Introduction The pericardium also called pericardial sac is
![DETERMINATION OF RISK AND NEED FOR HOSPITALIZATION • Fever (>38ºC [100. 4ºF]) and leukocytosis DETERMINATION OF RISK AND NEED FOR HOSPITALIZATION • Fever (>38ºC [100. 4ºF]) and leukocytosis](https://slidetodoc.com/presentation_image_h/11d67373c6cf6f452cc4af0304512f21/image-17.jpg)
- Slides: 34
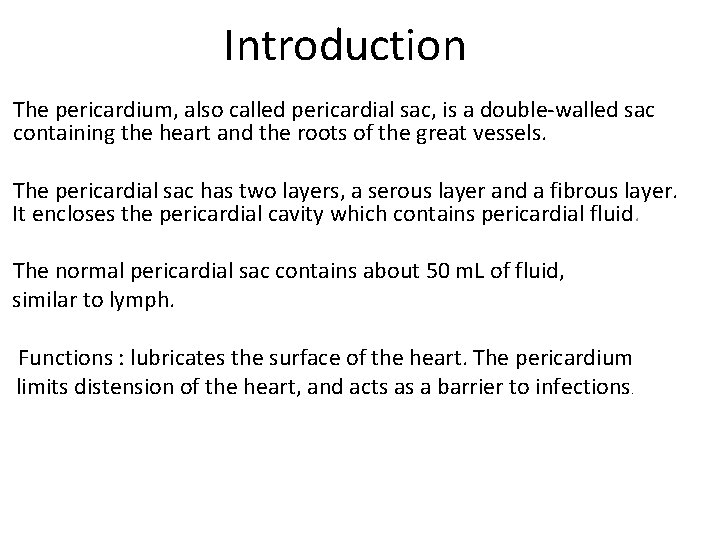
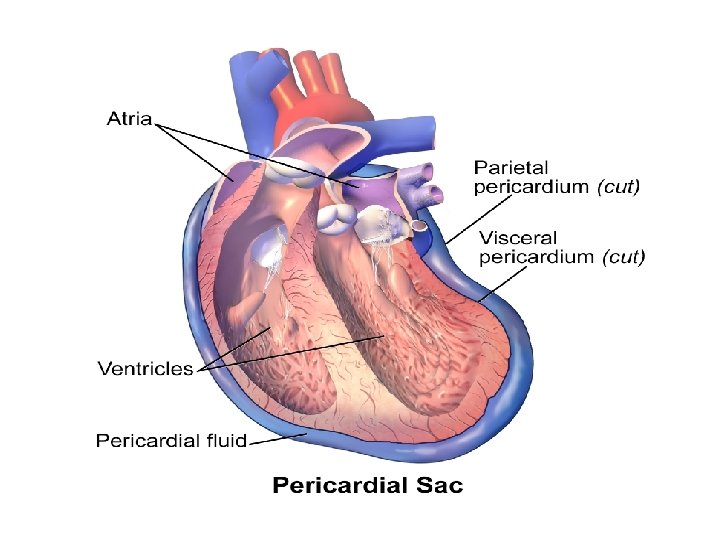
Introduction The pericardium, also called pericardial sac, is a double-walled sac containing the heart and the roots of the great vessels. The pericardial sac has two layers, a serous layer and a fibrous layer. It encloses the pericardial cavity which contains pericardial fluid. The normal pericardial sac contains about 50 m. L of fluid, similar to lymph. Functions : lubricates the surface of the heart. The pericardium limits distension of the heart, and acts as a barrier to infections.
