4 The Tissue Level of Organization Power Point



- Slides: 77
4 The Tissue Level of Organization Power. Point® Lecture Presentations prepared by Jason La. Pres Lone Star College—North Harris © 2012 Pearson Education, Inc.
An Introduction to Tissues: Group of cells with common embryonic origin that perform specialized functions. Histology: the study of tissues Pathology: the study of tissues associated with a disease Biopsy: the study of tissue sample from a patient to make medical diagnosis Autopsy: the study of tissue sample from a dead person to discover the cause of death © 2012 Pearson Education, Inc.
Studying Human Tissue is • Fixed • Preserved • Sectioned • Sliced thin enough to transmit light or electrons • Stained • Enhances contrast • Observed • Using microscopy © 2012 Pearson Education, Inc.
4 -1 Four Types of Tissue 1. Epithelial tissue: covers the body, lines body cavities, ducts, and forms glands. 2. Connective tissue: provides protection, support, immunity, energy storage site for the body, transports materials. 3. Muscle tissue: allows for body movement, heat generation and movement of material within the body. 4. Neural tissue: detects internal and external stimuli allowing the body to respond via electrical impulses. © 2012 Pearson Education, Inc.
4 -2 Epithelial Tissue Location of Epithelial Tissue 1. Covering epithelium - covers the body surface, lines internal organs, blood vessels and ducts. 2. Glandular epithelium - forms glands. Functions of Epithelial Tissue 1. Provide Physical Protection: 2. Control Permeability 3. Provide Sensation 4. Specialized Secretions (glandular epithelium) © 2012 Pearson Education, Inc.
Characteristics of Epithelia • Continuous sheet of cells---tightly packed together via cell junctions • Avascular- receives nourishment from underlying blood vessels via diffusion • Supplied with nerves that usually end at the base of the tissue • Regeneration-high rate of cell division • Polarity • Attachment to basement membrane • Functions include- protection, secretion, filtration, absorptions, excretions © 2012 Pearson Education, Inc.
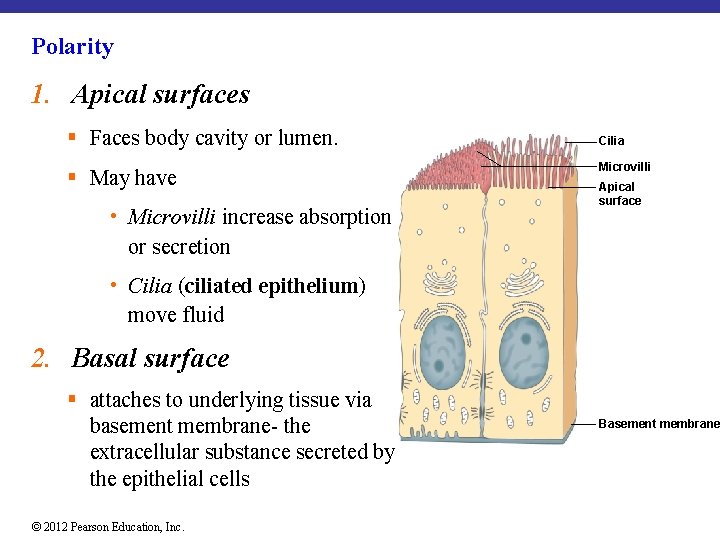
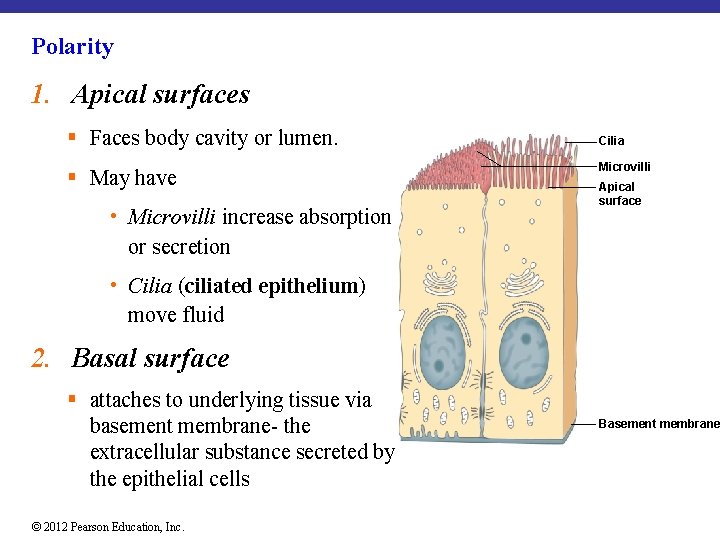
Polarity 1. Apical surfaces § Faces body cavity or lumen. § May have • Microvilli increase absorption or secretion Cilia Microvilli Apical surface • Cilia (ciliated epithelium) move fluid 2. Basal surface § attaches to underlying tissue via basement membrane- the extracellular substance secreted by the epithelial cells © 2012 Pearson Education, Inc. Basement membrane
Factors that help maintain the integrity of epithelia To be effective as a barrier, an epithelium must form a complete cover or lining 1. Intercellular connections 2. Attachment to the basement membrane 3. Epithelial maintenance and repair © 2012 Pearson Education, Inc.
Intercellular Connections Cell Junctions: the structures that connect and allow for the cells to work together as functional units in tissues. 1. Tight junctions 2. Gap junctions 3. Desmosomes © 2012 Pearson Education, Inc.
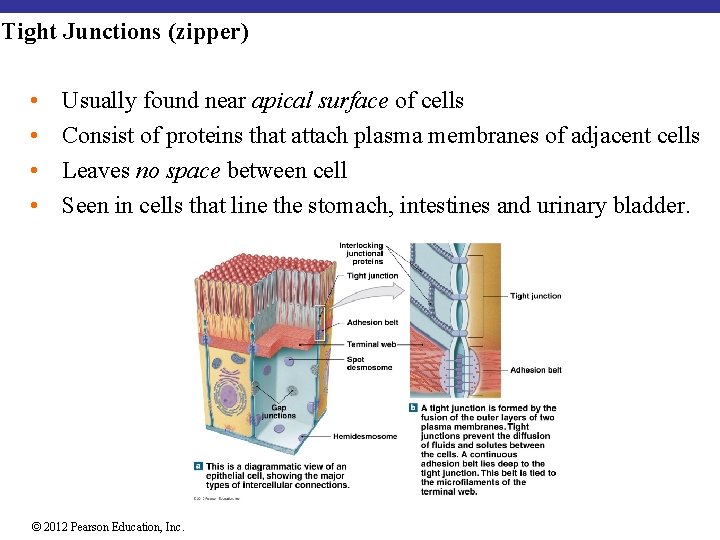
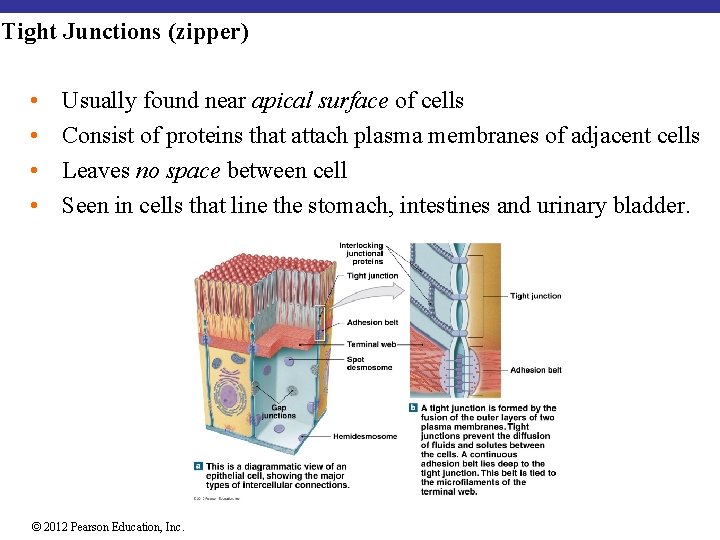
Tight Junctions (zipper) • • Usually found near apical surface of cells Consist of proteins that attach plasma membranes of adjacent cells Leaves no space between cell Seen in cells that line the stomach, intestines and urinary bladder. © 2012 Pearson Education, Inc.
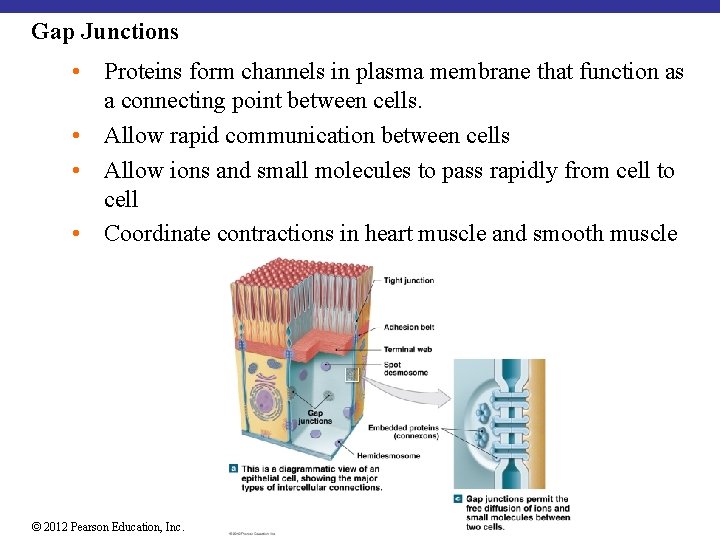
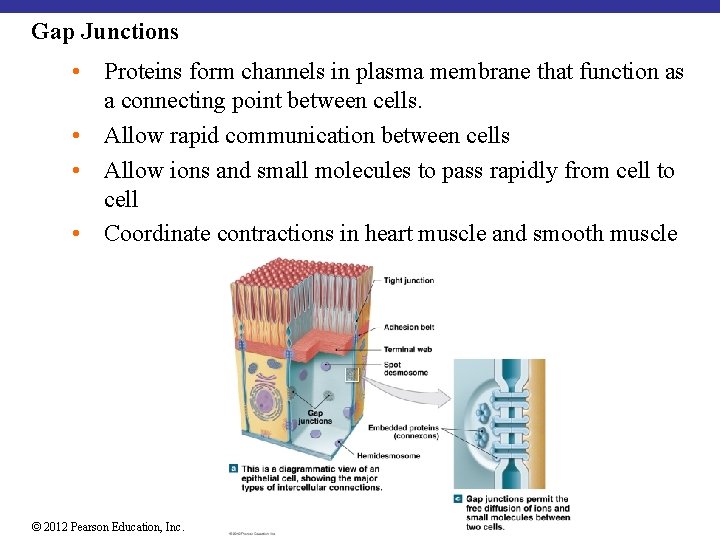
Gap Junctions • Proteins form channels in plasma membrane that function as a connecting point between cells. • Allow rapid communication between cells • Allow ions and small molecules to pass rapidly from cell to cell • Coordinate contractions in heart muscle and smooth muscle © 2012 Pearson Education, Inc.

Desmosomes (snap) • Strong, resist stretching and bending • Formed by cell adhesion molecules (CAMs) that attach to intermediate filaments of cytoskeleton • Leave a gap between cells • Seen in the epidermis and in cardiac muscle cells. © 2012 Pearson Education, Inc.
Epithelial Maintenance and Repair • Epithelial cells exposed to harsh conditions: are replaced by division of stem cells • Stem cells found near basement membrane • Epithelial tissue type has highest mitotic rate © 2012 Pearson Education, Inc.
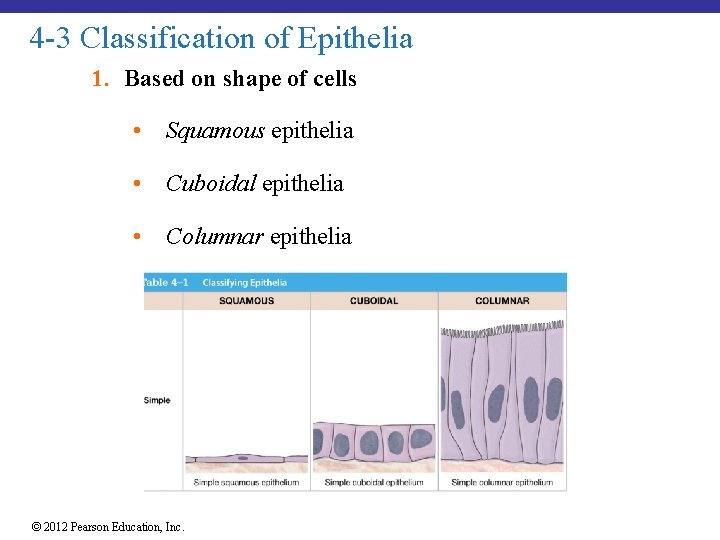
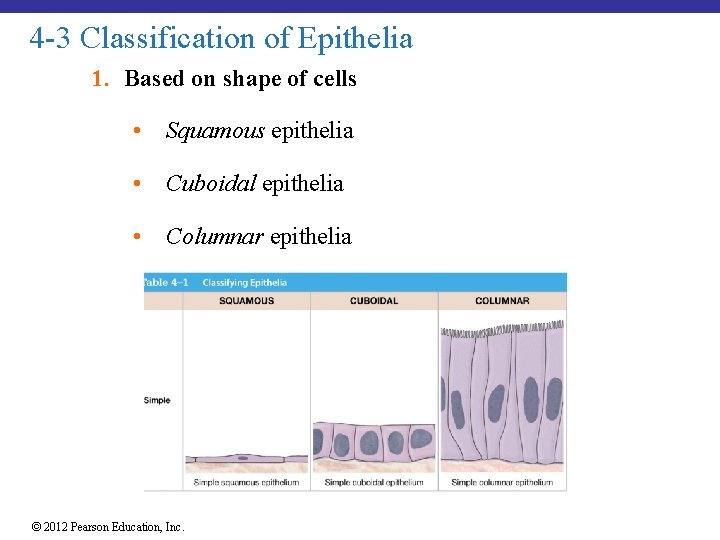
4 -3 Classification of Epithelia 1. Based on shape of cells • Squamous epithelia • Cuboidal epithelia • Columnar epithelia © 2012 Pearson Education, Inc.
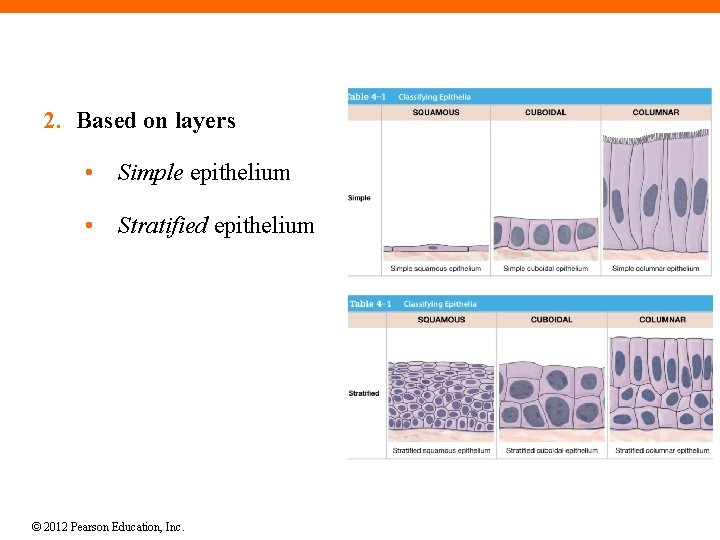
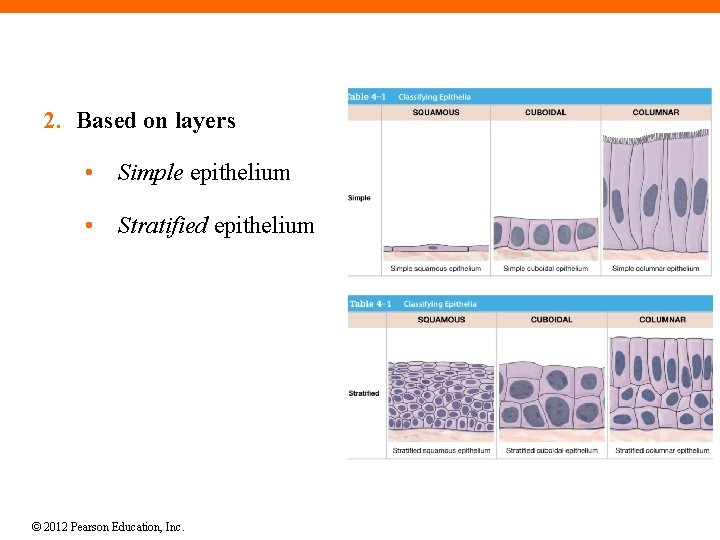
2. Based on layers • Simple epithelium • Stratified epithelium © 2012 Pearson Education, Inc.
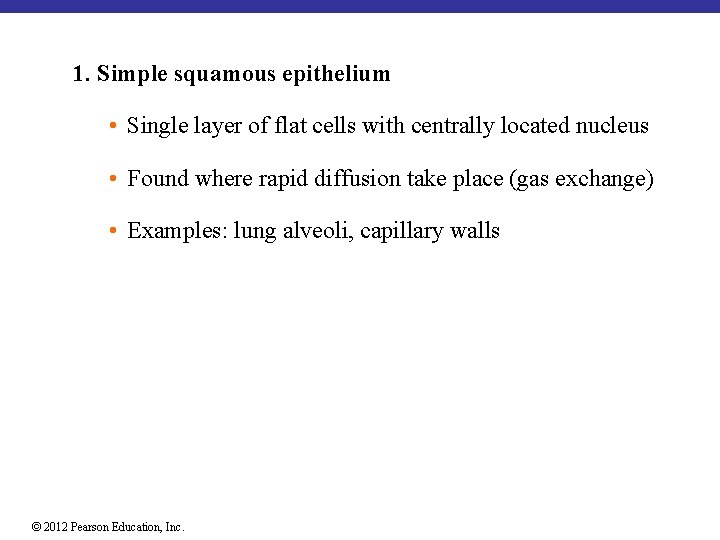
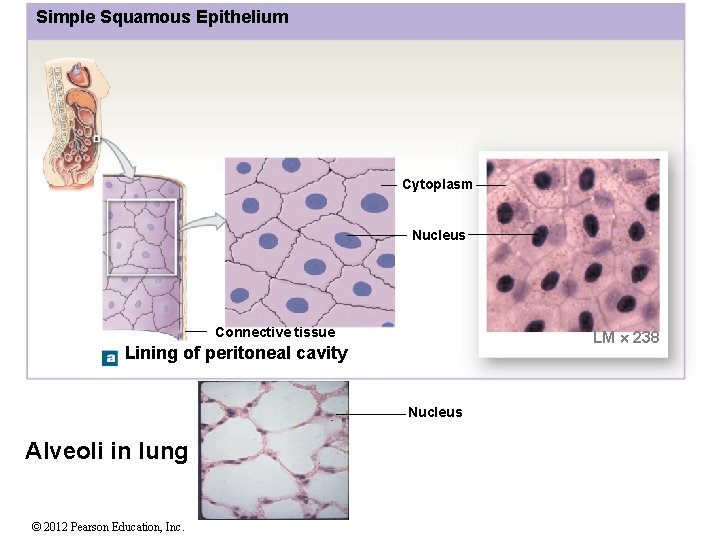
1. Simple squamous epithelium • Single layer of flat cells with centrally located nucleus • Found where rapid diffusion take place (gas exchange) • Examples: lung alveoli, capillary walls © 2012 Pearson Education, Inc.
