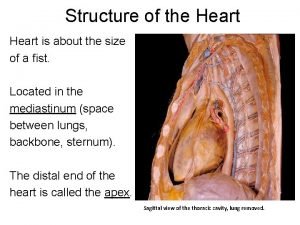
THE HEART Anatomy In pericardial sac win mediastinum
- Slides: 45
THE HEART
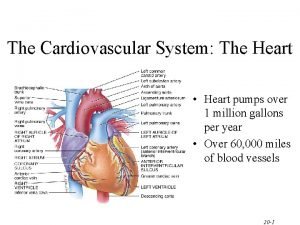
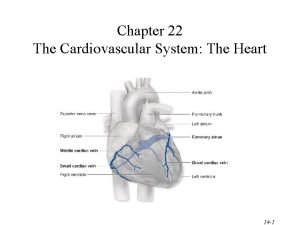
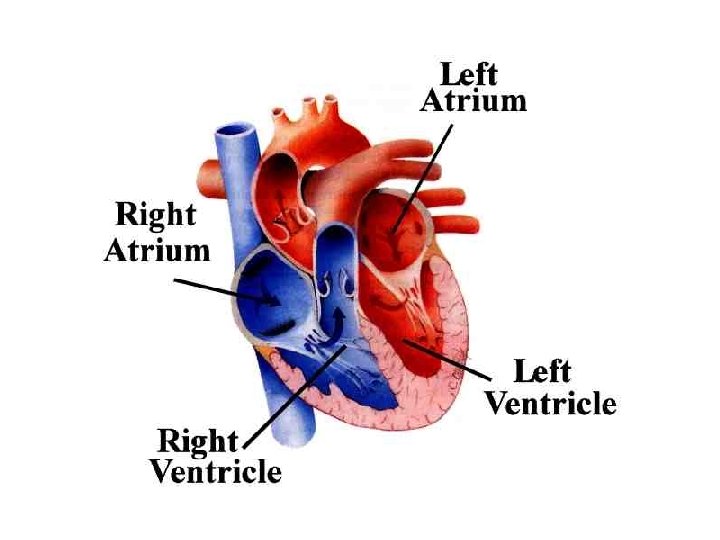
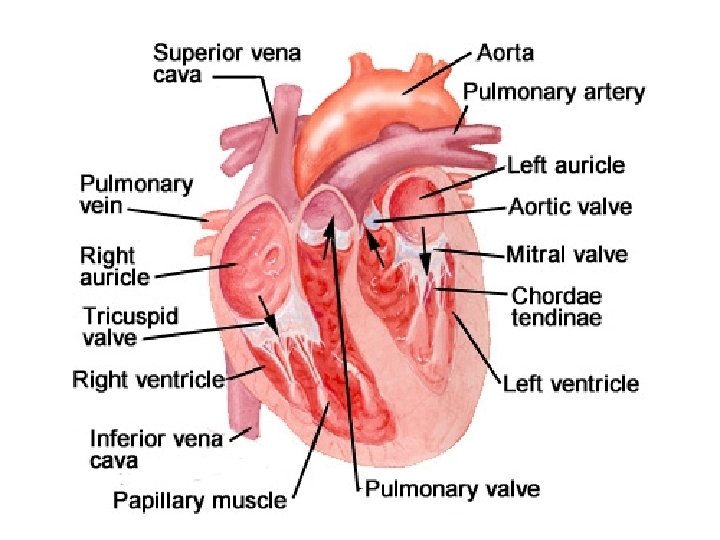
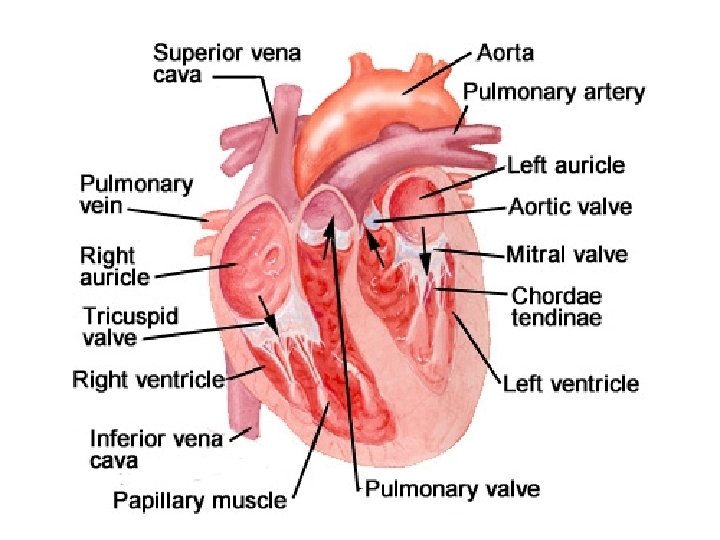
Anatomy • In pericardial sac – w/in mediastinum • Four muscular chambers (Fig. 22 -1) – Walls (Fig. 22 -2) • Myocardium -- thickest layer – Muscle fibers • Endocardium – Internal lining – Continuous with internal tissue layer of vessels
Anatomy – cont’d – L, R ventricles – pumping • At bottom • About 60% of heart volume • Left ventricle (LV) largest chamber – L, R atria - "priming" • At top • Thinner muscle layer than ventricles
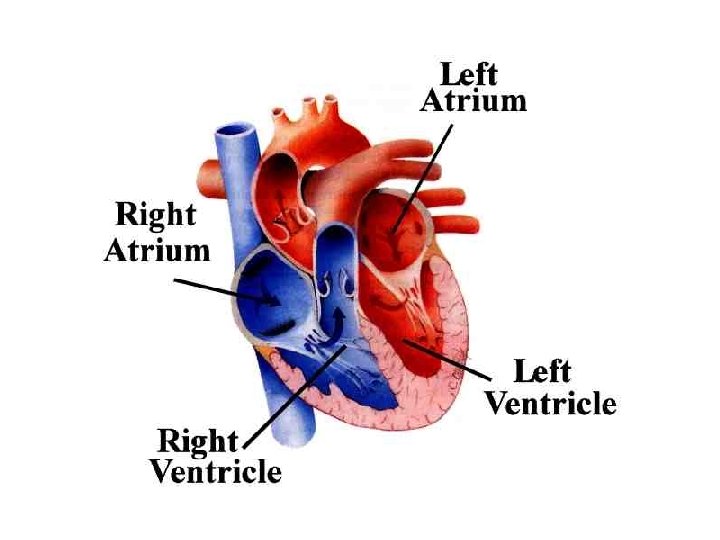
Anatomy – cont’d • Path of blood flow (Fig. 22 -3) – Vena cava RA RV lungs LA LV aorta systemic circulation vena cava (and repeat) • KNOW THIS!!!
