Continuing Care for Mothers Children and Families Following






- Slides: 92

Continuing Care for Mothers, Children, and Families Following Prevention of Mother-to-Child Transmission of HIV (PMTCT) Programmes 1
Objectives for this Module § Describe comprehensive HIV care for women, children, and their families. § Understand the basic principles and purpose of family-centred care. § Identify and strategically address gaps in the provision of comprehensive HIV care for women, children, and their families. 2
Objectives for this Module § Recognize common signs and symptoms of HIV in infants and young children. § Understand the importance of male involvement in PMTCT and HIV programmes and be able to suggest creative strategies to encourage their participation. § Describe the difference between linkages and referrals. 3

Objectives for this Module § Improve referral practices between PMTCT and HIV care and treatment programmes. § Discuss retention strategies for keeping women and their families in care. § practise problem-solving skills to address social issues affecting a client’s capacity to follow-up with care and treatment. 4
Session 1 Introduction to Comprehensive Care for Mothers, Children, and Families 5
Objectives of Session 1 § Describe comprehensive HIV care for women, children, and their families. § Understand the basic principles and purpose of family-centred care. § Identify and strategically address gaps in the provision of comprehensive HIV care for women, children, and their families. 6
Objectives of Session 1 § Recognize common signs and symptoms of HIV in infants and young children. § Understand the importance of male involvement in PMTCT and HIV programmes and be able to suggest creative strategies to encourage their participation. 7
Introductory Presentation PMTCT and HIV Care and Treatment Programmes 8
Large Group Discussion § Barriers to accessing HIV-related treatment, care, and support § Role of a PMTCT healthcare worker in comprehensive care 9
Role of PMTCT Healthcare Workers in HIV Care & Treatment § § Assess client needs Recognize clinical symptoms Understand when to refer Establish and maintain referral and linkage systems § Participate in client case management § Advocate for comprehensive care needs 10
Comprehensive Management of a Person with HIV § Shared responsibility for client: § Multi-disciplinary team § Community § Family § Client themselves 11

Components of comprehensive treatment, care, and support § For mother and partner § For child § For family 12
Comprehensive Care for Mother and Partner § HIV testing for partner § ARV therapy assessment and referral § Screening, prevention, and treatment of HIV-related conditions § Counselling and support on adherence and nutrition § Psychosocial and spiritual support 13
Comprehensive Care for Mother and Partner § Information, counselling, and support on infant feeding § Safer sex and family planning § Referral to community organizations § Disclosure counselling and support § Palliative care, when indicated § Drug and alcohol counselling and treatment 14
Comprehensive Care for Child § ARV therapy assessment and referral § Screening, prevention, and treatment of HIV-related infections § Growth and development monitoring § Immunizations § HIV diagnosis by laboratory test or presumptive diagnosis 15
