The digestive system is a group of organs


- Slides: 34
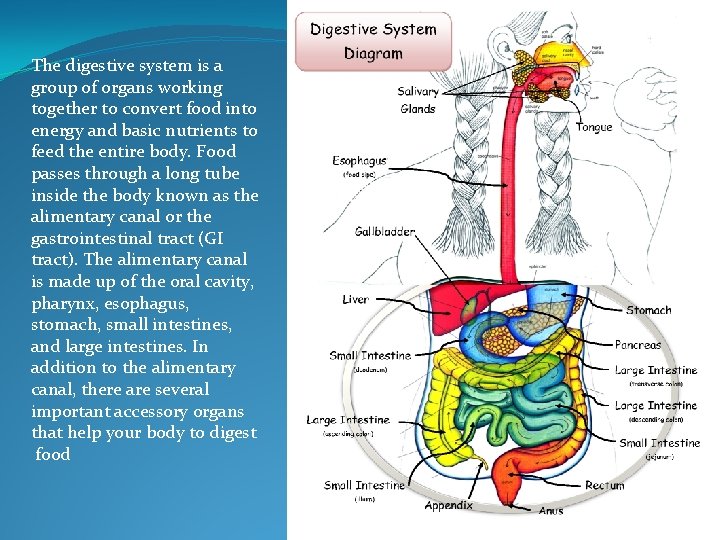
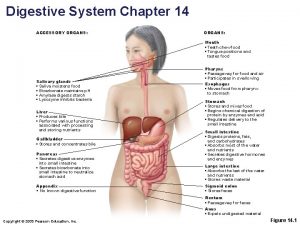
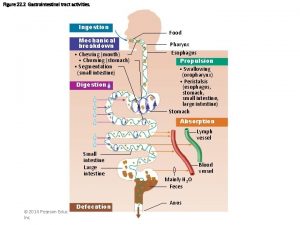
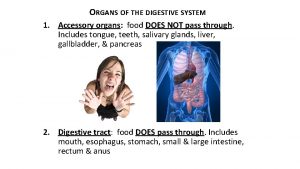
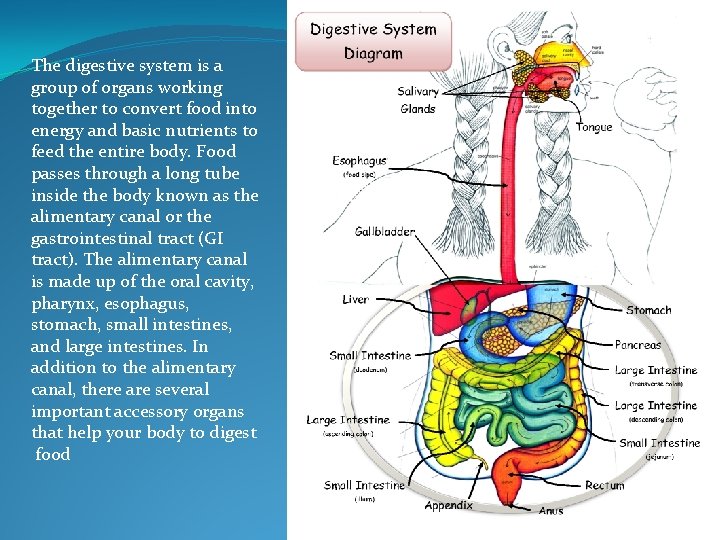
The digestive system is a group of organs working together to convert food into energy and basic nutrients to feed the entire body. Food passes through a long tube inside the body known as the alimentary canal or the gastrointestinal tract (GI tract). The alimentary canal is made up of the oral cavity, pharynx, esophagus, stomach, small intestines, and large intestines. In addition to the alimentary canal, there are several important accessory organs that help your body to digest food
The human digestive system consists of the gastrointestinal tract plus the accessory organs of digestion (the tongue, salivary glands, pancreas, liver, and gallbladder). In this system, the process of digestion has many stages, the first of which starts in the mouth (oral cavity). Digestion involves the breakdown of food into smaller and smaller components which can be absorbed and assimilated into the body. The secretion of saliva helps to produce a bolus which can be swallowed to pass down the oesophagus and into the stomach.
Saliva also contains a catalytic enzyme called amylase which starts to act on food in the mouth. Another digestive enzyme called lingual lipase is secreted by some of the lingual papillae on the tongue and also from serous glands in the main salivary glands. Digestion is helped by themastication of food by the teeth and also by the muscular actions of peristalsis and segmentation contractions. Gastric juice in the stomach is essential for the continuation of digestion as is the production of mucus in the stomach.