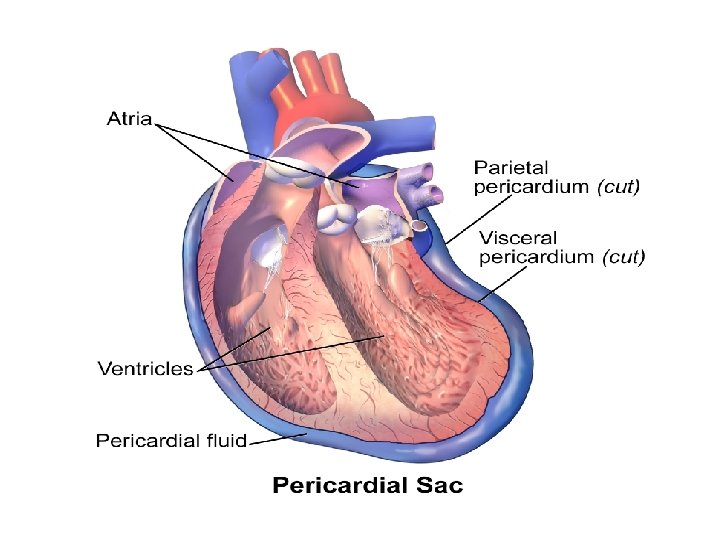
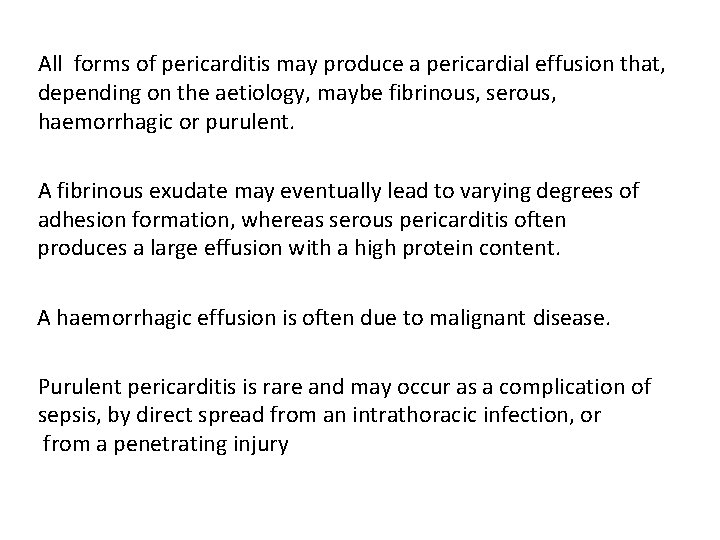
All forms of pericarditis may produce a pericardial effusion that, depending on the aetiology, maybe fibrinous, serous, haemorrhagic or purulent. A fibrinous exudate may eventually lead to varying degrees of adhesion formation, whereas serous pericarditis often produces a large effusion with a high protein content. A haemorrhagic effusion is often due to malignant disease. Purulent pericarditis is rare and may occur as a complication of sepsis, by direct spread from an intrathoracic infection, or from a penetrating injury
Acute pericarditis refers to inflammation of the pericardial sac. Acute pericarditis is the most common disorder involving the pericardium. Could be an isolated finding or associated with other diseases. The term myopericarditis, or perimyocarditis, is used for cases of AP that also demonstrate myocardial inflammation
Etiology Infection • Viral • Bacterial • Tuberculosis Inflammatory • Rheumatoid arthritis • Systemic lupus erythematosus • Rheumatic fever Other • Post-myocardial infarction • Uraemia • Malignancy • Trauma
The majority of patients recover within 1 -3 weeks , However some patients have a prolonged course or recurrent symptoms. Complications Pericardial effusion Cardiac tamponade
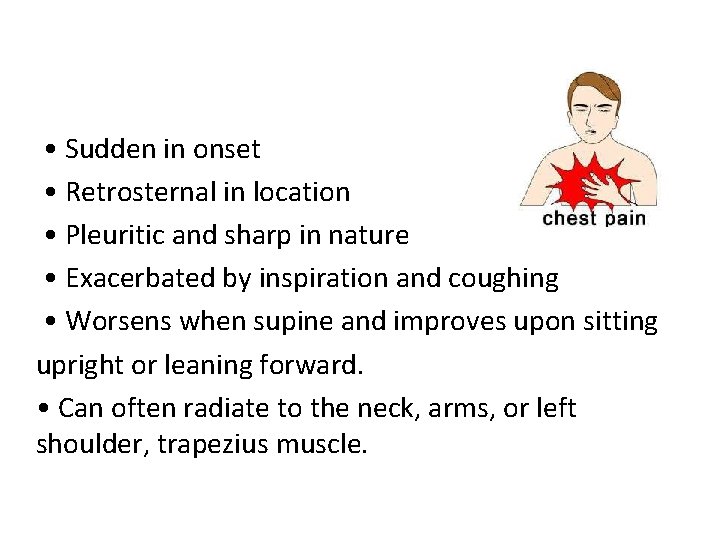
• Sudden in onset • Retrosternal in location • Pleuritic and sharp in nature • Exacerbated by inspiration and coughing • Worsens when supine and improves upon sitting upright or leaning forward. • Can often radiate to the neck, arms, or left shoulder, trapezius muscle.