Comprehensive Care for Child § HIV education (as appropriate) § Psychosocial support § Disclosure counselling (as appropriate) § Links and relationships with community service organizations and agencies to promote continuity of care 16
Comprehensive Care for Family § HIV testing for older children § Adherence counselling § Links and relationships with community service organizations and agencies to promote continuity of care § HIV education § Psychosocial and spiritual support 17
Comprehensive Care for Family § Referrals and links to domestic violence organizations § Bereavement counselling § Social support services § Legal advice and services § Employment, income-generation activities 18

Family-centred Care Family-centred care recognizes all persons who function as family members, as identified by the person living with HIV infection. 19
Goals of Family-based Care § Decrease morbidity and mortality § Improve the quality-of-life for HIV-infected women, children, and their families § Reduce transmission of HIV through secondary prevention counselling and education 20
Opportunities to Reach Families within PMTCT Programmes § HIV counselling and testing for all sexual partners § Family-focused adherence and disclosure counselling § Mechanisms to reach family members during appointments § Postpartum § MCH § Paediatric 21
Discussion Question § How has the role of PMTCT healthcare workers expanded? § Discuss how healthcare workers feel about this expanded role. 22
Postpartum Care for HIV-infected Mothers § Best practices in postpartum care include: § Mechanism to communicate mother’s ANC and L&D history to postpartum nursing staff § Mechanisms to target mothers who miss ANC appointments § Community resources to locate and link mothers to care Review Appendix A – “Checklist for Postpartum Visit for HIV-infected Women and HIV-exposed Newborns” 23
Exercise 1 Facilitating Referrals between PMTCT and HIV Care and Treatment large group discussion 24
Follow-up Care of the HIV-exposed Infant § Follows best practices applied to all infants and children § Assessment of growth, nutrition, and development § Vaccines § Full physical exam focusing on identification of HIVrelated infections § Cotrimoxazole prophylaxis at 4 -6 weeks of age Review Appendices B and C “Infant/Young Child Follow-up Visits” “Monitoring Growth, Nutrition, and Development of HIVexposed Infants and Children” 25
Diagnosis of HIV Infection in Infants § Immune system of HIV-infected children immature § Close follow-up and diagnosis critical to saving children’s lives § 1/3 rd die by 1 year old § ½ die by 2 years of age § Diagnosis using clinical symptoms or HIV testing 26
Diagnostic Testing of HIVexposed Infants and Young Children § Caribbean guidelines recommend HIV DNA PCR viral testing be performed for HIV-exposed infants starting at 6 -8 weeks of age. § HIV antibody tests may be difficult to interpret in children less than 18 months of age due to the presence of maternal antibodies to HIV. § HIV antibody tests can be used to diagnose HIV infection in children 18 months of age and older. Always refer to national guidelines and algorithms 27
