SURGICAL DISORDERS OF MEDIASTINUM AND DIAPHRAGM Sina Ercan








- Slides: 66
SURGICAL DISORDERS OF MEDIASTINUM AND DIAPHRAGM Sina Ercan MD Professor of Thoracic Surgery
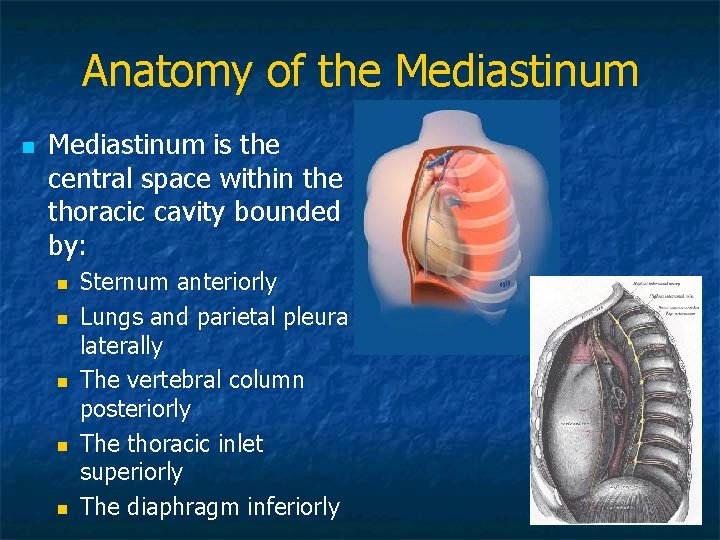
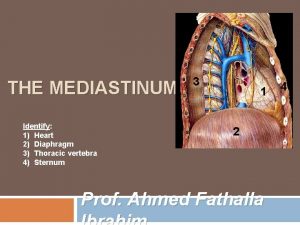
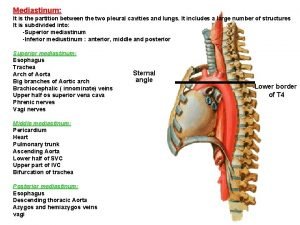
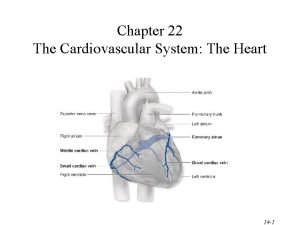
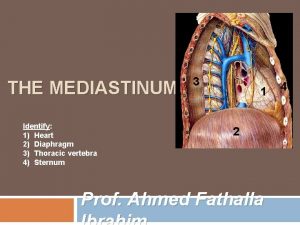
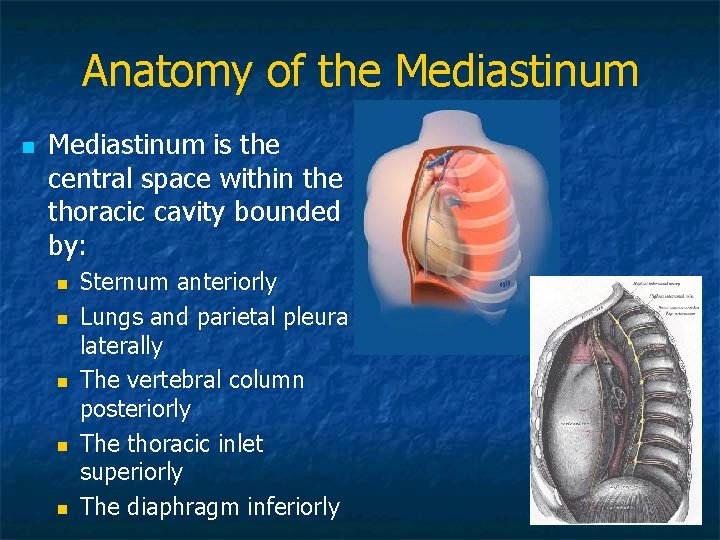
Anatomy of the Mediastinum n Mediastinum is the central space within the thoracic cavity bounded by: n n n Sternum anteriorly Lungs and parietal pleura laterally The vertebral column posteriorly The thoracic inlet superiorly The diaphragm inferiorly



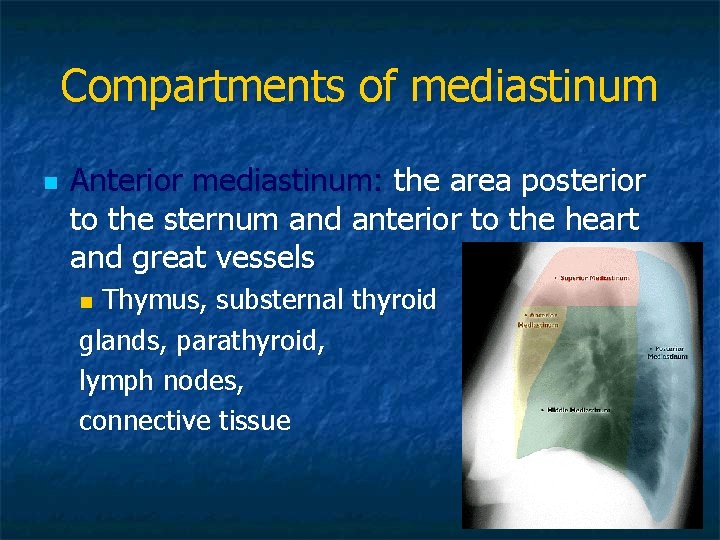
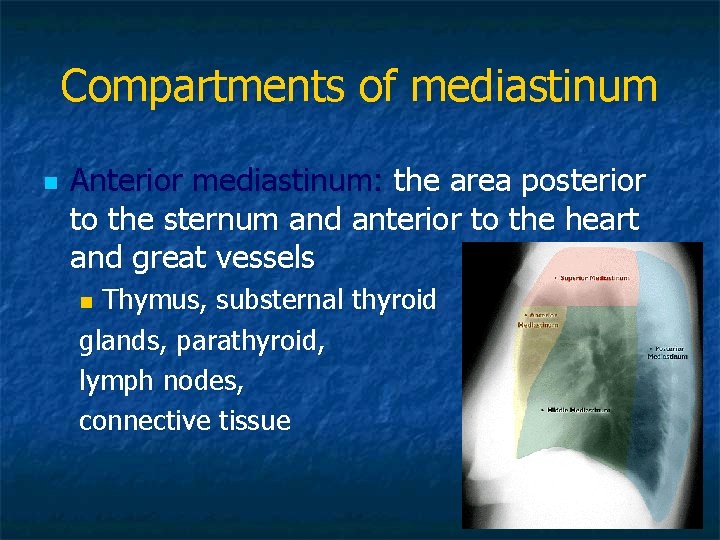
Compartments of mediastinum n Anterior mediastinum: the area posterior to the sternum and anterior to the heart and great vessels Thymus, substernal thyroid glands, parathyroid, lymph nodes, connective tissue n
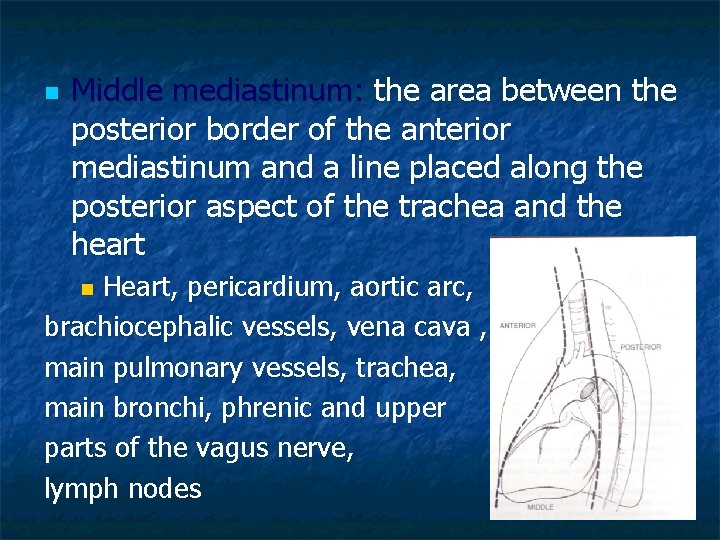
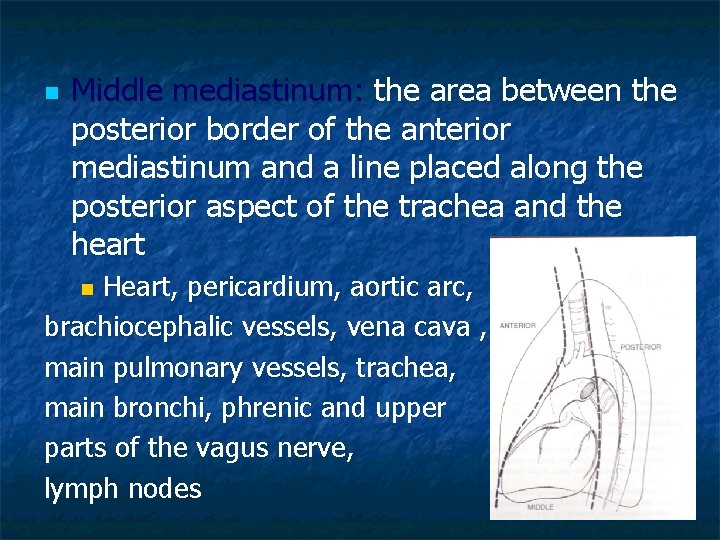
n Middle mediastinum: the area between the posterior border of the anterior mediastinum and a line placed along the posterior aspect of the trachea and the heart Heart, pericardium, aortic arc, brachiocephalic vessels, vena cava , main pulmonary vessels, trachea, main bronchi, phrenic and upper parts of the vagus nerve, lymph nodes n
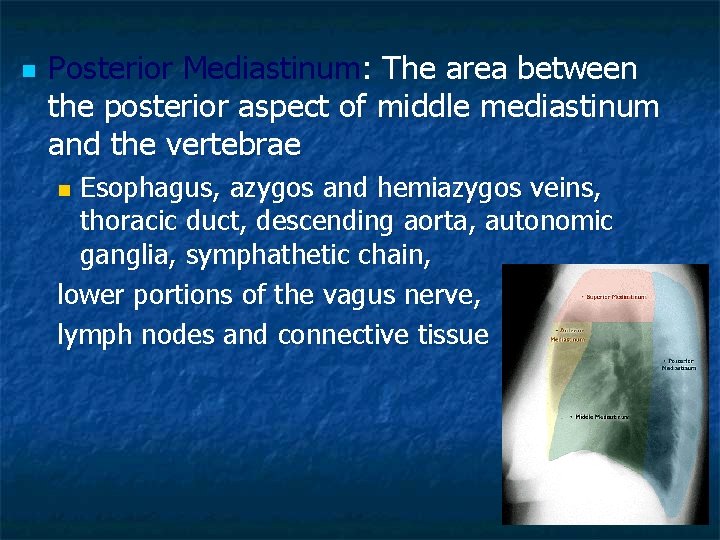
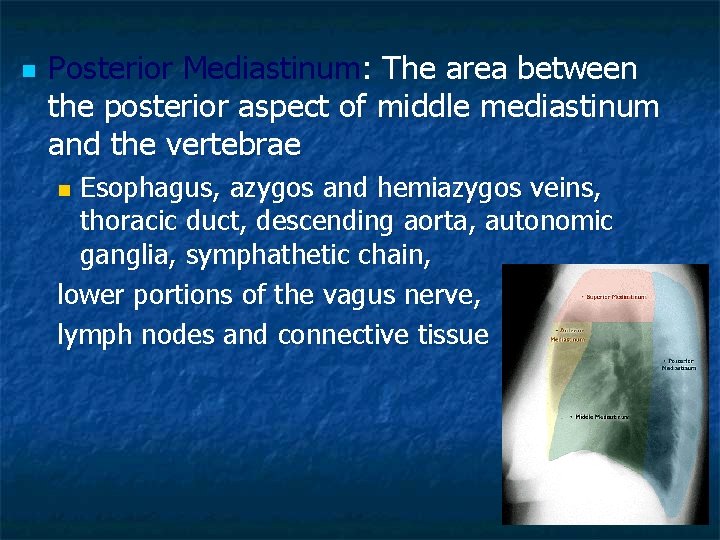
n Posterior Mediastinum: The area between the posterior aspect of middle mediastinum and the vertebrae Esophagus, azygos and hemiazygos veins, thoracic duct, descending aorta, autonomic ganglia, symphathetic chain, lower portions of the vagus nerve, lymph nodes and connective tissue n

