11216 INFECTIVE ULCERS OF THE INTESTINE DR A

- Slides: 38
11/2/16 INFECTIVE ULCERS OF THE INTESTINE DR. A. KSHEERA CARIAPPA ASSISTANT PROFESSOR
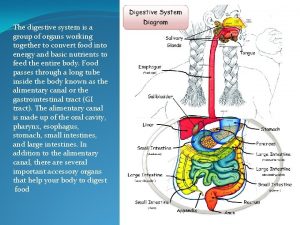
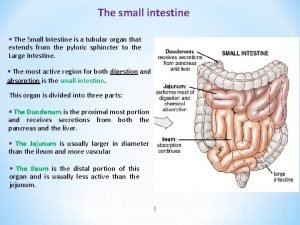
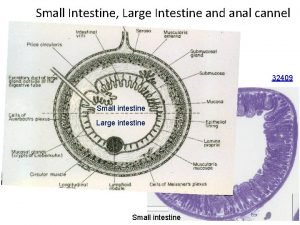
ULCERS • Ulcers are defined histologically as a breach in the continuity of the mucosa of the alimentary tract that may be superficial or extend through the muscularis mucosa into the submucosa or deeper. 1. Small Intestinal 2. Large Intestinal
SMALL & LARGE INTESTINE Infectious: • Typhoid ulcer • Tuberculous ulcer • Amoebic ulcer • H. Pylori - Duodenal ulcer • Bacillary Dysentry
1. TYPHOID Acute enteric infectious disease • caused by Salmonella typhi (S. Typhi). • Clinical features : prolonged fever, Relative bradycardia, apathetic facial expressions, roseola, splenomegaly, hepatomegaly, leukopenia. • Can lead to intestinal perforation, intestinal hemorrhage
SALMONELLOSIS Salmonella infection in man is caused by the enteric fever group of bacteria which includes: Salmonella typhi. ► Typhoid fever Salmonella paratyphi A. ► Paratyphoid fever Salmonella paratyphi B. ► Paratyphoid fever
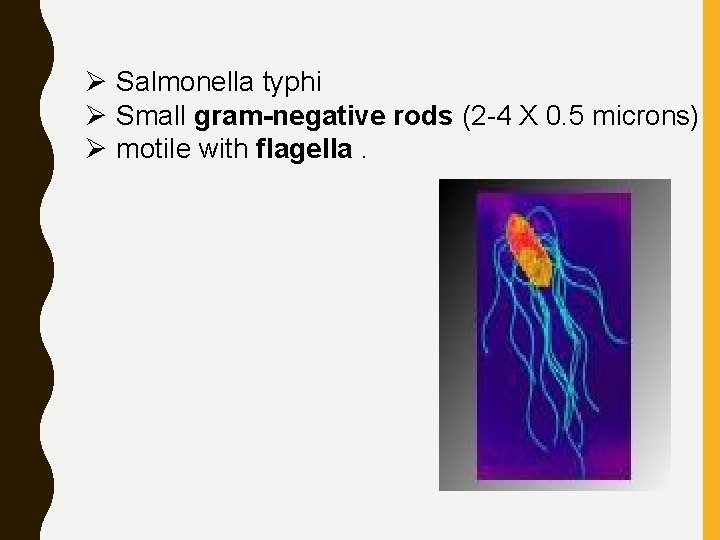
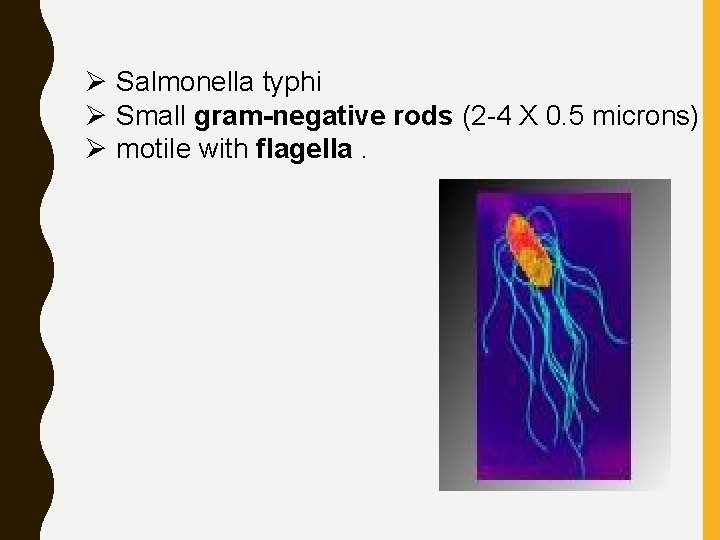
Ø Salmonella typhi Ø Small gram-negative rods (2 -4 X 0. 5 microns) Ø motile with flagella.
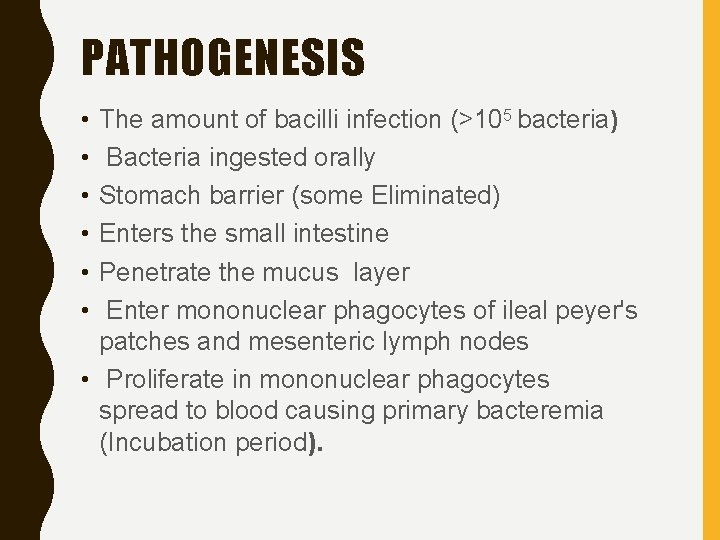
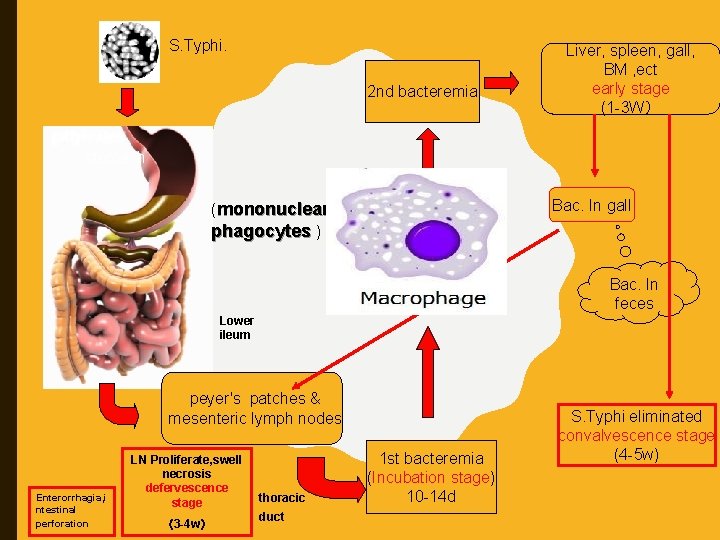
PATHOGENESIS • • • The amount of bacilli infection (>105 bacteria) Bacteria ingested orally Stomach barrier (some Eliminated) Enters the small intestine Penetrate the mucus layer Enter mononuclear phagocytes of ileal peyer's patches and mesenteric lymph nodes • Proliferate in mononuclear phagocytes spread to blood causing primary bacteremia (Incubation period).