Pericardial friction rub Caused by fricition between visceral and parietal layers Present in 85% of cases of pericarditis Usually diagnostic A high-pitched scratchy or squeaky sound best heard with the diaphragm at the LSB with the patient leaning forward during expiration. Have 3 compenents (patients may have any or all ) Presystole (atrial systole ) ventricular systole ( most frequent and loudest) early diastole
Usually heard in systole , but audiable in diastole Pericardial friction rub is audible throughout the respiratory cycle, whereas the pleural rub disappears when respirations are on hold. Low grade fever is common , leukocytosis may present
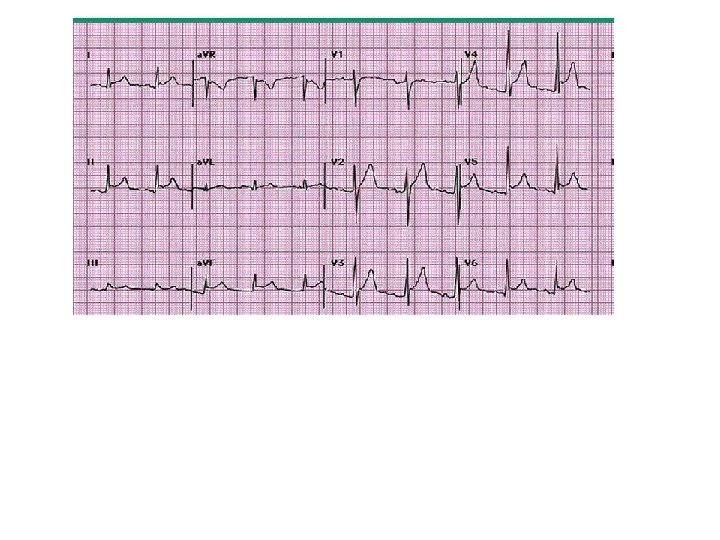
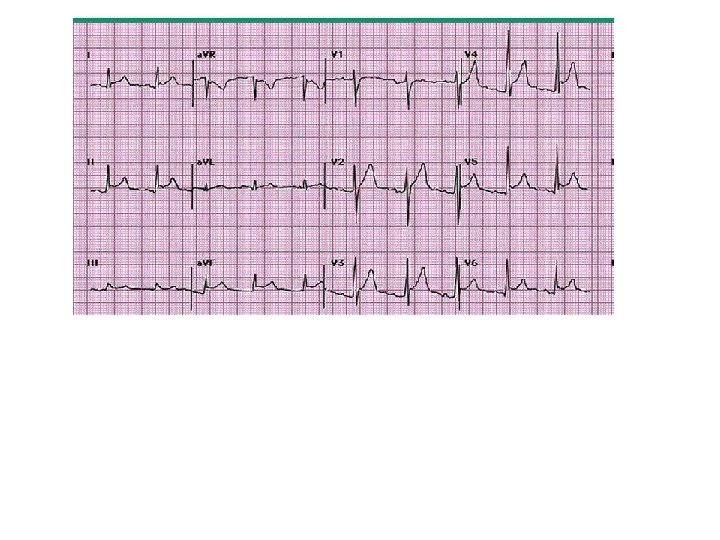
Diagnosis 1. Can be diagnosed clinically 2. ECG: Stage 1 (1 st hrs-dys) : characterized by diffuse ST elevation (typically concave up). Stage 2(1 st wk): characterized by normalization of the ST & PR segments. Stage 3: diffuse T wave inversions. Stage 4 : normalization of the ECG or indefinite persistence of T wave inversions.
3. others • Echocardiogram — Echocardiography is often normal unless there is a pericardial effusion. • Chest x-ray — typically normal • Cardiac biomarkers — may be a/w increases in biomarkers of myocardial injury such as cardiac T I or T. • Signs of inflammation — elevations in the WBC , ESR , and serum CRP concentration. • An elevated troponin level is not associated with a worse prognosis, and troponin levels usually return to normal within 1 to 2 weeks.
Management The pain usually responds to aspirin but a more potent anti-inflammatory agent, such as indometacin may be required. Colchicine or glucocorticoids can also suppress symptoms but there is no evidence that they accelerate cure.