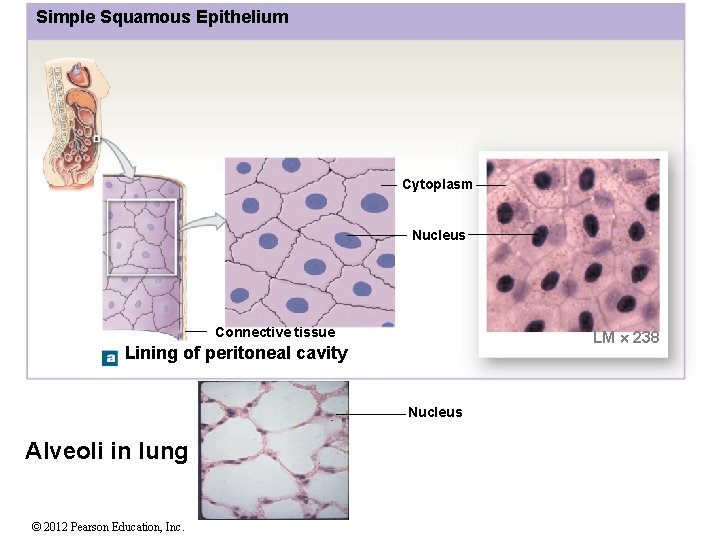
Simple Squamous Epithelium Cytoplasm Nucleus Connective tissue LM 238 Lining of peritoneal cavity Nucleus Alveoli in lung © 2012 Pearson Education, Inc.
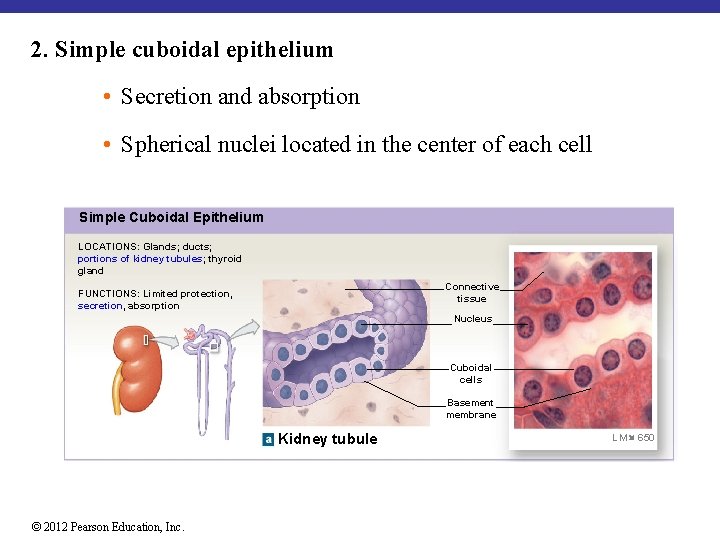
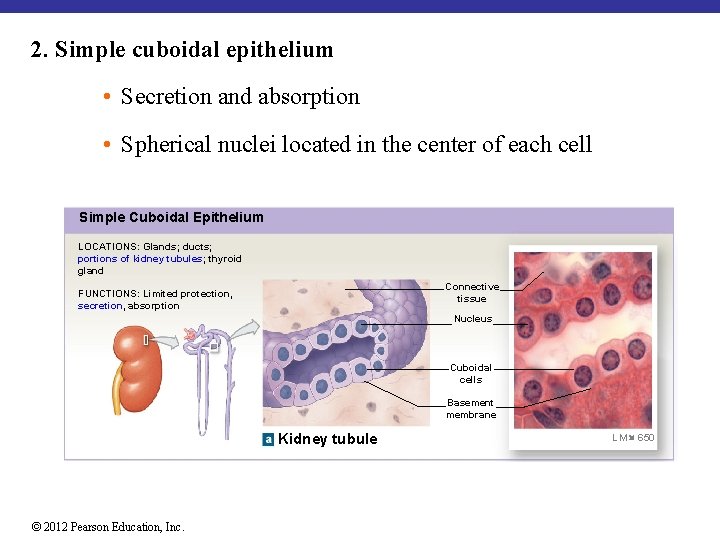
2. Simple cuboidal epithelium • Secretion and absorption • Spherical nuclei located in the center of each cell Simple Cuboidal Epithelium LOCATIONS: Glands; ducts; portions of kidney tubules; thyroid gland Connective tissue FUNCTIONS: Limited protection, secretion, absorption Nucleus Cuboidal cells Basement membrane Kidney tubule © 2012 Pearson Education, Inc. LM 650
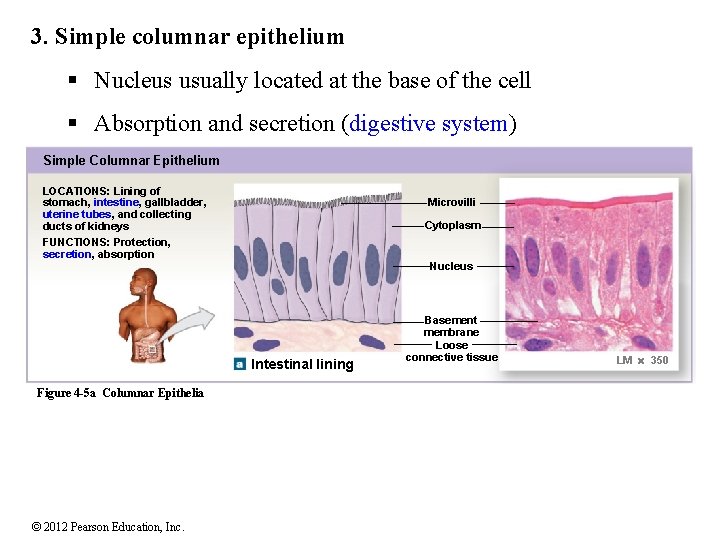
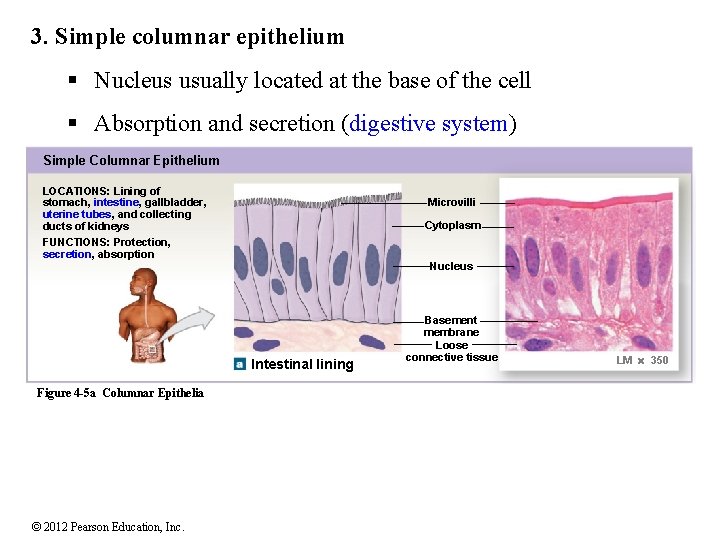
3. Simple columnar epithelium § Nucleus usually located at the base of the cell § Absorption and secretion (digestive system) Simple Columnar Epithelium LOCATIONS: Lining of stomach, intestine, gallbladder, uterine tubes, and collecting ducts of kidneys FUNCTIONS: Protection, secretion, absorption Microvilli Cytoplasm Nucleus Intestinal lining Figure 4 -5 a Columnar Epithelia © 2012 Pearson Education, Inc. Basement membrane Loose connective tissue LM 350
4. Stratified squamous epithelium • Cells at apical layer are squamous in shape; deeper layers may appear cuboidal or columnar • Protects against mechanical stresses • In locations of wear and tear (exposed to the outer environment) • Keratin protein adds strength and water resistance (on skin): keratinized stratified squamous epithelium © 2012 Pearson Education, Inc.

Stratified Squamous Epithelium LOCATIONS: Surface of skin; lining of mouth, throat, esophagus, rectum, anus, and vagina FUNCTIONS: Provides physical protection against abrasion, pathogens, and chemical attack Squamous superficial cells Stem cells Basement membrane Connective tissue Surface of tongue (non-keratinized) © 2012 Pearson Education, Inc. LM 310
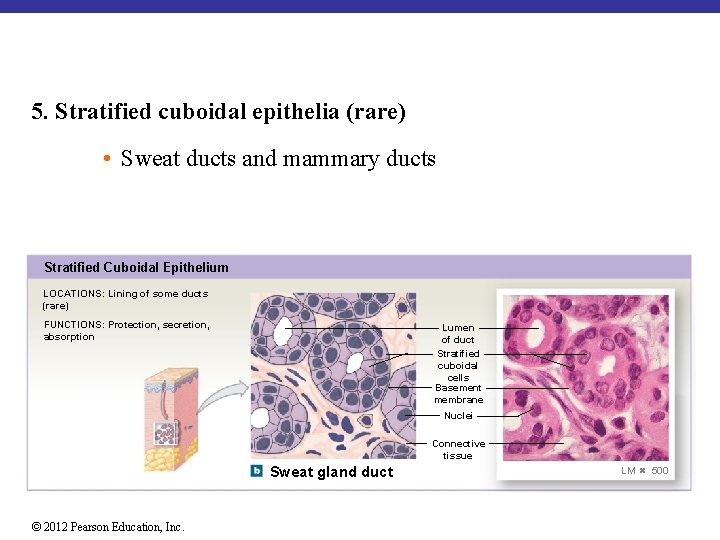
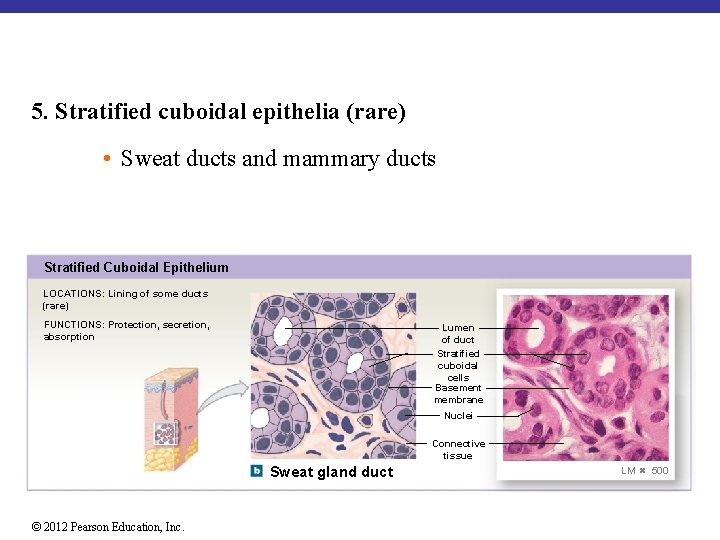
5. Stratified cuboidal epithelia (rare) • Sweat ducts and mammary ducts Stratified Cuboidal Epithelium LOCATIONS: Lining of some ducts (rare) FUNCTIONS: Protection, secretion, absorption Lumen of duct Stratified cuboidal cells Basement membrane Nuclei Connective tissue Sweat gland duct © 2012 Pearson Education, Inc. LM 500
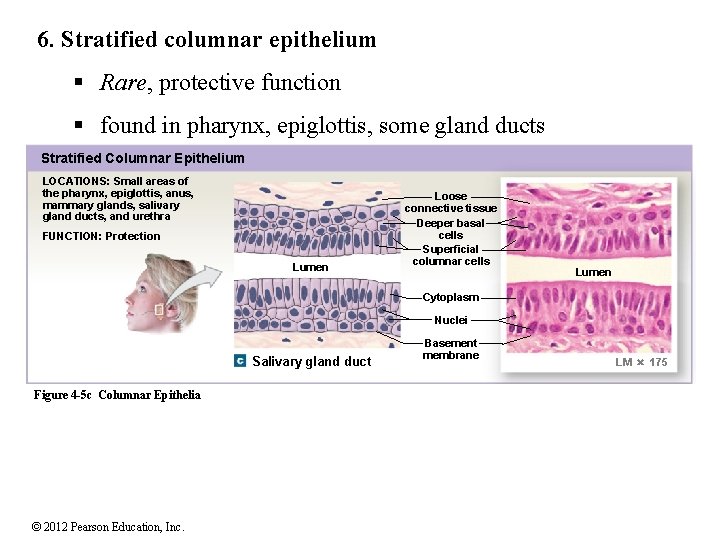
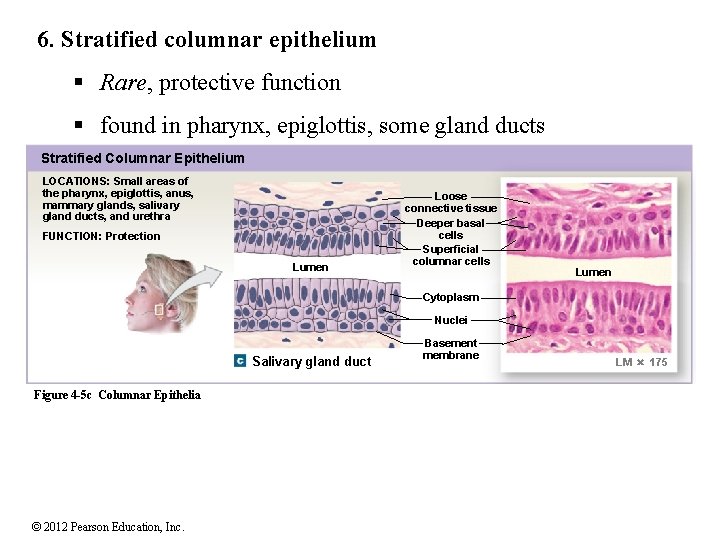
6. Stratified columnar epithelium § Rare, protective function § found in pharynx, epiglottis, some gland ducts Stratified Columnar Epithelium LOCATIONS: Small areas of the pharynx, epiglottis, anus, mammary glands, salivary gland ducts, and urethra FUNCTION: Protection Lumen Loose connective tissue Deeper basal cells Superficial columnar cells Lumen Cytoplasm Nuclei Salivary gland duct Figure 4 -5 c Columnar Epithelia © 2012 Pearson Education, Inc. Basement membrane LM 175
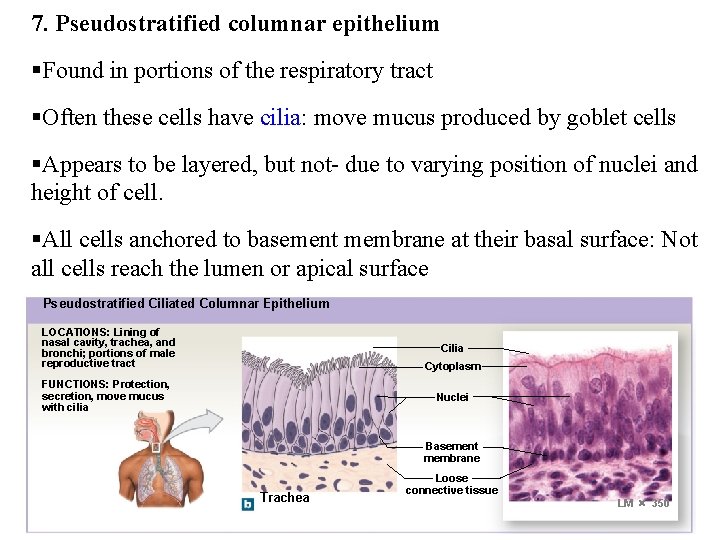
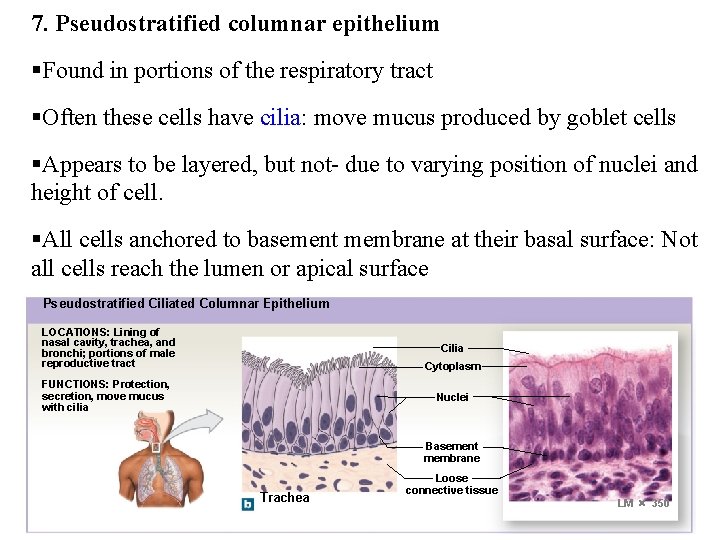
7. Pseudostratified columnar epithelium §Found in portions of the respiratory tract §Often these cells have cilia: move mucus produced by goblet cells §Appears to be layered, but not- due to varying position of nuclei and height of cell. §All cells anchored to basement membrane at their basal surface: Not all cells reach the lumen or apical surface Pseudostratified Ciliated Columnar Epithelium LOCATIONS: Lining of nasal cavity, trachea, and bronchi; portions of male reproductive tract Cilia Cytoplasm FUNCTIONS: Protection, secretion, move mucus with cilia Nuclei Basement membrane Trachea © 2012 Pearson Education, Inc. Loose connective tissue LM 350
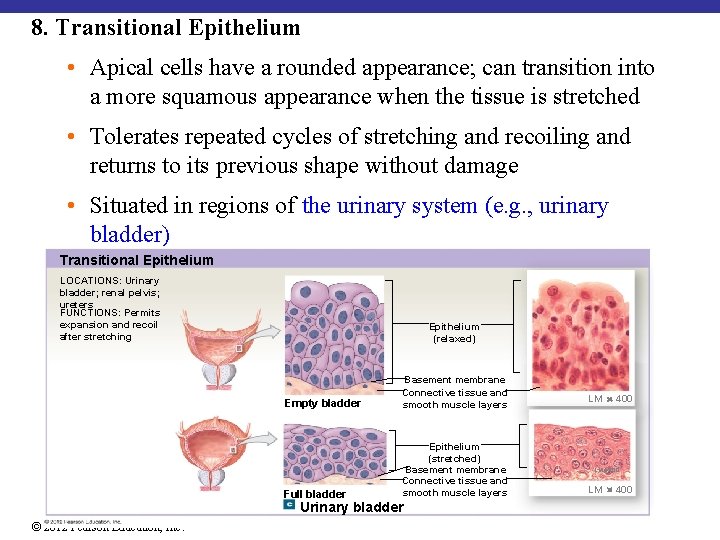
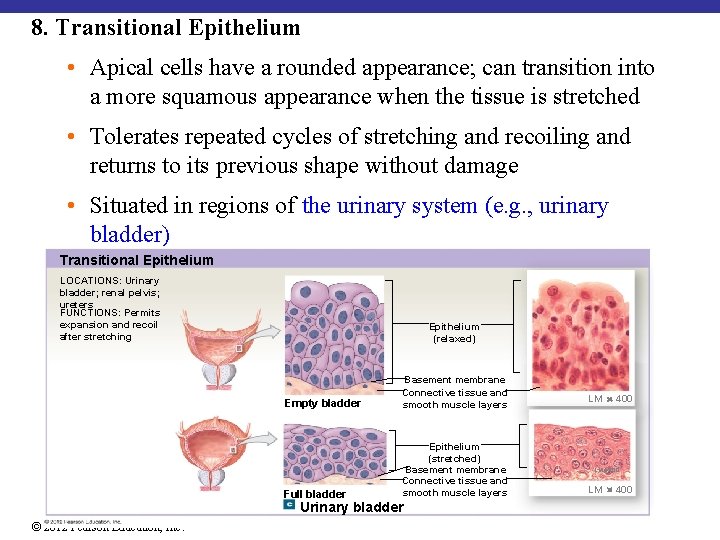