Recognizing HIV Infection in Children § All healthcare workers working with infants and children: § Identify the signs and symptoms of HIV-infection § Provide or refer for HIV diagnostic testing and HIV care and treatment 28
Suspecting HIV Infection in a Child § All infants/children born to mothers with unknown HIV status should be considered at risk § Encourage and support testing for all mothers § Refer to healthcare team specializing in HIV care if HIV infection is suspected 29
Risk factors for HIV if Mother’s HIV Status is Unknown § Mother has symptoms of HIV or another STI If mother is diagnosed with HIV, all of her children need to be tested 30
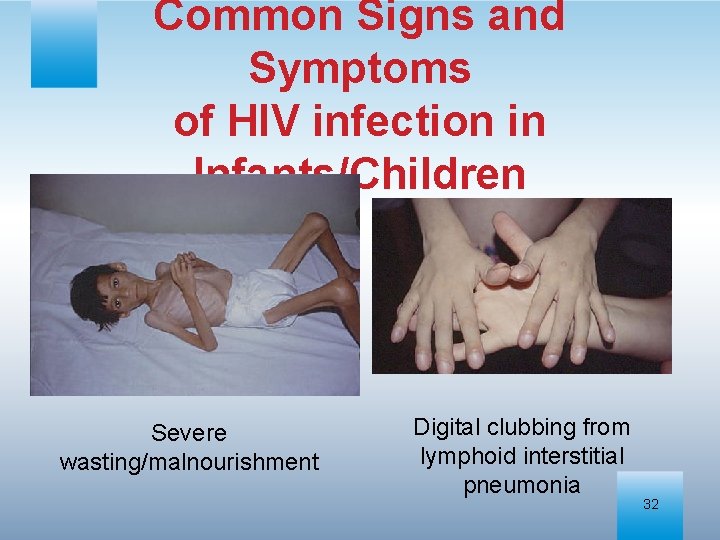
Common Signs and Symptoms of HIV infection in Infants/Children § Low weight and/or growth failure § § Lymphoid interstitial pneumonia (LIP) Hepatosplenomegaly Pneumonias, including PCP Oral candidiasis (thrush) 31
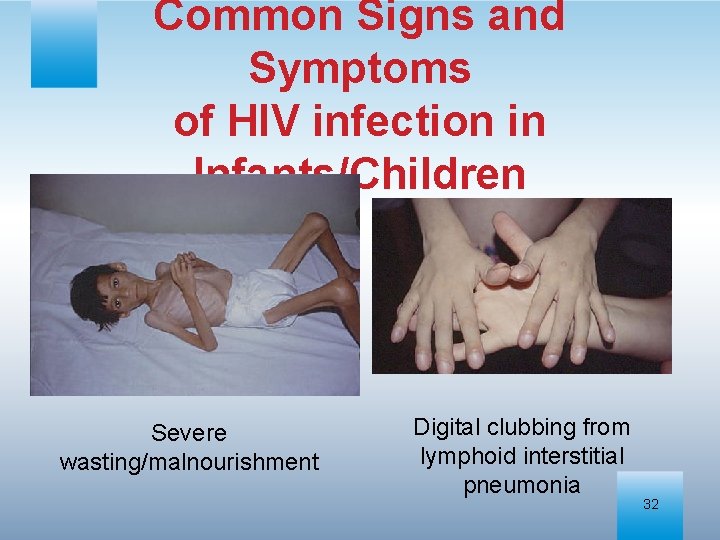
Common Signs and Symptoms of HIV infection in Infants/Children Severe wasting/malnourishment Digital clubbing from lymphoid interstitial pneumonia 32
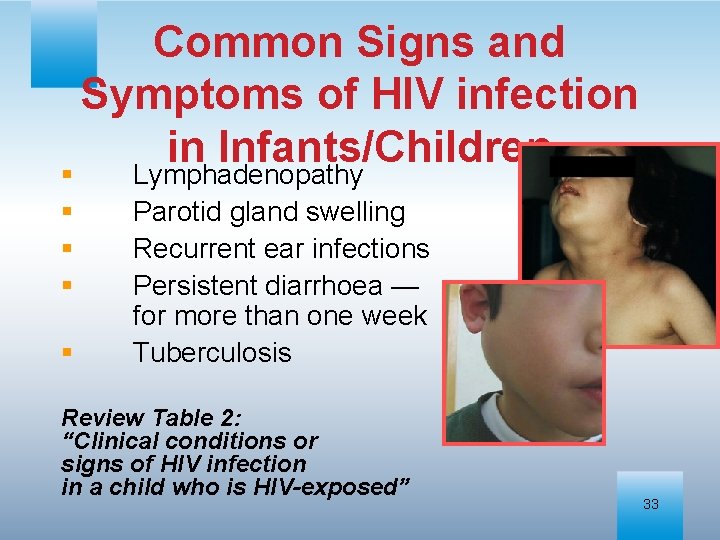
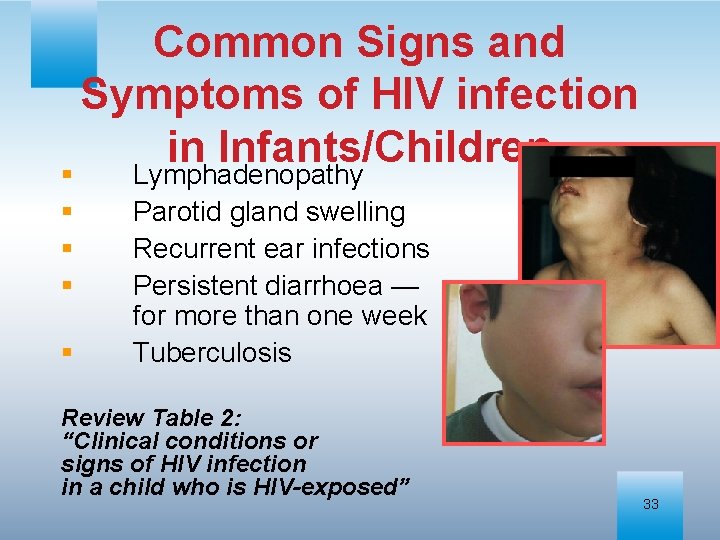
Common Signs and Symptoms of HIV infection in Infants/Children § Lymphadenopathy § § Parotid gland swelling Recurrent ear infections Persistent diarrhoea — for more than one week Tuberculosis Review Table 2: “Clinical conditions or signs of HIV infection in a child who is HIV-exposed” 33
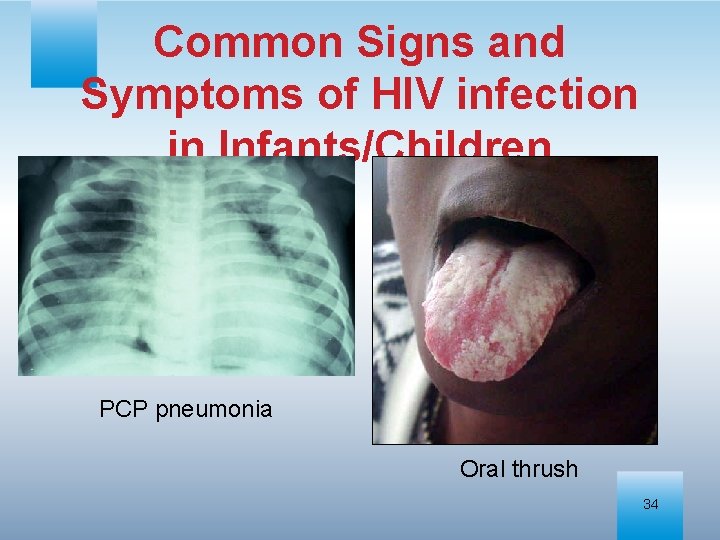
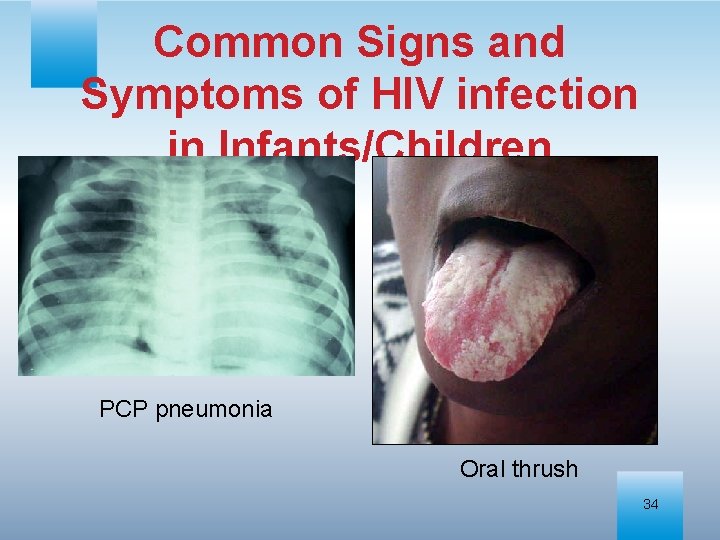
Common Signs and Symptoms of HIV infection in Infants/Children PCP pneumonia Oral thrush 34
Growth and HIV Infection § Growth failure reported in as many of 50% of HIV-infected children § Growth failure defined as the persistent and unexplained decline or levelling-off in weight and the speed of growth despite adequate nutrition. 35
Growth and HIV Infection § Growth monitoring and nutritional assessment performed for all for HIV-exposed and infected children. § Poor growth may be one of the first indicators of HIV infection in children. See Appendix C – Monitoring Growth, Nutrition, and Development of HIVexposed Infants and Children 36
Exercise 2 Clinical Presentation of HIV in Infants and Children large group discussion & case studies 37
Male Partners and HIV Prevention, Care, Treatment, and Support § Men have the power to alter the HIV epidemic in Caribbean § Can prevent HIV transmission to their partners § Can seek/support HIV care and treatment for self and families 38
Men and HIV Risk § Culturally acceptable to father multiple children with different partners § Multiple sex partners § Work migration § Expectations of “manhood” § Risky behaviors § Drug use § Paying for sex § Men expected to determine when, where, and how couples have sex 39
Barriers to Safe Sex for Couples § Misinformation about condoms § Clumsy § Reduction of sexual pleasure § Belief that contraception is a woman’s responsibility § Marriage not necessarily equated with mutual faithfulness 40

Barriers to Safe Sex for Couples § For women: § Difficulty of negotiating for safer sex § Fear of reprisal if condoms requested § Stigma against homosexuality § High risk sex may not be disclosed to female partners 41