Anatomy – cont’d • Valves (Fig. 22 -4) – Connective tissue covered in endothelium – Continuous with endothelium of heart – Open, close passively in response to ventricular contraction
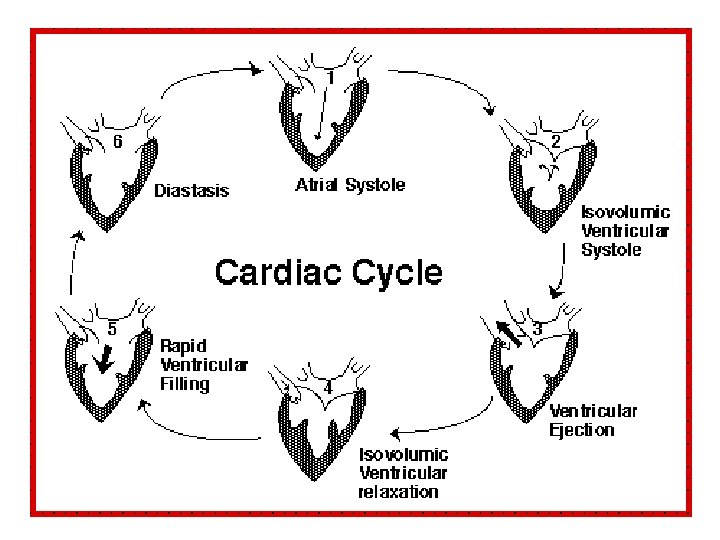
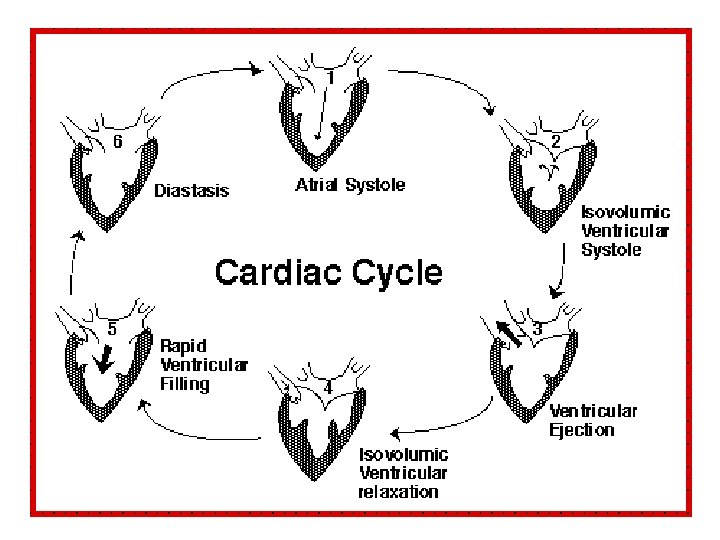
Anatomy – cont’d • Valves – cont’d – Two types: • Atrioventricular – between atria, ventricles – Tricuspid right – Bicuspid (mitral) left • Semilunar between ventricles, vessels – Pulmonary right – Aortic left • Cardiac Cycle (Fig. 22 -5) – Ventricular contraction during systole and diastole
Factors Affecting Cardiac Performance • Cardiac output (C. O. ) = heart rate x stroke volume – OR: amount of blood pumped from the ventricle with each contraction (in L/min) • Heart rate (h. r. ) measured in beats/min – Controlled by ANS • Dually innervated • Incr’d sympathetic signals incr’d h. r. • Parasymp signals decr’d h. r. – In control in resting heart
• Stroke volume (S. V. ) measured in L/beat • Dependent on – Contractility • Defined – ability of heart muscle to contract – Force of contraction of heart – Afterload • Defined – force that opposes ejection of blood • For LV, this is aortic blood pressure • If afterload incr’d decr’d stroke volume, so decr’d C. O.