Øenter spleen, liver and bone marrow (reticuloendothelial system) further proliferation occurs Ø A lot of bacteria enter blood again causing secondary bacteremia. Ø Recovery
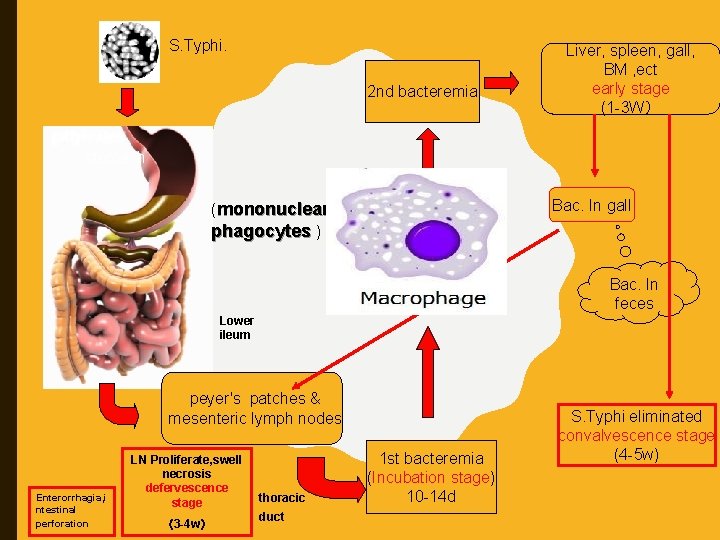
S. Typhi. 2 nd bacteremia Liver, spleen, gall, BM , ect early stage (1 -3 W) stomach Bac. In gall (mononuclear phagocytes ) Bac. In feces Lower ileum peyer's patches & mesenteric lymph nodes Enterorrhagia, i ntestinal perforation LN Proliferate, swell necrosis defervescence stage (3 -4 w) thoracic duct 1 st bacteremia (Incubation stage) 10 -14 d S. Typhi eliminated convalvescence stage (4 -5 w)
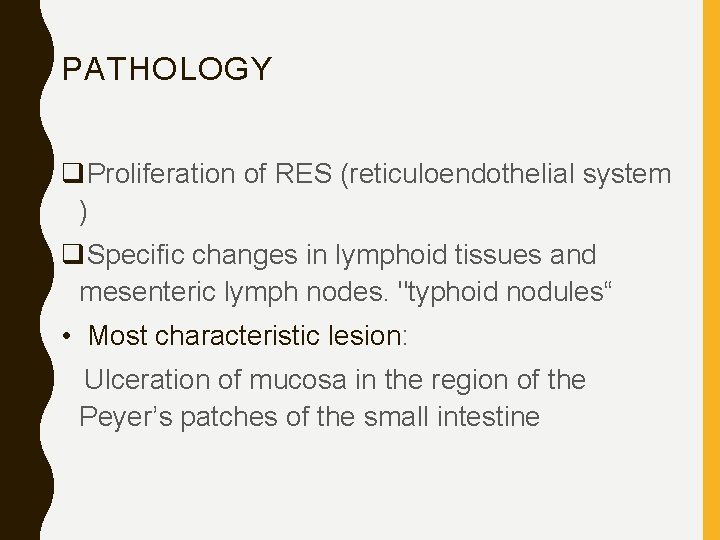
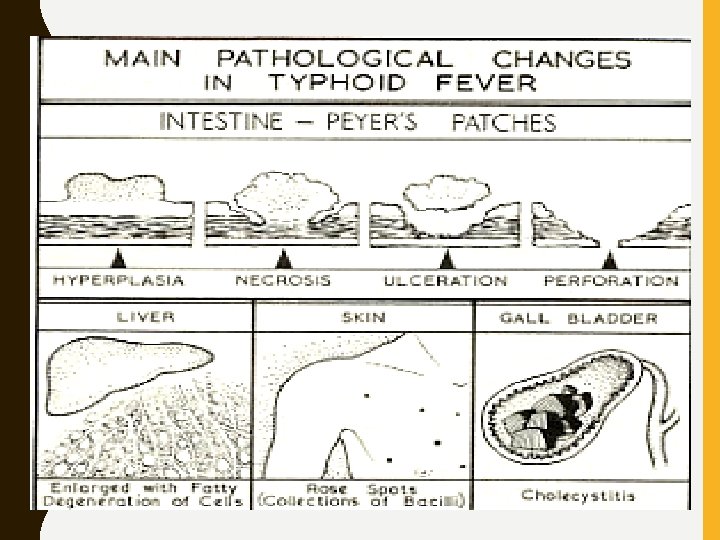
PATHOLOGY q. Proliferation of RES (reticuloendothelial system ) q. Specific changes in lymphoid tissues and mesenteric lymph nodes. "typhoid nodules“ • Most characteristic lesion: Ulceration of mucosa in the region of the Peyer’s patches of the small intestine
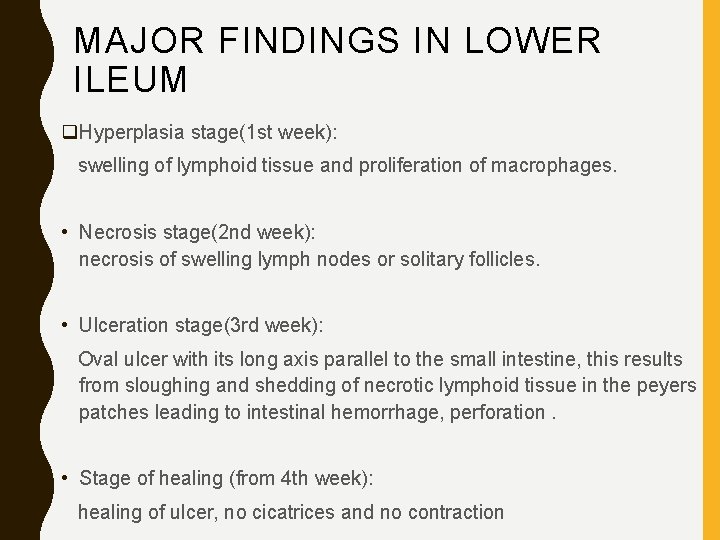
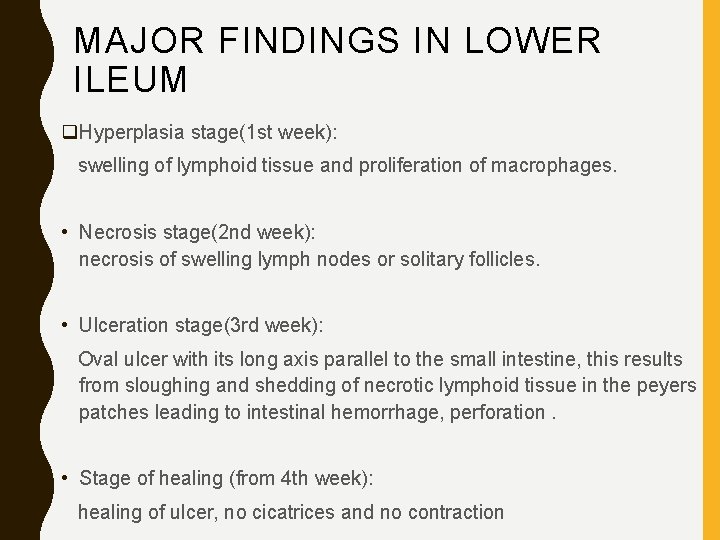
MAJOR FINDINGS IN LOWER ILEUM q. Hyperplasia stage(1 st week): swelling of lymphoid tissue and proliferation of macrophages. • Necrosis stage(2 nd week): necrosis of swelling lymph nodes or solitary follicles. • Ulceration stage(3 rd week): Oval