European Society of Cardiology guidelines — The 2004 European Society of Cardiology (ESC) guidelines recommended that systemic steroid therapy be restricted to patients with the following conditions : • Patients with symptoms refractory to standard therapy • Acute pericarditis due to connective tissue disease • Autoreactive (immune-mediated) pericarditis • Uremic pericarditis
In viral pericarditis, recovery usually occurs within a few days or weeks but there may be recurrences (chronic relapsing pericarditis). Purulent pericarditis requires treatment with antimicrobial therapy, pericardiocentesis and, if necessary, surgical drainage.
![DETERMINATION OF RISK AND NEED FOR HOSPITALIZATION Fever 38ºC 100 4ºF and leukocytosis DETERMINATION OF RISK AND NEED FOR HOSPITALIZATION • Fever (>38ºC [100. 4ºF]) and leukocytosis](https://slidetodoc.com/presentation_image_h/11d67373c6cf6f452cc4af0304512f21/image-17.jpg)
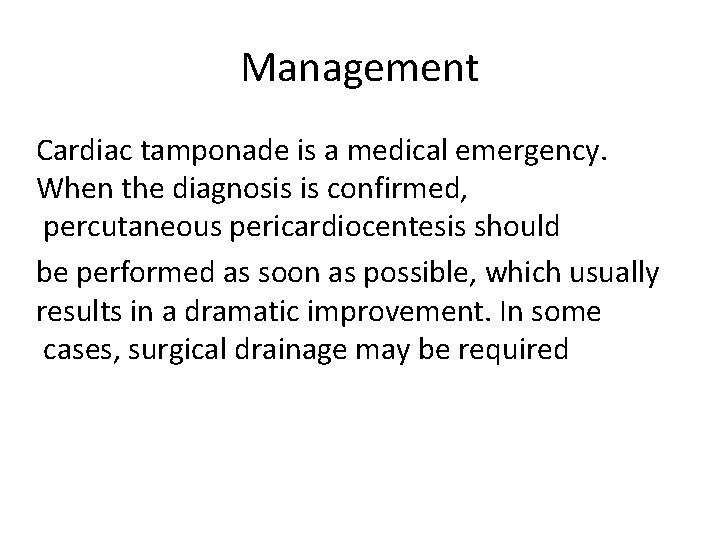
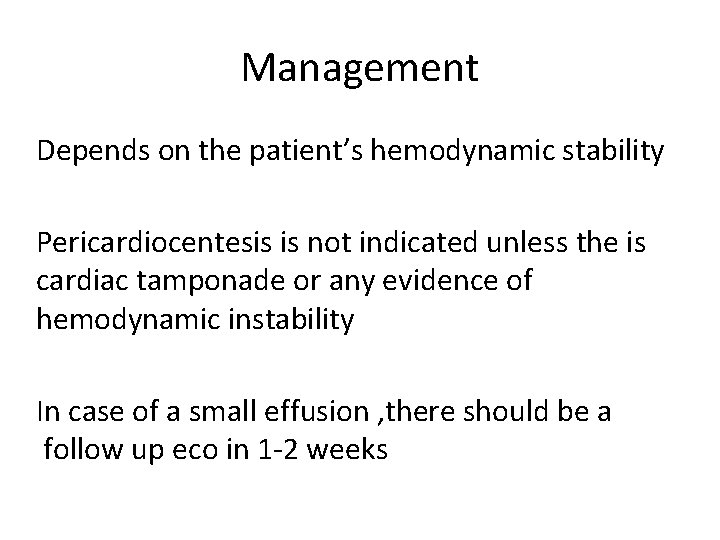
DETERMINATION OF RISK AND NEED FOR HOSPITALIZATION • Fever (>38ºC [100. 4ºF]) and leukocytosis • Evidence suggesting cardiac tamponade • A large pericardial effusion (ie, an echo-free space of more than 20 mm) • Immunosuppressed state • A history of oral anticoagulant therapy • Acute trauma • Failure to respond within seven days to NSAID therapy • Elevated cardiac troponin, which suggests myopericarditis
