1 Managed LongTerm Services and Supports The Potential



























- Slides: 93
1 Managed Long-Term Services and Supports: The Potential for Medicaid Managed Care to Integrate Acute and Long-Term Care Sponsored by
The audio and slide presentation will be delivered directly to your computer • Speakers or headphones are required to hear the audio portion of the webinar. • If you do not hear any audio now, check your computer’s speaker settings and volume. • If you need an alternate method of accessing audio, please submit a question through the Q&A pod. 2

Technical Assistance • Live technical assistance: • Call Adobe Connect at (800) 422 -3623 • Refer to the ‘Technical Assistance’ box in the bottom left corner for tips to resolve common technical difficulties. • Please turn off your pop-up blocker in order to take a survey 3
Questions may be submitted at any time during the presentation 4 To submit a question: • Click in the Q&A box on the left side of your screen • Type your question into the dialog box and click the Send button

Webinar Speakers

6 Howard B. Degenholtz University of Pittsburgh Larry Atkins LTQA
7 Camille Dobson Kevin Hancock National Association of States Pennsylvania Department United for Aging and Disabilities of Human Services (NASUAD) Patti Killingsworth Bureau of Tenn. Care

8 Merrill Friedman Anthem Leigh Davison Anthem Paul Saucier IBM Watson Health
Questions may be submitted at any time during the presentation 9 To submit a question: • Click in the Q&A box on the left side of your screen • Type your question into the dialog box and click the Send button
Introduction and Agenda Howard Degenholtz and Larry Atkins
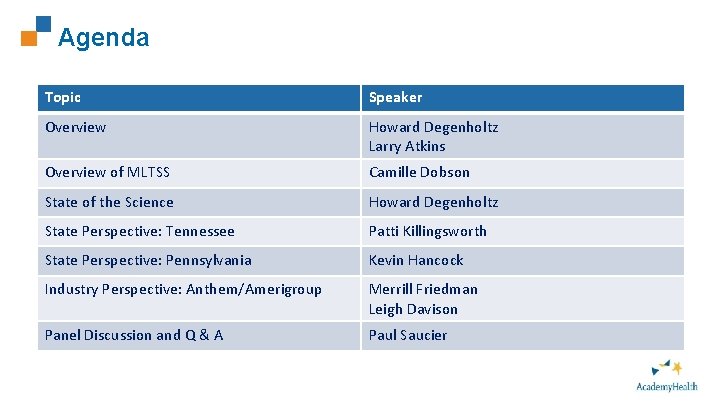
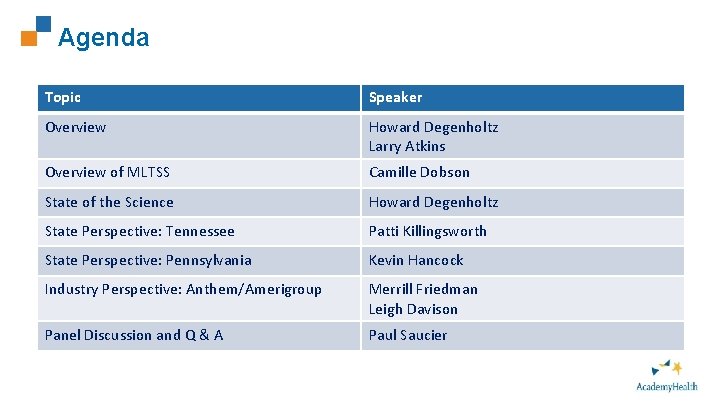
Agenda 11 Topic Speaker Overview Howard Degenholtz Larry Atkins Overview of MLTSS Camille Dobson State of the Science Howard Degenholtz State Perspective: Tennessee Patti Killingsworth State Perspective: Pennsylvania Kevin Hancock Industry Perspective: Anthem/Amerigroup Merrill Friedman Leigh Davison Panel Discussion and Q & A Paul Saucier

Overview of MLTSS Camille Dobson
NASUAD: Who We Are ■ State Association: 56 members, representing state and territorial agencies on aging and disabilities ■ Our Mission: To design, improve, and sustain state systems delivering home and community based services and supports for people who are older or have a disability, and their caregivers. Page 13

NASUAD: Who We Are ■ Our members include: State Unit on Aging directors Medicaid Long-term Services and Supports directors Developmental Disabilities Services directors ■ 11 staff manage Federal policy (congressional and executive branch), administer 6 Federal and Foundation grants, and publish Medicaid Integration Tracker and Friday Update ■ Convener of the National HCBS Conference – largest conference of its kind with over 1, 400 attendees, 5 plenaries, 5 all-day preconference intensives and 110 sessions over 3 ½ days Page 14