– Preload • Amount of filling of ventricle during relaxation • By Starling’s law: incr’d preload (within limits) incr’d force of contraction incr’d C. O. (Fig. 2217)
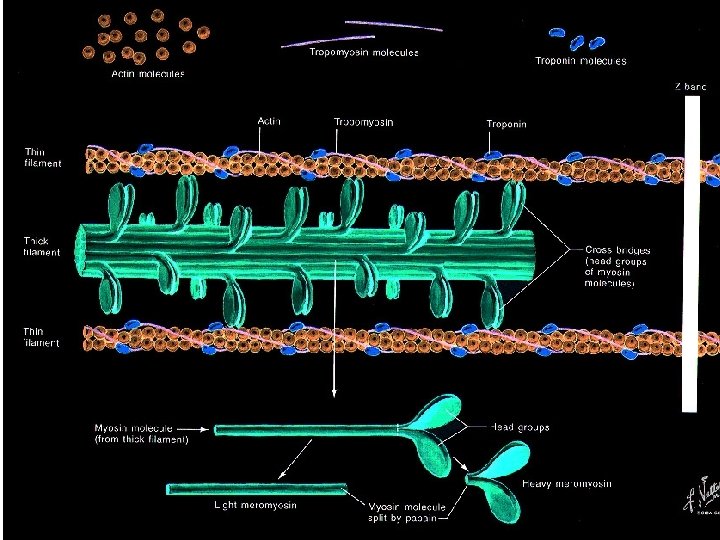
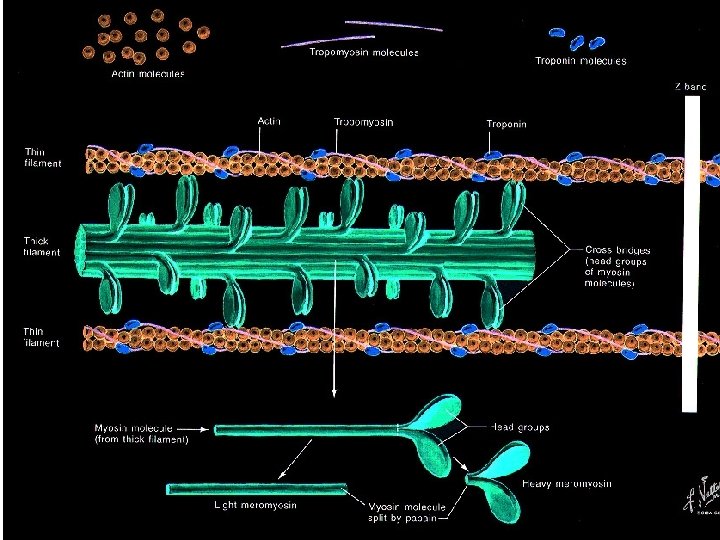
Myocytes (cells of heart) -- there are two types: • Contractile Fibers (“usual” cardiac muscle cells) – Contract during systole – Have actin and myosin proteins (Fig. 22 -15) – Contraction w/ sodium, calcium into and w/in muscle cells incr’d Ca+2 inside cell – Ca+2 binds to actin/myosin shift in actin w/ respect to myosin shortening of muscle fiber and contraction (Fig. 22 -16)
Myocytes – cont’d • Conduction system cells – VERY SIMPLISTICALLY: a hybrid of contractile fibers + neuronal cells – Depolarize quickly – Specialized to coordinate and conduct impulses proper timing of contractile fiber contraction in different heart areas
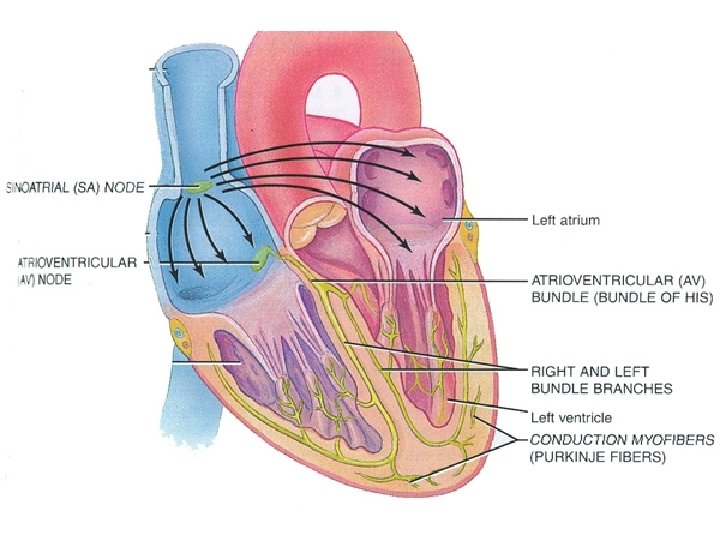
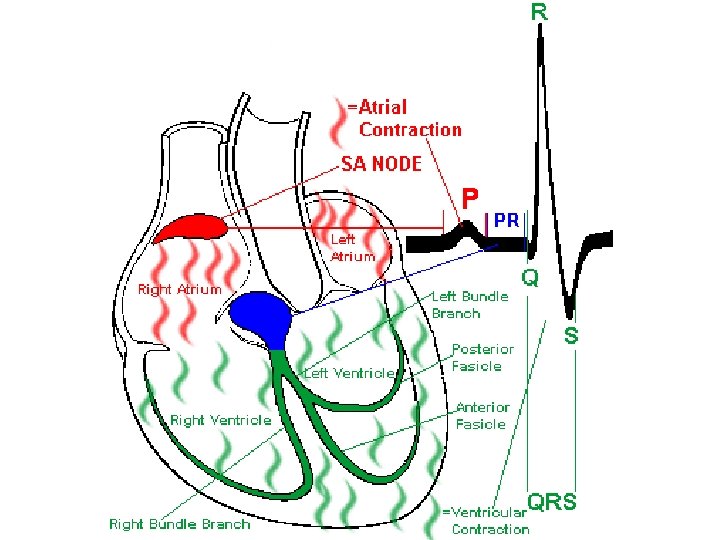
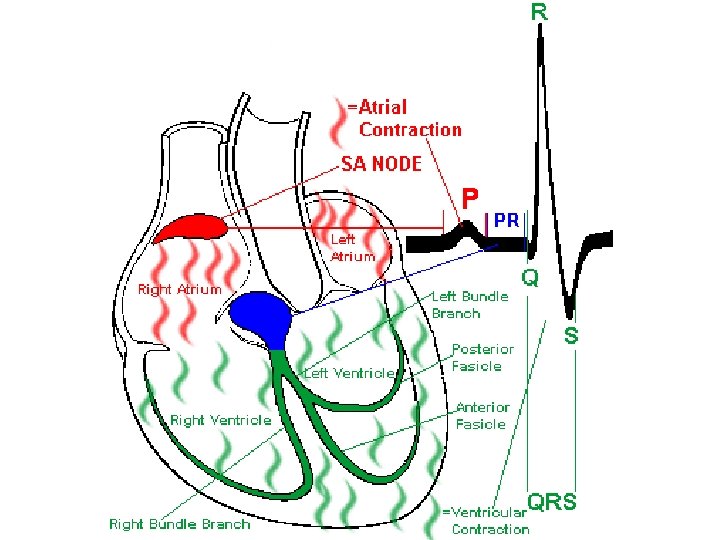
Conduction System – cont’d • Parts of the conduction system (Fig. 22 -11): – Sino. Atrial Node (SA) • In atrium • Receives autonomic input • When stimulated, signals atrial contractile fibers atria depolarization and contraction