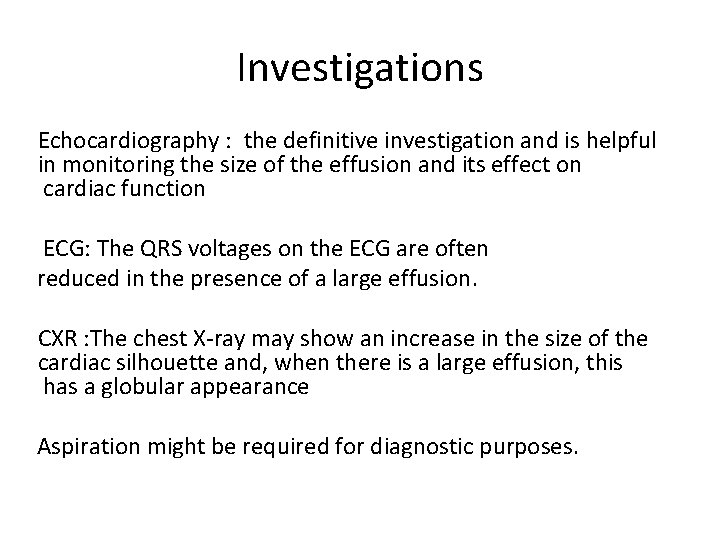
Pericardial effusion Muffeled heart sounds Raised jvp Hypotension Pulsus paradoxis Oligourea Dulness at left lung base Soft pmi
Friction rub may be present or absent Large effusion might be accompanied by a feeling of retrosternal oppresion If large enough or rapidly developing it might progress to cardiac tamponade
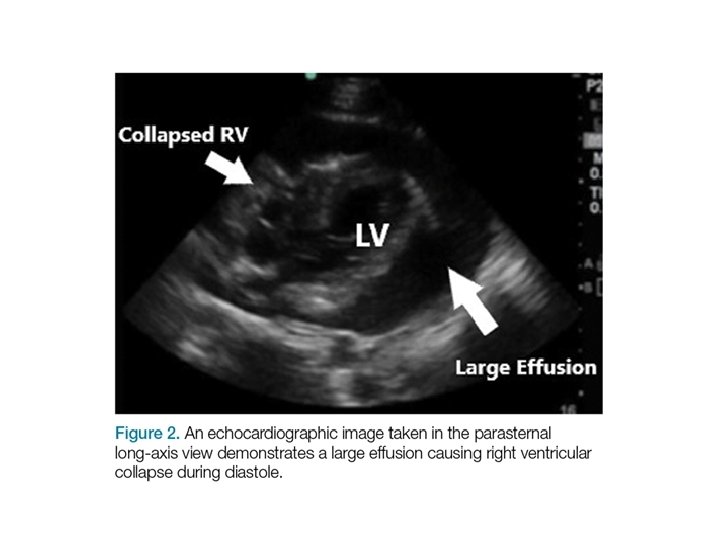
Investigations Echocardiography : the definitive investigation and is helpful in monitoring the size of the effusion and its effect on cardiac function ECG: The QRS voltages on the ECG are often reduced in the presence of a large effusion. CXR : The chest X-ray may show an increase in the size of the cardiac silhouette and, when there is a large effusion, this has a globular appearance Aspiration might be required for diagnostic purposes.
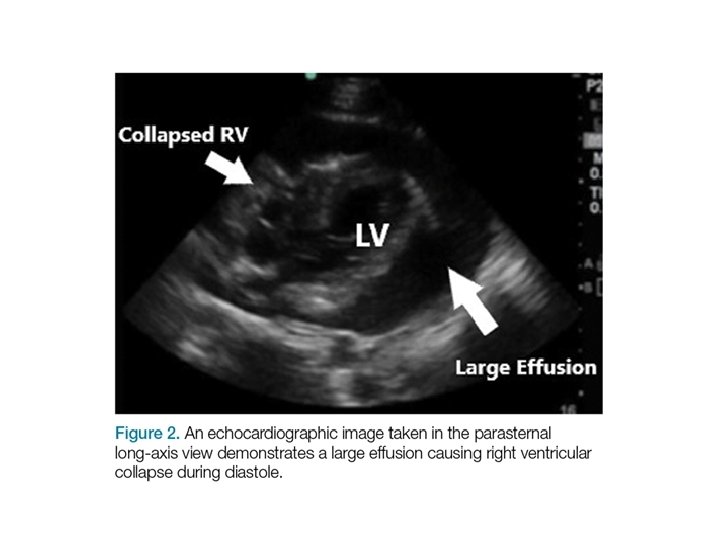
Management Depends on the patient’s hemodynamic stability Pericardiocentesis is not indicated unless the is cardiac tamponade or any evidence of hemodynamic instability In case of a small effusion , there should be a follow up eco in 1 -2 weeks
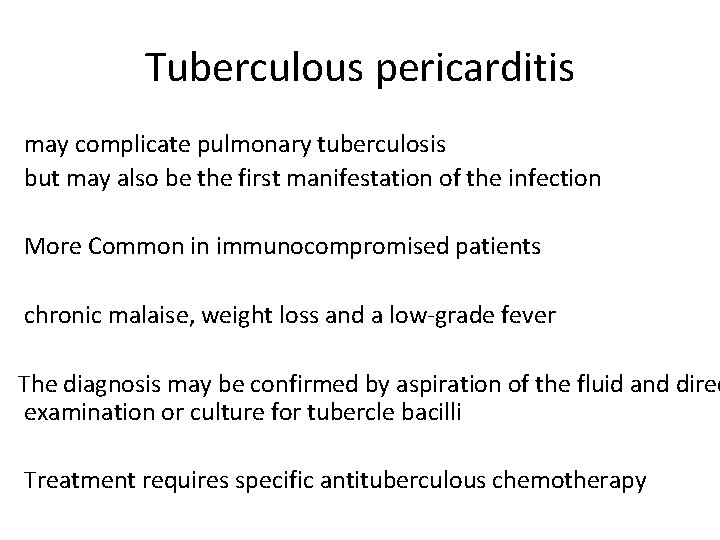