Peristalsis is the rhythmic contraction of muscles that begins in the oesophagus and continues along the wall of the stomach and the rest of thegastrointestinal tract. This initially results in the production of chyme which when fully broken down in the small intestine is absorbed as chyle into the lymphatic system. Most of the digestion of food takes place in the small intestine. Water and some minerals are reabsorbed back into the blood in the colon of the large intestine. The waste products of digestion are defecated from the anus via the rectum
Pharynx • Lined by Stratified non keratinized squamous epithelium in region continuous with esophagus. • Lined by ciliated pseudostratified columnar epithelium containing goblet cells in region close to nasal cavity. • Contains tonsils. • Mucosa of pharynx also has many small mucous salivary glands in its lamina propria • Compose of dense connective tissues
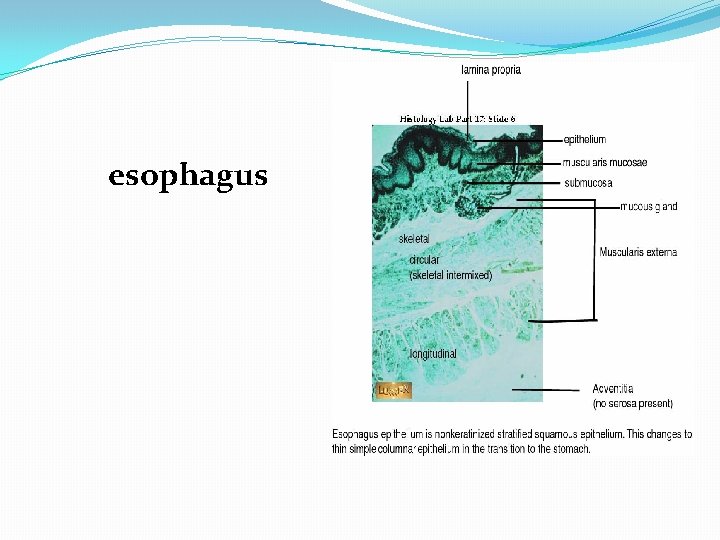
1. Esophagus 2. . Only striated muscle cells • Portion in peritoneal cavity covered by serosa • The other portion covered by layer of connective tissue, adventitia that blends into surrounding tissue. Mixture of striated and smooth muscle • Proximal end Only smooth muscle • Mid Portion groups of gland (esophageal cardiac gland) secrete mucus • Distal end muscular layer groups of small mucous secreting glands (esophageal glands) secretion facilitated transport of food stuff and protects mucosa. • Lamina Propria near stomach Esophagus • Muscular Tube function to transport food stuffs from mouth to stomach • Covered by non keratinized stratified squamous epithelium. • In general same layers as rest of digestive tract. • In submucosa 3. . Loweresophagus. Upperesophagus
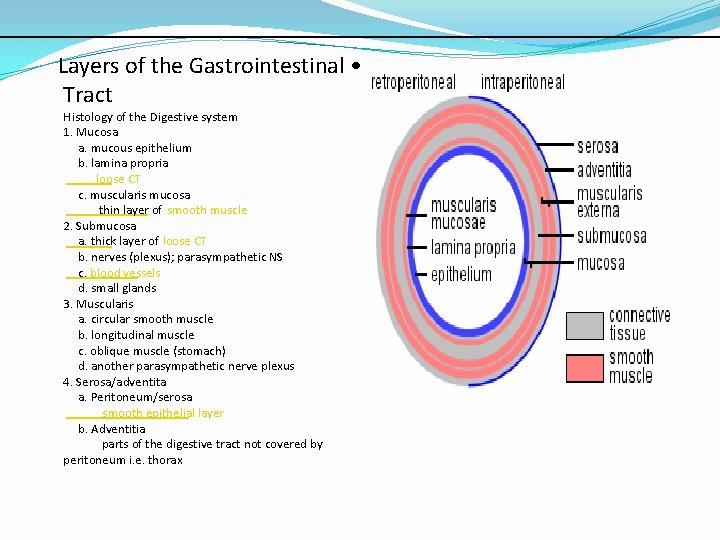
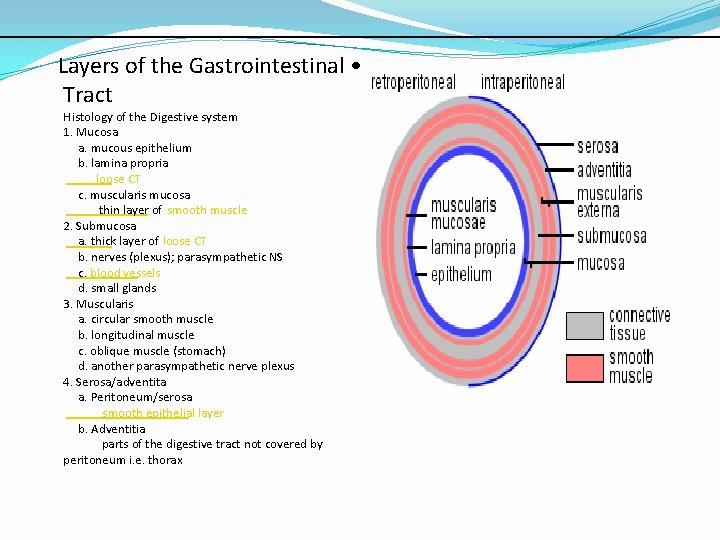
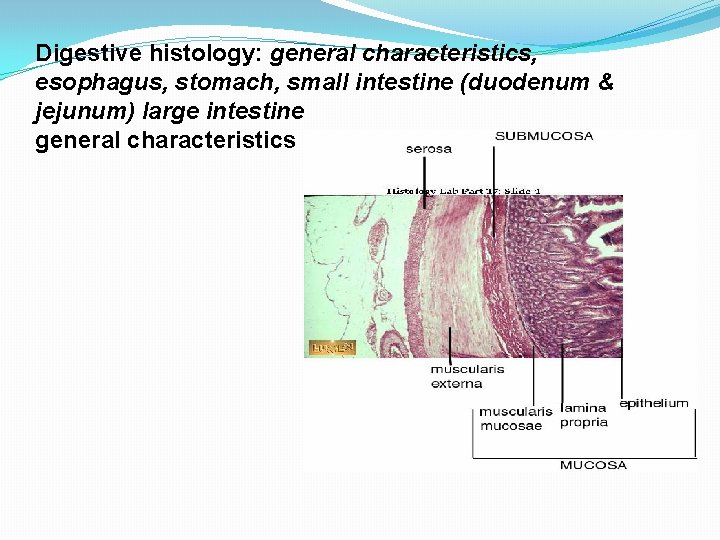
