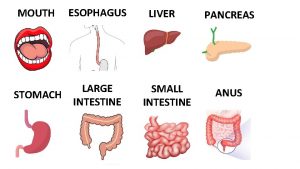
Large intestine appendix Anatomical regions of large intestine


- Slides: 36
Large intestine, appendix
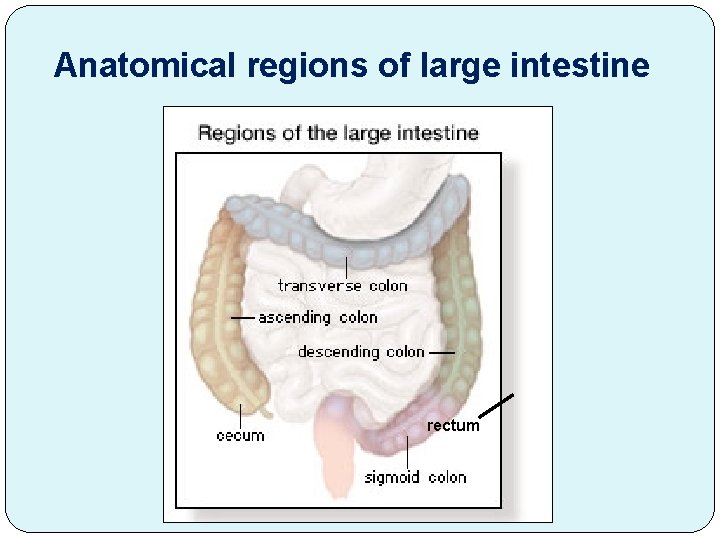
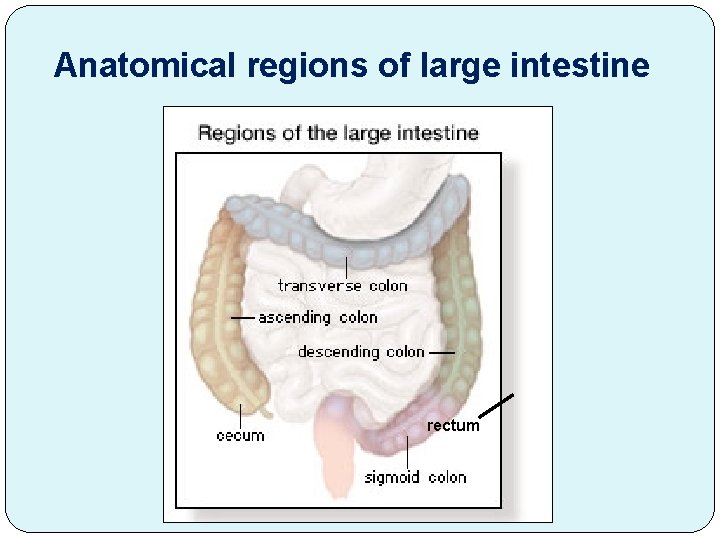
Anatomical regions of large intestine rectum
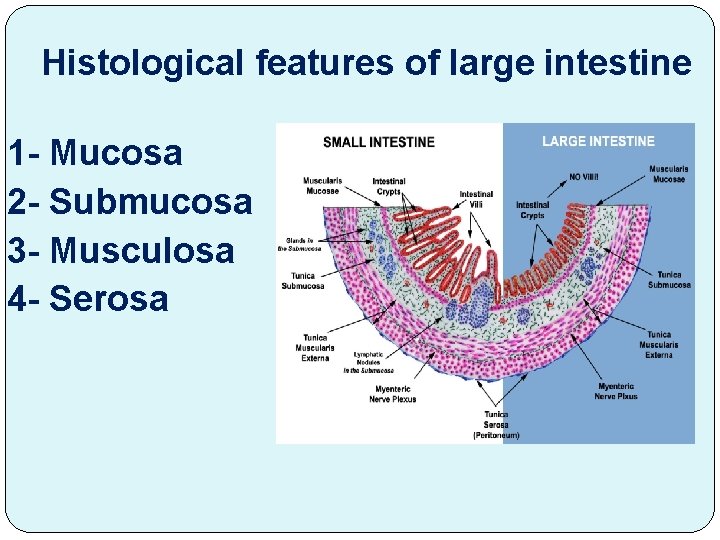
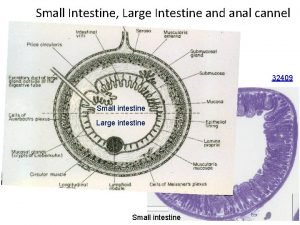
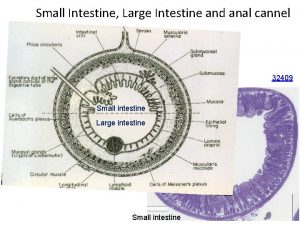
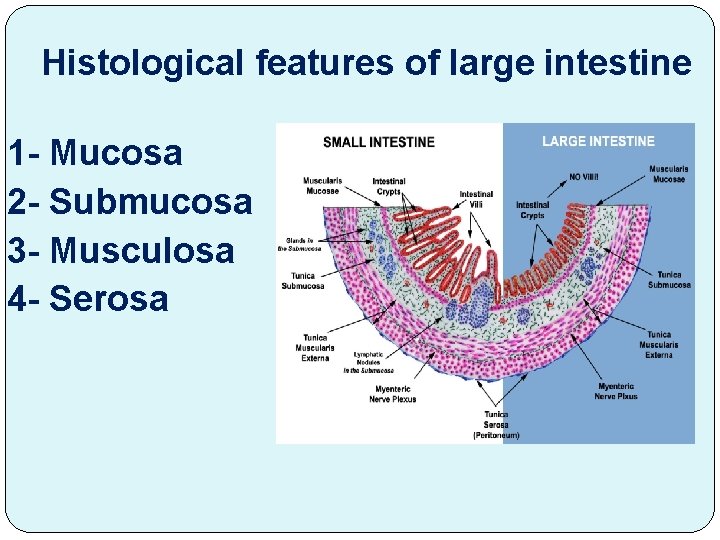
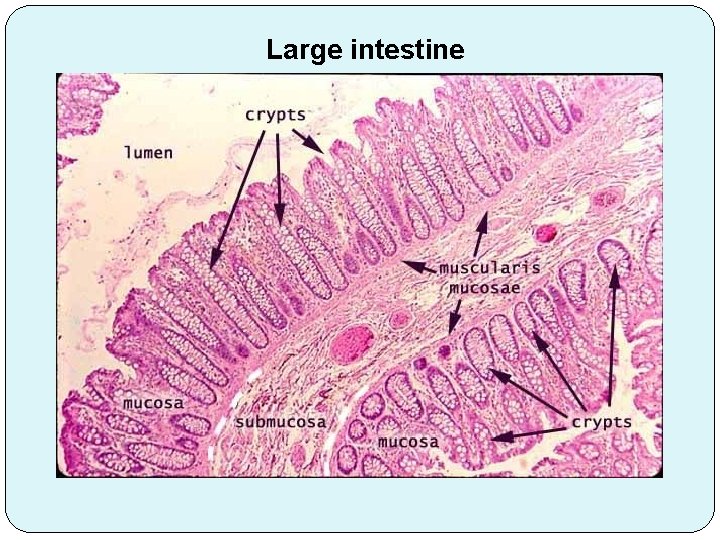
Histological features of large intestine 1 - Mucosa 2 - Submucosa 3 - Musculosa 4 - Serosa
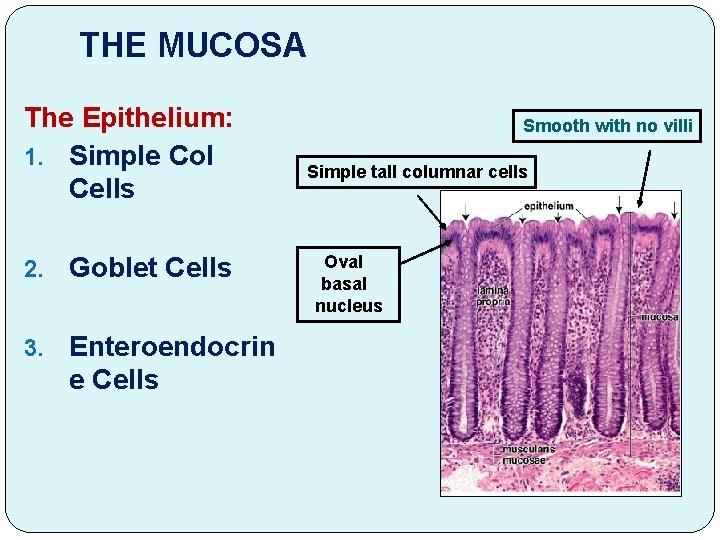
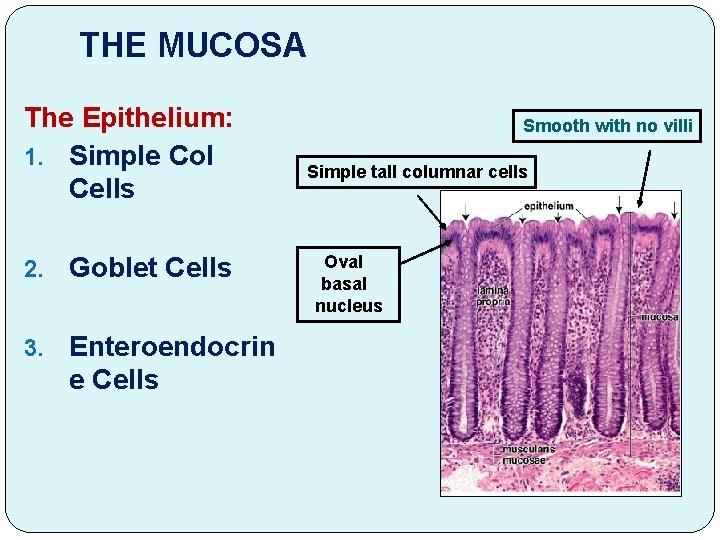
THE MUCOSA The Epithelium: 1. Simple Col Cells 2. Goblet Cells 3. Enteroendocrin e Cells Smooth with no villi Simple tall columnar cells Oval basal nucleus
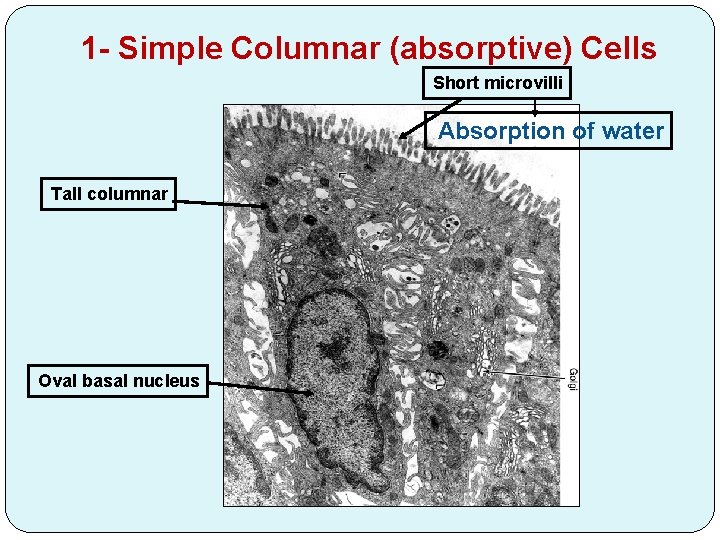
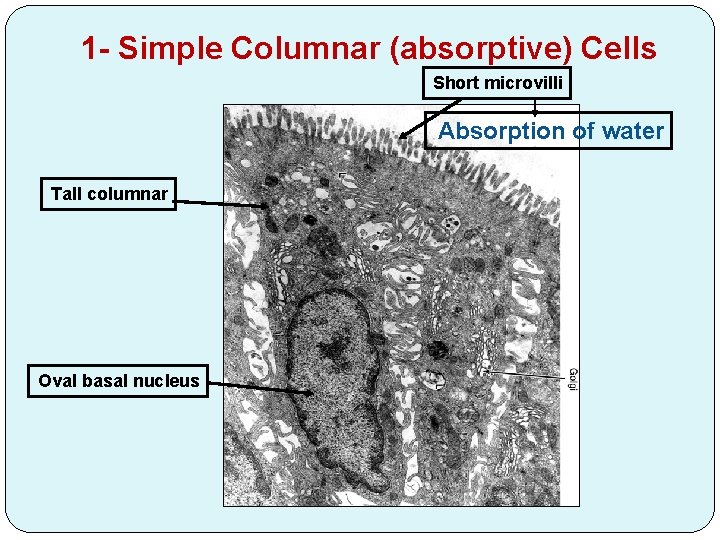
1 - Simple Columnar (absorptive) Cells Short microvilli Absorption of water Tall columnar Oval basal nucleus