8. Transitional Epithelium • Apical cells have a rounded appearance; can transition into a more squamous appearance when the tissue is stretched • Tolerates repeated cycles of stretching and recoiling and returns to its previous shape without damage • Situated in regions of the urinary system (e. g. , urinary bladder) Transitional Epithelium LOCATIONS: Urinary bladder; renal pelvis; ureters FUNCTIONS: Permits expansion and recoil after stretching Epithelium (relaxed) Empty bladder Basement membrane Connective tissue and smooth muscle layers Full bladder Epithelium (stretched) Basement membrane Connective tissue and smooth muscle layers Urinary bladder © 2012 Pearson Education, Inc. LM 400
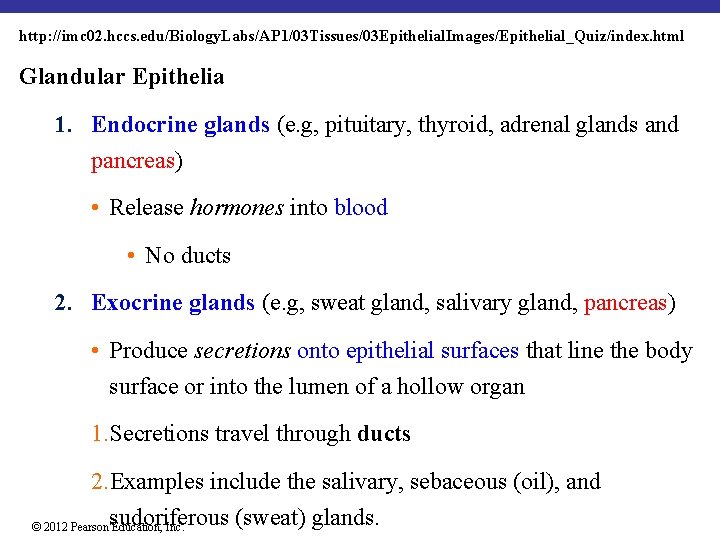
http: //imc 02. hccs. edu/Biology. Labs/AP 1/03 Tissues/03 Epithelial. Images/Epithelial_Quiz/index. html Glandular Epithelia 1. Endocrine glands (e. g, pituitary, thyroid, adrenal glands and pancreas) • Release hormones into blood • No ducts 2. Exocrine glands (e. g, sweat gland, salivary gland, pancreas) • Produce secretions onto epithelial surfaces that line the body surface or into the lumen of a hollow organ 1. Secretions travel through ducts 2. Examples include the salivary, sebaceous (oil), and sudoriferous (sweat) glands. © 2012 Pearson Education, Inc.
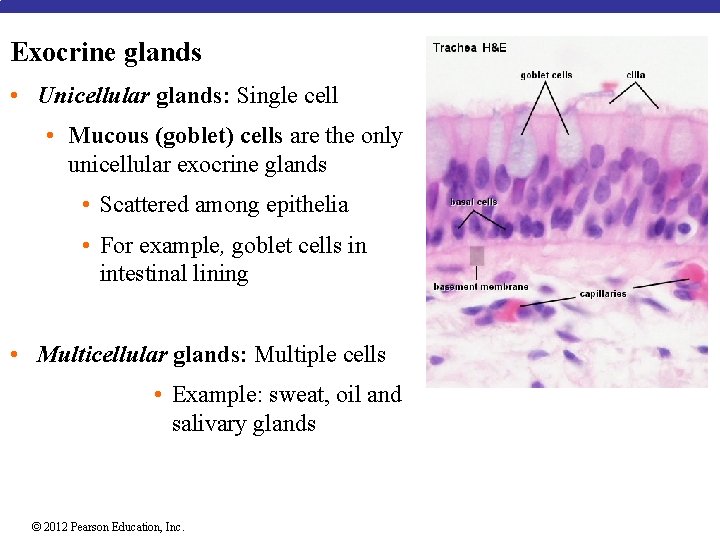
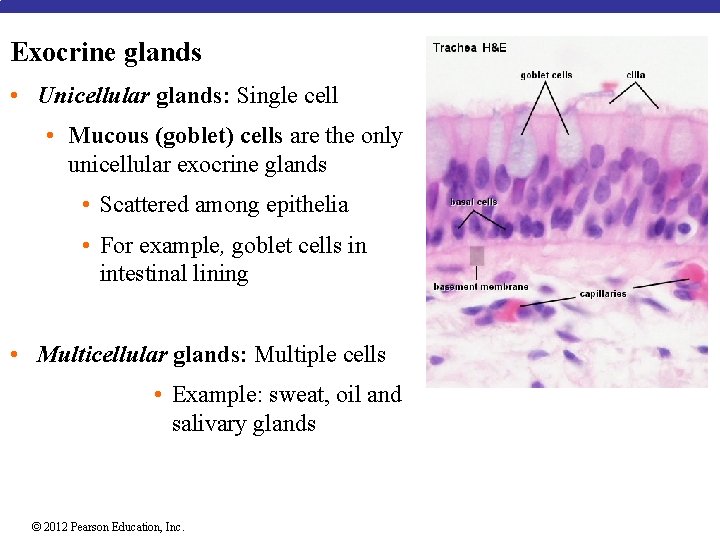
Exocrine glands • Unicellular glands: Single cell • Mucous (goblet) cells are the only unicellular exocrine glands • Scattered among epithelia • For example, goblet cells in intestinal lining • Multicellular glands: Multiple cells • Example: sweat, oil and salivary glands © 2012 Pearson Education, Inc.
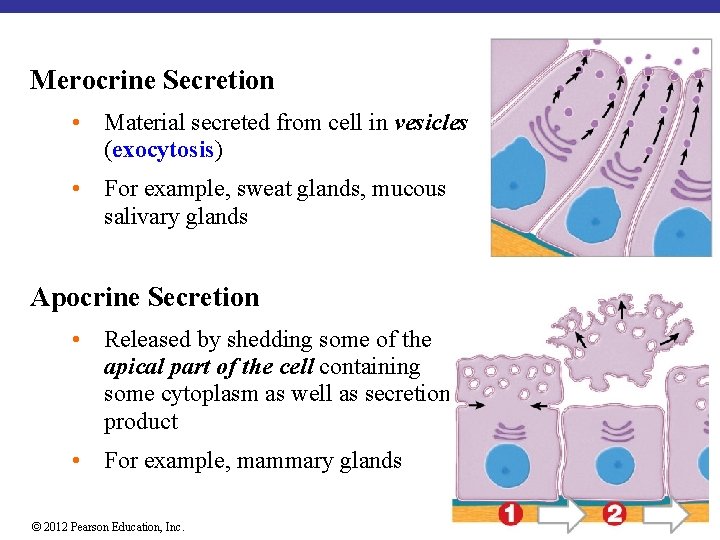
Exocrine glands Modes of Secretion 1. Merocrine secretion 2. Apocrine secretion 3. Holocrine secretion © 2012 Pearson Education, Inc.
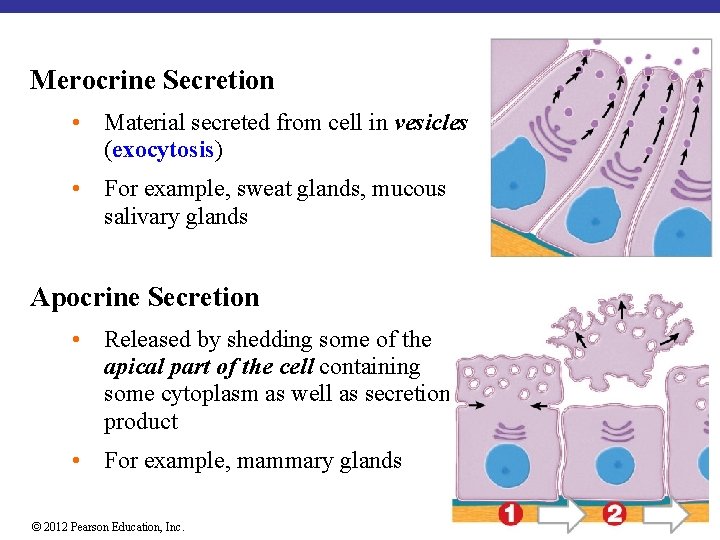
Merocrine Secretion • Material secreted from cell in vesicles (exocytosis) • For example, sweat glands, mucous salivary glands Apocrine Secretion • Released by shedding some of the apical part of the cell containing some cytoplasm as well as secretion product • For example, mammary glands © 2012 Pearson Education, Inc.
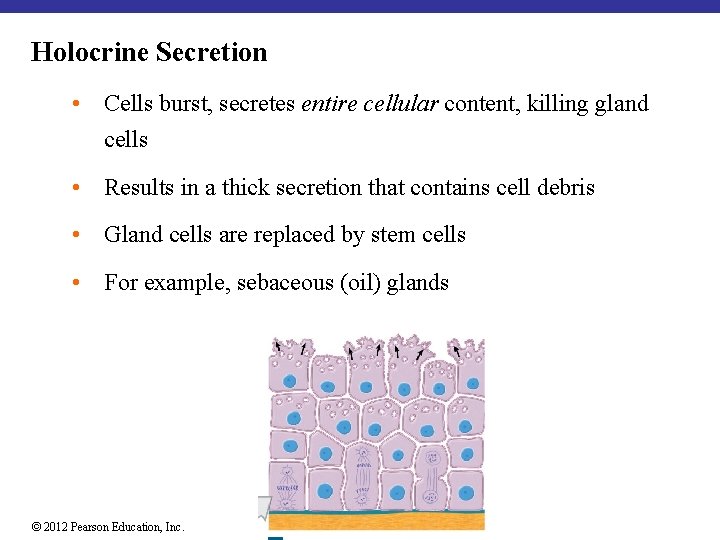
Holocrine Secretion • Cells burst, secretes entire cellular content, killing gland cells • Results in a thick secretion that contains cell debris • Gland cells are replaced by stem cells • For example, sebaceous (oil) glands © 2012 Pearson Education, Inc.
4 -4 Connective Tissue Examples: Blood, bone, cartilage, adipose tissue Functions: protection, support, transportation, immunity, and energy storage. Characteristics: • Abundant in the body • Found deeper in the body • Typically vascular (except cartilage and dense connective tissue) & supplied with nerves (except cartilage) • Few cells and much intercellular space (Extracellular matrix) © 2012 Pearson Education, Inc.
4 -4 Connective Tissue Extracellular Matrix (Matrix) • The non-living extracellular matrix makes up the majority of the CT • consists of ground substance and protein fibers - Fibers: made of protein - Ground substance: fluid, rubbery or solid © 2012 Pearson Education, Inc.
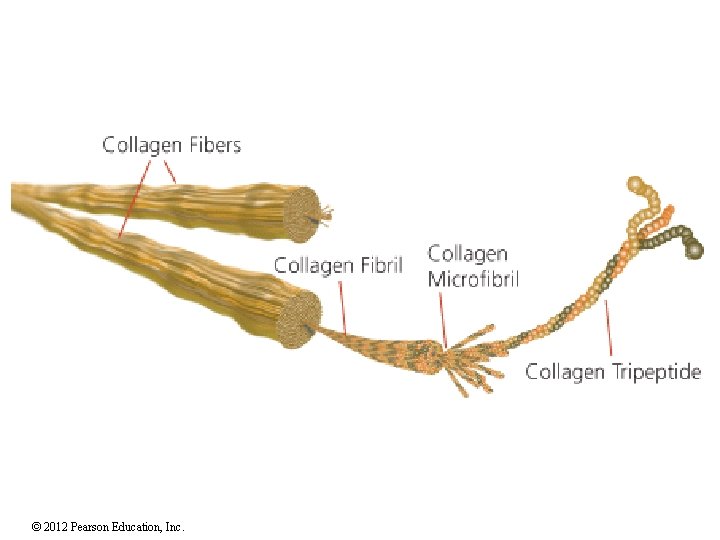
Connective Tissue: Fibers 1. Collagen fibers: most common, made of collagen. Long, strong, flexible, resist stretching, in dermis of the skin, in tendons, ligaments, cartilage, bone 2. Reticular fibers: thin bundle of collagen type III fibers that branch, strong and flexible, in lymph nodes, spleen, basement membranes 3. Elastic fibers: contain elastin, branched and wavy, elastic (return to original length after being stretched), in skin, lungs, arteries © 2012 Pearson Education, Inc.