Layers of the Gastrointestinal • Tract Histology of the Digestive system 1. Mucosa a. mucous epithelium b. lamina propria loose CT c. muscularis mucosa thin layer of smooth muscle 2. Submucosa a. thick layer of loose CT b. nerves (plexus); parasympathetic NS c. blood vessels d. small glands 3. Muscularis a. circular smooth muscle b. longitudinal muscle c. oblique muscle (stomach) d. another parasympathetic nerve plexus 4. Serosa/adventita a. Peritoneum/serosa smooth epithelial layer b. Adventitia parts of the digestive tract not covered by peritoneum i. e. thorax
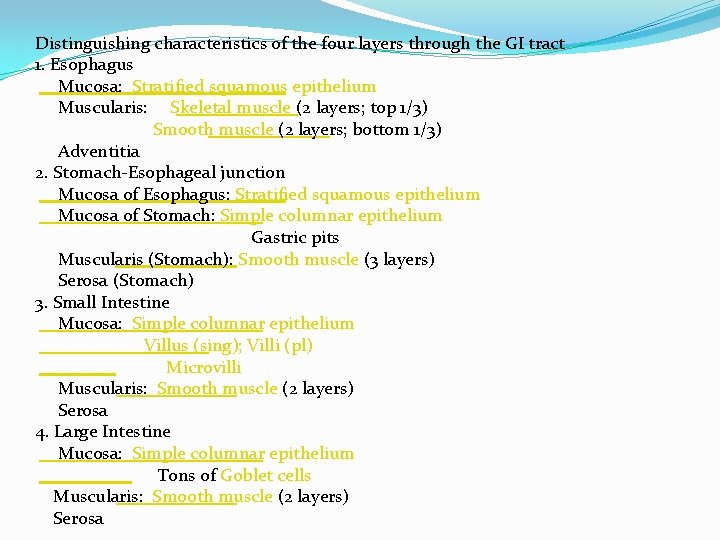
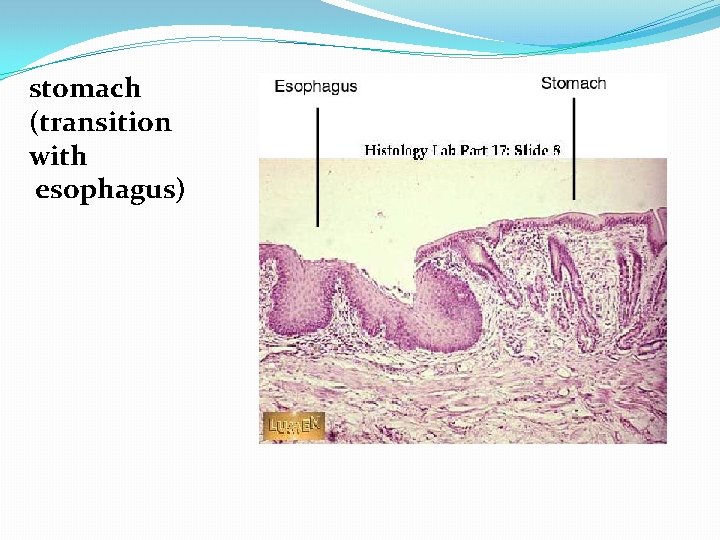
Distinguishing characteristics of the four layers through the GI tract 1. Esophagus Mucosa: Stratified squamous epithelium Muscularis: Skeletal muscle (2 layers; top 1/3) Smooth muscle (2 layers; bottom 1/3) Adventitia 2. Stomach-Esophageal junction Mucosa of Esophagus: Stratified squamous epithelium Mucosa of Stomach: Simple columnar epithelium Gastric pits Muscularis (Stomach): Smooth muscle (3 layers) Serosa (Stomach) 3. Small Intestine Mucosa: Simple columnar epithelium Villus (sing); Villi (pl) Microvilli Muscularis: Smooth muscle (2 layers) Serosa 4. Large Intestine Mucosa: Simple columnar epithelium Tons of Goblet cells Muscularis: Smooth muscle (2 layers) Serosa
Oesophagus The oesophagus is an organ which consists of a muscular tube through which food passes from the pharynx to the stomach. The oesophagus is continuous with the laryngeal part of the pharynx. It passes through the posterior mediastinum in the thorax and enters the stomach through a hole in the thoracic diaphragm–Its length averages 25 cm, varying with height. It is divided into cervical, thoracic and abdominal parts. The pharynx joins the oesophagus at the oesophageal inlet which is behind At rest the oesophagus is closed at both ends, by the upper and lower oesophageal sphincters. The opening of the upper sphincter is triggered by the swallowing reflex so that food is allowed through. The sphincter also serves to prevent back flow from the oesophagus into the pharynx.