ulcer with its long axis parallel to the small intestine, this results from sloughing and shedding of necrotic lymphoid tissue in the peyers patches leading to intestinal hemorrhage, perforation. • Stage of healing (from 4 th week): healing of ulcer, no cicatrices and no contraction
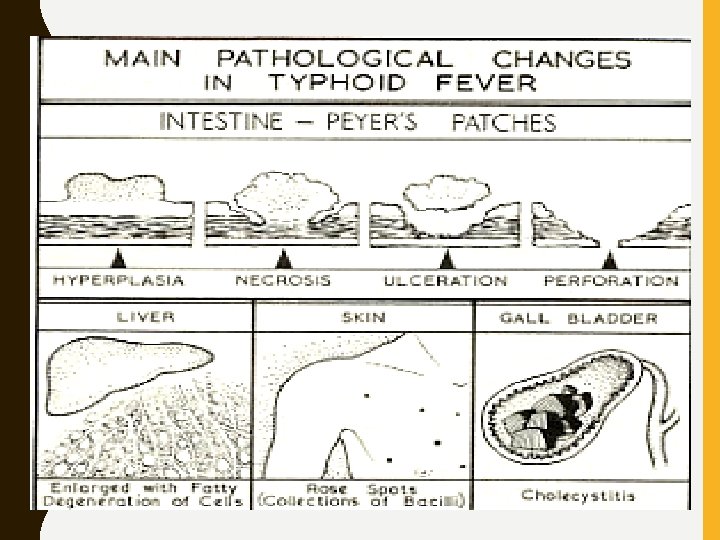
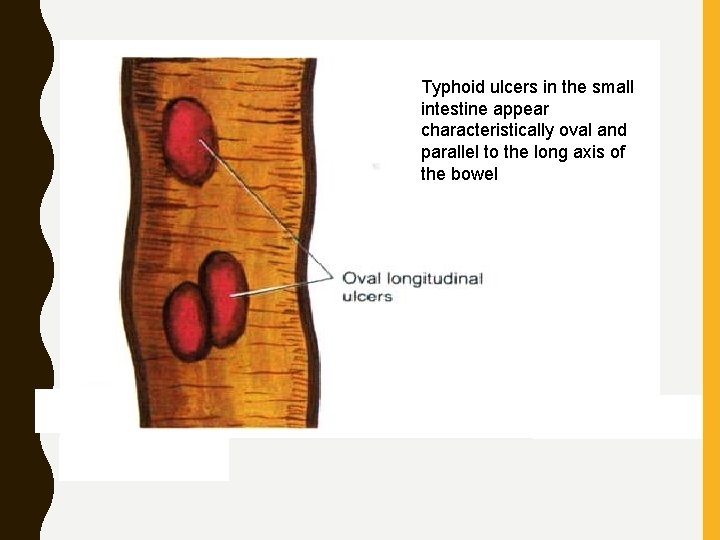
• Pathogenic Mechanism Invasion, translocation, lymphoid inflammation and dissemination • Typhoid ulcers are oval and longitudinal
Typhoid ulcers in the small intestine appear characteristically oval and parallel to the long axis of the bowel
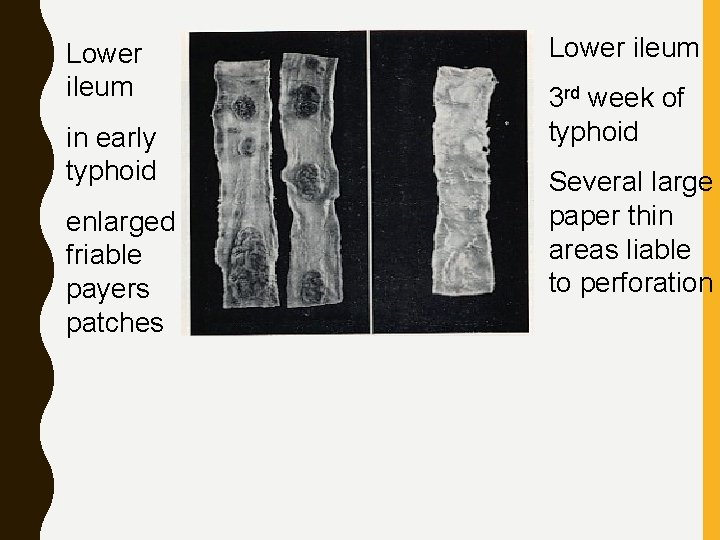
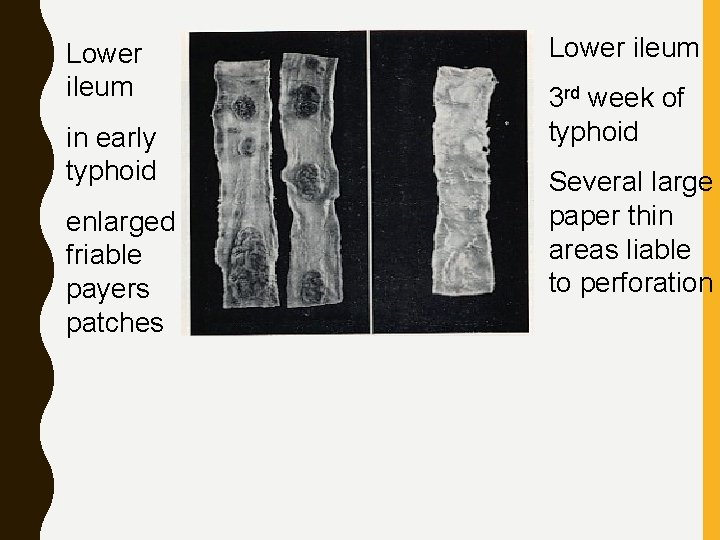
Lower ileum in early typhoid enlarged friable payers patches Lower ileum 3 rd week of typhoid Several large paper thin areas liable to perforation
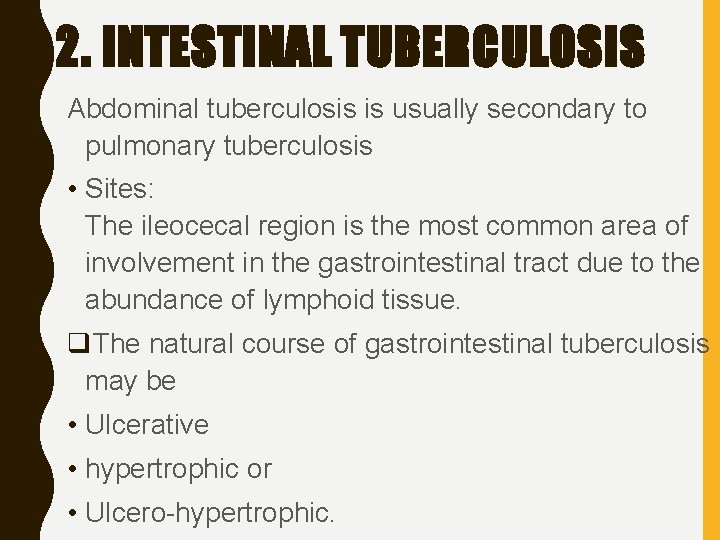
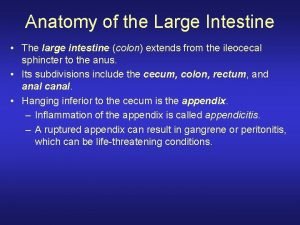
2. INTESTINAL TUBERCULOSIS Abdominal tuberculosis is usually secondary to pulmonary tuberculosis • Sites: The ileocecal region is the most common area of involvement in the gastrointestinal tract due to the abundance of lymphoid tissue. q. The natural course of gastrointestinal tuberculosis may be • Ulcerative • hypertrophic or • Ulcero-hypertrophic.
