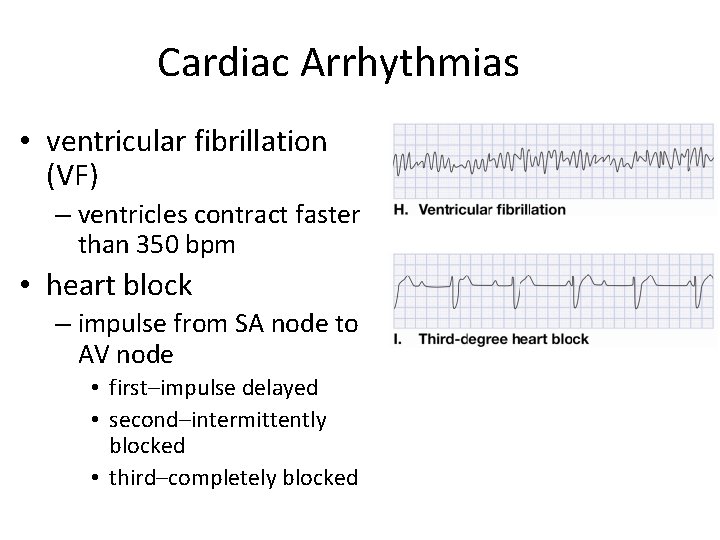
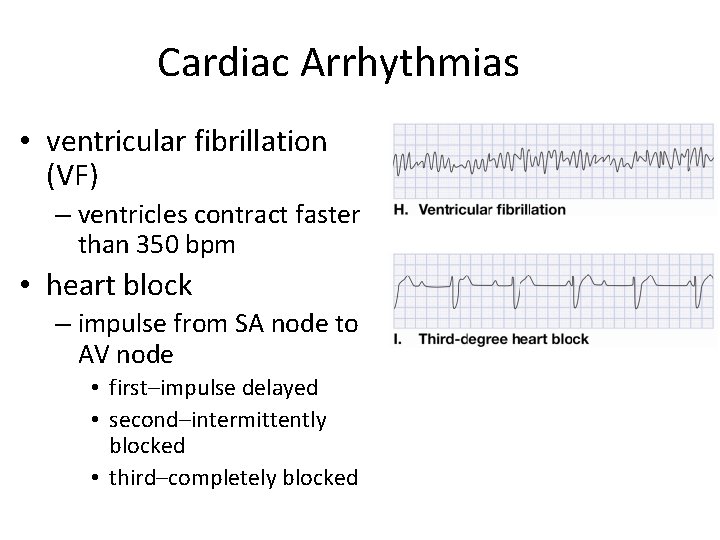
Cardiac Arrhythmias • ventricular fibrillation (VF) – ventricles contract faster than 350 bpm • heart block – impulse from SA node to AV node • first–impulse delayed • second–intermittently blocked • third–completely blocked
Blood Vessels and Circulation • • • blood vessels: the transport network circulation: moving blood around the body taking vital signs know your numbers Closed system – blood always in a vessel or heart
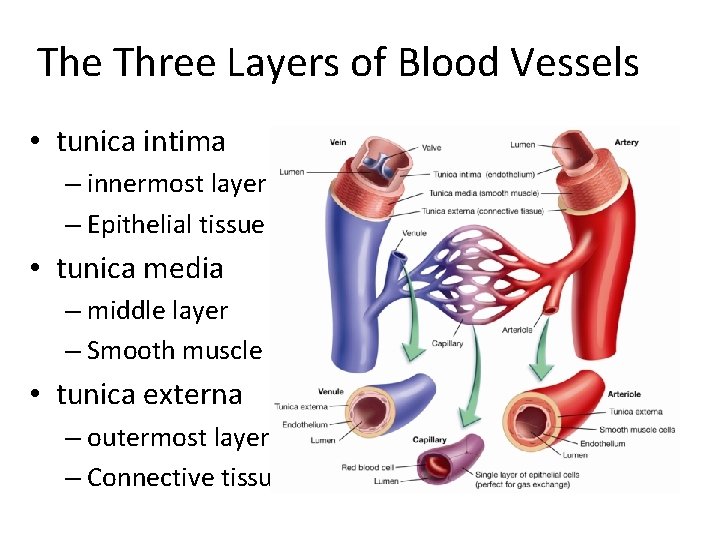
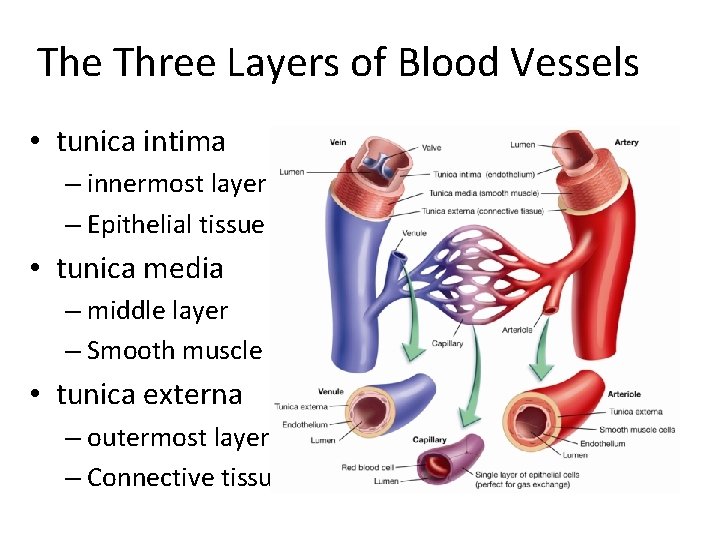
The Three Layers of Blood Vessels • tunica intima – innermost layer – Epithelial tissue • tunica media – middle layer – Smooth muscle • tunica externa – outermost layer – Connective tissue


Blood Pathway Heart Arteries Arterioles Capillaries Venules Veins Heart
Arteries • Carry blood AWAY from heart • Blood usually oxygenated – exception is pulmonary artery • Thick walls, narrow lumen • Walls elastic – expand contract with pulse • Arterioles – smaller arteries – Dilate and constrict to alter blood flow – Ex. Muscles dilate when running • Two organs blood supply never changes = brain and kidneys
Capillaries Smallest of all blood vessels Only one cell thick Narrow – blood cells flow single file Very large surface area for gas, nutrient, and waste exchange • Blood moves slower through here to allow time for exchanges • •
Veins • Carries deoxygenated back to the heart – Exception: Pulmonary vein • Thinner and less elastic, more flexible • Larger veins contain valves – Prevent backflow • Skeletal muscles and breathing help return blood to heart • When inhale, drop in pressure occurs in thorax causing large veins near heart to expand fill

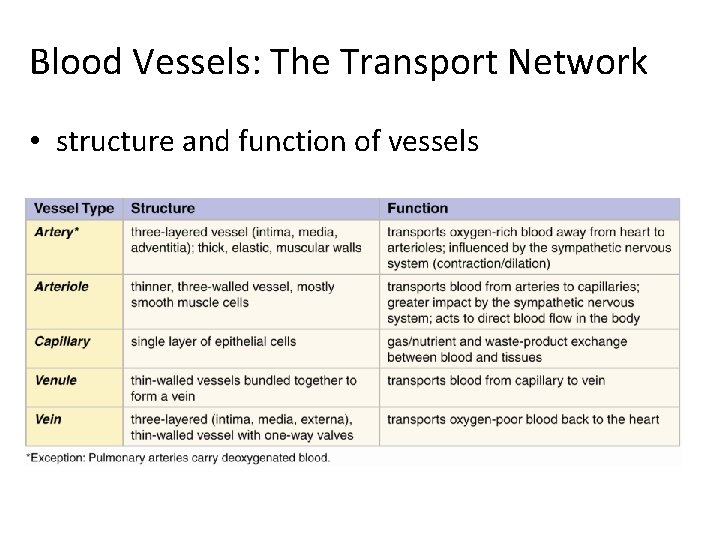
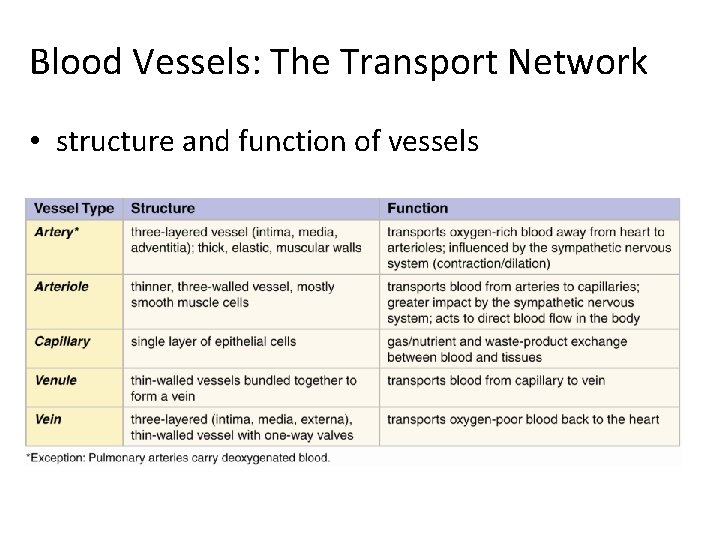
Blood Vessels: The Transport Network • structure and function of vessels
Factors Influencing Venous Return • Lumen of veins larger than arteries • Large veins have valves that prevent backflow • Skeletal muscles help “milk” blood through veins towards heart • When inhale, drop in pressure occurs in thorax causing large veins near heart to expand fill
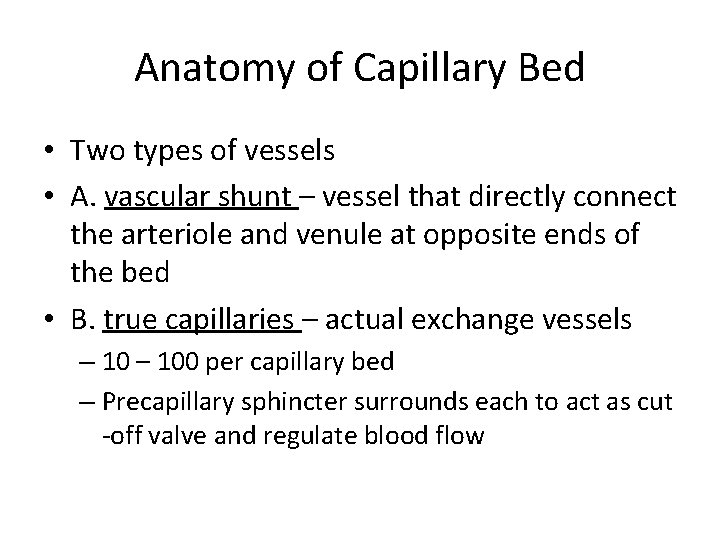
Anatomy of Capillary Bed • Two types of vessels • A. vascular shunt – vessel that directly connect the arteriole and venule at opposite ends of the bed • B. true capillaries – actual exchange vessels – 100 per capillary bed – Precapillary sphincter surrounds each to act as cut -off valve and regulate blood flow


Capillary Exchange • Substances tend to move into and out of body cells according to their concentration gradients. • Oxygen and nutrients: blood tissue cells • CO 2 and waster: tissue cells blood
How Solutes Move In and Out • 1. Diffusion – lipid soluble • 2. Endocytosis and Exocytosis – lipid insoluble • 3. Intercellular clefts – special diffusion through gaps between cell membranes of adjoining cells • 4. Fenestrated capillaries – special capillaries filled with pores. Found in areas where absorption and filtration important
Fluid Movement - due to differences in pressure • Blood pressure highest - arterial end – Fluid moves out of capillaries • Osmotic pressure highest - venule end – Fluid moves into capillaries
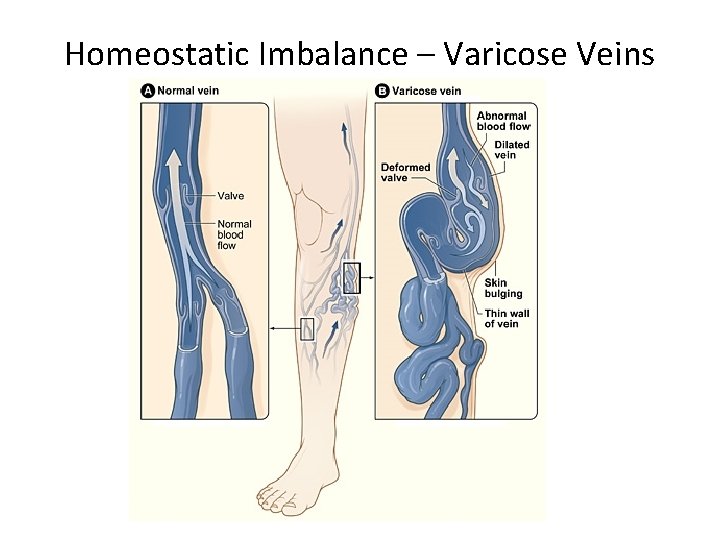
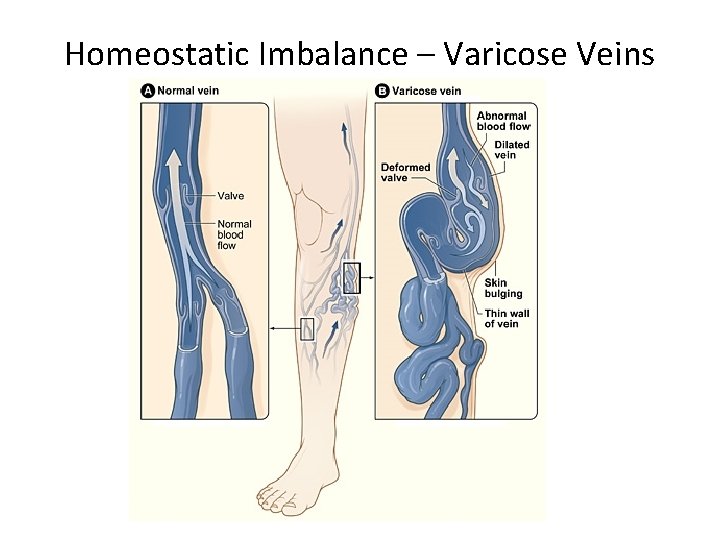
Homeostatic Imbalance – Varicose Veins
Thrombophlebitis • Complication of varicose veins • Inflammation of a vein that results when a clot forms in vein with poor circulation • Common Consequence: clot detachment and pulmonary embolism
Special Circulations • Arterial Supply of Brain and Circle of Willis – – Supplied by 2 sets of arteries – These blood supplies are united by special arteries – Result is complete circle of connecting blood vessels called the circle of Willis – Protects the brain because it provides more than one route for blood to reach the brain
Special Circulations • Hepatic Portal Circulation – Veins drain the digestive organs and deliver blood to liver – Liver processes nutrients before make it to systemic circulation • Fetal Circulation – All nutrient, excretory, and gas exchange occur through placenta – Umbilical veins and arteries
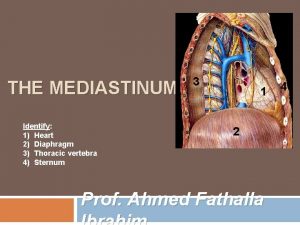
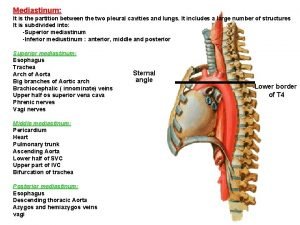
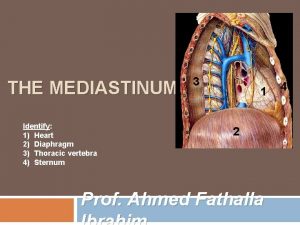
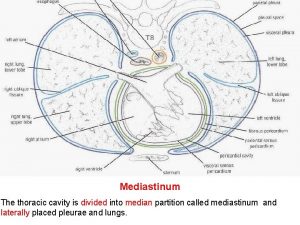
 Mediastinum heart
Mediastinum heart Mediastinum heart
Mediastinum heart Mediastinum heart
Mediastinum heart Mediastinum heart
Mediastinum heart Endocardium
Endocardium Where is the heart located
Where is the heart located Where is cow heart located
Where is cow heart located Regio thorax
Regio thorax Anterior mediastinum contents
Anterior mediastinum contents Lethenic
Lethenic Esophageal constrictions mnemonic
Esophageal constrictions mnemonic Occupied
Occupied Nerve