Tuberculous pericarditis may complicate pulmonary tuberculosis but may also be the first manifestation of the infection More Common in immunocompromised patients chronic malaise, weight loss and a low-grade fever The diagnosis may be confirmed by aspiration of the fluid and direc examination or culture for tubercle bacilli Treatment requires specific antituberculous chemotherapy
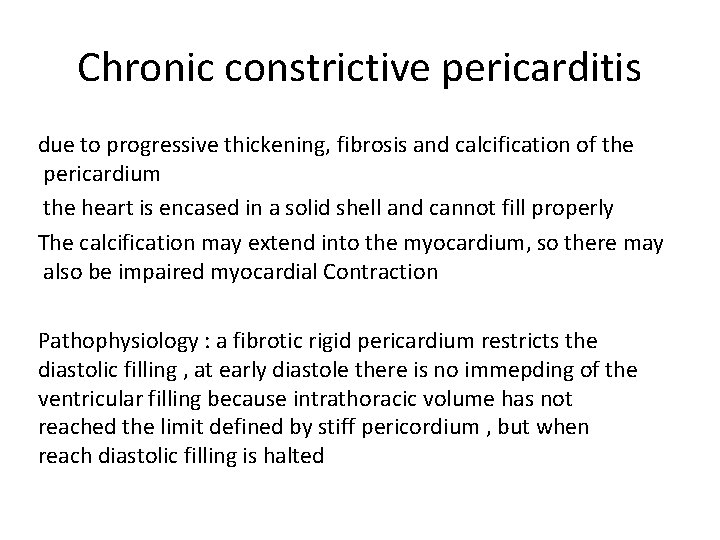
Chronic constrictive pericarditis due to progressive thickening, fibrosis and calcification of the pericardium the heart is encased in a solid shell and cannot fill properly The calcification may extend into the myocardium, so there may also be impaired myocardial Contraction Pathophysiology : a fibrotic rigid pericardium restricts the diastolic filling , at early diastole there is no immepding of the ventricular filling because intrathoracic volume has not reached the limit defined by stiff pericordium , but when reach diastolic filling is halted
Signs and symptoms Patient either presents with symptoms charesteristics of fluid overload such as edema , ascites , plural effusion or he might presents with symptoms related to deminished caridac output such as dyspnea , fatigue. . etc or both. Jvd is the most prominent finding
Clinical features of constrictive pericarditis • Fatigue • Rapid, low-volume pulse • Elevated JVP with a rapid y descent • Loud early third heart sound or ‘pericardial knock’ • Kussmaul’s sign • Hepatomegaly • Ascites • Peripheral oedema • Pulsus paradoxus