• Clinical presentation Abdominal pain mimicking peptic ulcer disease with stomach or duodenal infection; Malabsorption with infection of the small intestine; Pain, diarrhea, or hematochezia with infection of the colon.
Investigations • Blood routine • Urine routine - to detect diabetes mellitus • Plain X-ray of the abdomen • Laparoscopy • Laparoscopic biopsy of tubercles found in the peritoneum or other parts • Barium studies
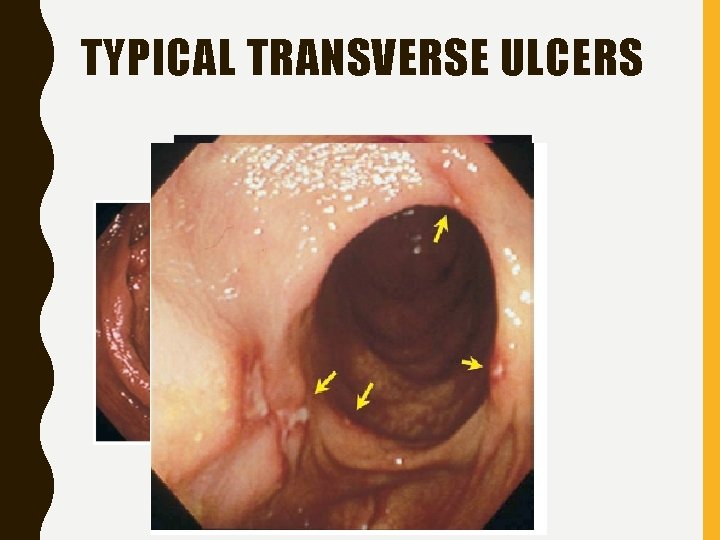
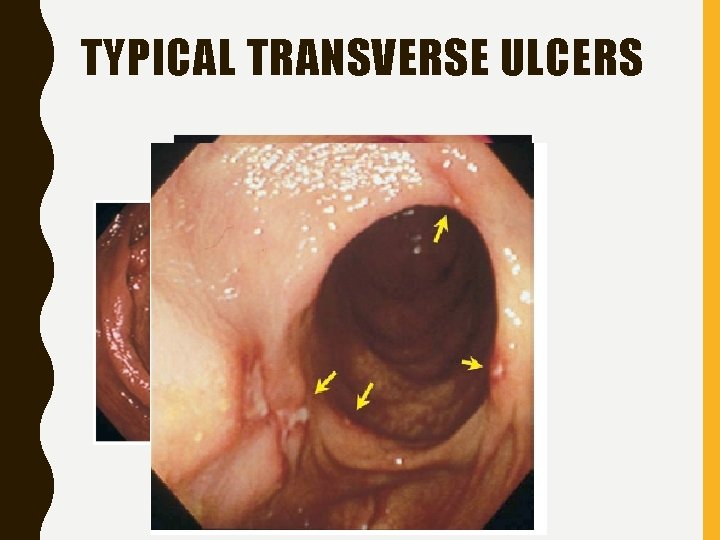
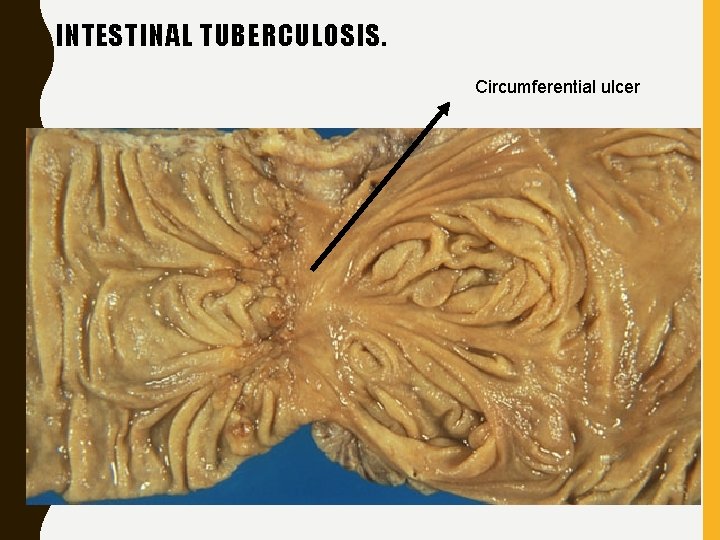
TYPICAL TRANSVERSE ULCERS
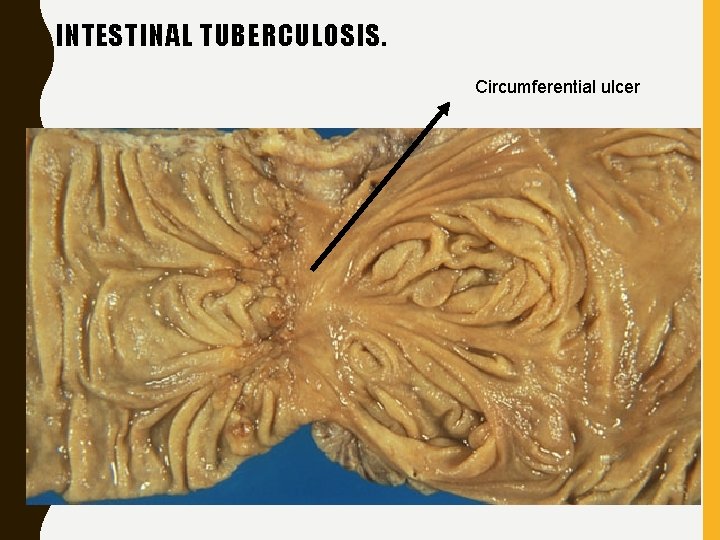
INTESTINAL TUBERCULOSIS. Circumferential ulcer
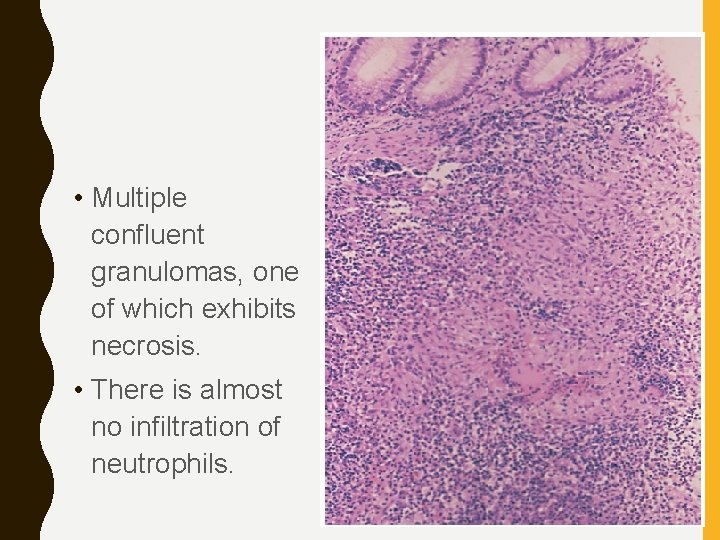
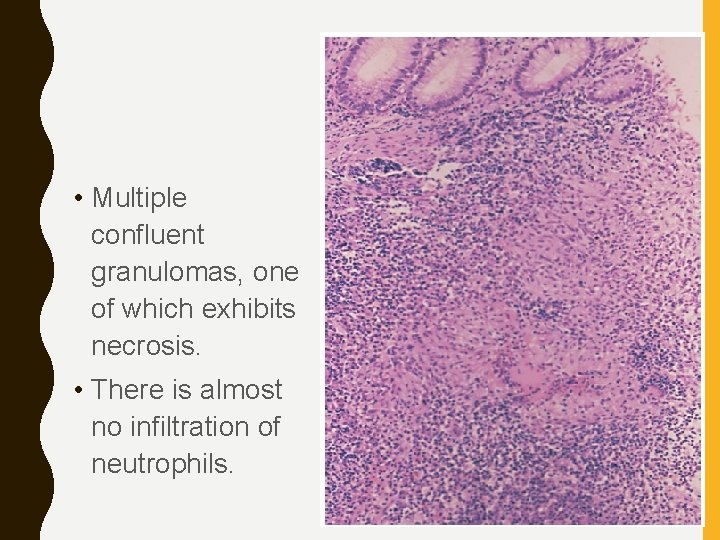
• Multiple confluent granulomas, one of which exhibits necrosis. • There is almost no infiltration of neutrophils.