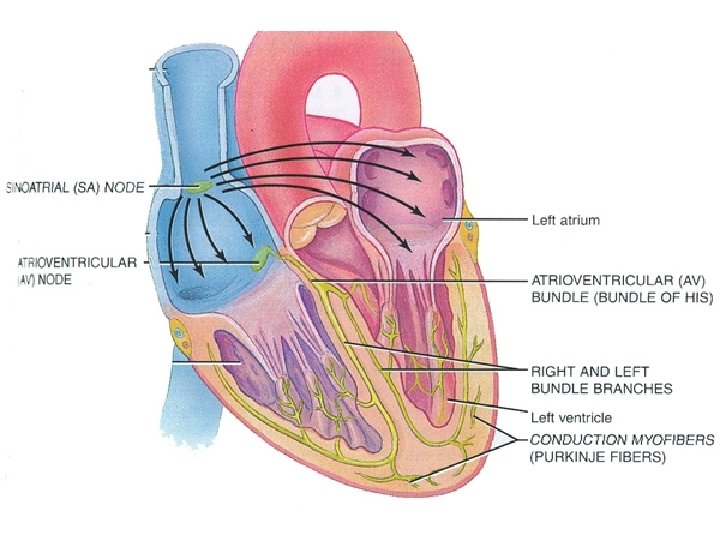
Conduction System – cont’d – Atrio. Ventricular Node (AV) • Between atrium/ventricle • Receives signal from SA node – His Bundle (= AV Bundle) • Receives signal from AV node • Sends signal from top to bottom of heart, between ventricles to:
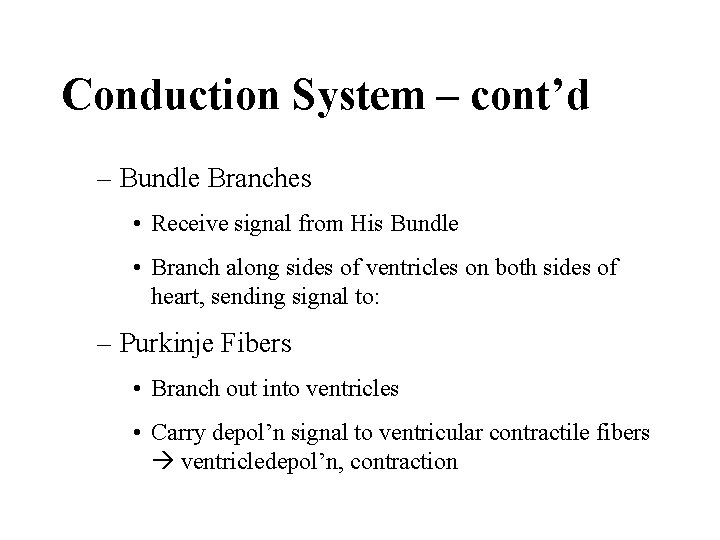
Conduction System – cont’d – Bundle Branches • Receive signal from His Bundle • Branch along sides of ventricles on both sides of heart, sending signal to: – Purkinje Fibers • Branch out into ventricles • Carry depol’n signal to ventricular contractile fibers ventricledepol’n, contraction
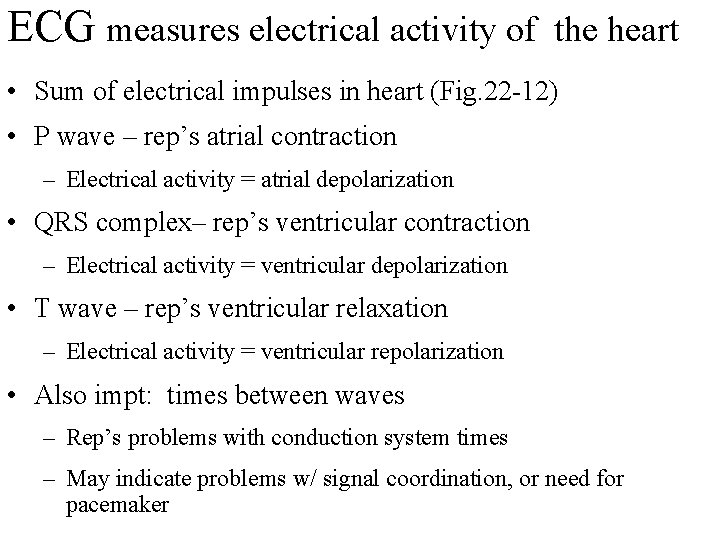
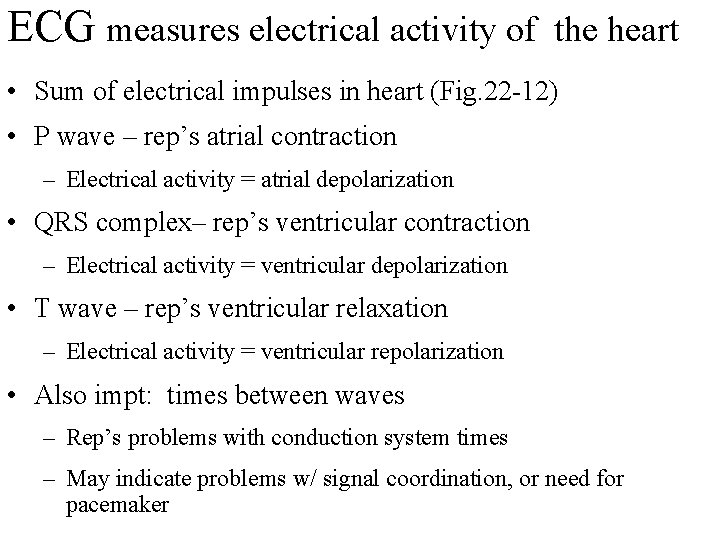
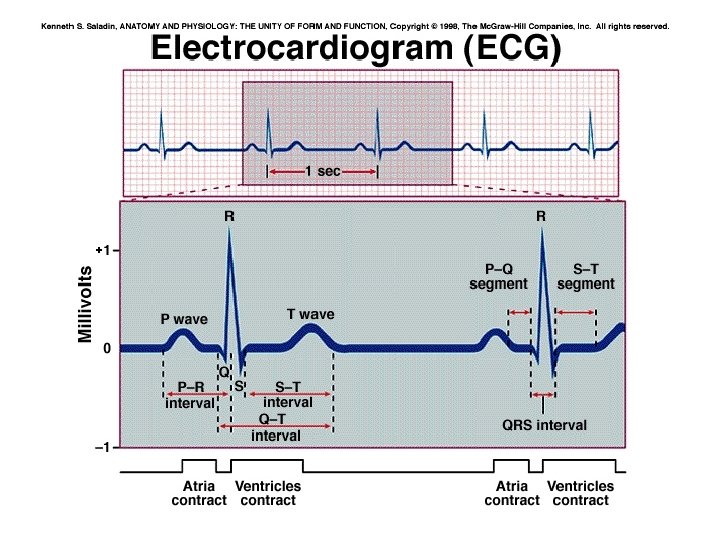
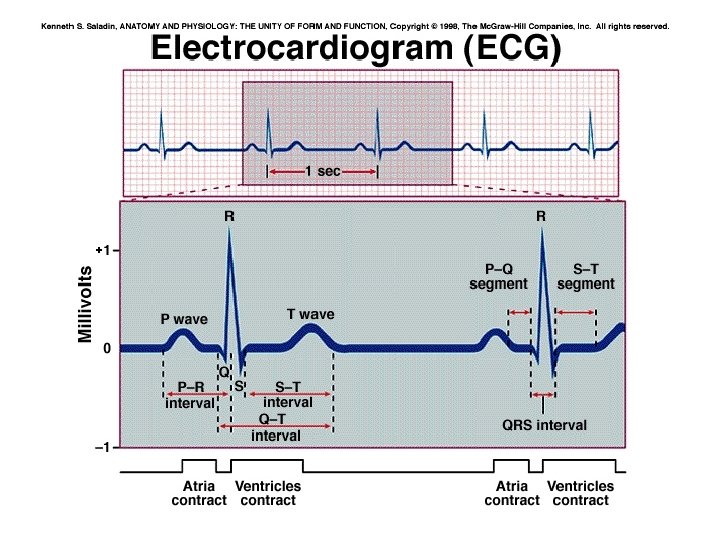
ECG measures electrical activity of the heart • Sum of electrical impulses in heart (Fig. 22 -12) • P wave – rep’s atrial contraction – Electrical activity = atrial depolarization • QRS complex– rep’s ventricular contraction – Electrical activity = ventricular depolarization • T wave – rep’s ventricular relaxation – Electrical activity = ventricular repolarization • Also impt: times between waves – Rep’s problems with conduction system times – May indicate problems w/ signal coordination, or need for pacemaker
Heart Failure • Defined: heart as pump is insufficient to meet metabolic requirements of tissues • Acute – develops quickly – Approx 65% survival rate • Chronic – gradual burden on heart – Most common cause: ischemic heart disease
Disorders of Heart Wall • Pericarditis – Acute – inflammation of pericardial membrane(s) • Caused by – Infection – Diseases of connective tissue – Radiotherapy • toughening of membrane
Disorders of Heart Wall – cont’d – Chronic -- may scarring and fibrotic lesions • encasing heart (membranes no longer compliant) • Also causes incr’d back pressures at veins entering heart, enlargement of liver and/or spleen
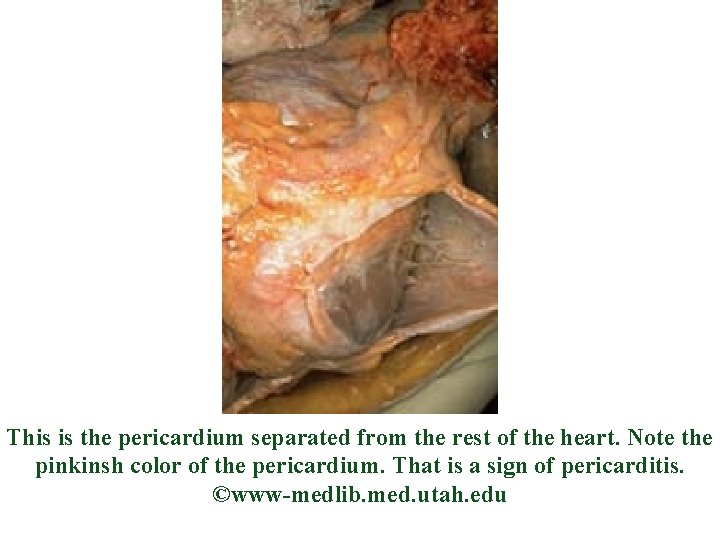
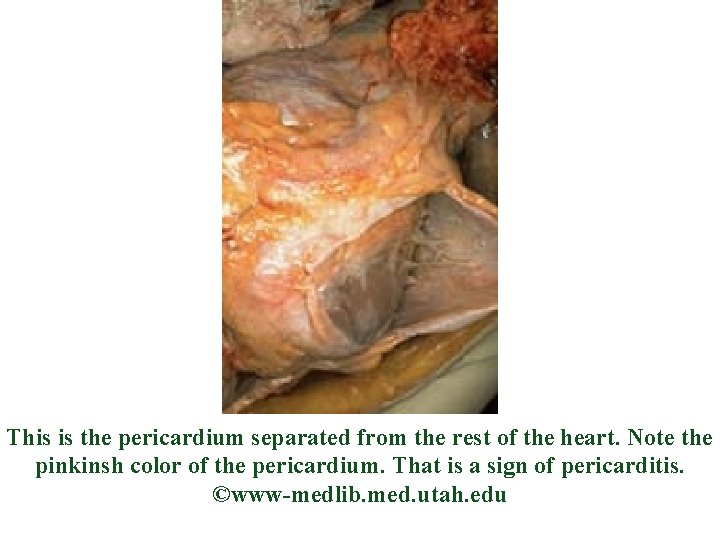
This is the pericardium separated from the rest of the heart. Note the pinkinsh color of the pericardium. That is a sign of pericarditis. ©www-medlib. med. utah. edu