The oesophagus has a mucous membrane and the epithelium which has a protective function is continuously replaced due to the volume of food that passes inside the oesophagus. During swallowing, food passes from the mouth through the pharynx into the oesophagus. The epiglottis folds down to a more horizontal position so as to prevent food from going into the trachea, instead directing it to the oesophagus. Once in the oesophagus, the bolus travels down to the stomach via rhythmic contraction and relaxation of muscles known as peristalsis. The lower oesophageal sphincter is a muscular sphincter surrounding the lower part of the oesophagus. The junction between the oesophagus and the stomach (the gastroesophageal junction) is controlled by the lower oesophageal sphincter, which remains constricted at all times other than during swallowing and vomiting to prevent the contents of the stomach from entering the oesophagus. As the oesophagus does not have the same protection from acid as the stomach, any failure of this sphincter can lead to heartburn. The oesophagus has a mucous membrane of epithelium which has a protective function as well as providing a smooth surface for the passage of food. Due to the high volume of food that is passed over time, this membrane is continuously renewed.
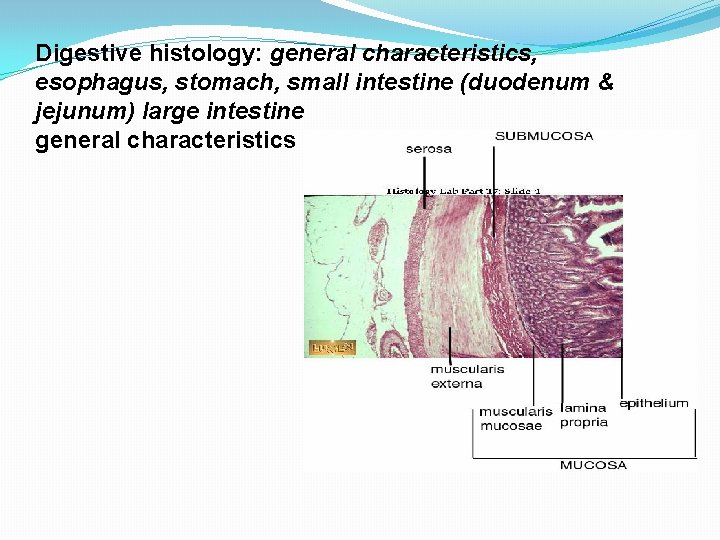
Digestive histology: general characteristics, esophagus, stomach, small intestine (duodenum & jejunum) large intestine general characteristics
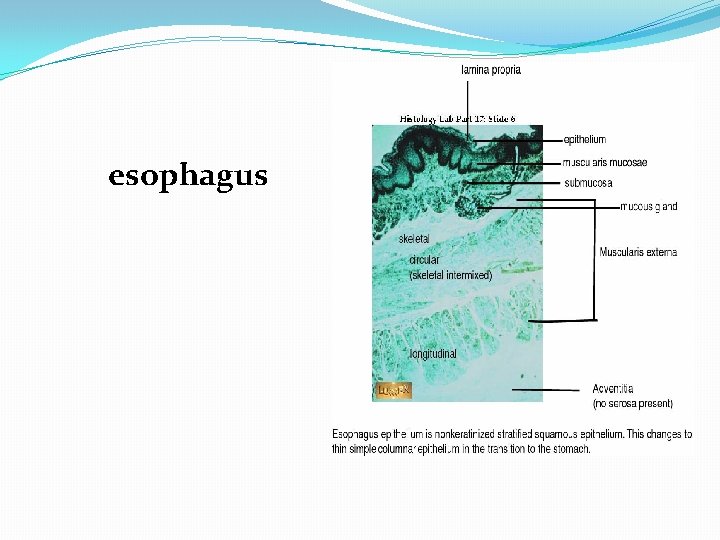
esophagus
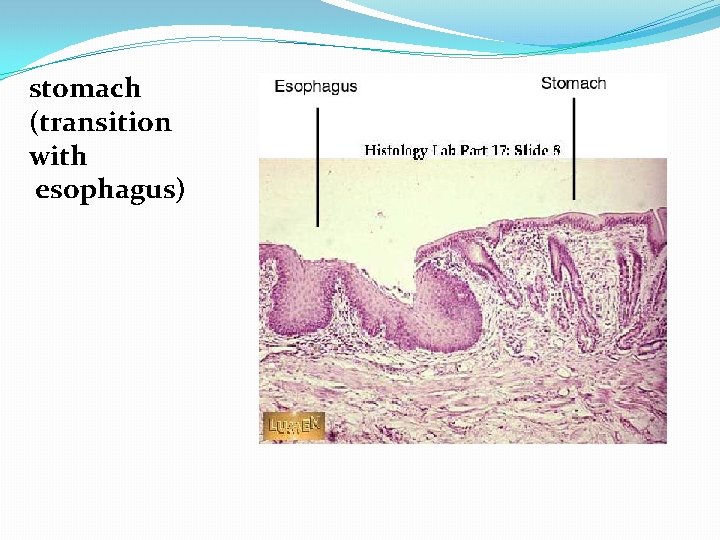
stomach (transition with esophagus)

Stomach Gastric acid (informally gastric juice), produced in the stomach plays a vital role in the digestive process, it mainly contains hydrochloric acid and sodium chloride. A peptide hormone gastrin produced by G cells in thegastric glands, stimulates the production of gastric juice which activates the digestive enzymes. Pepsinogen is a precursor enzyme (zymogen) produced by the gastric chief cells and gastric acid activates this to the enzyme pepsin which begins the digestion of proteins. As these two chemicals would damage the stomach wall, mucus is secreted by innumerable gastric glands in the stomach, to provide a slimy protective layer against the damaging effects of the chemicals. At the same time that protein is being digested, mechanical churning occurs through the action of peristalsis, waves of muscular contractions that move along the stomach wall
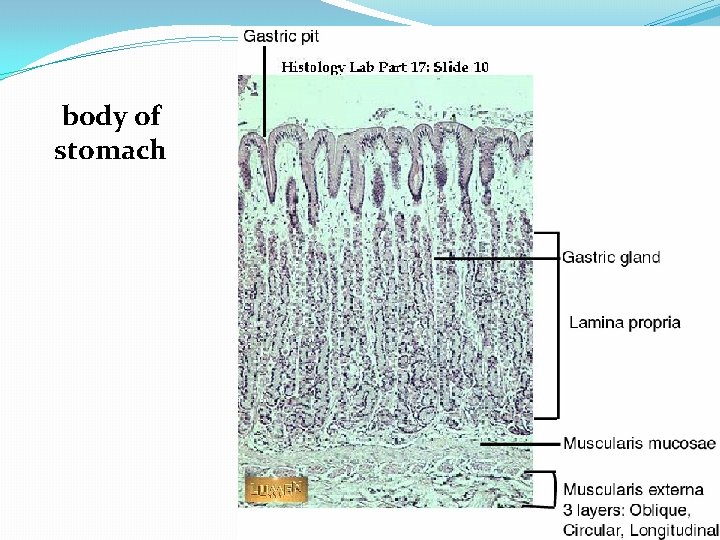