Mediastinal Pathologies n Non neoplastic diseases n n n Congenital pathologies n n n Mediastinitis Pneumomediastinum Cysts Hernias Acquired lesions n n Benign Malignant
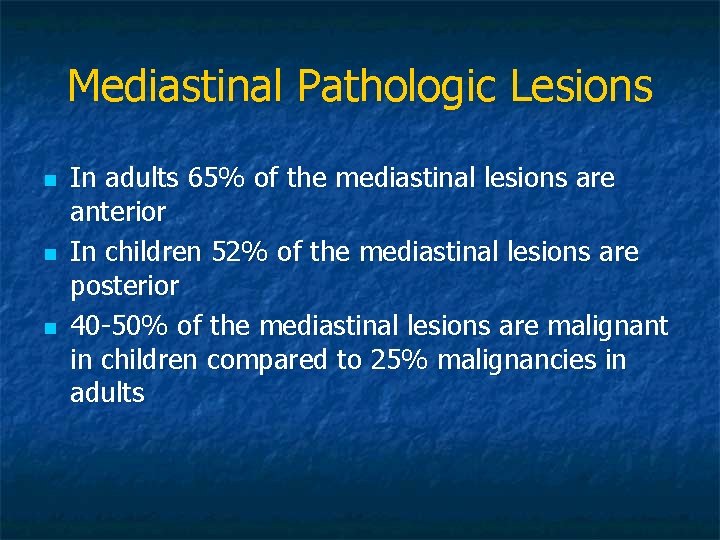
Mediastinal Pathologic Lesions n n n In adults 65% of the mediastinal lesions are anterior In children 52% of the mediastinal lesions are posterior 40 -50% of the mediastinal lesions are malignant in children compared to 25% malignancies in adults
Anterior mediastinal disorders n Thymic disorders n n n Thymoma, Thymic carcinoma Thymic carcinoid Thymolipoma Thymic cyst Thymic hyperplasia Thyroid disorders n Intrathoracic goiter n Germ cell tumors n n Lymphoma n n Teratoma Seminoma Others Hodgkin’s disease Non-Hodgkin’s Parathyroid adenoma Mesenchymal tumors
Thymoma n n n Most common adult 10 mediastinal neoplasm Usually >40 y/o 40 -70% have symptoms related to parathymic syndromes Myasthenia Gravis, n Hypogammaglobulinemia n Pure red cell aplasia n Nonthymic malignancies n
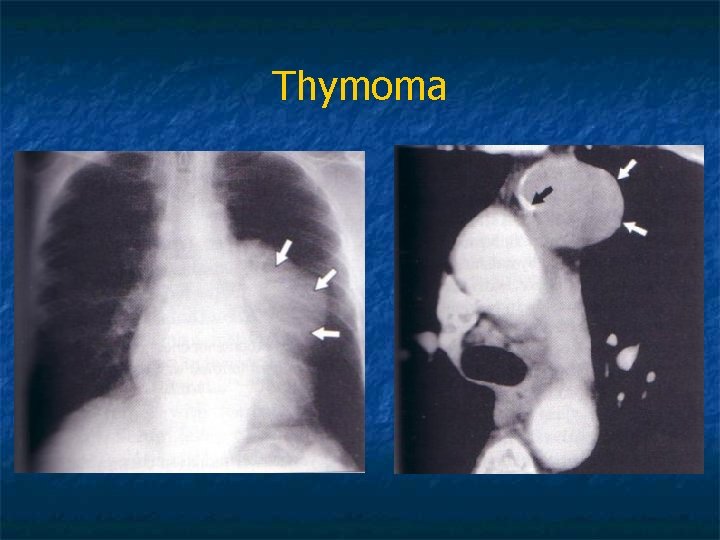
n n n Thymomas represent neoplastic proliferation of thymic epithelial cells mixed with mature lymphocytes CT demonstrates a homogenious soft tissue mass CT guided needle biopsy, mediastinoscopy, mediastinotomy or VATS for diagnosis
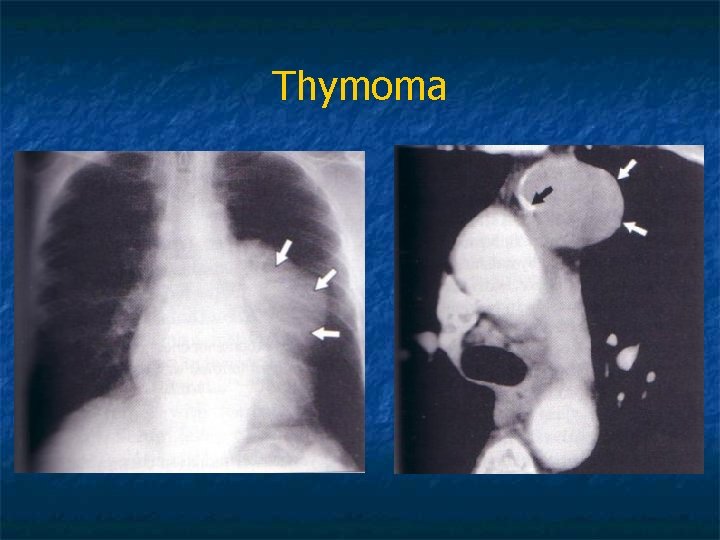
Thymoma
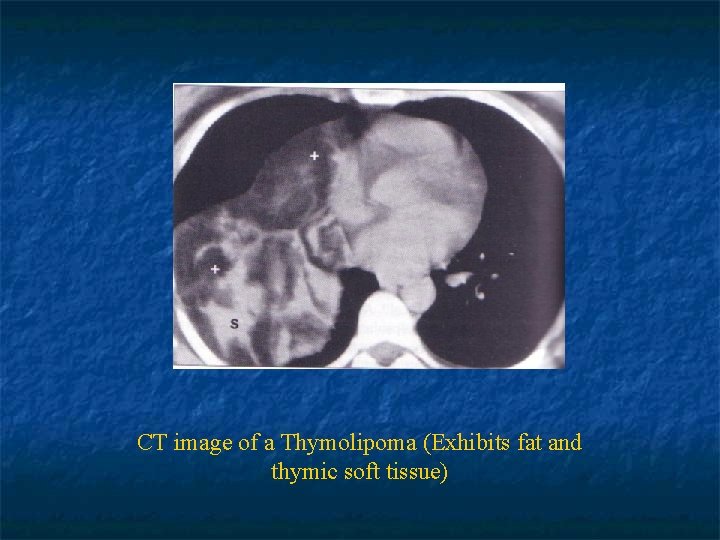
n Thymic Carcinoma: Malignant histologic features n Pulmonary, regional lymph node or pleural metastasis can be present n n Thymic carcinoid: n n a rare agressive neoplasm that originates from thymic neuroendocrine cells Thymolipoma: n a rare benign tumor composed of mature adipose and thymic tissue
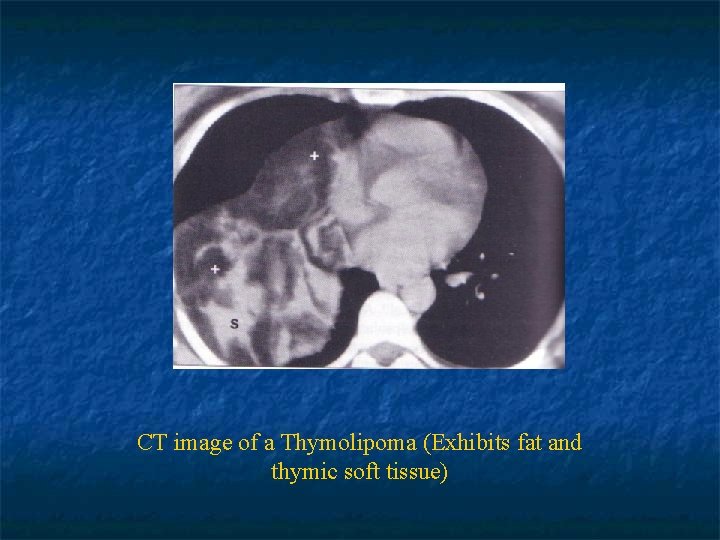