Discussion Questions § How can we encourage men to be more involved in the health of their families? § As healthcare workers what can we do to encourage the involvement of men? 42
The Evolving Role of Men § Male involvement in ANC increases rates of PMTCT uptake. § Involving men in the health of the family involves challenging beliefs about traditional roles. 43
Strategies to Include Men in HIV Prevention, Care, & Treatment § Offer HIV counselling and testing at flexible times § Promote HIV counselling and testing where men gather § Sporting events § Workplace 44
Strategies to Include Men in HIV Prevention, Care, & Treatment § Involve male role models § Support for HIV prevention efforts that target norms of masculinity § Adopt policies at health facilities that normalize male attendance § Provide family planning counselling to couples See Appendix F – “Family Planning in the Context of HIV Infection” 45
Session 2 Linkages, Referrals, and Retention Strategies 46
Objectives of Session 2 § Describe the difference between linkages and referrals. § Discuss retention strategies for keeping women and their families in care. § Improve referral practices between PMTCT and HIV care and treatment programmes. § Practise problem-solving skills to address social issues affecting a client’s capacity to follow-up with care and treatment. 47
Introduction to Linkages and Referrals § Both HIV-infected and uninfected women benefit from referrals to services outside of PMTCT programmes. § Linkages provide a “seamless” continuum of care as if there were a single entity delivering a range of services. 48
Linkages § Formal networks between organizations or agencies § Facilitate the referral of the client and her family for services § Foster a sense of joint purpose and joint achievement for healthcare workers 49
PMTCT Linkages PMTCT programmes should be linked to: § Tertiary referral hospitals, district hospitals, and peripheral health facilities § Other government organizations e. g. , schools, social welfare agencies, and local government § Communities they serve § Non-governmental and faith-based community organizations § Private doctors and healthcare providers 50
Advantages of Linkages promote: § Access of PLHIV to HIV care and treatment services § Better understanding of how to manage more complex ARV prophylaxis or treatment regimens § PMTCT activities and PMTCT messages amongst all healthcare workers 51
Advantages of Linkages can: § Reduce HIV-related stigma and discrimination § Improve coverage for underserved populations § Improve quality of care § Enhance programme effectiveness and efficiency 52
Discussion Questions § What community services do you refer patients to? § What services have you learned about from your clients (e. g. church groups, support groups)? 53
Community Linkages § Community-based HIV services include: § Support groups for PLHIV § Social activities § Income-generating or volunteer work § Advantages include: § Helping families cope with stigma and isolation § Assisting national programmes with meeting needs of PLHIV 54
Other Community Linkages Examples of other community services: § Faith-based programmes offering supportive counselling to families affected by HIV § Local and/or private businesses providing HIV education 55