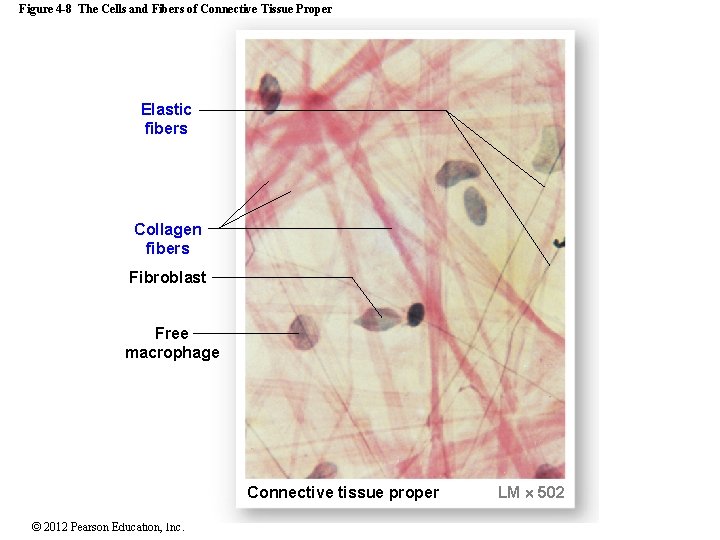
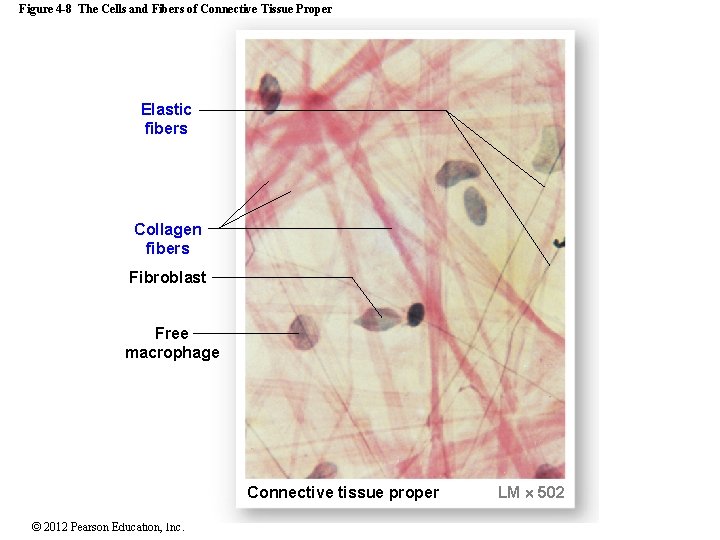
Figure 4 -8 The Cells and Fibers of Connective Tissue Proper Elastic fibers Collagen fibers Fibroblast Free macrophage Connective tissue proper © 2012 Pearson Education, Inc. LM 502
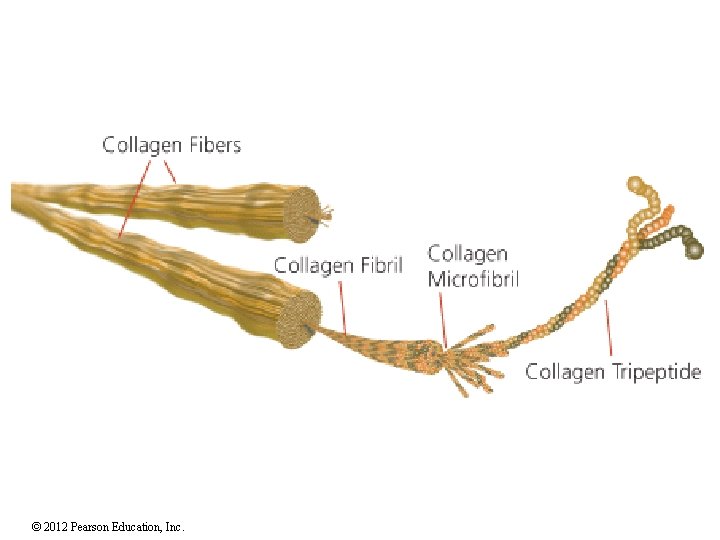
© 2012 Pearson Education, Inc.
Connective Tissue Matrix: Ground Substance • Present between cells • Consistency varies from fibrous to solid to semi-solid to liquid • Functions to bind cells, provide support and a medium for nutrients and gases • Composed of polysaccharides and proteins forming proteoglycans • Hyaluronic acid and chondroitin sulfate---examples of polysaccharides • Proteoglycans (proteins and polysaccharides) © 2012 Pearson Education, Inc.
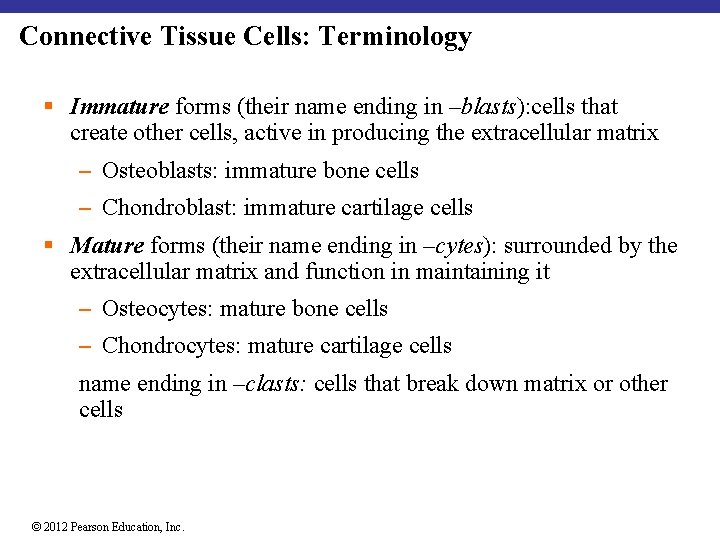
Connective Tissue Cells: Terminology § Immature forms (their name ending in –blasts): cells that create other cells, active in producing the extracellular matrix ─ Osteoblasts: immature bone cells ─ Chondroblast: immature cartilage cells § Mature forms (their name ending in –cytes): surrounded by the extracellular matrix and function in maintaining it ─ Osteocytes: mature bone cells ─ Chondrocytes: mature cartilage cells name ending in –clasts: cells that break down matrix or other cells © 2012 Pearson Education, Inc.
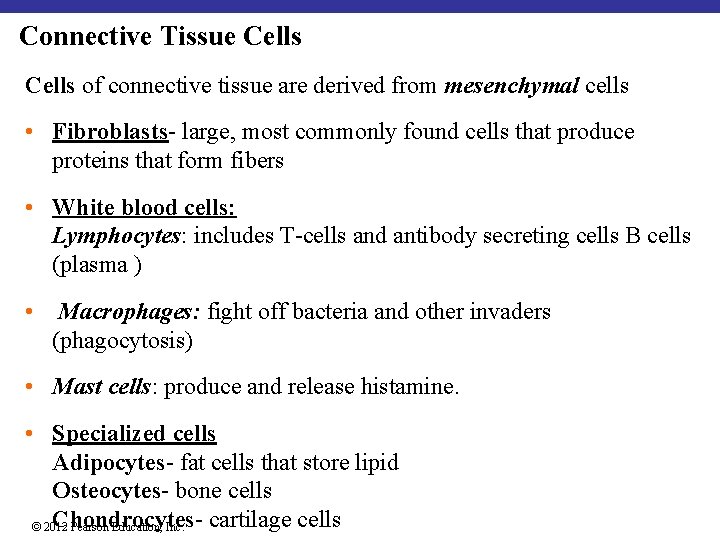
Connective Tissue Cells of connective tissue are derived from mesenchymal cells • Fibroblasts- large, most commonly found cells that produce proteins that form fibers • White blood cells: Lymphocytes: includes T-cells and antibody secreting cells B cells (plasma ) • Macrophages: fight off bacteria and other invaders (phagocytosis) • Mast cells: produce and release histamine. • Specialized cells Adipocytes- fat cells that store lipid Osteocytes- bone cells Chondrocytescartilage cells © 2012 Pearson Education, Inc.

Figure 4 -8 The Cells and Fibers of Connective Tissue Proper Reticular fibers Melanocyte Fixed macrophage Plasma cell Mast cell Elastic fibers Free macrophage Collagen fibers Blood in vessel Fibroblast Adipocytes (fat cells) Mesenchymal cell Ground substance © 2012 Pearson Education, Inc. Lymphocyte
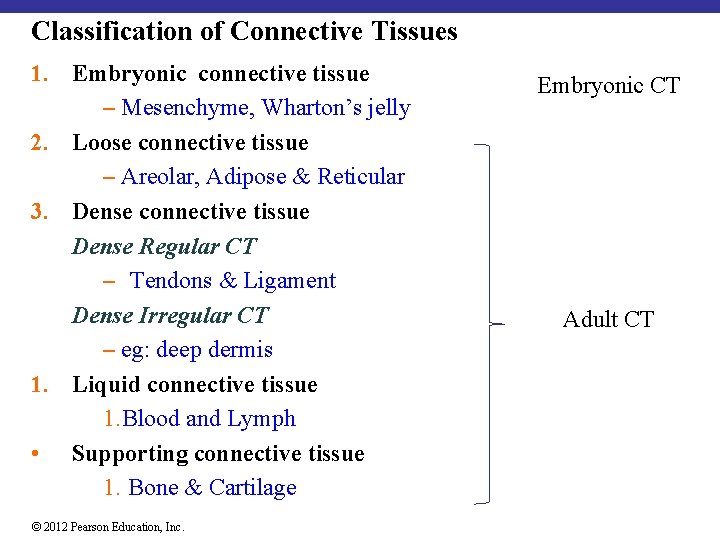
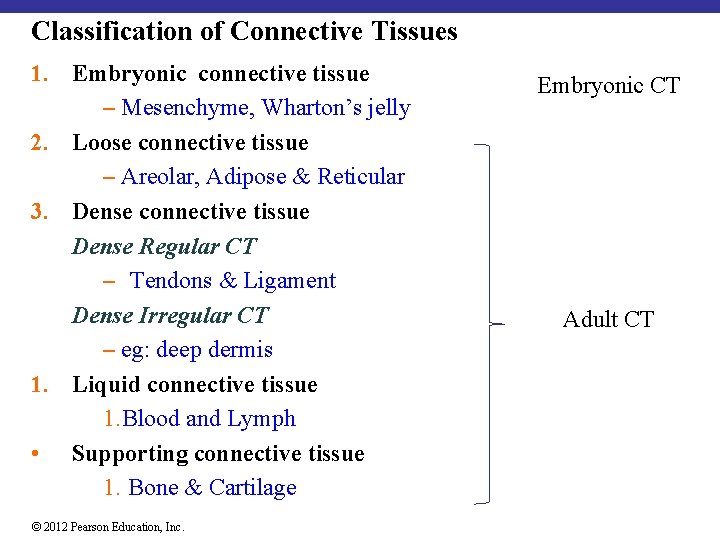
Classification of Connective Tissues 1. Embryonic connective tissue ─ Mesenchyme, Wharton’s jelly 2. Loose connective tissue ─ Areolar, Adipose & Reticular 3. Dense connective tissue Dense Regular CT ─ Tendons & Ligament Dense Irregular CT ─ eg: deep dermis 1. Liquid connective tissue 1. Blood and Lymph • Supporting connective tissue 1. Bone & Cartilage © 2012 Pearson Education, Inc. Embryonic CT Adult CT
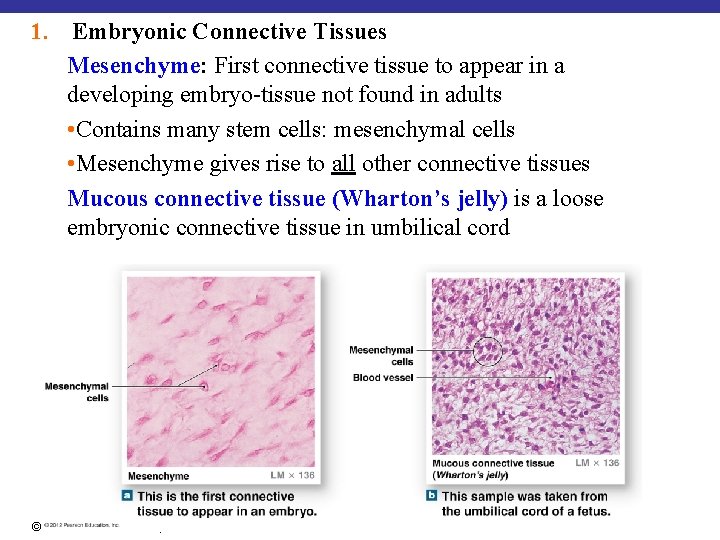
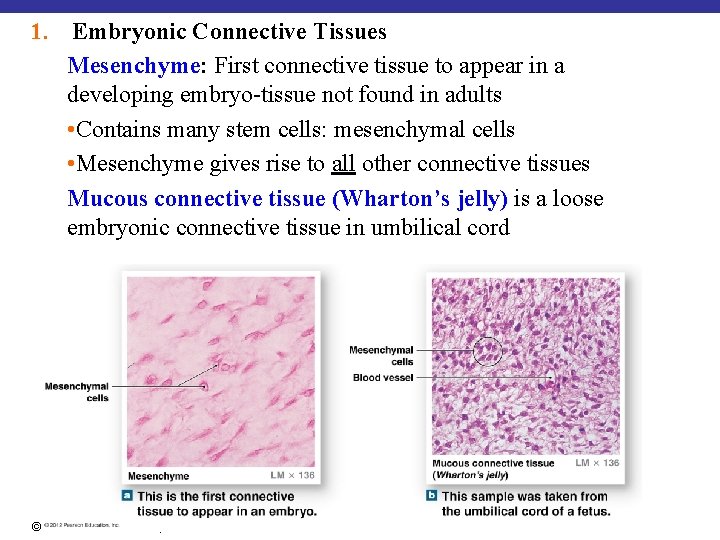
1. Embryonic Connective Tissues Mesenchyme: First connective tissue to appear in a developing embryo-tissue not found in adults • Contains many stem cells: mesenchymal cells • Mesenchyme gives rise to all other connective tissues Mucous connective tissue (Wharton’s jelly) is a loose embryonic connective tissue in umbilical cord © 2012 Pearson Education, Inc.
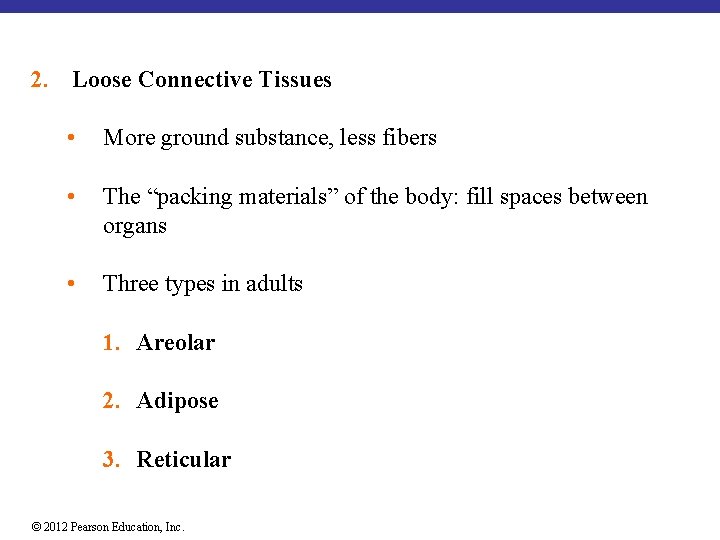
2. Loose Connective Tissues • More ground substance, less fibers • The “packing materials” of the body: fill spaces between organs • Three types in adults 1. Areolar 2. Adipose 3. Reticular © 2012 Pearson Education, Inc.
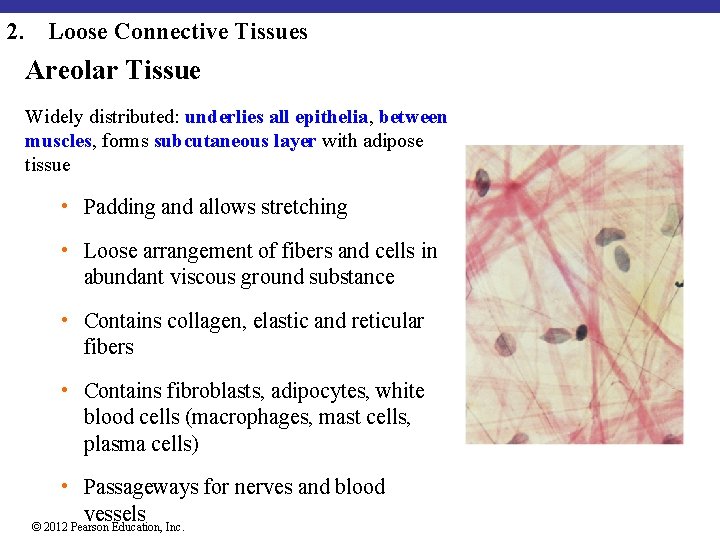
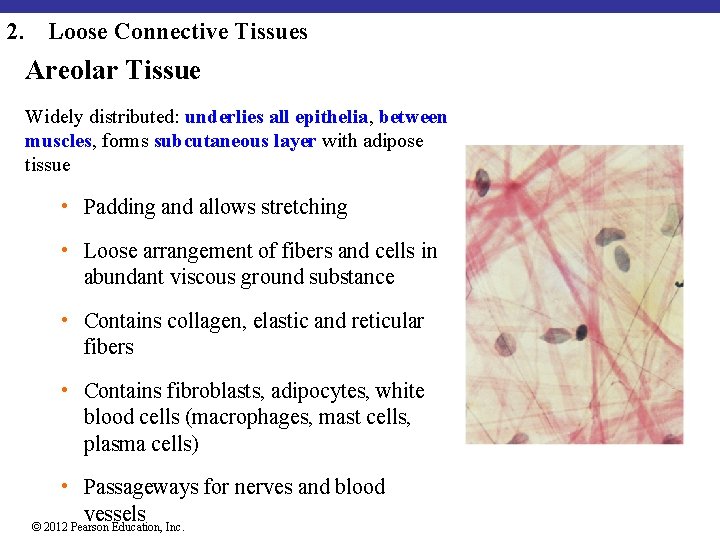
2. Loose Connective Tissues Areolar Tissue Widely distributed: underlies all epithelia, between muscles, forms subcutaneous layer with adipose tissue • Padding and allows stretching • Loose arrangement of fibers and cells in abundant viscous ground substance • Contains collagen, elastic and reticular fibers • Contains fibroblasts, adipocytes, white blood cells (macrophages, mast cells, plasma cells) • Passageways for nerves and blood vessels © 2012 Pearson Education, Inc.