What is Managed Long-Term Services and Supports (MLTSS)? ■ MLTSS is the delivery of long term services and supports (state plan, waiver or both) through capitated Medicaid managed care plans ■ Plans can be a managed care organization, pre-paid inpatient health plan, or a pre-paid ambulatory health plan (depending on scope of benefits provided) ■ In many cases, plans are covering medical services as well, which provides a comprehensive delivery system for beneficiaries Page 15
Why MLTSS? ■ Accountability rests with a single entity Financial risk for health plan provides opportunity to incentivize/penalize performance Plans can integrate siloed streams of care (primary/behavioral/long term care) more effectively ■ Administrative simplification for state Eliminates need to contract with and monitor hundreds/thousands of individual providers Managed care plans take on claims payment, member management, utilization review, etc. Page 16
Why MLTSS? ■ Budget predictability Capitation payments greatly minimize unanticipated spending Can more accurately project costs ■ Innovation and Quality MCOs can deliver services more flexibly than states They bring best practices from other states/product lines Demonstrated improvement in quality outcomes (HEDIS) over FFS Page 17
Why MLTSS? ■ Consumer becomes the center, not their services LTSS interventions can lower acute care costs ■ Shift focus of care to community settings Most consumers express preference for community-based services Health plans may be able to effectuate transfers from institutions to community more easily Page 18
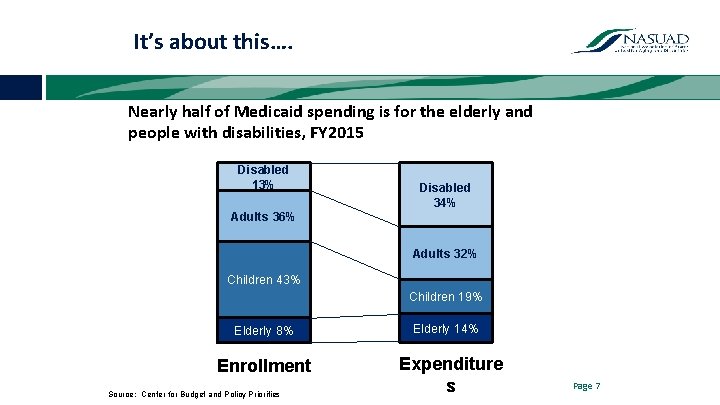
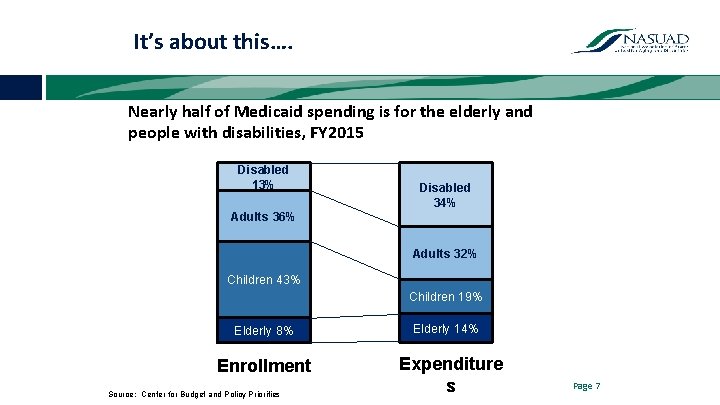
It’s about this…. Nearly half of Medicaid spending is for the elderly and people with disabilities, FY 2015 Disabled 13% Disabled 34% Adults 36% Adults 32% Children 43% Children 19% Elderly 8% Enrollment Source: Center for Budget and Policy Priorities Elderly 14% Expenditure s Page 7
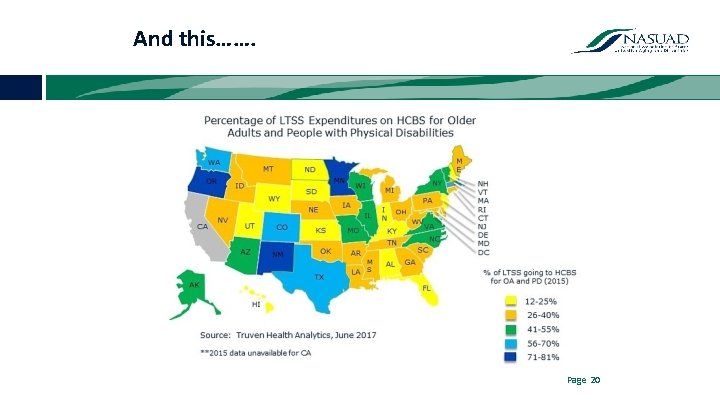
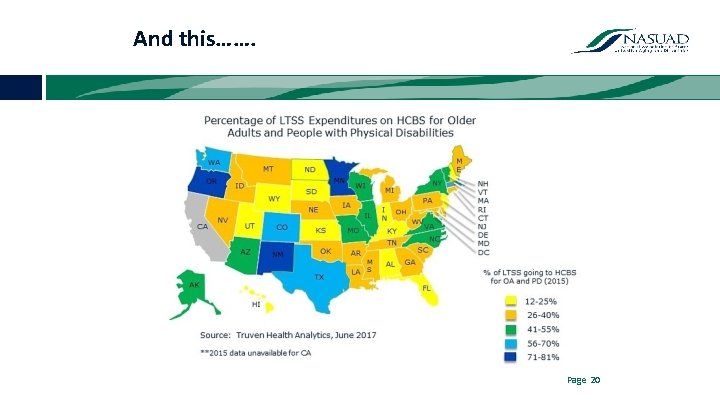
And this……. Page 20
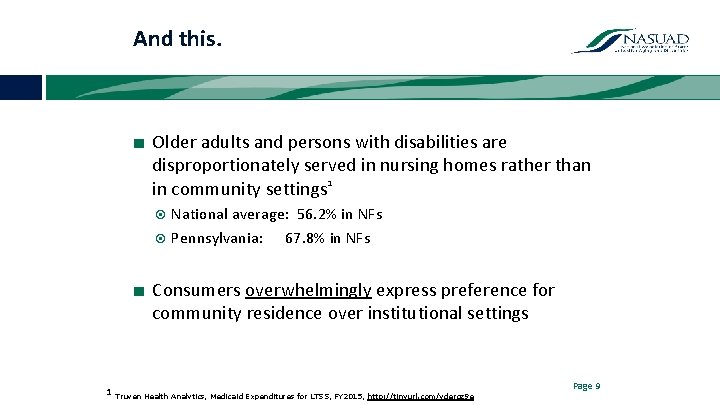
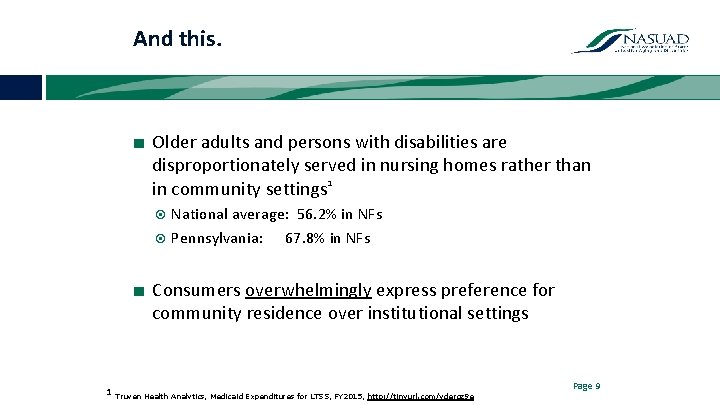
And this. ■ Older adults and persons with disabilities are disproportionately served in nursing homes rather than in community settings 1 National average: 56. 2% in NFs Pennsylvania: 67. 8% in NFs ■ Consumers overwhelmingly express preference for community residence over institutional settings 1 Truven Health Analytics, Medicaid Expenditures for LTSS, FY 2015, http: //tinyurl. com/ydergz 9 e Page 9
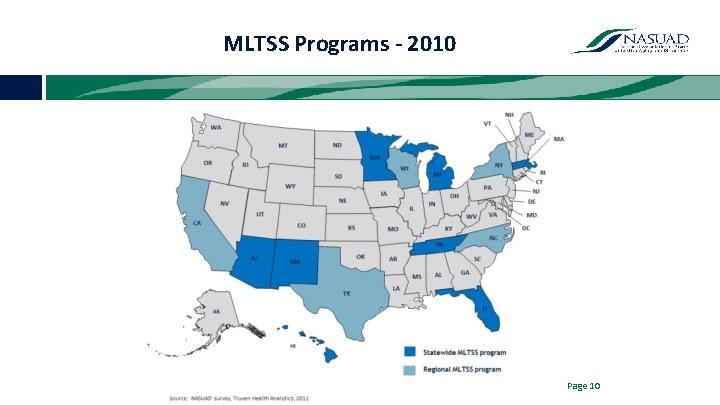
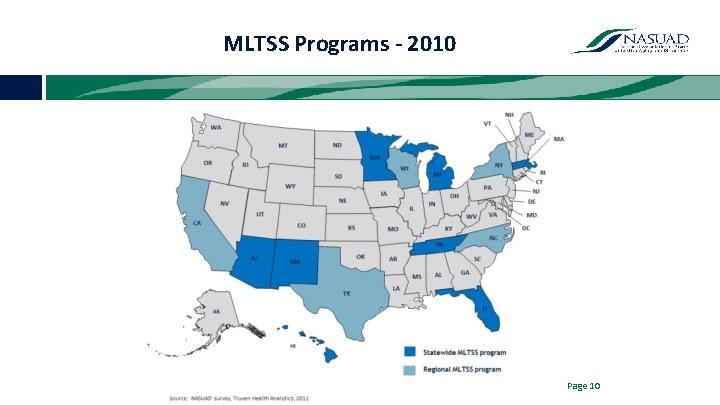
MLTSS Programs - 2010 Page 10
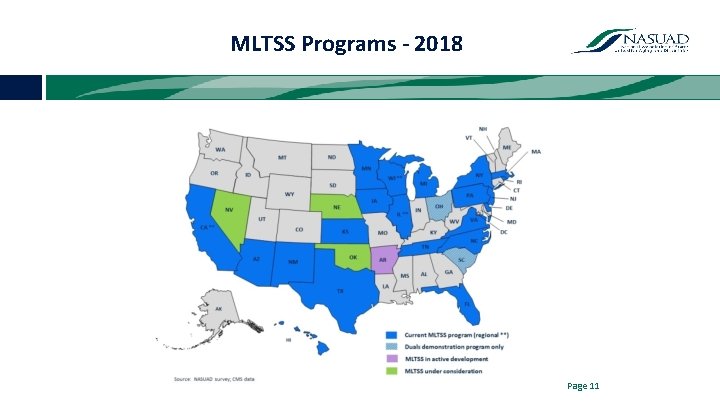
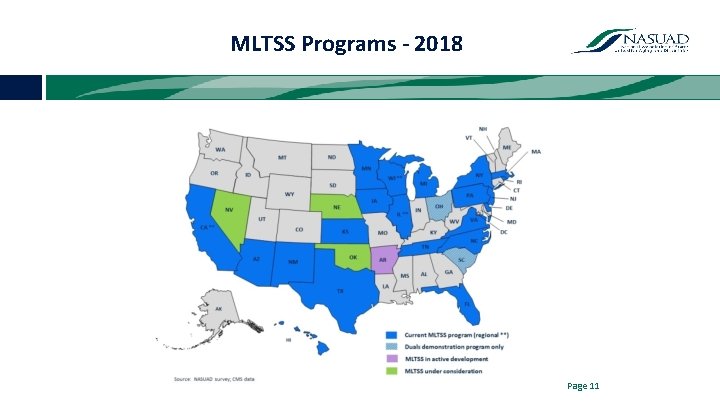
MLTSS Programs - 2018 Page 11
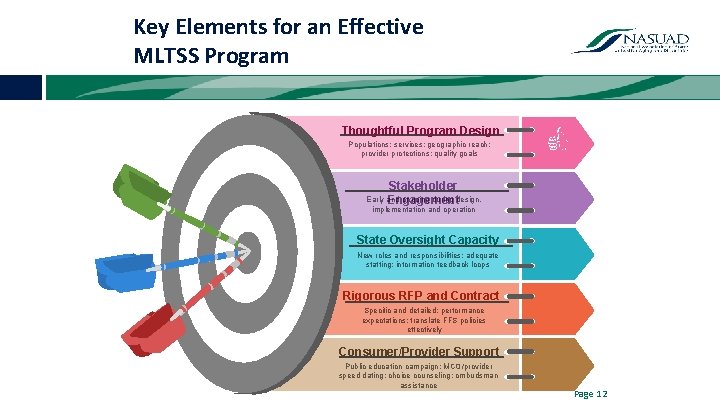
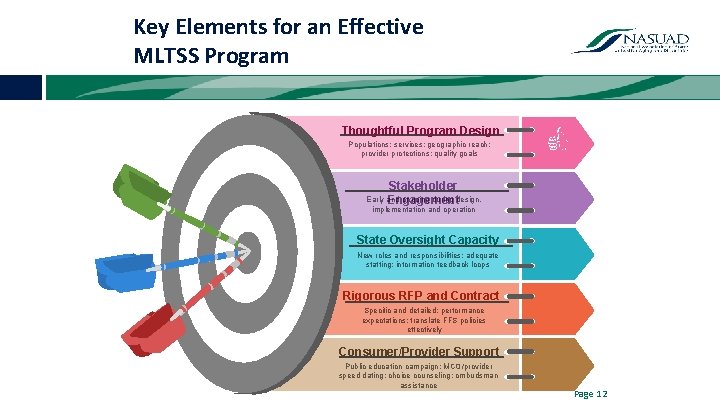
Key Elements for an Effective MLTSS Program Thoughtful Program Design Populations; services; geographic reach; provider protections; quality goals Stakeholder Early and ongoing during design, Engagement implementation and operation State Oversight Capacity New roles and responsibilities; adequate staffing; information feedback loops Rigorous RFP and Contract Specific and detailed; performance expectations; translate FFS policies effectively Consumer/Provider Support Public education campaign; MCO/provider speed dating; choice counseling; ombudsman assistance Page 12
Trends for 2018 and beyond ■ MLTSS continues to be the biggest trend/opportunity for states to address accountability, cost efficiency and better outcomes for consumers ■ Expansion of existing programs either statewide or beyond dual eligibles ■ Inclusion of LTSS services for individuals with intellectual/developmental disabilities in MLTSS programs Currently only IA, KS, and TN use commercial MCOs to deliver these services Page 25
Trends for 2018 and beyond ■ Focus on quality ■ States without managed care capacity or unwillingness to implement or expand acute care managed care looking at partial-risk alternatives (ACOs, PASSE) ■ States also looking at expanding pay-forperformance/value-based purchasing from NFs and other large providers to HCBS providers ■ More and more involvement by MCOs in states’ Olmstead plans, as well as housing and employment first initiatives Page 26
Final Thoughts ■ Quality and cost are inextricably linked. Improved quality outcomes will reduce costs ■ Managed care is a set of tools and principles that can help improve coordination, quality and cost-effectiveness of care for the most complex populations It is up to the state to wield that tool in the most effective way ■ Implementing managed care well requires a significant investment in the State’s capacity to ‘manage’ managed care plans It requires different skill sets and an accountability mindset Page 15

Final Thoughts ■ It takes time to implement managed care well. Moving too quickly will undermine the success of the program State should continue to get stakeholder feedback to make continuous improvements to the program ■ It takes time to realize savings from managed care. Focus on short-term savings imperils long-term sustainability of the program Page 16