Disorders of Myocardium = Cardiomyopathies • REMEMBER: myocardium = heart’s muscle layer • Most cases, cause unknown • All cases, heart loses ability as pump (because muscle fibers are dysfunctional)
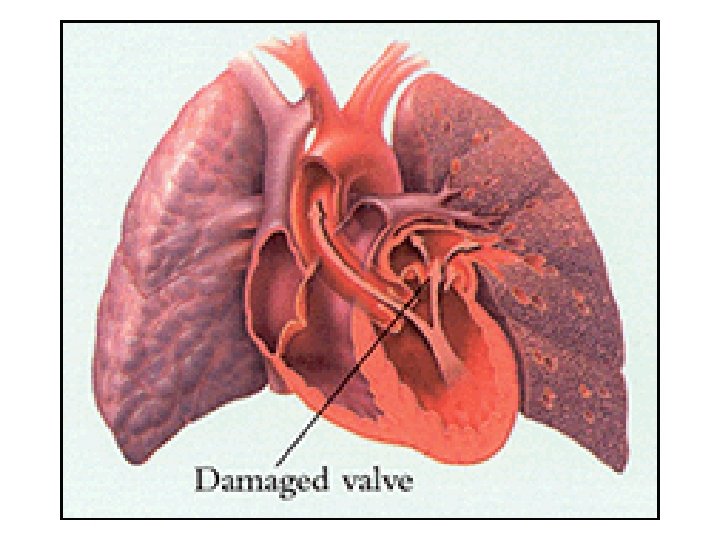
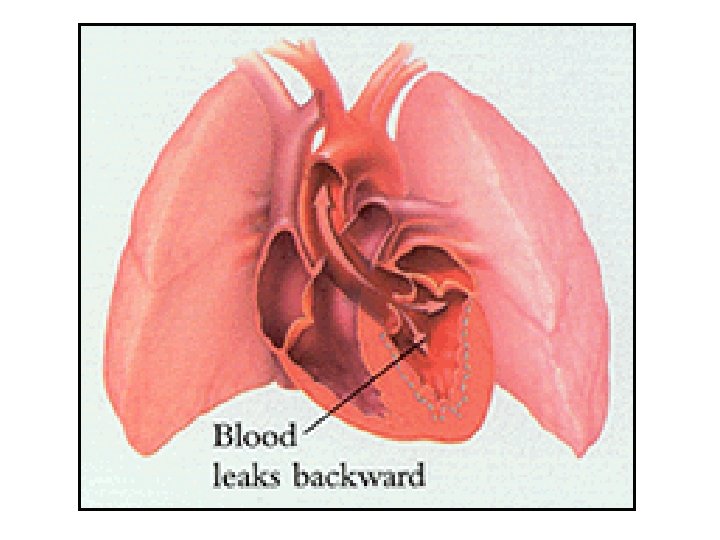
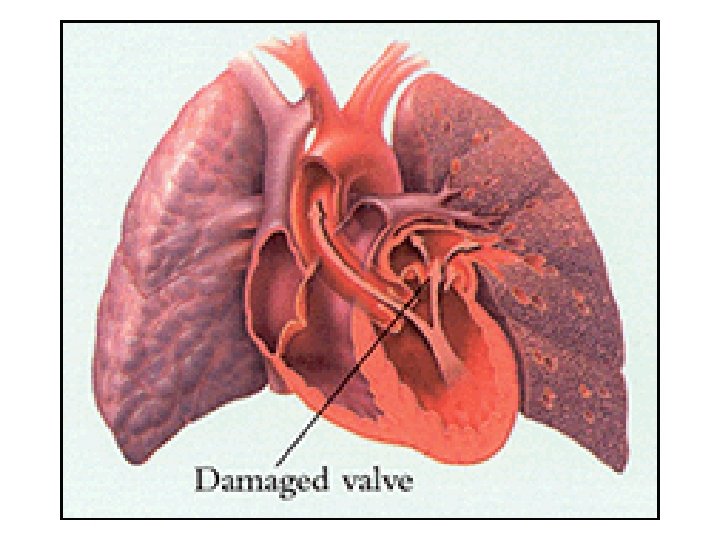
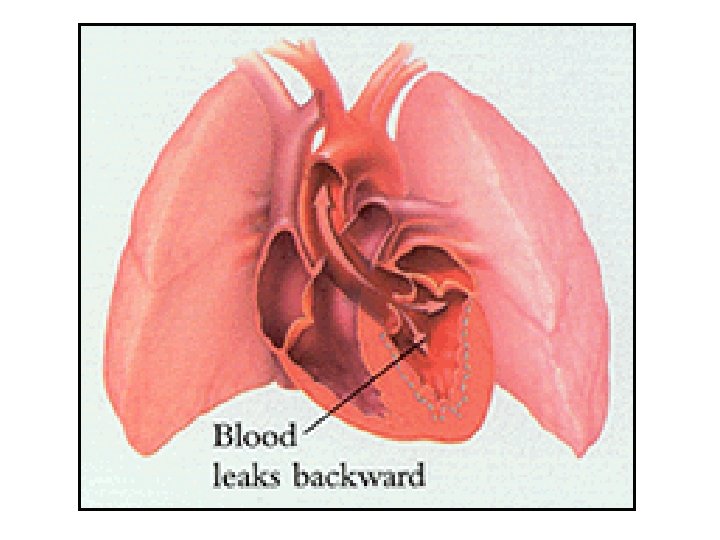
Disorders of Endocardium (Valvular Disease)(Table 23 -8) • Causes abnormal blood flow across valves and through heart • Two types (Fig. 23 -28): – Too narrow = stenosis – Too leaky = regurgitation • (Murmur = turbulent blood flow due to valvular lesions)
Valvular Diseases – cont’d • Overall both types cause – Incr’d cardiac work – Incr’d volume & pressures in heart chambers • Leads to – Chamber dilation – Hypertrophy of contractile fibers • Compensations to incr heart’s pumping capacity
Valvular Diseases – cont’d • Once believed due only to rheumatic fever – Strep infection damage of valve tissue by strep microorganism • Also, strep antigens appear similar to valve cell proteins • autoimmune response