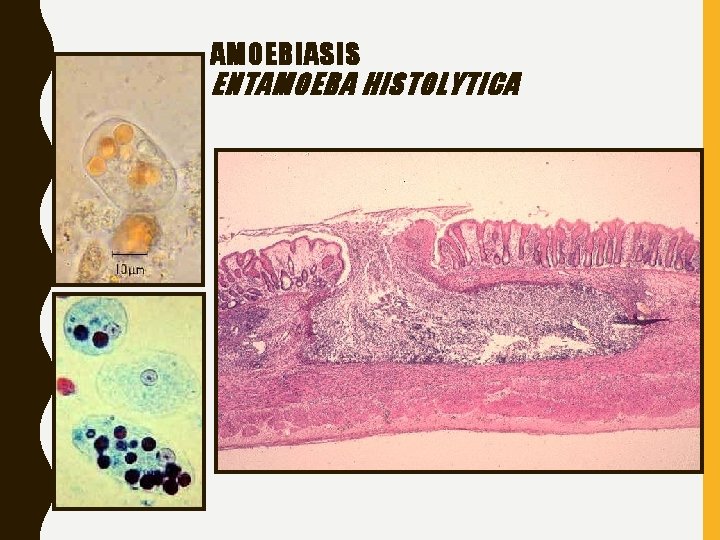
3. AMOEBIASIS • It is caused by a protozoan E. histolytica • Transmission: Fecal-oral contamination • Caecum, ascending colon, appendix, sigmoid colon
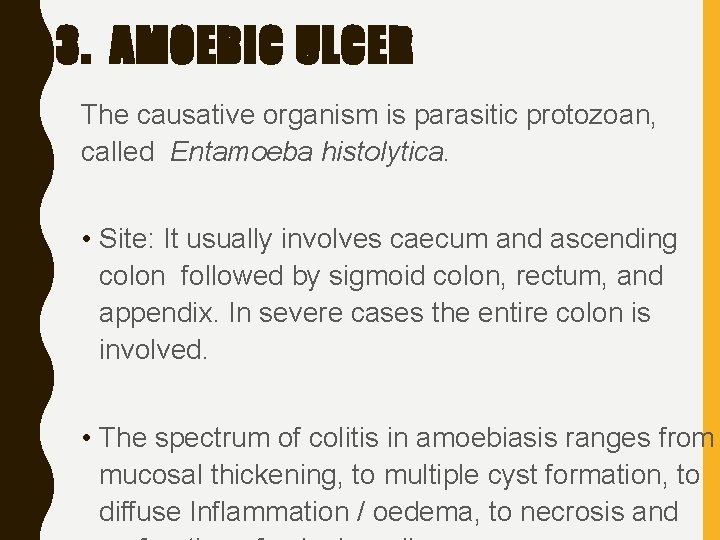
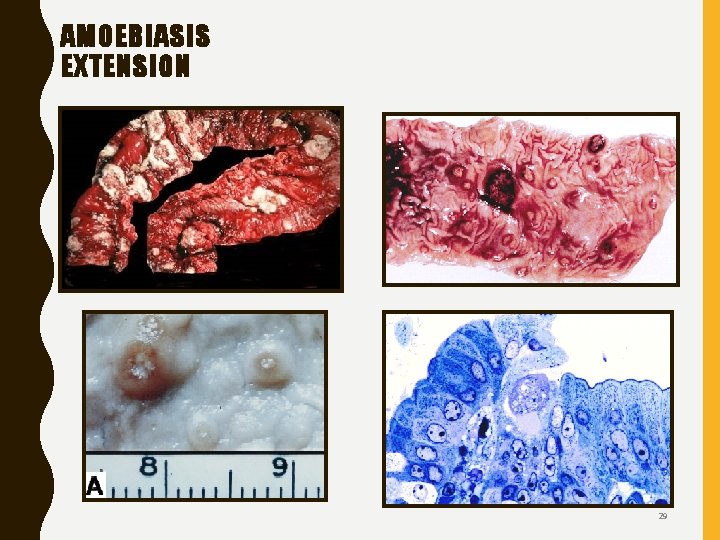
3. AMOEBIC ULCER The causative organism is parasitic protozoan, called Entamoeba histolytica. • Site: It usually involves caecum and ascending colon followed by sigmoid colon, rectum, and appendix. In severe cases the entire colon is involved. • The spectrum of colitis in amoebiasis ranges from mucosal thickening, to multiple cyst formation, to diffuse Inflammation / oedema, to necrosis and
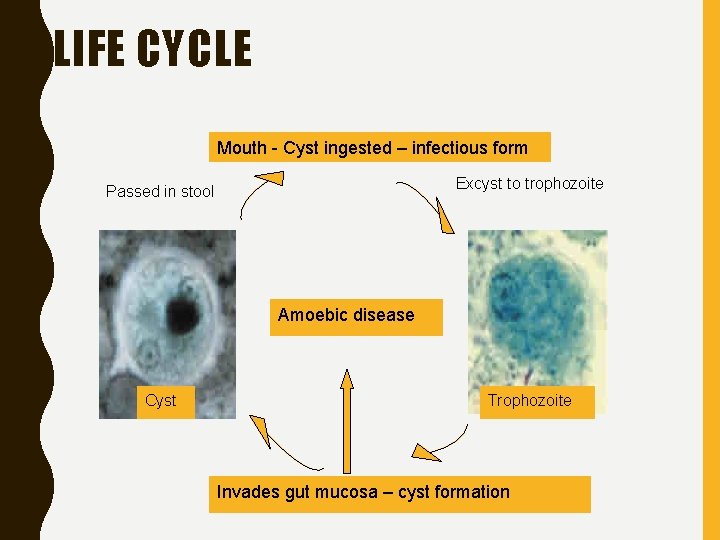
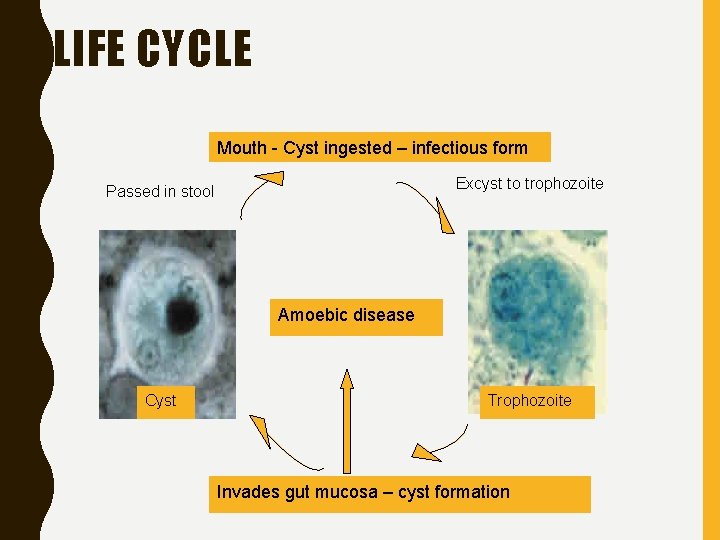
LIFE CYCLE Mouth - Cyst ingested – infectious form Excyst to trophozoite Passed in stool Amoebic disease Cyst Trophozoite Invades gut mucosa – cyst formation
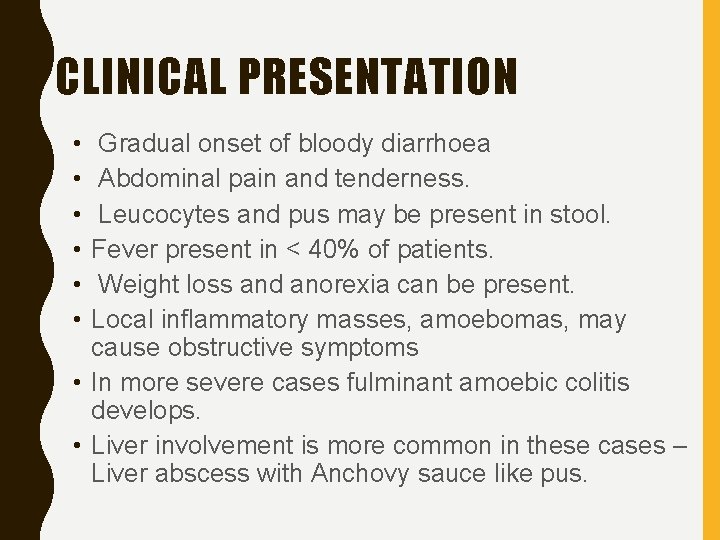
CLINICAL PRESENTATION • • • Gradual onset of bloody diarrhoea Abdominal pain and tenderness. Leucocytes and pus may be present in stool. Fever present in < 40% of patients. Weight loss and anorexia can be present. Local inflammatory masses, amoebomas, may cause obstructive symptoms • In more severe cases fulminant amoebic colitis develops. • Liver involvement is more common in these cases – Liver abscess with Anchovy sauce like pus.