State of the Science Howard B. Degenholtz
Examining the Evidence • MLTSS authorities have implications for the degree of financial integration Alignment and care coordination • Evidence from peer review and ‘grey’ literature • National Evaluations of FAI Demonstrations and 1115 Waivers • Summary 30
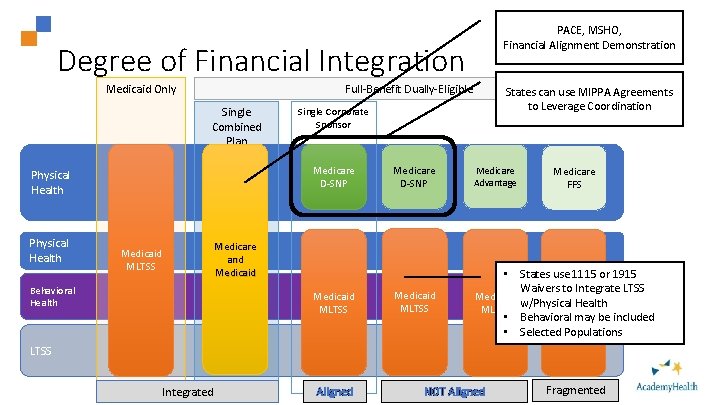
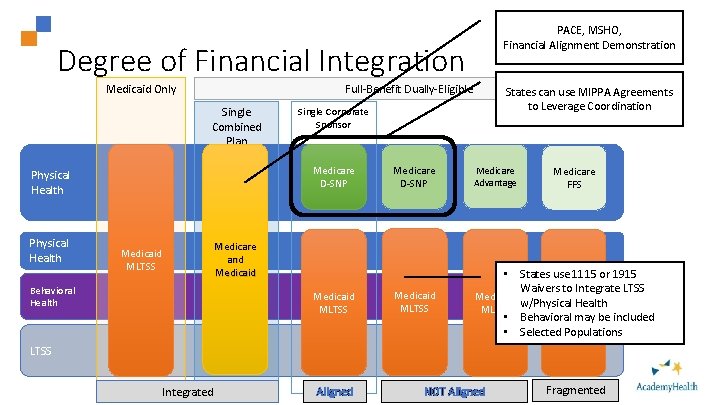
PACE, MSHO, 31 Financial Alignment Demonstration Degree of Financial Integration Full-Benefit Dually-Eligible Medicaid Only Single Combined Plan Physical Health Single Corporate Sponsor Medicare D-SNP Physical Health Medicaid MLTSS Behavioral Health States can use MIPPA Agreements to Leverage Coordination Medicare D-SNP Medicare Advantage Medicaid MLTSS • States use 1115 or 1915 Waivers to Integrate LTSS Medicaid w/Physical Health MLTSS • Behavioral may be included • Selected Populations Medicare and Medicaid MLTSS Medicare FFS LTSS Integrated Aligned NOT Aligned Fragmented
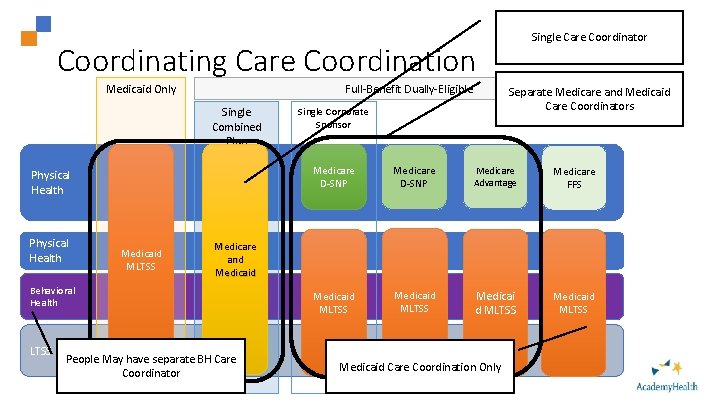
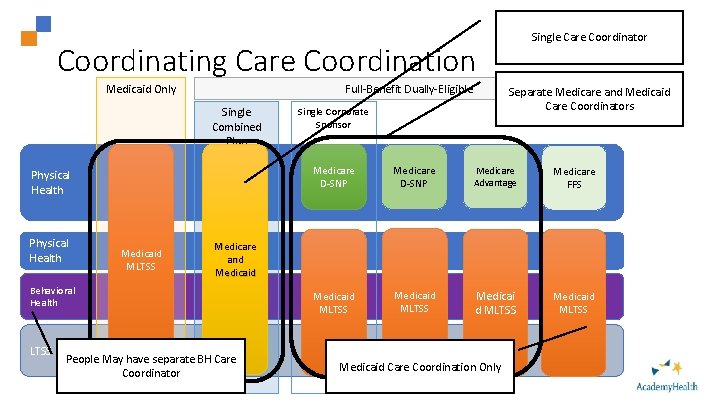
Single Care Coordinator Coordinating Care Coordination Full-Benefit Dually-Eligible Medicaid Only Single Combined Plan Physical Health Medicaid MLTSS Separate Medicare and Medicaid Care Coordinators Single Corporate Sponsor Medicare D-SNP Medicare Advantage Medicare FFS Medicaid MLTSS Medicaid MLTSS Medicare and Medicaid Behavioral Health People May have separate BH Care Coordinator 32 Medicaid Care Coordination Only
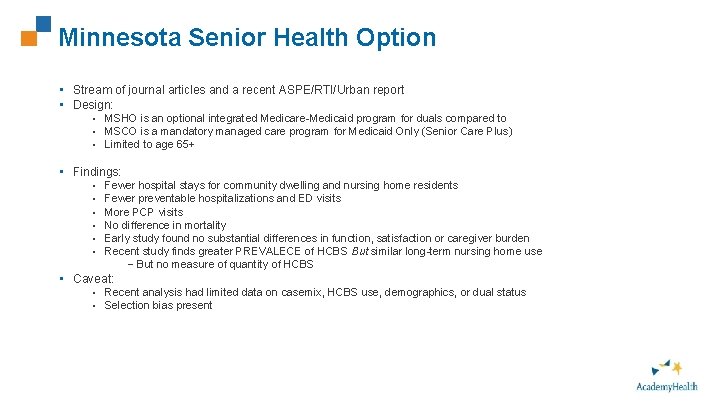
Minnesota Senior Health Option • Stream of journal articles and a recent ASPE/RTI/Urban report • Design: • MSHO is an optional integrated Medicare-Medicaid program for duals compared to • MSCO is a mandatory managed care program for Medicaid Only (Senior Care Plus) • Limited to age 65+ • Findings: • • • Fewer hospital stays for community dwelling and nursing home residents Fewer preventable hospitalizations and ED visits More PCP visits No difference in mortality Early study found no substantial differences in function, satisfaction or caregiver burden Recent study finds greater PREVALECE of HCBS But similar long-term nursing home use – But no measure of quantity of HCBS • Caveat: • Recent analysis had limited data on casemix, HCBS use, demographics, or dual status • Selection bias present 33
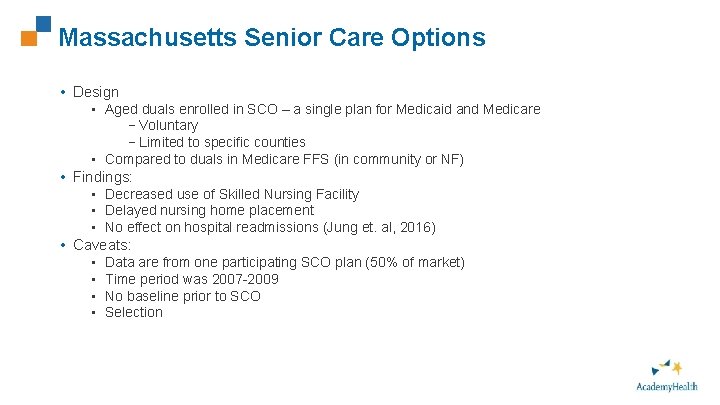
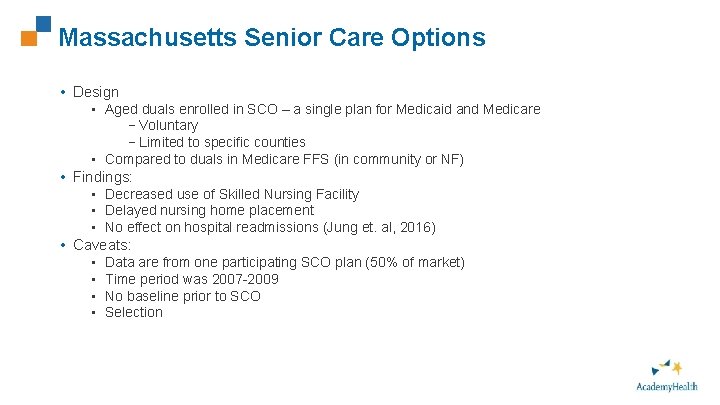
Massachusetts Senior Care Options • Design • Aged duals enrolled in SCO – a single plan for Medicaid and Medicare –Voluntary –Limited to specific counties • Compared to duals in Medicare FFS (in community or NF) • Findings: • Decreased use of Skilled Nursing Facility • Delayed nursing home placement • No effect on hospital readmissions (Jung et. al, 2016) • Caveats: • Data are from one participating SCO plan (50% of market) • Time period was 2007 -2009 • No baseline prior to SCO • Selection 34
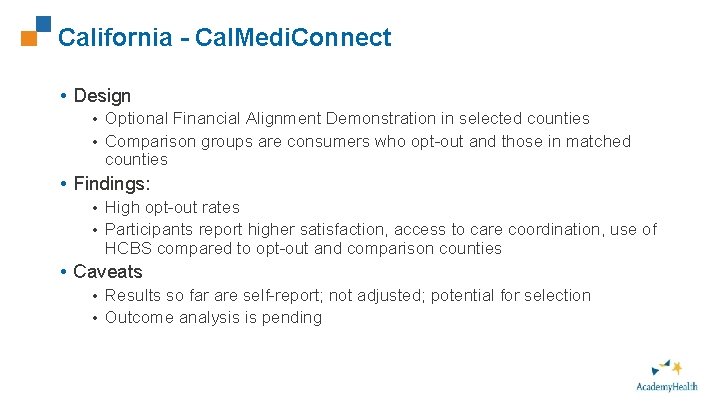
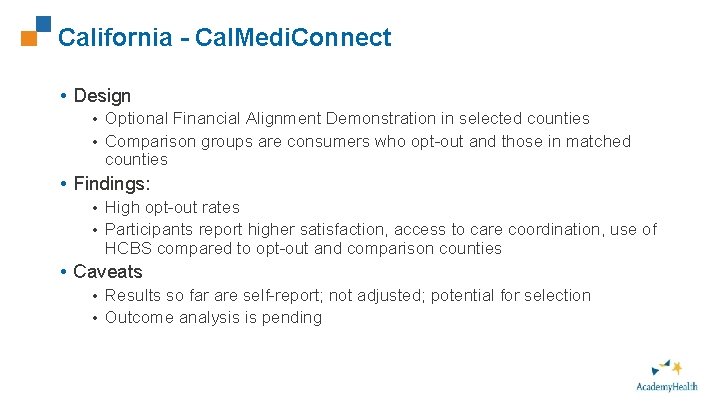
California - Cal. Medi. Connect 35 • Design • Optional Financial Alignment Demonstration in selected counties • Comparison groups are consumers who opt-out and those in matched counties • Findings: • High opt-out rates • Participants report higher satisfaction, access to care coordination, use of HCBS compared to opt-out and comparison counties • Caveats • Results so far are self-report; not adjusted; potential for selection • Outcome analysis is pending
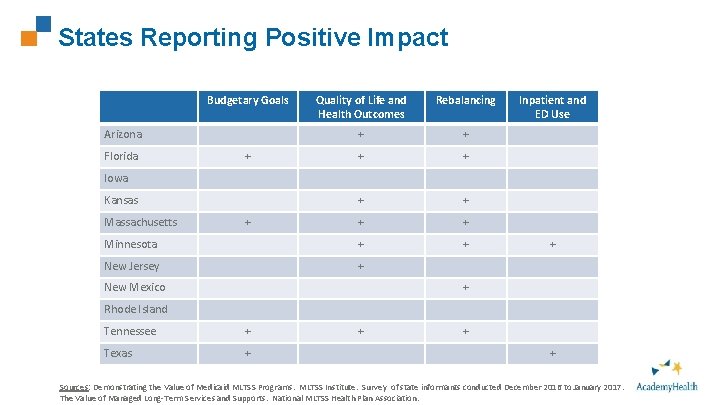
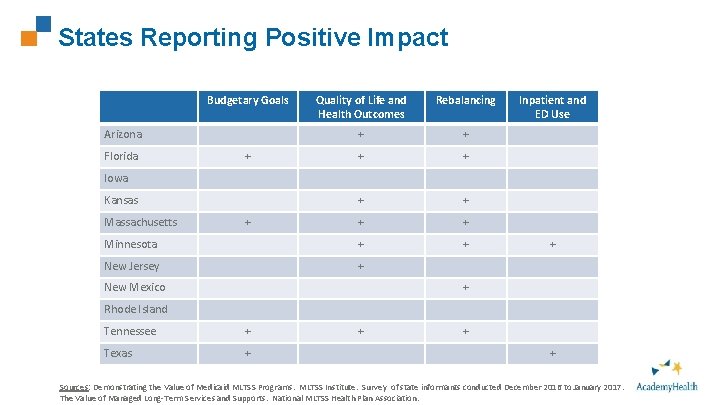
States Reporting Positive Impact Budgetary Goals 36 Quality of Life and Health Outcomes Rebalancing + + + + Minnesota + + New Jersey + Arizona Florida + Inpatient and ED Use Iowa Kansas Massachusetts + New Mexico + + Rhode Island Tennessee + Texas + + Sources: Demonstrating the Value of Medicaid MLTSS Programs. MLTSS Institute. Survey of state informants conducted December 2016 to January 2017. The Value of Managed Long-Term Services and Supports. National MLTSS Health Plan Association.
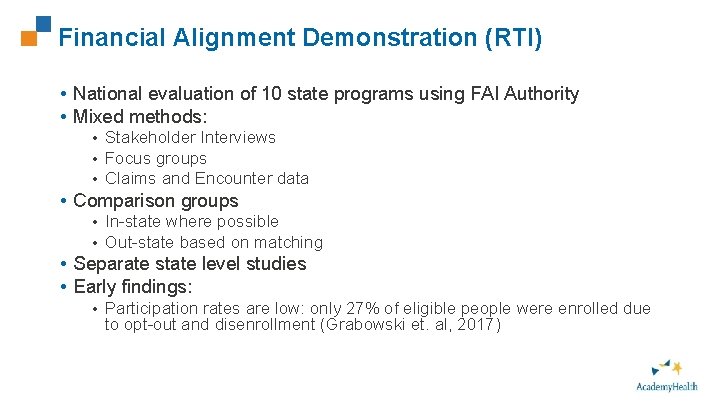
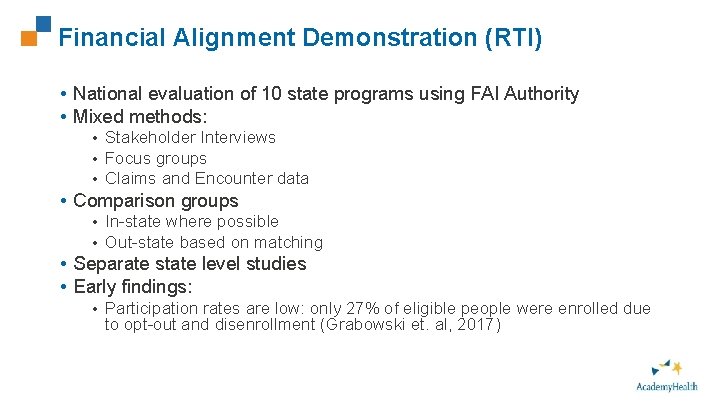
Financial Alignment Demonstration (RTI) • National evaluation of 10 state programs using FAI Authority • Mixed methods: • Stakeholder Interviews • Focus groups • Claims and Encounter data • Comparison groups • In-state where possible • Out-state based on matching • Separate state level studies • Early findings: • Participation rates are low: only 27% of eligible people were enrolled due to opt-out and disenrollment (Grabowski et. al, 2017) 37
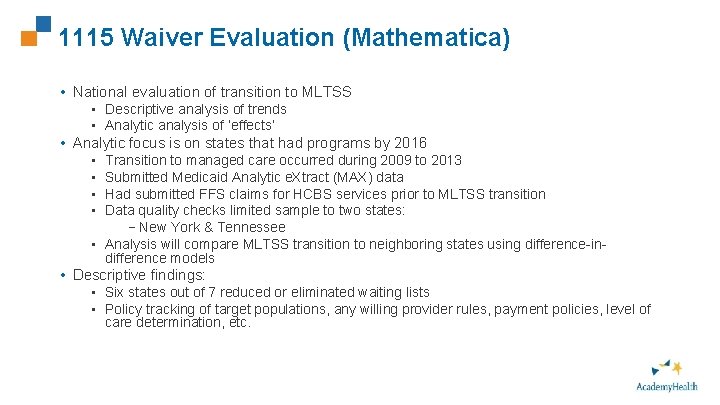
1115 Waiver Evaluation (Mathematica) • National evaluation of transition to MLTSS • Descriptive analysis of trends • Analytic analysis of ‘effects’ • Analytic focus is on states that had programs by 2016 Transition to managed care occurred during 2009 to 2013 Submitted Medicaid Analytic e. Xtract (MAX) data Had submitted FFS claims for HCBS services prior to MLTSS transition Data quality checks limited sample to two states: –New York & Tennessee • Analysis will compare MLTSS transition to neighboring states using difference-indifference models • • • Descriptive findings: • Six states out of 7 reduced or eliminated waiting lists • Policy tracking of target populations, any willing provider rules, payment policies, level of care determination, etc. 38
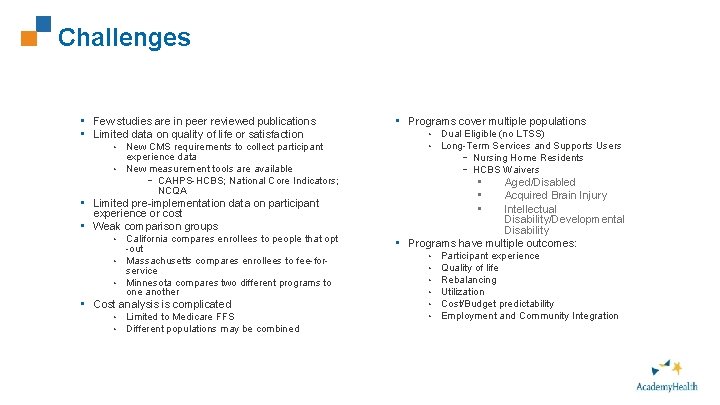
Challenges • Few studies are in peer reviewed publications • Limited data on quality of life or satisfaction New CMS requirements to collect participant experience data • New measurement tools are available – CAHPS-HCBS; National Core Indicators; NCQA • • Limited pre-implementation data on participant experience or cost • Weak comparison groups California compares enrollees to people that opt -out • Massachusetts compares enrollees to fee-forservice • Minnesota compares two different programs to one another • • Cost analysis is complicated • • Limited to Medicare FFS Different populations may be combined 39 • Programs cover multiple populations • • Dual Eligible (no LTSS) Long-Term Services and Supports Users – Nursing Home Residents – HCBS Waivers • • • Aged/Disabled Acquired Brain Injury Intellectual Disability/Developmental Disability • Programs have multiple outcomes: • • • Participant experience Quality of life Rebalancing Utilization Cost/Budget predictability Employment and Community Integration
Summary 40 • There have been few peer review studies on MLTSS programs: • No pre-program baseline data • Weak comparison groups • Voluntary programs introduce selection • Evidence suggests that in the aggregate: • No harm • Some shift toward HCBS • Programs meet cost goals, but limited evidence of significant savings • Voluntary programs have low uptake