CT image of a Thymolipoma (Exhibits fat and thymic soft tissue)
Mediastinal Lymphoma n n 10 -20% of all mediastinal neoplasms in adults May be 1 o in anterior or middle mediastinum or part of systemic malignancy 20 -30% of patients are asymptomatic Symptoms of local invasion or systemic symptoms (fever, weight loss, pruritis)
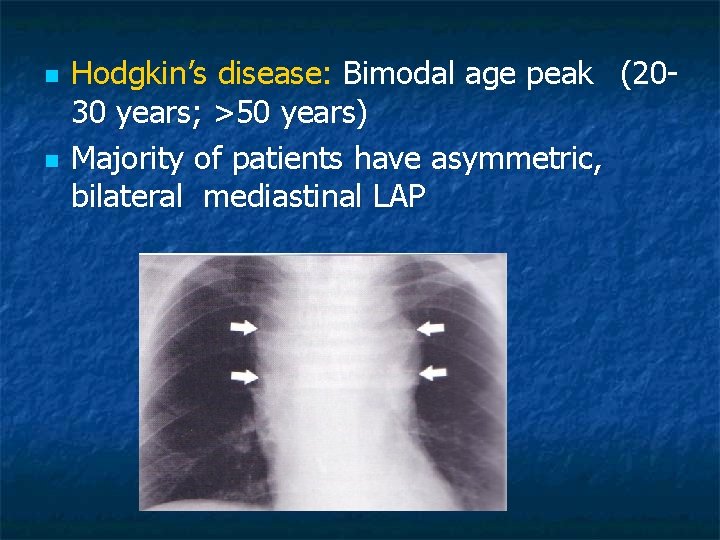
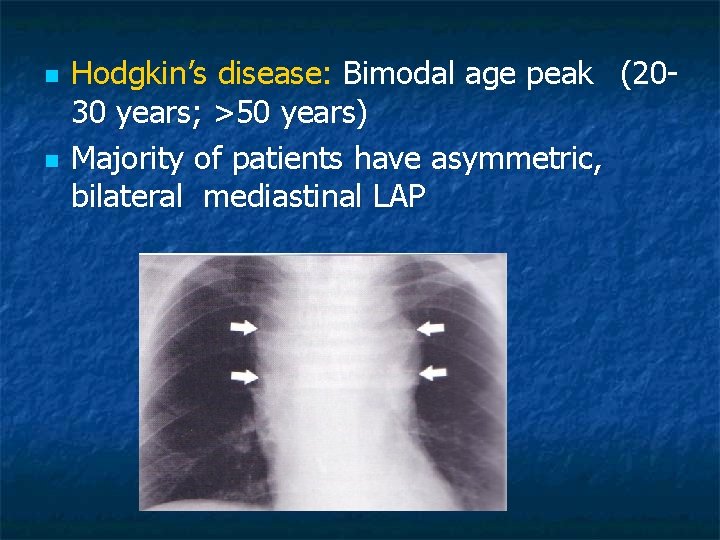
n n Hodgkin’s disease: Bimodal age peak (2030 years; >50 years) Majority of patients have asymmetric, bilateral mediastinal LAP
n n Non-Hodgkin’s Lymphoma: Usually in older patients Usually systemic upon presentation and spreads unpredictably n Diffuse Large B-cell Lymphoma n Lymphoblastic Lymphoma
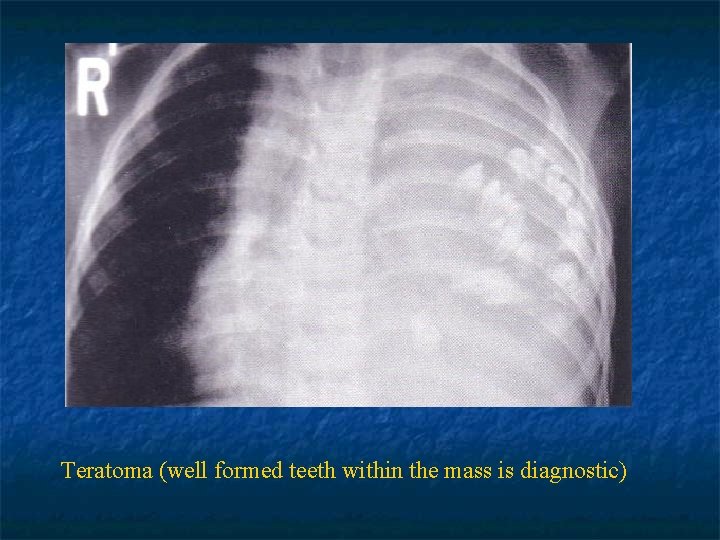
Mediastinal Germ-Cell Tumors n Teratomas: Account 60 -70% of cases n Consist of tissue that may derive from more than one of the germ cell layers n Mostly benign, radiologically spheric, lobulated, well circumscribed and may contain calcification n n Seminomas: Affect men in 3 rd and 4 th decades n 40 -50% of mediastinal malignant germ cell tumors n
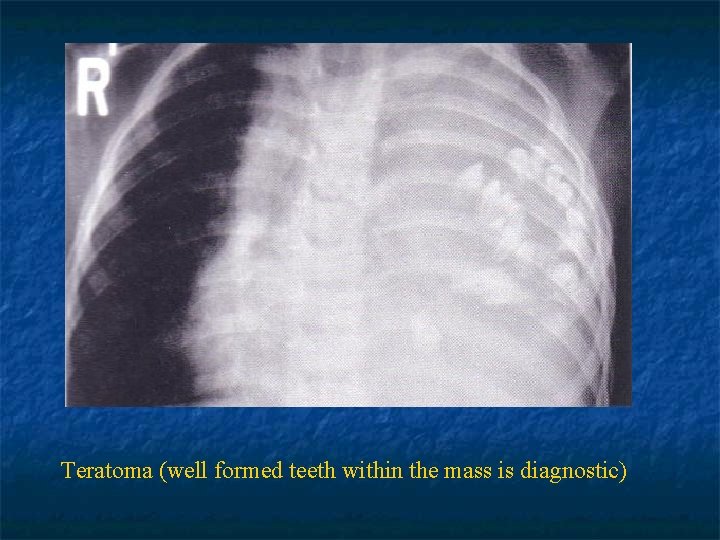
Teratoma (well formed teeth within the mass is diagnostic)

Germ cell tumor
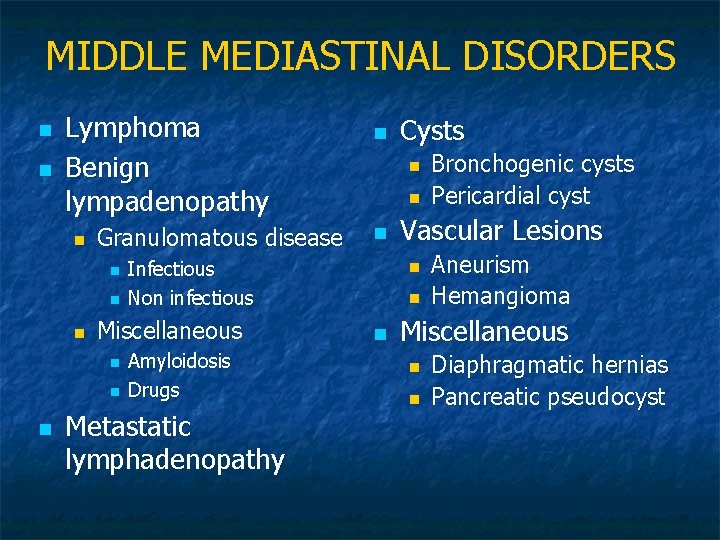
MIDDLE MEDIASTINAL DISORDERS n n Lymphoma Benign lympadenopathy n Granulomatous disease n n n Amyloidosis Drugs Metastatic lymphadenopathy Cysts n n n Infectious Non infectious Miscellaneous n n Vascular Lesions n n n Bronchogenic cysts Pericardial cyst Aneurism Hemangioma Miscellaneous n n Diaphragmatic hernias Pancreatic pseudocyst
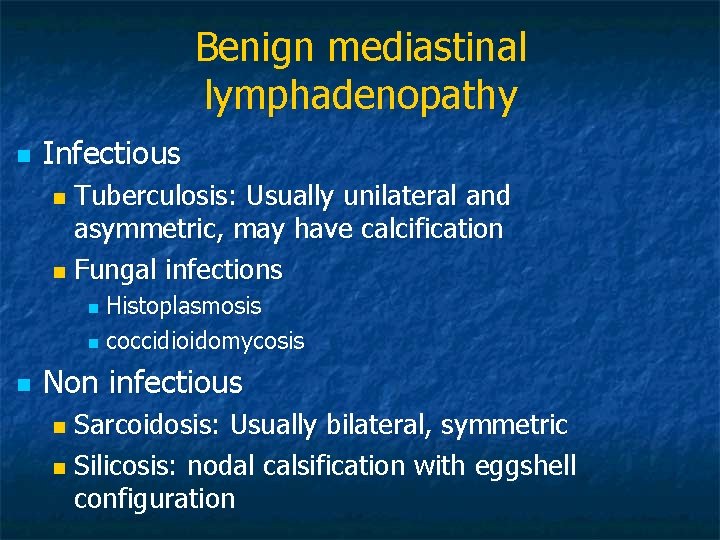
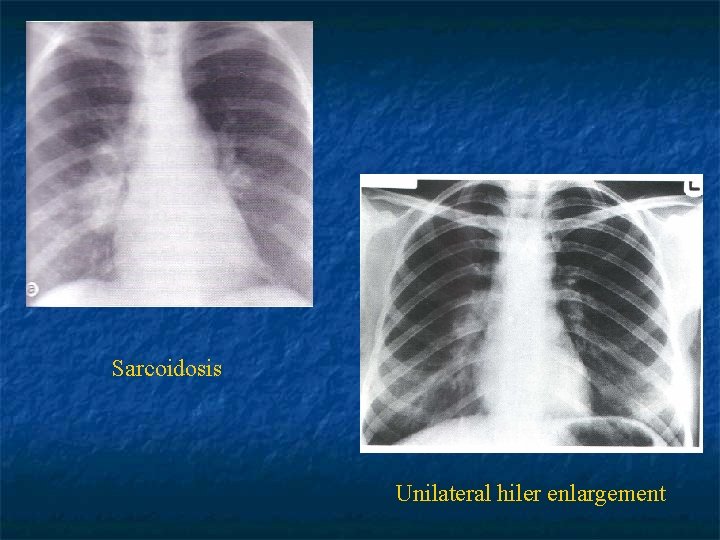