Valvular Diseases – cont’d – Results in • Adhesions on valves, or • Fusion of valve tissues, or • Calcification/fibrosis – Other causes now known • Congenital disorders • Degenerative disorders
Valvular Diseases – cont’d • Mitral stenosis (Fig. 23 -29) – Impedes blood flow from LA to LV • Most common of valve diseases • Decr’d flow from LA to LV during filling • LA must pump (hard) to move blood LV • Results in hypertrophy of LA – Also, decr’d preload at LV
Mitral Stenosis – cont’d – Change in pressure between chambers • By causing LA to become pump: – Get incr’d pulmonary vascular pressures » So pressures increase through LA into lung – pulmonary congestion – lung tissue changes to accommodate incr’d pressures – increased pressure in pulmonary artery – increased pressure in right heart – right heart failure
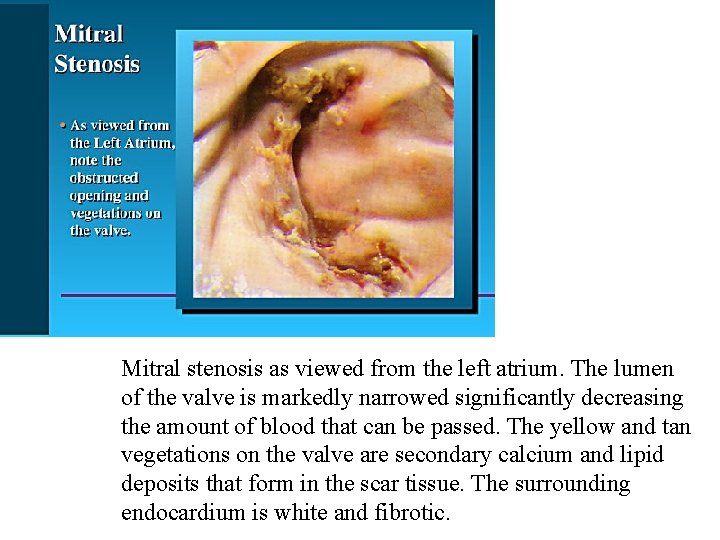
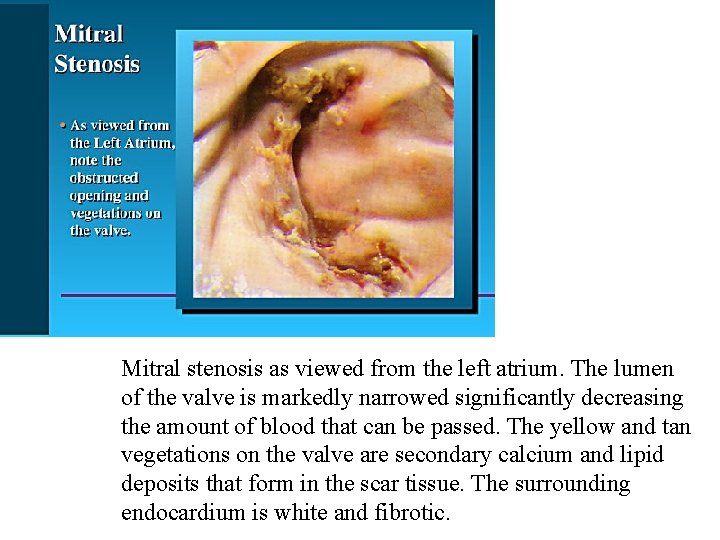
Mitral stenosis as viewed from the left atrium. The lumen of the valve is markedly narrowed significantly decreasing the amount of blood that can be passed. The yellow and tan vegetations on the valve are secondary calcium and lipid deposits that form in the scar tissue. The surrounding endocardium is white and fibrotic.
Mitral Stenosis – cont’d – Clinical • Dyspnea = difficulty breathing • Tachycardia = increased heart rate – Compensation for lowered C. O. • LA pressure
Valvular Diseases – cont’d • Mitral regurgitation (now same valve but too leaky) – As ventricle contracts, blood goes in two directions: – Get both LA LV and retrograde flow (LV to LA) • Blood simultaneously to aorta and back to LA • both LV and LA pump harder (move same blood twice) • LV hypertrophy and dilation as compensation • Compensation works awhile, then decr’d C. O. • heart failure
Mitral regurgitation – cont’d • Also LA hypertrophy – LA can’t protect lungs from incr’d fluid pressures in heart chambers (blood not moved through chambers effectively) • increased pressures through lungs incr’d pressures in right heart failure • Can see edema, shock
Mitral regurgitation – cont’d – Clinical • Weakness, fatigue – Why? • Dyspnea – Why? • Palpitations – If acute, heart can't compensate – Mitral valve prolapse -- common valve disorder (Fig. 23 -30) • Cusps of valve “billow” into atrium • Can mitral regurgitation
Valvular Diseases – cont’d • Aortic stenosis – Blood flow obstructed from LV into aorta during systole • Causes incr'd work of LV • LV hypertrophy as compensation • Results in LV wall stiffening • pressure changes between LV, aorta • prolonged contractions as compensation • Finally heart overwhelmed • increased pressures in LA, then lungs, then right heart
Aortic stenosis – cont’d – Clinical • Angina • Syncope • LV failure
Valvular Diseases – cont’d • Aortic regurgitation – Reflux blood from aorta to LV during ventricular relaxation • Causes LV to pump more blood w/ each contraction • LV hypertrophy – “Globular shape” • incr’d pressures in LA, lung, right heart
Aortic regurgitation – cont’d – Clinical • Palpitations • Fatigue • Dyspnea • Angina
Valvular Diseases – cont’d • Treatment for all valve disorders: – Antibiotics for strep – Antiinflammatories for autoimmune disorder – Analgesics for pain – Restrict physical activity – Valve replacement surgery
 Pericardium
Pericardium Win-win win-lose lose-lose
Win-win win-lose lose-lose Think win-win real life examples
Think win-win real life examples Win win win lose lose lose
Win win win lose lose lose Dot
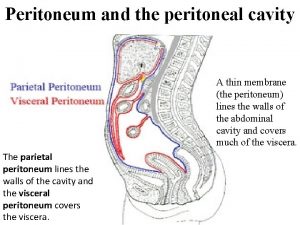
Dot Splenic recess of omental bursa
Splenic recess of omental bursa Omental (epiploic) foramen
Omental (epiploic) foramen Peritoneal cavity,
Peritoneal cavity, Greater and lesser sac of peritoneum
Greater and lesser sac of peritoneum Definition of mediastinum
Definition of mediastinum Mediastinal
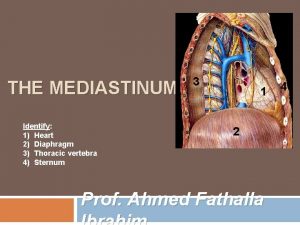
Mediastinal Mediastinum heart
Mediastinum heart Mediastinum heart
Mediastinum heart Heart orientation
Heart orientation Cadaver blood vessels
Cadaver blood vessels Win win nacin placanja
Win win nacin placanja Enlarging the pie
Enlarging the pie Conflict resolution win win
Conflict resolution win win Win win or no deal
Win win or no deal Win win situation examples
Win win situation examples Win win strategies
Win win strategies Lose-win attitude
Lose-win attitude Win win or no deal
Win win or no deal Think win win
Think win win Pericardial cavity
Pericardial cavity Pericardial friction
Pericardial friction Fossa ovalis and foramen ovale
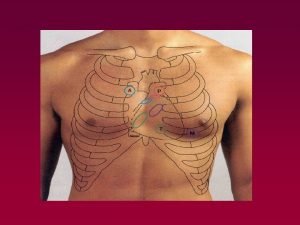
Fossa ovalis and foramen ovale Heart apex base
Heart apex base Sterno pericardial ligament
Sterno pericardial ligament Cardiac landmarks
Cardiac landmarks Pericardial fluid
Pericardial fluid Srijoy mahapatra
Srijoy mahapatra Sulcus terminalis heart
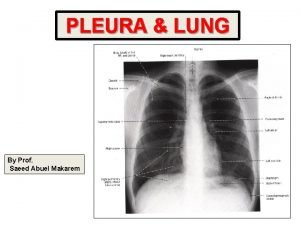
Sulcus terminalis heart Mediastinum
Mediastinum Septal ventricular defect
Septal ventricular defect Mediastinum structures
Mediastinum structures Posterior mediastinum contents
Posterior mediastinum contents Mediastinum
Mediastinum Mediastiinum
Mediastiinum Anterior mediastinum contents
Anterior mediastinum contents Spatia intercostalia
Spatia intercostalia Contents of the middle mediastinum
Contents of the middle mediastinum Hageløft
Hageløft Vas deferens and spermatic cord
Vas deferens and spermatic cord Mediastinum and diaphragm
Mediastinum and diaphragm Lig. vestibulare
Lig. vestibulare