State Experience: Tennessee Patti Killingsworth
Tennessee’s Experience Designing and Implementing Integrated MLTSS Programs
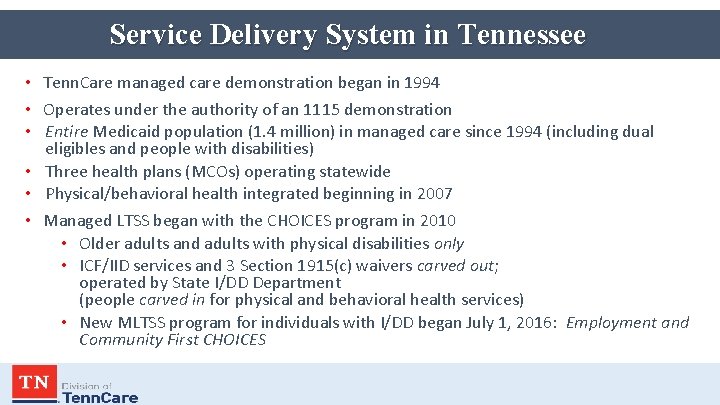
Service Delivery System in Tennessee • Tenn. Care managed care demonstration began in 1994 • Operates under the authority of an 1115 demonstration • Entire Medicaid population (1. 4 million) in managed care since 1994 (including dual eligibles and people with disabilities) • Three health plans (MCOs) operating statewide • Physical/behavioral health integrated beginning in 2007 • Managed LTSS began with the CHOICES program in 2010 • Older adults and adults with physical disabilities only • ICF/IID services and 3 Section 1915(c) waivers carved out; operated by State I/DD Department (people carved in for physical and behavioral health services) • New MLTSS program for individuals with I/DD began July 1, 2016: Employment and Community First CHOICES
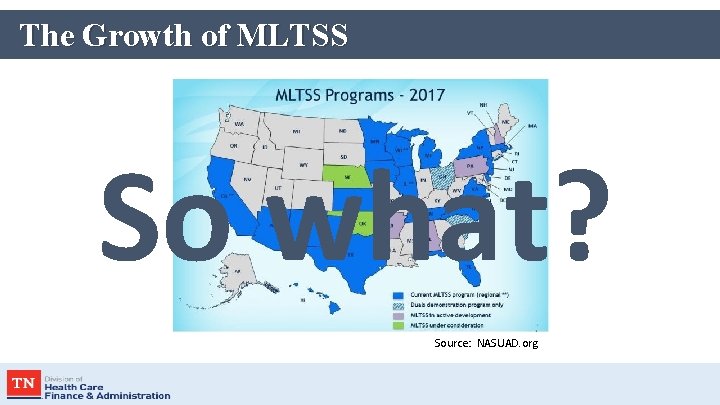
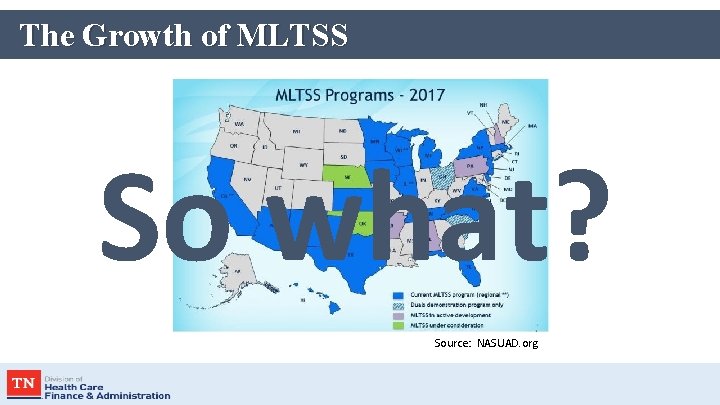
The Growth of MLTSS So what? Source: NASUAD. org
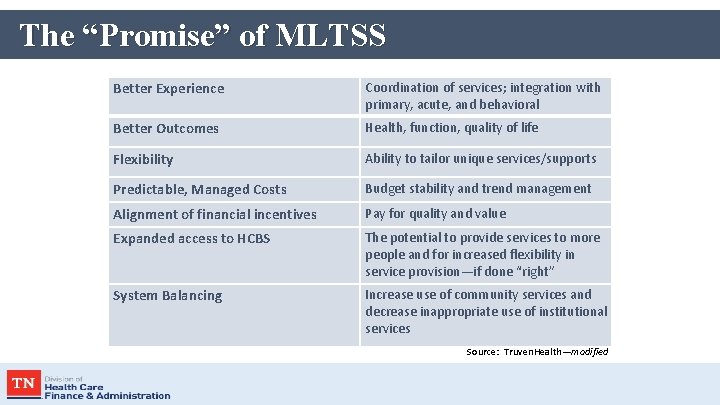
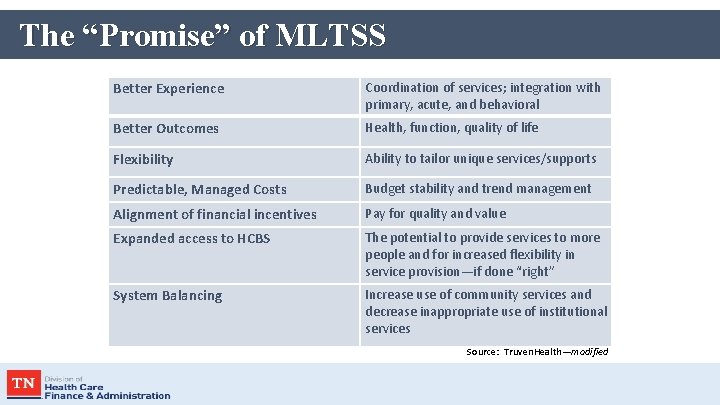
The “Promise” of MLTSS Better Experience Coordination of services; integration with primary, acute, and behavioral Better Outcomes Health, function, quality of life Flexibility Ability to tailor unique services/supports Predictable, Managed Costs Budget stability and trend management Alignment of financial incentives Pay for quality and value Expanded access to HCBS The potential to provide services to more people and for increased flexibility in service provision—if done “right” System Balancing Increase use of community services and decrease inappropriate use of institutional services Source: Truven. Health—modified
The “Promise” of MLTSS We must not promise what we ought not, lest we be called on to perform what we cannot. —Abraham Lincoln
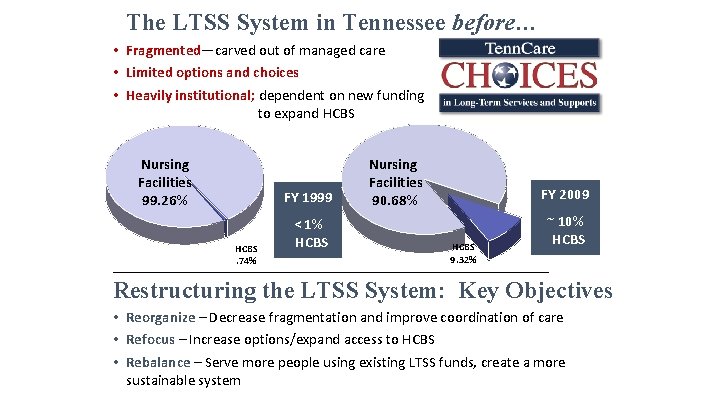
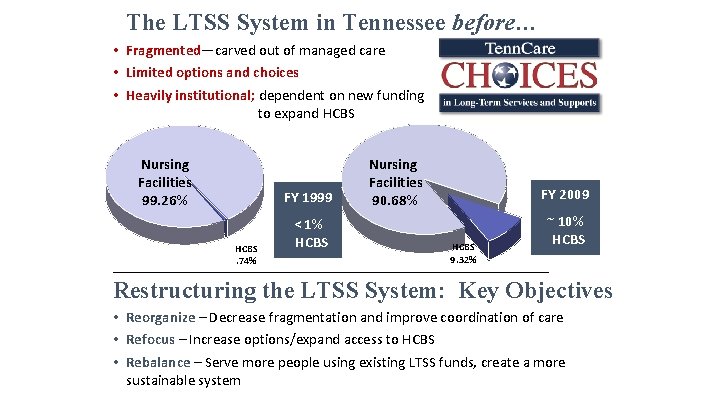
The LTSS System in Tennessee before… • Fragmented—carved out of managed care • Limited options and choices • Heavily institutional; dependent on new funding to expand HCBS Nursing Facilities 99. 26% FY 1999 HCBS. 74% < 1% HCBS Nursing Facilities 90. 68% FY 2009 HCBS 9. 32% ~ 10% HCBS _____________________________________ Restructuring the LTSS System: Key Objectives • Reorganize – Decrease fragmentation and improve coordination of care • Refocus – Increase options/expand access to HCBS • Rebalance – Serve more people using existing LTSS funds, create a more sustainable system

Program Design Choices to Accomplish Objectives • Nursing facility services and HCBS for older adults and adults with physical disabilities integrated into existing managed care program • People do not enter/leave managed care or change health plans when enrolling in LTSS • Blended capitation payment for all physical, behavioral and LTSS • MCOs at full risk for all services, including NF (not time-limited) • Enrollment target for HCBS supports controlled growth while developing community infrastructure to provide care (persons transitioning from a NF and certain persons at risk of NF placement exempt) • Cost and utilization managed via individual benefit limits, levels of care (LOC), and individual cost neutrality cap o Higher level of care standards for NF services, access to HCBS for “at-risk” • Nursing facility diversion and transition programs, including Money Follows the Person Rebalancing Demonstration with incentive structure

Baseline Data Plan to Measure Program Outcomes • Objective #1: Expand access to HCBS o • Objective #2: Rebalance LTSS spending o • Average person NF versus HCBS expenditures Objective #4: Delay or prevent institutional placement o o • Total HCBS versus NF expenditures Objective #3: Provide cost-effective HCBS as an alternative to institutional care o • # receiving HCBS versus NF services (point in time and unduplicated across the year) Average length of stay in HCBS Percent of new LTSS members admitted to NFs Objective #5: Facilitate transition from NF to HCBS o o Average length of stay in NF # NF-to-community transitions

Access to HCBS before and after… 16, 000 14, 000 12, 000 10, 000 8, 000 6, 000 4, 000 2, 000 0 HCBS Enrollment* 13, 240 Expanded access to 6, 000 4, 861 HCBS 0 HCBS enrollment at CHOICES implementation * Excludes the PACE program which serves <300 people almost exclusively in HCBS, and other limited waiver programs no longer in operation. 15 20 Slow growth in HCBS – enrollment reaches 1, 131 after two years. 10 20 CMS approves HCBS waiver and enrollment begins in 2004. 06 20 03 20 No state-wide HCBS alternative to NFs available before 2003. 1, 131 Well over twice as many people who qualify for nursing facility care receive cost-effective HCBS without a program expansion request; additional cost of NF services if HCBS not available approx. $250 million (federal and state). • Global budget approach: ØLimited LTSS funding spent based on needs and preferences of those who need care ØMore cost-effective HCBS serves more people with existing LTSS funds ØCritical as population ages and demand for LTSS increases HCBS waiting list eliminated in CHOICES

Keeping the “Promise“ of MLTSS Expanding HCBS; system balancing LTSS Enrollment before HCBS CHOICES (March/August 17% 2010) NF 83%
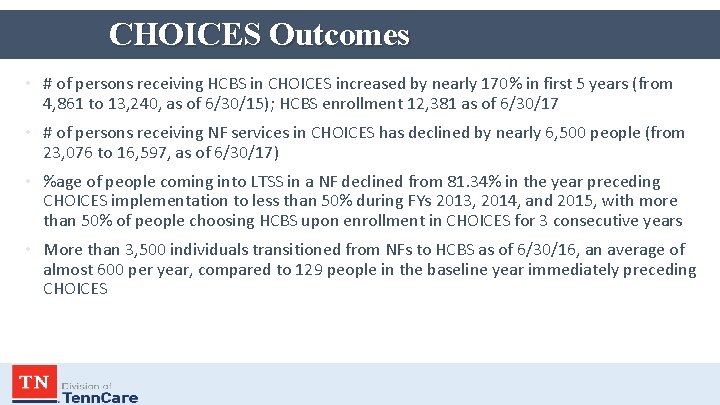
CHOICES Outcomes • # of persons receiving HCBS in CHOICES increased by nearly 170% in first 5 years (from 4, 861 to 13, 240, as of 6/30/15); HCBS enrollment 12, 381 as of 6/30/17 • # of persons receiving NF services in CHOICES has declined by nearly 6, 500 people (from 23, 076 to 16, 597, as of 6/30/17) • %age of people coming into LTSS in a NF declined from 81. 34% in the year preceding CHOICES implementation to less than 50% during FYs 2013, 2014, and 2015, with more than 50% of people choosing HCBS upon enrollment in CHOICES for 3 consecutive years • More than 3, 500 individuals transitioned from NFs to HCBS as of 6/30/16, an average of almost 600 per year, compared to 129 people in the baseline year immediately preceding CHOICES

Employment and Community First CHOICES
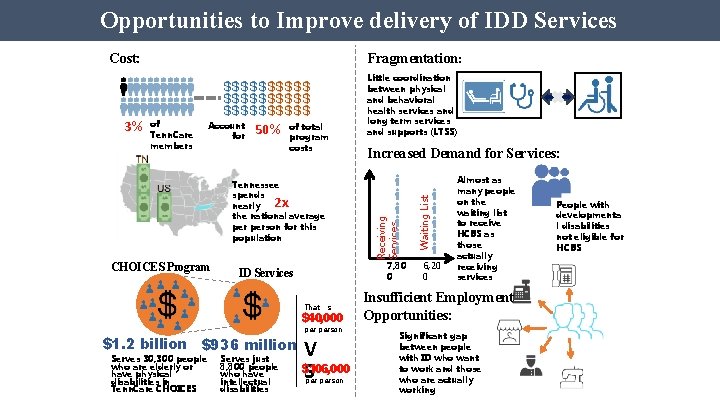
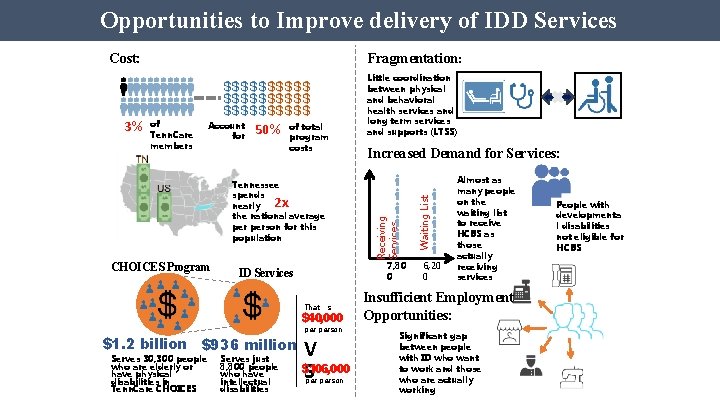
Opportunities to Improve delivery of IDD Services 3% Fragmentation: of Tenn. Care members Account for 50% of total program costs Tennessee spends nearly the national average person for this population Little coordination between physical and behavioral health services and long term services and supports (LTSS) Increased Demand for Services: CHOICES Program 7, 80 0 ID Services That’s $40, 000 $1. 2 billion $936 million Serves 30, 300 people who are elderly or have physical disabilities in Tenn. Care CHOICES Serves just 8, 800 people who have intellectual disabilities Receiving Services 2 x person V $106, 000 S person Waiting List Cost: 6, 20 0 Almost as many people on the waiting list to receive HCBS as those actually receiving services Insufficient Employment Opportunities: Significant gap between people with ID who want to work and those who are actually working People with developmenta l disabilities not eligible for HCBS
Program Design Choices to Accomplish Objectives • New MLTSS program component for individuals with I/DD integrated into existing managed care program • HCBS only; ICF/IID services and 1915(c) waivers remain carved out • Enrollment target supports controlled growth while developing sufficient community infrastructure to provide services (persons transitioning from a NF and certain persons at risk of NF placement are exempt) • People with employment-related needs/goals prioritized for enrollment • Cost and utilization managed via individual benefit limits, levels of care (LOC)—institutional/at-risk, and expenditure (including individual cost neutrality) caps • Tiered benefit structure based on needs of people in each group provides comprehensive and flexible service array, designed to promote employment, community integration, and individual/family empowerment • Array of 14 employment services create a pathway to employment, even for people with the most significant needs • Value-based reimbursement for employment services focused on achieving employment outcomes, and incentivizing fading (independence) over time

Baseline Data Plan to Measure Program Outcomes • Objective #1: Expand access to HCBS o • Objective #2: Provide more cost-effective HCBS as an alternative to institutional care o • Average person LTSS expenditures Objective #3: Continue balancing LTSS spending o • • # of individuals receiving HCBS (point in time and unduplicated across the year) Total HCBS versus ICF/IID expenditures Objective #4: Increase competitive, integrated employment Objective #5: Improve quality of life
ECF CHOICES Outcomes • • • More people with I/DD enrolled into HCBS in the last 20 months than in the previous 6 years For the first time in the State’s history, people with DD other than ID have access to HCBS 87% of people enrolled in an employment-related priority category Annualized cost of HCBS less than half the current average Most frequently utilized services include (in order) Employment, Community Integration Supports, Personal Assistance, Independent Living Skills Training, Respite, Community Transportation • Memorandum of Agreement with Vocational Rehabilitation operationalized through statewide joint training of VR and MCO staff; regional implementation calls • Over 20% of working-age individuals with I/DD working in competitive integrated employment (7% higher than national average with most people enrolled less than a year) • Average wages $8. 48/hour • Average hours worked 17 per week
Some Key Questions • Are states defining clear policy goals for MLTSS? • Do states define clear measures and collect data (including baseline) to know if they are achieving goals? • Can we measure/demonstrate the value of MLTSS? • For states; most importantly, for beneficiaries • Does the level of integration impact quality and cost-effectiveness outcomes? • Is “real” integration happening? • How well are MLTSS programs addressing social determinants of health—coordinating services and supports? • How do people with the most complex needs fare in these programs? • Are there replicable models (or components) of success? • What capacities do health plans need to provide MLTSS? • How capacities do states need to develop and oversee MLTSS? • How is MLTSS changing the face of managed care?
State Experience: Pennsylvania Kevin Hancock

Pennsylvania’s Recent MLTSS Launch: Design Components and Lessons Learned Kevin Hancock Deputy Secretary OFFICE OF LONG-TERM LIVING DEPARTMENT OF HUMAN SERVICES May 3, 2018
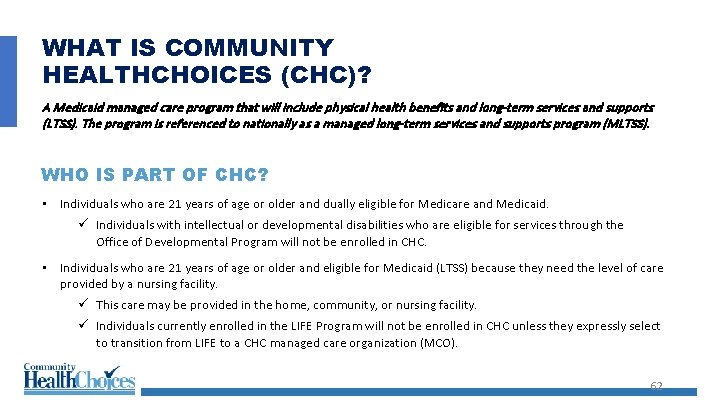
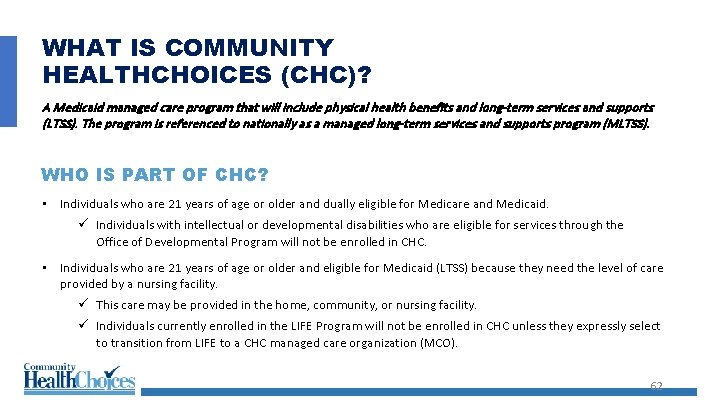
WHAT IS COMMUNITY HEALTHCHOICES (CHC)? A Medicaid managed care program that will include physical health benefits and long-term services and supports (LTSS). The program is referenced to nationally as a managed long-term services and supports program (MLTSS). WHO IS PART OF CHC? • Individuals who are 21 years of age or older and dually eligible for Medicare and Medicaid. ü Individuals with intellectual or developmental disabilities who are eligible for services through the Office of Developmental Program will not be enrolled in CHC. • Individuals who are 21 years of age or older and eligible for Medicaid (LTSS) because they need the level of care provided by a nursing facility. ü This care may be provided in the home, community, or nursing facility. ü Individuals currently enrolled in the LIFE Program will not be enrolled in CHC unless they expressly select to transition from LIFE to a CHC managed care organization (MCO). 62
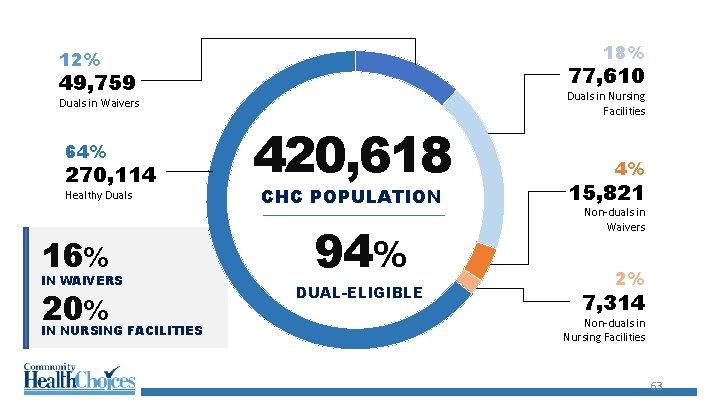
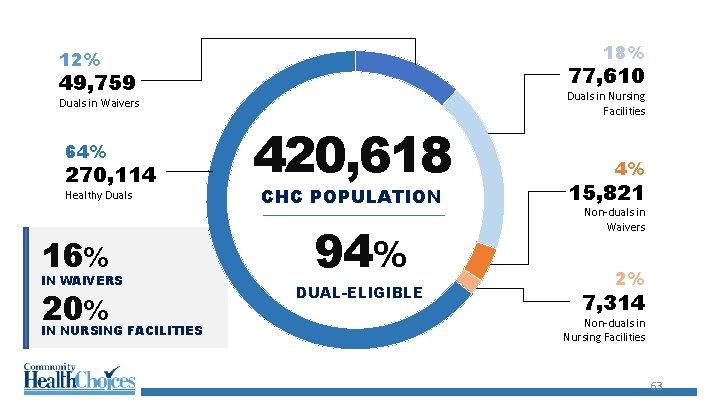
18% 12% 77, 610 49, 759 Duals in Waivers 64% 270, 114 Healthy Duals 16% IN WAIVERS 20% 420, 618 CHC POPULATION 94% DUAL-ELIGIBLE Duals in Nursing Facilities 4% 15, 821 Non-duals in Waivers 2% 7, 314 Non-duals in Nursing Facilities IN NURSING FACILITIES 63
WHO IS NOT PART OF CHC? • People receiving long-term services & supports in the OBRA waiver & are not nursing facility clinically eligible (NFCE) • A person with an intellectual or developmental disability receiving services through the Department of Human Services’ Office of Developmental Programs • A resident in a state-operated nursing facility, including the state veterans’ homes 64
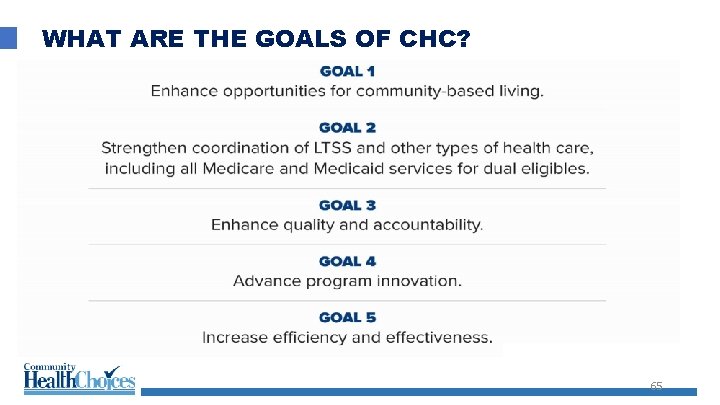
WHAT ARE THE GOALS OF CHC? 65

CHC DESIGN COMPONENTS 66
Extensive Stakeholder Engagement • Publication of Discussion Document and Concept Paper of the original program design for public comment • Six statewide listening sessions • Publication of the draft request for proposal for public comment • Development of an advisory committee designed with a cross-section of participants to support program design and oversight • Monthly webinars about program components • Bi-weekly provider communications and in-person provider outreach sessions • Participant outreach through mailings and in-person sessions • Participant hotlines independent of CHC-MCOs 67

INTERDISCIPLINARY PROJECT MANAGEMENT • Included Workgroups for: • Information systems requirements: • Eligibility and enrollment • Encounters • Case management • Quality data collection • Procurement • Quality Assurance and Program Evaluation • Operations Readiness and Readiness Review • CMS authority • Rate setting • Communications 68
CHC Configuration • Three managed care organizations supporting all five CHC zones • Amerihealth Caritas • UPMC Community Health. Choices • Pennsylvania Health and Wellness (Centene) 69
Considerations • Managed Care Final Rule • Existing managed care configuration with Physical Health. Choices • Behavioral health carve-out • Population carve-outs • Medicare Advantage enrollment penetration • Staffing constraints • Procurement process • Continuity of care 70

Regional Phase In Five Geographic Zones Phase One January 1, 2018: Southwest Zone Phase Two January 1, 2019: Southeast Zone Phase Three January 1, 2020: Lehigh/Capital Zone Northwest Zone; and Northeast Zone Three managed care organizations supporting all five CHC zones: • Amerihealth Caritas • UPMC Community Health. Choices • Pennsylvania Health and Wellness (Centene) 71

CHC LAUNCH UPDATE 72

2018 Community Health. Choices SW GOALS • ASSURING NO PARTICIPANT SERVICE INTERRUPTIONS • ASSURING NO INTERRUPTION IN PROVIDER PAYMENT • SUCCESSFUL LAUNCH FIRST PHASE 73
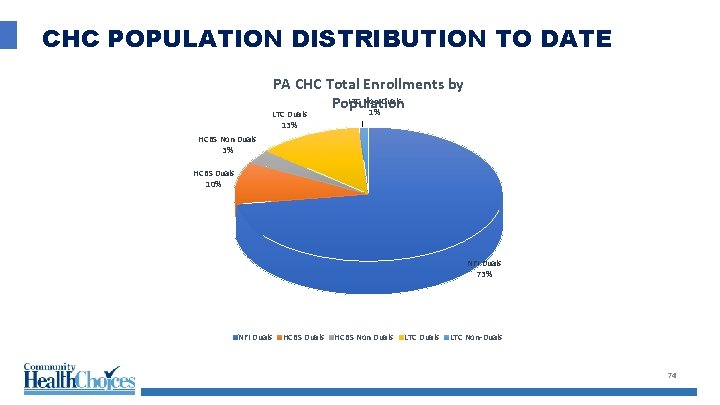
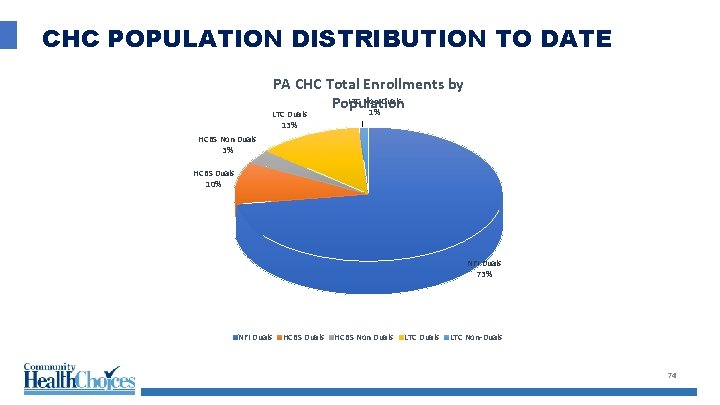
CHC POPULATION DISTRIBUTION TO DATE PA CHC Total Enrollments by LTC Non-Duals Population 1% LTC Duals 13% HCBS Non Duals 3% HCBS Duals 10% NFI Duals 73% NFI Duals HCBS Non Duals LTC Non-Duals 74

CHC SOUTHWEST JANUARY (Age Distribution) Population Over 60 Under 60 51. 2% 69. 4% 33. 3% 94. 7% 45. 0% 57. 9% NFI Duals HCBS Non Duals NF Non-Duals Total Population 48. 8% 30. 6% 66. 7% 5. 3% 55. 0% 42. 1% 75
LESSONS LEARNED (SO FAR): • Earlier stakeholder engagement opportunities with key population groups and group representatives • Earlier in-person provider communication sessions • Enhanced communication materials regarding Medicare vs. CHC • More education and communication on participant rights and protections • Addition report development on enrollment and plan transfer scenarios • More communication on the LIFE (PACE) program as an enrollment alternative • Earlier address of data integrity issues • Earlier pre-transition • More provider information on IEB website • More provider training on Medicare vs. CHC 76