Benign mediastinal lymphadenopathy n Infectious Tuberculosis: Usually unilateral and asymmetric, may have calcification n Fungal infections n Histoplasmosis n coccidioidomycosis n n Non infectious Sarcoidosis: Usually bilateral, symmetric n Silicosis: nodal calsification with eggshell configuration n
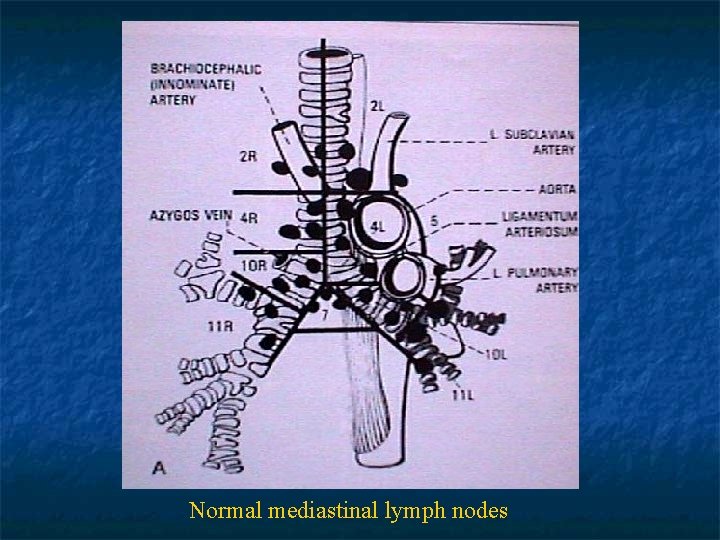
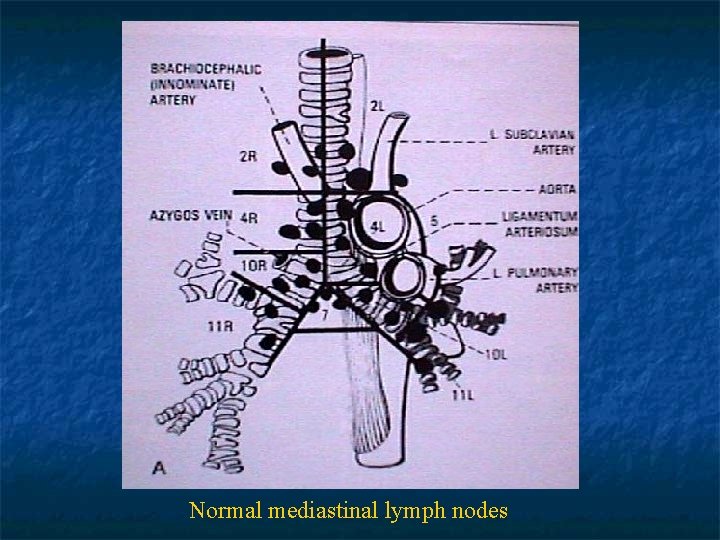
Normal mediastinal lymph nodes
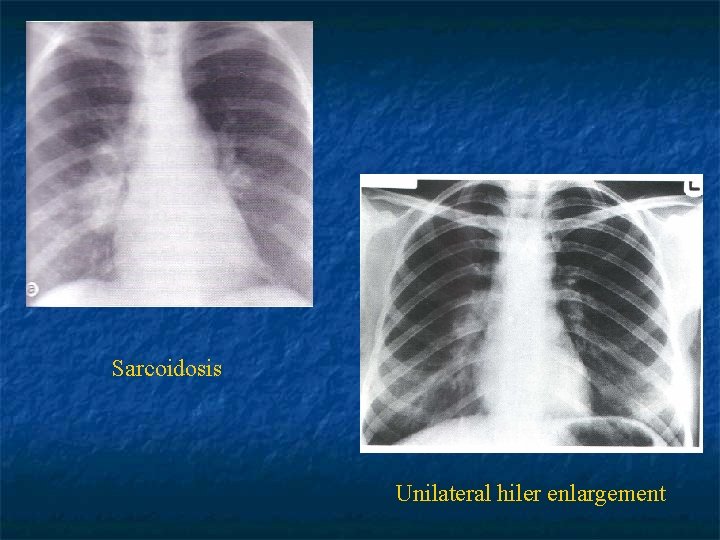
Sarcoidosis Unilateral hiler enlargement
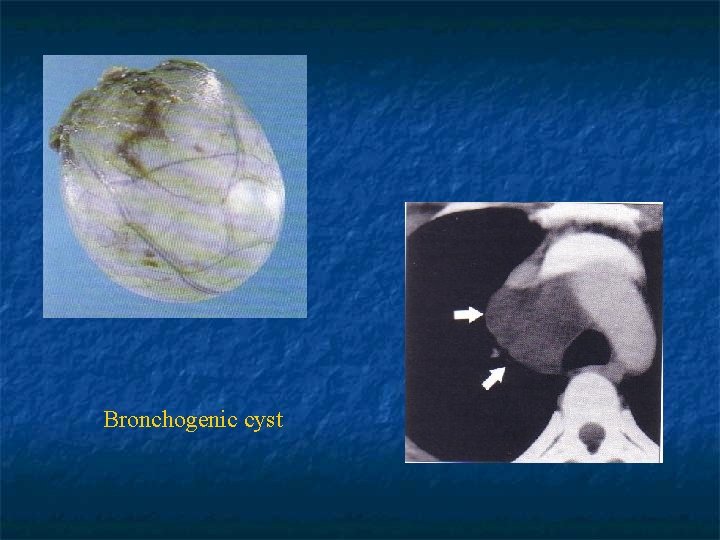
Cysts n n n Bronchogenic cyst: Originate from abnormal budding of ventral foregut Commonly in subcarinal and paratracheal regions 15% in pulmonary paranchyme Lined by respiratory epithelium and may contain serous fluid, mucus, milk of calcium, blood or purulent material
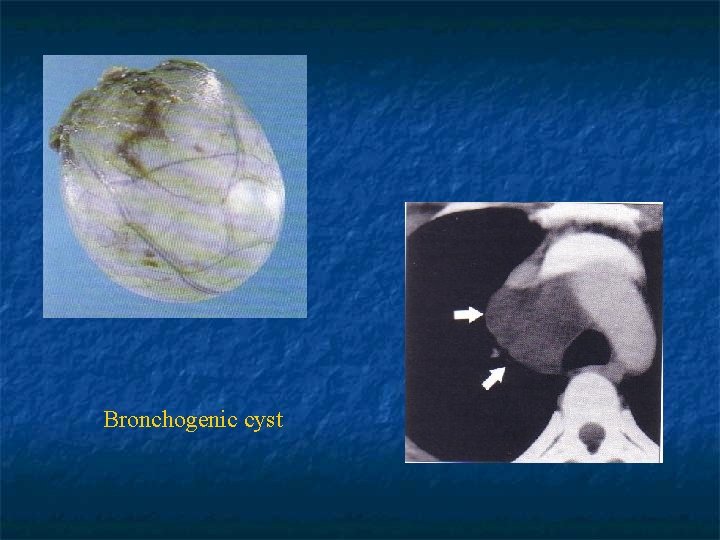
Bronchogenic cyst
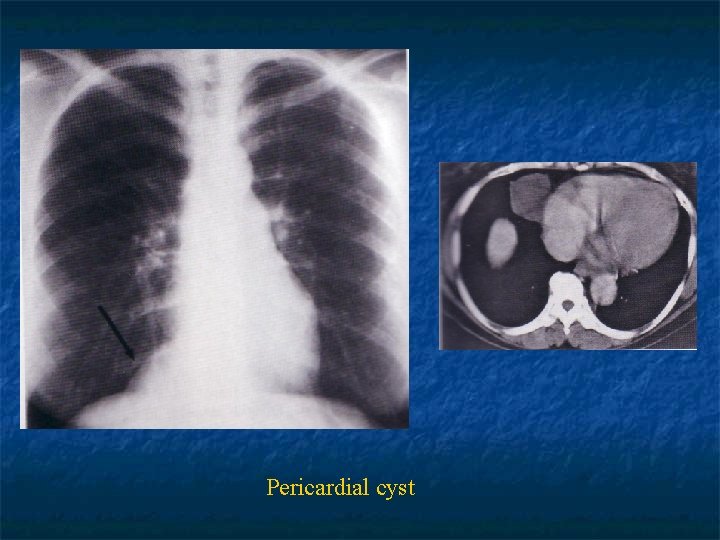
n Enterogenous cysts: Esophageal dublication and neurenteric cysts n Located in the middle or posterior mediastinum n n Pericardial Cysts: In the cardiophrenic angles (R>L) n Fibrous walls and contain clear fluid n n Diaphragmatic hernias: Hiatal hernia n Morgagni hernia n Bochdalek hernia n
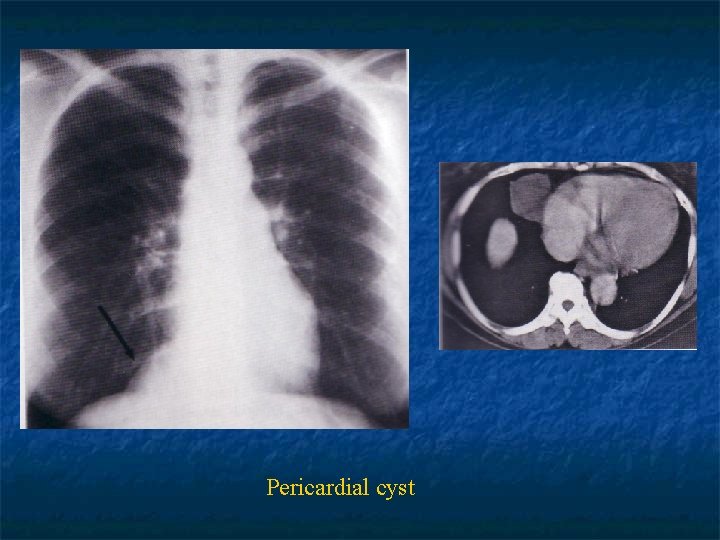
Pericardial cyst
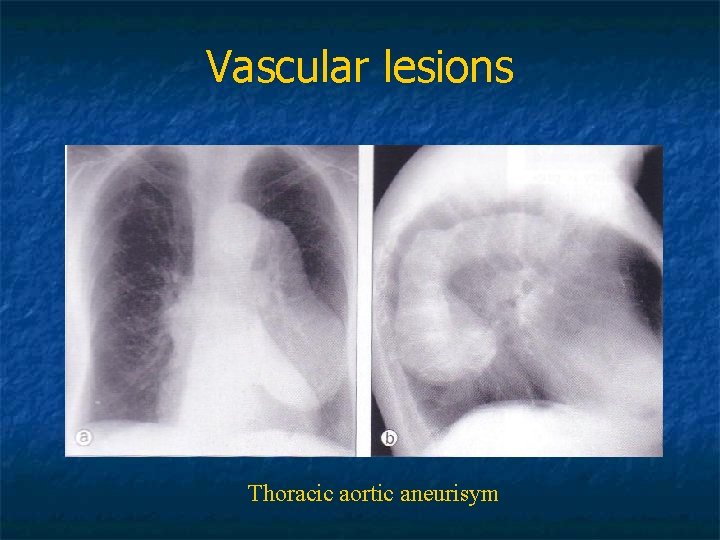
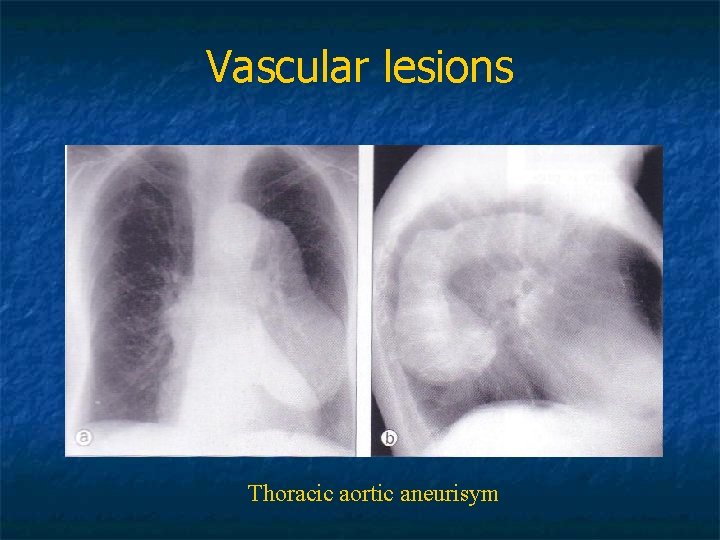
Vascular lesions Thoracic aortic aneurisym
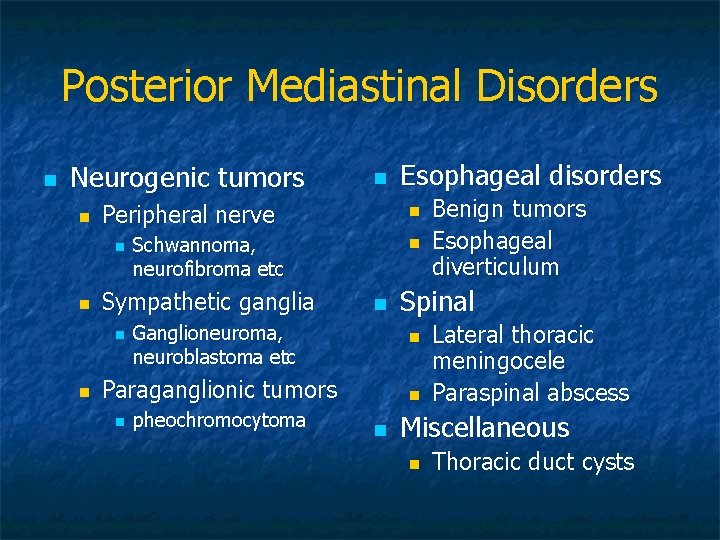
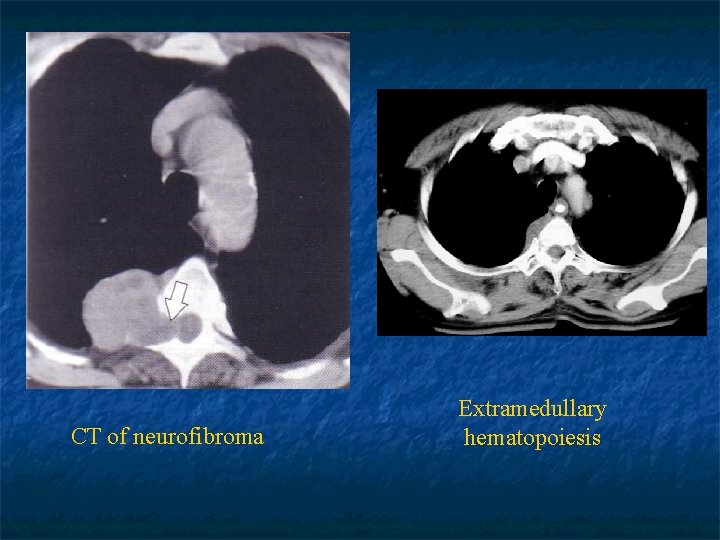
Posterior Mediastinal Disorders n Neurogenic tumors n Peripheral nerve n n Esophageal disorders n Schwannoma, neurofibroma etc Sympathetic ganglia n n n Paraganglionic tumors n n pheochromocytoma n Benign tumors Esophageal diverticulum Spinal Ganglioneuroma, neuroblastoma etc n n n Lateral thoracic meningocele Paraspinal abscess Miscellaneous n Thoracic duct cysts