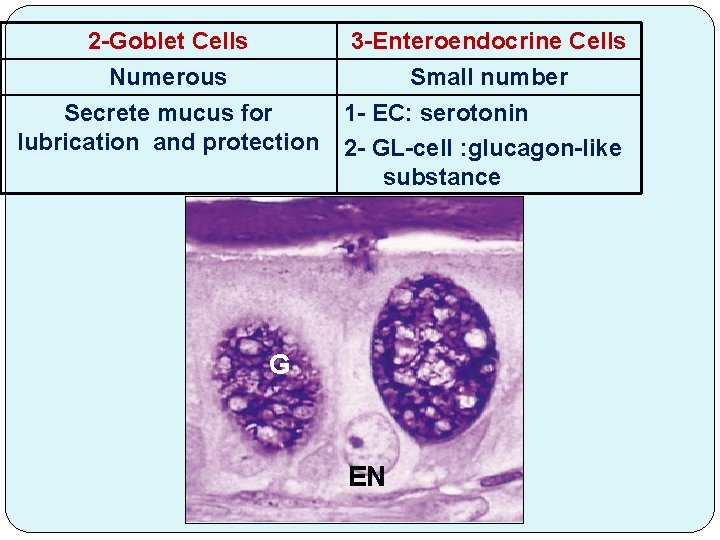
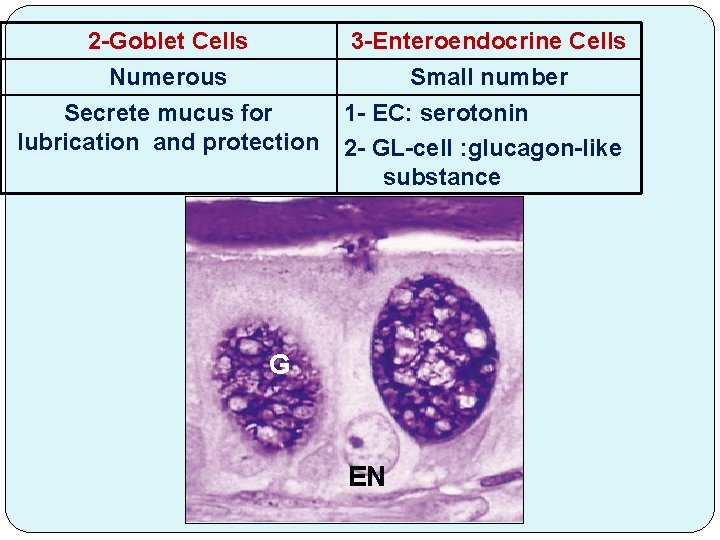
2 -Goblet Cells Numerous Secrete mucus for lubrication and protection 3 -Enteroendocrine Cells Small number 1 - EC: serotonin 2 - GL-cell : glucagon-like substance G EN
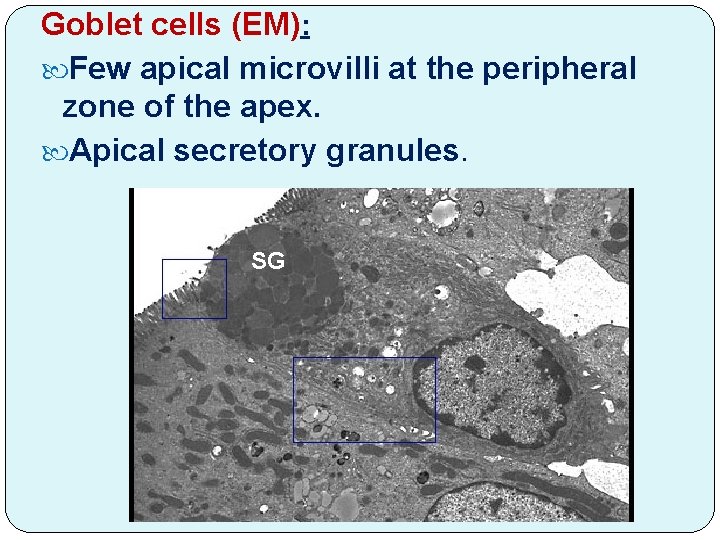
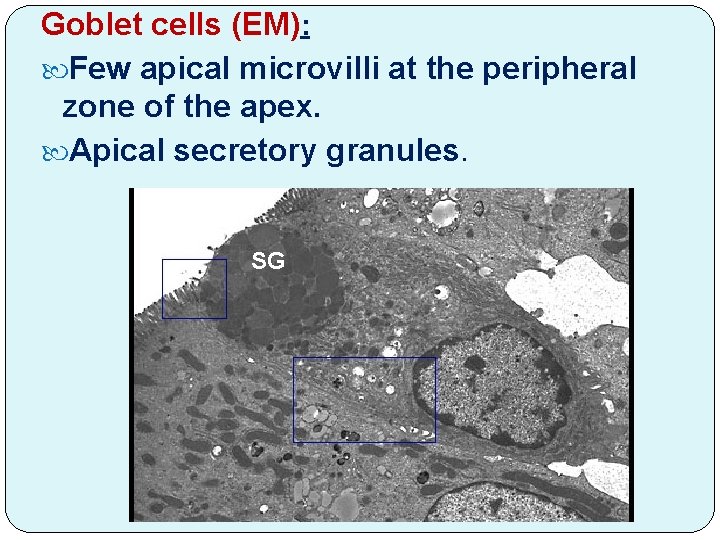
Goblet cells (EM): Few apical microvilli at the peripheral zone of the apex. Apical secretory granules. SG
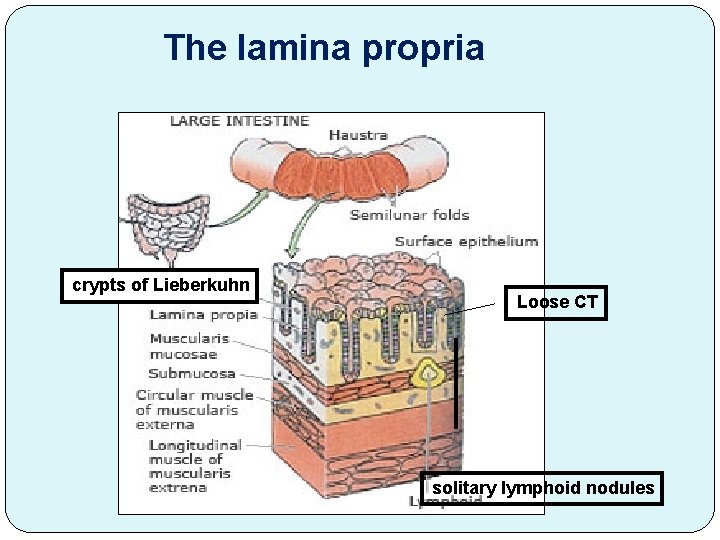
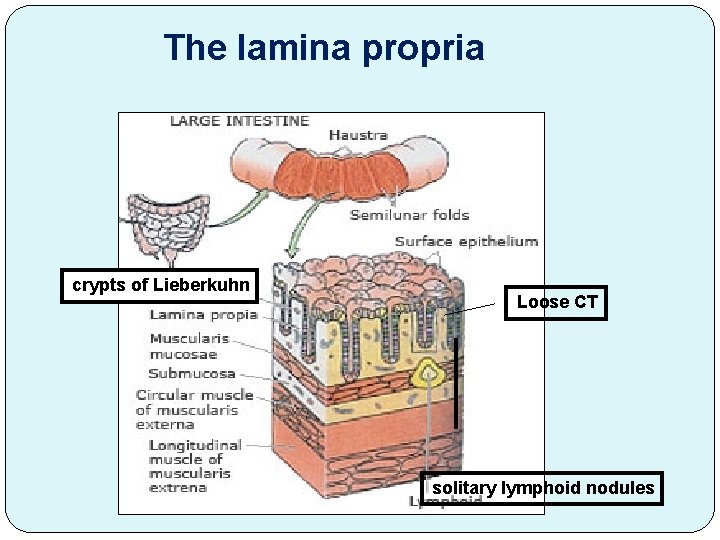
The lamina propria crypts of Lieberkuhn Loose CT solitary lymphoid nodules
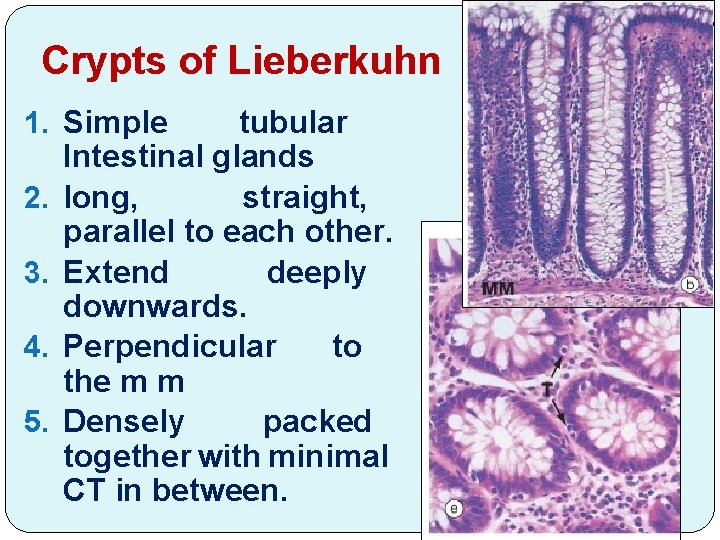
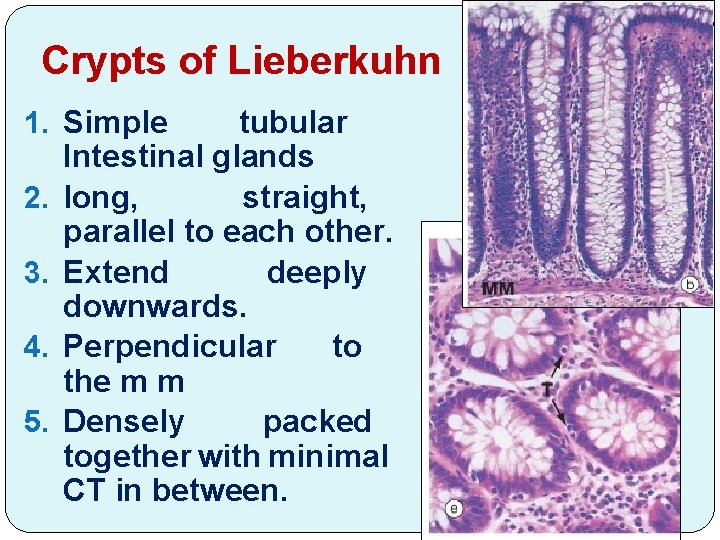
Crypts of Lieberkuhn 1. Simple tubular Intestinal glands 2. long, straight, parallel to each other. 3. Extend deeply downwards. 4. Perpendicular to the m m 5. Densely packed together with minimal CT in between.
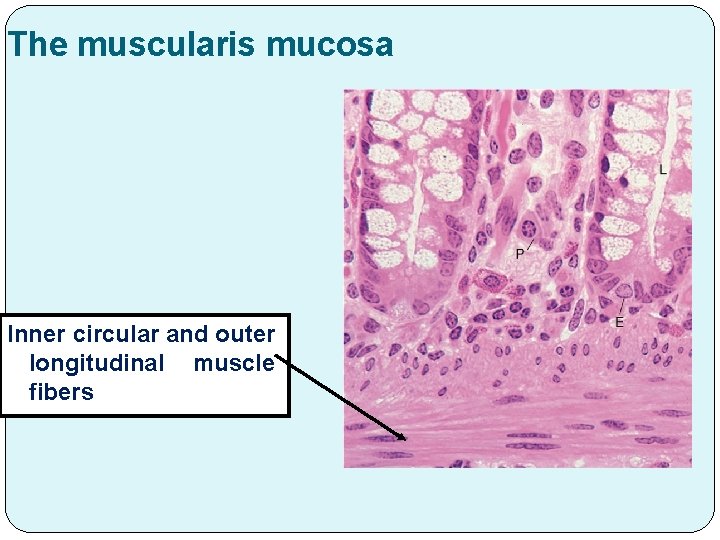
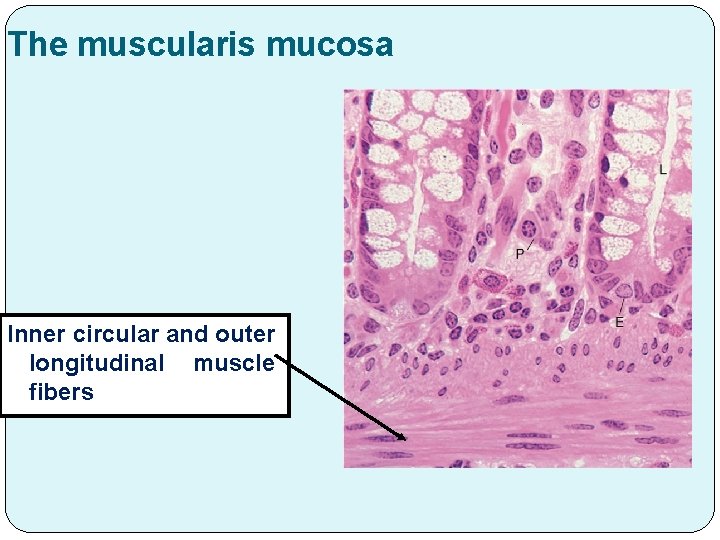
The muscularis mucosa Inner circular and outer longitudinal muscle fibers

The gland is lined by: 1. Undifferentiated Columnar Cells (stem cells): at the bases of the glands. They Proliferate and differentiate to the other types of lining cells. 2. Numerous goblet cells. 3. Few absorptive columnar cells. 4. Enteroendocrine Cells.
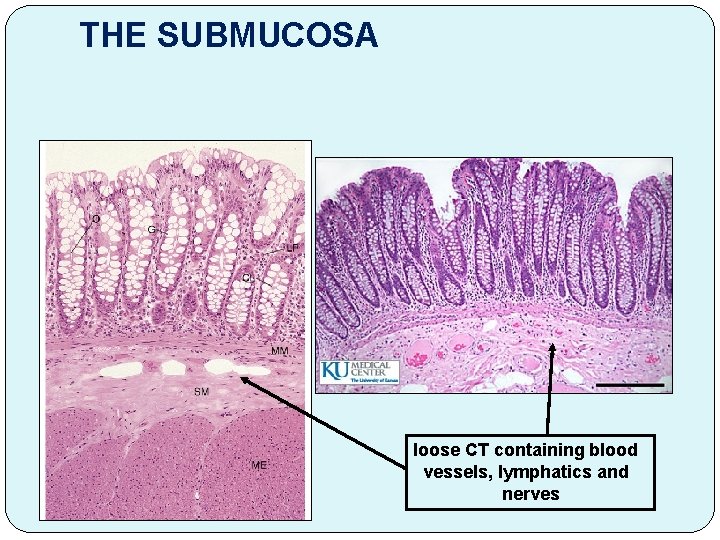
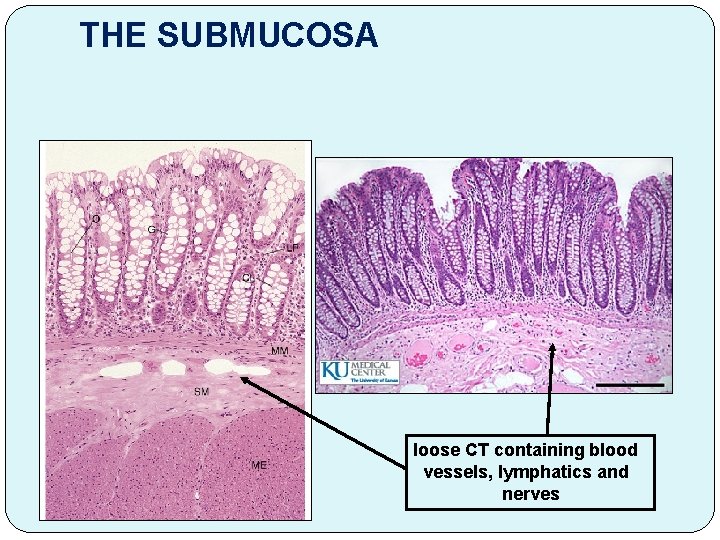
THE SUBMUCOSA loose CT containing blood vessels, lymphatics and nerves
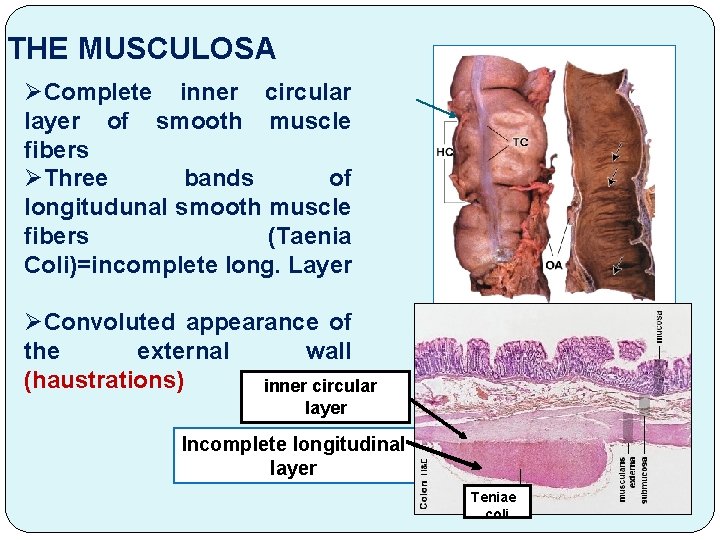
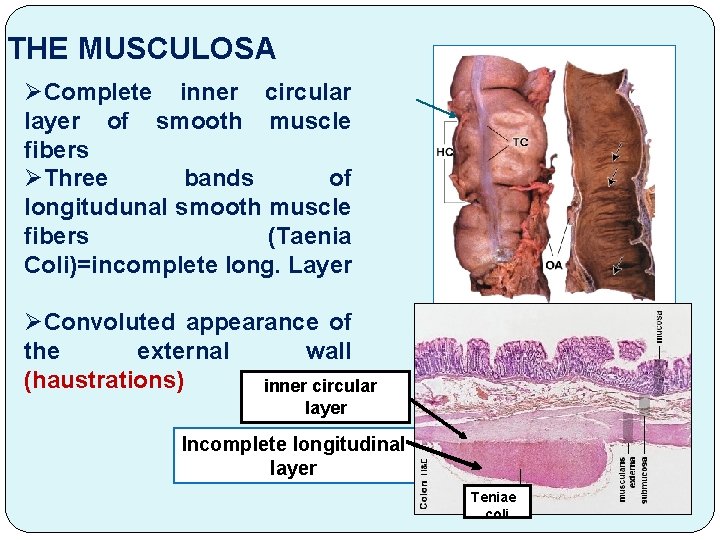
THE MUSCULOSA ØComplete inner circular layer of smooth muscle fibers ØThree bands of longitudunal smooth muscle fibers (Taenia Coli)=incomplete long. Layer ØConvoluted appearance of the external wall (haustrations) inner circular layer Incomplete longitudinal layer Teniae coli
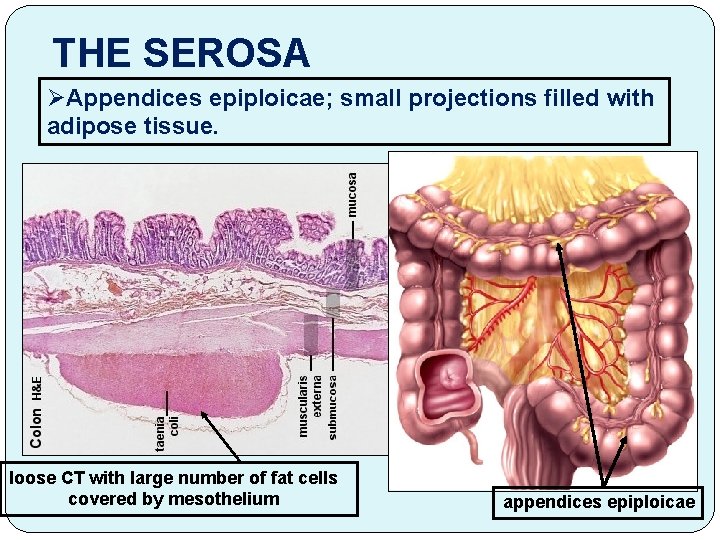
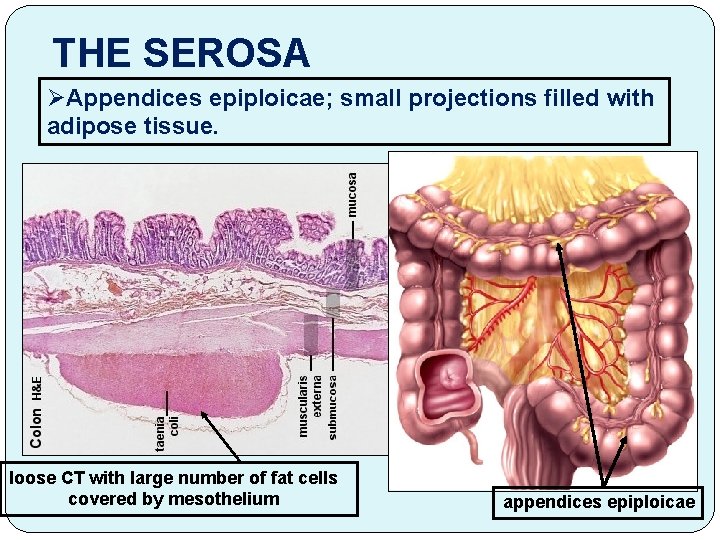
THE SEROSA ØAppendices epiploicae; small projections filled with adipose tissue. loose CT with large number of fat cells covered by mesothelium appendices epiploicae
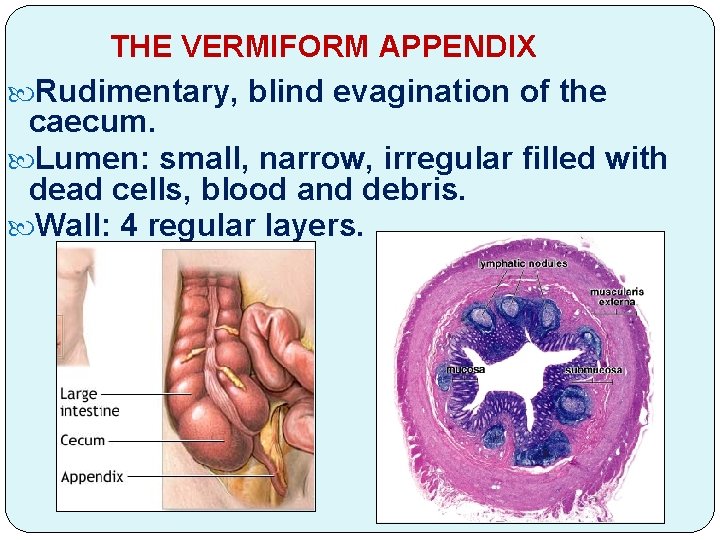
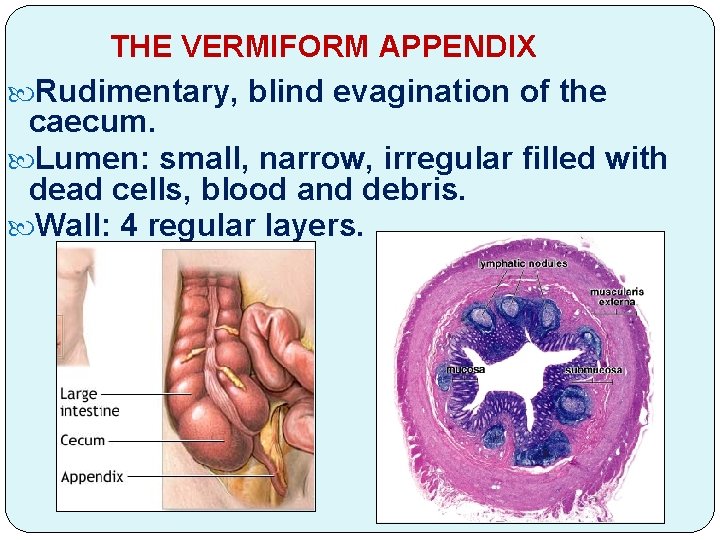
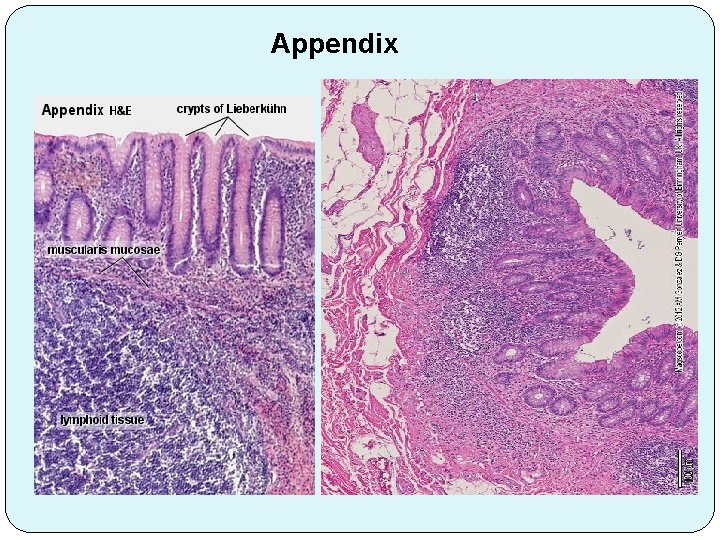
THE VERMIFORM APPENDIX Rudimentary, blind evagination of the caecum. Lumen: small, narrow, irregular filled with dead cells, blood and debris. Wall: 4 regular layers.
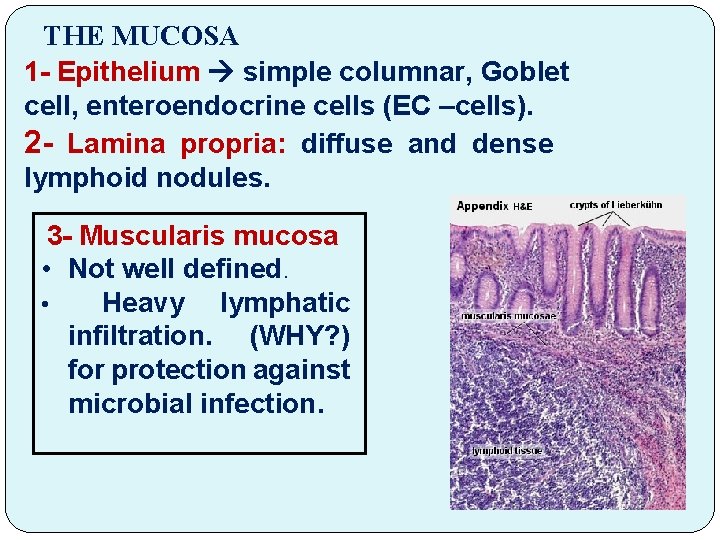
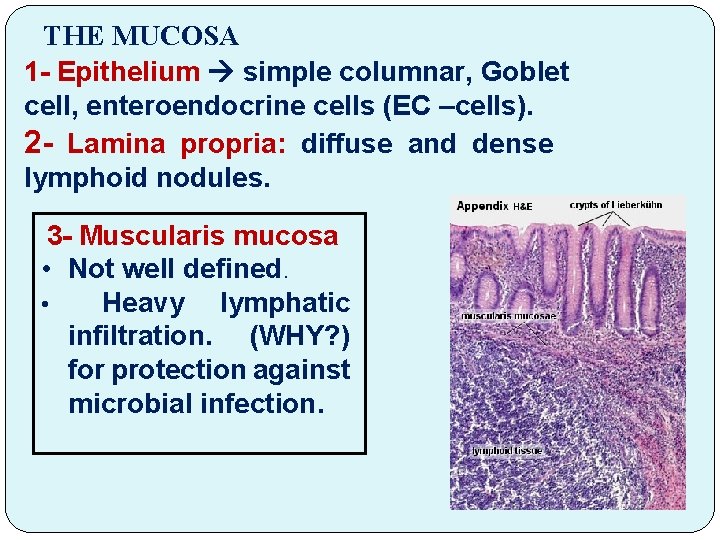
THE MUCOSA 1 - Epithelium simple columnar, Goblet cell, enteroendocrine cells (EC –cells). 2 - Lamina propria: diffuse and dense lymphoid nodules. 3 - Muscularis mucosa • Not well defined. • Heavy lymphatic infiltration. (WHY? ) for protection against microbial infection.
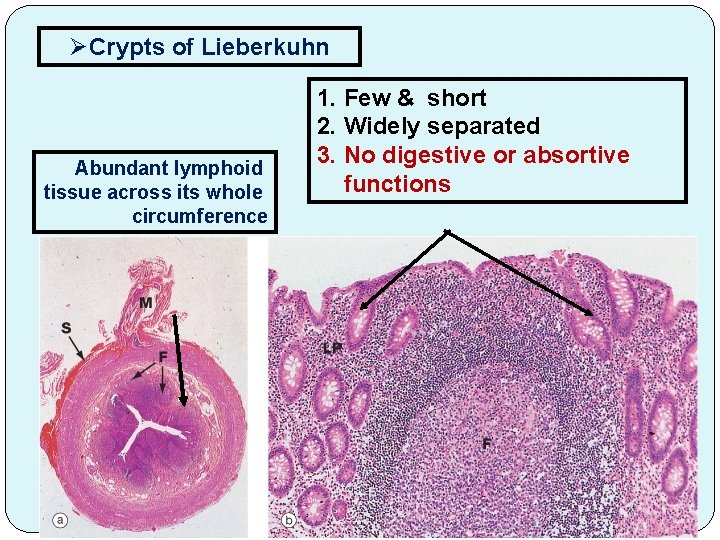
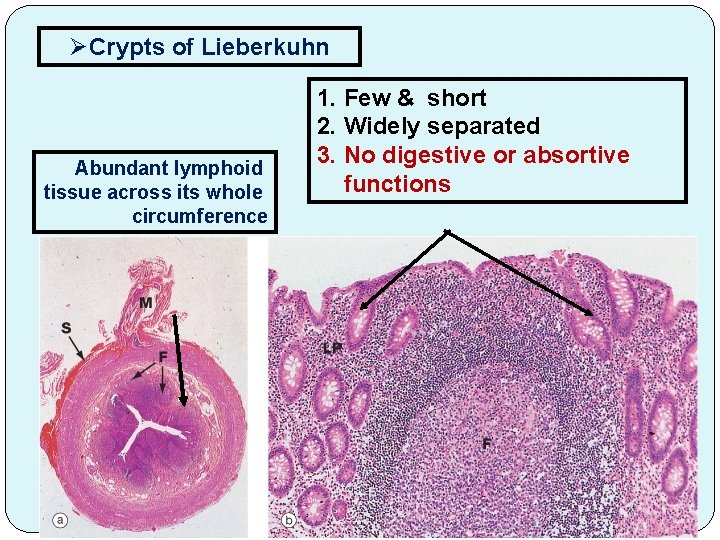
ØCrypts of Lieberkuhn Abundant lymphoid tissue across its whole circumference 1. Few & short 2. Widely separated 3. No digestive or absortive functions
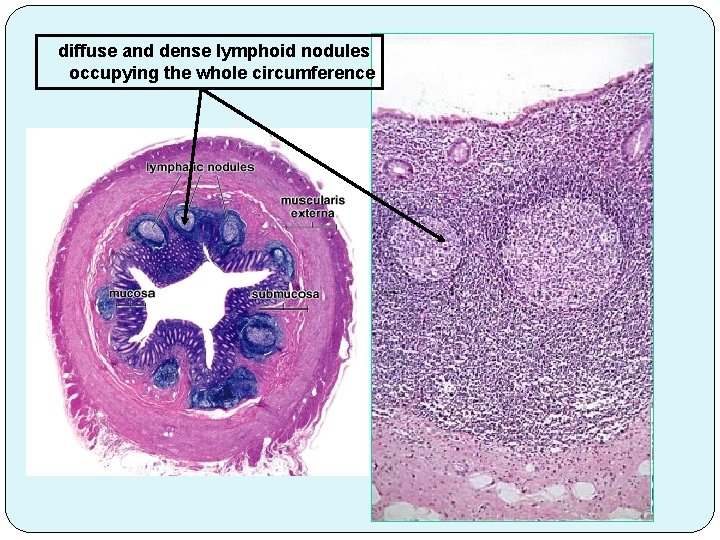
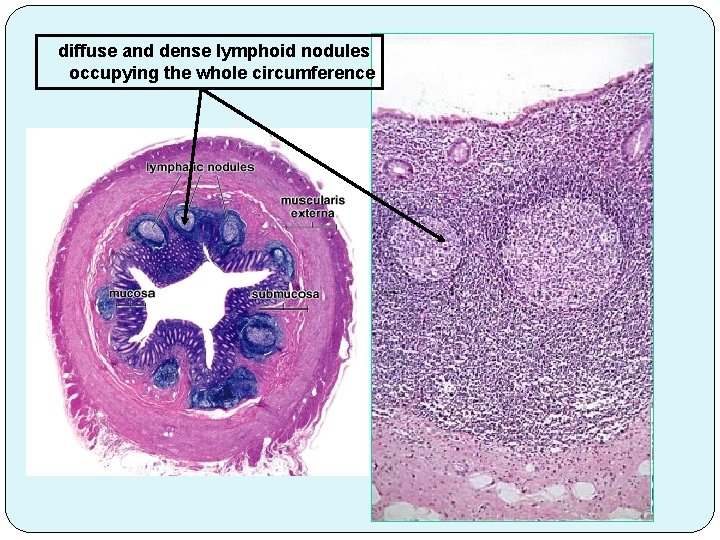
diffuse and dense lymphoid nodules occupying the whole circumference
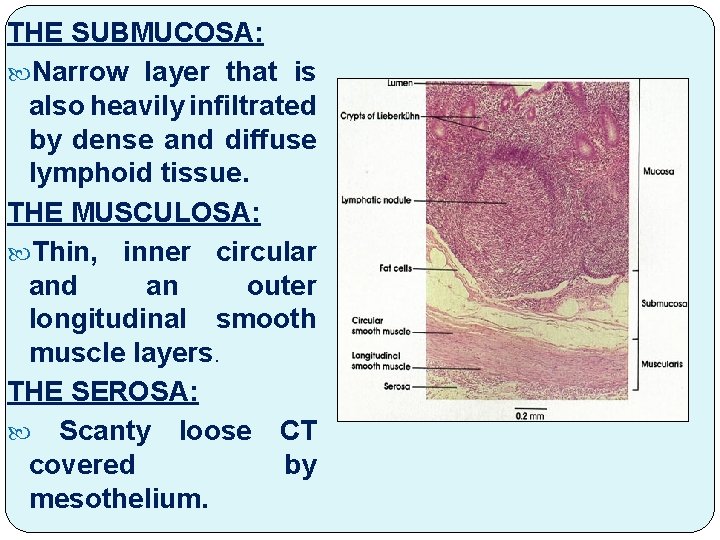
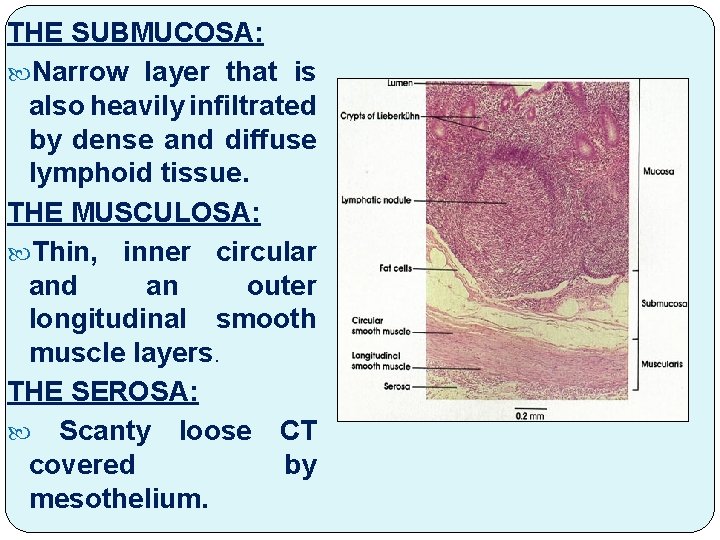
THE SUBMUCOSA: Narrow layer that is also heavily infiltrated by dense and diffuse lymphoid tissue. THE MUSCULOSA: Thin, inner circular and an outer longitudinal smooth muscle layers. THE SEROSA: Scanty loose CT covered by mesothelium.
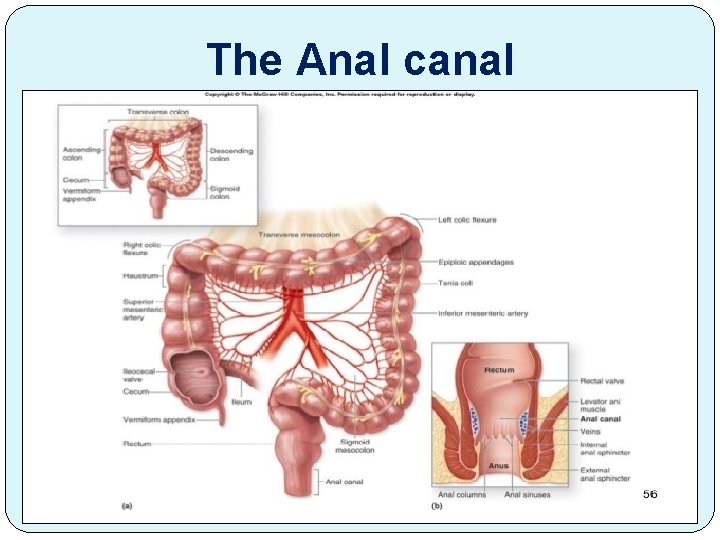
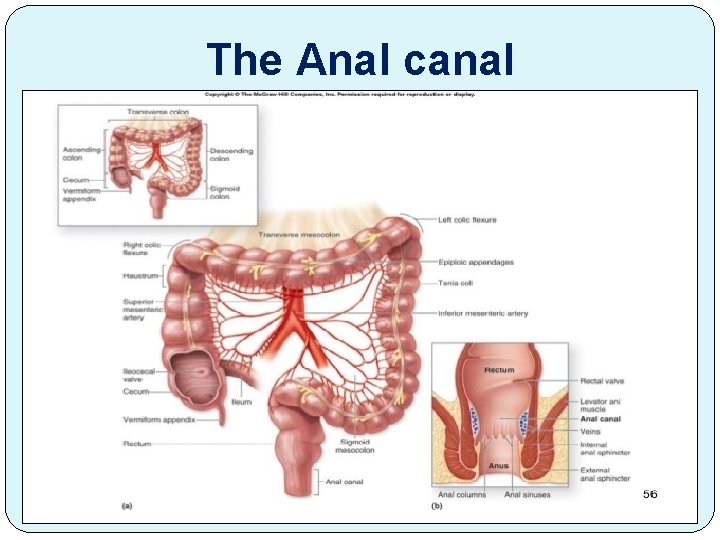
The Anal canal
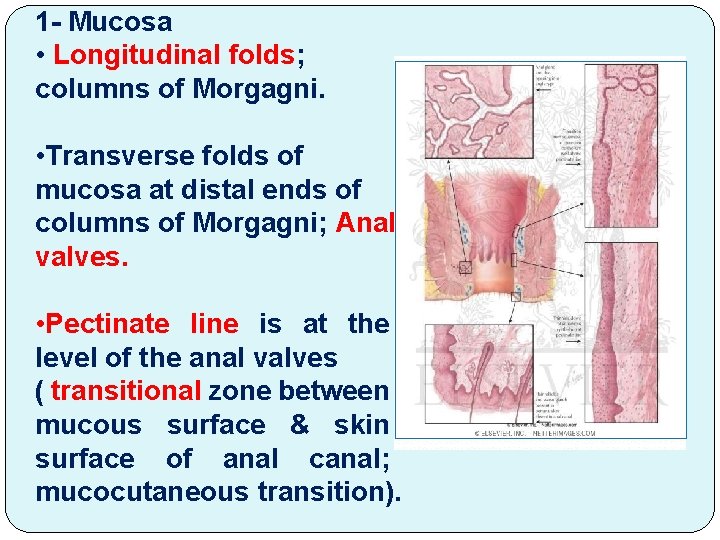
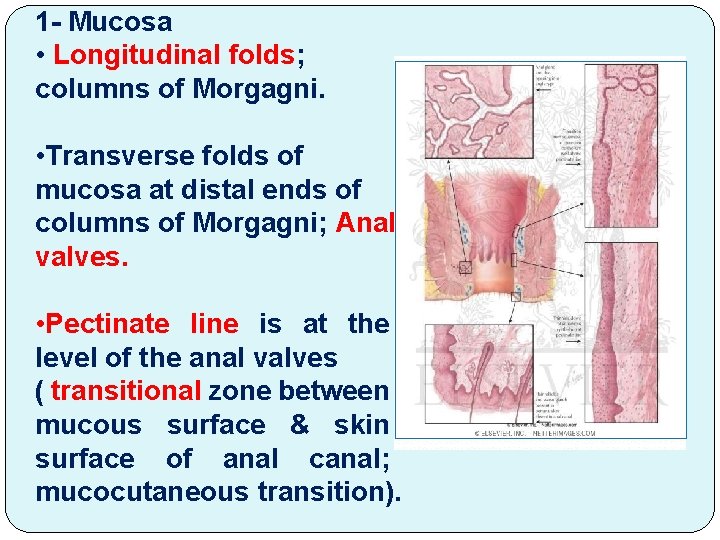
1 - Mucosa • Longitudinal folds; columns of Morgagni. • Transverse folds of mucosa at distal ends of columns of Morgagni; Anal valves. • Pectinate line is at the level of the anal valves ( transitional zone between mucous surface & skin surface of anal canal; mucocutaneous transition).
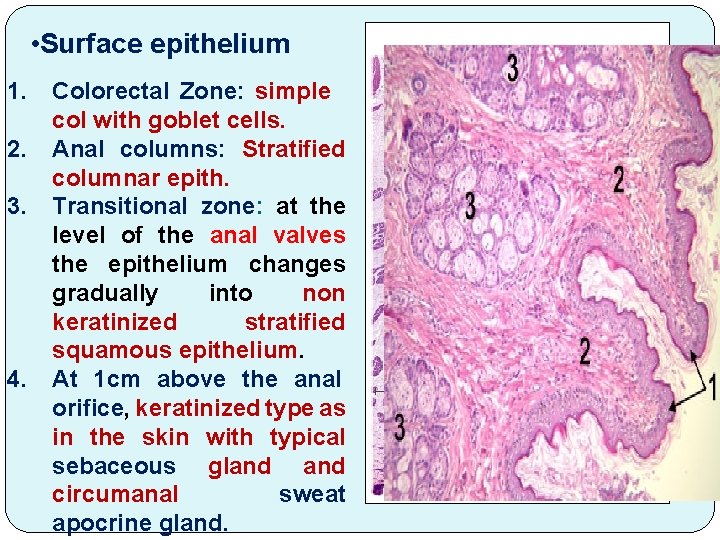
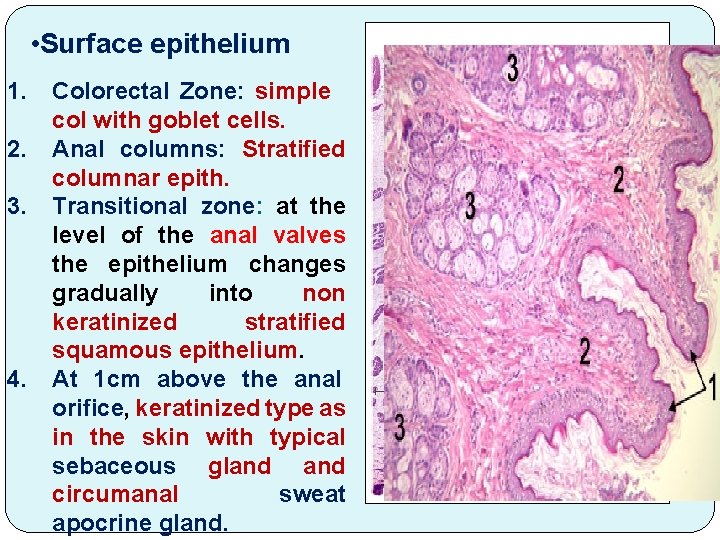
• Surface epithelium 1. 2. 3. 4. Colorectal Zone: simple col with goblet cells. Anal columns: Stratified columnar epith. Transitional zone: at the level of the anal valves the epithelium changes gradually into non keratinized stratified squamous epithelium. At 1 cm above the anal orifice, keratinized type as in the skin with typical sebaceous gland circumanal sweat apocrine gland.
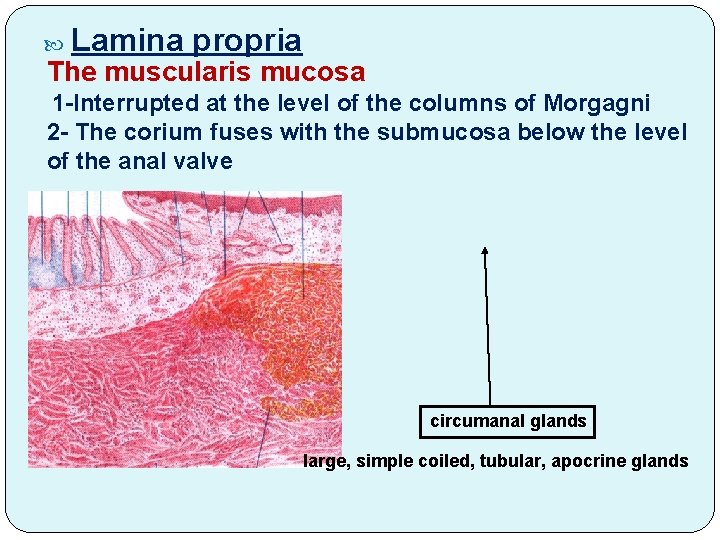
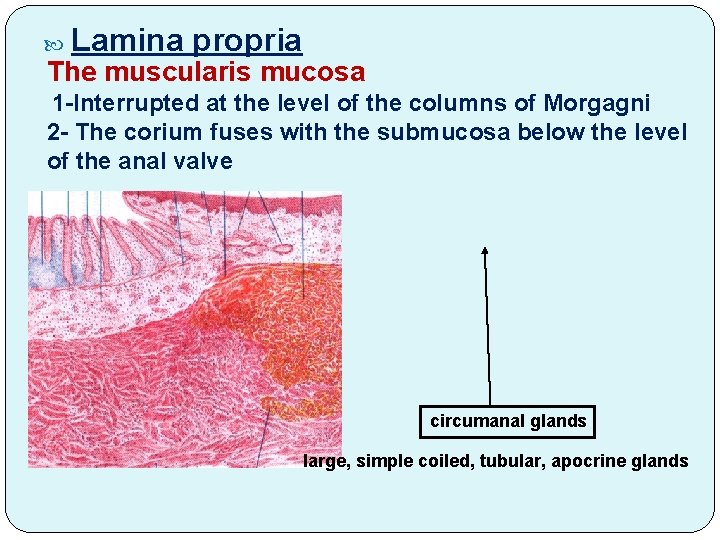
Lamina propria The muscularis mucosa 1 -Interrupted at the level of the columns of Morgagni 2 - The corium fuses with the submucosa below the level of the anal valve circumanal glands large, simple coiled, tubular, apocrine glands
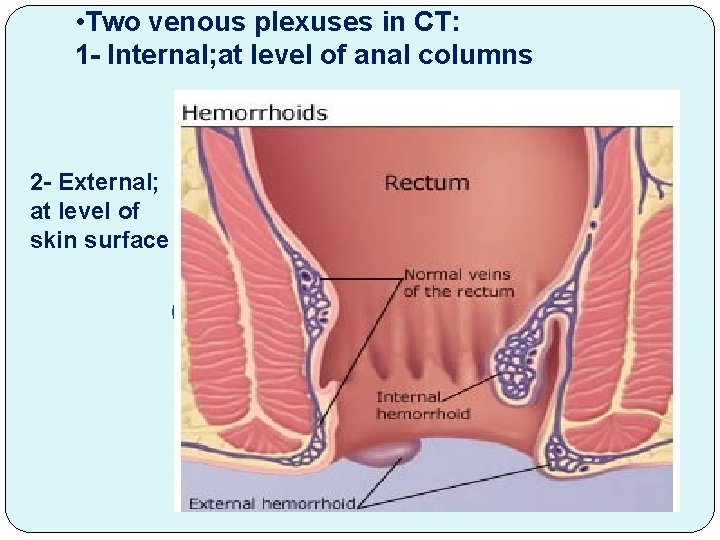
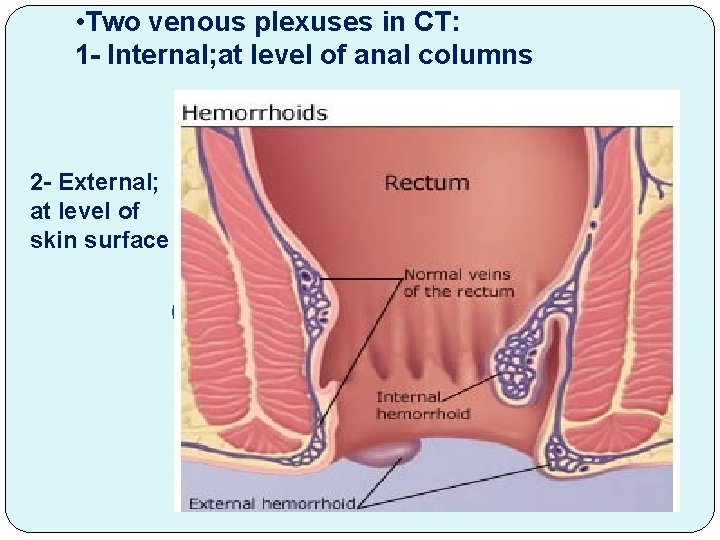
• Two venous plexuses in CT: 1 - Internal; at level of anal columns 2 - External; at level of skin surface
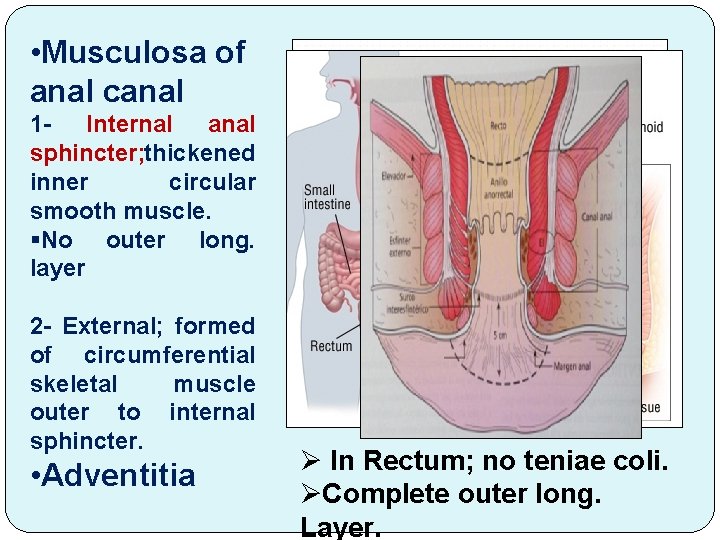
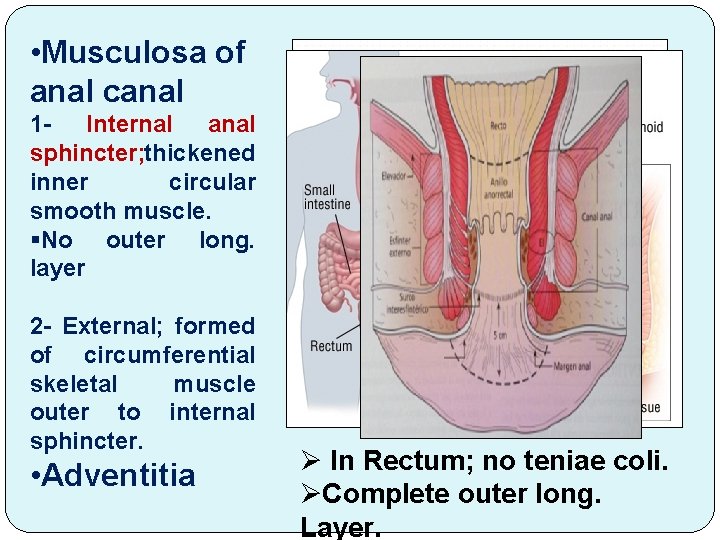
• Musculosa of anal canal 1 - Internal anal sphincter; thickened inner circular smooth muscle. §No outer long. layer 2 - External; formed of circumferential skeletal muscle outer to internal sphincter. • Adventitia Ø In Rectum; no teniae coli. ØComplete outer long. Layer.
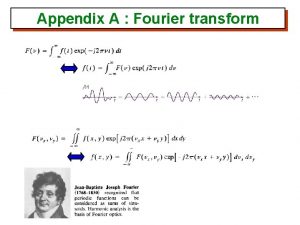
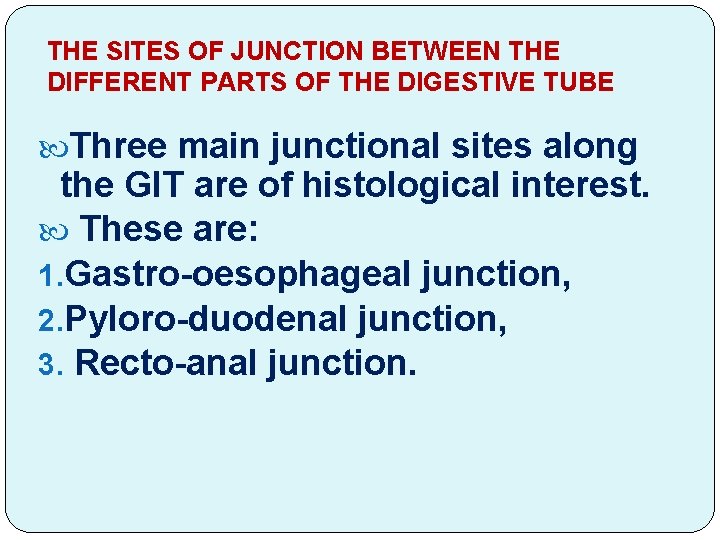
THE SITES OF JUNCTION BETWEEN THE DIFFERENT PARTS OF THE DIGESTIVE TUBE Three main junctional sites along the GIT are of histological interest. These are: 1. Gastro-oesophageal junction, 2. Pyloro-duodenal junction, 3. Recto-anal junction.

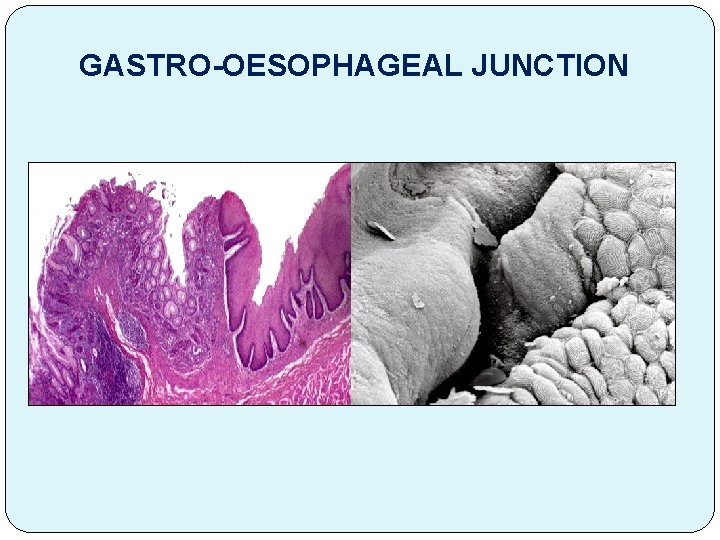
Gastro-oesophageal junction 1 - The epithelium: abrupt change from non ker st sq (oesophagus) to simple col interrupted by gastric pits(stomach).
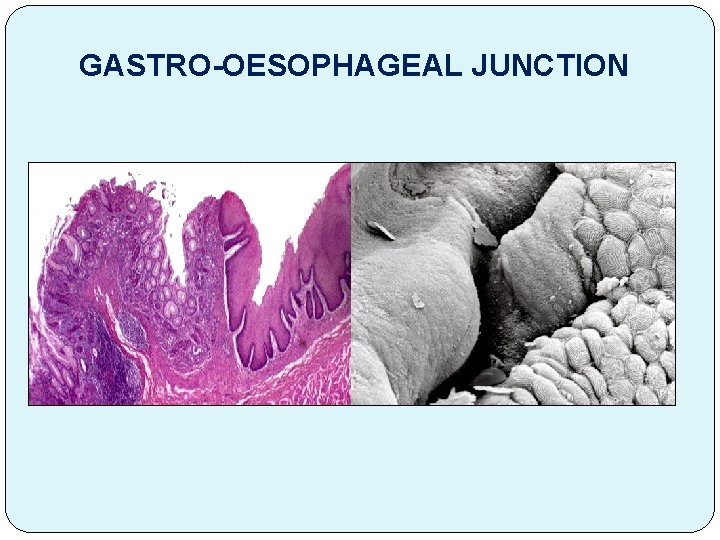
GASTRO-OESOPHAGEAL JUNCTION
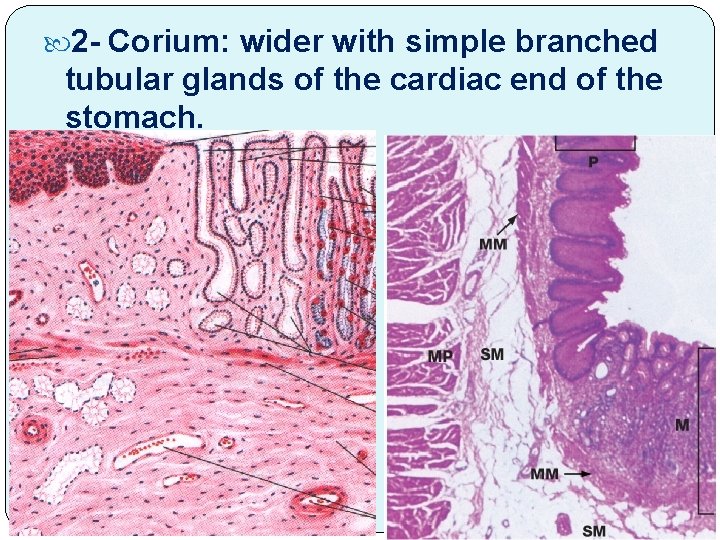
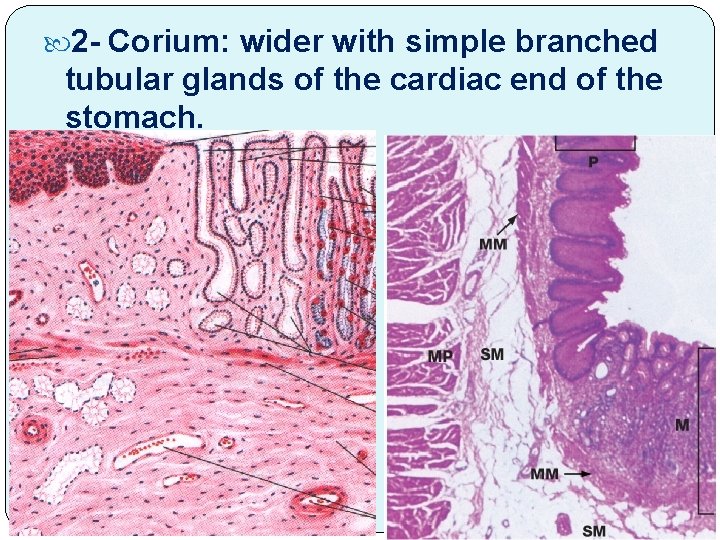
2 - Corium: wider with simple branched tubular glands of the cardiac end of the stomach.
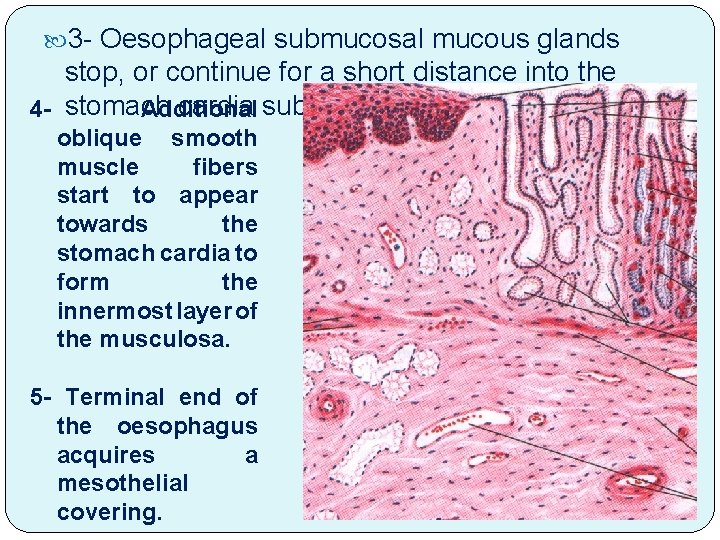
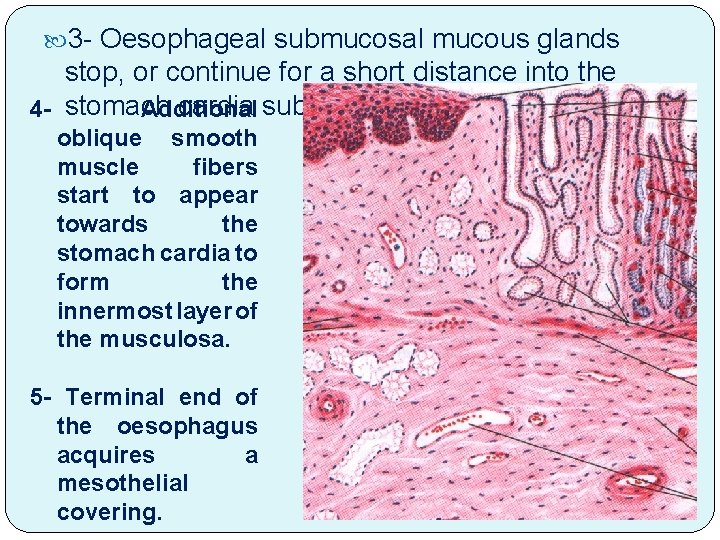
3 - Oesophageal submucosal mucous glands stop, or continue for a short distance into the cardia submucosa. 4 - stomach Additional oblique smooth muscle fibers start to appear towards the stomach cardia to form the innermost layer of the musculosa. 5 - Terminal end of the oesophagus acquires a mesothelial covering.
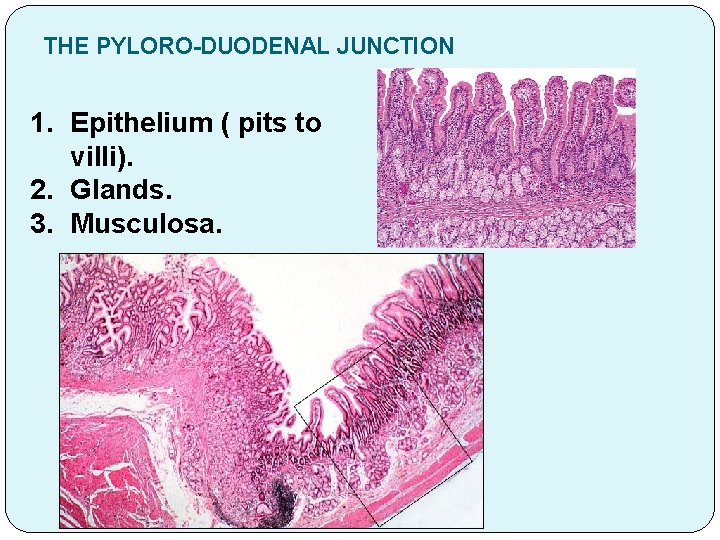
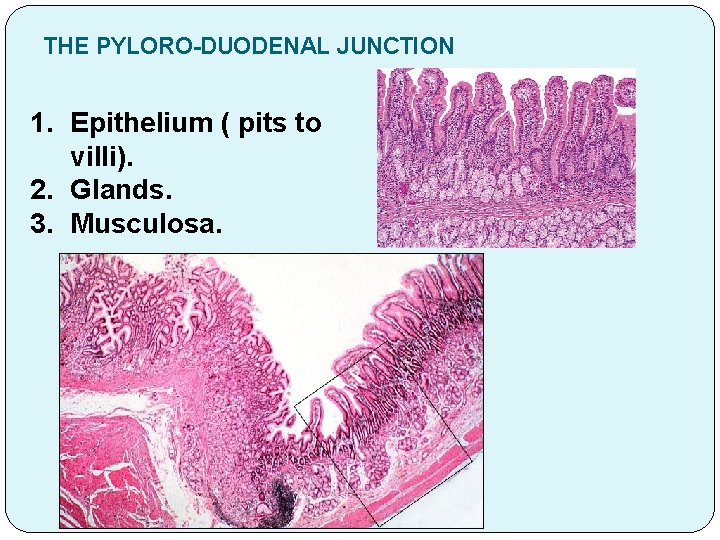
THE PYLORO-DUODENAL JUNCTION 1. Epithelium ( pits to villi). 2. Glands. 3. Musculosa.
Practical
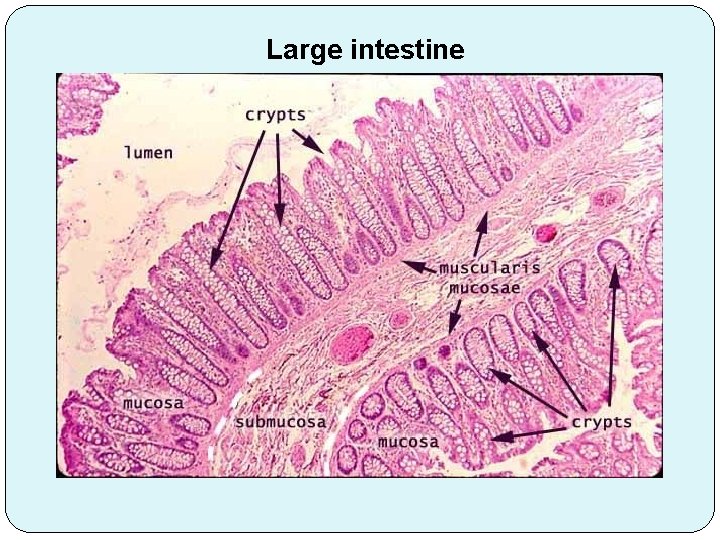
Large intestine
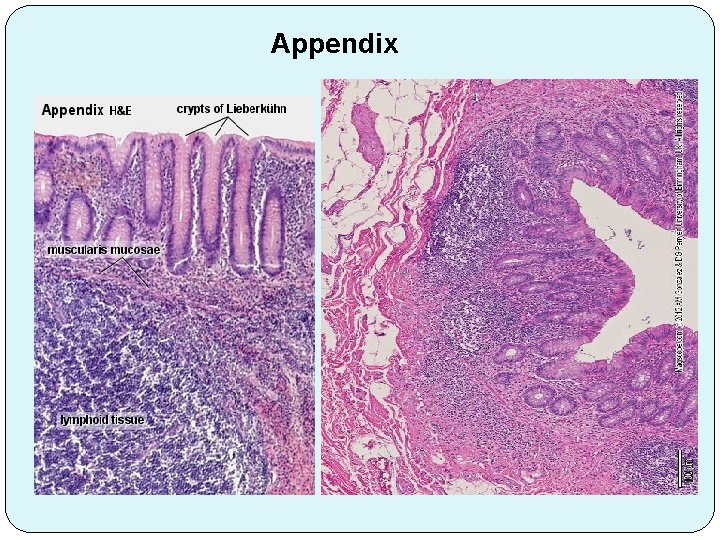
Appendix
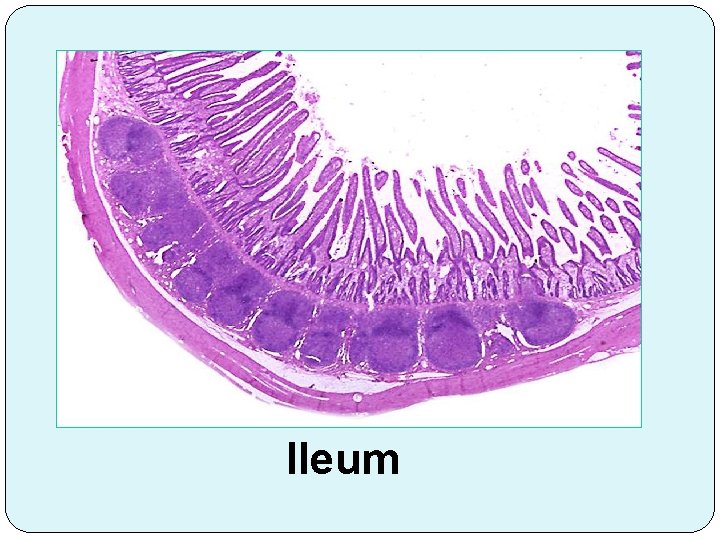
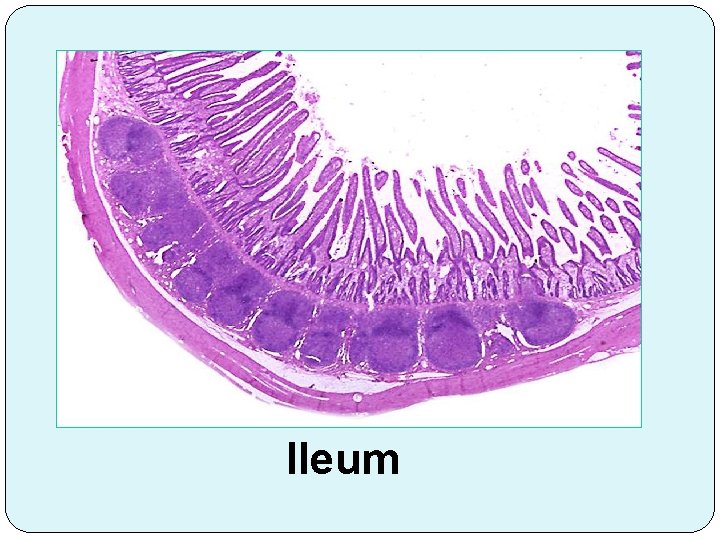
Ileum
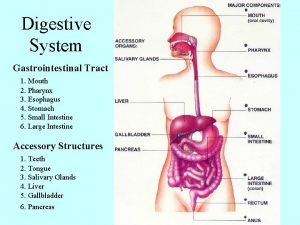
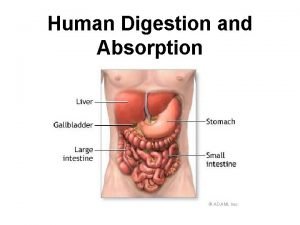
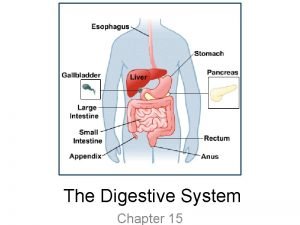
 Esophagus stomach small intestine large intestine
Esophagus stomach small intestine large intestine Micrographs
Micrographs Cephalic body region
Cephalic body region Body directional terms
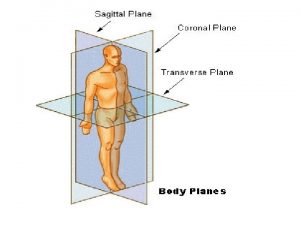
Body directional terms Body directions and planes
Body directions and planes Pharynx
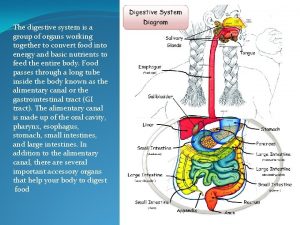
Pharynx Large intestine function in digestive system
Large intestine function in digestive system The main jobs of the large intestine are _____.
The main jobs of the large intestine are _____. Elsevier
Elsevier Large intestine function
Large intestine function Taenia histology
Taenia histology Orange juice ph
Orange juice ph Peristalsis definition
Peristalsis definition Small intestine main functions
Small intestine main functions Functions of the large intestine
Functions of the large intestine Large intestine function in digestive system
Large intestine function in digestive system Equine
Equine Lymphoid tissue in colon
Lymphoid tissue in colon Part of large intestine
Part of large intestine Lanz point
Lanz point Intertubercular plane
Intertubercular plane Label large intestine
Label large intestine Digestive system enzymes chart
Digestive system enzymes chart Root of mesentery
Root of mesentery Large intestine function in digestive system
Large intestine function in digestive system Cecum anatomy
Cecum anatomy Anatomical seclusion
Anatomical seclusion Anatomy of a journey
Anatomy of a journey Anatomical structure of urinary system
Anatomical structure of urinary system Gummy bear anatomy lab
Gummy bear anatomy lab Anatomical location
Anatomical location Anatomical modifier
Anatomical modifier Foot loves
Foot loves Uniform anatomical gift act
Uniform anatomical gift act Uniform anatomical gift act definition
Uniform anatomical gift act definition Anatomical position supine
Anatomical position supine Anatomical position
Anatomical position