Suggested Linkages and Referrals for HIV-negative Women § Counselling and testing (partner and family testing) § Routine well baby or well child care, including immunizations § Family planning and safer sex counselling 56
Suggested Linkages and Referrals for HIV-negative Women § Nutritional education and support for new mothers and infants § Treatment and support for drug and/or alcohol abuse § Mental health services § Domestic violence services 57
Suggested Linkages and Referrals for HIV-infected Women and Families § Counselling and testing § TB and STI (partner and family testing) programmes § HIV treatment, care, § Laboratory and support, including services ARV therapy § Support groups § Routine well baby or and positive well child care mothers’ clubs § Healthcare providers in § Community-based private specialized HIV groups practice 58
Suggested Linkages and Referrals for HIV-infected Women and Families § Family planning and safer sex counselling § Nutritional education and support § Safer infant feeding counselling and support § Community/homebased care services § Faith-based and community organizations § Treatment and support for drug and/or alcohol abuse § Mental health services § Domestic violence services 59
Linkage Enablers Strong linkages formed and maintained by: § Informal personal relationships e. g. , having studied together in nursing or medical school § Good communication systems from phones and E-mail § Comprehensive and standardized referral forms § Transport systems, good roads, and public transportation 60
Linkage Enablers Strong linkages formed and maintained by: § Shared continuing education or training courses § Integration of management and support functions such as planning, education and training, supplies and maintenance including ordering ARV drugs 61
Consequences of Poor Linkages § Gaps in services for clients § HIV-exposed children are not diagnosed and do not receive ARV therapy § Potentially infected siblings and male partners not tested for HIV § Women present back to PMTCT programmes only during another pregnancy § Service duplication § Higher expense 62
Discussion Question § Describe a situation where you referred a client for a service but the client did not attend. Why did they not attend? How did you handle the situation? § What mechanisms have been successful in your own communities and facilities to develop formal referral networks? 63
Referrals § Referrals are the guided or orchestrated movement of clients to obtain services based on the specific needs of the client. 64
Steps in the Referral Process 1. Assessment of client need 2. Outline available services 3. Assess and address potential barriers to attending referral § § § Transportation Lack of funds Fear of stigma 65
Steps in the Referral Process 4. Ensure client understands purpose of referral 5. Document referral accurately 6. Discuss confidentiality 7. Provide correct documentation for referral including § Time, location, and contact person 66
Steps in the Referral Process 8. Ask client for feedback on referral 9. Document and evaluate referral 10. Establish a mechanism with referral agencies to facilitate feedback 11. Reassess barriers 67