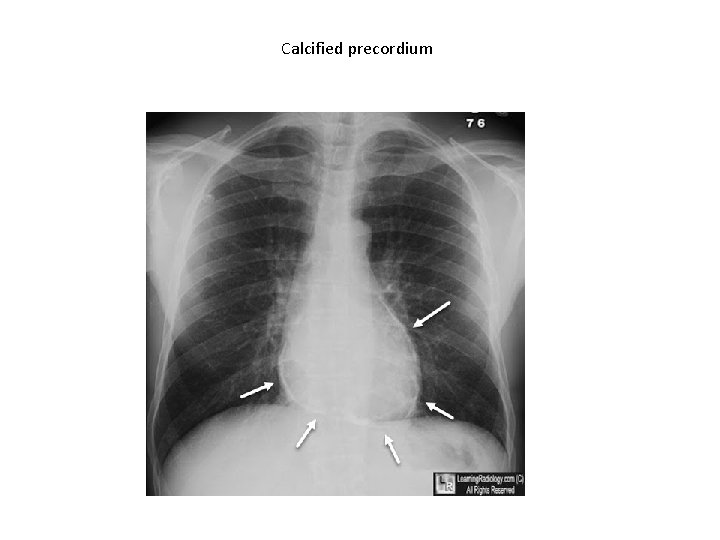
investigations CXR and ct : help to see pericardial calcification Echocardiogram Ecg : afib is more often seen in advanced disease echo–Doppler studies and cardiac catheterisation : might help in destinguishing restrective cardiomyopathy
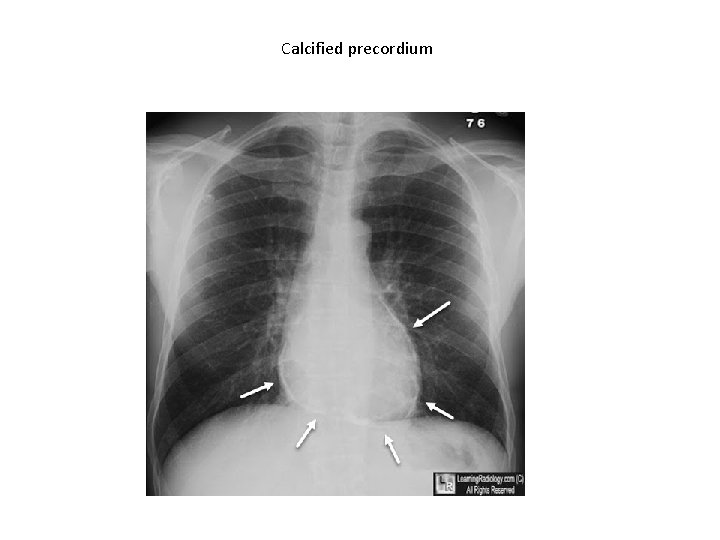
Calcified precordium
Management We should treat the underlying condition The resulting diastolic heart failure is treated using loop diuretics and aldosterone antagonists, such as spironolactone. Surgical resection of the diseased pericardium can lead to a dramatic improvement but carries a high morbidity, with disappointingresults in up to 50% of patients
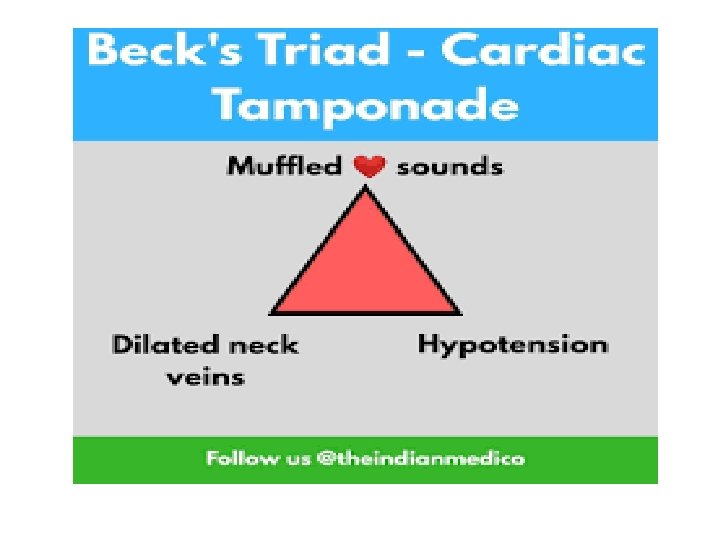
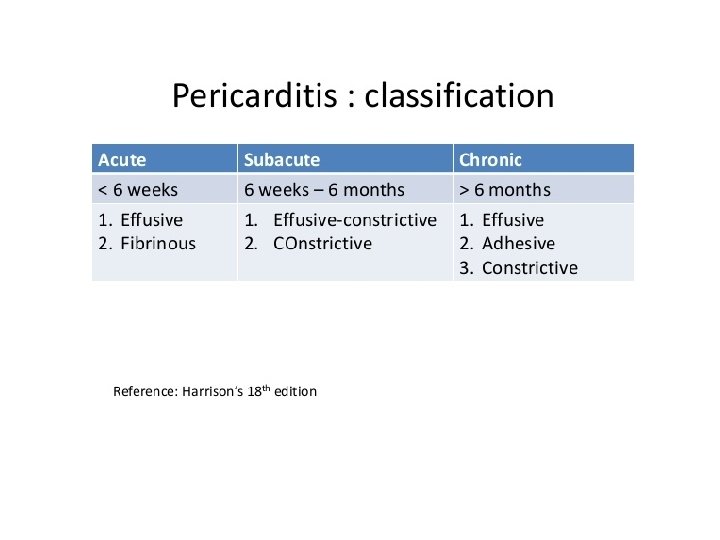
Cardiac tamponade This term is used to describe acute heart failure due to compression of the heart as the result of a large pericardial effusion. Tamponade may complicate any form of pericarditis but can be caused by malignant disease, by blood in the pericardial space following trauma, or by rupture of the free wall of the myocardium following MI Accumulation of pericardial fluid , it is the rate of accumulation that matters not the amount because when the amount accumulates slowly the pericardium adapts and stretches.
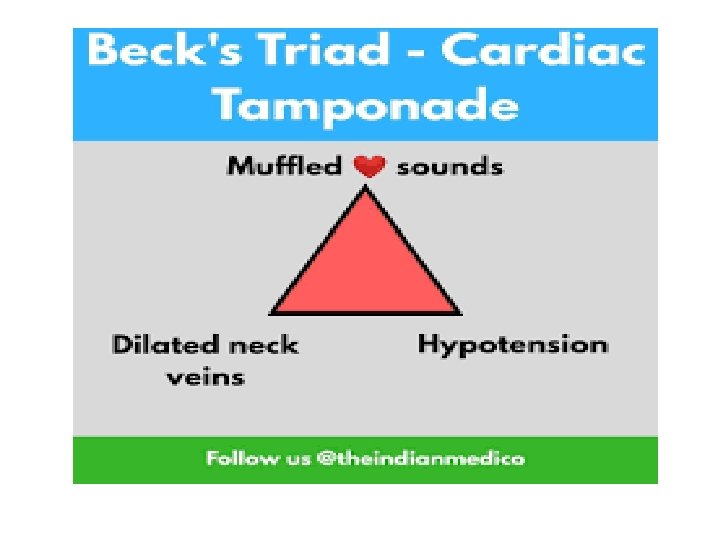
Other signs and symptoms Hemodynamic instability (cardiogenic shock : tachypnea , tachycarida etc) Pulsus paradoxus Elevated jvp is the most common finding
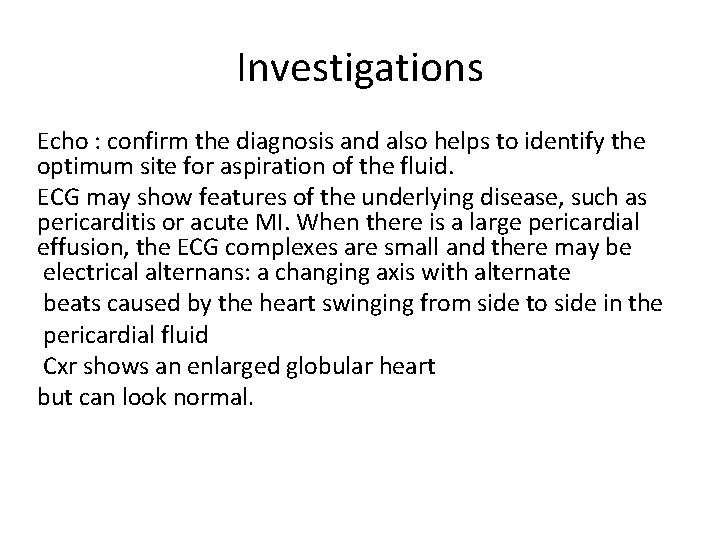
Investigations Echo : confirm the diagnosis and also helps to identify the optimum site for aspiration of the fluid. ECG may show features of the underlying disease, such as pericarditis or acute MI. When there is a large pericardial effusion, the ECG complexes are small and there may be electrical alternans: a changing axis with alternate beats caused by the heart swinging from side to side in the pericardial fluid Cxr shows an enlarged globular heart but can look normal.
Management Cardiac tamponade is a medical emergency. When the diagnosis is confirmed, percutaneous pericardiocentesis should be performed as soon as possible, which usually results in a dramatic improvement. In some cases, surgical drainage may be required