Industry Experience: Anthem/Amerigroup Merrill Friedman Leigh Davison

MCO Approach to MLTSS Programs Merrill Friedman Leigh Davison May 2018
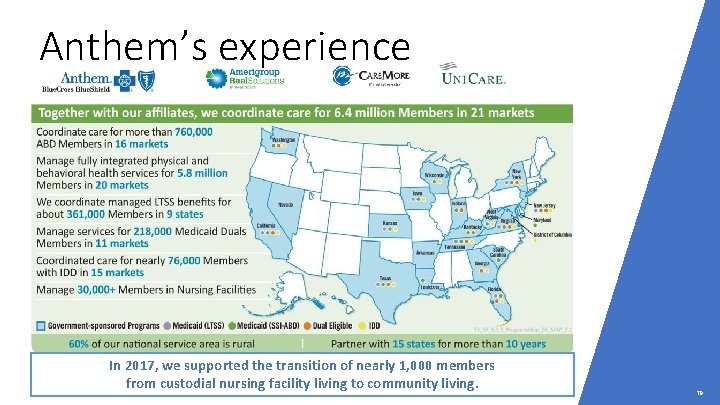
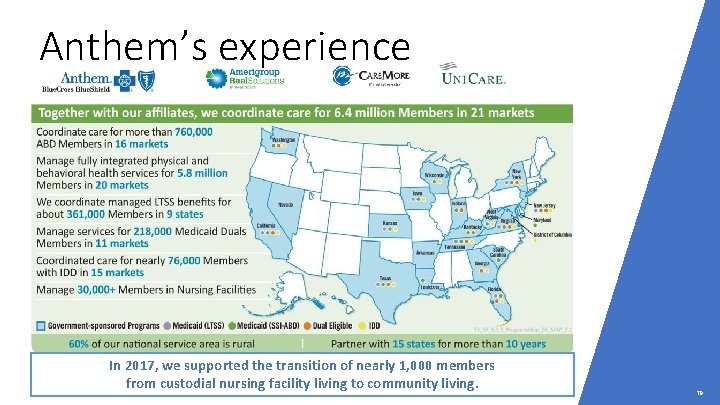
Anthem’s experience In 2017, we supported the transition of nearly 1, 000 members from custodial nursing facility living to community living. 79
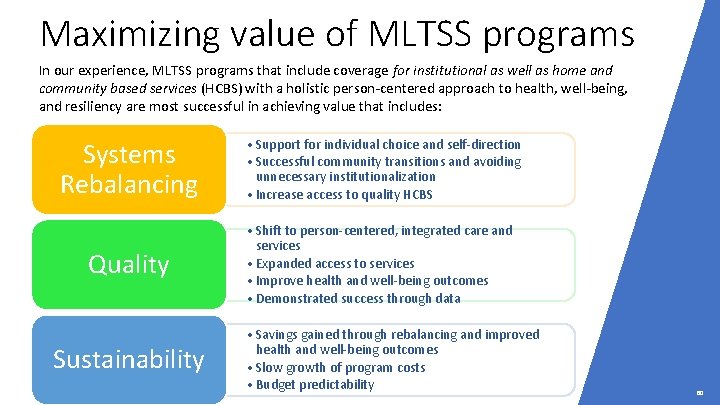
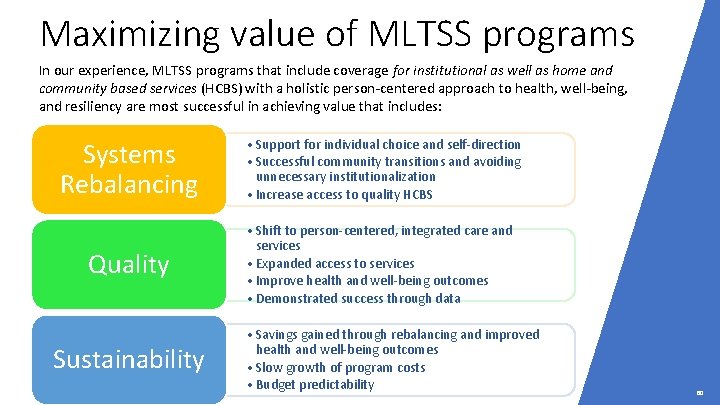
Maximizing value of MLTSS programs In our experience, MLTSS programs that include coverage for institutional as well as home and community based services (HCBS) with a holistic person-centered approach to health, well-being, and resiliency are most successful in achieving value that includes: Systems Rebalancing • Support for individual choice and self-direction • Successful community transitions and avoiding unnecessary institutionalization • Increase access to quality HCBS Quality • Shift to person-centered, integrated care and services • Expanded access to services • Improve health and well-being outcomes • Demonstrated success through data Sustainability • Savings gained through rebalancing and improved health and well-being outcomes • Slow growth of program costs • Budget predictability 80
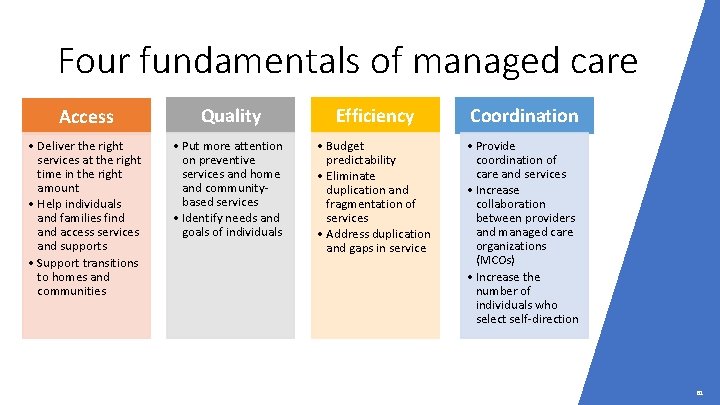
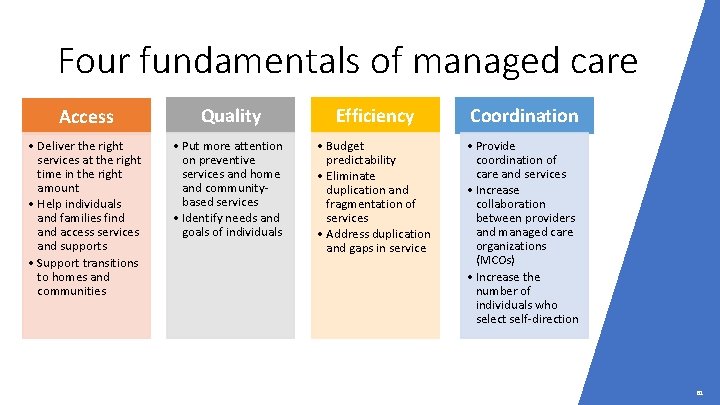
Four fundamentals of managed care Access Quality Efficiency Coordination • Deliver the right services at the right time in the right amount • Help individuals and families find access services and supports • Support transitions to homes and communities • Put more attention on preventive services and home and communitybased services • Identify needs and goals of individuals • Budget predictability • Eliminate duplication and fragmentation of services • Address duplication and gaps in service • Provide coordination of care and services • Increase collaboration between providers and managed care organizations (MCOs) • Increase the number of individuals who select self-direction 81
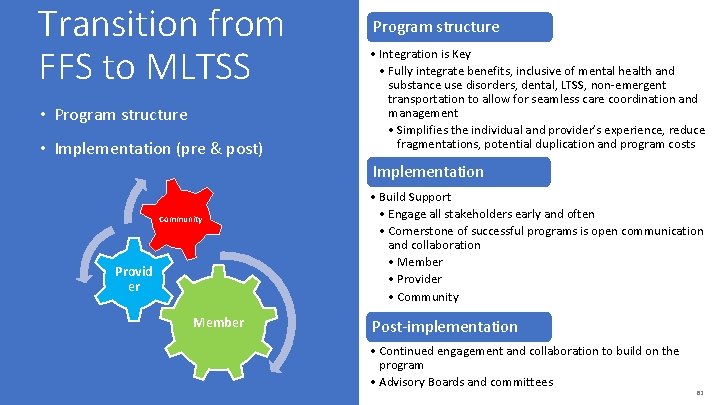
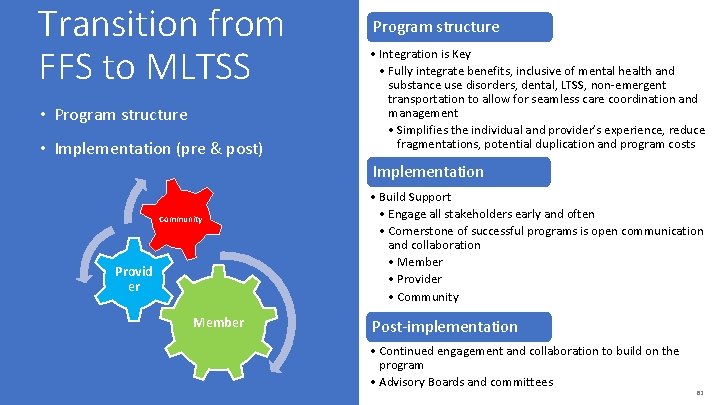
Transition from FFS to MLTSS • Program structure • Implementation (pre & post) Program structure • Integration is Key • Fully integrate benefits, inclusive of mental health and substance use disorders, dental, LTSS, non-emergent transportation to allow for seamless care coordination and management • Simplifies the individual and provider’s experience, reduce fragmentations, potential duplication and program costs Implementation Community Provid er Member • Build Support • Engage all stakeholders early and often • Cornerstone of successful programs is open communication and collaboration • Member • Provider • Community Post-implementation • Continued engagement and collaboration to build on the program • Advisory Boards and committees 82
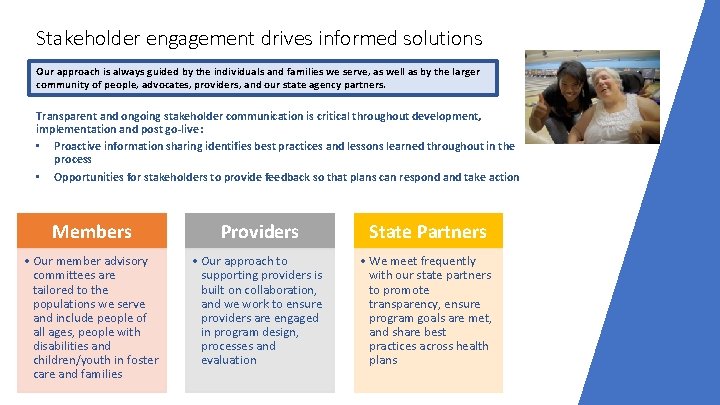
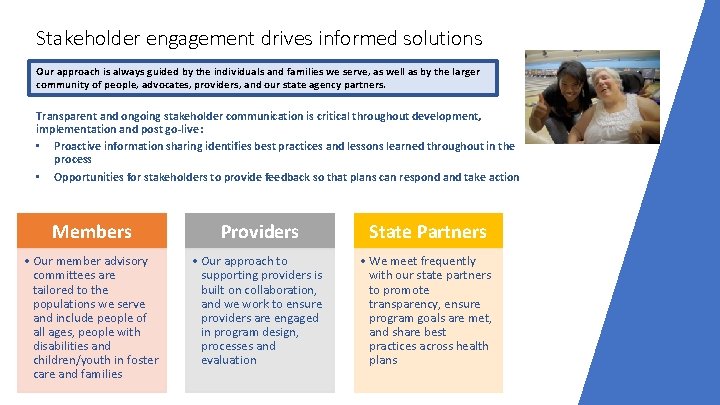
Stakeholder engagement drives informed solutions Our approach is always guided by the individuals and families we serve, as well as by the larger community of people, advocates, providers, and our state agency partners. Transparent and ongoing stakeholder communication is critical throughout development, implementation and post go-live: • Proactive information sharing identifies best practices and lessons learned throughout in the process • Opportunities for stakeholders to provide feedback so that plans can respond and take action Members Providers State Partners • Our member advisory committees are tailored to the populations we serve and include people of all ages, people with disabilities and children/youth in foster care and families • Our approach to supporting providers is built on collaboration, and we work to ensure providers are engaged in program design, processes and evaluation • We meet frequently with our state partners to promote transparency, ensure program goals are met, and share best practices across health plans
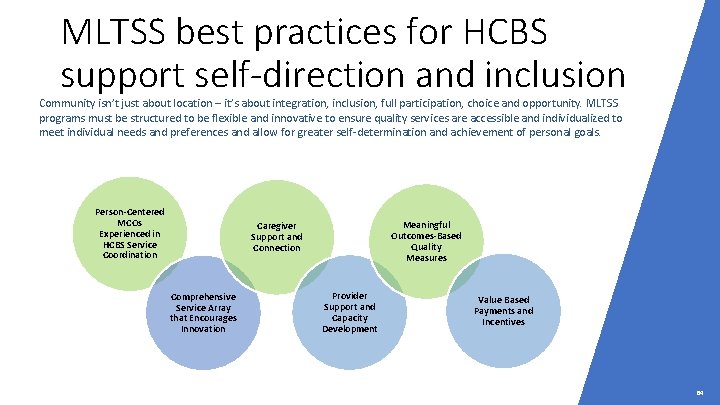
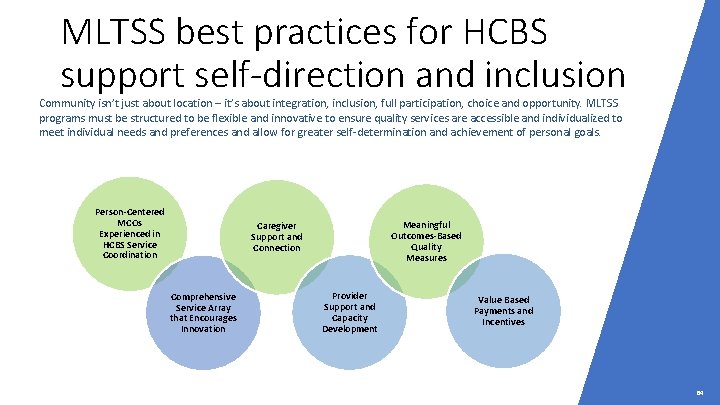
MLTSS best practices for HCBS support self-direction and inclusion Community isn’t just about location – it’s about integration, inclusion, full participation, choice and opportunity. MLTSS programs must be structured to be flexible and innovative to ensure quality services are accessible and individualized to meet individual needs and preferences and allow for greater self-determination and achievement of personal goals. Person-Centered MCOs Experienced in HCBS Service Coordination Meaningful Outcomes-Based Quality Measures Caregiver Support and Connection Comprehensive Service Array that Encourages Innovation Provider Support and Capacity Development Value Based Payments and Incentives 84

Best practices for MCOs Must be person-centered organizations, with leadership at all levels committed to: • Building bench strength within service coordination and cross-functional support teams to facilitate person centered planning and practices • Developing and implementing tools, policies and procedures to support person-centered practices • Delivering training and technical assistance to providers and other stakeholders Care management systems must include: • Interdisciplinary Service Coordination Teams with enhanced training and tools to coordinate Member needs across service systems • Comprehensive assessments and integrated care plans that address all Member health and support needs, including HCBS Settings rule requirements, natural supports and Social Determinants of Health (SDOH) • Population-specific clinical programs and innovative technologies to improve individual health and support independence and community engagement • Systems to identify and track Member outcomes to support payment innovations Anthem is committed to Person Centered Thinking© Trainer Certification as recognized by the Internal Learning Community for Person Centered Practices 85
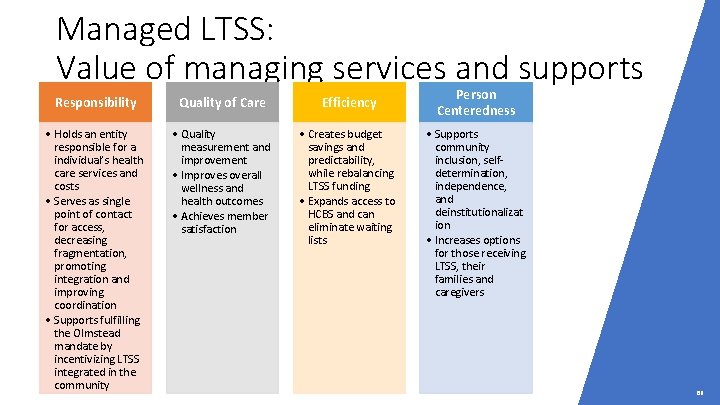
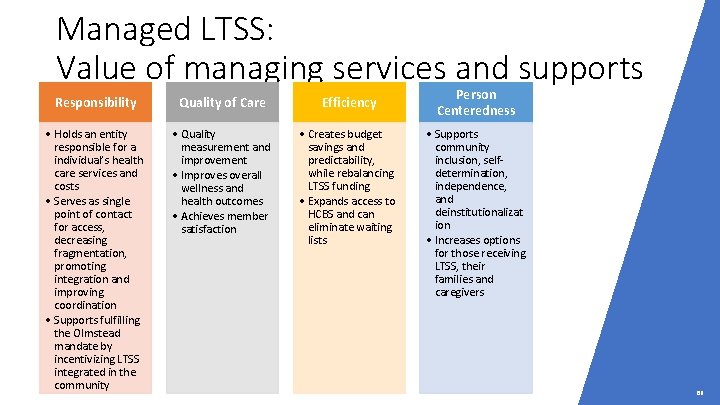
Managed LTSS: Value of managing services and supports Responsibility Quality of Care Efficiency • Holds an entity responsible for a individual’s health care services and costs • Serves as single point of contact for access, decreasing fragmentation, promoting integration and improving coordination • Supports fulfilling the Olmstead mandate by incentivizing LTSS integrated in the community • Quality measurement and improvement • Improves overall wellness and health outcomes • Achieves member satisfaction • Creates budget savings and predictability, while rebalancing LTSS funding • Expands access to HCBS and can eliminate waiting lists Person Centeredness • Supports community inclusion, selfdetermination, independence, and deinstitutionalizat ion • Increases options for those receiving LTSS, their families and caregivers 86
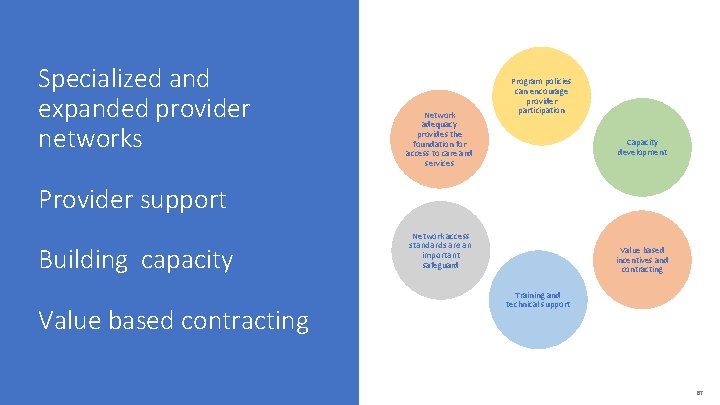
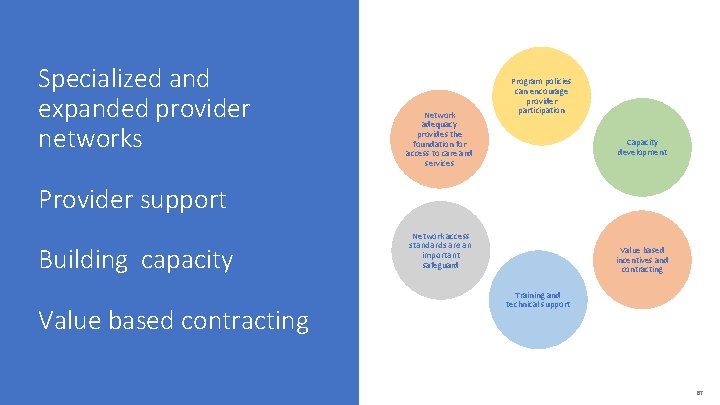
Specialized and expanded provider networks Network adequacy provides the foundation for access to care and services Program policies can encourage provider participation Capacity development Provider support Building capacity Value based contracting Network access standards are an important safeguard Value based incentives and contracting Training and technical support 87
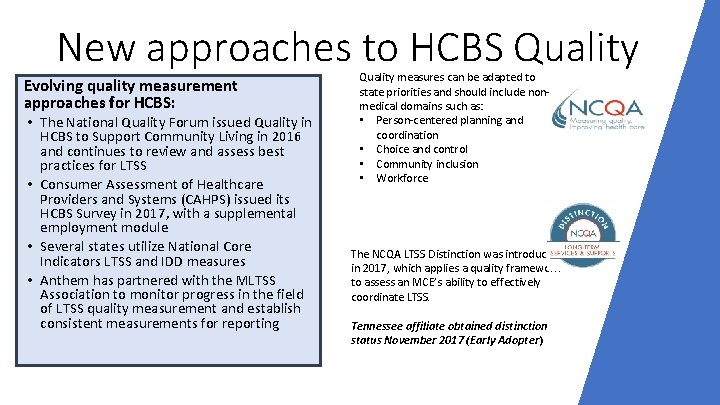
New approaches to HCBS Quality Evolving quality measurement approaches for HCBS: • The National Quality Forum issued Quality in HCBS to Support Community Living in 2016 and continues to review and assess best practices for LTSS • Consumer Assessment of Healthcare Providers and Systems (CAHPS) issued its HCBS Survey in 2017, with a supplemental employment module • Several states utilize National Core Indicators LTSS and IDD measures • Anthem has partnered with the MLTSS Association to monitor progress in the field of LTSS quality measurement and establish consistent measurements for reporting Quality measures can be adapted to state priorities and should include nonmedical domains such as: • Person-centered planning and coordination • Choice and control • Community inclusion • Workforce The NCQA LTSS Distinction was introduced in 2017, which applies a quality framework to assess an MCE’s ability to effectively coordinate LTSS. Tennessee affiliate obtained distinction status November 2017 (Early Adopter )
Innovations for health and independence HCBS best practices include comprehensive service arrays that are flexible to encourage innovation in areas such as: Self Directed Goods and Services innovations Wearable Sensors and Remote Supports (for proactive health solutions and to reduce reliance on 24/7 staff) Integrated, Competitive Employment Supports (including customized and selfemployment options) Assistive Technology and Home Modifications Peer Supports (including developmentally-adapted and caregiver peer options) Caregiver Supports Non-medical Transportation Training and Supports In Lieu of Services (options that are flexible to address emerging needs) 89
Closing • Ensure alignment of goals with state partners • Listen and collaborate with individuals, families, providers, and stakeholders • Commit to community engagement • Deliver on state and federal requirements • Mega Rules, HCBS Settings Rule, and State Contracts • Bring value to individuals (and their families) accessing long term services and supports by enhancing quality of services through personcentered planning and coordination 90

Panel Discussion And Q & A Moderator: Paul Saucier
Panel Question 92 What question about MLTSS ? would you like researchers to answer? What actions might you be able to take if you had the answer?
93 Thank You Please take a moment to fill out the brief evaluation which will appear in your browser