Monitoring Referrals § Feedback from referrals is necessary to ensure quality of services. § Referring facilities are responsible for the success and appropriateness of their referrals. The organization receiving the referred client may need to provide additional technical support to a healthcare worker (in the referring agency) e. g. , reviewing medical criteria for referral to TB programme. 68
Developing a Referral Network Referral networks § Take time and commitment to create and maintain § Are constantly changing § Require healthcare workers to be familiar with all available services 69
Referral Networks A referral network can include: § A lead organization to coordinate. § Regular meetings of healthcare workers. § Newsletters or method of communication. 70
Referral Networks A referral network can include: § Designated contact referral person at each agency. § Standardized referral forms. § A system that tracks referrals and lets network members know when a referral has been successfully completed. 71
Exercise 3 Community Resources small group discussion 72
Barriers to Comprehensive HIV Care § The circumstances of client’s lives can affect their ability to receive truly comprehensive care for themselves and their family. § Healthcare workers must continuously address barriers to HIV care. 73
Barriers to Comprehensive HIV Care Stigma § Fear of status being revealed § This can occur when HIV care and treatment are not integrated into mainstream care (e. g. , separate HIV clinic) 74

Barriers to Comprehensive HIV Care Financial § Hidden cost of “free” services § childcare § transportation § Cost of specialized services § e. g. , referral to doctor in private practice 75
Barriers to Comprehensive HIV Care Time commitment § Multiple referrals necessary for comprehensive care § Different sites § Different times § Different purposes 76
Barriers to Comprehensive HIV Care Healthcare workers, lack of knowledge and time § Lack of knowledge about available services § Lack of time to properly make and monitor referral 77
Strategies to Overcome Barriers § Strategies should be individually tailored § Implemented by multi-disciplinary team § Social workers § Physicians § Counsellors 78
Strategies to Overcome Barriers Disclosure counselling § Disclosure is first step in receiving care, treatment, and support for self, partner(s), and children § Disclosure is ongoing process that starts in pre-test counselling See Appendix I – Sample Disclosure Counselling Script 79
Strategies to Overcome Barriers Incentives § Letter to the client’s employer requesting time to attend appointments § Assistance with childcare § Transportation § Food, clothing, or prizes § Accompanying patient to appointments § Assistance with obtaining social welfare benefits 80
Strategies to Overcome Barriers A warm, welcoming non-stigmatizing clinic environment where clients are not singled out as HIV-infected will promote client retention. 81
Exercise 4 Retention Strategies role play 82
Discussion Questions § Think of a successful healthcare program, why was it successful and how did it become successful? § How could these strategies be applied to other clinics and programmes? § What resources would be needed to accomplish the goal? 83
Best Practices in Comprehensive Care § The Paediatric Case Management Meeting § PLHIV Trained as Adherence Counsellors 84
Module Key Points There are seven key points: 85