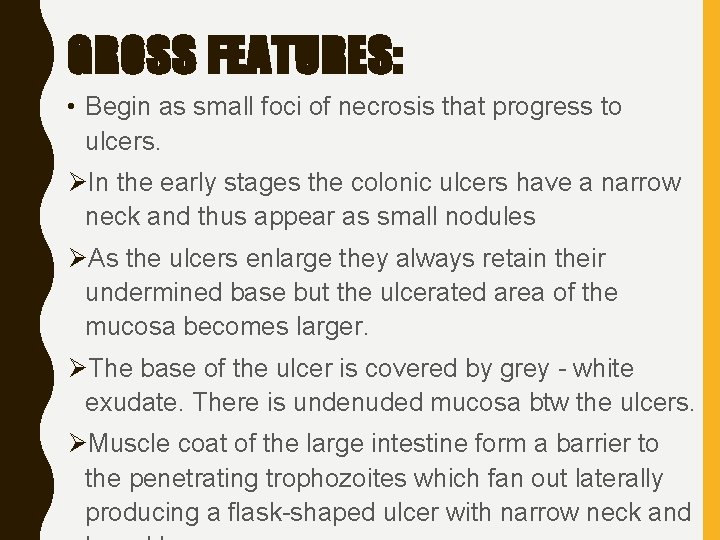
GROSS FEATURES: • Begin as small foci of necrosis that progress to ulcers. ØIn the early stages the colonic ulcers have a narrow neck and thus appear as small nodules ØAs the ulcers enlarge they always retain their undermined base but the ulcerated area of the mucosa becomes larger. ØThe base of the ulcer is covered by grey - white exudate. There is undenuded mucosa btw the ulcers. ØMuscle coat of the large intestine form a barrier to the penetrating trophozoites which fan out laterally producing a flask-shaped ulcer with narrow neck and
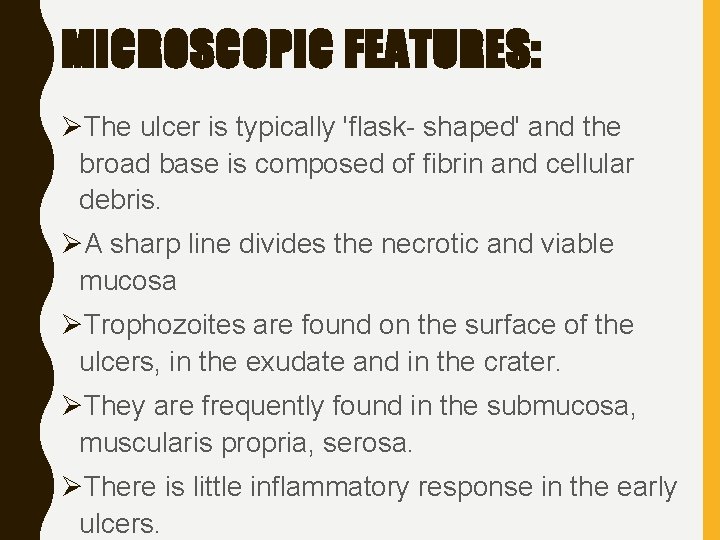
MICROSCOPIC FEATURES: ØThe ulcer is typically 'flask- shaped' and the broad base is composed of fibrin and cellular debris. ØA sharp line divides the necrotic and viable mucosa ØTrophozoites are found on the surface of the ulcers, in the exudate and in the crater. ØThey are frequently found in the submucosa, muscularis propria, serosa. ØThere is little inflammatory response in the early ulcers.
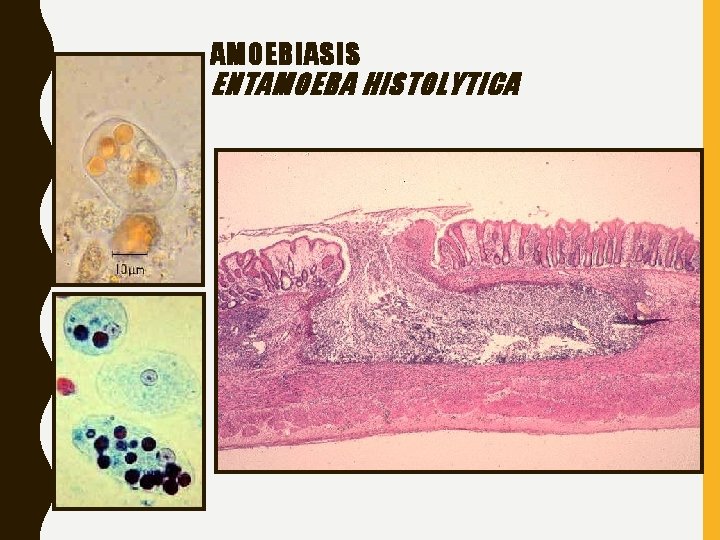
AMOEBIASIS ENTAMOEBA HISTOLYTICA
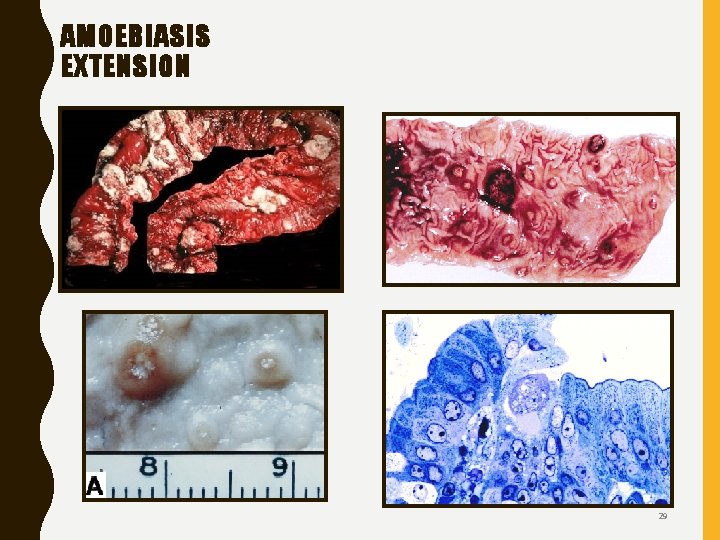
AMOEBIASIS EXTENSION 29
DIAGNOSIS: – Examination of the stool for cysts is required for diagnosis. Colonic mucosal biopsies may reveal the organisms. – Serologic titers may aid in diagnosis, particularly with disseminated infections.