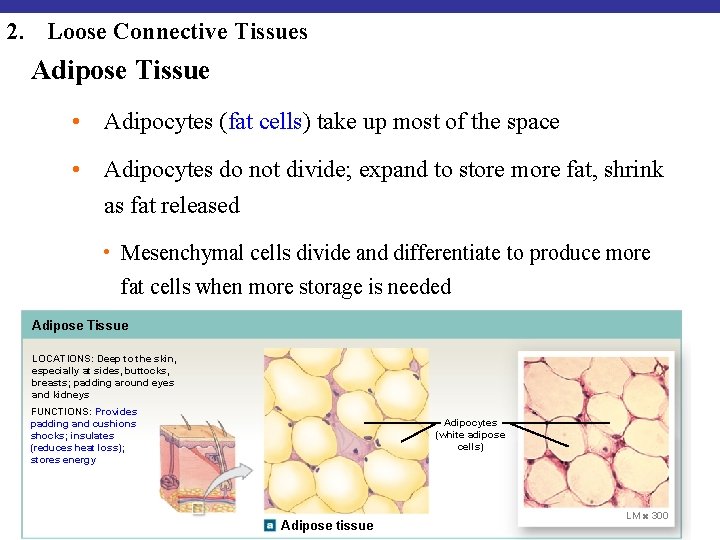
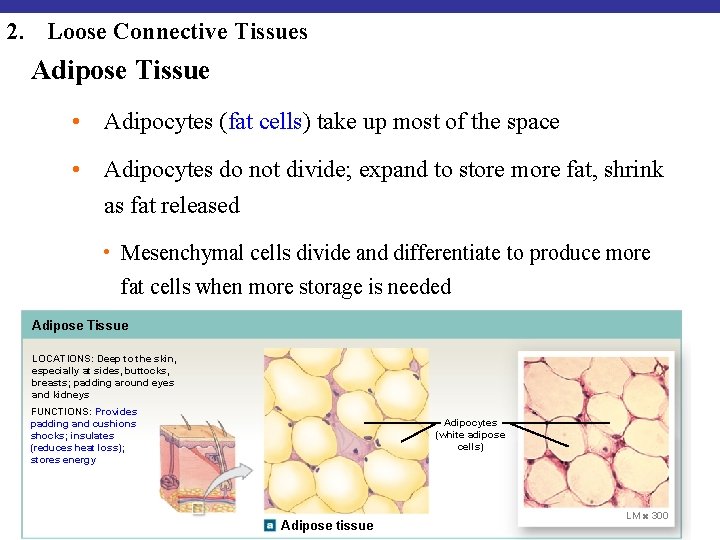
2. Loose Connective Tissues Adipose Tissue • Adipocytes (fat cells) take up most of the space • Adipocytes do not divide; expand to store more fat, shrink as fat released • Mesenchymal cells divide and differentiate to produce more fat cells when more storage is needed Adipose Tissue LOCATIONS: Deep to the skin, especially at sides, buttocks, breasts; padding around eyes and kidneys FUNCTIONS: Provides padding and cushions shocks; insulates (reduces heat loss); stores energy © 2012 Pearson Education, Inc. Adipocytes (white adipose cells) Adipose tissue LM 300
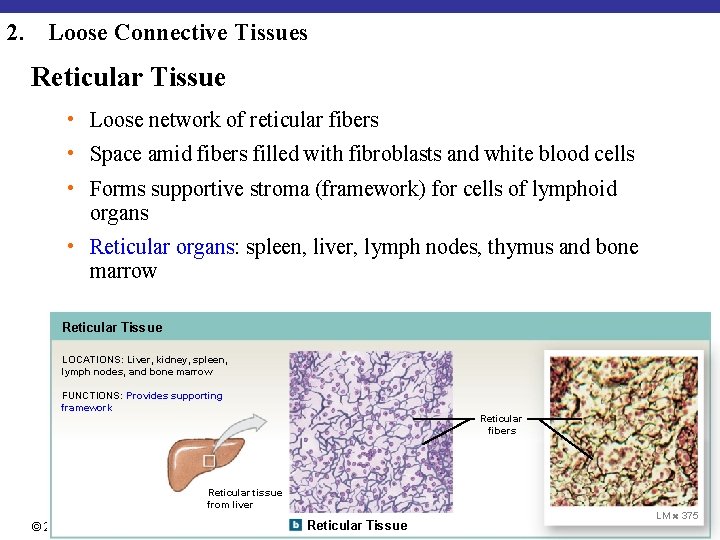
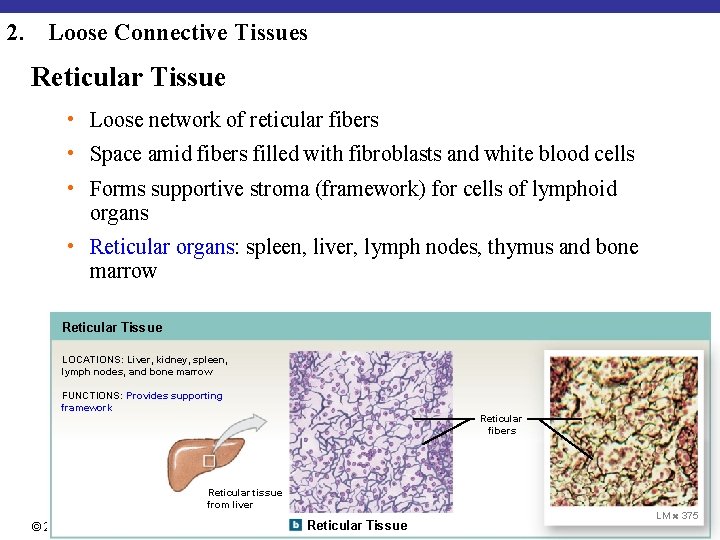
2. Loose Connective Tissues Reticular Tissue • Loose network of reticular fibers • Space amid fibers filled with fibroblasts and white blood cells • Forms supportive stroma (framework) for cells of lymphoid organs • Reticular organs: spleen, liver, lymph nodes, thymus and bone marrow Reticular Tissue LOCATIONS: Liver, kidney, spleen, lymph nodes, and bone marrow FUNCTIONS: Provides supporting framework Reticular fibers Reticular tissue from liver © 2012 Pearson Education, Inc. Reticular Tissue LM 375
3. Dense Connective Tissues • Tightly packed with high numbers of collagen fibers, little matrix. • Dependent on orientation of fibers, further classified into • Dense regular connective tissue-parallel • Dense irregular connective tissue-randomly arranged © 2012 Pearson Education, Inc.
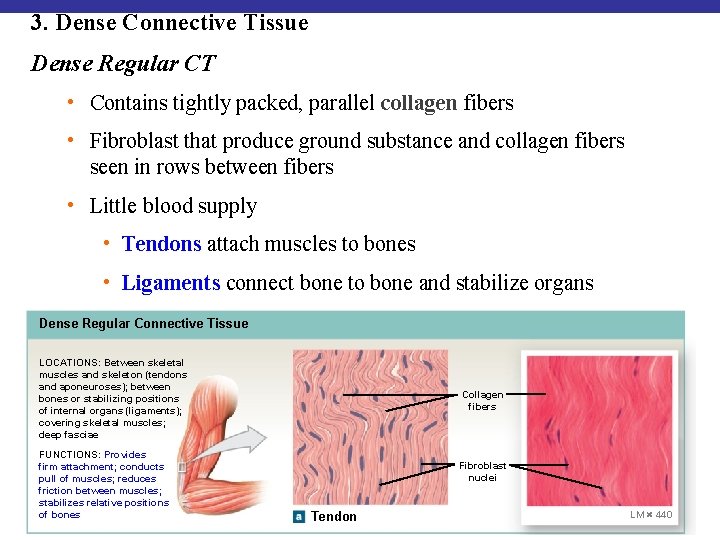
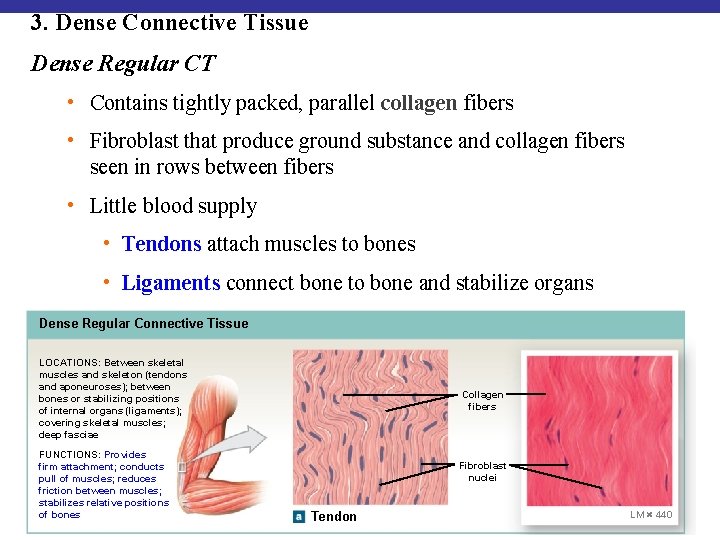
3. Dense Connective Tissue Dense Regular CT • Contains tightly packed, parallel collagen fibers • Fibroblast that produce ground substance and collagen fibers seen in rows between fibers • Little blood supply • Tendons attach muscles to bones • Ligaments connect bone to bone and stabilize organs Dense Regular Connective Tissue LOCATIONS: Between skeletal muscles and skeleton (tendons and aponeuroses); between bones or stabilizing positions of internal organs (ligaments); covering skeletal muscles; deep fasciae FUNCTIONS: Provides firm attachment; conducts pull of muscles; reduces friction between muscles; stabilizes relative positions of bones © 2012 Pearson Education, Inc. Collagen fibers Fibroblast nuclei Tendon LM 440
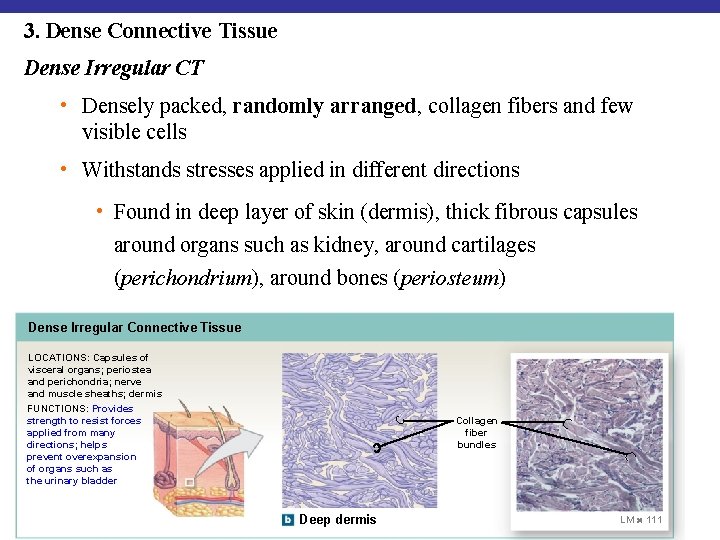
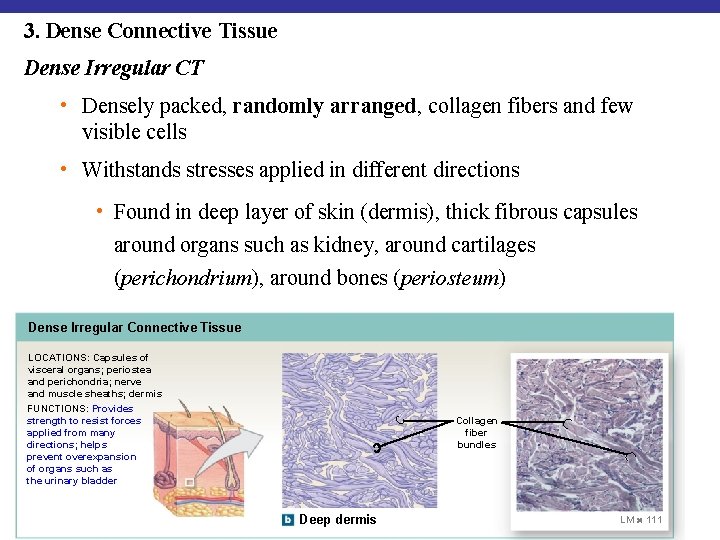
3. Dense Connective Tissue Dense Irregular CT • Densely packed, randomly arranged, collagen fibers and few visible cells • Withstands stresses applied in different directions • Found in deep layer of skin (dermis), thick fibrous capsules around organs such as kidney, around cartilages (perichondrium), around bones (periosteum) Dense Irregular Connective Tissue LOCATIONS: Capsules of visceral organs; periostea and perichondria; nerve and muscle sheaths; dermis • Around bones (periosteum) FUNCTIONS: Provides strength to resist forces applied from many directions; helps prevent overexpansion of organs such as the urinary bladder © 2012 Pearson Education, Inc. Collagen fiber bundles Deep dermis LM 111
4. Fluid Connective Tissues: Blood and lymph • Watery matrix of dissolved proteins (no fibers) Blood : Liquid matrix (plasma: water, electrolytes, dissolved proteins, nutrients, waste products, and hormones) containing cells and cell fragments • Red blood cells (erythrocytes): Transport oxygen • White blood cells (leukocytes): Immune protection • Platelets (thrombocytes-cell fragment): Blood clotting Lymph forms as interstitial fluid enters lymphatic vessels. © 2012 Pearson Education, Inc.
5. Supporting Connective Tissues Support Soft Tissues and Body Weight Cartilage • Gel-type ground substance • For shock absorption and protection Bone • Calcified (made rigid by calcium salts, minerals) • For weight support © 2012 Pearson Education, Inc.
5. Supporting Connective Tissues Cartilage • Cell types: • Chondroblasts produce matrix. • Chondrocytes: chondroblasts that have been trapped into matrix, lie within lacunae (chambers) within the extracellular matrix • Matrix: Rubbery (gel) matrix of chondroitin sulfates and protein fibers • Avascular: chondrocytes produce antiangiogenesis factor-slow repair • No nerves • Perichondrium: surrounding layer for protection, attachment to other tissues, maintenance and growth © 2012 Pearson Education, Inc.
Types of Cartilage 1. Hyaline cartilage 2. Elastic cartilage 3. Fibrocartilage (fibrous cartilage) © 2012 Pearson Education, Inc.