Nerve Middle mediastinum: contents mnemonic
Middle mediastinum: contents mnemonic Anterior mediastinum contents
Anterior mediastinum contents Posterior mediastinum contents
Posterior mediastinum contents Lig. hyoepiglotticum
Lig. hyoepiglotticum Luinen thorax
Luinen thorax Mediastiinum
Mediastiinum Aortaruptur
Aortaruptur Mediastinum contents
Mediastinum contents Inferior vena cava mediastinum
Inferior vena cava mediastinum Cardiac plexus
Cardiac plexus Testes
Testes Vein or lymph node
Vein or lymph node Mediastinal surface
Mediastinal surface Spatium intercostalis adalah
Spatium intercostalis adalah Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Ng-html
Ng-html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp tư thế worms-breton
Chụp tư thế worms-breton Alleluia hat len nguoi oi
Alleluia hat len nguoi oi Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Mật thư anh em như thể tay chân
Mật thư anh em như thể tay chân Làm thế nào để 102-1=99
Làm thế nào để 102-1=99 độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Biện pháp chống mỏi cơ
Biện pháp chống mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thứ tự các dấu thăng giáng ở hóa biểu
Thứ tự các dấu thăng giáng ở hóa biểu Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phối cảnh
Phối cảnh Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Các loại đột biến cấu trúc nhiễm sắc thể
Các loại đột biến cấu trúc nhiễm sắc thể Các số nguyên tố là gì
Các số nguyên tố là gì Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Hổ sinh sản vào mùa nào
Hổ sinh sản vào mùa nào Sự nuôi và dạy con của hươu
Sự nuôi và dạy con của hươu Hệ hô hấp
Hệ hô hấp