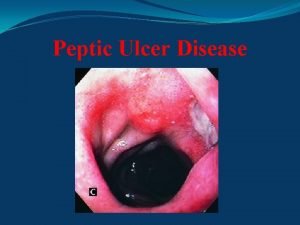
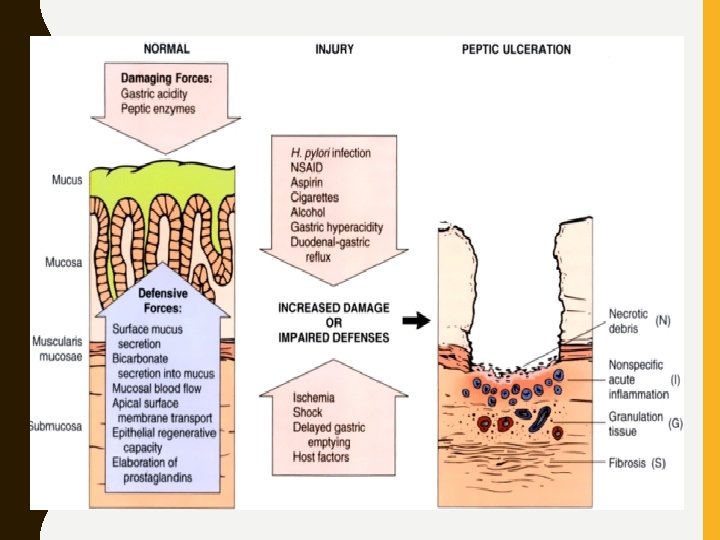
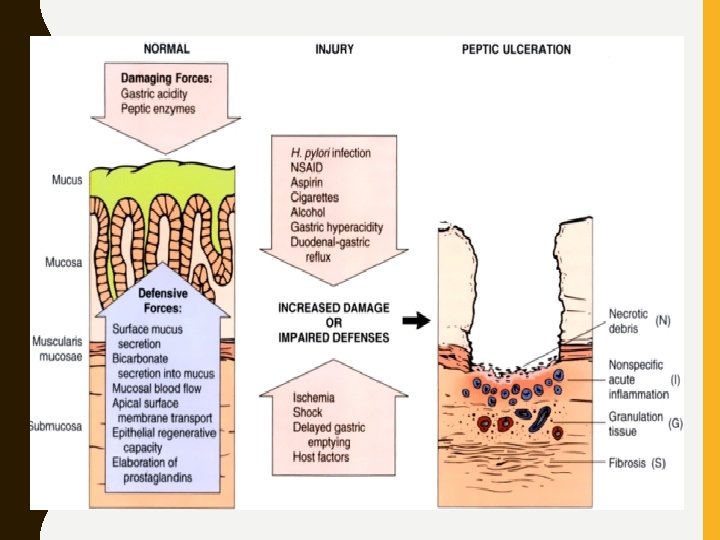
4. PEPTIC ULCERS • chronic, most often solitary, lesions occur in any portion of the gastrointestinal tract exposed to the aggressive action of acid/peptic juices
Sites: • Duodenum, first portion • Within the margins of a gastrojejunostomy • In the duodenum, stomach, and/or jejunum of patients with Zollinger-Ellison syndrome • Within or adjacent to an ileal Meckel diverticulum with ectopic gastric mucosa.
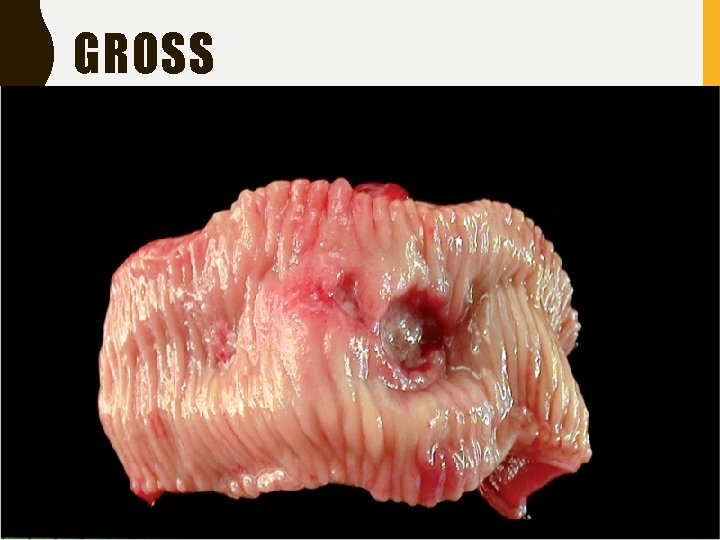
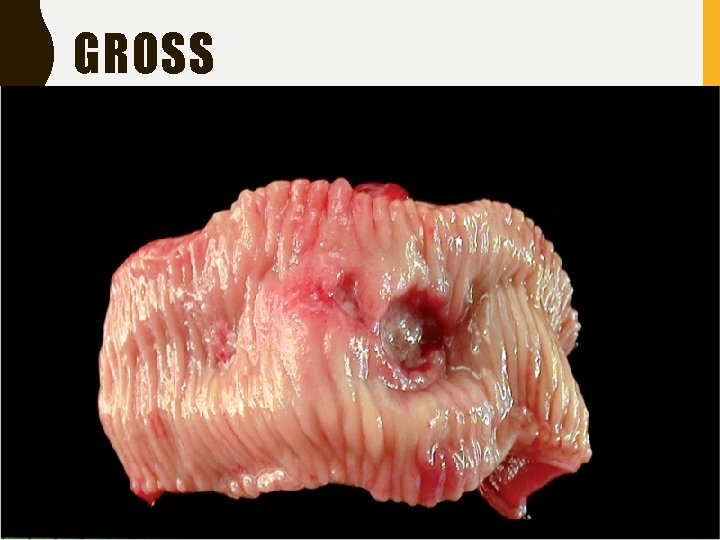
GROSS
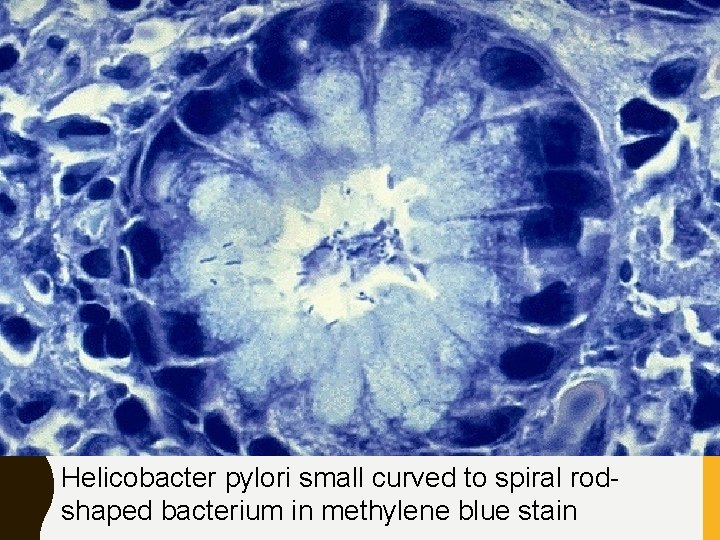
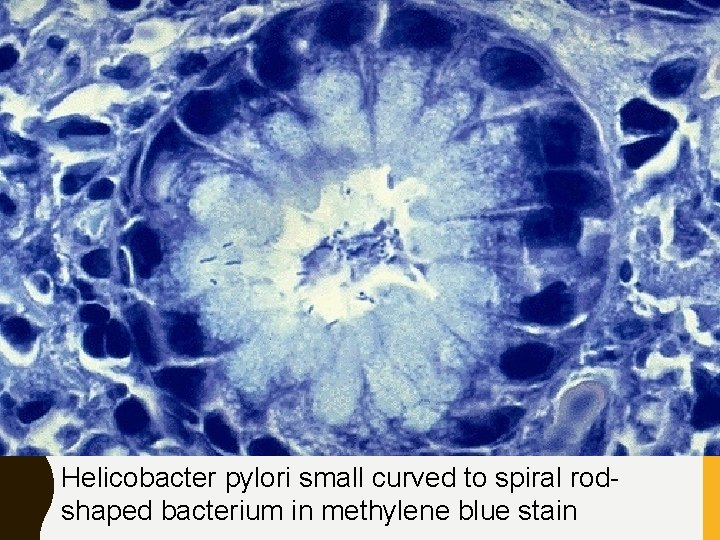
Helicobacter pylori small curved to spiral rodshaped bacterium in methylene blue stain
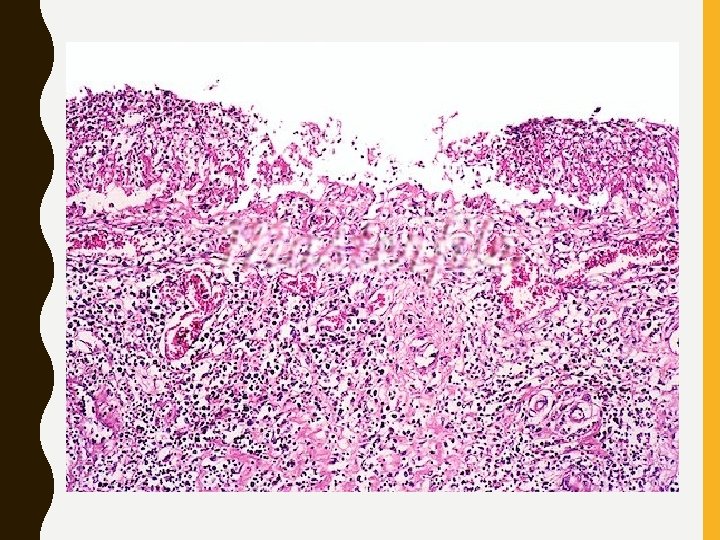
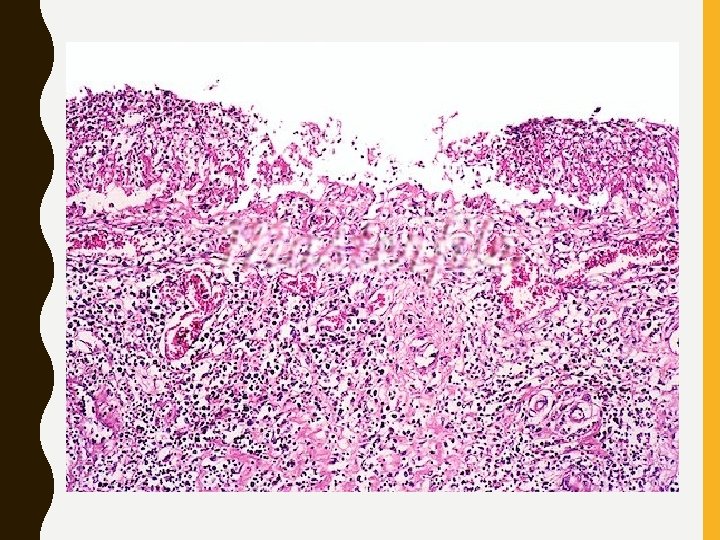
5. BACILLARY DYSENTRY • Shigella organisms • Distal colon • Mucosa soft and friable – Persian carpet appearance – If severe, denuded mucosa over large areas. • Irregular ulcers with neutrophils and congestion
OTHER UNCOMMON CAUSES • Infection from campylobacter jejuni, CMV, AIDS and transplant patients • Bacillary dysentry due to clostridium difficile • GVHD • Diverticulosis • Ischemic colitis • Intestinal worm infestation • Mesenteric artery ischemia

 Esophagus stomach small intestine large intestine
Esophagus stomach small intestine large intestine Acute gastritis
Acute gastritis Stomach ulcer definition
Stomach ulcer definition Fibrin cuff theory venous ulcers
Fibrin cuff theory venous ulcers Tuberculous ulcer and typhoid ulcer
Tuberculous ulcer and typhoid ulcer Vicaline pill application
Vicaline pill application Gastric ucler