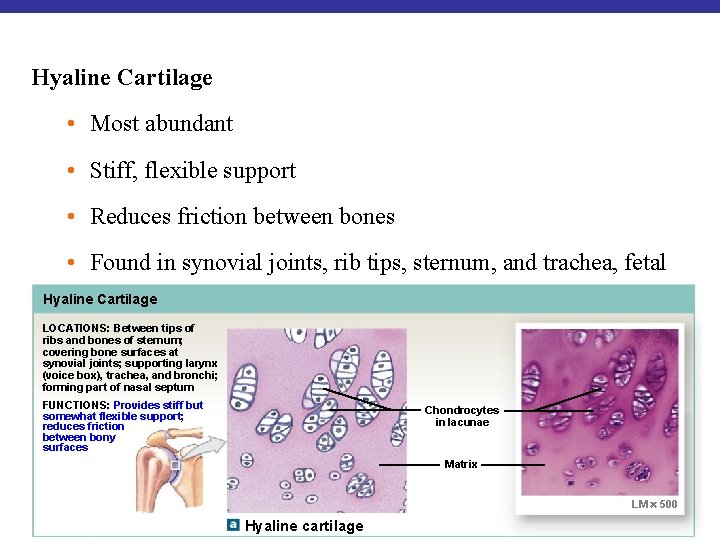
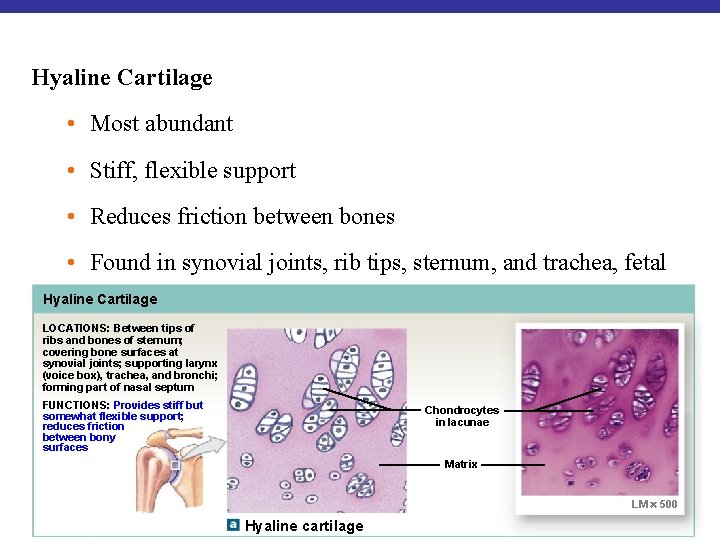
Hyaline Cartilage • Most abundant • Stiff, flexible support • Reduces friction between bones • Found in synovial joints, rib tips, sternum, and trachea, fetal Hyalineskeleton Cartilage LOCATIONS: Between tips of ribs and bones of sternum; covering bone surfaces at synovial joints; supporting larynx (voice box), trachea, and bronchi; forming part of nasal septum FUNCTIONS: Provides stiff but somewhat flexible support; reduces friction between bony surfaces Chondrocytes in lacunae Matrix LM 500 © 2012 Pearson Education, Inc. Hyaline cartilage
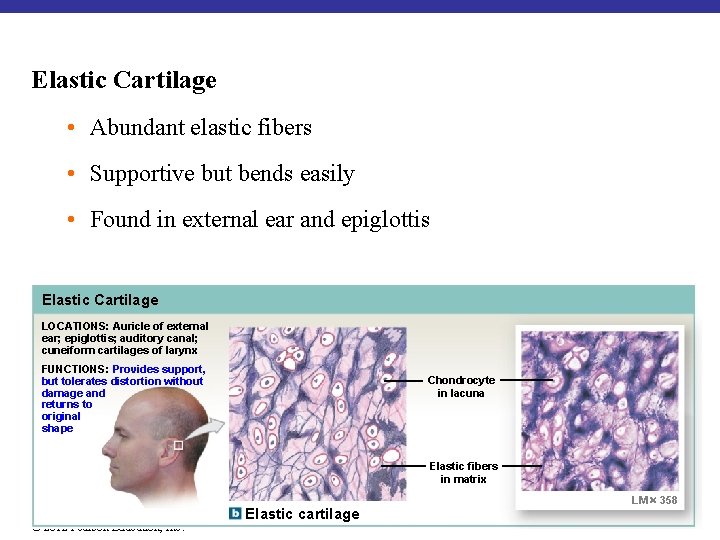
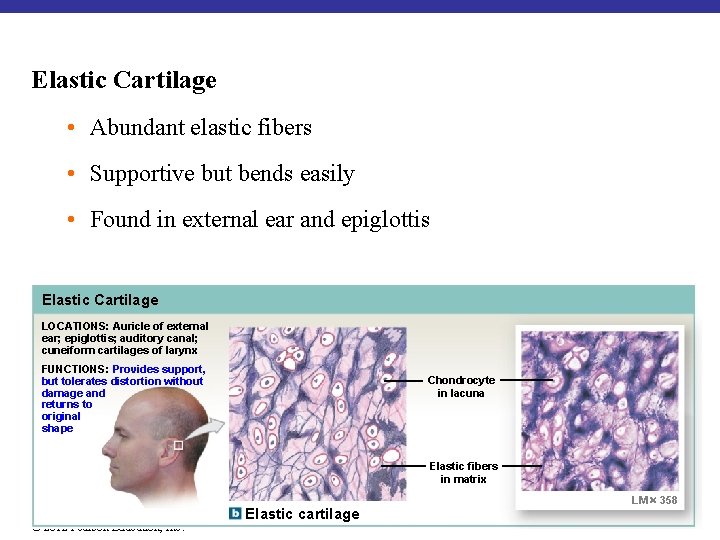
Elastic Cartilage • Abundant elastic fibers • Supportive but bends easily • Found in external ear and epiglottis Elastic Cartilage LOCATIONS: Auricle of external ear; epiglottis; auditory canal; cuneiform cartilages of larynx FUNCTIONS: Provides support, but tolerates distortion without damage and returns to original shape Chondrocyte in lacuna Elastic fibers in matrix © 2012 Pearson Education, Inc. Elastic cartilage LM 358
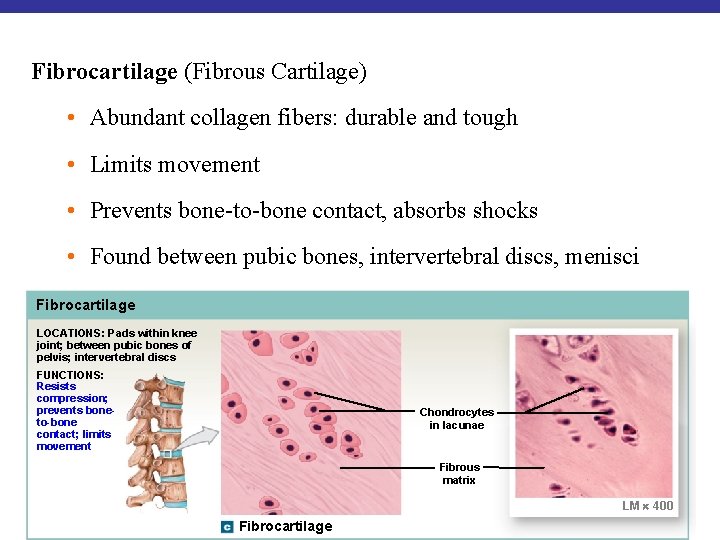
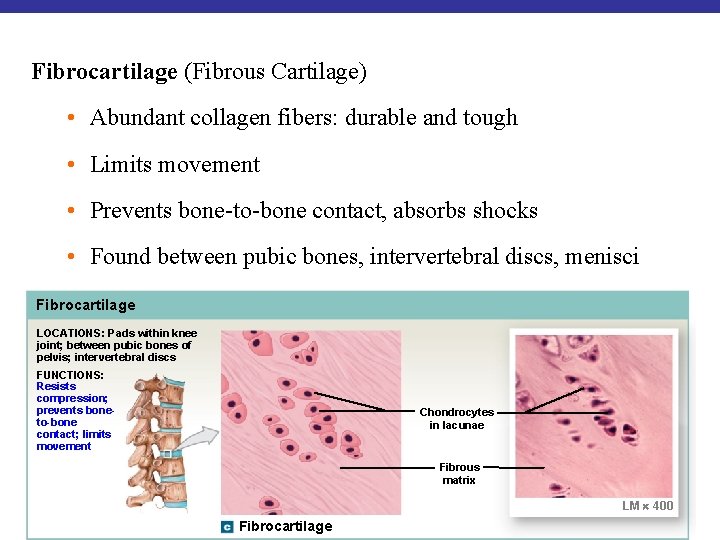
Fibrocartilage (Fibrous Cartilage) • Abundant collagen fibers: durable and tough • Limits movement • Prevents bone-to-bone contact, absorbs shocks • Found between pubic bones, intervertebral discs, menisci Fibrocartilage LOCATIONS: Pads within knee joint; between pubic bones of pelvis; intervertebral discs FUNCTIONS: Resists compression; prevents boneto-bone contact; limits movement Chondrocytes in lacunae Fibrous matrix LM 400 © 2012 Pearson Education, Inc. Fibrocartilage
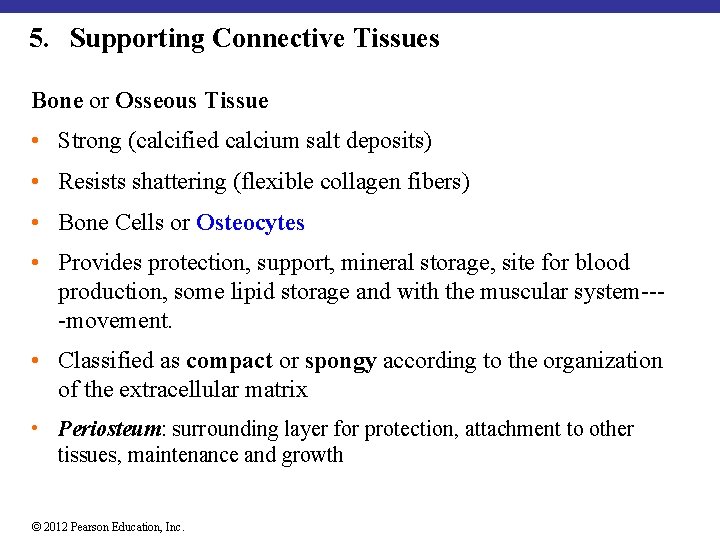
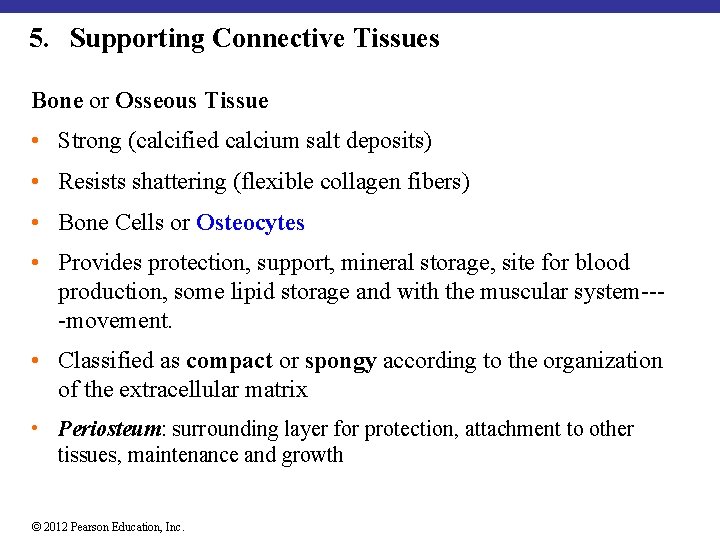
5. Supporting Connective Tissues Bone or Osseous Tissue • Strong (calcified calcium salt deposits) • Resists shattering (flexible collagen fibers) • Bone Cells or Osteocytes • Provides protection, support, mineral storage, site for blood production, some lipid storage and with the muscular system---movement. • Classified as compact or spongy according to the organization of the extracellular matrix • Periosteum: surrounding layer for protection, attachment to other tissues, maintenance and growth © 2012 Pearson Education, Inc.
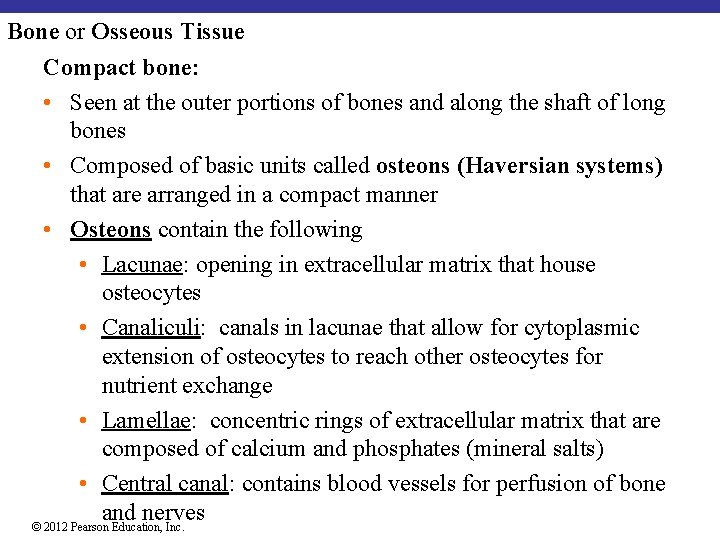
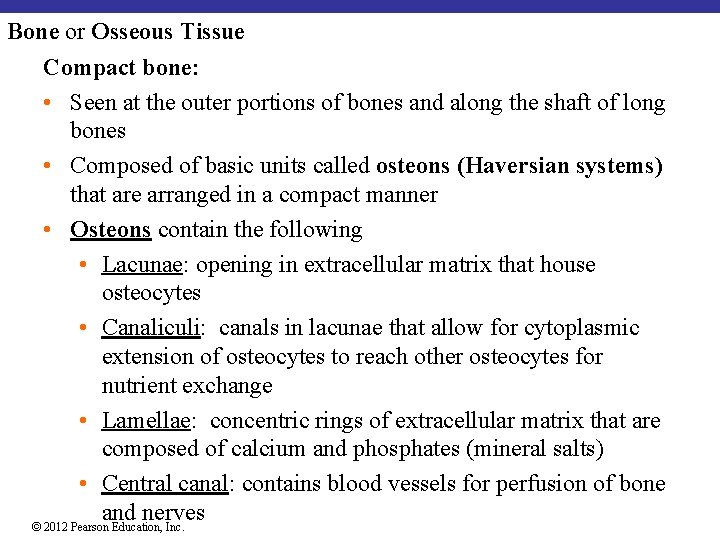
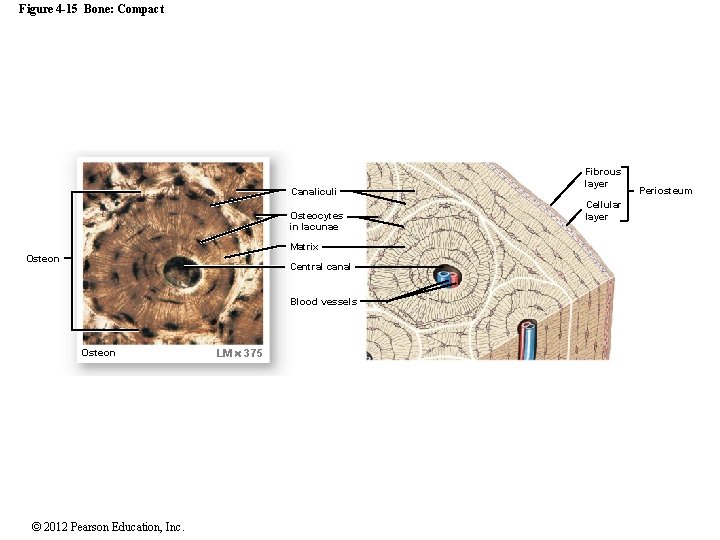
Bone or Osseous Tissue Compact bone: • Seen at the outer portions of bones and along the shaft of long bones • Composed of basic units called osteons (Haversian systems) that are arranged in a compact manner • Osteons contain the following • Lacunae: opening in extracellular matrix that house osteocytes • Canaliculi: canals in lacunae that allow for cytoplasmic extension of osteocytes to reach other osteocytes for nutrient exchange • Lamellae: concentric rings of extracellular matrix that are composed of calcium and phosphates (mineral salts) • Central canal: contains blood vessels for perfusion of bone and nerves © 2012 Pearson Education, Inc.
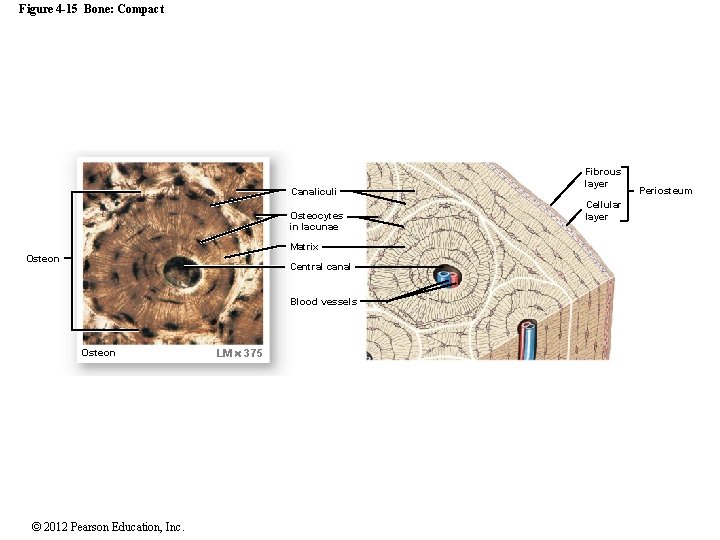
Figure 4 -15 Bone: Compact Canaliculi Osteocytes in lacunae Matrix Osteon Central canal Blood vessels Osteon © 2012 Pearson Education, Inc. LM 375 Fibrous layer Cellular layer Periosteum
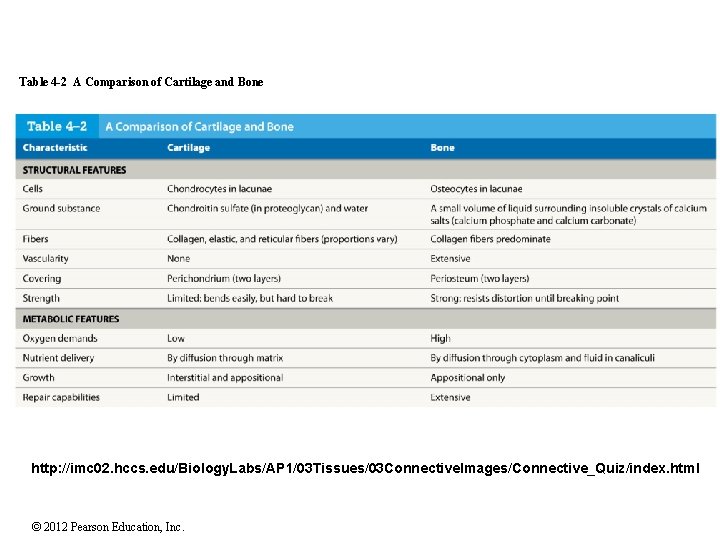
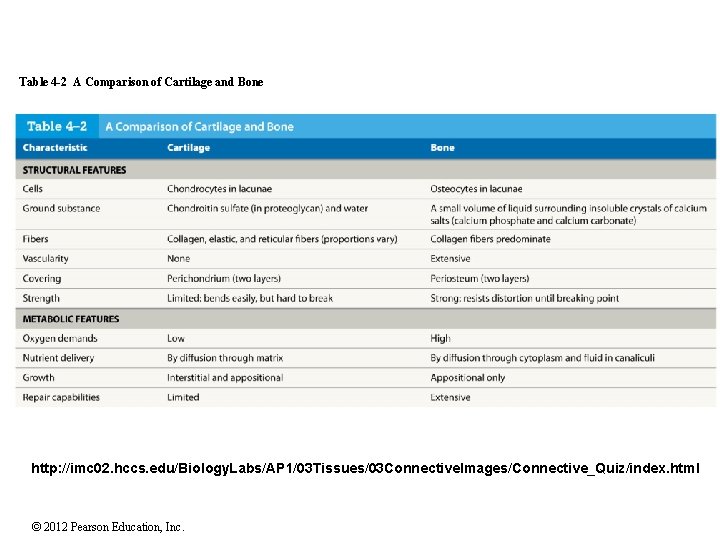
Table 4 -2 A Comparison of Cartilage and Bone http: //imc 02. hccs. edu/Biology. Labs/AP 1/03 Tissues/03 Connective. Images/Connective_Quiz/index. html © 2012 Pearson Education, Inc.