1. . Stomach (Cardia) • Mucosa contains simple or branched tubular cardiac glands • Terminal portion of these glands are frequently coiled, often with large lumens. • Similar in structure to cardiac glands of the terminal portion of esophagus. 2. . Stomach (Fundus & Body) • Simple columnar surface epithelium extends into gastric pits into which opens into gastric glands. • Lamina propria consist of fine reticular and collagen fibres fills the spaces between the packed gastric glands. • Each gastric gland has 3 distinct region: o Isthmus o Neck o Base • Isthmus contains differentiating mucous cells and undifferentiated stem cells and parietal cells. • Neck consist of stem, mucous neck and parietal cells. • Base contains parietal and chief (zymogenia) cells. • The muscularis mucosa composed of inner circular and outer longitudinal smooth muscle.
1. Stomach (Pylorus) • Deep gastric pits into which the branched tubular pyloric glands open. • The epithelium of the mucous membrane consist of tall columnar cells which lines the deep pits and short glands. • Longer pits and shorter coiled secretory portion compare to glands in cardiac region. • The acini of pyloric glands and their ducts are in lamina prorpia. • G (Gastrin) cells are enteroendocrine cells intercalated among mucous cells of pyloric glands. • D cells secrete Somatostatin • The muscularis externa is made up of thick circular muscle to form pyloric sphincter which helps to control emptying of the stomach.
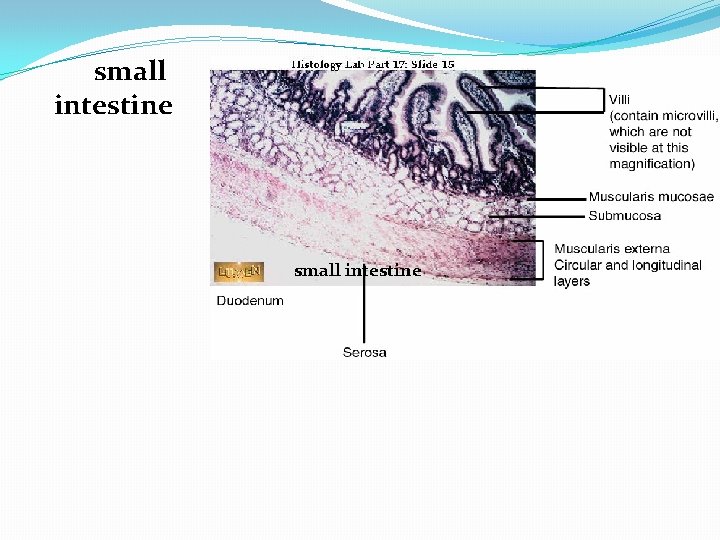
1. Small Intestine Duodenum Jejunum Ileum 2. . Small Intestine • 4 layers: 1. Mucosa 2. Submucosa 3. Muscularis externa 4. Serosa • Surface area of small intestine increased by 1. Length of small intestine 2. Valves of Kerkring/ Plica Circularis 3. Villi 4. Microvilli 5. Cypts Of Lieberkuhn 3. . Mucosa of Small Intestine 4. Valves of Kerkring • Also known as Plica Circulares • Permanent submucosal circular folds • Large, seen with naked eye • Prominent in duodenum & jejunum • Less marked in ileum • Significance: o Increases surface area o Slow down the passage of contents 5. . Villi • Central lacteal (lymphatic vessel) • Core capillaries • Core of connective tissue • Epithelial cells – Tall columnar with striated border
1. Crypt of Lieberkuhn (Intestinal gland) • Invaginations of lining epithelium into lamina propria • Wall of crypt is lined by the following cells: 1. Columnar cells 2. Goblet cells 3. Undifferentiated stem cells 4. Paneth / Zymogen cells 5. Argentaffin cells 2. . Crypt of Lieberkuhn • Absorptive columnar cells / Enterocytes o Microvilli which give it a striated border appearance • Goblet cells o Secretes mucus • Undifferenciated cells o Actively multiply, move upwards give rise to other cells 3. . Crypt of Lieberkuhn • Paneth cells / Zymogen cells o Seen in deeper parts of crypts o rich in Zinc, secrete lysozyme that destroys bacteria • Endocrine cells o Seen near lower ends of crypts
1. Submucosa of Small Intestine 2. . Brunner’s Gland • In duodenum (Also known as duodenal glands) • Clusters of ramified, coiled tubular glands that opens into the intestinal crypts. • Cells are mucous type. • Secretions are distinctly alkaline (PH 8. 1 – 9. 3), to protect duodenal mucous membrane from effects of acid gastric juice and to brings intestinal contents to optimum PH for pancreatic enzyme action.
1. Peyer’s Patches • Lymphoid Nodules. • Present in ileum, more prominent in terminal ileum. • In lamina propria and submucosa • Dome shaped area devoid of villi • Instead of absorptive cells, 2. . Differences between duodenum, jejunum & ileum Duodenum Jejunum Ileum Epithelium Columnar Striated border Few goblet cells Columnar Striated border goblet cells+ Columnar goblet cells++ Villi Broad Spatula Shaped Closely packed Tongueshaped Different heights Few thin finger- shaped Lamina Propria Crypts+ No Peyer’s patches Crypts+ Diffuse infiltration of lymphocytes No Peyer’s patches Crypts+ Peyer’s patches extend into submucosa Submucosa Mucus secreting Brunner’s glands Only connective tissues and blood vessels Peyer’s patches
This allows the mass of food to further mix with the digestive enzymes. Gastric lipase secreted by the chief cells in the fundic glands in the gastric mucosa of the stomach, is an acidic lipase, in contrast with the alkaline pancreatic lipase. This breaks down fats to some degree though is not as efficient as the pancreatic lipase. The pylorus, the lowest section of the stomach which attaches to the duodenum via the pyloric canal, contains countless glands which secrete digestive enzymes including gastrin. After an hour or two, a thick semi-liquid called chyme is produced. When the pyloric sphincter, or valve opens, chyme enters the duodenum where it mixes further with digestive enzymes from the pancreas, and then passes through the small intestine, where digestion continues. When the chyme is fully digested, it is absorbed into the blood. 95% of absorption of nutrients occurs in the small intestine. Water and minerals are reabsorbed back into the blood in the colon of the large intestine, where the environment is slightly acidic. Some vitamins, such as biotin and vitamin K produced by bacteria in the gut flora of the colon are also absorbed.
The parietal cells in the fundus of the stomach, produce a glycoprotein called intrinsic factor which is essential for the absorption of vitamin B 12. Vitamin B 12 (cobalamin), is carried to, and through the stomach, bound to a glycoprotein secreted by the salivary glands The stomach is a distensible organ and can normally expand to hold about one litre of food The stomach of a newborn baby will only be able to expand to retain about 30 ml.
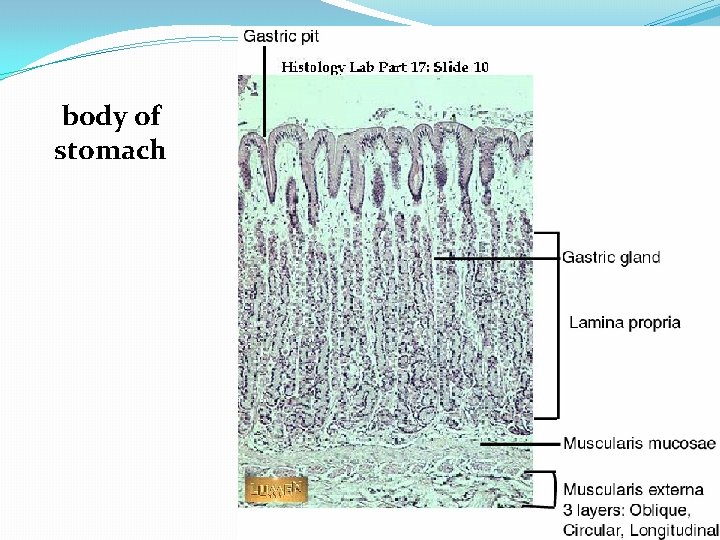
body of stomach
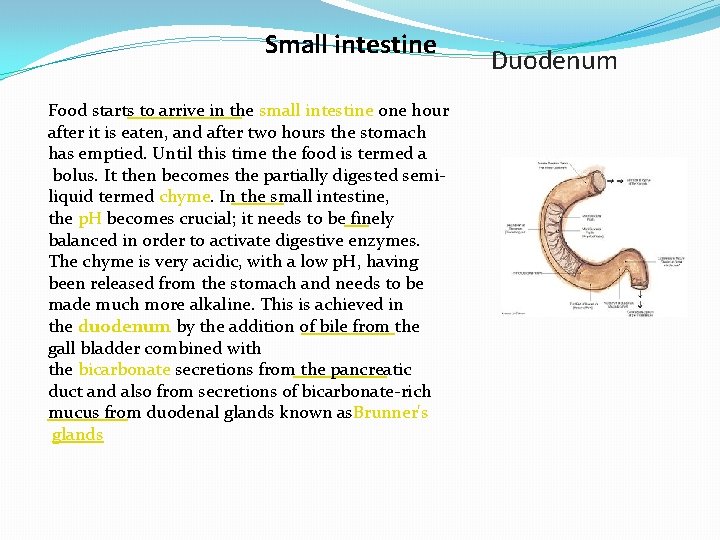
Small intestine Food starts to arrive in the small intestine one hour after it is eaten, and after two hours the stomach has emptied. Until this time the food is termed a bolus. It then becomes the partially digested semiliquid termed chyme. In the small intestine, the p. H becomes crucial; it needs to be finely balanced in order to activate digestive enzymes. The chyme is very acidic, with a low p. H, having been released from the stomach and needs to be made much more alkaline. This is achieved in the duodenum by the addition of bile from the gall bladder combined with the bicarbonate secretions from the pancreatic duct and also from secretions of bicarbonate-rich mucus from duodenal glands known as. Brunner's glands Duodenum
The chyme arrives in the intestines having been released from the stomach through the opening of the pyloric sphincter. The resulting alkaline fluid mix neutralises the gastric acid which would damage the lining of the intestine. The mucus component lubricates the walls of the intestine. When the digested food particles are reduced enough in size and composition, they can be absorbed by the intestinal wall and carried to the bloodstream. The first receptacle for this chyme is the duodenal bulb. From here it passes into the first of the three sections of the small intestine, the duodenum. (The next section is the jejunum and the third is the ileum). The duodenum is the first and shortest section of the small intestine. It is a hollow, jointed C-shaped tube connecting the stomach to the jejunum. .
Most food digestion takes place in the small intestine. In the duodenum, pancreatic lipase is secreted together with a coenzyme, colipase to further digest the fat content of the chyme. From this breakdown, smaller particles of emulsified fats called chylomicrons are produced. There also digestive cells called enterocytes lining the intestines (the majority being in the small intestine). They are unusual cells in that they have villi on their surface which in turn have innumerable microvilli on their surface. All these villi make for a greater surface area, not only for the absorption of chyme but also for its further digestion by large numbers of digestive enzymes present on the microvilli.
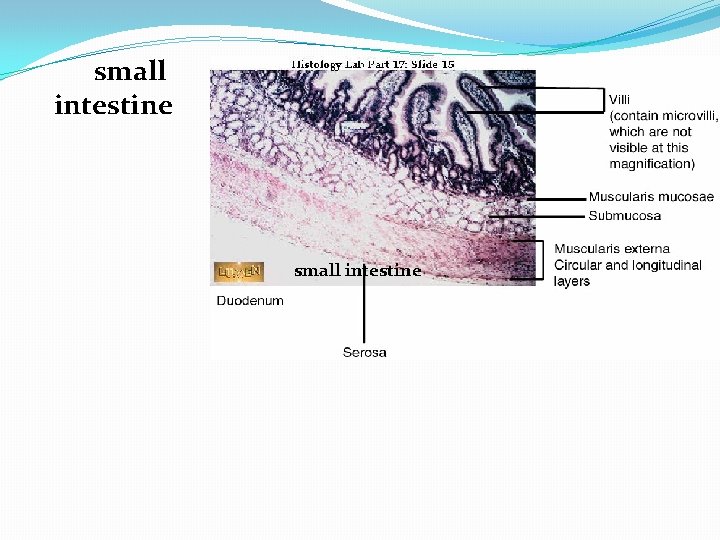
small intestine

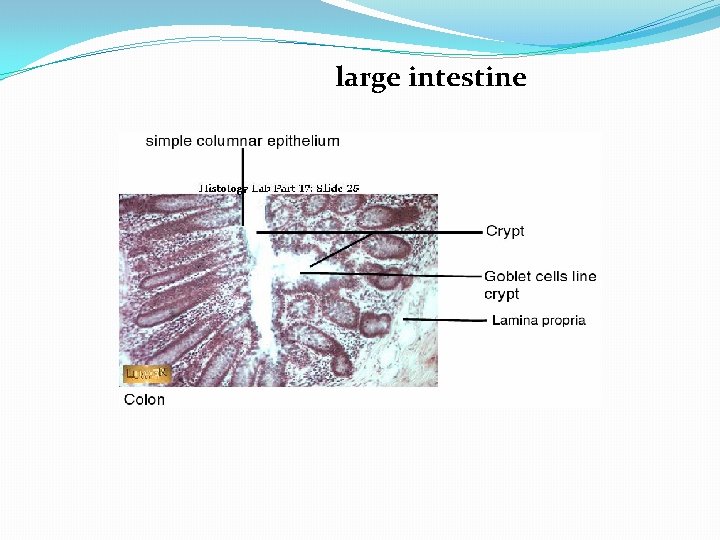
1. Large Intestine • Consists mucosal membrane with no folds except in its distal (rectal) portion. • No vili are present • Long intestinal glands • Great abundance of goblet and absorptive cells • Small number of enteroendocrine cells. • Fibers of outer longitudinal layer congregates in 3 thick longitudinal band (Teniae coli).
Large intestine In the large intestine, the passage of the digesting food in the colon is a lot slower, taking from 12 to 50 hours until it is removed by defecation. The colon mainly serves as a site for the fermentation of digestible matter by the gut flora. The time taken varies considerably between individuals. The remaining semisolid waste is termed faeces and is removed by the coordinated contractions of the intestinal walls, termed peristalsis, which propels the excreta forward to reach the rectum and exit via defecation from the anus. The wall has an outer layer of longitudinal muscles, thetaeniae coli, and an inner layer of circular muscles. The circular muscle keeps the material moving forward and also prevents any back flow of waste. Also of help in the action of peristalsis is the basal electrical rhythm that determines the frequency of contractions The taeniae coli can be seen and are responsible for the bulges (haustra) present in the colon. Most parts of the GI tract are covered with serous membranes and have a mesentery. Other more muscular parts are lined with adventitia
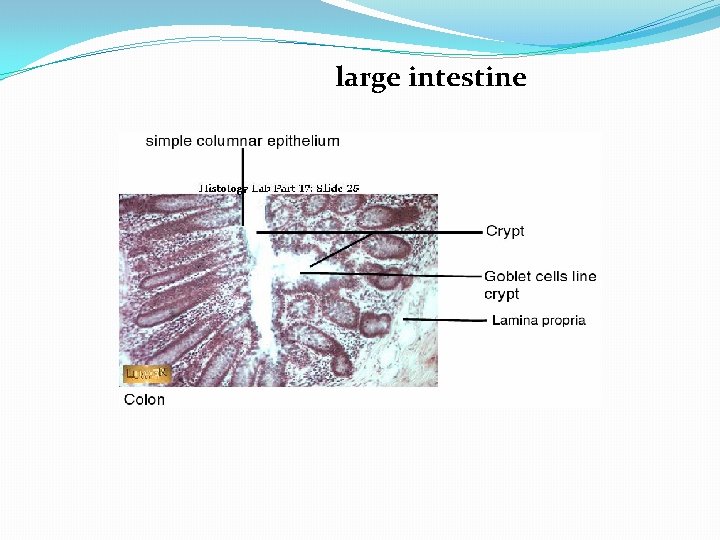
large intestine
1. Appendix • Evagination of cecum • Small, narrow and irregular lumen caused by presence of abundant lymphoid follicles in its wall. • Although general structure similar to large intestine, it contains fewer and shorter intestinal glands and has no teniae coli.
Thank You
 Figure 14-1 digestive system
Figure 14-1 digestive system Accessory organs of the digestive system
Accessory organs of the digestive system Digestive accessory organs
Digestive accessory organs 5 functions of the stomach
5 functions of the stomach Gastric pit
Gastric pit Internal organs
Internal organs Histology of accessory digestive organs
Histology of accessory digestive organs Respiratory system circulatory system digestive system
Respiratory system circulatory system digestive system Organs working together
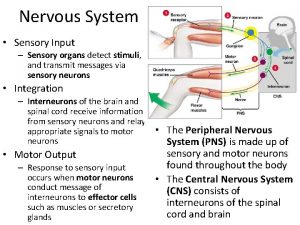
Organs working together Nervous system and digestive system
Nervous system and digestive system Sensory system organs
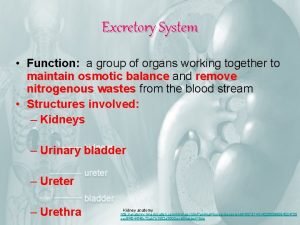
Sensory system organs What are the functions of excretory system
What are the functions of excretory system Lymphatic and urinary system
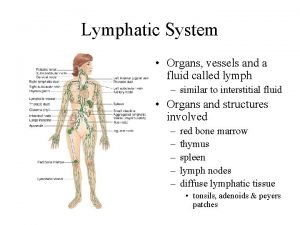
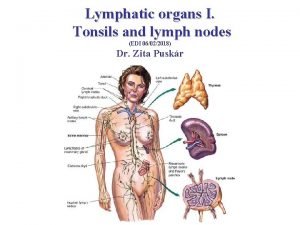
Lymphatic and urinary system Lymphatic system organs
Lymphatic system organs Tonsil
Tonsil Largest lymphoid organ
Largest lymphoid organ Organs of the sensory system
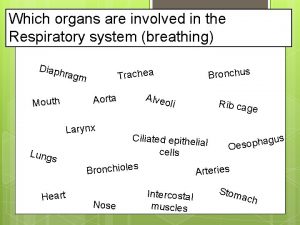
Organs of the sensory system Which organs are involved in respiratory system
Which organs are involved in respiratory system Chapter 13 respiratory system
Chapter 13 respiratory system Major endocrine glands male and female
Major endocrine glands male and female Hát kết hợp bộ gõ cơ thể
Hát kết hợp bộ gõ cơ thể Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Tư thế worms-breton
Tư thế worms-breton Hát lên người ơi
Hát lên người ơi Các môn thể thao bắt đầu bằng tiếng nhảy
Các môn thể thao bắt đầu bằng tiếng nhảy Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực Trời xanh đây là của chúng ta thể thơ
Trời xanh đây là của chúng ta thể thơ Cách giải mật thư tọa độ
Cách giải mật thư tọa độ 101012 bằng
101012 bằng độ dài liên kết
độ dài liên kết