Managed Medicaid LongTerm Services and Supports is the


- Slides: 18
Managed Medicaid Long-Term Services and Supports is the Answer, But What is the Question? Bob Applebaum Annual Meeting of the Gerontological Society of America November 2018
Context • Medicaid expenditures (25%) continue to dominate state policy • HCBS Waivers Have Grown Dramatically over the past two decades • The expansion means that HCBS and Nursing Homes need to be managed • States have been trying to shift risk– financial and management to others 2
Context • Two populations that states worry about: Duals and Medicaid only LTSS • Duals are 21 percent of Medicare and 15 percent of Medicaid populations, but health and long-term care costs account for 36 % of Medicare and 39% of Medicaid • Medicaid LTSS 15 -20% of 60 plus and vast majority of under 60 age group
Proposed Benefits of Management and Integration • Proponents argue that managed and integrated programs will: • Reduce costs: MLTSS and Integrated Care Programs have an incentive to reduce spending on LTSS and hopefully acute care. Feds less attention on specifics of Medicaid • Make services more cohesive and efficient: Providers do not communicate, causing poor transitions between settings • Reduce confusion: Demonstrations to simplify the process of receiving healthcare by providing a single set of comprehensive benefits (at least for Medicaid) 4
Managed LTSS • Top priorities– Control Medicaid costs, Payment and Delivery System Reform, Infrastructure Development • Medicare and Medicaid are criticized for misaligned financial incentives that lead to cost shifting and bad quality • What can previous experiences tell us
State Approaches in Managed Care: Results of Kaiser Medicaid Director Survey(s) • As of July 2018, 24 states have MLTSS -- 17 are statewide • MLTSS typically cover NF, HCBS, primary care and behavioral health Target population -- Some will enroll all dual eligible into managed care plans, but others will restrict the population by other criteria such as age, or diagnosis Geographic area -- Most states are pursing state demos, but others are restricting enrollment to specific areas. Financing -- Most states will pursue a capitated model, but others will test a managed fee-for-service Self-direction exists but except California all small (5%) 6

Research Results on Managed LTSS are Limited • • • The Wisconsin Family Care evaluation showed modest cost savings for managed care enrollees. Evaluation of Minnesota Senior Health Options showed higher costs for the managed care group. Evaluations measuring quality had mixed results. The Mass Health group spent less time in nursing facilities than the group not receiving managed care, but the evaluation of Minnesota. SHO showed no difference. Mathematica study– lower nursing home placement rates in New York, no difference in Tennessee. Most evaluations had no statistically significant difference in hospitalization, ER use, or mortality. Florida evaluation work found negative outcomes, especially on cost 7
Research Cont. GAO Report on Medicaid Managed Care GAO found CMS oversight of state payment structures was limited. GAO found states using 2010/11 to set 2015 rates GAO found problems with encounter data (used to set rates) RECs-- States need to report on progress in achieving MLTSS goals States need to fix rate setting process States need to verify encounter data
Research Cont. • GAO Report on Medicare Advantage (MA) in 2016 found problems with risk adjst • MA enrollees without functional limitations the capitated rate is $1, 000 too high • MA enrollees with functional impairments $225 too low • New HHS Inspector General Report, 2018 MA-- found 75 +% of denials reversed, but most don’t appeal (1%)
Lessons From the Previous Generation • Leutz (1999) review of previous integration efforts: • Integration cost before it pays • Can’t integrate square peg in a round hole • One who integrate calls the tune • S/HMO demonstration really tested integrated care. No major results, but now integrated care is the answer 10
Motivation: Ohio’s Challenges: • Today Ohio has 305, 000 individuals of all ages with severe disability and 122, 000 (40%) receive LTC services through Medicaid • Today 24% of state budget is Medicaid– 36% goes to LTC • By 2040, 600, 000 with severe disability and 237, 000 projected to receive Medicaid LTC services • Future is unclear, but policy-makers are worried
Integrated Care Demonstration in Ohio My. Care • DOM and CMS have agreed to a 3, now 4 year demonstration with evaluation (60% of state) • All older persons and individuals with disability will be required to enroll in Medicaid • 3 groups– NF, HCBS, Community non- LTSS • Medicare enrollment remains individual choice • 2 plan choices in each region, 3 in Cleveland • AAA’s will continue to manage HCBS participants during demo period • NF and AL providers rates set during demo 12
Ohio ICDS Demonstration cont. • Many unanswered questions both about the final intervention and outcomes • For HCBS 65% enroll in same Medicare and Medicaid plan, NF 50% Comm 53% • Unclear whether quality of care integration can be achieved • Can managed care providers understand the culture of long-term care • Will this save money for Medicaid, Medicare? 13
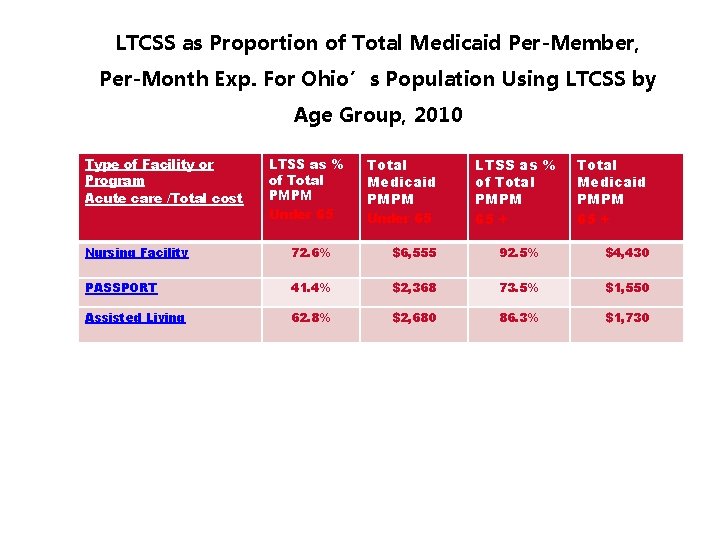
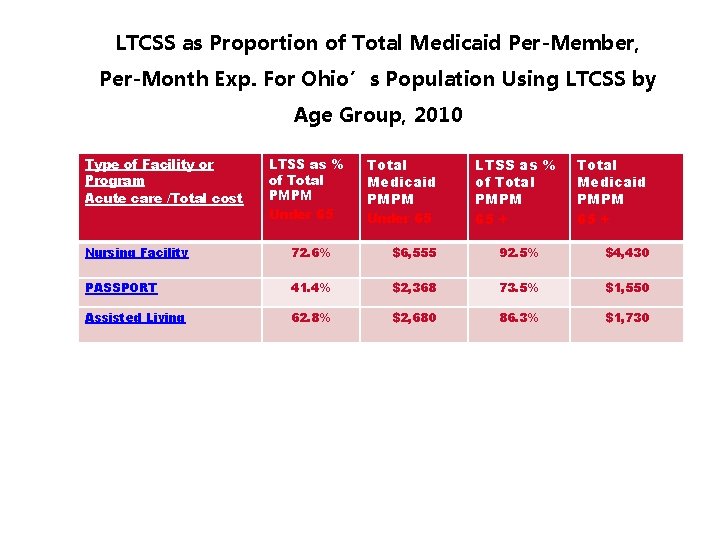
LTCSS as Proportion of Total Medicaid Per-Member, Per-Month Exp. For Ohio’s Population Using LTCSS by Age Group, 2010 Type of Facility or Program Acute care /Total cost LTSS as % of Total PMPM Under 65 Total Medicaid PMPM Under 65 LTSS as % of Total PMPM 65 + Total Medicaid PMPM 65 + Nursing Facility 72. 6% $6, 555 92. 5% $4, 430 PASSPORT 41. 4% $2, 368 73. 5% $1, 550 Assisted Living 62. 8% $2, 680 86. 3% $1, 730
The Challenges • Ohio data indicates that older people with high levels of disability spend a lot of Medicaid dollars on long-term services. Can this program save Medicaid money? • Acute care is from Mars and long-term services is from Venus. This clash of cultures is real and impacts success. • An ever complex managed care entity could easily move the consumer experience to less empowerment 15
Issues for “Duals” Approach • Strategy is Medicaid driven, but most older people who live in community are not on Medicaid 10% community, but 60%+ in NF • Does not do anything to keep elders from becoming Medicaid recipients • Could even incentivize Health Plans to get more folks on Medicaid to maximize waivers • Even if we make Medicaid a bit more efficient, we still have big problems 16

Is Policy Now All Just Ideology? • States Making Big Policy Moves to Integrated Care or MLTSS • However, the Evidence is Mostly not Available, Evidence that Exists is Mixed • Why Have States Embraced the Approach? • Perceived Certainty and Ideological Belief • Is this a Symptom of Overall Policy Development in the U. S? • Need Real Data to Make Good Decisions
Contact info • Bob Applebaum Applebra@miamioh. edu • Scrippsaging. org (Scripps web site) 18