Gastric ucler Types of ulcer edge
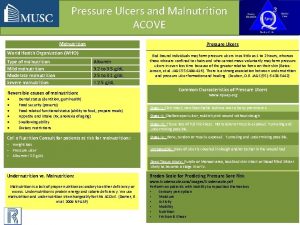
Types of ulcer edge Continuous bedside pressure mapping
Continuous bedside pressure mapping Anorexia and stomach ulcers
Anorexia and stomach ulcers Infective stage
Infective stage Duke criteria mnemonic
Duke criteria mnemonic Filariasis infective stage
Filariasis infective stage Classification of parasites
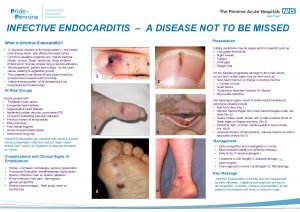
Classification of parasites Signs of infective endocarditis
Signs of infective endocarditis Bulky friable vegetations
Bulky friable vegetations Aschoff bodies
Aschoff bodies Periodontal management of medically compromised patients
Periodontal management of medically compromised patients Dukes criteria for infective endocarditis
Dukes criteria for infective endocarditis Endocarditis
Endocarditis Cestodes
Cestodes Essentials of medical parasitology
Essentials of medical parasitology Janway lesion
Janway lesion Infective endocarditis
Infective endocarditis Dạng đột biến một nhiễm là
Dạng đột biến một nhiễm là Vẽ hình chiếu đứng bằng cạnh của vật thể
Vẽ hình chiếu đứng bằng cạnh của vật thể Phản ứng thế ankan
Phản ứng thế ankan Các môn thể thao bắt đầu bằng tiếng chạy
Các môn thể thao bắt đầu bằng tiếng chạy Chó sói
Chó sói Thiếu nhi thế giới liên hoan
Thiếu nhi thế giới liên hoan Sự nuôi và dạy con của hổ
Sự nuôi và dạy con của hổ điện thế nghỉ
điện thế nghỉ Thế nào là sự mỏi cơ
Thế nào là sự mỏi cơ Một số thể thơ truyền thống
Một số thể thơ truyền thống Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Số nguyên là gì
Số nguyên là gì Vẽ hình chiếu vuông góc của vật thể sau
Vẽ hình chiếu vuông góc của vật thể sau Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới