Which Ulcers are Which DIAGNOSIS AND EVALUATION OF









- Slides: 94
Which Ulcers are Which? DIAGNOSIS AND EVALUATION OF CHRONIC ULCERS Thomas M. Bozzuto, DO, FACEP, UHM Medical Director Phoebe Wound Care and Hyperbaric Center Albany, GA Past President, American College of Hyperbaric Medicine
Course Outline • How to differentiate different types of ulcers • Tips in diagnosing • • Arterial ulcers Venous ulcers Pressure ulcers Dehisced surgical ulcers • Treatment suggestions • Resources
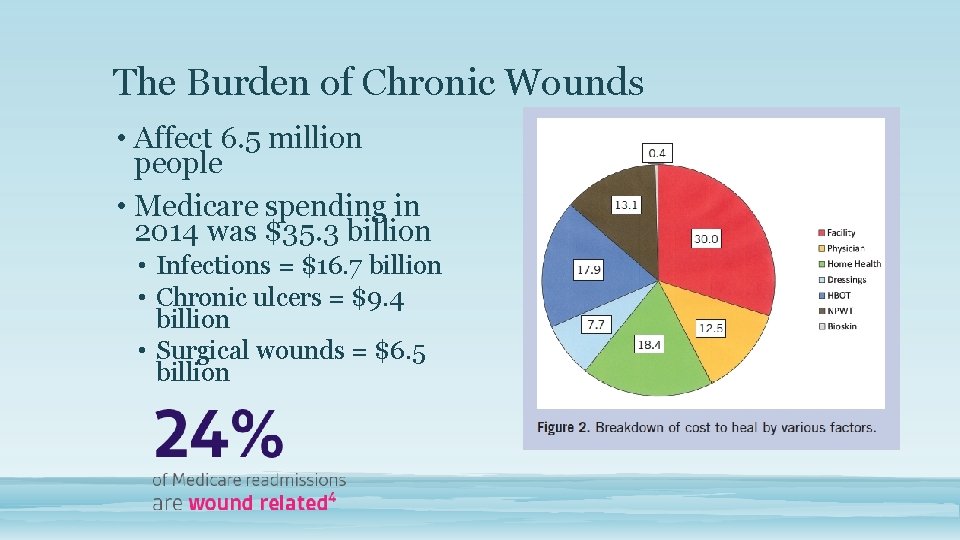
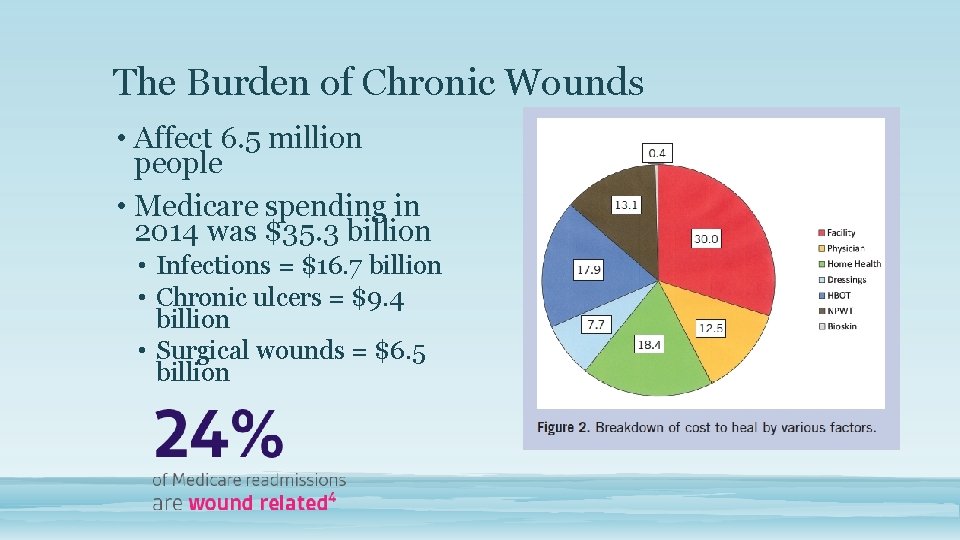
The Burden of Chronic Wounds • Affect 6. 5 million people • Medicare spending in 2014 was $35. 3 billion • Infections = $16. 7 billion • Chronic ulcers = $9. 4 billion • Surgical wounds = $6. 5 billion
Acute wounds • Definition: • Short duration (<6 weeks) • Normal Healing Process • Normal inflammatory phase • Normal granulation • Normal tensile strength • No local / systemic compromise • No underlying etiology • Cause: • Usually trauma / surgery
Chronic Wounds • Definition: • Long duration (>6 weeks) • Abnormal Healing Process • Prolonged inflammatory phase • Poor / absent granulation • Poor tensile strength / dehiscence • Local / systemic compromise (ischemia, corticosteroids) • Underlying etiology (DM; RA; SLE: etc. ) • Causes: • Local • Systemic
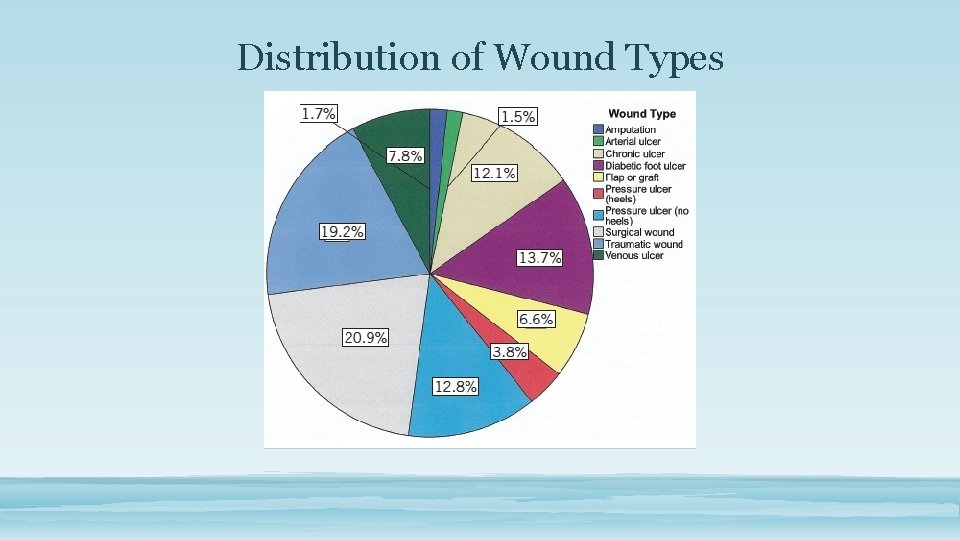
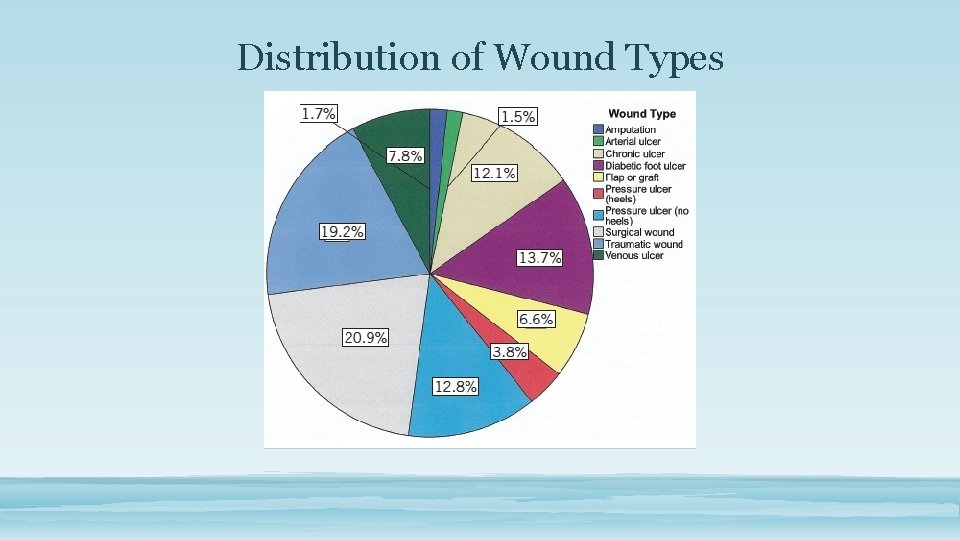
Distribution of Wound Types
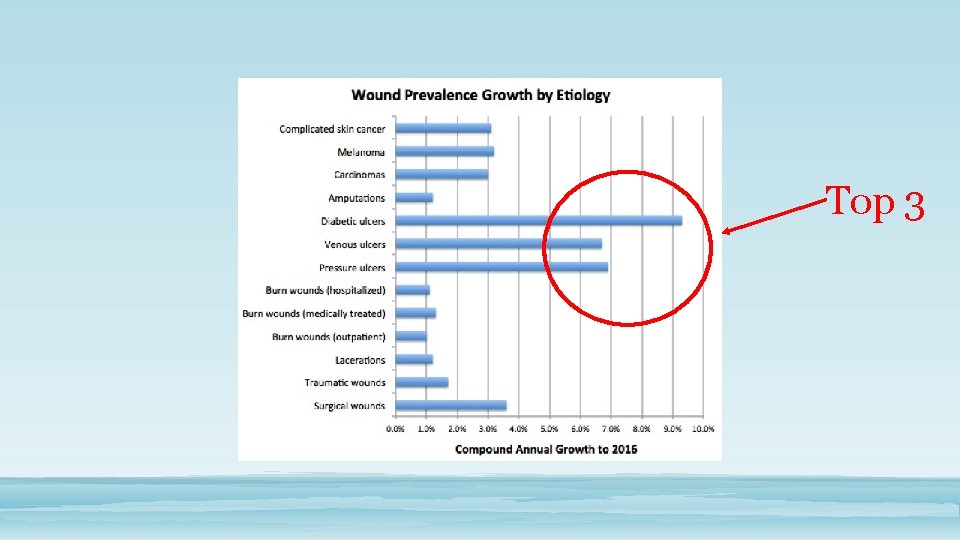
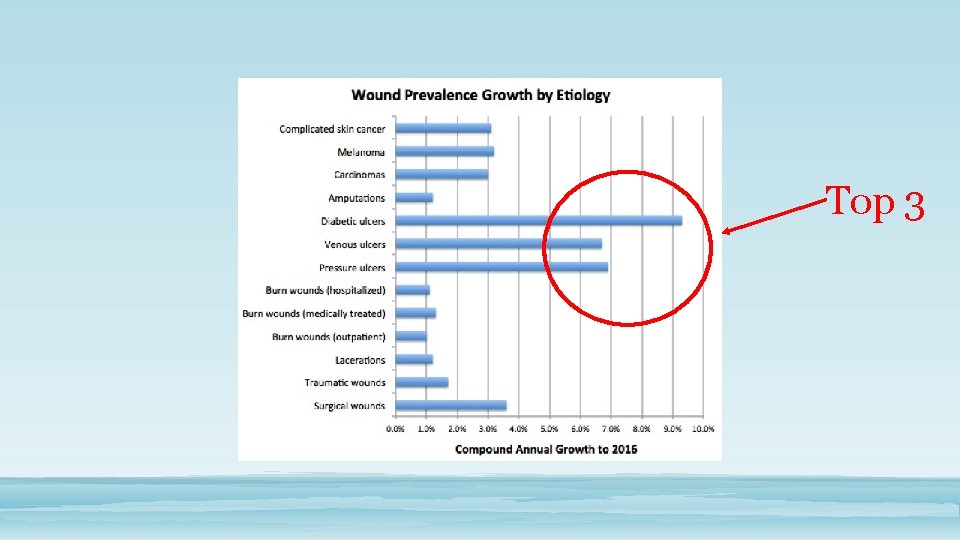
Top 3
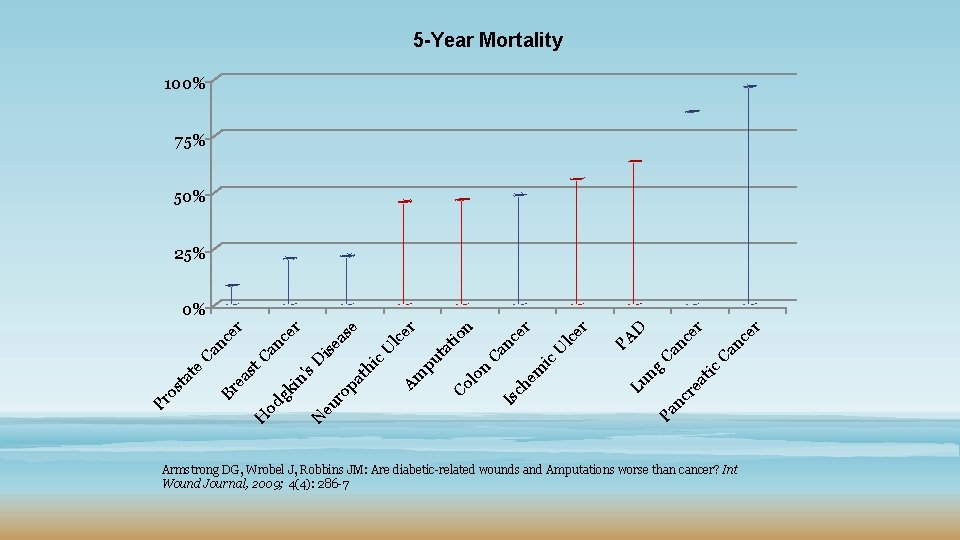
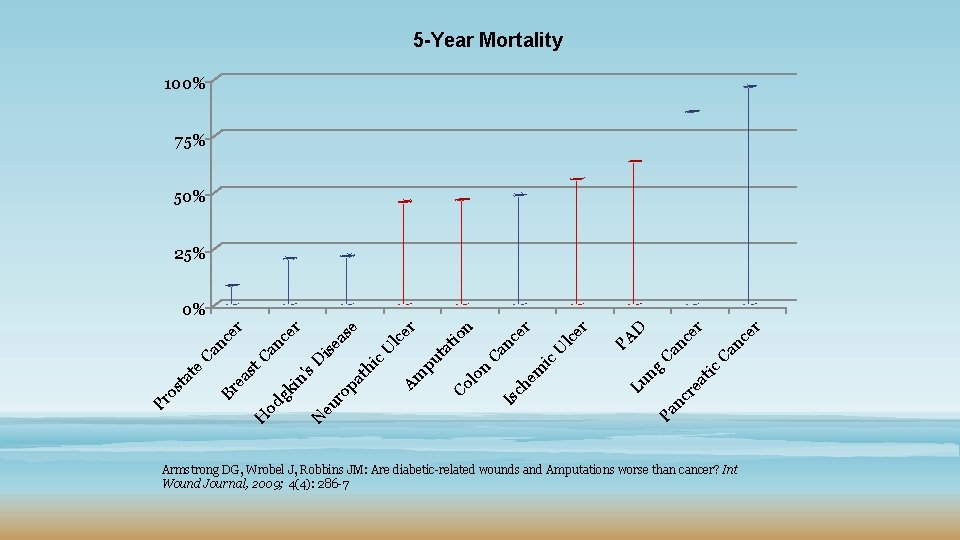
5 -Year Mortality 100% 75% 50% 25% er Ca nc Pa nc r ea tic ng Ca nc er D PA Lu em ic U lc nc Is ch Co lo n Ca ta pu er er n tio er Am th i c. U lc as e ro eu N H od gk pa in 's D is e nc Ca ea st Br Pr os ta t e Ca nc er er 0% Armstrong DG, Wrobel J, Robbins JM: Are diabetic-related wounds and Amputations worse than cancer? Int Wound Journal, 2009; 4(4): 286 -7

Systemic Illness Soft Tissue Infection Nutrition Oxygen Perfusion WOUND Osteomyelitis Pressure Systemic Healing Ability Edema Compliance
The Ideal Wound Approach • From diagnosis to follow up: • Evidence based • Recognition of wound characteristics • Criteria for assessment • Labs and imaging • Wound bed preparation • Appropriate treatment • Proactive follow-up
Approach • Wound etiology must be accurately identified • Clear treatment plan • Offloading DFU • Compressing VLU • Appropriate dressings
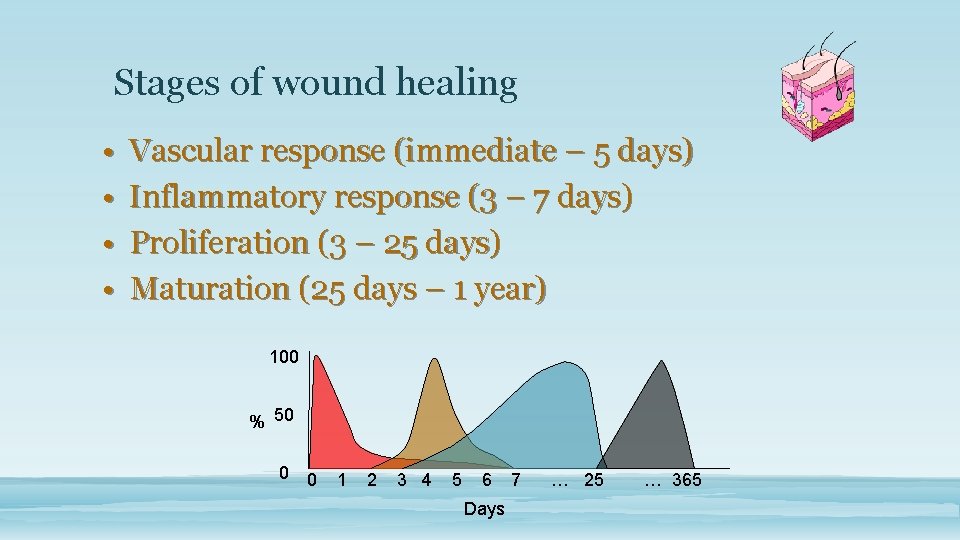
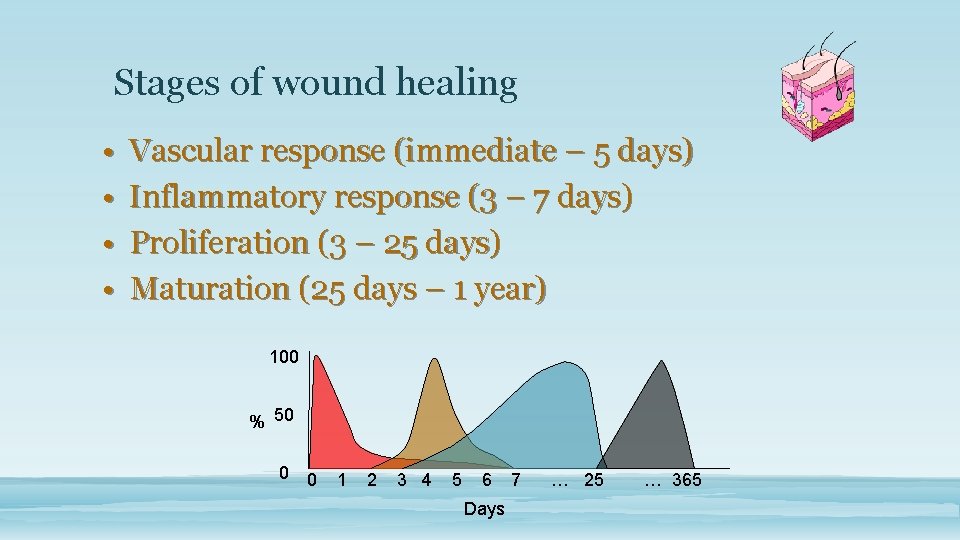
Stages of wound healing • • Vascular response (immediate – 5 days) Inflammatory response (3 – 7 days) Proliferation (3 – 25 days) Maturation (25 days – 1 year) 100 % 50 0 0 1 2 3 4 5 6 Days 7 … 25 … 365
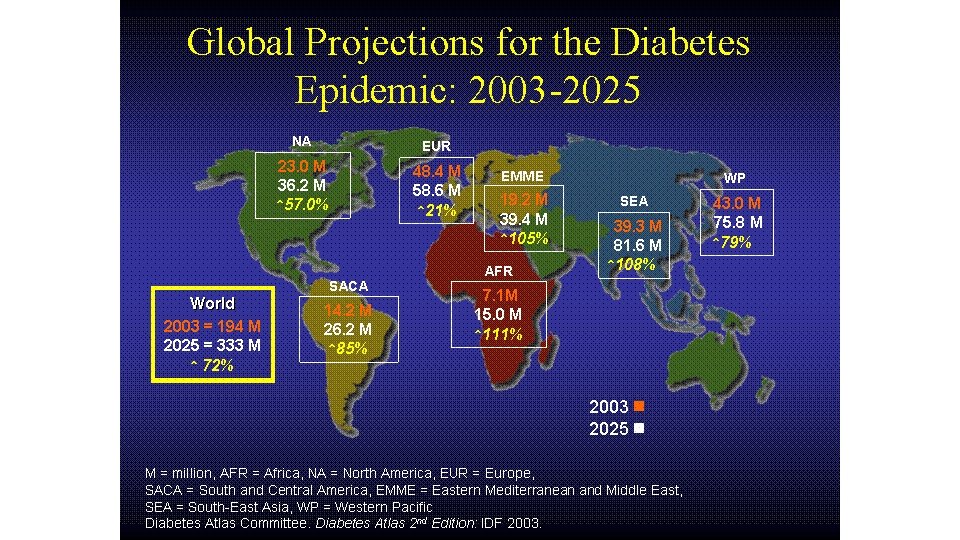
Metabolic Syndrome - Type 2 Diabetes
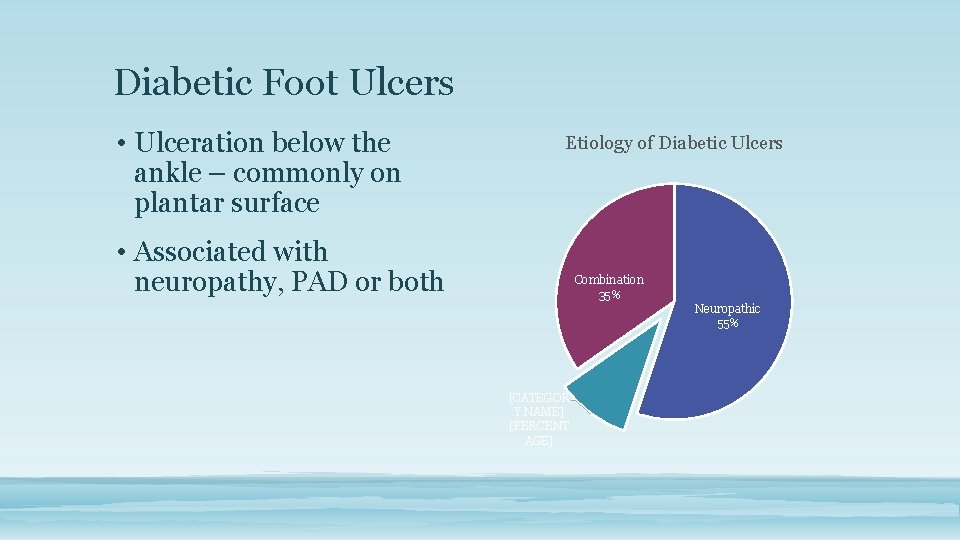
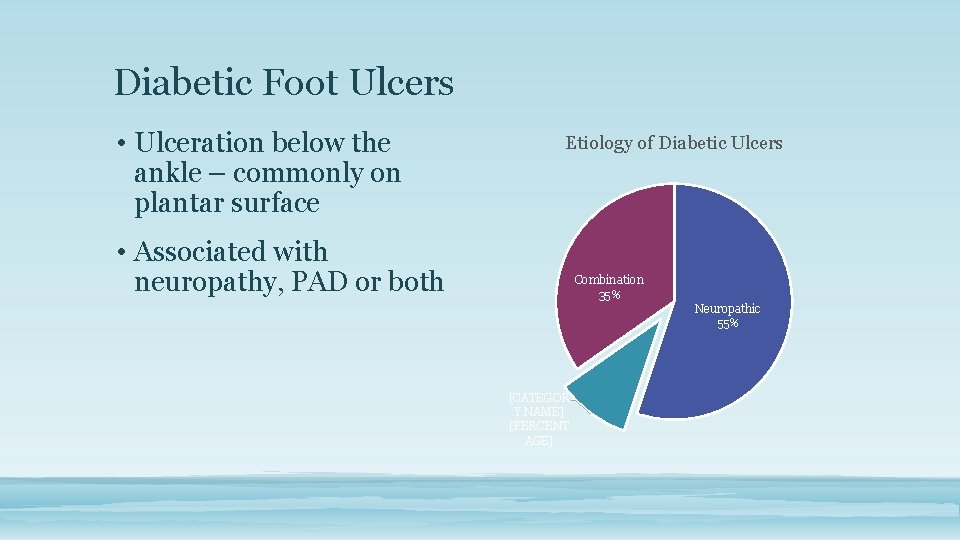
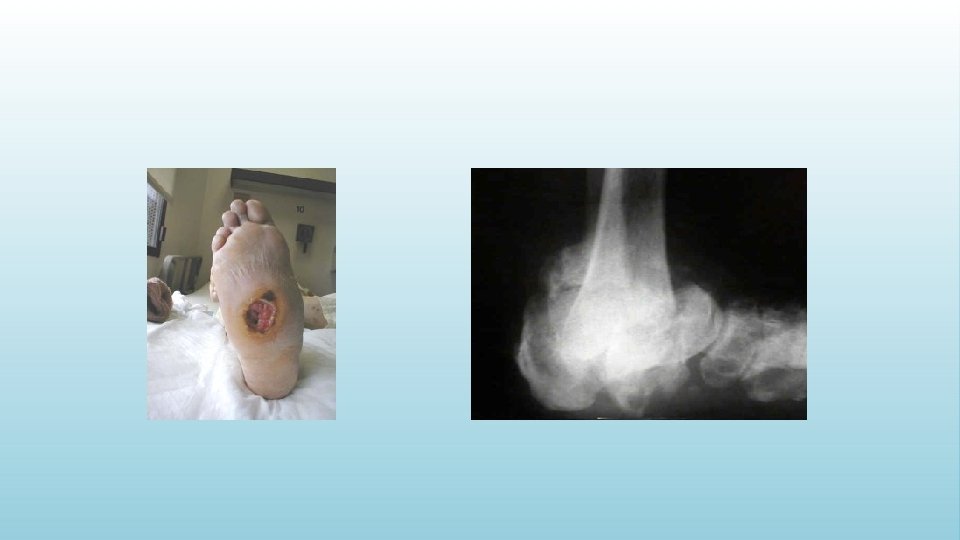
Diabetic Foot Ulcers • Ulceration below the ankle – commonly on plantar surface Etiology of Diabetic Ulcers • Associated with neuropathy, PAD or both Combination 35% Neuropathic 55% [CATEGOR Y NAME] [PERCENT AGE]
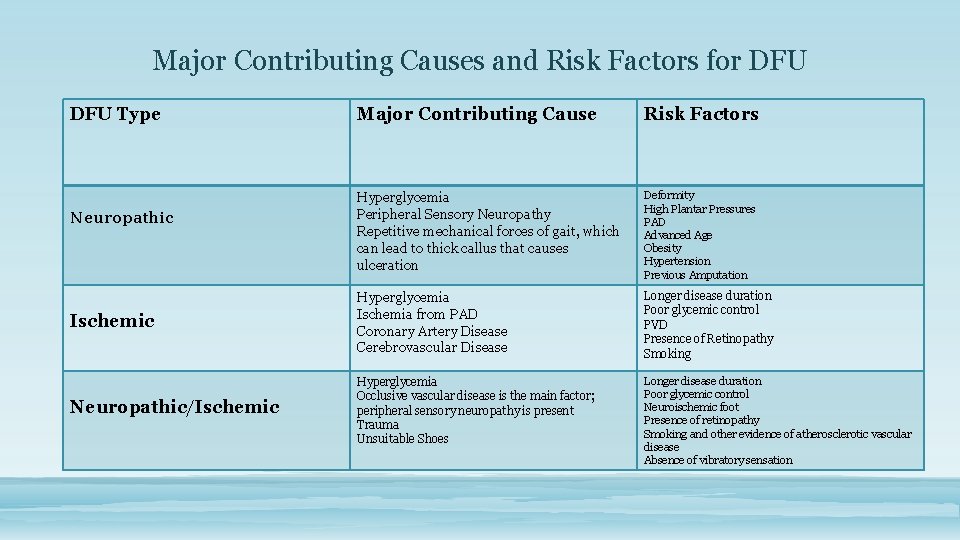
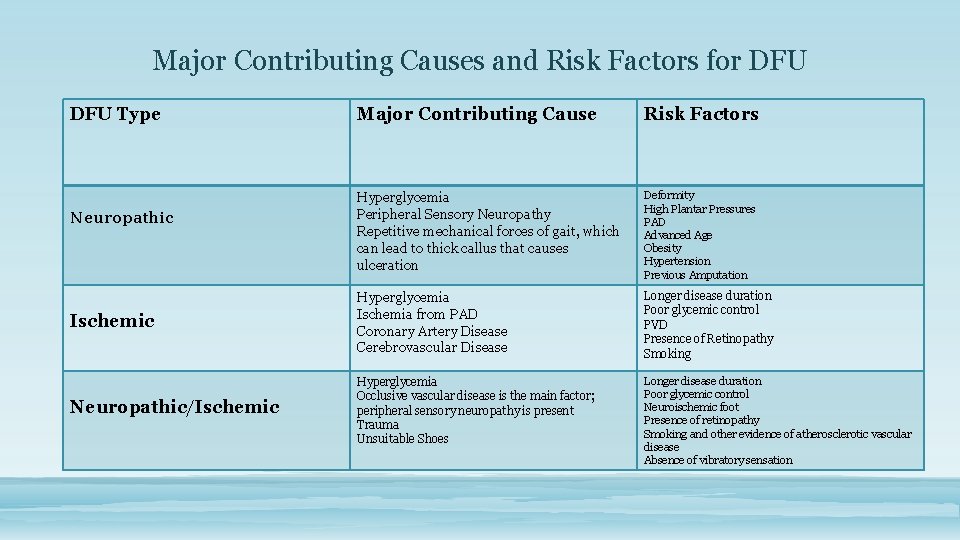
Major Contributing Causes and Risk Factors for DFU Type Major Contributing Cause Risk Factors Hyperglycemia Peripheral Sensory Neuropathy Repetitive mechanical forces of gait, which can lead to thick callus that causes ulceration Deformity High Plantar Pressures PAD Advanced Age Obesity Hypertension Previous Amputation Ischemic Hyperglycemia Ischemia from PAD Coronary Artery Disease Cerebrovascular Disease Longer disease duration Poor glycemic control PVD Presence of Retinopathy Smoking Neuropathic/Ischemic Hyperglycemia Occlusive vascular disease is the main factor; peripheral sensory neuropathy is present Trauma Unsuitable Shoes Longer disease duration Poor glycemic control Neuroischemic foot Presence of retinopathy Smoking and other evidence of atherosclerotic vascular disease Absence of vibratory sensation Neuropathic
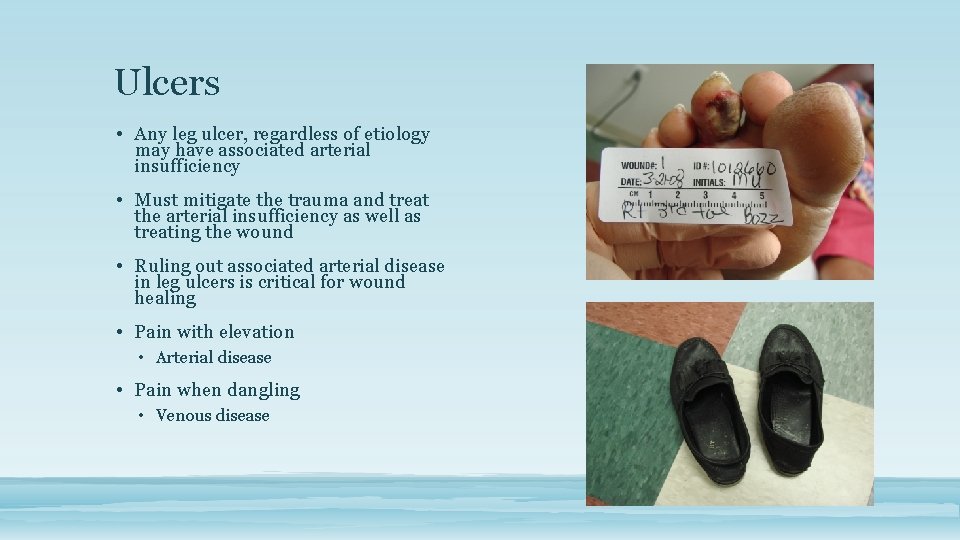
Ulcers • Any leg ulcer, regardless of etiology may have associated arterial insufficiency • Must mitigate the trauma and treat the arterial insufficiency as well as treating the wound • Ruling out associated arterial disease in leg ulcers is critical for wound healing • Pain with elevation • Arterial disease • Pain when dangling • Venous disease
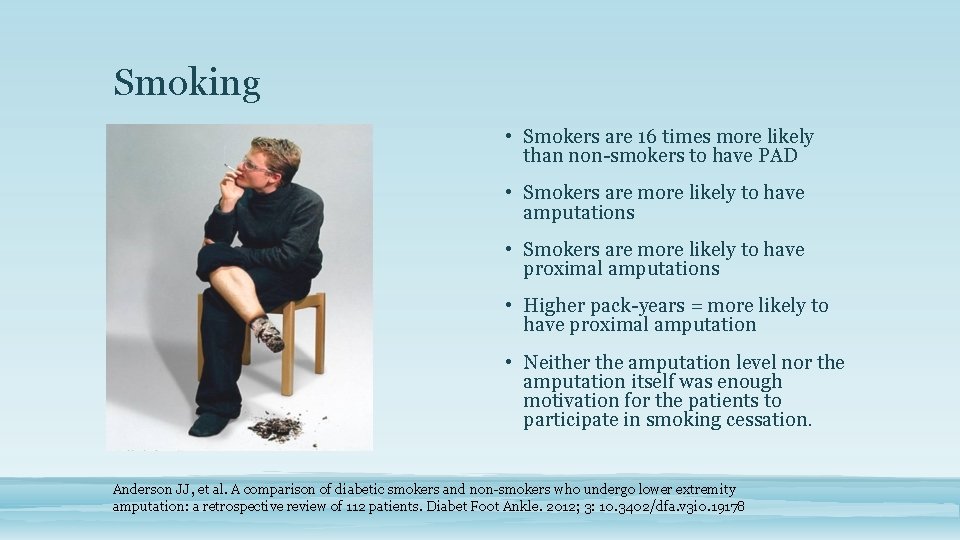
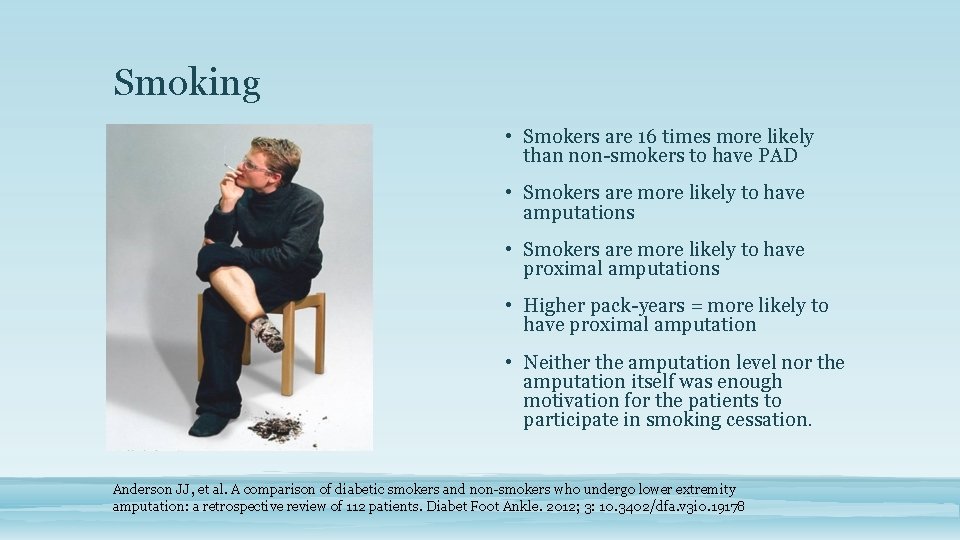
Smoking • Smokers are 16 times more likely than non-smokers to have PAD • Smokers are more likely to have amputations • Smokers are more likely to have proximal amputations • Higher pack-years = more likely to have proximal amputation • Neither the amputation level nor the amputation itself was enough motivation for the patients to participate in smoking cessation. Anderson JJ, et al. A comparison of diabetic smokers and non-smokers who undergo lower extremity amputation: a retrospective review of 112 patients. Diabet Foot Ankle. 2012; 3: 10. 3402/dfa. v 3 i 0. 19178
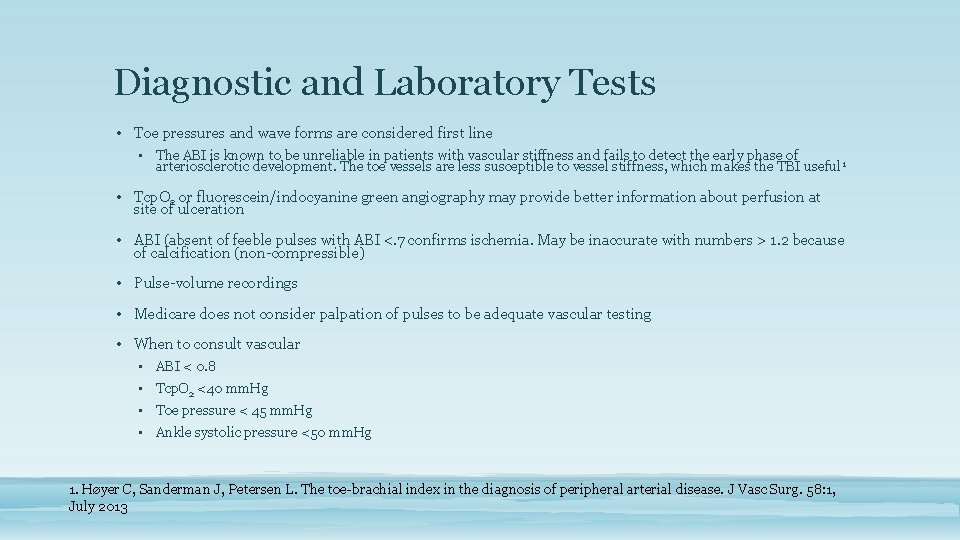
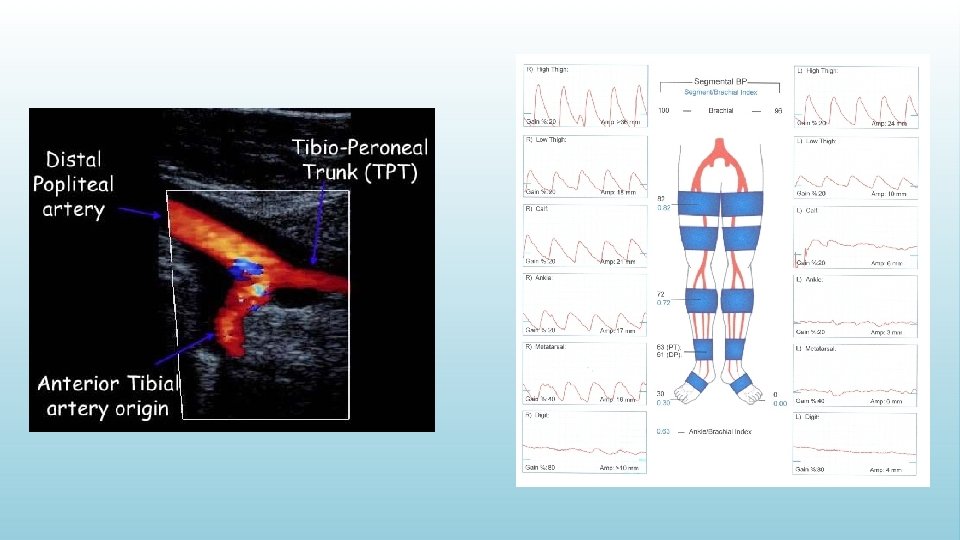
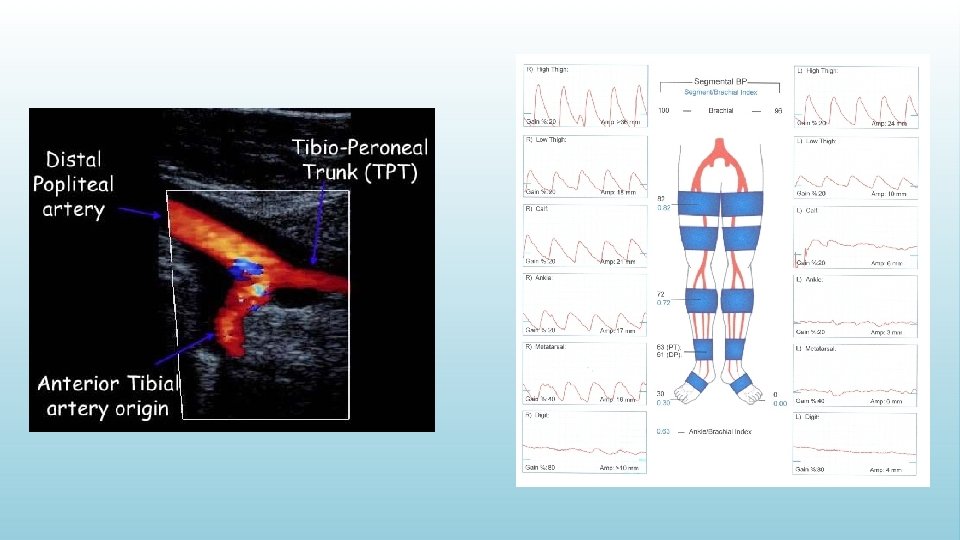
Diagnostic and Laboratory Tests • Toe pressures and wave forms are considered first line • The ABI is known to be unreliable in patients with vascular stiffness and fails to detect the early phase of arteriosclerotic development. The toe vessels are less susceptible to vessel stiffness, which makes the TBI useful 1 • Tcp. O 2 or fluorescein/indocyanine green angiography may provide better information about perfusion at site of ulceration • ABI (absent of feeble pulses with ABI <. 7 confirms ischemia. May be inaccurate with numbers > 1. 2 because of calcification (non-compressible) • Pulse-volume recordings • Medicare does not consider palpation of pulses to be adequate vascular testing • When to consult vascular • ABI < 0. 8 • Tcp. O 2 <40 mm. Hg • Toe pressure < 45 mm. Hg • Ankle systolic pressure <50 mm. Hg 1. Høyer C, Sanderman J, Petersen L. The toe-brachial index in the diagnosis of peripheral arterial disease. J Vasc Surg. 58: 1, July 2013
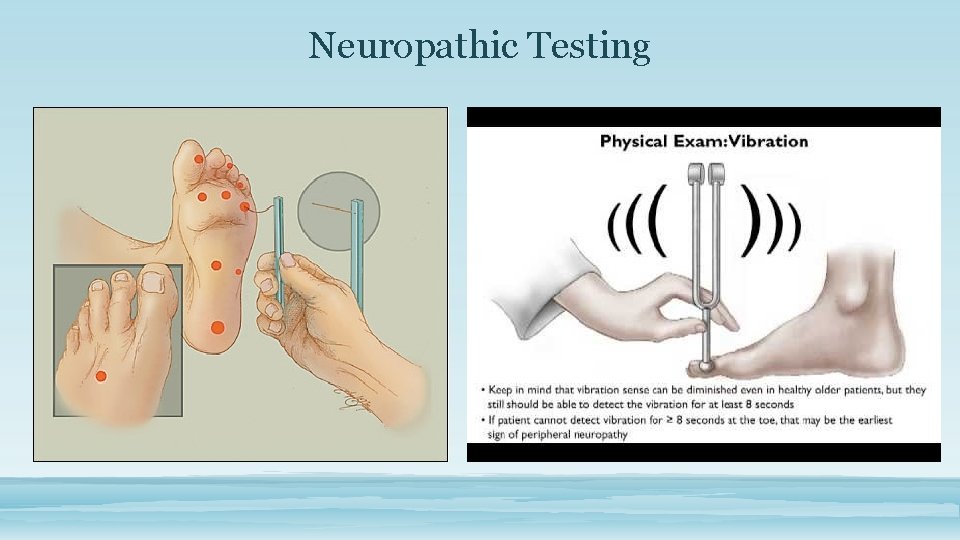
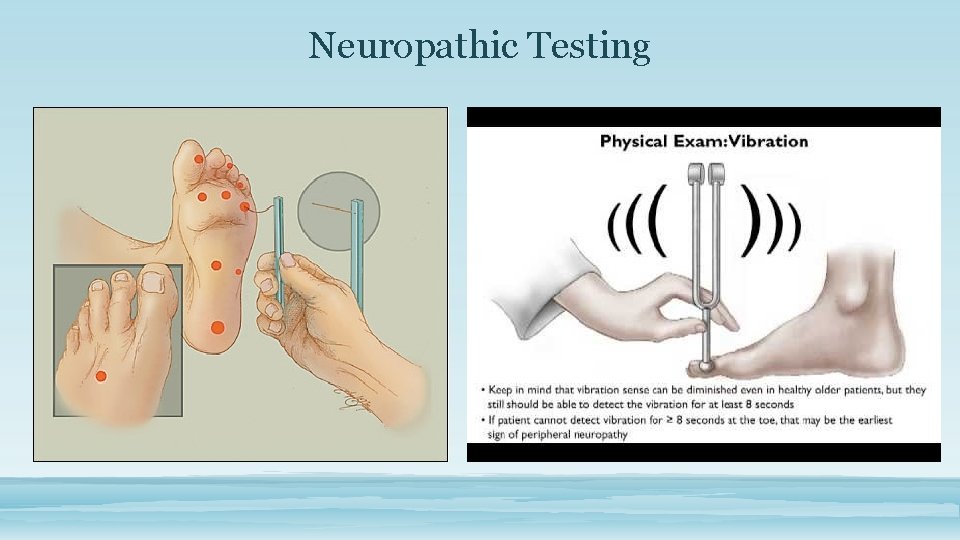
Neuropathic Testing
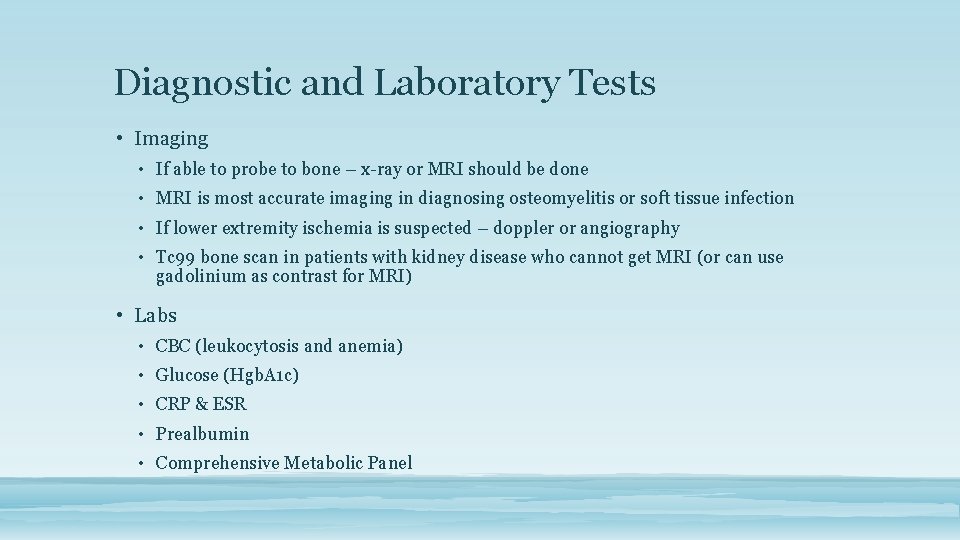
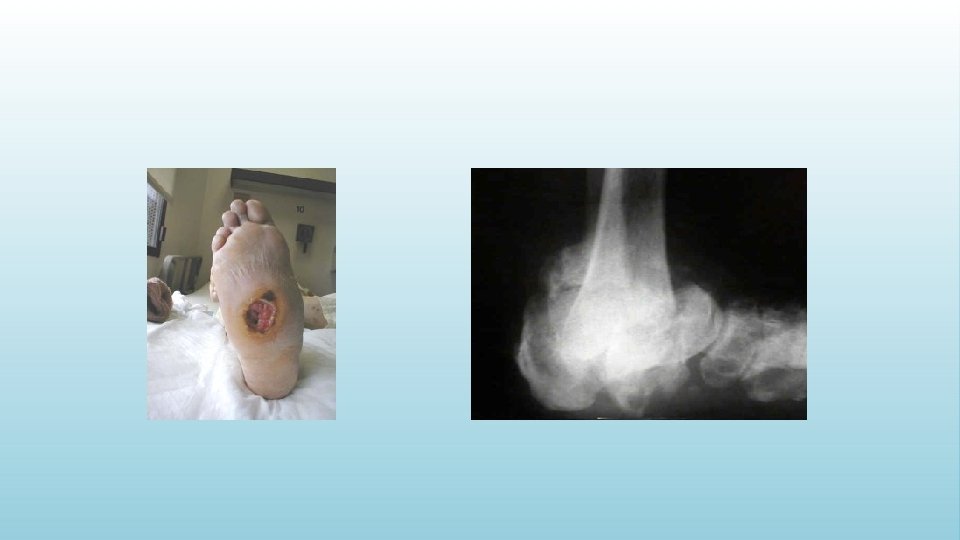
Diagnostic and Laboratory Tests • Imaging • If able to probe to bone – x-ray or MRI should be done • MRI is most accurate imaging in diagnosing osteomyelitis or soft tissue infection • If lower extremity ischemia is suspected – doppler or angiography • Tc 99 bone scan in patients with kidney disease who cannot get MRI (or can use gadolinium as contrast for MRI) • Labs • CBC (leukocytosis and anemia) • Glucose (Hgb. A 1 c) • CRP & ESR • Prealbumin • Comprehensive Metabolic Panel
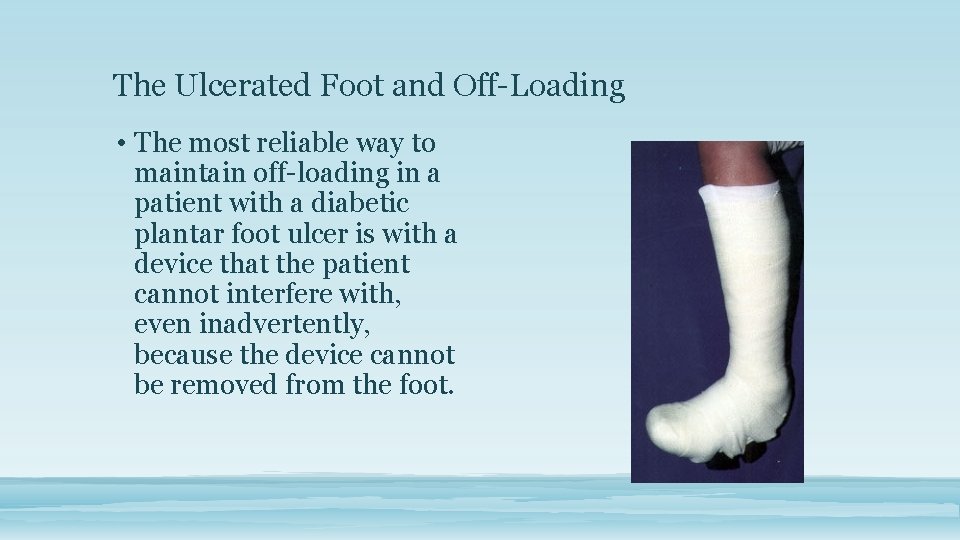
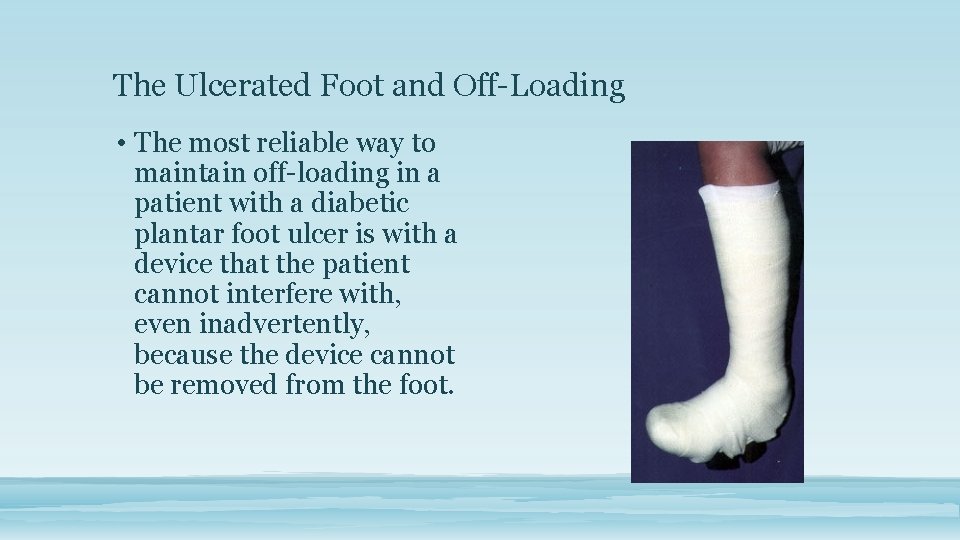
The Ulcerated Foot and Off-Loading • The most reliable way to maintain off-loading in a patient with a diabetic plantar foot ulcer is with a device that the patient cannot interfere with, even inadvertently, because the device cannot be removed from the foot.
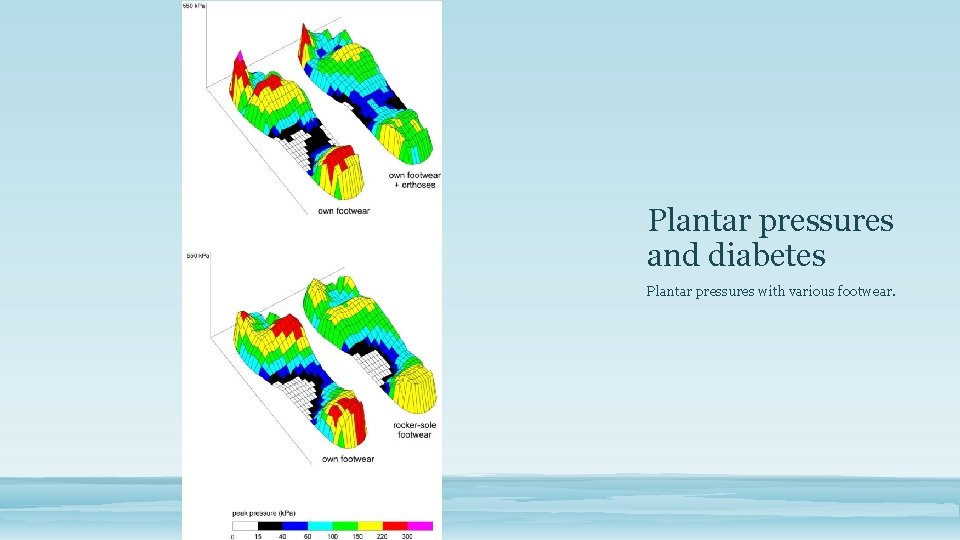
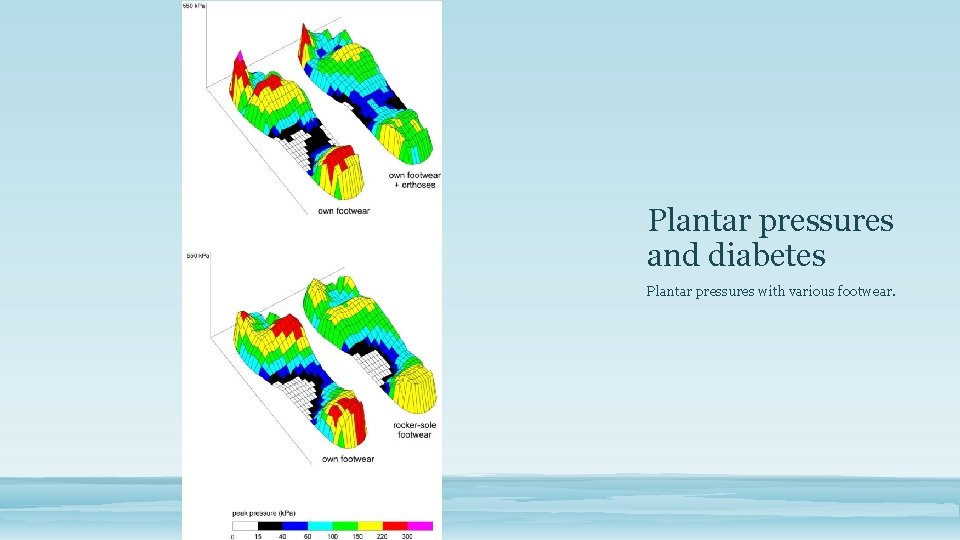
Plantar pressures and diabetes Plantar pressures with various footwear.
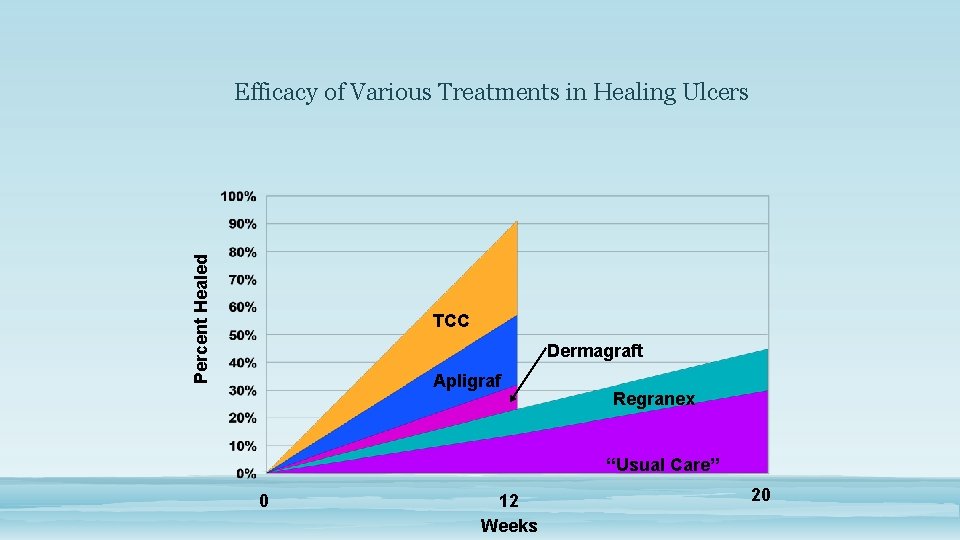
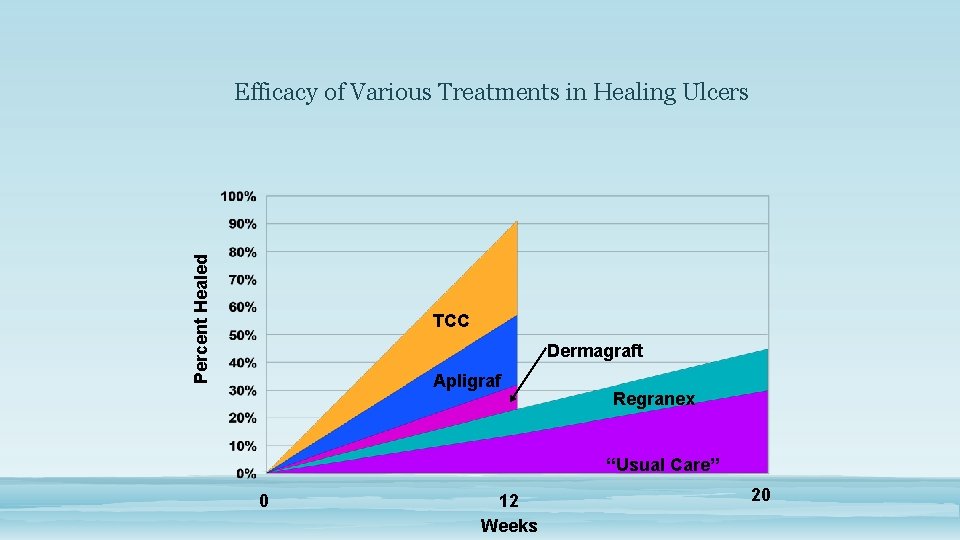
Percent Healed Efficacy of Various Treatments in Healing Ulcers TCC Dermagraft Apligraf Regranex “Usual Care” 0 12 Weeks 20
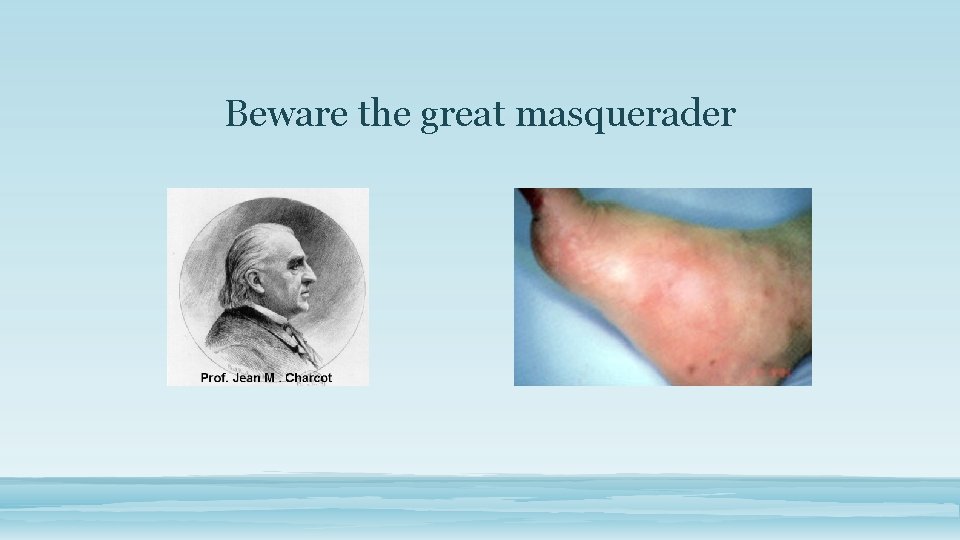
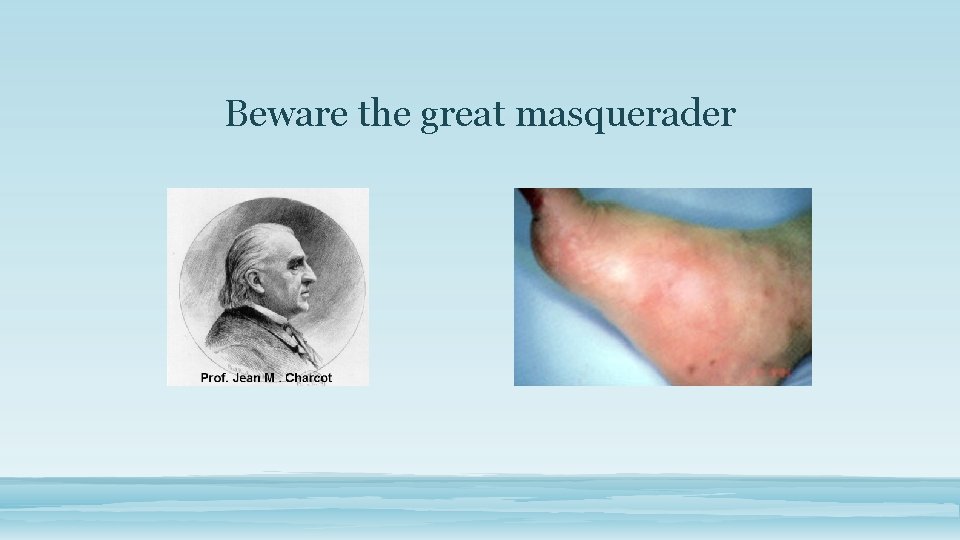
Beware the great masquerader
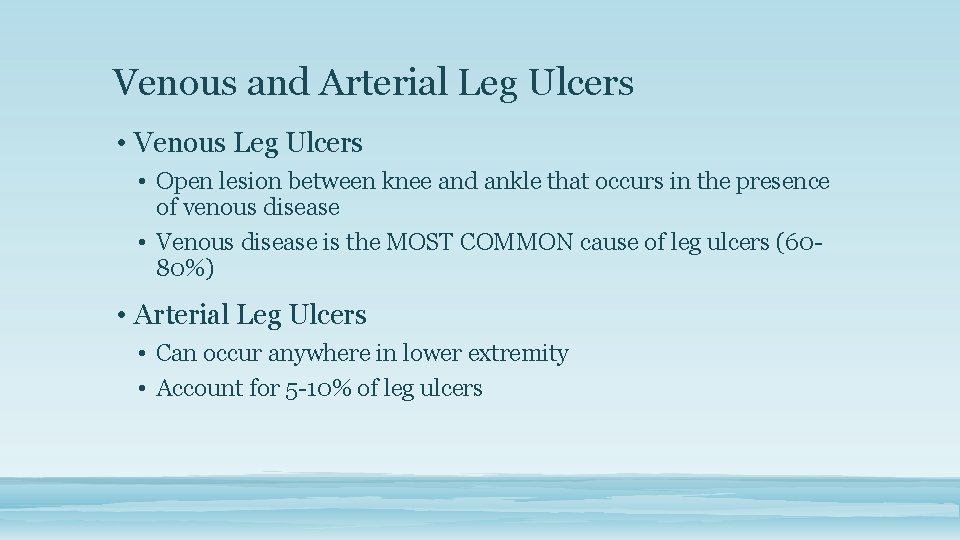
Venous and Arterial Leg Ulcers • Venous Leg Ulcers • Open lesion between knee and ankle that occurs in the presence of venous disease • Venous disease is the MOST COMMON cause of leg ulcers (6080%) • Arterial Leg Ulcers • Can occur anywhere in lower extremity • Account for 5 -10% of leg ulcers
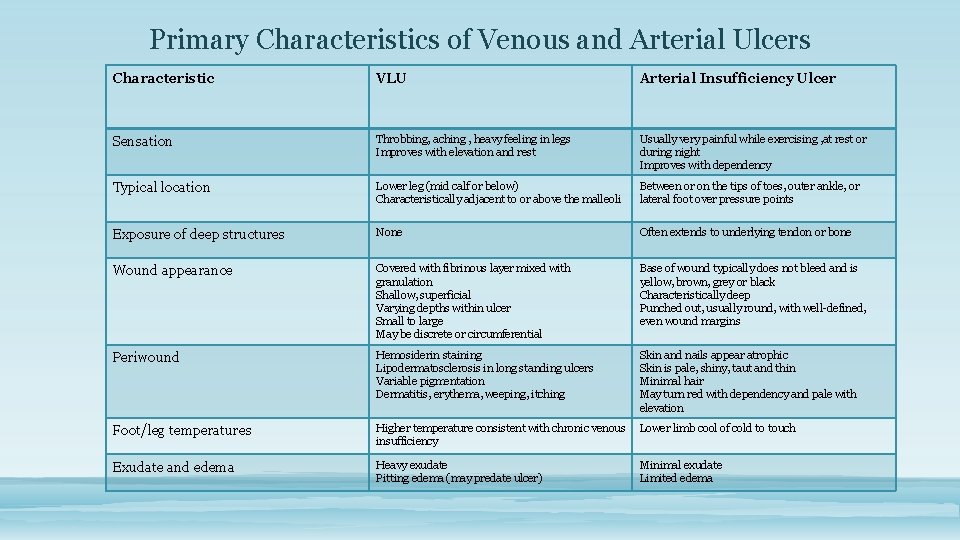
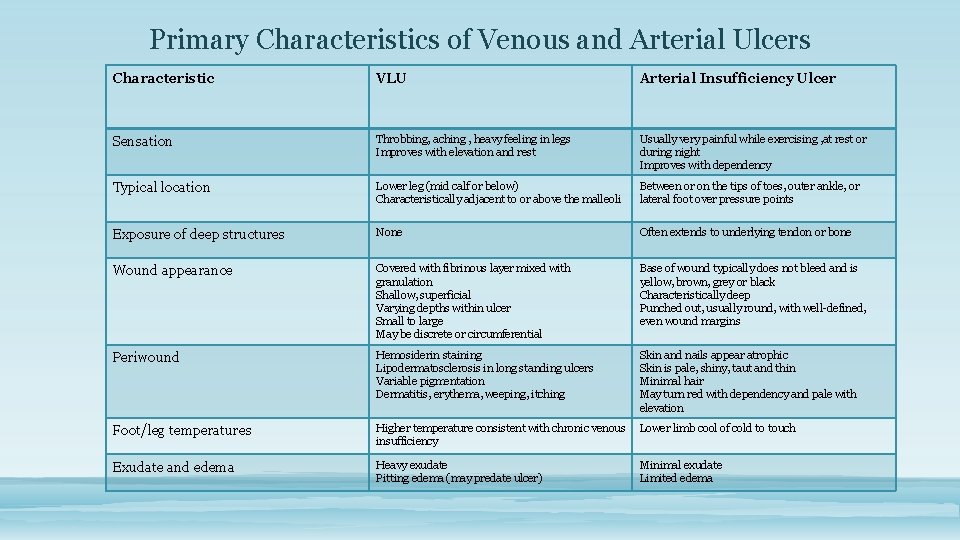
Primary Characteristics of Venous and Arterial Ulcers Characteristic VLU Arterial Insufficiency Ulcer Sensation Throbbing, aching , heavy feeling in legs Improves with elevation and rest Usually very painful while exercising , at rest or during night Improves with dependency Typical location Lower leg (mid calf or below) Characteristically adjacent to or above the malleoli Between or on the tips of toes, outer ankle, or lateral foot over pressure points Exposure of deep structures None Often extends to underlying tendon or bone Wound appearance Covered with fibrinous layer mixed with granulation Shallow, superficial Varying depths within ulcer Small to large May be discrete or circumferential Base of wound typically does not bleed and is yellow, brown, grey or black Characteristically deep Punched out, usually round, with well-defined, even wound margins Periwound Hemosiderin staining Lipodermatosclerosis in long standing ulcers Variable pigmentation Dermatitis, erythema, weeping, itching Skin and nails appear atrophic Skin is pale, shiny, taut and thin Minimal hair May turn red with dependency and pale with elevation Foot/leg temperatures Higher temperature consistent with chronic venous insufficiency Lower limb cool of cold to touch Exudate and edema Heavy exudate Pitting edema (may predate ulcer) Minimal exudate Limited edema
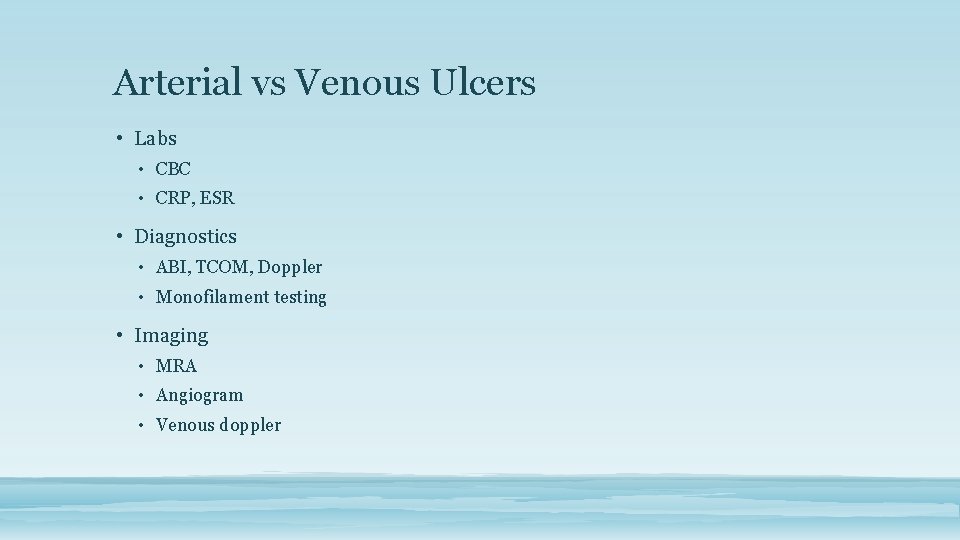
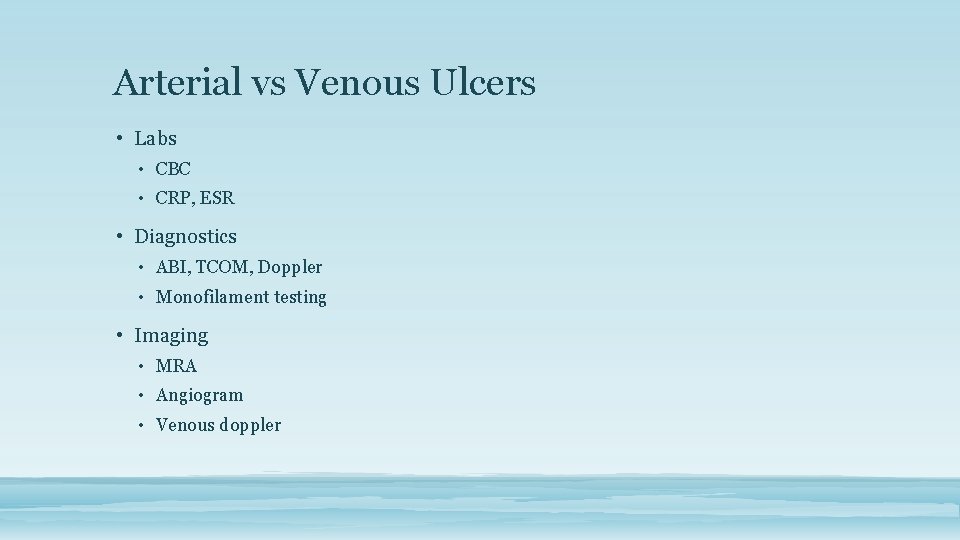
Arterial vs Venous Ulcers • Labs • CBC • CRP, ESR • Diagnostics • ABI, TCOM, Doppler • Monofilament testing • Imaging • MRA • Angiogram • Venous doppler
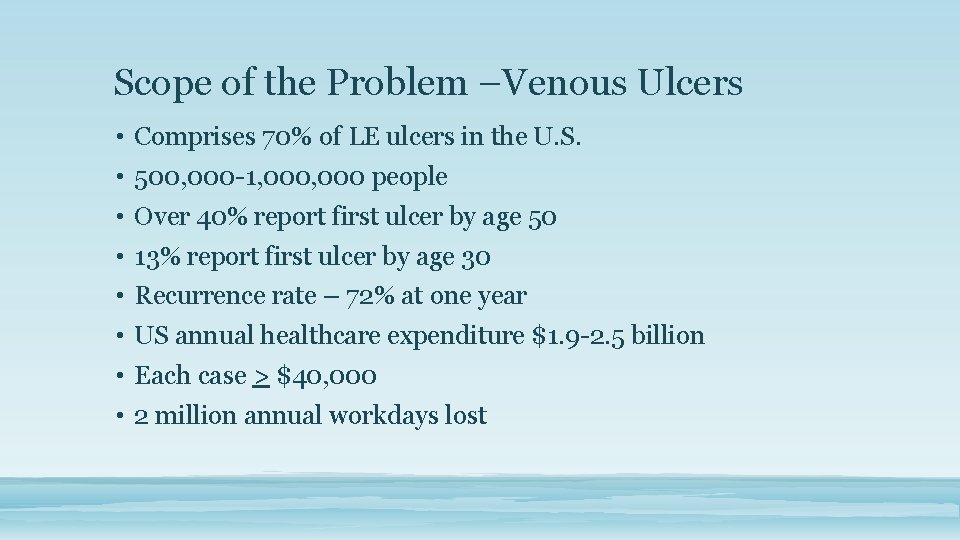
Scope of the Problem –Venous Ulcers • Comprises 70% of LE ulcers in the U. S. • 500, 000 -1, 000 people • Over 40% report first ulcer by age 50 • 13% report first ulcer by age 30 • Recurrence rate – 72% at one year • US annual healthcare expenditure $1. 9 -2. 5 billion • Each case > $40, 000 • 2 million annual workdays lost
Scope of the Problem • Median duration 9 months • 20% have not healed in one year • 66% had episodes of ulceration lasting 5 years • 2 -3% of total US healthcare budget
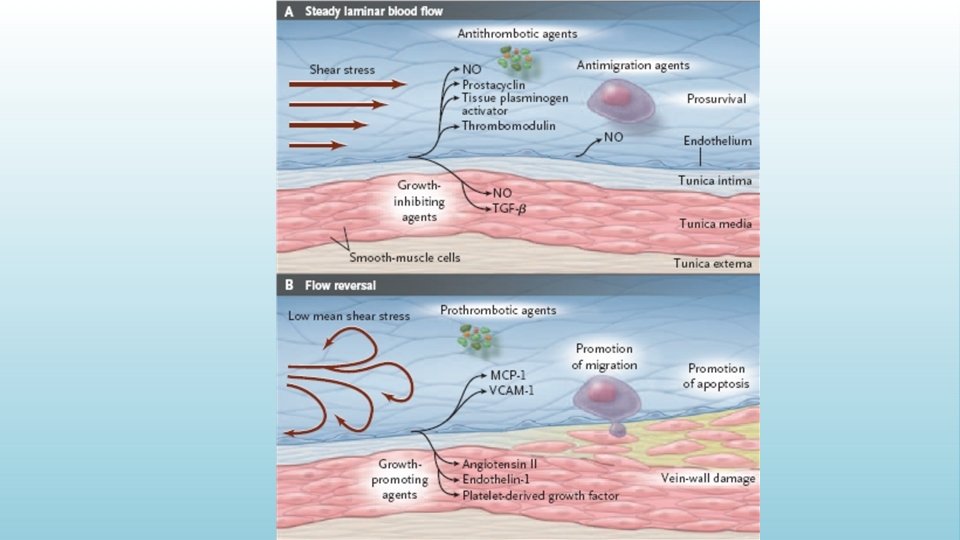
Etiology • Over 50% caused by previous DVT • Sedentary lifestyle • Obesity • Women • Standing • Men who smoke
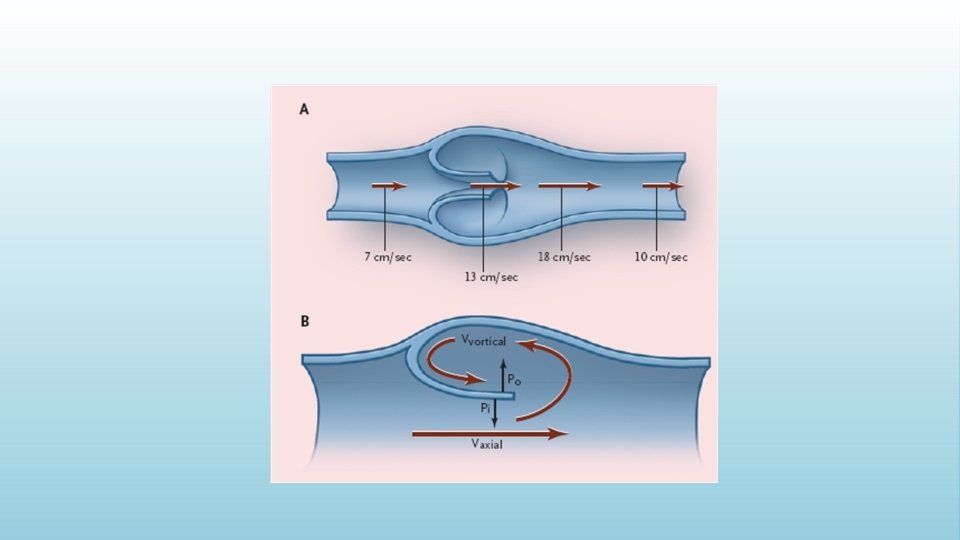
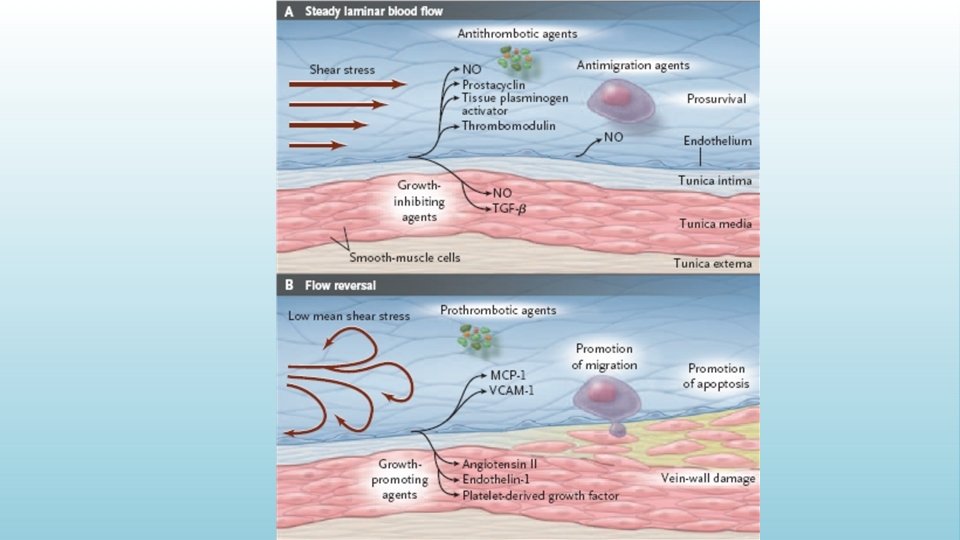
Etiology • Primary cause: • Reflux through incompetent valves • Venous outflow obstruction (DVT) • Superficial reflux – 45% • Deep reflux 12% • Mixed – 43%
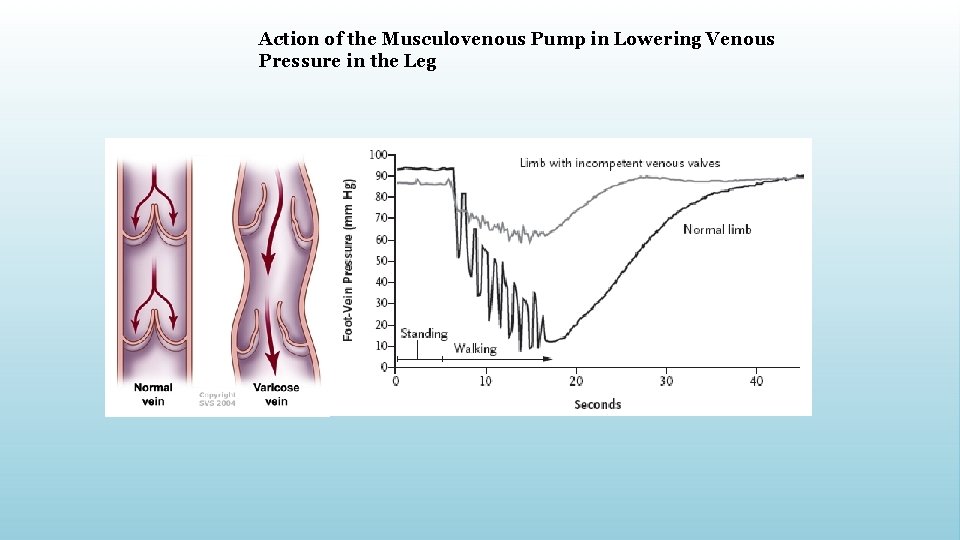
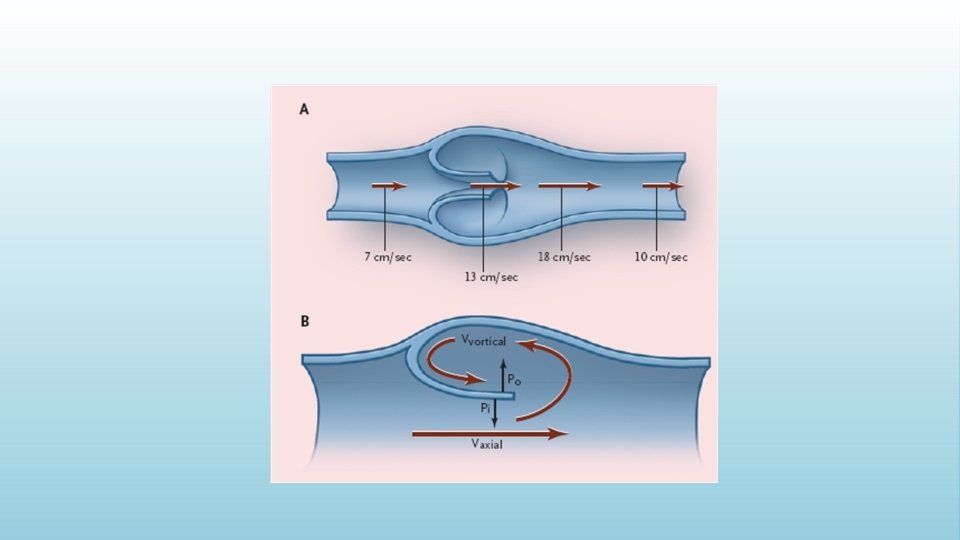
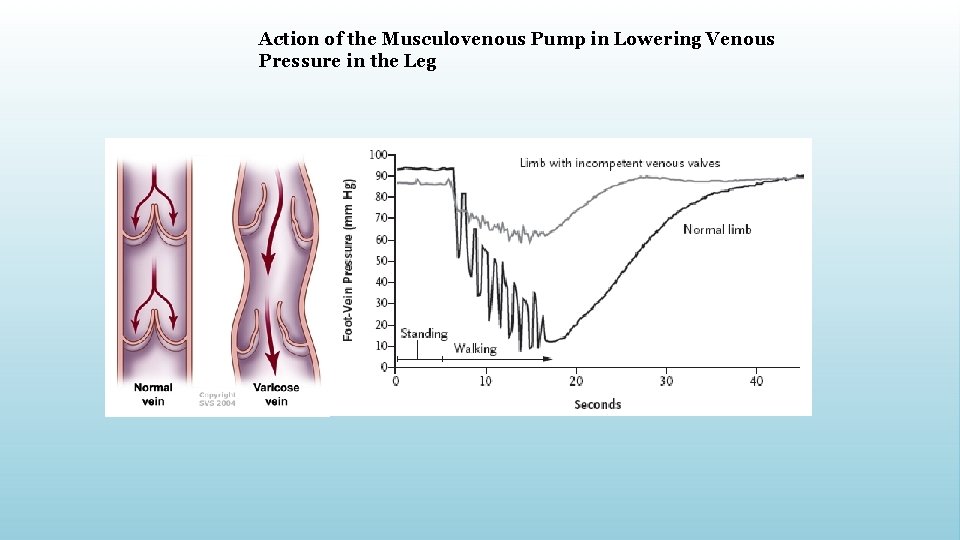
Action of the Musculovenous Pump in Lowering Venous Pressure in the Leg


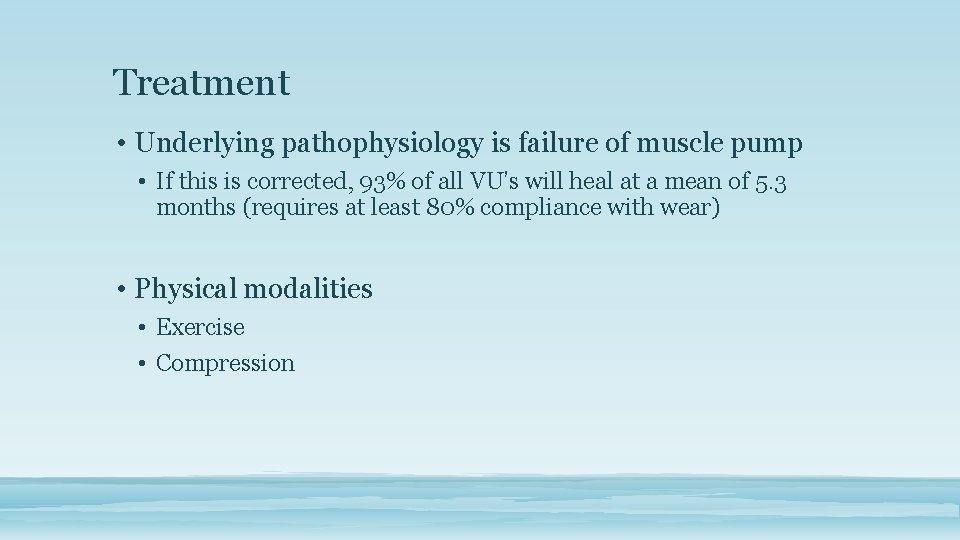
Treatment • Underlying pathophysiology is failure of muscle pump • If this is corrected, 93% of all VU’s will heal at a mean of 5. 3 months (requires at least 80% compliance with wear) • Physical modalities • Exercise • Compression
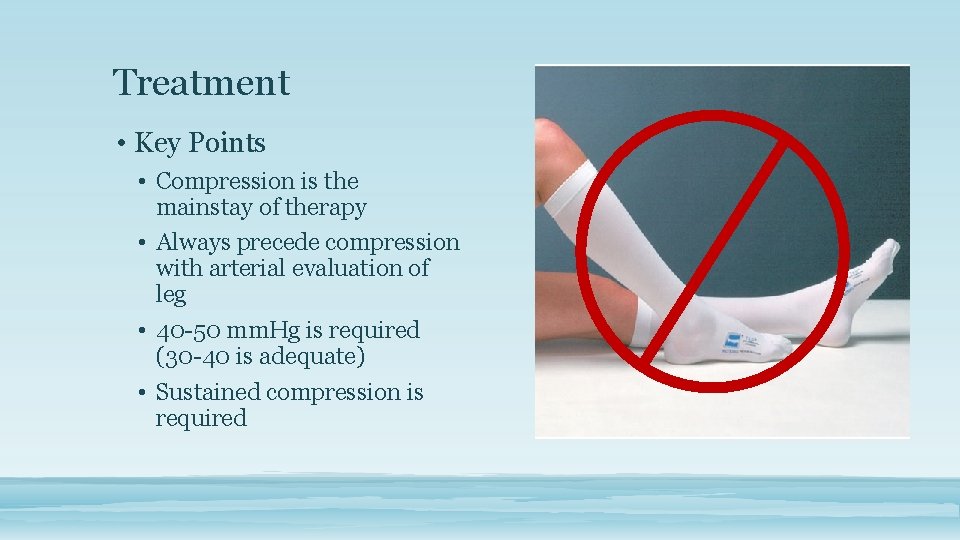
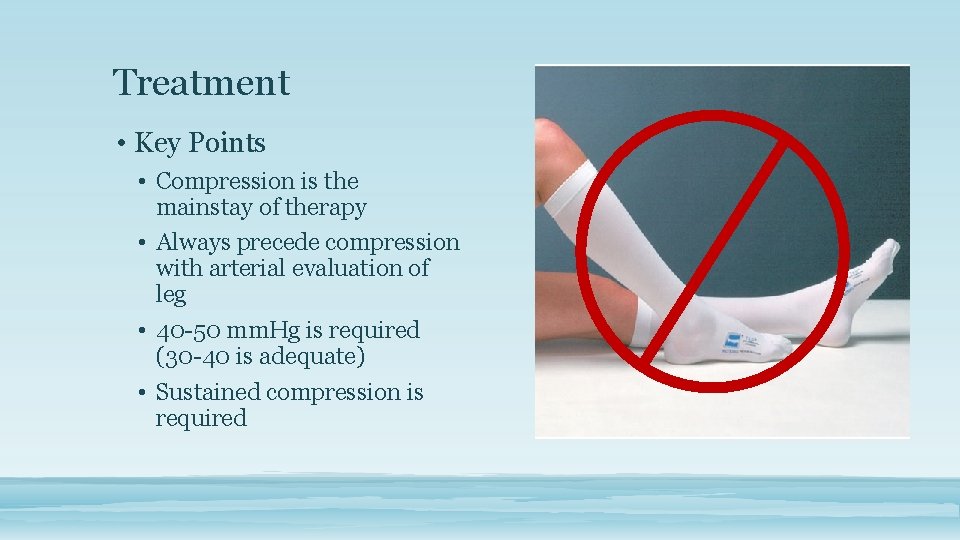
Treatment • Key Points • Compression is the mainstay of therapy • Always precede compression with arterial evaluation of leg • 40 -50 mm. Hg is required (30 -40 is adequate) • Sustained compression is required

Elastic vs. Inelastic Bandages • Inelastic Bandage • Unna’s Boot • Low resting pressure and high pressure on ambulation • Impregnated with • • • Zinc oxide Calamine Glycerin Sorbitol Mg silicate • Ace wrap or Coban over boot
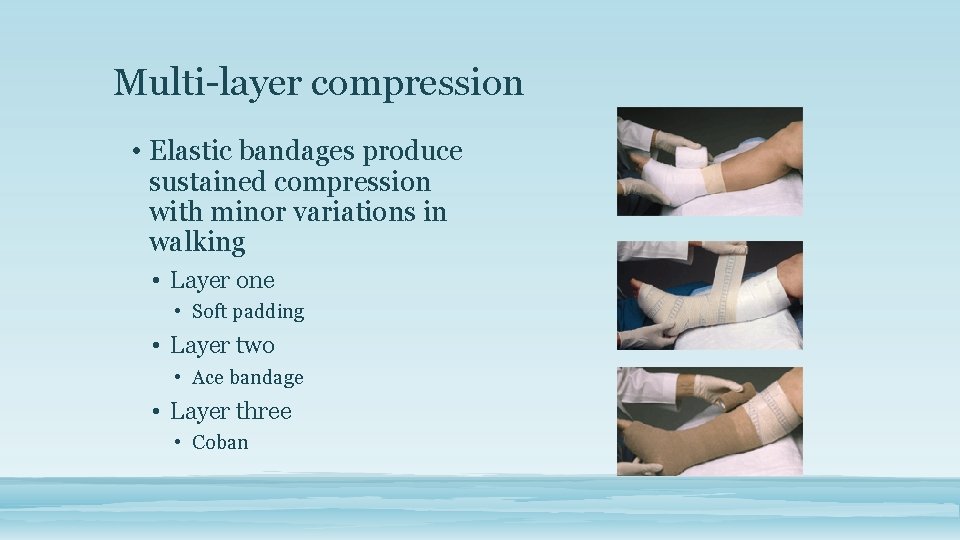
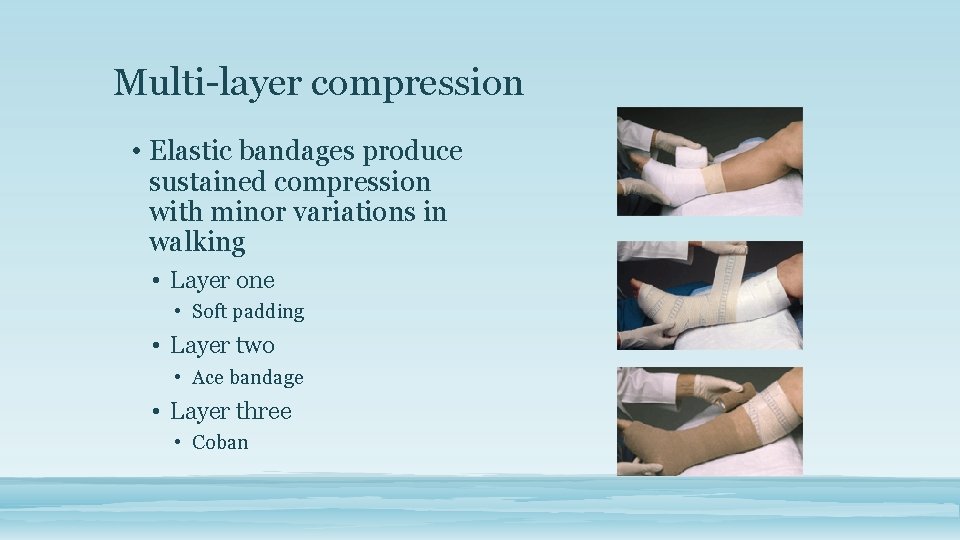
Multi-layer compression • Elastic bandages produce sustained compression with minor variations in walking • Layer one • Soft padding • Layer two • Ace bandage • Layer three • Coban
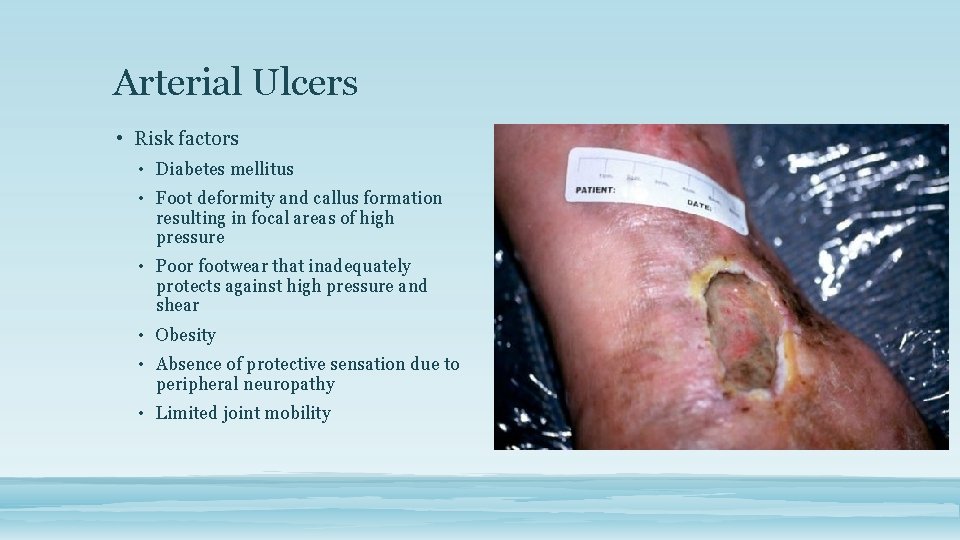
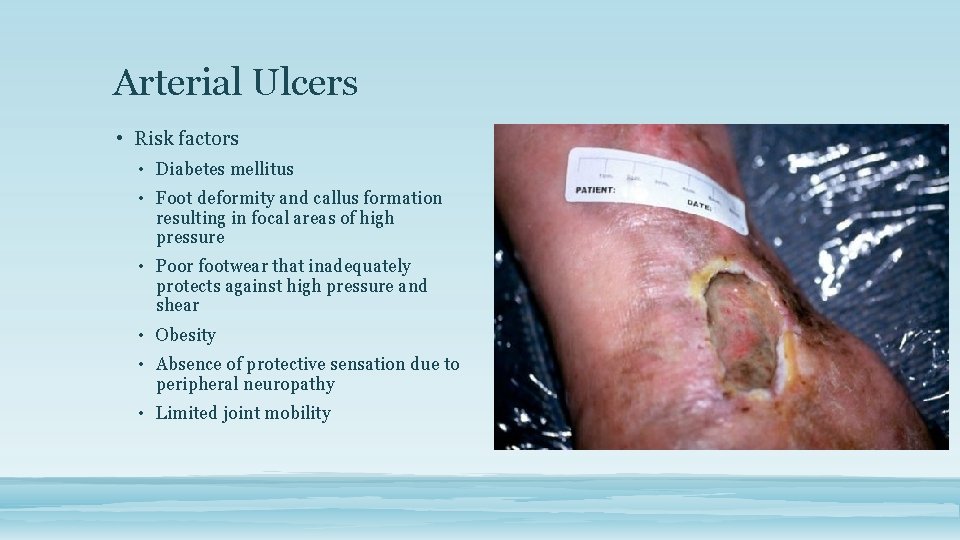
Arterial Ulcers • Risk factors • Diabetes mellitus • Foot deformity and callus formation resulting in focal areas of high pressure • Poor footwear that inadequately protects against high pressure and shear • Obesity • Absence of protective sensation due to peripheral neuropathy • Limited joint mobility
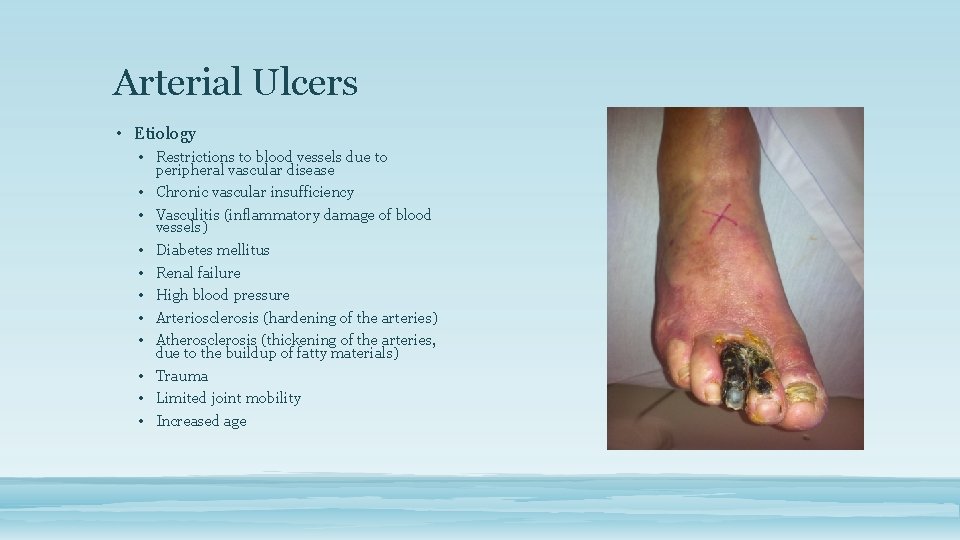
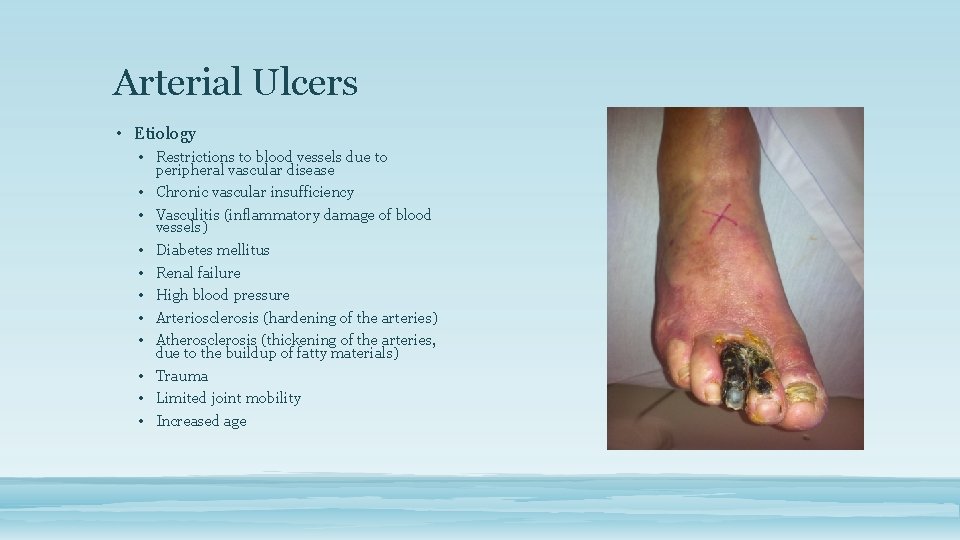
Arterial Ulcers • Etiology • Restrictions to blood vessels due to peripheral vascular disease • Chronic vascular insufficiency • Vasculitis (inflammatory damage of blood vessels) • Diabetes mellitus • Renal failure • High blood pressure • Arteriosclerosis (hardening of the arteries) • Atherosclerosis (thickening of the arteries, due to the buildup of fatty materials) • Trauma • Limited joint mobility • Increased age
Arterial Ulcers • Treatment • Examine feet (especially between the toes) and legs daily for any unusual changes in color or the development of sores. • Quit smoking. Smoking can harden or clog the arteries, leading to improper perfusion to the extremities. • Manage blood pressure, cholesterol, triglyceride and glucose levels. • Ensure that footwear is properly fitted to avoid points of rubbing or pressure. Avoid wearing constrictive socks. • Avoid crossing legs while sitting. • Avoid sitting or standing for extended periods. • Avoid cold temperature. • Protect legs and feet from injury and infection. • Exercise as frequently as is comfortable.
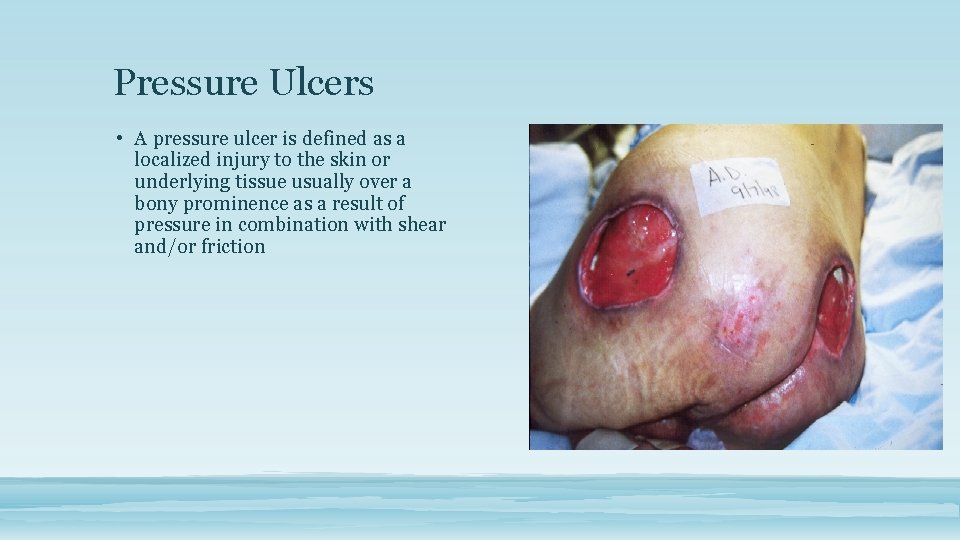
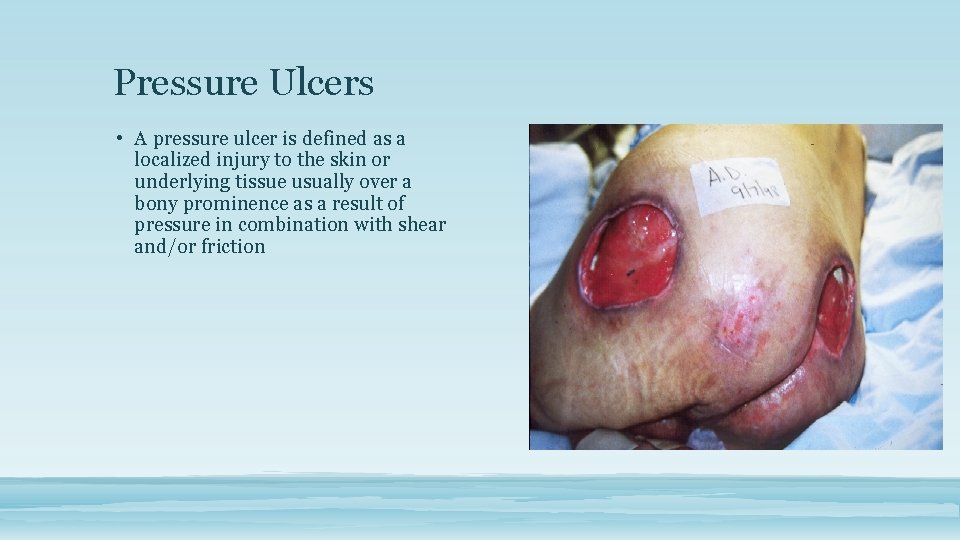
Pressure Ulcers • A pressure ulcer is defined as a localized injury to the skin or underlying tissue usually over a bony prominence as a result of pressure in combination with shear and/or friction
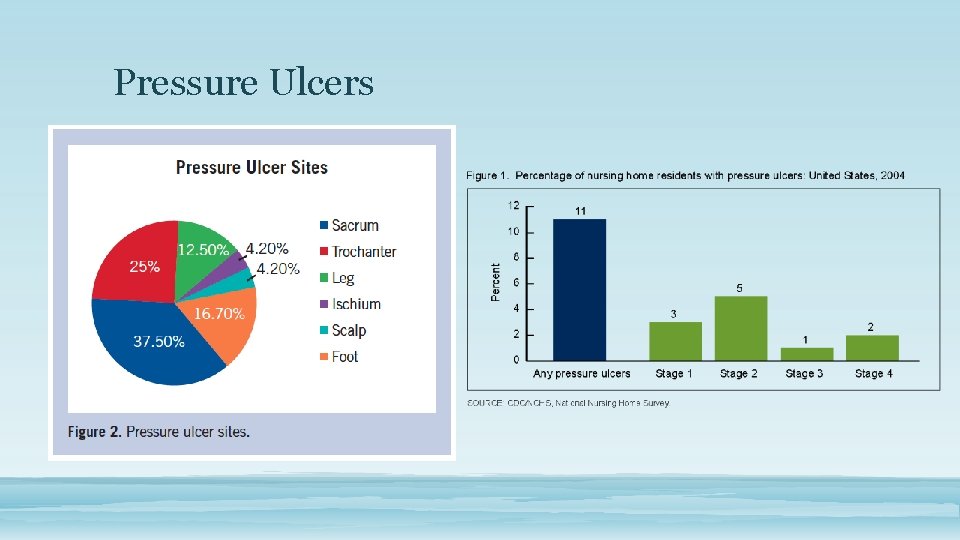
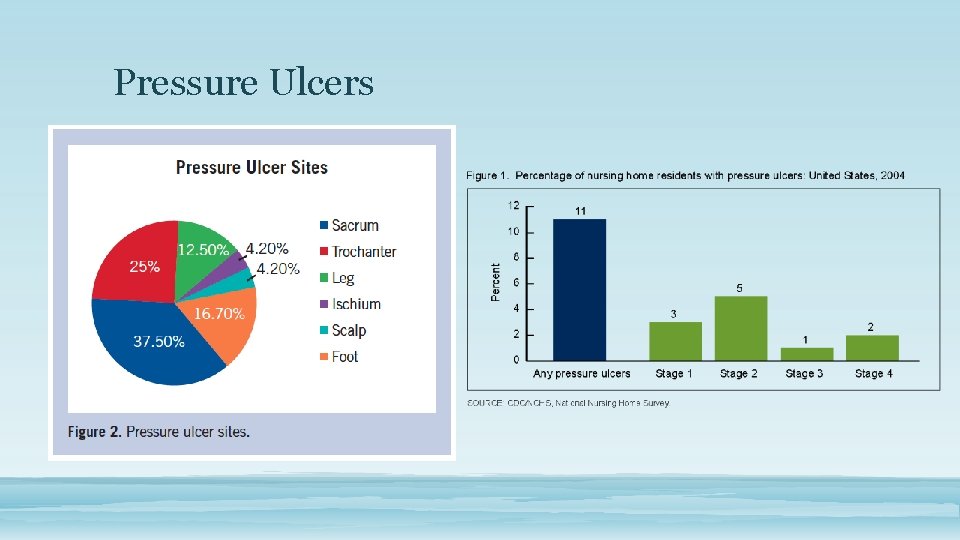
Pressure Ulcers
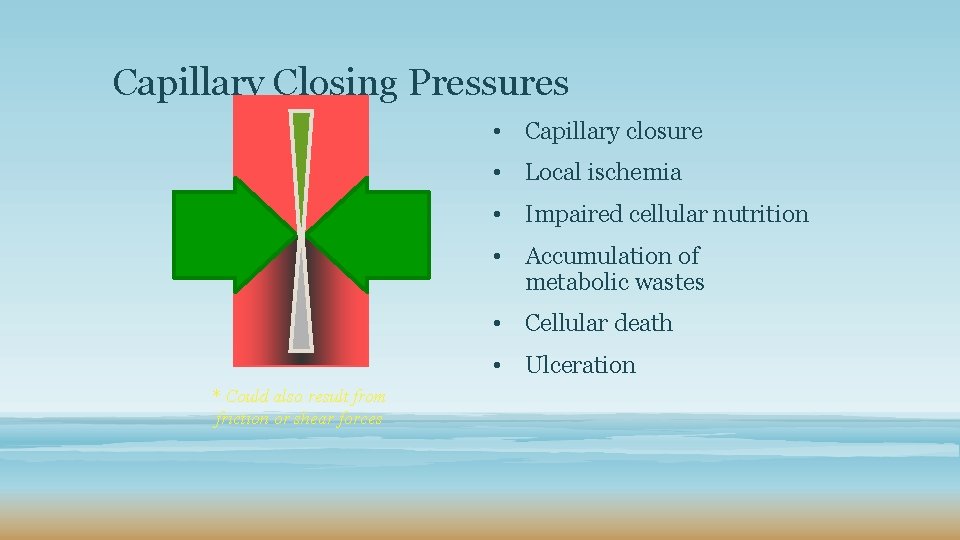
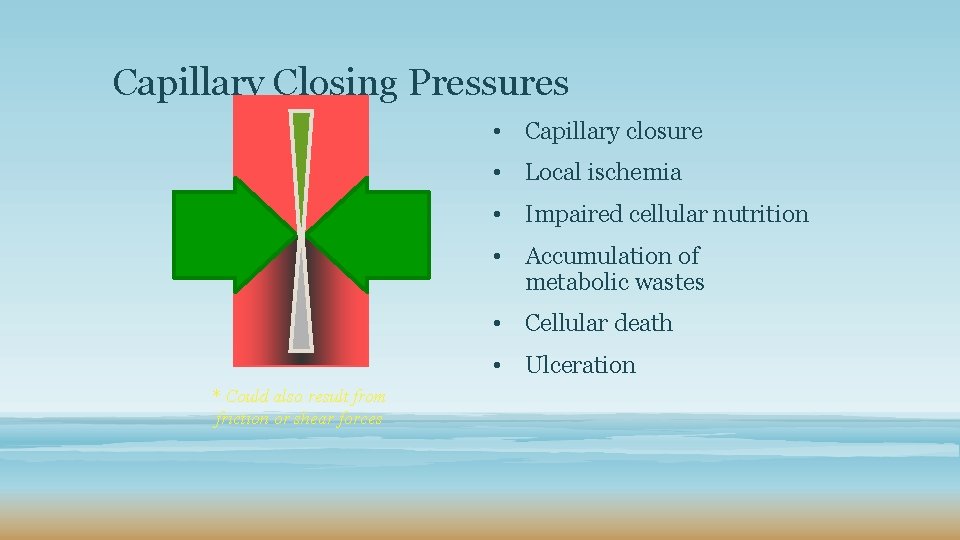
Capillary Closing Pressures • Capillary closure • Local ischemia • Impaired cellular nutrition • Accumulation of metabolic wastes • Cellular death • Ulceration * Could also result from friction or shear forces
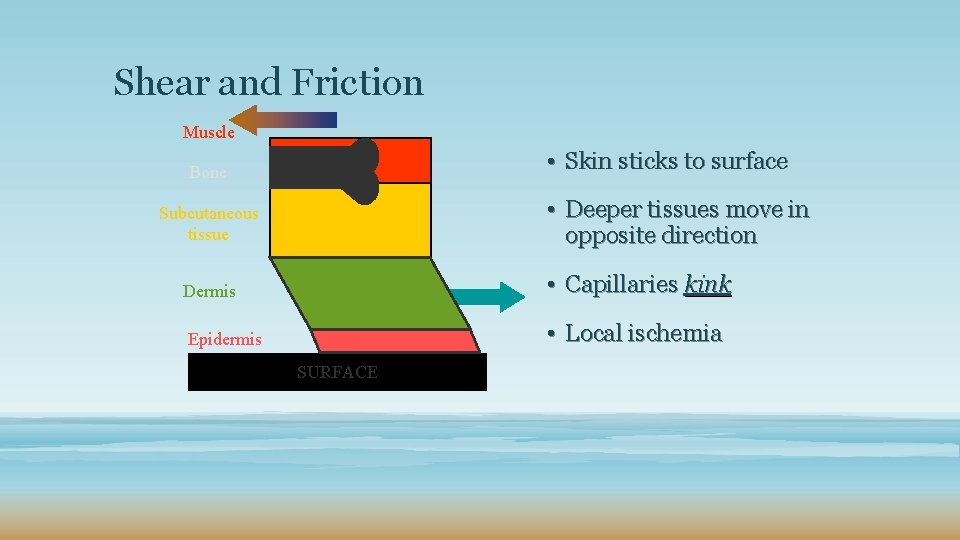
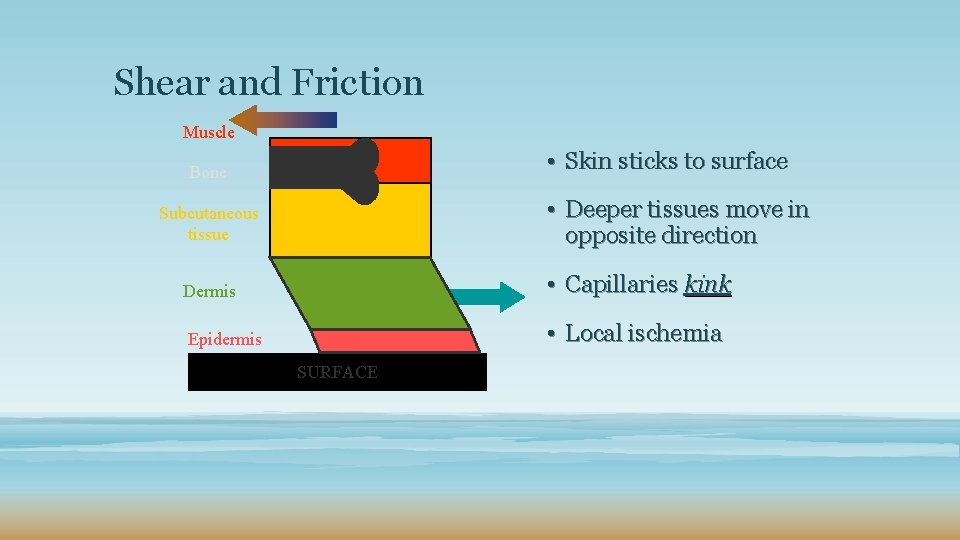
Shear and Friction Muscle • Skin sticks to surface Bone • Deeper tissues move in opposite direction Subcutaneous tissue Dermis • Capillaries kink Epidermis • Local ischemia SURFACE
Prevention is Key • Heel protectors • Paraplegic/quadriplegic • Post hip arthroplasty • Support surfaces (mattresses/beds) • Same as above • Altered mental status • Dehydrated or malnourished
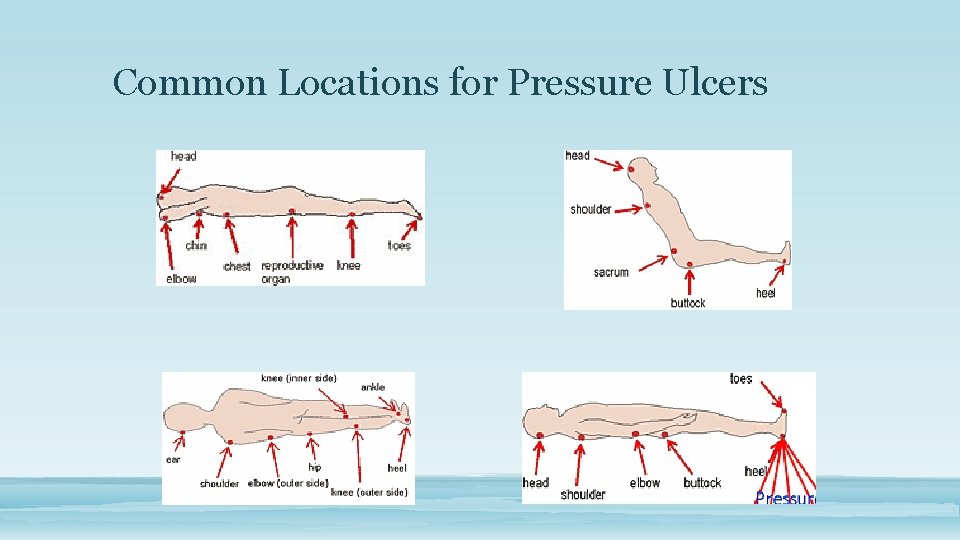
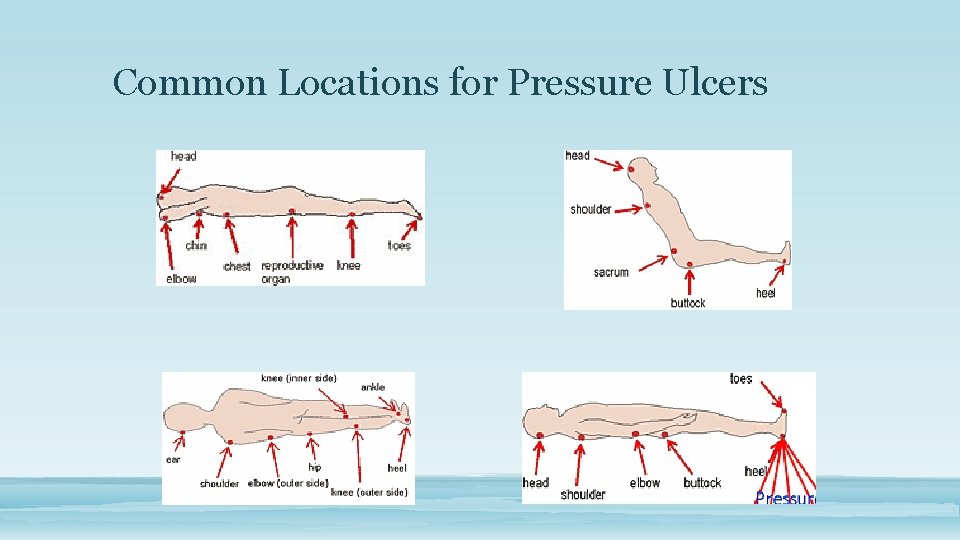
Common Locations for Pressure Ulcers
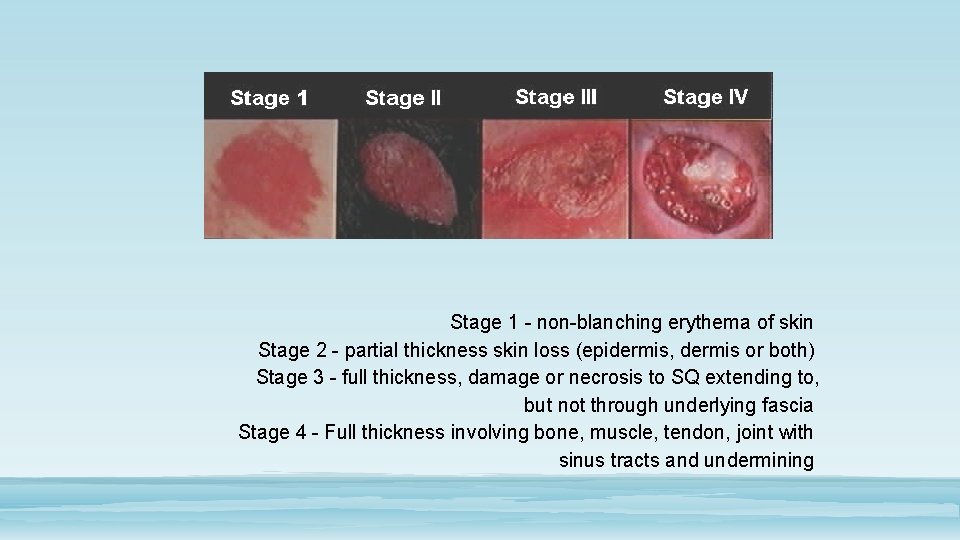
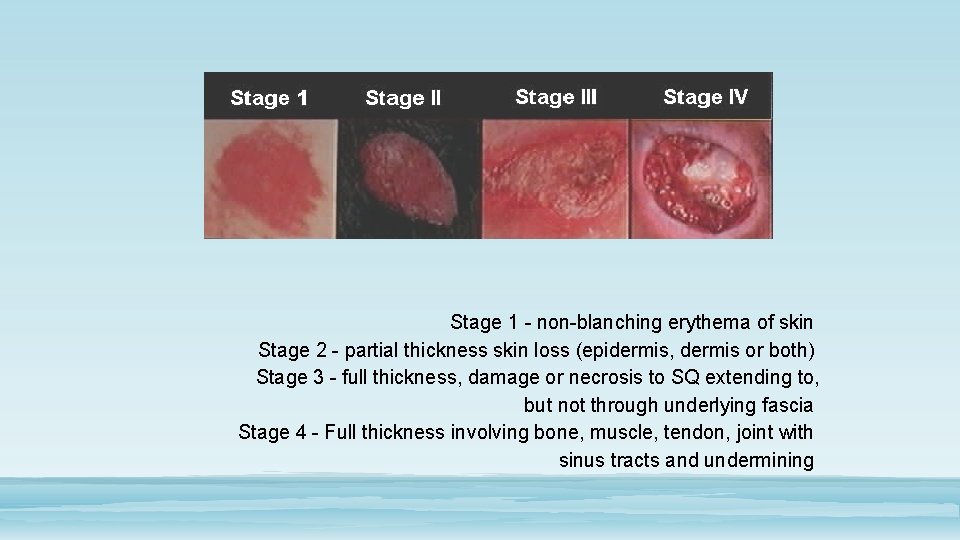
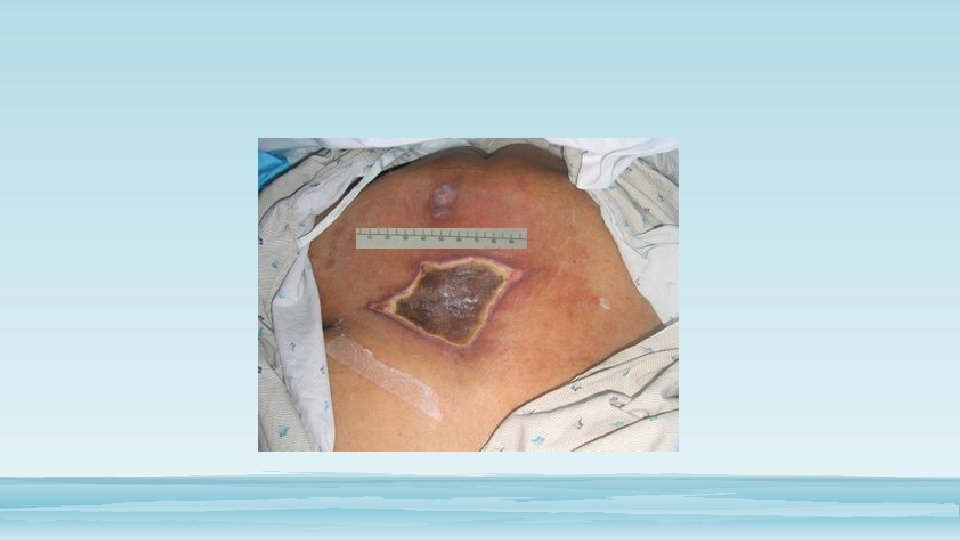
Stage 1 - non-blanching erythema of skin Stage 2 - partial thickness skin loss (epidermis, dermis or both) Stage 3 - full thickness, damage or necrosis to SQ extending to, but not through underlying fascia Stage 4 - Full thickness involving bone, muscle, tendon, joint with sinus tracts and undermining
The Deadly Sins of Staging • The Unstageable Wound • The Deep Tissue Injury (infarction of skin) • Reverse Staging • Shearing • Sepsis
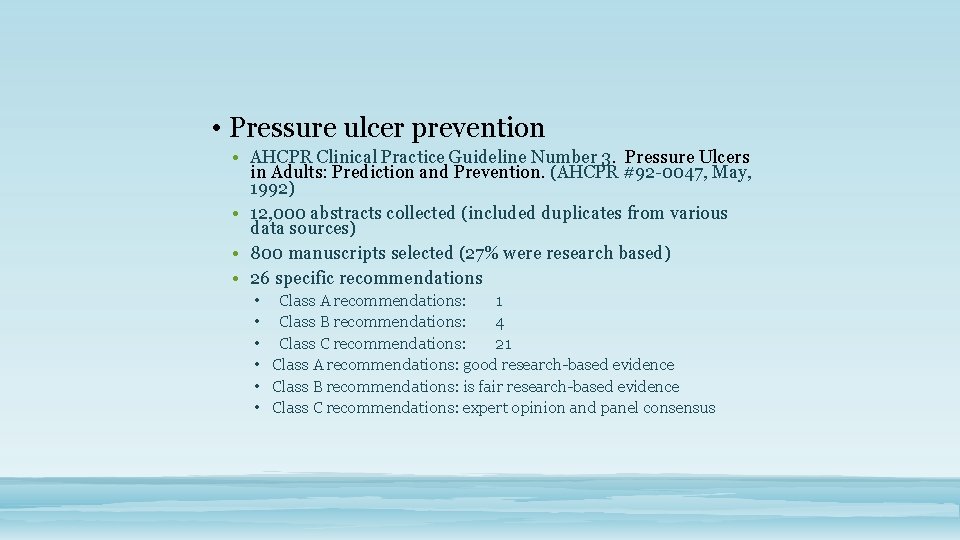
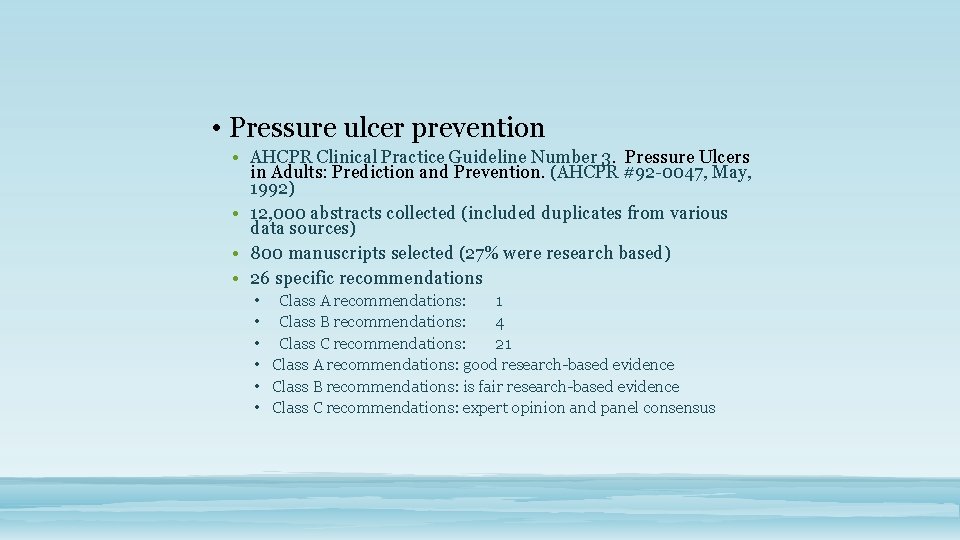
• Pressure ulcer prevention • AHCPR Clinical Practice Guideline Number 3. Pressure Ulcers in Adults: Prediction and Prevention. (AHCPR #92 -0047, May, 1992) • 12, 000 abstracts collected (included duplicates from various data sources) • 800 manuscripts selected (27% were research based) • 26 specific recommendations • Class A recommendations: 1 • Class B recommendations: 4 • Class C recommendations: 21 • Class A recommendations: good research-based evidence • Class B recommendations: is fair research-based evidence • Class C recommendations: expert opinion and panel consensus
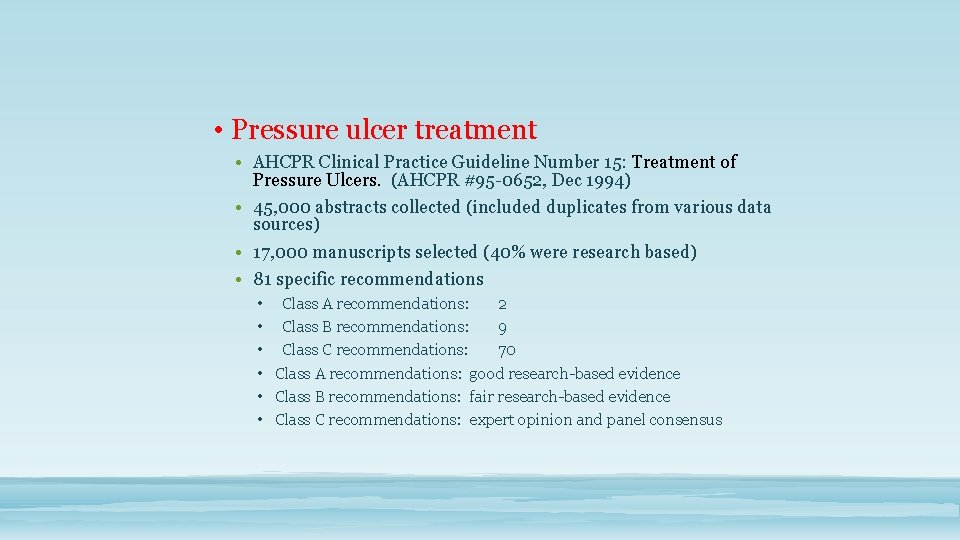
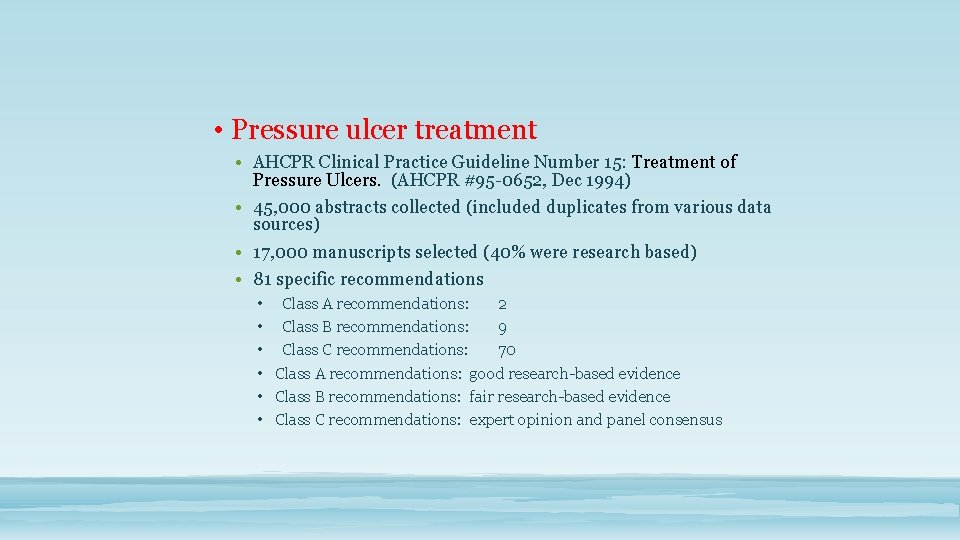
• Pressure ulcer treatment • AHCPR Clinical Practice Guideline Number 15: Treatment of Pressure Ulcers. (AHCPR #95 -0652, Dec 1994) • 45, 000 abstracts collected (included duplicates from various data sources) • 17, 000 manuscripts selected (40% were research based) • 81 specific recommendations • Class A recommendations: 2 • Class B recommendations: 9 • Class C recommendations: 70 • Class A recommendations: good research-based evidence • Class B recommendations: fair research-based evidence • Class C recommendations: expert opinion and panel consensus
Development of Pressure Ulcers Inside out OR Outside in
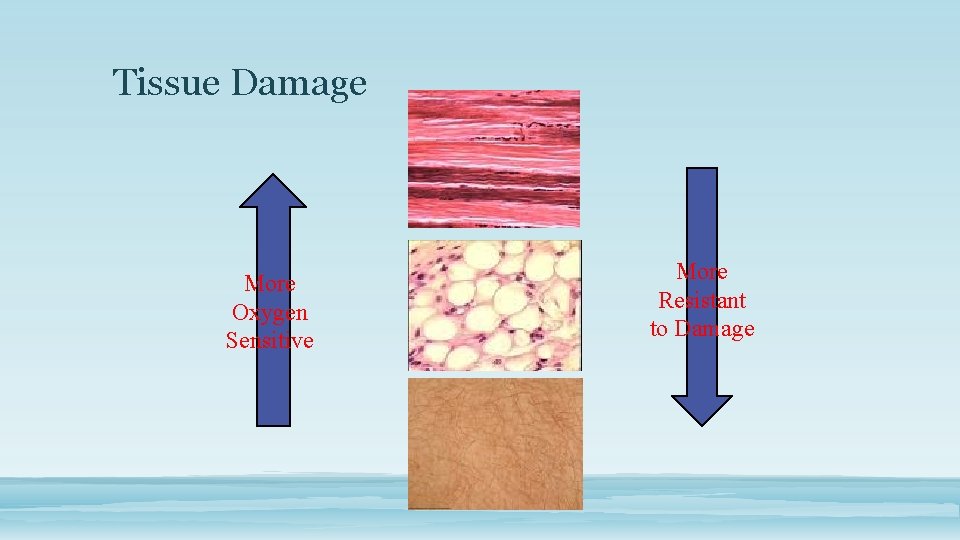
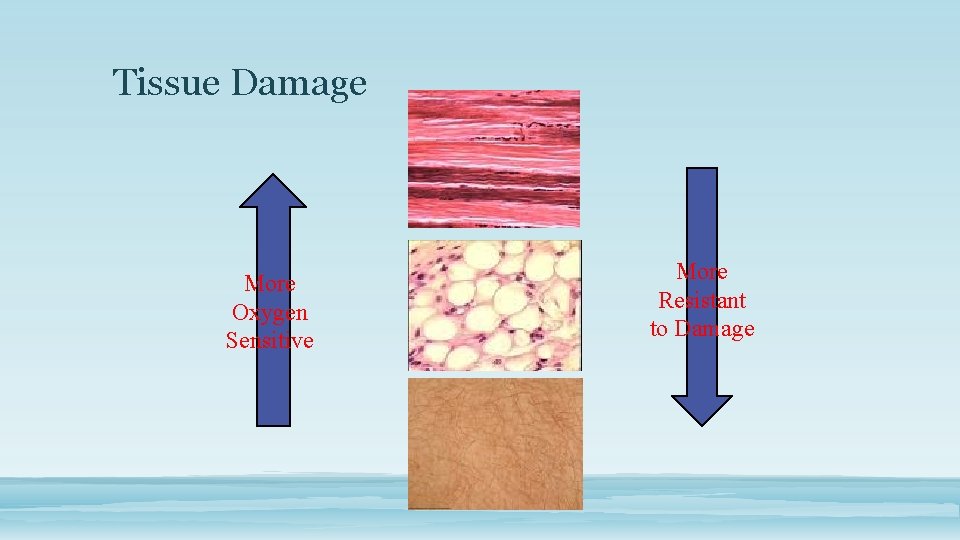
Tissue Damage More Oxygen Sensitive More Resistant to Damage
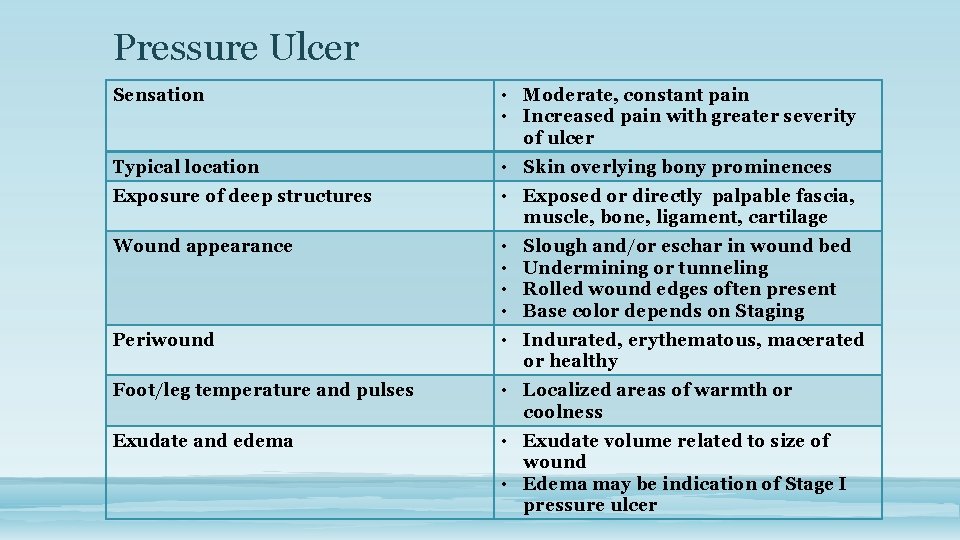
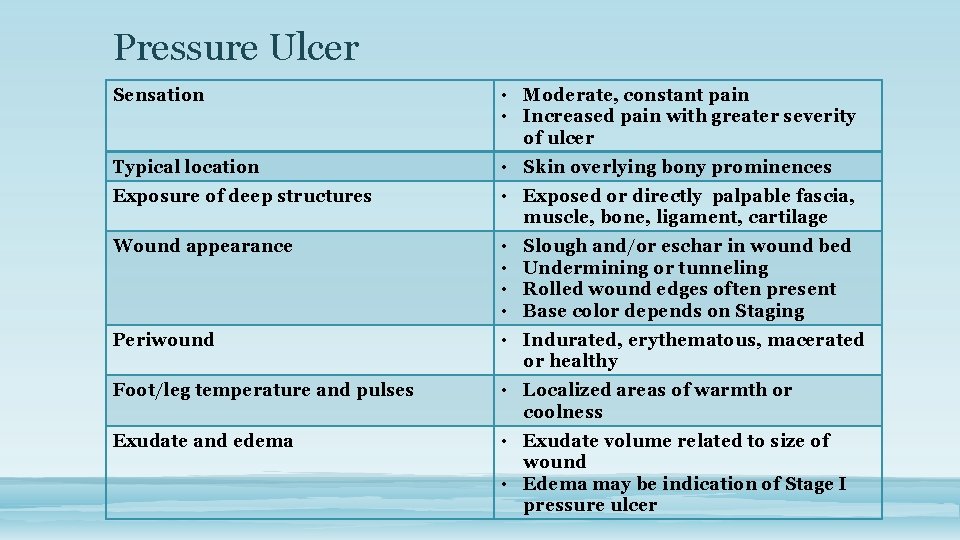
Pressure Ulcer Sensation • Moderate, constant pain • Increased pain with greater severity of ulcer Typical location • Skin overlying bony prominences Exposure of deep structures • Exposed or directly palpable fascia, muscle, bone, ligament, cartilage Wound appearance • • Periwound • Indurated, erythematous, macerated or healthy Foot/leg temperature and pulses • Localized areas of warmth or coolness Exudate and edema • Exudate volume related to size of wound • Edema may be indication of Stage I pressure ulcer Slough and/or eschar in wound bed Undermining or tunneling Rolled wound edges often present Base color depends on Staging
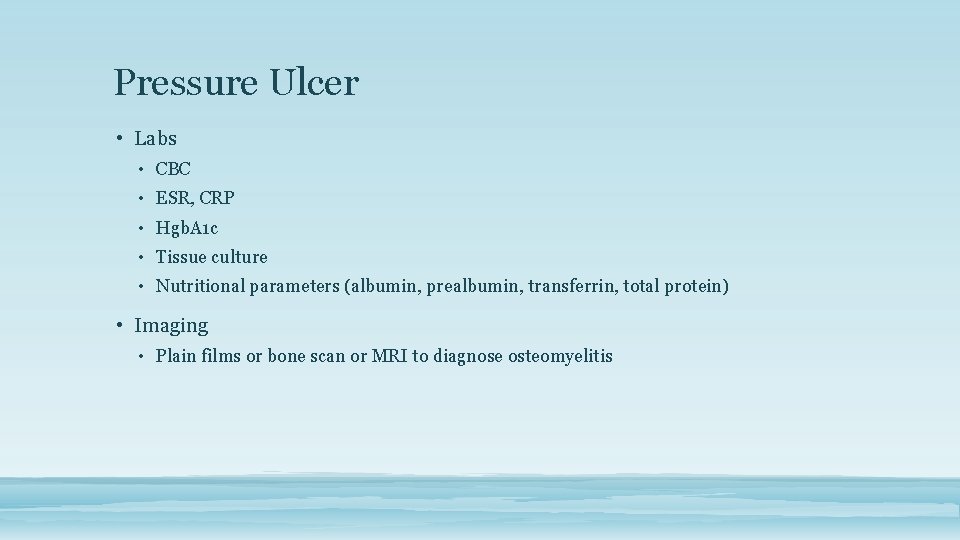
Pressure Ulcer • Labs • CBC • ESR, CRP • Hgb. A 1 c • Tissue culture • Nutritional parameters (albumin, prealbumin, transferrin, total protein) • Imaging • Plain films or bone scan or MRI to diagnose osteomyelitis
What ARE Risk Factors • Low serum albumin • Low total lymphocyte count • Fecal incontinence • Fractures • Increased age • Length of paralysis • Social state of patient • Smoking
Basic Wound Care Principles • Surgical Closure • 61% ulcer and 69% patient recurrence in 9. 3 months • 31% long term success
Guidelines 1. Repositioning schedule 2. Avoid elevation of HOB 3. Support surface 1. Static 2. Dynamic 4. Avoid prolonged sitting 5. Use seat cushion
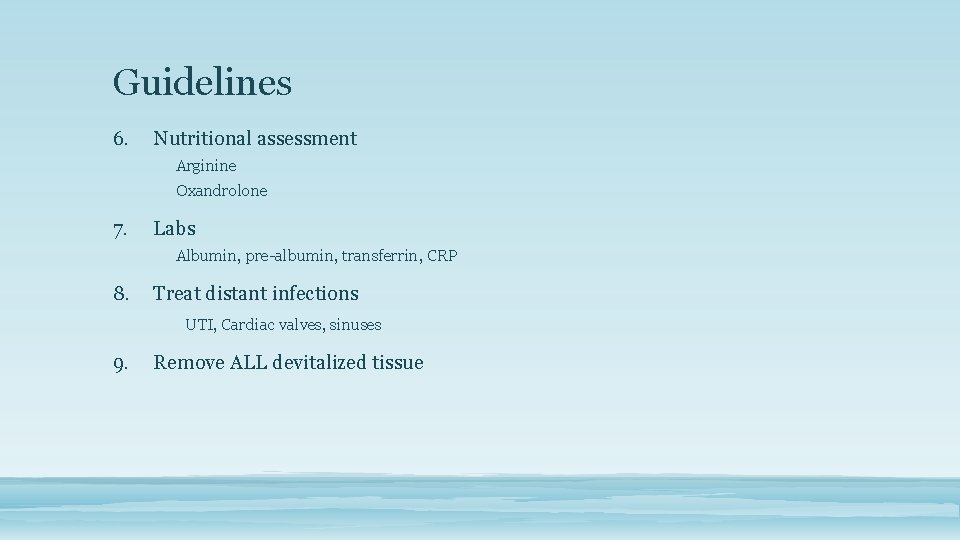
Guidelines 6. Nutritional assessment Arginine Oxandrolone 7. Labs Albumin, pre-albumin, transferrin, CRP 8. Treat distant infections UTI, Cardiac valves, sinuses 9. Remove ALL devitalized tissue
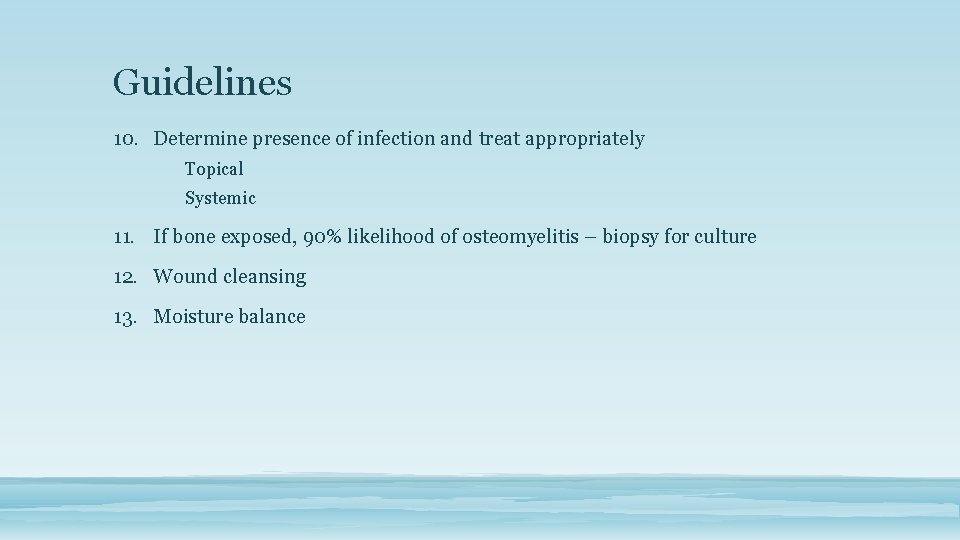
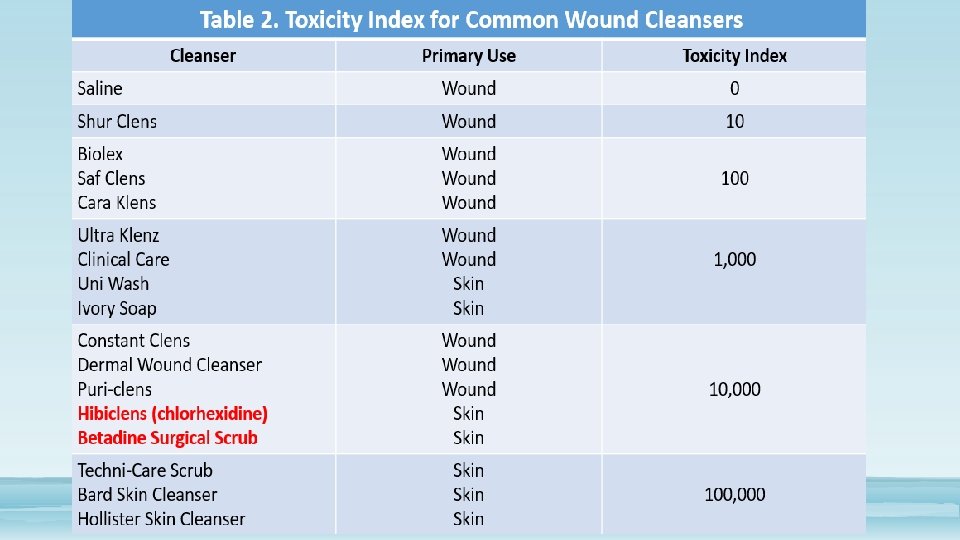
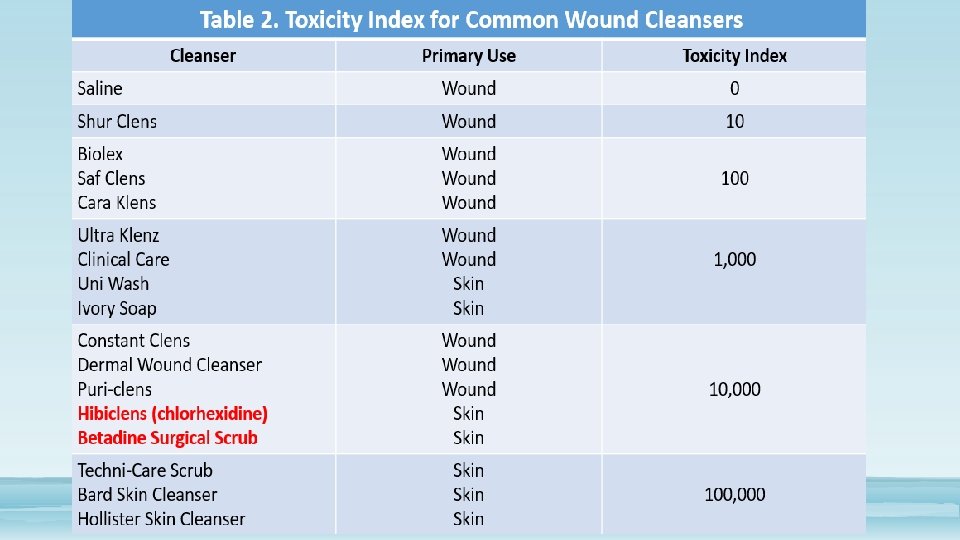
Guidelines 10. Determine presence of infection and treat appropriately Topical Systemic 11. If bone exposed, 90% likelihood of osteomyelitis – biopsy for culture 12. Wound cleansing 13. Moisture balance

Guidelines 14. Negative Pressure Wound Therapy

Dehisced Surgical Wounds • A complication where a wound breaks open along a surgical incision
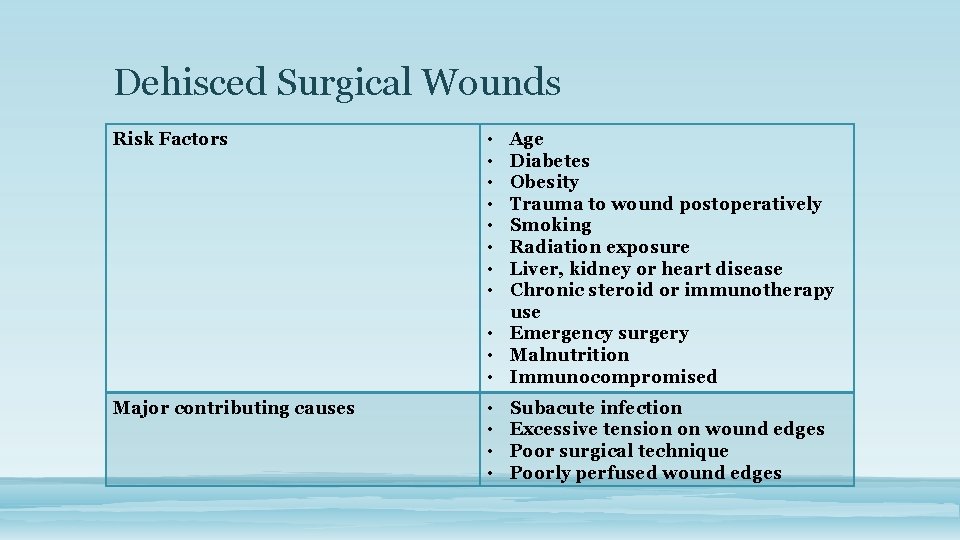
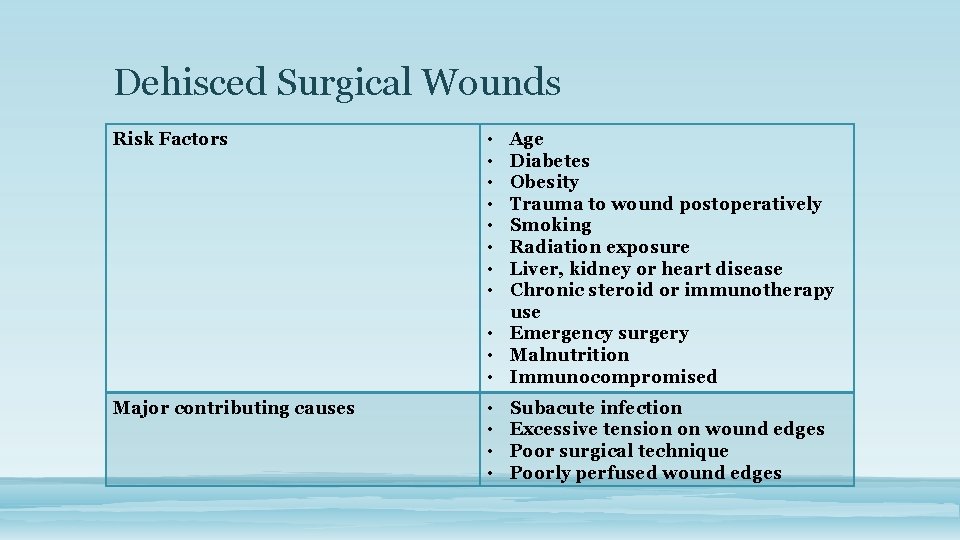
Dehisced Surgical Wounds Risk Factors • • Major contributing causes • • Age Diabetes Obesity Trauma to wound postoperatively Smoking Radiation exposure Liver, kidney or heart disease Chronic steroid or immunotherapy use • Emergency surgery • Malnutrition • Immunocompromised Subacute infection Excessive tension on wound edges Poor surgical technique Poorly perfused wound edges
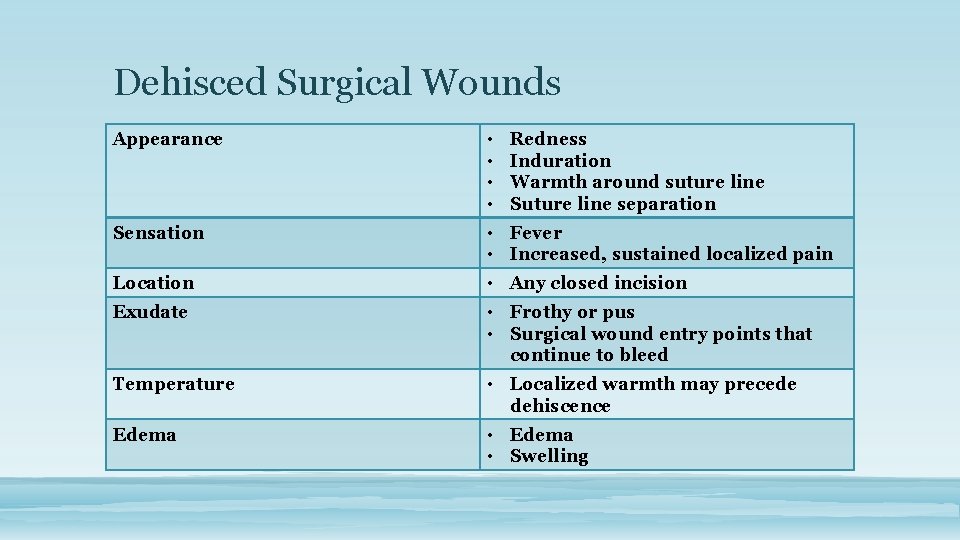
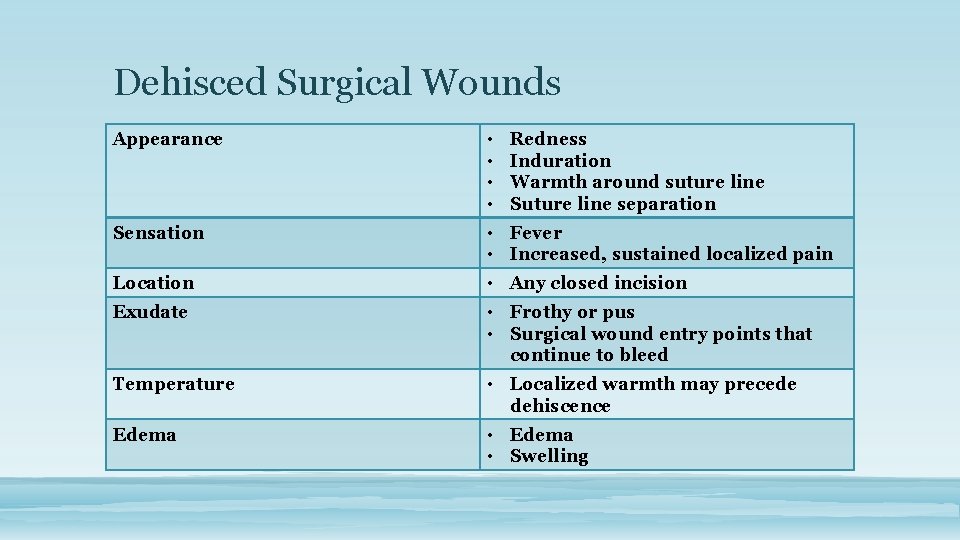
Dehisced Surgical Wounds Appearance • • Sensation • Fever • Increased, sustained localized pain Location • Any closed incision Exudate • Frothy or pus • Surgical wound entry points that continue to bleed Temperature • Localized warmth may precede dehiscence Edema • Edema • Swelling Redness Induration Warmth around suture line Suture line separation
Wound Bed Preparation • Moist - Optimal absorption / hydration • Warm - Coverage • Non toxic - No antiseptics • Uninfected - Monitor & manage bacterial loading • Clean - Mechanical / chemical debridement
The Ideal Wound Healing Environment • Moist • Warm • Non toxic • Uninfected • Clean of debris / devitalized tissue Granulation Contraction Epithelialization Healing is a preferred physiological process – if impairments are removed, healing occurs
Why Moist Healing • Acute Wounds: • Increased: • Leukocyte activity • Healing • Decreased: • Inflammation • Infection • Scarring (Fibrosis) Michie ‘ 94 • Chronic Wounds: – Increased: • • Autolytic debridement Growth Factors Granulation Epithelial migration & Healing – Decreased: • Pain Eaglestein ’ 91; Phillips ‘ 93

The Ideal Dressing • High moisture permeability • Non-adherence • High absorbency • Good adhesion to surrounding skin • Non allergenic • Comfortable • Cost-effective Scales 1956
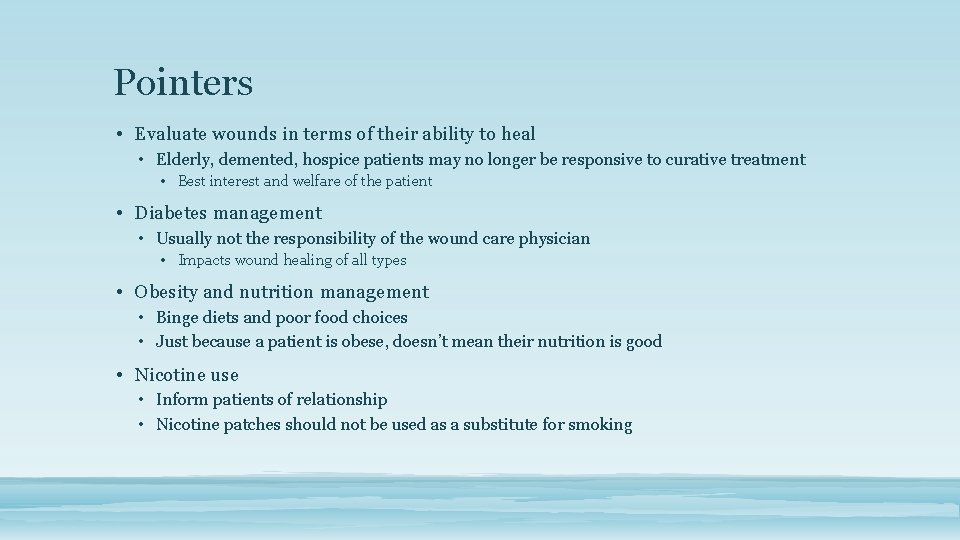
Pointers • Evaluate wounds in terms of their ability to heal • Elderly, demented, hospice patients may no longer be responsive to curative treatment • Best interest and welfare of the patient • Diabetes management • Usually not the responsibility of the wound care physician • Impacts wound healing of all types • Obesity and nutrition management • Binge diets and poor food choices • Just because a patient is obese, doesn’t mean their nutrition is good • Nicotine use • Inform patients of relationship • Nicotine patches should not be used as a substitute for smoking
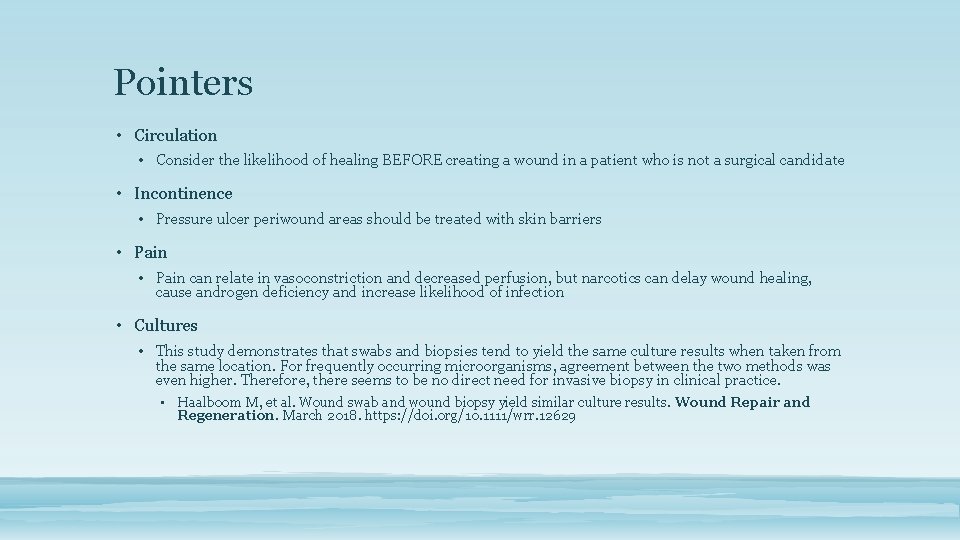
Pointers • Circulation • Consider the likelihood of healing BEFORE creating a wound in a patient who is not a surgical candidate • Incontinence • Pressure ulcer periwound areas should be treated with skin barriers • Pain can relate in vasoconstriction and decreased perfusion, but narcotics can delay wound healing, cause androgen deficiency and increase likelihood of infection • Cultures • This study demonstrates that swabs and biopsies tend to yield the same culture results when taken from the same location. For frequently occurring microorganisms, agreement between the two methods was even higher. Therefore, there seems to be no direct need for invasive biopsy in clinical practice. • Haalboom M, et al. Wound swab and wound biopsy yield similar culture results. Wound Repair and Regeneration. March 2018. https: //doi. org/10. 1111/wrr. 12629
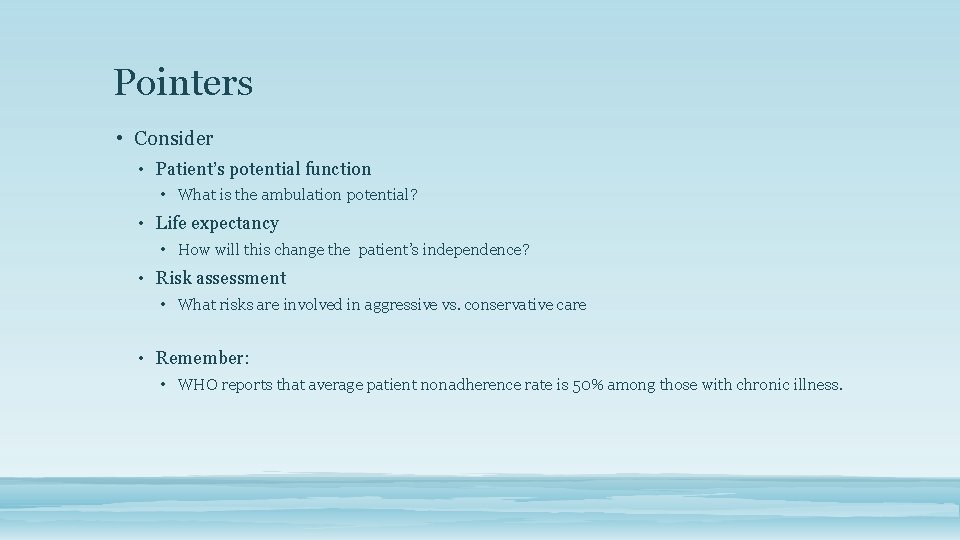
Pointers • Consider • Patient’s potential function • What is the ambulation potential? • Life expectancy • How will this change the patient’s independence? • Risk assessment • What risks are involved in aggressive vs. conservative care • Remember: • WHO reports that average patient nonadherence rate is 50% among those with chronic illness.

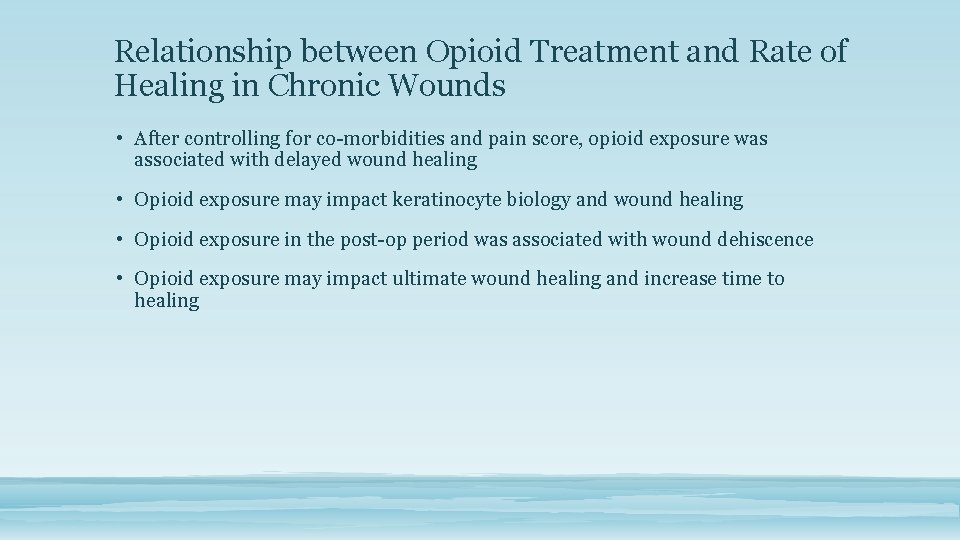
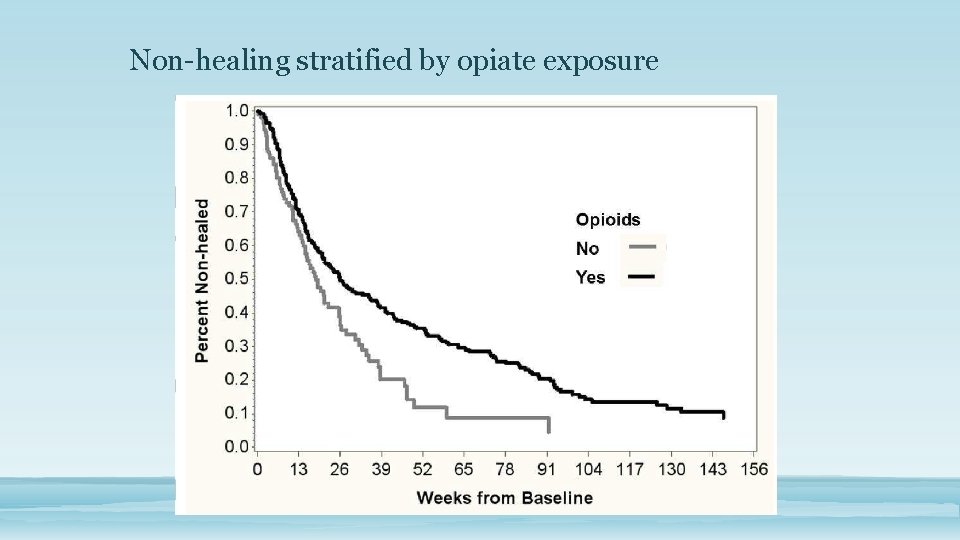
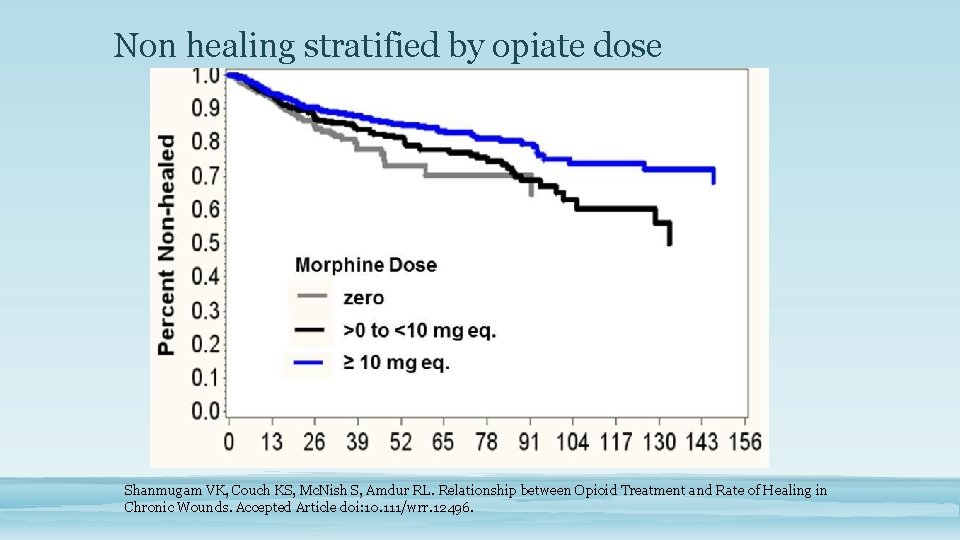
Relationship between Opioid Treatment and Rate of Healing in Chronic Wounds • After controlling for co-morbidities and pain score, opioid exposure was associated with delayed wound healing • Opioid exposure may impact keratinocyte biology and wound healing • Opioid exposure in the post-op period was associated with wound dehiscence • Opioid exposure may impact ultimate wound healing and increase time to healing
Why? • There are functionally active μ-opiate receptors on human keratinocytes. • Activation of these receptors by the μ-opiate agonist β-endorphin results upregulation of TGF-β and cytokeratin 16 • Shown that CK 16 response can be blocked by incubation together with the μopiate receptor antagonist naltrexone Biligardi PL, Sumanovski LT, Büchner S, et al. Different Expression of μ-Opiate Receptor in Chronic and Acute Wounds and the Effect of β-Endorphin on Transforming Growth Factor β Type II Receptor and Cytokeratin 16 Expression. J Invest Derm. 120: 1, Jan 2003. https: //www. sciencedirect. com/science/article/pii/S 0022202 X 15301287
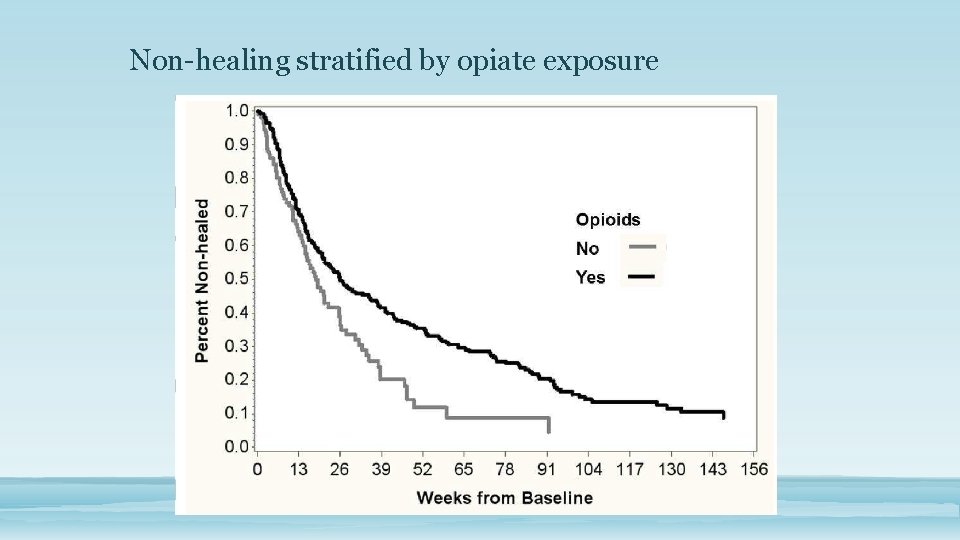
Non-healing stratified by opiate exposure
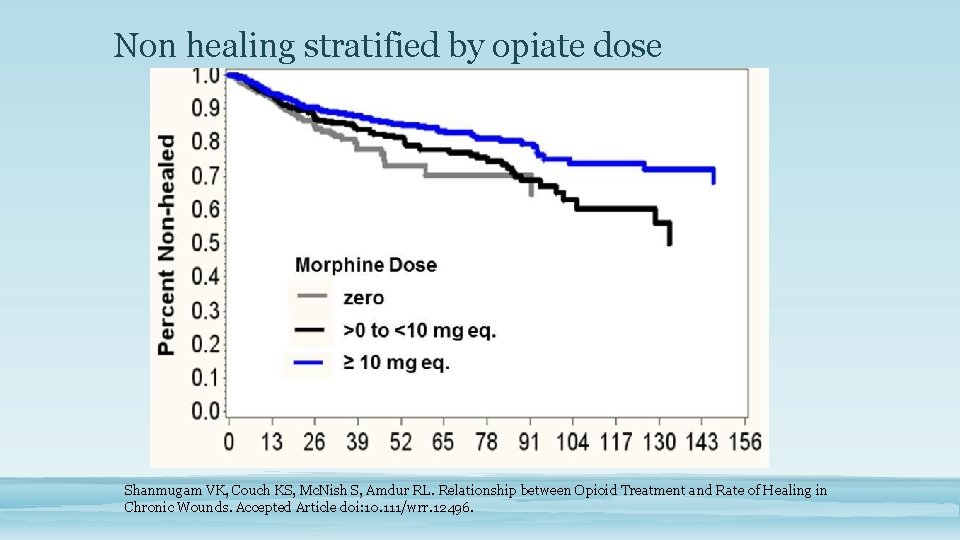
Non healing stratified by opiate dose Shanmugam VK, Couch KS, Mc. Nish S, Amdur RL. Relationship between Opioid Treatment and Rate of Healing in Chronic Wounds. Accepted Article doi: 10. 111/wrr. 12496.
Advances in Skin & Wound Care – March 2017
https: //onlinelibrary. wiley. com/doi/epdf/10. 1111/wrr. 12396
https: //onlinelibrary. wiley. com/doi/epdf/10. 1111/wrr. 12391
https: //onlinelibrary. wiley. com/doi/epdf/10. 1111/wrr. 12394
https: //onlinelibrary. wiley. com/doi/epdf/10. 1111/wrr. 12395

Questions?