Module Key Points 1. PMTCT healthcare workers play a vital role in ensuring that their clients with HIV receive the care, treatment, and support they need. When possible, care of an HIV-infected client should extend to all family members. 86
Module Key Points 2. Healthcare workers should ensure that mothers who are HIV-infected return for all postpartum appointments or are visited at home. 87
Module Key Points 3. It is important that healthcare workers recognize the signs and symptoms of HIV-related infections in infants and children so that they can make timely referrals for care and treatment. 88
Module Key Points 4. When male partners are involved in the care of their families, women are more likely to agree to PMTCT interventions. Partner support is also likely to be important in helping women adhere to ARV medications and attend follow-up care. Involving men in the care of their families involves challenging beliefs about traditional roles. 89
Module Key Points 5. Linkages are formal networks between organizations or an agency and the community, facilitating the referral of the client and her family for services. 90
Module Key Points 6. Referrals are the guided movement of clients to obtain services based on the specific identified needs for continuity of care. The referral process involves the ongoing assessment of a client’s needs, coupled with coordinated service delivery by a group of linked organizations. 91
Module Key Points 7. Referral networks take time and commitment to create and maintain. The first step in creating a network is to map all possible referral resources. 92
 Little families
Little families Effective support for children and families in essex
Effective support for children and families in essex Georgia department of children and families
Georgia department of children and families Assertive continuing care
Assertive continuing care Primary secondary tertiary health care definition
Primary secondary tertiary health care definition Two mothers one on one
Two mothers one on one Care and protection of children act
Care and protection of children act My mother's perfume poem
My mother's perfume poem Thank you god for mothers
Thank you god for mothers Proverbs 31
Proverbs 31 Mothers day finland
Mothers day finland Mothers day turkey
Mothers day turkey Happy mother's day in chinese
Happy mother's day in chinese God's plan for mothers
God's plan for mothers Romeo and juliet board game
Romeo and juliet board game Happy sad poems
Happy sad poems Tracing family descent through mothers rather than fathers
Tracing family descent through mothers rather than fathers 5-1 changing households
5-1 changing households Prayer points for pregnant mothers
Prayer points for pregnant mothers Cooking with my mother
Cooking with my mother Safeguarding children care certificate
Safeguarding children care certificate Nj children's system of care
Nj children's system of care Adult and continuing education
Adult and continuing education Continuous analysis and surveillance system
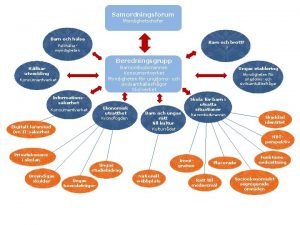
Continuous analysis and surveillance system Kontinuitetshantering i praktiken
Kontinuitetshantering i praktiken Typiska drag för en novell
Typiska drag för en novell Nationell inriktning för artificiell intelligens