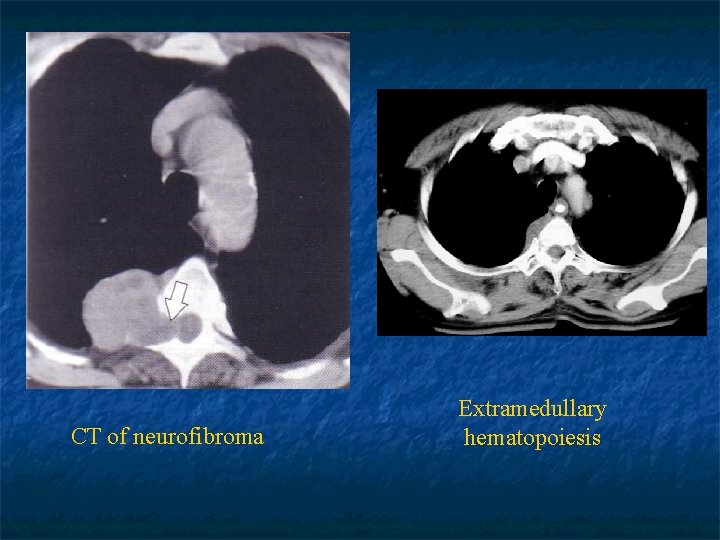
CT of neurofibroma Extramedullary hematopoiesis
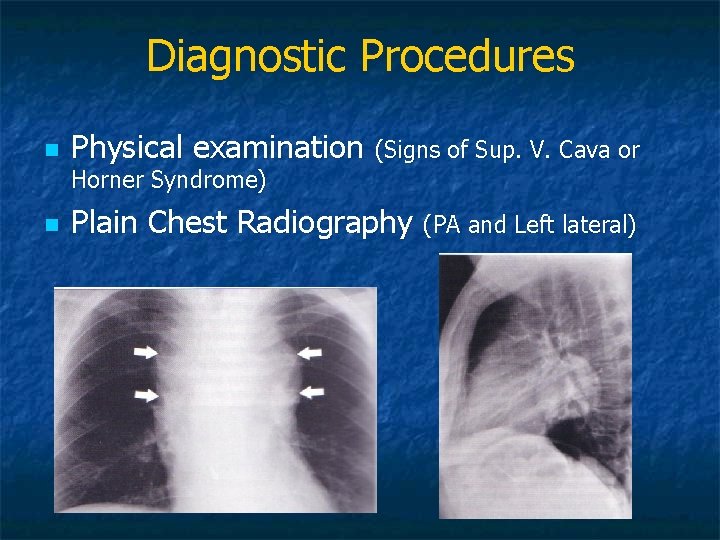
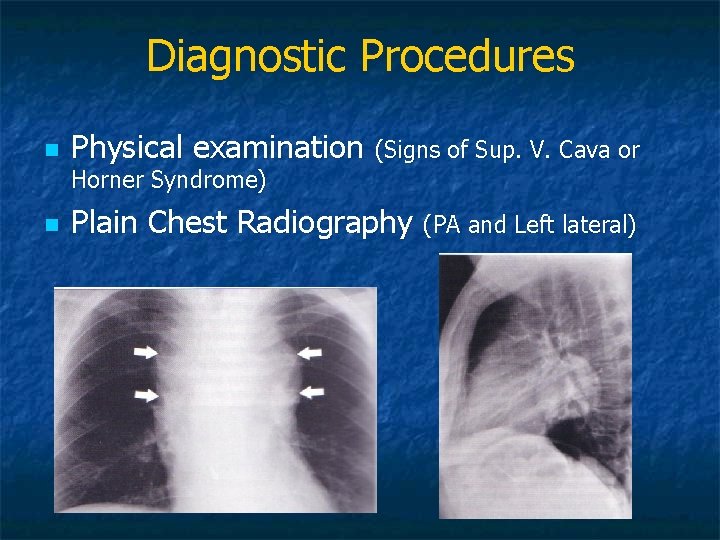
Diagnostic Procedures n Physical examination (Signs of Sup. V. Cava or Horner Syndrome) n Plain Chest Radiography (PA and Left lateral)
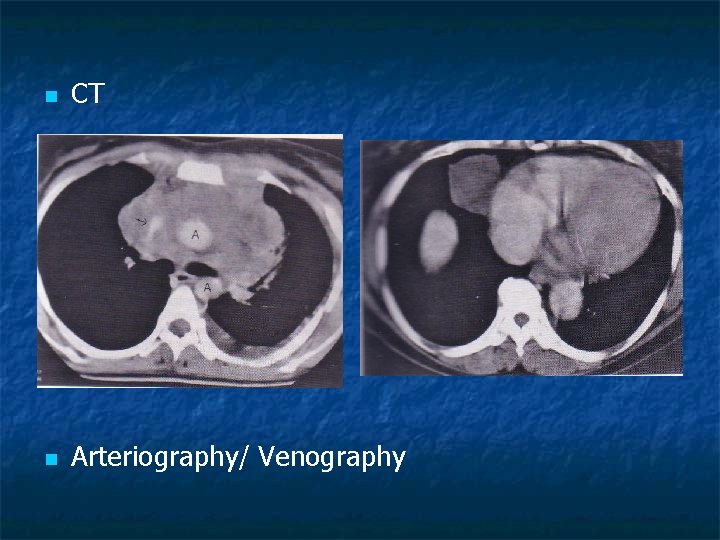
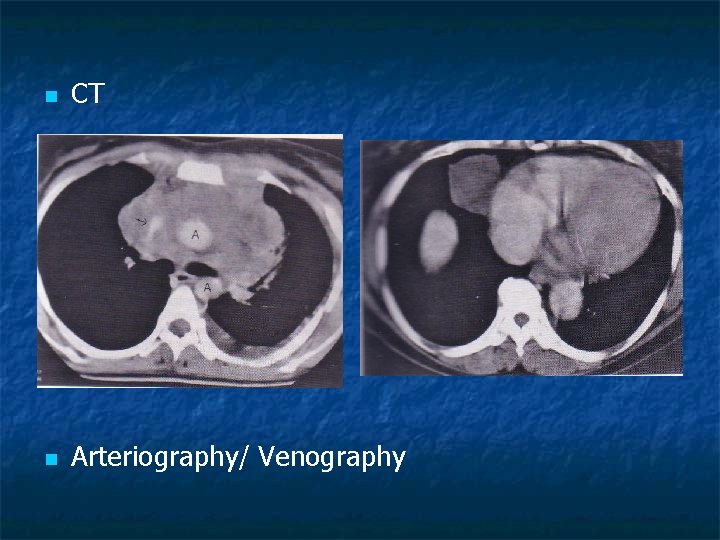
n CT n Arteriography/ Venography
n n Ultrasound MRI Barium esophagram Histologic evaluation Fine needle aspiration n Mediastinoscopy/mediastinotomy n Thoracoscopy (VATS) n Thoracotomy n
Non neoplastic Disorders of the Mediastinum n Pneumomediastinum n Pneumopericardium n Acute Mediastinitis n Chronic Mediastinitis
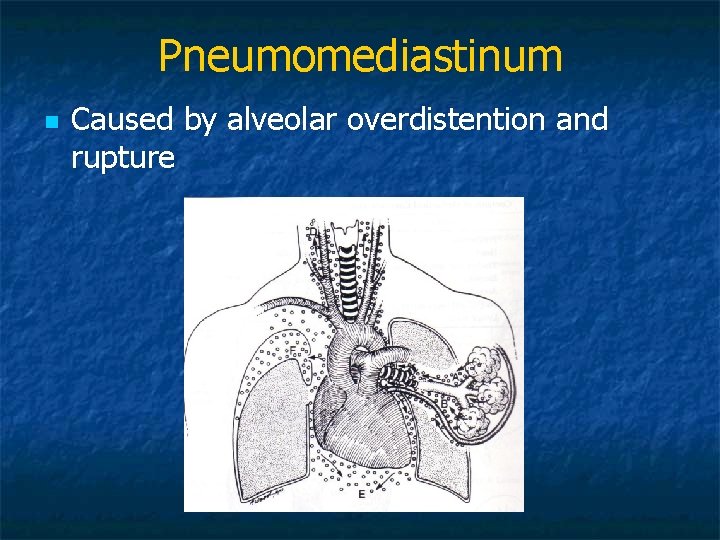
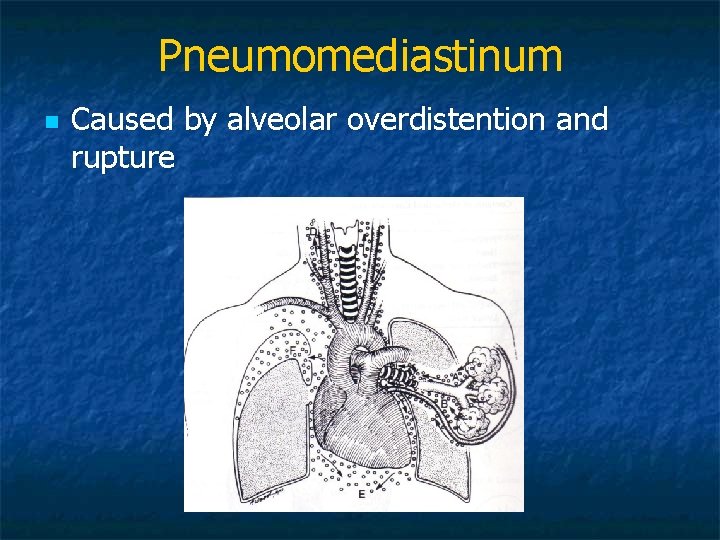
Pneumomediastinum n Caused by alveolar overdistention and rupture
Etiology of pneumomediastinum n Spontaneous n n n n Acute asthma attack Scuba diving Mechanic ventilation Vomiting Trauma Surgery Tracheostomy n n n Bronchoscopic procedures Respiratory tract infections Dental infections or procedures Acute mediastinitis Pneumoperitoneum Esophageal perforation
n n n Substernal chest pain is the most frequent symptom Crepitation; air dissecting under the skin Dyspnea Dysphagia Dysphonia Hypotension (hemodynamic changes)
n n Physical examination reveals palpable subcutaneous emphysema in the neck On auscultation of the chest a clicking sound over the pericardium synchronous with the heartbeat (Hamman’s sign)

n Treatment: Supportive n Supplemental oxygen n Management of causes n Surgery, chest tube insertion when hemodynamic deterioriation is present or when associated with mechanical ventilation n