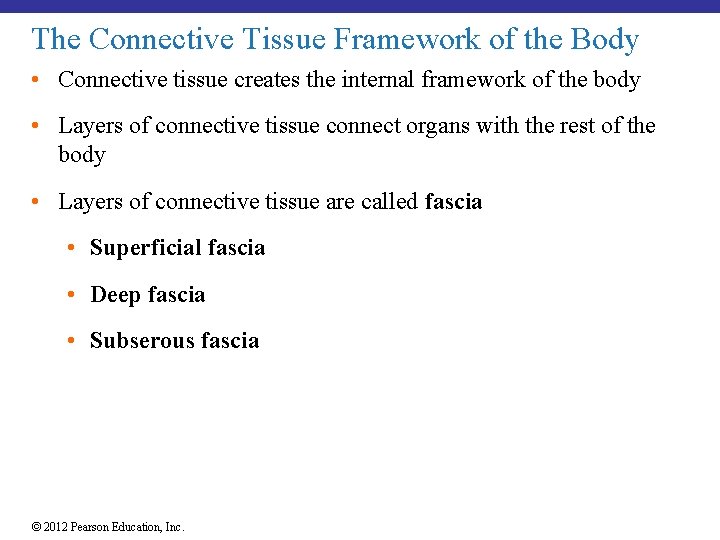
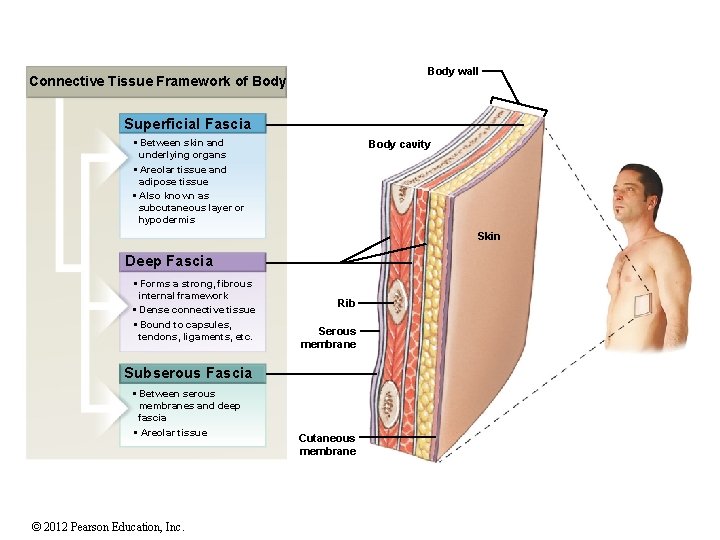
The Connective Tissue Framework of the Body • Connective tissue creates the internal framework of the body • Layers of connective tissue connect organs with the rest of the body • Layers of connective tissue are called fascia • Superficial fascia • Deep fascia • Subserous fascia © 2012 Pearson Education, Inc.
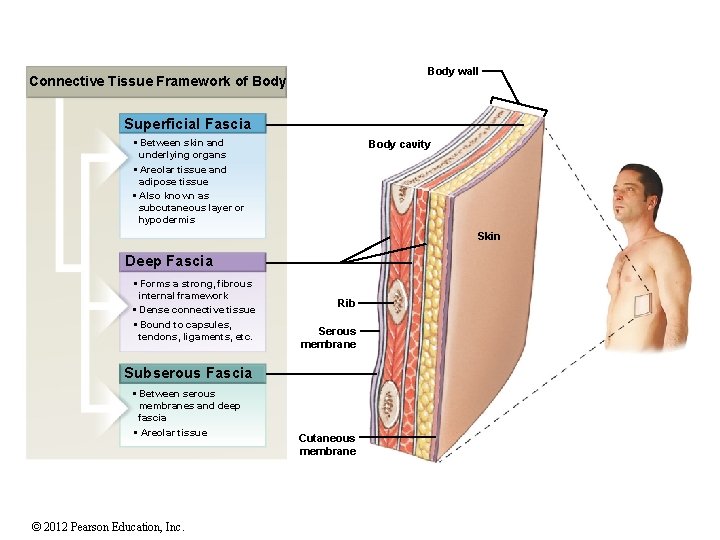
Body wall Connective Tissue Framework of Body Superficial Fascia • Between skin and underlying organs • Areolar tissue and adipose tissue • Also known as subcutaneous layer or hypodermis Body cavity Skin Deep Fascia • Forms a strong, fibrous internal framework • Dense connective tissue • Bound to capsules, tendons, ligaments, etc. Rib Serous membrane Subserous Fascia • Between serous membranes and deep fascia • Areolar tissue © 2012 Pearson Education, Inc. Cutaneous membrane
4 -6 Membranes • Physical barriers • Line or cover portions of the body • Consist of: • An epithelium • Supported by connective tissue © 2012 Pearson Education, Inc.
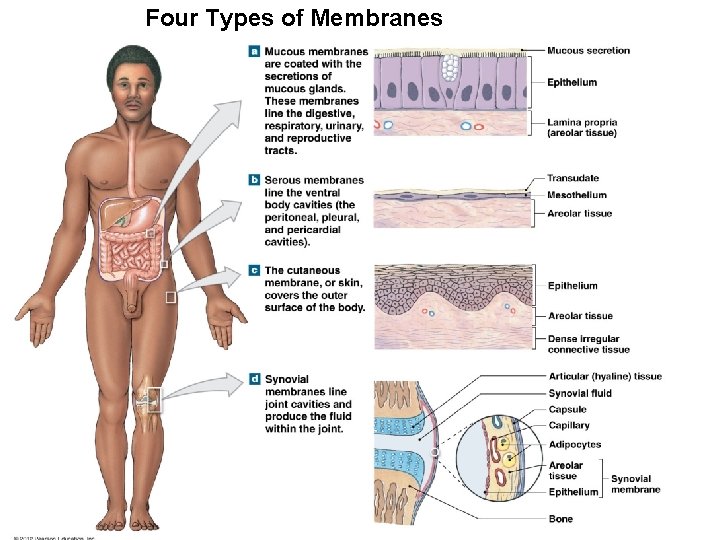
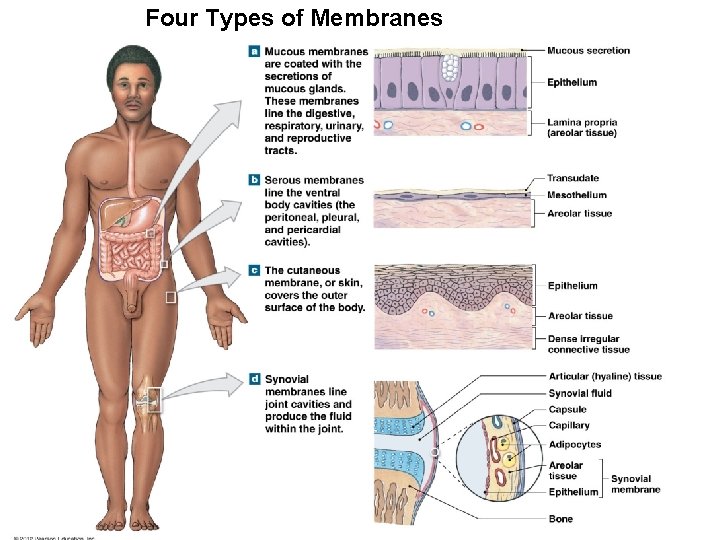
Four Types of Membranes © 2012 Pearson Education, Inc.
4 -8 Muscle Tissue is specialized for contraction Functions of muscle tissue: • body movements • heat generation • movement of material within the body Classified into three types: • Skeletal muscle • Cardiac muscle • Smooth muscle © 2012 Pearson Education, Inc.
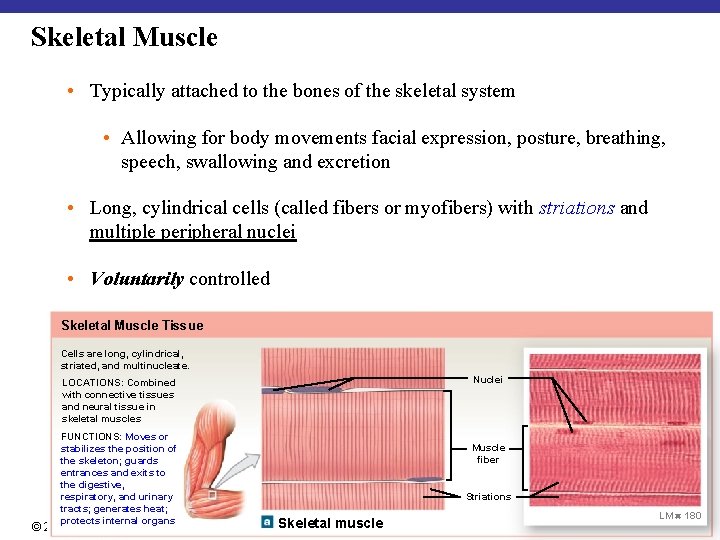
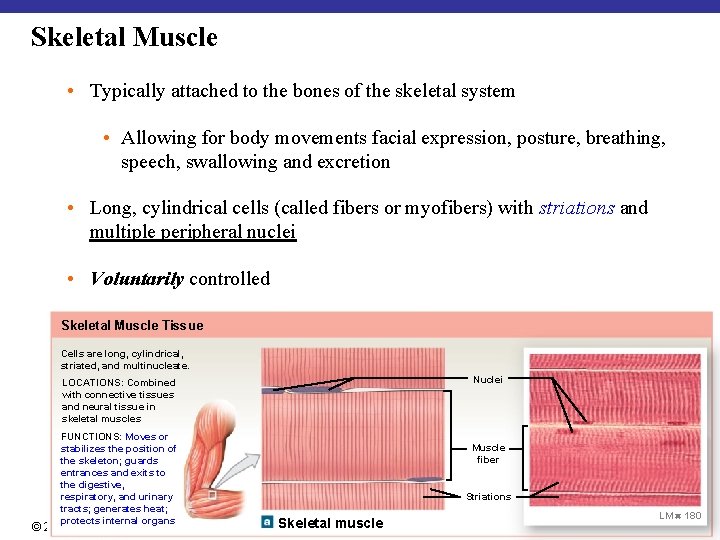
Skeletal Muscle • Typically attached to the bones of the skeletal system • Allowing for body movements facial expression, posture, breathing, speech, swallowing and excretion • Long, cylindrical cells (called fibers or myofibers) with striations and multiple peripheral nuclei • Voluntarily controlled Skeletal Muscle Tissue Cells are long, cylindrical, striated, and multinucleate. Nuclei LOCATIONS: Combined with connective tissues and neural tissue in skeletal muscles FUNCTIONS: Moves or stabilizes the position of the skeleton; guards entrances and exits to the digestive, respiratory, and urinary tracts; generates heat; protects internal organs © 2012 Pearson Education, Inc. Muscle fiber Striations Skeletal muscle LM 180
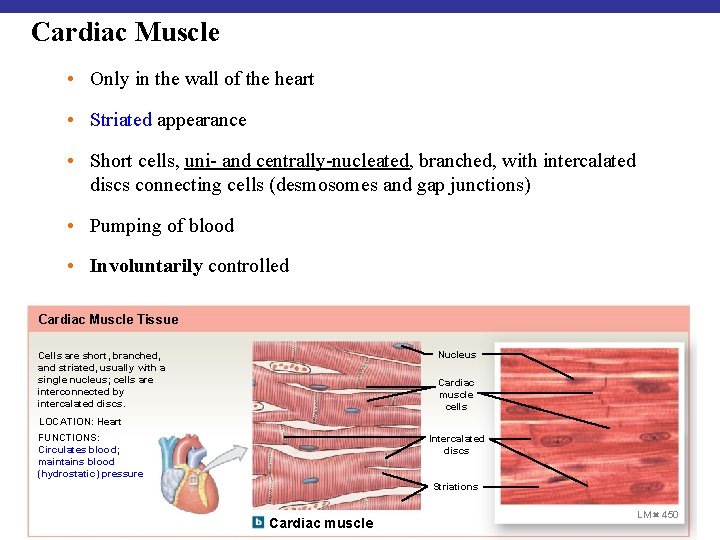
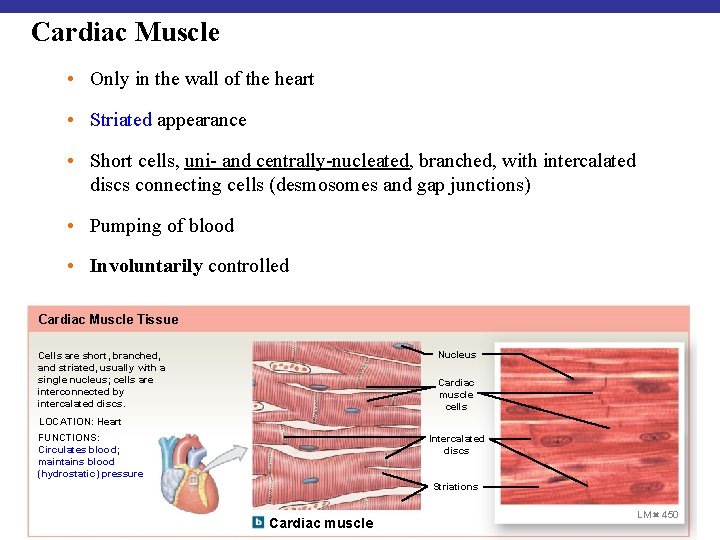
Cardiac Muscle • Only in the wall of the heart • Striated appearance • Short cells, uni- and centrally-nucleated, branched, with intercalated discs connecting cells (desmosomes and gap junctions) • Pumping of blood • Involuntarily controlled Cardiac Muscle Tissue Nucleus Cells are short, branched, and striated, usually with a single nucleus; cells are interconnected by intercalated discs. Cardiac muscle cells LOCATION: Heart FUNCTIONS: Circulates blood; maintains blood (hydrostatic) pressure Intercalated discs Striations © 2012 Pearson Education, Inc. Cardiac muscle LM 450
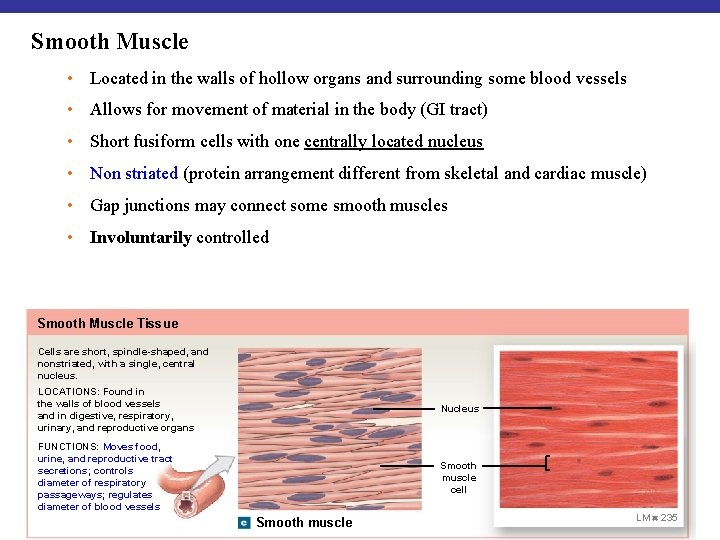
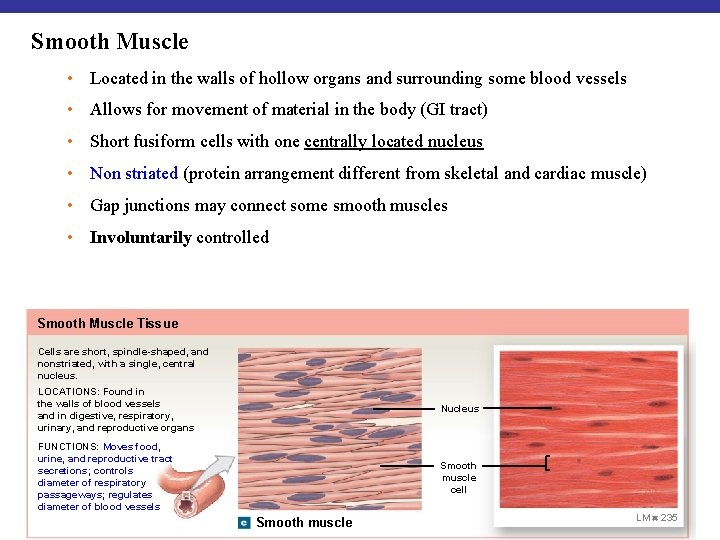
Smooth Muscle • Located in the walls of hollow organs and surrounding some blood vessels • Allows for movement of material in the body (GI tract) • Short fusiform cells with one centrally located nucleus • Non striated (protein arrangement different from skeletal and cardiac muscle) • Gap junctions may connect some smooth muscles • Involuntarily controlled Smooth Muscle Tissue Cells are short, spindle-shaped, and nonstriated, with a single, central nucleus. LOCATIONS: Found in the walls of blood vessels and in digestive, respiratory, urinary, and reproductive organs Nucleus FUNCTIONS: Moves food, urine, and reproductive tract secretions; controls diameter of respiratory passageways; regulates diameter of blood vessels Smooth muscle cell © 2012 Pearson Education, Inc. Smooth muscle LM 235
http: //imc 02. hccs. edu/Biology. Labs/AP 1/03 Tissues/03 Muscle. Images/Muscle_Quiz/ind x. html 4 -9 Neural Tissue • Also called nervous or nerve tissue • Specialized for conducting electrical impulses • Rapidly senses internal or external environment • Processes information and controls responses • Neural tissue is concentrated in the central nervous system • Brain • Spinal cord • Also in peripheral nervous system © 2012 Pearson Education, Inc.
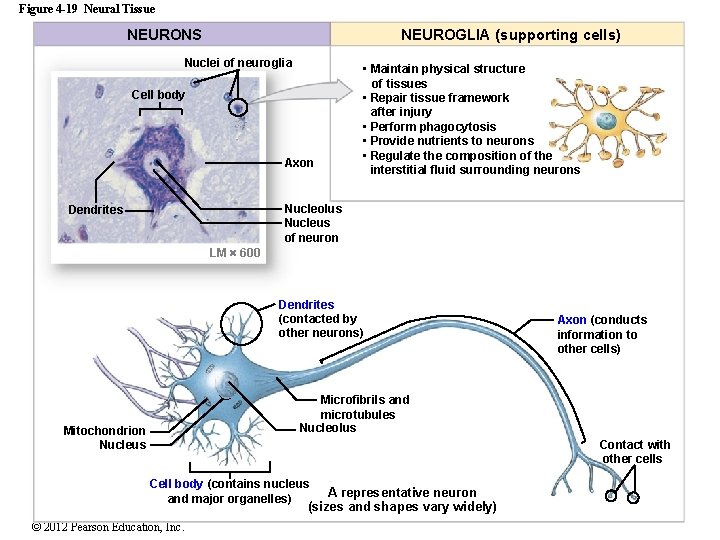
Two Types of Neural Cells 1. Neurons • Nerve cells • Perform electrical communication 2. Neuroglia • Supporting cells • Smaller, more numerous • Repair and supply nutrients to neurons © 2012 Pearson Education, Inc.
Cell Parts of a Neuron • Cell body • Contains the nucleus and nucleolus • Dendrites • Short branches extending from the cell body • Receive incoming signals • Axon (nerve fiber) • Long, thin extension of the cell body • Carries outgoing electrical signals to their destination © 2012 Pearson Education, Inc.
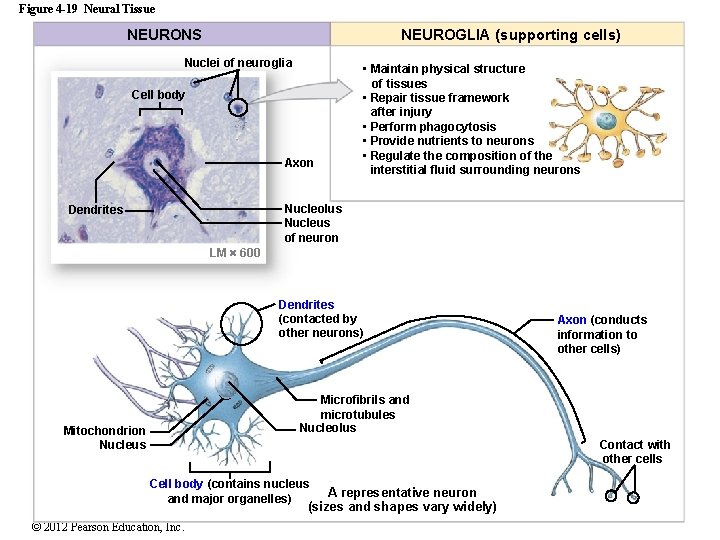
Figure 4 -19 Neural Tissue NEURONS NEUROGLIA (supporting cells) Nuclei of neuroglia Cell body Axon • Maintain physical structure of tissues • Repair tissue framework after injury • Perform phagocytosis • Provide nutrients to neurons • Regulate the composition of the interstitial fluid surrounding neurons Nucleolus Nucleus of neuron Dendrites LM 600 Dendrites (contacted by other neurons) Axon (conducts information to other cells) Microfibrils and microtubules Nucleolus Mitochondrion Nucleus Contact with other cells Cell body (contains nucleus and major organelles) A representative neuron (sizes and shapes vary widely) © 2012 Pearson Education, Inc.
http: //imc 02. hccs. edu/Biology. Labs/AP 1/03 Tissues/03 Nervous. Images/Nervous_Quiz/index. ht ml Tissue Repair • Replacement of dead, worn-out or damaged cells • Typically involves the generation of new cells • The four tissue types vary in their ability to regenerate and repair. • Ex. Epithelial tissue regeneration is good, nervous tissue regeneration is poor Fibrosis: replacement of damaged cells with scar tissue (composed mostly of collagen fibers produced by fibroblasts), holds the organ together but normal function is not restored – muscle injuries, scarring of lung tissue in TB, severe cuts and burns of the skin © 2012 Pearson Education, Inc.
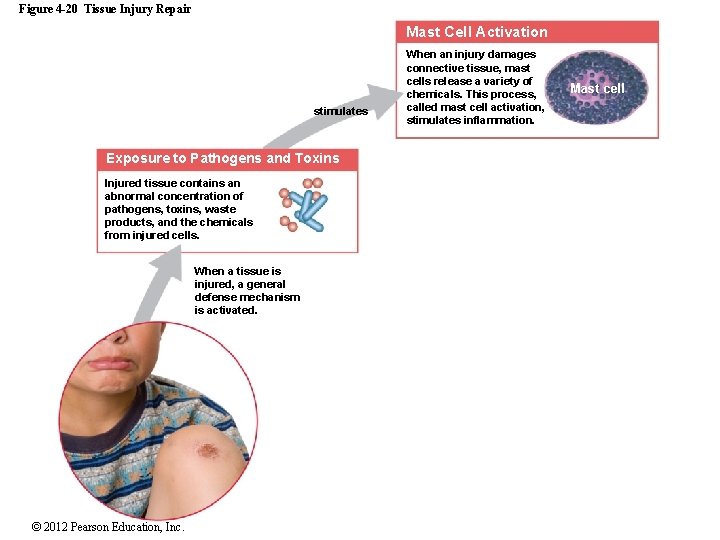
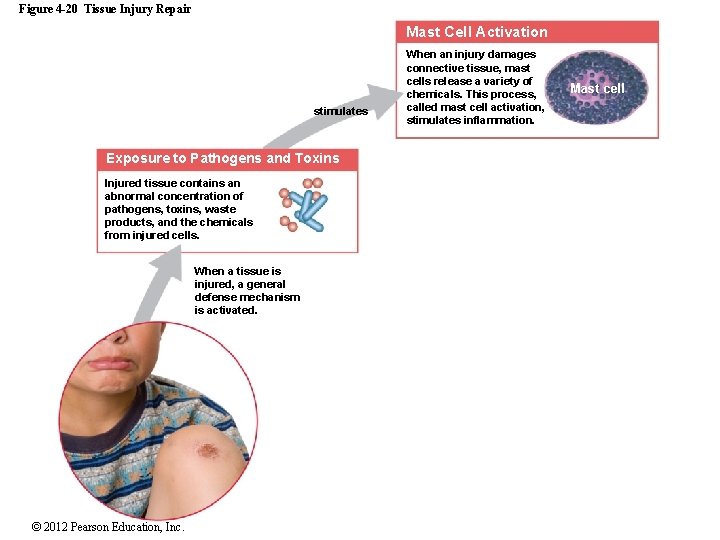
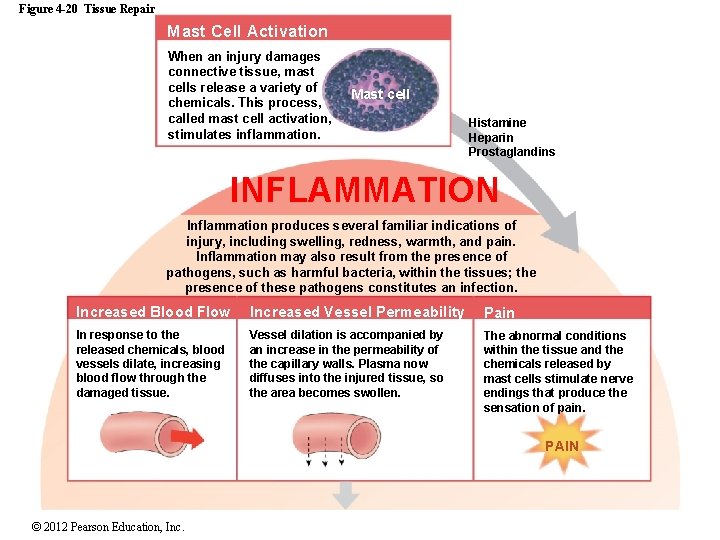
Figure 4 -20 Tissue Injury Repair Mast Cell Activation stimulates Exposure to Pathogens and Toxins Injured tissue contains an abnormal concentration of pathogens, toxins, waste products, and the chemicals from injured cells. When a tissue is injured, a general defense mechanism is activated. © 2012 Pearson Education, Inc. When an injury damages connective tissue, mast cells release a variety of chemicals. This process, called mast cell activation, stimulates inflammation. Mast cell
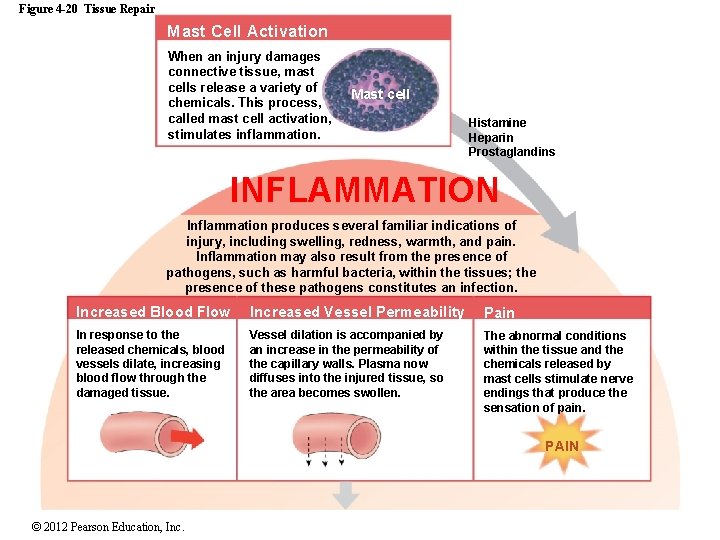
Figure 4 -20 Tissue Repair Mast Cell Activation When an injury damages connective tissue, mast cells release a variety of chemicals. This process, called mast cell activation, stimulates inflammation. Mast cell Histamine Heparin Prostaglandins INFLAMMATION Inflammation produces several familiar indications of injury, including swelling, redness, warmth, and pain. Inflammation may also result from the presence of pathogens, such as harmful bacteria, within the tissues; the presence of these pathogens constitutes an infection. Increased Blood Flow Increased Vessel Permeability Pain In response to the released chemicals, blood vessels dilate, increasing blood flow through the damaged tissue. Vessel dilation is accompanied by an increase in the permeability of the capillary walls. Plasma now diffuses into the injured tissue, so the area becomes swollen. The abnormal conditions within the tissue and the chemicals released by mast cells stimulate nerve endings that produce the sensation of pain. PAIN © 2012 Pearson Education, Inc.
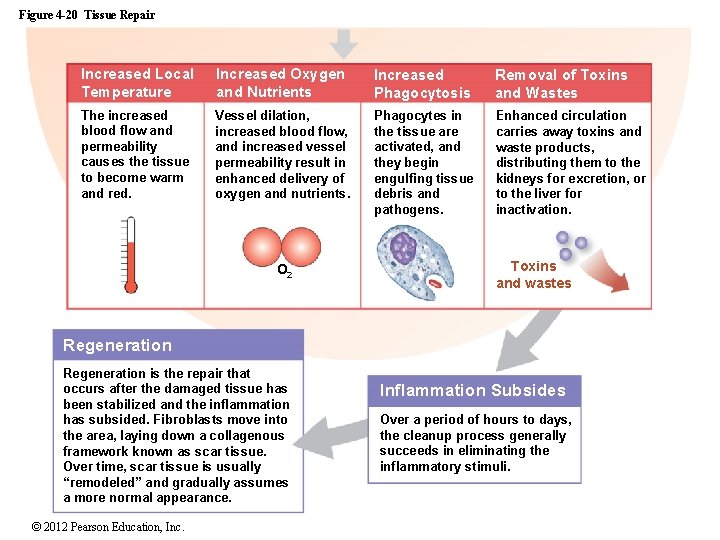
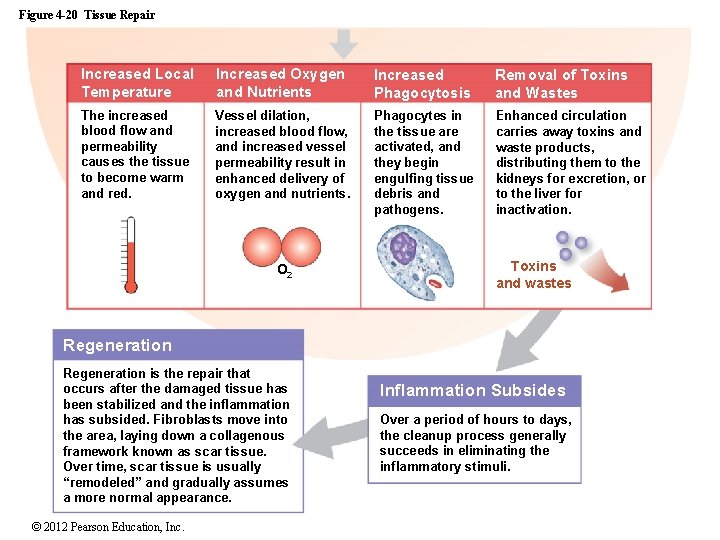
Figure 4 -20 Tissue Repair Increased Local Temperature Increased Oxygen and Nutrients Increased Phagocytosis Removal of Toxins and Wastes The increased blood flow and permeability causes the tissue to become warm and red. Vessel dilation, increased blood flow, and increased vessel permeability result in enhanced delivery of oxygen and nutrients. Phagocytes in the tissue are activated, and they begin engulfing tissue debris and pathogens. Enhanced circulation carries away toxins and waste products, distributing them to the kidneys for excretion, or to the liver for inactivation. O 2 Toxins and wastes Regeneration is the repair that occurs after the damaged tissue has been stabilized and the inflammation has subsided. Fibroblasts move into the area, laying down a collagenous framework known as scar tissue. Over time, scar tissue is usually “remodeled” and gradually assumes a more normal appearance. © 2012 Pearson Education, Inc. Inflammation Subsides Over a period of hours to days, the cleanup process generally succeeds in eliminating the inflammatory stimuli.
4 -11 Aging and Tissue Effects of Aging • Chemical and structural tissue changes • Thinning epithelia and connective tissues • Increased bruising and bone brittleness • Joint pain and broken bones • Cardiovascular disease • Mental deterioration • Regeneration slows down or stops © 2012 Pearson Education, Inc.
Aging and Cancer Incidence • Cancer rates increase with age • 25% of all people in the United States develop cancer • Cancer is the #2 cause of death in the United States • Environmental chemicals and cigarette smoke cause cancer © 2012 Pearson Education, Inc.
 Point by point arrangement
Point by point arrangement Chapter 4 the tissue level of organization
Chapter 4 the tissue level of organization Porifera level of organization
Porifera level of organization Chapter 4 the tissue level of organization
Chapter 4 the tissue level of organization Chapter 4 the tissue level of organization
Chapter 4 the tissue level of organization Power traiangle
Power traiangle Power bi power point
Power bi power point Point point power
Point point power Jaringan epitel dapat ditemukan di
Jaringan epitel dapat ditemukan di Process organization in computer organization
Process organization in computer organization Ecology pyramid of numbers
Ecology pyramid of numbers Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Lp html
Lp html Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Gấu đi như thế nào
Gấu đi như thế nào Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Chúa yêu trần thế
Chúa yêu trần thế Môn thể thao bắt đầu bằng chữ f
Môn thể thao bắt đầu bằng chữ f Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công thức tính độ biến thiên đông lượng
Công thức tính độ biến thiên đông lượng Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Phép trừ bù
Phép trừ bù độ dài liên kết
độ dài liên kết Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Thể thơ truyền thống
Thể thơ truyền thống Quá trình desamine hóa có thể tạo ra
Quá trình desamine hóa có thể tạo ra Một số thể thơ truyền thống
Một số thể thơ truyền thống Cái miệng nó xinh thế chỉ nói điều hay thôi
Cái miệng nó xinh thế chỉ nói điều hay thôi Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Thế nào là giọng cùng tên? *
Thế nào là giọng cùng tên? * Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Fecboak
Fecboak Thẻ vin
Thẻ vin đại từ thay thế
đại từ thay thế điện thế nghỉ
điện thế nghỉ Tư thế ngồi viết
Tư thế ngồi viết Diễn thế sinh thái là
Diễn thế sinh thái là Dot
Dot Bảng số nguyên tố lớn hơn 1000
Bảng số nguyên tố lớn hơn 1000 Tư thế ngồi viết
Tư thế ngồi viết Lời thề hippocrates
Lời thề hippocrates Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan ưu thế lai là gì
ưu thế lai là gì Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ Khi nào hổ con có thể sống độc lập
Khi nào hổ con có thể sống độc lập Sơ đồ cơ thể người
Sơ đồ cơ thể người Từ ngữ thể hiện lòng nhân hậu
Từ ngữ thể hiện lòng nhân hậu Thế nào là mạng điện lắp đặt kiểu nổi
Thế nào là mạng điện lắp đặt kiểu nổi Organization level
Organization level Organization-level diagnostic model
Organization-level diagnostic model Middle level management examples
Middle level management examples What is the least complex level of organization
What is the least complex level of organization Levels of organization ecology
Levels of organization ecology Level of organization organ system
Level of organization organ system Levels of data management
Levels of data management Smallest to largest level of organization
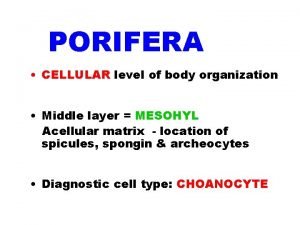
Smallest to largest level of organization Porifera cellular organization
Porifera cellular organization What is an mis
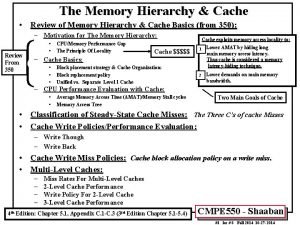
What is an mis Three level cache organization
Three level cache organization What level of organization
What level of organization Top level management
Top level management Different levels of ecological organization
Different levels of ecological organization What is this
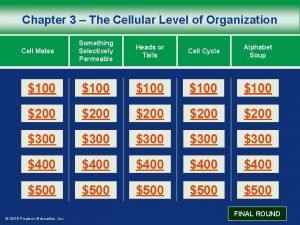
What is this Chapter 3 the cellular level of organization
Chapter 3 the cellular level of organization Chemical level of organization
Chemical level of organization The chemical level of organization chapter 2
The chemical level of organization chapter 2 Principles of ethical power for organization
Principles of ethical power for organization Power and politics organization theory
Power and politics organization theory Floating point representation in computer organization
Floating point representation in computer organization Molecular level vs cellular level
Molecular level vs cellular level Isis protocol
Isis protocol Significance level vs confidence level
Significance level vs confidence level Isis level 1 vs level 2
Isis level 1 vs level 2