Nationell inriktning för artificiell intelligens Ekologiskt fotavtryck
Ekologiskt fotavtryck Shingelfrisyren
Shingelfrisyren En lathund för arbete med kontinuitetshantering
En lathund för arbete med kontinuitetshantering Adressändring ideell förening
Adressändring ideell förening Tidbok för yrkesförare
Tidbok för yrkesförare A gastrica
A gastrica Förklara densitet för barn
Förklara densitet för barn Datorkunskap för nybörjare
Datorkunskap för nybörjare Boverket ka
Boverket ka Att skriva debattartikel
Att skriva debattartikel Autokratiskt ledarskap
Autokratiskt ledarskap Nyckelkompetenser för livslångt lärande
Nyckelkompetenser för livslångt lärande Påbyggnader för flakfordon
Påbyggnader för flakfordon Kraft per area
Kraft per area Svenskt ramverk för digital samverkan
Svenskt ramverk för digital samverkan Kyssande vind analys
Kyssande vind analys Presentera för publik crossboss
Presentera för publik crossboss Argument för teckenspråk som minoritetsspråk
Argument för teckenspråk som minoritetsspråk Bat mitza
Bat mitza Klassificeringsstruktur för kommunala verksamheter
Klassificeringsstruktur för kommunala verksamheter Fimbrietratt
Fimbrietratt Claes martinsson
Claes martinsson Cks
Cks Verifikationsplan
Verifikationsplan Mat för unga idrottare
Mat för unga idrottare Verktyg för automatisering av utbetalningar
Verktyg för automatisering av utbetalningar Rutin för avvikelsehantering
Rutin för avvikelsehantering Smärtskolan kunskap för livet
Smärtskolan kunskap för livet Ministerstyre för och nackdelar
Ministerstyre för och nackdelar Tack för att ni har lyssnat
Tack för att ni har lyssnat Referat mall
Referat mall Redogör för vad psykologi är
Redogör för vad psykologi är Matematisk modellering eksempel
Matematisk modellering eksempel Atmosfr
Atmosfr Borra hål för knoppar
Borra hål för knoppar Orubbliga rättigheter
Orubbliga rättigheter Variansen formel
Variansen formel Tack för att ni har lyssnat
Tack för att ni har lyssnat Steg för steg rita
Steg för steg rita Ledningssystem för verksamhetsinformation
Ledningssystem för verksamhetsinformation Tobinskatten för och nackdelar
Tobinskatten för och nackdelar Blomman för dagen drog
Blomman för dagen drog Gibbs reflekterande cykel
Gibbs reflekterande cykel Egg för emanuel
Egg för emanuel Elektronik för barn
Elektronik för barn Plagg i rom
Plagg i rom Strategi för svensk viltförvaltning
Strategi för svensk viltförvaltning Kung dog 1611
Kung dog 1611 Indikation för kejsarsnitt på moderns önskan
Indikation för kejsarsnitt på moderns önskan Romarriket tidslinje
Romarriket tidslinje Tack för att ni lyssnade
Tack för att ni lyssnade Multiplikation uppställning
Multiplikation uppställning Exempel på lyrik
Exempel på lyrik Inköpsprocessen steg för steg
Inköpsprocessen steg för steg Rbk-mätning
Rbk-mätning Etik och ledarskap etisk kod för chefer
Etik och ledarskap etisk kod för chefer Kolposkopi px
Kolposkopi px Myndigheten för delaktighet
Myndigheten för delaktighet Frgar
Frgar Tillitsbaserad ledning
Tillitsbaserad ledning Läkarutlåtande för livränta
Läkarutlåtande för livränta Karttecken stig
Karttecken stig Lek med former i förskolan
Lek med former i förskolan Shivaismen
Shivaismen Vanlig celldelning
Vanlig celldelning Bris för vuxna
Bris för vuxna