Esophageal perforation n n Iatrogenic esophageal perforation is the most common cause of acute mediastinitis Can also be: Postemetic (Boerhaave’s syndrome) n Trauma n Operative injury n Cancer erosion n Foreign body n
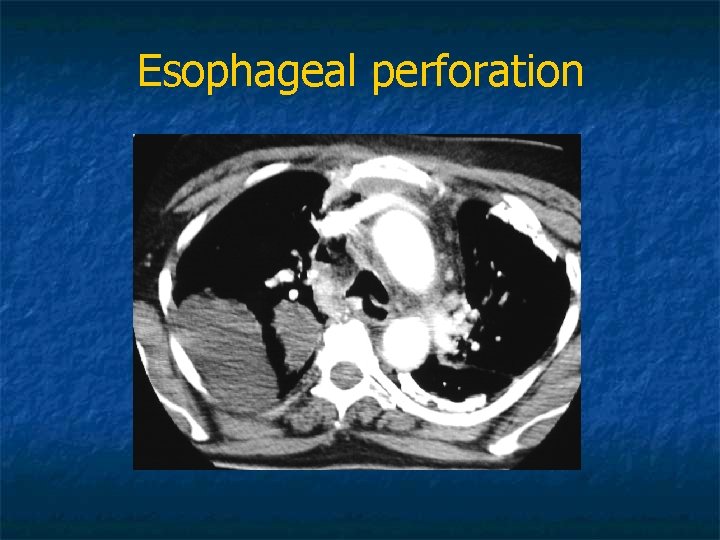
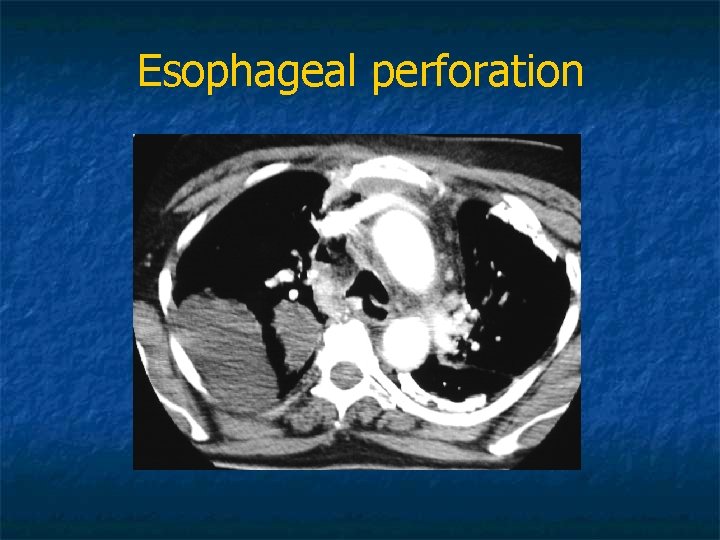
Esophageal perforation
Clinical signs and symptoms n n Abrupt onset of severe chest pain, fever, dyspnea, SVC symptoms Tachypnea, tachycardia, hypotension, cervical emphysema Shock develops quickly Chest Radiology: Upper mediastinal enlargement, emphysema, hydropnomothorax, multiple air fluid levels
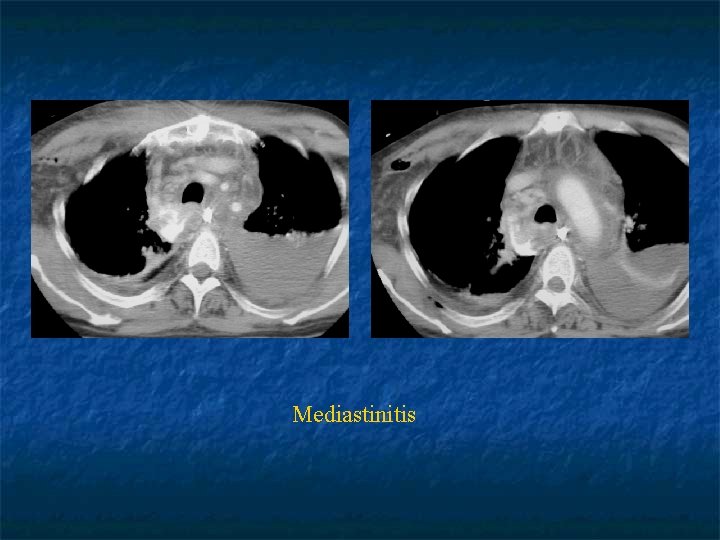
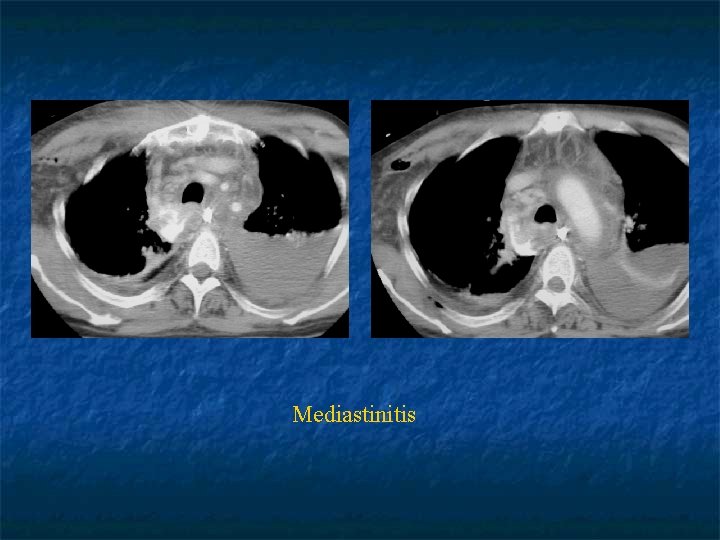
Mediastinitis
n Treatment: Surgical debridement of the necrotic tissue n Closure of the perforation n Drainage n Broad spectrum antibiotics with anaerobic coverage n Mortality rises when the treatment delay is more than 24 hours n
Diseases of the Diaphragm n n Diaphragma is a dome shaped musculotendinous structure that separates thoracic and abdominal cavities It consists of two parts: Right hemidiaphragm n Left hemidiaphragm n n Middle portion is made of the central tendon that doesn’t contract, it has two holes on The caval opening n The esophageal hiatus n
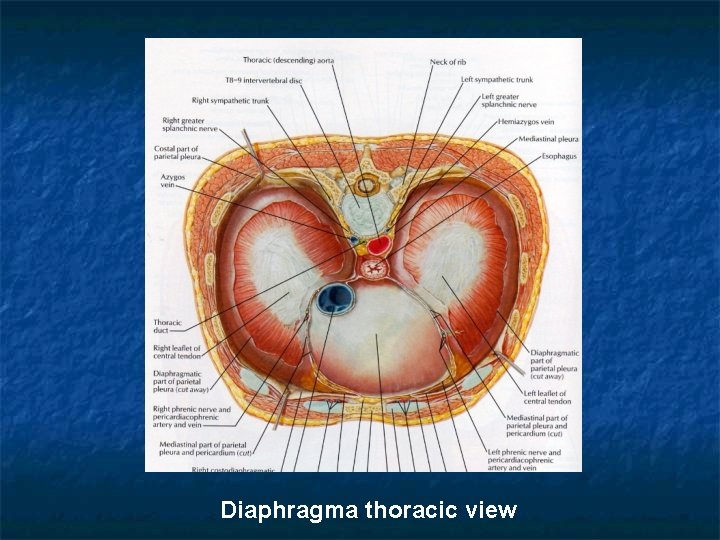
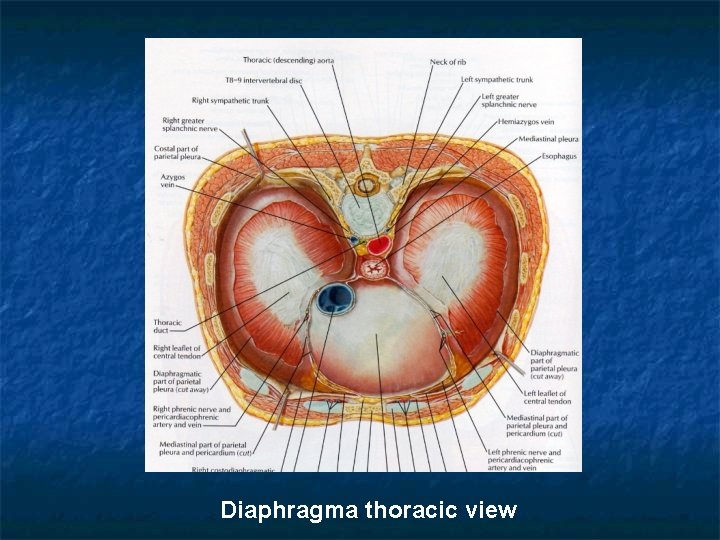
Diaphragma thoracic view
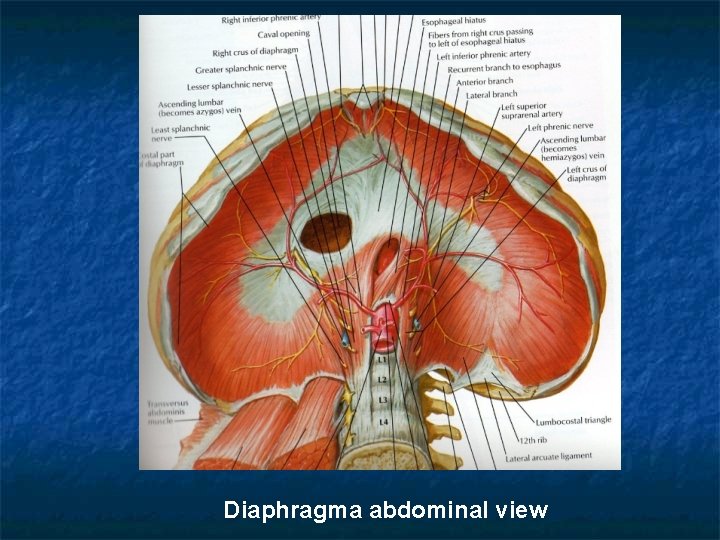
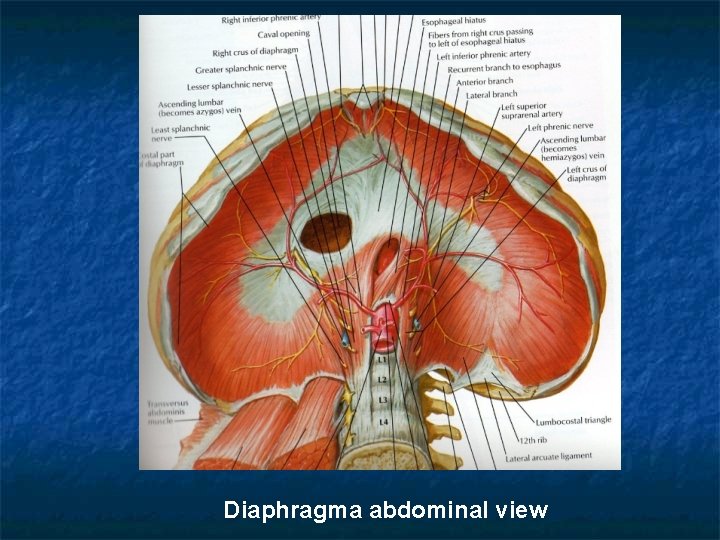
Diaphragma abdominal view
n n The muscle fibers of the crural part originate from lomber vertebrae The muscle fibers of the costal part originate from the processus xiphoideus and 7 -12 ribs The costal part contraction lowers the diaphragm and increases the rib cage When the crural part contracts only the diaphragm moves downward
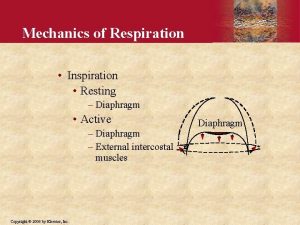
n n Motor inervation comes from cervical motor neurons (C 3 -5) conducted via N. Frenicus Diaphragm is the major inspiratuar muscle responsible from 70% of normal breathing.
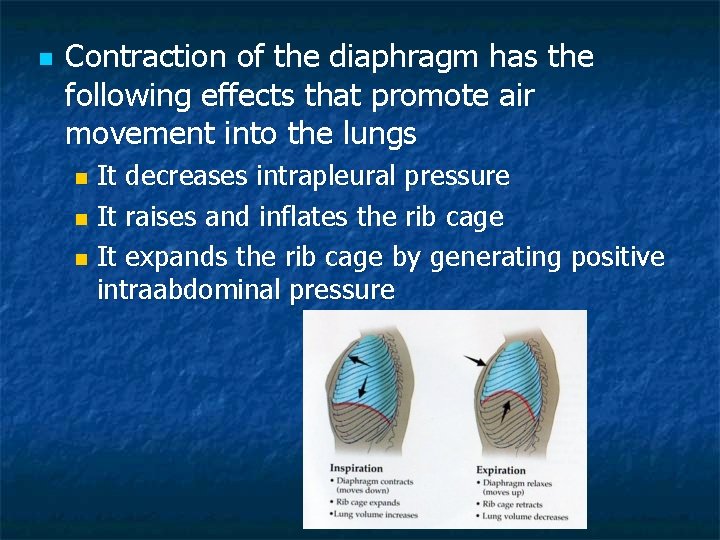
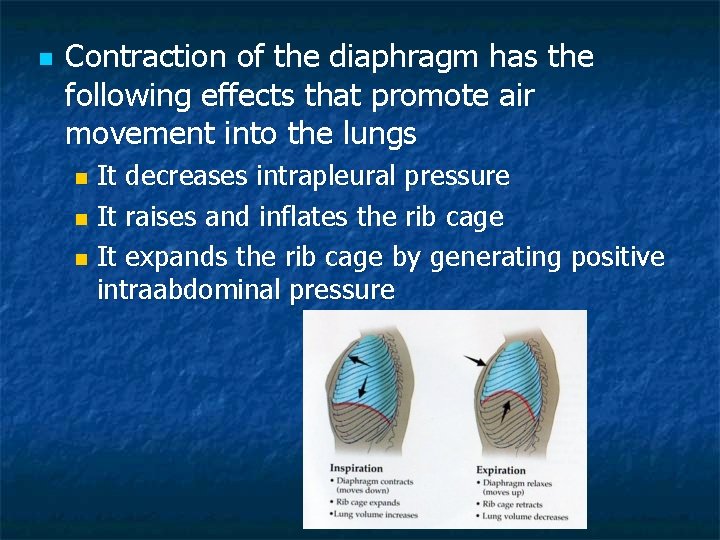
n Contraction of the diaphragm has the following effects that promote air movement into the lungs It decreases intrapleural pressure n It raises and inflates the rib cage n It expands the rib cage by generating positive intraabdominal pressure n
Diaphragmatic paralysis: n n Can be bilateral or involve only one side (unilateral) In this setting the accessory muscles of the respiration assume some or all the work of breathing

n n Patients with bilateral diaphragmatic paralysis typically present with dyspnea. It is associated with tachypnea and rapid shallow breathing Paradoxal motion of the anterior abdominal wall during inspiration can be detected Hypoxemia is common due to atelectasis and V/Q mismatch which worsens with sleep Disease progression is associated with progresive hypercapnia
n n Unilateral diaphragmatic paralysis is more common Often discovered incidentally on a chest radiograph and diagnosis can be made only by radiology (fluoroscopic sniff test) Patients who do not have underlying lung disease are usually asymphtomatic In fluoroscopic sniff test paradox elevation of the paralysed hemidiaphragm is positive >90% of the patients
Diaphragmatic Eventration n Eventration of the diaphragm is a disorder in which all or part of the diaphragmatic muscle is replaced by fibroelastic tissue.

n n Eventration of the diaphragm can be congenital or acquired Many patients are asymptomatic, especially when the eventration is localized Can be seen incidentally on chest x ray and The diagnosis is confirmed by fluoroscopy or ultrasonography. In infants the management depends on the extent of the respiratory distress, often no need to treatment
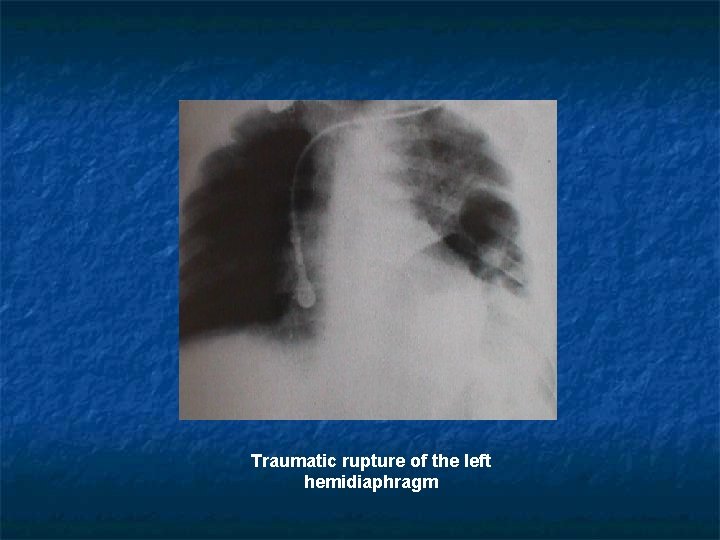
Diaphragmatic Hernia n Hiatal Hernias: Result when an abdominal structure usually the stomach extends through the diaphragmatic esophageal hiatus into the thorax. Manifests as a retrocardiac mass in the middle mediastinum n Traumatic rupture Seen in 1 -4% of blunt chest or abdominal trauma usually on the left posterolateral region
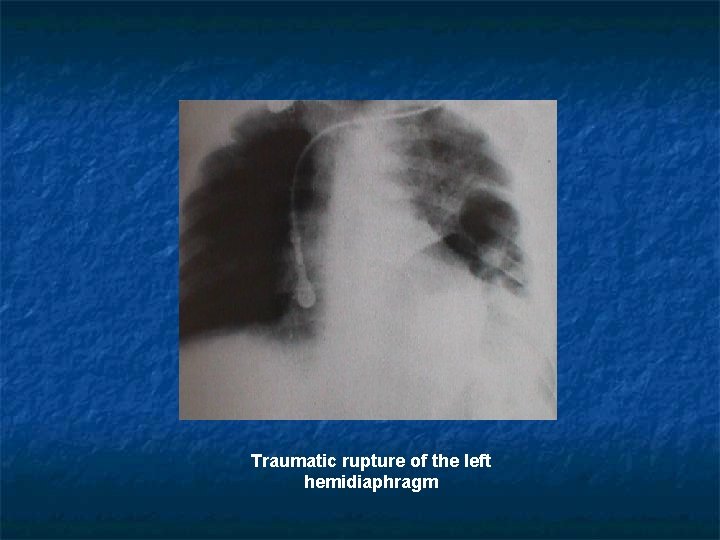
Traumatic rupture of the left hemidiaphragm
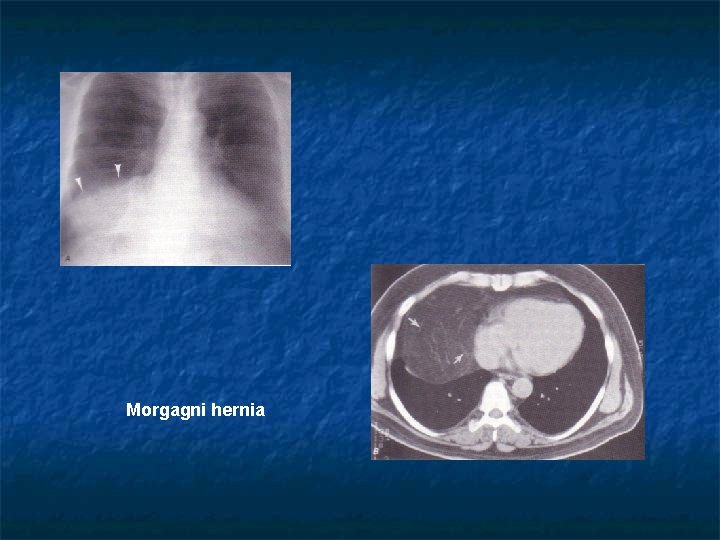
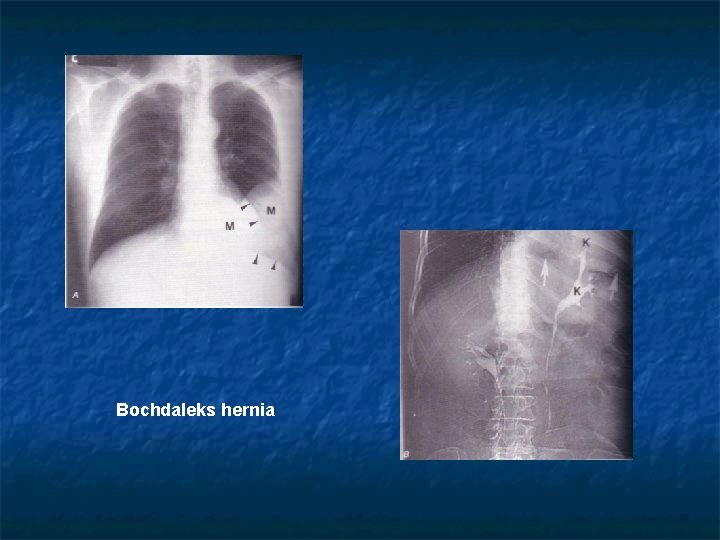
n Congenital Hernias: These are due to the failure of the normal fusion of the diaphragmatic components during embryologic development n Morgagni hernias: herniation of omentum and other abdominal contents into the thorax manifest as a right cardiophrenic angle mass n Bochdaleks hernias: May protrude into the posterior mediastinum Diagnosis can be established in diaphragmatic hernias by gastrointestinal barium study or CT. Treatment is surgical in symptomatic cases.
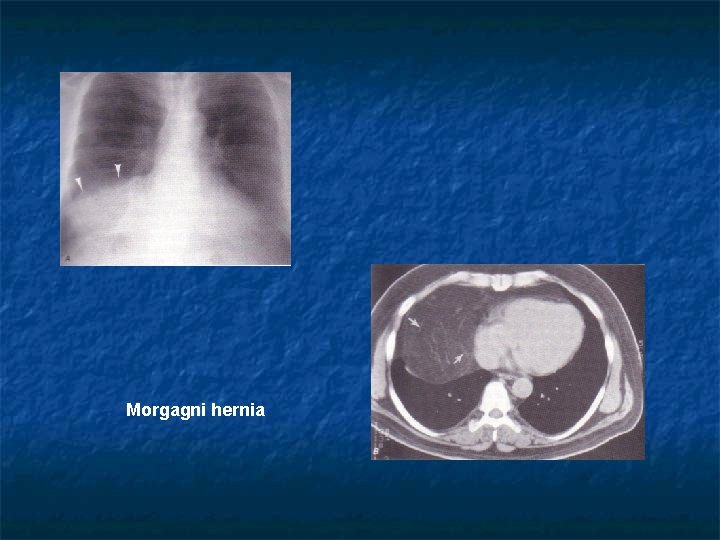
Morgagni hernia
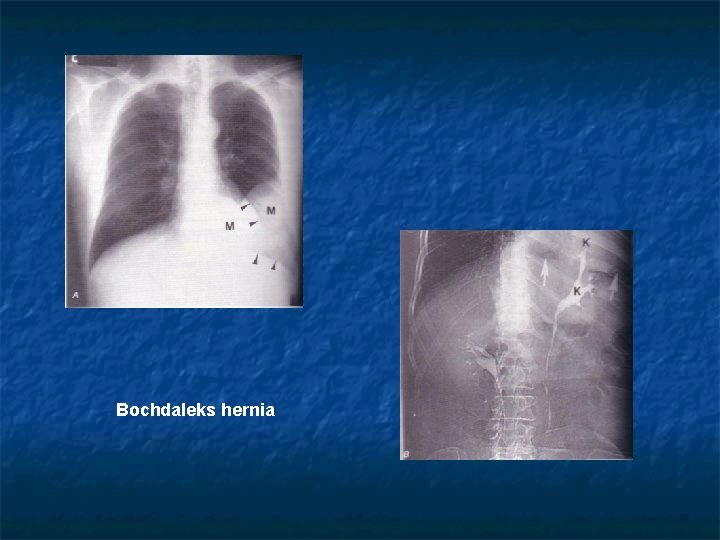
Bochdaleks hernia
 Lethenic
Lethenic Dr erdem ercan
Dr erdem ercan Mehmet ali ercan slayt
Mehmet ali ercan slayt Ercan güneri
Ercan güneri Metin ercan
Metin ercan Bulbin kivanc
Bulbin kivanc Awoss
Awoss Ercan tutak
Ercan tutak Dr ercan madenci
Dr ercan madenci Dr erdem ercan
Dr erdem ercan Mehmet ali ercan sunu
Mehmet ali ercan sunu Persantil
Persantil Flask shaped gland
Flask shaped gland Pericardium layers
Pericardium layers Difference between mercury cell and diaphragm cell
Difference between mercury cell and diaphragm cell Diaphragm muscle origin and insertion
Diaphragm muscle origin and insertion Diaphragm openings
Diaphragm openings Diaphram openings
Diaphram openings Kidney system
Kidney system Median arcuate ligament
Median arcuate ligament Maxp series pumps
Maxp series pumps Ibn sina university of medical and pharmaceutical sciences
Ibn sina university of medical and pharmaceutical sciences Mediastinum
Mediastinum Boundaries of mediastinum
Boundaries of mediastinum Bracnhes of aorta
Bracnhes of aorta Mediastinum subdivision
Mediastinum subdivision Anterior mediastinum contents
Anterior mediastinum contents Posterior mediastinum contents
Posterior mediastinum contents Burak oğuzhan karapınar
Burak oğuzhan karapınar Hilukset ja mediastinum
Hilukset ja mediastinum Mediastinum ehk
Mediastinum ehk Hageløft
Hageløft Mediastinum contents
Mediastinum contents Mediastinum heart
Mediastinum heart Mediastinum inferior
Mediastinum inferior Mediastinum heart
Mediastinum heart Cadaver blood vessels
Cadaver blood vessels Mediastinum heart
Mediastinum heart Cardiac plexus
Cardiac plexus Ejaculatory duct
Ejaculatory duct Lymphatic drainage of thorax
Lymphatic drainage of thorax Pleural recesses
Pleural recesses Spatium intercostalis
Spatium intercostalis Veterinary radiology middlesex county
Veterinary radiology middlesex county Male rat anatomy
Male rat anatomy Diaphragm of rat
Diaphragm of rat Air under diaphragm
Air under diaphragm A regulator diaphragm is often made from
A regulator diaphragm is often made from Increased retrosternal space
Increased retrosternal space Pillar microscope function
Pillar microscope function Hyperresonance sound
Hyperresonance sound Rhinarium
Rhinarium Cupola of the diaphragm
Cupola of the diaphragm Signo rigler
Signo rigler Centrum tendineum diaphragm
Centrum tendineum diaphragm Slack diaphragm gauge
Slack diaphragm gauge Plot
Plot Mesosalpinx
Mesosalpinx Pressure gauge wiki
Pressure gauge wiki Autoclave
Autoclave Oaw welding process
Oaw welding process Parts of the microscope
Parts of the microscope Pectoralis minor origo insertio
Pectoralis minor origo insertio Uneven diaphragm
Uneven diaphragm Linear immunofluorescence vs granular
Linear immunofluorescence vs granular Why do cells need oxygen?
Why do cells need oxygen? Aro diaphragm pump troubleshooting
Aro diaphragm pump troubleshooting